Mechanical Cues in Bone Organoid Development: From Biomechanical Sensing to Advanced Biofabrication
Bone organoids represent a transformative platform for studying bone development, disease modeling, and drug screening.
Mechanical Cues in Bone Organoid Development: From Biomechanical Sensing to Advanced Biofabrication
Abstract
Bone organoids represent a transformative platform for studying bone development, disease modeling, and drug screening. This article comprehensively explores the critical yet underexplored role of mechanical cues—including substrate stiffness, shear stress, and dynamic loading—in guiding the differentiation and maturation of these 3D biomimetic constructs. We examine foundational mechanobiology principles, advanced methodologies for applying mechanical stimulation, strategies for overcoming technical bottlenecks like vascularization and standardization, and the validation of bone organoids against traditional models. Targeting researchers and drug development professionals, this review synthesizes cutting-edge advancements to provide a roadmap for harnessing biomechanical forces to create more physiologically relevant and clinically translatable bone organoid systems.
The Mechanobiology of Bone: How Cells Sense and Respond to Physical Forces
The Bone Niche: Composition and Function
The bone niche is a dynamic and organizationally complex microenvironment essential for maintaining bone health, regulating stem cell fate, and facilitating regeneration after injury [1] [2]. This specialized niche consists of a intricate network of cellular components, extracellular matrix (ECM), and signaling molecules that work in concert to orchestrate bone homeostasis [2]. The bone marrow niche, a key part of this system, provides both structural and biochemical support, predominantly to regulate hematopoietic stem cell (HSC) function, differentiation, and self-renewal, ensuring a delicate balance between quiescence, proliferation, and lineage commitment [3].
The core function of this niche is to send biochemical and mechanical signals to maintain the stem cell pool and prevent its early depletion [3]. It acts as a protective barrier, shielding stem cells from external stressors such as oxidative stress, inflammation, and toxic insults, which is crucial for preventing DNA damage and mutations that could lead to hematological malignancies [3]. Furthermore, the bone microenvironment plays a critical role in disease processes, including the formation of pre-metastatic niches that facilitate cancer spread [1].
Table 1: Major Cellular Components of the Bone Niche
| Cell Type | Primary Function | Key Signaling Molecules Produced |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Differentiate into osteoblasts, adipocytes, chondrocytes; support HSCs by secreting regulatory factors. | SCF, CXCL12 [3] [2] |
| Osteoblasts | Bone formation; synthesize and deposit bone matrix; regulate HSC quiescence. | Osteopontin, Angiopoietin-1, Wnt, BMP [3] [2] |
| Osteoclasts | Bone resorption; regulate ECM turnover and niche remodeling. | Digestive enzymes, factors influencing HSC function [2] |
| Osteocytes | Regulate mineral homeostasis and respond to mechanical signals; embedded in the bone matrix. | Signals influencing osteoblast/osteoclast activity [2] |
| Endothelial Cells | Form the vascular niche; regulate HSC migration, maintenance, and activation. | VEGF, Notch ligands, Angiocrine factors [3] [2] |
| Macrophages | Support HSC maintenance; clear debris; preserve niche homeostasis. | IL-6, TGF-β [3] |
The extracellular matrix provides structural and biochemical support, with collagen, fibronectin, and proteoglycans influencing HSC adhesion, migration, and retention [3]. A network of signaling molecules, including CXCL12, SCF, VEGF, and TGF-β, regulates HSC retention, survival, self-renewal, and quiescence [3]. Disruptions in the niche, whether due to aging, disease, or external factors like chemotherapy, can lead to dysfunction, contributing to conditions such as anemia, immunodeficiency, or hematological malignancies [3].
Biomechanical Cues and Signaling Pathways
Mechanical stimuli are pivotal environmental cues within the bone niche, profoundly influencing bone adaptation, regeneration, and cellular differentiation. The stiffness, density, and architecture of the bone matrix directly influence cell behavior and fate decisions [2]. Mechanical forces, such as those from weight-bearing activities and muscle contractions, are sensed by osteoblasts and osteocytes, which in turn regulate bone formation and remodeling processes [2].
These biomechanical signals are transduced into biochemical responses through several evolutionarily conserved signaling pathways. Key among these are the Wnt/β-catenin, BMP, and Hippo (YAP/TAZ) pathways, which integrate mechanical cues to direct MSC differentiation toward the osteoblastic lineage [2].
Diagram 1: Mechanical Signaling to Osteoblastogenesis. Mechanical cues are transduced via integrins and the cytoskeleton, leading to YAP/TAZ nuclear translocation and activation of osteogenic genes.
The Hippo signaling pathway and its transcriptional co-activators YAP and TAZ are critical mechanotransducers. On a stiff substrate—mimicking the natural bone matrix—increased integrin clustering and F-actin polymerization promote the nuclear translocation of YAP/TAZ. Inside the nucleus, YAP/TAZ stimulate osteogenesis by upregulating the master osteogenic transcription factor RUNX2 while downregulating the adipogenic transcription factor PPARγ [2]. Conversely, a soft substrate leads to cytosolic sequestration of YAP/TAZ, promoting adipogenesis over bone formation [2]. This mechanism ensures that MSCs differentiate into osteoblasts in mechanically favorable environments.
Bone Organoids: Modeling the NicheIn Vitro
Bone organoids are three-dimensional (3D) biomimetic constructs that have emerged as a transformative platform for studying bone development, disease modeling, drug screening, and regenerative medicine [4]. These miniature, self-organized tissues are typically derived from stem cells—such as pluripotent stem cells (PSCs), induced pluripotent stem cells (iPSCs), or mesenchymal stem cells (MSCs)—and are designed to recapitulate the intricate 3D architecture and multicellular composition of native bone tissue [4] [5]. Compared to conventional two-dimensional (2D) cell cultures, bone organoids provide a more physiologically relevant system for investigating the complex cellular interactions and biological processes within the bone niche [5].
Key Construction Methodologies
The construction of a bone organoid involves the careful combination of cells, matrix scaffolds, and biochemical cues to guide self-organization and differentiation.
- Cell Sources: iPSCs and MSCs are the most commonly used cell sources due to their differentiation potential. MSCs can directly differentiate into osteoblasts, while iPSCs offer the ability to generate patient-specific models [4] [6] [7].
- Scaffolds/Matrix: Matrigel is a common but suboptimal scaffold due to its tumor origin and batch variability. Research is exploring alternative biomaterials, including collagen-based hydrogels and 3D-bioprinted scaffolds, to provide better mechanical support and osteoinductive properties [4].
- Biochemical Inducers: A combination of growth factors and morphogens is used to direct osteogenic differentiation. These include Bone Morphogenetic Proteins (BMPs, notably BMP-2), ascorbic acid, β-glycerophosphate, and dexamethasone [7] [5]. Neuropeptides like Calcitonin Gene-Related Peptide (CGRP) have also been shown to synergistically promote osteogenesis with BMP-2 at physiological doses [7].
Advanced technologies are being integrated to overcome the limitations of traditional organoid culture. 3D bioprinting enhances spatial precision and structural complexity, allowing for the creation of organoids with defined architectures [4] [7]. Assembloid techniques enable the assembly of multiple, distinct cellular components—such as vascular endothelial cells and osteoblasts—to better replicate the multicellular microenvironment of native bone [4]. Furthermore, artificial intelligence (AI) and machine learning are being leveraged to optimize organoid culture conditions and analyze complex single-cell RNA sequencing data from organoid-based regeneration studies [4] [7].
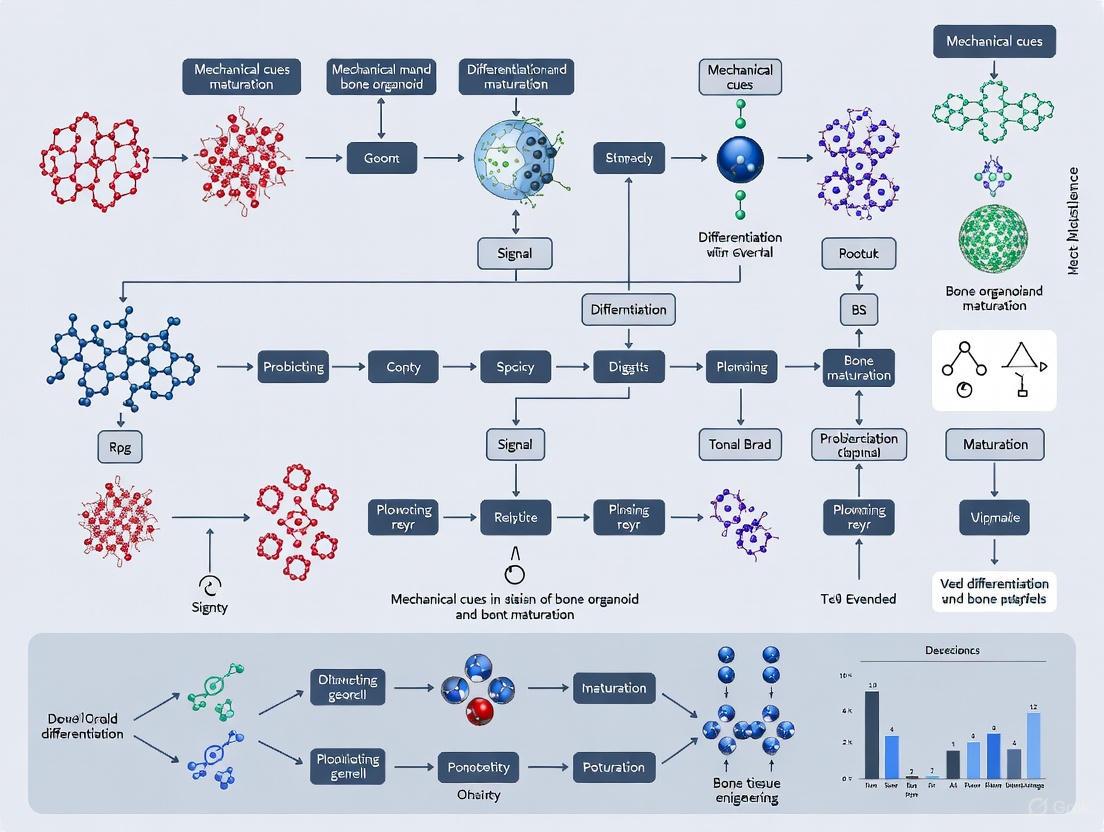
Diagram 2: Bone Organoid Construction Workflow. Key inputs and technologies are combined through 3D culture to generate functional organoids for diverse applications.
Current Challenges and Limitations
Despite their promise, bone organoid technology faces several significant hurdles. A primary challenge is the lack of vascularization, which restricts nutrient and oxygen exchange, limits the size of organoids, and impairs their ability to mimic large-scale bone structures [4] [5]. Another major limitation is the insufficient replication of the native biomechanical environment. Most organoid cultures are maintained in static conditions, lacking the dynamic mechanical loading that is critical for regulating bone cell differentiation, matrix deposition, and tissue maturation in vivo [4]. Additional challenges include the lack of standardized protocols across laboratories, the suboptimal nature of common scaffold materials like Matrigel, and the difficulty in replicating the full cellular complexity of the bone niche [4] [5].
Experimental Approaches for Studying Biomechanics in Bone Organoids
To effectively model the bone niche in vitro, researchers are developing sophisticated experimental methods to introduce and control mechanical stimuli within bone organoid cultures. The protocols below outline key methodologies for applying and assessing the effects of biomechanical cues.
Protocol: Applying Dynamic Mechanical Stimulation via Bioreactors
Purpose: To mimic the in vivo mechanical environment and promote osteogenic maturation of bone organoids. Materials:
- Pre-differentiated bone organoids (e.g., from MSCs in a 3D hydrogel).
- Bioreactor system capable of applying cyclic mechanical load or vibrational forces.
- Control culture vessel (static).
- Osteogenic medium.
Procedure:
- Organoid Preparation: Generate bone organoids using a standard protocol. Encapsulate MSCs in an appropriate hydrogel (e.g., collagen-based or a synthetic polymer) and pre-culture in osteogenic medium for 7-14 days to initiate differentiation.
- Experimental Setup: Divide organoids into two groups: an experimental group and a static control group.
- Mechanical Stimulation:
- Place the experimental group of organoids into the bioreactor chamber.
- Apply a defined cyclic mechanical stimulus. A representative regimen could be a uniaxial or compressive strain of 1-5% at a frequency of 1 Hz, for 1-2 hours per day.
- Maintain the static control group in the same osteogenic medium but without mechanical stimulation.
- Culture Duration: Continue the culture with daily stimulation for a period of 14-28 days, refreshing the medium as required.
- Endpoint Analysis: Assess osteogenic differentiation and matrix maturation (see Protocol 4.2).
Protocol: Assessing Osteogenic Differentiation and Matrix Maturation
Purpose: To quantify the biochemical and functional outcomes of mechanical stimulation on bone organoids. Materials:
- Stimulated and control organoids.
- Phosphate-Buffered Saline (PBS).
- Paraformaldehyde (4% in PBS).
- Alkaline Phosphatase (ALP) staining kit.
- Alizarin Red S (ARS) solution.
- RNA extraction kit, cDNA synthesis kit, and qPCR reagents.
- Primary antibodies for osteogenic markers (e.g., anti-OSTEOCALCIN, anti-RUNX2).
Procedure:
- Alkaline Phosphatase (ALP) Staining (Early osteogenic marker):
- Fix a subset of organoids with 4% PFA for 15-30 minutes at room temperature.
- Wash with PBS and incubate with an ALP staining solution according to the manufacturer's protocol.
- Quantify ALP activity via image analysis or by measuring absorbance after elution of the dye.
- Alizarin Red S (ARS) Staining (Mineralized matrix deposition):
- Fix organoids as above.
- Incubate with 2% ARS solution (pH 4.2) for 20-45 minutes.
- Wash extensively with distilled water to remove non-specific staining.
- To quantify, elute the bound dye with 10% cetylpyridinium chloride and measure the absorbance at 562 nm.
- Gene Expression Analysis (qPCR):
- Homogenize organoids and extract total RNA.
- Synthesize cDNA and perform qPCR for key osteogenic genes (e.g., RUNX2, ALPL/Alp, SP7/Osterix, COL1A1). Normalize data to a housekeeping gene (e.g., GAPDH).
- Immunofluorescence (Protein-level analysis):
- Fix, permeabilize, and block organoids.
- Incubate with primary antibodies against osteogenic markers (e.g., OSTEOCALCIN) overnight at 4°C.
- Incubate with fluorescently conjugated secondary antibodies.
- Image using confocal microscopy to visualize the spatial distribution of protein expression.
Table 2: Key Quantitative Assessments for Bone Organoid Maturation
| Analysis Method | Target Readout | Interpretation of Results |
|---|---|---|
| ALP Staining/Activity | Early osteogenic differentiation | Increased staining/activity indicates commitment to the osteoblast lineage. |
| ARS Staining & Quantification | Calcium deposition and mineralization | Higher absorbance confirms the formation of a mineralized bone-like matrix. |
| qPCR for RUNX2, ALPL | Osteogenic gene expression | Upregulation confirms activation of the genetic program for bone formation. |
| Immunofluorescence for Osteocalcin | Late osteogenic marker protein | Positive staining indicates mature, matrix-producing osteoblasts. |
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the construction and analysis of bone organoids, particularly in the context of biomechanical research.
Table 3: Essential Reagents for Bone Organoid Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific cell source for generating bone lineage cells; enable disease modeling. | Differentiate into MSCs and subsequently into osteoblasts within organoids [4] [6]. |
| Mesenchymal Stem Cells (MSCs) | Primary progenitor cells capable of osteogenic differentiation; workhorse for organoid formation. | Form the core cellular component of ossification center-like organoids (OCOs) [7] [2]. |
| Recombinant Human BMP-2 | Potent osteo-inductive growth factor; drives MSC commitment to the osteoblast lineage. | Used at low (physiological) doses in combination with CGRP to synergistically enhance osteogenesis [7]. |
| Calcitonin Gene-Related Peptide (CGRP) | Neuropeptide that synergistically promotes osteogenesis with BMP-2. | Incorporated into organoid culture to enhance osteogenic differentiation and matrix mineralization [7]. |
| 3D Bioprinting Scaffolds | Provides tunable structural and mechanical support for 3D cell growth and organization. | Printing MSC-laden hydrogels to create spatially defined "ossification center-like organoids" (OCOs) [4] [7]. |
| Collagen-Based Hydrogels | Biomimetic ECM scaffold that supports cell adhesion, migration, and 3D organization. | Serve as the primary matrix for encapsulating MSCs during organoid self-assembly [4]. |
| Osteogenic Induction Cocktail | Standardized medium supplement to induce osteoblast differentiation. | Typically contains ascorbic acid, β-glycerophosphate, and dexamethasone [5]. |
| Oleonuezhenide | Oleonuezhenide, CAS:112693-21-7, MF:C48H64O27, MW:1073.0 g/mol | Chemical Reagent |
| Urease-IN-6 | N-[2-(1H-Indol-3-yl)ethyl]-N'-(4-methoxyphenyl)thiourea | High-purity N-[2-(1H-indol-3-yl)ethyl]-N'-(4-methoxyphenyl)thiourea for research use only (RUO). Explore its potential in pharmaceutical and biological applications. Not for human consumption. |
The bone niche is a complex biomechanical microenvironment where cellular components, signaling pathways, and physical forces interact to maintain homeostasis and drive regeneration. Bone organoids represent a powerful and evolving technology to model this niche in vitro. The integration of advanced techniques such as 3D bioprinting for spatial patterning, bioreactors for applying mechanical stimuli, and AI-driven data analysis is rapidly enhancing the physiological relevance and utility of these models [4] [7].
Future progress in the field hinges on overcoming the key challenges of vascularization, innervation, and the replication of native tissue biomechanics. As these hurdles are addressed, bone organoids will become an indispensable tool for unraveling the fundamental role of mechanical cues in bone biology, advancing drug discovery for skeletal diseases, and ultimately, creating personalized regenerative therapies.
Bone is a dynamic, highly specialized tissue that continuously adapts to its mechanical environment through a process known as remodeling. This process involves the coordinated activity of bone-forming osteoblasts, bone-resorbing osteoclasts, and mechanosensitive osteocytes that orchestrate cellular responses to physical forces [8]. The mechanical environment of bone consists of multiple biophysical cues including substrate stiffness, topographical features, and fluid shear stress (FSS), all of which play critical roles in directing cellular behavior and tissue maturation [4] [8]. Understanding these mechanical determinants is particularly crucial in the emerging field of bone organoid development, where recreating a physiologically relevant microenvironment is essential for producing functional tissue models that accurately mimic native bone properties [4] [9].
Bone organoids—three-dimensional, miniaturized, and simplified in vitro versions of bone tissue—have emerged as promising platforms for studying bone development, disease modeling, drug screening, and regenerative medicine [4] [9]. However, a significant challenge in bone organoid technology lies in replicating the native mechanical microenvironment of bone tissue, which profoundly influences cellular differentiation and function [4]. Traditional culture systems often fail to incorporate these critical mechanical signals, resulting in organoids that lack key structural and functional characteristics of native bone [4] [10]. This technical gap underscores the importance of understanding and applying fundamental mechanical principles, particularly the interplay between substrate stiffness, topography, and fluid dynamics, to advance bone organoid research and its translational applications.
Substrate Stiffness in Bone Cell Differentiation
Fundamental Principles and Biological Significance
Substrate stiffness, defined as the resistance of a material to deformation, is a potent regulator of cell behavior through a process called mechanotransduction—how cells convert mechanical stimuli into biochemical signals. Cells sense substrate stiffness through integrin-mediated adhesion sites and respond by adjusting their cytoskeletal organization, gene expression, and differentiation pathways [11]. In native bone tissue, the extracellular matrix (ECM) undergoes dynamic changes in stiffness during development, healing, and remodeling processes, with stiffness values ranging from the soft granulation tissue in early healing phases to the rigid mineralized bone matrix in mature tissue [11]. The profound dependence of cell behavior on microenvironmental stiffness makes this parameter particularly critical for directing osteogenic commitment in bone organoid systems.
Quantitative Effects on Osteogenic Differentiation
Table 1: Effects of Substrate Stiffness on Bone Cell Behavior
| Stiffness Range | Biological Correlate | Cell Types Studied | Key Findings | References |
|---|---|---|---|---|
| 1.46 kPa | Soft tissue-like | Bone marrow mesenchymal stem cells (BM-MSCs) | Reduced osteogenic differentiation compared to stiff substrates | [12] |
| 15 kPa | Granulation tissue | Pre-osteoblasts (MC3T3-E1), Fibroblasts (NIH3T3) | Enhanced fibronectin (Fn1) and collagen type I (Col1a1) expression in fibroblasts | [11] |
| 26.12 kPa | Stiff tissue | Bone marrow mesenchymal stem cells (BM-MSCs) | Enhanced osteogenic differentiation with increased ALP activity, osteocalcin, Runx2 expression, and mineralization | [12] |
| 35 kPa | Osteoid tissue | Pre-osteoblasts (MC3T3-E1), Fibroblasts (NIH3T3) | Intermediate osteogenic response; decreased Fn1 and Col1a1 in fibroblasts compared to softer substrates | [11] |
| 150 kPa | Calcified bone matrix | Pre-osteoblasts (MC3T3-E1), Fibroblasts (NIH3T3) | Highest Runx2 expression in pre-osteoblasts; lowest Fn1 and Col1a1 in fibroblasts | [11] |
Research has demonstrated that osteogenic differentiation of bone marrow mesenchymal stem cells (BM-MSCs) is significantly enhanced on stiffer substrates (∼26 kPa) compared to softer ones (∼1.5 kPa), as evidenced by increased alkaline phosphatase (ALP) activity, elevated expression of osteoblast-specific markers including osteocalcin, Runx2, and collagen type I, and enhanced mineralization capacity [12]. Interestingly, the effect of substrate stiffness appears to be cell-type specific. While BM-MSCs show stiffness-dependent osteogenic differentiation, more committed bone-derived cells (BDCs) exhibit less variation in their differentiation capacity across different stiffness values [12]. This distinction highlights the importance of considering cell source and commitment state when designing biomaterials for bone organoid development.
The mechanism behind stiffness-dependent differentiation involves increased cell traction forces generated on stiffer substrates, which promote cytoskeletal tension and activation of mechanosensitive transcription factors such as Runx2, a master regulator of osteogenesis [11]. In pre-osteoblasts, Runx2 expression increases with increasing substrate stiffness, while genes associated with fibroblastic activity (Fn1 and Col1a1) decrease correspondingly [11]. This mechanical regulation helps explain why stiffer environments promote osteogenic lineage commitment while softer environments may maintain stemness or direct cells toward softer tissue lineages.
Experimental Protocol: Substrate Stiffness Testing
Polyacrylamide Substrate Preparation Protocol:
- Material Preparation: Prepare polyacrylamide (PAAm) solutions with varying acrylamide and bis-acrylamide concentrations to achieve target stiffness values (e.g., 15, 35, and 150 kPa) as outlined in Table 1 [11].
- Polymerization: Activate polymerization using ammonium persulfate (APS) and tetramethylethylenediamine (TEMED).
- Surface Functionalization: Treat polymerized substrates with sulfosuccinimidyl-6-[4'-azido-2'-nitrophenylamino] hexanoate (Sulfo-SANPAH) under UV light for 15 minutes to enable covalent binding of extracellular matrix proteins [11].
- ECM Coating: Incubate substrates with type I collagen (0.1 mg/mL) overnight at 4°C to create a bioactive surface for cell adhesion [11].
- Mechanical Validation: Characterize Young's moduli of resulting substrates using universal testing equipment with a spherical indenter probe to confirm target stiffness values [11].
- Cell Seeding: Plate cells (e.g., MC3T3-E1 pre-osteoblasts or NIH3T3 fibroblasts) at appropriate densities (e.g., 2×10â´/mL for immunostaining, 8×10â´/mL for PCR analysis) and culture under standard conditions [11].
- Analysis: Assess osteogenic differentiation using quantitative PCR for markers (Runx2, OPN, Col1a1), immunostaining, and mineralization assays (Alizarin Red S staining) [12] [11].
Topographical Cues in Bone Tissue Engineering
Biological Role of Surface Topography
Surface topography encompasses the physical features and nanoscale to microscale patterns on a material surface that influence cell behavior through contact guidance. In native bone, cells interact with a complex topographic landscape including collagen fibrils, mineral crystals, and macroporous structures that direct cell adhesion, migration, and tissue organization [4]. The hierarchical organization of bone tissue, ranging from nanoscale collagen fibrils to trabecular and cortical architectures, provides topographic cues that are essential for proper cell functioning and tissue-level mechanical properties [4]. Recreating these features in bone organoid systems is critical for achieving physiological relevance in vitro.
Implementation in Bone Organoid Design
Advanced fabrication techniques such as 3D bioprinting have enabled unprecedented control over topographical features in bone tissue engineering scaffolds [4]. These technologies allow for the creation of complex geometries with precise spatial patterning that can direct cellular self-organization and tissue maturation in bone organoids. Bioprinted constructs can incorporate microarchitectural features resembling native bone trabeculae, facilitating the development of more physiologically relevant organoid models [4]. The integration of topographical cues with biochemical signaling in these systems enhances the fidelity of bone organoids, enabling better replication of native tissue properties.
While specific quantitative data on topographical parameters was limited in the search results, the consensus literature emphasizes that topographical design is a critical consideration in bone organoid construction [4] [9]. The mechanical properties provided by topographic features interact with other mechanical cues, particularly substrate stiffness, to regulate cell fate decisions and tissue development in evolving organoid systems.
Fluid Shear Stress in Bone Mechanobiology
Physiological Role in Bone Tissue
Fluid shear stress (FSS) is the frictional force generated by interstitial fluid flow within the lacunar-canalicular network of bone tissue, primarily resulting from external loading during physical activity [8]. This mechanical cue plays a fundamental role in bone maintenance, adaptation, and healing processes. Osteocytes, the most abundant bone cells embedded within the mineralized matrix, are particularly sensitive to FSS and function as mechanosensors that coordinate the activity of osteoblasts and osteoclasts in response to mechanical loading [8]. In bone organoid systems, incorporating physiologically relevant fluid dynamics remains a significant challenge but is essential for creating functional tissue models.
Quantitative Effects on Osteogenic Differentiation
Table 2: Effects of Fluid Shear Stress on Bone Cell Behavior
| FSS Magnitude | Temporal Profile | Cell Type | Key Findings | References |
|---|---|---|---|---|
| 8-30 dynes/cm² | Physiological range | Bone marrow mesenchymal stem cells (BMSCs) | Promotes osteogenic differentiation | [13] |
| 16 dynes/cm² | Intermittent vs. Continuous | Bone marrow mesenchymal stem cells (BMSCs) | Intermittent FSS preserves mechanical sensitivity and enhances osteogenic differentiation compared to continuous FSS | [13] |
| 12 dynes/cm² | 2 hours | BMSCs at different differentiation phases | Enhanced osteogenic differentiation at early matrix maturation phase; suppressed expression at proliferation phase; decreased mineralization at late mineralization phase | [13] |
Fluid shear stress within the physiological range (8-30 dynes/cm²) significantly enhances osteogenic differentiation of bone marrow mesenchymal stem cells (BMSCs) [13]. The temporal pattern of FSS application is crucial, with intermittent stimulation proving more effective than continuous flow for promoting osteogenic commitment [13]. This mimics the natural loading patterns experienced by bone tissue during daily activities.
The effect of FSS is highly dependent on the differentiation stage of target cells. When applied to BMSCs at the early matrix maturation phase (approximately 7 days of osteogenic induction), FSS (12 dynes/cm², 2 hours) significantly promotes osteogenic differentiation, evidenced by enhanced expression of Runx2, ALP, OPN, and OCN genes [13]. In contrast, the same stimulus applied during the proliferation phase suppresses osteogenesis-related gene expression, while application during the late mineralization phase decreases nodule mineralization [13]. This stage-specific responsiveness highlights the importance of temporal considerations when applying mechanical stimulation in bone organoid culture protocols.
Molecular Mechanisms of FSS Signaling
Diagram Title: FSS Mechanotransduction Pathway in BMSCs
The molecular mechanism by which FSS promotes osteogenesis involves sophisticated mechanotransduction pathways. FSS initially induces cytoskeletal reorganization and actin stress fiber formation in BMSCs [13]. This mechanical stimulation enhances the expression of Lamin A, a key component of the nuclear lamina that stabilizes nuclear structure and regulates gene expression [13]. Upregulated Lamin A interacts with METTL3 (methyltransferase-like 3), the catalytic core of the N6-methyladenosine (m6A) methyltransferase complex, promoting its nuclear localization and stability [13].
The Lamin A/METTL3 interaction enhances m6A methylation on target mRNAs, an epigenetic modification that regulates their stability and translation efficiency [13]. This mechanosensitive epigenetic regulation ultimately promotes the expression of osteogenic genes, creating a direct link between mechanical stimulation and gene expression programming in bone cells. This pathway represents a crucial mechanism whereby physical forces are transduced into biochemical signals that direct cell fate decisions in bone tissue and organoid systems.
Experimental Protocol: Fluid Shear Stress Application
Fluid Shear Stress Application Protocol:
- Device Setup: Utilize a parallel-plate flow chamber system connected to a peristaltic pump and medium reservoir, maintaining constant temperature at 37°C and 5% CO₂ [13].
- Cell Preparation: Culture BMSCs in osteogenic induction medium for varying durations to achieve different differentiation phases: proliferation phase (1 day), early matrix maturation phase (7 days), and late mineralization phase (14 days) [13].
- Flow Application: Apply pulsatile fluid flow at physiological magnitude (e.g., 12 dynes/cm²) for specified durations (e.g., 2 hours) [13].
- Post-Stimulation Analysis:
- Assess cytoskeletal organization via F-actin staining using phalloidin.
- Evaluate osteogenic gene expression (Runx2, ALP, OPN, OCN) using quantitative RT-PCR.
- Analyze protein expression and localization via immunofluorescence and western blot.
- Examine mineralized nodule formation using Alizarin Red S staining [13].
- Mechanistic Studies: For pathway inhibition studies, employ specific inhibitors targeting actin polymerization (e.g., cytochalasin D) or METTL3 function (e.g., siRNA knockdown) to confirm mechanism [13].
Integration of Mechanical Cues in Bone Organoid Development
Current Challenges and Limitations
The integration of multiple mechanical cues into bone organoid systems presents several significant challenges. The complex hierarchical organization of native bone tissue, which confers exceptional mechanical strength and load-bearing capacity, is difficult to replicate in vitro [4]. Most current organoid cultures are maintained in static conditions or simple hydrogels that lack the dynamic mechanical stimulation inherent to living bone [4]. This mechanical deficiency likely contributes to the observed morphological and functional differences between current bone organoid models and native skeletal tissue.
Vascularization represents another major challenge, as native bone is highly vascularized while existing bone organoids typically lack mature vascular networks [4]. This limitation restricts nutrient exchange and organoid size, ultimately impairing long-term viability and functional maturation. Additionally, standardization issues across different laboratories, including variations in cell sources, scaffold materials, and culture conditions, have led to substantial batch-to-batch variability, complicating comparative analyses and clinical translation [4] [9].
Advanced Engineering Approaches
Emerging technologies are providing new solutions for incorporating mechanical cues into bone organoid development. Three-dimensional bioprinting enables precise spatial patterning of cells and biomaterials, allowing creation of complex structures with anatomically relevant topographical features [4]. Perfusion bioreactors can deliver physiological fluid shear stress to organoid cultures, promoting nutrient exchange and providing mechanical stimulation [8] [13]. These systems can apply controlled intermittent flow patterns that mimic natural loading cycles in bone tissue.
Assembloid technologies, which involve the assembly of multiple organoid units or different cell types, enable reconstruction of more complex tissue microenvironments with heterogeneous mechanical properties [4]. These approaches facilitate the creation of organoid systems that better replicate the multicellular composition and structural complexity of native bone. Additionally, the integration of artificial intelligence and machine learning in organoid culture optimization offers promising avenues for systematically analyzing the combined effects of multiple mechanical parameters and identifying optimal culture conditions [4].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Mechanical Cue Studies
| Reagent/Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| Engineered Substrates | Polyacrylamide (PAAm) hydrogels; Collagen-coated surfaces | Mimic variable stiffness of bone microenvironment; Study stiffness-dependent cell behavior | [12] [11] |
| 3D Scaffold Materials | Matrigel; Collagen-based hydrogels; Synthetic polymers | Provide three-dimensional support for organoid formation; Can be engineered with specific mechanical properties | [4] |
| Mechanotransduction Inhibitors | Cytochalasin D (actin disruptor); METTL3 siRNA; ROCK inhibitors | Probe specific mechanosensing pathways; Validate mechanism of mechanical cue response | [13] |
| Osteogenic Markers | Alkaline Phosphatase (ALP); Runx2; Osteocalcin; Osteopontin | Quantify osteogenic differentiation response to mechanical cues; Assess functional maturation | [12] [11] [13] |
| Flow Systems | Parallel-plate flow chambers; Perfusion bioreactors | Apply controlled fluid shear stress to cells; Mimic interstitial fluid flow in bone | [8] [13] |
| Ac2-26 | Ac2-26, MF:C141H210N32O44S, MW:3089.4 g/mol | Chemical Reagent | Bench Chemicals |
| CTCE-9908 | CTCE-9908, CAS:1030384-98-5, MF:C86H147N27O23, MW:1927.3 g/mol | Chemical Reagent | Bench Chemicals |
Substrate stiffness, topography, and fluid shear stress represent three fundamental mechanical cues that collectively direct bone cell fate and tissue maturation. The integration of these mechanical principles into bone organoid development is essential for creating physiologically relevant models that accurately recapitulate native bone properties. While significant progress has been made in understanding individual mechanical parameters, future research should focus on their synergistic integration and temporal application throughout organoid development and maturation processes. Advanced bioengineering approaches such as 3D bioprinting, perfusion bioreactors, and assembloid technologies offer promising avenues for addressing current limitations in bone organoid technology. As these methodologies continue to evolve, they will undoubtedly enhance the fidelity and functionality of bone organoids, ultimately advancing their applications in disease modeling, drug screening, and regenerative medicine.
Cellular mechanosensors, comprising integrins, focal adhesions (FAs), and the cytoskeleton, constitute a sophisticated mechanotransduction network that enables cells to perceive and respond to physical cues from their microenvironment. Within the context of bone biology, this mechanosensory apparatus is indispensable for directing osteogenic differentiation, bone remodeling, and maintaining skeletal homeostasis. This technical review delineates the core components, molecular architectures, and dynamic signaling pathways of these mechanosensors, with a specific emphasis on their integrated function in bone organoid differentiation and maturation. We synthesize current mechanistic insights, present quantitative data on mechanosensitive signaling, and provide detailed experimental protocols for investigating these processes. Furthermore, we outline a toolkit of research reagents and engineered platforms essential for advancing the field of bone organoid engineering, thereby offering a foundational resource for researchers and drug development professionals aiming to harness mechanobiology for regenerative medicine.
Bone is a quintessential mechanoresponsive tissue, whose mass and architecture are dynamically regulated by mechanical loading. The adaptation of bone to physical force is orchestrated by resident bone cells—osteocytes, osteoblasts, and osteoclasts—that translate mechanical signals into biochemical responses, a process known as mechanotransduction [14]. The emergence of bone organoids as three-dimensional, self-organizing model systems presents an unprecedented opportunity to study these complex processes in vitro. However, the fidelity of these organoids is critically dependent on the recapitulation of the native mechanical niche [5].
The extracellular matrix (ECM) provides more than just structural support; it is a biomechanical information reservoir. Cells probe this environment through a triad of interconnected mechanosensors: integrins, which are transmembrane receptors binding ECM ligands; focal adhesions, which are macromolecular assemblies that link integrins to the intracellular machinery; and the cytoskeleton, a dynamic network of filaments that confers cellular structure and transmits force [15] [14] [16]. In bone organoid engineering, the static, poorly defined nature of conventional matrices like Matrigel poses a significant limitation, often failing to provide the precise, dynamic mechanical cues necessary for robust organoid maturation [17] [18]. A deep understanding of these mechanosensors is therefore paramount for designing next-generation biomimetic environments that can guide organoid development with high physiological relevance and reproducibility. This review dissects the roles of this mechanosensory triad, framing their function within the specific context of bone organoid differentiation and maturation.
Core Components of Cellular Mechanosensing
Integrins: The Primary Mechanoreceptors
Integrins are heterodimeric transmembrane receptors, composed of α and β subunits, that serve as the primary link between the ECM and the intracellular cytoskeleton. They exist in a range of affinities, and their activation is a tightly regulated process crucial for mechanosensation [15] [19].
- Structure and Activation: Integrins transition between bent-closed (low affinity), extended-closed (intermediate affinity), and extended-open (high affinity) conformations. This activation can be triggered by ligand binding from the outside (outside-in activation) or by intracellular proteins binding the β-subunit's cytoplasmic tail (inside-out activation) [15]. The α5β1 integrin, the principal receptor for fibronectin, is of particular significance in bone. It recognizes the Arg-Gly-Asp (RGD) peptide sequence within fibronectin, and its expression is upregulated during osteogenic differentiation [20].
- Mechanosensation: Integrins are force-sensitive. Applied force stabilizes the high-affinity conformation and promotes clustering, which in turn initiates the assembly of focal adhesion complexes. Clinical and experimental data underscore its importance: expression of α5β1 is downregulated in osteoporotic bone but upregulated in osteoarthritic chondrocytes, highlighting its context-dependent role in skeletal pathology [20].
- Role in Bone Organoids: The specific repertoire of integrins expressed by stem cells dictates their response to the surrounding engineered matrix. Providing appropriate RGD-containing ligands within synthetic hydrogels is a key strategy to engage α5β1 and other RGD-binding integrins, thereby promoting osteogenic differentiation and bone organoid development [17] [18].
Focal Adhesions: The Mechanotransduction Hub
Focal adhesions are dynamic, layered protein complexes that form at the interface between ligated integrins and the actin cytoskeleton. They act as central signaling platforms, facilitating bidirectional mechanical communication [15].
- Layered Architecture: FAs are organized into functional layers:
- Structural Layer: Comprises proteins like talin and kindlin, which directly bind integrin β-tails and recruit vinculin and α-actinin, providing a mechanical link to actin [15].
- Signaling Layer: Includes kinases such as Focal Adhesion Kinase (FAK) and Src, which are activated by integrin clustering and mechanical force, initiating downstream signaling cascades [15] [19].
- Actin Cross-linking Layer: Contains proteins like α-actinin and VASP that regulate actin polymerization and bundling, reinforcing the mechanical connection [15].
- Mechanotransduction: Force-dependent unfolding of proteins like talin exposes cryptic binding sites for vinculin, reinforcing the adhesion and amplifying downstream signaling. This process is critical for the activation of pathways like MAPK/ERK and PI3K/AKT, which drive osteogenic gene expression [15] [21] [19].
The Cytoskeleton: The Intracellular Mechanoscaffold
The cytoskeleton is an integrated network of three primary filament systems that collectively define cell shape, provide mechanical stability, and serve as a conduit for intracellular force transmission.
- Actin Filaments: Actin networks, particularly stress fibers, generate contractile forces via myosin II and are directly attached to focal adhesions. This actomyosin contractility is a primary driver of cellular tension and a key regulator of mechanosensitive transcription factors like YAP/TAZ [14] [16].
