Optimizing Germ-Free Mouse Production: A Protocol for Female Reproductive Tract-Preserved Cesarean Section
This article details the Female Reproductive Tract-Preserved Cesarean Section (FRT-CS) protocol, an optimized surgical technique for generating germ-free (GF) mouse models.
Optimizing Germ-Free Mouse Production: A Protocol for Female Reproductive Tract-Preserved Cesarean Section
Abstract
This article details the Female Reproductive Tract-Preserved Cesarean Section (FRT-CS) protocol, an optimized surgical technique for generating germ-free (GF) mouse models. Aimed at researchers, scientists, and drug development professionals, the content covers the foundational theory behind FRT-CS, provides a step-by-step methodological guide, discusses troubleshooting and optimization strategies, and presents comparative data validating its superiority over traditional techniques. The protocol enhances fetal survival rates, improves experimental reproducibility via precise delivery timing control, and identifies optimal GF foster strains, offering significant advancements for biomedical research reliant on high-quality GF animal models.
The Rationale and Scientific Basis for Preserving the Reproductive Tract in Cesarean Section
Germ-Free Mice as a Foundational Research Tool
Germ-free (GF) mice, raised in completely sterile gnotobiotic facilities, are a cornerstone model for investigating host-microbiome interactions. They provide a "clean slate" with no resident microorganisms, allowing researchers to conclusively determine the causal effects of specific microbes or defined microbial communities on host physiology and disease states [1]. This model is indispensable for dissecting the functionality of the gut microbiome, which influences nearly every organ in the body and impacts a wide range of biological and medical disciplines [2].
The relevance of this model is magnified within the context of Female Reproductive Tract (FRT) Preserved C-section Protocol Research. Cesarean delivery is a major abdominal surgery involving incisions through the abdominal wall and uterus [3]. As with any major surgery, it carries risks of infection, bleeding, and longer recovery times compared to vaginal births [4]. Furthermore, the procedure and the sterile environment in which it is performed can directly alter the initial microbial colonization of the newborn, which has systemic implications for immune development [5]. Using germ-free mice, researchers can systematically investigate how the absence of microbiota, mimicking aspects of a sterile birth environment, affects the physiology and immunology of the female reproductive tract and overall systemic health.
Research Applications of Germ-Free Mouse Models
Germ-free mice are utilized across a diverse spectrum of biomedical research areas. The table below summarizes key applications and their significance.
Table 1: Key Research Applications of Germ-Free Mouse Models
| Research Area | Application and Significance |
|---|---|
| Immunology | GF mice exhibit significant alterations in immune cell numbers and an underdeveloped immune system, highlighting the microbiome's critical role in immune stimulation and priming, even at sites far from the intestine [5] [6]. |
| Infectious Disease | Serves as a controlled model to study pathogen-host interactions and for the development of new-generation probiotics [1]. |
| Cancer | Used in preclinical testing to understand how the microbiome influences cancer development and therapy response [7]. |
| Metabolic Disease | Enables the study of microbiome-derived metabolites (e.g., phenol sulfate, 5-amino valeric acid betaine) and their systemic impact on host metabolism [5]. |
| Inflammatory Bowel Disease (IBD) | Used with specific genetically modified strains (e.g., TNFΔARE, SAMP1/YitFc) to model human Crohn's disease and investigate microbial drivers of colitis [2] [1]. |
The FRT-Preserved C-section and Germ-Free Model Interface
Understanding the interplay between surgical birth procedures and the microbiome is crucial. The C-section procedure involves creating a laparotomy followed by a hysterotomy to deliver the fetus [3]. A key anatomical consideration is the vesicouterine peritoneum, which connects the bladder to the uterus. In patients with a history of prior C-sections, the bladder can be more challenging to separate from the uterus [3]. Preserving the integrity of the FRT during this surgery is paramount for patient recovery and future reproductive health.
Germ-free models are vital for probing the long-term systemic consequences of a sterile or altered initial microbial exposure, a condition relevant to C-section births. Research has demonstrated that germ-free mice display significant molecular and cellular changes in all tissues tested, including the ileum, colon, spleen, lung, liver, and kidney, with the most pronounced alterations occurring in the liver [5]. This indicates that the absence of microbiota has far-reaching, systemic effects, potentially impacting the healing and function of the FRT post-C-section.
The following workflow integrates a preservation-focused C-section protocol with subsequent experimentation using germ-free models.
Essential Protocols and Methodologies
Protocol for Generating and Maintaining a Germ-Free Mouse Colony
Maintaining a germ-free status requires specialized infrastructure and stringent procedures.
- Gnotobiotic Isolators: Mice are housed in flexible-film or rigid isolators that provide a physical barrier from the external environment. All materials entering the isolator (food, bedding, water) must be sterilized, typically using autoclaving or radiation.
- Sterility Monitoring: Regular screening is essential. Fecal pellets and swabs from the isolator interior are tested for bacterial, fungal, and viral contamination using both culture-based methods and molecular techniques (e.g., 16S rRNA PCR).
- Breeding within the Isolator: Germ-free colonies are sustained by breeding mice inside the isolator. This requires specialized techniques for transferring breeders and weaning pups without compromising sterility.
- Germ-Free Rederivation: This process is used to introduce a new mouse strain into a germ-free colony. It is typically performed via embryo transfer, where embryos are surgically implanted into a germ-free surrogate mother. This service can be obtained commercially, with costs around $9,300 per procedure [2].
Protocol for Microbiota Engraftment (Humanization)
A common experiment involves colonizing germ-free mice with a defined microbial community to study its function.
- Material Collection: Donor material is collected, such as human fecal samples or microbial cultures from wildling mice [6] [1].
- Sample Preparation: The sample is homogenized in an anaerobic, sterile buffer under strict anaerobic conditions to preserve oxygen-sensitive microbes.
- Oral Gavage: Adult, fully colonized germ-free mice are inoculated via a single oral gavage with the prepared microbial suspension [6]. Control mice receive a sterile vehicle.
- Verification of Engraftment: Fecal samples are collected regularly post-gavage (e.g., on day 0, 7, 14, 28) and analyzed via 16S rRNA gene sequencing to confirm the successful establishment of the new microbiota [6]. Metabolomic analysis of cecal contents can further verify functional engraftment [6].
The following diagram illustrates the key decision points in designing germ-free experiments.
Protocol for Phenotypic and Metabolic Characterization
Post-engraftment, detailed analysis is performed to characterize the host response.
- Spatial Metabolic Characterization: As demonstrated in recent studies, tissues (ileum, colon, liver, spleen, lung, kidney) are collected and analyzed using spatial biology approaches like imaging mass spectrometry to map the location of small molecules directly in the tissue [5].
