Decoding Toxicity in Mouse Embryo Cryopreservation: Mechanisms, Mitigation, and Model Validation
Mouse embryo cryopreservation is a cornerstone of biomedical research, enabling the preservation of valuable genetically engineered models.
Decoding Toxicity in Mouse Embryo Cryopreservation: Mechanisms, Mitigation, and Model Validation
Abstract
Mouse embryo cryopreservation is a cornerstone of biomedical research, enabling the preservation of valuable genetically engineered models. However, the toxicity of cryoprotectant agents (CPAs) remains a significant challenge, potentially compromising embryo viability and developmental potential. This article provides a comprehensive analysis for researchers and scientists, covering the foundational mechanisms of CPA toxicity, current methodological approaches for its mitigation, practical strategies for protocol optimization, and essential validation techniques. By synthesizing the latest research, we aim to equip professionals with the knowledge to improve cryopreservation outcomes, ensuring the integrity and reproducibility of mouse models in drug development and basic science.
The Cellular Battlefield: Unraveling the Mechanisms of Cryoprotectant Toxicity
Cryoprotectant toxicity represents the foremost obstacle in cryopreservation, particularly for sensitive biological systems like mouse embryos where viability must be meticulously preserved for research and reproductive applications [1]. As cryoprotective agents (CPAs) are employed to eliminate lethal ice formation during cooling to cryogenic temperatures, their inherent toxicity limits the concentrations that can be safely used, creating a significant barrier to effective vitrification [1] [2]. This technical guide examines CPA toxicity through the critical dichotomy of specific versus non-specific damage pathways, with specific focus on implications for mouse embryo cryopreservation research.
Specific toxicity refers to damage mechanisms unique to particular CPA chemical structures and their direct interactions with cellular components [1]. In contrast, non-specific toxicity encompasses damage resulting from the fundamental properties of CPAs as solutes, primarily through their disruption of water's hydrogen bonding network and the consequent effects on cellular structures and functions [1] [2]. Understanding this distinction is paramount for developing strategies to neutralize CPA toxicity and advance cryopreservation protocols for mouse embryos and other complex biological systems.
Cryoprotectant-Specific Toxicities
Penetrating CPAs exhibit distinct toxicity profiles stemming from their unique chemical properties and biological interactions. These specific toxic mechanisms must be carefully considered when selecting CPAs for mouse embryo cryopreservation.
Table 1: Specific Toxicities of Common Penetrating Cryoprotectants
| Cryoprotectant | Specific Toxicities | Relevance to Mouse Embryos |
|---|---|---|
| Dimethyl sulfoxide (DMSO) | • Alters membrane channel protein function [1]• Causes myocardial cell shrinkage and action potential duration increase [1]• Induces DNA methylation and histone modification at concentrations >5% [3] | • Reduces developmental competence in mouse oocytes and embryos• Epigenetic modifications may affect gene expression |
| Ethylene glycol (EG) | • Metabolized to glycolic and oxalic acids causing metabolic acidosis [1]• Forms calcium oxalate crystals in tissues [1] | • Lower molecular weight may reduce osmotic stress• Often preferred for mouse oocyte/embryo vitrification |
| Propylene glycol (PG) | • Decreases intracellular pH at high concentrations (>2.5 M) [1]• Impairs developmental potential of mouse zygotes [1] | • pH disruption particularly detrimental to preimplantation embryos• Requires careful concentration control |
| Glycerol (GLY) | • Depletes reduced glutathione leading to oxidative stress [1]• Polymerizes actin cytoskeleton in spermatozoa [1] | • Cytoskeletal disruptions may impact embryonic cell divisions• Oxidative stress can compromise embryo development |
| Formamide (FMD) | • Denatures DNA through displacement of hydrating water [1]• Strong self-association with hydrogen bonding strength exceeding water [1] | • DNA structural damage poses risk to genetic integrity• Limited use in embryo preservation due to high toxicity |
| Methanol (METH) | • Metabolized to formaldehyde and formic acid [1]• Dose-dependent reduction in mitochondrial function measures [1] | • Mitochondrial dysfunction impairs embryonic energy production• Metabolite accumulation detrimental to development |
The specific toxicities outlined in Table 1 demonstrate that CPA selection for mouse embryo cryopreservation requires careful consideration of multiple factors beyond cryoprotective efficacy. For instance, while DMSO offers excellent membrane penetration, its potential for epigenetic modifications warrants caution in research applications where maintaining unaltered gene expression patterns is critical [3]. Similarly, the pH-altering effects of propylene glycol may be particularly detrimental to preimplantation stage mouse embryos, which exhibit sensitivity to intracellular pH fluctuations [1].
Non-Specific Toxicity Pathways
Non-specific CPA toxicity arises from fundamental physicochemical properties shared across cryoprotectant compounds, primarily mediated through their effects on water structure and solute concentration.
Mechanisms of Non-Specific Damage
The hydrogen-bonding characteristics of CPAs with water molecules represent a primary non-specific toxicity pathway. CPAs prevent ice formation by interfering with hydrogen bonding between water molecules, and this disruption of water's normal structure has been proposed as a fundamental mechanism of non-specific toxicity [1]. All CPAs function by displacing water molecules, creating concentrated solutions that dramatically reduce freezing points, but simultaneously generate substantial osmotic stress and potentially disrupt the hydration shells essential for macromolecular function [1] [2].
During freezing procedures, extracellular ice formation excludes solutes, progressively increasing extracellular solute concentration. This establishes osmotic gradients that drive water efflux from cells, resulting in cellular dehydration and elevated intracellular solute concentrations—a phenomenon known as "solution effects" [2]. The consequent macromolecular crowding can denature proteins, disrupt membrane integrity, and alter critical biochemical pathways [2]. This non-specific damage pathway affects all cell types, though sensitivity varies between biological systems.
Intracellular Ice Formation
When cooling rates exceed cellular dehydration capacity, intracellular ice formation (IIF) occurs, representing a particularly lethal non-specific damage pathway [2]. IIF directly damages intracellular structures including organelles, cytoskeletal elements, and membranes. Mouse embryos are especially vulnerable to IIF due to their large volume and surface area-to-volume ratio, which limits water efflux efficiency [2]. The presence of CPAs moderates but does not eliminate IIF risk, particularly during the thawing process where devitrification (ice crystallization during warming) can cause significant damage [4].
Quantitative Toxicity Assessment in Mouse Embryos
Evaluating CPA toxicity requires standardized assays and quantitative measures. For mouse embryo research, specific endpoints include developmental competence, membrane integrity, metabolic activity, and genetic integrity.
Table 2: Quantitative Toxicity Measures for CPAs in Mouse Embryos
| Toxicity Measure | Experimental Method | Typical Values for Mouse Embryos | Significance |
|---|---|---|---|
| Developmental Competence | Blastocyst formation rate post-thaw | • >70% for low-toxicity CPAs [1]• <30% for high-toxicity CPAs | Primary endpoint for embryo viability |
| Membrane Integrity | Fluorescent dye exclusion (propidium iodide) | • >80% intact for viable embryos [3] | Indicator of structural damage |
| Mitochondrial Function | ATP levels, ADP/ATP ratios, membrane potential [1] | • Dose-dependent reduction with methanol [1] | Metabolic competence indicator |
| Oxidative Stress | ROS detection assays, glutathione depletion [1] | • Glycerol depletes reduced glutathione [1] | Oxidative damage marker |
| Cytoskeletal Integrity | Immunofluorescence for actin, tubulin [1] | • Glycerol polymerizes actin at >1.5% [1] | Structural integrity assessment |
The quantitative measures in Table 2 provide researchers with standardized approaches for comparing CPA toxicity in mouse embryo models. Developmental competence remains the most biologically relevant endpoint, as it integrates multiple aspects of embryo health and function [1]. However, mechanistic insights gained from membrane integrity, mitochondrial function, oxidative stress, and cytoskeletal assessments are invaluable for understanding specific toxicity pathways and developing targeted mitigation strategies.
Experimental Protocols for Assessing CPA Toxicity
Concentration-Dependent Toxicity Screening
Objective: To determine the maximum tolerated concentration of individual CPAs for mouse zygotes and early embryos.
Methodology:
- Collect mouse zygotes or 2-cell embryos following standard superovulation protocols.
- Prepare CPA solutions in modified PBS with 0.5% BSA at concentrations ranging from 0.5 M to 8 M in 0.5 M increments.
- Expose embryos to each CPA concentration using a two-step addition method (0.5 M/min) at room temperature (25°C).
- Maintain exposure for 10 minutes, then remove CPAs using reverse two-step dilution.
- Culture embryos in KSOM medium at 37°C, 5% CO₂ for 96 hours.
- Assess development to morula and blastocyst stages at 72 and 96 hours, respectively [1] [5].
Critical Parameters:
- Maintain consistent temperature during CPA addition/removal to minimize osmotic shock
- Include carrier solution controls (0 M CPA) to establish baseline development rates
- Use ≥30 embryos per experimental group for statistical power
- Record morphological abnormalities during culture period
Time-Dependent Toxicity at Low Temperatures
Objective: To evaluate the effect of prolonged CPA exposure at low temperatures on mouse embryo viability.
Methodology:
- Prepare mouse morulae-stage embryos in control medium.
- Equilibrate with 60% M22 vitrification solution using stepwise addition (10%, 20%, 40%, 60%) at 10-minute intervals at 2°C.
- Maintain embryos in 60% M22 at 2°C for 0, 1, 2, 3, 4, and 8 hours (n=15-20 per time point).
- Remove CPAs using sequential 10-minute intervals to 30%, 15%, 7.5%, and 3.75% M22 using 300-600 mM mannitol in LM5 carrier solution at 2°C.
- Culture embryos in fresh KSOM medium at 37°C with 5% CO₂.
- Quantify blastocyst formation rates at 48 hours post-treatment [5].
Applications: This protocol determines safe exposure windows for vitrification procedures and identifies time-dependent toxicity thresholds critical for protocol optimization.
Time-Dependent Toxicity Workflow
Molecular Toxicity Pathway Analysis
Objective: To identify activation of specific stress response pathways in mouse embryos following CPA exposure.
Methodology:
- Expose mouse blastocysts to sublethal CPA concentrations (EC₇₀) for 10 minutes at 25°C.
- Fix immediately for immunocytochemistry or extract RNA/protein for molecular analysis.
- For oxidative stress assessment: Measure ROS production using Hâ‚‚DCFDA fluorescence, glutathione levels via monochlorobimane assay, and antioxidant gene expression (Sod1, Sod2, Gpx1, Cat) by RT-qPCR.
- For apoptosis pathway analysis: Assess caspase-3/7 activation using fluorescent substrates, TUNEL staining for DNA fragmentation, and Bax/Bcl-2 ratio by Western blot.
- For epigenetic effects: Examine DNA methylation patterns via bisulfite sequencing and histone modifications (H3K4me3, H3K27me3) by immunostaining after DMSO exposure [3].
- For cytoskeletal evaluation: Fix and stain for F-actin (phalloidin) and tubulin (anti-α-tubulin) to assess structural integrity.
Data Interpretation: Compare pathway activation across CPA types and concentrations to establish specific toxicity signatures and identify particularly detrimental compounds for mouse embryos.
Protective Strategies and Toxicity Mitigation
Hormesis and Preconditioning
Strategic preconditioning with sublethal stress can activate endogenous cellular defense mechanisms, significantly improving resistance to subsequent CPA exposure. In yeast, heat shock pretreatment increased survival by 18-fold after formamide exposure and over 9-fold after M22 exposure at 30°C [6]. Similar protection was observed in C. elegans, where hydrogen peroxide pretreatment conferred nearly complete protection from M22-induced damage [6]. This approach capitalizes on evolutionarily conserved stress response pathways that can be mobilized prior to cryopreservation procedures.
For mouse embryo applications, mild oxidative preconditioning with low-dose hydrogen peroxide or metabolic preconditioning with mild nutrient restriction may enhance endogenous antioxidant capacity and stress resistance pathways without inducing collateral damage [6]. The timing and intensity of preconditioning require empirical optimization for each embryo stage and CPA combination.
Genetic Modulation of Toxicity Resistance
Forward genetic screening in mouse embryonic stem cells (ESCs) has identified specific mutations conferring cryoprotectant toxicity resistance (CTR). Transposon-mediated mutagenesis revealed six independent biochemical pathways not previously linked to CPA toxicity, including genes Gm14005, Myh9, Pura, Fgd2, and Opa1 [5]. These CTR mutants demonstrated significantly improved survival after freezing and thawing in 10% DMSO, providing direct evidence that CT can be reduced in mammalian cells by specific molecular interventions [5].
While genetic manipulation of mouse embryos is not practical for routine cryopreservation, identification of protective genetic variants informs the development of small molecule interventions that can mimic these protective effects. Pharmacological activation of the MYC signaling pathway, identified in multiple CTR mutants, represents a promising approach for reducing CPA toxicity in mouse embryos [5].
Biomaterial-Based Protection
Hydrogel microencapsulation technology presents a promising strategy for reducing CPA toxicity by creating a physical barrier that moderates solute exchange and provides structural support. Alginate-based microencapsulation enables effective cryopreservation of mesenchymal stem cells with as low as 2.5% DMSO while maintaining cell viability above the 70% clinical threshold [7]. The hydrogel matrix moderates ice crystal formation and growth during thawing, reducing mechanical damage to delicate cellular structures [7].
For mouse embryos, which are substantially larger than single cells, complete encapsulation may not be feasible. However, modified approaches using alginate matrices to support embryos during CPA exposure and freezing may mitigate specific toxicity pathways by moderating osmotic shock and providing physical protection against ice crystal penetration.
CPA Toxicity Pathways and Protective Strategies
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for CPA Toxicity Studies in Mouse Embryos
| Reagent/Material | Function/Application | Example Use in Mouse Embryo Research |
|---|---|---|
| M22 Vitrification Solution | Multi-component vitrification solution for organs | Toxicity studies at reduced concentrations (e.g., 9-60%) [5] |
| LM5 Carrier Solution | Isotonic carrier for M22 containing electrolytes, sugars, and glutathione | Control solution and CPA diluent [5] |
| CELLBANKER Series | Commercial cryopreservation media with reduced toxicity | Serum-free formulations for standardized freezing [3] |
| Alginate Hydrogels | Biomaterial for cell encapsulation and toxicity reduction | Microencapsulation to reduce CPA concentration requirements [7] |
| MTT Assay Kit | Cell viability and metabolic activity assessment | Quantitative toxicity screening after CPA exposure [5] |
| Caspase-3/7 Apoptosis Assay | Detection of programmed cell death | Assessment of apoptosis pathway activation [3] |
| ROS Detection Probes (Hâ‚‚DCFDA, DHE) | Reactive oxygen species measurement | Oxidative stress evaluation after CPA exposure [1] |
| Anti-Stress Response Antibodies (HSP70, HSP90, Nrf2) | Stress pathway activation analysis | Molecular mechanism studies via immunocytochemistry/Western blot [6] |
| Lanuginosine | Lanuginosine, CAS:23740-25-2, MF:C18H11NO4, MW:305.3 g/mol | Chemical Reagent |
| Levophacetoperane | Levophacetoperane, CAS:24558-01-8, MF:C14H19NO2, MW:233.31 g/mol | Chemical Reagent |
The reagents and materials outlined in Table 3 represent essential tools for comprehensive CPA toxicity assessment in mouse embryo models. Commercial solutions like CELLBANKER provide standardized platforms for comparative studies, while specialized assays enable mechanistic investigations into specific toxicity pathways [3]. Emerging materials such as alginate hydrogels offer innovative approaches to physical protection and toxicity reduction [7].
The distinction between specific and non-specific cryoprotectant toxicity pathways provides a crucial framework for understanding and addressing the primary limitation in mouse embryo cryopreservation. Specific toxicities, arising from unique molecular interactions of individual CPAs, demand careful agent selection and exposure control. Non-specific toxicities, stemming from fundamental solute effects on cellular water and structures, require broader strategic interventions including optimized freezing protocols, biomaterial support, and activation of endogenous cellular defense mechanisms.
Future research directions should focus on the discovery of novel CPA compounds with reduced specific toxicity profiles, such as the heterocyclic amines 1-methylimidazole and pyridazine identified through computer-aided molecular design approaches [8]. Additionally, pharmacological manipulation of identified toxicity resistance pathways, particularly those involving MYC signaling and stress response elements, holds promise for clinical application [5]. Integration of advanced biomaterials that provide physical protection while moderating solute exchange may further reduce CPA requirements and associated toxicity [7].
For mouse embryo research specifically, standardized toxicity assessment protocols that account for stage-specific vulnerabilities will enhance cross-study comparisons and accelerate protocol optimization. By systematically addressing both specific and non-specific toxicity pathways through combined chemical, biological, and materials science approaches, researchers can overcome the critical barriers to efficient mouse embryo cryopreservation, thereby supporting advancements in reproductive science, genetic conservation, and biomedical research.
Cryoprotective agents (CPAs) are indispensable tools in assisted reproductive technologies, enabling the long-term preservation of gametes and embryos by mitigating the damaging effects of ice crystallization. However, the same chemicals that confer protection also introduce risks of specific and non-specific toxicity, which can compromise embryo viability, developmental potential, and even the long-term health of resulting offspring [9]. For researchers working with mouse models, understanding these toxicological profiles is paramount for designing ethical and effective cryopreservation protocols. Specific toxicity refers to direct chemical damage caused by the CPA's inherent properties, such as inducing oxidative stress, disrupting cellular structures, or altering epigenetic patterns [10]. In contrast, non-specific toxicity arises from physical changes in the solution, such as osmotic stress or alterations in the hydrogen bonding network surrounding biomolecules, which can lead to protein denaturation or membrane destabilization [10]. This technical guide provides a comprehensive comparative analysis of three predominant penetrating CPAs—dimethyl sulfoxide (DMSO), glycerol, and ethylene glycol (EG)—within the context of mouse embryo research, integrating quantitative toxicity data, molecular mechanisms, and practical protocol considerations to inform experimental design.
Physicochemical and Toxicological Profiles
The molecular characteristics of CPAs directly influence their permeability, distribution, and toxicological impact on embryonic cells. The table below summarizes key physicochemical and ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) parameters for DMSO, glycerol, and ethylene glycol, which are critical for predicting their behavior in cryopreservation solutions.
Table 1: Physicochemical and ADMET Properties of Common CPAs
| Property | DMSO | Glycerol | Ethylene Glycol |
|---|---|---|---|
| Molecular Weight (g/mol) | 78.13 | 92.09 | 62.07 |
| Melting Point (°C) | 18.5 | 18.2 | -12.9 |
| XLogP3 | -1.35 | -2.32 | -1.36 |
| Topological Polar Surface Area (Ų) | 36.8 | 60.7 | 40.5 |
| Caco2 Permeability (log Papp in 10â»â¶ cm/s) | 0.84 | -0.62 (Low) | Data Not Available |
| Volume of Distribution (log L/kg) | -0.04 | -1.04 | Data Not Available |
| Unbound Fraction in Plasma | 0.895 | 0.198 | Data Not Available |
| Tetrahymena pyriformis Toxicity (log µg/L) | -0.303 | -2.230 | Data Not Available |
Data adapted from a comprehensive overview of small-molecule CPA toxicities [9].
The physicochemical data reveals distinct differences. Glycerol's lower Caco2 permeability and higher polar surface area suggest slower cellular uptake compared to DMSO and EG [9]. This can influence the equilibration time required in cryopreservation protocols to prevent osmotic shock. DMSO exhibits a high unbound fraction in plasma, indicating minimal protein binding and potentially greater bioavailability within cells, which may contribute to its specific toxicity profile [9].
Mechanisms of Specific Toxicity
Each CPA exhibits unique mechanisms of specific toxicity that can impact embryonic development at the cellular and molecular level.
DMSO: This CPA poses significant epigenetic risks. Recent studies on vitrified bovine embryos demonstrate that DMSO induces active DNA demethylation by significantly increasing levels of 5-hydroxymethylcytosine (5hmC) while decreasing 5-methylcytosine (5mC) [11]. This effect is linked to the upregulation of the demethylase TET3. Furthermore, DMSO can induce major morphological and physiological alterations in developing vertebrate embryos, including heart edema, altered heart beating frequency, and somite size defects, as observed in zebrafish models [12]. Its mechanism of action also includes interaction with phospholipid membranes, causing membrane fluidization and, at higher concentrations, pore formation and bilayer disintegration [12].
Ethylene Glycol (EG): EG is generally considered less toxic than DMSO, but its potency is concentration-dependent. Research on mouse oocyte vitrification shows that high concentrations (≥20%) can cause cytotoxic and osmotic damage, reducing survival rates [13]. However, the minimal concentration required for effective vitrification can be optimized. A study found that combining 15% EG with 2% polyvinylpyrrolidone (PVP) significantly improved mouse oocyte survival rates post-warming without compromising embryonic development, highlighting the importance of concentration balancing [13].
Glycerol: As one of the oldest CPAs, glycerol has a long history of use. However, it exhibits lower cellular permeability, which can lead to delayed efflux during thawing and consequent osmotic swelling and damage if not carefully managed [9]. Its low volume of distribution indicates high water solubility or protein binding, meaning it predominantly remains in the seminal plasma or extracellular space, which can alter the physiological properties of the cellular environment [9].
Experimental Data and Protocols in Mouse Research
Quantitative Toxicity and Efficacy Endpoints
Data from mouse models provides critical thresholds for CPA toxicity. The following table summarizes key experimental findings on the effects of these CPAs on mouse embryos and oocytes.
Table 2: Experimental Toxicity and Efficacy Data from Mouse Studies
| CPA | Experimental Model | Concentration | Key Findings | Reference |
|---|---|---|---|---|
| DMSO | Mouse embryos (long-term) | Standard vitrification | Significant differences in morphophysiological and behavioral features in elderly subjects; delayed effects observed. | [14] |
| Ethylene Glycol (EG) | Mouse MII oocytes | 15-20% EG ± 2% PVP | 15% EG + 2% PVP significantly increased survival. Higher EG concentrations (20%+) showed no benefit and increased abnormality. | [13] |
| DMSO | Zebrafish embryos (as a model vertebrate) | 1-5% | Concentrations >5% were lethal. 1-4% induced tail curvature, heart edema, and reduced somite size. | [12] |
| Glycerol | General carnivore semen | Varies by extender | Lower permeability requires longer equilibration times; can alter seminal plasma physiology. | [9] |
Detailed Mouse Oocyte Vitrification Protocol
The following is a standard protocol for mouse oocyte vitrification, adapted from a study optimizing ethylene glycol concentrations [13]. This protocol exemplifies the practical application of CPAs and the critical steps for minimizing toxicity.
Source of Oocytes:
- Female mice (e.g., CD-1 strain, 8-10 weeks old) are superovulated with an intraperitoneal (IP) injection of 5 IU PMSG, followed by 5 IU hCG 48 hours later.
- Oocytes are collected from the oviducts 14 hours post-hCG injection. Cumulus-oocyte complexes (COCs) are released and denuded of cumulus cells using 75 U/mL hyaluronidase and mechanical pipetting.
- Only morphologically normal metaphase II (MII) oocytes, identified by the presence of a first polar body, are selected for vitrification.
Vitrification Procedure using JY Straw and EG-based Solutions:
- Equilibration: Denuded MII oocytes are suspended in an equilibration solution (ES) based on Dulbecco's Phosphate Buffered Saline (DPBS) for 3 minutes at room temperature. The ES contains a lower concentration of permeating CPAs.
- Vitrification Solution: Oocytes are transferred to a DPBS-based vitrification solution (VS) for 1 minute at room temperature. The VS contains the final, high concentration of CPAs. The specific optimized formulation from the study is 15% Ethylene Glycol combined with 2% Polyvinylpyrrolidone (PVP) [13].
- Loading and Cooling: Oocytes are immediately loaded onto a JY Straw and plunged directly into liquid nitrogen. The cooling rate with this system is approximately 442–500 °C/min.
Warning Procedure:
- Thawing: The loading part of the JY Straw is inserted directly into a DPBS-based thawing solution (TS) containing 1.0 M sucrose (a non-permeating CPA for osmotic control) at room temperature for 3 minutes. The warming rate is very high, approximately 2,210–2,652 °C/min.
- Sucrose Dilution: Oocytes are step-wise transferred to solutions containing 0.5 M and 0.25 M sucrose, for 3 minutes each, to gradually remove the permeating CPAs while minimizing osmotic shock.
- Washing: Oocytes are washed twice in a washing medium before transfer to a culture incubator (37°C, 5% CO₂) for further assessment.
Assessment of Survival and Development:
- Survival Rate: Assessed morphologically based on plasma membrane integrity and the appearance of the ooplasm shortly after warming.
- Embryonic Development: Survived oocytes can be parthenogenetically activated (e.g., with 8.5 mM strontium chloride) and cultured to the blastocyst stage to evaluate developmental competence.
- Cytoskeletal Integrity: Meiotic spindle and chromosome alignment are assessed using immunofluorescence staining after warming to ensure cytoskeletal preservation [13].
Advanced Concepts: Toxicity Modeling and Novel Strategies
Mathematical Modeling of CPA Toxicity
Given the vast landscape of possible CPA mixtures and protocol variables, mathematical models are invaluable for in silico optimization. A recent multi-CPA toxicity model accounts for both specific and non-specific toxicity, as well as intermolecular interactions between CPAs in solution [10]. The model is based on a toxicity cost function, k_tox, which represents the exponential decay rate of cell viability during CPA exposure. The general form of the model is:
k_tox = k_ns + k_s
Where:
k_nsrepresents the non-specific toxicity, a function of the overall solution properties.k_srepresents the specific toxicity, which is a sum of the contributions from individual CPAs and their synergistic or antagonistic interactions [10].
This model, trained on high-throughput toxicity data for five common CPAs (including DMSO, glycerol, EG, and propylene glycol), allows researchers to predict the toxicity of custom CPA mixtures without exhaustive experimental trial and error, facilitating the design of less toxic vitrification solutions [10].
Strategies for Toxicity Mitigation
Research has identified several effective strategies to counter CPA-specific toxicity:
Replacement and Combination: Using less toxic CPAs like propylene glycol (PG) instead of DMSO has been shown to prevent DNA demethylation in vitrified bovine embryos [11]. Furthermore, combining CPAs in balanced mixtures can exploit their individual advantages while minimizing the concentration—and thus the toxicity—of any single agent [10].
Antioxidant Supplementation: Adding antioxidants like N-acetyl-l-cysteine (NAC, 5 mM) to the vitrification medium containing DMSO has been demonstrated to ameliorate DMSO-induced DNA demethylation, bringing methylation levels in embryos closer to those of fresh controls [11].
Macromolecular Additives: Polymers such as polyvinylpyrrolidone (PVP) can replace a portion of the penetrating CPAs, thereby reducing the total osmotic and toxic load [15]. PVP increases the viscosity of the solution, which decreases the propensity for ice crystal formation and can have a stabilizing effect on the cell membrane [13].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for CPA Toxicity Research in Mouse Embryos
| Reagent / Solution | Function / Explanation |
|---|---|
| Dimethyl Sulfoxide (DMSO) | A penetrating CPA; effective but requires caution due to epigenetic toxicity and morphological alteration risks. |
| Ethylene Glycol (EG) | A penetrating CPA with lower toxicity at optimized concentrations; often used in combination with other agents. |
| Glycerol | A penetrating CPA with lower permeability; requires careful management of equilibration and dilution times. |
| Polyvinylpyrrolidone (PVP) | A non-permeating polymer; increases solution viscosity, reduces ice crystallization, and can lower required CPA concentrations. |
| Sucrose | A non-penetrating cryoprotectant; used in thawing and dilution solutions to create an osmotic gradient that controls CPA efflux and minimizes swelling. |
| N-Acetyl-L-Cysteine (NAC) | An antioxidant supplement; shown to counteract DMSO-induced oxidative stress and DNA demethylation. |
| JY Straw / Cryotop | Device for vitrification; enables high cooling and warming rates critical for survival. |
| Hyaluronidase | Enzyme for digesting cumulus cells to obtain denuded oocytes for consistent cryopreservation. |
| Indatraline | Indatraline, CAS:97229-15-7, MF:C16H15Cl2N, MW:292.2 g/mol |
| Ligustroflavone | Ligustroflavone, CAS:260413-62-5, MF:C33H40O18, MW:724.7 g/mol |
Visualizing Toxicity Pathways and Experimental Workflows
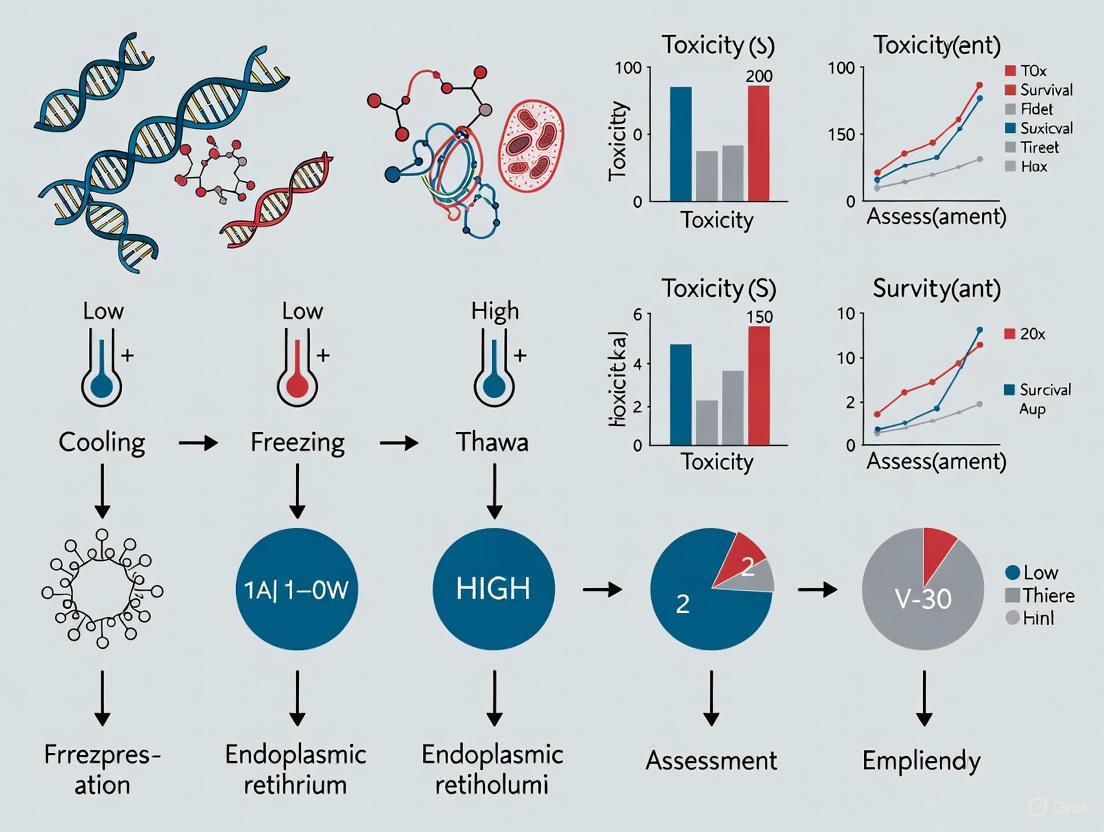
CPA Toxicity Pathways: This diagram outlines the primary mechanisms through which penetrating cryoprotectant agents (CPAs) exert specific and non-specific toxic effects on embryos, ultimately impacting their viability and developmental potential.
Mouse Oocyte Vitrification Workflow: This diagram illustrates the key steps in a standard mouse oocyte vitrification protocol, highlighting the stages of CPA exposure, rapid cooling/warming, and the crucial step-wise dilution process to remove CPAs post-warming.