- Microtubules: These hollow tubes provide compressive resistance and serve as tracks for intracellular transport. Their mechanosensory role is fine-tuned by post-translational modifications. Acetylation and detyrosination enhance microtubule flexibility and stability, allowing them to withstand mechanical stress and influence mechanosignaling [14].
- Intermediate Filaments: Networks of vimentin or keratins provide mechanical integrity and contribute to the viscoelastic response of the cell, distributing stresses and protecting the nucleus from deformation [14].
The interconnectedness of these three systems means that force applied at an integrin receptor is transmitted and distributed throughout the entire cellular architecture, ultimately influencing nuclear shape and gene expression.
Integrated Mechanotransduction Signaling in Bone
The mechanosensory components collaborate to activate specific signaling pathways that dictate bone cell fate. The following diagram illustrates the core integrated pathway from force sensing to osteogenic response, particularly in the context of bone organoid maturation.
Diagram 1: Integrated mechanotransduction pathway from initial force sensing to osteogenic response in bone cells, relevant to organoid maturation.
The pathway depicted above is driven by several key molecular players, whose activities and relationships have been quantified through experimental studies. The table below summarizes critical quantitative data on these mechanosensitive signaling dynamics.
Table 1: Quantitative Dynamics of Mechanosensitive Signaling in Osteoblasts
| Parameter | Value / Dynamic Range | Biological Context & Impact |
|---|---|---|
| Integrin Mechanosensitivity Threshold (MT) | 1% of Applied Force (Ultra-Sensitive) vs. 10% (Sensitive) | Ultra-sensitive (1%) threshold leads to sustained ERK activation beyond 4 days, while sensitive (10%) threshold leads to signal termination within 6 hours [21]. |
| pERK Activation Duration | > 4 days (Ultra-Sensitive MT) vs. ~6 hours (Sensitive MT) | Sustained pERK is linked to long-term osteogenic commitment and the emergence of a "mechanical memory" [21]. |
| Matrix Stiffness for Osteogenesis | ~25-40 kPa (for 2D culture) | Mimics the stiffness of collagenous bone matrix; promotes osteogenic differentiation of MSCs via enhanced integrin clustering and actomyosin contractility [16]. |
| YAP/TAZ Nuclear Translocation | Increased on stiff (>10 kPa) 2D substrates & in stiff 3D matrices | Serves as a key mechanosensitive readout; nuclear YAP/TAZ upregulates osteogenic transcription factors like Runx2 [17] [16]. |
Experimental Protocols for Mechanosensor Analysis
Protocol: Quantifying Integrin-Mediated Mechanotransduction via pERK Dynamics
Objective: To measure the duration and intensity of ERK activation (phosphorylation) in response to mechanical stimulation, as a readout of integrin-mediated mechanotransduction and its sensitivity.
Materials:
- Osteoblast precursor cells (e.g., MC3T3-E1 or human MSCs)
- Flexible-bottomed culture plates (e.g., from FlexCell International)
- Standard cell culture equipment
- Phospho-specific antibody against pERK1/2 (Thr202/Tyr204)
- Flow cytometer or Western blot apparatus
Method:
- Cell Seeding: Seed cells at a defined density on flexible membranes coated with a defined ECM protein (e.g., fibronectin for α5β1 integrin studies).
- Serum Starvation: Incubate cells in low-serum (e.g., 0.5% FBS) medium for 12-16 hours to synchronize cells and reduce background signaling.
- Mechanical Stimulation: Apply a defined cyclic uniaxial or equiaxial strain (e.g., 10% elongation at 1 Hz) using the strain device. Include static controls.
- Inhibition (Optional): Pre-treat a subset of cells with function-blocking anti-α5β1 integrin antibody or a FAK inhibitor (e.g., PF-573228) to confirm the specificity of the response.
- Cell Lysis and Analysis: At defined time points post-stimulation onset (e.g., 15, 30, 60, 90 mins, 4h, 24h), lyse cells.
- For Western Blot, probe lysates with anti-pERK and total ERK antibodies to quantify the pERK/ERK ratio.
- For Flow Cytometry, fix and permeabilize cells, then stain intracellularly with pERK antibody and a fluorescent secondary antibody. Analyze the geometric mean fluorescence intensity (gMFI) of the cell population.
- Data Interpretation: Plot pERK levels over time. As demonstrated in computational models, observe if the signal is transient (sensitive integrin response) or sustained for days (ultra-sensitive response), indicating a potential for long-term osteogenic commitment [21].
Protocol: Modulating Cytoskeletal Mechanics to Probe Osteocyte Response
Objective: To dissect the contribution of specific cytoskeletal elements to mechanosensing by using pharmacological agents and assessing downstream effector expression.
Materials:
- Osteocyte-like cells (e.g., MLO-Y4)
- Pharmacological agents: Nocodazole (microtubule destabilizer), Paclitaxel (Taxol, microtubule stabilizer), Latrunculin B (actin polymerization inhibitor), Jasplakinolide (actin stabilizer).
- ELISA or Western blot kits for Sclerostin (SOST) and Nitric Oxide (NO) detection.
Method:
- Cell Culture: Culture MLO-Y4 cells on type I collagen-coated plates until they develop dendritic processes.
- Pharmacological Perturbation: Pre-treat cells with cytoskeletal-modulating drugs for a predetermined duration (e.g., 2-4 hours). Use appropriate vehicle controls.
- Example:
- Microtubule Destabilization: 1 µM Nocodazole
- Microtubule Stabilization: 1 µM Paclitaxel
- Actin Depolymerization: 100 nM Latrunculin B
- Example:
- Mechanical Stimulation: Apply oscillatory fluid flow shear stress (e.g., 1 Pa, 1 Hz) to the cells for 30-60 minutes. Include static and drug-only controls.
- Assessment of Mechanoresponse:
- Sclerostin Downregulation: Collect cell lysates or supernatant after 1-6 hours post-flow. Quantify sclerostin protein levels via ELISA. Intact microtubules and actin are required for the flow-induced downregulation of sclerostin [14].
- Nitric Oxide Release: Measure NO in the culture medium immediately after flow cessation using a Griess assay. NO release is an early, rapid response to fluid shear stress.
- Data Interpretation: Compare the ability of mechanically stimulated cells to downregulate sclerostin and upregulate NO release in the presence of cytoskeletal perturbations. This reveals the relative contribution of each filament system to the transduction of the anabolic mechanical signal [14].
The Scientist's Toolkit: Research Reagent Solutions
Advancing research in bone organoid mechanobiology requires a specific toolkit of reagents and engineered materials. The following table details essential solutions for probing and controlling the mechanosensory environment.
Table 2: Essential Research Reagents and Platforms for Mechanobiology Studies in Bone Organoids
| Tool Category | Specific Examples | Function & Application |
|---|---|---|
| Engineered Hydrogels | PEG-based hydrogels; Alginate-DNA viscoelastic hydrogels; Decellularized ECM (dECM) hydrogels. | Provide a mechanically tunable 3D microenvironment with definable stiffness, viscoelasticity, and adhesive ligand presentation to study their impact on organoid morphogenesis [17] [18]. |
| Mechanosensing Agonists/Inhibitors | Function-blocking anti-Integrin antibodies (e.g., α5β1); FAK inhibitor (PF-573228); RGD motif peptides. | Used to perturb specific components of the mechanotransduction pathway to establish causal links between sensor activity and osteogenic outcomes [20] [15]. |
| Biosensors & Reporters | FRET-based tension biosensors (e.g., for Vinculin, Talin); YAP/TAZ localization reporters; Sclerostin-promoter driven fluorescent reporters. | Enable real-time visualization and quantification of molecular forces, pathway activation, and mechanosensitive gene expression in live cells [14] [19]. |
| Advanced 3D Culture Platforms | Organ-on-a-Chip devices with integrated mechanical actuation; 3D Bioprinting systems. | Allow for the application of physiologically relevant mechanical forces (e.g., fluid shear, compression) within complex 3D tissue constructs, enabling vascularized bone organoid models [5] [16]. |
| AC 187 | AC 187, MF:C127H205N37O40, MW:2890.2 g/mol | Chemical Reagent |
| MEN 11270 | B2 Receptor Research Peptide | High-purity H-D-Arg-Arg-Pro-Hyp-Gly-2Thi-Dab(1)-D-Tic-Oic-Arg-(1) for bradykinin B2 receptor studies. For Research Use Only. Not for human consumption. |
The strategic use of these tools, particularly the integration of tunable hydrogels into advanced 3D platforms, is revolutionizing bone organoid engineering. The following diagram outlines a generalized workflow for employing these materials to build and test bone organoids with defined mechanical properties.
Diagram 2: Workflow for engineering bone organoids using tunable hydrogel platforms, from material formulation to functional analysis.
Bone tissue exists in a constant state of dynamic equilibrium, continuously adapting its structure in response to mechanical demands—a principle encapsulated by Wolff's Law [22]. At the molecular heart of this phenomenon lies the YAP/TAZ signaling axis, which serves as a primary mechanotransduction pathway converting physical stimuli into biochemical signals that direct osteogenic gene expression [23] [24]. These transcriptional co-activators have emerged as central regulators of bone homeostasis, stem cell differentiation, and tissue regeneration [25] [22]. In the context of bone organoid engineering, understanding YAP/TAZ mechanobiology is paramount for creating physiologically relevant models that accurately mimic the native bone microenvironment [4] [26]. This technical guide comprehensively examines the molecular mechanisms of YAP/TAZ-mediated mechanotransduction, details experimental methodologies for its investigation in bone organoids, and synthesizes quantitative findings that underscore its pivotal role in osteogenic differentiation.
Molecular Mechanisms of YAP/TAZ Mechanotransduction
Core Hippo Pathway and Alternative Regulation
The Hippo pathway represents the canonical regulatory circuit controlling YAP/TAZ activity. This kinase cascade centers on MST1/2 and LATS1/2 kinases, which phosphorylate YAP/TAZ, promoting their cytoplasmic retention and proteasomal degradation [25] [27]. When the Hippo pathway is inactive, dephosphorylated YAP/TAZ translocate to the nucleus, associate with TEAD transcription factors, and activate genes controlling cell proliferation, survival, and differentiation [27]. However, in mechanical signaling, YAP/TAZ regulation often occurs through Hippo-independent mechanisms that respond directly to cytoskeletal tension and cell shape changes [25] [23].
The following diagram illustrates the integrated signaling pathways through which mechanical cues regulate YAP/TAZ activity to direct osteogenic gene expression:
Cytoskeletal Dynamics as a Mechanical Integrator
The actin cytoskeleton serves as a central mediator of YAP/TAZ mechanical responsiveness [25] [23]. Mechanical stimuli—including substrate stiffness, fluid shear stress, and cellular deformation—are transmitted to the actin cytoskeleton through mechanosensitive structures, resulting in actin polymerization and increased tension [25]. This tension directly influences YAP/TAZ activity, as evidenced by experiments showing that F-actin disrupting drugs (e.g., latrunculin A, cytochalasin D) prevent YAP/TAZ nuclear localization even on stiff substrates [23]. Importantly, the regulatory input stems not from total F-actin content but from specific actin architectures generated under mechanical load; rounded cells may contain more F-actin than spread cells yet exhibit cytoplasmic YAP/TAZ localization [23]. Key actin regulatory proteins including actin-capping proteins (CAPZ), cofilin (CFL), and angiomotin (AMOT) family members have been demonstrated to exert significant control over YAP/TAZ activity [23].
Experimental Analysis of YAP/TAZ in Bone Organoids
Methodologies for Mechanotransduction Investigation
Studying YAP/TAZ mechanobiology in bone organoids requires specialized approaches that enable precise control and measurement of mechanical parameters while assessing molecular responses. The following experimental workflow outlines key methodologies:
Essential Research Reagents and Tools
The following table catalogs crucial reagents and methodologies for investigating YAP/TAZ mechanobiology in bone organoid systems:
| Research Tool Category | Specific Examples | Experimental Function | Key Findings Enabled |
|---|---|---|---|
| Cytoskeletal Modulators | Latrunculin A, Cytochalasin D (F-actin disruptors); Jasplakinolide (F-actin stabilizer); Blebbistatin (myosin II inhibitor) | Dissect actin cytoskeleton contribution to YAP/TAZ regulation | F-actin disruption prevents YAP/TAZ nuclear localization even on stiff substrates [23] |
| Substrate Engineering | Tunable hydrogels (polyacrylamide, PEG); Stiffness gradients; Matrigel; Collagen-based scaffolds | Control mechanical microenvironment independent of biochemical cues | Stiff substrates (>5-10 kPa) promote nuclear YAP/TAZ while soft substrates (<1.5 kPa) retain YAP/TAZ in cytoplasm [23] [24] |
| Genetic Manipulation Tools | YAP/TAZ siRNA/shRNA; CRISPR/Cas9 knockout; Constitutively active YAP/TAZ mutants (S127A); YAP/TAZ fluorescent reporters | Establish causal relationship between YAP/TAZ and osteogenic outcomes | YAP/TAZ depletion prevents osteogenic differentiation even on osteoinductive stiff substrates [25] [22] |
| Mechanical Stimulation Systems | Cyclic stretch devices; Compression bioreactors; Fluid shear systems; Acoustic stimulators | Apply controlled mechanical forces mimicking physiological conditions | Cyclic stretching promotes nuclear YAP/TAZ and enhances osteogenic differentiation in MSCs [25] |
| Analysis & Detection | YAP/TAZ phosphorylation-specific antibodies; Immunofluorescence imaging; TEAD luciferase reporters; Osteogenic markers (RUNX2, ALPL, OCN) | Quantify YAP/TAZ activity and downstream osteogenic responses | Subcellular fractionation reveals mechanical regulation operates largely through nuclear translocation rather than total protein abundance [23] |
Quantitative Effects of Mechanical Cues on YAP/TAZ and Osteogenesis
The relationship between mechanical inputs, YAP/TAZ activation, and osteogenic outcomes has been quantitatively characterized across numerous experimental systems. The following table synthesizes key quantitative findings:
| Mechanical Input | Experimental System | YAP/TAZ Response | Osteogenic Outcome |
|---|---|---|---|
| Substrate Stiffness | MSCs on tunable hydrogels [25] [23] | Nuclear localization: <10% on soft (0.5-1 kPa) vs >80% on stiff (30-40 kPa) substrates | Stiff substrates (25-40 kPa): osteogenic differentiation; Soft substrates (0.5-1 kPa): adipogenic differentiation [25] |
| Cell Spreading Area | Micropatterned islands [23] [24] | Cytoplasmic on small islands (300 μm²); Nuclear on large islands (3000 μm²) | Apoptosis on small islands; Proliferation on large islands [23] |
| Fluid Shear Stress | Endothelial cells [25] [23] | Flow-induced nuclear translocation (2-20 dyn/cm²) | Enhanced vascular stability and angiogenesis [25] |
| Cyclic Stretch | Mouse embryonic fibroblasts [25] | Stretch-induced nuclear localization and target gene activation | Enhanced proliferation and stress fiber formation [25] |
| Cell Density | Epithelial and mesenchymal cells [25] [23] | High density: cytoplasmic; Low density: nuclear | Contact inhibition of proliferation at high density [25] [23] |
YAP/TAZ in Bone Organoid Engineering and Therapeutic Applications
Advancing Bone Organoid Technology Through Mechanobiology
The integration of YAP/TAZ mechanobiology principles has catalyzed significant advances in bone organoid engineering [4] [26]. Traditional organoid culture systems often fail to recapitulate the mechanical milieu of native bone tissue, limiting their physiological relevance [4] [5]. However, emerging approaches now deliberately incorporate mechanical cues known to activate YAP/TAZ signaling. For instance, researchers are employing 3D bioprinting to create organoids with controlled architectural features that direct cellular mechanical forces, and utilizing tunable biomaterials with bone-mimetic stiffness to promote osteogenic differentiation through YAP/TAZ activation [4] [26]. These engineered microenvironments have demonstrated that nuclear YAP/TAZ localization is a hallmark of the growing, stem-like compartments within organoids, while differentiated regions show predominantly cytoplasmic localization [23]. This spatial patterning mirrors the in vivo distribution observed in intestinal crypt-villus systems and suggests conserved mechanical regulation of stem cell maintenance across tissues [23].
Therapeutic Implications and Future Directions
The central role of YAP/TAZ in bone mechanobiology presents compelling therapeutic opportunities for bone regeneration and disease treatment [22] [27]. In bone repair contexts, YAP/TAZ activation represents a promising strategy to enhance fracture healing and combat disuse osteoporosis [22]. Recent innovations include the development of "ossification center-like organoids" (OCOs) that harness YAP/TAZ-mediated mechanical signaling to drive rapid bone regeneration in critical-sized defects [7]. These OCOs employ a "divide-and-conquer" strategy, where multiple organoid units collectively facilitate bone bridging through coordinated activation of developmental mechanosensitive programs [7]. For clinical translation, targeting YAP/TAZ signaling could revolutionize treatment for osteoporosis, osteoarthritis, and bone defects [22] [27]. Future research directions should focus on delineating the precise mechanical thresholds for therapeutic YAP/TAZ activation, developing biomaterials with spatially patterned mechanical properties to guide organoid maturation, and establishing standardized protocols that integrate mechanical conditioning as a fundamental aspect of bone organoid culture [4] [26] [5].
YAP/TAZ signaling represents the fundamental molecular bridge connecting mechanical cues with osteogenic gene expression programs. In bone organoid engineering, deliberate manipulation of this mechanosensitive axis enables the creation of more physiologically relevant models that faithfully recapitulate the mechanical aspects of bone development, homeostasis, and pathology. As the field advances, integrating increasingly sophisticated mechanical controls with emerging technologies—including 3D bioprinting, artificial intelligence-driven optimization, and multi-organoid assembloids—will further enhance our ability to harness YAP/TAZ biology for both fundamental discovery and therapeutic innovation in skeletal health and disease [4] [26].
The motor-clutch model is a fundamental theoretical framework in cellular mechanobiology that describes how cells transmit and sense mechanical forces through their environment. This model provides a mechanistic understanding of how cells sense extracellular matrix (ECM) stiffness through myosin-generated pulling forces acting on F-actin, which is mechanically coupled to the environment via adhesive proteins, functioning similarly to a clutch in a drivetrain [28]. At its core, the model consists of three essential components: myosin molecular motors that generate tension on actin filaments, integrin-based molecular clutches that transiently link these filaments to the extracellular substrate, and the substrate itself with its specific mechanical properties [29] [30]. The complex interplay between these components determines the force transmitted to the substrate, influencing fundamental cellular processes including migration, spreading, differentiation, and tissue remodeling [28] [31].
The mechanical stiffness of a cell's environment exerts a strong, but variable, influence on cell behavior and fate [32]. Different cell types cultured on compliant substrates show opposite trends of cell migration and traction as a function of substrate stiffness, which the motor-clutch model helps explain mechanistically [32] [33]. The model exhibits distinct regimes: at high substrate stiffness, clutches quickly build force and fail (frictional slippage), whereas at low substrate stiffness, clutches fail spontaneously before motors can load the substrate appreciably (a second regime of frictional slippage) [32]. Between these extremes lies a stiffness optimum where traction force is maximized—when the substrate load-and-fail cycle time equals the expected time for all clutches to bind [32]. At this optimal stiffness, clutches are used to their fullest extent, and motors are resisted to their fullest extent [32].
Core Mathematical Framework
Fundamental Equations
The motor-clutch system is governed by a set of equations that describe the mechanical interactions and stochastic binding dynamics. The velocity of actin retrograde flow (V_actin) is determined by a linear force-velocity relationship:
V_actin = V_u (1 - (∑F_clutch) / (n_m × F_m)) [29]
Where Vu is the unloaded velocity of the actin bundle, ∑Fclutch is the sum of forces from all bound clutches, nm is the number of motors, and Fm is the force per motor [29]. Each clutch acts as a Hookean spring with force calculated as:
F_clutch(i) = K_c × (X_i - X_sub) [29]
Where Kc is the clutch spring constant, Xi is the position of the ith clutch, and X_sub is the position of the substrate [29]. The substrate position is determined through an elastic force balance:
K_sub × X_sub = K_c × ∑(X_i - X_sub) [30]
The stochastic binding and unbinding of clutches follows first-order kinetics, with the Bell model describing force-dependent unbinding:
k_off* = k_off × exp(F_clutch / F_b) [30]
Where koff is the unloaded off-rate, and Fb is the characteristic bond rupture force [30].
Master Equation Formulation
A master equation-based ordinary differential equation (ODE) approach provides a mean-field treatment of the stochastic motor-clutch model, enabling more computationally efficient analysis of system behavior [30]. The change in probability that a clutch is bound (p_b) is given by:
dp_b/dt = (1 - p_b) × k_on - p_b × 〈k_off*〉 [30]
This formulation allows derivation of an analytical expression for a cell's optimum stiffness (the stiffness at which traction force is maximal) as a function of key cell-specific parameters [30]. The fundamental controlling parameters are the numbers of motors and clutches (constrained to be nearly equal), and the time scale of the on-off kinetics of the clutches (constrained to favor clutch binding over clutch unbinding) [30].
Table 1: Core Parameters in Motor-Clutch Models
| Parameter | Symbol | Description | Typical Units |
|---|---|---|---|
| Number of motors | n_m | Myosin II motors generating tension | dimensionless |
| Number of clutches | n_c | Integrin-based adhesion complexes | dimensionless |
| Clutch spring constant | K_c | Stiffness of individual clutches | pN/nm |
| Substrate spring constant | K_sub | Stiffness of extracellular substrate | pN/nm |
| Unloaded actin velocity | V_u | Maximum retrograde flow velocity | nm/s |
| Motor stall force | F_m | Force at which motor velocity reaches zero | pN |
| Bond rupture force | F_b | Characteristic force for clutch failure | pN |
| Clutch on-rate | k_on | Rate of clutch binding | sâ»Â¹ |
| Clutch off-rate | k_off | Unloaded rate of clutch unbinding | sâ»Â¹ |
Advanced Model Developments
Generalized Motor-Clutch Framework
Recent work has generalized the motor-clutch analytical framework to include imbalanced motor-clutch regimes, clutch reinforcement, and catch bond behavior [28]. This generalized approach investigates optimality with respect to all parameters and reveals that traction force is strongly influenced by clutch stiffness, with the discovery of an optimal clutch stiffness that maximizes traction force [28]. This suggests cells could tune their clutch mechanical properties to perform specific functions. On rigid substrates, the mean-field analysis identifies optimal motor properties, suggesting cells could regulate their myosin repertoire and activity to maximize force transmission [28]. Additionally, clutch reinforcement shifts the optimum substrate stiffness to larger values, whereas the optimum substrate stiffness is insensitive to clutch catch bond properties [28].
Whole-Cell Migration Simulator
To bridge the gap between molecular-scale clutch dynamics and whole-cell behavior, researchers have developed a stochastic whole-cell migration simulator built from the motor-clutch model [33]. This simulator links together multiple motor-clutch "modules" that each exert force on a central cell body, with cell migration arising from force balances among these modules [33]. The simulator predicts a stiffness optimum for cell migration that can be shifted by altering the numbers of active molecular motors and clutches [33]. Experimental tests with U251 glioma cells and embryonic chick forebrain neurons confirmed these predictions, showing that coordinate changes in motor and clutch numbers can shift the optimal stiffness for migration by orders of magnitude [33].
Table 2: Motor-Clutch Model Predictions and Experimental Validations
| Cell Type | Predicted Optimal Stiffness | Experimentally Confirmed Optimum | Key Regulators |
|---|---|---|---|
| Embryonic chick forebrain neurons | ~1 kPa | ~1 kPa | Low numbers of motors and clutches |
| U251 glioma cells | ~100 kPa | ~100 kPa | High numbers of motors and clutches |
| Drug-inhibited U251 cells | Shift to lower stiffness | Confirmed shift | Reduced myosin II and integrin activity |
Experimental Methodologies
Traction Force Microscopy
Traction force microscopy provides essential experimental validation for motor-clutch model predictions. This technique involves culturing cells on compliant substrates with embedded fluorescent beads, then imaging bead displacements as cells exert traction forces [33]. Computational algorithms calculate traction vectors from displacement fields, allowing quantification of total strain energy and force magnitudes [33]. For U251 glioma cells, this method confirmed they transmit approximately two orders of magnitude more force than embryonic chick forebrain neurons, consistent with predictions of increased motors and clutches in glioma cells [33].
F-Actin Retrograde Flow Measurement
Measuring F-actin retrograde flow rate provides critical insights into motor-clutch dynamics. This typically involves transfection with EGFP-actin and time-lapse imaging of actin dynamics at cell edges [33]. Kymograph analysis from these images quantifies flow rates, with the motor-clutch model predicting minimal flow at optimal stiffness [33]. Experimental measurements show ECFNs have minimal flow at ~1 kPa, while U251 glioma cells exhibit minimal flow at ~100 kPa, consistent with their different motor-clutch compositions [33].
Modulating Motor and Clutch Activity
Drug inhibition studies provide direct experimental manipulation of motor-clutch components. Simultaneous inhibition of myosin II motors (e.g., with blebbistatin) and integrin-mediated adhesions (e.g., with RGD peptides or integrin-blocking antibodies) shifts the stiffness optimum of U251 glioma cell migration, morphology, and F-actin retrograde flow rate to lower stiffness values [33]. This experimental approach directly tests model predictions about coordinate regulation of motors and clutches.
Application to Bone Organoid Research
Bone Organoid Development Framework
Bone organoid technology has evolved through a systematic five-stage iterative framework: 1.0 (physiological model), 2.0 (pathological model), 3.0 (structural model), 4.0 (composite model), and 5.0 (applied model) [26]. This progression represents advancement from basic physiological modeling to advanced, clinically applicable systems. The motor-clutch model provides theoretical guidance for optimizing mechanical cues at each stage, particularly in stages 3.0 and 4.0 where structural complexity and multi-tissue interactions are introduced [26].
Recent methodology developments have established cost-effective, well-characterized three-dimensional bone organoid models derived from murine cell lines [34]. These 3D murine-cell-derived bone organoid models (3D-mcBOM) use pre-osteoblast murine cell lines seeded into hydrogel extracellular matrices that differentiate into functional osteoblasts, mineralizing the hydrogel ECM and depositing hydroxyapatite into bone-like organoids [34]. The mechanical properties of these hydrogel systems directly influence osteogenic differentiation through motor-clutch mediated mechanosensing.
Mechanoregulation of Bone Cell Differentiation
The motor-clutch framework explains how osteoblasts and osteoclasts sense and respond to mechanical cues during bone organoid development. Osteoblasts derived from mesenchymal stromal/stem cells migrate to bone remodeling sites and differentiate under influence of various factors including bone morphogenic proteins (BMPs) and phosphate-containing compounds [34]. When osteoblasts become surrounded by bone matrix, they differentiate into osteocytes that maintain important mechano-sensing capabilities and regulate bone structure and remodeling in a load/stress-dependent manner [34].
In the 3D-mcBOM system, osteoblastogenic conditioning significantly increases levels of the transcription factor Runx2, with BMP2 identified as necessary for osteoblast differentiation [34]. Similarly, osteoclastogenic conditioning of RAW 264.7 cells significantly increases levels of TRAP protein, indicating phenotypic differentiation to osteoclasts [34]. These differentiation processes are mechanically regulated through motor-clutch mechanisms that sense substrate stiffness and viscoelasticity.
Optimizing Organoid Mechanical Properties
The generalized motor-clutch model provides specific guidance for maximizing accuracy of cell-generated force measurements in molecular tension sensors by designing mechanosensitive linker peptides to be as stiff as possible [28]. For bone organoid construction, this suggests that clutch stiffness optimization could enhance mechanical signaling fidelity. Additionally, the finding that cells can tune their motor-clutch parameters to sense specific stiffness ranges [28] [33] informs the design of biomaterials that match the mechanical properties of native bone tissue (which varies from ~100s of Pascals in trabecular bone to 10s of GPa in cortical bone) [35].
The recognition that tissues exhibit complex viscoelastic behavior rather than simple elasticity [35] further refines application of the motor-clutch model to bone organoids. As bone organoids advance through the developmental framework, incorporating viscoelastic matrices that better mimic native tissue mechanics will enhance their physiological relevance and predictive power for studying bone diseases and regenerative therapies [35] [26].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Motor-Clutch and Bone Organoid Research
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Polyacrylamide hydrogels | Tunable elastic substrates for stiffness screening | Testing cell migration, spreading, and traction forces across stiffness gradients [35] [33] |
| Polydimethylsiloxane (PDMS) | Elastic polymer for cell culture substrates | Creating substrates with defined mechanical properties [35] |
| Matrigel | Basement membrane matrix for 3D culture | Supporting organoid development and cell-ECM interactions [34] |
| Gelatin methacryloyl (GelMA) | Photocrosslinkable hydrogel for bioprinting | Creating 3D bone organoids with tunable mechanical properties [26] |
| Hydroxyapatite-blended bioinks | Mineralized matrix for bone tissue engineering | Recapitulating bone ECM architecture and mineralization [26] |
| Blebbistatin | Myosin II inhibitor for motor perturbation | Testing motor-clutch predictions by reducing motor activity [33] |
| RGD peptides | Integrin-binding adhesion blockers | Inhibiting clutch engagement to test model predictions [33] |
| BMP2 | Osteogenic differentiation factor | Promoting osteoblast differentiation in bone organoids [34] |
| RANKL | Osteoclast differentiation factor | Inducing osteoclast formation in bone organoid systems [34] |
| BOC-FlFlF | Boc-Phe-Leu-Phe-Leu-Phe|FPR Antagonist | |
| GRGDSPK | GRGDSPK, CAS:111119-28-9, MF:C28H49N11O11, MW:715.8 g/mol | Chemical Reagent |
The motor-clutch model continues to evolve, with recent generalizations incorporating more biological complexity such as clutch reinforcement and catch bond behavior [28]. These advances reveal novel features that can affect the design of molecular tension sensors and provide a generalized analytical framework for predicting and controlling cell adhesion and migration in immunotherapy and cancer [28]. For bone organoid research, integrating these refined motor-clutch principles will enhance the physiological relevance of engineered bone tissues.
The five-stage iterative framework for bone organoid development [26] provides a systematic approach for advancing from basic physiological models to clinically applicable systems. Throughout this progression, the motor-clutch model offers theoretical guidance for optimizing mechanical cues that drive osteogenic differentiation and bone tissue formation. As bone organoid technology incorporates advanced technologies like artificial intelligence and 3D bioprinting [26], motor-clutch principles will inform the design of systems that better recapitulate native bone mechanobiology.
In conclusion, the motor-clutch model provides an essential theoretical framework for understanding cellular force transmission that directly applies to the evolving field of bone organoid research. By elucidating how cells sense and respond to mechanical cues through coordinated motor-clutch interactions, this model guides the optimization of biomaterial properties and culture conditions for developing physiologically relevant bone organoids with enhanced translational potential for regenerative medicine and orthopedic therapies.
Engineering Mechanical Stimulation: Techniques for Directing Bone Organoid Fate
The emergence of bone organoid technology represents a transformative advance in the study of skeletal biology, disease modeling, and drug screening. These three-dimensional (3D) biomimetic constructs recapitulate key aspects of bone architecture and function, providing an unprecedented platform for investigating bone development and pathology in vitro [4]. However, a significant technical barrier has been the difficulty in replicating the native bone mechanical microenvironment within these model systems. Bone is a dynamic tissue whose development, homeostasis, and regenerative capacity are profoundly regulated by mechanical cues [4]. Conventional 3D culture systems, including those utilizing Matrigel, lack the spatiotemporal control of mechanical properties necessary to dissect mechanotransductive mechanisms in organoids [18]. This limitation impedes the formation of fully functional bone organoids that can accurately model the complexity of native bone tissue.
The design of hydrogels with bone-mimetic stiffness addresses this fundamental challenge. By engineering biomaterials that precisely recapitulate the mechanical properties of the native bone extracellular matrix (ECM), researchers can create engineered microenvironments that guide stem cell differentiation toward osteogenic lineages and support the maturation of bone organoids [18] [36]. These advanced hydrogel systems represent a paradigm shift in bone tissue engineering, moving beyond static scaffolds to dynamic, instructive matrices that actively participate in regulating cellular behavior. This technical guide explores the design principles, fabrication methodologies, and experimental applications of mechanically tuned hydrogels, framing them within the broader context of controlling mechanical cues for bone organoid differentiation and maturation research.
Mechanical Cues in Bone Development and Organoid Maturation
Biomechanical Regulation of Bone Biology
Native bone tissue possesses a complex hierarchical structure that confers exceptional mechanical strength and load-bearing capacity. This organization ranges from nanoscale collagen fibrils to trabecular and cortical architectures [4]. The bone ECM is a precise inorganic-organic composite, with the inorganic component consisting of carbonate-substituted calcium-deficient apatite and the organic fraction comprising primarily type I collagen (90%) along with proteoglycans and non-collagenous proteins [37]. This composite structure creates a mechanically dynamic environment where cells experience and respond to physical forces through mechanotransduction pathways.
Mechanical forces play a critical role in bone development by regulating cellular behaviors such as proliferation, differentiation, and matrix mineralization [4]. Osteoblasts, osteocytes, and mesenchymal stem cells (MSCs) are particularly sensitive to their mechanical environment, converting physical stimuli into biochemical signals that dictate lineage commitment and tissue formation. Dynamic loading promotes osteogenic differentiation of MSCs and enhances endothelial network formation, thereby supporting the coordinated development of vascularized bone tissue [4]. In conventional organoid cultures, which are maintained in static suspension or hydrogels, the absence of these essential mechanical cues often leads to deviations in osteogenic differentiation from physiological conditions, limiting the physiological relevance of the resulting models.
Current Limitations in Bone Organoid Technology
Despite significant advances, bone organoid construction faces several technical challenges related to mechanical stimulation:
- Lack of Physiological Mechanical Environment: Most organoid cultures are maintained in static conditions, lacking the mechanical cues native bone cells experience in vivo [4].
- Insufficient Structural Complexity: Conventional hydrogels fail to replicate the spatiotemporal mechanical heterogeneity of native bone ECM [18].
- Vascularization Deficit: The absence of vascular networks restricts organoid size and functionality, with mechanical factors playing a crucial role in vascular formation [4].
- Scaffold Limitations: Matrigel, a commonly used basement membrane extract, exhibits batch-to-batch variability, contains murine proteins, and possesses limited mechanical strength unsuitable for bone mimicry [4].
These limitations collectively impede the development of bone organoids with physiological relevance. Without proper mechanical stimulation, bone organoids fail to achieve the maturity, functionality, and structural organization necessary for accurate disease modeling and drug screening applications.
Hydrogel Design Principles for Bone-Mimetic Mechanics
Key Mechanical Properties and Their Biological Significance
Designing hydrogels with bone-mimetic properties requires careful consideration of multiple mechanical parameters that collectively influence cellular behavior. The table below summarizes these key properties and their roles in bone organoid development.
Table 1: Key Mechanical Properties in Hydrogel Design for Bone Organoids
| Mechanical Property | Biological Significance | Target Range for Bone | Cellular Response |
|---|---|---|---|
| Stiffness (Elastic Modulus) | Guides osteodifferentiation through mechanosensing | 10-40 kPa [18] | Activates YAP/TAZ signaling, promotes osteogenic gene expression |
| Viscoelasticity | Recapitulates stress relaxation of native ECM | Stress relaxation: 40-80% in 1-3 hours [18] | Enhances cell spreading, proliferation, and matrix deposition |
| Mechanical Heterogeneity | Mimics varying stiffness across bone regions | Spatially patterned stiffness gradients [36] | Directs spatially organized differentiation |
| Degradation Rate | Synchronizes with new tissue deposition | Tunable via crosslinker chemistry [36] | Enables cell migration and matrix remodeling |
Material Systems for Mechanically Tunable Hydrogels
Various natural, synthetic, and hybrid polymers are employed to achieve the mechanical properties outlined above:
- Natural Polymers: Alginate, collagen, and decellularized ECM components provide biocompatibility and cell adhesion motifs but often lack sufficient mechanical strength for bone mimicry without modification [37].
- Synthetic Polymers: Polyethylene glycol (PEG) and polyacrylamide offer precise control over mechanical properties and reproducible fabrication but require functionalization with adhesive ligands to support cell attachment [36].
- Hybrid Systems: Combining natural and synthetic polymers leverages the advantages of both, creating hydrogels with tailored mechanics and bioactivity. For example, PEG-dextran systems with interfacial protein self-assembly create macroporous structures with shell-hardened mechanical properties [36].
The selection of base materials significantly impacts the resulting hydrogel's mechanical behavior, degradation profile, and bioactivity. Researchers must consider the specific requirements of their bone organoid system when selecting material components.
Advanced Hydrogel Systems with Programmable Mechanics
Shell-Hardened Macroporous Hydrogels
A groundbreaking approach in bone-mimetic hydrogel design involves the creation of shell-hardened macroporous hydrogels with spatiotemporally programmed mechanical properties [36]. These systems address the challenge of maintaining mechanical integrity while supporting cell proliferation and tissue deposition. The fabrication process employs a soft-templating technique based on liquid-liquid phase separation between polyethylene glycol (PEG) and dextran, with PEG serving as the percolating phase and dextran forming nonpercolating droplets that template macropore formation.
The key innovation lies in the interfacial supramolecular self-assembly of protein fibers at the phase boundary, creating a rigid pore shell that provides sustained mechanical cues for guiding osteodifferentiation. The macroporous structure provides ample space to prevent contact inhibition during stem cell proliferation, while the rigid protein fiber-coated pore shell protects cells against mechanical loads and guides osteogenic differentiation. Temporally, the hydrogel exhibits tunable degradation rates that can synchronize with new tissue deposition through the use of mixed crosslinkers with degradable ester bonds and stable acrylamide bonds [36].
Table 2: Composition and Function of Shell-Hardened Macroporous Hydrogels
| Component | Function | Experimental Implementation |
|---|---|---|
| PEG-Dextran System | Liquid-liquid phase separation to create macroporous template | 80 mg/mL PEG, 50 mg/mL dextran [36] |
| Lysozyme Nanofibers | Interfacial self-assembly to form rigid pore shells | Acrylate-modified for covalent attachment to matrix [36] |
| Dual Crosslinkers | Control degradation rate to match tissue formation | PEG-ACLT (degradable) and PEG-ACA (non-degradable) [36] |
| Acrylated RGD | Promote cell adhesion and integrin signaling | Incorporated during polymerization [36] |
Experimental Protocol: Fabrication and Cell Encapsulation
The following detailed methodology outlines the fabrication of shell-hardened macroporous hydrogels for bone organoid culture:
Preparation of Phase-Separated Precursor:
- Dissolve PEG (80 mg/mL) and dextran (50 mg/mL) in aqueous solution containing the photoinitiator LAP (2 mM).
- Add acrylamide monomer (10-20% w/v), PEG-ACLT and PEG-ACA crosslinkers (total 3-5 mM), and acrylated RGD peptide (1-2 mM).
- Incorporate acrylated lysozyme nanofibers (5-10 mg/mL) for shell formation.
Cell Encapsulation:
- Resuspend mesenchymal stem cells or osteoprogenitor cells (e.g., MC3T3-E1) in the dextran phase at a density of 5-20 million cells/mL.
- Mix the cell suspension with the PEG phase and transfer to culture dishes.
- Allow phase separation to occur (15-30 minutes), resulting in macroporous structures with cell-containing dextran droplets.
Photopolymerization:
- Expose the phase-separated system to blue light (405 nm) at 5-10 mW/cm² for 5-10 minutes to initiate free radical polymerization.