- Immune Phenotyping: Organs are processed for flow cytometry to quantify and characterize immune cell populations (e.g., T-cells, B-cells, macrophages). Germ-free mice typically show significant alterations in immune cell numbers indicative of an aberrant immune response [5].
- Metabolomic Profiling: Cecal contents or blood plasma are analyzed using mass spectrometry-based global metabolomics to identify changes in microbiome-derived metabolites (e.g., phenol sulfate, 5-amino valeric acid betaine) [5] [6].
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and resources for establishing and utilizing germ-free mouse models.
Table 2: Essential Research Reagents and Resources for Germ-Free Mouse Research
| Item/Resource | Function and Application |
|---|---|
| C57BL/6 (B6) Mouse | The most widely used inbred, germ-free strain; a permissive background for maximal expression of most mutations [2]. |
| TNFΔARE & SAMP Mice | Specific germ-free models of Crohn's disease-like ileitis for studying inflammatory bowel disease (IBD) [2]. |
| Gnotobiotic Isolators | Specialized sterile housing units that provide a physical barrier to maintain germ-free conditions for mouse colonies. |
| Germ-Free Rederivation Service | Commercial service (e.g., via Taconic Biosciences) to introduce new mouse strains into a germ-free colony via embryo transfer [2]. |
| 16S rRNA Sequencing | Molecular method for verifying germ-free status and profiling bacterial community composition after engraftment [6]. |
| Experimental Support Services | Core facility services for procedures like gavaging, intraperitoneal injections, organ collection, and assistance with IACUC protocols [2]. |
| HBF-0259 | HBF-0259, MF:C16H12Cl2FN5, MW:364.2 g/mol |
| Fozivudine Tidoxil | Fozivudine Tidoxil, CAS:141790-23-0, MF:C35H64N5O8PS, MW:746.0 g/mol |
Quantitative Data and Market Context
The use of germ-free mice in research represents a significant and growing market, reflecting their increasing importance in biomedical science.
Table 3: Quantitative Data on the Germ-Free Mouse Market and Resources
| Parameter | Value / Specification | Context / Note |
|---|---|---|
| Global Market CAGR | 7.5% | Compound Annual Growth Rate from a base year to 2025 [7]. |
| Leading Vendor Market Share | >40% | Collective share held by The Jackson Laboratory, Charles River Laboratories, and Taconic Biosciences [7]. |
| Germ-Free Cage Per Diem | $4.00 / cage day | Standard housing cost at a university core facility [2]. |
| C57BL/6 Mouse Price | $150.00 each | Cost for academic/internal researchers at a core facility [2]. |
| Experimental Support Hourly Rate | $65.00 / hour | Charge for project support from core facility staff [2]. |
Limitations of Traditional Cesarean Section (T-CS) for GF Mouse Derivation
Germ-free (GF) mice are an indispensable animal model for studying the interaction between the microbiome and host genes in human health and disease [8]. The production of these animals is therefore a critical procedure in biomedical research. Caesarean section (C-section) rederivation is considered the gold standard method for obtaining GF mice and is based on the "sterile womb hypothesis," which posits that the placental epithelium acts as a barrier, protecting the fetus from microbial exposure [8]. The traditional C-section (T-CS) technique has been widely used for this purpose. However, this method presents significant challenges that can compromise the efficiency and reproducibility of deriving GF mouse colonies. This application note details the specific limitations of the T-CS technique within the context of research aimed at optimizing protocols, specifically those investigating Female Reproductive Tract preserved C-section (FRT-CS) methods. The information is intended to guide researchers, scientists, and drug development professionals in improving their experimental workflows for generating GF animal models.
Key Limitations of the T-CS Technique
The Traditional Cesarean Section (T-CS) technique, while foundational, suffers from several procedural and biological drawbacks that can impact the viability of pups and the overall success of GF mouse production.
- Compromised Fetal Survival Rates: The T-CS technique involves clamping both the cervix base and the top of the uterine horn. This invasive approach is associated with lower fetal survival rates compared to optimized methods [8].
- Disruption of Maternal Microbiome Transfer: C-section delivery fundamentally disrupts the normal initial colonization of the infant with the maternal vaginal and perineal microbiome. Instead, C-section-delivered infants are primarily colonized by skin and environmental bacteria, leading to suboptimal development of the infant's microbiome [9]. While the goal is a germ-free state, the initial separation from the maternal reproductive tract in a non-physiological manner may have unintended consequences.
- Enduring Behavioral and Physiological Effects: Studies in mouse models indicate that birth by C-section has long-term consequences. C-section-born mice exhibit marked but transient changes in gut microbiota composition, particularly a depletion in Bifidobacterium spp. These mice demonstrated enduring deficits in social, cognitive, and anxiety-related behaviors in early life and adulthood [10].
- Inefficiency in Experimental Planning: The reliance on natural mating (NM) for obtaining donor mice in T-CS protocols introduces variability. The difficulty in precisely predicting delivery dates leads to logistical challenges and inconsistencies in scheduling the C-section procedure, which is time-sensitive [8].
Quantitative Comparison: T-CS vs. FRT-CS
The following tables summarize experimental data comparing the T-CS technique with the optimized Female Reproductive Tract preserved C-section (FRT-CS) technique, which selectively clamps only the cervix base, preserving the entire reproductive tract [8].
Table 1: Comparison of Cesarean Section Surgical Techniques on Pup Survival
| Surgical Technique | Description | Fetal Survival Rate | Key Advantage |
|---|---|---|---|
| Traditional C-section (T-CS) | Clamps placed at both the cervix base and the top of the uterine horn. | Lower | Established, but less optimized, historical method. |
| FRT-preserved C-section (FRT-CS) | Selective clamping only at the cervix base, preserving ovary, uterine horn, and cervix. | Significantly Improved | Preserves female reproductive tract anatomy, improving neonatal survival while maintaining sterility. |
Table 2: Impact of Donor Conception Method on C-section Efficiency
| Donor Conception Method | Delivery Date Control | Experimental Reproducibility | Contamination Risk |
|---|---|---|---|
| Natural Mating (NM) | Low (High variability) | Low | Consistent with surgical sterility protocols |
| In Vitro Fertilization (IVF) | High (Precise control) | Enhanced | Consistent with surgical sterility protocols |
Table 3: Maternal Care Success of Different GF Foster Strains
| GF Foster Mother Strain | Nursing and Weaning Success | Relative Performance |
|---|---|---|
| BALB/c | Superior | High |
| NSG | Superior | High |
| KM (Outbred) | Moderate | Medium |
| C57BL/6J | Lowest | Low |
Detailed Experimental Protocols
Protocol A: Traditional Cesarean Section (T-CS) for GF Mouse Derivation
Objective: To aseptically derive germ-free mouse pups from a time-mated, pregnant SPF donor mouse using the Traditional C-section technique. Reagents & Equipment: Pregnant SPF donor mouse (e.g., C57BL/6), Clidox-S disinfectant, sterile surgical instruments (scissors, forceps, clamps), sterile gauze, sterile PBS or saline, germ-free isolator with transfer port, heating pad, timed GF foster mother. Procedure:
- Preparation: Euthanize the pregnant SPF donor mouse at the appropriate gestational stage (e.g., day 18.5) using an approved method (e.g., cervical dislocation). Saturate the abdomen with disinfectant (e.g., Clidox-S). Pre-heat the interior of the germ-free isolator to 40–45°C using a heating pad to prevent pup hypothermia [8].