Cryopreservation is an indispensable tool in biomedical research, particularly for the preservation of genetically engineered mouse lines, which represent significant scientific investments [16]. While this technology enables long-term storage of embryos at ultralow temperatures (typically -196°C), the freezing and thawing processes inevitably induce a spectrum of cellular and molecular injuries that can compromise embryo viability and developmental potential [14] [17]. These injuries extend beyond immediate cell death to include more subtle dysfunctions that may manifest at later developmental stages or even during senescence [14].
Understanding the precise nature of these injuries is crucial for developing safer, more effective cryopreservation protocols. This review synthesizes current knowledge on cryopreservation-induced damage in mouse embryos, with particular focus on membrane integrity, metabolic pathways, and mitochondrial function. We examine both immediate and delayed consequences of cryopreservation through the lens of molecular toxicology, providing researchers with a comprehensive framework for assessing and mitigating these injuries in experimental contexts.
Physical and Chemical Injuries During Cryopreservation
Membrane Damage and Permeability Alterations
The cell membrane constitutes the primary barrier against extracellular insults and serves as the initial site of cryoinjury. During freezing, membranes experience multiple stresses including osmotic shock, lipid phase transitions, and mechanical strain from ice crystals [17]. The fundamental mechanism of damage follows the "two-factor hypothesis" of freezing injury, which posits that cell survival depends critically on cooling rate [17].
At slow cooling rates, extracellular ice formation progressively concentrates solutes in the unfrozen fraction, creating osmotic gradients that draw water out of cells. This causes excessive cell shrinkage, potentially damaging the cytoskeleton and protein structures—a phenomenon termed "solution effect injury" [17]. Conversely, overly rapid cooling prevents adequate cellular dehydration, resulting in intracellular ice formation that mechanically disrupts membranes and organelles [17].
Table 1: Types of Membrane Damage During Cryopreservation
| Damage Type | Mechanism | Consequences |
|---|---|---|
| Solution Effect Injury | Extracellular ice formation increases solute concentration, causing osmotic water efflux | Cell shrinkage, cytoskeletal damage, protein denaturation |
| Intracellular Ice Formation | Rapid cooling prevents water efflux, leading to intracellular ice | Mechanical membrane rupture, organelle damage |
| Lipid Phase Transition | Temperature-dependent changes in membrane fluidity | Increased permeability, loss of compartmentalization |
| Osmotic Shock | Rapid water movement during CPA addition/removal | Membrane stretching or compression, transient pore formation |
Cryoprotectant Toxicity
Cryoprotectants (CPAs), while essential for mitigating ice formation, introduce their own toxicities. Traditional CPAs like dimethyl sulfoxide (DMSO) exhibit concentration-dependent and time-dependent toxicity [17] [18]. DMSO can induce cell apoptosis even at low concentrations and cause inappropriate differentiation in stem cells [17]. The molecular mechanisms of CPA toxicity include disruption of protein structure, alteration of membrane properties, and induction of oxidative stress [18].
Recent advances in CPA development focus on identifying less toxic alternatives. Natural osmolytes like betaine show promise as nontoxic CPAs that enable high post-thaw survival even with ultrarapid freezing protocols [19]. Similarly, synthetic polymers such as polyvinyl alcohol (PVA) and polyampholytes have demonstrated cryoprotective efficacy while minimizing toxicity [17].
Mitochondrial Dysfunction and Oxidative Stress
Mitochondrial Structural and Functional Impairments
Mitochondria play a pivotal role in cryopreservation injury as both targets and amplifiers of damage. These organelles are particularly vulnerable to cryoinjury due to their complex membrane systems and central role in cellular metabolism [20]. Studies across multiple cell types consistently demonstrate mitochondrial ultrastructural damage following cryopreservation, including vacuolization, reduced matrix density, and disruption of cristae architecture [21].
Functionally, these structural alterations manifest as decreased mitochondrial membrane potential (ΔΨm), impaired electron transport chain (ETC) activity, and reduced adenosine triphosphate (ATP) production [20] [21]. In goat sperm, cryopreservation significantly decreased levels of high-membrane potential mitochondria and ATP content, accompanied by substantial increases in reactive oxygen species (ROS) production [21]. Similar impairments likely occur in cryopreserved mouse embryos, compromising their developmental competence.
Oxidative Stress and Redox Imbalance
The intimate relationship between mitochondrial dysfunction and oxidative stress creates a self-perpetuating cycle of damage during cryopreservation [20]. Mitochondria are the primary intracellular source of ROS, with complexes I and III of the ETC being major production sites [20]. When mitochondrial ETC function is impaired, electron leakage increases, generating excessive superoxide ions (O₂•â») that are dismutated to hydrogen peroxide (Hâ‚‚Oâ‚‚) and other reactive species [20].
This ROS overproduction overwhelms cellular antioxidant defenses, creating a state of oxidative distress that damages proteins, lipids, and DNA [20]. Lipid peroxidation of mitochondrial membranes further compromises ETC function, establishing a vicious cycle of escalating damage. The mitochondrial genome is especially vulnerable due to its proximity to ROS generation sites and lack of histone protection [20].
Diagram 1: Oxidative Stress Pathway in Cryopreservation. This diagram illustrates the self-perpetuating cycle of mitochondrial damage and oxidative stress during freezing and thawing processes.
Metabolic Consequences and Energy Deficits
Disruption of Energy Metabolism
Cryopreservation induces profound disturbances in cellular energy metabolism that extend beyond immediate mitochondrial dysfunction. Metabolomic analyses of cryopreserved sperm reveal significant alterations in energy-related metabolites, including decreased levels of capric acid, creatine, and D-glucosamine-6-phosphate [21]. These changes reflect broad dysregulation of metabolic pathways essential for cellular function.
Key enzymatic activities in energy metabolism are particularly vulnerable to cryoinjury. Studies demonstrate considerable reduction in the activity of rate-limiting enzymes involved in fatty acid biosynthesis and β-oxidation, including acetyl-CoA carboxylase, fatty acid synthase, and carnitine palmitoyltransferase I [21]. This enzymatic impairment disrupts the coordinated metabolic processes required for normal embryo development.
Transcriptomic Alterations and Molecular Damage
Recent transcriptomic analyses provide comprehensive views of molecular damage induced by cryopreservation. In oyster D-larvae, cryopreservation significantly altered the expression of 611 genes compared to only 3 genes affected by cryoprotectant exposure alone [22]. The most significantly enriched gene ontology terms included "carbohydrate metabolic process," "integral component of membrane," and "chitin binding" [22].
These transcriptomic changes indicate that the freezing process itself, rather than CPA exposure, causes the most substantial molecular damage. Pathway analysis identified "neuroactive ligand-receptor interaction," "endocytosis," and "spliceosome" as the most enriched pathways, suggesting broad disruption of signaling, trafficking, and RNA processing mechanisms [22].
Table 2: Metabolic and Molecular Alterations Following Cryopreservation
| Affected System | Specific Alterations | Functional Consequences |
|---|---|---|
| Energy Metabolism | ↓ ATP content, ↓ metabolites (capric acid, creatine), ↓ β-oxidation enzymes | Energy deficit, reduced motility and developmental competence |
| Lipid Metabolism | Disrupted fatty acid biosynthesis and β-oxidation | Membrane synthesis impairment, alternative energy source depletion |
| Carbohydrate Metabolism | Altered carbohydrate metabolic processes | Glycolytic flux disruption, pentose phosphate pathway impairment |
| Gene Expression | 611 differentially expressed genes, spliceosome pathway alteration | Aberrant protein expression, disrupted cellular signaling |
| Antioxidant Systems | Downregulation of antioxidant metabolites (saikosaponin A, probucol) | Increased oxidative stress vulnerability |
Experimental Assessment Methodologies
Protocol for Evaluating Cryopreservation Injury in Mouse Embryos
Assessment of cryopreservation injuries requires integrated methodologies spanning structural, functional, and molecular analyses. The following protocol outlines key procedures for comprehensive evaluation:
Embryo Collection and Cryopreservation
- Superovulate 4-6 week old female mice using pregnant mare's serum gonadotropin (PMSG) followed by human chorionic gonadotropin (hCG) 48 hours later [16]
- Mate with proven male mice and collect embryos at appropriate developmental stage (typically 8-cell for mice) [16]
- Employ revised two-step freezing method: Equilibrate embryos in freezing medium (1.5 M glycerol in M2 medium, 1960-1980 mOsm) for 10 minutes [16]
- Cool from 0°C to -7°C at 1°C/minute, seed at -7°C, hold for 10 minutes, then cool to -30°C at 0.3°C/minute before plunging into liquid nitrogen [16]
- Thaw rapidly in 37°C water bath and remove CPAs in stepwise dilution [16]
Viability and Functional Assessment
- Evaluate membrane integrity using dye exclusion tests (trypan blue) or fluorescent markers (propidium iodide) [20]
- Assess developmental competence by in vitro culture to blastocyst stage with evaluation of blastocyst formation rates [16]
- Determine implantation potential by embryo transfer to pseudopregnant recipients [16]
Mitochondrial and Metabolic Analyses
- Measure mitochondrial membrane potential using JC-1 or TMRE fluorescent probes [20] [21]
- Quantify ATP content via luciferase-based assays [21]
- Assess ROS production with Hâ‚‚DCFDA or MitoSOX Red probes [20] [21]
- Conduct metabolomic profiling using LC-MS/MS to identify altered metabolic pathways [21]
Molecular and Transcriptomic Evaluation
- Perform RNA sequencing to identify differentially expressed genes [22]
- Validate key gene expression changes by quantitative RT-PCR [22]
- Analyze pathway enrichment using Gene Ontology and KEGG databases [22]
Diagram 2: Experimental Workflow for Assessing Cryoinjury. This workflow outlines the comprehensive evaluation of cryopreservation injuries from embryo collection through multi-parameter assessment.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Cryopreservation Injury
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Cryoprotectants | DMSO, glycerol, ethylene glycol, betaine [17] [19] | Ice formation inhibition, membrane stabilization |
| Membrane Integrity Probes | Propidium iodide, trypan blue, SYTOX Green | Viability assessment, membrane damage quantification |
| Mitochondrial Probes | JC-1, TMRE, MitoTracker, MitoSOX Red [20] [21] | Membrane potential measurement, ROS detection |
| Metabolic Assays | ATP luminescence kits, Seahorse XF Analyzer reagents | Energy status assessment, metabolic flux analysis |
| Antioxidants | N-acetylcysteine, glutathione, α-tocopherol | Oxidative stress mitigation, pathway analysis |
| Molecular Biology Kits | RNA extraction kits, cDNA synthesis kits, qPCR reagents [22] | Transcriptomic analysis, biomarker validation |
| Luffariellolide | Luffariellolide, CAS:111149-87-2, MF:C25H38O3, MW:386.6 g/mol | Chemical Reagent |
| Linetastine | Linetastine, CAS:159776-68-8, MF:C35H40N2O6, MW:584.7 g/mol | Chemical Reagent |
Mitigation Strategies and Future Directions
Advanced Cryoprotectant Formulations
Innovative CPA strategies focus on reducing toxicity while maintaining efficacy. Natural zwitterionic molecules like betaine show exceptional promise, enabling post-thaw survival efficiencies exceeding 90% with ultrarapid freezing protocols [19]. Betaine's mechanism involves strong water-binding capacity that depresses freezing point and regulates osmotic stress [19].
Macromolecular cryoprotectants represent another advancement. Polyampholytes—polymers containing both positive and negative charges—demonstrate remarkable ice inhibition properties while exhibiting minimal toxicity [17]. When combined with traditional CPAs, polyampholytes significantly enhance post-thaw recovery and minimize membrane damage [17].
Antioxidant and Metabolic Interventions
Given the central role of oxidative stress in cryoinjury, antioxidant supplementation presents a logical mitigation strategy. Supplementing freezing extenders with metabolites like capric acid (500 μM) significantly enhances motility of frozen-thawed sperm, indicating potential for similar applications in embryo preservation [21]. The targeted restoration of specific downregulated metabolites represents a precision medicine approach to cryopreservation injury.
Novel engineering strategies also show promise for mitigating cryoinjury. Photothermal and electromagnetic rewarming techniques enable more uniform heating rates, reducing devitrification and ice recrystallization [17]. Microencapsulation approaches provide physical protection during freezing and thawing, while synergistic ice inhibition strategies combine multiple protection mechanisms for enhanced efficacy [17].
Cryopreservation induces a complex cascade of cellular and molecular injuries in mouse embryos, spanning from initial membrane breaches to profound metabolic and mitochondrial dysfunction. These injuries are not random but follow specific pathophysiological pathways centered on osmotic stress, ice formation, and oxidative damage. The delayed consequences observed in senescent mice cryopreserved as embryos underscore that these injuries may have long-lasting implications beyond immediate survival [14].
Comprehensive assessment requires integrated methodologies evaluating structural integrity, functional competence, and molecular fidelity. Advanced transcriptomic and metabolomic approaches reveal that the freezing process itself, rather than CPA exposure, induces the most significant molecular damage [22]. Future directions should focus on targeted interventions that address specific injury mechanisms, particularly mitochondrial dysfunction and oxidative stress, while developing novel CPA formulations that balance ice inhibition with biological compatibility.
Understanding these injuries at fundamental levels enables more rational design of cryopreservation protocols, ultimately supporting the preservation of valuable genetic resources while minimizing unintended consequences that could confound experimental outcomes in mouse research.
Cryopreservation is an indispensable tool in biomedical research and assisted reproductive technologies, yet it imposes significant stress on living cells. A primary source of this stress is osmotic shock, the physical and chemical damage resulting from solute concentration imbalances and the resulting water flux across cell membranes during the freezing and thawing processes [23]. In the specific context of mouse embryo research, controlling osmotic shock is not merely a technical concern but a fundamental determinant of experimental success, influencing everything from immediate cell survival to long-term developmental potential [24] [25].
When an aqueous solution freezes, pure water crystallizes first, concentrating the dissolved solutes—salts, cryoprotectants (CPAs), and other molecules—in the remaining liquid phase. Cells suspended in this environment experience a sudden, dramatic increase in extracellular osmolality. This imbalance creates an osmotic gradient that drives water out of the cell, leading to potentially lethal cell shrinkage and solute toxicity [23]. The reverse process occurs during thawing; as extracellular ice melts and the environment becomes hypotonic relative to the dehydrated, CPA-loaded cell, water rushes in, causing uncontrolled swelling and risking cell lysis [26]. Understanding and mitigating these forces is critical for designing cryopreservation protocols that maximize the viability and fidelity of mouse embryos for research.
Core Principles and Quantifying Osmotic Stress
The Physical-Chemical Basis of Osmotic Shock
The journey of a cell through cryopreservation is a series of osmotic perturbations. The central challenge is summarized by Mazur's two-factor hypothesis, which posits that cell survival depends on finding a cooling rate that balances two competing injury mechanisms [23]. Excessively slow cooling permits extensive cellular dehydration, exposing the cell to high solute concentrations ("solution effects") and potential osmotic shock for prolonged periods. Excessively rapid cooling does not allow sufficient time for water to exit, resulting in intracellular ice formation (IIF), which is almost universally fatal [23].
The process of warming is equally critical. During the thawing of vitrified samples, there is a risk of devitrification, where ice crystals form as the temperature rises if warming is not sufficiently rapid [23]. Furthermore, ice recrystallization—the growth of larger ice crystals at the expense of smaller ones—can cause mechanical damage during the thawing phase [23]. The following diagram illustrates the damage pathways triggered by these imbalances.
Quantifying Osmotic Pressure in Embryonic Systems
Quantifying osmotic forces is essential for rational protocol design. Recent technological advances have enabled direct measurement of these parameters within living embryonic tissues. A 2023 study employed double emulsion droplet sensors to perform in situ quantification of osmotic pressure within early zebrafish embryos, a model system relevant to mammalian embryonic development [27].
These sensors consist of a biocompatible fluorocarbon oil shell surrounding an inner aqueous droplet containing a calibrated concentration of polyethylenglycol (PEG) osmolyte. The oil shell is permeable to water but not to solutes. When inserted into a cell or interstitial space, water moves across the shell until the osmotic pressure of the inner droplet matches that of its surroundings. By monitoring the resulting volume change of the inner droplet ((VI^E)), the local osmotic pressure ((Î E)) can be calculated using the equilibrium relationship [27]:
[ Î E = \frac{A}{VI^E - V_I^*} ]
Where (A) is a constant related to the inner droplet's osmolyte concentration and (V_I^*) is the osmotically inactive volume.
Using this technique, researchers measured an intracellular osmotic pressure of approximately 0.7 MPa in blastomeres of early zebrafish embryos, a value balanced by a similar interstitial pressure but creating a large pressure imbalance with the outside of the embryo [27]. The following table summarizes key quantitative findings and principles from osmotic stress research.
Table 1: Quantitative Data on Osmotic Stress in Biological Systems
| Parameter | Measured Value / Range | Biological Context | Significance |
|---|---|---|---|
| Intracellular Osmotic Pressure | ~0.7 MPa [27] | Blastomeres of early zebrafish embryos | Establishes baseline for physiological osmotic state; target for cryoprotectant solution design. |
| Physiological Osmolality Range | 255–295 mOsm/kg [28] | Human embryo culture media | Target osmolality for in vitro culture systems to minimize osmotic stress during non-frozen handling. |
| Osmolality Change in Dry Incubators | Significant increase from Day 1 to Day 7 (D7>D5>D3) [28] | Culture media in IVF lab conditions | Highlights importance of humidified incubators to prevent media evaporation and hyperosmotic stress. |
| Optimal Cooling Rate | Balance between slow (<1 °C/min) and fast (>100 °C/min) [23] | General cell cryopreservation (cell-type specific) | Governed by Mazur's two-factor hypothesis; must balance dehydration injury vs. intracellular ice formation. |
Experimental Methodologies for Analysis and Mitigation
Optimized Protocol: Two-Step CPA Loading for Mouse Oocytes
Directly addressing osmotic shock, a pivotal study developed and validated a mathematically optimized two-step method for loading dimethyl sulfoxide (Meâ‚‚SO) into mouse metaphase II (MII) oocytes [24]. This protocol was designed to minimize the combined damage from osmotic stress and CPA toxicity, outperforming conventional one-step loading.
Table 2: Key Reagent Solutions for Osmotic Stress Research
| Research Reagent / Tool | Function / Explanation |
|---|---|
| Double Emulsion Droplet Sensors [27] | Micro-osmometers for in situ quantification of osmotic pressure within individual cells and interstitial spaces of living embryonic tissues. |
| Hypotonic Diluents (e.g., hypo-PBS) [24] | Aqueous buffers with reduced salt concentration (~55 mOsmol/L); used to prepare CPA solutions to reduce osmotic shock during initial CPA exposure. |
| Non-Permeating CPAs (e.g., Sucrose, Trehalose) [23] [29] | High molecular weight solutes that remain extracellular; draw water out of cells osmotically, promoting protective dehydration and reducing required concentrations of toxic permeating CPAs. |
| Permeating CPAs (e.g., DMSO, EG, PROH) [23] [24] | Small molecules that cross the cell membrane; displace water to inhibit intracellular ice formation but introduce risks of chemical toxicity and osmotic shock. |
| Polyvinyl Alcohol (PVA) / Paraffin Oil [27] [28] | Used in droplet microfluidics and as an overlay for culture media; paraffin oil is superior to mineral oil in reducing media evaporation and osmolality shifts in dry incubators. |
Materials
- Mouse MII oocytes
- Isotonic Ca²âº/Mg²âº-free PBS supplemented with 4 mg/mL BSA
- Dimethyl sulfoxide (Meâ‚‚SO)
- Hypotonic diluent ("hypo-PBS"): Ca²âº/Mg²âº-free PBS diluted to ~55 mOsmol/L, with 10% (v/v) FBS
- Culture medium (e.g., Hypermedium with BSA and gentamycin)
Procedure
- Preparation: Prepare the two loading solutions using the hypotonic diluent.
- Solution A: 0.75 M Meâ‚‚SO in hypo-PBS.
- Solution B: 1.50 M Meâ‚‚SO in hypo-PBS.
- Step 1 - Equilibration: Transfer oocytes to Solution A (0.75 M Me₂SO) for a calculated, optimized duration (e.g., 2-3 minutes) at 23°C or 30°C. This step introduces CPA gradually, minimizing initial water efflux and cell shrinkage.
- Step 2 - Final Loading: After the optimized time, directly transfer oocytes to Solution B (1.50 M Meâ‚‚SO) for a second defined period. The cells are now partially equilibrated, reducing the osmotic differential and the associated stress of the final concentration jump.
- Vitrification: After completing the loading steps, proceed with standard vitrification protocols (ultra-rapid cooling in liquid nitrogen).
- Warming and Removal: For warming, use a multi-step dilution process in decreasing concentrations of Meâ‚‚SO (e.g., 1.0 M, 0.5 M) supplemented with 0.25 M sucrose. The non-permeating sucrose in these solutions acts as an osmotic buffer, preventing a massive, rapid influx of water and controlling rehydration to avoid swelling and lysis [24].
Validation In the foundational study, this optimized two-step protocol resulted in significantly higher rates of fertilization (85% vs. 34%) and embryonic development (87% vs. 60%) compared to conventional one-step loading of 1.5 M Meâ‚‚SO [24]. Subsequent experiments decoupled the factors of shrinkage and Meâ‚‚SO exposure, concluding that the damage from one-step loading results from a synergistic interaction between osmotic stress and CPA toxicity, both of which are mitigated by the optimized protocol.
Workflow for Osmotic Pressure Measurement in Embryos
The following diagram outlines the experimental workflow for using double emulsion droplets to measure osmotic pressure within living embryonic tissues, providing a direct method to quantify the central factor of this review.
Advanced Concepts and Future Directions
Novel Warming Techniques and Osmotic Considerations
The principle of minimizing osmotic shock is also being applied to the warming phase. Recent clinical research has investigated one-step warming protocols for vitrified blastocysts. This approach involves rehydrating embryos in a single solution of 1M sucrose for one minute, a significant simplification over traditional multi-step methods that use decreasing sucrose concentrations [29]. This protocol, which reduces procedure time by over 90%, leverages a high, sustained osmotic buffer (sucrose) to control water influx while rapidly removing CPAs. Studies report comparable survival, clinical pregnancy, and ongoing pregnancy rates to multi-step warming, suggesting it is a viable, efficient protocol that adequately manages osmotic stress during thawing [29].
Induced Cellular Tolerance and the Role of Apoptosis
Beyond physical protocol optimization, research is exploring biological interventions to enhance cellular resilience. One promising avenue is hormesis, where a mild, sublethal stress preconditions cells, making them more resistant to a subsequent, more severe stress. For example, pretreating yeast or nematodes with heat shock or hydrogen peroxide conferred significant protection against the toxicity of high concentrations of vitrification solutions [6]. This concept suggests that mobilizing endogenous cellular defense pathways could be a powerful strategy to mitigate the combined osmotic and chemical stress of cryopreservation.
Furthermore, the freezing process is known to trigger apoptotic pathways in oocytes and embryos [25]. Comparisons between frozen and non-frozen samples show alterations in the expression of key apoptotic regulators like Bcl-2 and Bax. This indicates that osmotic and other cryo-stresses are perceived by the cell at a fundamental level, activating programmed cell death. Therefore, the integration of apoptotic inhibitors into cryopreservation protocols represents a forward-looking strategy to improve survival rates by addressing the downstream cellular response to osmotic shock [25].
In mouse embryo research, cryopreservation is a pivotal technique for preserving genetic resources and managing reproductive cohorts in preclinical studies. While traditional focus has centered on preventing ice crystal formation, contemporary research reveals that cryodamage extends far beyond physical ice effects. Chilling injury and oxidative stress constitute two interconnected mechanistic pathways that significantly compromise embryo viability during freezing and thawing processes. This technical guide examines the sophisticated cellular and molecular mechanisms underlying these damage pathways, providing researchers with current experimental data and methodologies relevant to mouse model systems. Understanding these intricate processes is fundamental for developing targeted strategies to mitigate cryopreservation toxicity and enhance experimental reproducibility in pharmaceutical and basic research applications.
The Dual Assault: Chilling Injury and Oxidative Stress
Chilling Injury: A Cold-Activated Signaling Cascade
Chilling injury occurs at temperatures above the freezing point (typically 0-15°C) and represents a biologically active process rather than passive physical damage. Recent research on zebrafish oocytes, a valuable model for understanding cold sensitivity, has illuminated a mechanosensitive pathway where TRPA1 (Transient Receptor Potential Ankyrin 1) channels act as primary cold sensors [30].
The diagram below illustrates this cold-induced signaling cascade that leads to cell death:
This signaling cascade culminates in significant membrane damage and cell death. Experimental data demonstrates that TRPA1 inhibition with AP-18 dramatically improves oocyte survival from 9% to 70% after chilling at 0°C for 15 minutes, strongly implicating this specific pathway in cold-induced damage [30].
Oxidative Stress: The Free Radical Cascade
Concurrently with chilling injury, cryopreservation induces substantial oxidative stress through massive generation of reactive oxygen species (ROS). The freezing and thawing processes disrupt mitochondrial electron transport, leading to electron leakage and superoxide formation [31] [32]. Multiple factors exacerbate ROS production during cryopreservation, including cryoprotectant toxicity, temperature fluctuations, and exposure to ambient oxygen [31].
Table 1: Reactive Oxygen Species (ROS) and Their Cellular Impacts
| ROS Type | Chemical Formula | Half-Life | Primary Cellular Targets | Neutralizing Enzymes |
|---|---|---|---|---|
| Superoxide Radical | O₂•⻠| Short (milliseconds) | Mitochondrial complexes, Iron-sulfur proteins | Superoxide Dismutase (SOD) |
| Hydrogen Peroxide | Hâ‚‚Oâ‚‚ | Longer (minutes) | Thiol groups, Transcription factors | Catalase, Glutathione Peroxidase |
| Hydroxyl Radical | •OH | Extremely short (microseconds) | DNA, Proteins, Membrane lipids | None known (most damaging) |
The hydroxyl radical is particularly destructive due to the absence of known enzymatic neutralizing systems, enabling it to cause widespread damage to DNA, proteins, and lipid membranes [31] [32]. This oxidative assault activates several downstream damage pathways in mouse embryos.
Quantifiable Damage and Functional Consequences
Structural and Functional Compromises
The combined effects of chilling injury and oxidative stress manifest through multiple quantifiable damage parameters in mouse embryos and oocytes:
Table 2: Experimentally Measured Cryodamage in Mouse Models
| Damage Parameter | Experimental Measurement | Impact on Development | Reference Model |
|---|---|---|---|
| Blastocyst Formation Rate | Decrease from 27.8% to 20% | Reduced implantation potential | Mouse GV oocytes [32] |
| Mitochondrial Membrane Potential | Significant decrease post-thaw | Compromised ATP production | Vitrified mouse oocytes [33] |
| DNA Damage | Increased γH2AX foci, strand breaks | Genomic instability, apoptosis | Vitrified mouse blastocysts [34] |
| Reactive Oxygen Species | 2-3 fold increase in ROS levels | Oxidative damage to cellular components | Vitrified mouse oocytes/embryos [33] [34] |
| Cell Number in Blastocysts | Significant reduction | Altered fetal programming | Vitrified mouse embryos [34] |
Epigenetic and Transcriptional Alterations
Beyond immediate structural damage, vitrification induces long-term developmental consequences through epigenetic modifications. Recent research demonstrates that vitrified mouse blastocysts exhibit altered histone modifications, including elevated H3K4me2/3, H4K12ac, and H4K16ac levels, alongside reduced m6A RNA methylation [34]. These changes correlate with significant transcriptome alterations in E18.5 placentas and fetal brains, potentially explaining the reduced live pup rates observed following transfer of vitrified-warmed embryos [34].
The Interplay: How Chilling Injury Amplifies Oxidative Stress
The relationship between chilling injury and oxidative stress is not merely additive but synergistically destructive. The diagram below illustrates how these pathways interconnect to amplify damage:
This interconnected network creates feed-forward loops where calcium dysregulation disrupts mitochondrial function, generating additional ROS that further activate TRP channels and cPLA2α, perpetuating the damage cycle [31] [30] [32].
Experimental Models and Assessment Methodologies
Standardized Viability Assessment Protocols
Researchers have established rigorous experimental approaches for quantifying cryodamage in mouse models:
Oocyte Viability Staining Protocol (from zebrafish oocyte studies applicable to mammalian systems):
- Post-thaw incubation at 25°C for 2 hours
- Staining with propidium iodide (20 µg/mL) for 10 minutes
- Fluorescence examination using U-MWIG2 filter (520-550 nm excitation/580 nm emission)
- Viability determination: dead oocytes emit reddish-white fluorescence; live oocytes exclude dye [30]
Comprehensive Embryo Assessment (mouse model):
- ROS measurement: 10µM DCFH-DA incubation at 37°C for 30 minutes
- Mitochondrial membrane potential: JC-1 staining following manufacturer protocols
- Mitochondrial activity: 500nM MitoTracker Red CMXRos incubation at 37°C for 30 minutes
- DNA damage assessment: γH2AX immunofluorescence and COMET assays [34]
Antioxidant Intervention Studies
Multiple studies have systematically evaluated antioxidant strategies for mitigating oxidative damage:
Table 3: Experimentally Validated Antioxidant Interventions
| Antioxidant | Concentration | Protective Mechanism | Experimental Outcome |
|---|---|---|---|
| Imperatorin | 40 µM | Reduces ROS, increases GSH, improves mitochondrial function | Enhanced fertilization rate, reduced apoptosis in mouse oocytes [33] |
| Melatonin | 10â»Â¹â° M | Scavenges ROS, preserves mitochondrial function, reduces Ca²⺠| Increased inner cell mass, trophectoderm, and total cell count in blastocysts [35] |
| Astaxanthin | Varies by system | Membrane-associated antioxidant, upregulates SOD and catalase | Improved post-thaw sperm motility, oocyte quality across species [36] |
| N-acetylcysteine | 1 µM | Precursor to glutathione, direct ROS scavenging | Reduced ROS accumulation in vitrified mouse embryos [34] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Investigating Cryopreservation Damage Mechanisms
| Reagent Category | Specific Examples | Research Application | Mechanistic Target |
|---|---|---|---|
| TRP Channel Inhibitors | AP-18 (300 µM), Ruthenium Red | Chilling injury pathway dissection | TRPA1 cold-sensing channels [30] |
| Lipid Signaling Inhibitors | Pyrrophenone (cPLA2α), Indomethacin (COX), Zileuton (ALOX5) | Lipid mediator pathway analysis | Eicosanoid synthesis pathways [30] |
| Mitochondrial Probes | MitoTracker Red CMXRos, JC-1, TMRE | Mitochondrial function assessment | Membrane potential, distribution [33] [34] |
| ROS Detection Reagents | DCFH-DA, MitoSOX Red | Oxidative stress quantification | General ROS, mitochondrial superoxide [33] [34] |
| Exogenous Antioxidants | Melatonin, Imperatorin, Astaxanthin, N-acetylcysteine | Intervention studies | Direct ROS scavenging, endogenous antioxidant upregulation [33] [35] [36] |
| DNA Damage Markers | γH2AX antibodies, COMET assay kits | Genotoxicity assessment | DNA strand breaks, repair activation [34] |
| Apoptosis Detectors | Annexin V, TUNEL assay, Caspase inhibitors | Cell death pathway analysis | Phosphatidylserine exposure, DNA fragmentation [34] |
| Lysine hydroxamate | Lysine hydroxamate, CAS:25125-92-2, MF:C6H15N3O2, MW:161.20 g/mol | Chemical Reagent | Bench Chemicals |
| (+)-Magnoflorine | Magnoflorine | Research-grade Magnoflorine, a natural aporphine alkaloid. Explore its applications in neuroinflammation, metabolism, and OA studies. For Research Use Only. Not for human use. | Bench Chemicals |
Chilling injury and oxidative stress represent sophisticated biological response pathways that extend far beyond the physical damage of ice crystal formation in mouse embryo cryopreservation. The mechanistic understanding of TRPA1-initiated signaling cascades and mitochondrial ROS generation provides researchers with specific molecular targets for intervention. The experimental methodologies and reagent toolkit presented here offer practical approaches for investigating and mitigating these damage pathways. As cryopreservation continues to be essential for managing mouse research colonies and preserving valuable genetic resources, addressing these interconnected toxicity mechanisms will be crucial for enhancing experimental reproducibility and supporting rigorous scientific discovery in pharmaceutical development and basic research.