- This step creates a stable hydrogel network with integrated protein shells at the pore interfaces.
Culture and Differentiation:
- Maintain encapsulated cells in osteogenic medium containing β-glycerophosphate (2-10 mM) and ascorbic acid (50-100 μg/mL).
- Change medium every 2-3 days for up to 4 weeks to support extracellular matrix deposition and mineralization [37].
This protocol generates hydrogels with pore sizes of approximately 50 μm after swelling, suitable for cell encapsulation and culture. The shell-hardened macroporous architecture has demonstrated efficacy in supporting stem cell-mediated bone regeneration in both rabbit and porcine models, marking a substantial advancement in tailoring mechanical properties for bone tissue engineering [36].
Mechanotransduction Pathways in Osteodifferentiation
The mechanical properties of hydrogels influence osteogenic differentiation through specific mechanotransduction pathways that convert physical cues into biochemical signals. The diagram below illustrates the primary signaling pathways involved in this process.
Diagram 1: Hydrogel mechanics activate osteogenic signaling through YAP/TAZ pathway.
The mechanical signaling cascade begins with cells sensing hydrogel properties through integrin-mediated adhesion, leading to focal adhesion complex assembly and actin cytoskeleton remodeling. This mechanical activation triggers the nuclear translocation of YAP/TAZ transcriptional coactivators, which directly regulate the expression of osteogenic genes such as RUNX2, osteocalcin, and bone sialoprotein [18]. Stiffness-dependent activation of Notch signaling further enhances this osteodifferentiation process, creating a synergistic effect that promotes bone matrix production and mineralization.
Characterization Techniques for Bone-Mimetic Hydrogels and Organoids
Mechanical and Structural Analysis
Comprehensive characterization of hydrogel mechanical properties and bone matrix deposition is essential for validating bone-mimetic systems:
- Mechanical Testing: Rheological measurements to quantify storage modulus (G'), loss modulus (G"), and stress relaxation properties. Atomic force microscopy (AFM) for localized mechanical mapping of heterogeneity.
- Structural Analysis: Field emission scanning electron microscopy (FESEM) to visualize macroporous architecture and matrix deposition. Laser confocal fluorescence microscopy (LCFM) for 3D reconstruction of hydrogel porosity and cell distribution.
- Chemical Characterization: Fourier-transform infrared spectroscopy (FTIR) to assess mineral composition, and quantitative hydroxyproline assay to measure collagen content [37].
Assessment of Bone Matrix Deposition
Advanced imaging techniques are required to evaluate extracellular matrix production in 3D cultures:
- Second Harmonic Imaging Microscopy (SHIM): Enables label-free visualization of collagen fibrils within 3D hydrogels, leveraging the non-centrosymmetric structure of collagen that generates a strong second harmonic signal [37].
- Multi-Photon Microscopy: Uses infrared radiation to penetrate thick hydrogel samples with minimal scattering, allowing deep imaging of cell morphology and matrix organization.
- Transmission Electron Microscopy (TEM): Provides high-resolution analysis of collagen fibril organization and mineral crystal formation, confirming the native bone-like structure of deposited matrix [37].
These characterization methods collectively provide a comprehensive assessment of hydrogel mechanical properties, structural features, and the resulting bone matrix formation, enabling researchers to optimize systems for bone organoid development.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Bone-Mimetic Hydrogel Experiments
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Polyethylene Glycol (PEG) | Base polymer for hydrogel formation; provides mechanical tunability | Use 4-armed PEG acrylate (PEG-ACLT) with degradable ester bonds and 4-armed PEG acrylamide (PEG-ACA) for stability [36] |
| Dextran | Template for macroporous structure formation via phase separation | Combine with PEG at 50 mg/mL concentration for ~50 μm pores [36] |
| Lysozyme Nanofibers | Interfacial self-assembly to create rigid pore shells | Modify with acryl groups for covalent attachment to hydrogel matrix [36] |
| Acrylated RGD Peptide | Promotes cell adhesion via integrin binding | Incorporate at 1-2 mM during polymerization [36] |
| LAP Photoinitiator | Enables free radical polymerization under blue light | Use at 2 mM concentration with 405 nm light at 5-10 mW/cm² [36] |
| Alginate Hydrogel | Inert encapsulating scaffold for spheroid culture | Non-modified alginate (2% solution) prevents cell adhesion to dish surface [37] |
| Osteogenic Medium Supplements | Induces osteogenic differentiation | 50 μg/mL ascorbic acid 2-phosphate + 2-10 mM β-glycerophosphate [37] |
| AHK | AHK, CAS:126828-32-8, MF:C15H26N6O4, MW:354.41 g/mol | Chemical Reagent |
| N-Acetyl-L-arginine | N-Acetyl-L-arginine|High-Purity Reagent|RUO | N-Acetyl-L-arginine (NALA) is an enhanced protein aggregation suppressor for biopharmaceutical research. For Research Use Only. Not for human use. |
The development of hydrogels with bone-mimetic stiffness represents a critical advancement in bone organoid engineering. By recreating the mechanical microenvironment of native bone tissue, these biomaterial systems provide essential cues that direct stem cell differentiation, promote matrix mineralization, and support the formation of physiologically relevant bone models. The integration of programmable mechanics—through controlled stiffness, viscoelasticity, degradation, and spatial heterogeneity—enables researchers to overcome traditional limitations of static 3D culture systems.
Future directions in this field will likely focus on increasing complexity and functionality. The integration of bioprinting technologies with mechanically tuned hydrogels promises enhanced spatial patterning and structural fidelity [4]. Vascularization remains a critical challenge, and the development of mechanical cues that support endothelial network formation within bone organoids represents a priority for creating large-scale, functional tissue models. Additionally, the incorporation of dynamic mechanical stimulation through bioreactor systems will further advance the maturation of bone organoids, better recapitulating the in vivo mechanical environment [4]. As these technologies converge, hydrogel systems with bone-mimetic mechanics will accelerate progress in personalized medicine, disease modeling, and drug screening for skeletal disorders.
The integration of three-dimensional (3D) bioprinting technologies into bone tissue engineering represents a paradigm shift in creating architecturally complex scaffolds that recapitulate the native bone microenvironment. Unlike traditional fabrication methods, 3D bioprinting enables precise spatial control over scaffold architecture, cellular distribution, and biochemical cues at resolutions critical for directing bone organoid differentiation and maturation. This technical capability is particularly vital for mimicking the mechanically dynamic environment of native bone tissue, where structural cues directly influence cellular behavior through mechanotransduction pathways [4] [5]. The emerging field of volumetric bioprinting further expands these capabilities by enabling rapid fabrication of complex structures without layer-by-layer deposition, potentially overcoming significant limitations in creating vascularized bone constructs.
Within the context of bone organoid research, scaffold architecture serves not merely as a structural template but as an active signaling component that guides stem cell fate through biomechanical stimulation. The mechanical properties of scaffolds—including stiffness, porosity, and microarchitecture—directly influence osteogenic differentiation by activating specific cellular signaling pathways that mirror in vivo bone development processes [4]. This technical guide examines current bioprinting methodologies for creating architecturally complex scaffolds, with particular emphasis on how these engineered microenvironments can be leveraged to study the role of mechanical cues in bone organoid differentiation and maturation for advanced drug screening and disease modeling applications.
Core Bioprinting Technologies for Scaffold Fabrication
Comparative Analysis of 3D Bioprinting Techniques
Table 1: Technical Specifications of Primary 3D Bioprinting Modalities
| Technique | Working Principle | Resolution | Speed | Suitable Materials | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Extrusion-Based | Pneumatic or mechanical deposition of continuous bioink filaments [38] | 50-500 μm [39] | Medium | High-viscosity hydrogels (alginate, GelMA, hyaluronic acid), cell-laden bioinks [38] [39] | High cell density capability, structural stability [40] | Potential shear stress on cells, limited resolution [40] |
| Laser-Assisted (LAB) | Laser-induced forward transfer of bioink droplets [38] | 10-50 μm [39] | Slow | Biological materials coated on energy-absorbing layer [38] | High resolution, minimal cell damage, no nozzle clogging [39] | Low throughput, complex setup, high cost [39] |
| Inkjet-Based | Thermal or piezoelectric droplet ejection [38] | 50-300 μm [39] | Fast | Low-viscosity bioinks [38] | High speed, low cost [39] | Limited material viscosity, potential nozzle clogging, lower cell density [40] |
| Light-Curing (SLA/DLP) | Photopolymerization of photosensitive resins layer-by-layer [39] | 10-100 μm [39] | Medium to Fast | Photosensitive hydrogels, ceramics [39] | High resolution, smooth surface finish [39] | Potential cytotoxicity of photoinitiators, limited biodegradable options [39] |
| Selective Laser Sintering (SLS) | Laser fusion of powder particles [39] | 50-200 μm [39] | Medium | Thermoplastics (PLA), bioceramics (HA) [39] | No support structures needed, high mechanical strength [39] | High processing temperature unsuitable for live cells, post-processing required [39] |
Emerging Volumetric Bioprinting Approaches
Volumetric bioprinting represents a revolutionary approach that deviates from traditional layer-by-layer fabrication by creating entire structures simultaneously through computed axial lithography. This technique projects dynamically evolving light patterns into a rotating volume of photosensitive bioink, enabling rapid fabrication of complex geometric structures with continuous fluid channels ideally suited for vascular network integration [39]. While specific technical parameters for bone applications remain under investigation, preliminary studies demonstrate the ability to produce structures with feature sizes below 100 μm in minutes rather than hours—a critical advancement for creating perfusable vascular networks within bone organoids that address current diffusion limitations [4].
The non-layerwise nature of volumetric printing enables creation of intricate internal channels and overhanging structures without temporary supports, making it particularly suitable for replicating bone's complex porous architecture and integrating vascular networks essential for nutrient delivery in larger bone organoids [4]. Additionally, the absence of shear stress during the printing process potentially enhances cell viability compared to extrusion-based methods, addressing a significant challenge in creating high-density cellular constructs [40].
Biomaterial Strategies for Mechanically Functional Scaffolds
Bioink Composition and Properties
Table 2: Essential Bioink Components for Bone Organoid Scaffolds
| Material Category | Specific Examples | Key Properties | Role in Mechanical Signaling | Limitations |
|---|---|---|---|---|
| Natural Polymers | Gelatin methacryloyl (GelMA), alginate, hyaluronic acid, collagen [38] [39] | Biocompatibility, cell adhesion motifs, tunable physical properties [38] | Modifiable stiffness to mimic bone matrix (~20-40 kPa for osteogenic differentiation) [4] | Limited mechanical strength, batch-to-batch variability [4] |
| Synthetic Polymers | Poly(ε-caprolactone) (PCL), polylactic acid (PLA), polyethylene glycol (PEG) [38] [39] | Consistent properties, tunable degradation rates, enhanced printability [39] | Provides structural integrity and controlled mechanical environment [39] | Lack of natural bioactive sites, potential acidic degradation products [39] |
| Ceramic Materials | Hydroxyapatite (HA), tricalcium phosphate [39] | Osteoconductivity, compression resistance, bone-like composition [39] | Enhances mechanical competence and mineralized matrix deposition [26] | Brittleness, processing challenges [39] |
| Composite Bioinks | GelMA-HA, alginate-nanosilicate, PCL-HA [26] [39] [40] | Combines advantages of multiple material classes [39] | Enables replication of bone's hierarchical mechanical properties [26] | Optimization complexity for printability and bioactivity [40] |
Functionalization Strategies for Enhanced Osteogenic Cues
Advanced bioink formulations incorporate specific osteoinductive factors to enhance bone organoid maturation. Nanosilicate additives serve dual purposes: providing mechanical reinforcement through nano-scale reinforcement and delivering osteoinductive ions (silicon, magnesium) that activate osteogenic gene expression [40]. Similarly, incorporation of hydroxyapatite nanoparticles within bioinks not only improves mechanical properties but also enhances bioactivity by mimicking bone's natural mineral phase, promoting osteoblast differentiation and matrix mineralization [26] [39].
Growth factor delivery systems represent another critical functionalization strategy. Controlled release of bone morphogenetic proteins (BMP-2, BMP-7) or transforming growth factor-beta (TGF-β) from microspheres or within bioink matrices provides sustained biochemical stimulation that works synergistically with mechanical cues to direct stem cell differentiation toward osteogenic lineages [5]. These functionalized bioinks create scaffolds that actively participate in the bone formation process rather than serving as passive structural templates.
Experimental Protocols for Mechanically-Active Bone Organoid Construction
Protocol 1: Extrusion Bioprinting of Mineralizing Bone Organoids
Step 1: Bioink Preparation
- Formulate a composite bioink containing 7% (w/v) GelMA, 2% (w/v) alginate methacrylate, and 2% (w/v) nano-hydroxyapatite particles [26].
- Mix primary human mesenchymal stem cells (hMSCs) at a density of 10×10^6 cells/mL into the bioink solution, maintaining temperature at 4°C to prevent premature crosslinking [40].
- Centrifuge the cell-bioink mixture at 300×g for 30 seconds to remove air bubbles that may compromise print fidelity.
Step 2: Bioprinting Process
- Load the bioink into a temperature-controlled extrusion cartridge maintained at 18-20°C.
- Utilize a 22G nozzle (410 μm inner diameter) with pneumatic pressure settings between 20-25 kPa to achieve consistent filament deposition [40].
- Print onto a stage maintained at 37°C using a layer height of 150 μm and printing speed of 8 mm/s.
- Apply immediate post-printing crosslinking using 365 nm UV light at 5 mW/cm² for 60 seconds followed by immersion in 100 mM CaCl₂ solution for ionic crosslinking of alginate components [26].
Step 3: Dynamic Culture and Mechanical Stimulation
- Transfer printed constructs to bioreactor systems capable of applying cyclic mechanical strain (1-5% elongation, 1 Hz frequency) or fluid shear stress through perfusion culture [4].
- Maintain in osteogenic differentiation medium (DMEM supplemented with 10 mM β-glycerophosphate, 50 μg/mL ascorbic acid, and 100 nM dexamethasone) with medium changes every 3 days [5].
- Culture for 21-28 days to allow for substantial matrix mineralization and osteogenic maturation.
Protocol 2: Volumetric Bioprinting of Vascularized Bone Organoids
Step 1: Bioink Formulation for Volumetric Printing
- Prepare a photosensitive bioink comprising 7.5% (w/v) GelMA, 0.1% (w/v) LAP photoinitiator, and 3% (w/v) polyethylene glycol diacrylate (PEGDA) as a rheology modifier [39].
- Incorporate human umbilical vein endothelial cells (HUVECs) at 5×10^6 cells/mL and hMSCs at 10×10^6 cells/mL, maintaining cell viability through gentle mixing.
Step 2: Volumetric Printing Process
- Transfer 5 mL of cell-laden bioink to a cylindrical glass vial (25 mm diameter).
- Execute computed axial lithography using a digital light processing (DLP) projector with 405 nm wavelength, rotating the vial through 360° in 2° increments while projecting calculated light patterns based on the target structure [39].
- Maintain exposure intensity below 50 mW/cm² to minimize phototoxic effects on encapsulated cells.
- Complete the printing process within 2-3 minutes to ensure high cell viability post-fabrication.
Step 3: Post-Printing Culture and Maturation
- Gently transfer the printed construct to perfusion bioreactor systems to enhance nutrient delivery to the internal vascular channels.
- Culture in endothelial growth medium-2 for the first 7 days to promote endothelial network formation, then switch to osteogenic medium for subsequent bone matrix deposition.
- Apply intermittent hydrostatic pressure (10-20 kPa, 0.5 Hz) to mimic physiological mechanical loading conditions known to enhance both vascular organization and osteogenic differentiation [4].
Mechanotransduction Pathways in Bone Organoid Maturation
The architectural features of 3D bioprinted scaffolds directly influence bone organoid maturation through activation of specific mechanotransduction pathways. These pathways convert mechanical stimuli from the scaffold environment into biochemical signals that direct cellular differentiation and function.
Diagram 1: Core Mechanotransduction Pathways in Bone Organoid Differentiation (82 characters)
Scaffold stiffness directly influences the activation of YAP/TAZ transcriptional regulators, which translocate to the nucleus in response to mechanical cues and activate expression of osteogenic genes such as RUNX2 and osteocalcin [4]. Simultaneously, fluid shear stress resulting from perfusion culture or mechanical loading activates calcium signaling and MAPK pathways that further enhance osteogenic differentiation. These mechanotransduction pathways work synergistically with biochemical cues to drive the expression of bone-specific markers and ultimately facilitate matrix mineralization—a critical endpoint in bone organoid maturation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Bioprinted Bone Organoids
| Category | Specific Reagents | Function | Application Notes |
|---|---|---|---|
| Stem Cell Sources | Human mesenchymal stem cells (hMSCs), induced pluripotent stem cells (iPSCs) [41] [5] | Self-renewal capacity, multi-lineage differentiation potential including osteogenic lineage [41] | Patient-specific iPSCs enable personalized disease modeling; hMSCs offer well-characterized osteogenic potential [41] |
| Bioink Polymers | Gelatin methacryloyl (GelMA), hyaluronic acid methacrylate, alginate [38] [39] | Provide 3D scaffold structure, cell adhesion sites, tunable physical properties [38] | GelMA offers excellent cell compatibility; alginate provides rapid ionic crosslinking; often used in combination [38] |
| Osteoinductive Additives | Nano-hydroxyapatite, β-tricalcium phosphate, bioactive glass [26] [39] | Enhance osteoconductivity, improve mechanical properties, mimic bone mineral phase [26] [39] | Concentration typically 1-5% (w/v); higher concentrations may compromise printability [26] |
| Growth Factors | Bone morphogenetic proteins (BMP-2, BMP-7), transforming growth factor-β (TGF-β) [5] | Direct stem cell differentiation toward osteogenic lineage, enhance bone matrix production [5] | Often incorporated via encapsulation in microspheres for sustained release; typical concentrations 10-100 ng/mL [5] |
| Crosslinking Systems | Calcium chloride, UV light with photoinitiators (LAP, Irgacure 2959) [26] [39] | Stabilize printed structures, provide mechanical integrity [26] | Ionic crosslinkers for alginate; photointitiators for light-curable polymers; concentration critical for cell viability [26] |
| 3-Methyl-L-Histidine | 3-Methyl-L-Histidine, CAS:368-16-1, MF:C7H11N3O2, MW:169.18 g/mol | Chemical Reagent | Bench Chemicals |
| Aminoadipic acid | Aminoadipic acid, CAS:542-32-5, MF:C6H11NO4, MW:161.16 g/mol | Chemical Reagent | Bench Chemicals |
The convergence of 3D bioprinting technologies with advanced biomaterial strategies has created unprecedented opportunities for constructing architecturally complex scaffolds that actively direct bone organoid maturation through mechanical cues. The continuing evolution of these fabrication approaches, particularly through emerging volumetric bioprinting methods, promises to overcome current limitations in vascularization and scale that have constrained bone organoid development. As these technologies mature, they will increasingly enable researchers to create increasingly sophisticated bone models that more faithfully recapitulate the mechanical and biological complexity of native bone tissue, thereby accelerating both fundamental research in bone biology and translational applications in drug screening and regenerative medicine. The precise control over scaffold architecture afforded by these bioprinting technologies represents a critical enabling capability for systematically investigating the role of mechanical cues in bone organoid differentiation and maturation—a fundamental relationship with profound implications for understanding skeletal development, disease pathogenesis, and therapeutic interventions.
The development of physiologically relevant bone organoids represents a transformative approach in regenerative medicine, disease modeling, and drug development. Unlike traditional two-dimensional cultures, bone organoids are three-dimensional multicellular structures that recapitulate key architectural and functional features of native bone tissue [42]. However, current organoid models face significant challenges in achieving full functional maturation, largely because they often lack the dynamic biomechanical environment essential for bone development and homeostasis [17]. In vivo, bone cells are continuously exposed to various mechanical forces—including cyclic strain from muscular activity and compression from weight-bearing—that play a crucial role in directing cellular differentiation, tissue organization, and functional maturation [42] [43]. The emerging field of mechanobiological engineering highlights the critical role of matrix-derived physical and mechanical properties in directing organoid morphogenesis [17].
Mechanotransduction—the process by which cells convert mechanical stimuli into biochemical signals—governs fundamental cellular processes in bone development, including osteogenic differentiation, matrix mineralization, and tissue remodeling [17]. Transmembrane receptors such as integrins link the extracellular matrix to the cytoskeleton, initiating focal adhesion assembly and downstream activation of mechanosensitive signaling pathways including YAP/TAZ, Wnt/β-catenin, and MAPK/ERK [17]. For bone organoids to accurately mimic native tissue functionality, they must experience mechanical cues that replicate this natural mechanobiological environment. This technical guide explores the design principles, operational parameters, and experimental methodologies for bioreactor systems that apply controlled cyclic strain and compression to bone organoids, with a specific focus on enhancing their differentiation and maturation for research and therapeutic applications.
Fundamental Principles of Bone Mechanobiology
Cellular Mechanosensing in Bone Tissue
Bone tissue contains multiple cell types that respond to mechanical stimuli. Osteocytes, which comprise up to 95% of all bone cells in mineralized tissue, are particularly robust responders and translators of mechanical force [42]. These cells form an extensive network within the bone matrix and serve as primary mechanosensors [42]. In response to mechanical loading, osteocytes reduce production of inhibitors like Dickkopf-related protein 1 (DKK1) and sclerostin, thereby stimulating osteoblasts to produce more bone tissue through activation of WNT-β-catenin signaling [42]. Conversely, during mechanical unloading, osteocytes express receptor activator of nuclear factor kappa B ligand (RANKL), which activates osteoclasts and promotes bone resorption [42].
Osteoblasts, the bone-forming cells, also respond to mechanical stimuli by altering their synthetic activity. These polarized, cuboidal, mononuclear cells synthesize and secrete a distinctive extracellular matrix composed of osteocalcin, osteopontin, alkaline phosphatase, and significant amounts of type I collagen [42]. Mechanical loading enhances this synthetic activity and promotes osteoblast differentiation from mesenchymal stem cells and pre-osteoblasts [42]. The development of osteoblast lineage cells follows a complex and dynamic pathway from mesenchymal progenitors to preosteoblasts, mature osteoblasts, bone-lining cells, and ultimately osteocytes, with mechanical cues influencing each stage of this differentiation process [42].
Key Mechanotransduction Pathways
The following diagram illustrates the primary mechanotransduction pathways through which bone cells convert mechanical stimuli into biochemical responses:
Mechanotransduction Pathways in Bone Cells
Bioreactor Engineering and Design Parameters
Material Considerations for Bioreactor Construction
The selection of appropriate materials is critical for bioreactor design, particularly when creating systems for mechanical stimulation of bone organoids. Materials must meet specific physical, chemical, and biological requirements to ensure proper function, sterility, and compatibility with cell culture [44]. The following table summarizes key material considerations for bioreactor construction:
Table 1: Bioreactor Material Selection Criteria
| Criteria | Additional Considerations | Recommended Materials |
|---|---|---|
| Transparency | Necessary for visual monitoring and microscopy | Polycarbonate, Polystyrene, PDMS |
| Light Sensitivity | Placement location and light sensitivity of culture media | Polycarbonate, Acrylic (PMMA) |
| Non-leachable | Fluid path must meet industry guidance (BPOG, USP) | PTFE, Stainless Steel, C-Flex |
| Non-degradable | Resistance to hydrolysis in culture medium | PTFE, PEEK, Stainless Steel |
| Tissue Culture Compatibility | Known interactions with buffers/media/DMSO | Polystyrene, Glass, PDMS |
| Sterilization Technique | Autoclave, gamma radiation, or EO gas compatibility | Polycarbonate, PDMS, PTFE, PEEK |
| Manufacturing Considerations | Mass production, molding, or 3D printing capability | PDMS, Polycarbonate, Acrylic |
| Material Quality/Consistency | cGMP-grade requirement and documentation | PEEK, Stainless Steel, PTFE |
Polydimethylsiloxane (PDMS) has emerged as a particularly valuable material for constructing deformable substrates within stretch bioreactors due to its high biocompatibility, versatility, and ability to be cast in tailored shapes [43]. However, PDMS substrates present some limitations, including intrinsic surface hydrophobicity that requires additional surface functionalization to improve cell adhesion, and mechanical properties sensitive to manufacturing processes that may lead to non-uniform strain distribution [43]. For compression systems, polycarbonate and acrylic are commonly used for their rigidity, transparency, and gas sterilization compatibility [44].
Mass Transfer and Environmental Control
A critical engineering parameter in bioreactor design is mass transfer, including the delivery of oxygen and nutrients to the tissue construct and removal of metabolic wastes [44]. The absence of a vascular network in engineered bone organoids represents a principal limiting factor in maintaining cell survival during preconditioning and tissue maturation [44]. Bioreactor systems must therefore incorporate mechanisms for efficient mass transfer, typically through perfusion systems that circulate culture media through or around the developing organoids. For bone organoids specifically, oxygen tension plays a particularly important role as it influences osteogenic differentiation and bone formation processes [44].
Advanced bioreactor systems incorporate real-time monitoring sensors to track critical parameters including dissolved oxygen, pH, temperature, and glucose concentration [44]. These monitoring capabilities allow for dynamic adjustment of culture conditions to maintain optimal microenvironmental conditions throughout the organoid maturation process. For clinical applications, the integration of in-line quality assurance monitoring is essential for ensuring reproducible and standardized bone organoid production [44].
Experimental Protocols for Mechanical Stimulation
Application of Cyclic Strain
The following workflow diagram outlines a standardized protocol for applying cyclic strain to bone organoids using a bioreactor system:
Cyclic Strain Experimental Workflow
Detailed Protocol Steps:
Substrate Fabrication: Prepare polydimethylsiloxane (PDMS) membranes using a base-to-curing agent ratio of 10:1. Pour the mixture into custom-designed molds and cure at 65°C for 4 hours. The substrate geometry should be optimized to ensure uniform strain distribution during mechanical stimulation [43].
Surface Functionalization: Treat PDMS surfaces with oxygen plasma (100W, 1 minute) to enhance hydrophilicity, then coat with extracellular matrix proteins such as fibronectin (10 µg/mL) or collagen type I (50 µg/mL) to promote cell adhesion [43].
Cell Seeding: Seed human periodontal ligament stem cells (hPDLSCs) or mesenchymal stem cells (MSCs) at a density of 50,000-100,000 cells/cm². Allow cells to adhere for 24-48 hours under standard culture conditions before applying mechanical stimuli [43].
Strain Characterization: Characterize the mechanical behavior of the substrate via finite element analyses and experimental tensile tests combined with digital image correlation (DIC) analyses. This validation is crucial as research has shown that the actual deformation of substrates can be about half of what is expected in some commercial systems [43].
Mechanical Stimulation: Apply intermittent cyclic stretching using optimized parameters. Studies on hPDLSCs have demonstrated that increasing total daily cyclic stretch exposure enhances early response, including cell alignment along the stretch direction and upregulation of both osteogenic and ligament-related gene expression [43].
Biological Analysis: Following stimulation, assess osteogenic differentiation through gene expression analysis (RUNX2, OSX, osteocalcin), protein quantification (alkaline phosphatase activity), and histological staining for mineral deposition (Alizarin Red) [43].
Application of Cyclic Compression
Protocol for Compressive Stimulation:
Construct Preparation: Create bone organoids using mesenchymal stem cells encapsulated in a biomimetic hydrogel such as collagen type I (5-10 mg/mL) or fibrin (5-10 mg/mL). Allow matrix contraction and initial maturation for 7-14 days before mechanical stimulation [42] [5].
Bioreactor Setup: Place organoids in compression bioreactors between impermeable but porous platens to allow fluid expression during compression. Apply unconfined or confined compression based on experimental objectives [44].
Compression Parameters: Apply dynamic compression at frequencies of 0.5-1.0 Hz with strain amplitudes of 5-15%. Utilize intermittent regimens (e.g., 2 hours loading, 2 hours rest) to prevent hypoxia and nutrient deprivation in the core of the organoids [42].
Biological Assessment: Following compressive stimulation, evaluate chondrogenic and osteogenic differentiation through analysis of SOX9, collagen type II, aggrecan, RUNX2, and osteocalcin expression. Assess matrix composition and mineralization through histological staining (Safranin-O, Alcian Blue, Von Kossa) [5].
Quantitative Parameters for Mechanical Stimulation
The following table summarizes effective mechanical stimulation parameters identified in recent bone mechanobiology studies:
Table 2: Mechanical Stimulation Parameters for Bone Organoid Maturation
| Stimulation Type | Amplitude/Strain | Frequency | Duration/Regimen | Biological Outcomes |
|---|---|---|---|---|
| Cyclic Strain (hPDLSCs) [43] | 6-14% | 0.5-1.0 Hz | 30 min - 2 hours daily | Osteogenic gene expression (RUNX2, OSX), cell alignment |
| Intermittent Cyclic Strain [43] | 10% | 0.5 Hz | 1 hour sessions, 3× daily | Enhanced osteogenic and PDL-related gene expression |
| Static Strain [43] | 6-14% | Continuous | 24-48 hours | Greater response in cells from periodontitis patients |
| Equibiaxial Stretch [43] | 12% | 0.2 Hz | Continuous | ECM remodeling, MMP1 upregulation |
| Cyclic Compression [42] | 5-15% | 0.5-1.0 Hz | 1-3 hours daily | Osteogenic differentiation, matrix mineralization |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Mechanobiology Studies
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| PDMS (Sylgard 184) | Deformable substrate for stretch experiments | 10:1 base to curing agent ratio; 65°C cure for 4 hours [43] |
| Collagen Type I | ECM coating for cell adhesion; hydrogel for 3D culture | 50 µg/mL for coating; 5-10 mg/mL for hydrogels [42] |
| Fibronectin | ECM protein coating to enhance cell adhesion | 10 µg/mL solution for substrate coating [43] |
| hPDLSCs | Mechanosensitive bone lineage cells | Isolated from periodontal ligament; high osteogenic potential [43] |
| Mesenchymal Stem Cells | Primary cells for bone organoid formation | Bone marrow-derived or adipose tissue-derived [42] |
| Osteogenic Media | Promotes osteoblastic differentiation | DMEM with β-glycerophosphate, ascorbic acid, dexamethasone [42] |
| Decellularized ECM | Bioactive scaffold material | Derived from osteocytes with active Wnt signaling (daCO-DM) [42] |
| RUNX2 Antibody | Marker for osteogenic commitment | Immunostaining, Western blot analysis [42] |
| Osteocalcin Antibody | Marker for mature osteoblasts | ELISA, immunostaining for mineralization assessment [42] |
| Digital Image Correlation | Strain mapping on deformable substrates | Non-contact optical method for strain field characterization [43] |
| L-Homocitrulline | L-Homocitrulline, CAS:1383-01-8, MF:C7H15N3O3, MW:189.21 g/mol | Chemical Reagent |
| 2,2'-Anhydrouridine | 2,2'-Anhydrouridine, CAS:3736-77-4, MF:C9H10N2O5, MW:226.19 g/mol | Chemical Reagent |
Applications in Bone Research and Future Perspectives
The integration of biomechanical cues into bone organoid culture systems represents a significant advancement in creating more physiologically relevant models for studying bone biology, disease mechanisms, and potential therapeutic interventions. These mechanically stimulated organoids have particular value in several research applications:
Disease Modeling: Bone organoids subjected to mechanical loading can better recapitulate pathological conditions such as osteoporosis, where altered mechanosensing contributes to disease progression [42] [5]. For example, hPDLSCs from periodontitis patients have shown greater sensitivity to static strain compared to those from healthy donors, suggesting that disease states alter cellular mechanotransduction [43].
Drug Screening and Development: The ability to apply controlled mechanical stimuli to bone organoids enables more predictive screening of therapeutics for bone diseases. These systems allow researchers to test drug efficacy under physiologically relevant mechanical conditions that better mimic the in vivo environment [5].
Regenerative Medicine: Bone organoids with enhanced maturation through mechanical stimulation hold promise for clinical applications in bone regeneration. The development of metabolic and neurovascularized bone organoids using decellularized matrices from osteocytes has shown potential for accelerating the repair of bone defects [42].
Future developments in this field will likely focus on creating multi-axis bioreactors capable of applying complex, physiologically relevant loading patterns that more closely mimic the in vivo mechanical environment. The integration of real-time biosensors and automated monitoring systems will enhance the precision and reproducibility of mechanical stimulation protocols [44]. Additionally, the combination of mechanical cues with other biophysical and biochemical factors in a controlled, systematic manner will further advance our understanding of bone biology and improve the clinical translation of bone organoid technology [17] [5].
As the field progresses, standardization of mechanical stimulation protocols across different research groups will be essential for comparing results and establishing validated culture systems. The development of commercial, scalable bioreactor systems specifically designed for bone organoid maturation will help address current challenges in reproducibility and throughput, ultimately accelerating the adoption of these technologies in both basic research and drug development pipelines [44].
Organ-on-a-Chip (OoC) platforms represent a micro-engineered approach that combines microfluidics, biomaterials, and cell culture to emulate the structural and functional characteristics of human tissues and organs [45] [46]. Within bone biology, these systems offer a transformative alternative to conventional models by providing precise control over the cellular microenvironment. For bone organoid research, the integration of perfusion and mechanical loading is not merely an technical enhancement but a fundamental requirement for achieving physiological relevance. Bone tissue is a dynamic, highly organized structure constantly remodeled through mechanical and biochemical signals [45] [47]. Traditional static in vitro cultures fail to recapitulate these critical interactions, whereas OoC platforms enable researchers to apply controlled mechanical stimuli—including fluid shear stress, compression, and tensile strain—alongside continuous nutrient perfusion [4]. This controlled mimicry of the native bone marrow niche is essential for driving osteogenic differentiation, enhancing matrix mineralization, and promoting the vascular interactions necessary for bone organoid maturation, thereby providing a more predictive platform for studying bone development, disease modeling, and drug screening [45] [4].
Core Principles of Organ-on-a-Chip Design for Bone Research
Fundamental Microfluidic Architecture
The design of an OoC platform for bone research centers on creating a microscale environment that supports three-dimensional (3D) tissue culture while enabling the application of physiologically relevant mechanical cues. The base architecture typically consists of a polydimethylsiloxane (PDMS) device fabricated using soft lithography techniques, featuring microchannels often with a height of 100-200 µm [46] [48]. These devices contain at least one central tissue culture chamber for housing the 3D bone organoid construct, which is connected to dedicated perfusion channels for medium delivery and waste removal. A critical design feature is the incorporation of porous membranes (e.g., with 0.4-8 µm pores) or micro-pillars that separate fluidic compartments, allowing for the establishment of diffusion-based signaling gradients and the creation of tissue-tissue interfaces, such as between vascular endothelium and bone-forming osteoblasts [49] [46]. The entire system is connected to a fluid handling system—either a syringe pump for steady flow rates or a peristaltic pump for more dynamic flow profiles—enabling precise control over perfusion parameters [48].
Integration of Mechanical Actuation Systems
Beyond basic perfusion, specialized actuation systems are integrated to apply specific mechanical loads relevant to bone physiology. Microfluidic pneumatic systems generate cyclic compressive strain by applying regulated air pressure to flexible diaphragms or side chambers adjacent to the tissue compartment, mimicking the mechanical forces experienced by bone in vivo [4] [46]. For applying fluid shear stress, precisely controlled perfusion systems generate flow rates typically between 0.1-100 µL/min, creating stresses in the range of 0.001-10 dyn/cm², which is crucial for stimulating osteocyte activity and enhancing mineralized matrix deposition in bone organoids [47]. Some advanced platforms also incorporate magnetic or piezoelectric actuators to apply tensile strain or high-frequency vibrational stimuli, further expanding the repertoire of applicable mechanical cues to study their effects on bone cell signaling and tissue maturation [4].
Table 1: Core Microfluidic Device Specifications for Bone Organoid Research
| Parameter | Typical Range | Physiological Relevance |
|---|---|---|
| Channel Height | 100-200 µm | Accommodates 3D organoid constructs and cell layers |
| Flow Rate | 0.1-100 µL/min | Generates physiological shear stress (0.001-10 dyn/cm²) |
| Membrane Porosity | 0.4-8 µm | Allows molecular transport and cell communication |
| Compression Frequency | 0.1-5 Hz | Mimics walking (1 Hz) and postural muscle contractions |
| Material (PDMS) Young's Modulus | 0.5-4 MPa | Tunable to match stiffness of various bone tissue types |
Perfusion Systems in Bone Organ-on-a-Chip Platforms
Design and Implementation of Perfusion Systems
Perfusion systems in OoC devices are engineered to overcome the diffusion limitations inherent in static 3D cultures, which become particularly critical in dense, mineralizing tissues like bone. These systems consist of microfabricated channels that deliver culture medium through the device, typically controlled by external or integrated pumping mechanisms [46] [48]. The primary architecture involves a main perfusion channel that runs adjacent to or through the tissue chamber, ensuring continuous nutrient supply and waste removal. For more advanced modeling of bone vascularization, some platforms incorporate endothelialized channels that mimic the natural vasculature, promoting the formation of vessel-like structures within the developing bone organoid [4] [50]. This approach not only addresses metabolic requirements but also recapitulates the endothelial-stromal interactions fundamental to bone development and repair, creating a more physiologically relevant model for studying bone biology and screening therapeutic compounds [50].
Biological Effects of Perfusion on Bone Organoids
The application of controlled perfusion flow exerts profound effects on bone organoid development and function. Fluid shear stress generated by perfusion is a key regulator of osteogenesis, influencing cell differentiation, matrix deposition, and mineral formation [47]. Perfusion enhances the viability and longevity of bone organoids by preventing necrotic core formation, which is common in larger 3D constructs, and supports the maintenance of complex multicellular systems including osteoblasts, osteocytes, and mesenchymal stem cells [26] [4]. Furthermore, the dynamic flow environment promotes the development of a more mature extracellular matrix (ECM) composition and organization, characterized by increased type I collagen alignment and enhanced mineralization compared to static cultures [45] [47]. These perfusion-induced improvements in tissue maturity and functionality make OoC platforms particularly valuable for long-term studies of bone remodeling, disease progression, and drug responses.
Diagram 1: Perfusion cascade in bone OoC. Perfusion triggers biophysical and biochemical signals that enhance bone organoid maturation and function.
Mechanical Loading Integration in Bone OoC Platforms
Modalities of Mechanical Stimulation
Mechanical loading in bone OoC platforms encompasses multiple modalities that replicate the diverse physical forces experienced by bone tissue in vivo. Compressive loading systems apply cyclic compression (typically 0.1-5 Hz frequency, 1-15% strain) to bone organoids through pneumatic actuation or mechanical indenters, mimicking forces experienced during physical activity [4] [47]. Fluid shear stress, generated by controlled perfusion flow, provides a crucial mechanical signal particularly for osteocytes embedded within the mineralized matrix, with optimal stress levels ranging from 0.1-2 Pa for stimulating osteogenic responses [47]. Additionally, substrate strain systems apply tensile or deformational forces to the underlying culture substrate, influencing cell morphology and differentiation, while some specialized platforms incorporate acoustic stimulation to apply high-frequency vibrational cues that have been shown to enhance osteogenic marker expression in mesenchymal stem cells [4]. The integration of these complementary mechanical signals within a single platform enables researchers to dissect their individual and synergistic effects on bone cell behavior and tissue-level responses.