- Exteriorization: Make a midline laparotomy incision through the skin and abdominal wall to expose the uterine horns.
- T-CS Uterine Extraction: Place clamps at the cervix base and the top of each uterine horn. Excise the entire uterus between the clamps [8].
- Disinfection & Transfer: Immediately immerse the excised uterus in a fresh, activated disinfectant solution (e.g., Clidox-S) for a predetermined time to achieve surface sterility. Rapidly transfer the disinfected uterus into the germ-free isolator via a sterile liquid transfer port.
- Pup Extraction & Resuscitation: Inside the isolator, use sterile surgical scissors to incise the uterine wall and amniotic sac to expose each pup. Use a sterile cotton swab to gently wipe away amniotic fluid from the pup's nose and mouth until spontaneous breathing is noted. Cut the umbilical cord [8].
- Fostering: Immediately place the revived pups with a pre-conditioned GF foster mother that has recently given birth (within 1-3 days) to ensure acceptance and nursing.
Protocol B: Female Reproductive Tract Preserved C-section (FRT-CS)
Objective: To aseptically derive germ-free mouse pups with improved survival by preserving the integrity of the female reproductive tract during the C-section. Reagents & Equipment: As per Protocol A. Procedure:
- Steps 1-2: Identical to Protocol A (Preparation and Exteriorization).
- FRT-CS Uterine Extraction: Identify the cervix base. Place a clamp only at the cervix base, leaving the uterine horns, uterine junctions, and ovaries unclamped and intact. Carefully excise the reproductive tract above the single clamp [8].
- Steps 4-6: Identical to Protocol A (Disinfection, Transfer, Pup Extraction, Resuscitation, and Fostering). The entire procedure, from euthanization to pup transfer into the isolator, must be completed within 5 minutes to ensure pup viability and sterility [8].
Workflow and Pathway Diagrams
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents and Materials for Cesarean Derivation of GF Mice
| Item | Function/Application in Protocol | Brief Explanation |
|---|---|---|
| Clidox-S | Surface disinfection of the excised uterus. | A chlorine dioxide-based disinfectant used to sterilize the exterior of the uterine sac before transfer into the germ-free isolator, preventing contamination [8]. |
| Germ-Free Isolator | Housing and procedural environment. | A polyvinyl chloride (PVC) isolator providing a sterile barrier environment for performing pup extraction, resuscitation, and housing GF mice [8]. |
| SPF Donor Mice | Source of embryos for derivation. | Specific Pathogen-Free mice (e.g., C57BL/6, BALB/c) serve as donors to ensure the derived GF mice are free from specified pathogens from the outset. |
| GF Foster Mothers | Care and nutrition of derived pups. | Lactating GF females (e.g., BALB/c or NSG strains are superior) that provide maternal care and milk, crucial for the survival and weaning of C-section-derived pups [8]. |
| Sterile Surgical Tools | Performing the C-section and pup extraction. | Autoclaved instruments (scissors, forceps, clamps) for aseptic surgery both outside and inside the germ-free isolator. |
| Bifidobacterium breve / Prebiotics | Research intervention for microbiome restoration. | Probiotic strain or prebiotic mixture used in research to partially reverse C-section-induced behavioral deficits by modulating the gut microbiota [10]. |
| Furagin | Furagin, CAS:1672-88-4, MF:C10H8N4O5, MW:264.19 g/mol | Chemical Reagent |
| Lactenocin | Lactenocin | Lactenocin is a bacteriocin for research use only (RUO). Explore its applications in fighting drug-resistant bacteria and food biopreservation. |
The 'Sterile Womb Hypothesis' and Its Surgical Implications
The 'Sterile Womb Hypothesis' has been a foundational paradigm in reproductive biology, positing that the fetus develops in a sterile intrauterine environment and initial microbial colonization occurs during and after birth [8] [11]. This concept directly informs surgical practices in obstetrics, particularly cesarean section (C-section) techniques, which have been designed to maintain this sterility. However, emerging research challenges this dogma, suggesting the healthy fetal environment may harbor low levels of bacteria or their components prior to birth [12]. This evolution in understanding carries profound implications for refining surgical protocols, including the developing Female Reproductive Tract preserved C-section (FRT-CS) technique, which aims to optimize neonatal outcomes by potentially preserving early microbial exposure [8]. This Application Note synthesizes current evidence on the sterile womb debate and provides detailed experimental protocols for investigating microbial transmission within the context of surgical obstetric practices.
Current State of the Hypothesis: Evidence and Contention
The debate surrounding the sterile womb paradigm is characterized by contrasting findings, largely dependent on methodological rigor, particularly regarding contamination control in low-biomass sample analysis.
| Aspect | Evidence Supporting 'Sterile Womb' | Evidence Challenging 'Sterile Womb' |
|---|---|---|
| General Consensus | Historically accepted dogma; supported by ability to derive germ-free animals via C-section [11]. | Recent molecular studies suggest bacterial communities in placenta, amniotic fluid, and meconium [12] [11]. |
| Meconium Analysis | Early culture-based studies found majority (e.g., 62%) of meconium samples sterile [11]. | Bacterial DNA and SCFAs (acetate, propionate) detected in first-pass meconium [12]. |
| Placental & Amniotic Fluid Analysis | Placenta acts as barrier; bacterial presence associated with pregnancy complications/infection [11]. | Bacterial DNA profiles identified in amniotic fluid; microbiome distinct from contamination [12]. |
| Key Methodological Concern | Studies detecting bacteria often have insufficient controls for reagent/environmental contamination [11]. | Use of improved contamination controls (e.g., "mixome" removal) allows more sensitive profiling [12]. |
| Implication for Surgery | Supports traditional C-section goal of maintaining sterile environment until birth. | Suggests C-section techniques could be optimized to influence initial microbial exposure. |
Quantitative Evidence on Maternal-to-Neonatal Microbial Transmission
Recent clinical studies provide quantitative data on microbial transmission sources, which are crucial for evaluating the impact of surgical interventions.
