Key Factors Influencing Mouse Embryo Implantation Success: A Comprehensive Guide for Researchers
This article synthesizes current research on the molecular, cellular, and technical factors determining mouse embryo implantation success, a critical model for reproductive biology and drug development.
Key Factors Influencing Mouse Embryo Implantation Success: A Comprehensive Guide for Researchers
Abstract
This article synthesizes current research on the molecular, cellular, and technical factors determining mouse embryo implantation success, a critical model for reproductive biology and drug development. It explores foundational biological mechanisms, including the roles of the LIF/STAT3 pathway, blastocyst hatching dynamics, and immune gene regulation. The content further details advanced methodological approaches for improving embryo quality in vitro, troubleshooting common challenges like recurrent implantation failure, and validating embryo potential through novel imaging and biomarkers. Aimed at researchers and scientists, this review provides a framework for optimizing experimental design and translating findings to enhance clinical outcomes in assisted reproductive technologies.
Decoding the Core Molecular and Cellular Mechanisms of Implantation
In eutherian mammals, the successful establishment of pregnancy hinges on embryo implantation, a complex biological process representing the first critical point of interaction between the maternal endometrium and the developing blastocyst. The molecular dialogue between a receptive uterus and an implantation-competent blastocyst must be exquisitely synchronized, with disruptions in this process representing a significant cause of infertility in both humans and model organisms. Central to this dialogue is the Leukemia Inhibitory Factor (LIF) receptor/Glycoprotein 130-Janus Kinase-Signal Transducer and Activator of Transcription 3 (LIFR/Gp130-JAK/STAT3) signaling axis, which has emerged as a master regulator of uterine receptivity. Within the context of mouse embryo implantation success rates, this signaling pathway integrates hormonal cues with cellular responses to orchestrate the transition of the endometrium from a pre-receptive to a receptive state, enabling blastocyst attachment and subsequent decidualization. This technical guide synthesizes current research to provide an in-depth analysis of this critical signaling axis, its molecular mechanisms, experimental evidence of its functions, and the technical approaches used to investigate its role in embryo implantation.
Molecular Architecture of the LIFR/Gp130-JAK/STAT3 Signaling Axis
Core Signaling Components and Pathway Activation
The LIFR/Gp130-JAK/STAT3 pathway constitutes a highly specialized signaling cascade that translates extracellular cytokine signals into specific gene expression programs within uterine cells. The molecular architecture begins with LIF, a member of the interleukin-6 (IL-6) family of cytokines, binding to its heterodimeric receptor complex composed of the LIF-specific receptor (LIFR) and the signal-transducing subunit glycoprotein 130 (Gp130) [1]. This ligand-receptor interaction induces conformational changes that activate receptor-associated Janus kinases (JAKs), leading to tyrosine phosphorylation of the receptors and creation of docking sites for Src homology-2 (SH2) domain-containing proteins, most notably STAT3 [1]. Once recruited to the receptor complex, STAT3 molecules are phosphorylated on tyrosine 705 residues, inducing their dimerization and subsequent nuclear translocation. Within the nucleus, STAT3 dimers bind to specific promoter and enhancer regions of target genes, initiating transcriptional programs essential for uterine receptivity and embryo implantation [1] [2].
Parallel to the JAK/STAT3 pathway, LIF binding to the LIFRβ/gp130 receptor can also activate secondary signaling cascades, including the mitogen-activated protein kinase (MAPK) and phosphatidylinositol-3 phosphate kinase (PI3K) pathways [1]. The activated gp130 receptor associates with the protein tyrosine phosphatase SHP-2, which serves as a positive effector of the MAPK signaling cascade through recruitment of Gab1 adaptor protein, ultimately leading to activation of ERK1 and ERK2 kinases [1]. Similarly, PI3K activation leads to phosphorylation of AKT/PKB, influencing multiple cellular processes including cell survival, metabolism, and adhesion. This signaling diversification enables the LIF pathway to coordinate multiple aspects of uterine remodeling necessary for successful implantation.
Pathway Visualization
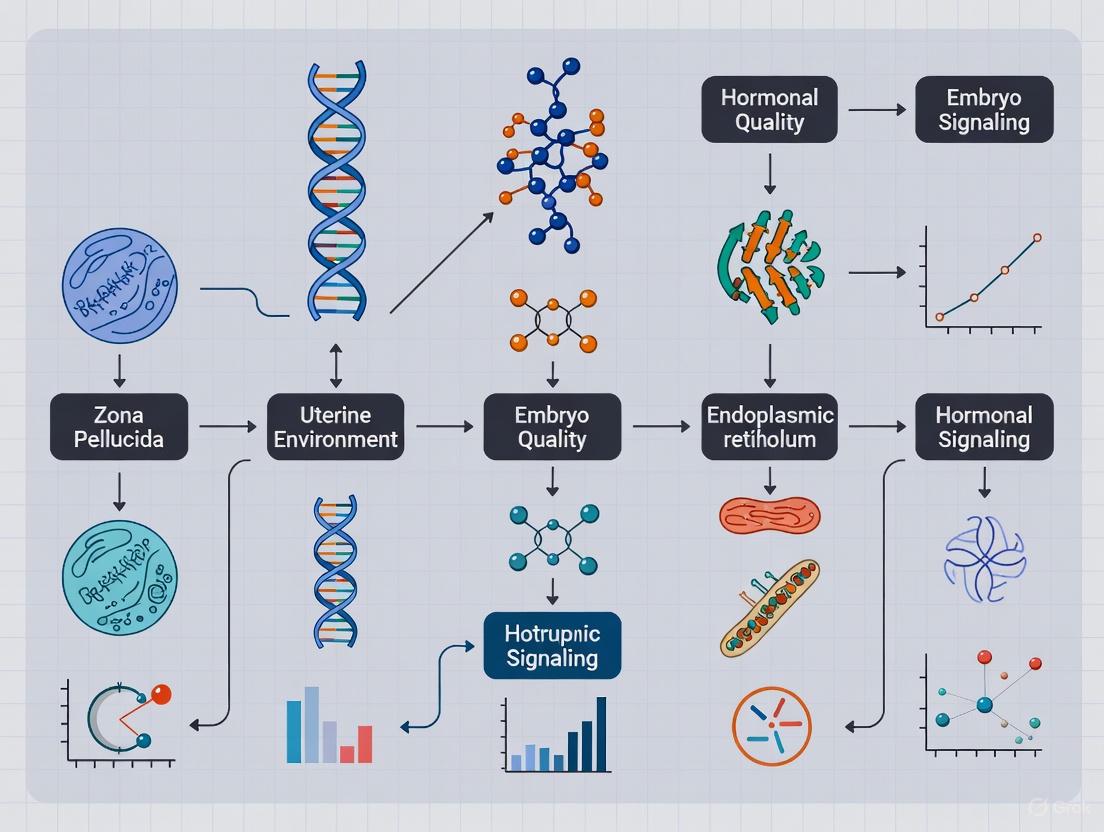
The following diagram illustrates the core LIFR/Gp130-JAK/STAT3 signaling pathway and its role in uterine receptivity:
Figure 1: The LIFR/Gp130-JAK/STAT3 Signaling Pathway in Uterine Receptivity. This diagram illustrates the core signaling cascade from LIF binding to transcriptional regulation of genes essential for uterine receptivity and embryo implantation. The negative feedback loop mediated by SOCS3 provides regulatory control.
Experimental Evidence: Establishing Essential Roles in Implantation
Genetic Knockout Models Reveal Non-Redundant Functions
The development of tissue-specific conditional knockout mouse models has been instrumental in elucidating the essential, non-redundant functions of the LIFR/Gp130-JAK/STAT3 signaling axis in uterine receptivity and embryo implantation. These genetic approaches have demonstrated that each component of this pathway plays indispensable but distinct roles in the implantation process.
Table 1: Phenotypes of Uterine Epithelium-Specific Knockout Mice in the LIFR/Gp130-JAK/STAT3 Pathway
| Genetic Model | Fertility Status | Primary Defect | Additional Phenotypic Features | Citation |
|---|---|---|---|---|
| Lifr eKO | Completely infertile | Implantation failure | Altered epithelial gene expression; Disrupted ERBB2 signaling | [3] [4] |
| Gp130 eKO | Completely infertile | Implantation failure | Defective epithelial remodeling; Reduced hormone responsiveness; Immune cell infiltration | [5] [3] |
| Stat3 eKO | Completely infertile | Implantation failure | Disrupted epithelial transition to attachment phase; Impaired decidualization | [5] [2] |
| Lif eKO | Completely infertile | Embryo attachment failure | Failure of luminal closure and crypt formation; Disrupted epithelial gene expression | [2] |
| Lif uKO | Completely infertile | Embryo attachment failure | Unrescued by recombinant LIF; Severe defects in implantation chamber formation | [2] |
The distinct expression patterns of LIFR and Gp130 in the uterine epithelium immediately prior to implantation initially suggested potential functional divergence, yet both receptors prove essential for successful implantation [3] [4]. While these receptors typically function as heterodimers, their non-overlapping knockout phenotypes indicate they may activate partially distinct downstream signaling effectors or interact with different co-receptors in uterine tissue.
Quantitative Analysis of Implantation Success in Intervention Studies
Pharmacological and biochemical interventions have further elucidated the functional significance of the LIFR/Gp130-JAK/STAT3 pathway and explored potential therapeutic applications for implantation failure.
Table 2: Quantitative Analysis of Implantation Success Following Experimental Interventions
| Experimental Intervention | Model System | Effect on Implantation | Molecular Outcome | Citation |
|---|---|---|---|---|
| RO8191 (STAT3 activator) | Delayed implantation model | Induced implantation; Rescue of implantation in Lifr eKO mice | Selective STAT3 activation in epithelial and stromal compartments; Partial decidual response in Stat3/Gp130 eKO | [5] |
| Recombinant LIF protein | Lif eKO mice | Rescued reproductive phenotype | Restoration of epithelial gene expression; Activation of nuclear STAT3 | [2] |
| Recombinant LIF protein | Lif uKO mice | Did not rescue attachment failure | Inability to restore implantation chamber formation | [2] |
| ERBB2 inhibitors (Tucatinib/Sapitinib) | Wild-type mice | Prevented embryo implantation | Disruption of LIFR-ERBB2 signaling axis | [3] [4] |
| Cardiotrophin-1 (CT-1) | Delayed implantation model | Induced implantation | Activation of STAT3 signaling in uterine epithelium | [3] |
The experimental compound RO8191, identified as a potent STAT3 activator, has demonstrated remarkable efficacy in inducing embryo implantation and decidual reaction in delayed implantation models through selective activation of STAT3 (but not STAT1) signaling in both epithelial and stromal compartments [5]. Notably, RO8191 administration was able to rescue implantation and establish pregnancy even in uterine epithelial-specific Lifr conditional knockout mice, which typically exhibit complete infertility due to implantation failure [5]. This suggests that direct STAT3 activation can bypass the requirement for upstream LIF-LIFR signaling. However, in uterine epithelial-specific Stat3 or Gp130 conditional knockout mice, RO8191 induced only a partial decidual response, indicating that both STAT3 and Gp130 are essential for the complete implantation response [5].
Experimental Methodologies for Investigating the Pathway
Delayed Implantation Model and RO8191 Treatment Protocol
The delayed implantation (DI) mouse model provides a valuable experimental system for investigating molecular mechanisms underlying embryo implantation and testing potential therapeutic compounds [5]. The following workflow and protocol detail the establishment of this model and the testing of STAT3 activators:
Figure 2: Experimental Workflow for Delayed Implantation Model and RO8191 Treatment. This diagram outlines the key procedural steps for establishing delayed implantation and testing STAT3 activators like RO8191.
Detailed Protocol:
- Ovariectomy Timing: Perform ovariectomy on plug-positive ICR females between 1300 and 1530 h on day 3 (D3) of pregnancy under sevoflurane anesthesia [5].
- Progesterone Administration: Administer siliconized medroxyprogesterone acetate (MPA, 100 µl/head) subcutaneously in the ventral region immediately following ovariectomy to maintain delayed implantation [5].
- Compound Treatment: On D7, prepare RO8191 (400 µg/head) dissolved in sesame oil and administer via single intraperitoneal injection at 1300 h. Use sesame oil alone as a negative control and E2 (25 ng/head) as a positive control [5].
- Tissue Collection and Analysis: Euthanize mice in a carbon dioxide chamber and dissect at 1300 h on D10 to count implantation sites. For molecular analysis, collect uterine tissues at 6 h (for immunohistochemistry) and 24 h (for Western blot analysis) after treatment [5].
- Exclusion Criteria: Exclude from statistical analysis any DI mice that have no implantation sites and from which no blastocyst can be recovered via uterine flushing with saline solution [5].
Conditional Knockout Mouse Generation and Validation
The generation of tissue-specific conditional knockout mice has been critical for delineating the uterine-specific functions of pathway components without the confounding effects of systemic knockout phenotypes:
Genetic Engineering Protocol:
- Mouse Strains: Utilize the following commercially available strains: LtfiCre/+ (JAX: 026030) for uterine epithelium-specific deletion, Stat3flox/flox, Gp130flox/flox, and Lifrflox/flox mice [5] [3].
- Crossing Strategy: Cross floxed mice with LtfiCre/+ mice to generate uterine epithelial-specific conditional knockout (cKO) models (Stat3 cKO, Gp130 cKO, or Lifr cKO) [5].
- Genotyping Primers:
- LtfiCre: 5'-GTTTCCTCCTTCTGGGCTCC-3', 5'-TTTAGTGCCCAGCTTCCCAG-3', and 5'-CCTGTTGTTCAGCTTGCACC-3' [5]
- Stat3flox: 5'-CCTGAAGACCAAGTTCATCTGTGTGAC-3', 5'-CACACAAGCCATCAAACTCTGGTCTCC-3', and 5'-GATTTGAGTCAGGGATCCTTATCTTCG-3' [5]
- Gp130flox: 5'-GGCTTTTCCTCTGGTTCTTG-3' and 5'-CAGGAACATTAGGCCAGATG-3' [5]
- Lifrflox: 5'-TGAGAGCACGGAAGCTCTTT-3' and 5'-ACTGCCCGACAAGGTTTTTA-3' [5]
- Phenotypic Validation: Confirm knockout efficiency through quantification of implantation sites following blue dye injection, histological analysis of uterine tissues, and molecular analysis of pathway component expression [3] [4].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating the LIFR/Gp130-JAK/STAT3 Pathway
| Reagent / Model | Specific Application | Function / Purpose | Source / Reference |
|---|---|---|---|
| RO8191 | STAT3 pathway activation | Small molecule STAT3 activator; induces implantation in delayed models | TargetMol (T22142) or Sigma-Aldrich (SML1200) [5] |
| Delayed Implantation Model | Implantation timing studies | Allows synchronization of implantation events; tests implantation competence | [5] |
| LtfiCre/+ mouse | Tissue-specific knockout | Enables uterine epithelium-specific gene deletion | JAX: 026030 [5] [3] |
| Recombinant LIF protein | Pathway stimulation | Rescues implantation in Lif-deficient models; tests LIF sufficiency | [2] |
| ERBB2 inhibitors (Tucatinib/Sapitinib) | Signaling inhibition | Blocks LIFR-ERBB2 signaling axis; tests pathway necessity | TargetMol (T2346); Selleck Chemicals (AZD8931) [3] [4] |
| Conditional knockout mice (Stat3, Gp130, Lifr floxed) | Genetic pathway dissection | Enables cell-type specific deletion of pathway components | [5] [3] |
| UT-B-IN-1 | UT-B-IN-1, MF:C20H17N5O2S3, MW:455.6 g/mol | Chemical Reagent | Bench Chemicals |
| 5-Methyl-4-phenyl-2-pyrimidinethiol | 5-Methyl-4-phenyl-2-pyrimidinethiol|CAS 857412-75-0 | High-purity 5-Methyl-4-phenyl-2-pyrimidinethiol for pharmaceutical research. CAS 857412-75-0. For Research Use Only. Not for human use. | Bench Chemicals |
Advanced Concepts and Emerging Research Directions
Spatiotemporal Regulation of Uterine Receptivity
Recent research has revealed sophisticated spatiotemporal regulation of LIF signaling within the uterine environment. LIF exhibits dynamic expression patterns, being abundantly expressed in the glandular epithelium during the blastocyst-receptive phase and subsequently induced in the stroma surrounding attached blastocysts [2]. This patterned expression suggests distinct functional roles for epithelial versus stromal LIF signaling. Studies using uterine epithelial-specific Lif knockout (Lif eKO) and uterine-specific Lif knockout (Lif uKO) mice demonstrate that epithelial LIF is sufficient for embryo attachment, while stromal LIF is essential for the formation of proper implantation chambers [2].
Three-dimensional imaging of the uterine epithelium has revealed that luminal closure and crypt formation—critical architectural changes required for embryo implantation—are regulated by the uterine LIF-STAT3 axis in coordination with the presence of blastocysts [2]. RNA sequencing analyses of luminal epithelia from Lif eKO mice have further identified that LIF governs the transition of uterine epithelium from the receptive to embryo-attaching phase by activating nuclear STAT3 and regulating genes associated with cytokine signaling and angiogenesis [2].
Cross-Talk with Other Signaling Pathways
The LIFR/Gp130-JAK/STAT3 axis does not function in isolation but engages in extensive cross-talk with other signaling pathways critical for uterine receptivity:
ERBB2 Signaling: Recent research has identified LIFR-mediated ERBB2 signaling as essential for successful embryo implantation [3] [4]. Hub gene analysis of differentially expressed genes in both Lifr eKO and Gp130 eKO mice identified Erbb2 and c-Fos as key regulators, suggesting novel signaling connections beyond the canonical JAK/STAT3 pathway [3].
Hormonal Signaling Pathways: The LIF-STAT3 axis interfaces with progesterone and estrogen signaling in complex ways. LIF appears to suppress Pgr-induced genes in the luminal epithelium, facilitating the transition to an attachment-competent state [2]. This interaction is critical given that sustained or excessive P4-Pgr signaling can disturb embryo attachment [2].
Immune Regulation: Gp130 eKO mice display defective epithelial remodeling accompanied by immune cell infiltration in the endometrium, suggesting connections between LIF signaling and immune regulation during implantation [3].
The LIFR/Gp130-JAK/STAT3 signaling axis represents a master regulatory circuit that coordinates uterine receptivity and embryo implantation through precise spatiotemporal control of gene expression programs in the uterine epithelium and stroma. Genetic evidence firmly establishes that each component of this pathway—LIF, LIFR, Gp130, and STAT3—is indispensable for successful implantation in murine models. The development of pharmacological activators like RO8191 that can bypass upstream signaling defects to directly activate STAT3 offers promising therapeutic avenues for addressing implantation failure in clinical contexts.
Future research directions should focus on elucidating the complete transcriptional networks downstream of STAT3 in uterine cells, understanding the molecular basis of sexual dimorphism in pathway regulation, and exploring potential cross-species conservation of these mechanisms to inform human fertility treatments. The continued investigation of this critical signaling axis will not only enhance our fundamental understanding of reproductive biology but may also yield novel diagnostic and therapeutic approaches for addressing infertility in human patients.
Blastocyst hatching, the process whereby the mammalian embryo escapes its zona pellucida (ZP), is a critical prerequisite for successful implantation. While traditionally viewed as a mechanical event, recent research reveals that hatching is a biologically nuanced process, with the specific site of ZP exit playing a potentially decisive role in subsequent implantation success. This review synthesizes emerging evidence from mouse models, demonstrating that the location of the hatching aperture is non-random and is linked to distinct molecular programs that influence embryonic developmental potential. We delve into the molecular mechanisms, including ion transporters, proteases, and immune-related gene expression, that underpin these site-specific dynamics. Furthermore, we evaluate the translational implications of these findings for assisted reproductive technologies (ART), particularly regarding the efficacy and methodology of assisted hatching. The synthesis of quantitative data, experimental protocols, and key signaling pathways provided herein aims to equip researchers and drug development professionals with a comprehensive toolkit for advancing this critical area of reproductive biology.
In mammalian embryonic development, blastocyst hatching represents the crucial transition from a free-floating entity to one capable of direct interaction with the maternal endometrium. This process, essential for implantation and the establishment of pregnancy, involves a combination of blastocoel cavity expansion, ZP thinning, and proteolytic degradation [6]. Historically, the focus has been on the timing and mere occurrence of hatching; however, a growing body of evidence suggests that the precise location of the hatching site relative to the inner cell mass (ICM) is a significant determinant of embryonic fate [7]. This technical guide explores the sophisticated dynamics of site-specific ZP exit, integrating foundational knowledge with recent breakthroughs that have begun to decipher how the hatching site governs implantation potential. Framed within broader research on factors affecting mouse embryo implantation success, this review provides an in-depth analysis of the mechanisms, consequences, and research methodologies central to understanding blastocyst hatching dynamics.
Molecular and Cellular Mechanisms of Hatching
The process of blastocyst hatching is governed by a concert of biophysical and biochemical mechanisms. The trophectoderm (TE), the outer cell layer of the blastocyst, plays the lead role in executing this escape.
- Biophysical Forces: A primary driver is the elevated osmotic pressure within the blastocoel cavity, created by the active transport of ions, particularly through Na+/K+ ATPase pumps located on TE cells. This pumping action draws water into the cavity, increasing internal pressure and exerting a mechanical force against the ZP [6] [7].
- Biochemical Degradation: Concurrently, TE cells produce and secrete a repertoire of proteases that hydrolyze the glycoprotein matrix of the ZP. These enzymes locally weaken the ZP, creating a focal point where the combined pressure and enzymatic activity can lead to rupture and embryo extrusion [6]. The site where the TE initially herniates through the ZP is defined as the hatching site.
The interplay between global pressure and localized degradation suggests an inherent capacity for the blastocyst to regulate the location of its exit, a process that appears to have significant developmental consequences.
Site-Specific Hatching and Its Impact on Implantation Potential
The hypothesis that the hatching site is random has been challenged by detailed morphological and transcriptomic analyses. Evidence from mouse models indicates a site preference that correlates strongly with subsequent implantation success and pregnancy outcomes.
A 2020 study by Liu et al. classified over 1,800 mouse hatching blastocysts based on the angle (θ) between the hatching site and the arc midpoint of the ICM. Their analysis revealed a non-random distribution [8]. The table below summarizes their key findings on site distribution and developmental outcomes after transfer.
Table 1: Distribution of Hatching Sites and Resulting Developmental Outcomes in Mice
| Hatching Site Category (Angle θ) | Distribution of Blastocysts | Implantation Rate | Development to Term |
|---|---|---|---|
| 0° ≤ θ ≤ 30° (near ICM) | 30.60% | No significant difference | ~30% (No significant difference) |
| 30° < θ ≤ 60° | 43.84% | No significant difference | ~30% (No significant difference) |
| 60° < θ ≤ 90° (opposite ICM) | 21.67% | No significant difference | ~30% (No significant difference) |
| Multiple Hatching Sites | 3.89% | Not reported | Not reported |
This study concluded that while hatching site distribution was not random, the site itself had no measurable impact on implantation rates, pregnancy maintenance, litter size, or offspring health [8].
In contrast, a more recent study by An et al. (2025) presented a different classification system and reached a contrasting conclusion. They classified hatching into sites relative to an "ICM clock" and found a strong correlation between hatching site and birth rate [7].
Table 2: Hatching Site Classification and Birth Rates by An et al.
| Hatching Site | Description | Birth Rate After Transfer |
|---|---|---|
| B-site | 3 o'clock (beside ICM) | 65.6% |
| A-site | 1-2 o'clock (near ICM) | 55.6% |
| C-site/D-site | 4-6 o'clock (opposite ICM) | 21.3% |
| Failure to Hatch | Non-hatching blastocysts | 5.1% |
This work demonstrated that blastocysts hatching from sites near or beside the ICM (A and B sites) had significantly higher developmental potential than those hatching from sites opposite the ICM [7].
Transcriptomic Underpinnings of Site-Specific Potential
The disparity in developmental outcomes is rooted in distinct gene expression profiles. RNA-seq analysis of blastocysts grouped by hatching site revealed that embryos with high implantation potential (A and B sites) cluster closely together, while those with poor potential (C site and non-hatching) form a separate cluster [7].
- Differentially Expressed Genes (DEGs): A comparison between B-site (high success) and C-site (low success) blastocysts identified 178 differentially expressed genes. These genes were significantly enriched in immune-related pathways [7].
- Key Regulators: Transcription factors TCF24 and DLX3 were identified as primary regulators of these DEGs. Furthermore, a specific transcriptional switch, involving upregulation by transcription factor ATOH8 and downregulation by SPIC, activates immune pathways as the blastocyst progresses from expansion to full hatching [7].
- Critical Immune Genes: Upregulated genes in successfully hatching blastocysts included
Ptgs1,Lyz2,Il-α, andCfb, whileCd36was downregulated. Immunofluorescence confirmed the presence of immune factors like C3 and IL-1β on the extra-luminal surface of the TE, suggesting their role in preparing for maternal-fetal crosstalk [7].
This work provides a molecular rationale for the observed phenotypic differences, positioning the immune properties of the preimplantation embryo as a major determinant of hatching success and subsequent implantation competence.
Essential Signaling Pathways Governing Implantation
Successful implantation depends on a synchronized dialogue between a receptive endometrium and a mature, hatched blastocyst. Key signaling pathways, particularly in the uterus, are essential for this process.
The LIFR/GP130-JAK-STAT3 Axis
The Leukemia Inhibitory Factor (LIF) signaling pathway is a master regulator of implantation in mice.
- LIF, expressed in the uterine glandular epithelium in response to estrogen, binds to a heterodimeric receptor complex composed of LIFR (LIF receptor) and GP130 on the luminal epithelium [9] [3].
- This binding activates the associated JAK kinases, which phosphorylate the transcription factor STAT3.
- Phosphorylated STAT3 (p-STAT3) dimerizes and translocates to the nucleus, driving the expression of genes essential for endometrial receptivity and embryo adhesion [9].
The non-redundant criticality of this pathway is demonstrated by the complete infertility observed in mouse models with uterine epithelial-specific knockout of Lif, Lifr, Gp130, or Stat3, all of which result in implantation failure [9] [3].
Figure 1: The LIFR/GP130-JAK-STAT3 Signaling Pathway in Implantation. This pathway is essential for establishing uterine receptivity in mice.
Novel Pharmacological Activation and Cross-Talk
Recent research has identified RO8191, a small-molecule interferon agonist that also acts as a potent STAT3 activator. In mouse delayed implantation models, RO8191 was able to induce embryo implantation and decidualization, even in uterine epithelial-specific Lifr conditional knockout mice [9]. This suggests that RO8191 can bypass the need for the LIF ligand and LIFR component to trigger the critical downstream STAT3 signaling.
Further investigation into Lifr and Gp130 knockout models revealed that while both receptors are required for fertility, they mediate non-identical signaling outputs. Hub gene analysis identified ERBB2 (a receptor tyrosine kinase) and c-Fos as key downstream regulators, outlining a crucial role for LIFR-mediated ERBB2 signaling in successful implantation [3].
Research Methodologies and Experimental Protocols
This section details key experimental approaches for studying blastocyst hatching and implantation in mouse models.
The following methodology, adapted from An et al. and Liu et al., is used to investigate the relationship between hatching site and developmental potential [8] [7].
- Embryo Collection: Superovulate 6-8 week old CD-1 or ICR female mice using PMSG and hCG. Mate with fertile males and check for vaginal plugs (designated 0.5 dpc). Flush expanding blastocysts from the uterus at 3.5 dpc using M2 medium.
- In Vitro Culture: Culture flushed blastocysts in KSOM medium under mineral oil in a standard cell culture incubator (37°C, 5% CO2).
- Site Classification: After 6-8 hours of culture, observe blastocysts and classify the hatching site based on the relative position to the ICM.
- Embryo Transfer: Use a non-surgical embryo transfer (NSET) device to transfer classified, hatching blastocysts into pseudopregnant recipient females.
- Outcome Assessment: Monitor recipients for implantation sites, pregnancy rates, litter size, and offspring health to correlate with the initial hatching site.
Protocol: The Delayed Implantation (DI) Model
The DI model is a powerful tool for dissecting the molecular requirements for implantation, as it uncouples embryo development from uterine receptivity [9].
- Ovariectomy: On day 3 of pregnancy (D3), perform ovariectomy on plug-positive female mice under anesthesia.
- Progesterone Maintenance: Administer medroxyprogesterone acetate (MPA) subcutaneously daily to maintain a state of delayed implantation. In this state, blastocysts hatch but remain dormant in the uterus.
- Experimental Intervention: On D7, administer a single injection of the experimental stimulus. This can be:
- Positive Control: Estradiol (E2, 25 ng/head).
- Test Compound: e.g., RO8191 (400 µg/head, i.p.) [9].
- Vehicle Control: Sesame oil.
- Tissue Collection: Euthanize mice 24-72 hours post-injection. Collect uterine tissue to:
- Count implantation sites visualized by Chicago Blue dye injection.
- Analyze molecular changes via Western blot or immunohistochemistry (e.g., p-STAT3 levels).
- Perform RNA sequencing for transcriptomic profiling.
The Scientist's Toolkit: Key Research Reagents
The table below catalogues essential reagents and their applications in studying blastocyst hatching and implantation.
Table 3: Essential Research Reagents for Embryo Implantation Research
| Reagent / Tool | Function / Application | Key Details / Example |
|---|---|---|
| RO8191 | A small-molecule STAT3 activator used to induce implantation in mouse models. | Can rescue implantation in Lifr cKO mice; useful for studying STAT3-dependent pathways [9]. |
| Tucatinib / Sapitinib | ERBB2 inhibitors used to probe the role of LIFR-ERBB2 signaling in implantation. | Orally administered; experiments with these inhibitors underscore the importance of ERBB2 signaling downstream of LIFR [3]. |
| SCADS Inhibitor Kits | Standardized libraries of low-molecular-weight inhibitors for screening novel developmental factors. | Used in high-throughput screens to identify proteins like Cathepsin D and CXCR2 as regulators of early development [10]. |
| Non-Surgical Embryo Transfer (NSET) Device | A device for transferring embryos into recipient mice without invasive surgery. | Minimizes stress and surgical complications; improves animal welfare and live birth rates in transfer experiments [8]. |
| Laser-Assisted Hatching (LAH) System | A microscopic laser used to create a precise opening in the ZP for assisted hatching studies. | Laser power ~400 mW, wavelength 1480 nm; used to study the effects of artificial hatching on re-expansion and implantation [11]. |
| ST-193 hydrochloride | ST-193 hydrochloride, MF:C24H26ClN3O, MW:407.9 g/mol | Chemical Reagent |
| 2-Cyclopropylethane-1-sulfonamide | 2-Cyclopropylethane-1-sulfonamide|CAS 1487784-84-8 | 2-Cyclopropylethane-1-sulfonamide for research. This sulfonamide derivative is for Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Discussion and Synthesis
The investigation into blastocyst hatching dynamics reveals a complex picture where the location of ZP exit is a biomarker of the embryo's underlying health and developmental potential. The apparent contradiction between studies finding no effect of hatching site [8] and those finding a strong correlation [7] may be reconciled by considering the molecular heterogeneity of blastocysts. The transcriptomic evidence from An et al. suggests that the hatching site itself may be a manifestation of pre-existing, global gene expression patterns, particularly in immune-related pathways, that ultimately dictate both the site selection and the capacity for successful maternal-fetal interaction [7].