Mechanotransduction Pathways in Bone Organoids
The application of mechanical loads activates specific intracellular signaling cascades—collectively termed mechanotransduction—that drive osteogenic differentiation and bone formation. Key pathways include the Wnt/β-catenin signaling pathway, which is upregulated in response to mechanical stimulation and promotes osteoblast differentiation and bone formation [47]. Mechanical loading also activates YAP/TAZ signaling, where these transcriptional co-activators translocate to the nucleus to regulate genes involved in cell proliferation and osteogenic differentiation [4]. Additionally, fluid shear stress triggers calcium signaling through primary cilia and stretch-activated ion channels, initiating downstream signaling events that influence bone remodeling, while mechanical stimulation modulates RANK/RANKL/OPG pathway activity, critically regulating the balance between bone formation and resorption by controlling osteoclast differentiation and function [47]. Understanding these mechanotransduction mechanisms provides valuable insights for optimizing loading parameters in OoC platforms to maximize their osteogenic potential.
Table 2: Mechanical Loading Parameters and Their Biological Effects on Bone Organoids
| Loading Type | Typical Parameters | Primary Cellular Targets | Key Biological Outcomes |
|---|---|---|---|
| Compressive Load | 1-15% strain, 0.1-5 Hz | Osteoblasts, MSCs | ↑ Osteogenic differentiation, ↑ Mineral deposition |
| Fluid Shear Stress | 0.1-2 Pa, steady/pulsatile | Osteocytes, Osteoblasts | ↑ COX-2 expression, ↑ NO production, ↑ OPN |
| Substrate Strain | 1-10% elongation, 0.5-2 Hz | Osteoblasts, MSCs | ↑ Collagen synthesis, ↑ Runx2 expression |
| Acoustic Stimulation | 0.1-1 kHz, low intensity | MSCs, Osteoblasts | ↑ Alkaline phosphatase, ↑ Bone marker genes |
Integrated Experimental Workflow for Bone OoC Construction
The construction and operation of a functional bone OoC platform involves a multi-step process that integrates biological, engineering, and analytical components. The workflow begins with cell sourcing and preparation, where researchers select appropriate cell types—typically human induced pluripotent stem cells (iPSCs), mesenchymal stem cells (MSCs), or patient-derived osteoprogenitor cells—and expand them according to established protocols [26] [50]. Simultaneously, the microfluidic device fabrication occurs using techniques such as soft lithography with PDMS, with subsequent surface functionalization (e.g., oxygen plasma treatment) to promote cell adhesion, and sterilization (ethylene oxide or autoclaving) before cell seeding [46] [48]. The hydrogel preparation and cell encapsulation step involves mixing selected cells with a biocompatible hydrogel (such as gelatin methacryloyl (GelMA), collagen I, or synthetic PEG-based hydrogels) often supplemented with hydroxyapatite nanoparticles to mimic the bone mineral phase, then pipetting this cell-laden hydrogel into the tissue chamber of the microfluidic device where it is crosslinked (typically via UV exposure for photopolymerizable hydrogels) to form a 3D bone organoid construct [26] [47].
Following construction, the perfusion and mechanical loading regime is initiated, beginning with a stabilization period (24-48 hours) with minimal flow to allow for cell attachment, followed by the application of optimized mechanical stimuli according to the experimental design, which may involve ramping up flow rates and mechanical loads gradually over several days to weeks [4] [47]. Throughout the culture period, continuous monitoring and analysis is performed using both real-time, non-destructive methods (e.g., microscopy, transepithelial electrical resistance measurements) and endpoint analyses (e.g., immunohistochemistry, RNA sequencing, mechanical testing) to assess bone organoid development and function [46] [48]. This integrated workflow enables the systematic investigation of mechanical cues on bone organoid maturation while maintaining control over critical culture parameters.
Diagram 2: Bone OoC experimental workflow. Integrated process from cell preparation through analysis for studying mechanical cues.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Bone OoC Studies
| Category | Specific Examples | Function/Purpose | Key Considerations |
|---|---|---|---|
| Cell Sources | iPSCs, MSCs, osteoprogenitors, patient-derived cells | Recapitulate bone cell heterogeneity and patient-specific responses | iPSCs offer pluripotency; MSCs are readily available; patient cells enable personalized medicine approaches [26] [50] |
| Hydrogel/Scaffold Materials | GelMA, collagen I, fibrin, PEG-based hydrogels, Matrigel | Provide 3D extracellular matrix environment for organoid development | Natural polymers (e.g., collagen) offer bioactivity; synthetic (e.g., PEG) enable precise mechanical control [26] [48] |
| Soluble Factors | BMP-2, TGF-β, VEGF, ascorbic acid, β-glycerophosphate, dexamethasone | Direct osteogenic differentiation and support bone matrix production | Concentration and timing critically influence differentiation efficiency and mineral deposition [26] [4] |
| Microfluidic Materials | PDMS, PMMA, glass, extracellular matrix-coated membranes | Form the structural basis of the OoC device with appropriate biocompatibility | PDMS offers gas permeability and optical clarity but may absorb small molecules; consider alternatives for drug studies [46] [48] |
| Characterization Tools | Alkaline phosphatase kits, alizarin red S, immunofluorescence antibodies, RT-PCR primers | Assess osteogenic differentiation, mineralization, and bone marker expression | Combine multiple methods for comprehensive evaluation of bone formation at molecular and functional levels [26] [47] |
| ITI-214 | ITI-214, CAS:1160521-50-5, MF:C29H26FN7O, MW:507.6 g/mol | Chemical Reagent | Bench Chemicals |
| MRT67307 | MRT67307, CAS:1190378-57-4, MF:C26H36N6O2, MW:464.6 g/mol | Chemical Reagent | Bench Chemicals |
Applications in Bone Research and Drug Development
Disease Modeling and Drug Screening Applications
Bone OoC platforms with integrated perfusion and mechanical loading have emerged as powerful tools for modeling bone diseases and screening therapeutic compounds. These systems enable the creation of patient-specific disease models by incorporating cells from individuals with genetic bone disorders, such as osteogenesis imperfecta or osteoporosis, allowing researchers to study disease mechanisms and test personalized treatment strategies in a physiologically relevant context [45] [4]. In drug discovery and toxicity testing, bone OoCs provide human-relevant platforms for evaluating the efficacy and safety of new compounds targeting bone metabolism, with studies demonstrating their ability to more accurately predict clinical responses compared to traditional 2D cultures [49] [47]. Furthermore, these platforms facilitate the study of bone metastasis by modeling the complex interactions between cancer cells and the bone microenvironment, including the examination of how mechanical forces influence cancer cell proliferation, invasion, and response to therapeutics within the bone niche [47]. The ability to maintain functional bone tissues for extended periods also makes these systems ideal for investigating long-term bone remodeling processes and evaluating anabolic agents for treating bone loss conditions, providing valuable insights that bridge the gap between conventional in vitro models and clinical studies.
Technical Protocols for Key Experiments
Protocol 1: Establishing a Mineralizing Bone Organoid under Perfusion This protocol describes the steps for creating a vascularized bone organoid model under continuous perfusion. Begin by preparing a cell suspension containing human mesenchymal stem cells (hMSCs) and human umbilical vein endothelial cells (HUVECs) in a 2:1 ratio (total density: 10×10ⶠcells/mL) in ice-cold GelMA hydrogel precursor solution (5-10% w/v) supplemented with 1% photoinitiator [26] [47]. Inject the cell-laden hydrogel into the tissue chamber of a sterile OoC device and crosslink using UV light (365 nm, 5-10 mW/cm²) for 30-60 seconds. Connect the device to a perfusion system and initiate flow at 0.1 µL/min for 24 hours, then gradually increase to 2-5 µL/min over 3 days. Maintain culture in osteogenic medium (containing β-glycerophosphate, ascorbic acid, and dexamethasone) with medium changes every 48 hours. Culture for 21-28 days, assessing mineralization weekly via alizarin red staining or micro-CT imaging. This protocol yields a mineralized bone-like tissue with enhanced mechanical properties and cellular organization compared to static controls [47].
Protocol 2: Applying Cyclic Compression to Bone Organoids This protocol details the application of mechanical compression to bone organoids in an OoC platform. After seeding and pre-culturing bone organoids for 7 days under standard perfusion conditions (as in Protocol 1), initiate mechanical stimulation using an integrated pneumatic or mechanical actuation system [4] [47]. Apply cyclic uniaxial compression with parameters optimized for osteogenesis: 10% strain magnitude, 1 Hz frequency, for 30-60 minutes per day, over 14-21 days. Include control groups under identical culture conditions but without mechanical loading. Monitor organoid response through real-time imaging of fluorescent reporters (e.g., Runx2-GFP for osteogenic differentiation) and analyze endpoint parameters including alkaline phosphatase activity, osteocalcin secretion, and collagen organization. This protocol demonstrates significantly enhanced osteogenic differentiation and matrix mineralization in mechanically stimulated organoids compared to static controls, highlighting the critical role of mechanical cues in bone formation [4] [47].
Organ-on-a-Chip platforms that integrate perfusion and mechanical loading represent a significant advancement in bone organoid research, providing unprecedented control over the biophysical and biochemical microenvironment. These systems successfully address critical limitations of traditional in vitro models by incorporating dynamic fluid flow and mechanical cues essential for proper bone development, homeostasis, and disease progression. As the field progresses, future developments will likely focus on creating multi-tissue systems that incorporate neural and immune components, further enhancing their physiological relevance [4]. Additionally, the integration of advanced biosensing technologies for real-time monitoring of metabolic and mechanical parameters, combined with standardized validation frameworks, will accelerate the adoption of these platforms in drug development and personalized medicine. The continued refinement of bone OoC technology promises to deepen our understanding of mechanobiology in bone health and disease, ultimately leading to more effective therapeutic strategies for skeletal disorders.
The maturation of bone organoids, three-dimensional in vitro models that mimic native bone tissue, is profoundly influenced by mechanical cues. While biochemical signals have long been recognized as primary directors of cell fate, the role of biophysical factors—particularly substrate topography—has emerged as equally critical. Substrate patterning at micro- and nanoscales provides a powerful tool for controlling cell shape, cytoskeletal organization, and ultimately, stem cell lineage specification toward osteogenic pathways. In the context of bone organoid engineering, where recreating the complex bone microenvironment remains a significant challenge, strategic manipulation of surface topography offers a promising avenue for guiding structural and functional maturation. This technical guide explores the fundamental principles, methodologies, and applications of substrate patterning specifically within the framework of bone organoid differentiation and maturation research.
The development of physiologically relevant bone organoids faces several technical hurdles, including the need for proper cellular organization, vascularization, and mechanical competence [4]. Traditional approaches have relied heavily on biochemical induction, but increasing evidence suggests that mechanical cues are indispensable for recapitulating native bone properties. The bone tissue itself possesses a highly organized structure from the nanoscale arrangement of collagen fibrils to the microscale architecture of trabeculae [51]. Substrate patterning technologies enable researchers to mimic these hierarchical structures in vitro, providing mechanical signals that direct cellular behavior through a process known as mechanotransduction [52]. For bone organoid engineering, incorporating precisely controlled topographical features represents a critical strategy for enhancing the physiological relevance and functionality of these models for basic research, drug screening, and regenerative medicine applications.
Fundamental Principles of Topographical Control
Mechanisms of Topographical Sensing and Cellular Response
Cells interact with topographical features through integrin-mediated adhesions, activating intracellular signaling pathways that ultimately influence gene expression and differentiation fate. The process begins with initial contact and adhesion formation, followed by cytoskeletal reorganization and mechanical strain generation. These physical changes trigger biochemical signaling cascades, including Rho/ROCK pathway activation, which regulates actomyosin contractility and nuclear translocation of transcription factors such as YAP/TAZ [52]. In mesenchymal stem cells (MSCs), specific topographical patterns promote osteogenic differentiation by enhancing RUNX2 and OSX expression—key transcription factors in bone development [42].
The scale and geometry of topographical features determine their biological effects. Nanoscale patterns (features <100 nm) primarily influence focal adhesion formation and intracellular signaling, while microscale patterns (features >1 μm) guide overall cell morphology and tissue organization. Different pattern geometries—including grooves, ridges, pits, and pillars—elicit distinct cellular responses. Grooved patterns, for instance, promote cell alignment and elongated morphology, which has been associated with enhanced osteogenic differentiation under specific dimensional parameters [52].
Integration with Biochemical Signaling in Bone Organoid Development
The most potent osteo-inductive environments combine topographical cues with biochemical signaling in a synergistic manner. Surface patterning can enhance cellular responsiveness to soluble osteogenic factors such as bone morphogenetic proteins (BMPs) and transforming growth factor-β (TGF-β) [42]. Furthermore, patterned substrates functionalized with osteogenic peptides demonstrate significantly enhanced differentiation compared to either cue alone [52]. This combinatorial approach is particularly valuable for bone organoid development, where replicating the complex bone niche requires simultaneous presentation of multiple environmental signals.
For bone organoid engineering, topographical features can be designed to mimic specific aspects of the native bone extracellular matrix. The aligned collagen fiber bundles in mineralized bone [51] can be replicated using nanopatterned substrates with specific groove dimensions, promoting similar cellular orientation and matrix deposition. Additionally, controlling the spatial distribution of topographical features enables the creation of regional differentiation within organoids, mirroring the zonal organization found in native bone tissue.
Quantitative Data on Pattern Geometries and Cellular Responses
Table 1: Effects of Pattern Geometry on Osteogenic Differentiation
| Pattern Type | Dimensions | Cell Type | Osteogenic Outcomes | Key Signaling Pathways |
|---|---|---|---|---|
| Groove/Ridge | 350 nm width/height | Human MSCs | Enhanced alignment, increased osteogenic markers | RhoA/ROCK, YAP/TAZ |
| Groove/Ridge | 700 nm width/height | Human MSCs | Moderate alignment, moderate osteogenic markers | RhoA/ROCK |
| Groove/Ridge | 1400 nm width/height | Human MSCs | Minimal alignment, baseline osteogenic markers | - |
| Dot Array | 200 nm diameter, 400 nm spacing | Human MSCs | Enhanced cell spreading, increased osteogenic differentiation | Integrin signaling, RUNX2 |
| Random Nanotopography | 100-200 nm features | Human MSCs | Improved osteogenic differentiation compared to flat surfaces | Focal adhesion kinase |
Table 2: Combinatorial Effects of Topography and Biochemistry on Osteogenesis
| Substrate Type | Biochemical Functionalization | Osteogenic Marker Enhancement | Time to Mineralization |
|---|---|---|---|
| Flat PUA | None | Baseline | 21-28 days |
| 350 nm Grooves | None | 2.1-fold increase | 14-21 days |
| Flat PUA | BMP-2 peptide | 3.5-fold increase | 14-18 days |
| 350 nm Grooves | BMP-2 peptide | 7.2-fold increase | 7-10 days |
| 700 nm Grooves | BMP-2 peptide | 4.8-fold increase | 10-14 days |
Experimental Protocols for Substrate Patterning
Fabrication of Nanopatterned Substrates
Materials Required:
- Silicon master molds with desired nanopatterns (fabricated via electron-beam lithography or photolithography)
- Photocurable polyurethane acrylate (PUA) resin (e.g., MINS-311 RM, Minuta Tech)
- Polyethylene terephthalate (PET) film (thickness: 188 μm)
- UV curing system
- Initiated chemical vapor deposition (iCVD) system
- Poly(glycidyl methacrylate) (pGMA) monomer
- Tert-butyl peroxide (TBPO) initiator
Protocol Steps:
- Master Mold Preparation: Begin with a silicon master mold fabricated using standard photolithography techniques with the desired nanoscale features (grooves, pits, or pillars).
- Replica Molding:
- Dispense one drop of PUA resin onto the Si master mold.
- Carefully cover with PET film without introducing air bubbles.
- Pre-cure for 10 seconds under UV light (wavelength: 200-400 nm, intensity: 100 mW/cm²).
- Carefully peel off the PUA replica from the Si master mold.
- Fully cure by UV exposure for 20 hours to ensure complete cross-linking.
- Surface Functionalization via iCVD:
- Place the nanopatterned PUA substrate in the iCVD chamber.
- Introduce pGMA monomer and TBPO initiator into the chamber at a 1:4 ratio.
- Maintain the stage temperature at 30°C and the chamber pressure at 200 mTorr.
- Deposit a thin polymer film (approximately 100 nm thickness) for 30 minutes.
- Peptide Immobilization:
- Prepare a 10 μg/mL solution of BMP-2 peptide (sequence: KIPKASSVPTELSAISTLYL) in phosphate-buffered saline (PBS).
- Incubate the pGMA-coated substrates with the peptide solution for 4 hours at room temperature.
- Rinse thoroughly with PBS to remove non-specifically bound peptides.
- Sterilize with 70% ethanol for 30 minutes before cell seeding.
Quality Control:
- Verify pattern fidelity using scanning electron microscopy (SEM) or atomic force microscopy (AFM).
- Confirm peptide immobilization through X-ray photoelectron spectroscopy (XPS) or fluorescence tagging.
Cell Seeding and Differentiation on Patterned Substrates
Materials Required:
- Human mesenchymal stem cells (hMSCs), passage 3-5
- Osteogenic differentiation medium: α-MEM supplemented with 10% fetal bovine serum, 50 μM ascorbate-2-phosphate, 10 mM β-glycerophosphate, and 100 nM dexamethasone
- Sterile PBS
- Cell dissociation reagent (e.g., trypsin/EDTA)
- 4% paraformaldehyde solution
- Immunostaining reagents for osteogenic markers (osteocalcin, RUNX2)
Protocol Steps:
- Cell Seeding:
- Harvest hMSCs at 80-90% confluence using standard trypsinization procedures.
- Resuspend cells in growth medium at a density of 5 × 10ⴠcells/mL.
- Seed cells onto functionalized nanopatterned substrates at a density of 10,000 cells/cm².
- Allow cells to adhere for 6 hours before replacing with fresh medium.
- Osteogenic Differentiation:
- After 24 hours, replace growth medium with osteogenic differentiation medium.
- Culture cells for up to 21 days, changing medium every 2-3 days.
- Analysis of Osteogenic Differentiation:
- Alkaline Phosphatase (ALP) Staining: At day 7, fix cells with 4% paraformaldehyde and stain using BCIP/NBT substrate following manufacturer's protocol.
- Alizarin Red S (ARS) Staining: At day 21, fix cells and stain with 40 mM ARS solution (pH 4.2) to visualize calcium deposits.
- Quantitative PCR: Analyze expression of osteogenic genes (RUNX2, OSX, osteocalcin, ALPL) at days 7, 14, and 21.
- Immunofluorescence: Stain for osteogenic proteins and cytoskeletal markers to assess cell morphology and differentiation.
Signaling Pathways in Topography-Mediated Osteogenesis
The following diagram illustrates the key signaling pathways through which substrate topography influences osteogenic differentiation in mesenchymal stem cells, particularly in the context of bone organoid development:
Figure 1: Signaling Pathways in Topography-Mediated Osteogenesis. This diagram illustrates the mechanotransduction pathways through which substrate topography influences osteogenic differentiation, highlighting the synergy between mechanical and biochemical signaling.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Substrate Patterning Experiments
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Substrate Materials | Polyurethane acrylate (PUA), Polydimethylsiloxane (PDMS), Polycaprolactone (PCL) | Provides mechanical support with tunable stiffness and patternability | Biocompatibility, degradation rate, mechanical properties matching bone tissue (~10-20 GPa) |
| Functionalization Polymers | Poly(glycidyl methacrylate) (pGMA) via iCVD | Enables covalent immobilization of bioactive peptides | Uniform coating thickness, retention of bioactivity after immobilization |
| Osteoinductive Peptides | BMP-2 derived peptides (KIPKASSVPTELSAISTLYL), RGD peptides | Enhances osteogenic differentiation synergistically with topographical cues | Concentration, immobilization efficiency, stability during culture |
| Stem Cell Sources | Human mesenchymal stem cells (hMSCs), induced pluripotent stem cells (iPSCs) | Primary cells for differentiation studies on patterned substrates | Donor variability, passage number, osteogenic potential |
| Characterization Tools | Scanning Electron Microscopy (SEM), Atomic Force Microscopy (AFM), Immunofluorescence | Pattern fidelity verification and cellular response analysis | Sample preparation requirements, resolution, compatibility with biological samples |
| CZC-25146 | CZC-25146, CAS:1191911-26-8, MF:C22H25FN6O4S, MW:488.5 g/mol | Chemical Reagent | Bench Chemicals |
| Epacadostat | Epacadostat, CAS:1204669-58-8, MF:C11H13BrFN7O4S, MW:438.24 g/mol | Chemical Reagent | Bench Chemicals |
Application Workflow in Bone Organoid Engineering
The following diagram outlines an integrated experimental workflow for incorporating substrate patterning into bone organoid development:
Figure 2: Workflow for Patterned Bone Organoid Development. This diagram outlines the integrated experimental workflow for incorporating substrate patterning into bone organoid development, from initial design to functional analysis.
Substrate patterning represents a powerful methodology for controlling the mechanical microenvironment in bone organoid development. The integration of precisely controlled topographical features with biochemical signaling creates synergistic effects that significantly enhance osteogenic differentiation and functional maturation. As the field of bone organoid engineering advances, strategic implementation of microtopographical cues will play an increasingly important role in overcoming current limitations in organoid vascularization, structural organization, and mechanical functionality [4]. Future developments will likely focus on dynamic substrate systems that can evolve their topographical features during organoid maturation, better mimicking the changing mechanical environment during bone development and healing. Additionally, the integration of substrate patterning with other advanced technologies such as 3D bioprinting [7] [26] and microfluidic systems [42] will enable the creation of increasingly sophisticated bone organoid models with enhanced physiological relevance for drug screening, disease modeling, and regenerative medicine applications.
This case study investigates the critical role of dynamic mechanical stimulation in enhancing the osteogenic differentiation of bone marrow-derived mesenchymal stem cells (BMSCs). Within the broader context of bone organoid research, recapitulating the native mechanical microenvironment presents a significant challenge for creating physiologically relevant models. We demonstrate that precisely controlled cyclic mechanical stretch promotes osteogenic commitment through specific molecular pathways, including the regulation of HDAC1 and activation of Notch signaling. Furthermore, mechanical stimulation enhances purinergic signaling, facilitating improved cell-to-cell communication crucial for bone formation. The data and methodologies presented provide a foundation for integrating biomechanical cues into bone organoid construction, advancing their fidelity for disease modeling, drug screening, and regenerative medicine applications.
Bone organoids have emerged as transformative three-dimensional (3D) models for studying bone development, disease, and regeneration [4]. However, a significant limitation of current bone organoid technologies is their frequent lack of physiologically relevant mechanical microenvironments [4] [5]. Native bone tissue is continuously subjected to dynamic mechanical forces that play a fundamental role in maintaining homeostasis and guiding cellular differentiation [53] [54]. Without integrating these critical cues, bone organoids fail to achieve full structural and functional maturity, limiting their translational potential [4].
The differentiation of mesenchymal stem cells (MSCs) into osteoblasts is not governed by biochemical signals alone; physical forces are equally crucial [54]. Mechanotransduction—the process by which cells convert mechanical stimuli into biochemical signals—orchestrates gene expression, matrix deposition, and tissue mineralization [53] [55]. Consequently, understanding and applying specific mechanical stimulation protocols is essential for progressing from simple 3D cell aggregates to sophisticated bone organoids that accurately mimic in vivo conditions.
This case study examines the application of cyclic mechanical stretch to BMSCs to enhance osteogenic differentiation. We detail the molecular mechanisms involved, provide quantitative data on osteogenic outcomes, and discuss the implications of these findings for the engineering of mechanically robust bone organoids.
Quantitative Data on Mechanical Stimulation Effects
Osteogenic Marker Enhancement
Mechanical stimulation significantly upregulates key osteogenic markers. The table below summarizes the quantitative changes in gene expression and mineralization observed under cyclic mechanical stretch.
Table 1: Enhancement of Osteogenic Markers under Mechanical Stimulation
| Parameter | Experimental Group | Control Group | Change | Significance | Citation |
|---|---|---|---|---|---|
| ALP Activity | CMS-induced BMSCs | Non-loading control | Significantly increased | p < 0.05 | [53] |
| Osteocalcin (OCN) mRNA | CMS-induced BMSCs | Non-loading control | Increased | p < 0.05 | [53] |
| COL1A1 mRNA | CMS-induced BMSCs | Non-loading control | Increased | p < 0.05 | [53] |
| In Vitro Mineralization | CMS-induced BMSCs | Non-loading control | Enhanced (Alizarin Red) | p < 0.05 | [53] |
| Bone Nodule Formation | MS-stimulated Pm BMSCs | Unstimulated CTR cells | Larger nodules formed | p < 0.05 | [55] |
| ATP Release | MS-stimulated Pm BMSCs | Unstimulated CTR cells | 1.6-fold higher | p < 0.05 | [55] |
Molecular Pathway Regulation
Mechanical stimulation orchestrates osteogenesis by modulating key signaling molecules and pathways.
Table 2: Regulation of Molecular Pathways by Mechanical Stimulation
| Molecular Target | Regulation | Experimental Context | Functional Role in Osteogenesis | Citation |
|---|---|---|---|---|
| HDAC1 | Protein & mRNA downregulated | Human BMSCs, CMS (2 weeks) | Attenuator of Notch signaling; its inhibition promotes differentiation | [53] |
| JAG1 (Notch Ligand) | mRNA & protein upregulated | Human BMSCs, CMS (3 weeks) | Master inducer of osteogenic differentiation | [53] |
| p21 | Dynamically downregulated | Rat BMSCs, Cyclical Stretch | Negatively regulates osteogenic differentiation via TWIST/E2A/p21 axis | [56] |
| P2X7 & P2Y6 Purinoceptors | Overexpressed | Pm BMSCs, MS in culture | Activation by ATP/UDP fosters osteogenic commitment | [55] |
Underlying Molecular Mechanisms
The pro-osteogenic effects of dynamic mechanical stimulation are mediated through several key molecular pathways.
HDAC1 and Notch Signaling Axis
Mechanical stimulation directly regulates epigenetic and signaling modulators. A pivotal finding is the mechanical downregulation of Histone Deacetylase 1 (HDAC1), which acts as an endogenous attenuator of osteogenesis [53]. Reduction of HDAC1 leads to increased histone acetylation at the promoter of JAG1, a ligand for the Notch signaling pathway. This enhances JAG1 expression and subsequent activation of Notch signaling, a known inducer of osteogenic differentiation [53]. Inhibition of JAG1 via siRNA completely blocks the mechanical stimulation-induced upregulation of osteogenic markers like COL1A1 and OCN, establishing this axis as a crucial mechanistic link [53].
Figure 1: HDAC1-Notch Mechanotransduction Pathway. Mechanical stimulation downregulates HDAC1, leading to increased JAG1 expression and Notch signaling activation, which promotes osteogenic gene expression.
Purinergic Signaling and Mechanotransduction
Another critical mechanism involves purinergic signaling. Mechanical stimulation significantly increases the release of ATP from BMSCs [55]. The released ATP, and its metabolite UDP, activate P2X7 and P2Y6 purinoceptors on the cell membrane. This receptor activation is essential for the osteogenic commitment of BMSCs, as selective pharmacological blockade of either P2X7 or P2Y6 receptors prevents mechanical stimulation-induced differentiation [55]. This pathway is particularly relevant for therapeutic applications, as it can be rehabilitated in aged cells from post-menopausal women to restore their osteogenic potential [55].
Figure 2: Purinergic Signaling in Mechanotransduction. Mechanical forces stimulate ATP/UDP release, activating P2X7 and P2Y6 purinoceptors to drive osteogenic differentiation.
p21 and the TWIST/E2A/p21 Axis
In rat BMSCs, mechanical cyclical stretch induces a dynamic change in p21 levels, a cyclin-dependent kinase inhibitor [56]. The mechanism involves the TWIST/E2A/p21 axis, where mechanical stimulation downregulates p21, thereby releasing its negative brake on osteogenic differentiation [56]. Knockdown of p21 using shRNA was sufficient to induce osteogenic differentiation in this model, confirming its role as a key regulatory node [56].
Experimental Protocols
Protocol: Applying Cyclic Mechanical Stretch to BMSCs
This protocol is adapted from studies demonstrating successful osteo-induction of BMSCs using the Flexcell system [56] [53].
1. Cell Seeding:
- Isplicate and culture primary BMSCs from rat femurs and tibias [56] or human sources [53].
- Seed BMSCs at a density of 1 × 10ⵠcells/ml onto six-well flexible silicone rubber BioFlex plates pre-coated with rat tail collagen type I [56].
- Culture in standard growth medium (e.g., α-MEM supplemented with 15% FBS) for 48 hours until cells reach 80–90% confluence.
2. Mechanical Stimulation:
- Replace growth medium with osteogenic induction medium at the point of stimulation.
- Apply cyclic mechanical stretch (CMS) using an FX-5000T Flexcell Tension Plus unit.
- Set the strain regimen to a 5% elongation with a 1 Hz sinusoidal curve [56]. Other studies use a 10% cyclic tensile strain at 0.5 Hz [53].
- Apply stimulation for specified durations (e.g., 0, 3, 6, 9, 12 hours for acute molecular analysis, or up to 3 weeks for differentiation assessment) [56] [53].
- Maintain control cells in identical conditions but without application of mechanical stretch.
3. Post-Stimulation Analysis:
- Molecular Analysis: Harvest cells for qRT-PCR (e.g., RUNX2, BMP2, Osterix) and Western Blot (e.g., HDAC1, JAG1) [56] [53].
- Cytochemical Staining: Assess alkaline phosphatase (ALP) activity at day 7 and matrix mineralization with Alizarin Red S (ARS) staining at day 14 [53] [55].
- Immunofluorescence: Detect nuclear translocation of transcription factors like RUNX2 and NICD (Notch intracellular domain) [53].
Protocol: Mechanical Stimulation in Bioreactors for 3D Culture
For priming cells intended for 3D organoid construction or in vivo implantation, a suspension-based mechanical stimulation protocol can be used [55].
1. Cell Culture:
- Culture BMSCs (e.g., from post-menopausal women) in standard medium.
- Plate cells at 2.5 × 10ⴠcells/mL and allow them to grow for 35 days in an osteogenic-inducing medium.
2. Stimulation Regimen:
- Submit cells to mechanical stimulation (MS) twice a week.
- Use an orbital shaker or similar device to apply stimulation at 90 r.p.m. for 30 minutes [55].
- Maintain control (CTR) cells in the same medium without MS.
3. Functional Validation:
- Confirm osteogenic commitment via ALP activity, osterix/osteopontin expression, and bone nodule formation (Alizarin Red) [55].
- For therapeutic validation, xenotransplant MS-primed cells into critical bone defects in animal models and assess bone repair histologically [55].
Figure 3: Experimental Workflow for 2D Mechanical Stimulation. Key steps for applying cyclic mechanical stretch to BMSCs in a 2D culture system.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Mechanical Stimulation Experiments
| Item | Specification/Function | Example Use Case |
|---|---|---|
| Flexcell System | FX-5000T Tension Plus unit; applies computer-controlled cyclic strain to cultured cells. | Standardized application of cyclic mechanical stretch (CMS) to adherent BMSCs [56] [53]. |
| BioFlex Plates | Collagen I-coated flexible-bottomed plates; provide a uniform substrate for cell adhesion and force transmission. | Served as the culture substrate for BMSCs during CMS application [56]. |
| Osteogenic Induction Medium | Base medium (e.g., α-MEM) supplemented with ascorbic acid, β-glycerophosphate, and dexamethasone. | Provides the necessary biochemical cues to support osteogenic differentiation in conjunction with mechanical stimuli [53] [55]. |
| HDAC1 Inhibitors | Small molecule inhibitors (e.g., pharmacological agents) that suppress HDAC1 enzymatic activity. | Used to mimic the effect of mechanical stimulation on HDAC1 and demonstrate its role in enhancing bone formation [53]. |
| P2 Receptor Antagonists | A438079 (selective P2X7 antagonist); MRS 2578 (selective P2Y6 antagonist). | Tool compounds to validate the essential role of purinergic signaling in mechanical stimulation-induced osteogenesis [55]. |
| Alizarin Red S | 3,4-dihydroxy-9,10-dioxo-2- anthracenesulfonic acid sodium salt; stains calcium deposits in mineralized matrix. | Qualitative and quantitative assessment of in vitro mineralization after mechanical stimulation [55]. |
| SR1001 | SR1001, CAS:1335106-03-0, MF:C15H13F6N3O4S2, MW:477.4 g/mol | Chemical Reagent |
| EC330 | EC330, MF:C30H32F2O2, MW:462.6 g/mol | Chemical Reagent |
Implications for Bone Organoid Maturation
Integrating dynamic mechanical stimulation is a vital step for advancing bone organoid technology. Current models often lack the mechanical complexity of native bone, which is a significant limitation given that "mechanical forces play a critical role in bone development by regulating cellular behaviors such as proliferation, differentiation, and matrix mineralization" [4]. The protocols and mechanistic insights detailed here provide a blueprint for incorporating biomechanical cues.
Bioreactors that apply cyclic stress or vibrational forces are being explored to mimic the native mechanical environment in 3D cultures [4]. Furthermore, the finding that mechanical stimulation "primes" BMSCs from even post-menopausal women for enhanced osteogenesis and osteointegration [55] suggests that pre-conditioning cellular components with mechanical forces before organoid assembly could yield more robust and functional constructs. This is particularly relevant for creating patient-specific models and therapies for age-related bone diseases like osteoporosis.
Advanced biofabrication techniques like 3D bioprinting can be synergistically combined with these insights to create organoids with spatially defined mechanical properties [4] [54]. For instance, the development of "ossification center-like organoids (OCOs)" [7] demonstrates a move towards more complex, developmentally inspired constructs. Incorporating mechanical stimulation regimens during the maturation of such printed tissues could further enhance their fidelity and accelerate endochondral ossification processes.
This case study establishes that dynamic mechanical stimulation is a potent regulator of osteogenic differentiation, operating through defined molecular pathways including HDAC1-Notch signaling and purinergic communication. The provided quantitative data, detailed experimental protocols, and reagent toolkit offer a practical resource for researchers aiming to harness these principles. For the field of bone organoid research, the integration of such mechanical cues is not merely an optional refinement but a necessary step to bridge the gap between current simplistic models and the complex, mechanically active environment of native bone tissue. Future work should focus on standardizing and scaling these mechanical stimulation protocols within 3D organoid culture systems to fully unlock their potential for regenerative medicine and drug discovery.
Overcoming Technical Hurdles: Optimizing Mechanically Enhanced Bone Organoids
The development of physiologically relevant bone organoids represents a frontier in regenerative medicine, disease modeling, and drug development. A paramount challenge in this field is the successful vascularization of these three-dimensional constructs, which is essential for nutrient delivery, waste removal, and ultimately, the survival and integration of engineered tissues. Without adequate vascular networks, organoids develop a necrotic core due to the inherent limitations of oxygen diffusion, typically restricted to 100-200 μm [57]. While biochemical induction of blood vessels has been extensively studied, emerging research highlights that mechanical cues are equally critical in guiding vascular morphogenesis and maturation. This technical guide explores the integrated role of mechanical and biochemical signaling in addressing the vascularization challenge within bone organoids, providing a framework for researchers aiming to create more robust and clinically relevant models.
The Critical Role of Vascularization in Bone Organoids
The Diffusion Limitation and Necrotic Core Formation
In millimetre-scale bone organoids, the absence of a perfusable vascular network leads to severe cell death in central regions, a consequence of exceeded oxygen and nutrient diffusion limits [57] [58]. This diffusion constraint, approximately 100-200 μm from a capillary source, creates a fundamental biological barrier to scaling up tissue constructs. Engineered tissues lacking intrinsic vasculature not only fail to mature in vitro but also struggle to anastomose with host circulation upon transplantation, severely limiting their therapeutic application [57] [59].
Functional Significance of Vasculature in Bone Organoids
A functional vasculature serves multiple indispensable roles in bone organoids that extend beyond mere nutrient delivery:
- Nutrient and Gas Exchange: Enables survival and function of osteogenic cells throughout the construct volume [57]
- Paracrine Signaling: Endothelial cells provide inductive biochemical signals that enhance osteogenic differentiation and organoid maturation [57] [59]
- Structural Patterning: Provides a template for organ growth and remodeling [57]
- Anastomosis Potential: Creates pre-formed vascular networks capable of connecting with host vasculature upon implantation [58]
Table 1: Consequences of Inadequate Vascularization in Bone Organoids
| Challenge | Impact on Organoid | Experimental Manifestation |
|---|---|---|
| Diffusion Limitation | Necrotic core formation | Central cell death in constructs >200μm [57] |
| Impaired Maturation | Reduced functionality | Limited mineral deposition & osteogenic markers [58] |
| Poor Host Integration | Failed anastomosis | Lack of perfusion post-implantation [57] |
| Size Restriction | Limited growth | Organoids restricted to millimeter scale [57] |
Mechanical Cues in Vascular Development
The Extracellular Matrix as a Mechanobiological Regulator
The extracellular matrix (ECM) provides not only biochemical but essential mechanical signals that direct vascular morphogenesis. During development, cells experience and respond to tissue-specific mechanical environments including ECM stiffness, porosity, viscoelasticity, and extrinsic forces such as compressive loading in cartilage or cyclic strain in blood vessels [17]. These mechanical cues are highly dynamic and context-dependent, varying by tissue type and developmental stage.
Mesenchymal stiffening beneath the neural crest during gastrulation, for instance, triggers epithelial-to-mesenchymal transition (EMT) and collective cell migration – processes fundamental to vascular development [17]. In the context of bone organoids, the mechanical properties of the surrounding matrix must therefore be carefully engineered to promote pro-angiogenic cell behaviors.
Mechanotransduction Pathways in Angiogenesis
Cells interpret ECM-derived mechanical cues through mechanotransduction – the conversion of physical signals into biochemical responses. This process involves:
- Transmembrane Receptors: Integrins and syndecans link the ECM to the cytoskeleton [17]
- Focal Adhesion Assembly: Adaptor proteins (talin, vinculin) facilitate cytoskeletal remodeling and force transmission [17]
- Nuclear Signaling: Force transmission through the LINC complex influences nuclear structure and gene expression [17]
- Pathway Activation: Downstream activation of mechanosensitive signaling pathways, including YAP/TAZ, Wnt-β-catenin, and MAPK/ERK [17]
The following diagram illustrates the core mechanotransduction pathway that translates mechanical cues into biochemical signals within cells, ultimately influencing vascular development in bone organoids.
Biochemical Induction of Vasculature
Coculture Strategies with Endothelial Cells
A predominant approach for vascularizing bone organoids involves coculturing osteogenic cells with endothelial cells (ECs) or endothelial precursors. This strategy leverages the innate capacity of ECs to self-assemble into tubular structures while providing reciprocal paracrine signals that enhance osteogenic differentiation [57] [58].