From Theory to Practice: Implementing Low-Toxicity Cryopreservation Protocols
For researchers investigating embryo cryopreservation toxicity in mouse models, selecting the optimal cryopreservation method is paramount to experimental validity and translational relevance. The debate between conventional slow freezing and newer vitrification techniques encompasses critical considerations of cellular survival, functional integrity, and potential cryoinjury—each method presenting distinct advantages and challenges for reproductive biology research. This technical analysis synthesizes current evidence to guide scientists in selecting the most appropriate methodology based on specific research endpoints, from basic morphological preservation to complex physiological functionality and long-term developmental outcomes.
Core Principles and Mechanisms of Action
Slow Freezing: Controlled-Rate Cryopreservation
Slow freezing operates on the principle of equilibrium freezing, characterized by a gradual, controlled cooling process that typically ranges from -0.3°C/min to -0.5°C/min [37] [38]. This method employs relatively low concentrations of cryoprotective agents (CPAs)—usually between 1.0-1.5 mol/L—such as propanediol, glycerol, or dimethyl sulfoxide (DMSO) [38]. The gradual cooling process allows for controlled dehydration of cells, as water migrates out of the cell before freezing extracellularly. This minimizes the formation of intracellular ice crystals, which are mechanically destructive to cellular structures [37]. However, the unavoidable extracellular ice formation can potentially cause structural damage to the stromal matrix and disrupt cell-to-cell connections [39]. The process requires specialized, expensive programmable freezing equipment and is more time-consuming than vitrification, but benefits from using lower, potentially less toxic concentrations of CPAs [37] [38].
Vitrification: Ultra-Rapid Glass Transition
Vitrification represents a non-equilibrium approach that completely avoids ice crystal formation through ultra-rapid cooling rates (as high as -20,000°C/min) and high CPA concentrations (ranging from 4-8 mol/L) [37] [38]. This technique converts the liquid cell solution directly into a glass-like amorphous solid without undergoing crystalline formation [40]. The process typically employs a combination of permeating CPAs like ethylene glycol (EG) and DMSO, often supplemented with non-permeating agents such as sucrose and macromolecules like Ficoll [41] [42]. The extremely rapid cooling prevents water molecules from organizing into ice crystals, instead immobilizing them in a vitreous state [37]. While vitrification eliminates mechanical damage from ice formation, it introduces potential chemical toxicity and osmotic stress due to high CPA concentrations [41]. The technique requires minimal equipment but demands significant technical skill for proper execution [37].
Table 1: Fundamental Principles of Cryopreservation Methods
| Parameter | Slow Freezing | Vitrification |
|---|---|---|
| Physical Principle | Equilibrium freezing | Non-equilibrium solidification |
| Cooling Rate | Slow (≈ -0.3°C/min) | Ultra-rapid (up to -20,000°C/min) |
| CPA Concentration | Low (1.0-1.5 mol/L) | High (4-8 mol/L) |
| Ice Formation | Extracellular only | None |
| Primary Equipment | Programmable freezer | Cryocarriers (loops, straws) |
| Technical Skill Required | Moderate | High |
| Process Duration | Several hours | Minutes |
Comparative Performance Analysis in Research Models
Cellular Survival and Morphological Integrity
Multiple studies across different biological systems demonstrate consistently higher immediate post-thaw survival rates with vitrification compared to slow freezing. In human cleavage-stage embryos, vitrification achieved a remarkable 96.9% survival rate versus 82.8% with slow freezing [38]. Morphological integrity followed a similar pattern, with 91.8% of vitrified embryos showing excellent morphology with all blastomeres intact compared to only 56.2% in the slow-frozen group [38].
Research on mouse embryo-derived inner cell mass (ICM) cells revealed that vitrification protocols yielded 100% survival rates (78/78) with 95% attachment capability to feeder layers post-warming, comparable to non-vitrified controls [42]. These vitrified ICM cells maintained expression of critical stem cell markers including SSEA-1, Sox-2, and Oct-4, confirming preservation of pluripotent characteristics [42].
In ovarian tissue cryopreservation, a meta-analysis of 19 studies found significantly better preservation of stromal cell integrity with vitrification, though primordial follicle preservation showed no significant difference between methods [37]. This suggests that vitrification may offer particular advantages for complex tissue architectures where stromal support is crucial for subsequent function.
Functional Recovery and Angiogenic Potential
Functional recovery after transplantation represents a critical endpoint for evaluating cryopreservation efficacy. In heterotopic transplantation of human ovarian tissue to nude mice, vitrification demonstrated superior recovery of endocrine function, with significantly higher estradiol levels at 6 weeks post-transplantation compared to slow-frozen tissue [39]. The proportion of normal follicles was also higher in vitrified tissue at both 4 and 6 weeks post-transplantation [39].
Angiogenic potential—a crucial factor for graft survival—showed no significant differences between vitrification and slow freezing in human ovarian tissue cultured under hypoxic conditions [40]. Analysis of ten angiogenic factors including VEGF, angiogenin, and hepatocyte growth factor revealed comparable expression profiles between the two methods, suggesting both adequately preserve this critical functional aspect [40].
In Vivo Development and Offspring Outcomes
Mouse model research provides valuable insights into the long-term developmental consequences of different cryopreservation methods. One comprehensive study comparing vitrification and slow freezing found no significant differences in postnatal physiology, spatial learning capabilities, or cerebral development parameters in resulting offspring [41]. Expression and distribution of brain development-related proteins GFAP and MBP showed comparable patterns across all groups [41].
However, researchers noted that offspring from both cryopreservation groups demonstrated higher body weights at 8 weeks compared to fresh controls, accompanied by increased expression of fat-associated genes FTO and PGC-1α [41]. This suggests that both cryopreservation methods may induce similar epigenetic or metabolic alterations unrelated to the specific freezing technology.
Experimental Protocols for Mouse Embryo Research
Mouse Embryo Vitrification Protocol
The following protocol has been successfully applied for vitrification of mouse cleavage-stage embryos and ICM cells [41] [42]:
Reagents and Equipment:
- Base medium: HTF medium supplemented with 10% human serum albumin (HSA)
- Equilibration Solution (ES): 7.5% (v/v) ethylene glycol + 7.5% (v/v) DMSO in base medium
- Vitrification Solution (VS): 15% (v/v) EG + 15% (v/v) DMSO + 0.5M sucrose + 10μg/ml Ficoll in base medium
- Warming solutions: Sucrose gradients (0.25M, 0.125M) in base medium
- Cryocarriers: Cryoloops or HSV straws
- Liquid nitrogen storage system
Procedure:
- Equilibration: Transfer embryos to ES at room temperature for 15 minutes
- Vitrification solution exposure: Move embryos to VS for <45 seconds
- Loading: Rapidly load 1-2 embryos in minimal volume onto cryocarrier
- Plunging: Immediately immerse cryocarrier into liquid nitrogen
- Storage: Transfer to long-term LNâ‚‚ storage tanks
Warming process:
- Rapid warming: Immerse cryocarrier directly in 37°C base medium with 0.25M sucrose for 2 minutes
- Sucrose dilution: Transfer embryos to 0.125M sucrose solution for 3 minutes
- Rehydration: Rinse in base medium for 5 minutes
- Culture: Transfer to pre-equilibrated culture medium for further development
Mouse Embryo Slow Freezing Protocol
This protocol adapts traditional slow freezing methods for mouse embryo research [41]:
Reagents and Equipment:
- Freezing medium: DMEM/F12 with 10% glycerol, 10% DPBS, and 10% fetal calf serum (FCS)
- Thawing solutions: Gradients of glycerol (6%, 3%) with 0.3M sucrose, followed by sucrose-only (0.3M) solution
- Programmable freezer (e.g., Cryologic CL3300)
- Seeding forceps
- 0.25ml plastic straws
Procedure:
- Equilibration: Incubate embryos in freezing medium for 15 minutes
- Loading: Pipette embryos into labeled straws
- Programmed freezing:
- Cool from room temperature to -7°C at -0.7°C/min
- Hold at -7°C for 10 minutes, perform manual seeding
- Cool to -33°C at -0.3°C/min
- Plunge into liquid nitrogen for storage
- Thawing:
- Hold straws at room temperature for 60 seconds
- Immerse in 25°C water bath for 30 seconds
- Expel contents into glycerol/sucrose solutions
- Stepwise dilution through decreasing CPA concentrations (6% glycerol/0.3M sucrose → 3% glycerol/0.3M sucrose → 0.3M sucrose → PBS+20% FCS), 5 minutes each
- Transfer to culture medium
Toxicity Considerations for Mouse Research
Cryoprotectant Toxicity Profiles
The differential toxicity profiles of each method represent a critical consideration for experimental design:
Slow Freezing Toxicity:
- Primarily associated with DMSO at concentrations typically around 10% [39]
- Extended exposure during slow cooling may affect epigenetic markers [41]
- Reduced expression of Oct-4 pluripotency marker in human embryonic stem cells after slow freezing with DMSO [43]
Vitrification Toxicity:
- Higher cumulative toxicity from CPA cocktails (EG + DMSO at 15% each) [41]
- Shorter exposure times mitigate toxic effects (typically <20 minutes total) [42]
- Potential for osmotic shock during addition/removal steps
- Demonstrated preservation of pluripotency markers (SSEA-1, Sox-2, Oct-4) in vitrified ICM cells [42]
Molecular and Genetic Impacts
Research in mouse models has revealed that both cryopreservation methods can induce subtle molecular changes in resulting offspring:
- Increased expression of fat mass and obesity-associated (FTO) and PPARγ co-activator-1 (PGC-1α) genes in offspring from both cryopreservation groups compared to fresh controls [41]
- No significant alterations in brain development-related proteins GFAP and MBP [41]
- Comparable spatial learning and cerebral development parameters across all groups [41]
These findings suggest that observed effects may represent generalized stress responses rather than method-specific toxicity.
Decision Framework for Research Applications
Method Selection Guidelines
Table 2: Method Selection Based on Research Objectives
| Research Focus | Recommended Method | Rationale |
|---|---|---|
| Maximum cell survival | Vitrification | Superior survival rates across multiple cell types |
| Structural integrity | Vitrification | Better stromal preservation in tissues |
| Angiogenic potential | Equivalent | Comparable angiogenic factor expression |
| Long-term development | Equivalent | Similar postnatal outcomes in mouse models |
| Minimizing CPA toxicity | Slow freezing | Lower CPA concentrations |
| Metabolic/epigenetic studies | Requires controls | Both methods show gene expression alterations |
| High-throughput applications | Vitrification | Faster process, higher consistency |
The Researcher's Toolkit: Essential Reagents and Materials
Cryoprotective Agents:
- Permeating CPAs: Ethylene glycol (vitrification), DMSO (both methods), Glycerol (slow freezing)
- Non-permeating CPAs: Sucrose (both methods), Ficoll (vitrification)
- Commercial media: Pre-formulated solutions (e.g., CryoSure, Irvine Scientific)
Specialized Equipment:
- Vitrification: Cryoloops, HSV straws, Cryotops
- Slow freezing: Programmable freezer (e.g., Cryologic CL3300), seeding tools
- General: Liquid nitrogen storage systems, precision timers, sterile workstations
Quality Assessment Tools:
- Viability staining (Trypan blue, FDA/EtBr)
- Molecular markers (Pluripotency: Oct-4, Sox-2; Differentiation markers)
- Functional assays (Hormone secretion, angiogenic factor arrays)
Visualizing Cryopreservation Pathways and Outcomes
Experimental Workflow for Toxicity Assessment
Signaling Pathways Affected by Cryopreservation
The comparative analysis of slow freezing versus vitrification for mouse embryo cryopreservation reveals a complex landscape where neither method demonstrates universal superiority. Vitrification offers distinct advantages in immediate survival rates and structural preservation, while slow freezing benefits from reduced CPA exposure. Critically, both methods produce comparable long-term developmental outcomes in mouse offspring, with similar patterns of altered gene expression related to metabolic function. The optimal choice depends primarily on specific research objectives, technical capabilities, and the particular endpoints being measured. Future research should focus on protocol refinements that minimize method-specific toxicities while preserving the demonstrated strengths of each approach.
Cryopreservation is a cornerstone of modern biomedical research, particularly in the field of genetically engineered mouse models. The ability to reliably preserve oocytes and embryos is crucial for managing research colonies, preserving valuable genetic material, and facilitating scientific collaboration. Traditional cryopreservation methods have been divided between slow freezing and vitrification approaches, each with distinct advantages and limitations. Slow freezing allows processing in a near-equilibrium state with minimal supercooling but requires extended processing times and specialized equipment. Vitrification offers rapid processing and high survival rates but typically employs high concentrations of potentially toxic cryoprotectants and requires continuous storage below -130°C to maintain the vitrified state [44].
Equilibrium vitrification represents an innovative hybrid approach that combines the benefits of both conventional methods. This technique enables vitrification in a highly dehydrated/concentrated state using significantly lower concentrations of cryoprotectants, thereby reducing chemical toxicity while maintaining the practical advantages of vitrification. Developed primarily through mouse model research, this method addresses the critical challenge of cryoprotectant toxicity while enabling practical applications such as dry ice transportation [45] [46]. This technical guide examines the principles, methodologies, and applications of equilibrium vitrification, with particular focus on its implementation in mouse embryo and oocyte research.
Theoretical Foundation and Principles
Defining Equilibrium Vitrification
Equilibrium vitrification bridges the fundamental principles of slow freezing and vitrification. In conventional slow freezing, cells are cooled gradually to approximately -70°C, allowing sufficient dehydration and concentration of intracellular solutes in a near-equilibrium state before plunging into liquid nitrogen. Traditional vitrification, in contrast, employs high cooling rates and high cryoprotectant concentrations to achieve a glassy state without ice formation, but does so under considerable supercooling (non-equilibrium conditions) [44] [46].
The equilibrium vitrification method achieves the glassy state characteristic of vitrification while maintaining the cell in a highly dehydrated/concentrated state similar to that achieved by slow freezing. This is accomplished through optimized combinations of permeating and non-permeating cryoprotectants that promote sufficient cellular dehydration at relatively low overall concentrations [46]. The resulting cellular state exhibits minimal supercooling, significantly reducing the risks associated with both intracellular ice formation and cryoprotectant toxicity.
Comparative Advantages
The equilibrium vitrification approach offers several distinct advantages over conventional methods:
- Reduced Cryoprotectant Toxicity: By utilizing lower concentrations of permeating cryoprotectants (total 20% v/v versus 35-40% in conventional vitrification), the method minimizes chemical damage to sensitive cellular structures [46].
- Simplified Storage and Transport: Specimens vitrified using this method can be maintained at -80°C for extended periods (up to 28 days demonstrated) and transported on dry ice, eliminating the requirement for continuous liquid nitrogen storage during transit [45] [44].
- Enhanced Operational Flexibility: The method can be performed at room temperature without programmable freezing equipment, simplifying laboratory workflows [46].
- Compatibility with Multiple Developmental Stages: With appropriate modifications, the technique has proven effective for oocytes, two-cell embryos, four-cell embryos, eight-cell embryos, and blastocysts [45] [44].
Material and Methodological Framework
Research Reagent Solutions
The following table details the essential reagents utilized in equilibrium vitrification protocols:
Table 1: Essential Research Reagents for Equilibrium Vitrification
| Reagent | Composition/Description | Primary Function |
|---|---|---|
| EDFS10/10a | 10% (v/v) EG, 10% (v/v) DMSO, 0.4 M sucrose, 24% (w/v) Ficoll PM-70 in FSa solution [45] [46] | Primary vitrification solution with low toxicity and osmolality |
| ED5/5 | 5% (v/v) EG, 5% (v/v) DMSO in PB1 medium [44] | Pretreatment solution for gradual cryoprotectant introduction |
| FSa Solution | PB1 medium with 30% (w/v) Ficoll PM-70 and 0.5 M sucrose [44] | Base solution for vitrification medium |
| S-PB1 | PB1 medium containing 0.5 M sucrose [44] | Osmotic buffering during cryoprotectant removal |
| Modified M16 Medium | Standard embryo culture medium [44] | Post-warming embryo culture and development |
| Melitracen Hydrochloride | Melitracen Hydrochloride - CAS 10563-70-9 | Melitracen hydrochloride is a tricyclic antidepressant for research. This product is for Research Use Only (RUO), not for human consumption. |
| Martinomycin | Martinomycin, MF:C49H84O17, MW:945.2 g/mol | Chemical Reagent |
Experimental Workflow
The following diagram illustrates the complete equilibrium vitrification experimental workflow:
Core Methodology
The equilibrium vitrification protocol follows a standardized two-step approach:
1. Specimen Preparation: Mature oocytes or embryos are collected from superovulated mice. For ICR strain oocytes, superovulation is induced using 5 IU equine chorionic gonadotropin (eCG) followed by 5 IU human chorionic gonadotropin (hCG) 48 hours later. Oocytes are collected from oviducts approximately 16-18 hours post-hCG administration [45]. For embryos, appropriate developmental stages are collected at specific timepoints post-fertilization: four-cell embryos at 53-55 hours, eight-cell embryos at 67-68 hours, and morulae at 76-78 hours [44].
2. Vitrification Procedure: Specimens are first exposed to ED5/5 pretreatment solution for 2 minutes at 25°C, allowing gradual introduction of permeating cryoprotectants. Subsequently, 5-8 oocytes/embryos are transferred to EDFS10/10a vitrification solution, washed three times, and loaded into 0.25-ml plastic insemination straws with minimal solution volume. After 60 seconds of exposure, the straws are immediately plunged into liquid nitrogen for vitrification [44].
3. Storage Conditions: Vitrified specimens can be maintained in liquid nitrogen indefinitely or transferred to -80°C storage for periods up to 28 days, enabling practical transport on dry ice [45] [44].
4. Warming and Recovery: For specimens stored at -80°C, straws are directly immersed in a 25°C water bath. For specimens maintained in liquid nitrogen, straws are first held in air at 25°C for 10 seconds to pass through the glass transition temperature gradually, preventing fracture damage, before water bath immersion. Cryoprotectant removal is performed in S-PB1 medium with 0.5 M sucrose, after which specimens are transferred to culture media for further assessment [44].
Experimental Outcomes and Validation
Performance Metrics with Mouse Oocytes
Equilibrium vitrification demonstrates exceptional efficacy for mature mouse oocytes cryopreservation:
Table 2: Experimental Outcomes for Vitrified Mouse Oocytes
| Parameter | EDFS10/10a Vitrification | Fresh Control | EDFS15/15a Vitrification |
|---|---|---|---|
| Survival Rate | 88-99% [45] [47] | N/A | 0% [45] |
| Fertilization Rate | 80-82% [47] | Comparable [45] | Not applicable |
| Blastocyst Formation | 55-77% [45] [47] | Similar [45] | Not applicable |
| Offspring Development | Normal [47] | Normal [47] | Not applicable |
The data demonstrates that oocytes vitrified using EDFS10/10a maintain developmental competence equivalent to fresh controls across multiple parameters, including preimplantation development and full-term offspring production. Notably, higher concentration formulations (EDFS15/15a) prove completely lethal, underscoring the critical importance of optimized cryoprotectant concentrations [45].
Efficacy Across Embryonic Stages
The equilibrium vitrification method shows variable but generally favorable outcomes across different embryonic developmental stages:
Table 3: Developmental Stage-Specific Outcomes Post-Vitrification
| Developmental Stage | Survival After -80°C Storage | Notable Requirements |
|---|---|---|
| Two-Cell Embryos | High survival after 28 days at -80°C [44] | No special requirements |
| Four-Cell Embryos | High survival after 28 days at -80°C [44] | No special requirements |
| Eight-Cell Embryos | High survival after 28 days at -80°C [44] | No special requirements |
| Morulae | Low survival after 4 days at -80°C [44] | Requires artificial shrinkage |
| Blastocysts | Low survival after 4 days at -80°C [44] | Requires artificial shrinkage |
Later stage embryos (morulae and blastocysts) require additional processing steps, specifically artificial shrinkage of the blastocoel cavity using microneedle puncture, to achieve satisfactory survival rates after -80°C storage. This modification facilitates sufficient dehydration of these structurally complex stages [44].
Comparative Solution Performance
The reduced toxicity of EDFS10/10a represents a significant advantage over conventional vitrification solutions:
Table 4: Vitrification Solution Toxicity Comparison
| Solution | Composition | Developmental Ability After 10min Exposure | Osmolality (moles/kg) |
|---|---|---|---|
| EDFS10/10a | 10% EG, 10% DMSO, 0.4M sucrose, 24% Ficoll [46] | High (similar to fresh control) [46] | 6.43 [44] |
| EFS35c | 35% EG, 0.98M sucrose [46] | Significantly decreased after 2min exposure [46] | 23.3 [44] |
The dramatically lower osmolality of EDFS10/10a (6.43 versus 23.3 moles/kg) significantly reduces osmotic stress, while the reduced permeating cryoprotectant concentration minimizes chemical toxicity, collectively contributing to enhanced specimen viability [46].
Technical Considerations and Applications
Practical Implementation Guidelines
Successful implementation of equilibrium vitrification requires attention to several critical technical factors:
- Temperature Consistency: All procedures should be performed at consistent room temperature (25°C) to ensure reproducible dehydration and cryoprotectant permeation kinetics [44].
- Timing Precision: Adherence to specified exposure durations (2 minutes in ED5/5; 60 seconds in EDFS10/10a) is essential for optimal dehydration while minimizing cryoprotectant toxicity [45] [44].
- Volume Minimization: Loading specimens with minimal vitrification solution volume into straws enhances cooling rates and reduces the probability of ice crystallization during cooling [44].
- Stage-Specific Modifications: Later stage embryos (morulae and blastocysts) require artificial shrinkage to achieve sufficient dehydration for successful -80°C storage [44].
Research Applications and Implications
The equilibrium vitrification method enables several valuable applications in biomedical research:
- Genetic Resource Management: Provides a low-toxicity alternative for preserving valuable genetically engineered mouse strains, particularly important for sensitive genotypes vulnerable to cryoprotectant toxicity [46].
- Research Collaboration Enhancement: Facilitates secure transport of vitrified specimens between institutions using dry ice, eliminating logistical challenges associated with liquid nitrogen shipping [45] [44].
- Emergency Preparedness: Offers a contingency method for temporary specimen storage at -80°C during liquid nitrogen system failures or facility emergencies [44].
- Developmental Biology Studies: Enables reliable cryopreservation of oocytes and early embryos with maintained developmental competence, supporting longitudinal studies of development [45] [47].
Equilibrium vitrification using low-concentration cryoprotectant solutions represents a significant methodological advancement in oocyte and embryo cryopreservation. By combining the practical advantages of vitrification with the reduced toxicity of near-equilibrium processing, this approach addresses critical limitations of conventional cryopreservation methods. Experimental validation using mouse models demonstrates excellent survival, fertilization, and developmental rates comparable to fresh controls, while enabling flexible storage and transport conditions. As research continues to refine these techniques, equilibrium vitrification holds promise for broader application across multiple species and specimen types, potentially including human assisted reproductive technologies where minimizing cryoprotectant exposure is particularly valuable.
Cryopreservation has become an indispensable tool in mouse research, enabling the archiving and distribution of valuable genetically engineered strains while significantly reducing the costs associated with maintaining live colonies [48] [49]. However, the very agents that enable successful cryopreservation—cryoprotectants—also present a significant toxicity challenge that can compromise embryo viability and developmental potential. The core challenge lies in navigating the delicate balance between preventing intracellular ice formation, which requires sufficient cryoprotectant penetration, and minimizing the cytotoxic and osmotic stress that these chemicals impose on sensitive mouse embryos [50] [23].
The fundamental tradeoff is clear: permeating cryoprotectants like dimethyl sulfoxide (DMSO) and glycerol penetrate cell membranes to provide intracellular protection but exhibit significant toxicity, while non-permeating agents like trehalose and sucrose provide extracellular stabilization with lower toxicity but cannot protect intracellular components [51] [52]. This technical guide examines the mechanisms of cryoprotectant toxicity in mouse embryos and provides evidence-based strategies for optimizing cryoprotectant cocktails that effectively balance permeating and non-permeating agents to maximize survival rates and maintain embryonic developmental competence.
Theoretical Foundations: Mechanisms of Cryoprotectant Action and Toxicity
Permeating Cryoprotectants: Intracellular Protection with Toxic Consequences
Permeating cryoprotectants are typically small, amphiphilic molecules capable of crossing cell membranes. Their primary function is to displace intracellular water, thereby reducing ice crystal formation during freezing [51]. The most common permeating agents include DMSO, glycerol, ethylene glycol, and propylene glycol. These compounds share a common mechanism of action—they form hydrogen bonds with water molecules, disrupting the water-water interactions necessary for ice nucleation [52].
However, this beneficial action comes with significant toxic liabilities. DMSO, while highly effective, demonstrates dose-dependent toxicity that disrupts membrane integrity, interferes with mitochondrial function, and increases reactive oxygen species production [52]. Importantly, DMSO cytotoxicity is temperature-dependent, with greater destabilization of proteins occurring above 0°C [52]. Glycerol, though less toxic than DMSO, can still cause osmotic stress and membrane damage at higher concentrations [52]. For mouse embryos, which are particularly sensitive to chemical insults, these toxic effects can manifest as reduced developmental rates, altered gene expression, and compromised viability after thawing.
Non-Permeating Cryoprotectants: Extracellular Stabilization with Minimal Toxicity
Non-permeating cryoprotectants are larger molecules or polymers that cannot cross cell membranes, including sugars like trehalose and sucrose, and polymers like polyethylene glycol and hydroxyethyl starch [51]. These agents function primarily in the extracellular space, where they create an osmotic gradient that promotes controlled cell dehydration before freezing, thereby reducing the likelihood of intracellular ice formation [23] [51]. Additionally, they stabilize membranes and proteins by forming a protective, glassy matrix during freezing [52].
The primary advantage of non-permeating agents is their significantly lower cytotoxicity profile. Trehalose, for instance, has FDA GRAS (Generally Recognized as Safe) status and demonstrates negligible adverse effects on cellular function [52]. Sucrose similarly exhibits minimal cytotoxicity, with osmotic shock during addition or removal representing its main risk [52]. However, their inability to penetrate cells means they cannot provide direct intracellular protection, making them insufficient as standalone cryoprotectants for most applications.
The Cocktail Advantage: Synergistic Protection
Combining permeating and non-permeating cryoprotectants creates a synergistic system that leverages the strengths of each component while mitigating their weaknesses [53]. Research demonstrates that "the tandem use of a permeating and non-permeating CPA has been shown to require lower concentrations of both species than would be required if each worked alone to achieve the desired effect" [53]. This synergy allows researchers to reduce the concentration of toxic permeating agents like DMSO while maintaining or even enhancing overall cryoprotective efficacy.
The theoretical basis for this synergy involves multiple mechanisms:
- Reduced Osmotic Stress: Non-permeating agents help control the rate and extent of water efflux during cryoprotectant addition and removal, minimizing volume excursions that can damage embryonic cells [53] [51].
- Toxicity Dilution: Lower concentrations of individual permeating agents reduce specific toxicity pathways while maintaining sufficient intracellular protection.
- Glass Formation Enhancement: Sugar-based non-permeating agents promote vitrification at achievable cooling rates, reducing ice crystal formation [23].
Experimental Approaches and Protocols
Microfluidic CPA Loading for Controlled Exposure
Traditional batch methods for CPA loading expose embryos to abrupt osmotic shocks, but emerging microfluidic technologies enable gradual, controlled introduction of cryoprotectant cocktails. One sophisticated approach utilizes a microchannel device with multiple inlets for different CPAs, creating stable laminar flows that gradually introduce embryos to increasing concentrations of cryoprotectants [53].
Protocol: Microfluidic Cocktail Loading
- Device Setup: Utilize a microchannel with a central sample inlet for embryos and multiple perpendicular inlets for different CPAs spaced 12.5 cm downstream [53].
- Flow Rate Optimization: Adjust inlet flow rates between 0.25-4 μL/min to control extracellular concentration profiles and minimize intracellular concentration gradients [53].
- Cocktail Introduction: Introduce permeating CPAs (e.g., 1,2-propanediol and DMSO) sequentially or simultaneously with non-permeating agents (e.g., sucrose or trehalose) through separate inlets.
- Validation: Use computational modeling to predict cellular experience and validate with viability assays [53].
This approach maintains water and CPA fluxes below lethal levels, significantly improving survival rates during loading compared to traditional step-wise methods [53].
Vitrification Protocols for Mouse Oocytes and Embryos
Vitrification represents an alternative approach that uses high CPA concentrations to achieve a glassy state without ice formation. An improved protocol for mouse oocytes demonstrates the effective integration of permeating and non-permeating agents:
Protocol: Oocyte Vitrification
- Solution Preparation: Create equilibration and vitrification solutions combining permeating agents (e.g., DMSO and ethylene glycol) with non-permeating sugars (e.g., sucrose) [54].
- Stepwise Exposure: Expose oocytes to equilibration solution (lower CPA concentration) for 10-15 minutes, then to vitrification solution (higher CPA concentration) for 60-90 seconds immediately before cooling [54].
- Device Selection: Use practical storage formats like straws or slimline vitrification devices rather than cryovials [54].
- Cooling and Warming: Employ ultrarapid cooling in liquid nitrogen and rapid warming in a 37°C water bath with sequential dilution to remove CPAs [54].
This protocol achieves high viability and fertilization rates comparable to fresh oocytes, even with genetically altered strains [54].
Stepwise Addition and Removal for Toxicity Reduction
For sea urchin eggs, which share sensitivity characteristics with mouse embryos, research shows that stepwise addition of cryoprotectants significantly reduces toxicity. This approach can be adapted for mouse embryos:
Protocol: Stepwise Toxicity Reduction
- Incremental Addition: Introduce cryoprotectant cocktails in 2-4 steps of increasing concentration, allowing embryos to equilibrate osmotically at each step [55].
- Temperature Control: Perform additions at chilled temperatures (4°C) to reduce chemical toxicity, as demonstrated by minimal impact on egg viability at this temperature [55].
- Combination Strategy: Utilize DMSO in combination with other agents like DMF or methanol rather than as a single permeating CPA [55].
- Reverse Stepwise Removal: Apply the same stepwise principle in reverse during thawing to prevent osmotic shock during CPA elution.
Table 1: Cryoprotectant Toxicity Profiles and Operational Parameters
| Cryoprotectant | Type | Common Concentrations | Key Toxicity Concerns | Temperature Considerations |
|---|---|---|---|---|
| DMSO | Permeating | 5-10% (v/v) [52] | Disrupts membrane integrity, mitochondrial function, ROS production [52] | Increased toxicity above 0°C; rapid cooling essential [52] |
| Glycerol | Permeating | 5-15% (v/v) [52] | Osmotic stress, membrane damage at high concentrations [52] | Cytotoxicity increases with temperature [52] |
| Ethylene Glycol | Permeating | 4-6 M (vitrification) [23] | Metabolic conversion to toxic metabolites | Less toxic than DMSO at room temperature |
| Trehalose | Non-permeating | 0.1-0.5 M [52] | Minimal toxicity; osmotic shock during addition/removal | Stable across temperature ranges |
| Sucrose | Non-permeating | 0.1-0.5 M [52] | Minimal toxicity; osmotic shock primary risk | Stable performance across temperatures |
Quantitative Data and Cocktail Formulations
Performance Metrics of CPA Cocktails
The effectiveness of optimized CPA cocktails can be evaluated through multiple performance metrics. The developmental rate percentage serves as a key quantitative endpoint, calculated as: Developmental rate (%) = (N-developed/N-total) × 100, where N-developed is the number of embryos reaching target development stages and N-total is the total embryos used [56].