From a translational perspective, these findings have significant implications for ART. The development of a predictive model for implantation success based on DEGs like Lyz2, Cd36, Cfb, and Cyp17a1 offers a potential new tool for embryo selection [7]. Furthermore, the nuanced effects of assisted hatching (AH)—where it may benefit poor-quality blastocysts (TE grade C) while potentially impairing the re-expansion of competent vitrified-warmed blastocysts—argues for a more refined, patient-specific application of this technique [11]. The discovery of pharmacological agents like RO8191 that can activate key implantation pathways also opens avenues for therapeutic intervention in cases of recurrent implantation failure [9].
The journey of the mammalian blastocyst out of its zona pellucida is far from a simple escape. It is a dynamic, biologically programmed event where the site of exit provides a critical window into the embryo's molecular constitution and future developmental potential. Research in mouse models has been instrumental in uncovering the intricate relationships between hatching location, immune gene activation, and implantation success. As the molecular players and signaling pathways continue to be elucidated, the opportunity to develop more sophisticated diagnostic tools and targeted interventions for human infertility grows. The ongoing challenge for researchers and clinicians is to translate these dynamic biological principles into strategies that improve outcomes in assisted reproduction and regenerative medicine.
The success of mouse embryo implantation is a complex biological process dependent on precise orchestration of immune-related gene expression at the maternal-fetal interface. This intricate crosstalk between maternal decidua and fetal trophoblast cells establishes a unique immunological microenvironment that facilitates embryonic acceptance while maintaining host defense capabilities. Recent advances in single-cell RNA sequencing and spatial transcriptomics have revealed unprecedented details about the transcriptional dynamics governing this relationship, providing new insights into the molecular mechanisms that determine implantation success. The maternal immune system undergoes remarkable adaptations during pregnancy, transitioning through pro-inflammatory, anti-inflammatory, and again pro-inflammatory phases to accommodate implantation, fetal development, and parturition [12] [13]. Understanding how immune-related gene networks coordinate these phases offers significant potential for improving outcomes in assisted reproductive technologies and addressing implantation failure.
Within the context of mouse embryo implantation research, this whitepaper examines how transcriptional regulation of immune mediators—including cytokines, growth factors, and epigenetic regulators—shapes the uterine environment for embryonic acceptance. We focus specifically on the molecular dialogue between maternal immune cells and developing embryos, highlighting technical approaches for quantifying these interactions and their implications for developmental success.
Quantitative Landscape of Immune-Mediated Implantation Success
Analysis of multiple studies reveals consistent quantitative relationships between specific immune-related gene expression patterns and embryo implantation outcomes in mouse models. The data demonstrate that transcriptional stability and specific immune signatures strongly correlate with implantation success rates.
Table 1: Key Quantitative Relationships in Immune-Related Gene Expression and Implantation Outcomes
| Experimental Factor | Measured Parameter | Impact on Implantation | Reference Model |
|---|---|---|---|
| Allogeneic MHC combinations | 25-30% reduction in "intrinsic" gene noise | Positive impact on embryonic mass | C57BL/6J embryos in surrogate mothers [14] |
| Maternal HFD-induced sncRNA alterations | 72.3% rsRNAs in UF vs 58.3% in controls (P=0.036) | Impaired blastocyst metabolic gene expression | Pre-implantation maternal HFD mouse model [15] |
| Ex vivo uterine culture system | >90% embryonic attachment efficiency | Enables implantation and embryogenesis | Air-liquid interface culture with PDMS devices [16] |
| Sequential embryo transfer | Significantly higher CPR and IR (P<0.01) | Beneficial for patients with repeated implantation failures | Frozen embryo transfer cycles [17] |
| "Intrinsic" gene noise | Negative correlation with embryonic mass & PLGF | Associated with phenotypic growth instability | C57BL/6J in NOD-SCID/BALB/c mothers [14] |
Table 2: Immune Cell Populations at the Maternal-Fetal Interface in Normal vs RM Conditions
| Cell Type | Normal Pregnancy (%) | Recurrent Miscarriage (RM) (%) | Primary Function |
|---|---|---|---|
| Dendritic Cells (DCs) | Lower proportion | Higher proportion | Antigen presentation, immune tolerance |
| Macrophages | Lower proportion | Higher proportion | Tissue remodeling, immune regulation |
| Villous Cytotrophoblasts (VCTs) | Lower proportion | Higher proportion | Trophoblast stem cells |
| Extravillous Trophoblasts (EVTs) | Higher proportion | Lower proportion | Spiral artery remodeling, invasion |
| Uterine Natural Killer (uNK) cells | 60-90% of decidual immune cells | Altered proportions | Vascular remodeling, cytokine secretion |
Methodologies for Assessing Transcriptional Landscapes
Single-Cell RNA Sequencing Analysis
Protocol Overview: Single-cell RNA sequencing (scRNA-seq) enables comprehensive profiling of transcriptional heterogeneity at the maternal-fetal interface. The standard protocol involves: (1) tissue collection and dissociation into single-cell suspensions from paired placental and decidual tissues; (2) cell partitioning and barcoding using microfluidic devices; (3) library preparation and sequencing; (4) bioinformatic analysis using Seurat and CellChat pipelines [18].
Technical Specifications: Cells with <600 detected genes or total mitochondrial gene expression >5% are typically removed during quality control. Differential expression analysis employs the FindMarkers function in Seurat with test.use = MAST, setting significance thresholds at p-value <0.05 and |log2(fold change)| >0.58. Cell communication analysis utilizes the CellChat R package to predict major signaling inputs and outputs and identify differentially expressed ligand-receptor pairs between normal and pathological pregnancies [18].
Application: This approach has revealed alterations in the cellular organization of the decidua and placenta in recurrent miscarriage (RM), identifying dysregulated interactions between trophoblast cells and decidual immune cells that contribute to implantation failure [18].
Statistical Framework for Developmental Instability Components
Protocol Overview: A specialized statistical framework dissects "extrinsic" (canalization) and "intrinsic" (fluctuating asymmetry, FA) components of developmental instability from bilateral trait measurements [14].
Technical Specifications: The method employs Principal Component Analysis (PCA) projection of left/right measurements on eigenvectors followed by Generalized Additive Models for Location Scale and Shape (GAMLSS) modeling of eigenvalues. The first eigenvalue represents "extrinsic" developmental instability, while the second represents "intrinsic" components. For a bilateral trait measured on left (l) and right (r) sides, "extrinsic" variance is calculated as Var[E(x|ξ)] = Var(l+r/2) ≈ ¼σ²l+r, while "intrinsic" variance is E[Var(x|ξ)] ≈ ¼FA = ¼σ²l-r [14].
Application: This framework demonstrated that allogeneic MHC combinations in C57BL/6J embryos developing in surrogate NOD-SCID and BALB/c mothers decreased both "extrinsic" and "intrinsic" gene expression noise, correlating with improved embryonic growth and developmental stability [14].
Ex Vivo Uterine Culture System
Protocol Overview: An ex vivo uterine system recapitulates bona fide implantation at >90% efficiency using authentic mouse embryos and uterine tissue [16].
Technical Specifications: The system utilizes air-liquid interface (ALI) culture with originally developed polydimethylsiloxane (PDMS) devices manufactured for optimal gas permeability. Day post coitum (dpc) 3.75 endometria are isolated and co-cultured with E3.75 blastocysts. The optimized EXiM medium, based on IVC2 medium containing KnockOut Serum Replacement (KSR) instead of Fetal Calf Serum (FCS), maintains physiological ovarian hormone levels (3 pg/mL for 17β-estradiol and 60 ng/mL for progesterone). The system uses 750 μm-thick PDMS ceilings, which produce optimal attachment efficiency (95.8%) while facilitating observation under fluorescent upright microscopes [16].
Application: This system has replicated the robust induction of maternal implantation regulator COX-2 at the attachment interface, accompanied by trophoblastic AKT activation, suggesting possible signaling mediating maternal-embryonic communication that accelerates implantation [16].
Signaling Pathways in Maternal-Fetal Crosstalk
Immune Signaling Pathways at Maternal-Fetal Interface
The diagram illustrates key signaling pathways mediating maternal-fetal crosstalk, highlighting how allogeneic MHC combinations decrease transcriptional noise to promote developmental stability and embryonic growth. Critical interactions include: (1) PVR-CD226/TIGIT signaling between extravillous trophoblasts and T cells/dendritic cells; (2) VEGF/PLGF secretion by uterine NK cells to promote vascular remodeling; (3) ADM-CALCRL signaling between EVTs and dendritic cells to promote immune tolerance; and (4) cytokine-mediated facilitation of trophoblast invasion by macrophages [14] [12] [18].
Epigenetic Regulation of Immune Gene Expression
Epigenetic mechanisms serve as critical interfaces between environmental signals and transcriptional responses at the maternal-fetal interface. DNA methylation patterns significantly influence immune cell function and trophoblast development through gene silencing mechanisms. DNMT1 maintains methylation status, while DNMT3A and DNMT3B act on unmethylated DNA, with TET proteins mediating demethylation processes. At the maternal-fetal interface, abnormal DNA methylation regulation affects embryonic development ability and interferes with the immune microenvironment, contributing to adverse pregnancy outcomes [13].
Histone modifications, including acetylation, methylation, and phosphorylation, provide another layer of epigenetic control that modulates chromatin structure and accessibility. Histone acetylation by HAT and HDAC enzymes balances transcriptional activation and repression, with specific HDACs (HDAC8, HDAC9) regulating M1/M2 macrophage polarization. Histone methylation at various lysine residues (H3K4, H3K9, H3K27, H3K36) either activates or represses transcription depending on the specific site and methylation level [13].
Non-coding RNAs, particularly small non-coding RNAs (sncRNAs) in reproductive fluids, have emerged as important mediators of maternal-embryonic communication. PANDORA-seq analysis revealed that tRNA-derived small RNAs (tsRNAs) and rRNA-derived small RNAs (rsRNAs) comprise over 80% of sncRNAs in oviduct and uterine fluids, exhibiting dynamic changes in response to maternal dietary factors like high-fat diet. These sncRNAs may reflect maternal metabolic status and transmit dietary information to early embryos, influencing implantation success and offspring health [15].
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Maternal-Fetal Transcriptional Landscapes
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Cell Markers | CD56, CD16, CD11c, KLRK1, NCR3 | Immune cell phenotyping | Distinguish uNK (CD56bright CD16-) from pbNK (CD56dim CD16+) cells [12] |
| Cytokines/Growth Factors | VEGF, PLGF, CSF1, CSF2, IL15 | Functional assays | uNK-derived angiogenic factors; stromal cell-mediated NK expansion [14] [12] |
| Epigenetic Tools | DNMT inhibitors, HDAC inhibitors, HAT activators | Epigenetic regulation studies | Modulate DNA methylation and histone acetylation at interface [13] |
| sncRNA Analysis | PANDORA-seq, LC-MS | sncRNA profiling | Comprehensive tsRNA/rsRNA detection with modification analysis [15] |
| Culture Media | EXiM medium, IVC2 with KSR | Ex vivo implantation models | Supports embryo development with optimized hormone levels [16] |
| Animal Models | C57BL/6J, NOD-SCID, BALB/c | MHC interaction studies | Allogeneic vs syngeneic maternal-fetal immune interactions [14] |
Experimental Workflow for Transcriptional Analysis
Workflow for Maternal-Fetal Interface Transcriptomics
The workflow outlines a comprehensive pipeline for analyzing transcriptional landscapes at the maternal-fetal interface, beginning with tissue collection and progressing through single-cell sequencing, bioinformatic analysis, and functional validation. Critical quality control metrics include filtering cells with fewer than 600 detected genes or greater than 5% mitochondrial gene expression. The analytical phase utilizes Seurat for cell clustering and differential expression analysis with MAST test, followed by CellChat for predicting cell-cell communication networks. Functional validation employs ex vivo uterine systems or targeted gene modulation to confirm identified pathways [16] [18].
The transcriptional landscape of immune-related gene expression at the maternal-fetal interface represents a sophisticated regulatory network that determines implantation success in mouse models. Key determinants include MHC-mediated interactions that reduce transcriptional noise and stabilize development, epigenetic mechanisms that fine-tune immune responses, and sncRNA-mediated communication that transmits maternal metabolic information to embryos. The integrated analysis of these elements through advanced technologies like scRNA-seq and ex vivo culture systems provides unprecedented insights into the molecular dialogue governing implantation. These findings not only illuminate fundamental biological processes but also offer promising avenues for developing targeted interventions to address implantation failure in clinical settings. Future research should focus on translating these mechanistic insights into diagnostic and therapeutic strategies that can improve pregnancy outcomes in assisted reproduction.
{/* Main content of the technical guide begins */}
Endocannabinoids and Other Signaling Molecules: Exploring the Uterine Milieu
The success of mouse embryo implantation is not an autonomous process but is critically dependent on a synchronized dialogue between the developing blastocyst and a receptive uterine environment. This review delves into the intricate signaling networks within the uterine milieu, with a particular focus on the endocannabinoid system as a pivotal regulator. We explore how molecules such as anandamide (AEA) and 2-arachidonoylglycerol (2-AG), signaling through their cognate receptors CB1 and CB2, create a precise biochemical landscape that guides preimplantation embryo development, oviductal transport, and decidualization. Disruption of this finely tuned system, through either genetic ablation of its components or pharmacological manipulation, leads to asynchronous development and implantation failure, ultimately compromising pregnancy rates. This whitepaper synthesizes key quantitative data and experimental methodologies from foundational studies, providing a technical resource for researchers and drug development professionals working to elucidate the fundamental mechanisms governing reproductive success.
Embryo implantation is a complex and critically timed biological process that represents a major rate-limiting step in mammalian pregnancy. In mice, successful implantation requires the simultaneous achievement of two key milestones: the development of the preimplantation embryo to the blastocyst stage, and the differentiation of the uterine endometrium into a receptive state, often termed the "window of implantation" [19]. A failure in this synchrony is a significant cause of early pregnancy loss. The uterine milieu, composed of a dynamic mix of signaling molecules, is the medium through which this maternal-embryonic cross-talk occurs. Among these signals, endocannabinoids—a class of endogenous lipid-based neurotransmitters—have emerged as crucial directors of early pregnancy events [20] [21]. Historically, the adverse effects of cannabis (marijuana) on female fertility were observed for decades, but the underlying molecular mechanisms remained elusive until the discovery of the endocannabinoid system [20]. This system, comprising endogenous ligands (e.g., AEA and 2-AG), their synthetic and degradative enzymes, and cannabinoid receptors, provides a molecular framework for understanding how the uterine environment is actively shaped to support reproduction. Framed within broader research on factors affecting mouse embryo implantation success, this review examines the endocannabinoid system as a central, model component of the signaling uterine milieu.
The Molecular Players: Composition of the Uterine Milieu
The biochemical environment of the uterus during the periimplantation period is defined by a precise balance of numerous factors, with the endocannabinoid system playing a prominent role.
Core Components of the Endocannabinoid System
The two most well-characterized endocannabinoids are anandamide (AEA) and 2-arachidonoylglycerol (2-AG). Both are lipid-derived molecules synthesized on demand that activate G-protein coupled cannabinoid receptors [20]. Despite their similar functions, they possess distinct biochemical properties and signaling efficacies. AEA often acts as a partial agonist of cannabinoid receptors, while 2-AG acts as a full agonist. However, the binding affinity of 2-AG to these receptors is approximately 24 times less than that of AEA [20].
Their levels are tightly regulated by specialized synthetic and degradative enzymes:
- AEA Synthesis and Degradation: AEA is primarily derived from the precursor N-arachidonoylphosphatidylethanolamine (NAPE). The canonical pathway involves cleavage by NAPE-hydrolyzing phospholipase D (NAPE-PLD) [20]. Alternative pathways via α/β-hydrolase 4 (Abh4) and a phospholipase C/protein tyrosine phosphatase (PTPN22) pathway also contribute [20] [21]. Its degradation is predominantly mediated by a membrane-bound fatty acid amide hydrolase (FAAH), which hydrolyzes AEA into ethanolamine and arachidonic acid [20] [22].
- 2-AG Synthesis and Degradation: 2-AG is produced from diacylglycerol (DAG) by sn1-diacylglycerol lipase (DAGL), which has two isoforms, DAGLα and DAGLβ [20]. It is degraded primarily by monoacylglycerol lipase (MAGL), and to a lesser extent by FAAH [20] [22].
The primary receptors for endocannabinoids are:
- Cannabinoid Receptor 1 (CB1): Encoded by the Cnr1 gene, CB1 is widely expressed in the central nervous system but is also found in peripheral tissues, including the uterus, oviduct, and preimplantation embryo [20] [21]. In blastocysts, CB1 is localized primarily in the trophectoderm [21].
- Cannabinoid Receptor 2 (CB2): Encoded by the Cnr2 gene, CB2 is predominantly expressed in immune cells but is also present in the preimplantation embryo, specifically in the inner cell mass (ICM) from the one-cell stage [20] [21].
Interaction with Other Signaling Pathways
The endocannabinoid system does not operate in isolation. It exhibits cross-talk with other critical pathways in the uterus:
- Vanilloid Receptors: AEA can also activate the transient receptor potential vanilloid 1 (TRPV1), a ligand-gated ion channel, triggering calcium influx and distinct cellular responses [20].
- Angiogenic Factors: Vascular endothelial growth factor (VEGF) and its receptor FLK1 are key regulators of uterine blood vessel remodeling. Their expression is intricately linked to endocannabinoid signaling during decidualization [23].
- Decidualization Markers: Morphogens and transcription factors such as BMP2 and HOXA10 are critical for stromal cell differentiation and are downstream of proper endocannabinoid signaling [23].
- Cyclooxygenase-2 (COX-2) / Prostaglandin Pathway: This enzyme, critical for implantation, also participates in metabolizing 2-AG, creating a direct biochemical link between the endocannabinoid and prostaglandin systems in the uterus [22].
The following diagram illustrates the core synthesis, signaling, and degradation pathways of the two major endocannabinoids.
Endocannabinoid Synthesis and Signaling Pathways
Quantitative Data: Concentrations, Localization, and Phenotypes
A comprehensive understanding of the uterine milieu requires an integration of quantitative data on endocannabinoid levels, spatiotemporal expression patterns, and the phenotypic outcomes of experimental manipulations. The following tables summarize key quantitative findings from foundational studies in mouse models.
Table 1: Endocannabinoid Levels and Receptor Expression in the Mouse Uterine Milieu
| Parameter | Measurement / Localization | Biological Significance | Experimental Context |
|---|---|---|---|
| Uterine 2-AG Level | One order of magnitude higher than AEA [22] | High basal level suggests 2-AG has distinct, non-redundant functions in uterine physiology. | Day 5-6 of pregnancy in mice [22]. |
| Uterine AEA Gradient | Lower at implantation sites; higher at interimplantation sites [22] | Creates a localized environment permissive for blastocyst implantation. | Day 5 of pregnancy in mice [22]. |
| CB1 Receptor Expression | Oviduct & uterus; Trophectoderm of blastocyst [20] [21] | Mediates effects on oviductal embryo transport and trophectoderm development. | Immunohistochemistry, in situ hybridization, RT-PCR [20] [21]. |
| CB2 Receptor Expression | Inner Cell Mass (ICM) of blastocyst [21] | Suggests a specific role in regulating development of the embryo proper. | Immunohistochemistry, in situ hybridization, RT-PCR [20] [21]. |
| AEA Trophic Effect | Trophoblast outgrowth promoted at 7 nM; retarded at 28 nM [21] | Demonstrates the biphasic, concentration-dependent effect of AEA on embryonic development. | In vitro blastocyst culture assay [21]. |
Table 2: Phenotypic Outcomes in Cannabinoid Receptor Mutant Mice
| Genotype | Embryo Development Phenotype | Implantation / Decidualization Phenotype | Key Molecular Alterations |
|---|---|---|---|
| Cnr1-/- | Retarded development in vivo; Resistant to AEA-induced arrest in vitro [19] [21] | Compromised primary decidual zone (PDZ) formation; retained blood vessels & macrophages [23]. | Dysregulated angiogenic factors (VEGFA, FLK1) in PDZ [23]. |
| Cnr2-/- | Mild developmental aberrations [21] | Less severe decidual defects compared to Cnr1-/- [23]. | Increased uterine edema before implantation [23]. |
| Cnr1-/- Cnr2-/- (Double KO) | Severely retarded development; oviductal retention [19] [21] | Severely compromised PDZ; defective Bmp2/Hoxa10 expression; flat uterine lumen [23]. | Significant retention of F4/80+ macrophages and CD45+ hematopoietic cells near embryo [23]. |
| Wild-type | Normal development to blastocyst | Normal formation of an avascular PDZ; proper embryo-uterine synchrony. | Normal spatiotemporal expression of Ptgs2, Bmp2, and Vegfa [23]. |
Experimental Protocols: Methodologies for Investigating the Uterine Milieu
To enable replication and critical evaluation, this section outlines detailed protocols for key experiments that have elucidated the role of endocannabinoids in mouse embryo implantation.
Assessing Preimplantation Embryo Development In Vitro
Objective: To determine the direct effects of endocannabinoids on the developmental competence of preimplantation embryos.
Materials:
- Research Reagents:
- Cannabinoid Agonists: Anandamide (AEA), 2-Arachidonoylglycerol (2-AG), Δ9-Tetrahydrocannabinol (Δ9-THC), synthetic agonist WIN55212-2.
- Receptor Antagonists: SR141716A (CB1-selective), AM251 (CB1-selective), SR144528 (CB2-selective).
- Culture Media: HEPES-buffered medium for handling; specific culture media like HTF (Human Tubal Fluid) under oil for extended culture [24].
- Embryos: One-cell or two-cell stage mouse zygotes collected from superovulated females.
Methodology:
- Embryo Collection: Sacrifice mated female mice and flush one-cell or two-cell embryos from the oviducts.
- Experimental Groups: Randomize and allocate embryos into control and treatment groups.
- Control: Culture medium with vehicle (e.g., DMSO, ethanol).
- Treatment: Culture medium supplemented with specific concentrations of cannabinoid agonists (e.g., 7 nM, 28 nM AEA) [21].
- Antagonist Co-treatment: Include groups with agonist plus a receptor antagonist (e.g., AEA + SR141716A) to confirm receptor specificity.
- Culture Conditions: Culture embryos in a humidified incubator at 37°C with 5% CO2 for 72-96 hours.
- Outcome Assessment: Monitor and record embryo development every 24 hours. Key endpoints include:
- Rate of development to the morula and blastocyst stages.
- Blastocyst cell number (e.g., by differential staining of ICM and TE).
- Blastocyst zona hatching rate [21].
In Vivo Analysis of Embryo Transport and Uterine Receptivity
Objective: To investigate the role of maternal cannabinoid signaling in transporting embryos from the oviduct to the uterus and preparing the uterus for implantation.
Materials:
- Animal Models: Wild-type and cannabinoid receptor knockout (e.g., Cnr1-/-, Cnr2-/-, Cnr1-/-Cnr2-/-) mice.
- Reagents: Miniosmotic pumps for sustained delivery of (-)THC [19].
- Detection Tools: Specific RNA probes for in situ hybridization (e.g., for Ptgs2, Bmp2, Hoxa10); antibodies for immunohistochemistry (e.g., against FLK1, F4/80, Scribble) [23].
Methodology:
- Mating and Drug Administration: Mate female mice with proven males. Confirm mating by vaginal plug (day 1 of pregnancy). Implant miniosmotic pumps containing vehicle or (-)THC from day 2 to day 5 [19].
- Tissue Collection: Sacrifice mice on specific days of pregnancy (e.g., day 4 for embryo location; day 5-6 for implantation site analysis).
- Embryo Recovery and Localization: Flush embryos from the oviducts and uterus on day 4. The number and location of embryos are recorded. Fewer embryos in the uterus of knockout females indicates oviductal retention [21].
- Analysis of Uterine Receptivity and Decidualization:
- In situ hybridization: Analyze the expression patterns of receptivity (Ptgs2) and decidualization (Bmp2, Hoxa10) markers in uterine sections [23].
- Immunohistochemistry: Stain uterine sections from day 6 of pregnancy to assess PDZ integrity (Scribble), vascularization (FLK1), and immune cell presence (F4/80 for macrophages) [23].
In Vitro Decidualization Assay
Objective: To model stromal cell differentiation in culture and dissect the cell-autonomous role of endocannabinoid signaling in decidualization.
Materials:
- Cell Source: Primary uterine stromal cells isolated from day 4 pregnant wild-type or Cnr1-/- mice.
- Decidualization Cocktail: Culture media containing progesterone (P4) and cyclic adenosine monophosphate (cAMP) to induce decidualization [23].
- Neutralizing Agents: CB1 receptor neutralizing antibody or specific antagonists.
Methodology:
- Stromal Cell Isolation: Dissect uteri from day 4 pregnant mice, enzymatically digest, and isolate the stromal cell fraction.
- Induction of Decidualization: Plate stromal cells and treat with control media or decidualization media (P4 + cAMP) for 5-7 days.
- Experimental Intervention: Include treatment groups with CB1 antagonists or neutralizing antibodies during the decidualization process.
- Assessment of Decidualization:
- Morphological: Observe transformation from fibroblastic to epithelioid morphology.
- Molecular: Quantify mRNA or protein levels of decidual markers (e.g., Bmp2, Hoxa10) via qRT-PCR or western blot.
- Functional: Measure the expression of angiogenic factors (e.g., VEGFA) in the culture supernatant [23].
The workflow for these key methodologies is summarized in the following diagram.
Experimental Workflow for Key Methodologies
The Scientist's Toolkit: Essential Research Reagents
A systematic investigation of endocannabinoids in the uterine milieu relies on a specific toolkit of reagents, animal models, and detection methods. The following table catalogs essential resources for researchers in this field.
Table 3: Research Reagent Solutions for Endocannabinoid Studies
| Reagent / Model Category | Specific Example | Function / Application in Research |
|---|---|---|
| Cannabinoid Receptor Agonists | Anandamide (AEA), 2-Arachidonoylglycerol (2-AG), Δ9-THC, WIN55212-2 | Activate CB1 and/or CB2 receptors to mimic elevated endocannabinoid signaling and test effects on embryo development and uterine function [20] [21]. |
| Cannabinoid Receptor Antagonists | SR141716A (Rimonabant), AM251 (CB1-selective); SR144528 (CB2-selective) | Block specific cannabinoid receptors to elucidate their individual roles and confirm receptor-mediated effects [19] [21]. |
| Genetic Mouse Models | Cnr1-/- (CB1 KO), Cnr2-/- (CB2 KO), Cnr1-/- Cnr2-/- (Double KO) | Provide loss-of-function models to study the physiological roles of cannabinoid receptors in embryo transport, implantation, and decidualization without pharmacological confounding [19] [23] [21]. |
| Key Enzymatic Targets | FAAH inhibitors (e.g., URB597), MAGL inhibitors (e.g., JZL184) | Elevate endogenous levels of AEA or 2-AG, respectively, by blocking their degradation, allowing study of tonic endocannabinoid signaling [20]. |
| Molecular Detection Tools | RNA probes for Ptgs2, Bmp2, Hoxa10; Antibodies for FLK1, F4/80, Scribble | Used in in situ hybridization and immunohistochemistry to visualize spatial and temporal patterns of gene expression and protein localization in uterine tissues [23]. |
| Culture Media & Supplements | HEPES-buffered handling media; HTF (Human Tubal Fluid) culture media; Hormones (Progesterone, Estrogen) | Ensure optimal embryo viability during manipulation and culture, and for preparing the uterus in experimental models [24]. |
| Phenamil methanesulfonate | Phenamil methanesulfonate, CAS:1161-94-0; 2038-35-9, MF:C13H16ClN7O4S, MW:401.83 | Chemical Reagent |
| 1-(azidomethoxy)-2-methoxyethane | 1-(Azidomethoxy)-2-methoxyethane|Research Chemical | 1-(Azidomethoxy)-2-methoxyethane is a valuable azide-containing building block for research applications. This product is for research use only (RUO). |
The evidence from mouse models unequivocally establishes the endocannabinoid system as a central rheostat in the uterine milieu, fine-tuning the critical stages of early pregnancy. The precise spatiotemporal gradients of AEA and 2-AG, achieved through the regulated expression of their synthetic and catabolic enzymes, create a conducive environment for synchronized embryo-uterine dialogue. The concentration-dependent, biphasic effects of ligands like AEA, coupled with the distinct but complementary roles of CB1 and CB2 receptors, highlight the exquisite sensitivity of reproductive processes to this signaling system. Disruption of this balance, as evidenced by studies in knockout mice, leads to a cascade of failures including oviductal embryo retention, defective decidualization, impaired formation of the protective PDZ, and ultimately, pregnancy loss.
Future research must bridge the gap between these detailed mechanistic studies in mice and human reproductive health. While mice have been invaluable models, differences in reproductive physiology and placentation necessitate careful extrapolation [25]. Investigating the role of endocannabinoids in human endometrial stromal cell decidualization and trophectoderm invasion is a critical next step. Furthermore, the interplay between endocannabinoids and other signaling pathways, such as prostaglandins and angiogenic factors, represents a complex regulatory network that is only beginning to be understood. From a translational perspective, components of the endocannabinoid system, such as FAAH in lymphocytes, have been implicated in human miscarriage [19], suggesting potential as diagnostic biomarkers or therapeutic targets for treating infertility. As our understanding deepens, manipulating the endocannabinoid tone may emerge as a novel strategy to improve outcomes in assisted reproductive technologies by optimizing the embryonic environment.