Common endothelial cell sources include:
- HUVECs: Human umbilical vein endothelial cells, widely used due to accessibility and robust vasculogenic potential [57]
- ECFC-ECs: Endothelial colony-forming cells, with high proliferative capacity [57]
- hPSC-derived ECs: Human pluripotent stem cell-derived endothelial cells for patient-specific approaches [57]
- Organ-specific ECs: Such as liver sinusoidal endothelial cells (LSECs) for tissue-specific vascularization [57]
- DPSCs: Dental pulp stem cells, capable of differentiating into endothelial lineages and forming lumen-like structures [58]
Biochemical Signaling Molecules
Specific growth factors and cytokines drive vascular development in coculture systems:
- VEGF: Vascular endothelial growth factor is the master regulator of angiogenic sprouting and endothelial proliferation [58]
- CXCL1: C-X-C motif chemokine ligand 1, involved in angiogenic signaling [58]
- Matrix-Bound Factors: Laminin and type IV collagen in basement membranes support endothelial network stability [17]
Table 2: Biochemical Inducers of Vascularization in Bone Organoids
| Biochemical Factor | Function in Vascularization | Experimental Application |
|---|---|---|
| VEGF165 | Promotes endothelial migration, proliferation & tube formation | 50 ng/mL in endothelial differentiation medium [58] |
| CXCL1 | Chemokine signaling in angiogenesis | Upregulated in endothelial differentiation [58] |
| Laminin | Basement membrane assembly; endothelial adhesion | Key component of Matrigel [17] |
| Type IV Collagen | Structural support for nascent vessels | Key component of Matrigel [17] |
Coupling Mechanical and Biochemical Cues: Experimental Approaches
Engineered Biomaterial Platforms
Advanced culture platforms now enable precise control over both mechanical and biochemical properties to enhance vascularization:
Dynamic Hydrogel Systems:
- PEG-based hydrogels: Allow tunable stiffness and dynamic presentation of adhesion ligands [17]
- Alginate- and DNA-based hydrogels: Feature programmable viscoelasticity [17]
- Photo-responsive hydrogels: Enable spatiotemporal control of mechanical properties [17]
- ECM-DNA-CPO bionic hydrogels: Engineered matrices incorporating bone-derived decellularized ECM, salmon DNA, and calcium phosphate oligomers via photo-crosslinking [59]
Decellularized ECM (dECM): dECMs derived from specific tissues retain organ-specific biochemical compositions and mechanical properties more akin to native tissues than generic matrices like Matrigel. For example, brain-derived dECMs contain approximately 90 brain-specific matrisome proteins, offering improved biological relevance for organoid culture [17].
Experimental Protocol: Creating Pre-vascularized Bone Organoids via DPSC Incorporation
The following workflow details a methodology for creating vascularized bone organoids using dental pulp stem cells (DPSCs), which have demonstrated superior vasculogenic potential compared to bone marrow-derived mesenchymal stem cells (BMSCs) [58]:
Key Methodology Details:
- Construct Fabrication: Spherical cell constructs are fabricated using a temperature-responsive poly-N-isopropylacrylamide (pNIPAAm) hydrogel with hemispherical domes (φ = 1.5 mm) created via 3D printing [58]
- Cell Ratios: Optimal BMSC to DPSC ratios between 95:5 and 80:20 significantly suppress cell necrosis and improve construct viability [58]
- Culture Conditions: Dynamic culture on a seesaw shaker prevents adhesion and promotes three-dimensional organization [58]
- Validation: Successful vascularization evidenced by CD31-positive endothelial lineage cells, lumen-like structures visualized with fluorescently labeled nanoparticles, and significantly reduced necrotic core [58]
Experimental Protocol: Sequential Construction of Vascularized and Mineralized Bone Organoids Using Bionic Matrices
An alternative approach using engineered bionic matrices enables the sequential development of vascularized and mineralized bone organoids:
Key Methodology Details:
- Matrix Composition: Combination of bone-derived decellularized ECM (dECM), salmon-derived DNA, and calcium phosphate oligomers (CPO) [59]
- Fabrication Strategy: Photo-crosslinking and dynamic self-assembly create double-network structure [59]
- Sequential Culture: In vitro dynamic culture followed by in vivo heterotopic ossification [59]
- Functional Outcomes: Efficient bone repair in cranial defect models, demonstrating clinical relevance [59]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Vascularized Bone Organoid Research
| Reagent/Material | Function | Example Application |
|---|---|---|
| Temperature-responsive pNIPAAm hydrogel | Temporary support for 3D cell aggregation | Fabrication of scaffold-free spherical cell constructs [58] |
| Decellularized ECM (dECM) | Organ-specific biochemical and mechanical cues | Provides tissue-specific microenvironment for organoid development [17] [59] |
| DPSCs (Dental Pulp Stem Cells) | Vasculogenic cell source | Endothelial differentiation and lumen formation in BMSC constructs [58] |
| HUVECs (Human Umbilical Vein Endothelial Cells) | Vascular network formation | Coculture for prevascularization in various tissue models [57] |
| Recombinant VEGF165 | Induces endothelial differentiation | 50 ng/mL in endothelial differentiation medium [58] |
| Engineered ECM-DNA-CPO bionic hydrogels | Multifunctional bone-mimicking matrix | Sequential construction of vascularized and mineralized bone organoids [59] |
| Matrigel | Basement membrane matrix for angiogenesis assays | Capillary sprouting assays; initial organoid culture [17] [58] |
| ANQ-11125 | ANQ-11125, CAS:153966-48-4, MF:C86H125N19O21, MW:1761.0 g/mol | Chemical Reagent |
The integration of mechanical and biochemical cues presents a powerful strategy for overcoming the vascularization challenge in bone organoids. By engineering biomaterial systems that recapitulate both the physical properties and signaling environments of native bone tissue, researchers can guide the self-organization of functional vascular networks within developing organoids. The experimental protocols outlined herein, utilizing either DPSC incorporation in scaffold-free constructs or sequential culture in engineered bionic matrices, provide validated approaches for creating pre-vascularized bone organoids with enhanced viability and maturation potential. As these strategies continue to evolve, coupling advanced biomaterial platforms with precise mechanical stimulation will enable the development of increasingly complex and clinically relevant bone organoid models for regenerative medicine, disease modeling, and drug screening applications.
In the evolving field of bone organoid research, the replication of the native skeletal microenvironment—including its mechanical forces—is paramount for producing physiologically relevant models. However, significant batch-to-batch variability currently impedes the reliability and broader adoption of this technology. This variability stems from inconsistencies in cell sources, scaffold materials, culture protocols, and the application of mechanical cues [4] [60]. This technical guide outlines standardized methodologies and quality control measures designed to mitigate this variability, with a specific focus on integrating mechanical stimulation to drive robust bone organoid differentiation and maturation.
The construction of bone organoids is a multi-factorial process, and inconsistencies at any stage can compromise reproducibility. The table below summarizes the primary sources of variability.
Table 1: Key Sources of Batch-to-Batch Variability in Bone Organoid Culture
| Source of Variability | Impact on Organoid Phenotype | Standardization Challenge |
|---|---|---|
| Cell Source (e.g., iPSCs, MSCs, ESCs) [4] [60] | Differentiation efficiency, cellular composition, and ultimate organoid function. | Donor-specific genetic backgrounds, varying differentiation competencies, and passage number effects. |
| Scaffold Material (e.g., Matrigel, collagen hydrogels) [4] | Matrix stiffness, ligand density, and diffusion of nutrients/signals, all critical for mechanotransduction. | Batch-to-batch composition differences in animal-derived products (e.g., Matrigel); poor mechanical stability in synthetic alternatives. |
| Soluble Factors (Growth factors, cytokines) [60] | Directs lineage specification (e.g., osteogenic vs. chondrogenic) and maturation. | Concentration fluctuations, supplier variability, and stability in culture media. |
| Mechanical Cues (e.g., cyclic strain, compression) [4] | Regulates osteogenic commitment, matrix mineralization, and tissue maturation through mechanotransduction pathways. | Lack of standardized equipment, defined loading regimens (frequency, magnitude, duration), and methods for real-time monitoring. |
| Culture Protocol (Differentiation timelines, media changes) [60] | Self-organization potential, structural development, and functional output. | Absence of unified, step-by-step protocols across different laboratories. |
Standardization Strategies for Core Culture Components
Cell Source and Pre-culture Validation
A defined and consistent cellular starting population is the foundation of reproducible organoids.
- Strategy: Utilize well-characterized, low-passage induced pluripotent stem cell (iPSC) or mesenchymal stem cell (MSC) lines. Establish and adhere to a strict banking policy.
- Validation Protocol: Prior to organoid formation, confirm the pluripotency (via flow cytometry for markers like OCT4, SOX2, NANOG) or trilineage differentiation potential (osteogenic, chondrogenic, adipogenic) of the stem cell population. Only use cell batches that pass pre-defined quality thresholds [60].
Defined Scaffold and Extracellular Matrix (ECM)
Moving away from ill-defined, animal-derived matrices is critical for reducing variability.
- Strategy: Employ synthetic or recombinant hydrogels with tunable mechanical properties (e.g., stiffness matching native bone, ~10-30 kPa). Materials like polyethylene glycol (PEG)-based hydrogels functionalized with RGD peptides can provide a defined mechanical and biochemical environment [4].
- Standardization Method: Characterize each hydrogel batch for its storage and loss moduli via rheology. Pre-qualify batches for their ability to support osteogenic differentiation of embedded MSCs over a 14-day period.
Biochemical Signaling and Media Formulation
Precise control over the biochemical milieu minimizes unintended differentiation.
- Strategy: Use a defined, serum-free osteogenic induction media. This eliminates the unknown factors present in fetal bovine serum (FBS).
- Base Formulation: Start with a high-glucose DMEM base. Key components must be aliquoted from single-use, concentrated stocks to ensure consistency [5]. The table below details a proposed formulation.
Table 2: Defined Osteogenic Induction Media for Standardized Bone Organoids
| Component | Final Concentration | Function in Osteogenesis | Critical Quality Control Step |
|---|---|---|---|
| Ascorbic Acid | 50 µg/mL | Essential co-factor for collagen synthesis and matrix maturation. | Prepare fresh weekly; protect from light. |
| β-Glycerophosphate | 10 mM | Source of organic phosphate for matrix mineralization. | Filter sterilize; test for endotoxin levels. |
| Dexamethasone | 100 nM | Glucocorticoid that promotes osteoblast differentiation. | Use a single, qualified supplier; verify biological activity with a reference cell line. |
| BMP-2 | 50 ng/mL | Potent osteoinductive growth factor of the TGF-β superfamily. | Use recombinant human protein; confirm activity via a cell-based assay. |
| WNT Agonist (e.g., CHIR99021) | 3 µM | Activates WNT/β-catenin signaling, crucial for osteoblast lineage commitment [42]. | Verify purity and stability by HPLC. |
Integrating and Standardizing Mechanical Cues
Mechanical stimulation is a defining feature of the bone microenvironment and is indispensable for creating mature, functional organoids.
Mechanotransduction Signaling Pathway
Mechanical forces are converted into biochemical signals that drive osteogenic gene expression. The following diagram illustrates this core pathway.
Standardized Protocol for Applying Dynamic Mechanical Stimulation
To ensure reproducibility, a precise protocol for mechanical loading must be implemented.
- Equipment: Utilize a bioreactor system capable of delivering controlled, uniaxial cyclic strain (e.g., a Flexcell system).
- Differentiation Primer: Pre-differentiate organoids in defined osteogenic media (Table 2) for 7 days to establish a progenitor population.
- Loading Regimen: Initiate mechanical stimulation on day 7. Apply a cyclic strain of 5-10% at a frequency of 0.5 Hz (1 second stretch, 1 second relaxation), for 1 hour per day, over a period of 14 days [4].
- Control: Maintain a static control group of organoids within the same bioreactor chamber but not subjected to strain.
The workflow below outlines the integrated process for creating mechanically stimulated bone organoids.
Quality Control and Analytical Endpoints
Rigorous, quantitative assessment is required to validate organoid reproducibility and functionality across batches.
Table 3: Essential Quality Control Metrics for Bone Organoids
| Analytical Method | Target / Readout | Function in Quality Control | Acceptability Criterion (Example) |
|---|---|---|---|
| qRT-PCR | Gene expression of RUNX2, OSX/SP7, Osteocalcin [42] | Quantifies commitment to and progression of osteogenic differentiation. | >50-fold increase in Osteocalcin vs. undifferentiated control. |
| Immuno-fluorescence/Histology | Protein expression and spatial organization of Osteopontin, Collagen I; Alizarin Red S staining for mineralization. | Visualizes matrix production, cellular organization, and calcium deposition. | Positive, contiguous Alizarin Red S staining in >70% of organoid cross-section. |
| Micro-CT | 3D mineralized tissue volume and trabecular morphology. | Non-destructive quantification of bone-like structure and density. | Bone Volume/Tissue Volume (BV/TV) ratio of 15% ± 3%. |
| Mechanical Testing | Compressive modulus via nanoindentation. | Directly measures functional tissue stiffness and mechanical integrity. | Compressive modulus of 5-30 kPa, correlating with early bone tissue [60]. |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagent Solutions for Standardized Bone Organoid Research
| Item | Function | Critical Specification for Standardization |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Self-renewing, patient-specific cellular starting material for organoid generation [4] [5]. | Use a master cell bank with validated pluripotency and normal karyotype. |
| Tunable Synthetic Hydrogel | Defined 3D scaffold that provides structural support and controllable mechanical cues [4]. | Stiffness tunable between 2-50 kPa; functionalized with cell-adhesive peptides (e.g., RGD). |
| Defined Osteogenic Supplement Kit | A pre-mixed set of growth factors and inducters to direct osteoblast differentiation without serum [60]. | Lyophilized, single-use vials with Certificate of Analysis for precise concentration and activity. |
| Cyclic Strain Bioreactor | Equipment to apply controlled, dynamic mechanical loading to organoids in culture [4]. | Calibrated system capable of delivering precise strain magnitudes (1-15%) and frequencies (0.1-2 Hz). |
| Osteogenesis Antibody Panel | Antibodies for key markers (RUNX2, OSX, Osteocalcin, Osteopontin) for quality control via immunofluorescence. | Validated for immunofluorescence on 3D hydrogel-embedded cultures; lot-to-lot consistency. |
The development of physiologically relevant bone organoids represents a transformative advancement in orthopedic research, disease modeling, and regenerative medicine. Unlike traditional two-dimensional cell cultures, three-dimensional bone organoids aim to recapitulate the complex multicellular architecture and functional properties of native bone tissue [26]. Within this context, the role of mechanical cues has emerged as a fundamental determinant of successful organoid differentiation and maturation. Bone is a dynamic tissue that continuously adapts to mechanical loads in vivo, a process governed by intricate mechanotransduction pathways that regulate osteogenic differentiation, matrix deposition, and mineral homeostasis [4]. Consequently, defining an optimal mechanical regime that avoids the pitfalls of both under-stimulation and over-stimulation is paramount for generating bone organoids with high physiological fidelity.
The challenge lies in identifying the precise mechanical parameters—including the type, magnitude, frequency, and duration of stimulation—that promote osteogenic maturation without inducing pathological responses or cellular damage. Under-stimulation fails to provide essential mechanical signaling, resulting in organoids that lack structural organization and functional properties of native bone. Conversely, over-stimulation can induce excessive mineralization, aberrant cellular differentiation, or even mechanical failure of the construct [61]. This technical review examines current methodologies for applying mechanical stimuli to bone organoids, synthesizes quantitative data on optimal parameters, and provides detailed experimental protocols for implementing these regimes in research settings, all within the framework of advancing bone organoid technology for basic science and therapeutic applications.
Quantitative Analysis of Mechanical Stimulation Parameters
The following tables summarize key quantitative parameters for different mechanical stimulation methods, synthesized from current bone organoid and tissue engineering research. These parameters provide guidelines for establishing regimes that avoid both under-stimulation and over-stimulation.
Table 1: Mechanical Stimulation Parameters for Osteogenic Enhancement
| Stimulation Type | Optimal Magnitude | Frequency | Duration | Key Outcomes |
|---|---|---|---|---|
| Cyclic Uniaxial Strain [4] | 5-10% elongation | 0.5-1 Hz | 30-60 min/day for 7-21 days | Enhanced osteogenic gene expression (Runx2, OPN); Improved collagen alignment |
| Hydrostatic Pressure [26] | 1-10 MPa | 0.1-1 Hz | 30 min/day, 4-5 days/week | Upregulation of osteogenic markers; Increased mineral deposition |
| Shear Stress (Perfusion) [4] | 0.1-1 Pa | Continuous | 7-28 days | Improved nutrient/waste exchange; Enhanced vascular network formation |
| Substrate Stiffness [61] | 10-40 kPa (hydrogel) | Constant | Throughout culture | Directs mesenchymal stem cell fate toward osteogenic lineage |
Table 2: Indicators of Under-Stimulation and Over-Stimulation
| Parameter | Under-Stimulation Indicators | Over-Stimulation Indicators |
|---|---|---|
| Gene Expression | Low Runx2, Osterix, Osteocalcin | Elevated Sox9, PPARγ; Cellular stress markers |
| Mineralization | Delayed or absent mineral nodules | Excessive, disorganized mineralization |
| Cellular Morphology | Reduced cell spreading; Rounded morphology | Cytoskeletal disorganization; Cell detachment |
| Viability/Proliferation | Normal or slightly reduced viability | Significantly reduced viability; Apoptosis |
| Extracellular Matrix | Thin, disorganized collagen network | Abnormally dense, brittle matrix |
Experimental Protocols for Mechanical Conditioning
Protocol 1: Applying Cyclic Strain to Bone Organoids
This protocol details a methodology for applying controlled uniaxial cyclic strain to bone organoids cultured within elastomeric membranes, mimicking the mechanical environment experienced by bone tissue during physical activity.
Research Reagent Solutions:
- Elastomeric Culture Membranes: Flexible silicone-based substrates that undergo precise deformation to transmit strain to adherent cells [4].
- Osteogenic Differentiation Medium: Typically contains β-glycerophosphate, ascorbic acid, and dexamethasone to support bone matrix production [26].
- Fibrin Hydrogel or Calcium-Phosphate Ceramic Scaffolds: Provide a three-dimensional microenvironment that supports cell-matrix interactions and osteogenic differentiation [26].
Methodology:
- Organoid Seeding: Seed mesenchymal stem cells (MSCs) or iPSC-derived osteoprogenitors at a density of 1-5×10^6 cells/mL within a fibrin hydrogel or compatible scaffold on the elastomeric membrane.
- Pre-culture Period: Maintain organoids in osteogenic medium for 7 days without mechanical stimulation to allow for initial cell adhesion and matrix production.
- Stimulation Regime: Apply cyclic uniaxial strain at 5-10% elongation with a frequency of 0.5-1 Hz. Begin with shorter durations (15-30 minutes daily) and gradually increase to 60 minutes over 7-10 days.
- Environmental Control: Perform mechanical stimulation within a standard cell culture incubator (37°C, 5% CO₂) to maintain physiological conditions.
- Assessment: Analyze osteogenic markers (Runx2, Osterix, Osteocalcin) via qPCR and immunohistochemistry after 7, 14, and 21 days of stimulation. Quantify mineralization using von Kossa staining or micro-CT imaging.
Protocol 2: Implementing Hydrostatic Pressure in a Bioreactor System
This protocol describes the application of controlled hydrostatic pressure to bone organoids, simulating the interstitial fluid forces present in bone tissue.
Research Reagent Solutions:
- Hydrostatic Pressure Bioreactor: A sealed, temperature-controlled chamber that allows for precise regulation of pressure levels using compressed gases or pistons [26].
- Collagen-Based or Synthetic Hydrogels: Serve as the 3D scaffold for organoid culture, transmitting hydrostatic forces while supporting osteogenic differentiation.
- Mineralization-Assaying Kits: Contain reagents like Alizarin Red S or OsteoImage for quantifying calcium deposition.
Methodology:
- Organoid Preparation: Encapsulate MSCs at a density of 2×10^6 cells/mL within collagen-based hydrogels and culture in osteogenic medium for 5-7 days to form pre-mineralized organoids.
- Bioreactor Loading: Transfer organoids to the hydrostatic pressure bioreactor chamber filled with pre-warmed osteogenic medium.
- Pressure Application: Apply intermittent hydrostatic pressure at 1-10 MPa with a frequency of 0.1-1 Hz (e.g., 30 minutes of stimulation followed by 30 minutes of rest) for 1-2 cycles daily.
- Medium Exchange: Refresh the osteogenic medium every 2-3 days to ensure adequate nutrient supply throughout the culture period (typically 14-28 days).
- Outcome Measurement: Assess mineralization extent through micro-computed tomography (μCT) and quantify osteogenic gene expression via RNA sequencing. Evaluate matrix composition using immunohistochemistry for collagen type I and osteopontin.
Signaling Pathways in Mechanotransduction
The following diagram illustrates the key signaling pathways through which mechanical stimuli are transduced into biochemical signals that direct osteogenic differentiation in bone organoids.
Mechanotransduction Pathways in Bone Organoids
This diagram illustrates how mechanical stimuli are converted into biochemical signals through key pathways including focal adhesion complexes, mechanosensitive ion channels, and direct nuclear strain. These signals converge on master transcription factors (Runx2, Osterix, ATF4) that drive the expression of osteogenic genes, ultimately leading to bone matrix production and mineralization. Proper mechanical regime design ensures optimal activation of these pathways without reaching saturation or stress-induced downregulation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Mechanical Stimulation Studies
| Reagent/Category | Specific Examples | Function in Mechanical Studies |
|---|---|---|
| Stem Cell Sources | Mesenchymal Stem Cells (MSCs), Induced Pluripotent Stem Cells (iPSCs) | Provide progenitor cells capable of osteogenic differentiation in response to mechanical cues [26]. |
| 3D Scaffold Materials | Fibrin hydrogels, GelMA, Collagen-based scaffolds, Calcium-phosphate ceramics | Create a three-dimensional microenvironment that transmits mechanical forces to encapsulated cells [26] [61]. |
| Advanced Hydrogels | Shell-hardened macroporous hydrogels with tunable degradation | Provide sustained mechanical cues while allowing space for proliferation and protecting cells from excessive load [61]. |
| Osteogenic Media Components | β-glycerophosphate, Ascorbic acid, Dexamethasone | Support bone matrix production and mineralization in conjunction with mechanical stimulation [26]. |
| Mechanosensing Inhibitors | YAP/TAZ inhibitors, Calcium channel blockers, ROCK inhibitors | Experimental tools to dissect specific mechanotransduction pathways [4]. |
| Analysis Kits | Alizarin Red S, OsteoImage, PCR arrays for osteogenic genes | Quantify mineralization and osteogenic differentiation outcomes following mechanical stimulation. |
Establishing an optimal mechanical regime for bone organoid development requires careful balancing of stimulation parameters to avoid both under-stimulation and over-stimulation. The quantitative guidelines, experimental protocols, and reagent toolkit provided herein offer researchers a foundation for implementing mechanical conditioning strategies that enhance the physiological relevance of bone organoids. As the field advances, integrating these mechanical cues with other critical factors such as vascularization and neural innervation will be essential for creating truly biomimetic bone models for research and therapeutic applications [26] [4]. The continued refinement of these approaches will accelerate the development of more predictive in vitro models for bone disease and more effective regenerative therapies for skeletal defects.
The construction of physiologically relevant bone organoids represents a transformative approach in tissue engineering, offering unprecedented opportunities for studying bone biology, disease modeling, and regenerative medicine. The intricate skeletal microenvironment, or niche, governs cellular behavior, tissue organization, and functional maturation through orchestrated interactions between cellular components (skeletal cells, stem cells, vascular cells, immune cells) and non-cellular components (extracellular matrix, soluble signals, vascular networks) [42]. Successfully replicating this complex multicellular system in vitro requires precise coordination of the primary bone lineages: the skeletal lineage (osteoblasts, osteocytes, chondrocytes) and the hematopoietic lineage (osteoclasts, immune cells), integrated with vascular endothelial networks [42]. This coordination is further modulated by mechanical cues, which play a decisive role in directing stem cell differentiation, matrix mineralization, and tissue maturation [4]. The emergence of advanced technologies—including 3D bioprinting, assembloids, and AI-driven optimization—is now enabling researchers to overcome historical challenges in bone organoid construction, particularly the integration of multiple cell types under physiologically relevant mechanical conditions [4].
Core Cellular Components and Their Interactions
Osteoblasts: The Bone-Forming Units
Osteoblasts, the primary bone-forming cells, are polarized, cuboidal, mononuclear cells that synthesize and secrete a distinctive extracellular matrix composed of osteocalcin, osteopontin, alkaline phosphatase, and significant amounts of type I collagen [42]. Their development follows a complex and dynamic pathway, beginning with mesenchymal progenitors that express SOX9, progressing to preosteoblasts marked by RUNX2 expression, and maturing into osteoblasts through WNT-β-catenin signaling which promotes production of osterix (OSX/SP7) [42]. Within the bone microenvironment, osteoblasts function as key regulators by influencing osteoclast differentiation through expression of M-Csf and RANKL, while also mediating hematopoietic stem cell expansion [42].
Osteoclasts: The Bone-Resorbing Counterparts
Osteoclasts, derived from the hematopoietic lineage, are multinucleated giant cells responsible for bone resorption, working in concert with osteoblasts to maintain skeletal homeostasis through the bone remodeling process [42]. Their differentiation is primarily regulated by RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand) expressed by osteoblasts and osteocytes, along with M-CSF (Macrophage Colony-Stimulating Factor) [42]. This tight coupling between osteoblastic and osteoclastic activity ensures balanced bone formation and resorption, a critical interaction that must be recapitulated in advanced bone organoid systems.
Endothelial Cells: The Vascular Network
Endothelial cells form the vascular networks essential for nutrient delivery, waste removal, and oxygen supply in bone tissue. The integration of vascular components is particularly challenging in bone organoid engineering, as native bone tissue is highly vascularized, while existing organoid models typically lack mature vascular networks [4]. Recent approaches have attempted to introduce microvascular endothelial cells into culture systems or employ microfluidic devices to provide fluid perfusion, partially alleviating nutrient transport limitations [4]. Co-culture systems combining human osteoblast-like cells (hOB) and human umbilical vein endothelial cells (HUVECs) have demonstrated the potential for in vitro angiogenesis processes within bone-mimetic environments [42].
Table 1: Core Cellular Components of the Bone Microenvironment
| Cell Type | Lineage Origin | Primary Function | Key Molecular Markers |
|---|---|---|---|
| Osteoblasts | Skeletal/Mesenchymal | Bone matrix synthesis and mineralization | RUNX2, OSX, Alkaline Phosphatase, Osteocalcin [42] |
| Osteocytes | Skeletal/Mesenchymal (terminal differentiation) | Mechanosensing, regulation of bone remodeling | Sclerostin, DKK1, RANKL [42] |
| Osteoclasts | Hematopoietic | Bone resorption | TRAP, Cathepsin K, RANK [42] |
| Endothelial Cells | Mesenchymal | Vasculature formation, nutrient transport | CD31, VE-cadherin, vWF [42] [4] |
| Mesenchymal Stem Cells (MSCs) | Mesenchymal | Osteoprogenitor cells, niche maintenance | SOX9, CD73, CD90, CD105 [42] [7] |
Signaling Pathways Governing Multicellular Crosstalk
The coordination between osteoblasts, osteoclasts, and endothelial cells is mediated through several key signaling pathways. The RANK-RANKL-OPG axis serves as the primary communication channel between osteoblasts and osteoclasts, where osteoblastic RANKL stimulates osteoclast differentiation and activation, while osteoprotegerin (OPG) acts as a decoy receptor to inhibit this process [42]. The WNT-β-catenin pathway plays a crucial role in osteoblast differentiation and bone formation, with osteocytes producing antagonists like sclerostin and DKK1 that regulate WNT signaling activity in response to mechanical loading [42]. Neurotrophic factors, including CGRP and NGF, have recently been identified as significant regulators that promote osteogenic differentiation, angiogenesis, and innervation [7]. Mechanical stimulation induces osteocytes to reduce production of WNT antagonists, thereby promoting osteoblastic bone formation while simultaneously modulating RANKL expression to influence osteoclastic activity [42].
Advanced Construction Methodologies for Multicellular Integration
Biomaterial Scaffolds and 3D Bioprinting Strategies
The choice of scaffold materials significantly impacts the maturation and reproducibility of bone organoids. While Matrigel has been widely used as a 3D scaffold, it presents limitations including batch-to-batch variability, murine protein content, and insufficient mechanical strength comparable to native bone [4]. Advanced bioprinting approaches now enable precise spatial patterning of multiple cell types within tunable hydrogels. For instance, digital light-processing (DLP) printing technology has been utilized to create injectable microsphere-based callus-like organoids that highly recapitulate diverse cell compositions and behaviors of developing bone [7]. These engineered constructs allow for compartmentalized organization of different cellular components, such as creating ossification center-like organoids (OCOs) with inner-core bone morphogenetic and neurotrophic spheroids alongside outer-shell proangiogenic phases [7].
Assembloid Approaches for Heterotypic Cellular Integration
Assembloid technology enables the integration of distinct cellular populations to reconstruct physiological tissue complexity. This approach involves generating separate spheroids of different cell lineages—osteoblastic, endothelial, and osteoclastic—and subsequently fusing them into a single, more complex structure [4]. A notable application involves creating vascularized bone assembloids by combining MSC-derived bone organoids with endothelial network assembloids, thereby addressing the critical limitation of vascularization in traditional bone organoids [4]. These assembloids can further incorporate neurovascular components by including sensory neuron spheroids, recapitulating the neuro-vascular-bone axis that is essential for physiological bone function and repair [7].
Mechanical Conditioning Bioreactors
Mechanical forces play a critical role in bone development by regulating cellular behaviors such as proliferation, differentiation, and matrix mineralization through mechanotransduction pathways [4]. specialized bioreactor systems have been developed to apply controlled mechanical stimuli—including cyclic compression, fluid shear stress, and vibrational forces—to developing bone organoids [4]. Dynamic loading has been shown to promote osteogenic lineage commitment of MSCs and enhance endothelial network formation, thereby supporting coordinated development of vascularized bone tissue [4]. These systems aim to mimic the native mechanical environment of bone, which is largely absent in conventional static culture conditions, leading to improved matrix organization and mineralization.
Table 2: Advanced Technologies for Multicellular Bone Organoid Construction
| Technology | Primary Application | Key Advantages | Impact on Multicellular Integration |
|---|---|---|---|
| 3D Bioprinting with DLP | Spatial patterning of cell types | Precise microarchitecture, compartmentalized organization | Enables creation of OC-like organoids with distinct zones [7] |
| Microfluidic Systems | Vascular network formation | Continuous perfusion, physiological shear stress | Enhances endothelial cell organization and vessel maturation [4] |
| Assembloid Technology | Integration of heterotypic cells | Modular design, self-organization capacity | Facilitates fusion of vascular and bone modules [4] |
| Mechanical Bioreactors | Application of mechanical cues | Mimics physiological loading conditions | Promotes osteocyte maturation, matrix mineralization [4] |
| Gene Editing (CRISPR) | Cell fate programming | Precise genetic manipulation, lineage tracing | Enables generation of reporter lines for different cell types [4] |
Experimental Protocols for Multicellular Bone Organoid Generation
Protocol 1: Engineering Ossification Center-like Organoids (OCOs)
This protocol describes the generation of ossification center-like organoids with integrated neurotrophic and angiogenic components, based on the "divide-and-conquer" strategy reported for rapid bone regeneration [7].
Materials and Reagents:
- Human Mesenchymal Stem Cells (MSCs)
- Fibrin-based bioink supplemented with gelatin methacrylate
- Bone Morphogenetic Protein-2 (BMP-2) at 0.5 μg/mL
- Calcitonin Gene-Related Polypeptide (CGRP) at 10â»â¸ M
- Endothelial Growth Medium-2
- Digital Light Processing (DLP) bioprinter
Methodology:
- Inner Core Formation: Prepare a spheroid of 2×10ⶠMSCs/mL in fibrin-gelatin methacrylate bioink supplemented with BMP-2 (0.5 μg/mL) and CGRP (10â»â¸ M). Bioprint using DLP technology into spherical constructs of 500 μm diameter.
- Outer Shell Assembly: Suspend the printed inner cores in a secondary bioink containing HUVECs (1×10ⶠcells/mL) and additional angiogenic factors (VEGF, FGF-2).
- Maturation Culture: Transfer the assembled OCOs to osteogenic differentiation medium (DMEM with 10% FBS, 50 μg/mL ascorbate-2-phosphate, 10 mM β-glycerophosphate) under dynamic culture conditions for 14-21 days.
- In Vivo Implantation (Optional): For translational applications, implant OCOs collectively into critical-sized bone defects using a "divide-and-conquer" approach to achieve rapid bone bridging through successive ossification center formation.
Validation:
- Single-cell RNA sequencing to identify recruited stem cell populations (Krt8+ skeletal stem cells)
- Micro-CT analysis for mineralization assessment
- Immunohistochemistry for osteogenic (RUNX2, Osteocalcin), angiogenic (CD31), and neurotrophic (CGRP) markers
Protocol 2: Vascularized Bone Assembloid via Modular Assembly
This protocol describes the generation of vascularized bone assembloids through the fusion of separately pre-differentiated bone and vascular modules [4].
Materials and Reagents:
- Human induced Pluripotent Stem Cells (iPSCs)
- Mesenchymal Stem Cell Expansion Medium
- Endothelial Cell Growth Medium-2
- Matrigel (or alternative synthetic hydrogel)
- Transforming Growth Factor-β (TGF-β)
- Vascular Endothelial Growth Factor (VEGF)
Methodology:
- Bone Module Differentiation: Differentiate iPSCs toward osteoblastic lineage using a staged protocol:
- Days 0-3: Mesoderm induction with BMP-4 (10 ng/mL) and FGF-2 (20 ng/mL)
- Days 3-10: Osteoprogenitor specification with ascorbic acid (50 μg/mL) and β-glycerophosphate (10 mM)
- Days 10-28: Osteogenic maturation with dexamethasone (100 nM) and BMP-2 (50 ng/mL)
- Vascular Module Formation: Differentiate iPSCs toward endothelial lineage:
- Days 0-4: Mesoderm induction with BMP-4 (10 ng/mL) and Activin A (10 ng/mL)
- Days 4-8: Endothelial specification with VEGF (50 ng/mL) and FGF-2 (20 ng/mL)
- Days 8-15: Vascular network maturation in 3D fibrin gel with VEGF (50 ng/mL)
- Assemblod Fusion: Combine bone and vascular modules at a 2:1 ratio in a low-adhesion U-bottom plate. Centrifuge at 300×g for 5 minutes to initiate contact and culture in a 1:1 mixture of osteogenic and endothelial media.
- Mechanical Conditioning: Subject fused assembloids to cyclic uniaxial compression (10% strain, 1 Hz, 30 min/day) using a custom bioreactor system to enhance matrix organization and mineralization.
Validation:
- Confocal microscopy of perfusable vascular networks
- Quantification of osteocalcin secretion by ELISA
- Mechanical testing of mineralized matrix properties
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Multicellular Bone Organoid Research
| Reagent/Material | Function | Application Example | Considerations |
|---|---|---|---|
| BMP-2 (0.5 μg/mL) | Osteoinductive morphogen | Synergizes with CGRP to enhance osteogenic differentiation at physiological doses [7] | High concentrations lead to ectopic bone formation; optimal at 0.5 μg/mL with CGRP [7] |
| CGRP (10â»â¸ M) | Neuropeptide, osteogenic amplifier | Significantly increases ALPL and RUNX2 expression in combination with BMP-2 [7] | Reduces cell senescence (γh2AX) while increasing proliferation (Ki67) [7] |
| Fibrin-GelMA Bioink | 3D bioprinting matrix | Provides tunable mechanical properties and cell adhesion sites for DLP printing [7] | Offers superior printability and biocompatibility compared to Matrigel alone [7] [4] |
| Decellularized ECM (daCO-DM) | Osteocyte-derived niche matrix | Increases expression of RANKL, MCSF, Vegfa, Angpt1, and Ngf in BMSCs [42] | Prepared from osteocytes with active WNT signaling via freeze-thaw cycling and DNase I treatment [42] |
| RANKL (100 ng/mL) | Osteoclast differentiation factor | Essential for generating functional osteoclasts in tri-culture systems | Must be balanced with M-CSF (25-50 ng/mL) for proper osteoclastogenesis [42] |
| VEGF (50 ng/mL) | Angiogenic factor | Critical for endothelial network formation in vascularized assembloids | Optimal concentration prevents excessive vascular leakage while supporting stable tubulogenesis [4] |
Quantitative Analysis of Multicellular Integration Outcomes
Table 4: Quantitative Metrics for Evaluating Multicellular Bone Organoids
| Evaluation Parameter | Measurement Technique | Expected Outcome | Significance |
|---|---|---|---|
| Osteogenic Differentiation | ALP activity (Day 7), Alizarin Red staining (Day 14) | 2.5-3.5 fold increase with CGRP+BMP-2 vs. BMP-2 alone [7] | Confirms synergistic effect of neuro-osteogenic coupling |
| Gene Expression | qRT-PCR for RUNX2, OSX, Osteocalcin | Significant upregulation of RUNX2 and OSX with combinatorial cues [7] | Indicates osteoblast lineage commitment and maturation |
| Cell Proliferation/Senescence | Immunostaining for Ki67 and γh2AX | Increased Ki67+, decreased γh2AX+ with CGRP treatment [7] | Demonstrates maintained MSC potency and reduced stress |
| Vascularization | CD31+ tubular structures, perfusion assays | Formation of interconnected networks with lumen after 14 days [4] | Essential for nutrient transport in larger organoids |
| Stem Cell Recruitment | scRNA-seq for Krt8+ SSCs | Specific expansion of Krt8+ SSCs with concomitant reduction of Has1+ MFs [7] | Indicates recapitulation of developmental niche |
| Mineralization | Micro-CT, Energy Dispersive X-ray Spectroscopy | Hydroxyapatite deposition with Ca/P ratio of 1.6-1.7 [42] | Confirms bone-like matrix composition |
The integration of multiple cell types—osteoblasts, osteoclasts, and endothelial cells—within mechanically conditioned bone organoids represents a paradigm shift in bone tissue engineering. By employing advanced biofabrication strategies such as 3D bioprinting, assembloid technology, and mechanical bioreactors, researchers can now create increasingly sophisticated models that recapitulate key aspects of the native bone microenvironment. The synergistic combination of biochemical cues (BMP-2, CGRP) with appropriate mechanical stimulation and scaffold design enables the development of organoids that not only exhibit structural similarity to bone tissue but also demonstrate functional properties including mineralization, vascularization, and remodeling capability. As these technologies continue to evolve, integrated multicellular bone organoids will play an increasingly important role in advancing our understanding of bone biology, disease mechanisms, and regenerative therapeutic strategies.
The extracellular matrix (ECM) serves as a dynamic biomechanical regulator of cellular behavior, orchestrating key processes in bone development, homeostasis, and regeneration [18]. Conventional three-dimensional (3D) culture systems, particularly those reliant on Matrigel, a murine sarcoma-derived basement membrane extract, have been instrumental in the rise of organoid technology. However, for the field of bone organoid engineering, Matrigel's fundamental limitations—its batch-to-batch variability, tumorigenic origin, and, most critically, its static and soft mechanical properties—pose a significant barrier to progress [62] [4]. Bone is a mechanically robust tissue whose development is guided by precise biomechanical cues; Matrigel's inability to recapitulate the stiff, viscoelastic microenvironment of native bone compromises the maturation and physiological relevance of bone organoids [4] [5].
This whitepaper delineates the critical need to transition from ill-defined, animal-derived matrices to precisely engineered synthetic hydrogels. Framed within the context of bone organoid research, we explore how defined synthetic hydrogels provide the necessary mechanical control to dissect mechanotransductive pathways, enhance osteogenic differentiation, and ultimately generate more predictive in vitro models for drug screening and regenerative medicine.