Table 2: Maternal Source Contributions to Neonatal Gut Colonization (Source-Tracking Analysis) [13]
| Maternal Source | Contribution to Neonatal Meconium (Control Group) | Effect of Prenatal Probiotics |
|---|---|---|
| Maternal Gut | Major contributor, with input increasing over time. | Consistent, non-significant reduction in contribution. |
| Placenta | Major contributor to neonatal meconium colonization. | Significantly increased contribution (P=0.02). |
| Maternal Vagina | Minimal contribution throughout early neonatal period. | Consistent, non-significant reduction in contribution. |
| Overall Neonatal Microbiome | -- | Transiently altered composition; enhanced microbial stability Days 1-3 (P<0.001). |
This data demonstrates that the maternal gut and placenta are significant microbial sources for the neonate. Furthermore, prenatal probiotic supplementation can modulate these transmission patterns, notably increasing the placental contribution [13]. This interaction between maternal intervention and microbial source highlights a potential mechanism through which surgical and pre-surgical protocols could be designed to influence neonatal outcomes.
Experimental Protocols for Investigating Microbial Transmission
To advance research in this field, standardized protocols for sample collection and analysis are essential, especially within surgical settings like C-section.
Protocol: Sample Collection from Feto-Maternal Units during Cesarean Section
Application: To obtain sterile, high-quality samples for microbiomic analysis from mothers and neonates during elective C-section.
Materials & Reagents:
- Sterile nylon swabs (e.g., ESwab with Liquid Amies Medium)
- Sterile syringes and 20G needles
- Sterile surgical drapes, gloves, and instruments
- Sterile 50 mL centrifuge tubes and Eppendorf tubes
- Specimen freezing boxes and -80°C freezer
Procedure:
- Pre-operative Preparation: Perform C-section under standard aseptic conditions. The surgical site is scrubbed with alternating antiseptic solutions (e.g., 70% ethanol and 2% povidone iodine) [14].
- Intra-operative Collection:
- Placental Tissue: Within 10 minutes of delivery, rinse the fetal side with sterile saline. Remove the surface amniotic membrane and excise 4-6 blocks (approx. 1 cm³ each) of superficial placental tissue from different fetal-side regions using sterile scalpels. Immediately transfer to cryovials [13].
- Amniotic Fluid: From a closed amniotic sac, aspirate approximately 10 mL of fluid using a sterile syringe and needle [12]. Aliquot for DNA extraction (200 µL pellet) and other analyses.
- Endometrial Swab: Sample the placental attachment site on the endometrium using two sterile swabs—one for culture, one for molecular analysis [14].
- Neonatal Collection:
- Controls: Include environmental controls (e.g., swabs left open on the surgical tray) and no-template controls (sterile water) during DNA extraction and amplification [13] [12] [14].
- Storage: Immediately transport all samples on ice and store at -80°C until processing.
Protocol: Microbial Community Profiling using 16S rRNA Gene Sequencing
Application: To characterize and compare bacterial communities in low-biomass feto-maternal samples.
Materials & Reagents:
- DNA extraction kit (e.g., CTAB/SDS method)
- Phusion High-Fidelity PCR Master Mix
- Primers for 16S V3-V4 region: 341F (5'-CCTACGGGNGGCWGCAG-3') and 806R (5'-GGACTACHVGGGTWTCTAAT-3')
- Ion Plus Fragment Library Kit & Ion S5 XL sequencing platform
Procedure:
- DNA Extraction: Extract genomic DNA from all samples and controls using a standardized kit. Assess DNA purity and concentration via gel electrophoresis [13].
- 16S rRNA Gene Amplification: Amplify the hypervariable V3-V4 region via PCR (30 cycles). Include a no-template control to monitor for contamination [13].
- Library Preparation & Sequencing: Purify PCR products, construct libraries, and sequence on an appropriate platform (e.g., Ion S5 XL) [13].
- Bioinformatic Analysis:
- Process sequences to obtain clean tags and cluster into Operational Taxonomic Units (OTUs) at 97% similarity.
- Perform taxonomic annotation using a reference database (e.g., Silva).
- Conduct diversity analyses (alpha/beta diversity) and source-tracking analysis using tools like the FEAST algorithm to estimate maternal contributions to the neonatal microbiome [13].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Feto-Maternal Microbiome Studies
| Reagent / Kit | Function | Application Note |
|---|---|---|
| Liquid Amies Medium ESwab | Preservation of bacterial viability for culture-dependent analysis. | Crucial for comparing culture results with DNA-based molecular findings [14]. |
| CTAB/SDS DNA Extraction Method | Lysis and purification of genomic DNA from diverse sample types. | Effective for difficult-to-lyse gram-positive bacteria often present in low-biomass samples [13]. |
| Phusion High-Fidelity PCR Master Mix | High-fidelity amplification of the 16S rRNA gene target. | Reduces PCR errors in community analysis [13]. |
| PacBio SMRT Cell Technology | Full-length 16S rRNA gene sequencing. | Provides higher taxonomic resolution compared to short-read sequencing [12]. |
| FEAST Algorithm | Computational source-tracking for microbial communities. | Quantifies the contribution of maternal sources (gut, placenta, vagina) to the neonatal microbiome [13]. |
| Clidox-S Disinfectant | Sterilization of tissue samples and the sterile isolator environment. | Used in germ-free animal research following C-section derivation [8]. |
| I-BRD9 | I-BRD9, MF:C22H22F3N3O3S2, MW:497.6 g/mol | Chemical Reagent |
| Furmecyclox | Furmecyclox, CAS:60568-05-0, MF:C14H21NO3, MW:251.32 g/mol | Chemical Reagent |
Surgical Implications and the FRT-CS Protocol
The evolving understanding of the "sterile womb" directly informs the development of advanced surgical techniques like the Female Reproductive Tract preserved C-section (FRT-CS).