The use of mice as model organisms to study human biology is predicated on the genetic and physiological similarities between the species. Nonetheless, mice and humans have evolved in and become adapted to different environments and, despite their phylogenetic relatedness, have become very different organisms [26]. This is particularly true in the field of reproductive physiology, where the limitations of mouse models are critical for researchers to understand when investigating complex processes such as embryo implantation. Within the context of a broader thesis on factors affecting mouse embryo implantation success rates, this review synthesizes the fundamental genetic, physiological, and anatomical differences that complicate the extrapolation of mouse data to human reproductive biology. It further provides detailed experimental protocols and reagent solutions to guide rigorous research design in this field.
Evolutionary, Anatomical, and Physiological Divergence
Fundamental Evolutionary Differences
Since the lineages leading to modern rodents and primates diverged from a common ancestor approximately 85 million years ago, they have evolved distinct biological strategies [26]. The most fundamental difference is body size: humans are roughly 2,500 times larger than mice. Size is not merely a physical attribute but a major target of natural selection that correlates with a suite of metabolic and life history traits [26].
This size difference drives profound physiological divergence. The specific metabolic rate (metabolic rate per gram of tissue) of a mouse is roughly seven times that of a human [26]. This elevated metabolic rate is correlated with anatomic and biochemical differences, including:
- Higher mitochondrial density and capillary density in mouse tissues.
- Higher rates of reactive oxygen species production and oxidative damage.
- Differences in membrane phospholipid composition, with mouse cells having a higher content of readily oxidizable docosahexaenoic acid [26].
These underlying metabolic disparities can significantly influence cellular processes, including those critical for embryonic development and implantation.
Life History and Reproductive Strategies
Mice and humans exhibit vastly different life history strategies, which are tightly linked to their differences in body size and metabolic rate. These strategies directly impact reproductive physiology and experimental design.
Table 1: Comparison of Key Life History and Reproductive Traits Between Mice and Humans
| Trait | Mouse | Human |
|---|---|---|
| Time to Sexual Maturity | 6-8 weeks [26] | >12 years |
| Gestation Length | 19-20 days [26] | ~40 weeks |
| Litter Size | 5-8 pups [26] | Typically 1 |
| Life Span | 3-4 years (lab strains) [26] | >70 years |
| Energy Investment in Reproduction | High proportion [26] | Lower proportion |
These differences underscore that mice are selected for rapid, high-quantity reproduction, whereas humans invest heavily in a few, highly developed offspring. These divergent evolutionary pressures inevitably shape the molecular and physiological mechanisms governing reproduction.
Anatomical Differences in the Reproductive Tract
Significant anatomical differences exist between the reproductive tracts of mice and humans, which must be considered when studying implantation.
- Uterine Anatomy: The human uterus is a single, pear-shaped organ (simplex), while the mouse uterus is bipartite, consisting of two separate uterine horns (bicornuate). This fundamental structural difference affects the spatial context of implantation.
- Placentation: The type and invasiveness of placentation differ between the species, affecting the nature of the maternal-fetal interface.
- Penile Anatomy: The mouse penis contains a bone (os penis) and a substantial fibrocartilaginous projection (the male urogenital mating protuberance, MUMP), both absent in humans. Mice also have six penile erectile bodies, compared to two in humans [27]. These differences highlight divergent developmental pathways for structures dependent on androgen signaling.
Critical Differences in Embryo Implantation
Molecular Signaling in Implantation
A critical window for embryo implantation exists in both mice and humans, but the key molecular regulators, while sometimes sharing nomenclature, often play distinct roles. The leukemia inhibitory factor (LIF) pathway is a prime example.
In mice, LIF is considered a master regulator of implantation. Uterine LIF expression is induced by a transient surge of nidatory estrogen on day 4 of pregnancy [9] [3]. LIF binds to a heterodimeric receptor complex of LIFR and GP130 on the uterine luminal epithelium, activating the JAK/STAT3 signaling pathway. This activation is absolutely essential for embryo implantation in mice; genetic deletion of Lif, Lifr, Gp130, or Stat3 in the uterine epithelium results in complete implantation failure and infertility [9] [3].
However, the role of LIF in human implantation is less clear-cut and appears to be more modulatory than essential. While LIF is present in the human endometrium, its functional redundancy with other cytokines and its absolute necessity are not fully established. Recent research highlights further complexity within the mouse model itself. While LIFR and GP130 were thought to function solely as a heterodimer, their distinct expression patterns in the uterus suggest potential independent roles. A 2025 study using uterine epithelium-specific Lifr knockout (Lifr eKO) mice confirmed complete infertility but, through comprehensive gene expression analysis, identified ERBB2 (HER2/neu) as a key downstream signaling hub essential for implantation [3]. This reveals a more complex signaling network than previously appreciated.
The following diagram illustrates this essential signaling pathway for mouse embryo implantation:
Experimental Models for Studying Implantation
Researchers have developed several sophisticated mouse models to dissect the mechanics of implantation. Two key protocols are detailed below.
The Delayed Implantation (DI) Model
This model is invaluable for uncoupling embryo viability from uterine receptivity, allowing researchers to study the window of implantation directly [9].
Experimental Workflow: Delayed Implantation Model
Detailed Protocol:
- Timed Mating: House female mice with fertile males and check for vaginal plugs each morning. The day a plug is found is designated as day 1 of pregnancy (D1) [9] [3].
- Ovariectomy (OVX): On D3 (between 1300 and 1530 hours), anesthetize plug-positive females and perform ovariectomy to remove the primary source of endogenous hormones [9].
- Hormonal Maintenance: Immediately following OVX, administer a subcutaneous injection of the synthetic progestin medroxyprogesterone acetate (MPA, 100 µl/head) to maintain the uterus in a neutral, non-receptive state [9].
- Implantation Arrest: With only P4 present, embryos will develop to the blastocyst stage but enter a state of "diapause" or developmental arrest. They can remain viable in the uterus for several days.
- Experimental Trigger: On D7, administer the experimental stimulus to initiate implantation. In a control group, a single injection of estradiol (E2, 25 ng/head) is given to mimic the natural nidatory E2 surge. In the test group, the compound of interest (e.g., RO8191, 400 µg/head, dissolved in sesame oil) is administered via intraperitoneal injection [9].
- Assessment: Sacrifice mice 72 hours post-injection (D10) and count the number of implantation sites, visible as distinct blue bands if a dye like Chicago Blue is injected intravenously prior to sacrifice [3]. Uterine horns can be flushed to recover embryos if no implantation sites are visible.
Conditional Knockout (cKO) Models
To define the cell-specific role of a gene, researchers use uterine epithelium-specific conditional knockout mice.
Detailed Protocol for Validating Gene Function in Implantation:
- Mouse Generation: Cross mice carrying a "floxed" allele of the target gene (e.g., Lifrflox/flox, Stat3flox/flox, Gp130flox/flox) with mice expressing Cre recombinase under the control of a uterine epithelial-specific promoter (e.g., *LtfiCre/+) [9] [3].
- Genotyping: Confirm the genotypes of offspring via PCR using tail clip DNA and specific primers for the Cre transgene and the floxed allele.
- Phenotyping:
- Fertility Test: House adult female cKO mice with proven fertile wild-type males for 4-6 months. Record the number of litters and pups born to assess long-term fertility [3].
- Implantation Site Analysis: Set up timed matings with cKO and control females. On D5 or D6, visualize implantation sites by intravenous injection of 1% Chicago Blue dye. The absence of blue bands indicates implantation failure [3].
- Rescue Experiments: To test if a pathway is sufficient to overcome a genetic defect, administer a candidate compound (e.g., RO8191) to pregnant cKO mice on D4 and assess implantation outcomes as in the DI model [9].
The Scientist's Toolkit: Key Reagents and Models
Table 2: Essential Research Reagents and Models for Mouse Implantation Studies
| Reagent / Model | Function / Purpose | Key Consideration / Limitation |
|---|---|---|
| RO8191 [9] | A small-molecule interferon agonist that acts as a potent STAT3 activator; can induce implantation in delayed implantation models. | Its effect is partial in Stat3 or Gp130 cKO mice, indicating it requires a functional GP130/STAT3 axis. |
| Lifr eKO / Gp130 eKO Mice [3] | Genetically engineered models to study the specific role of LIF signaling in the uterine epithelium. | Reveals distinct and overlapping gene networks downstream of LIFR and GP130, complicating the simple heterodimer model. |
| Delayed Implantation Model [9] | Allows precise temporal control over the implantation process, useful for testing specific agonists/antagonists. | An artificial system that may not fully recapitulate the dynamics of natural conception. |
| Tucatinib / Sapitinib [3] | ERBB2 (HER2) inhibitors; used to pharmacologically validate the role of ERBB2 signaling in implantation. | Demonstrates the critical role of the LIFR-ERBB2 axis beyond the classic JAK-STAT3 pathway. |
| SCADS Inhibitor Kits [10] | Standardized libraries of chemical inhibitors for high-throughput screening of factors involved in early embryonic development. | Identified novel regulators like Cathepsin D and CXCR2, whose roles in human implantation are unknown. |
| JMJD7-IN-1 | JMJD7-IN-1, CAS:311316-96-8, MF:C16H8Cl2N2O4, MW:363.15 | Chemical Reagent |
| DMPQ Dihydrochloride | DMPQ Dihydrochloride, CAS:1123491-15-5; 137206-97-4, MF:C16H16Cl2N2O2, MW:339.22 | Chemical Reagent |
Impact of Assisted Reproduction and Staging on Data Fidelity
Assisted Reproductive Technologies (ART) and Genetic Integrity
The use of in vitro fertilization (IVF) and embryo transfer in mouse models is common. However, a 2025 study indicates that mouse pups conceived via IVF have about 30% more de novo single-nucleotide variants in their DNA compared to naturally conceived pups [28]. While the absolute risk of a harmful mutation remains low, this finding highlights that ART procedures can alter the genetic landscape of the model organism, potentially introducing a confounding variable in studies of embryonic development and implantation.
Embryo Staging and Developmental Asynchrony
A significant technical challenge in mouse embryology is accurate developmental staging. Relying solely on harvesting age (time post-conception) is unreliable due to uncertainties in fertilization timing and developmental asynchrony between embryos, even within the same litter [29]. The eMOSS (embryonic mouse ontogenetic staging system) provides a solution. This tool determines the developmental stage (morphometric age) with a typical uncertainty of only 2 hours, based on a geometric morphometric analysis of the hindlimb bud shape from 2D images [29]. Using precise staging tools is critical for obtaining reproducible data when analyzing molecular events during the peri-implantation period.
Mouse models provide indispensable, experimentally tractable systems for investigating the fundamental mechanisms of embryo implantation. However, their utility is bounded by significant limitations arising from evolutionary divergence in size, life history, anatomy, and the specific molecular wiring of key pathways like LIF signaling. The essential role of the LIF-STAT3 axis in mice is not directly transferable to humans, and recent work revealing complex downstream hubs like ERBB2 further underscores the intricacy of these networks. Researchers must therefore exercise caution when extrapolating findings from mouse to human. The future of implantation research lies in leveraging sophisticated mouse models—such as conditional knockouts and the delayed implantation protocol—with a clear understanding of their inherent limitations, while increasingly seeking validation through human endometrial cell and tissue models to bridge the translational gap.
Advanced Techniques for Culturing and Manipulating Embryo Viability
Within the broader investigation of factors affecting mouse embryo implantation success rates, the optimization of in vitro culture (IVC) conditions stands as a critical frontier. Among various environmental parameters, oxygen tension is a predominant factor influencing embryonic developmental competence. The physiological oxygen concentration within the mammalian female reproductive tract is significantly lower than atmospheric air, ranging between 2% and 8% [30] [31]. While many assisted reproductive technology (ART) laboratories have adopted culture under 5% Oâ‚‚, the potential benefits of a more profound physiological hypoxia (2% Oâ‚‚), particularly during the later stages of preimplantation development, remain a subject of active investigation. This whitepaper synthesizes current research to provide an in-depth technical guide on the impact of 5% versus 2% oxygen tension on embryo development, offering evidence-based insights and methodologies for researchers and scientists in the field.
Physiological Context and Scientific Rationale
The rationale for using low oxygen tensions in embryo culture is rooted in the in vivo environment of the developing embryo. Measurements in the oviducts and uteri of several mammalian species, including mice, consistently report low oxygen levels, creating a physiological hypoxic milieu [31] [32]. For instance, the oxygen tension in the mouse uterus is approximately 1.5% to 2% [32]. This low oxygen environment is believed to minimize oxidative stress by reducing the generation of reactive oxygen species (ROS), which can damage cellular structures like DNA, proteins, and lipids, and impair embryonic development [33] [34].
A pivotal concept in optimizing culture conditions is the "sequential" or "back-to-nature" system, which posits that the oxygen concentration in vitro should mirror the changing environment the embryo experiences in vivo. As the embryo travels from the oviduct (higher Oâ‚‚) to the uterus (lower Oâ‚‚), the oxygen tension decreases [35]. This has led to the hypothesis that a sequential culture system, starting at a higher physiological oxygen level (e.g., 5-6%) until the cleavage or morula stage, followed by culture under ultrahypoxic conditions (e.g., 2%) until the blastocyst stage, may be most beneficial [35]. The supporting theory is that oxidative stress is particularly detrimental before embryonic genome activation, but that later stages may benefit from the ultralow oxygen levels of the uterus, potentially enhancing traits like invasive ability crucial for implantation [30] [31].
Comparative Analysis of 5% vs. 2% Oxygen Tension
Key Developmental Outcomes
Recent studies provide direct comparisons between 5% and 2% Oâ‚‚, yielding critical insights for protocol optimization.
A 2024 mouse study offers a head-to-head comparison. Embryos cultured under 5% Oâ‚‚ demonstrated a significantly higher mean percentage of blastocyst formation and greater total cell number compared to those cultured under 2% Oâ‚‚. Furthermore, blastocyst expansion was greatest in the 5% Oâ‚‚ group. Molecular analysis revealed that embryos in the 2% Oâ‚‚ group had a significant upregulation of stress-response genes and lower expression of antioxidant-related genes compared to both the 5% Oâ‚‚ and in vivo-derived control groups. This suggests that 2% Oâ‚‚ may induce a suboptimal stress response, thereby compromising developmental competence [36].
A 2025 bovine model study, relevant due to the similarity of bovine embryogenesis to human, investigated a sequential system. This research cultured embryos in constant 6% Oâ‚‚, constant 20% Oâ‚‚, or a sequential regimen of 6% Oâ‚‚ until the 16-cell stage, followed by 2% Oâ‚‚. The results were striking: the highest blastocyst formation rate (36%) was achieved under constant 6% Oâ‚‚, while the sequential 2% Oâ‚‚ condition yielded a very low blastocyst rate of only 4.6%. This indicates that while a degree of hypoxia is beneficial, ultrahypoxia (2%) at the blastocyst stage can be severely detrimental to development rates in vitro. Transcriptomic profiles showed that both hypoxic and ultrahypoxic conditions promoted a metabolic profile (upregulation of glycolysis and lipid metabolism genes) more akin to in vivo embryos, whereas normoxic conditions failed to do so. However, this metabolic normalization under 2% Oâ‚‚ did not translate into survival for the vast majority of embryos [35].
Table 1: Comparative Developmental Outcomes of Mouse Embryos Cultured under 5% vs. 2% Oâ‚‚
| Developmental Parameter | 5% Oâ‚‚ Tension | 2% Oâ‚‚ Tension | In Vivo Derived (Control) | Citation |
|---|---|---|---|---|
| Blastocyst Formation Rate | Significantly higher | Significantly lower | Benchmark (Highest) | [36] |
| Total Cell Number | Significantly higher | Significantly lower | Benchmark (Highest) | [36] |
| Blastocyst Expansion | Greatest | Reduced | Not specified | [36] |
| Stress Response Gene Expression | Lower | Significantly upregulated | Benchmark (Lower) | [36] |
| Antioxidant Gene Expression | Higher | Significantly lower | Benchmark (Highest) | [36] |
Molecular and Functional Consequences
Beyond developmental rates, oxygen tension profoundly influences molecular pathways and functional competence.
Research indicates that low oxygen tension (5%) promotes the invasive ability of blastocysts, a critical function for successful implantation. A mouse study demonstrated that blastocysts cultured under 5% Oâ‚‚ had a significantly higher implantation rate compared to those cultured under 20% Oâ‚‚. This was linked to the upregulation of key proteolytic enzymes, Mmp-9 and uPA, which are essential for trophoblast invasion into the endometrial lining [31].
At the ultrastructural level, culture under 20% Oâ‚‚ is associated with significant abnormalities in preimplantation mouse embryos, including an increase in vacuolated mitochondria, cytoplasmic vacuolization, and altered chromatin structure [32]. While a direct ultrastructural comparison between 5% and 2% Oâ‚‚ is less common, the severe developmental compromise and stress observed at 2% Oâ‚‚ in other studies suggest it may not rescue these morphological defects [36].
Table 2: Molecular and Functional Consequences of Different Oxygen Tensions
| Parameter | Atmospheric (20%) Oâ‚‚ | Physiological (5%) Oâ‚‚ | Ultrahypoxic (2%) Oâ‚‚ | Citation |
|---|---|---|---|---|
| Invasive Competence | Lower implantation rate, reduced Mmp-9/uPA | Higher implantation rate, upregulated Mmp-9/uPA | Not thoroughly investigated | [31] |
| Cellular Ultrastructure | Vacuolated mitochondria, high cytoplasmic vacuolization | Improved over 20%, but abnormal vs. in vivo | Not thoroughly investigated | [32] |
| Energy Metabolism | Relies on oxidative phosphorylation; fails to upregulate glycolysis | Upregulates glycolysis and lipid metabolism (in vivo-like) | Upregulates glycolysis and lipid metabolism (in vivo-like) | [35] |
| Apoptosis | Increased apoptotic cells in blastocysts | Reduced apoptotic cells | Higher Caspase-3 activity vs. 5% Oâ‚‚ and in vivo | [36] [34] |
Experimental Protocols for Oxygen Tension Research
Protocol: Comparative Culture of Mouse Embryos under 5% vs. 2% Oâ‚‚
This protocol is adapted from a 2024 study comparing the developmental competence of in vitro-produced mouse embryos [36].
1. Experimental Groups:
- Group 1 (5% Oâ‚‚): Culture in a multi-gas incubator with a humidified atmosphere of 5% Oâ‚‚, 6% COâ‚‚, and balance Nâ‚‚.
- Group 2 (2% Oâ‚‚): Culture in a multi-gas incubator with a humidified atmosphere of 2% Oâ‚‚, 6% COâ‚‚, and balance Nâ‚‚.
- Control Group (In vivo): Embryos flushed from the uteri of mated females to serve as a developmental benchmark.
2. Materials:
- Animals: CD-1 or similar strain of reproductively competent mice.
- Culture Medium: Potassium Simplex Optimized Medium (KSOM) supplemented with amino acids.
- Incubators: Two tri-gas incubators capable of precisely maintaining 5% or 2% O₂ tension, respectively, with 6% CO₂ and at 37°C.
- Mineral Oil: Pre-equilibrated with the respective culture media and gas atmospheres.
3. Methodology:
- Embryo Collection: Superovulate female mice and mate with fertile males. Collect zygotes from the oviducts approximately 20-24 hours post-hCG injection.
- Randomization and Culture: Pool and randomly allocate zygotes to the two experimental groups. Culture embryos in groups (e.g., 10-15 embryos per 50μL drop of KSOM under oil) in their respective pre-equilibrated incubators.
- Developmental Assessment: Monitor and record cleavage rates at 24-48 hours. Assess blastocyst formation rates, blastocyst expansion grades, and total cell counts at 96-120 hours post-insemination. Total cell counts can be performed using a standard nuclear stain like Hoechst 33342.
- Molecular Analysis (Optional): For a subset of blastocysts, perform quantitative PCR (qPCR) for a panel of stress-related genes (e.g., Hif1α, Caspase-3) and antioxidant genes. Alternatively, perform immunofluorescence for Caspase-3 to quantify apoptosis levels.
The following workflow diagram summarizes this experimental protocol:
Protocol: Sequential Culture System in a Bovine Model
This protocol is based on a 2025 study that investigated transcriptomic changes under different Oâ‚‚ tensions, using bovine embryos as a model for human development [35].
1. Experimental Groups:
- Normoxia (20% Oâ‚‚): Constant culture in a humidified atmosphere of 20% Oâ‚‚ and 5% COâ‚‚.
- Hypoxia (6% Oâ‚‚): Constant culture in a humidified atmosphere of 6% Oâ‚‚, 5% COâ‚‚, and balance Nâ‚‚.
- Sequential Ultrahypoxia (6%→2% O₂): Culture in 6% O₂ until the 16-cell stage (approximately 96 hours post-fertilization), then transfer to an incubator with 2% O₂, 5% CO₂, and balance N₂ until blastocyst stage (Day 8).
2. Materials:
- Biological Material: Bovine cumulus-oocyte complexes (COCs) from slaughterhouse ovaries.
- Media: Standard in vitro production suite: In Vitro Maturation (IVM) medium, Fertilization (IVF) medium (e.g., Fert-TALP), and Culture (IVC) medium (e.g., modified Synthetic Oviduct Fluid - SOF).
- Incubators: One standard COâ‚‚ incubator (for 20% Oâ‚‚) and two multi-gas incubators (for 6% and 2% Oâ‚‚).
3. Methodology:
- IVM & IVF: Mature COCs for 22-24 hours. Perform IVF using frozen-thawed, capacitated sperm for 19-20 hours.
- In Vitro Culture (IVC): Denude presumptive zygotes and wash thoroughly. Randomly allocate to the three culture condition groups in SOF medium.
- Embryo Collection and Analysis: Collect a subset of embryos at key stages (zygote, 4-cell, 8-cell, 16-cell, blastocyst) for transcriptomic analysis (e.g., RNA-sequencing). For control dishes, calculate cleavage rates (Day 2) and final blastocyst formation rates (Day 8).
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Oxygen Tension Studies
| Item | Specific Example | Function in Experiment | Citation |
|---|---|---|---|
| Tri-Gas Incubator | Binder, CB series; or equivalent | Precisely maintains low Oâ‚‚ (2%, 5%), COâ‚‚ (5-6%), and Nâ‚‚ balance for physiological culture. | [33] [35] |
| Basal Culture Medium | Potassium Simplex Optimized Medium (KSOM); Synthetic Oviduct Fluid (SOF) | Provides nutritional base and osmotic support for embryo development in vitro. | [36] [35] [34] |
| Serum Supplement | Fetal Calf Serum (FCS); Bovine Serum Albumin (BSA) | Provides proteins, growth factors, and lipids; acts as a surfactant in medium. | [33] [35] |
| Antioxidants | Melatonin (10â»âµ M); Ascorbic Acid (50 µM) | Added to maturation or culture medium to mitigate oxidative stress, especially in high Oâ‚‚. | [33] |
| Hormones for Superovulation | Pregnant Mare's Serum Gonadotropin (PMSG); Human Chorionic Gonadotropin (hCG) | Stimulate follicular growth and trigger oocyte maturation in donor female mice. | [34] [32] |
| RNA-Sequencing Kits | STRT-N seq kit; Smart-seq2 kit | For transcriptomic profiling of single embryos to analyze gene expression changes. | [35] |
| TAK-960 hydrochloride | TAK-960 hydrochloride, CAS:2108449-45-0, MF:C27H35ClF3N7O3, MW:598.07 | Chemical Reagent | Bench Chemicals |
| 6-(Trifluoromethoxy)chroman-4-one | 6-(Trifluoromethoxy)chroman-4-one, CAS:874774-49-9, MF:C10H7F3O3, MW:232.158 | Chemical Reagent | Bench Chemicals |
The collective evidence indicates that a one-size-fits-all approach to oxygen tension is not optimal for in vitro embryo culture. For researchers focusing on mouse embryo implantation success rates, the balance of evidence currently favors 5% Oâ‚‚ as the more robust and effective concentration for extended culture, compared to 2% Oâ‚‚. While 2% Oâ‚‚ may more closely mimic the uterine environment, it appears to impose a suboptimal stress that compromises preimplantation development [36]. However, the concept of sequential culture remains valid, with the critical caveat that the later-stage oxygen concentration should not fall to ultrahypoxic (2%) levels, as this drastically reduces blastocyst yield [35].
Future research should prioritize several key areas:
- Patient-Specific Factors: Investigate how maternal pathologies, such as hyperglycemia, alter embryonic susceptibility to oxygen-induced stress, potentially necessitating individualized culture protocols [34].
- Mechanistic Insights: Further elucidate the precise molecular pathways, particularly those related to energy metabolism and epigenetic regulation, that are differentially affected by 5% versus 2% Oâ‚‚.
- Long-Term Outcomes: Extend studies beyond blastocyst formation to assess fetal development rates, placental function, and the long-term health of offspring derived from embryos cultured under these refined conditions.
In conclusion, while 5% Oâ‚‚ is established as superior to atmospheric oxygen, the pursuit of the optimal culture system continues. Researchers are encouraged to validate these findings within their specific experimental models, as the quest to fully recapitulate the in vivo environment remains a central challenge in reproductive biology and ART.
Embryo implantation is a critical determinant of reproductive success, with STAT3 signaling playing a central role in establishing uterine receptivity. This technical guide examines RO8191, a novel small-molecule interferon-α receptor 2 agonist that directly activates STAT3 signaling, as a potential therapeutic intervention for rescuing implantation failure. Through evaluation of multiple genetically engineered mouse models, we demonstrate that RO8191 effectively induces embryo implantation and decidualization even in contexts of specific molecular deficiencies. Our findings position RO8191 as a promising pharmacological tool for investigating implantation mechanisms and developing treatments for recurrent implantation failure, particularly in cases where traditional cytokine signaling pathways are compromised.
Embryo implantation represents the pivotal bottleneck in mammalian pregnancy, with implantation failure constituting a major challenge in infertility treatment. In both humans and mice, successful implantation requires precise synchronization between a receptive endometrium and a developmentally competent blastocyst [9]. The signal transducer and activator of transcription 3 (STAT3) pathway has emerged as a master regulator of uterine receptivity, acting as a crucial node in the molecular network that controls embryo attachment and stromal decidualization [37] [38].
In mice, the implantation window is regulated by ovarian hormones progesterone and a transient estrogen surge on day 4 of pregnancy (D1 = vaginal plug). This estrogen surge stimulates the expression of leukemia inhibitory factor (LIF) in uterine glandular epithelium, which subsequently activates the JAK/STAT3 pathway in luminal epithelium [9] [3]. The critical nature of this pathway is evidenced by the complete infertility observed in mice with uterine-specific deletions of Lif, Lifr, Gp130, or Stat3, all of which exhibit identical phenotypes of implantation failure despite normal blastocyst development [9] [38] [3].
While the essential role of STAT3 activation in implantation is well-established, a fundamental question remains whether pharmacological activation of STAT3 alone is sufficient to induce the complex process of embryo implantation. This whitepaper examines RO8191 as a tool to address this question and explores its potential therapeutic applications for overcoming implantation failure.
RO8191: Mechanism of Action and Signaling Pathways
RO8191 is a recently characterized small molecule initially identified as an interferon-α receptor 2 agonist [9]. Subsequent investigations have revealed its potent ability to activate STAT3 signaling through a mechanism that appears distinct from classical cytokine signaling pathways. Unlike LIF, which requires the formation of a LIFR-GP130 receptor heterodimer to initiate JAK/STAT3 activation, RO8191 directly engages intracellular signaling components to achieve STAT3 phosphorylation and nuclear translocation [9] [39].
The molecular actions of RO8191 exhibit notable specificity within the STAT signaling family. Experimental evidence indicates that RO8191 preferentially activates STAT3 but not STAT1, highlighting its selective mechanism of action [39]. This specificity is particularly valuable for delineating the unique contributions of STAT3 to implantation processes, as it minimizes confounding effects from parallel signaling pathways.
Table 1: Key Characteristics of RO8191
| Property | Description | Experimental Evidence |
|---|---|---|
| Chemical Class | Small molecule interferon-α receptor 2 agonist | [9] |
| Primary Action | Selective STAT3 activation | [9] [39] |
| Specificity | Activates STAT3 but not STAT1 | [39] |
| Administration | Intraperitoneal injection (400 µg/head in mice) | [9] |
| Solubility | Dissolved in sesame oil | [9] |
| Therapeutic Potential | Rescues implantation in Lifr cKO mice | [9] [39] |
The signaling pathways involved in RO8191 action and their interplay with conventional implantation signaling are illustrated below:
Figure 1: RO8191 Activation of STAT3 Signaling Pathway. RO8191 acts through both interferon-α receptor 2 (IFNAR2) and direct STAT3 activation mechanisms (dashed lines) to bypass traditional LIF signaling requirements.
Experimental Models and Methodologies
Delayed Implantation Model
The delayed implantation (DI) model provides a valuable experimental system for investigating molecular mechanisms underlying embryo implantation [9]. This model achieves precise temporal control over implantation through surgical and pharmacological interventions:
- Surgical Procedure: ICR or C57BL/6J plug-positive females are ovariectomized between 1300 and 1530 h on D3 under sevoflurane anesthesia [9].
- Hormonal Maintenance: Siliconized medroxyprogesterone acetate (MPA, 100 µl/head) is injected subcutaneously to maintain delayed implantation [9].
- RO8191 Activation: A single intraperitoneal injection of RO8191 (400 µg/head dissolved in sesame oil) is administered at 1300 h on D7 to activate implantation [9].
- Assessment: Implantation sites are evaluated at 1300 h on D10 by counting visible sites or flushing uterine horns to recover embryos if no implantation sites are visible [9].
This model demonstrates that RO8191 can effectively induce embryo implantation and decidual reaction by activating STAT3 signaling in both epithelial and stromal compartments, mimicking the natural implantation process [9] [39].
Conditional Knockout Models
The therapeutic potential of RO8191 was rigorously evaluated using uterine epithelium-specific conditional knockout (cKO) mice:
- Lifr cKO Mice: Generated by crossing Lifr-floxed mice with LtfiCre/+ mice to delete LIF receptor specifically in uterine epithelium [9] [3].
- Stat3 cKO Mice: Created using Stat3-floxed mice crossed with LtfiCre/+ mice to eliminate STAT3 in uterine epithelium [9] [38].
- Gp130 cKO Mice: Produced by crossing Gp130-floxed mice with LtfiCre/+ mice to delete the GP130 co-receptor in uterine epithelium [9].
These cKO models exhibit complete infertility due to implantation failure despite normal blastocyst development, providing stringent systems for testing RO8191's efficacy [9] [38] [3]. RO8191 administration (400 µg/head via intraperitoneal injection) occurs between 1330 and 1700 h on D4 of pregnancy [9].