The Case for Change: Limitations of Matrigel in Bone Research
Matrigel's composition is complex and undefined, leading to substantial batch-to-batch variations that undermine experimental reproducibility and data reliability [62] [4]. Its murine tumor origin introduces xenogenic proteins and growth factors that can skew human cell differentiation and preclude clinical translation [62]. From a mechanical perspective, Matrigel is fundamentally mismatched with bone biology. Its soft, static properties fail to provide the sustained mechanical cues necessary for osteogenic lineage commitment [4] [63].
A primary technical bottleneck in bone organoid construction is replicating the biomechanical environment of native bone tissue. Mechanical forces play a critical role in bone development by regulating cellular behaviors such as proliferation, differentiation, and matrix mineralization through mechanotransduction pathways [4]. Most organoid cultures in Matrigel are maintained in static conditions, lacking these essential mechanical cues, which can lead to deviations from physiological osteogenic differentiation [4]. Furthermore, Matrigel possesses limited mechanical strength and fails to provide a rigid microenvironment comparable to native bone, which is essential for guiding stem cell differentiation towards osteoblasts [4] [63].
Synthetic Hydrogels: A Platform for Precision Mechanics
Defined synthetic hydrogels, most notably those based on poly(ethylene glycol) (PEG), offer a solution to Matrigel's limitations. Their synthesis allows for independent tuning of key biomechanical properties, creating a tailored microenvironment for bone organoid development [18] [63].
Table 1: Tunable Mechanical Properties of Synthetic Hydrogels and Their Impact on Osteogenesis
| Mechanical Property | Definition | Influence on Osteogenic Differentiation | Optimal Range for Osteogenesis |
|---|---|---|---|
| Elasticity (Stiffness) | Resistance to deformation under applied stress; measured by Young's or shear modulus. | A primary driver of osteogenesis; stiffer substrates promote osteodifferentiation via mechanosensitive pathways like YAP/TAZ [63]. | Shear modulus of ~30-50 kPa is often optimal, though consensus varies [63]. |
| Viscoelasticity | Time-dependent, energy-dissipating response to stress (a combination of solid and liquid properties). | High viscoelasticity enhances cell spreading, proliferation, and osteogenic marker expression compared to purely elastic substrates [63]. | A high loss tangent (ratio of viscous to elastic modulus) is favorable [63]. |
| Degradability | The rate at which the hydrogel network breaks down, creating space for new matrix deposition. | Must synchronize with new tissue formation; too slow hinders cell proliferation, too fast compromises mechanical integrity [36]. | Tunable via crosslinker chemistry (e.g., degradable ester bonds) [36]. |
The synergy between mechanical properties and biochemical functionalization is critical. Research demonstrates that the mechanical properties of hydrogels are a primary factor in driving differentiation, as biofunctionalization alone is insufficient to induce robust osteogenesis [63]. Functionalization with osteogenic peptides like BMP-2 mimetics can boost osteodifferentiation, but only in materials with adequate mechanical properties [63].
Experimental Protocols: Designing and Validating Mechanically Defined Hydrogels
Protocol: Fabricating Tunable PEGDA Hydrogels for Osteogenic Screening
This protocol details the creation of a hydrogel library with varying mechanical and biochemical properties to screen for optimal osteo-inductive conditions [63].
- Hydrogel Precursor Preparation: Prepare stock solutions of PEG-diacrylate (PEGDA) with different molecular weights (e.g., 400 Da and 4000 Da) in phosphate-buffered saline (PBS). To create hydrogels with a range of stiffness and viscoelasticity, mix the long and short PEGDA chains at varying ratios (e.g., 100/0, 50/50, 0/100) and total polymer concentrations (e.g., 10%, 20%, 30% w/v).
- Biofunctionalization: Covalently incorporate cell-adhesive and osteo-inductive peptides into the hydrogel network. A common approach is to use acryloyl-PEG-RGD (e.g., CG-K-GGRGDS) and a BMP-2 mimetic peptide. These are added to the precursor solution before polymerization. The ratio of RGD to BMP-2 peptide can be systematically varied (e.g., 100:0, 75:25, 50:50).
- Polymerization: Add the photoinitiator Irgacure 2959 (0.7 wt%) to the precursor solution. Cast the solution into cylindrical molds and polymerize under UV light (365 nm) for 15 minutes.
- Swelling and Sterilization: Swell the polymerized hydrogels in PBS for at least 24 hours to reach equilibrium swelling. Sterilize according to standard cell culture protocols.
- Mechanical Validation: Characterize the elastic and viscous shear moduli (G' and G") of each hydrogel formulation using rheometry.
Protocol: Assessing Osteogenic Outcomes in 3D Culture
- Cell Encapsulation: Suspend human Mesenchymal Stem Cells (hMSCs) in the sterile hydrogel precursor solution at the desired density (e.g., 1-10 million cells/mL). Proceed with polymerization as in step 1.3.
- Culture: Maintain cell-laden hydrogels in standard growth or osteogenic differentiation medium. Use hydrogels with minimal biofunctionalization as a negative control.
- Outcome Analysis:
- Early Markers (7 days): Quantify gene expression of early osteogenic markers like ALPL (Alkaline Phosphatase) and RUNX2 via qPCR. Perform Alkaline Phosphatase (ALP) staining as a functional assay.
- Late Markers (14-21 days): Assess matrix mineralization using Alizarin Red S (ARS) staining. Analyze gene and protein expression of late markers like Osteopontin (OPN) and Osteocalcin (OCN).
- Mechanotransduction Signaling: Perform immunocytochemistry to visualize the nuclear localization of YAP/TAZ, key effectors of mechanotransduction.
Advanced Hydrogel Systems and Engineering Strategies
Innovations in hydrogel design are pushing the boundaries of bone organoid engineering. Shell-hardened macroporous hydrogels utilize liquid-liquid phase separation to create structures where a rigid, lysozyme nanofiber-coated pore shell provides sustained mechanical cues for osteodifferentiation, while a softer, degradable hydrogel matrix accommodates cell proliferation and new tissue deposition [36]. This decouples the mechanical cue for differentiation from the degradable bulk material.
Furthermore, the field is moving towards spatiotemporally programmed mechanical properties. For instance, "ossification center-like organoids" (OCOs) can be engineered using 3D bioprinting to create constructs with dual-modular compartments, delivering neurotrophic and osteogenic factors (e.g., CGRP and BMP-2) in a spatially controlled manner to mimic developmental niches and recruit endogenous stem cells for rapid bone regeneration [7].
The diagram below illustrates the key mechanotransduction pathway through which hydrogel mechanics influence cell fate.
Diagram 1: Mechanotransduction in Osteogenic Differentiation. This pathway illustrates how a hydrogel's mechanical properties are biochemically sensed by cells, leading to osteogenic commitment via YAP/TAZ signaling.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Defined Synthetic Hydrogel Research
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| PEG-diacrylate (PEGDA) | Synthetic polymer backbone for hydrogel formation; modulus tuned by MW & concentration. | Various molecular weights (e.g., 400 Da, 4000 Da); from Sigma-Aldrich or PolyScience [63]. |
| Acryloyl-PEG-RGD | Peptide conjugate for integrin-mediated cell adhesion. | Critical for cell survival and mechanosensing; e.g., CG-K-GGRGDS [63]. |
| BMP-2 Mimetic Peptide | Peptide sequence mimicking Bone Morphogenetic Protein-2 to induce osteogenesis. | Synergizes with mechanical cues; e.g., KRKIPKASSVPTELSAISMLYLC [63]. |
| Photoinitiator | Initiates free-radical polymerization upon UV exposure. | Irgacure 2959; requires UV light at 365 nm [63]. |
| Lysozyme Nanofibers | Protein nanofiber for creating reinforced, stiff pore shells in macroporous hydrogels. | Modified with acryl groups for covalent attachment to hydrogel matrix [36]. |
| Fibrinogen/Thrombin | Animal-free, human-derived natural polymer system for 3D culture. | Supports robust vascular network formation; a key Matrigel alternative [62]. |
| Vitronectin | Recombinant human protein for xeno-free 2D cell culture and expansion. | Used as a substrate for hiPSCs prior to 3D differentiation; e.g., Vitronectin XF [62]. |
The following diagram integrates these components into a representative workflow for creating and testing advanced bone organoid culture platforms.
Diagram 2: Workflow for Building Bone Organoids in Defined Hydrogels. This experimental workflow outlines the key steps from cell preparation to analysis, highlighting the use of defined materials at each stage.
The transition from Matrigel to defined synthetic hydrogels is not merely a technical improvement but a fundamental necessity for advancing bone organoid research. The precise control over mechanical and biochemical cues afforded by systems like tunable PEG hydrogels enables researchers to dissect complex mechanobiological mechanisms with unprecedented clarity. The integration of these advanced biomaterial platforms with other cutting-edge technologies—such as 3D bioprinting for spatial patterning, AI for data-driven optimization of culture conditions, and organ-on-a-chip systems for incorporating perfusion and mechanical loading—will further accelerate the development of physiologically relevant, vascularized bone organoids [18] [4]. This convergence of disciplines promises to yield robust, human-based in vitro models that will profoundly impact our understanding of bone biology, enhance preclinical drug screening, and pave the way for new regenerative therapies.
The Role of Artificial Intelligence in Optimizing Complex Mechanical Culture Parameters
The development of physiologically relevant bone organoids represents a frontier in regenerative medicine, disease modeling, and drug screening. Unlike traditional two-dimensional cultures, bone organoids aim to recapitulate the complex three-dimensional (3D) architecture and multicellular composition of native bone tissue [4] [5]. A critical but often overlooked aspect of this complexity is the mechanobiological microenvironment—the dynamic physical forces and mechanical properties that profoundly influence bone development, homeostasis, and disease progression [17]. In vivo, bone cells exist within a carefully tuned mechanical environment characterized by specific stiffness, viscoelasticity, fluid shear stress, and topographic cues that guide their differentiation and function [64]. Replicating this environment in vitro presents a formidable challenge due to the multivariate nature of these parameters and their complex interactions with biochemical signaling pathways.
Artificial intelligence (AI) and machine learning (ML) are emerging as transformative tools to decode and optimize these complex mechanical culture systems [4] [64]. By analyzing high-dimensional datasets extracted from advanced imaging, force measurements, and molecular profiling, AI can identify non-intuitive relationships between mechanical parameters and biological outcomes that escape conventional analysis. This technical guide explores how AI methodologies are being deployed to optimize the mechanical culture parameters for bone organoid development, thereby accelerating the creation of more physiologically relevant and reproducible model systems for researchers, scientists, and drug development professionals.
Fundamental Mechanical Cues in Bone Organoid Culture
The successful maturation of bone organoids depends on recapitulating key mechanical properties of the native bone marrow and mineralized matrix microenvironment. The following parameters are particularly critical.
Substrate Stiffness and Viscoelasticity
The extracellular matrix (ECM) stiffness, typically measured in kilopascals (kPa), provides essential physical cues that direct stem cell lineage commitment. For osteogenic differentiation, stiffer matrices (ranging from 20-40 kPa) have been shown to promote osteoblast differentiation and bone matrix mineralization by enhancing cellular contractility and activating mechanosensitive transcription factors such as YAP/TAZ [64] [17]. Beyond static stiffness, the viscoelasticity of the culture substrate—its ability to exhibit both solid-like (elastic) and fluid-like (viscous) properties—has emerged as an equally important regulator of cell behavior. Viscoelastic matrices that allow for stress relaxation promote osteogenic differentiation by enabling cells to remodel their surroundings and generate traction forces more effectively [17].
Dynamic Mechanical Stimulation
Native bone tissue constantly experiences dynamic loads. In vitro, applying cyclic strain (typically 0.5-10% elongation at 0.5-1 Hz) or compressive loading (1-15% compression) through specialized bioreactors mimics this physiological mechanical environment, promoting osteogenic marker expression (e.g., Runx2, Osterix) and mineral deposition [4]. Furthermore, fluid shear stress (0.1-3 Pa) generated by perfusion systems within 3D scaffolds enhances nutrient delivery, waste removal, and osteogenic differentiation while also supporting the formation of vascular networks—a major limitation in current bone organoid systems [4] [65].
Matrix Topography and 3D Architecture
The spatial organization of the ECM at both micro- and nano-scales significantly influences cell morphology and signaling. In 3D cultures, pore size (100-400 μm), fiber alignment, and surface roughness of scaffold materials direct cell migration, proliferation, and differentiation [64] [65]. Computational models have revealed that scaffolds with higher surface-area-to-volume ratios and specific architectural features can enhance both bone regeneration and angiogenesis by creating distinct mechanical microenvironments [65].
Table 1: Key Mechanical Parameters for Bone Organoid Culture and Their Biological Impact
| Mechanical Parameter | Typical Optimal Range for Osteogenesis | Primary Biological Effects | Key Signaling Pathways Involved |
|---|---|---|---|
| Substrate Stiffness | 20-40 kPa | Enhances osteoblast differentiation, matrix mineralization | YAP/TAZ, Rho/ROCK, FAK/MAPK |
| Viscoelasticity (Stress Relaxation) | Timescale: seconds to minutes | Facilitates cell spreading, traction force generation, osteogenic commitment | Integrin clustering, Actomyosin contractility |
| Cyclic Strain (Tensile) | 0.5-10% at 0.5-1 Hz | Promotes alignment, collagen organization, osteogenic marker expression | Wnt/β-catenin, TGF-β |
| Fluid Shear Stress | 0.1-3 Pa | Enhances osteogenic differentiation, mineral deposition, vascular network formation | PGE2, NO, BMP/Smad |
| Scaffold Pore Size | 100-400 μm | Influences cell infiltration, spatial organization, nutrient diffusion | Integrin-mediated adhesion |
AI-Driven Methodologies for Parameter Optimization
The multivariate optimization of mechanical culture parameters presents an ideal application for AI and ML approaches, which can identify complex patterns in high-dimensional datasets that would be intractable through traditional experimental design.
Predictive Modeling of Cell Response to Mechanical Cues
AI models, particularly supervised learning algorithms including Random Forests and Support Vector Machines, can be trained on multimodal experimental data to predict osteogenic outcomes based on specific mechanical input parameters [64]. Training data typically includes quantitative measurements of substrate mechanical properties, temporal loading patterns, and corresponding biological responses such as gene expression profiles, protein secretion, and matrix mineralization metrics. For instance, ML models can learn to predict the expression of key osteogenic markers (e.g., RUNX2, OCN) based on specific combinations of stiffness, strain magnitude, and fluid shear stress, thereby guiding the design of optimal culture regimens [64].
Image-Based Analysis of Organoid Morphology and Maturation
Convolutional Neural Networks (CNNs) can automate the quantitative analysis of bone organoid images obtained through microscopy, micro-CT, or scanning electron microscopy. These models can rapidly characterize critical features such as organoid size, shape, spatial distribution of mineralized nodules, and capillary network formation—morphological indicators that correlate with functional maturation [4] [5]. This approach dramatically increases analysis throughput and objectivity compared to manual scoring, enabling large-scale screening of mechanical culture conditions.
Experimental Design and High-Throughput Screening
Bayesian optimization and other active learning strategies can efficiently navigate the vast parameter space of mechanical culture conditions (e.g., stiffness ranges, loading regimes, scaffold architectures) to identify optimal combinations with minimal experimental iterations [4]. These AI-driven design frameworks can be integrated with high-throughput screening platforms where hundreds of organoids are cultured under slightly varied mechanical conditions in parallel. The AI algorithm iteratively refines testing hypotheses based on previous outcomes, dramatically accelerating the optimization process compared to traditional one-factor-at-a-time approaches.
Table 2: AI/ML Approaches for Optimizing Mechanical Culture Parameters
| AI Methodology | Primary Application in Mechanobiology | Input Data Types | Output Predictions |
|---|---|---|---|
| Random Forests / Gradient Boosting | Predicting differentiation outcomes from multivariate mechanical cues | Stiffness, load magnitude/frequency, cytokine levels | Osteogenic score, Mineralization potential, Gene expression patterns |
| Convolutional Neural Networks (CNNs) | Automated analysis of organoid morphology and microstructure | 2D/3D microscopy images, μCT scans | Mineralized area, Spatial organization, Vessel formation, Cell alignment |
| Bayesian Optimization | Efficient experimental design for culture parameter screening | Historical experimental results, Real-time sensor data | Optimal parameter sets for next experimental iteration |
| Recurrent Neural Networks (RNNs) | Modeling temporal responses to dynamic mechanical stimulation | Time-series data (e.g., calcium signaling, gene expression) | Long-term differentiation trajectories, Oscillatory gene expression |
Integrated AI-Driven Workflow for Mechanobiological Optimization
The following diagram illustrates the continuous feedback loop between AI prediction and experimental validation in optimizing bone organoid culture systems:
AI-Driven Optimization Workflow
Experimental Protocols for AI-Guided Mechanobiological Studies
Protocol: High-Throughput Screening of Substrate Mechanics
This protocol details the integration of AI with experimental screening to identify optimal substrate properties for bone organoid formation.
Materials:
- PEG-based hydrogels with tunable stiffness and viscoelasticity [17]
- Human induced pluripotent stem cells (iPSCs) or mesenchymal stem cells (MSCs)
- 24-well or 96-well hydrogel array plates with varying mechanical properties
- Osteogenic induction media (ascorbic acid, β-glycerophosphate, dexamethasone)
- Automated live-cell imaging system
- RNA sequencing and immunostaining capabilities
Method:
- Fabricate hydrogel arrays with systematic variation in stiffness (1-50 kPa) and stress relaxation timescales using PEG-based hydrogels with controlled crosslink density and degradable linkages [17].
- Seed iPSCs or MSCs in osteogenic induction media on hydrogel arrays at standardized density (e.g., 10,000 cells/well for 96-well format).
- Apply dynamic mechanical stimulation using a programmable bioreactor system that imposes cyclic compression (1-10% strain, 0.5-1 Hz) or fluid shear stress (0.1-3 Pa).
- Monitor organoid development over 14-28 days using automated brightfield and fluorescence microscopy to track morphology, size, and mineralization (via Alizarin Red staining).
- Harvest organoids at multiple timepoints for transcriptomic analysis (RNA-seq) and protein expression profiling (immunostaining for OPN, OCN, BSP).
- Train ML models using mechanical parameters as inputs and morphological/ molecular readouts as targets to identify optimal conditions.
- Validate AI predictions by testing recommended parameter sets in independent culture experiments.
Protocol: Computational Modeling of Scaffold Architecture Effects
This in silico protocol complements experimental approaches by predicting how 3D scaffold architecture influences bone regeneration and angiogenesis.
Materials:
- Scaffold design files (STL format) for 3D-printed architectures
- Mechanical testing system for quantifying scaffold properties
- Custom computational model integrating angiogenesis and osteogenesis
- Micro-CT imaging for scaffold and tissue structure analysis
Method:
- Design scaffold variations with controlled differences in strut spacing, pore size (100-400 μm), and surface-area-to-volume ratio using CAD software.
- 3D print scaffolds using melt electrowriting (for micro-scale features) or fused deposition modeling (for larger features) with biocompatible materials [65].
- Characterize mechanical properties of each scaffold design using compression testing to determine effective stiffness and porosity.
- Implement computational model that simulates oxygen/nutrient diffusion, cell migration, and mechanosensitive tissue formation based on local mechanical strains [65].
- Validate model predictions by seeding scaffolds with MSCs and monitoring bone formation and vessel infiltration over 4-8 weeks in vivo or in advanced bioreactors.
- Apply gradient boosting regression to identify the most influential architectural features predicting successful bone regeneration.
- Generate design rules for optimal scaffold architectures tailored to specific bone defect applications.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Mechanobiological Studies of Bone Organoids
| Reagent/Platform | Function | Mechanical Parameters Addressed |
|---|---|---|
| PEG-based Hydrogels | Synthetic, tunable 3D culture matrix with definable mechanical properties | Stiffness (1-100 kPa), Viscoelasticity, Ligand density |
| Matrigel/Decellularized ECM (dECM) | Biologically derived matrices providing complex biochemical cues | Baseline stiffness (~20-450 Pa), Limited biological cues [17] |
| Cyclic Strain Bioreactors | Application of controlled tensile or compressive forces | Strain magnitude (0.5-15%), Frequency (0.1-2 Hz), Duration |
| Perfusion Bioreactor Systems | Continuous medium flow through 3D constructs | Fluid shear stress (0.1-10 Pa), Mass transport enhancement |
| Atomic Force Microscopy (AFM) | Nanoscale measurement of local mechanical properties | Elastic modulus, Viscoelastic parameters, Adhesion forces |
| Tunable Organ-on-Chip Platforms | Microfluidic systems with integrated mechanical actuation | Tissue-level deformation, Endothelial-epithelial mechanical crosstalk |
Mechanotransduction Signaling Pathways in Bone Organoids
The following diagram summarizes the key mechanotransduction pathways through which optimized mechanical parameters influence bone organoid differentiation and maturation:
Mechanotransduction Signaling Pathways
The integration of artificial intelligence with mechanobiological engineering represents a paradigm shift in the development of advanced bone organoid systems. By systematically decoding the complex relationships between mechanical parameters and biological responses, AI-driven approaches enable the rational design of culture environments that closely mimic the native bone microenvironment [4] [64]. This synergy addresses critical challenges in bone organoid development, including vascularization, structural complexity, and functional maturation, which have traditionally limited their physiological relevance and translational potential [4] [5].
Future advancements in this field will likely involve the development of closed-loop AI systems that continuously adapt mechanical stimulation parameters based on real-time monitoring of organoid development. Furthermore, the integration of multi-omics data with mechanical signaling information will provide unprecedented insights into the molecular mechanisms underlying mechanotransduction in bone formation and regeneration. As these technologies mature, AI-optimized bone organoids will become indispensable tools for personalized medicine, drug screening, and fundamental studies of skeletal biology, ultimately bridging the gap between in vitro models and human bone physiology.
Benchmarking Success: Validating Mechanically Matured Bone Organoids Against Established Models
Within the rapidly advancing field of bone organoid research, the need for robust, standardized functional readouts is paramount for assessing model fidelity and maturation. This guide details core methodologies for evaluating key physiological processes in developing bone organoids, with particular emphasis on how these readouts illuminate the role of mechanical cues in differentiation and maturation. As three-dimensional biomimetic constructs, bone organoids aim to recapitulate the intricate cellular interactions and biological processes of native bone tissue, providing a transformative platform for studying bone development, disease modeling, and drug screening [4] [5]. However, the current generation of bone organoids faces significant challenges in achieving full functional equivalence with natural tissues, particularly in replicating the biomechanical properties and mineralized matrix of native bone [5]. Accurately measuring mineralization, matrix deposition, and gene expression is therefore essential not only for validating these models but also for elucidating how mechanical forces—integral to bone's physiological environment—orchestrate cellular behavior and tissue-level organization. These functional assessments provide the critical data necessary to bridge the gap between experimental models and clinical translation, ultimately advancing personalized medicine and therapeutic interventions for skeletal diseases [4].
Core Functional Readouts and Their Interrelationships
The maturation and functionality of bone organoids are evaluated through a triad of core assessments: mineralization, matrix deposition, and gene expression. These readouts are not independent; rather, they exist in a tightly regulated, interdependent relationship that drives the bone formation process, a relationship profoundly influenced by mechanical cues as illustrated below.
This feedback loop is critical for bone organoid maturation. The state of matrix mineralization itself provides a functional signal to osteoblasts, independently controlling gene expression [66]. Studies demonstrate that osteoblasts residing on mineralized versus demineralized osseous surfaces exhibit markedly different gene expression signatures, with mineralized surfaces favoring intracellular protein production [66]. Furthermore, spatial and temporal correlations between gene expression and mineralization have been established in model systems like the avian leg tendon, where genes such as Bone Sialoprotein (BSP) appear to be key markers for impending mineral formation [67].
Quantitative Assessment Methodologies
A suite of techniques is employed to quantitatively assess these functional readouts. The table below summarizes the primary assays, their applications, and key experimental considerations.
Table 1: Core Methodologies for Assessing Bone Organoid Functionality
| Assessment Category | Specific Assay/Technique | Primary Readout / Measurement | Key Experimental Considerations |
|---|---|---|---|
| Mineralization | Fourier Transform Infrared (FTIR) Spectroscopy | Phosphate/Amide I ratio; Collagen maturity ratio; Carbonate content [66] | Requires dehydrated samples; multiple spectra should be collected from different regions per sample [66]. |
| Osteodensitometry (DXA) | Bone Mineral Density (BMD) [66] | Useful for overall density; lower spatial resolution compared to spectroscopic methods [66]. | |
| Alizarin Red S Staining | Visualization and semi-quantification of calcium deposits | Requires careful dye extraction and normalization for quantification. | |
| Matrix Deposition | FTIR Spectroscopy | Collagen/Amide I peak ratio; Collagen maturity (1660/1690 ratio) [66] | Provides information on relative collagen content and cross-linking [66]. |
| Immunohistochemistry (IHC) / Immunofluorescence (IF) | Spatial localization of matrix proteins (e.g., Collagen I, BSP, OPN) [67] | Antibody specificity and antigen retrieval are critical for validity. | |
| Histology (e.g., Trichrome, Sirius Red) | Visualization of overall collagen architecture and distribution | Qualitative to semi-quantitative; provides topological context. | |
| Gene Expression | RNA Sequencing & Gene Set Enrichment Analysis (GSEA) | Genome-wide expression profiles; enrichment of functional gene sets (e.g., protein synthesis, matrix formation) [66] | Powerful for unbiased discovery; requires robust bioinformatics analysis [66]. |
| Quantitative PCR (qPCR) | Targeted quantification of osteogenic marker genes (e.g., BSP, OCN, OPN, COL1A1) [67] | Requires high-quality RNA and careful normalization to reference genes. | |
| In Situ Hybridization | Spatial localization of specific mRNA transcripts within the organoid [67] | Links gene expression directly to tissue morphology and mineralization fronts [67]. |
Detailed Experimental Protocols
Protocol: FTIR Spectroscopy for Mineralized Matrix Assessment
This protocol is adapted from studies on native bone surfaces and is directly applicable to mineralized organoids [66].
- Sample Preparation: Fix organoids in 4% paraformaldehyde for 24 hours. Dehydrate through a graded ethanol series (e.g., 70%, 95%, 100%) and allow to air-dry completely.
- Data Acquisition:
- Place the dried organoid in close contact with the diamond crystal of an FTIR spectrometer equipped with an Attenuated Total Reflection (ATR) accessory.
- Collect spectra with 4 cmâ»Â¹ resolution and 32 co-added scans to improve the signal-to-noise ratio.
- Perform an ATR correction on all collected spectra using instrument software.
- Data Analysis:
- Use appropriate software to obtain second-derivative spectra to resolve overlapping peaks.
- Integrate the area under the peaks for:
- Phosphate (900–1185 cmâ»Â¹) for mineral content.
- Amide I (1585–1720 cmâ»Â¹) for total protein.
- Collagen (1325–1355 cmâ»Â¹) for collagen content.
- Carbonate (855–890 cmâ»Â¹) for mineral substitution.
- Calculate the Phosphate/Amide I ratio as a key indicator of relative mineralization and the 1660/1690 ratio within the Amide I peak to assess collagen maturity [66].
Protocol: Genome-Wide Gene Expression Analysis via RNA-Seq & GSEA
This approach can identify how mechanical cues or matrix mineralization broadly regulate osteoblast biology [66].
- RNA Extraction and Sequencing:
- Mechanically dissociate organoids and homogenize cells in Trizol reagent. Isolate total RNA following the manufacturer's protocol.
- Assess RNA integrity (RIN > 8.0 is recommended). Prepare sequencing libraries from high-quality RNA (e.g., 1 µg) using a standardized kit (e.g., Illumina).
- Sequence libraries on an appropriate platform to generate a minimum of 30 million paired-end reads per sample.
- Bioinformatic Analysis:
- Align raw sequencing reads to a reference genome (e.g., GRCh38) using a splice-aware aligner (e.g., STAR).
- Quantify transcript abundances and generate a count matrix for all genes.
- Perform Gene Set Enrichment Analysis (GSEA) using established molecular signatures databases (e.g., Hallmark, GO). This method identifies coordinated changes in predefined gene sets (e.g., "ECM-associated genes" or "ribosomal protein synthesis") rather than focusing on individual genes [66]. An FDR q-value < 0.25 is generally considered significant.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs critical reagents and materials required for the construction and functional assessment of bone organoids, as derived from the cited methodologies.
Table 2: Research Reagent Solutions for Bone Organoid Studies
| Reagent/Material | Function/Application | Specific Examples & Notes |
|---|---|---|
| Cell Sources | Foundation of organoid self-organization and differentiation. | Human osteosarcoma cell lines (MG63, Saos-2, Hos); Primary Human Osteoblasts (HOB); Induced Pluripotent Stem Cells (iPSCs) [66] [4] [5]. |
| 3D Scaffolds | Provides a biomimetic extracellular matrix for 3D growth. | Matrigel; Collagen-based hydrogels; synthetic polymers; decellularized bone matrix [4] [5]. |
| Osteogenic Inducers | Directs stem/progenitor cells toward the osteoblastic lineage. | Dexamethasone; β-Glycerophosphate (mineralization precursor); L-Ascorbic Acid (collagen synthesis) [5]. |
| Key Antibodies | Detection and spatial analysis of matrix proteins via IHC/IF. | Anti-Collagen I, Anti-Bone Sialoprotein (BSP), Anti-Osteopontin (OPN), Anti-Osteocalcin (OC) [67]. |
| Gene Expression Assays | Quantification of osteogenic differentiation markers. | qPCR primers/probes for BSP, OPN, OC, COL1A1, RUNX2 [67]; RNA-Seq library prep kits [66]. |
| Mineralization Assay Kits | Histochemical and quantitative assessment of calcium deposits. | Alizarin Red S staining kits; OsteoImage mineralization assay. |
| Decellularized Bone Surfaces | Physiologically relevant substrate for studying cell-matrix interactions. | Prepared from fresh porcine or bovine bone; demineralized with 0.5 M EDTA (pH 7) [66]. |
Integrating Mechanical Cues: An Experimental Workflow
The following diagram outlines a consolidated experimental workflow for investigating the role of mechanical cues in bone organoid maturation, incorporating the functional readouts described in this guide.
This integrated approach, leveraging the detailed protocols and reagents outlined, empowers researchers to systematically deconstruct the complex interplay between mechanical forces and biological function, thereby accelerating the development of more physiologically relevant and clinically predictive bone organoid models.
The study of bone biology and the development of new therapeutics for skeletal disorders have long relied on traditional two-dimensional (2D) cell cultures and animal models. However, these conventional approaches present significant limitations in accurately recapitulating human-specific bone physiology and pathology. Bone organoids, defined as three-dimensional (3D) in vitro miniature organ models that mimic the micro-anatomy and function of native bone tissue, have emerged as a transformative technology bridging the gap between simplistic 2D cultures and complex in vivo systems [68] [5]. These self-organizing structures, derived from pluripotent stem cells or tissue-specific progenitor cells, offer unprecedented opportunities for investigating bone development, disease modeling, drug screening, and regenerative medicine strategies [4] [69].
The significance of bone organoids is particularly evident when framed within research on the role of mechanical cues in bone differentiation and maturation. Native bone tissue exists in a dynamic mechanical environment where forces profoundly influence cellular behavior, tissue development, and homeostasis [4]. This review provides a comprehensive technical analysis of bone organoids in direct comparison to traditional 2D cultures and animal models, with special emphasis on their capacity to incorporate biomechanical signaling—a critical dimension often lost in conventional systems.
Technical Foundations: Model System Architectures
Bone Organoids: Construction and Key Characteristics
Bone organoids are 3D biomimetic constructs formed through the self-organization of stem cells under defined in vitro culture conditions, capable of recapitulating the intricate 3D architecture and multicellular composition of native bone tissue [4]. These structures typically contain key cellular components of bone, including osteoblasts, osteoclasts, and bone progenitor cells, and have demonstrated the ability to mimic bone mineralization processes and mechanical responses [4]. The construction of bone organoids involves several critical components:
- Cell Sources: Pluripotent stem cells (embryonic or induced), mesenchymal stem cells (MSCs), or tissue-specific progenitor cells [4] [5]
- Scaffold Materials: Natural (e.g., Matrigel, collagen-based hydrogels) or synthetic biomaterials that provide structural support and biochemical cues [4]
- Signaling Molecules: Growth factors (e.g., BMPs, TGF-β), morphogens, and small molecules that direct osteogenic differentiation [7] [5]
- Biophysical Cues: Mechanical stimulation, fluid flow, and topographical guidance [4]
The development timeline of bone organoid technology has progressed rapidly, building upon the foundational organoid work initiated in 2009 when Hans Clevers' team first cultured intestinal stem cells into 3D structures with crypt-villus organization [4] [5]. Since this breakthrough, organoid technology has expanded to encompass various tissue types, with bone and cartilage organoid research advancing particularly in recent years [5].
Traditional 2D Cell Culture Systems
Traditional 2D cell culture involves growing cells as a monolayer on flat, rigid surfaces such as plastic or glass. This approach has been the mainstay of in vitro research due to its simplicity, low cost, and highly controlled conditions [70]. However, 2D systems lack critical microenvironmental cues found in vivo, including oxygen and nutrient gradients, 3D cell-to-cell interactions, and proper extracellular matrix (ECM) composition, which severely limits their ability to replicate tissue complexity [70]. In bone biology specifically, 2D cultures fail to recapitulate the spatial organization and mechanical microenvironment essential for osteogenic differentiation and bone matrix formation.
Animal Models in Bone Research
Animal models, particularly mice, have long been the cornerstone of preclinical bone research due to their physiological similarities to humans and manipulability [71]. These models provide a complex systemic environment encompassing immune responses, hormonal regulation, and vascularization that cannot be replicated in vitro. However, significant cross-species differences in gene expression, developmental timing, immune function, and bone remodeling processes limit their predictive value for human physiology and therapeutic responses [68] [71]. The high attrition rate of drugs that successfully pass animal testing but fail in human clinical trials underscores this limitation [71].
Table 1: Fundamental Characteristics of Bone Research Models
| Characteristic | Bone Organoids | Traditional 2D Cultures | Animal Models |
|---|---|---|---|
| Dimensionality | 3D structure | 2D monolayer | 3D in vivo environment |
| Cellular Complexity | Multiple cell types (osteoblasts, osteoclasts, progenitors) | Typically single cell type | All native cell types + systemic factors |
| Microenvironment | Tunable ECM, biophysical cues | Rigid, flat surface lacking ECM complexity | Native ECM with physiological biomechanics |
| Mechanical Cue Integration | Possible with specialized systems (bioreactors) | Limited | Native mechanical environment |
| Human Specificity | High (human-derived cells) | High (human-derived cells) | Low (interspecies differences) |
| Throughput | Medium | High | Low |
| Cost | Medium | Low | High |
| Timeline | Weeks to months | Days to weeks | Months to years |
Comparative Efficacy Across Research Applications
Physiological Relevance and Biomimicry
The physiological relevance of bone organoids represents their most significant advantage over 2D cultures. While 2D cultures lack spatial organization and proper cell-ECM interactions, bone organoids recapitulate key aspects of native bone architecture, including mineralized matrix deposition, osteocyte network formation, and multicellular communication [4] [5]. This enhanced biomimicry extends to gene expression profiles, with studies demonstrating that 3D organoid cultures more closely mirror in vivo expression patterns compared to 2D systems [70].
However, current bone organoid models still exhibit significant limitations in fully replicating the complexity of native bone tissue. A primary challenge is the lack of vascularization, which restricts nutrient exchange and organoid size, ultimately limiting long-term viability and maturation [4] [5]. Additionally, while animal models provide complete physiological context, cross-species differences often render them poor predictors of human biology. For instance, fundamental disparities in immune system function, bone remodeling rates, and developmental timing between mice and humans complicate the translation of findings [68] [71].
Disease Modeling Capabilities
Bone organoids show particular promise in disease modeling, as they can be generated from patient-specific cells to recapitulate genetic disorders, cancerous conditions, and metabolic bone diseases. Patient-derived tumor organoids preserve the molecular and histological characteristics of the original bone tumors, enabling highly personalized disease modeling and drug testing [72]. For example, osteosarcoma organoids have been successfully established from patient biopsy tissues with success rates exceeding 90%, maintaining stable phenotypes for several months [72].
In contrast, 2D cultures of bone-related diseases fail to capture the 3D tissue architecture and cellular heterogeneity characteristic of in vivo conditions, particularly for tumors [72]. While animal models can simulate systemic disease processes, species-specific differences in disease pathogenesis often limit their clinical relevance. Brain organoid studies of Zika virus infection exemplify this limitation; whereas mouse models failed to replicate Zika-induced microcephaly unless the virus was injected directly into fetal brain tissue, human brain organoids naturally recapitulated the condition due to human-specific cellular responses [71].
Drug Development and Toxicity Testing
In drug discovery and development, bone organoids offer a balanced platform that combines human specificity with reasonable throughput. Their enhanced physiological relevance leads to better predictions of drug efficacy and toxicity compared to 2D models, reducing false positives and negatives in compound screening [70]. For instance, 3D organoid models have demonstrated higher sensitivity and specificity in toxicology assessments across various tissue types compared to traditional 2D approaches [70].
The transition from 2D to 3D systems for high-throughput screening introduces technical challenges, including consistent organoid production and assay compatibility. Traditional 2D assays often don't translate well to 3D systems, necessitating the development of new analytical methods [70]. Animal models, while providing whole-body pharmacokinetic and pharmacodynamic data, suffer from interspecies metabolic differences that frequently yield misleading results about human drug responses. This is evidenced by the staggering statistic that over 90% of drugs that appear effective in animal trials fail during human clinical testing [71].
Table 2: Performance Comparison Across Research Applications
| Application | Bone Organoids | Traditional 2D Cultures | Animal Models |
|---|---|---|---|
| Disease Modeling | High (patient-specific, 3D pathology) | Low (lacks tissue context) | Medium (systemic but species-specific) |
| Drug Efficacy Screening | Medium-high (physiologically relevant) | Low-medium (high false positive rate) | Medium (species-specific responses) |
| Toxicity Testing | Medium-high (human-specific toxicity) | Low (insufficient predictive value) | Medium (species-specific metabolism) |
| Personalized Medicine | High (patient-derived models) | Medium (patient cells but in non-physiological context) | Not applicable |
| Mechanistic Studies | Medium-high (3D signaling analysis) | Low (simplified signaling) | High (systemic integration) |
| High-Throughput Capability | Medium (improving with automation) | High (easily scalable) | Low (time and cost intensive) |
The Critical Role of Mechanical Cues in Bone Organoid Maturation
Mechanical Signaling in Native Bone Physiology
Mechanical forces play a fundamental role in bone development, homeostasis, and repair through mechanotransduction pathways that regulate cellular behaviors such as proliferation, differentiation, and matrix mineralization [4]. Native bone tissue exhibits a hierarchical structure ranging from nanoscale collagen fibrils to trabecular and cortical architectures, which confers exceptional mechanical strength and load-bearing capacity [4]. This complex organization is dynamically regulated by mechanical cues, with osteocytes functioning as principal mechanosensors that coordinate adaptive responses to loading and unloading conditions.