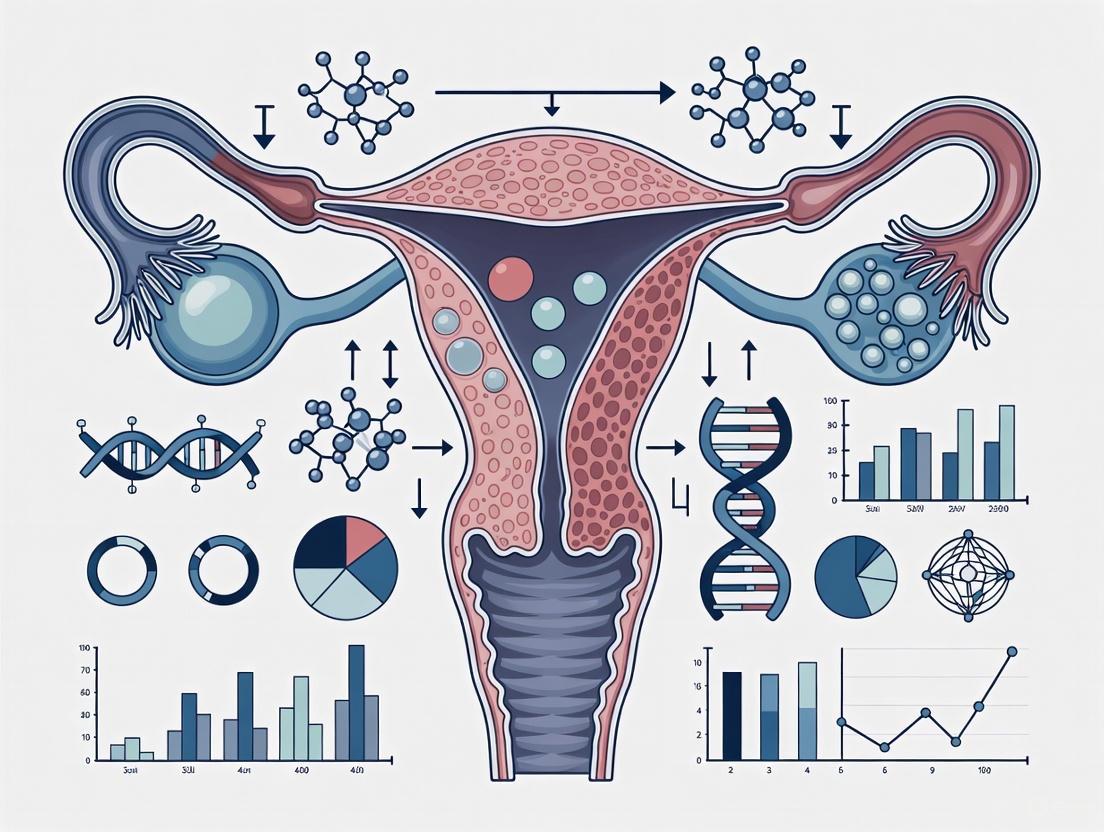
Diagram 1: FRT-CS protocol workflow and rationale. The surgical decision pathway compares the FRT-CS technique with traditional C-section, driven by the reevaluation of the Sterile Womb Hypothesis. FRT-CS aims to improve fetal survival and may influence microbial exposure [8].
The core principle of FRT-CS is the preservation of the entire female reproductive tract during fetal extraction, contrasting with traditional techniques that may involve more extensive clamping [8]. This optimization has been shown to significantly improve fetal survival rates in animal models, a critical outcome in germ-free mouse production and potentially translatable to human obstetric practice [8]. The rationale for exploring such techniques is intrinsically linked to the ongoing reevaluation of the sterile womb. If in utero microbial exposure is confirmed and its importance established, surgical protocols may be refined not just for safety, but to actively modulate this initial colonization event.
The 'Sterile Womb Hypothesis' remains a contested area of science, with significant implications for surgical obstetrics. While definitive proof of a consistent and viable in utero microbiome in healthy pregnancies is still lacking, evidence confirms that maternal microbial sources (gut, placenta) significantly influence the neonatal microbiome at birth. The development of the FRT-CS protocol represents a forward-looking surgical innovation that acknowledges this complex interplay. Future research must employ stringent contamination-controlled protocols to definitively characterize the fetal environment. This will enable the development of evidence-based, refined C-section techniques and associated interventions—such as prenatal probiotic supplementation—that optimize not only immediate surgical outcomes but also the long-term health of the neonate by influencing the foundational stages of microbial colonization.
Defining the Female Reproductive Tract-Preserved C-Section (FRT-CS) Technique
The Female Reproductive Tract-Preserved Cesarean Section (FRT-CS) represents a refined surgical technique developed to enhance germ-free (GF) mouse production efficiency. This protocol is situated within a broader research thesis aiming to optimize rederivation methods for biomedical research, where the generation of GF animal models is paramount for studying host-microbiome interactions [8]. Traditional cesarean section (T-CS) techniques involve clamping at both the cervix base and the top of the uterine horn, which causes more extensive tissue disruption. In contrast, the FRT-CS technique selectively clamps only at the cervix base, thereby preserving the anatomical and functional integrity of the entire female reproductive tract, including the ovary, uterine horn, uterine junction, and cervix [8]. This preservation is hypothesized to improve fetal survival rates by minimizing surgical trauma and maintaining a more physiological environment for the pups during the critical derivation process, without compromising sterility—a cornerstone principle in GF mouse production based on the "sterile womb hypothesis" [8].
Comparative Performance Data of FRT-CS vs. Traditional C-Section
The following table summarizes quantitative data comparing the FRT-CS technique against the traditional C-section (T-CS) approach, based on experimental findings from 80 pregnant SPF mice (40 C57BL/6 and 40 BALB/c) equally divided between the two groups [8].
Table 1: Comparative Outcomes of FRT-CS versus Traditional C-Section in Germ-Free Mouse Production
| Performance Metric | FRT-CS Technique | Traditional C-Section (T-CS) |
|---|---|---|
| Fetal Survival Rate | Significantly improved [8] | Lower than FRT-CS [8] |
| Sterility Maintenance | Maintained [8] | Maintained [8] |
| Reproductive Tract Preservation | Complete (ovary, uterine horn, uterine junction, cervix) [8] | Not preserved [8] |
| Surgical Clamping Points | Cervix base only [8] | Cervix base and top of uterine horn [8] |
Beyond the metrics in Table 1, the integration of In Vitro Fertilization (IVF) with FRT-CS has demonstrated significant advantages over using naturally mated (NM) donors. IVF allows for precise synchronization of donor delivery dates, thereby enhancing experimental reproducibility and planning efficiency. This controlled timing enables the scheduling of pre-labor FRT-CS, which is associated with higher pup survival compared to procedures performed after natural labor has begun [8].
Detailed FRT-CS Experimental Protocol
Pre-Surgical Preparation
- Isolator Setup: All procedures must be performed within a polyvinyl chloride (PVC) sterile isolator. Activate a heating pad inside the isolator, setting it to 40–45°C for at least 15 minutes prior to surgery to prevent pup hypothermia [8].
- Disinfectant Preparation: Prepare a chlorine dioxide disinfectant (e.g., Clidox-S) using a 1:3:1 dilution and activate for 15 minutes before use [8].