Quantitative Findings and Efficacy Assessment
RO8191 Efficacy in Rescue Experiments
Table 2: RO8191 Efficacy in Different Mouse Models of Implantation Failure
| Mouse Model | Baseline Phenotype | RO8191 Treatment Outcome | Molecular Mechanism |
|---|---|---|---|
| Delayed Implantation | No implantation without activation | Induces implantation and decidualization [9] | Activates STAT3 in epithelium and stroma [9] [39] |
| Lifr cKO | Infertile (no implantation) [9] [3] | Rescues implantation and establishes pregnancy [9] [39] | Bypasses LIFR requirement via direct STAT3 activation [9] |
| Stat3 cKO | Infertile (no implantation) [9] [38] | Partial decidual response only [9] [39] | Requires STAT3 for full effect [9] |
| Gp130 cKO | Infertile (no implantation) [9] | Partial decidual response only [9] [39] | Independent of GP130 but limited by STAT3 absence [9] |
The differential responses to RO8191 across these models provide critical insights into its mechanism of action. The complete rescue observed in Lifr cKO mice demonstrates RO8191's ability to bypass LIFR deficiency entirely, indicating its action downstream of the receptor complex or through alternative activation pathways [9] [39]. In contrast, the partial response in Stat3 cKO mice confirms that RO8191's primary mechanism depends ultimately on STAT3 availability and activation [9].
Temporal Dynamics of STAT3 Activation
The timing and localization of STAT3 activation following RO8191 administration were characterized through detailed immunohistochemical analyses:
- Early Activation (6 hours post-treatment): Robust nuclear phospho-STAT3 detection in both epithelial and stromal compartments [9].
- Sustained Signaling (24 hours post-treatment): Continued STAT3 phosphorylation confirmed by Western blot analysis [9].
- Spatial Pattern: Activation observed in both luminal and glandular epithelium, mimicking the natural STAT3 activation pattern during the implantation window [9] [38].
This spatiotemporal activation profile correlates with the induction of downstream implantation markers and decidualization factors, supporting RO8191's ability to recapitulate the natural implantation signaling cascade [9].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for RO8191 and Implantation Studies
| Reagent / Model | Source / Reference | Primary Research Application |
|---|---|---|
| RO8191 Compound | TargetMol (T22142) or Sigma-Aldrich (SML1200) [9] | Direct STAT3 activation in implantation studies |
| LtfiCre/+ Mice | JAX: 026030 [9] [3] | Uterine epithelial-specific gene deletion |
| Stat3-floxed Mice | Stat3tm2Aki [9] [38] | Generation of epithelial-specific Stat3 cKO |
| Lifr-floxed Mice | EMMA: EM:06941 [9] [3] | Generation of epithelial-specific Lifr cKO |
| Gp130-floxed Mice | Il6sttm1Wme [9] | Generation of epithelial-specific Gp130 cKO |
| Delayed Implantation Model | [9] | Synchronized implantation induction model |
| Recombinant LIF | Santa Cruz [37] | Positive control for implantation induction |
| Chicago Blue Dye | Sigma-Aldrich (C8679) [3] | Visualization of implantation sites |
| 4-Ethenyloxane-4-carboxylic acid | 4-Ethenyloxane-4-carboxylic Acid|C8H12O3|RUO | 4-Ethenyloxane-4-carboxylic acid (CAS 2305255-31-4) is a high-purity building block for research. This product is For Research Use Only. Not for human or veterinary use. |
| 2-(quinoxalin-2-yloxy)acetic acid | 2-(Quinoxalin-2-yloxy)acetic Acid |
Discussion and Research Implications
The characterization of RO8191 as a pharmacological activator of STAT3 signaling represents a significant advancement in reproductive biology, with both basic research and potential clinical applications. The compound's ability to rescue implantation in Lifr cKO mice demonstrates that bypassing specific receptor deficiencies via direct STAT3 activation represents a viable therapeutic strategy for certain forms of implantation failure [9] [39].
From a mechanistic perspective, the differential effects of RO8191 across various cKO models reveal intriguing aspects of implantation signaling. The complete rescue in Lifr cKO models versus partial responses in Stat3 and Gp130 cKO models suggests that while RO8191 can circumvent LIFR requirements, it ultimately depends on STAT3 as a final common pathway [9] [39]. This observation aligns with previous findings that both epithelial and stromal STAT3 are independently essential for implantation, with epithelial STAT3 controlling luminal architecture and stromal STAT3 regulating estrogen responsiveness [38].
The experimental workflows and signaling pathways delineated in this guide provide researchers with comprehensive frameworks for investigating STAT3-centric implantation mechanisms. The combination of delayed implantation models with tissue-specific knockout systems offers a powerful approach for dissecting complex uterine signaling pathways and evaluating potential therapeutic interventions [9] [38].
While the translational potential of RO8191 for human recurrent implantation failure requires substantial additional investigation, the robust effects observed in multiple mouse models suggest that pharmacological activation of STAT3 represents a promising avenue for future therapeutic development. Further research should focus on optimizing administration protocols, identifying potential off-target effects, and elucidating the complete molecular network through which RO8191 coordinates the implantation process.
In the field of reproductive biology and assisted reproductive technologies (ART), the successful development of preimplantation embryos remains a significant challenge. Somatic cell nuclear transfer (SCNT), a pivotal technique in animal cloning and regenerative medicine, frequently produces embryos with reduced developmental potential compared to those from natural reproduction. A primary factor contributing to this limitation is compromised cytoskeletal integrity, leading to aberrant actin filaments, tubulin disorganization, and chromosomal instability in cloned embryos. These cytoskeletal defects manifest as blastomere fragmentation, abnormal spindle formation, and increased DNA damage, ultimately impairing embryonic development and live birth rates.
Kinase inhibitors have emerged as powerful chemical tools to intervene in these cellular processes. This technical guide focuses on JNJ-7706621, a specific inhibitor of cyclin-dependent kinase 1 (CDK1) and aurora kinases, which has demonstrated remarkable efficacy in enhancing cytoskeletal organization and developmental outcomes in mouse SCNT embryos. By targeting key regulators of the cell cycle and chromosomal segregation, JNJ-7706621 represents a promising chemical intervention within the broader context of improving embryo implantation success rates.
Scientific Rationale and Mechanism of Action
The Cytoskeletal Challenge in SCNT Embryos
Somatic cell nuclear transfer embryos consistently exhibit deficiencies in microtubule organization and actin filament polymerization, crucial components for proper chromosome segregation and cell division. These cytoskeletal abnormalities frequently result in mitotic errors during early embryonic development, contributing to the notoriously low success rates of cloning procedures. The cytoskeleton not only provides structural support but also facilitates intracellular transport, cell signaling, and the mechanical processes of division—all essential for the precise series of cleavages that transform a zygote into a blastocyst.
Molecular Targets of JNJ-7706621
JNJ-7706621 is a dual-specificity kinase inhibitor that primarily targets:
- CDK1: A central regulator of cell cycle progression, particularly the G2/M transition and mitotic entry. CDK1/cyclin B complexes phosphorylate numerous substrates that control nuclear envelope breakdown, chromatin condensation, and spindle assembly.
- Aurora Kinases: Key regulators of mitotic events, including centrosome maturation, bipolar spindle formation, chromosome segregation, and cytokinesis.
By selectively inhibiting these kinases, JNJ-7706621 modulates the phosphorylation status of critical substrates involved in cytoskeletal dynamics, promoting proper assembly and organization of microtubule networks and actin filaments during the delicate early stages of embryonic development.
Table 1: Key Kinase Targets of JNJ-7706621 and Their Functions in Early Embryos
| Kinase Target | Primary Function | Effect of Inhibition |
|---|---|---|
| CDK1 | Regulates G2/M transition; phosphorylates proteins involved in nuclear envelope breakdown and spindle assembly | Prevents premature mitotic entry; allows for proper cytoskeletal reorganization |
| Aurora A | Promotes centrosome maturation and separation; regulates bipolar spindle formation | Ensures proper centrosome function and mitotic spindle geometry |
| Aurora B | Chromosome bi-orientation and attachment to spindle microtubules; regulates cytokinesis | Prevents chromosomal missegregation and aneuploidy |
Signaling Pathway Integration
The efficacy of JNJ-7706621 must be understood within the complex signaling network that governs preimplantation development. While directly targeting cytoskeletal regulators, its effects intersect with critical developmental pathways, including:
- Hippo signaling: regulates trophectoderm specification and blastocyst formation
- Wnt/β-catenin: influences cell fate determination and embryonic patterning
- FGF signaling: crucial for inner cell mass proliferation and lineage specification
The cross-talk between these pathways and the cytoskeletal machinery underscores the importance of temporal and spatial precision in chemical interventions during embryonic development.
Diagram 1: JNJ-7706621 mechanism of action. The inhibitor targets CDK1 and Aurora kinases, leading to improved cytoskeletal integrity and developmental outcomes.
Quantitative Efficacy Data
The therapeutic potential of JNJ-7706621 in embryo biotechnology is substantiated by robust quantitative data demonstrating significant improvements across multiple developmental parameters compared to conventional treatments.
Preimplantation Development Metrics
In controlled studies using mouse SCNT embryos, treatment with 10 μM JNJ-7706621 as a post-activation intervention yielded remarkable enhancements in developmental competence. The blastocyst formation rate increased from 39.9% ± 6.4 in cytochalasin B (CB)-treated controls to 61.4% ± 4.4 in JNJ-treated embryos, representing a 53.9% relative improvement [40].
Beyond the mere progression to blastocyst stage, JNJ-7706621 treatment significantly enhanced embryo quality, as evidenced by:
- Increased total cell number (70.7 ± 2.9 vs. 52.7 ± 3.6 in controls)
- Expansion of the inner cell mass (15.4 ± 1.1 vs. 10.4 ± 0.7 in controls)
- Enhancement of trophectoderm cells (55.3 ± 2.5 vs. 42.3 ± 3.3 in controls)
These quantitative improvements in cellular composition are critically important, as they directly correlate with the embryo's potential to successfully implant and develop to term.
Terminal Development Outcomes
The most compelling evidence for JNJ-7706621's efficacy comes from its dramatic enhancement of post-implantation developmental outcomes:
Table 2: Comparative Efficacy of JNJ-7706621 vs. Cytochalasin B in Mouse SCNT Embryos
| Developmental Parameter | CB Control | JNJ-7706621 Treatment | Relative Improvement |
|---|---|---|---|
| Blastocyst Formation Rate | 39.9% ± 6.4 | 61.4% ± 4.4 | 53.9% |
| Total Cell Number | 52.7 ± 3.6 | 70.7 ± 2.9 | 34.2% |
| Inner Cell Mass Cells | 10.4 ± 0.7 | 15.4 ± 1.1 | 48.1% |
| Trophectoderm Cells | 42.3 ± 3.3 | 55.3 ± 2.5 | 30.7% |
| Implantation Rate | 50.8% ± 3.7 | 68.3% ± 4.3 | 34.4% |
| Live Birth Rate | 2.4% ± 2.4 | 10.9% ± 2.8 | 354.2% |
The substantial improvement in live birth rate (from 2.4% to 10.9%) is particularly noteworthy, as this parameter represents the ultimate measure of success in reproductive technologies and has proven notoriously difficult to enhance in SCNT applications [40].
Detailed Experimental Protocol
Reagent Preparation
JNJ-7706621 Stock Solution:
- Obtain JNJ-7706621 (commercially available from suppliers such as TargetMol or Sigma-Aldrich)
- Prepare a 10 mM stock solution in dimethyl sulfoxide (DMSO)
- Aliquot and store at -20°C protected from light
- Avoid repeated freeze-thaw cycles to maintain compound stability
Working Solution Preparation:
- Thaw stock solution at room temperature
- Dilute in pre-equilibrated embryo culture medium to achieve final concentration of 10 μM
- Ensure final DMSO concentration does not exceed 0.1% (v/v)
- Prepare fresh working solutions for each experiment
Embryo Treatment Protocol
Optimal Treatment Window:
- Initiate treatment immediately after oocyte activation and nuclear transfer
- Continue exposure for the duration specified in the experimental design (typically 2-6 hours post-activation)
Culture Conditions:
- Maintain embryos in microdrop cultures under mineral oil
- Use standard embryo culture conditions (37°C, 5% CO₂, 95% humidity)
- Employ appropriate control groups:
- Negative control: Culture medium with vehicle only (0.1% DMSO)
- Positive control: Conventional treatment (5 μg/mL cytochalasin B)
Concentration Optimization:
- Titrate JNJ-7706621 concentration (1-50 μM) to establish dose-response relationship
- 10 μM consistently demonstrates optimal efficacy with minimal toxicity
- Higher concentrations (50 μM) may exhibit inhibitory effects on development
Assessment Methodologies
Cytoskeletal Integrity Evaluation:
- Fix embryos at desired developmental stages (typically one-cell and two-cell stages)
- Permeabilize with 0.5% Triton X-100 in PBS
- Stain with:
- Phalloidin conjugates for F-actin visualization
- Anti-α-tubulin antibodies for microtubule network
- DAPI or Hoechst for chromatin configuration
- Image using confocal or structured illumination microscopy
- Quantify fluorescence intensity and distribution using image analysis software
Developmental Competence Assessment:
- Culture treated embryos in sequential media systems for 5 days
- Record cleavage rates at 24 hours (two-cell stage)
- Assess morula formation at 72 hours
- Evaluate blastocyst development at 96-120 hours
- Perform differential staining for inner cell mass and trophectoderm quantification
Apoptosis Assessment:
- Apply TUNEL assay at blastocyst stage to quantify apoptotic cells
- Counterstain with propidium iodide for total cell counting
- Calculate apoptotic index (TUNEL-positive cells/total cells × 100)
Integrated Signaling Pathways in Preimplantation Development
The efficacy of cytoskeletal-targeting interventions must be contextualized within the complex signaling network governing early embryonic development. Several critical pathways interact with cytoskeletal elements to coordinate the precise sequence of events from zygote to blastocyst.
Hippo Signaling and Cytoskeletal Regulation
The Hippo signaling pathway plays a pivotal role in lineage specification, particularly in trophectoderm formation. Crucially, this pathway is mechanically coupled to the cytoskeleton through cell-cell contact and polarity complexes. During compaction at the 8-cell stage, establishment of apical-basal polarity influences the spatial distribution of Hippo pathway components, ultimately determining YAP/TAZ localization and transcriptional activity [41].
The interplay between cytoskeletal organization and Hippo signaling creates a feedback loop wherein proper actin polymerization reinforces developmental patterning, while disrupted cytoskeletal integrity can aberrantly activate or suppress this critical pathway.
Wnt Signaling Implications
Wnt/β-catenin signaling represents another developmental pathway with implications for cytoskeletal function and implantation competence. Recent evidence indicates that persistent Wnt signaling during the peri-implantation stage can adversely affect implantation rates and gene expression patterns in the epiblast [42]. While not directly targeted by JNJ-7706621, the coordination between Wnt-mediated transcription and cytoskeletal dynamics underscores the interconnected nature of developmental signaling.
Diagram 2: Signaling pathway integration. Cytoskeletal elements interact with major developmental pathways to influence embryonic outcomes.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Cytoskeletal Intervention Studies
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Kinase Inhibitors | JNJ-7706621 | Dual CDK1/Aurora kinase inhibition; enhances microtubule and actin organization | Optimal at 10 μM; superior to cytochalasin B for SCNT embryos |
| Cytoskeletal Stains | Phalloidin conjugates, Anti-α-tubulin antibodies | Visualize F-actin and microtubule structures | Use with confocal microscopy for high-resolution imaging |
| Cell Fate Markers | Anti-CDX2 (TE), Anti-NANOG (ICM) | Lineage specification assessment | Combine with differential staining for quantitative analysis |
| Apoptosis Assays | TUNEL kit, Caspase substrates | Quantify programmed cell death | Perform at blastocyst stage; normalize to total cell count |
| Small Molecule Modulators | TRULI (Hippo inhibitor), IWP2 (Wnt inhibitor) | Pathway-specific manipulation | Context-dependent effects on lineage specification |
| Cytokine Agonists | RO8191 (STAT3 activator) | Implantation induction | Activates JAK/STAT3 signaling; useful for implantation studies |
| GSK-J4 hydrochloride | GSK-J4 hydrochloride, CAS:1373423-53-0; 1797983-09-5, MF:C24H28ClN5O2, MW:453.97 | Chemical Reagent | Bench Chemicals |
| Mps1-IN-1 dihydrochloride | Mps1-IN-1 dihydrochloride, CAS:1883548-93-3, MF:C28H35Cl2N5O4S, MW:608.58 | Chemical Reagent | Bench Chemicals |
The strategic application of kinase inhibitors like JNJ-7706621 represents a sophisticated chemical intervention to address the fundamental challenge of cytoskeletal integrity in manipulated embryos. By specifically targeting CDK1 and Aurora kinases, this compound stabilizes microtubule networks and actin filaments, thereby reducing chromosomal missegregation, blastomere fragmentation, and DNA damage in SCNT-derived embryos.
The quantitative evidence demonstrates that JNJ-7706621 treatment significantly enhances both preimplantation development metrics and terminal reproductive outcomes, including a remarkable 4.5-fold increase in live birth rates compared to conventional cytochalasin B treatment. This efficacy stems not only from direct cytoskeletal stabilization but also from beneficial interactions with key developmental signaling pathways, including Hippo and Wnt.
For researchers pursuing factors affecting mouse embryo implantation success rates, JNJ-7706621 provides both a practical tool for improving SCNT efficiency and a mechanistic probe for investigating the fundamental relationship between cytoskeletal dynamics and developmental competence. Its incorporation into standardized protocols offers substantial promise for advancing reproductive technologies and elucidating the intricate processes governing the earliest stages of mammalian development.
Embryo implantation failure remains a significant challenge in assisted reproductive technologies (ART). This whitepaper explores a novel combined treatment of Prolactin (PRL), Epidermal Growth Factor (EGF), and 4-Hydroxyestradiol (4-OH-E2)—termed the PEC protocol—to enhance the implantation potential of IVF-derived blastocysts. Research in mouse models demonstrates that this combination synergistically upregulates key protein expression in the trophectoderm, significantly improving implantation rates compared to controls or individual factor applications. The PEC protocol represents a promising strategy to overcome recurrent implantation failure by targeting multiple physiological pathways essential for embryo-uterine crosstalk.
Despite the transfer of high-quality blastocysts, the implantation rate following in vitro fertilization and embryo transfer (IVF-ET) remains suboptimal. This often stems from inadequate blastocyst activation and impaired dialogue with the receptive uterus [43]. Successful implantation requires synchronized development of a competent blastocyst and a receptive endometrium, processes governed by complex molecular and cellular events [44]. In vivo, these events are coordinated by ovarian hormones, growth factors, and cytokines. However, in vitro culture conditions may fail to replicate these precise signals, resulting in embryos with reduced implantation potential. Targeting this deficiency, research has focused on identifying key humoral factors that can be added to culture media to "rescue" the implantation potential of IVF-derived embryos [45]. The PEC combination emerges as a compelling solution, simultaneously engaging multiple regulatory mechanisms to enhance embryonic readiness for implantation.
Molecular and Cellular Mechanisms of the PEC Combination
The individual components of the PEC protocol activate distinct but complementary pathways that collectively prime the blastocyst for successful interaction with the endometrium.
Key Signaling Pathways and Protein Expression
The synergistic effect of the PEC combination is evidenced by its impact on specific protein levels within the blastocyst's trophectoderm (TE), the tissue responsible for attachment and invasion [45]:
- Prolactin (PRL) promotes the expression of both Breast Cancer 1 (BRCA1) and the Epidermal Growth Factor Receptor (EGFR/ERBB1) in the TE.
- Epidermal Growth Factor (EGF) upregulates BRCA1, EGFR, and another EGF receptor, ERBB4.
- 4-Hydroxyestradiol (4-OH-E2) enhances BRCA1 and Tubulointerstitial Nephritis Antigen-Like 1 (TINAGL1), a protein involved in basement membrane formation.
Critically, while each factor individually increases BRCA1, this single effect is insufficient to improve implantation rates. Combined treatment is necessary for functional synergy [45]. The PEC combination collectively boosts levels of EGFR, ERBB4, TINAGL1, and BRCA1 in the TE. Notably, it does not upregulate Estrogen Receptor-α (ESR1), which undergoes selective proteolysis via the ubiquitin-proteasome pathway in implantation-competent blastocysts [45] [43]. This precise regulation of protein expression is vital for achieving implantation-competent status.
Table 1: Molecular Targets of Individual PEC Components in the Blastocyst Trophectoderm
| Additive | BRCA1 | EGFR | ERBB4 | TINAGL1 |
|---|---|---|---|---|
| Prolactin (PRL) | Increases | Increases | No Effect | No Effect |
| Epidermal Growth Factor (EGF) | Increases | Increases | Increases | No Effect |
| 4-Hydroxyestradiol (4-OH-E2) | Increases | No Effect | No Effect | Increases |
Integrated Signaling Pathway
The following diagram summarizes the coordinated molecular actions of the PEC combination on a blastocyst, leading to improved implantation potential.
Quantitative Efficacy Data from Mouse Models
Robust experimental data from mouse studies underpins the efficacy of the PEC protocol, demonstrating its significant impact on both molecular markers and functional implantation outcomes.
Implantation Rate Outcomes
The primary evidence for the PEC combination's success comes from embryo transfer experiments. One study treated IVF-derived mouse blastocysts with the PEC combination for 24 hours prior to transfer into pseudopregnant recipients [45]. The number of implantation sites was recorded on day 6 using a blue dye method. Results showed that the combined treatment with PRL, EGF, and 4-OH-E2 significantly improved blastocyst implantation rates versus the control group (P = 0.009). Importantly, treatment with PRL, EGF, or 4-OH-E2 alone did not produce this improvement, highlighting the necessity of the synergistic combination [45].
Separate research on 4-OH-E2 alone corroborates its role in improving implantation-related outcomes. Culture media supplemented with 4-OH-E2 during the morula-to-blastocyst transition increased embryo attachment to endometrial cells in vitro and improved viable pregnancy rates in vivo, reaching levels similar to those of in vivo-derived embryos [46]. A key mechanism identified was the improvement of the embryos' ability to bind EGF [46].
Table 2: Summary of Key Efficacy Findings from Mouse Studies
| Study Focus | Treatment Group | Key Outcome Measure | Result |
|---|---|---|---|
| PEC Combination [45] | Control (No PEC) | Implantation Rate | Baseline |
| PRL, EGF, or 4-OH-E2 alone | Implantation Rate | No Significant Improvement | |
| PRL + EGF + 4-OH-E2 (PEC) | Implantation Rate | Significant Increase (P=0.009) | |
| 4-OH-E2 Alone [46] | Control (No 4-OH-E2) | EGF-binding capability | Baseline |
| 4-OH-E2 | EGF-binding capability | Improved | |
| Control (No 4-OH-E2) | Viable Pregnancy Rate | Lower | |
| 4-OH-E2 | Viable Pregnancy Rate | Improved, similar to in vivo embryos |
Detailed Experimental Protocol for PEC Treatment
For researchers seeking to replicate or build upon these findings, the following detailed methodology outlines the key procedures from the seminal study [45].
Embryo Production and Culture
- Animal Model: ICR mice.
- Superovulation: Administer gonadotropins to female mice to induce oocyte production.
- In Vitro Fertilization (IVF): Collect oocytes and fertilize with spermatozoa in HTF medium.
- Baseline Culture: Culture fertilized oocytes in Potassium Simplex Optimized Medium (KSOM) without phenol red (KSOM-P) for 90–96 hours until the blastocyst stage.
PEC Treatment Phase
- Treatment Medium: KSOM-P supplemented with the three additives:
- Prolactin (PRL): 10 or 20 mIU/mL
- Epidermal Growth Factor (EGF): 5 or 10 ng/mL
- 4-Hydroxyestradiol (4-OH-E2): 1 or 10 nM
- Treatment Duration: Incubate blastocysts in the PEC-supplemented medium for 24 hours.
Assessment and Embryo Transfer
- Molecular Analysis (Immunohistochemistry): Post-treatment, a subset of blastocysts can be analyzed for protein expression (e.g., BRCA1, EGFR, ERBB4, TINAGL1, ESR1) using immunofluorescence and confocal laser scanning microscopy.
- Functional Assessment (Embryo Transfer):
- Recipient Preparation: Use pseudopregnant female mice as recipients (Day 1 = day of vaginal plug).
- Embryo Transfer: On the morning of Day 4 of pseudopregnancy, suspend six treated blastocysts in HEPES-buffered KSOM-P medium.
- Surgical Transfer: Transfer the blastocysts into one uterine horn of each recipient mouse.
- Outcome Measurement: On Day 6 of pregnancy, count the number of implantation sites using the blue dye method.
The Scientist's Toolkit: Essential Research Reagents
Implementing the PEC protocol requires specific, high-quality reagents. The following table details the essential materials as used in the cited research.
Table 3: Key Research Reagents for the PEC Protocol
| Reagent / Material | Specifications / Function | Source Example |
|---|---|---|
| Potassium Simplex Optimized Medium (KSOM) | Base medium for embryo culture; used without phenol red (KSOM-P) in studies. | ARK Resources [10] |
| Prolactin (PRL) | Recombinant protein; used at 10-20 mIU/mL to promote BRCA1 and EGFR. | Not specified in search results |
| Epidermal Growth Factor (EGF) | Recombinant protein; used at 5-10 ng/mL to promote BRCA1, EGFR, and ERBB4. | Not specified in search results |
| 4-Hydroxyestradiol (4-OH-E2) | Estradiol metabolite; used at 1-10 nM to promote BRCA1 and TINAGL1. | Sigma-Aldrich [9] |
| HTF Medium | Medium used for in vitro fertilization steps. | ARK Resources [10] |
| Anti-BRCA1, Anti-EGFR, etc. | Primary antibodies for immunohistochemical validation of protein levels. | Proteintech [10] |
| Cryopreservation Solutions | DMSO and DAP213 solutions for freezing one-cell stage embryos. | ARK Resources [10] |
Future Research Directions and Clinical Translation
While the PEC protocol is promising, several important research avenues remain open. Current studies were conducted in a mouse model, and conclusions are drawn from results obtained from one species [45]. The influence of combined PEC supplementation on human blastocysts requires further examination and optimization before it can be considered for clinical use in ART [45]. Key questions include determining the optimal concentrations for human embryos and assessing long-term safety.
Other emerging strategies also show potential for improving implantation rates. For instance, inhibiting persistent Wnt signaling in IVF embryos has been shown to improve implantation and intrauterine development in mice and promote the development of human peri-implantation embryos [42]. Furthermore, regulating blastocyst hatching, a prerequisite for implantation, by targeting immune-related genes (e.g., Ptgs1, Lyz2, Il-α, Cfb) may offer another lever to improve ART success [7]. The future of implantation research likely lies in combining such targeted approaches, carefully tailored to the specific deficiencies of in vitro culture systems.
In mammalian reproductive biology, particularly in mouse models used for infertility research, the quality of a preimplantation embryo is a paramount factor influencing successful implantation and pregnancy establishment. Embryo quality assessment, or grading, is a morphological evaluation system that provides a predictive indicator of an embryo's developmental potential. Within the context of investigating factors affecting mouse embryo implantation success rates, robust and standardized grading is indispensable. It enables researchers to correlate embryonic phenotypes with molecular and physiological outcomes, such as the efficacy of novel compounds or the impact of genetic manipulations. The process involves scrutinizing specific developmental milestones and cellular features at precise timepoints, from the early cleavage stages to the formation of the complex blastocyst structure. This guide details the application of these grading systems, with a focus on the universally employed Gardner criteria for blastocysts, providing a technical foundation for research and drug development aimed at enhancing embryonic viability and resolving implantation failure.
Cleavage Stage Embryo Grading (Day 2/3)
During the initial cleavage stages (approximately days 2-3 in mice and humans), the embryo undergoes rapid mitotic divisions without a significant increase in overall volume. Grading at this phase focuses on the number of cells (blastomeres), their symmetry, and the degree of fragmentation [47] [48].
The cell number is an objective and critical metric. Studies indicate that embryos with certain cell counts at specific timepoints possess a higher potential to develop into viable blastocysts. For instance, a good-quality day 3 embryo is typically expected to have between 6 and 10 cells [47]. The embryo's grade also subjectively assesses the appearance of the blastomeres and the presence of anuclear cytoplasmic fragments. Excessive fragmentation is indicative of compromised cellular integrity and reduced developmental potential [48].
Table 1: Cleavage Stage Embryo Grading Criteria
| Grade | Description | Developmental Potential |
|---|---|---|
| Grade 1 | Cells are of equal size; no fragmentation seen [47]. | High potential for blastocyst development [47]. |
| Grade 2 | Cells are of equal size; minor fragmentation only (<10-25%) [47] [48]. | Good potential for development [48]. |
| Grade 2.5 | Cells are mostly of equal size; moderate fragmentation [47]. | Considered suitable for transfer [48]. |
| Grade 3 | Cells are of unequal size; no fragmentation to moderate fragmentation [47]. | Variable potential; may be suitable if cell number is adequate [47]. |
| Grade 4 | Cells are of equal or unequal size; fragmentation is moderate to heavy (>25%) [47] [48]. | Significantly reduced potential; often not selected for transfer [48]. |
It is crucial to note that while grade is important, the cell number is often a superior predictor of potential than the appearance grade alone. For example, an 8-cell Grade 3 embryo may have better potential than a 4-cell Grade 2 embryo [47]. Furthermore, cleavage can be asynchronous, and the observation of 3, 5, or 6-cell embryos is common and not necessarily an indication of poor quality [47].
Blastocyst Stage Embryy Grading: The Gardner Criteria
By day 5-6, successful embryos form a blastocyst, characterized by a fluid-filled cavity (blastocoel), and the differentiation into two distinct cell lineages: the inner cell mass (ICM), which forms the fetus, and the trophectoderm (TE), which contributes to the placenta [47]. The Gardner grading system provides a standardized alphanumeric score that captures the blastocyst's expansion level and the quality of both the ICM and TE [49] [47].
The system assigns three distinct scores:
- Numerical Score (1-6): Indicates the degree of blastocyst expansion and hatching status [49] [48].
- First Letter (A-C): Grades the quality of the Inner Cell Mass (ICM) [49] [47].
- Second Letter (A-C): Grades the quality of the Trophectoderm (TE) [49] [47].