Recapitulating Mechanical Environments in Bone Organoids
A significant challenge in bone organoid engineering involves replicating the biomechanical environment of native bone tissue. Most conventional organoid cultures are maintained in static suspension or hydrogels, lacking the mechanical stimulation essential for proper osteogenic differentiation [4]. Emerging approaches to address this limitation include:
- Bioreactor Systems: Applying cyclic stress or vibrational forces to mimic the mechanical environment of native bone [4]
- 3D Bioprinting: Creating spatially patterned constructs with controlled mechanical properties [4] [7]
- Specialized Scaffolds: Developing biomaterials with appropriate mechanical stiffness and degradation profiles [4]
- Dynamic Culture Conditions: Incorporating fluid flow and mechanical compression systems [4]
Recent advances in these technologies have enabled progressive improvements in bone organoid maturation and functionality. For instance, a 2025 study demonstrated an engineered "ossification center-like organoid" (OCO) that incorporated mechanical conditioning to enhance its regenerative potential [7].
Limitations of Traditional Models in Mechanical Studies
Both 2D cultures and animal models present significant limitations for studying mechanical influences on bone biology. Traditional 2D systems are characterized by unnatural stiffness (typically ~1 GPa for tissue culture plastic) that differs markedly from native bone ECM (~10-20 kPa for osteoid), profoundly altering cell behavior and mechanosensing [70]. While animal models experience physiological loading, their bone structure, remodeling rates, and gait-induced mechanical forces often differ substantially from humans, complicating the translation of mechanobiological findings [71].
Diagram 1: Mechanical Cue Integration in Bone Organoid Maturation. This workflow illustrates how external mechanical stimuli are applied to bone organoids and translated through cellular mechanotransduction pathways into functional tissue outcomes.
Technical Protocols and Methodological Considerations
Bone Organoid Construction Protocol
The construction of bone organoids involves a multi-step process requiring careful optimization at each stage:
Cell Source Selection and Expansion:
3D Scaffold Seeding and Differentiation:
- Embed cells in appropriate scaffold material (e.g., Matrigel, collagen hydrogel, synthetic polymers)
- Optimal cell density: 1-5 × 10^6 cells/mL for most protocols [4]
- Initiate osteogenic differentiation using specialized media formulations:
- Supplement with specific growth factors (BMP-2, VEGF, FGF) as required
Mechanical Conditioning (Critical for Maturation):
- Transfer constructs to biomechanical stimulation systems after 7-14 days
- Apply cyclic mechanical strain (0.5-2 Hz, 1-10% elongation) for bone-like organoids
- Alternatively, use hydrostatic pressure or fluid shear stress systems
- Culture under mechanical stimulation for 14-28 days with medium changes every 2-3 days [4] [7]
Maturation and Analysis:
Advanced Engineering Approaches
Recent methodological advances have significantly enhanced bone organoid construction:
- 3D Bioprinting: Enables precise spatial patterning of multiple cell types and creation of complex architectural features. Digital light-processing (DLP) printing technology has been used to create callus-like organoids that recapitulate diverse cell compositions and behaviors of developing bone [7].
- Microfluidic and Organ-on-a-Chip Platforms: Incorporate dynamic fluid flow and mechanical stimulation while allowing real-time monitoring of organoid responses [70].
- Assembloid Technology: Enables the assembly of multicellular systems to better replicate bone tissue microenvironments by combining different organoid types [4].
- Gene Editing: CRISPR-Cas9 and other gene editing techniques allow precise manipulation of genetic programs for disease modeling and functional modifications [4].
Table 3: Essential Research Reagents for Bone Organoid Construction
| Reagent Category | Specific Examples | Function | Technical Considerations |
|---|---|---|---|
| Stem Cell Sources | iPSCs, MSCs, skeletal stem cells | Foundation for organoid formation | Patient-derived for personalized models; check differentiation potential |
| Scaffold Materials | Matrigel, collagen hydrogels, synthetic PEG-based hydrogels | 3D structural support, mechanical cues | Batch variability in natural matrices; tunable stiffness in synthetic systems |
| Osteogenic Inducers | Dexamethasone, β-glycerophosphate, ascorbic acid | Promote osteoblastic differentiation | Concentration-dependent effects; temporal sequencing critical |
| Growth Factors | BMP-2, VEGF, FGF, TGF-β | Direct lineage specification, support vascularization | Short half-life requires sustained delivery systems; cost considerations |
| Mechanical Conditioning | Cyclic strain bioreactors, perfusion systems, acoustic stimulators | Apply physiologically relevant mechanical cues | Amplitude, frequency, and duration require optimization |
| Analysis Reagents | Alizarin Red, Osteocalcin antibodies, phalloidin | Assess mineralization, matrix production, cellular organization | 3D imaging requires specialized protocols and analysis software |
Current Challenges and Future Directions
Persistent Technical Limitations
Despite significant advances, bone organoid technology faces several substantial challenges that must be addressed to enhance its physiological relevance and practical utility:
- Vascularization: The absence of functional vascular networks remains a primary limitation, restricting organoid size and longevity due to inadequate nutrient and oxygen exchange [4] [5]. Current approaches to address this include the incorporation of endothelial cells and the use of microfluidic systems to provide fluid perfusion, but establishing fully functional vascular networks remains elusive [4].
- Standardization and Reproducibility: Significant batch-to-batch variability resulting from differences in cell sources, scaffold materials, and culture conditions hampers comparability across laboratories and reliable data interpretation [4] [70]. The absence of standardized protocols represents a major obstacle to clinical translation.
- Matrix Complexity: Native bone ECM possesses intricate biochemical and biophysical properties that are challenging to replicate with current scaffold materials [4]. Matrigel, the most commonly used substrate, suffers from batch variability, undefined composition, and suboptimal mechanical properties for bone tissue engineering [4].
- Innervation and Immune Components: Most current bone organoids lack integrated nervous and immune system elements, which play crucial roles in bone physiology, healing, and disease [71] [5]. Incorporating these components represents a critical next step in organoid complexity.
Emerging Technologies and Converging Approaches
Future advances in bone organoid technology will likely stem from interdisciplinary approaches integrating cutting-edge technologies:
- Artificial Intelligence and Machine Learning: AI-driven approaches are being employed to optimize organoid culture conditions, analyze complex imaging data, and predict differentiation outcomes [4] [70]. These technologies can identify subtle patterns in high-dimensional data that escape conventional analysis, potentially accelerating protocol optimization and standardization.
- Advanced Bioprinting Techniques: 3D bioprinting technologies are evolving to create increasingly complex spatial architectures with multiple cell types and graded mechanical properties [4] [6]. The integration of bioprinting with organoid technology enables the creation of more anatomically realistic bone constructs.
- Multi-Organoid Systems: The development of "assembloids" that combine different organoid types enables the study of systemic interactions, such as between bone and bone marrow or between bone and metastatic cancer cells [4] [72].
- Sensing and Monitoring Technologies: Incorporating biosensors within organoid cultures allows real-time monitoring of metabolic parameters, mechanical forces, and cellular responses, providing dynamic data on organoid development and function [70].
Diagram 2: Challenges and Future Directions in Bone Organoid Technology. This diagram maps the primary current limitations of bone organoids to emerging technological solutions aimed at enhancing physiological relevance.
Bone organoids represent a transformative technology that effectively bridges the critical gap between traditional 2D cell cultures and animal models in bone research. By offering human-specific, physiologically relevant systems that recapitulate key aspects of native bone architecture and function, organoids enable investigations of bone development, disease mechanisms, and therapeutic responses with enhanced predictive validity. Their capacity to incorporate biomechanical signaling—a fundamental regulator of bone biology—positions organoids as particularly valuable tools for advancing our understanding of mechanotransduction in skeletal tissues.
While challenges remain in achieving full vascularization, standardization, and complete replication of bone's complex microenvironment, rapid technological advances in bioprinting, AI-driven optimization, and assembloid integration are progressively addressing these limitations. As these innovations converge, bone organoids are poised to accelerate drug discovery, enable personalized medicine approaches for skeletal disorders, and potentially reduce reliance on animal models in accordance with the principles of the 3Rs (Replacement, Reduction, and Refinement).
For researchers focusing on the role of mechanical cues in bone organoid differentiation and maturation, current evidence strongly supports the integration of biomechanical conditioning protocols to enhance organoid maturation and functional competence. Future work should prioritize the development of standardized mechanical stimulation platforms, correlation of in vitro loading regimes with in vivo mechanical environments, and investigation of how mechanical signals interact with biochemical cues to direct bone organoid development. Through continued refinement and validation, bone organoids hold exceptional promise for revolutionizing both fundamental bone biology research and clinical translation in orthopedics.
Bone is a dynamic living tissue that relies on mechanical cues for development, homeostasis, and repair. The process of bone remodeling—the coordinated activity of bone cells that remove and deposit new bone tissue—is delicately balanced through biochemical and biomechanical signaling [73]. Within the bone microenvironment, mechanical forces regulate cellular behaviors including proliferation, differentiation, and matrix mineralization through mechanotransduction pathways. When these mechanical signals operate within a homeostatic range, bone removal and formation activities remain balanced. However, perturbations outside this range can cause significant imbalances leading to pathological bone loss conditions such as osteoporosis and osteoarthritis [73]. Traditional two-dimensional (2D) cell culture systems fail to replicate these critical mechanical interactions, limiting their utility for studying bone disease mechanisms and therapeutic interventions.
Bone organoids, as three-dimensional (3D) biomimetic constructs, have emerged as a promising platform for studying bone development and disease modeling while incorporating essential mechanical inputs [4]. These miniature, self-organized 3D tissue cultures partially mirror the architecture and functionality of native bone, offering a more physiologically relevant system for investigating complex disease pathologies [5]. By integrating mechanical stimulation protocols into bone organoid culture systems, researchers can now create more accurate models of pathological bone conditions that better recapitulate the dynamic mechanical environment of native bone tissue. This technical guide explores current methodologies, quantitative parameters, and experimental protocols for recapitulating pathological bone conditions with mechanical inputs using advanced bone organoid technology.
Fundamental Principles of Bone Mechanobiology
Mechanotransduction in Bone Tissue
Mechanotransduction—the process by which mechanical stimuli are converted into biochemical signals—plays a fundamental role in bone biology. In native bone tissue, mechanical loading generates fluid shear stress and strain within the bone matrix, which are detected by various bone cells including osteocytes, osteoblasts, and osteoclasts [73]. Osteocytes, which comprise over 90% of bone cells, form an extensive network throughout the mineralized matrix and serve as the primary mechanosensors. When mechanical loads are applied, osteocytes release signaling molecules such as sclerostin, RANKL, and nitric oxide that regulate the activities of osteoblasts and osteoclasts, thereby controlling bone remodeling processes [73].
The complex interplay between mechanical forces and biochemical signaling creates a feedback loop that maintains bone mass and architecture according to mechanical demands. Disruptions in this mechanobiological regulation contribute significantly to various bone pathologies. For instance, reduced mechanical loading during disuse or immobilization leads to rapid bone loss, while abnormal loading patterns can accelerate joint degeneration in osteoarthritis [5]. Recapitulating these mechanobiological processes in vitro requires carefully controlled application of mechanical stimuli alongside appropriate biochemical cues within 3D organoid cultures.
Mechanical Signaling in Bone Pathologies
Different bone pathologies exhibit distinct mechanobiological dysregulations. In osteoporosis, reduced mechanical loading or impaired mechanosensing leads to an imbalance where bone resorption outpaces formation [4]. The Wnt/β-catenin signaling pathway, which is mechanically regulated, plays a crucial role in this process, with mechanical strain promoting bone formation through inhibition of sclerostin [73]. In osteoarthritis, abnormal mechanical loading of joints triggers catabolic responses in chondrocytes and subchondral bone cells, leading to progressive cartilage degradation and bone remodeling [5]. Understanding these pathology-specific mechanobiological disruptions is essential for designing relevant disease models using bone organoids.
Current Methodologies for Applying Mechanical Inputs in Bone Organoids
Biomechanical Culture Systems
Various bioreactor systems have been developed to apply controlled mechanical stimuli to bone organoids, each offering distinct advantages for specific research applications:
Table 1: Biomechanical Culture Systems for Bone Organoids
| System Type | Mechanical Input | Application in Disease Modeling | Key Advantages | Technical Limitations |
|---|---|---|---|---|
| Compression Bioreactors | Cyclic compressive strain | Osteoarthritis, fracture healing | Mimics joint loading; High-throughput capability | Potential scaffold deformation; Limited strain uniformity |
| Perfusion Systems | Fluid shear stress | Bone metastasis, osteoporosis | Enhanced nutrient/waste exchange; Promotes vascularization | Requires specialized chambers; Optimization challenging |
| Acoustic Stimulation | Low-intensity vibrations | Osteoporosis, age-related bone loss | Non-invasive; Uniform energy distribution | Difficult to quantify local forces; Equipment specificity |
| Magnetic Stimulation | Magnetic forces via functionalized nanoparticles | Bone repair, genetic disorders | Remote activation; Spatiotemporal control | Complex nanoparticle functionalization; Potential cytotoxicity |
These systems enable researchers to replicate specific mechanical environments associated with various bone pathologies. For instance, compression bioreactors can simulate the abnormal joint loading patterns found in osteoarthritis, while perfusion systems can model the altered interstitial fluid flow occurring in disuse osteoporosis [4] [5].
Scaffold-Based Mechanical Cues
The scaffold material itself provides mechanical cues that significantly influence cell behavior and disease progression in bone organoids. Different scaffold strategies offer varying mechanical properties:
Table 2: Scaffold Strategies for Mechanical Regulation in Bone Organoids
| Scaffold Material | Elastic Modulus | Degradation Profile | Ideal Disease Application | Notable Characteristics |
|---|---|---|---|---|
| Matrigel | 0.1-0.5 kPa | Enzyme-mediated (variable) | Cancer metastasis, early development | Basement membrane composition; Limited mechanical strength |
| Collagen-Based Hydrogels | 0.2-5 kPa | Enzymatic (weeks-months) | Osteoporosis, healing defects | Natural bone ECM component; Tunable crosslinking |
| Synthetic Polymers (PEG, PLA) | 1-2000 kPa | Hydrolytic (controlled) | Mechanopathology studies | Highly tunable mechanics; Batch consistency |
| Hybrid/Composite | 10-3000 kPa | Multi-phase degradation | Complex disease modeling | Graded mechanical properties; Enhanced biofunctionality |
The choice of scaffold material critically impacts the organoid's mechanical microenvironment. While Matrigel remains common for general organoid culture, its limited mechanical strength and batch-to-batch variability make it suboptimal for mechanobiological studies [4]. Alternative scaffolds such as collagen-based hydrogels and synthetic polymers provide more controlled mechanical environments that better replicate the stiffness of native bone tissue (ranging from ~100 MPa for cortical bone to ~1-50 MPa for trabecular bone) [5]. Recent advances in 3D bioprinting enable precise spatial patterning of multiple materials with graded mechanical properties, allowing creation of organoids with region-specific mechanics that more accurately mimic pathological conditions like osteochondral defects [4].
Quantitative Analysis of Mechanical Parameters in Bone Organoid Models
Establishing standardized quantitative parameters is essential for creating reproducible and clinically relevant bone organoid disease models. The following table summarizes key mechanical parameters derived from current literature:
Table 3: Quantitative Mechanical Parameters for Bone Disease Modeling
| Pathological Condition | Optimal Mechanical Stimulus | Frequency/Duration | Measured Outcomes | Validation Markers |
|---|---|---|---|---|
| Disuse Osteoporosis | 0.5-2% strain cyclic compression | 0.5-1 Hz, 1-2 hours/day | Increased osteoclast activity; Reduced mineralization | TRAP↑, CTSK↑, RANKL/OPG ratio↑ |
| Osteoarthritis (subchondral) | 5-20% strain high-magnitude compression | 0.1-1 Hz, 1-4 hours/day | Altered remodeling; Sclerotic changes | SOST↑, MMP13↑, ALP↓ |
| Mechanically-accelerated Healing | 1-5% strain dynamic compression | 1 Hz, 30-60 min/day | Enhanced osteogenic differentiation; Accelerated mineralization | RUNX2↑, OCN↑, COL1A1↑ |
| Age-related Bone Loss | Low-intensity vibrations (0.3-1g) | 30-90 Hz, 10-30 min/day | Improved osteoblast survival; Reduced adipogenesis | OPN↑, PPARγ↓, BSP↑ |
These quantitative parameters provide a foundation for standardizing mechanical stimulation protocols across different research settings. The measured outcomes and validation markers enable researchers to verify that their mechanical input protocols successfully recapitulate key features of target pathologies.
Experimental Protocols for Bone Organoid Disease Modeling
Protocol: Establishing Osteoporotic Bone Organoids with Reduced Mechanical Stimulation
This protocol details the creation of bone organoids modeling disuse osteoporosis through controlled reduction of mechanical stimulation:
Step 1: Organoid Initiation
- Isolate human mesenchymal stem cells (hMSCs) from bone marrow aspirates (passage 3-5 recommended)
- Prepare hydrogel suspension: Mix 5×10^6 cells/mL with 1:1 ratio of collagen type I (3 mg/mL) and Matrigel
- Plate 50 μL droplets in 24-well culture plates and polymerize at 37°C for 30 minutes
- Add osteogenic medium: α-MEM supplemented with 10% FBS, 10 mM β-glycerophosphate, 50 μg/mL ascorbic acid, and 10 nM dexamethasone [4] [5]
Step 2: Pre-culture Mineralization
- Culture for 14 days without mechanical stimulation, changing medium every 2-3 days
- Verify early mineralization via Alizarin Red staining at day 14 (≥30% mineralization area recommended before proceeding)
Step 3: Application of Disuse Conditions
- Transfer organoids to biomechanical bioreactor system
- Apply minimal mechanical stimulation protocol: 0.5% cyclic strain at 0.1 Hz for 15 minutes daily
- Maintain control group with physiological stimulation: 2% cyclic strain at 1 Hz for 1 hour daily
- Culture for additional 14-21 days with continued osteogenic medium [4]
Step 4: Analysis and Validation
- Quantify osteoclast activity: TRAP staining and cathepsin K immunohistochemistry
- Assess resorption pits: SEM analysis of devitalized bovine bone slices
- Evaluate gene expression: qPCR for RANKL, OPG, TRAP, and CTSK
- Measure mineralization: Micro-CT analysis and quantitative Alizarin Red extraction
This protocol reliably generates organoids with key features of disuse osteoporosis, including elevated osteoclast activity, reduced mineralization, and altered RANKL/OPG ratio, providing a valuable model for screening anti-osteoporotic therapeutics [4] [5].
Protocol: Osteoarthritic Subchondral Bone Organoid Model
This protocol creates bone organoids modeling the subchondral bone changes characteristic of osteoarthritis through application of pathological mechanical loading:
Step 1: Organoid Construction with Chondrogenic Integration
- Prepare co-culture system: 3:1 ratio of hMSCs to human articular chondrocytes
- Encapsulate in stratified hydrogel: Bottom layer (bone compartment) - collagen I/hydroxyapatite nanocomposite; Top layer (cartilage compartment) - agarose/collagen II blend
- Culture in chondro-osteogenic medium: DMEM-F12 with 10% FBS, 1% ITS+ premix, 50 μg/mL ascorbic acid, 10 mM β-glycerophosphate, and 10 ng/mL TGF-β3 for 7 days [5]
Step 2: Pathological Mechanical Loading
- Transfer to compression bioreactor system
- Apply high-magnitude, low-frequency compression: 15% strain at 0.5 Hz for 2 hours daily, 5 days/week
- Maintain control group with physiological loading: 3% strain at 1 Hz for 1 hour daily
- Continue culture for 21-28 days with medium changes every 2-3 days
Step 3: Phenotypic Analysis
- Assess hypertrophic differentiation: ALP activity, type X collagen immunohistochemistry
- Evaluate catabolic response: MMP-13 and ADAMTS-5 gene expression
- Analyze tissue structure: Histology (Safranin O/Fast Green) and micro-CT for bone volume fraction
- Measure sclerostin expression: Western blot and immunohistochemistry [5]
This model recapitulates key features of osteoarthritic subchondral bone, including increased bone volume, sclerotic changes, elevated sclerostin expression, and abnormal remodeling activity, providing a platform for studying OA pathogenesis and therapeutic interventions.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful construction of mechanically-stimulated bone organoids requires specific reagents and materials optimized for 3D culture and mechanobiological studies:
Table 4: Essential Research Reagents for Bone Organoid Mechanobiology
| Reagent Category | Specific Products | Function in Organoid Culture | Recommended Concentrations | Quality Considerations |
|---|---|---|---|---|
| Stem Cell Sources | Human MSCs (bone marrow), iPSCs | Organoid initiation and differentiation | 5-10×10^6 cells/mL for encapsulation | Check differentiation potential (≥70% CD105+, CD73+, CD90+) |
| Matrix Materials | Collagen Type I, Fibrin, Hyaluronic Acid | 3D structural support and mechanical signaling | 3-6 mg/mL collagen; 5-10 mg/mL fibrin | Lot-to-lot consistency testing; Endotoxin screening |
| Osteogenic Inducers | β-glycerophosphate, Ascorbic Acid, Dexamethasone | Promote osteoblastic differentiation | 10 mM, 50 μg/mL, 10-100 nM respectively | Pharmaceutical grade; Filter sterilization |
| Mechanosensing Modulators | Cytochalasin D, Y27632, TRPV4 agonists/antagonists | Investigate specific mechanotransduction pathways | 0.1-10 μM depending on agent | Dose-response validation required |
| Analysis Reagents Alizarin Red, TRAP stain, Antibodies for osteogenic markers | Quantification of differentiation and mineralization | Follow manufacturer protocols; validate specifically for 3D culture | Batch testing against known standards |
Selection of appropriate reagents is critical for generating reproducible and reliable results. Researchers should prioritize reagents specifically validated for 3D culture systems, as traditional 2D culture reagents may not perform optimally in organoid models. Additionally, strict quality control measures should be implemented for matrix materials, as batch-to-batch variability can significantly impact mechanical properties and experimental outcomes [4].
Signaling Pathways in Bone Mechanotransduction
The following diagram illustrates key signaling pathways involved in mechanical stimulation of bone organoids:
Diagram 1: Bone mechanotransduction signaling pathways. This diagram illustrates the key molecular mechanisms through which mechanical stimuli are converted into biochemical signals that regulate bone formation and remodeling in organoid cultures.
Workflow for Constructing Disease-Specific Bone Organoids
The following diagram outlines the comprehensive workflow for constructing bone organoids with mechanical inputs for disease modeling:
Diagram 2: Workflow for constructing bone organoids with mechanical inputs. This diagram outlines the key steps in creating mechanically-stimulated bone organoids for disease modeling applications, from initial cell selection through final validation and therapeutic screening.
The integration of mechanical inputs into bone organoid systems represents a significant advancement in our ability to model complex bone pathologies in vitro. By recapitulating the essential mechanobiological environment of native bone tissue, these advanced organoid models provide more physiologically relevant platforms for studying disease mechanisms and screening potential therapeutics. Current methodologies enable researchers to apply controlled mechanical stimuli that mimic specific pathological conditions, from the reduced loading of disuse osteoporosis to the abnormal loading patterns of osteoarthritis.
Future developments in this field will likely focus on enhancing the complexity and physiological relevance of bone organoid models. The integration of vascular networks, immune cells, and neural elements will create more comprehensive models that better capture the multifaceted nature of bone pathologies [4]. Additionally, the convergence of bone organoid technology with advanced engineering approaches such as 3D bioprinting and artificial intelligence-driven optimization holds tremendous potential for creating standardized, reproducible, and high-throughput compatible models [4] [5]. As these technologies mature, mechanically-stimulated bone organoids are poised to become indispensable tools for both fundamental bone biology research and translational drug development, ultimately contributing to improved therapeutic strategies for patients suffering from debilitating bone diseases.
The repair of critical-sized bone defects remains a formidable challenge in orthopedic clinical practice, as these defects often lack sufficient self-regeneration capacity and can lead to non-union or poor healing without external intervention [74]. While autologous bone grafting represents the current gold standard treatment, it suffers from significant limitations including donor site morbidity, limited availability, and unpredictable postoperative resorption rates [74]. Bone tissue engineering (BTE), which integrates scaffolds, cells, and bioactive factors, has emerged as a promising alternative strategy [74]. Recently, the advent of bone organoid technology has provided a revolutionary approach for developing physiologically relevant bone substitutes that can bridge the gap between conventional two-dimensional cell cultures and complex in vivo environments [4] [74].
This technical guide focuses specifically on the role of mechanical cues in bone organoid differentiation and maturation, framing this discussion within the broader thesis that biomechanical conditioning is essential for developing functional bone organoids with enhanced regenerative capacity. Bone is a dynamic tissue that constantly remodels in response to mechanical forces, and replicating this mechanical microenvironment in vitro presents significant technical challenges [4]. Conventional organoid cultures maintained in static suspension or hydrogels lack these critical mechanical cues, which may lead to deviations in osteogenic differentiation from physiological conditions [4]. This whitepaper comprehensively explores advanced strategies for constructing mechanically preconditioned bone organoids, their in vivo validation, and the transformative potential they hold for orthopedic regenerative medicine.
Bone Organoid Construction Methodologies
The selection of appropriate cell sources is fundamental to successful bone organoid construction. Current approaches utilize diverse cell types, each with distinct advantages and limitations.
Table 1: Cell Sources for Bone Organoid Construction
| Cell Type | Key Characteristics | Advantages | Limitations |
|---|---|---|---|
| Urine-Derived Stem Cells (USCs) | Mesenchymal stem cell properties; isolated from urine [74] | Non-invasive acquisition; widely available; sustainable source; comparable osteogenic potential to BMSCs [74] | Relatively new cell source; requires further characterization |
| Bone Marrow Mesenchymal Stem Cells (BMSCs) | Traditional stem cell source for bone tissue engineering [74] | Well-characterized; proven osteogenic differentiation capacity | Invasive harvesting procedure; limited availability; donor site morbidity |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells with pluripotent capacity [4] | Unlimited expansion potential; patient-specific applications | Complex differentiation protocols; potential genomic instability |
Urine-derived stem cells (USCs) represent a particularly promising cell source due to their non-invasive acquisition process, widespread availability, and sustainable isolation from metabolic waste [74]. Recent studies have demonstrated that USCs possess comparable osteogenic potential to traditional bone marrow mesenchymal stem cells (BMSCs), making them highly suitable for bone organoid construction [74]. When supported by appropriate three-dimensional carriers, USCs can efficiently generate functional bone organoids (designated uBOs) within 14 days through osteogenic directional induction [74].
Scaffold Systems and Biomaterials
The three-dimensional scaffold provides critical structural support and biochemical cues that direct stem cell differentiation and tissue maturation. Selection of appropriate scaffold materials significantly impacts the fidelity and functionality of resulting bone organoids.
Decellularized Bone Matrix Microparticles (DBM-MPs) represent a highly biomimetic scaffold system that preserves the natural extracellular matrix composition and microstructure of native bone tissue [74]. Prepared through an independent decellularization system followed by freeze-milling and filtration, DBM-MPs exhibit excellent biocompatibility, superior osteoinductivity, and low immunogenicity [74]. These micron-sized particles facilitate efficient stem cell loading and can be delivered to defect sites through minimally invasive injection for complete filling of irregular bone defects.
Alternative scaffold materials include Matrigel, a basement membrane extract commonly used in organoid culture, though it suffers from batch-to-batch variability, murine protein contamination, and limited mechanical strength [4]. Synthetic hydrogels such as GelMA offer greater control over mechanical properties but often lack the complex biochemical signaling present in native bone matrix [4]. The choice between these scaffold systems involves trade-offs between biomimicry, manufacturability, and clinical translation potential.
Mechanical Preconditioning Strategies
Mechanical forces play a fundamental role in bone development by regulating cellular behaviors such as proliferation, differentiation, and matrix mineralization through mechanotransduction pathways [4]. Incorporating mechanical conditioning into bone organoid culture is therefore essential for developing physiologically relevant models.
Table 2: Mechanical Preconditioning Methods for Bone Organoids
| Method | Application | Physiological Relevance | Technical Implementation |
|---|---|---|---|
| Bioreactor Systems | Application of cyclic stress or vibrational forces [4] | Mimics natural loading patterns during locomotion | Specialized equipment required; parameter optimization needed |
| Perfusion Systems | Continuous medium flow through scaffold [4] | Recapitulates nutrient transport in vascularized bone | Can be integrated with microfluidic platforms |
| Static Compression | Constant mechanical pressure | Models constant load-bearing function | Technically simpler but less physiologically accurate |
| Substrate Stretching | Cyclic stretching of culture substrate | Simulates tendon/ligament pull on bone | Particularly relevant for interface tissue engineering |
Advanced bioreactor systems that apply cyclic mechanical stress or vibrational forces to developing bone organoids have demonstrated promising results in enhancing osteogenic lineage commitment and matrix mineralization [4]. Dynamic loading not only promotes osteogenic differentiation of mesenchymal stem cells but also enhances endothelial network formation, thereby supporting coordinated development of vascularized bone tissue [4]. These approaches remain at an early stage and require further refinement to fully replicate the complex mechanical environment of native bone.
Advanced Technologies in Bone Organoid Engineering
Interdisciplinary Technological Integration
The convergence of multiple advanced technologies is driving significant progress in bone organoid engineering, enabling researchers to overcome traditional limitations and enhance physiological relevance.
3D Bioprinting provides precise spatial control over cell placement and scaffold architecture, allowing creation of complex, hierarchical structures that better mimic native bone tissue [4]. This technology enhances structural complexity and enables incorporation of vascular channels within bone organoids, addressing the critical limitation of nutrient diffusion in larger constructs [4].
Artificial Intelligence (AI) and machine learning algorithms accelerate organoid optimization through data-driven analysis of complex multivariate culture parameters [4]. These approaches can identify non-intuitive relationships between mechanical conditioning regimes, biochemical factor combinations, and resulting organoid functionality, significantly reducing the experimental burden required to establish optimal protocols.
Assembloid Technology enables the integration of multiple cell types into coordinated 3D structures, recreating the multicellular complexity of native bone tissue microenvironments [4]. This approach facilitates the incorporation of osteoblasts, osteocytes, osteoclasts, and vascular endothelial cells within a single organoid, better replicating the dynamic remodeling processes essential for bone homeostasis.
Gene Editing tools, particularly CRISPR-Cas9 systems, allow precise manipulation of genetic programs governing bone differentiation and maturation [4]. These technologies enable creation of reporter lines for real-time monitoring of differentiation progress, as well as disease-specific models for studying pathological conditions and screening therapeutic interventions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Bone Organoid Construction
| Reagent/Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Stem Cell Sources | USCs, BMSCs, iPSCs [74] [4] | Self-renewing cells with osteogenic differentiation capacity | USC source offers non-invasive acquisition [74] |
| Scaffold Materials | DBM-MPs, Matrigel, collagen hydrogels, synthetic polymers [74] [4] | 3D structural support; biochemical cues; mechanical environment | DBM-MPs provide highly biomimetic microenvironment [74] |
| Osteogenic Inducers | Dexamethasone, β-glycerophosphate, ascorbic acid [74] | Direct stem cell differentiation toward osteogenic lineage | Standard cocktail components; concentration-dependent effects |
| Growth Factors | BMP-2, VEGF, FGF, TGF-β [4] | Enhance osteogenesis and vascularization | Short half-lives; controlled delivery systems advantageous |
| Mechanoculture Systems | Bioreactors, microfluidic devices, stretching apparatus [4] | Apply controlled mechanical stimuli | Parameter optimization required (frequency, magnitude, duration) |
In Vivo Validation of Preconditioned Bone Organoids
Experimental Models and Assessment Methods
Rigorous in vivo validation is essential to demonstrate the functional efficacy of preconditioned bone organoids in bone defect repair. Well-established animal models, particularly critical-sized femoral condyle defects in rats, provide standardized systems for evaluating regenerative capacity [74].
In recent groundbreaking work, uBOs (USCs@DBM-MPs derived bone organoids) were injected into rat femoral condyle defect models, achieving complete bone regeneration within 6 weeks [74]. These uBOs demonstrated exceptional capacity to fill defect areas completely and actively promote angiogenesis and osteogenesis through potent paracrine functions [74]. Comparative analysis revealed that uBOs exhibited biological activity, proliferation characteristics, and osteogenic potential comparable to BMSC-derived organoids (bBOs), while offering the significant advantage of non-invasive cell acquisition [74].
The successful regeneration of critical-sized bone defects requires not only osteogenic differentiation but also establishment of functional vascular networks to support nutrient and waste exchange. Preconditioned bone organoids address this requirement through dual mechanisms: direct differentiation into bone-forming cells and secretion of angiogenic factors that stimulate host blood vessel ingrowth [74]. This paracrine functionality represents a crucial advantage over acellular scaffold approaches, enabling more rapid and complete integration with host tissues.
Quantitative Outcomes and Functional Metrics
Table 4: In Vivo Performance Metrics of Preconditioned Bone Organoids
| Assessment Method | Experimental Group | Control Group | Significance/Outcome |
|---|---|---|---|
| Time to Complete Healing | 6 weeks [74] | >8 weeks (untreated defects) | Significant acceleration of repair process |
| Bone Volume Fraction | ~65% of native bone [74] | <25% (scaffold alone) | Enhanced bone matrix deposition |
| Angiogenic Marker Expression | VEGF, Ang-1 upregulated [74] | Baseline expression | Potent paracrine pro-angiogenic activity |
| Mechanical Properties | ~70% of native bone strength [74] | <30% (untreated defects) | Functional load-bearing capacity |
| Host Integration | Seamless integration with host tissue [74] | Fibrous tissue interface | Direct bone fusion without scar formation |
Technical Protocols and Methodologies
Comprehensive Protocol for USC-Derived Bone Organoid Construction
Step 1: Preparation of Decellularized Bone Matrix Microparticles (DBM-MPs)
- Harvest cancellous bone blocks from porcine vertebrae and process through an established decellularization system [74]
- Confirm complete cell removal through Hematoxylin-Eosin staining and DAPI/COL-1α fluorescence staining [74]
- Process decellularized bone matrix using freeze-milling and filtration to generate micron-sized particles (DBM-MPs) [74]
- Sterilize DBM-MPs through gamma irradiation or ethylene oxide treatment before cell seeding
Step 2: Isolation and Expansion of Urine-Derived Stem Cells (USCs)
- Collect fresh urine samples and isolate USCs through differential centrifugation [74]
- Culture USCs in expansion medium (α-MEM supplemented with 10% FBS, 1% penicillin-streptomycin)
- Passage cells at 80-90% confluence and characterize mesenchymal stem cell markers (CD73, CD90, CD105) via flow cytometry
- Use cells at passages 3-5 for organoid construction to maintain optimal differentiation potential
Step 3: Organoid Assembly and Osteogenic Induction
- Seed USCs onto DBM-MPs at a density of 5×10^5 cells/mg scaffold material [74]
- Culture in osteogenic induction medium (DMEM supplemented with 10% FBS, 10 mM β-glycerophosphate, 50 μg/mL ascorbic acid, and 100 nM dexamethasone) for 14 days [74]
- Apply mechanical conditioning using bioreactor systems (cyclic strain at 0.5-2% elongation, 1 Hz frequency) during the differentiation process [4]
- Refresh culture medium every 2-3 days throughout the differentiation period
Step 4: In Vivo Implantation and Assessment
- Create critical-sized femoral condyle defects (3mm diameter) in rat models [74]
- Implant preconditioned uBOs via minimally invasive injection to completely fill defect areas [74]
- Monitor bone regeneration over 6 weeks using micro-CT imaging at 2-week intervals [74]
- Perform histological analysis (H&E, Masson's Trichrome, Goldner's staining) to assess tissue maturation and integration [74]
Mechanical Preconditioning Parameters
The following protocol details optimal parameters for mechanical preconditioning of bone organoids:
Cyclic Strain Protocol:
- Apply uniaxial cyclic strain at 0.5-2% elongation
- Maintain frequency of 1 Hz (60 cycles per minute)
- Duration: 30-60 minutes per day, for 7-14 consecutive days
- Use flexible membrane culture plates compatible with mechanical stimulation systems
Perfusion Bioreactor Protocol:
- Establish continuous medium flow at 0.1-1 mL/min through scaffold
- Maintain physiological glucose levels (>3.5 mM) throughout culture
- Incorporate simulated microgravity or vibrational stimuli at 10-100 Hz frequencies
- Monitor oxygen concentration throughout culture period (maintain >80% saturation)
Combined Stimulation Regimen:
- Days 1-3: Static culture for initial cell attachment
- Days 4-7: Apply low-magnitude mechanical stimulation (0.5% strain, 0.5 mL/min flow)
- Days 8-14: Increase stimulation intensity (1-2% strain, 1 mL/min flow)
- Throughout culture: Apply intermittent vibrational stimuli (30 Hz, 15 min/day)
The integration of mechanical preconditioning strategies into bone organoid construction represents a paradigm shift in orthopedic tissue engineering. The successful in vivo validation of preconditioned organoids, particularly those derived from non-invasive cell sources like USCs, demonstrates their tremendous potential for clinical translation [74]. These advanced constructs not only serve as effective bone substitute units for defect filling but also actively promote regenerative processes through potent paracrine signaling mechanisms [74].
Future developments in bone organoid technology will likely focus on enhancing vascularization capabilities, establishing standardized evaluation frameworks, and addressing regulatory considerations for clinical application [4]. The continued convergence of interdisciplinary technologies—including 3D bioprinting for structural precision, artificial intelligence for culture optimization, and gene editing for functional enhancement—will further advance the physiological relevance and therapeutic efficacy of bone organoids [4]. As these technologies mature, mechanically preconditioned bone organoids hold significant promise for revolutionizing treatment outcomes for skeletal diseases and critical-sized bone defects, ultimately enabling personalized orthopedic approaches tailored to individual patient needs.
The inherent complexity and heterogeneity of human tumors and tissues pose substantial challenges for the development of effective oncology therapeutics and regenerative medicine strategies [75]. Organoids, three-dimensional (3D) in vitro miniature organ models, have emerged as a transformative tool in preclinical research, offering significant advantages in faithfully recapitulating key features of primary tissues, including molecular, phenotypic, and histopathological characteristics [4] [75]. These 3D models address the critical limitations of conventional two-dimensional (2D) cell cultures, which fail to capture the architectural and cellular complexity of in vivo biology, and animal models, which exhibit high heterogeneity and costs while not always accurately predicting human physiological responses [76]. Bone organoids, as biomimetic 3D constructs, have particularly gained prominence for studying bone development, disease modeling, drug screening, and regenerative medicine applications [4] [6].
The structural and functional similarities between organoids and native tissues make them highly effective preclinical tools for evaluating drug efficacy, toxicity, and safety profiles [75]. Patient-derived organoids (PDOs) maintain the architectural integrity, in vivo-like microenvironmental cues, and essential cellular heterogeneity of parental tissues, which is critical for modeling therapeutic responses [76] [75]. Increasing evidence highlights a strong correlation between therapeutic responses in PDOs and clinical outcomes, positioning them as valuable predictive platforms for personalized medicine and precision oncology [75]. Notably, organoid systems reduce the occurrence of false-positive drug hits and improve the accuracy of safety predictions during preclinical screenings compared to conventional 2D cultures [75].
Despite their substantial potential in drug screening and therapeutic development, traditional organoid models face significant limitations that impede their broader application in high-throughput preclinical settings. These challenges include variability in cell composition, lack of standardization, high costs, scalability issues, and inter-individual heterogeneity [75]. A key concern is the inadequate replication of the native tissue microenvironment in conventional organoid systems, particularly the absence of essential mechanical cues that profoundly influence bone cell differentiation, matrix deposition, and tissue maturation [4]. This review comprehensively explores the integration of advanced technologies with bone organoid culture systems to enhance drug screening accuracy, throughput, and physiological relevance, with particular emphasis on the role of mechanical cues in bone organoid maturation and its implications for high-throughput drug screening platforms.