- Sterile Supplies: All surgical instruments, bedding, food, and water must be autoclaved at 121°C for a minimum of 1200 seconds (20 minutes) prior to introduction into the isolator [8].
- Donor Euthanasia: Euthanize the pregnant SPF donor female via cervical dislocation immediately before the C-section procedure [8].
Surgical Procedure: Step-by-Step Workflow
The core FRT-CS procedure is conducted under strict aseptic conditions and must be completed within a 5-minute window to ensure both sterility and pup viability [8].
- Abdominotomy and Uterine Exposure: Make a midline abdominal incision to access and expose the uterine horns.
- Selective Clamping: Place a clamp only at the cervix base, deliberately avoiding any clamping at the top of the uterine horn. This is the definitive step that distinguishes FRT-CS from T-CS and ensures preservation of the reproductive tract [8].
- Uterine Excision: Carefully excise the entire uterus.
- Disinfection Transfer: Immediately transfer the excised uterus into the sterile isolator and submerge it in the prepared chlorine dioxide disinfectant (e.g., Clidox-S) for thorough surface sterilization [8].
- Pup Extraction: Inside the isolator, incise the uterine sac with sterile surgical scissors. Gently peel back the amniotic membrane to expose the pup.
- Umbilical Cord Severance: Cut the umbilical cord using sterile instruments.
- Neonatal Resuscitation: Use a sterile cotton swab to gently wipe away amniotic fluid from the pup's airways until spontaneous breathing is noted [8].
Diagram 1: FRT-CS protocol workflow. The key preservation step is highlighted in green, and the final transfer to a foster mother is indicated in red.
Post-Surgical Pup Management and Foster Strain Selection
Following the C-section, the viable GF pups must be transferred to a lactating GF foster mother. The choice of foster strain is a critical factor influencing weaning success. Experimental evidence indicates significant variation in maternal care capabilities among different GF strains:
Table 2: Germ-Free Foster Mother Strain Performance Assessment
| Foster Mother Strain | Weaning Success & Maternal Care Rating | Key Performance Notes |
|---|---|---|
| BALB/c | Superior [8] | Exhibits superior nursing and weaning success [8]. |
| NSG (NOD/SCID Il2rg–/–) | Superior [8] | Exhibits superior nursing and weaning success [8]. |
| KM (Kunming, Outbred) | Moderate | Adequate maternal care performance [8]. |
| C57BL/6J | Lowest [8] | Demonstrates the lowest weaning rate among assessed strains [8]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for FRT-CS Derivation
| Item | Specification / Function | Experimental Application |
|---|---|---|
| Chlorine Dioxide Disinfectant | Clidox-S (1:3:1 dilution), activated for 15 min [8]. | Surface sterilization of the excised uterus prior to entry into the sterile isolator. |
| Sterile Isolator | Polyvinyl chloride (PVC) isolator [8]. | Maintains a germ-free environment for surgery and pup housing. |
| Heating Pad | Set to 40-45°C [8]. | Prevents neonatal hypothermia during the surgical procedure inside the isolator. |
| Autoclave | 121°C for 1200 seconds [8]. | Sterilizes all surgical instruments, bedding, food, and water. |
| SPF Donor Mice | BALB/c, C57BL/6; confirmed pathogen-free [8]. | Source of embryos for germ-free derivation. |
| GF Foster Mice | BALB/c, NSG, KM, C57BL/6J strains [8]. | Provide postnatal care and nursing for derived GF pups. |
| Lagunamycin | Lagunamycin, CAS:150693-65-5, MF:C19H21N3O4, MW:355.4 g/mol | Chemical Reagent |
| IFN alpha-IFNAR-IN-1 | IFN alpha-IFNAR-IN-1, MF:C18H17NS, MW:279.4 g/mol | Chemical Reagent |
Integrated Strategy for Enhanced Germ-Free Mouse Production
The successful implementation of the FRT-CS technique can be significantly augmented by integrating it with strategic decisions regarding donor conception method and foster mother selection. The following diagram illustrates this comprehensive, optimized workflow for maximizing the efficiency of GF mouse production.
Diagram 2: An integrated strategy for germ-free mouse production. Green nodes and paths indicate optimal choices (IVF, FRT-CS, BALB/c or NSG foster mothers), while red nodes indicate suboptimal choices that can reduce efficiency. This holistic approach combines optimized techniques to maximize success.
This document provides detailed application notes and experimental protocols for the Female Reproductive Tract Preserved Cesarean Section (FRT-CS) technique, framed within a broader thesis research context. The primary objective of these protocols is to enhance the efficiency of germ-free (GF) mouse production by refining sterile cesarean section techniques, optimizing donor selection strategies, and identifying the most suitable GF foster strains [8]. The core principle of FRT-CS is the anatomical preservation of the donor's reproductive tract during surgery, which has been shown to significantly improve fetal survival rates while maintaining sterility, thereby providing a robust model for reproductive and developmental biology research [8]. These protocols are designed for researchers, scientists, and drug development professionals working in the fields of microbiome research, reproductive science, and animal model generation.
The following tables consolidate key quantitative findings from the optimization of germ-free mouse production, highlighting the impact of surgical techniques, donor sources, and foster mother selection.
Table 1: Impact of Cesarean Section Technique on Fetal Survival [8]
| Surgical Technique | Donor Strain | Key Surgical Difference | Fetal Survival Outcome |
|---|---|---|---|
| Traditional C-section (T-CS) | C57 & BALB/c (40 mice each) | Clamps placed at cervix base and top of uterine horn | Lower fetal survival rate |
| Female Reproductive Tract Preserved C-section (FRT-CS) | C57 & BALB/c (40 mice each) | Selective clamping only at cervix base, preserving entire reproductive tract | Significantly improved fetal survival rate |
Table 2: Comparison of Donor Mouse Source for C-Section [8]
| Donor Source | Delivery Timing | Experimental Reproducibility | Contamination Rate |
|---|---|---|---|
| Natural Mating (NM) | Variable, less predictable | Lower due to timing variability | Comparable, maintained sterility |
| In Vitro Fertilization (IVF) | Precise control over predicted delivery date | Enhanced via precise date control | Comparable, maintained sterility |
Table 3: Evaluation of GF Foster Mother Strains for Weaning Success [8]
| Foster Mother Strain | Strain Type | Maternal Care Performance | Weaning Success |
|---|---|---|---|
| BALB/c | Inbred | Superior nursing capabilities | High |
| NSG | Inbred | Superior nursing capabilities | High |
| KM | Outbred | Moderate maternal care | Moderate |
| C57BL/6J | Inbred | Lowest maternal care in GF state; contrast to SPF findings | Lowest weaning rate |
Experimental Protocols
Protocol: Female Reproductive Tract Preserved Cesarean Section (FRT-CS)
This protocol describes the aseptic surgical technique for deriving germ-free pups while preserving the donor's reproductive anatomy.