Table 2: Gardner Blastocyst Grading System Components
| Parameter | Grade | Description |
|---|---|---|
| Expansion & Hatching Status | 1 | Early blastocyst; blastocoel less than half the embryo volume [49]. |
| 2 | Blastocyst; blastocoel half of or greater than half the volume [49]. | |
| 3 | Full blastocyst; blastocoel completely fills the embryo [49]. | |
| 4 | Expanded blastocyst; blastocoel larger than early embryo, with thinning zona [49]. | |
| 5 | Hatching blastocyst; trophectoderm starting to herniate through the zona [49]. | |
| 6 | Hatched blastocyst; blastocyst has completely escaped from the zona [49]. | |
| Inner Cell Mass (ICM) Quality | A | Tightly packed, many cells [49]. Prominent, easily discernible [48]. |
| B | Loosely grouped, several cells [49]. Easily discernible, many loosely grouped cells [48]. | |
| C | Very few cells [49]. Difficult to discern, few cells [48]. | |
| Trophectoderm (TE) Quality | A | Many cells forming a cohesive epithelium [49]. Many cells forming a cohesive, even layer [48]. |
| B | Few cells forming a loose epithelium [49]. Fewer cells forming a loose layer [48]. | |
| C | Very few large cells [49]. Very few cells, significant granularity [48]. |
A blastocyst graded as 4AA would therefore be an expanded blastocyst with an excellent inner cell mass and a superior trophectoderm. In a research and clinical setting, blastocysts graded 3-6 with ICM and TE scores of A or B are generally considered to have the highest implantation potential [48]. However, pregnancies can result from embryos across all grades, and the system serves as a tool rather than an absolute predictor [47] [48].
Experimental Protocols for Assessing Implantation Success in Mice
To investigate the factors influencing implantation rates, researchers employ sophisticated mouse models and precise experimental protocols. The following sections detail key methodologies cited in recent literature.
The Delayed Implantation (DI) Model and RO8191 Treatment
The DI model is a powerful tool for studying the molecular triggers of embryo implantation independently of the hormonal milieu [9].
Methodology:
- Animal Models: ICR or C57BL/6J plug-positive female mice are used.
- Ovariectomy: Mice are ovariectomized between 1300 and 1530 h on day 3 of pregnancy (D3) to remove the endogenous source of hormones.
- Implantation Arrest: Implantation is arrested by subcutaneous injection of medroxyprogesterone acetate (MPA).
- Experimental Intervention: On D7, a single intraperitoneal injection of the STAT3 pathway activator RO8191 (400 µg/head, dissolved in sesame oil) is administered. Control groups receive sesame oil or E2 (25 ng/head).
- Outcome Assessment: Mice are dissected on D10, and the number of implantation sites is counted. Uterine tissues can be collected at 6h (for immunohistochemistry) and 24h (for Western blot analysis) post-treatment to analyze molecular changes such as STAT3 phosphorylation [9].
Application: This protocol was used to demonstrate that RO8191, by activating the JAK/STAT3 pathway, can successfully induce embryo implantation and decidualization in the absence of an estrogen surge [9].
Uterine Fluid sncRNA Isolation and Embryo Transfection
This protocol explores the impact of maternal environment on embryo quality by analyzing the sncRNA content of uterine fluid (UF) and directly testing its effect on embryos.
Methodology:
- Fluid Collection: Oviduct fluid (OF) is collected from days 1-3 and UF on day 4 of pregnant mice.
- RNA Extraction: Total RNA is extracted from the fluid samples.
- sncRNA Sequencing: The diverse repertoire of sncRNAs, particularly tRNA-derived small RNAs (tsRNAs) and rRNA-derived small RNAs (rsRNAs), is profiled using PANDORA-seq, a panoramic small noncoding RNA sequencing method.
- Dietary Manipulation: To assess the impact of metabolism, a group of female mice is exposed to a high-fat diet (HFD) exclusively during the pre-implantation period.
- Functional Validation: To establish causality, UF-derived sncRNAs (altered by HFD) are transfected into early embryos cultured in vitro. The subsequent effects on blastocyst metabolic gene expression and development are then analyzed [15].
Application: This method identified that maternal diet significantly alters the tsRNA and rsRNA landscape of UF, and that these altered sncRNAs can impair blastocyst metabolic gene expression and compromise offspring health [15].
Time-Lapse 3D Optical Coherence Microscopy (OCM) for Label-Free Evaluation
This advanced imaging protocol provides a non-invasive, high-resolution method for assessing embryo quality and predicting developmental potential.
Methodology:
- System Setup: A compact OCM system is integrated with bright-field (BF) imaging and placed inside an incubator to maintain strict environmental control (5% O2, 6% CO2).
- Image Acquisition: Mouse embryos are cultured from the one-cell stage to the fully hatched blastocyst. Co-registered 3D OCM and BF images are acquired automatically at frequent intervals (e.g., every 10 minutes) for over 150 hours.
- Structural Analysis: OCM provides micron-level resolution to visualize and quantify key microstructural features, including:
- Cell/Nuclei Counts: From 1-cell to 8-cell stage.
- Compaction and Cavitation: Initiation and progression of the blastocoel.
- Lineage Formation: Differentiation and quality of the ICM and TE.
- Zona Pellucida Thickness and Uniformity.
- Kinetic Correlation: The timing of key developmental events (e.g., the duration of the second and third cell cycles) is correlated with subsequent blastocyst formation and quality [50].
Application: OCM-based time-lapse imaging has demonstrated that early cell cycle kinetics and specific 3D morphological features are strong indicators of an embryo's ability to form a high-quality, hatching blastocyst [50].
Signaling Pathways in Mouse Embryo Implantation
A critical pathway for embryo implantation in mice is the Leukemia Inhibitory Factor (LIF)-mediated JAK/STAT3 pathway. The following diagram illustrates the key components and experimental activation of this pathway.
Diagram 1: LIF-JAK-STAT3 Signaling Pathway in Implantation. The diagram shows the canonical LIF-induced pathway and the direct STAT3 activation by the experimental compound RO8191, which can bypass LIFR to induce implantation [9].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Research Reagents for Mouse Embryo Implantation Studies
| Reagent / Material | Function / Application | Example Use in Context |
|---|---|---|
| RO8191 | A small-molecule interferon agonist and potent activator of the STAT3 signaling pathway [9]. | Used to experimentally induce embryo implantation and decidualization in delayed implantation mouse models, bypassing the need for LIF [9]. |
| Recombinant LIF | A cytokine crucial for embryo implantation; binds to LIFR/GP130 receptor complex to activate JAK/STAT3 [9]. | Positive control in implantation studies; rescues implantation in Lif-deficient models [9]. |
| Medroxyprogesterone Acetate (MPA) | A synthetic progestin used for hormonal maintenance. | Used in the delayed implantation model to maintain a state of implantation arrest after ovariectomy [9]. |
| PANDORA-seq Kit | A panoramic small non-coding RNA sequencing method that provides a comprehensive profile of sncRNAs beyond miRNAs (e.g., tsRNAs, rsRNAs) [15]. | Used to identify and quantify dynamic changes in sncRNA populations in uterine and oviduct fluid under different dietary conditions [15]. |
| KSOM Medium | Potassium Simplex Optimized Medium; a widely used culture medium for preimplantation mouse embryos. | Serves as the base medium for in vitro culture of embryos during experiments, including those involving inhibitor screening or sncRNA transfection [10]. |
| SCADS Inhibitor Kit | A standardized library of low-molecular-weight inhibitors targeting various enzymes and signaling pathways. | Used in high-throughput screening to identify novel regulatory factors essential for preimplantation embryonic development [10]. |
The systematic grading of embryos from cleavage to blastocyst stage provides an indispensable, standardized framework for quantifying embryo quality in mouse implantation research. While morphological assessment via the Gardner system remains a cornerstone, contemporary research is increasingly leveraging advanced models like delayed implantation, sophisticated omics techniques like PANDORA-seq, and non-invasive imaging like OCM. These tools enable a deeper, more mechanistic understanding of the molecular dialogues between the embryo and uterus, with pathways like LIF-JAK-STAT3 being central. The integration of these morphological, molecular, and functional protocols empowers researchers and drug developers to precisely evaluate embryonic health, unravel the complexities of implantation failure, and rigorously test novel therapeutic interventions for infertility.
Identifying and Overcoming Common Causes of Implantation Failure
Recurrent Implantation Failure (RIF) presents a significant challenge in assisted reproductive technology (ART), characterized by the failure to achieve a clinical pregnancy after multiple transfers of good-quality embryos. While definitions vary, one widely accepted clinical definition specifies failure after transfer of at least four good-quality embryos in a minimum of three fresh or frozen cycles in women under 40 years of age [51]. The pathogenesis of RIF is multifactorial, involving embryonic, endometrial, and immunologic factors that disrupt the intricate dialogue required for successful implantation [52]. Emerging research highlights that endometrial dysfunction plays a critical role in a substantial proportion of RIF cases, with molecular heterogeneity representing a key factor underlying varied treatment responses and clinical outcomes [53]. This technical review examines the molecular mechanisms underpinning RIF and explores innovative diagnostic and therapeutic strategies emerging from both clinical studies and advanced mouse models, providing a scientific framework for developing targeted interventions.
Molecular Subtypes of Endometrial Dysfunction in RIF
Transcriptomic Profiling Reveals Distinct RIF Subtypes
Comprehensive computational analysis integrating endometrial transcriptomic datasets has revolutionized our understanding of RIF heterogeneity. A 2025 study identified 1,776 robust differentially expressed genes (DEGs) between RIF and normal endometrial samples, with unsupervised clustering revealing two biologically distinct molecular subtypes [53]:
Table 1: Molecular Subtypes of Recurrent Implantation Failure
| Subtype | Key Characteristics | Enriched Pathways | Immune Features | Potential Therapeutic Candidates |
|---|---|---|---|---|
| RIF-I (Immune-Driven) | Immune and inflammatory activation | IL-17 signaling, TNF signaling, allograft rejection | Increased effector immune cell infiltration; Elevated T-bet/GATA3 ratio | Sirolimus (mTOR inhibition) |
| RIF-M (Metabolic-Driven) | Metabolic dysregulation | Oxidative phosphorylation, fatty acid metabolism, steroid hormone biosynthesis | Altered circadian clock gene PER1 expression | Prostaglandins |
The RIF-I (Immune-Driven) subtype demonstrates enrichment in immune and inflammatory pathways including IL-17 signaling, TNF signaling, and allograft rejection pathways (p < 0.01) [53]. This subtype shows increased infiltration of effector immune cells and a characteristically higher T-bet/GATA3 expression ratio, indicating a pro-inflammatory endometrial microenvironment [53].
In contrast, the RIF-M (Metabolic-Driven) subtype is characterized by dysregulation of metabolic processes including oxidative phosphorylation, fatty acid metabolism, and steroid hormone biosynthesis [53]. This subtype also shows altered expression of the circadian clock gene PER1, suggesting a connection between metabolic and circadian regulation in implantation competence [53].
Diagnostic Classification and Validation
To translate these findings into clinical practice, researchers developed the MetaRIF classifier using machine learning algorithms, which accurately distinguishes these subtypes in independent validation cohorts with AUC values of 0.94 and 0.85 [53]. This classifier significantly outperformed previously published models (AUC: 0.88 vs. 0.48-0.72 for other signatures), providing a robust tool for molecular subtyping of RIF patients [53].
Critical Signaling Pathways in Embryo Implantation
The LIF-STAT3 Signaling Axis
The leukemia inhibitory factor (LIF)-STAT3 signaling pathway represents a critical regulatory axis for embryo implantation across mammalian species. In mice, embryo implantation occurs on day 4 of pregnancy and is triggered by a transient elevation of estrogen, which stimulates LIF release from uterine glandular epithelium [9]. LIF binds to its receptor LIFR, forming a heterodimer with glycoprotein 130 (Gp130), which activates the JAK/STAT3 signaling pathway [9].
Table 2: Essential Components of the LIF-STAT3 Signaling Pathway
| Component | Function | Validation in KO Models |
|---|---|---|
| LIF | Cytokine triggering implantation signaling | Lif-deficient mice exhibit complete implantation failure |
| LIFR | Receptor subunit for LIF binding | Uterine epithelial-specific Lifr cKO mice are infertile |
| Gp130 | Co-receptor in signaling complex | Uterine epithelial-specific Gp130 cKO mice are infertile |
| STAT3 | Transcription factor activated by phosphorylation | Uterine epithelial-specific Stat3 cKO mice are infertile |
| JAK | Kinase initiating signal transduction | Critical for STAT3 phosphorylation |
The necessity of this pathway has been validated through multiple conditional knockout (cKO) models. Mice with uterine epithelial-specific knockouts of Lifr, Gp130, or Stat3 all exhibit infertility due to complete embryo implantation failure, confirming the non-redundant role of this signaling axis [9].
Pharmacological Activation of Implantation Pathways
Recent research has identified RO8191, an interferon-α receptor 2 agonist that also functions as a potent STAT3 activator [9]. In delayed implantation mouse models, a single intraperitoneal injection of RO8191 (400 μg/head) successfully induced both embryo implantation and decidual reaction by activating STAT3—but not STAT1—signaling in uterine epithelial and stromal compartments [9].
Most remarkably, RO8191 administration rescued implantation and established pregnancy even in uterine epithelial-specific Lifr cKO mice, which are otherwise infertile due to implantation failure [9]. However, in uterine epithelial-specific Stat3 or Gp130 cKO mice, RO8191 induced only a partial decidual response, suggesting that STAT3, Gp130, and LIFR each play distinct roles in the implantation process [9].
Diagram 1: LIF-STAT3 Signaling Pathway in Implantation. The core pathway shows how natural LIF (yellow) and pharmacological RO8191 (green) activate implantation through membrane receptor complexes (blue), kinase activation (red), and nuclear transcription, culminating in successful implantation (green).
Experimental Models and Screening Approaches
Advanced Mouse Models for Implantation Research
Mouse models remain indispensable for investigating implantation mechanisms and testing potential interventions. The delayed implantation (DI) model provides a particularly valuable experimental system, achieved through ovariectomy prior to the estrogen surge on day 4 of pregnancy, with implantation arrest maintained via continuous progesterone supplementation [9]. This model allows precise investigation of molecular triggers capable of initiating implantation.
Recent technical advances include the development of a novel screening system combining ultra-superovulation technology with one-cell stage embryo cryopreservation in mice [10]. This approach enables large-scale screening experiments using inhibitor libraries to identify novel regulatory factors in preimplantation development, overcoming previous limitations in simultaneously processing large numbers of fertilized eggs from the same parents [10].
High-Throughput Screening for Embryonic Regulators
Using the SCADS Inhibitor Kit II and III libraries (95 inhibitors total), researchers screened for factors essential for mouse fertilized egg development, identifying 16 critical factors including 5 previously known and 11 novel regulators [10]. Each inhibitor was tested at 1μM concentration with 20 thawed one-cell stage embryos per treatment group, with three independent replications (288 total culture experiments) [10].
Notable discoveries from this screening include:
- PRIMA-1: A p53 activator affecting embryonic development
- Cathepsin D inhibition: Disrupts embryonic development; validated by CRISPR-Cas9 knockout
- CXCR2 inhibition: Chemokine receptor essential for development; validated by gene knockout
- SK2/SK3 potassium channel blockade: Apamin-sensitive K+ channels required for development
Developmental rates were calculated as: Developmental rate (%) = (N developed / N total) × 100, where N developed represents the number of developed embryos and N total the total number of embryos used [10].
Diagnostic Innovations and Immune Microenvironment
Endometrial Receptivity Assessment
Inadequate endometrial receptivity accounts for approximately two-thirds of implantation failures, highlighting the critical importance of diagnostic tools that can accurately assess endometrial status [54]. The window of implantation (WOI) typically occurs between days 19-24 of a 28-day menstrual cycle, but shows significant individual variation [54].
RNA-seq-based endometrial receptivity tests (rsERT) have been developed utilizing 175 differentially expressed genes coupled with artificial intelligence algorithms to precisely predict the WOI [54]. Clinical implementation of rsERT-guided personalized embryo transfer (pET) in RIF patients has demonstrated significant improvements in clinical outcomes, with one study reporting increased positive β-hCG rates (56.3% vs. 30.5%, P=0.003) and clinical pregnancy rates (43.8% vs. 24.2%, P=0.017) compared to standard frozen embryo transfer [54].
Immune Cell Dynamics in Implantation
The endometrial immune microenvironment plays a crucial role in implantation success. Comprehensive analysis of immune cell ratios in RIF patients has revealed distinct profiles associated with implantation outcomes [55]:
Diagram 2: Immune Cell Balance in Implantation. Successful implantation (green) requires balanced immune cell ratios, particularly Treg/Th cells (~1.6), while failure (red) associates with immune dysregulation across multiple cell types including macrophages, T cells, and NK cells.
Critical immune parameters include:
- Treg/Th ratio: A ratio of approximately 1.6 is associated with implantation success, reflecting appropriate immune tolerance [55]
- CD68+/CD8+ T-cell ratio: Elevated macrophage to T-cell ratios support implantation through VEGF production and tissue remodeling [55]
- Uterine NK cells: Represent up to 80% of endometrial immune cells during the mid-secretory phase, with both quantitative and functional alterations linked to RIF [55]
Therapeutic Strategies and Research Tools
Evidence-Based Interventions for RIF
An umbrella review of 47 systematic reviews evaluating RIF interventions has provided graded evidence for various therapeutic approaches [56]:
Table 3: Evidence-Based Interventions for Recurrent Implantation Failure
| Intervention | Mechanism | Clinical Pregnancy Rate Improvement | Live Birth Rate Improvement | GRADE Evidence Strength |
|---|---|---|---|---|
| G-CSF | Immunomodulation, endometrial receptivity | 9/13 MAs (69.2%) | 1/7 MAs (14%) | High-Moderate |
| Intralipid Infusion | Immunomodulation, NK cell activity regulation | 4/6 MAs (57.1%) | 3/4 MAs (75%) | High-Moderate |
| PBMC | Immunomodulation, enhances endometrial acceptance | 4/8 MAs (50%) | 3/5 MAs (60%) | High-Moderate |
| PRP | Growth factors, endometrial regeneration | 6/10 MAs (60%) | 1/5 MAs (20%) | High-Moderate |
| hCG | Embryo-endometrial signaling, immunomodulation | 3/3 MAs (100%) | Not reported | High-Moderate |
| Hysteroscopy | Correct uterine abnormalities | 1/2 MAs (50%) | Not reported | High-Moderate |
It is important to note that 88% of the included systematic reviews were appraised as critically low or low quality using AMSTAR 2 criteria, highlighting the need for more rigorous clinical trials in this field [56].
Research Reagent Solutions
Table 4: Essential Research Reagents for Implantation Studies
| Reagent/Cell Line | Application | Key Features | Research Utility |
|---|---|---|---|
| RO8191 | STAT3 pathway activation | Interferon-α receptor 2 agonist; induces implantation in DI models | Proof-of-concept for STAT3-targeted therapy; rescues implantation in Lifr cKO mice |
| SCADS Inhibitor Kits | Screening embryonic regulators | 95 inhibitors targeting diverse pathways; standardized libraries | Identified novel regulators (cathepsin D, CXCR2, SK channels) of preimplantation development |
| Delayed Implantation Mouse Model | Implantation timing studies | Ovariectomy + progesterone maintenance; precisely timed activation | Reveals molecular triggers of implantation; tests pharmacological inducers |
| Ultra-superovulation + Cryopreservation | Large-scale embryo production | Combines HyperOva stimulation with 1-cell embryo freezing | Enables high-throughput screening with genetically identical embryos |
| Conditional Knockout Mice (Lifr, Stat3, Gp130) | Pathway necessity testing | Uterine epithelial-specific gene deletion using Cre-lox system | Validates essential implantation pathway components; mechanistic studies |
| rsERT | Endometrial receptivity assessment | 175-gene panel with AI analysis; RNA-seq based | Personalizes embryo transfer timing; identifies displaced WOI in RIF patients |
The molecular dissection of RIF has revealed unprecedented complexity in implantation biology, with distinct immune and metabolic subtypes requiring different therapeutic approaches. The development of targeted interventions such as sirolimus for the immune-driven RIF-I subtype and prostaglandins for the metabolic RIF-M subtype represents a promising direction for personalized medicine in reproductive medicine [53]. Meanwhile, pharmacological activation of the STAT3 pathway with compounds like RO8191 offers innovative rescue strategies even in cases of specific receptor deficiencies [9].
Future research directions should focus on validating these subtype-specific treatments in clinical trials, refining diagnostic classifiers for routine clinical use, and exploring the crosstalk between immune and metabolic pathways in the endometrial microenvironment. The integration of high-throughput screening approaches with advanced mouse models will continue to identify novel regulatory factors and therapeutic targets. As our understanding of the molecular basis of RIF deepens, the prospect of developing truly personalized, effective interventions for this challenging condition grows increasingly attainable, ultimately transforming the clinical management of implantation failure.
Controlled ovarian hyperstimulation (COH) is a cornerstone of assisted reproductive technologies (ART), designed to induce multiple follicular development and thereby increase the number of oocytes retrieved for in vitro fertilization (IVF). [57] While COH has substantially improved pregnancy rates from IVF by allowing extended embryo culture and selection of high-quality embryos, growing evidence indicates that the resulting supraphysiological hormonal environment has detrimental consequences for endometrial receptivity. [57] [58] Successful embryo implantation requires a highly synchronized dialogue between a viable blastocyst and a receptive endometrium during a narrow window known as the window of implantation. [59] This review examines the pathophysiological mechanisms through which COH compromises uterine receptivity, focusing on histological, molecular, and vascular alterations within the endometrium that ultimately impair embryo implantation success.
Molecular and Cellular Mechanisms of COH-Induced Receptivity Failure
Disruption of Hormonal Milieu and Endometrial Development
COH protocols lead to significant deviations from the natural cycle's endocrine profile, creating a suboptimal environment for embryo implantation.
- Supraphysiological Hormone Levels: COH results in estradiol (Eâ‚‚) levels that can be 10-20 times higher than those in natural cycles during the follicular phase. The subsequent luteal phase is characterized by supraphysiological levels of both Eâ‚‚ and progesterone, produced by multiple corpora lutea. [58] This abnormal endocrine environment disrupts the delicate estrogen-to-progesterone ratio critical for normal endometrial development. [58]
- Altered Implantation Window: Histological studies reveal that under COH, the expression of endometrial pinopods—specialized epithelial structures indicative of receptivity—occurs at an earlier stage of endometrial maturation. This shift suggests a potential temporal displacement of the implantation window, creating asynchrony between embryo development and endometrial readiness. [58]
- Impaired Luteal Function: COH is associated with reduced serum levels of estradiol, progesterone, and prolactin, which collectively contribute to impaired endometrial preparation for implantation. [60]
HIF-2α Signaling Pathway Dysregulation
Recent research has identified hypoxia-inducible factor 2α (HIF-2α) as a critical mediator of COH-induced endometrial dysfunction. [60]
Table 1: HIF-2α Pathway Alterations in COH and Functional Consequences
| Molecular Change | Direction | Downstream Effects | Functional Outcome |
|---|---|---|---|
| HIF-2α mRNA & Protein | Significantly Downregulated | Reduced pathway activation | Impaired implantation signaling |
| RAB27B/MMP9 Axis | Dysregulated | Compromised extracellular matrix remodeling | Inhibited trophoblast invasion |
| LOX/ADM Axis | Dysregulated | Altered vascular function & tissue integrity | Failed luminal epithelial detachment |
Studies on COH mouse models demonstrate that the downregulation of uterine HIF-2α disrupts two key axes: the HIF-2α-RAB27B/MMP9 and HIF-2α-LOX/ADM pathways. [60] These disruptions are directly associated with:
- Impaired luminal epithelium detachment, a necessary step for embryo invasion.
- Compromised trophoblast cell invasion into the endometrial stroma.
- Preserved luminal epithelium integrity with increased microvillus density, contrary to the changes needed for successful implantation. [60]
Impairment of Angiogenic Signaling
Adequate vascular development is crucial for endometrial receptivity and subsequent placental development. COH disrupts this process through multiple mechanisms:
- Impaired Endometrial Angiogenesis: COH models demonstrate abnormal expression of pro-angiogenic factors, including HIF1α and the COX2-PGE2 pathway. [61]
- Dysregulation of Downstream Effectors: The expression of critical factors for vascular remodeling and trophoblast invasion—including MMP2, MMP9, TIMP2, and FGF2—is significantly impaired following COH. [61] This dysregulation creates an unfavorable microenvironment for embryo implantation and subsequent placental development.
Table: Key Research Reagent Solutions for Studying COH Effects
| Research Reagent | Application in COH Research | Experimental Function |
|---|---|---|
| Pregnant Mare's Serum Gonadotropin (PMSG) | COH mouse model induction [61] | Mimics FSH activity to stimulate multi-follicular development |
| Human Chorionic Gonadotropin (hCG) | COH mouse model induction [61] | Triggers final oocyte maturation and luteinization (LH surge analog) |
| Gonadotropin-releasing Hormone Agonist (GnRH-a) | COH mouse model establishment [60] | Provides pituitary downregulation to control cycle timing |
| Human Menopausal Gonadotropin (hMG) | COH mouse model establishment [60] | Provides FSH and LH activity for follicular stimulation |
| Ishikawa Cell Line | In vitro implantation model [62] | Provides human endometrial epithelium for co-culture with embryos |
| KSOM Medium | In vitro embryo culture [62] | Supports development of mouse zygotes to blastocysts |
| M2 Medium | Embryo handling and transfer [62] | Provides buffered medium for embryo manipulation outside incubator |
Experimental Models and Methodologies
In Vivo Mouse Model of COH
The COH mouse model is a well-established system for investigating the effects of ovarian stimulation on endometrial receptivity and implantation outcomes.
Protocol for COH Mouse Model Establishment:
- Animal Selection: Use 6-8 week old female mice (e.g., Kunming breed). [61]
- Superovulation Induction:
- Mating: Following hCG administration, house female mice with fertile males and check for vaginal plugs the next morning to confirm mating. [62]
- Tissue Collection: Sacrifice mice at specific time points (e.g., embryonic day 4, 5, 6, or 8) for analysis of implantation sites, endometrial collection, and serum hormone measurement. [60] [61]
Endpoint Measurements:
- Implantation Rate Calculation: Compare number of implantation sites to number of corpora lutea or transferred embryos. [60]
- Hormone Assays: Measure serum Eâ‚‚, Pâ‚„, and prolactin levels using radioimmunoassay or ELISA. [60] [61]
- Molecular Analysis: Examine endometrial tissues for gene and protein expression of relevant pathways (HIF-2α, MMPs, angiogenic factors) using qRT-PCR, Western blot, and immunohistochemistry. [60] [61]
- Histological Evaluation: Assess endometrial microvasculature using CD31 immunostaining and examine ultrastructural changes via transmission electron microscopy. [60] [61]
In Vitro Embryo Implantation Model
The in vitro implantation model provides a controlled system for investigating specific molecular interactions between embryos and the endometrium.
In Vitro Implantation Model Workflow
Detailed Co-culture Methodology:
- Mouse Blastocyst Acquisition:
- Induce superovulation in female mice (6-8 weeks old) with 10 IU PMSG followed by 10 IU hCG 42-48 hours later. [62]
- After mating, collect zygotes by dissecting oviducts and puncturing the ampulla to release cumulus-zygote complexes. [62]
- Treat with 0.5 mg/mL hyaluronidase to remove cumulus cells, then wash zygotes in M2 medium with BSA. [62]
- Culture in KSOM microdroplets under mineral oil at 37°C with 5% CO₂ for 4 days to blastocyst stage. [62]
Endometrial Cell Preparation:
Co-culture and Assessment:
Application for Hormonal Studies: This model has been utilized to test the effects of supraphysiological hormone concentrations on implantation. Studies demonstrate that 100 nM Eâ‚‚ significantly reduces embryo implantation rates, while the addition of progesterone can dose-dependently alleviate this negative effect. [62]
Compensatory Strategies and Therapeutic Interventions
Segmentation and Freeze-All Strategy
Segmentation of IVF treatment, commonly referred to as the "freeze-all" strategy, involves cryopreserving all embryos from a COH cycle and transferring them in a subsequent natural or artificially prepared cycle. [57] This approach addresses COH-induced receptivity issues by:
- Allowing embryo transfer in a more physiologic uterine environment without the confounding effects of supraphysiological hormone levels. [57]
- Decreasing uterine contractility, which may be increased following COH. [57]
- Diminishing the impact of premature luteinization and permitting individualized ovarian stimulation based on patient response. [57]
Pharmacological Approaches
Research has investigated various pharmacological interventions to counteract the detrimental effects of COH on endometrial receptivity:
- Bushen Huoxue Recipe (BSHXR): This traditional Chinese medicine formulation has demonstrated efficacy in improving embryo implantation in COH mouse models by:
- Restoring supraphysiological serum progesterone levels to normal ranges. [61]
- Significantly improving the abnormal expression of endometrial pro-angiogenic factors, including HIF1α and the COX2-PGE2 pathway. [61]
- Normalizing downstream factors critical for implantation, including MMP2, MMP9, TIMP2, and FGF2. [61]
Endometrial Receptivity Testing
Endometrial receptivity tests (ERTs), such as the Endometrial Receptivity Array (ERA), analyze the expression of 238 genes from endometrial tissue biopsies to identify a personal window of implantation. [59] The clinical rationale is to:
- Identify displaced windows of implantation in women with recurrent implantation failure. [59]
- Personalize the timing of embryo transfer based on individual endometrial receptivity rather than standard protocols. [59]
- However, recent Cochrane protocol highlights ongoing uncertainty regarding the effectiveness of personalized embryo transfer timing compared to standard timing, with studies reporting conflicting outcomes. [59]
Controlled ovarian hyperstimulation induces a complex cascade of molecular and structural changes in the endometrium that collectively compromise uterine receptivity. The key mechanisms include disruption of the hormonal milieu, downregulation of the HIF-2α signaling pathway with consequent impairment of epithelial detachment and trophoblast invasion, and dysregulation of angiogenic factors. These findings provide a mechanistic explanation for the reduced implantation rates observed in fresh ART cycles following COH. Ongoing research focuses on developing targeted interventions to mitigate these effects, either through segmentation of treatment cycles, pharmacological approaches to restore normal endometrial function, or personalized transfer timing through receptivity testing. A comprehensive understanding of these pathways will enable the development of novel strategies to overcome COH-induced endometrial deficiencies, ultimately improving success rates in assisted reproduction.
The in vitro production (IVP) of embryos is a cornerstone of assisted reproductive technologies (ART) and fundamental research, particularly in mouse models studying embryo implantation. A significant impediment to the success of these techniques is oxidative stress, a state of imbalance between the production of reactive oxygen species (ROS) and the capacity of the biological system to readily detoxify the reactive intermediates or repair the resulting damage [63] [64]. While physiological levels of ROS act as crucial signaling molecules in processes like sperm capacitation and oocyte maturation, their pathological accumulation during in vitro culture compromises the structural and functional integrity of gametes and embryos [63] [65]. This damage manifests as lipid peroxidation, protein modification, and DNA fragmentation, ultimately accelerating cell apoptosis and impairing developmental potential, thereby affecting implantation success rates in broader thesis research [66] [64]. This technical guide outlines the sources of oxidative stress in embryo culture, details the mechanisms of damage, and provides evidence-based strategies for its mitigation.