Research demonstrates that cocktail approaches can achieve significant improvements compared to single-CPA systems. In microfluidic loading systems, appropriate flow rate optimization (0.25-4 μL/min) creates intracellular CPA concentrations that balance dehydration and toxicity, significantly improving post-thaw survival [53]. For vitrification protocols, the combination of permeating and non-permeating agents has enabled high fertilization rates comparable to fresh oocytes even with genetically altered mouse strains [54].
Practical Cocktail Formulations for Mouse Embryos
Based on current research, several cocktail formulations show promise for mouse embryo cryopreservation:
Formulation 1: DP6-Based Cocktail
- Permeating Agents: 1,2-propanediol and DMSO combination
- Non-Permeating Component: HEPES buffer or sucrose
- Application: Microfluidic loading systems for pre-freeze CPA equilibration
- Rationale: Lower concentrations of both permeating agents required when used together [53]
Formulation 2: Vitrification Cocktail
- Permeating Agents: DMSO + ethylene glycol combination
- Non-Permeating Agent: 0.2-0.5 M sucrose
- Application: Ultrarapid cooling for ice-free preservation
- Rationale: Sugar promotes glass formation while permeating agents provide intracellular protection [54]
Formulation 3: Toxicity-Reduced Equilibrium Cocktail
- Permeating Agent: Reduced-concentration DMSO or glycerol
- Non-Permeating Agents: Trehalose (0.1-0.3 M) + sucrose (0.1-0.3 M) combination
- Application: Slow freezing protocols with controlled rate cooling
- Rationale: Multiple non-permeating agents provide enhanced extracellular stabilization
Table 2: Optimization Strategies for Cryoprotectant Cocktails in Mouse Embryo Research
| Challenge | Solution | Mechanism | Experimental Evidence |
|---|---|---|---|
| High Cytotoxicity of Permeating CPAs | Use combinatorial cocktails with multiple permeating agents at reduced individual concentrations [53] | Dilutes specific toxicity pathways while maintaining sufficient intracellular cryoprotection | Microfluidic studies show lower concentrations of both 1,2-propanediol and DMSO required when used together [53] |
| Osmotic Shock During CPA Addition/Removal | Stepwise addition and removal protocols combined with non-permeating agents [55] | Allows gradual osmotic equilibration; non-permeating agents control water flux | Sea urchin egg studies demonstrate significantly reduced toxicity with stepwise addition [55] |
| Intracellular Ice Formation | Balance permeating and non-permeating agents to control dehydration while providing intracellular protection [23] | Permeating agents displace intracellular water; non-permeating agents create protective osmotic gradient | Optimized cooling rates balance dehydration and ice formation according to two-factor hypothesis [50] [23] |
| Cell-Type Specific Sensitivity | Tailor cocktail formulations to specific mouse strains and embryo stages | Addresses genetic background differences in membrane composition and metabolic function | Validation required for each strain; JAX has cryopreserved over 20,000 strains with tailored protocols [49] |
| Post-Thaw Apoptosis | Include antioxidants in base medium and control cooling/warming rates | Reduces reactive oxygen species generation; minimizes apoptosis triggers | T-cells show ~40% apoptosis 8 hours post-thaw without optimization [51] |
Implementation Framework and Quality Control
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for CPA Cocktail Optimization
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Permeating CPAs (DMSO, glycerol, ethylene glycol, 1,2-propanediol) | Intracellular ice prevention | Use high-purity, compendial-grade materials; concentration and combination dependent on protocol [52] |
| Non-Permeating CPAs (trehalose, sucrose, hydroxyethyl starch) | Extracellular stabilization, osmotic control | Sucrose common for vitrification; trehalose offers superior glass-forming properties [52] |
| Microfluidic Devices | Controlled, gradual CPA introduction | Enables laminar flow for precise concentration profiles; reduces osmotic shock [53] |
| Controlled Rate Freezer | Optimized cooling rate implementation | Active CRC devices provide programmable profiles with seeding capability [50] |
| Cryogenic Storage Vessels (straws, slimline devices) | Practical storage format | Superior to cryovials for handling and storage efficiency [54] |
| Viability Assays | Post-thaw assessment | Developmental scoring, membrane integrity tests, metabolic activity assays |
| Mesosulfuron-methyl | Mesosulfuron-methyl, CAS:208465-21-8, MF:C17H21N5O9S2, MW:503.5 g/mol | Chemical Reagent |
| Mgb-bp-3 | Mgb-bp-3, CAS:1000277-08-6, MF:C36H37N7O4, MW:631.7 g/mol | Chemical Reagent |
Quality Control and Validation Protocols
Implementing rigorous quality control measures is essential for successful cryopreservation. The Jackson Laboratory employs a tiered QC approach that includes:
- Basic QC: Motility assessment of thawed sperm samples
- Intermediate QC: In vitro fertilization trials to confirm fertilizing capacity
- Comprehensive QC: Full cryorecovery producing live mice with genotyping confirmation [48]
For research laboratories, recommended validation includes:
- Developmental Competence Assessment: Culture thawed embryos to blastocyst stage with developmental rate calculation [56]
- Genetic Integrity Verification: Post-thaw genotyping to confirm genetic stability
- Functional Testing: Embryo transfer to confirm full developmental potential
Optimizing cryoprotectant cocktails through strategic balancing of permeating and non-permeating agents represents a critical advancement in mouse embryo cryopreservation. The synergistic combination of these agents allows researchers to achieve sufficient protection against freezing injury while minimizing the toxic consequences that compromise embryo viability and developmental potential. As cryopreservation continues to enable more efficient management of mouse research colonies and the preservation of valuable genetic resources, refined CPA cocktails that address the specific sensitivity of mouse embryos will play an increasingly important role in supporting biomedical research advancements.
Visualizations
Workflow for CPA Cocktail Optimization
CPA Mechanisms and Toxicity Pathways
Embryo cryopreservation is a cornerstone of modern biomedical research, enabling the archiving and distribution of valuable genetically engineered mouse models. Within this field, a central thesis is that a deep understanding of cryopreservation-induced toxicity is paramount for ensuring the viability and genetic integrity of preserved samples. This toxicity primarily manifests through two mechanisms: the chemical toxicity of cryoprotective agents (CPAs) and physical damage from ice crystal formation. The interplay between exposure time, temperature, and the composition of carrier solutions is critical in mitigating these risks. This technical guide details the core protocols and principles that underpin successful mouse embryo cryopreservation, providing researchers with the experimental frameworks needed to optimize recovery rates and ensure reproducible results in drug development and basic research.
Core Parameters: Balancing Toxicity and Survival
The success of any cryopreservation protocol hinges on the precise control of several key parameters. These factors directly influence the delicate balance between achieving sufficient cryoprotection and minimizing damage to the embryos.
Exposure Time
The duration that embryos are exposed to CPAs is a critical determinant of outcome. Prolonged exposure increases the risk of chemical toxicity, while insufficient exposure prevents adequate dehydration and permeation of CPAs, leading to lethal intracellular ice formation during cooling.
- Vitrification Protocol: In the ethylene glycol (EG)-based vitrification method, a two-step exposure is standard.
- Equilibration Solution (EFS20): Embryos are first transferred to a lower-concentration solution for 2 minutes at room temperature. During this phase, embryos undergo osmotic shrinkage as water is withdrawn, a process that must be monitored morphologically [57].
- Vitrification Solution (EFS40): Embryos are then moved to a high-concentration solution for a brief 1 minute before being plunged into liquid nitrogen. This step is deliberately short to limit the toxic effects of the concentrated CPAs [57].
- Thawing Protocol: The thawing process similarly uses a stepped reduction in osmolarity. Embryos are typically held in a 0.75 M sucrose solution (TS1) for 3 minutes before being transferred through a 0.25 M sucrose solution (TS2) for another 3 minutes to rehydrate the cells gradually [57].
Temperature
Temperature governs the rate of cellular metabolism and the kinetic toxicity of CPAs. Performing procedures at sub-optimal temperatures can drastically reduce embryo survival.
- Room Temperature (Ambient): Many validated protocols, including the EG-based vitrification method, are designed to be performed at room temperature (approximately 22-25°C). This temperature allows for sufficiently rapid permeation of CPAs while being more tolerant of handling variations compared to warmer conditions [57].
- Physiological Temperature (37°C): Some advanced media systems now recommend performing vitrification and warming at 37°C. This approach helps maintain spindle integrity in oocytes and embryos and can shorten the required exposure time to CPAs, thereby minimizing their toxic impact [58].
- Chilled Conditions (0-4°C): While less common in modern vitrification, some protocols use chilled solutions to suppress the chemical activity and toxicity of CPAs, though this can slow down permeation [59].
Carrier Solutions and Cryoprotectants
The composition of the solutions used to prepare and suspend embryos during freezing is a primary focus of toxicity studies. The choice of CPAs and supporting osmolytes is crucial.
- Cryoprotectant Agents: Different CPAs have varying levels of toxicity and permeability.
- Ethylene Glycol (EG): Often preferred for its rapid permeation and relatively lower toxicity, making it a common choice for mouse embryo vitrification [57].
- Dimethyl Sulfoxide (DMSO): Also widely used, though its toxicity profile can be less favorable than EG. Research has shown that a combination of 10% EG + 10% Me2SO in the first vitrification solution and 20% EG + 20% Me2SO in the second can yield survival rates of ~65-70% for oocytes [59].
- Supporting Osmolytes: Non-permeating sugars like sucrose are essential components. They induce osmotic dehydration before freezing and control rehydration during thawing. Concentrations typically range from 0.3 M to 0.9 M, with adjustments made for more sensitive strains [57].
- Macromolecules: Additives like Ficoll (at 18-24% w/v) and serum (e.g., 20% Fetal Calf Serum) are used to increase the solution's viscosity, which aids in achieving the glass-like state of vitrification and provides protective coating for cells [57] [59].
Table 1: Optimized Parameters for Mouse Embryo Vitrification
| Parameter | Protocol Specification | Impact & Rationale |
|---|---|---|
| Exposure Time (EFS20) | 2 minutes [57] | Allows for initial dehydration; shorter times lead to insufficient dehydration, longer times increase toxicity. |
| Exposure Time (EFS40) | 1 minute [57] | Limits exposure to high-concentration, highly toxic CPAs while achieving sufficient permeation. |
| Exposure Time (TS1 Thawing) | 3 minutes [57] | Allows for controlled initial rehydration in a hypertonic environment. |
| Process Temperature | Room Temperature (22-25°C) [57] | Balances CPA permeation rate with manageable toxicity; simplifies handling. |
| Primary Cryoprotectant | Ethylene Glycol (EG) [57] | Favored for its rapid permeation and relatively lower toxicity compared to other CPAs. |
| Supporting Osmolyte | Sucrose (0.3 M - 0.9 M) [57] | Controls osmotic pressure, inducing dehydration and preventing devitrification. |
| Viscosity Enhancer | Ficoll (18-24% w/v) [57] | Increases solution viscosity to support the vitrified state and prevents ice crystal growth. |
Detailed Experimental Protocols
Ethylene Glycol-Based Vitrification
This protocol, optimized for a broad application across mouse strains, uses ethylene glycol as the primary CPA [57].
Reagent Preparation:
- Base Medium (PB1): A phosphate-buffered saline solution containing electrolytes, glucose, pyruvate, and penicillin.
- Ficoll-Sucrose (FS) Solution: Dissolve 6.0 g Ficoll 70 and 3.424 g sucrose in 14 ml PB1, then add 42.0 mg BSA and dissolve at 4°C.
- Equilibration Solution (EFS20): 20% (v/v) ethylene glycol, 24% (w/v) Ficoll, and 0.4 M sucrose in PB1 with BSA. (1 ml ethylene glycol + 4 ml FS solution).
- Vitrification Solution (EFS40): 40% (v/v) ethylene glycol, 18% (w/v) Ficoll, and 0.3 M sucrose in PB1 with BSA. For BALB/c or ICR strains, use 0.9 M sucrose. (2 ml ethylene glycol + 3 ml FS solution).
- Thawing Solutions: TS1 (0.75 M sucrose in PB1) and TS2 (0.25 M sucrose in PB1).
Vitrification Procedure:
- Aliquot 50 µl of EFS40 into a cryotube.
- Place a 50 µl drop of EFS20 in a plastic Petri dish.
- Transfer up to 30 two-cell embryos into the EFS20 drop. Start a timer for 2 minutes. Observe embryos; they should show a shrunken morphology due to dehydration.
- At ~1.5 minutes, pick up the embryos and transfer them to the EFS40 in the cryotube, aiming to complete the transfer at the 2-minute mark.
- Wait for 1 minute in EFS40.
- Put the cryotube directly into liquid nitrogen for storage [57].
Thawing Procedure:
- Warm TS1 to 37°C.
- Retrieve the cryotube from liquid nitrogen, open it, and discard the LN2. Wait 30 seconds.
- Add 850 µl of warm TS1 to the tube and mix by gentle pipetting for about 25 seconds until the solution is clear.
- Transfer the entire volume to a 60 mm Petri dish.
- Start a timer for 3 minutes.
- After 3 minutes, transfer the embryos to the first of three 50 µl drops of TS2, spending 3 minutes in each drop.
- Transfer the embryos to pre-equilibrated culture medium and place in a CO2 incubator [57].
Automated Vitrification and Thawing System (AVTS)
To minimize human error and improve consistency, automated systems have been developed.
System Description:
- The AVTS consists of a main controlling unit with a carrier holder, a motion dish platform, and a pocket programmer that controls the movement and timing of the cryo-handle through different solutions [60].
- The cryo-handle is a carrier featuring a mesh-like copper casing that holds the embryos in a small cavity (1.5 µL volume) [60].
Procedure:
- The programmer pre-sets the positions and time intervals for the cryo-handle to be moved sequentially through Equilibrium (ES), Vitrification (VS), and other solutions with precise timing.
- For thawing, the system reverses the process, moving the cryo-handle through Thawing (TS), Dilution (DS), and Washing (WS) solutions [60].
- Studies confirm that this automated process maintains proper osmolality exchange and achieves reliable cooling/warming rates, producing oocyte survival and embryo development rates comparable to manual methods [60].
The Scientist's Toolkit: Research Reagent Solutions
Successful cryopreservation relies on a suite of specialized reagents and tools. The following table details essential materials and their functions in the context of mouse embryo cryopreservation.
Table 2: Essential Reagents and Materials for Embryo Cryopreservation
| Reagent/Material | Function & Application | Example/Notes |
|---|---|---|
| Ethylene Glycol (EG) | Permeating cryoprotectant | Primary CPA in many vitrification protocols due to lower toxicity [57]. |
| Dimethyl Sulfoxide (Me2SO) | Permeating cryoprotectant | Used in combination with EG for oocyte vitrification [59]. |
| Ficoll 70 | Non-permeating polymer | Increases viscosity to prevent ice crystal growth and support vitrification [57]. |
| Sucrose | Non-permeating osmolyte | Controls osmotic pressure during freezing/thawing; induces dehydration [57]. |
| Fetal Calf Serum (FCS) | Protein supplement | Mitigates osmotic shock and stabilizes the cell membrane; 20% concentration is often optimal [59]. |
| Cryotube / Straw | Sample container | Holds embryos during storage in LN2; can be open or closed systems [57] [58]. |
| Open Pulled Straw (OPS) | Vitrification carrier | A fine-drawn straw that allows ultra-rapid cooling; an open system [59]. |
| Nylon Loop | Vitrification carrier | A small nylon loop for holding a thin film of solution; an open system [59]. |
| Rapid-i / RapidStraw | Closed vitrification system | A sealed device that minimizes risk of contamination during storage [58]. |
| Cryo-handle (AVTS) | Automated system carrier | A mesh-like copper casing used with an automated vitrification/thawing system [60]. |
| Octamylamine | Octamylamine, CAS:502-59-0, MF:C13H29N, MW:199.38 g/mol | Chemical Reagent |
| Mianserin Hydrochloride | Mianserin Hydrochloride, CAS:21535-47-7, MF:C18H21ClN2, MW:300.8 g/mol | Chemical Reagent |
Workflow and Decision Pathways
The following diagrams illustrate the core experimental workflow and the strategic decisions involved in selecting a cryopreservation method.
Vitrification and Thawing Workflow
This diagram outlines the key steps in the manual vitrification and thawing process for mouse embryos, highlighting critical time and temperature parameters.
Cryopreservation Method Selection
This diagram provides a logical framework for choosing between sperm and embryo cryopreservation, based on the genetic characteristics of the mouse model.
Cryopreservation represents a pivotal technology in biomedical research, particularly for managing valuable genetic resources in mouse models. However, the very agents that enable ice-free preservation—cryoprotectants (CPAs)—also pose significant toxicity risks that can compromise embryo viability and developmental potential. For sensitive embryos, this toxicity presents a major obstacle, as high CPA concentrations can disrupt cellular structures, alter organelle function, and impair post-warming development. Within this context, the emergence of equilibrium vitrification using EDFS10/10a offers a promising approach that specifically addresses CPA toxicity through methodological innovation. This case study examines the application, efficacy, and mechanistic basis of this novel solution within the broader framework of understanding and mitigating embryo cryopreservation toxicity in mice research.
Cryoprotectant toxicity remains the greatest obstacle to cryopreservation, standing in the way of cryogenic cryopreservation of biological materials that could potentially save many lives [1]. High levels of penetrating cryoprotectants can eliminate ice formation during cryopreservation to cryogenic temperatures, but these CPAs become increasingly toxic as concentration increases [1]. For researchers working with sensitive or genetically valuable embryos, this creates a critical trade-off between preventing ice formation and maintaining embryonic developmental competence.
Understanding Cryoprotectant Toxicity: Mechanisms and Impact
Fundamental Toxicity Mechanisms
Cryoprotectant toxicity manifests through multiple interconnected pathways that collectively jeopardize embryo viability. CPAs can be deemed toxic if cell membranes are breached or damaged, enzyme function is impaired, cell or embryo development is diminished, mitochondrial function is reduced, or if DNA, protein, or other macromolecules are damaged [1]. Some effects deemed to be due to CPA toxicity may actually be due to osmotic shock, oxidative stress, chilling injury, or other causes of damage [1].
The toxicity can be categorized as either specific to a particular CPA (specific toxicity) or consequence of being a CPA (non-specific toxicity) [1]. CPAs are believed to prevent ice formation by interfering with hydrogen bonding between water molecules, and this effect has been proposed to cause non-specific toxicity [1]. For sensitive mouse embryos, these toxic effects can significantly reduce survival rates and developmental competence, particularly for more advanced developmental stages like morulae and blastocysts that demonstrate increased vulnerability to cryopreservation-induced damage.
Organelle-Specific Impacts
The detrimental effects of CPAs extend to critical intracellular organelles essential for embryonic development:
Mitochondrial Damage: Studies on zebrafish ovarian follicles cryopreserved with methanol showed a dose-dependent reduction in five mitochondrial function measures—membrane potential, mitochondrial distribution, mitochondrial DNA copy number, adenosine triphosphate (ATP) levels, and adenosine diphosphate (ADP)/ATP ratios [1]. In mouse oocytes, conventional vitrification significantly adversely affected mitochondrial distribution and membrane potential (ΔΨm) compared to ultra-fast vitrification approaches [62].
Endoplasmic Reticulum Disruption: The ER, as a crucial component of the calcium release system, can be damaged by physical trauma or high-concentration toxicity of CPA. This triggers the release of calcium ions (Ca2+) from the ER, leading to increased intracellular calcium ([Ca2+]i) levels in the mitochondria and decreased mitochondrial membrane potential [62]. These changes substantially impact oocyte survival, fertilization, and developmental potential [62].
Cytoskeletal Alterations: In stallion spermatozoa, glycerol in concentrations over 1.5% polymerizes the actin cytoskeleton, a phenomenon unrelated to osmolality [1]. Similar effects may impact embryonic cytoskeletal elements critical for cell division and differentiation.
The diagram below illustrates the primary cellular damage pathways activated during conventional cryopreservation protocols and how novel approaches target these pathways.
Cellular Toxicity Pathways and Protective Mechanisms - This diagram contrasts damage pathways in conventional vitrification with the protective approach of EDFS10/10a, highlighting how reduced CPA concentration and controlled dehydration mitigate key toxicity mechanisms.
EDFS10/10a Equilibrium Vitrification: A Novel Solution
Methodological Foundation
Equilibrium vitrification using EDFS10/10a represents a significant departure from conventional vitrification approaches. This method enables the vitrification of mouse embryos in liquid nitrogen in a highly dehydrated/concentrated state using notably low concentrations of cryoprotectants [63]. The EDFS10/10a solution specifically contains 10% (v/v) ethylene glycol and 10% (v/v) DMSO in FSa solution, where the FSa solution is PB1 medium containing 30% (w/v) Ficoll PM-70 plus 0.5 M sucrose [63].
The theoretical foundation of this approach builds on the understanding that intracellular water removal by osmosis in the equilibration solution stage is a crucial protective mechanism, which has a stronger effect than promoting intracellular glass transition [62]. This perspective emphasizes dehydration management over high CPA concentrations, thereby directly addressing the core toxicity challenge.
Experimental Validation Across Developmental Stages
Research has systematically evaluated the efficacy of EDFS10/10a equilibrium vitrification across multiple embryonic developmental stages:
Early-Stage Embryos: When two-cell, four-cell, and eight-cell mouse embryos were vitrified with EDFS10/10a in liquid nitrogen and then stored at -80°C, the survival rate remained high even after 28 days, with relatively high developmental ability [63].
Advanced-Stage Embryos: In contrast, the survival of morulae and blastocysts vitrified in liquid nitrogen and stored at -80°C for four days was low [63]. This indicates that morulae and blastocysts cannot be vitrified in a highly dehydrated/concentrated state using the same method as with two-cell embryos without protocol adjustments.
Protocol Adaptation for Blastocysts: When blastocysts were shrunken artificially before vitrification, survival was high after storage at -80°C for four days with high developmental ability [63]. This demonstrates the method's flexibility and the importance of stage-specific modifications.
The table below summarizes the survival outcomes across different embryonic stages using the EDFS10/10a equilibrium vitrification approach.
Table 1: Survival Rates of Mouse Embryos After EDFS10/10a Equilibrium Vitrification
| Developmental Stage | Storage Condition | Storage Duration | Survival Outcome | Key Requirement |
|---|---|---|---|---|
| Two-cell embryos | -80°C | 28 days | High survival | Standard protocol |
| Four-cell embryos | -80°C | 28 days | High survival | Standard protocol |
| Eight-cell embryos | -80°C | 28 days | High survival | Standard protocol |
| Morulae | -80°C | 4 days | Low survival | Protocol adjustment needed |
| Blastocysts | -80°C | 4 days | Low survival | Artificial shrinkage required |
| Blastocysts (with shrinkage) | -80°C | 4 days | High survival | Artificial shrinkage applied |
Comparative Advantage Over Conventional Methods
The EDFS10/10a method demonstrates clear advantages over conventional vitrification approaches. Conventional vitrification (C-VIT) overcomes ice crystal formation by using high-concentration cryoprotectants and rapid cooling to transform cells into an amorphous glass-like state [62]. However, this method introduces significant challenges related to the toxicity of high-concentration CPA and osmotic stress resulting from osmotic equilibrium [62].
In contrast, the equilibrium vitrification approach using EDFS10/10a achieves vitrification with substantially lower CPA concentrations while maintaining effectiveness through optimized dehydration control. This method also enables the convenient transportation of vitrified embryos using dry ice, significantly enhancing practical applications in research settings [63].
Experimental Protocols and Methodologies
EDFS10/10a Equilibrium Vitrification Procedure
The following detailed protocol outlines the specific steps for implementing EDFS10/10a equilibrium vitrification for mouse embryos:
Solution Preparation:
- Prepare EDFS10/10a solution containing 10% (v/v) ethylene glycol and 10% (v/v) DMSO in FSa solution
- Ensure FSa solution consists of PB1 medium with 30% (w/v) Ficoll PM-70 plus 0.5 M sucrose
- Prepare all solutions under sterile conditions using embryo-tested reagents
Vitrification Process:
- Equilibrate embryos in EDFS10/10a solution at room temperature for 12-15 minutes
- Load embryos onto vitrification device (Cryotop or minimum volume straw)
- Immediately plunge into liquid nitrogen for storage
- For blastocysts, implement artificial shrinkage before vitrification using a specialized micropipette or laser pulse system
Storage and Transportation:
- Store vitrified embryos in liquid nitrogen for long-term preservation
- For transportation, maintain at -80°C using dry ice
- Limit storage at -80°C to 28 days for early-stage embryos, 4 days for artificially shrunken blastocysts
Warning Process:
- Warm vitrified embryos rapidly in a 37°C water bath
- Stepwise dilution to remove cryoprotectants using decreasing sucrose concentrations
- Final wash in embryo culture medium before transfer to culture conditions
Assessment Methodologies for Toxicity and Efficacy
Comprehensive evaluation of cryopreservation outcomes requires multiple assessment modalities:
Survival Rate Analysis: Assess membrane integrity, morphology, and re-expansion (for blastocysts) immediately post-warming and after 2-4 hours in culture [63]
Developmental Competence Evaluation: Culture embryos in vitro to assess progression to blastocyst stage and beyond [63]
Organelle Function Assessment:
- Mitochondrial Analysis: Evaluate distribution patterns, membrane potential (ΔΨm) using JC-1 staining, and fluorescence intensity [62]
- Endoplasmic Reticulum Assessment: Analyze distribution in equatorial and cortical regions, fluorescence intensity, and IP3 receptor clustering [62]
- Spindle and Chromosomal Morphology: Examine meiotic spindle structure and chromosomal alignment using immunostaining or Polscope analysis [62]
Functional Testing: Perform embryo transfer to assess in vivo developmental potential and live birth rates
The workflow below illustrates the complete experimental pipeline for evaluating EDFS10/10a efficacy in mouse embryo cryopreservation.
Experimental Workflow for EDFS10/10a Evaluation - This diagram outlines the key steps in applying and assessing the EDFS10/10a equilibrium vitrification method, from embryo collection through comprehensive post-warming analysis.
Research Reagent Solutions and Materials
Table 2: Essential Research Reagents for EDFS10/10a Equilibrium Vitrification
| Reagent/Material | Composition/Type | Function in Protocol |
|---|---|---|
| EDFS10/10a Solution | 10% EG, 10% DMSO in FSa | Primary vitrification solution |
| FSa Solution | PB1 + 30% Ficoll PM-70 + 0.5M sucrose | Base medium with macromolecule |
| Ethylene Glycol (EG) | Permeating CPA | Penetrates cell membrane, suppresses ice formation |
| Dimethyl Sulfoxide (DMSO) | Permeating CPA | Enhances vitrification tendency, cryoprotection |
| Ficoll PM-70 | Synthetic polymer | Non-permeating CPA, promotes glassy state |
| Sucrose | Disaccharide | Osmotic buffer, controls dehydration |
| PB1 Medium | Balanced salt solution | Physiological base medium |
| Liquid Nitrogen | Cryogenic fluid | Ultra-rapid cooling, long-term storage |
| Vitrification Device | Cryotop/Straw | Minimum volume carrier |
| Artificial Shrinkage System | Laser/Micropipette | Blastocyst collapse before vitrification |
Comparative Analysis with Alternative Approaches
Ultra-Fast Vitrification Strategies
Recent research has explored ultra-fast vitrification (UF-VIT) as an alternative strategy to mitigate CPA toxicity. This approach involves preserving oocytes with minimal volume just before the introduction of CPA and water, effectively bypassing the typical osmotic equilibrium phase during the ES stage [62]. Compared to conventional vitrification (C-VIT), UF-VIT presents considerably fewer negative effects on key mitochondrial parameters and results in a notably higher blastocyst formation rate [62].
While UF-VIT and EDFS10/10a equilibrium vitrification employ different mechanistic approaches—the former minimizing exposure time and the latter utilizing lower CPA concentrations—both strategies share the common objective of reducing the intrinsic toxicity associated with conventional cryopreservation methods. This convergence underscores the research priority of managing CPA toxicity while maintaining effective vitrification.
Machine Learning in Cryopreservation Optimization
Emerging technologies, particularly machine learning, are being integrated into cryopreservation research to enhance predictive modeling and protocol optimization. Machine learning algorithms have demonstrated superior performance in predicting blastocyst formation compared to traditional linear regression models, with LightGBM emerging as an optimal model due to utilizing fewer features and offering superior interpretability [64].
Feature importance analysis has identified the number of extended culture embryos, mean cell number on Day 3, and proportion of 8-cell embryos as critical predictors of blastocyst yield [64]. These computational approaches complement experimental methods like EDFS10/10a by providing data-driven insights for protocol refinement and outcome prediction.
The development and application of EDFS10/10a equilibrium vitrification represents a significant advancement in addressing the persistent challenge of cryoprotectant toxicity in mouse embryo cryopreservation. By enabling vitrification through a highly dehydrated state with reduced CPA concentrations, this method directly targets the primary source of toxicity while maintaining functional efficacy across multiple embryonic stages. The experimental evidence demonstrates successful preservation of early-stage embryos with high survival rates even after extended storage at -80°C, with protocol adaptations available for more sensitive advanced-stage embryos.
Future research directions should focus on several key areas. First, further elucidation of the specific molecular mechanisms through which EDFS10/10a provides cytoprotection could reveal additional opportunities for toxicity mitigation. Second, exploration of stage-specific optimizations for more sensitive embryo types may enhance the universal applicability of this approach. Third, integration of this method with emerging technologies like machine learning prediction models and nanotechnology-assisted warming could further improve outcomes. Finally, investigation of potential applications in other sensitive biological systems beyond mouse embryos may expand the impact of this approach across cryopreservation science.
As cryopreservation continues to play an indispensable role in biomedical research, particularly in managing valuable genetic resources in mouse models, innovations like EDFS10/10a equilibrium vitrification provide crucial tools for balancing preservation efficacy with physiological integrity. By directly addressing the fundamental challenge of CPA toxicity, this approach represents a meaningful step toward more secure and effective preservation of sensitive biological materials.
Maximizing Embryo Viability: Strategic Troubleshooting and Protocol Refinement
Cryopreservation is a cornerstone technique in biomedical research, enabling the long-term storage of biologically viable embryos, gametes, and cell lines. However, the process is fraught with potential failure points that can compromise specimen viability and experimental integrity. For researchers working with mouse models, suboptimal cryopreservation outcomes can lead to significant data variability, loss of valuable genetic lines, and reduced reproductive potential in revitalized embryos. This technical guide provides a systematic framework for diagnosing the critical failure points in cryopreservation protocols, with particular emphasis on embryo toxicity within mouse research. By understanding the mechanisms of cryodamage and implementing rigorous quality control measures, researchers can significantly improve post-thaw recovery rates and maintain the genetic fidelity of preserved specimens.
Understanding the Triad of Cryodamage
The first step in diagnosing cryopreservation failure is recognizing the three primary mechanisms of cellular injury that occur during freezing and thawing processes. These interrelated damage pathways often manifest in combination, creating complex post-thaw viability profiles.
Osmotic Damage: During slow freezing, extracellular ice formation increases solute concentration in the unfrozen fraction, creating a hypertonic environment that drives osmotic water efflux from cells. This dehydration can cause irreversible membrane damage and cellular shrinkage beyond critical volume thresholds [65]. The rate of cooling directly influences the extent of this damage, as insufficient time for dehydration results in intracellular ice formation, while excessive dehydration causes solution effects injury.
Mechanical Damage: Rapid cooling rates prevent adequate cellular dehydration, leading to detrimental intracellular ice nucleation and recrystallization during warming [65]. These ice crystals physically disrupt organelles and compromise membrane integrity through mechanical shearing forces. The large size and low surface-to-volume ratio of mature oocytes and multi-cell embryos make them particularly vulnerable to mechanical cryodamage [66].