3.1.1 Pre-operative Preparations
- Isolator Preparation: Sterilize the polyvinyl chloride (PVC) isolator using chlorine dioxide (e.g., Clidox-S in a 1:3:1 dilution, activated for 15 minutes). Pre-heat the interior with a heating pad to 40–45°C for at least 15 minutes prior to surgery to prevent pup hypothermia [8].
- Materials Sterilization: Autoclave all life supplements (food, water, bedding) and surgical instruments at 121°C for 1200 seconds [8].
- Donor Animal: Use a timed-pregnant SPF donor mouse. Euthanize via cervical dislocation immediately before the procedure [8].
3.1.2 Surgical Procedure
- Aseptic Setup: Perform all steps under strict aseptic conditions. The entire procedure from euthanasia to pup transfer must be completed within 5 minutes to ensure sterility and pup viability [8].
- Reproductive Tract Exposure: Make a midline incision to expose the gravid uterus.
- FRT-CS Clamping: Instead of clamping both the cervix and the top of the uterine horn (as in T-CS), selectively clamp only the base of the cervix. This preserves the integrity of the entire reproductive tract, including the ovary, uterine horn, uterine junction, and cervix [8].
- Uterine Sac Transfer: Excise the uterine horns and immediately transfer them into the sterile isolator chamber containing disinfectant [8].
3.1.3 Pup Derivation and Resuscitation Inside Isolator
- Amniotic Membrane Incision: Carefully incise the amniotic membrane using sterile surgical scissors to expose the pup [8].
- Umbilical Cord Cutting: Sever the umbilical cord.
- Stimulation for Breathing: Wipe the pup with a sterile cotton swab to remove amniotic fluid until spontaneous breathing is noted [8].
- Foster Introduction: Immediately introduce the resuscitated pups to a pre-conditioned GF foster mother [8].
Protocol: In Vitro Fertilization (IVF) for Timed Donor Generation
This protocol supports the FRT-CS workflow by providing precisely timed pregnant donors.
3.2.1 Embryo Production
- Superovulation: Hormonally prime SPF donor females (e.g., C57BL/6) to induce superovulation.
- Fertilization: Collect oocytes and fertilize them in vitro with sperm from males of the desired strain.
- Culture: Culture embryos to the two-cell stage [8].
3.2.2 Embryo Transfer and Timing
- Recipient Preparation: Transfer two-cell stage embryos into the uterus of a pseudo-pregnant recipient female (e.g., SPF CD-1 strain) [8].
- Date Designation: Designate the day of embryo implantation as embryonic day 0.5 (E0.5) [8].
- Scheduling: Schedule the FRT-CS procedure for the predicted delivery date, typically around E19.5, based on the strain used.
Protocol: Evaluation and Selection of Germ-Free Foster Mothers
This protocol outlines the criteria for selecting optimal GF foster strains to maximize pup survival post-derivation.
3.3.1 Strain Selection and Preparation
- Strain Choice: Prioritize GF BALB/c and NSG strains as foster mothers based on their superior weaning success. Avoid using GF C57BL/6J females as fosters due to their documented poor performance [8].
- Foster Conditioning: Select foster mothers that are approximately four months old and have successfully given birth and weaned a litter at least once previously [8].
- Mating with Vasectomized Males: Mate GF foster females with pre-vasectomized GF males to ensure they are in a synchronous pseudo-pregnant state, which promotes maternal instinct and milk production [8].
3.3.2 Pup Transfer and Monitoring
- Introduction of Pups: Gently transfer the derived GF pups to the foster mother's nest.
- Monitoring: Monitor the nest daily for signs of active nursing, pup retrieval, and lack of cannibalism.
- Weaning Record: Record the number of pups successfully weaned at 21 days of age to calculate the weaning rate for each foster strain.
Workflow and Signaling Diagrams
Diagram Title: Germ-Free Mouse Production via FRT-CS Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Reagents for FRT-CS Protocol
| Item Name | Function/Application | Specifications/Notes |
|---|---|---|
| Chlorine Dioxide (Clidox-S) | Sterilizing isolator interior and disinfecting tissue samples | Use 1:3:1 dilution, activate for 15 min before use [8] |
| Polyvinyl Chloride (PVC) Isolator | Primary sterile housing for derived pups and GF foster mothers | Requires integrated heating pad to maintain 40-45°C for pup hypothermia prevention [8] |
| SPF Donor Mice (e.g., BALB/c, C57) | Source of embryos/pups for GF derivation | Confirmed free of specific pathogens listed in standard guidelines [8] |
| GF Foster Strains (BALB/c, NSG) | Nursing and weaning of derived GF pups | Select 4-month-old, previously fertile females; avoid C57BL/6J fosters [8] |
| Autoclave | Sterilization of all supplies | Standard cycle: 121°C for 1200 seconds for food, water, bedding, instruments [8] |
| (Z)-Lanoconazole | (Z)-Lanoconazole, CAS:101530-10-3, MF:C14H10ClN3S2, MW:319.8 g/mol | Chemical Reagent |
| Lanomycin | Lanomycin, CAS:141363-91-9, MF:C17H27NO4, MW:309.4 g/mol | Chemical Reagent |
Step-by-Step Protocol: Implementing the FRT-CS Technique in the Laboratory
Pre-surgical preparation is a critical determinant of success in surgical research, particularly in studies involving the female reproductive tract such as preserved C-section protocols. The integrity of experimental data and the validity of surgical outcomes are contingent upon rigorous aseptic technique, proper sterilization of instruments, and the correct setup of the surgical isolator environment. Adherence to evidence-based guidelines from organizations like the Association of periOperative Registered Nurses (AORN) and the Centers for Disease Control and Prevention (CDC) provides the foundation for reproducible and contamination-free surgical procedures [15] [16]. This document outlines detailed application notes and protocols for establishing a controlled surgical research environment, with specific consideration for studies involving C-section procedures and female reproductive tract research.
Core Principles of Sterilization and Processing
Sterilization in a research context requires a comprehensive program that ensures operator competence and proper methods for cleaning instruments, packaging, loading sterilizers, and monitoring the entire process [15]. The goal is to provide sterile products while preserving the value and function of delicate research instruments.
Sterilization Cycle Verification
A sterilization process must be verified before implementation. All steam and low-temperature sterilizers should be tested with biological and chemical indicators upon installation, after major repairs, and periodically for ongoing quality assurance [15]. For prevacuum steam sterilizers, three consecutive empty cycles are run with a Bowie-Dick test to detect air removal problems. The sterilizer should not be used until all biological indicators are negative and chemical indicators show a correct end-point response [15].