The in vitro environment presents multiple non-physiological stressors that can lead to excessive ROS generation. Understanding these sources is the first step in developing effective mitigation protocols.
Table 1: Sources of Reactive Oxygen Species (ROS) in Embryo Culture Systems
| Source Category | Specific Examples | Impact on Gametes/Embryos |
|---|---|---|
| Physical Environment | Atmospheric oxygen (20-21%), visible light, temperature fluctuations, pH instability [63] [66] | Disruption of redox homeostasis, increased intracellular ROS, metabolic stress. |
| Culture Procedures | Centrifugation during sperm preparation, handling of gametes, physical manipulation of embryos [63] | Mechanical stress leading to ROS production from sperm and embryos. |
| Cryopreservation | Slow-freezing methods, osmotic shock, dilution of samples, exposure to cryoprotectants [63] [64] | Increased ROS production, apoptosis, and cellular damage post-thaw. |
| Cellular Sources | Immature sperm, oocytes, and embryos; activated leukocytes; mitochondrial metabolism [63] [66] | Endogenous production of superoxide anion (O₂•â») and hydrogen peroxide (Hâ‚‚Oâ‚‚). |
The laboratory atmosphere is a primary concern. While most body tissues, including the fallopian tubes, function at oxygen concentrations between 4% and 10%, standard embryo culture often occurs at atmospheric oxygen levels (20-21%) [63]. This hyperoxic condition is a significant driver of OS, mediating its effects through excessive ROS production that damages cellular components [63] [66]. Furthermore, procedures such as sperm preparation, which involves centrifugation and removal of protective seminal plasma, can increase ROS generation [63]. The cryopreservation-thawing process also induces OS, with slow-freezing methods particularly prone to causing ice crystal formation and oxidative damage [63] [64].
Molecular Mechanisms of ROS-Induced Damage and Apoptosis
Excessive ROS inflicts damage on all major classes of biomolecules, activating pathways that can lead to arrested development or apoptosis.
- Lipid Peroxidation: ROS, particularly the hydroxyl radical (•OH), attacks the polyunsaturated fatty acids (PUFAs) in cell membranes. This cascade produces highly reactive and mutagenic end products like malondialdehyde (MDA), which further damages membranes and disrupts cellular functions like capacitation and sperm-oocyte fusion [63] [66].
- DNA Damage: The hydroxyl radical reacts with DNA, causing base modifications such as the formation of 8-oxodeoxyguanosine (8-oxo-dG) and single- or double-strand breaks [66]. This is especially critical for mitochondrial DNA (mtDNA), which lacks the protective histones of nuclear DNA and is in close proximity to ROS production sites [66]. High levels of sperm DNA fragmentation (SDF) have been correlated with poor embryo quality and low pregnancy rates [63].
- Protein Damage: ROS can alter the primary and secondary structures of proteins, leading to loss of enzymatic function, disruption of signaling pathways, and improper folding [66].
- Induction of Apoptosis: Sustained oxidative damage triggers programmed cell death. Key indicators include the externalization of phosphatidylserine (PS), detectable by Annexin V staining, and the loss of membrane integrity, indicated by propidium iodide (PI) uptake [67]. While one study found that apoptosis in granulosa cells did not significantly impact fertilization, increased ROS production in these cells was linked to fewer oocytes retrieved and a diminished implantation rate [67].
The following diagram illustrates the interconnected pathways of ROS generation and their detrimental effects on embryonic cells:
Experimental Protocols for Assessing Oxidative Stress
Accurate assessment is crucial for evaluating oxidative stress levels in gametes and embryos. The following table summarizes key methodologies and reagents used in this field.
Table 2: Research Reagent Solutions for Assessing Oxidative Stress and Apoptosis
| Research Reagent / Kit | Function / Target | Experimental Application |
|---|---|---|
| Hydroethidine (HE) / MitoSOX Red | Detection of superoxide anion (O₂•â») | Flow cytometry or fluorescence microscopy to detect intracellular ROS in granulosa cells, sperm, or embryos [67]. |
| 2',7'-Dichlorodihydrofluorescein diacetate (DCFH-DA) | General detection of intracellular ROS | Widely used fluorescent staining for ROS in sperm, cumulus-oocyte complexes (COCs), and embryos [64]. |
| Nitro Blue Tetrazolium (NBT) | Reduces to formazan in presence of ROS | Simple histochemical staining to detect and quantify intracellular ROS in oocytes, cumulus cells, and embryos [64]. |
| Annexin V-FITC / Propidium Iodide (PI) | Detection of apoptosis (PS externalization) & necrosis | Flow cytometry to classify cells as apoptotic (Annexin V+/PI-), necrotic (Annexin V+/PI+), or normal (Annexin V-/PI-) [67]. |
| Antibody: anti-8-oxo-dG | Specific detection of oxidative DNA damage | Immunofluorescence staining to visualize and quantify ROS-induced DNA lesions [66]. |
| Olink Development Panel (PEA) | Multiplexed quantitation of 92 proteins | Proximity extension assay (PEA) technology to analyze secretomic profiles in spent blastocyst media for non-invasive embryo assessment [68]. |
| SCADS Inhibitor Kit | Library of chemical inhibitors | Screening for novel factors involved in embryonic development by targeting specific enzymes or pathways [10]. |
Detailed Protocol: Flow Cytometry for ROS and Apoptosis in Granulosa Cells
This protocol, adapted from a human IVF study, details the simultaneous analysis of ROS production and apoptosis in granulosa cells, which are key indicators of oocyte quality [67].
- Cell Isolation and Preparation: Isolate granulosa cells from follicular fluid aspirates by centrifugation. Resuspend the pelleted cells in Universal IVF medium or RPMI. Separate granulosa cells from leukocytes and other contaminants using a density gradient centrifugation (e.g., PureSperm 50%) [67].
- Cell Staining:
- For ROS Detection: Incubate cell suspensions (1 × 10ⶠcells/ml) with 10 μmol/L hydroethidine (HE) for 15 minutes at 37°C with continuous shaking. To measure the oxidative burst capacity, split the suspension and stimulate one aliquot with phorbol 12-myristate 13-acetate (PMA, 320 nmol/L) for 15 minutes [67].
- For Apoptosis Detection: Label another cell suspension with Annexin V-FITC and propidium iodide (PI, 1 μg/ml). Incubate in the dark for 15 minutes at 18°C [67].
- Flow Cytometry Analysis:
- Analyze the samples on a flow cytometer (e.g., FACSCalibur).
- For ROS: Detect HE fluorescence (ethidine) under 488 nm excitation using a 586-nm band-pass filter. Report the results as the percentage of ROS-producing granulosa cells [67].
- For Apoptosis: Use a cytogram of Annexin V-FITC fluorescence versus PI fluorescence to distinguish between live (Annexin V-/PI-), apoptotic (Annexin V+/PI-), and necrotic (Annexin V+/PI+) cell populations [67].
Mitigation Strategies: Optimizing Culture Conditions and Using Antioxidants
A multi-faceted approach is required to minimize oxidative stress during embryo culture. The most effective strategy involves optimizing the entire culture system.
Optimization of the Physical Environment
- Reduced Oxygen Culture: Lowering the oxygen tension in incubators from atmospheric levels (20%) to a more physiological range (5-7%) is one of the most effective ways to reduce ROS generation and improve embryo development [63] [66].
- Control of Light and Temperature: Minimize exposure of gametes and embryos to visible light and prevent temperature fluctuations by using pre-warmed handling media and working quickly under stable conditions [63].
Use of Antioxidant Supplements
The supplementation of culture media with antioxidants is a direct method to scavenge excess ROS. These can be broadly classified as enzymatic or non-enzymatic.
Table 3: Efficacy of Antioxidant Supplementation in Embryo Culture Media
| Antioxidant | Type | Proposed Mechanism of Action | Reported Outcome in IVP |
|---|---|---|---|
| Superoxide Dismutase (SOD) | Enzymatic | Converts superoxide anion (O₂•â») into hydrogen peroxide (Hâ‚‚Oâ‚‚) and oxygen [66]. | Part of intrinsic defense; external supplementation helps mitigate OS. |
| Catalase (CAT) | Enzymatic | Converts hydrogen peroxide (Hâ‚‚Oâ‚‚) into water and oxygen [66]. | Works in synergy with SOD to detoxify ROS. |
| Glutathione (GSH) | Low Molecular Weight | Major intracellular antioxidant; electron donor for GPx to reduce Hâ‚‚Oâ‚‚ [66] [64]. | Improved sperm viability post-thaw; critical for redox homeostasis in oocytes/embryos. |
| Vitamin C | Vitamin | Water-soluble antioxidant that directly scavenges free radicals [64]. | Can improve oocyte maturation and embryo quality. |
| Vitamin E | Vitamin | Lipid-soluble antioxidant that protects cell membranes from lipid peroxidation [64]. | Shown to reduce oxidative damage in gametes and embryos. |
The following workflow diagram integrates these strategies into a cohesive protocol for mitigating oxidative stress during in vitro embryo production:
Advanced Screening and Non-Invasive Assessment Techniques
Emerging technologies are providing new tools to non-invasively identify embryos with the highest developmental potential, thereby improving implantation success rates in research.
- Inhibitor Library Screening: A 2025 study developed a novel screening system combining ultra-superovulation with one-cell embryo cryopreservation in mice to screen an inhibitor library [10]. This approach identified 16 factors essential for the development of fertilized eggs, including known regulators like ATPases and novel factors such as cathepsin D and CXCR2. Genome editing via CRISPR-Cas9 knockout of these genes verified their critical role in embryonic development, highlighting new potential targets for modulating embryo quality [10].
- Secretomic and Morphometric Profiling: A powerful non-invasive method involves analyzing the secretome (proteins secreted into the culture medium) and the morphometry (shape and size) of blastocysts. A 2025 study quantified 92 proteins in spent blastocyst media using a proximity extension assay (PEA) and combined this with image analysis [68]. They found that implanting blastocysts secreted higher levels of Matrilin-2 (MATN2) and legumain (LGMN), and lower levels of thymosin beta-10 (TMSB10). A predictive model combining these secretomic markers with morphometric shape descriptors (e.g., internal circularity, roundness) showed exceptional predictive power for implantation outcomes [68].
The successful management of reactive oxygen species and the suppression of apoptosis are critical for maximizing the efficacy of mouse embryo culture and, by extension, the validity of research on implantation success. A comprehensive strategy that includes optimizing the physical culture environment, judiciously supplementing with antioxidants, and employing advanced non-invasive assessment techniques provides a robust framework for mitigating cellular stress. As the field advances, the development of standardized, safe, and effective antioxidant supplement systems, alongside the discovery of novel regulatory factors through high-throughput screening, will further enhance the quality and translational relevance of embryo culture research.
Somatic cell nuclear transfer (SCNT) has revolutionized biomedical research by enabling the reprogramming of differentiated somatic cells into a totipotent state. This technology is invaluable for generating genetically engineered animal models, conserving endangered species, and advancing regenerative medicine [69] [70]. Despite these applications, the clinical utility of SCNT remains severely limited by low efficiency, with only 1-5% of reconstructed embryos typically developing to term in mammalian species [71] [72]. The predominant scientific consensus identifies incomplete epigenetic reprogramming as the primary bottleneck, wherein the somatic cell's epigenetic memory fails to be adequately erased and reset to an embryonic state [69] [73] [74]. This whitepaper examines the epigenetic barriers impairing SCNT success and details evidence-based strategies to enhance reprogramming efficacy, with a specific focus on implications for mouse embryo implantation research.
Epigenetic Barriers to Successful SCNT
The developmental failure of SCNT embryos can be largely attributed to specific, persistent epigenetic marks inherited from the donor somatic cell that resist reprogramming.
Key Reprogramming Obstacles
- Abnormal DNA Methylation Patterns: SCNT embryos demonstrate delayed DNA demethylation and incomplete DNA remethylation compared to their in vitro fertilized (IVF) counterparts. The somatic cell genome is highly methylated, and this methylation must be erased for proper embryonic gene activation. Specifically, pluripotency-related genes like
Oct4often retain hypermethylation, while tissue-specific genes may show hypomethylation [69] [74]. - Repressive Histone Modifications: The mark H3K9me3 is a major reprogramming barrier. It creates repressive chromatin domains that prevent the activation of genes essential for zygotic genome activation (ZGA). These regions, termed "reprogramming-resistant regions" (RRRs), are enriched in H3K9me3 and block transcription factor binding [72]. Additionally, aberrant levels of H3K27me3 and low levels of activating marks like H3K9ac and H3K14ac are commonly observed [69] [75].
- Defective Genomic Imprinting and X-Chromosome Inactivation: SCNT embryos frequently fail to maintain proper methylation at imprinted loci such as
H19/Igf2[69] [73]. In female cloned embryos, the X-chromosome is often inappropriately inactivated due to faulty DNA methylation of theXistgene [73] [74].
The following diagram illustrates how these epigenetic barriers impede the normal reprogramming process after nuclear transfer.
Strategic Interventions to Enhance Epigenetic Reprogramming
Several targeted approaches have been developed to overcome these epigenetic barriers, ranging from pharmacological interventions to genetic manipulation.
Pharmacological Epigenetic Modulators
Small molecule inhibitors targeting epigenetic enzymes have shown significant promise in improving SCNT outcomes.
Table 1: Epigenetic Modulators to Improve SCNT Efficiency
| Category | Compound | Target | Effect on SCNT Embryos | Key Outcome |
|---|---|---|---|---|
| HDAC Inhibitors | Trichostatin A (TSA) | Histone deacetylases | Increases histone acetylation, opens chromatin | Improves blastocyst development; macaque cloning success [69] [72] |
| DNMT Inhibitors | 5-Aza-2'-deoxycytidine | DNA methyltransferases | Reduces global DNA methylation | Enhances reprogramming of pluripotency genes [70] |
| H3K9me3 Demethylation | KDM4D | H3K9me3 | Reduces repressive H3K9me3 marks | Overcomes RRRs, improves ZGA and mouse cloning efficiency [72] |
| Antioxidants | Lycopene (0.2 µM) | Reactive oxygen species | Reduces ROS, decreases H3K9me3 and DNA methylation | Improves blastocyst rate, cell number, and ZGA in porcine models [75] |
Genetic and RNA Interference Approaches
Direct manipulation of epigenetic regulators has proven highly effective in research settings.
- KDM4D Overexpression: Forced expression of the H3K9me3 demethylase KDM4D directly removes the H3K9me3 barrier, facilitating the activation of ZGA genes and significantly improving mouse SCNT efficiency [72].
- Long Non-coding RNA (lncRNA) Modulation: Regulating specific lncRNAs involved in X-chromosome inactivation and imprinting, such as Xist, helps correct aberrant silencing patterns in cloned embryos [69] [74].
Technical and Procedural Optimizations
- Handmade Cloning (HMC): This simplified, zona-free technique reduces mechanical stress on oocytes and has successfully produced cloned offspring in cattle, pigs, and other species [70].
- Oocyte Quality Selection: Using Brilliant Cresyl Blue (BCB) staining to select developmentally competent oocytes from slaughterhouse-derived ovaries improves the cytoplasmic reprogramming capacity [70].
- Robotic Enucleation: A recently developed robotic label-free enucleation system reduced cytoplasmic loss by 60% and doubled the cleavage rate of cloned pig embryos compared to traditional methods [70].
The workflow below integrates these strategic interventions into a cohesive SCNT protocol.
Experimental Protocols for SCNT Improvement
Lycopene Supplementation Protocol for Enhanced Reprogramming
A 2025 study demonstrated that the antioxidant lycopene significantly improves epigenetic reprogramming and ZGA in porcine SCNT embryos [75].
- Compound Preparation: Prepare a 10 mM lycopene stock solution in DMSO. Dilute to a 0.2 μM working concentration in post-activation and in vitro culture (IVC) medium. The final DMSO concentration should not exceed 0.01%.
- Treatment Protocol: Culture SCNT embryos in lycopene-supplemented medium for the entire IVC period (typically 6 days for pig embryos). Maintain control groups in medium with vehicle (DMSO) only.
- Key Outcome Measures:
- Developmental Rates: Assess 4-5 cell cleavage (Day 2) and blastocyst formation (Day 6-7).
- Epigenetic Marks: Quantify global levels of H3K4me3, H3K9me3 (histone methylation), and 5mC (DNA methylation) via immunofluorescence at the 4-cell stage.
- Gene Expression: Analyze expression of ZGA-related genes (
ZSCAN4,UBTFL1,MYC) and antioxidant genes (SOD1,SOD2,CAT) by qPCR. - Functional Assays: Measure intracellular ROS levels, mitochondrial membrane potential (JC-1 assay), and apoptosis rates (TUNEL assay) in blastocysts.
H3K9me3 Barrier Reduction via KDM4D
- Experimental Approach: Inject
KDM4DmRNA into oocytes immediately after SCNT or treat with specific H3K9me3 demethylase inhibitors. - Validation Methods:
- Chromatin immunoprecipitation (ChIP) to assess H3K9me3 levels at reprogramming-resistant regions.
- RNA-seq to monitor transcriptional activation of ZGA genes.
- Expected Outcome: Significant improvement in developmental progression beyond the 2-cell stage in mouse SCNT embryos [72].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SCNT Reprogramming Research
| Reagent/Category | Specific Examples | Function/Application | Research Context |
|---|---|---|---|
| HDAC Inhibitors | Trichostatin A (TSA), Scriptaid | Increases histone acetylation, relaxes chromatin | Added to embryo culture medium post-activation (0.1-0.5 µM) [72] [70] |
| DNMT Inhibitors | 5-Aza-2'-deoxycytidine, RG108 | Reduces global DNA methylation | Donor cell pretreatment or short-term embryo exposure [70] |
| Antioxidants | Lycopene (0.2 µM), Melatonin | Scavenges ROS, reduces oxidative stress | Supplemented in culture medium throughout IVC [75] |
| H3K9me3-Targeting Reagents | KDM4D mRNA, SUV39H1/2 inhibitors | Directly reduces H3K9me3 barrier | Microinjected into cytoplasm post-SCNT [72] |
| Oocyte Selection Dyes | Brilliant Cresyl Blue (BCB) | Identifies oocytes with high developmental competence | Staining of oocytes prior to IVM [70] |
| Pathway Agonists | RO8191 (STAT3 activator) | Induces embryo implantation signaling | Used at 400 µg/mouse in implantation studies [9] |
The strategic manipulation of epigenetic pathways presents the most promising avenue for overcoming the current limitations of SCNT. Targeted approaches, including H3K9me3 demethylation, antioxidant supplementation, and the use of small molecule epigenetic modulators, have demonstrated significant improvements in reprogramming efficiency and embryonic development. The integration of these biochemical strategies with refined technical protocols such as handmade cloning and robotic enucleation provides a comprehensive framework for enhancing SCNT outcomes. For research focused on mouse embryo implantation, these advances are particularly relevant, as improved epigenetic resetting directly correlates with better embryo quality and uterine receptivity. Future work should prioritize the identification of additional reprogramming-resistant loci and the development of even more specific epigenetic editors to further optimize this powerful technology.
Successful embryo implantation is a pivotal stage in mammalian pregnancy, representing the first point of physical and biological contact between the developing embryo and the maternal endometrium. Within the context of mouse embryo implantation research, this process demands exquisitely precise synchronization between a competent blastocyst and a receptive endometrium, orchestrated through complex molecular dialogues that occur within a limited temporal window. Despite concerted efforts in assisted reproductive technologies, implantation failure remains a significant challenge, with success rates plateauing between 25% and 30% in human IVF treatments, underscoring the critical need to understand the fundamental mechanisms governing this process [76].
The concept of the "window of implantation" (WOI) describes the brief period during which the endometrial environment becomes permissive for blastocyst attachment and invasion. In mice, this window is tightly regulated by ovarian hormones—progesterone and a transient surge of 17β-estradiol on gestation day 4 (D4)—which activate sophisticated signaling cascades essential for uterine receptivity and embryo activation [9] [3]. This review examines the molecular determinants of embryo-endometrial synchrony, explores experimental approaches for investigating this dialogue, and highlights emerging therapeutic targets that may ultimately improve implantation success rates in both basic research and clinical applications.
Embryo Competence and Developmental Trajectory
Morphological and Morphokinetic Parameters
Embryo quality assessment traditionally relies on morphological evaluation at both cleavage and blastocyst stages. According to the Istanbul consensus criteria, 'good' quality cleavage-stage embryos exhibit specific characteristics: 4 blastomeres on Day 2 and at least 8 blastomeres on Day 3 post-fertilization, with even-sized blastomeres, <10% fragmentation, and no multinucleation [76]. The presence of multinucleated blastomeres is widely associated with diminished developmental potential, manifested by reduced blastocyst formation and significantly lower implantation rates [76].
Blastocyst evaluation incorporates expansion stage, inner cell mass (ICM) appearance, and trophectoderm (TE) cohesiveness. Higher-quality ICM and TE are linked to increased euploidy rates, while poor-quality ICM and TE are associated with complex aneuploidy [76]. Time-lapse technology (TLT) has enhanced dynamic monitoring of embryo development, revealing that aneuploid blastocysts often exhibit extended durations for specific developmental milestones (t8, t9, and initiation of expansion - tEB), along with higher fragmentation grades and persistent multinucleation [76].
Table 1: Morphological Criteria for Embryo Quality Assessment
| Development Stage | Assessment Parameters | Quality Indicators | Implications for Development |
|---|---|---|---|
| Cleavage Stage (Day 2-3) | Cell number, fragmentation, multinucleation, blastomere symmetry | 4 cells (Day 2), ≥8 cells (Day 3), <10% fragmentation, no multinucleation | Reduced developmental potential with slow cleavage or multinucleation |
| Blastocyst Stage (Day 5-7) | Expansion state, Inner Cell Mass (ICM), Trophectoderm (TE) | Good expansion, cohesive TE, compact ICM | Higher euploidy rates with better ICM/TE quality; Day 5 blastocysts show higher pregnancy rates than Day 6/7 |
| Morphokinetic Parameters | Timing of cell divisions (t2-t8), blastulation (tB), expansion (tEB) | Specific time intervals for development | Extended t8, t9, tEB associated with aneuploidy; controversial predictive value for implantation |
Molecular Determinants of Embryo Viability
Beyond morphological assessment, molecular markers provide insights into embryonic developmental competence. Mitochondrial DNA (mtDNA) quantification has emerged as a potential biomarker, with concentrations in embryonic cells postulated to play a key role in determining embryonic competence [76]. Additionally, recent research has identified novel regulators affecting various developmental stages, including p53 activators (PRIMA-1), cathepsin D, CXCR2, and potassium channels (SK2 and SK3), as demonstrated through inhibitor library screening in mouse models [10].
Gene expression changes during blastocyst hatching significantly affect implantation success. Transcriptomic analyses of mouse blastocysts have revealed distinct gene expression profiles correlated with hatching outcomes. Embryos hatched from specific sites (B-site) near the inner cell mass showed 65.6% birth rates compared to 21.3% for C-site (opposite ICM) and 5.1% for hatching failure [7]. Differentially expressed genes identified in these studies were primarily involved in immune function and regulated by transcription factors TCF24 and DLX3 [7].
Endometrial Receptivity: Preparing the Maternal Environment
Structural and Molecular Transformation
The endometrium undergoes precisely orchestrated changes to achieve a receptive state capable of supporting embryo implantation. In mice, this process is regulated by progesterone and a transient surge of 17β-estradiol on gestation day 4 [3]. Structural changes include the appearance of pinopodes—microvilli projections on the apical surface of luminal epithelial cells—which facilitate embryo attachment through increased expression of adhesion molecules [77].
Molecular markers of endometrial receptivity include cytokines, growth factors, and cell adhesion molecules. Leukemia inhibitory factor (LIF) represents a critical mediator, with maximal expression during the mid-secretory phase that plays an essential role in embryo attachment [77]. Women with recurrent implantation failure often demonstrate decreased LIF production, highlighting its clinical significance [77]. Other crucial molecules include integrins, selectins, and glycoproteins that mediate the physical interaction between embryo and endometrium [78].
Table 2: Key Molecular Players in Embryo-Endometrial Dialogue
| Molecule Category | Specific Factors | Primary Function | Expression Pattern |
|---|---|---|---|
| Cytokines | LIF (Leukemia Inhibitory Factor) | Embryo attachment, pinopode formation | Maximal at mid-secretory phase; uterine epithelium |
| Cell Adhesion Molecules | Integrins, Selectins, Cadherins | Mediate physical adhesion between trophectoderm and endometrium | Apical surface of luminal epithelium during WOI |
| Signaling Receptors | LIFR, GP130, ERBB2 | Activate JAK/STAT3 pathway for implantation | Epithelium and stroma; precise temporal expression |
| Transcription Factors | STAT3, TCF24, DLX3 | Regulate gene networks for implantation | Nuclear translocation upon pathway activation |
| Embryonic Signals | Human Chorionic Gonadotropin (hCG) | Promotes progesterone production, uterine receptivity | Trophoblast cells post-hatching |
The Window of Implantation: Temporal Regulation
The window of implantation (WOI) represents a self-limited period when the endometrium acquires functional status allowing blastocyst adhesion. In a normal 28-day human menstrual cycle, the WOI occurs around days 20-24 [79] [78]. In mice with regular 4-5 day cycles, implantation occurs on day 4 after the detection of a vaginal plug (D1) [3]. The WOI is finely regulated by a plethora of factors, including hormones, cytokines, growth factors, and immunomodulatory factors, all driving morphological and molecular changes fundamental for correct blastocyst-endometrial dialogue [76].
The precise timing of the WOI shows inter-individual variability, necessitating personalized assessment in clinical contexts. In artificial cycles, the WOI typically occurs 4-7 days after progesterone administration [76]. Evaluation methods have evolved from histological dating according to Noyes criteria to more sophisticated omics approaches, including the Endometrial Receptivity Array (ERA), which assesses the gene expression signature characterizing the receptive endometrium [76].
Molecular Mechanisms of Embryo-Endometrial Synchronization
Signaling Pathways Governing Implantation
The LIFR-GP130-JAK-STAT3 signaling axis represents a cornerstone of implantation regulation in mice. LIF, expressed in the uterine glandular epithelium during the pre-implantation phase, interacts with the LIF receptor (LIFR) on the luminal epithelium, forming a heterodimer with glycoprotein 130 (GP130) [9]. This complex activates the JAK-STAT3 pathway, leading to STAT3 phosphorylation and nuclear translocation, where it mediates expression of genes essential for implantation [9].
Recent research has identified ERBB2 as a crucial downstream effector in LIFR-mediated signaling. Comprehensive gene expression analysis of Lifr eKO and Gp130 eKO mice revealed Erbb2 and c-Fos as key hub genes, with ERBB2 inhibition significantly disrupting implantation processes [3]. This discovery expands our understanding of the molecular network beyond the canonical JAK-STAT3 pathway and identifies potential therapeutic targets for implantation failure.
Figure 1: Core Signaling Pathway in Mouse Embryo Implantation. The LIF-LIFR/GP130-JAK-STAT3 axis is essential for implantation, with recent findings identifying ERBB2 as a key downstream effector [9] [3].
Embryo-Derived Signals in Maternal Recognition
The developing embryo actively participates in the implantation dialogue through secretion of signaling molecules. Chorionic gonadotropin (CG) represents one of the major embryonic signals in primates, modulating the uterine environment to promote receptivity [77]. In mice, embryonic signals interact with uterine epithelial and stromal cells to facilitate attachment and decidualization.
Extracellular vesicles (EVs) have emerged as crucial mediators of embryo-endometrial communication. These membrane-bound nanoparticles transfer bioactive molecules—including proteins, lipids, and nucleic acids—between embryonic and maternal tissues, reprogramming cellular functions to support implantation [78]. EVs contribute to immune modulation and tissue remodeling essential for successful nidation.
Experimental Models and Methodologies
Animal Models for Implantation Research
Genetically engineered mouse models have been instrumental in elucidating implantation mechanisms. Uterine epithelium-specific conditional knockout mice for critical implantation genes (Lifr eKO, Gp130 eKO, Stat3 eKO) consistently demonstrate complete infertility due to implantation failure, establishing the non-redundant functions of these factors [3]. These models enable precise dissection of molecular pathways in specific uterine compartments.
The delayed implantation (DI) model provides a valuable experimental system for investigating molecular mechanisms underlying embryo implantation. This model achieves implantation arrest through ovariectomy performed prior to the E2 surge on D4, with delayed implantation maintained via continuous progesterone supplementation [9]. Administration of implantation-inducing factors (LIF, CT-1, or RO8191) then synchronously activates implantation, enabling study of the initial events in this process [9].
Figure 2: Delayed Implantation Model Workflow. This experimental model enables synchronized study of implantation initiation by maintaining blastocysts in diapause until administration of activating signals [9].
Screening Approaches for Novel Factors
High-throughput screening methods have identified previously unrecognized regulators of embryonic development. A novel screening system combining ultra-superovulation technology with one-cell stage embryo cryopreservation in mice enabled evaluation of 95 inhibitors, identifying 16 factors essential for development of fertilized eggs [10]. Among these, a p53 activator (PRIMA-1), cathepsin D, CXCR2, and potassium channels (SK2 and SK3) were validated as novel regulators affecting various developmental stages [10].
Table 3: Essential Research Reagent Solutions for Implantation Studies
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| Inhibitor Libraries | SCADS Inhibitor Kit II & III | High-throughput screening for embryonic development factors | Identified novel regulators (cathepsin D, CXCR2, SK2/SK3 channels) [10] |
| STAT3 Activators | RO8191 | Mechanistic studies in delayed implantation models | Confirmed STAT3 sufficiency for inducing implantation [9] |
| Recombinant Cytokines | LIF, CT-1 | Rescue experiments in knockout models | Established LIF as critical implantation factor [9] [3] |
| ERBB2 Inhibitors | Tucatinib, Sapitinib | Pathway dissection in Lifr eKO models | Identified ERBB2 as essential downstream effector [3] |
| Genetically Engineered Mice | Lifr eKO, Gp130 eKO, Stat3 eKO | Tissue-specific gene function analysis | Demonstrated complete implantation failure with uterine epithelium-specific deletions [3] |
Implications for Reproductive Medicine and Future Directions
Translational Applications
Understanding embryo-endometrial synchronization has direct implications for addressing recurrent implantation failure (RIF), defined as the failure to achieve pregnancy after transfer of at least 3 good-quality embryos [76]. The discovery that RO8191 can induce embryo implantation and decidualization by activating STAT3 signaling, even in uterine epithelial-specific Lifr conditional knockout mice, suggests potential therapeutic applications for treating RIF [9].