Oxidative Damage: The cryopreservation process generates reactive oxygen species (ROS) that oxidize lipids, proteins, and nucleic acids [65]. This oxidative stress triggers apoptotic pathways that may not manifest immediately post-thaw but significantly impact long-term cellular function and developmental potential. Studies on human bone marrow-derived mesenchymal stem cells (hBM-MSCs) have demonstrated increased apoptosis levels persisting for hours after thawing, even when initial viability appears acceptable [67].
Table 1: Primary Cryodamage Mechanisms and Their Cellular Manifestations
| Damage Mechanism | Primary Causes | Key Cellular Effects | Visible Indicators |
|---|---|---|---|
| Osmotic Damage | Slow cooling, improper cryoprotectant concentration | Membrane shrinkage, dehydration, solute toxicity | Shrunken cytoplasm, irregular cell shape |
| Mechanical Damage | Rapid cooling, suboptimal thawing rates | Intracellular ice formation, organelle disruption | Darkened cytoplasm, membrane rupture |
| Oxidative Damage | Temperature fluctuations, inadequate antioxidants | Lipid peroxidation, DNA fragmentation, apoptosis | Delayed cell death, reduced metabolic activity |
Critical Failure Points in the Cryopreservation Workflow
A methodical examination of each cryopreservation workflow stage reveals specific vulnerabilities where suboptimal conditions most frequently compromise outcomes.
Pre-Freeze Specimen Quality and Handling
Specimen condition before freezing fundamentally determines cryopreservation success. Embryos harvested from mice under nutritional stress or of advanced maternal age show significantly reduced post-thaw survival. Research demonstrates that the average age of patients providing oocytes for cryopreservation has increased from 31.8 to 35.4 years over a decade, with a corresponding decline in frozen embryo survival rates from 89% to 81% [66]. Similar trends affect research mice, where donor animal health, hormonal priming, and precise developmental staging critically impact embryo cryotolerance.
The harvesting process itself introduces potential failure points. Over-exposure to enzymatic dissociation agents during cell harvesting can damage surface receptors and membrane integrity. Temperature fluctuations between collection and processing activate stress responses that reduce cryotolerance. For mouse embryos, the developmental stage significantly impacts freezing success; eight-cell embryos generally demonstrate higher post-thaw development rates compared to earlier stages or mature oocytes [16].
Cryoprotectant Toxicity and Permeation Issues
Cryoprotective agents (CPAs) are essential for survival but introduce toxicity risks that must be carefully managed. Dimethyl sulfoxide (DMSO) at 5-10% concentration remains the most common permeable CPA but exhibits concentration-dependent and time-dependent toxicity [65]. Inadequate equilibration time prevents sufficient CPA permeation, resulting in intracellular ice formation, while excessive exposure damages cellular structures.
Different developmental stages and cell types demonstrate markedly different membrane permeability characteristics. Earlier stage embryos are generally less permeable to cryoprotectants like glycerol compared to propylene glycol or ethylene glycol [66]. Individual mature oocytes can vary in permeability by up to 7-fold, creating population heterogeneity in cryotolerance [66]. These differences necessitate stage-specific and cell type-specific optimization of CPA composition, concentration, and exposure duration.
Diagram 1: Cryoprotectant Optimization and Failure Pathways
Controlled-Rate Freezing and Vitrification Parameters
The cooling rate represents perhaps the most technically sensitive cryopreservation parameter. Suboptimal cooling causes either excessive dehydration (too slow) or destructive intracellular ice (too fast). For mouse embryos, a cooling rate of approximately 0.3°C to 0.5°C per minute to temperatures between -30°C and -80°C before transfer to liquid nitrogen has proven successful [66] [16]. However, ideal rates vary by cell type, specimen size, and CPA composition.
Vitrification, an ultrarapid cooling technique that forms a glassy state without ice crystallization, presents different failure points. Inadequate CPA concentrations, suboptimal cooling rates, or volume issues can cause "devitrification" (ice formation during warming) that destroys cellular integrity. Successful vitrification protocols for mouse embryos utilize high CPA concentrations (e.g., 40% ethylene glycol) with sucrose to prevent devitrification [68].
Storage and Thawing Procedures
Even optimal freezing cannot compensate for improper storage or thawing. Storage temperature fluctuations during liquid nitrogen tank maintenance cause ice crystal growth through recrystallization, mechanically damaging cellular structures. The 2018 cryostorage failure at University Hospitals Medical Center, which resulted in the loss of over 4000 embryos and eggs, was attributed in part to alarm system failures during manual liquid nitrogen refilling [69].
Thawing rates must be optimized to complement freezing parameters. Rapid thawing is generally essential for vitrified specimens to prevent devitrification, while slow frozen specimens may require more controlled warming. Improper CPA removal post-thaw creates osmotic shock, damaging recently stabilized membranes. A systematic review of stem cell cryopreservation notes that post-thaw removal of DMSO is critical as residual CPA causes adverse effects in clinical applications, including abdominal cramps, nausea, and cardiac arrhythmias [65].
Quantitative Assessment of Post-Thaw Viability
Comprehensive post-thaw assessment must distinguish between immediate survival and retained functional capacity, as these parameters frequently diverge.
Immediate Post-Thaw Viability and Apoptosis
Standard viability assessment using dye exclusion tests (e.g., Trypan Blue) immediately post-thaw provides limited information, as membrane integrity does not guarantee functional retention. More meaningful assessment includes time-course analysis of viability and apoptosis, as apoptotic pathways activated during cryopreservation may require hours to manifest.
Research on hBM-MSCs demonstrates significantly reduced cell viability immediately post-thaw, with apoptosis levels peaking at 2-4 hours before declining by 24 hours [67]. This delayed apoptosis means that immediate viability assessment alone substantially overestimates true recovery rates. For mouse embryos, morphological integrity immediately post-thaw provides an initial viability indicator, but developmental competence through subsequent cell divisions offers more meaningful data.
Table 2: Post-Thaw Recovery Timeline of hBM-MSCs Following Cryopreservation
| Time Post-Thaw | Viability | Apoptosis Level | Metabolic Activity | Adhesion Potential |
|---|---|---|---|---|
| 0 hours | Significantly reduced | Moderate | Significantly reduced | Significantly reduced |
| 2-4 hours | Beginning recovery | Peak apoptosis | Reduced | Reduced |
| 24 hours | Substantially recovered | Declining, but elevated | Reduced, but improving | Reduced, but improving |
| Beyond 24 hours | Near complete recovery | Approaches normal | Variable recovery | Variable recovery |
Functional Assessment and Developmental Competence
For stem cells and therapeutic applications, functional assays post-thaw are essential. Studies consistently show that cryopreservation reduces metabolic activity and adhesion potential of hBM-MSCs, with these parameters recovering more slowly than simple membrane integrity [67]. Colony-forming unit ability and differentiation potential are variably affected across different cell lines, indicating lineage-specific cryotolerance [67].
For mouse embryos, developmental competence represents the ultimate functional assay. Research comparing fresh and cryopreserved mouse embryos demonstrates that vitrified-thawed embryos can achieve implantation and live offspring rates comparable to fresh embryos in some strains (e.g., 51.7% for vitrified vs. 61.1% for fresh in C57BL/6J) [68]. However, strain-specific variations exist, with BALB/c and ICR strains sometimes requiring protocol modifications due to increased cryosensitivity [68].
In human assisted reproduction, quantitative analysis reveals that fully intact thawed 4-cell embryos implant at rates (16.9%) equivalent to their fresh counterparts (16.6%), while partially damaged embryos show implantation rates directly proportional to blastomere loss [70]. This highlights that proper cryopreservation preserves embryonic potential, with damage primarily manifesting as physical cell loss rather than reduced developmental capacity of surviving cells.
The Scientist's Toolkit: Essential Reagents and Materials
Successful cryopreservation requires carefully selected reagents and equipment, each playing specific protective roles.
Table 3: Essential Research Reagents for Embryo Cryopreservation
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Permeable CPAs | DMSO, Ethylene Glycol, Propylene Glycol, Glycerol | Penetrate cells, reduce ice formation, mitigate freezing point. Ethylene glycol often preferred for mouse embryo vitrification [68]. |
| Non-Permeable CPAs | Sucrose, Trehalose, Ficoll, Proteins (BSA) | Create osmotic gradient, promote dehydration, prevent devitrification. Sucrose concentration critical (0.3-0.9M) [68] [66]. |
| Base Media | PB1, M2, DPBS, DMEM | Provide ionic and pH stability during freezing procedures. Must be serum-free for certain applications. |
| Protein Supplements | Fetal Bovine Serum (FBS), Bovine Serum Albumin (BSA) | Membrane stabilization, antioxidant effects. FBS with 10% DMSO common for cell freezing [71] [67]. |
| Specialized Media | Recovery Cell Culture Freezing Medium, Synth-a-Freeze | Commercially optimized formulations with balanced CPAs for specific cell types. |
| Viability Assays | Trypan Blue, Automated Cell Counters, Apoptosis Kits | Quantify immediate survival and delayed apoptosis. Essential for protocol validation. |
Systematic Diagnostic Approach for Troubleshooting
When facing suboptimal cryopreservation outcomes, a structured diagnostic workflow efficiently identifies root causes and directs corrective actions.
Diagram 2: Systematic Diagnostic Workflow for Cryopreservation Failure
Specimen Quality Control Pathway
The diagnostic pathway begins with pre-freeze quality assessment. Specimens with inherent quality issues will yield poor outcomes regardless of protocol optimization. Monitoring donor animal health, genetic background, and hormonal status provides crucial context. For mouse embryos, the genetic background significantly impacts cryotolerance, with some transgenic lines demonstrating particular sensitivity [16]. Documenting embryo developmental stage and morphological quality before freezing establishes a baseline for post-thaw comparison and helps distinguish pre-existing conditions from cryopreservation-induced damage.
Protocol-Specific Failure Analysis
When pre-freeze quality is confirmed, investigation turns to protocol-specific parameters. Inconsistent outcomes across multiple operators often indicate technique-sensitive steps requiring standardization. Reviewing cryoprotectant preparation records, exposure times, and temperature documentation during processing can reveal deviations. Equipment calibration records for controlled-rate freezers and storage tank fill levels provide critical maintenance data. The catastrophic failure at University Hospitals was attributed to a disabled alarm system during tank maintenance, highlighting the importance of equipment monitoring and safety protocols [69].
Strain and Cell-Type Specific Adjustments
Recognizing intrinsic biological variation is essential for troubleshooting. Different mouse strains show varying sensitivity to cryopreservation protocols; the BALB/c and ICR strains require modified sucrose concentrations (0.9 mol/L) in vitrification solutions compared to other strains [68]. Similarly, research comparing three discrete hBM-MSC cell lines demonstrated variable responses to cryopreservation, with differential effects on differentiation potential and colony-forming ability [67]. This biological variability necessitates cell line-specific and strain-specific protocol validation rather than assuming universal application of standardized methods.
Diagnosing suboptimal cryopreservation outcomes requires methodical investigation of the entire workflow from pre-freeze specimen quality to post-thaw functional assessment. Researchers must recognize that viability immediately post-thaw provides an incomplete picture, with delayed apoptosis and functional impairment often manifesting hours later. The triad of cryodamage—osmotic, mechanical, and oxidative—frequently operates in concert, requiring multi-faceted intervention strategies. By implementing the structured diagnostic approach outlined in this guide, researchers can systematically identify failure points, implement targeted corrections, and significantly improve cryopreservation outcomes. In mouse embryo research, where genetic lines represent years of investment, such rigorous approach to cryopreservation troubleshooting is not merely technical refinement but essential scientific practice.
Cryopreservation of mouse embryos is an indispensable technique in biomedical research, enabling the long-term preservation of valuable genetic strains. The process relies on cryoprotective agents (CPAs) to prevent lethal ice crystal formation during cooling to cryogenic temperatures. However, a significant obstacle remains: CPA toxicity. As CPA concentration increases to achieve effective vitrification (ice-free preservation), so does its damaging effect on biological samples [1]. For mouse embryo research, this toxicity can compromise developmental potential, alter gene expression, and even induce long-term phenotypic effects, threatening the integrity of research outcomes and the preservation of irreplaceable transgenic lines [14] [49]. This technical guide explores advanced toxicity neutralization strategies, specifically focusing on the roles of sugars, antioxidants, and macromolecules, framed within the context of mouse embryo cryopreservation.
Understanding CPA toxicity requires recognizing it as a multifactorial problem. Toxicity can be specific to a particular CPA's chemical properties or a non-specific consequence of its hypertonic presence and its disruption of water's hydrogen-bonding network [1]. For instance, dimethyl sulfoxide (DMSO), a common penetrating CPA, can induce drastic changes in cellular processes and the epigenetic landscape in vitro [72]. Similarly, propylene glycol (PG) in excess of 2.5 M can impair the developmental potential of mouse zygotes by decreasing intracellular pH [1]. The challenge, therefore, is to devise strategies that mitigate these diverse damage pathways without compromising the cryoprotective efficacy essential for successful vitrification.
Core Mechanisms of Cryoprotectant Toxicity
A deep understanding of the injury mechanisms is a prerequisite for developing effective neutralization strategies. The damage incurred during cryopreservation is not monolithic but occurs through several distinct yet interconnected pathways.
Specific Molecular Toxicity
Each penetrating CPA exhibits a unique profile of biochemical injuries. DMSO, for example, at concentrations above 1.41 M (10% vol/vol) can cause irreversible ultrastructural alterations in rat myocardium at 30°C, with osmotic stress and direct blocking of membrane channel proteins suggested as explanations [1]. Glycerol, meanwhile, can deplete reduced glutathione in the kidney, leading to oxidative stress [1]. For mouse embryos, such specific toxicities can manifest as reduced blastocyst formation rates or altered metabolic function.
Osmotic Stress
The addition and removal of CPAs subject cells to severe volumetric changes. If not carefully controlled, these changes can cause lethal mechanical damage to cell membranes and cytoskeletal structures. This osmotic shock is a critical consideration during the loading and unloading of CPAs in any embryo cryopreservation protocol [72].
Oxidative Stress
The freeze-thaw process can promote the generation of reactive oxygen species (ROS). This leads to oxidative stress, a key mediator of sublethal cryodamage, resulting in lipid peroxidation, protein dysfunction, and DNA damage [14] [72]. The susceptibility of mouse embryos to oxidative stress makes this a primary target for intervention.
Apoptosis Activation
Cryoinjury can trigger programmed cell death pathways. Studies on dissociated human embryonic stem cells have shown that apoptotic pathways are a significant reason for low recovery rates after cryopreservation [72]. This mechanism is highly relevant to preimplantation embryo survival.
Table 1: Primary Damage Pathways in Embryo Cryopreservation
| Damage Pathway | Key Manifestations | Impact on Mouse Embryos |
|---|---|---|
| Specific Molecular Toxicity | Altered intracellular pH; enzyme inhibition; cytoskeletal polymerization [1]. | Arrested development; impaired blastocyst formation [1] [56]. |
| Osmotic Stress | Cell swelling/shrinking; membrane rupture [72]. | Lysis of blastomeres; loss of structural integrity. |
| Oxidative Stress | Lipid peroxidation; protein carbonylation; DNA strand breaks [14]. | Reduced mitochondrial function; compromised developmental potential [1]. |
| Apoptosis Activation | Caspase activation; phosphatidylserine externalization [72]. | Low post-thaw cell survival and recovery rates. |
Toxicity Neutralization Strategies
To counter the aforementioned damage pathways, three strategic approaches have shown significant promise: the use of non-penetrating saccharides, the application of antioxidants, and the deployment of functional macromolecules.
Saccharides as Non-Penetrating Cryoprotectants
Natural saccharides are a broad class of biomolecules—including monosaccharides (e.g., glucose), disaccharides (e.g., sucrose, trehalose), and polysaccharides—that provide cryoprotection primarily from outside the cell [73]. Their mechanisms are multi-faceted and powerful for protecting embryos.
- Colligative Action & Ice Crystal Inhibition: Saccharides lower the freezing point of water and reduce the amount of ice formed at any given temperature through colligative properties. More importantly, they inhibit ice recrystallization during thawing, a primary source of physical damage [73].
- Stabilization of Macromolecules and Membranes: Saccharides are known to act as "water substitutes," forming hydrogen bonds with phospholipid heads and proteins in the absence of hydration water. This stabilizes the native structure of membranes and proteins against dehydration-induced denaturation [73]. Trehalose, a non-reducing disaccharide, is particularly effective in this role.
- Mitigation of Osmotic Shock: When used in combination with penetrating CPAs like DMSO or PG, saccharides can help balance osmotic pressure, reducing the extreme volumetric shifts that embryos experience during CPA equilibration [72].
In practice, sucrose is widely used as a non-penetrating CPA in mouse embryo vitrification solutions. It helps to shrink the embryo osmotically before the addition of penetrating CPAs, reducing the required concentration of the more toxic agents and providing protection during dilution post-thaw [56] [49].
Antioxidants for Oxidative Stress Management
Integrating antioxidants into cryopreservation media directly counteracts the oxidative stress induced by the freeze-thaw cycle.
- Targeting Lipid Peroxidation: The peroxidation of membrane lipids is a key consequence of oxidative stress. Antioxidants such as reduced glutathione (GSH) can mitigate this damage, preserving membrane integrity and function. Studies have linked GLY-induced renal toxicity to a depletion of reduced glutathione, underscoring its importance [1].
- Preservation of Mitochondrial Function: The mitochondria are both a source and a target of ROS. The addition of antioxidants to the cryopreservation medium has been shown to improve post-thaw outcomes by maintaining mitochondrial membrane potential and ATP production, which are critical for embryo development [1] [72].
Table 2: Experimentally Supported Reagent Solutions for Toxicity Neutralization
| Reagent / Solution | Category | Primary Function | Example Application in Mouse Embryo Cryopreservation |
|---|---|---|---|
| Sucrose | Non-penetrating Saccharide | Osmotic buffer; ice crystal inhibitor; stabilizes membranes/proteins [73]. | Standard component of vitrification and thawing solutions (e.g., 0.2-0.5 M) [56]. |
| Trehalose | Non-penetrating Saccharide | Superior membrane and protein stabilizer via water substitution [73]. | Investigated as a supplement to standard cryopreservation media. |
| Reduced Glutathione (GSH) | Antioxidant | Scavenges ROS; mitigates lipid peroxidation; supports redox state [1]. | Additive to pre-culture or post-thaw recovery media (concentration range 1-5 mM). |
| DAP213 Solution | Permeating CPA Mix | Combines DMSO, Acetamide, and Polyethylene glycol for lower toxicity vitrification [56]. | Cryopreservation solution for one-cell stage mouse embryos [56]. |
| Polyethylene Glycol (PEG) | Macromolecule | Modifies ice crystal growth; inhibits recrystallization; stabilizes cell surfaces [72]. | Component of DAP213 solution; used in novel polymer-based formulations. |
| KSOM Medium | Culture Medium | Optimized for preimplantation embryo development post-thaw. | Standard medium for post-thaw culture of mouse embryos [56]. |
Functional Macromolecules as Ice-Recrystallization Inhibitors
A newer class of cryoprotectants includes synthetic polymers and bio-inspired macromolecules that address physical damage from ice.
- Inhibition of Ice Recrystallization: During the thawing process, small ice crystals can fuse into larger, more damaging ones. Synthetic polymers like poly(vinyl alcohol) and certain amphipathic polymers have been shown to effectively inhibit this ice recrystallization, a mechanism distinct from traditional CPAs [72]. This allows for improved recovery even when the concentration of toxic penetrating CPAs is reduced.
- Membrane Stabilization: Some macromolecules can interact with the outer leaflet of the cell membrane, providing a stabilizing scaffold that helps the membrane withstand the physical stresses of freezing and thawing [72].
Integrated Experimental Workflows
The successful application of these strategies requires their integration into robust and reproducible experimental protocols. The following workflow, adapted from a screening study for mouse embryonic developmental factors, provides a template for evaluating cryopreservation outcomes [56].
Detailed Protocol: Cryopreservation of One-Cell Stage Mouse Embryos
Animal Model and Embryo Preparation:
- Use 4-week-old C57BL/6N female mice. Induce ultra-superovulation via intraperitoneal injection of HyperOva. Follow with 7.5 IU of human chorionic gonadotropin (hCG) 48 hours later [56].
- Harvest oocytes from oviducts 16 hours post-hCG. Perform in vitro fertilization in HTF medium. Four hours after fertilization, remove excess sperm and prepare the resulting one-cell stage embryos for cryopreservation [56].
Cryopreservation and Thawing:
- CPA Loading: Expose embryos to a cryoprotectant solution. An example is a solution containing 1 M DMSO, potentially supplemented with sucrose (e.g., 0.25 M) for toxicity mitigation and osmotic control [56].
- Vitrification: Use the "DAP213" method, which involves a brief incubation (2 minutes) in a solution of 2 M DMSO, 1 M acetamide, and 3 M propylene glycol at room temperature, before plunging into liquid nitrogen. The combination of CPAs can lower overall individual CPA toxicity [56].
- Thawing and Dilution: Rapidly thaw embryos by placing them in 0.25 M sucrose solution. Perform two washes in KSOM medium to gradually remove the penetrating CPAs. The sucrose in the thawing solution acts as an osmotic buffer to prevent swelling from the rapid influx of water as CPAs leave the cells [56].
Viability and Toxicity Assessment:
- Developmental Rate: Culture thawed embryos in KSOM medium and calculate the developmental rate as (Number of developed embryos / Total number of embryos) × 100. Monitor development to the 2-cell, 4-cell, morula, and blastocyst stages over several days [56].
- Comprehensive Viability Assays: Beyond morphology, employ more sensitive assays to detect subtler toxicity. These can include:
- Immunofluorescence Staining: For specific protein targets (e.g., CTSD, CXCR2) to assess cellular integrity and function [56].
- Mitochondrial Function Assays: Measure membrane potential, ATP levels, and ADP/ATP ratios, as these are sensitive indicators of CPA-induced stress [1].
- Long-Term Phenotypic Studies: Monitor offspring for any delayed effects on morphology, physiology, or behavior, as cryopreservation has been associated with such outcomes in senescence-accelerated mice [14].
Data Presentation and Analysis
Rigorous quantification is essential for evaluating the efficacy of any toxicity neutralization strategy. The following table summarizes key quantitative findings from the literature, providing a benchmark for comparison.
Table 3: Quantitative Data on Cryoprotectant Effects and Neutralization Strategies
| CPA / Strategy | Concentration | Biological System | Key Quantitative Outcome | Source |
|---|---|---|---|---|
| Propylene Glycol (PG) | > 2.5 M | Mouse Zygotes | Decreased developmental potential via intracellular acidification. | [1] |
| DMSO | 7.5% to 10% | Peripheral Blood Progenitor Cells | Reduction in clonogenic potential. | [1] |
| Glycerol | > 1.5% | Stallion Spermatozoa | Polymerization of actin cytoskeleton. | [1] |
| Sucrose-Sorbitol Mix | 4% each | Ling Cod Surimi (Food Model) | Optimal cryoprotection; preserved protein integrity and texture. | [73] |
| Embryo Cryopreservation | N/A | Senescence-Accelerated Mice | Significant differences in morphophysiological/behavioral features in elderly subjects. | [14] |
| Inhibitor Screening | 1 µM | Mouse One-Cell Embryos | Identified 16 factors (e.g., p53, Cathepsin D) arresting development. | [56] |
The relationship between the core damage pathways and the corresponding neutralization strategies can be visualized as an integrated defense network.
The neutralization of cryoprotectant toxicity is a multifaceted challenge that demands a multi-pronged solution. As detailed in this guide, the integrated use of non-penetrating saccharides, antioxidants, and functional macromolecules presents a powerful strategy to protect mouse embryos from the specific molecular, osmotic, oxidative, and physical injuries inherent to the cryopreservation process. The experimental workflows and quantitative data provided offer a roadmap for researchers to implement and validate these strategies in their own work.
The future of cryopreservation lies in the rational design of next-generation solutions. This includes the application of bottom-up molecular modeling to predict CPA-biomolecule interactions, library-based discovery approaches to rapidly screen novel cryoprotectants, and the adoption of advanced materials science tools to create synthetic ice-shaping polymers [72]. Furthermore, techniques like magnetic nanoparticle heating for ultra-rapid nanowarming are emerging as methods to reduce overall CPA requirements by minimizing ice crystallization during thawing, thereby directly lowering the toxic load [72]. By embracing these innovative chemical and physical approaches, the field can move closer to the ultimate goal of true toxicity-neutral cryopreservation, ensuring the flawless long-term preservation of mouse models that are critical to advancing biomedical research.
The successful cryopreservation of mouse embryos and oocytes represents a cornerstone of biomedical research, enabling advanced studies in genetics, drug development, and reproductive biology. At the heart of this technique lies the precise control of thermal dynamics during cooling and warming processes. The fundamental objective is to transition biological materials to and from a state of suspended animation at ultra-low temperatures without incurring lethal damage from ice crystal formation [74]. When properly executed, this process effectively halts all biochemical and metabolic activities, preserving cellular viability indefinitely [74].
The formation of more than trace amounts of intracellular ice is universally lethal to cells, with calculations suggesting the limiting amount is as little as 2-4% of cellular water content [75]. Two primary approaches have emerged to avoid this fate: slow equilibrium freezing and vitrification. Slow freezing relies on controlled dehydration of cells during gradual cooling, while vitrification uses high concentrations of cryoprotectants combined with rapid cooling to achieve a glass-like, non-crystalline state [76] [75]. Both methods present distinct challenges in managing thermal dynamics, with cooling and warming rates representing critical variables that ultimately determine preservation success.
Fundamental Principles of Thermal Dynamics in Cryobiology
Defining the Thermal Spectrum
In cryopreservation science, thermal rates fall into distinct categories with specific technical definitions. Rapid cooling, often referred to in the literature as vitrification, involves temperature reduction typically at rates exceeding -2,500°C/min before storage in liquid nitrogen at -196°C [76]. In practice, advanced vitrification procedures achieve even more extreme rates ranging from -10,000°C/min to -50,000°C/min [76]. In contrast, slow cooling employs gradual temperature reduction at rates of -0.1°C/min to -3°C/min to -30°C or lower before final storage [76]. This method promotes extracellular ice crystal formation while minimizing intracellular freezing through controlled dehydration.
The terminology surrounding warming processes requires similar precision. Warming (often incorrectly called "thawing" or "rewarming") refers to the rapid increase in temperature of cells stored in liquid nitrogen to room temperature or above under defined laboratory conditions [76]. The rate of this warming process has emerged as a potentially more critical factor than cooling rates for ensuring cellular survival [75].
The Physics of Ice Formation and Avoidance
Vitrification represents a physical process wherein aqueous solutions transition to an amorphous, glass-like solid without forming crystalline ice structures [76]. This phenomenon depends on an interplay of four key variables: cooling rate, warming rate, solution viscosity, and sample volume [76]. The relationship between these variables can be expressed through the following conceptual equation:
Vitrification Success = f(Cooling Rate, Warming Rate, Viscosity, Volume)
Current rapid-cooling vitrification procedures expose cells suspended in minimal volumes (typically 1-3μL) to high concentrations of cryoprotectants for brief periods, followed by rapid cooling in liquid nitrogen [76]. The high osmolarity of vitrification solutions rapidly dehydrates the cell, and submersion into liquid nitrogen quickly solidifies the cell so remaining intracellular water doesn't form damaging ice crystals [76]. The cell undergoes a temperature transition from room temperature to -196°C in less than 2 seconds, resulting in extremely fast cooling rates [76].
During warming, the threat of recrystallization emerges as a primary concern. As the sample warms, existing microscopic ice nuclei can grow into larger, damaging crystals through a process called recrystallization [75]. The lethality of slow warming is a direct consequence of allowing time for the development and growth of small intracellular ice crystals by this mechanism [76] [75]. This understanding has led to a paradigm shift in cryobiology, with increasing recognition that warming rate may be more critical than cooling rate for successful recovery of vitrified samples [77].
Quantitative Analysis of Cooling and Warming Rate Effects
The Dominance of Warming Rate
Groundbreaking research has systematically isolated the relative contributions of cooling and warming rates to oocyte survival. In a comprehensive study examining mouse oocyte vitrification, investigators tested cooling rates ranging from 37°C/min to 1,827°C/min paired with warming rates from 139°C/min to 2,950°C/min [75]. The results demonstrated unequivocally that warming rate exerts a more powerful influence on survival outcomes than cooling rate.
Table 1: Survival Rates of Vitrified Mouse Oocytes at Different Thermal Rates
| Cooling Rate (°C/min) | Warming Rate (°C/min) | Survival Rate (%) |
|---|---|---|
| 37-1,827 | 139 | ~0% |
| 187 | 2,950 | >80% |
| 1,827 | 2,950 | >80% |
When samples were warmed at the highest rate (2,950°C/min), survivals exceeded 80% across the entire range of cooling rates from 187°C/min to 1,827°C/min [75]. Conversely, when samples were warmed at the lowest rate (139°C/min), survivals plummeted to near 0% regardless of the cooling rate employed [75]. This demonstrates that ultra-rapid warming can compensate for suboptimal cooling, but even excellent cooling cannot overcome the damage caused by slow warming.
Thermal Rate Thresholds in Embryo Development
Beyond the cryopreservation process itself, thermal conditions during embryo culture significantly impact developmental competence. Research using mouse models has demonstrated that temperature variations mimicking physiological conditions can either support or disrupt embryonic development.
Table 2: Effects of Temperature Variation on Mouse Embryo Development
| Temperature Protocol | Developmental Rate | Blastocyst Quality | Gene Expression Changes |
|---|---|---|---|
| Constant 37°C (Control) | Normal | Good | Baseline |
| 37°C day/35.5°C night (T1) | Slow cleavage | Poor | ↑ Apaf1 (apoptotic gene) |
| 38.5°C day/37°C night (T2) | Normal | Good | Similar to control |
The lower-temperature group (T1) showed consistent negative effects on mouse embryo development with "slow" cleaving embryos, poor-quality blastocysts, higher expression of the apoptotic gene Apaf1, and metabolic profiles indicating cellular stress [78]. Conversely, the higher-temperature group (T2) showed results comparable to the control group, with no adverse effects on blastocyst viability [78]. This suggests that mouse embryos tolerate slight temperature increases better than decreases during in vitro culture.
Molecular Mechanisms of Thermal Damage
Cellular Stress Pathways
Thermal stress during cryopreservation activates multiple cellular damage pathways. Research on Sepiella japonica embryos revealed that temperature extremes significantly influence the expression of autophagy-related genes (LC3, BECN1, Inx4) and apoptosis marker genes (Cas3, p53) [79]. These molecular responses correlate strongly with observed mortality and malformation rates, highlighting the intricate relationship between thermal conditions and cellular stress mechanisms.
Autophagy and apoptosis often coexist during embryonic development under thermal stress [79]. Apoptosis, known as type I programmed cell death, significantly influences organism development, cell renewal, and internal environment stability [79]. Studies across multiple species have found that excessively high or low temperatures can trigger cell apoptosis, resulting in abnormal physiological activities [79].
Heat Shock Response
Mouse embryoid bodies (mEBs) exposed to heat shock conditions (39°C or 41°C) demonstrated delayed expression of key germ layer markers and increased cell death [80]. Heat shock also triggered the production of heat shock proteins (HSP70 and HSP72), which function as molecular chaperones to protect cells from heat stress by preventing protein misfolding and cellular apoptosis [80]. This stress response represents a fundamental cellular defense mechanism against thermal damage.
Thermal Damage Pathways in Cryopreservation
Experimental Protocols for Thermal Rate Optimization
Vitrification Methodology for Mouse Oocytes
A proven protocol for investigating thermal rate effects on mouse oocytes utilizes the EAFS 10/10 vitrification solution [75]. This solution consists of 10% (v/v) ethylene glycol (EG) and 10.7% (w/v) acetamide dissolved in a stock containing 30% (w/v) Ficoll 70 and 0.5 M sucrose in PB1 medium [75]. The final concentrations are 0.4 M sucrose and 24% (w/v) Ficoll, creating an optimized environment for vitrification while minimizing cryoprotectant toxicity.