The Critical Role of Mechanical Cues in Bone Organoid Maturation
Biomechanical Regulation of Bone Biology
Bone is a dynamic, mineralized connective tissue that exhibits continuous remodeling regulated by mechanical cues, which profoundly influence cell differentiation, matrix deposition, and tissue maturation [4]. This complex organization confers exceptional mechanical strength and load-bearing capacity, supporting locomotion, organ protection, and calcium-phosphate homeostasis. The biomechanical environment plays a critical role in bone development by regulating cellular behaviors such as proliferation, differentiation, and matrix mineralization through mechanotransduction pathways [4]. Native bone tissue possesses a hierarchical structure ranging from nanoscale collagen fibrils to trabecular and cortical architectures, with mechanical forces serving as essential regulators of skeletal homeostasis and adaptation [4] [6].
Unlike conventional organoids derived from tissues such as the intestine or liver, bone organoids are particularly challenging to cultivate due to the unique anatomical and physiological characteristics of bone tissue [4]. The mechanical milieu of native bone encompasses multiple biophysical cues, including substrate stiffness, cyclic strain, fluid shear stress, and compressive loads, which collectively direct mesenchymal stem cell (MSC) fate decisions toward osteogenic lineages. Dynamic loading promotes osteogenic lineage commitment of MSCs and enhances endothelial network formation, thereby supporting the coordinated development of vascularized bone tissue [4]. These critical biomechanical factors are largely absent in conventional organoid culture platforms, contributing to the difficulty in replicating bone-specific features in vitro and limiting their physiological relevance for drug screening applications.
Current Limitations in Mechanical Stimulation of Bone Organoids
Most conventional organoid cultures are maintained in static suspension or hydrogels, lacking essential mechanical cues, which may lead to deviations in osteogenic differentiation from physiological conditions [4]. Current bone organoid models still exhibit significant morphological and functional differences from human skeletal tissue, making it difficult to fully recapitulate the complexity of native bone [4]. The choice of culture media and scaffold materials significantly impacts the maturation and reproducibility of bone organoids, with most models relying on Matrigel as a 3D scaffold [4]. Nevertheless, Matrigel possesses limited mechanical strength and fails to provide a rigid microenvironment comparable to native bone, while alternative scaffolds such as collagen-based hydrogels often suffer from poor mechanical stability and uncontrolled degradation rates [4].
The absence of standardized protocols across different laboratories, including variations in cell sources such as embryonic stem cells, induced pluripotent stem cells, and adult stem cells, as well as in differentiation factor combinations and culture media formulations, has led to substantial batch-to-batch variability, limiting the comparability of results and posing challenges for clinical translation [4]. This variability is particularly problematic for high-throughput screening platforms that require standardized, reproducible model systems to generate reliable, comparable data across multiple screening campaigns and experimental conditions.
Table 1: Key Mechanical Properties of Native Bone Tissue and Current Organoid Model Limitations
| Mechanical Property | Native Bone Tissue | Current Bone Organoid Limitations |
|---|---|---|
| Compressive Strength | 130-220 MPa (cortical bone) | Limited mechanical strength in hydrogel-based systems |
| Elastic Modulus | 15-25 GPa (cortical bone) | Matrigel and collagen hydrogels exhibit significantly lower stiffness |
| Load-Bearing Capacity | High, adapts to mechanical demands | Static culture conditions lack mechanical stimulation |
| Fluid Shear Stress | Critical for osteocyte function | Limited nutrient diffusion in avascular organoids |
| Matrix Mineralization | Highly organized mineral deposition | Often disorganized mineralization in vitro |
Advanced Technologies for Enhanced Bone Organoid Platforms
Engineering-Driven Approaches
Recent technological advancements are progressively addressing the limitations of traditional organoid models through interdisciplinary convergence. Engineering-driven approaches include bioprinting, artificial intelligence, and microfluidic systems that enhance structural fidelity and culture optimization [4]. Bioprinting enables precise spatial patterning and scaffold fabrication, allowing the creation of complex 3D architectures that better mimic native bone tissue [4]. The rise of 3D bioprinting in tissue engineering has provided a powerful foundation for precise structural reconstruction of bone organoids with enhanced spatial control over cell placement and matrix composition [4].
Artificial intelligence (AI) accelerates organoid optimization through data-driven approaches, facilitating the analysis of complex datasets and predicting optimal culture conditions [4]. AI algorithms can process high-content imaging data from organoid screening campaigns, identify subtle morphological patterns associated with specific functional states, and guide the refinement of mechanical stimulation parameters to enhance organoid maturity. Microfluidic systems and organ-on-a-chip (OoC) platforms provide fine-tuned control of the culture microenvironment, including nutrient and growth factor gradients, while enabling the application of physiologically relevant mechanical forces such as fluid shear stress and cyclic strain [75]. These systems decrease reliance on supraphysiological concentrations of exogenous supplements and enhance the translational relevance of organoid models for pharmacological testing [75].
Biology-Oriented Strategies
Biology-oriented advances include assembloid technology and gene editing, which enrich cellular complexity and genetic programmability [4]. Assembloids enable the assembly of multicellular systems to better replicate bone tissue microenvironments, incorporating various cell types such as osteoblasts, osteocytes, osteoclasts, and stromal cells in spatially organized configurations [4]. This approach mediates the integration of heterogeneous cell populations to reconstruct physiological complexity, enabling the recreation of critical cell-cell interactions that govern bone homeostasis and disease processes.
Gene editing technologies, particularly CRISPR-Cas9 systems, refine disease modeling and functional modifications by allowing precise manipulation of genetic sequences to introduce or correct disease-associated mutations, create reporter lines for tracking specific cell populations, or modulate signaling pathways involved in mechanotransduction [4]. These tools enable the creation of genetically defined model systems that facilitate the investigation of gene function in bone biology and provide platforms for screening targeted therapeutics. The convergence of engineering-driven and biology-oriented approaches represents a powerful framework for advancing bone organoid technology and enhancing its utility for high-throughput drug screening applications.
High-Throughput Screening Platforms for Bone Organoids
Automated Imaging and Analysis Pipelines
The implementation of high-throughput screening platforms for organoids requires automated systems for image acquisition, processing, and data analysis. Recent studies have demonstrated that high-throughput confocal microscopy and automated analysis techniques can effectively evaluate 3D organoid morphological and structural features [77]. These approaches illustrate the potential of high-throughput confocal imaging and computerized analysis methods for phenotypic profiling in complex 3D organoid models. A recently developed 96-well plate-based automated pipeline enables rapid imaging and quantification of fluorescent labeling in organoids using a high-throughput confocal microscope and image analysis software [77].
This platform offers a novel approach to efficiently and rapidly image and quantify fluorescent staining and immunolabeling in organoids with many potential applications, including drug screening, toxicity testing, barrier integrity studies, host-pathogen interactions, and lineage tracking [77]. The pipeline can quantify varying levels of cell proliferation among donor organoid lines in response to various stimuli and measure cytoplasmic fluorescence of cell identity markers, enabling detection of inter-donor variability and cell-specific responses [77]. When utilizing 3D organoids for high-throughput studies, their inherent variability in size, shape, and organization increases imaging complexity and processing requirements, making the development of robust analytical pipelines essential for reliable screening outcomes.
Standardization and Quality Control
Standardization of organoid culture protocols is crucial for ensuring the reliability and reproducibility of experimental results in high-throughput screening applications [76]. In the context of organoid culture systems, every step from cell acquisition to organoid culture, drug screening, and validation must adhere to standardized operating procedures (SOPs) [76]. This approach encompasses pre-laboratory preparation, laboratory protocols, and post-laboratory processing to minimize experimental errors and uncertainties while enhancing the credibility and reproducibility of experiments [76].
The application of defined and tunable biomaterials, micropatterning techniques, and 3D bioprinting methods provides several advantages for high-throughput screening, including enabling spatial guidance for organoid growth and morphogenesis, enhancing the efficiency of cell-cell interactions, and improving reproducibility across experimental batches [75]. These platforms allow precise regulation of both the type and concentration of supplemented factors, thereby facilitating the rational design of minimal media formulations that reduce unnecessary variables and enhance screening consistency [75]. The implementation of automated robotic systems for drug treatment, detection, and liquid handling further standardizes organoid manipulation and reduces technical variability in high-throughput screening workflows [76].
Table 2: High-Throughput Solutions for Organoid-Based Drug Screening
| Screening Stage | Conventional Approach | High-Throughput Solution | Key Benefits |
|---|---|---|---|
| Sample Processing | Manual tissue digestion | Microfluidic single-cell preparation | Standardized digestion, improved cell viability |
| Organoid Culture | Manual plating in low-density formats | Automated robotic plating in 384-well plates | Increased throughput, reduced labor costs |
| Mechanical Stimulation | Static culture conditions | Bioreactor arrays with controlled mechanical loading | Enhanced physiological relevance, improved maturation |
| Drug Treatment | Manual compound addition | Automated liquid handling systems | Precision dosing, reduced human error |
| Image Acquisition | Manual confocal microscopy | High-content spinning disk confocal systems | Rapid acquisition, 3D reconstruction capability |
| Data Analysis | Manual quantification | Automated image analysis pipelines | Objective assessment, high-dimensional data extraction |
Experimental Protocols for Mechanically-Stimulated Bone Organoids
Protocol 1: Bioreactor-Based Mechanical Stimulation
This protocol describes the application of cyclic mechanical stimulation to bone organoids using commercially available bioreactor systems to enhance their maturation and physiological relevance for drug screening applications.
Materials and Reagents:
- Mesenchymal stem cells (MSCs) derived from human induced pluripotent stem cells (iPSCs)
- Osteogenic differentiation medium: DMEM supplemented with 10% FBS, 100 nM dexamethasone, 10 mM β-glycerophosphate, 50 μg/mL ascorbic acid-2-phosphate
- Fibrin hydrogel matrix: 5 mg/mL fibrinogen solution in PBS combined with 2 U/mL thrombin
- 24-well bioreactor plates with programmable mechanical loading systems
- 4% paraformaldehyde fixation solution
- Immunostaining reagents: primary antibodies for osteocalcin, collagen I, RUNX2; fluorescently-labeled secondary antibodies
Procedure:
- Organoid Formation: Harvest MSCs at passage 3-5 and resuspend in fibrinogen solution at a density of 10 × 10^6 cells/mL. Combine with thrombin solution (1:1 ratio) and pipette 50 μL droplets into each well of the bioreactor plate. Allow polymerization for 30 minutes at 37°C.
- Osteogenic Differentiation: Add 1 mL of osteogenic differentiation medium to each well and culture for 7 days to allow initial matrix deposition.
- Mechanical Stimulation: Initiate cyclic compressive loading using the following parameters: 10% strain, 1 Hz frequency, 1 hour per day, for 14 consecutive days. Maintain control organoids in identical conditions without mechanical stimulation.
- Monitoring and Analysis: Monitor organoid contraction daily and refresh medium every 2-3 days. Following the stimulation period, fix organoids in 4% paraformaldehyde for 2 hours at 4°C for subsequent analysis.
- Assessment: Perform immunostaining for osteogenic markers and quantitative analysis of mineralization via micro-CT or Alizarin Red staining. Compare mechanically stimulated organoids with static controls to assess enhancement of maturation.
Protocol 2: High-Throughput Drug Screening with Mature Bone Organoids
This protocol outlines a standardized workflow for conducting high-throughput drug screening campaigns using mechanically-stimulated bone organoids in 96-well plate formats.
Materials and Reagents:
- Mature bone organoids pre-conditioned with mechanical stimulation
- Compound libraries dissolved in DMSO at 10 mM concentration
- Automated liquid handling system
- 96-well black-walled imaging plates with clear bottoms
- Cell viability assay reagents: Alamar Blue, Calcein-AM/Ethidium homodimer-1 live/dead staining
- Osteogenesis assay reagents: OsteoImage mineralization staining
- High-content imaging system with environmental control
- Image analysis software (e.g., ImageJ, CellProfiler)
Procedure:
- Organoid Transfer: Transfer individual mechanically-stimulated bone organoids to 96-well imaging plates using wide-bore pipette tips, ensuring one organoid per well in 100 μL of maintenance medium.
- Compound Treatment: Using an automated liquid handling system, add test compounds to achieve final concentrations ranging from 1 nM to 10 μM, maintaining DMSO concentration below 0.1%. Include appropriate controls (vehicle, positive controls for osteogenesis modulation).
- Incubation and Monitoring: Culture organoids for 7-14 days with compound treatment, refreshing medium and compounds every 2-3 days. Monitor organoid viability and morphology throughout the treatment period.
- Endpoint Assessment:
- Viability Assessment: Add Alamar Blue reagent (10% v/v) to each well and incubate for 4 hours. Measure fluorescence at 560Ex/590Em.
- Mineralization Analysis: Fix a subset of organoids with 4% PFA for 20 minutes, then stain with OsteoImage reagent according to manufacturer's instructions to quantify hydroxyapatite deposition.
- Morphological Analysis: For live organoids, stain with Calcein-AM (2 μM) and Ethidium homodimer-1 (4 μM) for 1 hour to assess viability and structure in 3D.
- High-Content Imaging: Image organoids using an automated high-content imaging system with z-stacking capability to capture full 3D structure. Acquire a minimum of 5 z-slices per organoid with 20μm spacing.
- Data Analysis: Extract quantitative features from images including organoid size, shape, fluorescence intensity, and texture features. Normalize data to vehicle controls and calculate dose-response curves for compound efficacy.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Bone Organoid Research and High-Throughput Screening
| Reagent Category | Specific Products | Function in Bone Organoid Research |
|---|---|---|
| Stem Cell Sources | Human iPSCs, Bone Marrow-derived MSCs, Adipose-derived Stem Cells | Provide cellular foundation for organoid formation with osteogenic potential |
| Matrix Materials | Fibrin Hydrogels, Collagen Type I, Defined Synthetic PEG Hydrogels, Modified Matrigel | 3D scaffold supporting cell organization and matrix deposition with tunable mechanical properties |
| Osteogenic Factors | Recombinant BMP-2, BMP-4, BMP-7, Dexamethasone, β-Glycerophosphate, Ascorbic Acid | Induce and enhance osteogenic differentiation and mineralization |
| Mechano-Modulatory Compounds | Y-27632 (ROCK inhibitor), Cytochalasin D, TRPV4 Agonists, FAK Inhibitors | Modulate cellular response to mechanical stimuli and investigate mechanotransduction pathways |
| Neuropeptides | CGRP, Substance P, VIP, NPY | Enhance innervation and synergize with osteogenic factors; CGRP synergistically promotes osteogenesis with BMP-2 at physiological dosages [7] |
| Analysis Reagents | OsteoImage Mineralization Assay, Alizarin Red S, ALP Staining Kits, Live/Dead Viability Assays | Quantify osteogenic differentiation progression and cellular viability |
| High-Throughput Tools | 384-Well Microplates, Automated Liquid Handlers, Spinning Disk Confocal Systems, High-Content Analyzers | Enable scalable screening with standardized conditions and automated readouts |
Signaling Pathways and Experimental Workflows
Bone Organoid Workflow and Mechanotransduction Pathways
CGRP and BMP-2 Synergistic Signaling
The integration of mechanically-stimulated bone organoids into high-throughput drug screening platforms represents a transformative approach in preclinical research, offering enhanced physiological relevance and predictive capability compared to traditional 2D culture systems. The critical role of mechanical cues in bone biology necessitates their incorporation into organoid maturation protocols to better recapitulate native tissue environments and improve the clinical translatability of screening outcomes. Recent advances in bioreactor technologies, imaging platforms, and automated analysis pipelines have enabled the scaling of these complex 3D model systems for efficient drug discovery and development applications.
Future developments in bone organoid technology will likely focus on enhancing model complexity through the integration of vascular and neural components, further improving their physiological relevance and screening utility [4] [7]. The continued convergence of engineering principles with biological insights will drive the creation of next-generation organoid platforms with precisely controlled mechanical environments and enhanced reproducibility. As regulatory agencies increasingly recognize the value of human cell-based models for safety and efficacy assessment - evidenced by the FDA's recent announcement outlining plans to phase out traditional animal testing in favor of advanced non-animal testing platforms - the importance of robust, predictive organoid-based screening systems will continue to grow [75]. Through continued refinement and standardization, mechanically-stimulated bone organoids are poised to become indispensable tools in the drug development pipeline, accelerating the discovery of novel therapeutics for skeletal diseases and injuries while improving the efficiency and success rates of clinical translation.
The field of bone organoid research represents a paradigm shift in studying skeletal development, disease modeling, and regenerative medicine. These three-dimensional (3D) biomimetic constructs, which mimic the complex architecture and multicellular composition of native bone tissue, offer unprecedented opportunities for advancing personalized orthopedics and bone disease intervention [4]. However, the translational potential of bone organoids is currently constrained by significant challenges including lack of vascularization, insufficient mechanical stimulation, and critical standardization issues across different models [4] [5]. The establishment of rigorous evaluation frameworks is therefore paramount for ensuring these advanced models can reliably predict clinical outcomes and safely transition to therapeutic applications.
Within this context, the role of mechanical cues in bone organoid differentiation and maturation emerges as a particularly critical dimension. Bone is a dynamic tissue whose development and homeostasis are profoundly regulated by biomechanical forces [4]. Native bone tissue possesses exceptional mechanical strength and load-bearing capacity, supporting locomotion and organ protection while exhibiting dynamic remodeling regulated by mechanical cues that profoundly influence cell differentiation, matrix deposition, and tissue maturation [4]. Unfortunately, these essential biomechanical factors are largely absent in conventional organoid culture platforms, creating a significant gap between experimental models and physiological reality [4]. This whitepaper establishes a comprehensive evaluation framework that specifically addresses mechanical cue integration alongside traditional assessment parameters, providing researchers with standardized methodologies for quantifying bone organoid maturation and functional capacity.
Critical Evaluation Dimensions for Bone Organoid Maturation
Structural and Compositional Assessment
Comprehensive structural evaluation forms the foundation of bone organoid assessment. Histological analysis remains indispensable for characterizing tissue organization and cellular distribution. Standard staining protocols including hematoxylin and eosin (H&E) for general morphology, Masson's trichrome for collagen deposition, and picrosirius red under polarized light for collagen alignment provide essential qualitative data on matrix composition and organization [78]. Immunohistochemical staining further enables specific protein localization—collagen I for osteogenic matrix, osteoprotegerin (OPG) and receptor activator of nuclear factor kappa-B ligand (RANKL) for bone metabolic activity, and specific markers like Ki67 for proliferation and γh2AX for senescence [78] [7].
Advanced imaging technologies offer quantitative assessment of bone microarchitecture. Micro-computed tomography (μCT) provides three-dimensional evaluation of mineralized tissue formation, revealing critical parameters such as bone volume fraction (BV/TV), trabecular thickness (Tb.Th), trabecular number (Tb.N), and trabecular separation (Tb.Sp) [78]. These parameters significantly correlate with functional healing outcomes, as demonstrated in osteoporosis models where CT-based bone microarchitectural parameters showed strong correlation with tendon-to-bone healing capacity [78]. Additionally, emerging techniques including second harmonic generation (SHG) imaging for collagen organization and Raman spectroscopy for molecular composition provide further dimensionality to structural assessment.
Table 1: Structural and Compositional Evaluation Parameters for Bone Organoids
| Evaluation Category | Specific Parameters | Quantitative Metrics | Assessment Methodology |
|---|---|---|---|
| Matrix Composition | Collagen Organization | Fiber alignment, density | Picrosirius red staining, SHG imaging |
| Mineralization | Mineral density, distribution | μCT, von Kossa staining, ARS | |
| Protein Expression | Collagen I, OPG/RANKL | Immunohistochemistry, Western blot | |
| Cellular Organization | Cell Distribution | Uniformity, stratification | H&E staining, confocal microscopy |
| Proliferation/Senescence | Ki67+, γh2AX+ cells | Immunofluorescence, flow cytometry | |
| Differentiation Status | Osteocalcin+, RUNX2+ cells | qPCR, single-cell RNA sequencing | |
| 3D Architecture | Trabecular Structure | BV/TV, Tb.Th, Tb.N, Tb.Sp | μCT analysis |
| Tissue Integration | Boundary definition, continuity | Histomorphometry, μCT | |
| Vascular Network | Vessel density, connectivity | CD31 immunostaining, perfusability assays |
Functional and Biomechanical Evaluation
Functional assessment represents the most clinically relevant dimension of bone organoid evaluation, with biomechanical properties serving as critical indicators of functional maturation. Standardized biomechanical testing must evaluate elastic modulus, ultimate tensile strength, and compressive strength using instruments such as universal mechanical testers [78]. In osteoporosis research, parameters like Young's modulus have demonstrated significant correlation with healing outcomes, with studies showing reduced modulus values in osteoporotic groups (50% interface failure) compared to controls [78].
The role of mechanical stimulation in bone organoid maturation necessitates specialized culture systems that apply physiologically relevant forces. Bioreactors that provide cyclic strain, compression, or vibrational forces can significantly enhance osteogenic differentiation and matrix organization [4]. These systems mimic the native mechanical environment of bone tissue, promoting maturation through mechanotransduction pathways that regulate cellular behaviors including proliferation, differentiation, and matrix mineralization [4]. Evaluation should include both the application of mechanical cues during culture and subsequent assessment of the organoids' functional response to these stimuli.
Molecular analysis of mechanotransduction pathways provides insight into the biological mechanisms underlying functional maturation. Gene expression profiling of markers such as RUNX2, ALPL, and osteocalcin reveals osteogenic differentiation status, while YAP/TAZ localization indicates activation of mechanosensitive pathways [7]. The synergistic relationship between mechanical cues and biochemical signaling is exemplified by research showing that the neuropeptide CGRP significantly enhances osteogenic differentiation when combined with BMP-2, increasing ALPL and RUNX2 expression and producing more robust mineralization [7].
Table 2: Functional and Biomechanical Evaluation Parameters for Bone Organoids
| Functional Category | Evaluation Method | Measured Parameters | Significance |
|---|---|---|---|
| Biomechanical Properties | Uniaxial tensile/compression testing | Young's modulus, ultimate strength | Indicates structural integrity and load-bearing capacity |
| Nanoindentation | Hardness, elastic modulus | Measures local mechanical properties at tissue interfaces | |
| Rheology | Storage/loss moduli | Assesses viscoelastic properties of developing matrix | |
| Mechanobiological Response | Bioreactor culture with mechanical stimulation | Gene expression changes (RUNX2, ALPL) | Evaluates osteogenic response to mechanical cues |
| Calcium imaging | Intracellular Ca2+ flux | Measures real-time mechanosensitive signaling | |
| Immunofluorescence | YAP/TAZ nuclear localization | Indicates activation of mechanotransduction pathways | |
| Metabolic Activity | Biochemical assays | ALP activity, calcium deposition | Quantifies osteogenic differentiation capacity |
| Media analysis | OPG/RANKL ratio, osteocalcin secretion | Measures bone metabolic marker secretion | |
| Resazurin reduction | Metabolic activity | Evaluates overall cell viability and proliferation |
Protocol for Standardized Mechanical Conditioning and Assessment
Materials Required:
- Commercially available cyclic strain bioreactor system (e.g., Flexcell, Strex)
- Mesenchymal stem cells (MSCs) derived from human induced pluripotent stem cells (iPSCs)
- Osteogenic differentiation media: α-MEM supplemented with 10% FBS, 10 mM β-glycerophosphate, 50 μg/mL ascorbic acid, and 10 nM dexamethasone
- Type I collagen hydrogel (3 mg/mL concentration)
- RNA extraction kit and qPCR reagents
- Primary antibodies: anti-RUNX2, anti-osteocalcin, anti-YAP/TAZ
- 4% paraformaldehyde fixation solution and permeabilization buffer (0.1% Triton X-100)
Methodology:
- Organoid Generation: Suspend 2×10^6 MSCs in 200 μL collagen hydrogel solution. Pipette into cylindrical molds (5mm diameter × 2mm height) and polymerize at 37°C for 30 minutes. Culture in osteogenic media for 7 days before mechanical stimulation.
Mechanical Conditioning: Transfer organoids to bioreactor plates and subject to cyclic uniaxial strain (10% elongation, 1 Hz frequency, 4 hours/day) for 14 days. Maintain control organoids in static culture with identical media conditions.
Biomechanical Testing: Following conditioning, assess organoids using a universal testing system with a 10N load cell. Perform unconfined compression testing at 0.1 mm/min strain rate until failure. Calculate elastic modulus from the linear region of the stress-strain curve.
Molecular Analysis: Extract RNA and perform qPCR for osteogenic markers (RUNX2, ALPL, osteocalcin, collagen I). Fix parallel samples for immunostaining and confocal microscopy to quantify nuclear YAP/TAZ localization.
Data Normalization: Normalize all mechanical and molecular data to DNA content using commercially available quantification kits.
This protocol standardizes the application and assessment of mechanical cues, enabling direct comparison across different bone organoid platforms and research laboratories.
Advanced Technologies Enhancing Evaluation Frameworks
Integrated Engineering Approaches
Advanced engineering technologies are revolutionizing bone organoid evaluation by enabling precise control over the mechanical microenvironment. Three-dimensional bioprinting allows fabrication of organoids with spatially defined architectures, incorporating multiple cell types and gradient biomaterial properties that mimic native tissue heterogeneity [4] [7]. Digital light processing (DLP) printing technology has been used to create callus-like organoids that recapitulate diverse cell compositions and behaviors of developing bone [7]. These engineered constructs provide more physiologically relevant platforms for evaluating mechanical responses compared to traditional self-assembled organoids.
Microfluidic systems address the critical challenge of vascularization by enabling fluid perfusion that enhances nutrient delivery and waste removal, partially alleviating transport limitations that restrict organoid size and maturation [4]. These "organ-on-a-chip" platforms permit application of shear stress forces that simulate blood flow, further enhancing the physiological relevance of mechanical cue evaluation. Recent studies have successfully introduced microvascular endothelial cells into culture systems, creating preliminary vascular networks that improve organoid viability and functional maturation [4].
Data-Driven Assessment Technologies
Artificial intelligence (AI) and machine learning are transforming bone organoid evaluation through data-driven optimization approaches. AI algorithms can analyze complex multidimensional data from imaging, molecular, and biomechanical assessments to identify subtle patterns indicative of functional maturation [4]. Machine learning approaches enable cross-species comparisons that reveal fundamental biological principles, as demonstrated by research showing high similarity in Krt8+ skeletal stem cell activation between organoid-driven bone repair and developmental bone tissue structures [7].
Single-cell RNA sequencing provides unprecedented resolution for evaluating cellular responses to mechanical cues, identifying distinct subpopulations such as Krt8+ skeletal stem cells that expand during regeneration while injury-responsive Has1+ migratory fibroblasts concurrently decrease [7]. This granular analysis enables researchers to precisely map how mechanical stimulation influences specific cellular trajectories and lineage commitments within complex organoid systems.
Implementation Framework for Standardized Evaluation
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Bone Organoid Evaluation
| Category | Specific Reagents/Platforms | Function in Evaluation | Key Considerations |
|---|---|---|---|
| Stem Cell Sources | Human iPSCs, MSCs | Organoid foundation | Differentiation efficiency, donor variability |
| Biomaterial Scaffolds | Type I collagen, Matrigel, synthetic hydrogels | 3D structural support | Batch variability, mechanical properties |
| Mechanical Stimulation | Cyclic strain bioreactors, compression systems | Application of mechanical cues | Frequency, magnitude, duration optimization |
| Osteogenic Inducers | BMP-2 (0.5 μg/mL), CGRP (10^-8 M), β-glycerophosphate | Enhance osteogenic differentiation | Synergistic combinations, concentration effects |
| Imaging Platforms | μCT, confocal microscopy, second harmonic generation | Structural and compositional analysis | Resolution, penetration depth, quantification |
| Molecular Analysis | scRNA-seq, qPCR, Western blot | Mechanotransduction pathway evaluation | Sensitivity, multiplexing capability |
Quality Control and Validation Metrics
Establishing robust quality control measures is essential for standardizing bone organoid evaluation across research laboratories. Reference materials including standardized hydroxyapatite phantoms for μCT calibration and control organoids from validated cell lines should be implemented to enable cross-laboratory comparison [79]. Quantitative thresholds for key parameters including minimum elastic modulus (≥0.5 kPa), mineralization density (≥150 mg HA/cm³), and osteogenic gene expression (≥5-fold increase in RUNX2) provide objective benchmarks for functional maturation [78] [79].
Validation against clinical standards remains crucial for translational relevance. Correlation with established assessment methodologies including quantitative CT analysis, which has demonstrated strong association with fracture risk (AUC 0.748 for QCT vs 0.575 for areal BMD in discriminating fracture patients), ensures organoid models accurately reflect human physiology [79] [80]. Incorporating multiple validation endpoints creates a comprehensive evaluation framework that reliably predicts clinical performance.
The establishment of rigorous, standardized evaluation frameworks for bone organoids represents a critical prerequisite for clinical translation. By systematically addressing structural, compositional, and functional dimensions—with particular emphasis on the role of mechanical cues in maturation and differentiation—researchers can develop more physiologically relevant models that faithfully recapitulate human bone biology. The integration of advanced engineering technologies with data-driven assessment approaches will further enhance evaluation precision, enabling quantitative prediction of clinical performance.
Future standards must continue to evolve, incorporating emerging understanding of bone developmental biology and increasingly sophisticated assessment technologies. Through collaborative efforts across research institutions, standardization bodies, and regulatory agencies, the field can establish universally accepted evaluation criteria that accelerate the translation of bone organoid technologies from laboratory discoveries to clinical applications that improve patient care in orthopedics and regenerative medicine.
Mechanotransduction Evaluation Pathway
Standardized Mechanical Assessment Workflow
Conclusion
The integration of mechanical cues is paramount for advancing bone organoid technology from a simplistic cellular aggregate to a truly physiologically relevant model. As this review has detailed, a deep understanding of foundational mechanobiology, combined with sophisticated engineering approaches, enables the directed differentiation and functional maturation of bone organoids. Overcoming persistent challenges in vascularization, standardization, and biomaterial design will be crucial. Future research must focus on interdisciplinary convergence, leveraging AI, advanced bioprinting, and multi-omics to decode the complex interplay between physical forces and biological signaling. The ultimate goal is the creation of personalized 'ex vivo skeletal systems' that can revolutionize precision medicine, drug discovery, and regenerative therapies for skeletal diseases, thereby bridging the critical gap between experimental models and clinical application.
References
- 1. How the bone microenvironment shapes the pre-metastatic ... [https://pubmed.ncbi.nlm.nih.gov/39672975]
- 2. The bone microenvironment: new insights into the role of stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04288-4]
- 3. Understanding the Bone Marrow Niche: A Key to ... [https://blog.crownbio.com/understanding-the-bone-marrow-niche]
- 4. Innovative strategies for bone organoid - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362404/]
- 5. Engineering bone/cartilage organoids: strategy, progress, ... [https://www.nature.com/articles/s41413-024-00376-y]
- 6. Advancements in bone organoids: perspectives on ... [https://www.sciencedirect.com/science/article/pii/S2090123225003972]
- 7. Divide-and-conquer strategy with engineered ossification ... [https://www.nature.com/articles/s41467-025-61619-y]
- 8. In Vitro Bone Cell Models: Impact of Fluid Shear Stress on ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2016.00087/full]
- 9. Standardization and consensus in the development and application of bone organoids [https://www.thno.org/v15p0682.htm]
- 10. Trabecular bone organoids: a micron-scale 'humanised' ... [https://www.nature.com/articles/s41526-021-00146-8]
- 11. Substrate Stiffness of Bone Microenvironment Controls Functions of Pre-Osteoblasts and Fibroblasts In Vitro [https://www.mdpi.com/2313-7673/8/4/344]
- 12. Effect of substrate stiffness on the osteogenic differentiation of bone marrow stem cells and bone-derived cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/23447501/]
- 13. Fluid shear stress promotes osteogenesis of bone ... [https://www.sciencedirect.com/science/article/abs/pii/S1369703X22003540]
- 14. The Cytoskeleton and Connected Elements in Bone Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8217329/]
- 15. Roles of focal adhesion proteins in skeleton and diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10031257/]
- 16. Mechanobiology in Action: Biomaterials, Devices, and the ... [https://www.mdpi.com/2218-273X/15/6/848]
- 17. Mechanobiological engineering strategies for organoid culture [https://pmc.ncbi.nlm.nih.gov/articles/PMC12276045/]
- 18. Dynamic hydrogel mechanics in organoid engineering [https://www.sciencedirect.com/science/article/pii/S2452199X2500427X]
- 19. Integrin and Its Associated Proteins as a Mediator for ... [https://www.mdpi.com/2218-273X/15/2/166]
- 20. Role and mechanism of Integrin α5β1 in bone formation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12391163/]
- 21. Heterogeneity in The Mechanical Properties of Integrins ... [https://www.nature.com/articles/s41598-019-47958-z]
- 22. Role of YAP/TAZ in bone diseases: A transductor from ... [https://www.sciencedirect.com/science/article/pii/S2214031X24001633]
- 23. of Mechanobiology and YAP in physiology and disease - PMC TAZ [https://pmc.ncbi.nlm.nih.gov/articles/PMC6192510/]
- 24. of Mechanobiology and YAP in physiology and disease TAZ [https://www.nature.com/articles/nrm.2017.87?error=cookies_not_supported]
- 25. Control of cellular responses to mechanical cues through YAP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6873206/]
- 26. Bone organoid construction and evolution - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270736/]
- 27. The Hippo signalling pathway and its implications in ... [https://www.nature.com/articles/s41392-022-01191-9]
- 28. Optimal cell traction forces in a generalized motor-clutch model [https://pubmed.ncbi.nlm.nih.gov/37475213/]
- 29. A mechanistic motor-clutch model that explains cell shape ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9250388/]
- 30. Master equation-based analysis of a motor-clutch model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3896613/]
- 31. Review The motor-clutch model in mechanobiology and ... [https://www.sciencedirect.com/science/article/pii/S2949907024000305]
- 32. Determinants of maximal force transmission in a motor-clutch ... [https://pubmed.ncbi.nlm.nih.gov/23931306/]
- 33. Shifting the optimal stiffness for cell migration [https://www.nature.com/articles/ncomms15313]
- 34. Methodology and Characterization of a 3D Bone Organoid ... [https://www.mdpi.com/1422-0067/25/8/4225]
- 35. The impact of extracellular matrix viscoelasticity on cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7676152/]
- 36. Hydrogels with programmed spatiotemporal mechanical ... [https://www.nature.com/articles/s41467-025-59016-6]
- 37. Long-Term Culture of Cellular Spheroids in Novel Hydrogel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347893/]
- 38. Bioprinting revolution: Innovative design of 3D bioactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617564/]
- 39. Mechanical and biological properties of 3D printed bone ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1545693/full]
- 40. Advances and challenges in three-dimensional bioprinting ... [https://accscience.com/journal/IJB/0/0/10.36922/IJB025190183]
- 41. 3D bioprinting bone/cartilage organoids - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451290/]
- 42. From niche to organoid: Engineering bone tissues through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12314253/]
- 43. A bioreactor-based platform for investigating the early ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1634143/full]
- 44. Bioreactor design and validation for manufacturing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8870603/]
- 45. Potential of organ-on-a-chip in advancing synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635794/]
- 46. A guide to the organ-on-a-chip [https://www.nature.com/articles/s43586-022-00118-6]
- 47. Bone microphysiological models for biomedical research [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00762j]
- 48. Organ-on-a-Chip: A Roadmap for Translational Research in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610883/]
- 49. Organoids and organs-on-chips: insights into predicting the ... [https://www.nature.com/articles/s41420-023-01354-9]
- 50. Generation of complex bone marrow organoids from ... [https://www.nature.com/articles/s41592-024-02172-2]
- 51. Trabecular bone organoid model for studying the regulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7817107/]
- 52. BMP-2 peptide-functionalized nanopatterned substrates for ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961213007059]
- 53. Mechanical stimulation orchestrates the osteogenic ... [https://www.nature.com/articles/cddis2016112]
- 54. The role of physical cues in the development of stem cell- ... [https://link.springer.com/article/10.1007/s00249-021-01551-3]
- 55. Mechanical stimulation-induced purinome priming fosters ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03775-4]
- 56. Mechanical stimulation induced osteogenic differentiation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7199451/]
- 57. Getting Blood out of a Stone: Vascularization via Spheroids and Organoids in 3D Bioprinting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071597/]
- 58. Vascularization of a Bone Organoid Using Dental Pulp ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10188257/]
- 59. Sequential construction of vascularized and mineralized ... [https://www.sciencedirect.com/science/article/pii/S2452199X25000891]
- 60. Standardization and consensus in the development and application of bone organoids - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11671374/]
- 61. Hydrogels with programmed spatiotemporal mechanical for stem... cues [https://www.nature.com/articles/s41467-025-59016-6?error=cookies_not_supported&code=15e2fd71-e440-44fa-bbea-b0c9d7e6bc73]
- 62. Animal-free alternatives for Matrigel in human iPSC- ... [https://www.nature.com/articles/s41598-025-20091-w]
- 63. effects of hydrogel mechanics and biofunctionalization on ... [https://pubs.rsc.org/en/content/articlehtml/2025/ma/d5ma00165j]
- 64. Exploring the intersection of mechanobiology and artificial ... [https://www.nature.com/articles/s44341-025-00010-w]
- 65. An in silico study reveals how architectural and mechanical ... [https://www.sciencedirect.com/science/article/pii/S0010482525009254]
- 66. Matrix mineralization controls gene expression in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6185740/]
- 67. Correlations between gene expression and mineralization ... [https://www.sciencedirect.com/science/article/abs/pii/S8756328218304265]
- 68. (PDF) Comparative Efficacy of 3Dimensional (3D) Cell Culture ... [https://www.academia.edu/144456380/Comparative_Efficacy_of_3Dimensional_3D_Cell_Culture_Organoids_Vs_2Dimensional_2D_Cell_Cultures_Vs_Experimental_Animal_Models_In_Disease_modeling_Drug_development_And_Drug_Toxicity_Testing]
- 69. Advances in Bone Organoids Research and Future ... [https://pubmed.ncbi.nlm.nih.gov/40865550/]
- 70. 3D Organoids Cell Lines in Drug Discovery & Disease vs 2 D Modeling [https://www.moleculardevices.com/lab-notes/3d-biology/3d-organoids-vs-2d-cell-lines-drug-discovery]
- 71. Could Organoids Make Animal Obsolete in Research? Models [https://www.news-medical.net/health/Can-Organoids-Replace-Animal-Models-in-Human-Disease-Research.aspx]
- 72. A novel perspective on bone tumors: advances in organoid ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1550163/full]
- 73. A review of mathematical modeling of bone remodeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11864782/]
- 74. Urine-derived stem cells efficiently assemble into micro-bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639860/]
- 75. Iteration of Tumor Organoids in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566727/]
- 76. High-throughput solutions in tumor organoids: from culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11811636/]
- 77. A pipeline for rapid, high-throughput imaging and quantitative ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0332418]
- 78. Quantitative computed tomography analysis of bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273285/]
- 79. Comparison Between Quantitative Computed Tomography ... [https://www.mdpi.com/2076-3417/15/6/3248]
- 80. Thoracic vertebral bone mineral density measured by ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1672551/full]