The development of predictive models for implantation success represents another promising application. A LASSO regression-based model incorporating differentially expressed genes (Lyz2, Cd36, Cfb, and Cyp17a1) shows potential for predicting implantation outcomes based on blastocyst transcriptional profiles [7]. Such models could enhance embryo selection in assisted reproductive technologies.
Unresolved Questions and Research Opportunities
While significant progress has been made in elucidating implantation mechanisms, numerous questions remain. The biological implications of assisted reproductive technologies on embryonic development require further investigation. Recent studies in mice suggest that IVF-conceived pups have about 30% more new single-nucleotide variants compared to naturally conceived pups, highlighting the need to understand how fertility treatments affect embryonic genetics [28].
The distinct roles of GP130 and LIFR in endometrial signaling represent another area for exploration. Although they function as heterodimeric receptors, their different expression patterns in the endometrium during implantation suggest potential functional specializations that warrant further investigation [3]. Additionally, the application of novel in vitro models, including advanced co-culture systems and organoids, will enhance our understanding of human-specific implantation mechanisms while addressing ethical constraints associated with in vivo research [78].
The synchronization of embryo development with endometrial receptivity through precise molecular dialogue constitutes the fundamental basis for successful implantation. Core signaling pathways, particularly the LIF-LIFR/GP130-STAT3 axis with its newly identified downstream effector ERBB2, coordinate this complex process alongside embryonic signals and immune adaptations. Advanced experimental models, including conditional knockout mice, delayed implantation systems, and high-throughput screening approaches, continue to unravel the intricacies of this relationship. As research progresses, the translation of these findings into clinical applications holds promise for addressing recurrent implantation failure and improving outcomes in assisted reproductive technologies. The continued integration of basic mechanistic studies with technological innovations will undoubtedly enhance our ability to modulate the embryo-endometrial dialogue for successful nidation.
Cutting-Edge Tools for Assessing and Predicting Embryo Quality
The selection of high-quality embryos is paramount for enhancing implantation rates in in vitro fertilization (IVF). This technical guide explores the application of time-lapse Optical Coherence Microscopy (OCM) as a novel, non-invasive method for the three-dimensional evaluation of mouse embryo quality. Positioned within the broader research on factors affecting mouse embryo implantation success rates, we detail how OCM provides label-free, high-resolution imaging of developmental dynamics. The content includes comprehensive experimental protocols, quantitative data on developmental kinetics, and visualization of key workflows, offering researchers and scientists a robust framework for integrating this technology into developmental biology and reproductive medicine research.
Infertility affects a significant portion of the global population, and in vitro fertilization (IVF) remains a primary assisted reproductive technology (ART). A critical challenge in IVF is the selection of embryos with the highest reproductive potential to improve success rates. In mouse models, which exhibit genetic and developmental similarity to humans, live birth rates for embryos generated by IVF are significantly lower compared to those generated in vivo (predicted likelihood of 44.7% for in vivo versus 14.7% for IVF) [80]. Furthermore, suboptimal culture conditions can exacerbate this disparity, highlighting the need for advanced, non-invasive evaluation methods [80].
Traditional embryo selection methods, such as morphological evaluation and preimplantation genetic testing (PGT), have limitations. Morphological assessment is subjective and provides only static snapshots, while PGT is invasive and may affect IVF outcomes [81]. Time-lapse imaging has emerged as a powerful alternative, allowing continuous monitoring of development. However, many systems are limited to two-dimensional imaging [81].
Optical Coherence Microscopy (OCM) combines the principles of optical coherence tomography and confocal microscopy to provide volumetric, high-resolution imaging without the need for labels or contrast agents [81]. This guide details the implementation of time-lapse OCM for evaluating mouse embryo quality, providing in-depth technical protocols and data analysis methods relevant to researchers investigating the factors influencing implantation success.
Technical Foundations of OCM
Optical Coherence Microscopy is a label-free imaging modality that provides three-dimensional, high-resolution images of developing embryos. Its key technical attributes include:
- Principle: OCM utilizes a broadband superluminescent diode and a high numerical aperture objective lens to achieve micron-level resolutions. In a typical setup for embryo imaging, it can achieve an axial resolution of ~2.1 μm and a lateral resolution of ~1.0 μm in tissue [81].
- Non-invasiveness: As a label-free technique, OCM avoids potential phototoxicity or biochemical disruption associated with fluorescent dyes or stains, making it ideal for longitudinal studies on live embryos [81].
- Volumetric Data: Unlike conventional 2D bright-field imaging, OCM captures entire 3D structural information at each time point, enabling the visualization of internal microstructures such as nuclei, cell boundaries, and the initiation of cavitation [81].
Experimental Methodology & Protocol
Integrated Imaging System Design
To enable longitudinal imaging while maintaining optimal embryo health, a custom dual-modality imaging system that fits inside a standard incubator is required.
- Imaging Platform: A compact OCM system integrated with a bright-field (BF) microscope. The entire setup must be housed within an incubator (e.g., Heracell VIOS 160i) to maintain critical culture conditions: 5% O₂, 6% CO₂, constant temperature (37°C), and relative humidity [81].
- Culture Vessel: Use a commercial embryo imaging dish (e.g., IVF store V005001) capable of holding up to 25 embryos for high-throughput data acquisition [81].
- Automation: A 3-axis motorized sample stage is incorporated for efficient and precise movement between embryo wells. An automated acquisition pipeline is implemented, using prior knowledge of well locations followed by image-guided auto-tracking and auto-focusing to center each embryo [81].
Image Acquisition Protocol
The following protocol details the steps for time-lapse imaging of mouse embryos from the one-cell stage to the fully hatched blastocyst.
- Embryo Preparation: Collect one-cell mouse zygotes and place them in the pre-equilibrated culture medium under oil in the imaging dish.
- System Initialization: Place the imaging dish inside the customized sample arm within the incubator. Allow the system to stabilize to ensure temperature and gas equilibrium.
- Time-lapse Programming: Set the acquisition software to capture co-registered 3D OCM and BF images at intervals of approximately 10 minutes for a total duration of over 150 hours [81]. This frequency is sufficient to capture key mitotic events and morphological changes.
- Automated Imaging: Initiate the automated pipeline. For each embryo position, the system will:
- Move the stage to the well's pre-defined coordinates.
- Perform auto-focusing and auto-tracking to center the embryo.
- Acquire a 3D OCM stack and a co-registered BF image.
- Proceed to the next well until all embryos are imaged.
- Data Handling: Transfer the large-volume time-lapse data to a dedicated storage server for subsequent analysis. Data typically requires several terabytes of storage capacity per experimental run.
The workflow below summarizes the key stages of the experimental process:
Research Reagent Solutions and Essential Materials
The following table catalogs the key materials and reagents essential for implementing the described time-lapse OCM experiments.
Table 1: Essential Research Materials and Reagents for Time-Lapse OCM Embryo Evaluation
| Item Name | Function/Application | Specifications/Notes |
|---|---|---|
| Mouse Zygotes | Biological model for development | Exhibit genetic and developmental similarity to humans [81]. |
| Culture Medium | Supports embryo development in vitro | Formulations like HTF may yield superior development rates compared to others like Tyrode's [24]. |
| Embryo Imaging Dish | Vessel for culture and imaging | Holds up to 25 embryos; compatible with motorized stage (e.g., IVF store V005001) [81]. |
| OCM/BF Imaging System | Core imaging apparatus | Custom-built system with SLD light source, 20X objective, fits inside incubator [81]. |
| Motorized 3-Axis Stage | Precise positioning for high-throughput | Enables automated movement between multiple embryo wells [81]. |
| Incubator | Maintains physiological culture conditions | Controls temperature, COâ‚‚ (6%), and Oâ‚‚ (5%) levels [81]. |
Key Findings and Quantitative Data
Time-lapse OCM provides rich, quantitative data on embryonic development, revealing structural features and kinetic parameters predictive of blastocyst formation and quality.
Visualization of 3D Microstructures Across Developmental Stages
OCM surpasses traditional BF imaging by revealing critical internal structures without invasion.
- Early Cleavage Stages (1-cell to 8-cell): OCM provides clear visualization of nuclei, including their size and location, allowing accurate identification of cleavage events and quantification of symmetry. Cell boundaries and the thickness and uniformity of the zona pellucida are also clearly resolved in 3D [81].
- Compaction and Morula Stage: As cells become densely packed, boundaries become less distinct. OCM imaging can still provide volumetric data on the overall morphology during this key transitional phase [81].
- Blastocyst Stage: OCM enables detailed characterization of blastocoel cavity formation, the emerging inner cell mass (ICM), and the trophectoderm (TE). It can reveal the initiation of cavitation as separate chambers, a feature not easily identifiable in BF images. Furthermore, OCM allows for accurate grading of blastocysts according to established systems like the Gardner grading system (stages 1-6) based on expansion, ICM quality, and TE coherence [81].
Correlation of Early Kinetic Parameters with Blastocyst Outcomes
The time-lapse capability of OCM facilitates morphokinetic analysis, identifying early biomarkers of developmental potential.
- Critical Cell Cycles: Research indicates that the timing of the second (t2) and third (t3) embryonic cell cycles is significantly associated with subsequent blastocyst formation and the embryo's hatching capability [81] [82].
- Predictive Potential: Deviations from normal time intervals for these early divisions can serve as non-invasive indicators of reduced developmental competence, allowing for earlier and more objective embryo selection.
The following diagram illustrates the key developmental milestones and structural features that can be quantified using OCM:
Quantitative Data from OCM Studies
The table below summarizes key quantitative findings from OCM-based embryo evaluation studies.
Table 2: Quantitative OCM Imaging Data and Correlations with Embryo Quality
| Parameter Category | Specific Measurement | Correlation with Embryo Outcome |
|---|---|---|
| Developmental Kinetics | Timing of 2nd (t2) and 3rd (t3) cell cycles | Associated with blastocyst formation and hatching capability [81]. |
| Blastocyst Grading | Expansion grade (1-6) according to Gardner system | Direct measure of embryo quality and developmental progress [81]. |
| Zona Pellucida | Thickness and uniformity | Indicator of embryo health; thins naturally during expansion [81]. |
| Live Birth Rate (Context) | Predicted likelihood for in vivo vs. IVF embryos | In vivo: 44.7%; IVF: 14.7% (highlights need for better selection) [80]. |
Discussion and Future Directions
Time-lapse OCM represents a significant advancement in the non-invasive evaluation of embryo quality. By providing high-resolution, 4D structural data (3D space + time), it enriches our understanding of early embryo development and addresses limitations of traditional selection methods. The technology's ability to correlate early kinetic parameters, like the timing of specific cell cycles, with later developmental outcomes such as blastocyst formation, offers a powerful tool for predicting embryo viability [81].
Within the broader context of factors affecting mouse embryo implantation success, OCM-derived data can be layered with other metrics, such as molecular analyses of spent culture medium or genetic screening data, to build multi-parametric models for embryo selection. This is particularly relevant given the documented lower live birth rates and altered fetal placental development associated with IVF-derived embryos in mouse models [80].
Future developments in this field will likely focus on:
- Integration of Artificial Intelligence (AI): Automating the analysis of large OCM datasets to identify subtle morphological and kinetic patterns beyond human perception.
- Enhanced Throughput and Standardization: Refining system design to allow for faster imaging and easier adoption in clinical and research settings.
- Molecular Contrast: Exploring advanced OCM techniques that can provide functional or molecular information in addition to structural data.
In conclusion, time-lapse OCM holds immense potential to streamline embryo selection within IVF clinics and to serve as a powerful research tool for fundamental studies in developmental biology, ultimately contributing to improved success rates in assisted reproduction.
In the field of assisted reproductive technologies (ART), selecting the embryo with the highest developmental potential is a paramount challenge [83]. Morphokinetic analysis, enabled by time-lapse monitoring (TLM) systems, provides a non-invasive method to dynamically observe and quantify the exact timing of early embryonic cell divisions [83] [84]. Research in both human and mouse models has established a clear correlation between specific early developmental timings and subsequent success in reaching the blastocyst stage and undergoing hatching, a prerequisite for implantation [83] [10]. This technical guide synthesizes current research to outline the key morphokinetic parameters predictive of developmental success, provides detailed experimental protocols for their analysis, and integrates these findings into the broader context of factors influencing mouse embryo implantation rates.
Core Morphokinetic Parameters and Their Predictive Value
Morphokinetics involves the precise measurement of the timing of key cell cycle events in the early embryo. The most commonly analyzed parameters and their correlations with blastocyst development are summarized below.
Table 1: Key Morphokinetic Parameters and Their Definitions
| Parameter | Abbreviation | Description |
|---|---|---|
| Pronucleus Appearance | tPNa | Time of pronuclei appearance [84] |
| Time to 2-Cell | t2 | Time from fertilization to the 2-cell stage [84] |
| Time to 3-Cell | t3 | Time from fertilization to the 3-cell stage [84] |
| Time to 4-Cell | t4 | Time from fertilization to the 4-cell stage [84] |
| Time to 5-Cell | t5 | Time from fertilization to the 5-cell stage [84] |
| Second Cell Cycle | CC2 | Duration of the 2-cell stage (t3 - t2) [83] [84] |
| Time to 8-Cell | t8 | Time from fertilization to the 8-cell stage [83] |
| Time to Morula | tM | Time from fertilization to the morula stage [83] |
| Time to Start of Blastulation | tSB | Time from fertilization to the start of blastulation [83] |
| Time to Blastocyst | tB | Time from fertilization to the full blastocyst stage [83] |
Quantitative analyses reveal that embryos developing into high-quality blastocysts often exhibit a distinct morphokinetic signature. A study on 1011 human blastocysts found that shorter morphokinetic parameters (tPNa, t2, t3, t4, t5, t8, tM, tSB, tB) were generally associated with high-quality blastocysts, whereas a significantly prolonged CC2 time was also observed in this group [83]. Furthermore, late morphokinetic parameters (tM, tSB, tB) were identified as independent risk factors influencing blastocyst quality [83]. In a separate prospective study, the timing of pronucleus appearance (tPNa) emerged as a potential modulator of subsequent developmental events [84].
Table 2: Morphokinetic Parameters as Predictors of Developmental Outcomes
| Predictive For | Key Morphokinetic Parameters | Observed Correlation |
|---|---|---|
| Blastocyst Quality | tM, tSB, tB, CC2 [83] | Shorter tM, tSB, tB and prolonged CC2 are independent factors for high-quality blastocyst formation. |
| Chromosomal Ploidy (Euploidy) | tPNa, S3, tSC, tM, tSB, tB, CC2 [83] | Aneuploid embryos show significant extensions in tPNa, S3, tSC, tM, tSB, tB and a reduced CC2. |
| Clinical Pregnancy | S3, t8, tPB2 [83] | S3 (< 12.01 h), t8 (< 62.48 h), and tPB2 (< 3.36 h) are potential predictors of successful clinical pregnancy. |
| Blastocyst Formation | tPNa, t2, t3, t4, t5, CC2, S2 [84] | Significant differences exist in these parameters between blastocyst-forming and arrested embryos. |
Experimental Protocols for Morphokinetic Analysis
Embryo Culture and Time-Lapse Monitoring (TLM)
A standardized protocol for TLM, as used in human clinical studies, is outlined below [83]:
- Fertilization & Culture: Perform ICSI and culture fertilized zygotes (with 2 pronuclei, 2PN) in a specialized 12-well culture dish (e.g., EmbryoSlide) with G-1 Plus medium until day 3 (D3).
- Medium Change: On D3, transfer embryos to a new dish containing G-2 Plus medium for culture until day 5 (D5) or day 6 (D6).
- Incubation & Imaging: Culture all embryos in a time-lapse incubator (e.g., EmbryoScope) under stable conditions (37°C, 6% CO2, 5% O2). The system automatically captures images at frequent intervals.
- Blastocyst Grading: Grade resulting blastocysts according to the Gardner grading system. Blastocysts of stage 3 or higher are classified as AA, AB, or BB (high-quality) or AC, BC, etc. (low-quality) based on inner cell mass (ICM) and trophectoderm (TE) cells [83].
Screening for Developmental Regulators Using Inhibitor Libraries
A novel screening protocol in mice combines ultra-superovulation with cryopreservation to efficiently identify factors essential for early development [10]:
- Embryo Preparation: Induce ultra-superovulation in 4-week-old C57BL/6N female mice using HyperOva and hCG. Collect oocytes and fertilize them in vitro in HTF medium. Cryopreserve the resulting one-cell stage embryos in a solution containing 1M DMSO and DAP213 [10].
- Inhibitor Screening:
- Thaw cryopreserved one-cell embryos and culture in KSOM medium.
- For each treatment group, culture 20 embryos in KSOM medium supplemented with a single inhibitor from a standardized library (e.g., SCADS Inhibitor Kit) at a final concentration of 1µM.
- Include a control group with no inhibitor. Each group should be independently replicated three times (n=3) [10].
- Developmental Assessment: Calculate the developmental rate for each group by dividing the number of embryos that develop to the target stage (e.g., blastocyst) by the total number of embryos used, multiplied by 100. Compare rates between treatment and control groups to identify inhibitors that significantly arrest development [10].
- Validation: Validate positive hits from the screen using genetic approaches, such as CRISPR-Cas9 mediated knockout of the target gene (e.g., Ctsd or Cxcr2), to confirm the arrest of embryonic development [10].
Visualizing the Role of Morphokinetics and Key Regulators
The following diagram illustrates the integrated workflow of morphokinetic analysis and the key molecular regulators of early embryonic development identified through functional screening.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Morphokinetic Studies
| Item | Function / Application | Example / Specification |
|---|---|---|
| Time-Lapse Incubator | Enables continuous culture and imaging of embryos without removing them from stable culture conditions. | EmbryoScope (Vitrolife) [83] |
| Specialized Culture Media | Sequential media designed to support the changing metabolic needs of the preimplantation embryo. | G-IVF Plus, G-1 Plus, G-2 Plus (Vitrolife) [83] |
| Inhibitor Libraries | Systematic tool for screening and identifying novel factors involved in embryonic development. | SCADS Inhibitor Kit II & III [10] |
| KSOM Medium | A common, defined medium used for the culture of preimplantation mouse embryos. | ARK Resources [10] |
| HyperOva | Hormone treatment for inducing ultra-superovulation in mice, yielding a high number of oocytes. | KYUDO CO., Ltd. [10] |
| Cryopreservation Solutions | Allows for the banking and batch use of one-cell stage embryos, standardizing experimental conditions. | Solutions with 1M DMSO and DAP213 [10] |
Embryo implantation is a critical determinant of pregnancy success in both natural conception and assisted reproductive technologies (ART). In mammalian embryonic development, blastocyst hatching from the zona pellucida is essential for normal implantation and subsequent fetal development [7]. Despite advances in reproductive medicine, success rates for ART have plateaued at approximately 30%, presenting a considerable challenge for couples facing infertility [85]. The ability to predict implantation success remains a significant hurdle in clinical practice.
Recent research has revealed that blastocyst hatching exhibits site preferences that strongly correlate with pregnancy outcomes [7]. In mouse models, embryos hatching from specific sites (B-site, 3 o'clock position) demonstrated significantly higher birth rates (65.6%) compared to those hatching from other sites (C-site, 4-5 o'clock position; 21.3%) [7]. This discovery highlights the substantial impact of preimplantation embryonic development on implantation efficiency.
The emergence of transcriptomic analytics has enabled researchers to identify differentially expressed genes (DEGs) that serve as molecular biomarkers for implantation potential. This technical guide explores the development and implementation of LASSO regression models utilizing key DEGs to forecast embryo implantation success, providing researchers with a framework for reproducible experimental design and analysis.
Molecular Basis of Embryo Implantation
Blastocyst Hatching and Site-Specific Gene Expression
Blastocyst hatching involves complex molecular coordination between the developing embryo and maternal environment. Research using mouse models has demonstrated that the location where the blastocyst hatches from the zona pellucida significantly influences implantation success through distinct transcriptomic profiles [7].
Principal component and hierarchical cluster analyses of blastocyst transcriptomes have revealed that gene expression profiles cluster according to hatching site and correlate strongly with fertility outcomes [7]. Blastocysts hatching from sites associated with good fertility (A-site and B-site) cluster closely, while those from poor-outcome sites (C-site) cluster with non-hatching embryos, indicating profound molecular determinants of implantation success.
Critical Signaling Pathways in Implantation
Successful embryo implantation requires precisely coordinated signaling pathways that mediate maternal-fetal crosstalk. The leukemia inhibitory factor (LIF) receptor-STAT3 signaling axis has been identified as essential for initiating implantation in mice [9] [3]. Activation of this pathway triggers downstream events necessary for embryo adhesion and decidualization.
Recent studies have identified RO8191, a compound that activates STAT3 signaling, as capable of inducing embryo implantation in delayed implantation mouse models [9]. This discovery confirms the central role of STAT3 activation in the implantation process and highlights potential therapeutic applications for addressing implantation failure.
Table 1: Key Signaling Pathways in Embryo Implantation
| Pathway | Key Components | Biological Function | Experimental Evidence |
|---|---|---|---|
| JAK/STAT3 Signaling | LIF, LIFR, GP130, STAT3 | Embryo adhesion, decidualization | Uterine epithelial-specific knockout mice show complete infertility [9] [3] |
| Immune-Related Pathways | C3, IL-1β, Lyz2, Cd36 | Maternal-fetal immune tolerance, blastocyst hatching | Immunofluorescence shows C3 and IL-1β on trophectoderm surface [7] |
| ERBB2 Signaling | ERBB2, c-Fos | Epithelial remodeling, implantation competence | Hub gene analysis identifies ERBB2 as key regulator [3] |
Biomarker Discovery and LASSO Regression Modeling
Identification of Differentially Expressed Genes
Transcriptomic analysis of mouse blastocysts with different hatching outcomes has identified 178 differentially expressed genes (DEGs) between blastocysts hatching from high-success (B-site) versus low-success (C-site) locations [7]. These DEGs are predominantly involved in immune processes and show positive correlation with birth rates.
Among these DEGs, immune-related genes including Ptgs1, Lyz2, Il-α, Cfb (upregulated) and Cd36 (downregulated) undergo significant regulation during blastocyst hatching [7]. Transcription factors TCF24 and DLX3 primarily regulate these DEGs, establishing a molecular framework that determines implantation competence.
Table 2: Key Biomarker Genes for Predicting Implantation Success
| Gene Symbol | Expression Pattern | Biological Function | Regulatory Transcription Factors |
|---|---|---|---|
| Lyz2 | Upregulated | Innate immunity, bacterial cell wall degradation | TCF24, DLX3 |
| Cd36 | Downregulated | Fatty acid transport, immune signaling | TCF24, DLX3 |
| Cfb | Upregulated | Complement factor B, alternative complement pathway | TCF24, DLX3 |
| Cyp17a1 | Regulation confirmed | Steroid hormone synthesis | Not specified |
| Ptgs1 | Upregulated | Prostaglandin synthesis, inflammation | TCF24, DLX3 |
| Il-α | Upregulated | Pro-inflammatory cytokine | TCF24, DLX3 |
LASSO Regression Model Development
The LASSO (Least Absolute Shrinkage and Selection Operator) regression approach has been successfully applied to develop a predictive model for blastocyst implantation success [7]. This method is particularly suited for high-dimensional biological data where the number of potential predictors (genes) may exceed the number of observations.
The model was constructed using validated DEGs as variables, with a nomogram graph developed based on LASSO regression and cross-validation data [7]. The final model incorporated four key genes: Lyz2, Cd36, Cfb, and Cyp17a1, which collectively provide strong predictive power for implantation outcomes.
Experimental Protocols and Methodologies
Embryo Collection and Culture
Animal Models and Ethics: All procedures should be approved by the institutional animal care and use committee. Female CD-1 mice (6-8 weeks old) and male CD-1 mice (8-9 weeks old) are commonly used [7]. Mice should be housed in specific pathogen-free facilities under standard 12-h light/12-h dark cycles with free access to food and water.
Superovulation and Embryo Collection:
- Treat female mice with pregnant mare serum gonadotropin (PMSG) and human chorionic gonadotropin (hCG) to induce superovulation [7]
- Mate with male mice and check for copulatory plugs next morning (designated as 0.5 days post-coitus, dpc)
- Recover uterus with Fallopian tube at 3.5 dpc
- Flush expanding blastocysts from uterus using 200 μL of M2 medium
- Collect embryos and culture in KSOM medium under mineral oil
Hatching Classification: After 6-8 hours of culture, classify blastocyst hatching based on site relative to ICM position [7]:
- A-site: 1-2 o'clock position (55.6% birth rate)
- B-site: 3 o'clock position (65.6% birth rate)
- C-site: 4-5 o'clock position (21.3% birth rate) After 16 hours of culture, divide blastocysts into hatched (H) and hatching failure (N) groups.
Transcriptomic Analysis
RNA Extraction and Sequencing:
- Extract total RNA from embryo pools (10 embryos per group) using TRIzol method [7]
- Perform RNA sequencing using Smart-Seq protocol for high-resolution transcriptome analysis
- Include these experimental groups: expanding (E), A-site hatching (A), B-site hatching (B), C-site hatching (C), hatched (H), and non-hatching (N)
Differential Expression Analysis:
- Identify differentially expressed genes (DEGs) using standardized bioinformatics pipelines
- Set significance thresholds (e.g., fold change > 2, adjusted p-value < 0.05)
- Perform functional enrichment analysis (GO, KEGG) to identify biological processes
Single Blastocyst RT-qPCR Validation:
- Lyse individual embryos in 5 μL scaled-down reaction solution on a plastic dish covered with mineral oil [7]
- Synthesize cDNA using All-In-One 5× RT MasterMix with modified reaction volumes
- Perform qPCR analysis for key genes (Lyz2, Cd36, Cfb, Cyp17a1)
- Use appropriate housekeeping genes for normalization
Figure 1: Experimental workflow for LASSO regression model development
Immunofluorescence Staining
Protocol for Protein Localization:
- Fix embryos in 4% paraformaldehyde solution
- Permeabilize with 0.1-0.5% Triton X-100
- Block with appropriate serum (e.g., 5% BSA or normal serum)
- Incubate with primary antibodies:
- Anti-C3 for complement component detection
- Anti-IL-1β for cytokine localization
- Anti-Cdx2 for trophoblast differentiation marker
- Anti-Plac1 for placental development marker
- Incubate with fluorophore-conjugated secondary antibodies
- Counterstain with DAPI for nuclear visualization
- Image using confocal or fluorescence microscopy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Implantation Success Studies
| Reagent/Category | Specific Examples | Function/Application | Supplier Examples |
|---|---|---|---|
| Embryo Culture Media | KSOM medium, M2 medium, HTF medium | In vitro embryo culture and manipulation | Sigma-Aldrich, ARK Resources |
| Superovulation Agents | PMSG, hCG | Induce superovulation for embryo collection | Sigma-Aldrich |
| RNA Sequencing Kits | Smart-Seq reagents | High-resolution transcriptome analysis of embryos | Applied Biological Materials Inc (abm) |
| Reverse Transcription & qPCR | All-In-One 5× RT MasterMix | cDNA synthesis and gene expression validation | Applied Biological Materials Inc (abm) |
| Primary Antibodies | Anti-C3, Anti-IL-1β, Anti-Cdx2, Anti-Plac1 | Protein localization via immunofluorescence | Proteintech Group Inc |
| STAT3 Pathway Activators | RO8191 | Induce embryo implantation in delayed models | TargetMol, Sigma-Aldrich |
| ERBB2 Inhibitors | Tucatinib, Sapitinib | Investigate LIFR-ERBB2 signaling pathway | TargetMol, Selleck Chemicals |
Biological Mechanisms and Pathway Integration
The DEGs identified in implantation competence represent interconnected biological systems that collectively determine implantation success. The immune-related genes (Lyz2, Cfb, Il-α) play crucial roles in establishing appropriate immune tolerance at the maternal-fetal interface [7]. Simultaneously, metabolic regulators like Cd36 facilitate essential nutrient transport supporting early embryonic development.
Recent research has revealed that during blastocyst development from expansion to fully hatched state, 307 DEGs are either upregulated by transcription factor ATOH8 or downregulated by SPIC to activate immune pathways [7]. This sophisticated transcriptional reprogramming prepares the embryo for interaction with the maternal endometrium.
Figure 2: Molecular pathways regulating implantation competence
The transcriptional regulation network involves complex interactions between multiple transcription factors and their target genes. Analysis of hatched versus non-hatched blastocysts reveals three distinct transcription patterns, with failed embryos showing disrupted regulatory networks compared to their successful counterparts [7].
The LIFR-ERBB2 signaling axis has been identified as another essential pathway for successful implantation [3]. Hub gene analysis of uterine epithelium-specific Lifr and Gp130 knockout mice identified Erbb2 and c-Fos as key regulators, suggesting this pathway works in concert with immune-related gene networks to ensure implantation competence.
The development of LASSO regression models using DEG biomarkers represents a significant advancement in predicting embryo implantation potential. The integration of transcriptomic data with machine learning approaches provides a powerful framework for assessing embryonic competence prior to transfer.
Future applications of this methodology may extend to human ART, where current success rates remain suboptimal. The discovery of novel regulators of embryonic development, such as cathepsin D and CXCR2 identified through inhibitor library screening [10], may further enhance our ability to identify critical biomarkers for implantation success.
As research in this field progresses, the refinement of predictive models using larger datasets and additional biomarker classes will continue to improve their clinical utility. This approach holds promise for ultimately increasing success rates in assisted reproduction and addressing the challenge of recurrent implantation failure.
In mammalian reproductive biology and assisted reproductive technologies (ART), the developmental competence of a blastocyst—its ability to hatch, implant, and establish a successful pregnancy—is paramount. This competence is profoundly influenced by the embryo's environment during its early development. The comparison between embryos derived and developed in a natural, in vivo environment and those produced and cultured in an artificial, in vitro setting reveals critical differences in molecular, cellular, and functional characteristics. These differences directly impact the success rates of applications ranging from clinical infertility treatments to transgenic animal production. Understanding the distinct molecular pathways, gene expression profiles, and physiological outcomes associated with each method is not merely an academic exercise; it is essential for diagnosing the limitations of current ART and developing targeted strategies to overcome them, thereby improving embryo quality and pregnancy outcomes. This review synthesizes recent evidence to provide a comparative analysis of the developmental competence of in-vitro and in-vivo derived blastocysts.