The procedural workflow begins with collecting ovulated unfertilized oocytes from superovulated mature female ICR mice at 13 hours post-hCG injection [75]. Oocytes are freed from cumulus cells by suspension in modified phosphate-buffered saline (PB1) containing 0.5 mg/ml hyaluronidase followed by washing with fresh PB1 medium [75]. For vitrification, oocytes are maintained at 25°C while successive solutions are aspirated into 0.25-ml straws: a 60 mm column of PB1 medium containing 0.5 M sucrose, a 20 mm column of air, and a specific column of EAFS 10/10 solution containing the oocytes [75]. This method enables systematic testing of different cooling and warming rate combinations.
Thermal Rate Measurement and Validation
Precise quantification of thermal rates requires rigorous measurement protocols. Temperature validation should be performed prior to data collection using validated thermometers and gas analyzers [78]. For time-lapse culture studies investigating temperature variation effects, embryos can be cultured in specialized incubators with precisely controlled temperature settings that can be programmed to change at specific times (e.g., 9 am and 9 pm) to simulate circadian rhythms [78]. Each embryo is typically captured with an in-built camera every 15 minutes at multiple focal planes to track developmental progress [78].
Thermal Rate Experimental Workflow
Advanced Technologies for Thermal Rate Control
High-Intensity Focused Ultrasound (HIFU) Warming
Emerging technologies offer promising alternatives for achieving ultra-rapid warming rates. High-Intensity Focused Ultrasound (HIFU) has demonstrated potential as a scalable rewarming technology capable of preventing recrystallization in cryopreserved systems [77]. Proof-of-concept studies using the nematode Caenorhabditis elegans have successfully revived adult worms preserved at -80°C after HIFU-mediated warming [77].
The great advantage of HIFU technology is its scalability and compatibility with real-time monitoring through MRI thermography [77]. The attenuation and penetrability of ultrasound is frequency-dependent, with lower frequencies (e.g., 1 MHz) enabling deeper tissue penetration [77]. For large-sized samples, arrays of transducers can enhance effective wave penetration and scalability by controlling relative phases of each channel's wave, accommodating biomaterial inhomogeneities in real time [77].
Novel Cryodevice Engineering
Microvolume cryopreservation devices have been engineered to maximize thermal transfer rates. At least 30 different carrier tools have been described, with approximately 15 versions commercially available [76]. Most represent modifications of initially introduced carrier tools, including:
- Open Pulled Straw (OPS): Enables minimal volume (1-2μL) vitrification [76]
- Cryoloop: Uses a small nylon loop to suspend samples in minimal fluid [76]
- Cryotop: Features a thin plastic strip for ultra-thin film vitrification [76]
These devices achieve extremely fast cooling rates (greater than -10,000 to -50,000°C/min) when plunged into liquid nitrogen from room temperature, primarily through minimal volume design and direct contact with liquid nitrogen [76]. While open systems generally provide faster thermal rates, closed systems have been developed to address potential contamination concerns [76].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Thermal Rate Studies
| Reagent/Device | Function | Application Notes |
|---|---|---|
| Ethylene Glycol (EG) | Permeating cryoprotectant | Often used at 10% concentration in EAFS 10/10 solution [75] |
| Dimethyl Sulfoxide (DMSO) | Permeating cryoprotectant | Common component in vitrification solutions; potential toxicity concerns [76] |
| Acetamide | Permeating cryoprotectant | Used in EAFS 10/10 at 10.7% concentration [75] |
| Ficoll 70 | Non-permeating polymer | Provides viscosity for glass formation; 24% final concentration in EAFS [75] |
| Sucrose | Non-permeating osmolyte | Facilitates dehydration; 0.4 M final concentration in EAFS [75] |
| Open Pulled Straw (OPS) | Microvolume cryodevice | Enables cooling rates >10,000°C/min [76] |
| Cryotop System | Microvolume cryodevice | Mass-marketed commercial system; technically challenging [76] |
| High-Intensity Focused Ultrasound | Alternative warming technology | Scalable rewarming with MRI thermography monitoring [77] |
The precise control of cooling and warming rates represents a fundamental determinant of success in mouse embryo and oocyte cryopreservation. While both thermal parameters are important, compelling evidence demonstrates that warming rate exerts a more powerful influence on survival outcomes than cooling rate. The lethal effects of slow warming, primarily mediated through ice recrystallization, cannot be overcome by even the most optimized cooling protocols. This understanding necessitates a paradigm shift in cryopreservation research, with increased emphasis on developing technologies capable of achieving ultra-rapid, uniform warming throughout biological samples.
Future advancements in thermal rate control will likely emerge from interdisciplinary approaches combining novel materials science, engineering innovations, and molecular biology. Promising directions include the refinement of HIFU warming technologies, development of next-generation cryoprotectant cocktails with reduced toxicity, and engineering of smart cryodevices that optimize heat transfer while minimizing sample volume. Furthermore, elucidation of the precise molecular mechanisms linking thermal stress to cellular damage will enable targeted interventions that enhance cryotolerance. As these technologies mature, researchers will gain unprecedented control over thermal dynamics, ultimately expanding the applications and improving the reliability of mouse embryo cryopreservation for biomedical research and drug development.
In mouse reproductive technologies, the genetic background of the model strain is a critical determinant of success in embryo and sperm cryopreservation. Research consistently demonstrates significant variation in how different mouse strains respond to identical cryopreservation protocols, particularly in their tolerance to cryoprotectant agents (CPAs) and freezing procedures. This technical guide examines the molecular and physiological basis for these differences and provides strain-adapted protocols to optimize viability and developmental competence. The core challenge lies in the balance between achieving sufficient cryoprotection to prevent ice crystal formation while minimizing the toxic effects of CPAs, a balance that varies considerably across genetically diverse mouse strains [81] [1].
Understanding these strain-specific responses is essential for establishing reliable biobanking practices and ensuring reproducible research outcomes. The placenta serves as a crucial regulator of intrauterine fetal development, playing a vital role in nutrient exchange, and compromised placental function underlies various perinatal complications observed in assisted reproductive technologies [82]. Recent studies have revealed that alterations in placental gene expression, particularly in imprinted genes, differ significantly between in vitro manipulated embryos and naturally conceived counterparts, with these effects potentially modulated by genetic background [82].
Strain-Specific Responses to Cryoprotectants
Quantitative Analysis of Strain Variations
Extensive research has documented substantial differences in cryopreservation outcomes across common laboratory mouse strains. These variations manifest in survival rates, fertilization capability post-thaw, and embryonic development. The C57BL/6J strain, one of the most widely used inbred lines, presents particular challenges for sperm cryopreservation, showing markedly lower post-thaw fertilization rates compared to other strains like the outbred Y3F mice [83].
Table 1: Strain-Specific Responses to Sperm Cryopreservation Protocols
| Mouse Strain | Cryoprotectant Formulation | Post-Thaw IVF Rate | Key Observations | Citation |
|---|---|---|---|---|
| C57BL/6J | R18S3 + 15-20% egg yolk supernatant | 36-40% | Highest success with non-permeating protectants | [83] |
| C57BL/6J | R18S3 + 1-6% glycerol | 6-18.1% | Concentration-dependent toxicity observed | [83] |
| C57BL/6J | Glycerol (various concentrations) | Significant strain variation reported | High sensitivity to chemical toxicity | [81] |
| Y3F (outbred) | R18S3 alone | 52.2% | Better inherent cryosurvival than C57BL/6J | [83] |
The toxicity of CPAs exhibits both general and strain-specific patterns. While high concentrations of penetrating CPAs like dimethylsulfoxide (DMSO), ethylene glycol (EG), propylene glycol (PG), and glycerol can eliminate ice formation, they become increasingly toxic as concentration increases [1]. The molecular mechanisms underlying this toxicity may involve disruption of hydrogen bonding between water molecules, interference with membrane channel proteins, induction of oxidative stress, and apoptosis activation [1]. The sensitivity to these mechanisms varies by genetic background, necessitating customized approaches.
Molecular Mechanisms of Differential Cryoprotectant Toxicity
The variation in strain responses to cryopreservation protocols stems from fundamental differences in cellular and molecular physiology. Membrane composition, including cholesterol-to-phospholipid ratios and saturated-to-unsaturated fatty acid balances, differs between strains and significantly affects membrane fluidity and permeability to CPAs [81]. These biophysical properties directly influence a cell's susceptibility to osmotic shock and cold-induced damage.
Metabolic characteristics also contribute to strain-specific responses. Differences in mitochondrial function, ATP production, and antioxidant capacity affect how cells manage the metabolic stresses imposed by cryopreservation. Studies on zebrafish ovarian follicles have demonstrated that cryopreservation with methanol causes dose-dependent reductions in multiple mitochondrial function parameters, including membrane potential, ATP levels, and mitochondrial DNA copy number [1]. Genetic backgrounds with inherently lower mitochondrial resilience would manifest greater sensitivity to such insults.
Additionally, strain variations in the expression of imprinted genes, which play pivotal roles in placental and fetal development, may explain differences in postnatal outcomes following embryo cryopreservation. Research has shown that both fresh embryo transfer (Fresh-ET) and frozen embryo transfer (FET) disrupt imprinted gene expression in placenter, though the specific patterns of alteration differ between procedures [82].
Adapted Protocols for Different Mouse Strains
C57BL/6J Sperm Cryopreservation Protocol
The C57BL/6J strain presents particular challenges for sperm cryopreservation, requiring specifically optimized protocols to achieve acceptable post-thaw viability and fertilization rates.
Table 2: Optimized Cryoprotectant Formulations for C57BL/6J Mouse Sperm
| Component | Concentration Range | Optimal Concentration | Function | Performance (IVF Rate) |
|---|---|---|---|---|
| Egg yolk supernatant | 5-25% | 15-20% | Non-permeating protectant, membrane stabilization | 36-40% |
| Glycerol | 1-6% | 1-2% | Permeating cryoprotectant, reduces ice formation | 16.9-22.9% (in combination) |
| R18S3 base medium | 100% | 100% | Base cryopreservation medium | 25% |
Detailed Methodology:
Sperm Collection and Preparation: Collect sperm from bilateral epididymides of 12-16 week old C57BL/6J male mice. Place fresh semen in a droplet of CYTH medium for 30 minutes before processing [82].
Cryoprotectant Formulation: Prepare the optimal cryoprotectant by adding 15-20% egg yolk to R18S3 base medium followed by centrifugation. Use the supernatant as the cryoprotectant medium without additional glycerol [83].
Cooling and Thawing Procedures: Implement controlled cooling rates between 5-50°C/min, as studies indicate C57BL/6J sperm exhibits specific sensitivity to cooling velocity [81]. For thawing, use a rapid warming method (approximately 500°C/min) to minimize recrystallization damage.
Post-Thaw Assessment and IVF: After thawing, assess sperm motility and membrane integrity. For in vitro fertilization, use oocytes from 6-8 week old C57BL/6J females superovulated with PMSG (5IU) and HCG (10IU) with a 46-48 hour interval between injections [82].
The avoidance of high glycerol concentrations is particularly important for this strain, as research demonstrates that glycerol in concentrations over 1.5% polymerizes the actin cytoskeleton in sensitive cell types, an effect unrelated to osmolality [1]. For C57BL/6J sperm, formulations using both yolk and glycerol yield lower success rates than those using yolk alone, though they still perform better than glycerol-only formulations [83].
Embryo Cryopreservation and Strain Considerations
While this guide focuses primarily on sperm cryopreservation, embryo cryopreservation also demonstrates strain-specific considerations. Vitrification procedures using non-constant high concentrations of CPAs with rapid temperature changes have largely replaced slow-freezing methods for embryos [84]. However, the high concentrations of DMSO and other CPAs used during vitrification may exert strain-dependent toxic effects on embryos [84].
For embryo cryopreservation across different strains, consider:
Strain-Specific CPA Sensitivities: Test multiple CPAs (DMSO, EG, PG, glycerol) at varying concentrations to identify optimal formulations for each strain.
Developmental Stage Optimization: Certain strains may show better survival when cryopreserved at specific embryonic stages (zygote, 2-cell, blastocyst).
In Vitro Culture Conditions: Post-thaw culture media may require optimization for different strains to support continued development.
Research has shown that even within standardized protocols, cryopreservation duration affects outcomes differently across genetic backgrounds. While prolonged storage of vitrified embryos negatively impacts survival rates and clinical pregnancy rates across all strains, the magnitude of this effect varies [84].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Mouse Strain Cryopreservation Research
| Reagent/Category | Specific Examples | Function/Application | Strain-Specific Considerations |
|---|---|---|---|
| Permeating CPAs | DMSO, EG, PG, Glycerol, Butanediol | Penetrate cell membranes, reduce intracellular ice formation | C57BL/6J shows high glycerol sensitivity; DMSO preferred for some strains |
| Non-Penetrating CPAs | Sugars (trehalose, raffinose), egg yolk fractions | Extracellular protection, membrane stabilization | Egg yolk (15-20%) optimal for C57BL/6J sperm |
| Base Media | R18S3, HTF, KSOM, CYTH | Supportive chemical environment during processing | KSOM enhances preimplantation development for sensitive strains [81] |
| Metabolic Additives | Oxyrase (E. coli membrane preparation) | Reduces oxygen concentration, decreases oxidative stress | Enhances C57BL/6J sperm survival post-thaw [81] |
| Assessment Tools | Mitochondrial function assays, viability stains, motility analysis | Quantify post-thaw recovery and functionality | Strain-specific reference ranges needed for accurate interpretation |
Decision Framework for Protocol Adaptation
The following workflow diagram illustrates the systematic approach to adapting cryopreservation protocols based on genetic background:
Diagram 1: Protocol Adaptation Workflow for Different Mouse Strains. This decision framework outlines a systematic approach to customizing cryopreservation protocols based on genetic background assessment and known strain sensitivity parameters.
Genetic background significantly influences cryopreservation success in mouse models, necessitating customized approaches for different strains. The C57BL/6J strain, in particular, requires specialized protocols that minimize exposure to permeating cryoprotectants like glycerol while leveraging non-permeating alternatives such as egg yolk fractions. These adaptations address the fundamental differences in membrane composition, metabolic function, and stress response pathways that underlie strain-specific variations in cryosurvival.
Future research directions should focus on elucidating the specific genetic determinants of cryotolerance, potentially identifying key regulatory genes that could be targeted to enhance cryosurvival across strains. Additionally, further investigation into the molecular mechanisms behind CPA toxicity may yield novel cryoprotectant formulations that maintain protective efficacy while reducing strain-specific toxic effects. As the field advances, developing comprehensive databases of strain-specific optimization parameters will be invaluable for the research community, ensuring both the preservation of valuable genetic resources and the reproducibility of scientific studies involving mouse models.
In the field of mouse research, embryo cryopreservation is an indispensable tool for safeguarding valuable genetic resources, managing colony costs, and ensuring the reproducibility of biomedical studies [49]. However, the toxicity induced by cryopreservation procedures remains a significant challenge, potentially compromising embryo viability and developmental potential, which in turn can confound experimental outcomes [85] [86]. The core of this problem lies in the phase change of water, where ice formation and the requisite cryoprotective agents (CPAs) act as primary sources of injury [87] [72]. This whitepaper delves into two advanced, interconnected approaches poised to mitigate these detrimental effects: ice nucleation control and soft matter applications. By examining the latest research and techniques, this document provides a technical guide for researchers and scientists aiming to optimize embryo cryopreservation protocols, thereby enhancing reliability in drug development and basic research.
Fundamental Cryoinjuries and the Need for Advanced Control
Understanding the specific mechanisms of cryoinjury is paramount for developing effective preservation strategies. For mouse embryos, damage primarily occurs through two physical pathways and one biochemical pathway.
- Intracellular Ice Formation (IIF): At high cooling rates, intracellular water does not have sufficient time to efflux, leading to lethal intracellular ice crystallization that disrupts cellular structures [85] [17].
- Solution Effects and Osmotic Shock: At slow cooling rates, extracellular ice formation concentrates solutes and CPAs. This creates an osmotic gradient, drawing water out of the cell and causing excessive dehydration, membrane damage, and solute toxicity [85] [86].
- Oxidative Stress: The cryopreservation process itself, including CPA exposure and temperature shifts, can generate excessive reactive oxygen species (ROS) [86]. This oxidative stress leads to lipid peroxidation, protein oxidation, and DNA damage, further compromising embryo viability and developmental potential.
The following table summarizes the primary damage mechanisms and their consequences for the embryo.
Table 1: Primary Cryoinjury Mechanisms in Embryo Cryopreservation
| Damage Mechanism | Conditions Favored | Consequences for Embryos |
|---|---|---|
| Intracellular Ice Formation (IIF) | Rapid cooling rates | Physical disruption of organelles, cytoskeleton, and membranes; fatal cell injury [85] [87] |
| Solution Effect & Osmotic Shock | Slow cooling rates | Cellular dehydration and shrinkage; solute concentration-induced toxicity; membrane damage [85] [17] |
| Oxidative Stress | Freeze-thaw cycle, CPA exposure | Lipid peroxidation, protein dysfunction, DNA damage, and impaired developmental potential [86] |
The Critical Role of Controlled Ice Nucleation
Ice nucleation is the initial step in ice formation. Left uncontrolled, it is a significant source of sample-to-sample variability and cell death [88]. Controlled ice nucleation (also known as ice seeding) deliberately initiates freezing at a specified, elevated sub-zero temperature (e.g., -5°C to -10°C). This intervention standardizes the process and mitigates the damaging effects of supercooling.
- The Problem of Supercooling: Under uncontrolled conditions, aqueous solutions can supercool significantly below their equilibrium freezing point before nucleation occurs spontaneously [88] [86]. When this supercooled water finally freezes, it does so rapidly and explosively, leading to widespread ice crystallization that is particularly damaging to sensitive biological samples like embryos.
- Mechanism of Benefit: By initiating ice formation at a higher temperature, controlled nucleation minimizes supercooling. This allows for a slower, more orderly progression of ice growth in the extracellular space. Consequently, water has more time to leave the cell osmotically, reducing the probability of lethal intracellular ice formation during subsequent cooling [88]. This process is a cornerstone of slow freezing protocols and is critical for standardizing cryopreservation outcomes for biobanking and clinical applications [88].
Soft Matter Approaches to Cryopreservation
The field of soft matter provides innovative tools and materials to address the physical and chemical challenges of cryopreservation at multiple length scales [89]. These approaches move beyond traditional small-molecule CPAs.
Advanced Cryoprotectants and Ice-Binding Materials
- Ice Recrystallization Inhibitors (IRIs): Materials like antifreeze proteins (AFPs) and their synthetic mimics (e.g., polyvinyl alcohol, PVA) do not prevent ice nucleation but inhibit the growth of larger, more damaging ice crystals from smaller ones during the warming phase, a process known as recrystallization [89] [17] [86]. This is crucial for maintaining cell membrane integrity.
- Biomimetic and Synthetic Polymers: Inspired by natural cryoprotective systems in extremophiles, polymers such as polyampholytes have shown tremendous promise. These molecules, which contain both positive and negative charges, demonstrate exceptional ability to suppress ice nucleation and enhance vitrification, often with lower toxicity than DMSO [17] [72]. For example, carboxylated poly-L-lysine (COOH-PLL) has been shown to yield higher viability for rat mesenchymal stem cells compared to DMSO [17].
- Nanomaterials for Ultrafast Warming: A major bottleneck in vitrification is devitrification (ice formation during warming). To overcome this, nanomaterials with high photothermal conversion efficiency, such as soft liquid metal nanoparticles (e.g., EGaIn), graphene oxide, and magnetic nanoparticles, are used to achieve ultrarapid and uniform warming when activated by near-infrared lasers or electromagnetic fields [90] [17]. This "nanowarming" approach allows for the use of lower CPA concentrations and successfully prevents ice recrystallization in larger volume samples, including cells and blood vessels [90].
Supporting Engineering Strategies
- Microencapsulation: Encapsulating cells in hydrogels like alginate provides a physical barrier that suppresses ice crystal growth and protects the cells from mechanical stress during freezing and thawing [17] [86].
- Synergistic Ice Inhibition: Combining different strategies, such as using IRIs alongside traditional CPAs or employing dehydration strategies before freezing, creates a synergistic protective effect, enabling high survival rates with reduced CPA toxicity [17].
Table 2: Soft Matter Materials and Their Functions in Cryopreservation
| Material Category | Example Compounds | Primary Function | Key Advantage |
|---|---|---|---|
| Synthetic Polymers | Polyvinyl alcohol (PVA), Polyampholytes (e.g., COOH-PLL) | Ice recrystallization inhibition; vitrification enhancement [17] | Reduced cytotoxicity compared to DMSO; highly designable [17] [72] |
| Biomimetic Proteins | Antifreeze Proteins (AFPs) | Thermal hysteresis; ice recrystallization inhibition [17] [86] | High potency; natural origin |
| Nanomaterials for Warming | Liquid Metal NPs (EGaIn), Magnetic Iron Oxide NPs | Ultrafast, uniform warming via photothermal/electromagnetic conversion [90] [17] | Prevents devitrification; applicable to larger sample volumes [90] |
| Encapsulation Matrices | Alginate, Chitosan | Physical barrier against ice crystal penetration; modulates dehydration [17] [86] | Protects complex cellular structures; enables low-CPA vitrification |
Experimental Protocols for Mouse Embryo Cryopreservation
This section outlines a detailed methodology for the cryopreservation of mouse one-cell stage embryos, incorporating advanced techniques as utilized in recent screening studies [56].
Protocol 1: Preparation and Cryopreservation of One-Cell Stage Embryos
Objective: To harvest, fertilize, and cryopreserve one-cell stage embryos from transgenic mouse strains for long-term storage and subsequent experimental use.
Materials and Reagents:
- Animals: C57BL/6N male (8 weeks old) and female (4 weeks old) mice [56].
- Hormones: HyperOva (or equivalent PMSG), human chorionic gonadotropin (hCG).
- Media: HTF medium for fertilization, KSOM medium for embryo culture, Sucrose solution (0.25 M).
- CPAs: Dimethyl sulfoxide (DMSO), DAP213 solution (a commercial vitrification solution often containing DMSO, acetamide, and propylene glycol in a saline base) [56].
Workflow:
Procedure:
- Ultra-Superovulation: Induce superovulation in 4-week-old C57BL/6N female mice by intraperitoneal injection of HyperOva. After 48 hours, administer 7.5 IU of hCG [56].
- Oocyte Collection: Harvest oocytes from the oviducts 16 hours post-hCG injection.
- In Vitro Fertilization (IVF): Place harvested oocytes into HTF medium designed for IVF and incubate with sperm. After 4 hours, remove excess sperm [56].
- Pre-equilibration: Incubate the fertilized embryos in a 200 µL drop of HTF medium supplemented with 20% fetal bovine serum for 10 minutes [56].
- Cryopreservation: Cryopreserve the embryos in liquid nitrogen using a freezing solution containing 1 M DMSO, followed by exposure to DAP213 solution [56].
- Storage: Store embryos in liquid nitrogen indefinitely.
Protocol 2: Thawing and High-Throughput Screening Using Inhibitor Libraries
Objective: To rapidly thaw cryopreserved embryos and employ them in a high-throughput screen to identify novel factors regulating early embryonic development.
Materials and Reagents:
- Cryopreserved Embryos: One-cell stage embryos from Protocol 1.
- Thawing Solution: 0.25 M sucrose solution.
- Culture Medium: KSOM medium.
- Inhibitor Library: A standardized library of chemical inhibitors (e.g., SCADS Inhibitor Kit) [56].
Workflow:
Procedure:
- Thawing: Rapidly thaw frozen embryos by transferring them to 900 µL of a 0.25 M sucrose solution [56].
- Washing: Wash the thawed embryos twice in KSOM medium to remove residual CPAs [56].
- Screening Setup: For each inhibitor in the library, prepare a treatment group by adding the inhibitor to KSOM medium at a final concentration (e.g., 1 µM). Use 20 thawed one-cell stage embryos per treatment group [56].
- Culture and Observation: Culture the embryos and monitor their development. The developmental rate is calculated as:
Developmental rate (%) = (Number of developed embryos / Total number of embryos) × 100[56]. - Validation: Confirm the role of identified factors using genome editing techniques like CRISPR-Cas9 to knock out candidate genes in zygotes, then assess the impact on embryonic development [56].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Embryo Cryopreservation and Screening
| Reagent / Solution | Composition / Example | Primary Function |
|---|---|---|
| Vitrification Solution | DAP213 solution (often contains DMSO, acetamide, propylene glycol) [56] | A high-concentration CPA mixture to promote glassy solidification without ice crystals. |
| Slow Freezing CPA | 1.5 M DMSO or Ethylene Glycol (EG) | Permeating CPA used in controlled-rate freezing to protect against slow cooling injuries [85]. |
| Non-Permeating CPA | Sucrose, Trehalose (0.5 M) | Provides osmotic support during CPA addition/removal; reduces required concentration of toxic permeating CPAs [85] [87]. |
| Thawing / Dilution Solution | 0.25 M Sucrose solution [56] | Creates a hypertonic environment during thawing to prevent osmotic shock from rapid water influx as CPAs leave the cell. |
| Embryo Culture Medium | KSOM Medium [56] | Supports the continued development and viability of embryos post-thaw during experimental assays. |
| Chemical Inhibitor Library | SCADS Inhibitor Kit [56] | A curated collection of pathway-specific inhibitors for high-throughput screening of developmental regulators. |
The integration of controlled ice nucleation and soft matter applications represents a paradigm shift in overcoming the persistent challenge of toxicity in mouse embryo cryopreservation. By moving from empirical optimization to a mechanistic, design-driven approach, these advanced techniques offer unprecedented control over the physical and chemical environment of the cell during freezing and thawing. For the research community, this translates to more reliable preservation of precious genetic material, reduced experimental variability, and the opening of new avenues for high-throughput screening in developmental biology. As these technologies continue to mature, they will undoubtedly become standard tools in the scientist's toolkit, ensuring the integrity and reproducibility of mouse-based research for years to come.
Ensuring Success: Rigorous Validation and Comparative Method Assessment
Evaluating post-thaw embryo viability is crucial for advancing reproductive science, particularly in understanding cryopreservation toxicity in mouse research models. As cryopreservation techniques become increasingly integral to assisted reproductive technologies and toxicological studies, standardized metrics for assessing embryo survival and developmental potential are essential. This technical guide establishes key benchmarks and methodologies for researchers and drug development professionals working with cryopreserved murine embryos, providing a framework for consistent evaluation across experimental contexts.
Essential Viability Metrics and Benchmarks
A multi-faceted approach to assessing post-thaw embryo viability provides comprehensive insights into cryopreservation success and identifies potential toxicity endpoints. The following quantitative metrics serve as fundamental benchmarks for evaluating cryopreservation outcomes in murine embryos.
Table 1: Core Post-Thaw Viability Metrics for Murine Embryos
| Metric Category | Specific Parameter | Benchmark for Success | Measurement Method |
|---|---|---|---|
| Immediate Survival | Morphological Integrity | ≥ 95% post-thaw survival [91] | Microscopic inspection for membrane integrity, zona pellucida damage, and cytoplasmic abnormalities |
| Developmental Competence | Blastocyst Formation Rate | ~80-86% (vs. 86.4% fresh control) [91] | Culture to blastocyst stage (typically 96-111 hours post-insemination) [92] |
| Developmental Timing | Key Milestone Timing | Specific cell counts at standardized times [92] | Time-lapse imaging or static observation at 43h (Day 2), 63h (Day 3), 93h (Day 4), and 111h (Day 5) post-insemination [92] |
| In Vivo Potential | Live Birth Rate | ~39-48% (mouse model) [91] | Embryo transfer to synchronized recipients and assessment to term |
Beyond these core metrics, additional qualitative assessments provide deeper insights into embryo health. These include evaluating fragmentation levels (with <10% considered optimal and >25% indicating poor prognosis), cell size uniformity (where significant unevenness suggests reduced potential), and the absence of multinucleation, which is linked to chromosomal abnormalities [92]. For cleavage-stage embryos, the ideal benchmarks include 4 cells on day 2 and 8 cells on day 3 of development [92].
Standardized Embryo Assessment Protocols
Implementing consistent assessment protocols ensures reproducible evaluation of post-thaw embryo quality. Standardized timing and criteria are fundamental for obtaining reliable, comparable data across experiments.
Temporal Assessment Windows
The developmental pace of embryos provides critical information about their viability. Assessments should be conducted at specific intervals post-thawing and post-insemination to ensure accurate benchmarking [92]:
- Day 1 (16-17 hours post-insemination): Fertilization check for pronuclei observation
- Day 2 (43 hours post-ICSI, 45 hours post-IVF): Cleavage-stage assessment for cell division initiation
- Day 3 (63 hours post-ICSI, 65 hours post-IVF): Cleavage-stage evaluation for 8-cell stage progression
- Day 4 (93 hours post-ICSI, 95 hours post-IVF): Morula stage assessment for compaction initiation
- Day 5 (111 hours post-ICSI, 112 hours post-IVF): Blastocyst stage evaluation for formation and expansion
Morphological Grading Criteria
A standardized morphological assessment system enables objective quality evaluation across different operators and laboratories. The following criteria align with the 2025 ESHRE/ALPHA consensus guidelines [92]:
- Zygote Assessment: Document abnormal fertilization patterns (0PN, 1PN, 3PN) but note that some 1PN zygotes may be diploid and viable
- Cleavage-Stage Embryos: Evaluate cell number, fragmentation percentage (<10% optimal, >25% poor), cell size regularity, and multinucleation presence
- Blastocyst Evaluation: Assess expansion degree, inner cell mass cohesion and cell number, and trophectoderm regularity and cell number
Advanced Functional Assessment Techniques
Beyond standard morphological evaluation, advanced techniques provide deeper insights into embryonic health and the functional impact of cryopreservation toxicity.
Molecular and Genetic Screening
Innovative screening approaches help identify specific factors affecting embryonic development post-thaw. The inhibitor library screening method combines ultra-superovulation with one-cell stage embryo cryopreservation to systematically identify developmental regulators [93].
Table 2: Research Reagent Solutions for Embryo Viability Assessment
| Reagent/Category | Specific Example | Function/Application |
|---|---|---|
| Cryopreservation Media | Vitrification solutions with cryoprotectants | Prevent intracellular ice crystal formation; enable ultra-rapid freezing [91] [94] |
| Inhibitor Libraries | SCADS Inhibitor Kits (II ver. 2.0 & III ver. 1.6) | Systematic screening of factors essential for embryonic development [93] |
| Macromolecular Cryoprotectants | Synthetic polyampholytes | Extracellular cryoprotectants that reduce intracellular ice formation and osmotic shock [94] |
| Ice Nucleators | Pollen-derived ice nucleators | Control ice formation in multi-well plate formats; reduce well-to-well variability [94] |
| Differentiation Inducers | Phorbol-12-myristate-13-acetate (PMA) | Induce monocyte-to-macrophage differentiation in THP-1 cells for toxicity studies [94] |
Cryopreservation Toxicity Endpoints
When investigating cryopreservation toxicity in mouse models, several specific endpoints provide insight into molecular and cellular damage:
- Meiotic Spindle Integrity: Assess via immunofluorescence staining for chromosomal alignment post-thaw [91]
- Apoptosis Markers: Evaluate caspase activation and other apoptotic indicators post-thaw [94]
- Oxidative Stress Indicators: Measure reactive oxygen species generation and antioxidant depletion
- Epigenetic Alterations: Analyze DNA methylation patterns and histone modifications that may be affected by cryopreservation [95]
- Gene Expression Profiling: Monitor developmental gene expression changes using single-cell RNA-seq approaches [93]
Experimental Workflow for Toxicity Assessment
A systematic workflow ensures comprehensive evaluation of cryopreservation effects on embryonic viability and identifies specific toxicity mechanisms.
Experimental workflow for systematic assessment of cryopreservation toxicity in murine embryos.