Comparative Outcomes: In-Vitro vs. In-Vivo Blastocysts
Morphological and Developmental Rate Disparities
A direct comparative study of mouse embryos revealed significant morphological differences based on their culture environment. Embryos cultured in vitro under 5% Oâ‚‚, as well as those derived in vivo, showed a significantly higher mean percentage of blastocyst development and greater total cell number compared to those cultured under 2% Oâ‚‚. Furthermore, blastocyst expansion was greatest in the group cultured under 5% Oâ‚‚ [36]. This suggests that the oxygen concentration in standard in vitro culture (IVC) systems, if not optimized, can compromise key developmental metrics. Beyond mice, studies in bovine models confirm that in-vitro produced embryos consistently lag behind their in-vivo counterparts in terms of developmental competence, quality, and the viability of the resulting blastocysts [86].
Molecular and Genetic Integrity
The divergence between in-vitro and in-vivo embryos is profoundly evident at the molecular level. A study in mice conceived through ART, including IVF and embryo transfer, showed about 30% more new single-nucleotide variants (tiny DNA sequence changes) compared to naturally conceived pups. Although the vast majority of these mutations are neutral and spread randomly across the genome, this finding indicates that fertility treatments can increase the overall rate of genetic errors. The absolute risk of a harmful mutation, however, remains very low—estimated at one additional problematic change for every 50 IVF-conceived mice [28].
Transcriptomic analyses provide further evidence. A comprehensive study in bovine blastocysts identified 1,052 differentially expressed genes (DEGs) between in-vitro and in-vivo derived groups. Many of these genes are involved in crucial pathways such as:
- Ubiquitin-mediated proteolysis
- Proteasome activity
- Cell cycle regulation [86]
The specific environment during and after oocyte maturation has distinct and lasting effects on the embryonic transcriptome. The in vitro environment following maturation was responsible for altering the expression of 913 genes, while the environment during maturation affected another 109 genes, many involved in cholesterol biosynthesis and lipid metabolism. The origin of the immature oocyte itself predetermines the expression of 28 genes later in the blastocyst, including DLD and PLAC8, which are implicated in implantation success and live birth [86].
Table 1: Key Morphological and Molecular Differences Between In-Vitro and In-Vivo Derived Blastocysts
| Parameter | In-Vivo Derived Blastocysts | In-Vitro Derived Blastocysts | Significance/Consequence |
|---|---|---|---|
| Blastocyst Development Rate | High [36] | Variable; depends on culture conditions (e.g., Oâ‚‚ levels) [36] | Directly impacts the yield of transferable embryos. |
| Total Cell Number | High [36] | Can be reduced, especially in suboptimal Oâ‚‚ [36] | Correlates with embryo viability and developmental potential. |
| Blastocyst Expansion | Normal [36] | Can be impaired [36] | Affects subsequent hatching and implantation potential. |
| DNA Mutation Rate | Baseline level [28] | ~30% higher single-nucleotide variants in mice [28] | Absolute increase in harmful mutations is very low. |
| Transcriptomic Profile | Physiological norm [86] | Altered; >1000 DEGs in bovine vs. in-vivo [86] | Disruption of pathways for protein degradation, cell cycle, and metabolism. |
| Stress Response | Physiological levels | Upregulation of stress-related genes under 2% Oâ‚‚ [36] | Induces cellular stress, potentially reducing viability. |
Underlying Molecular Mechanisms
Stress Responses and Apoptosis
The in vitro environment can induce significant cellular stress in developing embryos. Mouse embryos cultured under a subphysiological 2% Oâ‚‚ tension showed a significant upregulation of stress response genes and significantly lower expression of antioxidant-related genes compared to both in-vivo derived embryos and those cultured under 5% Oâ‚‚. This was coupled with a significant increase in Caspase-3 immunofluorescence, a key marker of apoptosis, in all cultured embryos versus in-vivo derived counterparts [36]. This demonstrates that suboptimal in vitro conditions can compromise embryo quality by activating stress pathways and programmed cell death.
Blastocyst Hatching and Site-Specific Gene Expression
Blastocyst hatching is a critical prelude to implantation, and its mechanism is closely linked to developmental competence. Research in mice has revealed that the site where the blastocyst hatches from its zona pellucida is not random but determines implantation efficiency. Blastocysts hatching from the "B-site" (beside the inner cell mass) achieved a birth rate of 65.6%, whereas those hatching from the "C-site" (opposite the ICM) had a birth rate of only 21.3% [7].
Transcriptomic analysis of these site-specific blastocysts showed that those with good fertility outcomes (A and B-sites) clustered closely together, while those with poor outcomes (C-site and non-hatching) formed a separate cluster. A comparison of B-site vs. C-site blastocysts identified 178 differentially expressed genes, primarily involved in immune function. Key among these were upregulated genes like Ptgs1, Lyz2, Il-α, and Cfb, and the downregulated gene Cd36. These immune-related genes, along with transcription factors TCF24 and DLX3, are crucial for successful maternal-fetal interactions during implantation [7].
Key Signaling Pathways in Implantation
Successful implantation requires precise coordination between an activated blastocyst and a receptive endometrium, mediated by specific signaling pathways.
The LIF-STAT3 Pathway: In mice, the cytokine Leukemia Inhibitory Factor (LIF) is a master regulator of implantation. It is expressed in the endometrial glands and binds to a heterodimeric receptor (LIFR and GP130) on the uterine luminal epithelium, activating the JAK/STAT3 signaling pathway [9] [3]. The critical nature of this pathway is demonstrated by the complete infertility of uterine epithelium-specific Lifr, Gp130, and Stat3 knockout mice, all of which fail at the implantation stage [9] [3]. Recent research using the small molecule RO8191, which acts as a STAT3 activator, was able to induce embryo implantation and decidualization in delayed implantation models and even rescue implantation in uterine epithelial-specific Lifr conditional knockout mice [9].
LIFR-Mediated ERBB2 Signaling: Building on the core LIF pathway, a 2025 study performing a comprehensive gene expression analysis on Lifr and Gp130 conditional knockout mice identified ERBB2 (a receptor tyrosine kinase) and c-Fos as key hub genes downstream of LIFR signaling. Inhibition of ERBB2 signaling disrupted implantation, suggesting that LIFR-ERBB2-mediated signaling is an essential component of the implantation process [3].
Diagram 1: LIF-STAT3 and Related Signaling Pathways in Mouse Embryo Implantation. The diagram shows the core LIF-STAT3 pathway (blue/green) and the more recently identified LIFR-ERBB2 axis (red), highlighting the point of action for the experimental compound RO8191.
Advanced Experimental Models and Screening Methods
Novel Screening for Developmental Factors
To systematically identify novel regulators of preimplantation development, a 2025 study established a high-throughput screening system combining ultra-superovulation with cryopreservation of one-cell stage mouse embryos. This platform enabled the screening of 95 inhibitors, which led to the identification of 16 factors essential for the development of fertilized eggs. These included known factors like various ATPases, as well as novel regulators:
- PRIMA-1 (a p53 activator)
- Cathepsin D (a lysosomal protease)
- CXCR2 (a chemokine receptor)
- SK2/SK3 (potassium channels)
The essential roles of Cathepsin D and CXCR2 were further validated through CRISPR-Cas9 mediated knockout experiments, which resulted in arrested embryonic development [10]. This screening method provides a powerful tool for discovering previously unrecognized modulators of embryonic development.
Diagram 2: Workflow for High-Throughput Screening of Embryonic Developmental Factors. The process involves generating large numbers of synchronized embryos, screening them against a library of chemical inhibitors, and validating hits with genome editing.
3D Embryoid Models for Toxicity Testing
Beyond traditional 2D cultures, advanced models like 3D mouse embryoids are being developed to better mimic the peri-implantation stage. These models, such as those combining embryonic stem cells (ESCs), trophoblast stem cells (TSCs), and extra-embryonic endoderm stem cells (XENCs) into ETX embryoids, provide a more physiologically relevant system for studying developmental and reproductive toxicity (DART) [87]. They offer a promising alternative to animal models for screening potential embryolethal compounds.
The Scientist's Toolkit: Key Reagents and Experimental Models
Table 2: Essential Research Tools for Studying Blastocyst Competence and Implantation
| Reagent / Model | Function / Application | Key Findings Enabled |
|---|---|---|
| RO8191 [9] | Small-molecule activator of STAT3 signaling. | Induced implantation in delayed and Lifr cKO models;è¯æ˜Žäº†STAT3 activation can be sufficient for implantation. |
| SCADS Inhibitor Kits [10] | Standardized libraries of low molecular-weight inhibitors for high-throughput screening. | Identified novel developmental regulators (Cathepsin D, CXCR2, SK2/SK3 channels). |
| Conditional Knockout Mice (Lifr, Gp130, Stat3) [9] [3] | Enables tissue-specific (e.g., uterine epithelium) gene deletion to study gene function in implantation. | Established LIFR/GP130/STAT3 axis as non-redundant for embryo implantation; revealed role of LIFR-ERBB2 signaling. |
| Delayed Implantation (DI) Model [9] | Surgical and hormonal manipulation to pause embryo development, allowing study of implantation triggers. | Used to test the efficacy of implantation-inducing agents like RO8191 and recombinant LIF/CT-1. |
| 3D Mouse Embryoids (ETX) [87] | In vitro stem cell-based models of the peri-implantation embryo. | Provides an alternative model for embryolethality testing during the peri-implantation stage. |
The divergence in developmental competence between in-vitro and in-vivo derived blastocysts is a multi-faceted phenomenon, rooted in distinct morphological, genetic, and molecular landscapes. In-vitro conditions, if not meticulously optimized, can induce cellular stress, alter the transcriptome of key metabolic and regulatory pathways, and even slightly increase genetic mutation rates. The critical processes of blastocyst hatching and implantation are governed by precise molecular dialogues, such as the LIF-STAT3 pathway and site-specific immune-related gene expression, which are often suboptimal in IVP embryos. The ongoing development of sophisticated tools—from high-throughput screening of developmental regulators and specific pathway agonists like RO8191 to advanced 3D embryoid models—provides a powerful arsenal for deconstructing these complex processes. The insights gained are fundamental for refining ART protocols, not merely to increase blastocyst yield, but to ensure that in-vitro derived embryos possess the molecular and functional competence of their in-vivo counterparts, thereby ultimately improving success rates in both clinical and research applications.
The selection of viable embryos with the highest implantation potential remains a significant challenge in assisted reproductive technology (ART). Current methods primarily rely on morphological grading, a subjective approach with limited predictive value [88]. The quest for more objective, reliable biomarkers capable of predicting an embryo's potential to implant and lead to a healthy live birth represents a critical frontier in reproductive medicine, particularly within the context of mouse embryo implantation success rates research.
Embryo development is intricately linked to its microenvironment. In vivo, the embryo's progression involves dynamic changes in its surroundings and continuous interactions with maternal tissues that support and regulate development. In contrast, in vitro conditions depend on a stationary, low-viscosity culture medium that lacks these maternal contributions [88]. This discrepancy underscores the importance of understanding both embryonic and maternal factors that influence implantation success. Analyzing the biochemical dialogue between the embryo and its environment offers promising avenues for identifying robust biomarkers that correlate with functional outcomes like implantation and live birth.
Biomarker Discovery Approaches
Spent Culture Media (SCM) Metabolomics
Spent culture media (SCM) analysis offers a promising, non-invasive strategy for assessing embryo viability and implantation potential. By profiling the consumption and secretion of low molecular weight metabolites, SCM analysis provides valuable insights into embryonic metabolic activity and developmental competence [88]. A recent Bayesian meta-analysis synthesized quantitative evidence from studies reporting metabolite concentrations in SCM in relation to IVF outcomes, identifying specific metabolic patterns associated with success.
Key Metabolites Identified in SCM Analysis:
| Metabolite Category | Specific Metabolites | Association with Favorable Outcome | Proposed Biological Role |
|---|---|---|---|
| Amino Acids | Glutamine, Aspartate | Positive [88] | Energy metabolism, cellular signaling |
| Amino Acids | Taurine, Glycine, Alanine | Positive (as osmolytes) [88] | Osmolytes, antioxidants, metabolic precursors |
| Energy Substrates | Pyruvate | Positive (early cleavage) [88] | Primary energy source during initial cleavage |
| Energy Substrates | Glucose | Positive (post-cleavage) [88] | Increased uptake supports higher energy demands |
| Energy Substrates | Lactate | Positive (blastocyst stage) [88] | May support implantation processes |
The table above summarizes key metabolites whose concentrations in SCM have been correlated with embryo viability. The dynamic nature of metabolic requirements during different embryonic stages is a critical consideration for biomarker interpretation [88].
Maternal Fluid sncRNA Profiling
Beyond the embryo's secretions, the maternal reproductive environment provides a rich source of biomarkers. Uterine fluid (UF) facilitates embryo-maternal communication and supports early embryonic development. Recent studies using advanced sequencing techniques like PANDORA-seq have revealed a diverse repertoire of small non-coding RNAs (sncRNAs) in mouse oviduct and uterine fluids, with tRNA-derived small RNAs (tsRNAs) and rRNA-derived small RNAs (rsRNAs) being predominant [15].
Maternal diet-induced alterations in these sncRNAs can significantly impact embryo development. A high-fat diet (HFD) during the preimplantation period significantly alters tsRNA and rsRNA expression in uterine fluid compared to a normal diet. These alterations can disrupt blastocyst metabolic gene expression, impair mid-gestation embryonic and placental growth, and result in reduced birth weight and metabolic disorders in offspring [15]. The following diagram illustrates the experimental workflow and key findings of this discovery process:
Figure 1: Experimental workflow for identifying uterine fluid sncRNA biomarkers.
Validation Methodologies and Experimental Protocols
Analytical Protocol for SCM Metabolomics
Robust validation of SCM biomarkers requires standardized, reproducible protocols. The following methodology is adapted from studies included in the recent meta-analysis [88]:
Sample Collection and Preparation:
- Culture Conditions: Culture embryos individually in microdroplets of a defined, sequential culture medium under oil.
- SCM Harvesting: Collect spent culture media at specific timepoints (e.g., day 3 for cleavage stage, day 5/6 for blastocyst stage) following embryo transfer or vitrification.
- Control Media: Collect and analyze unused culture media from the same batch as controls.
- Sample Storage: Immediately freeze SCM samples at -80°C to prevent metabolite degradation.
Metabolite Analysis:
- Platform: Utilize targeted analytical platforms such as Liquid Chromatography-Mass Spectrometry (LC-MS) or Nuclear Magnetic Resonance (NMR) spectroscopy. LC-MS is preferred for its sensitivity in detecting low-abundance metabolites.
- Calibration: Quantify absolute metabolite concentrations using calibration curves with internal standards. Studies providing only signal responses (e.g., peak intensities) without proper calibration were excluded from the meta-analysis due to insufficient quantitative rigor [88].
- Data Normalization: Normalize metabolite concentrations against control media and, where possible, to per-embryo values or total protein content to account for variations.
Statistical Analysis and Validation:
- Data Integration: Employ a multilevel modeling approach to integrate data across heterogeneous study designs. A Bayesian framework can handle sparsity and complexity effectively [88].
- Outcome Correlation: Correlate metabolite concentrations with definitive clinical or phenotypic outcomes such as blastocyst formation, euploidy (if available), implantation, or live birth.
Functional Validation of sncRNA Biomarkers
To establish causality and move beyond correlation, functional validation of sncRNA biomarkers is essential. The following protocol, derived from mouse model studies, outlines this process [15]:
In Vivo Model:
- Dietary Intervention: Expose female mice to a high-fat diet (HFD) or normal diet (ND) throughout the first 4 days of pregnancy.
- Fluid Collection: Collect oviduct fluid (OF) from days 1-3 and uterine fluid (UF) on day 4 of pregnancy.
- RNA Extraction: Extract total RNA from OF and UF samples, typically yielding ~100 ng of total RNA per uterus/oviduct.
Functional Assays:
- Embryo Transfection: Transfert early embryos with synthetic sncRNAs (e.g., specific tsRNAs or rsRNAs) that were identified as being altered by maternal HFD.
- In Vitro Development Assessment: Culture transfected embryos and assess rates of blastocyst formation, blastocyst metabolic gene expression via qPCR, and metabolic activity.
- In Vivo Transfer and Phenotyping: Transfer transfected embryos into healthy, non-manipulated surrogate dams. Assess:
- Implantation rates
- Mid-gestation embryonic and placental growth
- Birth weight and offspring length
- Postnatal metabolic health of offspring (e.g., glucose tolerance)
This comprehensive protocol validates not only the biomarker's association but also its functional role in influencing embryonic development and long-term offspring health.
From Correlation to Causation: Functional Validation in Mouse Models
Establishing a correlation between a molecular signature and an outcome is merely the first step. The gold standard in biomarker validation is demonstrating a causal relationship through functional experiments. The following table summarizes key functional validation experiments and their readouts, as applied in mouse models:
Functional Validation Experiments for Implantation Biomarkers:
| Validation Experiment | Experimental Input | Key Readouts & Measurements | Interpretation of Positive Validation |
|---|---|---|---|
| Embryo Transfection [15] | Synthetic sncRNAs (tsRNAs, rsRNAs) | Blastocyst formation rate, metabolic gene expression (qPCR) | Altered sncRNAs recapitulate HFD-induced developmental defects |
| In Vivo Embryo Transfer [15] | Embryos exposed to altered biomarkers | Implantation sites, fetal & placental weight at mid-gestation, live birth metrics | Exposure to biomarker mimics HFD-induced growth restriction |
| Maternal Diet Manipulation [15] | High-Fat Diet (HFD) vs. Normal Diet (ND) | sncRNA profile in UF/OF, offspring birth weight, offspring metabolic health | Maternal environment alters biomarkers, leading to functional deficits |
| SCM Supplementation/Deprivation | Specific metabolites (e.g., glutamine, glucose) | Cleavage kinetics, blastocyst rate, trophectoderm quality | Direct metabolic requirement confirmed; biomarker has functional role |
The data generated from these experiments move the biomarker from a correlative signal to a functional mediator of implantation and developmental success. For instance, transfection of embryos with UF-derived sncRNAs altered by maternal HFD was sufficient to mimic the in vivo effects of the diet, including impaired blastocyst gene expression and subsequent fetal growth restriction [15]. This provides strong evidence for a causal role.
The Scientist's Toolkit: Essential Research Reagents
Successful execution of the described validation protocols requires a suite of specific reagents and tools. The following table details essential components of the research toolkit for biomarker validation in embryo implantation research.
Research Reagent Solutions for Biomarker Validation:
| Reagent / Material | Function / Application | Example / Key Specification |
|---|---|---|
| Defined Culture Media | Supports embryo development in vitro; base for SCM collection | Sequential media formulations (e.g., G1/G2) with stable dipeptides (Ala-Gln) [88] |
| PANDORA-seq Kit | Comprehensive sncRNA profiling from low-input samples | Enables detection of tsRNAs, rsRNAs beyond canonical miRNAs [15] |
| LC-MS/MS System | Targeted quantification of metabolites in SCM | High-sensitivity platform for absolute concentration measurement [88] |
| Synthetic sncRNAs | Functional validation via embryo transfection | Custom-designed tsRNA/rsRNA mimics and inhibitors [15] |
| High-Fat Diet Formulation | Modeling maternal metabolic stress in rodents | Defined fat-content diet (e.g., 60% kcal from fat) for preimplantation exposure [15] |
| Antibody Panels | Immunostaining of embryonic and placental tissues | Targets for key metabolic proteins (e.g., GLUTs) and lineage markers (OCT4, CDX2) |
Integrated Workflow for Biomarker Validation
The journey from biomarker discovery to clinical application is a multi-stage process. The following diagram synthesizes the key steps, methodologies, and decision points into a cohesive validation workflow, integrating the concepts of SCM metabolomics and sncRNA analysis.
Figure 2: Integrated workflow for biomarker validation from discovery to clinical translation.
The validation of biomarkers for implantation and live birth outcomes is progressing beyond simple correlation toward establishing functional, causal relationships. The integration of advanced metabolomics from SCM with deep sncRNA profiling of the maternal microenvironment provides a powerful, multi-omics approach. However, as the meta-analysis on SCM metabolomics highlights, recurring methodological challenges and a lack of standardized protocols have impeded clinical translation [88]. Future research must prioritize rigorous functional validation in model systems, like the mouse studies on uterine fluid sncRNAs [15], and subsequent validation in large-scale, prospective human clinical trials. By adhering to stringent analytical standards and focusing on functional relevance, the field can move closer to the ultimate goal: reliable, non-invasive biomarkers that objectively guide embryo selection and improve live birth rates in clinical ART.
Conclusion
Successful mouse embryo implantation is a multifactorial process governed by precise molecular signaling, optimal embryo quality, and a receptive uterine environment. The LIF-STAT3 pathway is a critical regulator, but its context within a broader network of immune-related genes and blastocyst hatching dynamics is paramount. While mouse models are indispensable, their limitations necessitate cautious extrapolation to human reproduction. Future research should focus on refining in vitro culture systems to better mimic in vivo conditions, developing more sophisticated non-invasive biomarkers for embryo selection, and bridging the gap between mechanistic discoveries in mice and clinical applications in human infertility treatments. The integration of advanced imaging, transcriptomics, and targeted pharmacological interventions holds great promise for significantly improving implantation success rates in both research and clinical settings.
References
- 1. The Role of the Leukemia Inhibitory Factor (LIF) — Pathway in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3924847/]
- 2. Spatiotemporal functions of leukemia inhibitory factor in ... [https://www.nature.com/articles/s41420-024-02228-4]
- 3. LIFR-Mediated ERBB2 Signaling Is Essential for ... [https://www.mdpi.com/2218-273X/15/5/698]
- 4. LIFR-Mediated ERBB2 Signaling Is Essential for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109566/]
- 5. RO8191, a new compound for initiating embryo implantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420812/]
- 6. Effect of blastocyst development on hatching and embryo ... [https://www.sciencedirect.com/science/article/pii/S0093691X23004053]
- 7. Gene expression changes in blastocyst hatching affect ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1496298/full]
- 8. Blastocyst hatching site is regularly distributed and does ... [https://www.nature.com/articles/s41598-020-59424-2]
- 9. RO8191, a new compound for initiating embryo ... [https://www.nature.com/articles/s41598-025-18471-3]
- 10. Screening for novel factors involved in mouse early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575340/]
- 11. Laser-assisted hatching is associated with reduced re ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182662/]
- 12. Embryo-maternal cross-talk: key players in successful ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548195/]
- 13. Epigenetics of maternal-fetal interface immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1549839/full]
- 14. Mother–Fetus Immune Cross-Talk Coordinates “Extrinsicâ€/“ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9604428/]
- 15. Maternal diet-induced alterations in uterine fluid sncRNAs ... [https://www.nature.com/articles/s41467-025-63054-5]
- 16. An ex vivo uterine system captures implantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217791/]
- 17. Stratified analysis of clinical pregnancy outcomes of ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-023-06111-5]
- 18. Crosstalk between Placental Trophoblast and Decidual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10416716/]
- 19. Endocannabinoid signaling in synchronizing embryo ... [https://www.sciencedirect.com/science/article/abs/pii/S0009308402001561]
- 20. Aspects of endocannabinoid signaling in periimplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2435201/]
- 21. Endocannabinoid Signaling in Female Reproduction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3382454/]
- 22. Differential regulation of endocannabinoid synthesis and ... [https://pubmed.ncbi.nlm.nih.gov/17259073/]
- 23. Pregnancy success in mice requires appropriate ... [https://elifesciences.org/articles/61762]
- 24. Culture factors affecting the success rate of in vitro ... [https://pubmed.ncbi.nlm.nih.gov/3860035/]
- 25. Of Mice and (Wo)men: Factors Influencing Successful ... [https://pubmed.ncbi.nlm.nih.gov/24306146/]
- 26. Mouse models of human disease: An evolutionary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4875775/]
- 27. Reproductive tract biology: Of mice and men - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7339118/]
- 28. In mice, fertility treatments linked to higher mutations than ... [https://www.jax.org/news-and-insights/2025/november/in-mice-fertility-treatments-linked-to-higher-mutations-than-natural-conceptions]
- 29. A quantitative method for staging mouse embryos based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5963863/]
- 30. Impact of oxygen tension according to embryo stage ... [https://www.nature.com/articles/s41598-021-01488-9]
- 31. Low oxygen tension promotes invasive ability and embryo ... [https://www.sciencedirect.com/science/article/abs/pii/S1642431X18300275]
- 32. Pre-Implantation Mouse Embryos Cultured In Vitro under ... [https://www.mdpi.com/1660-4601/17/10/3384]
- 33. Effect of oxygen tension and antioxidants on the ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7896883/]
- 34. Embryos from Prepubertal Hyperglycemic Female Mice ... [https://www.mdpi.com/2073-4409/13/11/954]
- 35. Oxygen level alters energy metabolism in bovine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965477/]
- 36. Comparison of the developmental competence of in vitro- ... [https://pubmed.ncbi.nlm.nih.gov/39313714/]
- 37. STAT3 Regulates Uterine Epithelial Remodeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3857199/]
- 38. Differential roles of uterine epithelial and stromal STAT3 ... [https://www.nature.com/articles/s41598-020-72640-0]
- 39. RO8191, a new compound for initiating embryo ... [https://pubmed.ncbi.nlm.nih.gov/40925951/]
- 40. Enhancing embryonic and full-term development during ... [https://pubmed.ncbi.nlm.nih.gov/40367542/]
- 41. Signaling Pathways in Human Blastocyst Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452331/]
- 42. Persistent Wnt signaling affects IVF embryo implantation ... [https://www.sciencedirect.com/science/article/pii/S2095927325004724]
- 43. Molecular and cellular regulators of embryo implantation and their... [https://pubmed.ncbi.nlm.nih.gov/39866379/]
- 44. Uterine receptivity, embryo attachment, and embryo invasion... | CoLab [https://colab.ws/articles/10.1002%2Frmb2.12280]
- 45. Improvement of implantation potential in mouse blastocysts ... [https://pubmed.ncbi.nlm.nih.gov/28810691/]
- 46. 4-Hydroxyestradiol improves mouse embryo quality, ... [https://pubmed.ncbi.nlm.nih.gov/33237288/]
- 47. Understanding IVF Embryo Grading Systems [https://www.arcfertility.com/understanding-embryo-grading/]
- 48. How embryos are graded [https://www.adorafertility.com.au/how-embryos-are-graded/]
- 49. Grading Scales [https://www.asrm.org/asrm-academy/asrm-academy-on-the-go/embryo-data-grading--evaluation/grading-scales/]
- 50. Label-free evaluation of mouse embryo quality using time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12000469/]
- 51. What to do when good-quality embryos repeatedly fail ... [https://www.sciencedirect.com/science/article/abs/pii/S1521693418301627]
- 52. A review of the pathophysiology of recurrent implantation ... [https://www.sciencedirect.com/science/article/pii/S0015028221020525]
- 53. Molecular subtype of recurrent implantation failure reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257665/]
- 54. Personalized embryo transfer guided by rsERT improves ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1369317/full]
- 55. Endometrial immune cell ratios and implantation success ... [https://www.sciencedirect.com/science/article/abs/pii/S0165037823000220]
- 56. Interventions for recurrent embryo implantation failure [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011071/]
- 57. The endometrium during and after ovarian ... [https://pubmed.ncbi.nlm.nih.gov/30770200/]
- 58. Endometrial Receptivity and its Predictive Value for IVF ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4168536/]
- 59. Endometrial receptivity testing for assisted reproductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12216806/]
- 60. Controlled ovarian hyperstimulation reduces mouse ... [https://pubmed.ncbi.nlm.nih.gov/40934816/]
- 61. Bushen Huoxue recipe attenuates early pregnancy loss via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7809844/]
- 62. Establishment of an Embryo Implantation Model In Vitro [https://www.jove.com/t/66873/establishment-of-an-embryo-implantation-model-in-vitro]
- 63. Oxidative Stress and Assisted Reproduction - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8944628/]
- 64. Antioxidants as alleviating agents of in-vitro embryo ... [https://www.e-jarb.org/journal/view.html?doi=10.12750/JARB.38.2.47]
- 65. The roles of cellular reactive oxygen species, oxidative ... [https://www.sciencedirect.com/science/article/abs/pii/S1357272510001962]
- 66. An Overview of Reactive Oxygen Species Damage ... [https://www.mdpi.com/2076-2615/14/2/330]
- 67. Effect of apoptosis and reactive oxygen species production ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3454987/]
- 68. Predictive potential of combined secretomics and image ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11992772/]
- 69. Epigenetic Reprogramming During Somatic Cell Nuclear ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7093498/]
- 70. Strategies to Improve the Efficiency of Somatic Cell Nuclear ... [https://www.mdpi.com/1422-0067/23/4/1969]
- 71. Somatic Cell Nuclear Transfer Efficiency: How Can It Be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4718708/]
- 72. Epigenetic manipulation to improve mouse SCNT embryonic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9468881/]
- 73. Epigenetic reprogramming in mammalian species after ... [https://www.sciencedirect.com/science/article/abs/pii/S0093691X16300528]
- 74. Epigenetic Reprogramming During Somatic Cell Nuclear ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.00205/full]
- 75. Lycopene enhances epigenetic reprogramming and ... [https://www.nature.com/articles/s41598-025-15672-8]
- 76. When the Embryo Meets the Endometrium - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10931638/]
- 77. Physiologic Events of Embryo Implantation and ... [https://www.mdpi.com/1422-0067/21/6/1973]
- 78. actors behind the endometrial receptivity and successful ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816621001725]
- 79. What is the embryo implantation process [https://www.juanacrespo.es/en/embrio-implantation-process/]
- 80. Effect of culture conditions and method of conception on ... [https://www.sciencedirect.com/science/article/abs/pii/S2666335X20300367]
- 81. Label-free evaluation of mouse embryo quality using time- ... [https://www.nature.com/articles/s42003-025-08044-5]
- 82. Label-free evaluation of mouse embryo quality using time ... [https://pubmed.ncbi.nlm.nih.gov/40234728/]
- 83. Exploring key embryonic developmental morphokinetic ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-024-07080-z]
- 84. Morphokinetics and amino acid consumption in pre ... [https://www.sciencedirect.com/science/article/abs/pii/S0301211525009169]
- 85. Predictive models for live birth outcomes following fresh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462326/]
- 86. Comparative transcriptome analysis of bovine blastocysts ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11848-8]
- 87. In vitro embryolethality testing during the peri-implantation ... [https://www.sciencedirect.com/science/article/pii/S0890623825001121]
- 88. The quest for metabolic biomarkers of IVF outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575374/]