Data Interpretation and Troubleshooting
Proper interpretation of viability data requires understanding common pitfalls and their solutions in cryopreservation toxicity studies.
Common Toxicity Indicators
- Consistently low survival rates (<90%) may indicate issues with cryoprotectant toxicity, ice crystal formation, or osmotic shock during freezing/thawing [94]
- Arrest at specific developmental stages often correlates with inhibitor treatments or genetic manipulations targeting stage-specific processes [93]
- High variability between replicates in multi-well formats frequently stems from uncontrolled ice nucleation during freezing [94]
Technical Optimization Strategies
- Implement controlled ice nucleation using macromolecular cryoprotectants to improve consistency in high-throughput formats [94]
- Validate findings through multiple approaches such as combining inhibitor studies with genetic knockout models [93]
- Include appropriate controls such as fresh embryos and non-toxic cryoprotectant formulations to distinguish specific toxicity effects
Robust assessment of post-thaw embryo viability requires integration of multiple metrics spanning morphological, developmental, and molecular domains. The standardized benchmarks and methodologies presented here provide a framework for consistent evaluation of cryopreservation outcomes in mouse research models. By implementing these comprehensive assessment strategies, researchers can more accurately identify cryopreservation toxicity mechanisms and develop optimized protocols that maximize embryonic viability and developmental potential.
In mouse research, the integrity of preimplantation embryos is paramount, especially within the critical context of evaluating cryopreservation toxicity. Cryopreservation introduces multiple stressors, including cryoprotectant toxicity, osmotic shock, and oxidative stress, which can compromise embryonic viability and developmental potential [95] [62]. A robust quality control (QC) framework, spanning from morphological assessment to functional validation in culture, is therefore essential for accurately interpreting research outcomes. This technical guide details the protocols and benchmarks for a multi-stage QC system designed to assess embryo health after cryopreservation, providing researchers with a standardized approach to quantify cryodamage and optimize preservation strategies.
Morphological Assessment Pre- and Post-Cryopreservation
The first line of quality control is a rigorous morphological evaluation conducted both before cryopreservation and after warming. This non-invasive assessment provides the initial viability screen.
Pre-Cryopreservation Criteria
Prior to vitrification, only morphologically intact embryos should be selected. Key criteria include:
- Cell Integrity: Embryos must have blastomeres of uniform size and shape, with intact and smooth zona pellucida [16].
- Cytoplasmic Appearance: The cytoplasm should be clear and uniform, without excessive granularity or dark areas [96].
- Stage Appropriateness: The embryonic stage should be consistent with the post-coital timing. For collection at the 2-cell stage, this is typically 24 hours post-hCG injection [96].
Post-Warming Assessment
Following thawing, embryos are immediately examined for signs of cryoinjury. The survival rate is a primary quantitative metric. A study on ultra-fast vitrification reported a survival rate of 98.5% (200/203), which was not significantly different from fresh controls, whereas conventional vitrification showed a slightly lower, though not statistically different, survival rate [62]. Non-viable embryos often exhibit signs such as ruptured zona pellucida, lysed or dark blastomeres, and highly vacuolated or shrunken cytoplasm [97].
In Vitro Culture: The Functional Viability Test
Following morphological screening, in vitro culture provides a functional test of embryonic developmental competence. The culture system must be optimized to support development while allowing researchers to detect sublethal damage inflicted by cryopreservation.
Culture Protocols and Media
- Media Formulations: Two primary media are used sequentially to mimic the changing environment of the female reproductive tract. M2 medium is used for collection and handling of embryos outside the incubator [96]. For extended culture, M16 medium supplemented with bovine serum albumin (BSA) is used inside a CO2 incubator [96]. An alternative is the use of KSOM medium, particularly for culturing one-cell stage embryos after thawing [93].
- Culture Conditions: Embryos are cultured in 50 µL drops of medium under mineral oil in a humidified incubator at 37°C with 5% CO2 [96].
- Developmental Scoring: Embryos are observed daily and classified based on their progression: 2-cell, 4-cell, morula, early blastocyst, blastocyst, expanded blastocyst, and hatched blastocyst [96].
Interpreting Developmental Competence
The percentage of embryos that develop to the blastocyst stage is a critical endpoint. Table 1 summarizes the development rates for vitrified embryos from different genetically modified mouse strains, illustrating the genotype-dependent response to cryopreservation. Significant differences from control groups highlight strains that are more sensitive to cryopreservation toxicity [96].
Table 1: In Vitro Development of Vitrified Embryos from Genetically Modified Mouse Strains
| Strain | Developmental Rate to Blastocyst (%) | p-value vs. Control |
|---|---|---|
| Ccr2 | 66.7 | 0.0889 (NS) |
| Ccr5 | 63.04 | 0.0806 (NS) |
| D6 | 55.0 | 0.0685 (NS) |
| Tlr6 | 52.8 | 0.0806 (NS) |
| Ccl3 | 50.0 | 0.0006 () |
| Nos2 | 24.7 | 0.0434 (*) |
| Cd28 | 45.8 | 0.034 (*) |
| Alox5 | 4.8 | 0.0166 (*) |
NS: Not Significant; *: Statistically Significant [96]
Advanced Blastocyst Evaluation
Successful development to the blastocyst stage is a positive indicator, but a deeper analysis of blastocyst quality can reveal more subtle effects of cryopreservation.
Morphological Grading
Blastocysts are graded based on the degree of expansion, the integrity and cohesion of the inner cell mass (ICM), and the organization of the trophectoderm (TE) cells. High-quality blastocysts are typically expanded with a clear, compact ICM and a cohesive TE [98].
Molecular and Cellular Analysis
Morphological assessment alone is insufficient to detect all forms of cryodamage. Advanced techniques are required to probe cellular health.
- Membrane Integrity Assays: Fluorescence staining with Hoechst 33342 (membrane-permeant, labels live cells) and propidium iodide (membrane-impermeant, labels dead cells) provides a quantitative measure of viability. One study found significantly higher membrane permeability in vitrified embryos (69.8%) compared to slow-frozen (48.4%) and fresh control (13.8%) embryos [97].
- Ultrastructural and Organelle Analysis: Transmission electron microscopy (TEM) can identify subcellular damage. Studies comparing vitrification and slow freezing have shown that vitrification can cause more severe cellular alterations, including condensation of the cytoplasm and nuclear pycnosis, indicating processes of oncosis and apoptosis [97]. Research on oocytes has shown that vitrification can disrupt the distribution and function of critical organelles like the endoplasmic reticulum (ER) and mitochondria (MT), with conventional vitrification causing significant MT aggregation and reduced mitochondrial membrane potential (ΔΨm) compared to ultra-fast vitrification and fresh controls [62].
The following diagram illustrates the complete quality control workflow for assessing mouse embryos post-cryopreservation, from initial thawing to final advanced analysis.
Figure 1: Embryo Quality Control Workflow. This flowchart outlines the sequential stages of quality control for cryopreserved mouse embryos, from initial post-thaw morphological screening to final functional and molecular assessment.
The Scientist's Toolkit: Essential Reagents and Materials
A successful embryo quality control pipeline relies on specific, high-quality reagents and materials. The following table details key components and their functions in the process.
Table 2: Essential Research Reagents for Embryo QC and Cryopreservation Studies
| Reagent/Material | Function/Application | Example & Notes |
|---|---|---|
| Cryoprotective Agents (CPAs) | Protect cells from ice crystal formation during freezing/vitrification. | Ethylene Glycol, DMSO. Used in specific cocktails (e.g., Tsang and Chow solution) [96]. |
| Basal Culture Media | Provide essential nutrients and energy sources for embryo development. | M2 (for handling), M16 or KSOM (for long-term culture) [96] [93]. |
| Macromolecule Supplement | Prevents embryo adherence to culture dishes and provides nutrients. | Fatty acid-free Bovine Serum Albumin (BSA) [96]. |
| Hormones for Superovulation | Stimulate production of multiple oocytes in female donors. | eCG (e.g., Novormon) and hCG (e.g., Chorulon) [96]. |
| Viability Stains | Differentiate between live and dead cells based on membrane integrity. | Hoechst 33342 & Propidium Iodide (H/PI) [97]. |
| Inhibitor Libraries | Screen for novel factors regulating embryonic development and toxicity pathways. | SCADS Inhibitor Kits; used to identify key enzymes/channels [93]. |
Data Analysis and Interpretation in Toxicity Context
Quantifying the results from the QC stages is essential for drawing meaningful conclusions about cryopreservation toxicity.
- Key Metrics: The primary metrics include post-warming survival rate and developmental rate to blastocyst. These should be calculated as percentages and compared to fresh control groups [96].
- Statistical Analysis: Data are typically analyzed using Analysis of Variance (ANOVA) followed by post-hoc tests like Tukey's test to determine if differences between experimental and control groups are statistically significant. A p-value of less than 0.05 is generally considered significant [96].
- Benchmarking Against Controls: The most crucial comparison is between cryopreserved embryos and non-cryopreserved controls cultured in parallel. A significant drop in development rates in the cryopreserved group is a direct indicator of cryopreservation-associated toxicity [96] [97].
The cellular pathways affected by cryopreservation stressors are complex. The following diagram maps the primary mechanisms of cryodamage and their impacts on embryonic components, which are the ultimate targets of the quality control measures.
Figure 2: Pathways of Cryopreservation Toxicity. This diagram outlines the primary mechanisms through which cryopreservation stressors like cryoprotectant (CPA) toxicity, osmotic stress, and oxidative stress lead to cellular damage and impaired embryonic development.
In the field of reproductive biology, particularly in mouse research focused on cryopreservation toxicity, the ultimate validation of any experimental intervention rests on demonstrating an embryo's capacity to develop into live, healthy offspring. While in vitro assessments of embryonic development provide valuable preliminary data, they remain insufficient proxies for true developmental competence. Embryo transfer followed by the quantification of live birth rates represents the most stringent and biologically relevant endpoint for evaluating cryopreservation protocols, genetic manipulations, or toxicological exposures. This whitepaper provides an in-depth technical guide for researchers requiring robust experimental methodologies to validate developmental potential through embryo transfer, with specific emphasis on the context of cryopreservation toxicity studies in mouse models.
The critical importance of this final validation step is highlighted by research demonstrating that in vitro development does not always correlate with in vivo viability. Studies have identified specific factors, such as the inhibition of cathepsin D or CXCR2, which can arrest embryonic development despite promising in vitro progression [56]. Furthermore, the very tools used to enable cryopreservation—cryoprotectants (CPAs)—introduce their own toxicological challenges that can compromise developmental potential independent of freezing efficacy [1]. This technical guide outlines comprehensive protocols, data analysis frameworks, and practical tools to definitively assess embryonic developmental competence through embryo transfer and live birth measurement, providing researchers with the methodological rigor required for conclusive toxicity assessments in cryopreservation research.
The Critical Link Between Cryopreservation Toxicity and Developmental Potential
Cryopreservation protocols inherently expose embryos to multiple stressors, including cryoprotectant toxicity, osmotic shock, chilling injury, and oxidative stress. The assessment of live birth rates following embryo transfer provides the most comprehensive integration of these cumulative insults on embryonic health. Cryoprotectant toxicity remains the greatest obstacle to successful embryo cryopreservation, with toxicity being both concentration and time-dependent [1]. Different cryoprotectants exhibit distinct toxicological profiles; for instance, propylene glycol in excess of 2.5 M has been shown to impair the developmental potential of mouse zygotes by decreasing intracellular pH, while dimethyl sulfoxide (DMSO) can disrupt membrane integrity and mitochondrial function [1] [52].
The genotype of the mouse strain significantly influences how embryos respond to cryopreservation methods, with varying survival rates observed across different genetically modified strains subjected to identical vitrification protocols [96]. This variability underscores the necessity of empirical validation through embryo transfer for each new strain or modified cryopreservation protocol. Research has demonstrated that even when cryopreserved embryos appear morphologically intact after thawing and progress to the blastocyst stage in culture, their ultimate developmental potential, as measured by live birth rates, may be compromised by subtle cellular damage incurred during the freezing process [16]. The embryo transfer and live birth validation process thus serves as a critical quality control measure that integrates the cumulative effects of cryoprotectant toxicity, osmotic stress, and genotype-specific vulnerabilities that may not be apparent in in vitro assessments alone.
Experimental Design and Methodologies
Strategic Framework for Validation Experiments
Proper experimental design is fundamental to obtaining statistically valid and biologically relevant live birth data. The strategic framework must account for critical variables including the choice of embryo developmental stage, control groups, sample size calculations, and recipient animal management. A robust experimental design should include both positive controls (fresh, untreated embryos) and negative controls (embryos subjected to known toxic conditions) to establish the expected range of developmental competence. Randomization of embryos across recipient females is essential to minimize confounding effects of recipient variability, while sample sizes must provide sufficient statistical power to detect clinically relevant differences in live birth rates.
For cryopreservation toxicity studies, researchers should employ a stratified approach that assesses multiple developmental stages. Studies indicate that eight-cell mouse embryos often exhibit higher development rates and greater resilience to cryopreservation damage compared to earlier stages, making them particularly suitable for toxicity assessments [16]. Furthermore, different genetic backgrounds respond variably to cryopreservation; evaluation of embryos from multiple mouse strains provides a more comprehensive understanding of toxicity profiles [96]. The experimental timeline must accommodate the complete reproductive cycle, from embryo transfer through pregnancy confirmation, parturition, and assessment of offspring viability.
Detailed Embryo Transfer Protocol
The embryo transfer procedure requires precise technical execution to maximize the reliability of live birth outcomes. The following protocol has been optimized for validating developmental potential in cryopreservation toxicity studies:
Recipient Preparation: Utilize healthy, proven foster mothers (typically 8-12 weeks old) that have been naturally mated with vasectomized males to induce pseudopregnancy. The timing of the recipient's reproductive cycle must be synchronized with the developmental stage of the embryos being transferred—typically, day 2.5 pseudopregnant recipients for 8-cell to morula stage embryos, or day 0.5 pseudopregnant recipients for blastocyst stage embryos [16].
Anesthesia and Surgical Preparation: Anesthetize the recipient mouse using an approved anesthetic regimen (e.g., ketamine/xylazine combination). Apply ophthalmic ointment to prevent corneal drying, and place the animal in ventral recumbency on a warm surface. Shave and surgically prepare the dorsal lumbar region using alternating betadine and alcohol scrubs.
Surgical Approach and Uterine Exposure: Make a 1-1.5 cm longitudinal skin incision approximately 1 cm lateral to the midline at the level of the last rib. Bluntly dissect through the subcutaneous tissues until the abdominal musculature is visualized. Make a 0.5-1 cm incision through the muscle layer to expose the intra-abdominal contents. Gently exteriorize the ovarian fat pad, which will bring the uterine horn into view. Place a moistened sterile gauze sponge under the exposed reproductive tract to maintain positioning and prevent desiccation.
Embryo Loading and Transfer: Using a stereomicroscope, prepare a transfer pipette (e.g., Pasteur pipette) with an approximately 120° bent tip. Draw a small air bubble into the pipette, followed by the embryos suspended in a minimal volume of culture medium (5-10 embryos in 1-2 μL), then another air bubble. Carefully insert the pipette tip into the uterine lumen through a puncture made with a 27-gauge needle approximately 0.5-1 cm from the uterotubal junction. Expel the embryos with the air bubbles into the uterine lumen and withdraw the pipette slowly.
Closure and Post-operative Care: Return the uterine horn to the abdominal cavity and close the muscle layer with 1-2 interrupted absorbable sutures (e.g., 5-0 Vicryl). Close the skin incision with wound clips or non-absorbable sutures. Administer postoperative analgesia (e.g., buprenorphine) and monitor the animal until fully recovered from anesthesia. House recipients individually or in small groups with nestlets for environmental enrichment.
Pregnancy Monitoring and Data Collection: Monitor recipients for weight gain and abdominal distension. Record litter size, pup weights, and any abnormalities at birth. Track survival to weaning (postnatal day 21) to comprehensively assess developmental competence.
Quantitative Metrics and Data Analysis
Robust quantitative assessment requires tracking multiple outcome measures to fully capture developmental potential. The core metrics and their calculation methods are summarized in the table below.
Table 1: Key Metrics for Assessing Developmental Potential Following Embryo Transfer
| Metric | Calculation | Interpretation |
|---|---|---|
| Implantation Rate | (Number of implantation sites / Number of embryos transferred) × 100 | Measures initial embryo-uterine interaction; can be assessed mid-gestation via uterine dissection [99]. |
| Live Birth Rate | (Number of live offspring / Number of embryos transferred) × 100 | The primary endpoint; definitive measure of full developmental competence [100]. |
| Pregnancy Rate | (Number of pregnant females / Number of recipients with transferred embryos) × 100 | Assesses overall receptivity and initial success [101]. |
| Litter Size | Mean number of live offspring per pregnant female | Indicator of reproductive efficiency and potential developmental toxicity. |
| Offspring Viability | (Number of offspring surviving to weaning / Number of live births) × 100 | Assesses postnatal health and development. |
Statistical analysis should employ appropriate methods for proportional data, such as chi-square tests or logistic regression, with adjustments for potential confounding factors like recipient age, parity, and experimental batch effects. For cryopreservation toxicity studies, comparison of live birth rates between experimental groups (e.g., different cryoprotectants, concentrations, or freezing protocols) and fresh control embryos provides direct evidence of toxicity impacts on developmental potential.
Essential Research Reagents and Tools
Successful validation of developmental potential through embryo transfer requires specific reagents and specialized equipment. The following table summarizes the essential research toolkit for these experiments.
Table 2: Research Reagent Solutions for Embryo Transfer Validation Experiments
| Category | Specific Items | Application and Function |
|---|---|---|
| Animal Models | • C57BL/6N mice (embryo donors)• Proven vasectomized males• Healthy foster mothers (8-12 weeks) | • Standardized genetic background for toxicity studies [56]• Induction of pseudopregnancy in recipients• Embryo recipients with proven maternal instinct |
| Surgical Supplies | • Stereomicroscope• Transfer pipettes/Pulled glass capillaries• Fine forceps and scissors• Absorbable and non-absorbable sutures• Animal warming pad | • Visualization of transfer procedure• Precise embryo placement into uterine lumen• Surgical exposure of reproductive tract• Wound closure• Maintenance of physiological temperature during surgery |
| Hormonal Agents | • eCG (PMSG)• hCG | • Superovulation induction in donor females [96]• Final oocyte maturation and ovulation timing |
| Culture Media | • M2 medium• KSOM medium• Cryoprotectant solutions (DMSO, glycerol, ethylene glycol) | • Embryo collection and handling outside incubator [96]• Long-term embryo culture• Cryopreservation protocols with varying toxicity profiles [1] |
| Anesthesia/Analgesia | • Ketamine/Xylazine or Isoflurane• Buprenorphine• Ophthalmic ointment | • Surgical anesthesia• Post-operative pain management• Corneal protection during anesthesia |
Data Visualization and Workflow Mapping
Experimental Pathway for Live Birth Validation
The complete experimental pathway for validating developmental potential through embryo transfer and live birth rates involves multiple critical decision points and assessment stages. The following diagram illustrates this comprehensive workflow, from initial embryo preparation through final data analysis:
Cryopreservation Stress Signaling Pathways
Cryopreservation toxicity impacts embryonic development through multiple interconnected stress response pathways. The following diagram maps these critical signaling pathways that can compromise developmental potential and ultimately reduce live birth rates:
Advanced Applications and Research Implications
Integration with Novel Screening Platforms
The embryo transfer validation method serves as the definitive endpoint for emerging high-throughput screening technologies in reproductive toxicology. Recent advances combine ultra-superovulation techniques with one-cell stage embryo cryopreservation to enable large-scale screening of factors affecting embryonic development [56]. Such screening platforms systematically evaluate multiple inhibitors or toxicants simultaneously, but ultimately require embryo transfer to confirm functional developmental competence. This approach has identified novel regulators of embryonic development, including p53 activators, cathepsin D, CXCR2, and potassium channels, whose impacts on live birth potential were subsequently validated through transfer experiments [56].
The validation of cryopreservation protocols for specific transgenic mouse lines represents another critical application. Research demonstrates significant variability in post-thaw survival rates across different genetically modified strains, highlighting the necessity of empirical testing through embryo transfer [96]. For instance, while strains like Ccr2 and Ccr5 showed favorable development after vitrification (66.7% and 63.0% respectively), others like Alox5 exhibited markedly poor survival (4.8%) [96]. These strain-specific differences underscore how genetic background interacts with cryopreservation toxicity, necessitating individualized validation of developmental potential through embryo transfer rather than relying on generalized assumptions.
Statistical Considerations and Predictive Modeling
Robust statistical analysis is paramount when interpreting live birth data from embryo transfer experiments. Recent research has employed machine learning approaches to predict developmental potential, with models identifying key predictors including the number of extended culture embryos, mean cell number on day 3, and the proportion of 8-cell embryos [64]. While these computational models enhance prediction accuracy for in vitro development, they do not replace the biological validation provided by actual embryo transfer and live birth assessment.
For cryopreservation toxicity studies, sample size calculation must account for the expected effect size of the toxicological intervention. Research indicates that even subtle reductions in live birth rates (10-15%) can have significant implications for cryopreservation protocol optimization [1]. Statistical approaches such as logistic regression with generalized estimating equations appropriately account for the clustered nature of embryo transfer data (multiple embryos per recipient) while adjusting for potential confounders including recipient age, parity, and technician experience [101]. These rigorous analytical frameworks ensure that conclusions regarding developmental potential are statistically sound and biologically relevant.
Embryo transfer followed by live birth assessment remains the unequivocal gold standard for validating developmental potential in mouse cryopreservation research. This comprehensive technical guide has outlined the methodological framework, practical protocols, and analytical approaches required to implement this definitive endpoint in toxicity studies. As cryopreservation techniques continue to evolve and novel cryoprotectant formulations emerge, the rigorous application of embryo transfer validation will remain essential for distinguishing between mere morphological survival and true functional competence. By anchoring developmental assessment in the biologically relevant outcome of live offspring, researchers can generate conclusive evidence regarding the safety and efficacy of cryopreservation protocols, ultimately advancing both basic reproductive science and the preservation of valuable genetic resources.
The preservation of genetically engineered mouse models is a critical component of modern biomedical research, ensuring the stability, reproducibility, and accessibility of valuable genetic resources. Cryopreservation techniques provide a reliable means to protect these resources against loss from disease, genetic drift, or catastrophic events while reducing the costs associated with maintaining live colonies. Two principal methodologies have emerged for this purpose: sperm cryopreservation and embryo cryopreservation. Each approach offers distinct advantages and limitations that researchers must carefully consider when developing archiving strategies.
This technical guide provides an in-depth comparison of these two preservation methods, focusing specifically on their application within mouse research. Particular attention is given to the context of cryoprotectant toxicity and its implications for embryo development, a crucial consideration highlighted in the broader thesis on understanding embryo cryopreservation toxicity in mice. By synthesizing current protocols, empirical data, and technical requirements, this document aims to equip researchers, scientists, and drug development professionals with the knowledge needed to make informed decisions about preserving their mouse models.
Technical Comparison of Preservation Methods
Embryo Cryopreservation: The "Gold Standard"
Embryo cryopreservation involves the freezing of pre-implantation stage embryos, typically at the 8-cell stage, using cryoprotective agents that allow long-term storage in liquid nitrogen at -196°C [102] [103]. The process begins with superovulation of donor females, mating with stud males, and harvesting of fertilized embryos, which are then infused with a cryoprotectant, slowly cooled to approximately -35°C, and rapidly submerged in liquid nitrogen for storage [102] [103].
This method is widely regarded as the "gold standard" for mouse cryopreservation due to its robustness and reliability [104]. The primary advantage lies in preserving the complete genotype, including both nuclear and mitochondrial genomes, which is particularly important for strains with specific cytoplasmic backgrounds [104] [102]. Embryo cryopreservation also enables the freezing of homozygous embryos, simplifying future recovery efforts [104]. Additionally, the recovery process is generally more straightforward and less expensive compared to sperm cryopreservation, as thawed embryos can be directly transferred to recipient females without additional manipulation [104] [102].
However, embryo cryopreservation carries significant upfront costs and logistical challenges. The process requires substantial animal resources, typically needing 15 females and 15 males per strain, resulting in higher initial expenses [104] [102]. Furthermore, some mouse strains exhibit poor response to superovulation or produce embryos that cannot withstand the freeze-thaw process, limiting the universal applicability of this method [104].
Sperm Cryopreservation: A Cost-Effective Alternative
Sperm cryopreservation offers a simpler and more economical approach for archiving mouse strains. The procedure involves harvesting the cauda epididymis from euthanized males, releasing sperm into a cryoprotective solution, loading the suspension into straws, and freezing them in the vapor phase of liquid nitrogen before permanent storage [102] [103]. Recent technical advances, particularly the development of cryoprotectants containing raffinose and skim milk with additives like L-glutamine, have significantly improved fertility rates for previously challenging strains such as C57BL/6 and BALB/c [104] [105].
The most compelling advantage of sperm cryopreservation is its cost-effectiveness and efficiency. The process requires only 2-3 males per strain and can typically be completed in a single day [102] [106]. This translates to significantly lower upfront costs compared to embryo cryopreservation. Additionally, sperm cryopreservation generates abundant material for future use, with approximately 30 million sperm preserved per male, potentially yielding thousands of embryos through in vitro fertilization (IVF) [104].
However, sperm cryopreservation has notable biological limitations. As haploid cells, sperm preserve only half of the genome, requiring careful breeding strategies to reconstruct complex genotypes involving multiple mutations or transgenes [104] [102]. The method also cannot preserve mitochondrial DNA, as mitochondria are exclusively inherited through the maternal lineage [102]. Furthermore, strain-to-strain variation in post-thaw fertility remains a concern, despite recent improvements [102] [103].
Table 1: Strategic Comparison of Embryo and Sperm Cryopreservation Methods
| Parameter | Embryo Cryopreservation | Sperm Cryopreservation |
|---|---|---|
| Biological Material Preserved | Diploid embryos (complete genotype) | Haploid sperm (half genome) |
| Mice Required | ~30 (15 females + 15 males) [102] | 2-3 males [102] [106] |
| Time to Freeze | 1-2 weeks [102] | 1 day [102] [106] |
| Initial Cost | Higher [104] [106] | Lower [104] [106] |
| Recovery Cost | Lower [104] [102] | Higher (requires IVF) [104] [102] |
| Mitochondrial DNA Preservation | Yes [102] | No [102] |
| Success Rate Variations | Strain-dependent embryo viability [104] | Strain-dependent sperm fertility [102] [103] |
| Potential Offspring | Dozens [102] | Hundreds [104] [102] |
Cryoprotectant Toxicity in Embryo Cryopreservation
Mechanisms of Toxicity and Cellular Damage
The cryopreservation process inevitably exposes biological materials to various stressors, with cryoprotectant toxicity representing a significant challenge for embryo preservation. Cryoprotectants are essential for preventing lethal ice crystal formation during freezing, but they can induce cellular damage through multiple mechanisms. Research indicates that even when cryopreservation does not induce clear-cut anomalies at detectable rates, several mechanisms exist for nonlethal damage during the freeze-thaw process [14].
Studies comparing cryopreserved and control mice have revealed significant differences in morphophysiological and behavioral features, with some manifestations appearing later in life during senescence [14]. These findings suggest that embryo cryopreservation may have delayed effects beyond immediate toxicity, drawing attention to the preimplantation stages in developmental toxicology [14].
The toxicity profiles vary considerably among different cryoprotectants. Dimethyl sulfoxide (DMSO), commonly used in vitrification protocols, has been shown to cause dose-dependent cellular damage. For instance, dermal fibroblasts exposed to increasing DMSO concentrations demonstrated decreasing viability with higher concentration, temperature, and exposure time [1]. Similarly, propylene glycol (PG) in excess of 2.5 M has been shown to impair the developmental potential of mouse zygotes by decreasing intracellular pH [1].
Molecular and Metabolic Consequences
At the molecular level, cryoprotectants can disrupt cellular function through various pathways. Some cryoprotectants have been shown to deplete reduced glutathione in kidneys, leading to oxidative stress [1]. Others can polymerize the actin cytoskeleton in spermatozoa, an effect unrelated to osmolality [1]. Methanol, when used as a cryoprotectant, demonstrates dose-dependent reduction in multiple mitochondrial function measures, including membrane potential, mitochondrial distribution, mitochondrial DNA copy number, ATP levels, and ADP/ATP ratios [1].
The process of vitrification, which involves ultra-rapid cooling to form a glassy state, requires high concentrations of cryoprotectants that can be particularly challenging for embryos. While vitrification solutions typically contain mixtures like DMSO with acetoamide and propanediol (DAP213), the toxicity of these compounds remains a significant concern [105]. Research into mitigating these effects has identified potential protective agents, such as N-acetyl cysteine (NAC), which has been shown to recover the fertilizing ability of vitrified-warmed mouse oocytes by alleviating zona hardening [105].
Table 2: Cryoprotectants Used in Mouse Embryo and Sperm Cryopreservation
| Cryoprotectant | Common Applications | Toxicity Concerns | Protective Strategies |
|---|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Embryo vitrification [105] | Dose-dependent reduction in cell viability; myocardial alterations at high concentrations [1] | Concentration optimization; controlled cooling rates [1] |
| Propylene Glycol (PG) | Embryo cryopreservation [1] | Impairs developmental potential of zygotes via pH decrease [1] | Concentration limitation (<2.5 M) [1] |
| Glycerol (GLY) | Sperm cryopreservation [1] | Depletes glutathione causing oxidative stress; polymerizes actin cytoskeleton [1] | Antioxidant supplementation [1] |
| Raffinose-Skim Milk | Sperm cryopreservation (Nakagata method) [105] | Relatively low toxicity; strain-specific variations [105] | Addition of L-glutamine [105] |
| Methanol (METH) | Specialized applications [1] | Mitochondrial dysfunction; metabolic conversion to formaldehyde [1] | Strict concentration control [1] |
Experimental Protocols and Methodologies
Standardized Embryo Cryopreservation Workflow
The embryo cryopreservation process follows a systematic protocol to maximize viability post-thaw. The standard method involves collecting 8-cell stage embryos, which demonstrate superior freeze-thaw resilience compared to other developmental stages [102] [103]. The process begins with superovulation of 3-4 week old or 8-10 week old female donors through administration of equine chorionic gonadotropin (eCG) followed by human chorionic gonadotropin (hCG) 48 hours later [102]. The females are then mated with proven stud males, and embryos are harvested approximately 1.5 days post-coitum.
The cryopreservation protocol typically uses a slow freezing approach with 8-cell stage embryos infused with cryoprotectant, gradually cooled to -35°C, and then rapidly submerged in liquid nitrogen [102] [103]. For vitrification, a standardized protocol using 1M DMSO followed by a mixture of 2M DMSO, 1M acetoamide, and 3M propanediol (DAP213) has proven effective, with more than 90% of vitrified-warmed embryos surviving and 30-50% developing into pups after embryo transfer [105].
Recent advancements in superovulation techniques have significantly improved embryo yields. The coadministration of inhibin antiserum (IAS) with eCG, known as ultrasuperovulation, can produce over 100 oocytes per female mouse compared to the average 25 oocytes obtained with conventional eCG and hCG treatment [105]. This enhancement reduces the number of oocyte donors needed and enables more efficient archiving of valuable strains.
Figure 1: Embryo Cryopreservation Workflow with Toxicity Considerations. This diagram illustrates the standardized protocol for mouse embryo cryopreservation, highlighting key stages where cryoprotectant toxicity may impact embryo viability and long-term outcomes.
Advanced Sperm Cryopreservation Techniques
Sperm cryopreservation methodologies have evolved significantly, with the Nakagata method—using a cryoprotectant composed of 18% raffinose pentahydrate and 3% skim milk—serving as the fundamental system for mouse sperm cryopreservation [105]. Recent modifications have further enhanced this technique, particularly for challenging strains like C57BL/6. The addition of 100 mM L-glutamine to the raffinose- and skim-milk-based cryoprotectant (modified R18S3) has improved fertility rates for cryopreserved C57BL/6 sperm [105].
The IVF process using frozen-thawed sperm has been optimized through specific chemical treatments. During sperm preincubation, methyl-β-cyclodextrin (MBCD) at 0.75 mM concentration enhances the fertilization rate by stimulating cholesterol efflux from the sperm membrane [105]. Additionally, incorporating 1.0 mM reduced glutathione (GSH) or cysteine analogs in the fertilization medium supports sperm penetration through the zona pellucida by dissecting disulfide bonds [105].
Recent innovations have simplified sperm cryopreservation through methods like the Easy and Quick (EQ) protocol, which enables sperm preservation at -80°C without immediate requirement for liquid nitrogen [107]. This method involves dissecting a single cauda epididymis in a microtube containing 20% raffinose solution, which is then stored directly in a -80°C freezer. Frozen-thawed sperm preserved this way retain practical fertilization rates (51% after 1 month, 25% after 3 months) with C57BL/6J strains, the most sensitive strain for sperm freezing [107].
Figure 2: Sperm Cryopreservation and Recovery Workflow. This diagram outlines the primary pathways for mouse sperm cryopreservation, including both standard and emergency protocols, with attention to strain-specific variables that impact success rates.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Mouse Germplasm Cryopreservation
| Reagent/Chemical | Application | Function | Technical Notes |
|---|---|---|---|
| Equine Chorionic Gonadotropin (eCG) | Superovulation | Stimulates follicular development | Often combined with IAS for ultrasuperovulation [105] |
| Human Chorionic Gonadotropin (hCG) | Superovulation | Triggers ovulation | Administered 48 hours after eCG [102] |
| Inhibin Antiserum (IAS) | Ultrasuperovulation | Blocks negative feedback on FSH secretion | Increases oocyte yield to >100 per female [105] |
| Raffinose Pentahydrate | Sperm cryoprotectant | Principal cryoprotective agent | Used at 18-20% concentration in freezing medium [105] [107] |
| Skim Milk | Sperm cryoprotectant | Protects sperm during freeze-thaw | Chemically undefined component of standard cryoprotectant [105] [107] |
| Dimethyl Sulfoxide (DMSO) | Embryo vitrification | Penetrating cryoprotectant | Prevents ice crystal formation; concentration-dependent toxicity [105] [1] |
| Methyl-β-cyclodextrin (MBCD) | Sperm preincubation | Stimulates cholesterol efflux | Enhances fertilization rate of frozen-thawed sperm [105] |
| Reduced Glutathione (GSH) | Fertilization medium | Reduces disulfide bonds in zona pellucida | Facilitates sperm penetration; improves IVF efficiency [105] |
| N-acetyl cysteine (NAC) | Oocyte vitrification | Alleviates zona hardening | Recovers fertilizing ability of vitrified-warmed oocytes [105] |
Strategic Implementation in Research Programs
Decision Framework for Method Selection
Choosing between sperm and embryo cryopreservation requires careful consideration of multiple factors, including research objectives, available resources, and specific strain characteristics. Embryo cryopreservation is generally recommended when complete genotype preservation is essential, such as for strains with multiple genetic modifications, those requiring specific mitochondrial backgrounds, or lines anticipated for high-demand distribution [102] [103]. This approach ensures that the entire genetic constitution is preserved intact, simplifying future recovery efforts.
Sperm cryopreservation offers a practical solution for large-scale archiving of multiple strains with limited resources. It is particularly suitable for emergency preservation situations, backing up ongoing lines, or preserving strains with single gene modifications [102] [103]. The development of simplified methods like the EQ freezing protocol enables rapid response preservation even by inexperienced personnel during urgent situations such as microbiological contamination or facility closures [107].
For comprehensive genetic resource management, many institutions implement a hybrid approach. The Center for Animal Resources and Development (CARD) at Kumamoto University, for instance, maintains both sperm and embryo cryopreservation capabilities to accommodate diverse researcher needs [105]. This integrated strategy allows for optimal resource allocation while ensuring the security of valuable genetic materials.
Global Mouse Banking Infrastructure
The establishment of international mouse banking networks has significantly enhanced the accessibility and security of mouse genetic resources. repositories worldwide have collectively archived over 60,000 strains of genetically engineered mice, with searchable databases like the International Mouse Strain Resource (IMSR) facilitating resource sharing among researchers [105]. Regional collaborations such as the Asian Mouse Mutagenesis and Resource Association (AMMRA) further promote the production, preservation, and distribution of mouse resources [105].
These banking infrastructures employ rigorous quality control measures to ensure the viability of preserved materials. For embryo cryopreservation, quality assurance typically involves thawing a representative sample of embryos shortly after freezing and transferring them to foster mothers to confirm successful recovery of live mice [102]. For sperm cryopreservation, one straw of frozen sperm from each cryopreservation is typically used to perform IVF to demonstrate the ability to produce fertilized embryos, with at least 20% of oocytes developing into embryos considered a successful preservation [102].
Biosecurity protocols represent another critical component of mouse banking operations. Frozen sperm or embryos are routinely split into multiple batches stored in separate liquid nitrogen freezers in different buildings to safeguard against catastrophic loss [102]. Additionally, closed storage systems minimize the risk of pathogen transmission through direct contact with liquid nitrogen, a documented concern in shared storage tanks [108].
Sperm and embryo cryopreservation represent complementary approaches for preserving mouse models, each with distinct advantages and limitations. Embryo cryopreservation remains the "gold standard" for complete genotype preservation despite higher initial costs and greater animal requirements. In contrast, sperm cryopreservation offers a cost-effective, efficient alternative for large-scale archiving, though with limitations in preserving complex genotypes and mitochondrial DNA.
The consideration of cryoprotectant toxicity remains central to both methods, influencing protocol development and optimization strategies. Ongoing research continues to refine cryopreservation techniques, with recent advances in ultrasuperovulation, vitrification methods, and simplified sperm freezing protocols enhancing the efficiency and accessibility of mouse model preservation.
As mouse banking infrastructures expand globally, researchers are increasingly able to leverage these resources to safeguard their valuable genetic materials. By understanding the technical considerations, toxicity implications, and practical requirements outlined in this guide, research professionals can develop informed cryopreservation strategies that ensure the long-term security and accessibility of their mouse models, thereby supporting the advancement of biomedical science.
Cryopreservation is an indispensable tool in biomedical research, enabling the long-term storage of biological samples ranging from single cells to complex tissues. Within the specific context of mouse research, which is fundamental to genetic and therapeutic studies, the technology serves two primary purposes: the preservation of valuable, genetically unique mouse strains and the facilitation of complex experiments on early embryonic development. The core challenge that underpins both the technical feasibility and economic viability of these endeavors is cryoprotectant agent (CPA) toxicity. High concentrations of CPAs, necessary to prevent lethal ice crystal formation, simultaneously introduce a toxicity that can compromise embryo viability and developmental potential [109] [1]. Consequently, optimizing cryopreservation protocols to mitigate CPA toxicity is not merely a technical goal but a critical factor in a strategic cost-benefit analysis. This review will evaluate the long-term value of such optimized cryopreservation, framing the discussion within the economic and practical realities of managing transgenic mouse colonies for research and drug development.
The Dual Challenge: CPA Toxicity and Its Impact on Research
Mechanisms and Manifestations of CPA Toxicity
Cryoprotectant toxicity is widely recognized as the most significant obstacle to the successful cryopreservation of cells, tissues, and organs [1]. The toxicity is multifaceted, manifesting as damage to cell membranes, alteration of metabolic and mitochondrial function, induction of DNA single-strand breaks, and disruption of the cytoskeleton [1] [49]. The severity of this damage is influenced by the specific CPA used, its concentration, the temperature of exposure, and the duration of contact with the biological sample [1].
Different CPAs exhibit distinct "specific toxicities". For instance, glycerol can deplete reduced glutathione in kidneys, leading to oxidative stress, and has been shown to polymerize the actin cytoskeleton in stallion spermatozoa [1]. Dimethyl sulfoxide (DMSO) can cause irreversible ultrastructural alterations to myocardium at concentrations above 1.41 M and reduce the clonogenic potential of peripheral blood progenitor cells even at modest concentrations [1]. Formamide is a highly corrosive amide that can denature DNA, an effect believed to be due to the displacement of hydrating water molecules [1]. The molecular mechanisms underlying these toxic effects are complex, often involving disruption of hydrogen bonding, induction of osmotic stress, and direct interference with protein function [1].
The Economic Imperative for Mouse Colony Cryopreservation
The financial burden of maintaining live mouse colonies is substantial. Cryopreservation offers a powerful strategy to mitigate these costs and protect invaluable genetic resources. As illustrated in Figure 1, the cumulative cost of maintaining a live colony increases steeply over time, far outstripping the one-time investment in cryopreservation, even when accounting for periodic recoveries for experiments [49].
Maintaining a heterozygous colony that requires frequent genotyping can cost from several thousand to over $10,000 per year [49]. In contrast, the upfront cost of cryopreservation is typically recouped through cage-cost savings in a matter of months [49]. Beyond direct cost savings, cryopreservation acts as a vital risk management tool. Natural disasters, disease outbreaks, breeding cessation, or genetic drift can lead to the catastrophic loss of irreplaceable strains. The loss of over 3,000 mouse lines at NYU Langone Medical Center during Hurricane Sandy serves as a stark reminder of the non-economic value of cryopreservation for ensuring research continuity [49].
Table 1: Economic and Practical Considerations for Mouse Strain Preservation
| Factor | Sperm Cryopreservation | Embryo Cryopreservation |
|---|---|---|
| Preserved Genetics | Paternal genome only | Full maternal and paternal genotype |
| Best For | Single-gene mutations on common inbred backgrounds | Hybrid/unique backgrounds; multiple unlinked mutations |
| Recovery Outcome | Heterozygous offspring (requires further breeding) | Exact original genotype (including homozygotes) |
| Upfront Resource Need | Two males | Males and superovulated females |
| Relative Upfront Cost | Generally more cost-effective | Generally higher |
Quantitative Frameworks for Evaluating Cryopreservation
High-Throughput Screening of CPAs
The discovery of less toxic and more effective CPAs is crucial for advancing cryopreservation. Recent methodological innovations have focused on increasing the throughput of toxicity and permeability screening. One such method uses an automated plate reader to measure cell membrane permeability and toxicity simultaneously in a 96-well format [110].
This technique utilizes intracellular calcein as a fluorescent marker for cell volume. When cells are exposed to a hypertonic solution containing a permeating solute, they initially shrink, causing a decrease in calcein fluorescence. As the solute permeates the membrane, water re-enters the cell, and the volume and fluorescence recover. The kinetics of this fluorescence recovery are used to calculate the solute permeability coefficient (P~CPA~) [110]. Following the permeability measurement, the same well plate is used for a toxicity assay. The underlying assumption is that healthy cells retain calcein, while dead cells with compromised membranes release it into the surrounding medium, leading to high background fluorescence [110]. This method enables the rapid screening of dozens of candidate chemicals, identifying those with an optimal combination of high membrane permeability and low toxicity—key properties for effective vitrification [110].
Figure 1: High-Throughput CPA Screening Workflow. This diagram outlines the process for simultaneously screening the membrane permeability and toxicity of candidate cryoprotectants using an automated plate reader. Bovine Pulmonary Artery Endothelial Cells (BPAEC) are seeded and loaded with a fluorescent dye. The kinetics of fluorescence change upon CPA exposure allow for permeability calculation, while fluorescence after CPA removal indicates toxicity. (Adapted from [110])
Toxicity Kinetics and Mixture Optimization
Moving beyond single-CPA screening, another quantitative approach involves characterizing the toxicity kinetics of multi-CPA mixtures. This is vital because vitrification solutions often rely on combinations of permeating and non-permeating agents to achieve ice suppression while mitigating the toxicity of any single component [109] [72].
Using automated liquid handling, researchers have characterized the toxicity kinetics of five common CPAs—glycerol, dimethyl sulfoxide (DMSO), propylene glycol, ethylene glycol, and formamide—as well as their binary and ternary mixtures on bovine pulmonary artery endothelial cells (BPAEC) [109]. The results confirm common trends, such as the relatively low toxicity of ethylene glycol and a general increase in toxicity with concentration. They also revealed surprising interactions, such as a "toxicity neutralization effect" where glycerol reduced the toxicity of formamide [109]. This dataset enables the application of a mathematical "toxicity cost function" to design improved CPA equilibration methods. By modeling toxicity as a function of CPA concentration and exposure time, this approach can computationally optimize the path and timing of CPA addition and removal, minimizing the integrated toxic load experienced by the cells [109].
Experimental Protocols for Mouse Embryo Research
Protocol 1: Cryopreservation of One-Cell Stage Mouse Embryos
This protocol is adapted from methods used in a screening study for novel embryonic developmental factors [56].
Materials:
- Animals: C57BL/6N male (8 weeks old) and female (4 weeks old) mice.
- Reagents: HyperOva (for ultra-superovulation), human chorionic gonadotropin (hCG), HTF medium (for in vitro fertilization), DMSO, DAP213 solution, 0.25 M sucrose solution, KSOM medium (for embryo culture).
Method:
- Superovulation: Intraperitoneally inject 4-week-old female mice with HyperOva. After 48 hours, inject 7.5 IU of hCG.
- Oocyte Collection: Harvest oocytes from the oviducts 16 hours after the hCG injection.
- In Vitro Fertilization: Incubate oocytes with sperm in HTF medium. After 4 hours, remove excess sperm and incubate the fertilized embryos in HTF supplemented with 20% fetal bovine serum for 10 minutes.
- Cryopreservation: Transfer the one-cell stage embryos into a freezing solution containing 1 M DMSO and DAP213 solution. Subsequently, plunge and store the embryos in liquid nitrogen.
- Thawing: Rapidly thaw frozen embryos by placing them in 900 µL of a 0.25 M sucrose solution. Perform two washes in KSOM medium before use in subsequent experiments [56].
Protocol 2: Inhibitor Library Screening on Thawed Embryos
This protocol describes a method for identifying novel factors involved in early embryonic development using cryopreserved embryos [56].
Materials:
- Inhibitor Library: A standardized library of chemical inhibitors (e.g., SCADS Inhibitor Kit).
- Reagents: KSOM medium, 50% methanol.
Method:
- Preparation: Thaw cryopreserved one-cell stage embryos as described in Protocol 1.
- Inhibitor Dilution: Dilute inhibitors from the library stock to create 100 µM working solutions in KSOM medium. The final concentration used in the embryo culture is typically 1 µM.
- Embryo Culture: Culture 20 thawed one-cell stage embryos per treatment group in KSOM medium containing the specified inhibitor. Include a control group with no inhibitor.
- Assessment: Culture the embryos and calculate the developmental rate at defined time points using the formula: Developmental rate (%) = (N~developed~ / N~total~) × 100, where N~developed~ is the number of embryos that develop to the target stage (e.g., blastocyst) and N~total~ is the total number of embryos cultured [56].
The Scientist's Toolkit: Key Reagents for Cryopreservation Research
Table 2: Essential Research Reagents for Cryopreservation and Developmental Screening
| Reagent / Solution | Function / Application |
|---|---|
| DAP213 Solution | A non-permeating cryoprotectant mixture often used in vitrification protocols for mouse embryos [56]. |
| KSOM Medium | Potassium-Simplex Optimized Medium; a widely used, chemically defined culture medium for supporting preimplantation development of mouse embryos [56]. |
| HTF Medium | Human Tubal Fluid medium; used for in vitro fertilization of mouse oocytes [56]. |
| SCADS Inhibitor Kits | Standardized libraries of low-molecular-weight inhibitors used in high-throughput screening to identify novel regulatory factors in biological processes like embryonic development [56]. |
| Calcein-AM | A cell-permeant fluorescent dye used in viability and permeability assays. It is converted by intracellular esterases into calcein, which is retained in live cells [110]. |
| HyperOva | A hormone preparation used to induce "ultra-superovulation" in juvenile female mice, yielding a high number of oocytes for research [56]. |
Toxicity Pathways and Long-Term Storage Considerations
Molecular Pathways of Toxicity
Understanding the specific molecular injuries caused by CPAs is key to developing mitigation strategies. Research has identified several key pathways and targets, as illustrated in Figure 2. DMSO can induce drastic changes in the cellular epigenetic landscape and alter differentiation pathways [72]. Glycerol can deplete antioxidants like glutathione, leading to oxidative stress and apoptosis in renal cells [1]. Formamide can denature DNA by displacing hydrating water molecules, disrupting its native structure [1]. Methanol's toxicity is partly attributed to its metabolism to formaldehyde, which can cause metabolic acidosis and damage mitochondria, reducing ATP levels and membrane potential [1]. These diverse mechanisms highlight that CPA toxicity is not a single entity but a collection of chemical-specific insults that must be individually addressed.
Figure 2: Key Molecular Pathways of CPA Toxicity. Different cryoprotectants induce toxicity through distinct molecular mechanisms. Understanding these pathways is essential for developing strategies to neutralize toxicity, such as using antioxidant supplements or designing less disruptive CPA mixtures.
The Impact of Prolonged Cryostorage
While properly maintained cryopreserved material is considered viable indefinitely [49], some clinical studies in human assisted reproduction suggest that prolonged storage might negatively impact pregnancy outcomes. A large, multicenter retrospective study found that cryostorage duration was inversely associated with the likelihood of pregnancy and live birth following frozen embryo transfer [111]. Another study concluded that storage exceeding 24 months negatively affected pregnancy outcomes, with the negative impact progressing as storage duration increased, particularly beyond 72 months [112]. In contrast, other analyses, including one with 47,006 cycles, found that while freezing for more than one year was associated with diminished clinical pregnancy and live birth rates, there were no statistically significant differences in neonatal birth weight between groups [113]. These findings highlight an area of ongoing investigation. For mouse research, the consensus from major repositories like The Jackson Laboratory is that no significant decrease in recovery rates is observed with time in storage when proper protocols are followed [49].
The long-term value of optimized cryopreservation in mouse research is unequivocal. The economic calculus, as demonstrated in Figure 1, firmly supports cryopreservation as a cost-effective strategy for managing research colonies, with the initial investment being quickly offset by the significant recurring costs of maintaining live animals. The scientific value is equally profound: by enabling sophisticated experimental workflows like high-throughput inhibitor screening and ensuring the perpetual availability of genetically precise models, optimized cryopreservation accelerates discovery. The central challenge of CPA toxicity is being met with innovative quantitative approaches, including high-throughput screening platforms and mathematical modeling of toxicity kinetics. These advancements are steadily transforming cryopreservation from a simple storage technique into a predictable and highly optimized component of the biomedical research infrastructure, thereby protecting invaluable genetic resources and enhancing the overall efficiency and reproducibility of scientific inquiry.
Conclusion
The successful cryopreservation of mouse embryos hinges on a deep understanding of CPA toxicity and the meticulous application of optimized protocols. As this analysis has detailed, progress involves moving from foundational damage mechanisms to the practical implementation of advanced methods like equilibrium vitrification, which minimizes chemical toxicity. Rigorous troubleshooting and validation are non-negotiable for ensuring the genetic integrity and viability of preserved models. Looking forward, the field is poised for transformation through bio-inspired CPA discovery, the application of soft matter techniques to control ice formation, and the development of novel toxicity-neutralization strategies. These advancements will not only secure invaluable genetic resources but also pave the way for broader applications in regenerative medicine and the conservation of complex tissues, solidifying the role of cryopreservation as a pillar of modern biomedical research.
References
- 1. Cryoprotectant Toxicity: Facts, Issues, and Questions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4620521/]
- 2. Winter is coming: the future of cryopreservation - BMC Biology [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-021-00976-8]
- 3. Cryopreservation: A Review Article - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9756256/]
- 4. The mechanism and protective strategies of follicle injury after ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01793-1]
- 5. Genetic Suppression of Cryoprotectant Toxicity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7001869/]
- 6. Model biological systems demonstrate the inducibility of ... [https://www.sciencedirect.com/science/article/pii/S0011224024000361]
- 7. Hydrogel microcapsulation technology reduces the DMSO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639263/]
- 8. A circular exploration of cryoprotective agents for stem cells ... [https://www.sciencedirect.com/science/article/pii/S2772508125000328]
- 9. Comprehensive overview of the toxicities of small-molecule ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897285/]
- 10. Multiple cryoprotectant toxicity model for vitrification ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224022000943]
- 11. Dimethyl sulfoxide–induced DNA demethylation during ... [https://link.springer.com/article/10.1007/s10815-025-03415-7]
- 12. DMSO induces major morphological and physiological ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330348]
- 13. The effect of minimal concentration of ethylene glycol (EG) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3909135/]
- 14. Long-term effects of embryo freezing in mice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC42787/]
- 15. Studies on Replacing Most of the Penetrating ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224001923351]
- 16. Cryopreservation of transgenic mouse embryos — an eight ... [https://www.sciencedirect.com/science/article/abs/pii/S0939860004000240]
- 17. the critical step to utilize stem cell products [https://pmc.ncbi.nlm.nih.gov/articles/PMC10393932/]
- 18. Multiple cryoprotectant toxicity model for vitrification solution... [https://pubmed.ncbi.nlm.nih.gov/36113568/]
- 19. Natural zwitterionic betaine enables cells to survive ... [https://www.nature.com/articles/srep37458]
- 20. Mitochondrial Dysfunction and Oxidative Stress Caused by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7996228/]
- 21. Abnormalities in mitochondrial energy metabolism induced ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2024.1514362/full]
- 22. Comparative transcriptome analysis reveals molecular damage... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10473-1]
- 23. Chemical approaches to cryopreservation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9294745/]
- 24. Optimization of Cryoprotectant Loading into Murine and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4036103/]
- 25. The role of apoptosis in cryopreserved animal oocytes and ... [https://pubmed.ncbi.nlm.nih.gov/34365139/]
- 26. Cryopreservation of Gametes and Embryos and Their ... [https://www.mdpi.com/1422-0067/22/19/10864]
- 27. In situ quantification of osmotic pressure within living ... [https://www.nature.com/articles/s41467-023-42024-9]
- 28. How to optimize culture media osmolality during Assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10065773/]
- 29. Efficacy and safety of a one-step warming protocol ... [https://www.medrxiv.org/content/10.1101/2025.10.02.25337068v1.full-text]
- 30. Chilling injury mechanism in the immature oocytes of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511777/]
- 31. Antioxidant strategies to mitigate oxidative stress-induced ... [https://www.degruyterbrill.com/document/doi/10.1515/fzm-2025-0009/html?srsltid=AfmBOoo0ejoADj5k2ppuvJnQiYgT7matksqcBxdfrnF3QzrEtJ01w2It]
- 32. Oxidative Stress and Oocyte Cryopreservation: Recent ... [https://www.mdpi.com/2073-4409/11/22/3573]
- 33. Effects and Mechanisms of Imperatorin on Vitrified Mouse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898152/]
- 34. Vitrification affects the post-implantation development of ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01826-y]
- 35. Melatonin Enhances Vitrified Mouse Blastocyst ... [https://pubmed.ncbi.nlm.nih.gov/41208044/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1TkPOxkdaxttnpzufm0HcTPRDrxydl3CYSWuLR2PKx8fqi2M0I&fc=None&ff=20251111015434&v=2.18.0.post22+67771e2]
- 36. Protective effect of astaxanthin on reproductive cell ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224025001324]
- 37. Vitrification versus slow freezing of human ovarian tissue [https://pmc.ncbi.nlm.nih.gov/articles/PMC10033773/]
- 38. Vitrification versus slow freezing gives excellent survival ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2729856/]
- 39. Comparative effectiveness of vitrification and slow freezing ... [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-024-03505-1]
- 40. Comparison of angiogenic potential in vitrified vs. slow ... [https://www.nature.com/articles/s41598-023-39920-x]
- 41. Comparison of the effects of vitrification and slow freezing ... [https://www.imrpress.com/journal/CEOG/47/5/10.31083/j.ceog.2020.05.2079/htm]
- 42. Vitrification of mouse embryo-derived ICM cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3059526/]
- 43. Tolerance of human embryonic stem cell derived islet ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224015000565]
- 44. Equilibrium vitrification of mouse embryos at various ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8075728/]
- 45. Equilibrium vitrification of oocytes using low concentrations ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224023000858]
- 46. Equilibrium vitrification of mouse embryos using low ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224020306611]
- 47. Equilibrium vitrification of oocytes using low concentrations ... [https://pubmed.ncbi.nlm.nih.gov/37722470/]
- 48. Efficient Mouse Colony Management [https://www.jax.org/news-and-insights/jax-blog/2025/september/mouse-colony-management-faqs]
- 49. Cryopreservation of Transgenic Mice [https://www.jax.org/news-and-insights/jax-blog/2025/september/cryopreservation-of-transgenic-mice]
- 50. Cryopreservation: An emerging paradigm change - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2781087/]
- 51. The Role of Cryoprotectants in ATMP Cryopreservation [https://www.susupport.com/blogs/knowledge/stressing-cells-role-cryoprotectants-atmp-cryopreservation]
- 52. Cryoprotectant Toxicity: Balancing Safety and Efficacy [https://allanchem.com/cryoprotectant-toxicity-safety-efficacy/]
- 53. A numerical study on the loading of cryoprotectant cocktails ... [https://www.sciencedirect.com/science/article/abs/pii/S0017931014006140]
- 54. An improved vitrification protocol for the fast and safe ... [https://pubmed.ncbi.nlm.nih.gov/40981676/]
- 55. Understanding osmoregulation, cryoprotectant toxicity, and ... [https://www.sciencedirect.com/science/article/pii/S0011224025000410]
- 56. Screening for novel factors involved in mouse early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575340/]
- 57. Cryopreservation of Mouse Embryos by Ethylene Glycol-Based Vitrification - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3308583/]
- 58. Cryopreservation - Vitrification [https://www.vitrolife.com/ivf-journey/cryopreservation/]
- 59. High survival of mouse oocytes using an optimized ... [https://www.nature.com/articles/srep19465]
- 60. Automation in vitrification and thawing of mouse oocytes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10764471/]
- 61. Cryopreservation Protocols for Genetically Engineered Mice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8211118/]
- 62. Ultra-Fast Vitrification: Minimizing the Toxicity of ... [https://www.mdpi.com/1422-0067/25/3/1884]
- 63. Equilibrium vitrification of mouse embryos at various ... [https://pubmed.ncbi.nlm.nih.gov/33563870/]
- 64. Development and validation of machine learning models ... [https://www.nature.com/articles/s41598-025-06998-4]
- 65. Principles and Protocols For Post-Cryopreservation Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9113563/]
- 66. Cryopreservation of Embryos and Oocytes in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3980916/]
- 67. Quantitative assessment of the impact of cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02054-2]
- 68. Cryopreservation of Mouse Embryos by Ethylene Glycol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3308583/]
- 69. Cryostorage failures: a medicolegal review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6603075/]
- 70. A quantitative analysis of the impact of cryopreservation on ... [https://pubmed.ncbi.nlm.nih.gov/10611209/]
- 71. Cell Freezing Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 72. Chemical approaches to cryopreservation [https://www.nature.com/articles/s41570-022-00407-4]
- 73. Protective role of natural saccharides in frozen animal food ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025067790]
- 74. Cryopreservation of biological materials: applications and ... [https://link.springer.com/article/10.1007/s11626-025-01027-0]
- 75. The Dominance of Warming Rate Over Cooling Rate in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2729265/]
- 76. A review of best practices of rapid-cooling vitriï¬cation for ... [https://www.asrm.org/practice-guidance/practice-committee-documents/a-review-of-best-practices-of-rapid-cooling-vitrication-for-oocytes-and-embryos-a-committee-opinion-2021/]
- 77. Sound waves for solving the problem of recrystallization in ... [https://www.nature.com/articles/s41598-023-34681-z]
- 78. The effects of temperature variation treatments on ... [https://www.nature.com/articles/s41598-022-06158-y]
- 79. The Effect of Temperature on the Embryo Development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10607546/]
- 80. Heat Shock Differentially Compromises Embryonic ... [https://www.mdpi.com/2076-2615/15/22/3293]
- 81. Comparison of Permeating and Nonpermeating ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224001923004]
- 82. Safety of embryo cryopreservation: insights from mid-term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11241961/]
- 83. The Comparative Studies on Spermatozoa ... [https://www.slarc.org.cn/dwyx/EN/abstract/abstract3485.shtml]
- 84. Effects of vitrified cryopreservation duration on IVF and ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-022-01035-8]
- 85. Cryopreservation and its clinical applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5395684/]
- 86. Overcoming ice: cutting-edge materials and advanced ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03265-6]
- 87. Ice formation and its elimination in cryopreservation of ... [https://www.nature.com/articles/s41598-024-69528-8]
- 88. Controlled ice nucleation in cryopreservation--a review [https://pubmed.ncbi.nlm.nih.gov/23246475/]
- 89. Applying soft matter techniques to solve challenges in ... [https://www.frontiersin.org/journals/soft-matter/articles/10.3389/frsfm.2023.1219497/full]
- 90. Soft liquid metal nanoparticles achieve reduced crystal ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706119307640]
- 91. Preclinical validation of fast oocyte vitrification and ... [https://pubmed.ncbi.nlm.nih.gov/40334080/]
- 92. 2025 ESHRE/ALPHA consensus on how eggs, embryos ... [https://www.remembryo.com/2025-eshre-alpha-consensus-on-how-eggs-embryos-are-evaluated-in-the-ivf-lab/]
- 93. Screening for novel factors involved in mouse early ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1643551/full]
- 94. Cryopreservation and post-thaw differentiation of monocytes ... [https://pubs.rsc.org/en/content/articlehtml/2025/lp/d5lp00131e]
- 95. Association Between Human Embryo Culture Conditions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298697/]
- 96. Establishment of a mouse embryo bank at ICTB/FIOCRUZ [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614882/]
- 97. Morphological changes in mouse embryos cryopreserved ... [https://pubmed.ncbi.nlm.nih.gov/17177277/]
- 98. Blastocyst culture and transfer in clinically assisted ... [https://www.asrm.org/practice-guidance/practice-committee-documents/blastocyst-culture-and-transfer-in-clinically-assisted-reproduction-a-committee-opinion-20182/]
- 99. Three simple metrics to define in vitro fertilization success ... [https://www.sciencedirect.com/science/article/pii/S0015028220304246]
- 100. Live birth rates in natural compared to artificial frozen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257601/]
- 101. Determining Factors Influencing The Successful Embryo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11589970/]
- 102. Embryo & Sperm Cryopreservation and Revival Services [https://transgenic.uci.edu/services/embryo-sperm-cryopreservation-and-revival-services/]
- 103. Cryopreservation of Mouse Embryos of Sperm [https://www.ibr.hawaii.edu/tmii/services1/cryopreservation-of-mouse-embryos-or-sperm.html]
- 104. Embryo vs. Sperm Cryopreservation [https://www.cgm.northwestern.edu/cores/ttml/cryopreservation-of-mouse-lines/methods/index.html]
- 105. Cryopreservation of mouse resources - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7495967/]
- 106. Embryo Cryopreservation [https://biotech.wisc.edu/animalmodels/embryo-cryopreservation/]
- 107. Easy and quick (EQ) sperm freezing method for urgent ... [https://www.nature.com/articles/s41598-021-93604-y]
- 108. Emerging applications of sperm, embryo and somatic cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3472131/]
- 109. Rapid quantification of multi-cryoprotectant toxicity using an ... [https://pubmed.ncbi.nlm.nih.gov/33157080/]
- 110. High throughput method for simultaneous screening of ... [https://www.nature.com/articles/s41598-025-85509-x]
- 111. Prolonged Cryopreservation Negatively Affects Embryo ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.709648/full]
- 112. Prolong cryopreservation duration negatively affects ... [https://www.sciencedirect.com/science/article/abs/pii/S0301211522006248]
- 113. Study on the optimal time limit of frozen embryo transfer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10977551/]