Table 1: Sterilization Cycle Verification Protocol
| Verification Type | Frequency | Method | Acceptance Criteria |
|---|---|---|---|
| Initial Qualification | Upon installation, relocation, or major repair | Three consecutive empty cycles with biological and chemical indicators | All biological indicators negative; chemical indicators show correct endpoint [15] |
| Bowie-Dick Test | For prevacuum steam sterilizers during initial qualification | Single cycle with Bowie-Dick test sheet | Uniform color change on test sheet [15] |
| Routine Monitoring | According to manufacturer's IFU and policy | Physical monitors, chemical indicators, biological indicators | Parameters met; chemical indicators passed; biological indicators negative [16] |
| Process Change Qualification | When changing packaging, wraps, or load configuration | Three consecutive cycles with test packs in a full load | All biological indicators negative; items quarantined until results known [15] |
Cleaning and Decontamination
Effective sterilization mandates thorough cleaning to reduce bioburden and remove organic residue that can act as a barrier to the sterilization agent [15]. Surgical instruments should be presoaked or prerinsed to prevent drying of biological material. Several methods facilitate cleaning:
- Mechanical cleaning: Ultrasonic cleaners, washer-sterilizers, and washer-disinfectors can improve effectiveness and decrease researcher exposure to biohazards [15].
- Manual cleaning: Delicate and intricate research instruments may require careful hand cleaning [15].
- Personnel protection: Researchers in the decontamination area should wear household-cleaning-type rubber or plastic gloves, with face masks, eye protection, and gowns when exposure may occur during manual cleaning [15].
Packaging and Loading
Instruments requiring sterilization must be wrapped or placed in rigid containers according to professional guidelines such as those from AAMI [15]. Key principles include:
- Packaging Materials: Must allow sterilant penetration, provide protection against contact contamination, and maintain sterility after processing. Options include sterilization wraps, peel-open pouches, and rigid containers [15].
- Preparation: Hinged instruments should be opened, and items with removable parts should be disassembled. Device manufacturer's instructions should be followed for complex instruments [15].
- Loading: Arranged to allow free circulation of the sterilant. Perforated trays should be placed parallel to the shelf, while basins should be placed on their edge [15].
Facility Design and Environmental Controls
The physical layout for processing research instruments is critical for containing contamination. The central processing area should ideally be divided into at least three distinct areas with physical barriers [15]:
- Decontamination Area: For receiving, sorting, and decontaminating contaminated supplies. This area should have negative pressure and a minimum of 6-10 air exchanges per hour to contain contaminants [15].
- Packaging Area: For inspecting, assembling, and packaging clean, but not sterile, materials.
- Sterilization and Storage Area: A limited-access area with controlled temperature (up to 75°F) and relative humidity (not exceeding 70%) [15].
For smaller research settings, a conditional one-room design is acceptable. In this configuration, a physical separation of at least four feet must be maintained between the instrument-washing sink and the clean preparation area, achievable via a separating wall or screen [17].
Updated Sterilization Guidelines and Research Applications
AORN's updated sterilization guidelines include several key areas relevant to surgical research [16] [17]:
- Short-Cycle Sterilization: Defined for packaged items with a reduced dry-cycle time, suitable for storage. This is distinct from Immediate Use Steam Sterilization (IUSS). If the drying time is shortened, the research organization must perform verification testing to demonstrate that the abbreviated time produces dry packages, unless specified in the manufacturer's Instructions for Use (IFU) [17].
- Water Quality: Monitoring water used in steam generators and boilers is essential to ensure steam quality and purity, aligning with ANSI/AAMI ST108 standards [16].
- 3D-Printed/Experimental Devices: For custom or experimental devices manufactured onsite without FDA-cleared sterilization instructions, the facility must establish a validated process. This often requires resources and expertise beyond typical healthcare facilities [17].
Experimental Protocol: Sterilization Setup for C-Section Research
The following protocol details the setup for sterilizing instruments for a preserved C-section procedure in a research setting.
Pre-Sterilization Phase
Objective: To ensure all instruments are thoroughly cleaned and prepared for sterilization. Materials: Enzymatic cleaner, ultrasonic cleaner, personal protective equipment (PPE), deionized water, soft-bristled brushes, lint-free cloths. Procedure:
- Point-of-Use Precleaning: Immediately after the surgical procedure, immerse instruments in a dedicated container with enzymatic cleaner and a lid to prevent drying of biological material [15].
- Transport: Secure the container and transport it to the decontamination area.
- Manual Cleaning: Don appropriate PPE. Disassemble all instruments with removable parts. Brush and flush all surfaces under water to remove all visible soil, paying attention to grooves and joints [15].
- Inspection: Visually inspect each instrument under magnification for residual debris or damage. One study found that while 91% of instruments were clean visually, 84% had residual debris when examined microscopically [15].
- Drying: Dry instruments thoroughly with lint-free cloths before packaging.
Packaging and Loading
Objective: To package instruments to maintain sterility until point of use. Materials: Sterilization wraps (e.g., non-woven), peel pouches, rigid containers, chemical indicators. Procedure:
- Selection: Choose packaging compatible with the sterilization method (e.g., avoid linens and paper for hydrogen peroxide gas plasma) [15].
- Preparation: Open all hinged instruments. Place delicate instruments in a protected location within the tray. Add an internal chemical indicator to the package or tray [15].
- Wrapping: Use a sequential double-wrap technique (two separate wraps) or a non-sequential technique (two sheets simultaneously) to create a package within a package [15].
- Loading the Sterilizer: Place perforated trays so they are parallel to the shelf. Position basins and containers on their edge. Place peel pouches on edge in mesh-bottom racks. Ensure packs do not touch the chamber walls [15].
Sterilization Cycle and Monitoring
Objective: To achieve sterility and verify the process. Materials: Steam sterilizer, chemical indicators, biological indicators. Procedure:
- Cycle Selection: Select the appropriate cycle based on the device manufacturer's IFU and load contents. For heat-stable, non-porous items, a gravity-displacement or dynamic-air-removal steam cycle is typically used [15].
- Monitoring: Place an external chemical indicator on the outside of each pack. For routine monitoring, place a biological indicator (e.g., Geobacillus stearothermophilus for steam) in a test pack and process with the load [15] [16].
- Release: Do not use items processed during a cycle with a positive biological indicator. Quarantine items from evaluation cycles until test results are negative [15].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Surgical Research Sterilization
| Item | Function/Application | Research Considerations |
|---|---|---|
| Enzymatic Cleaner | Breaks down proteinaceous and carbohydrate biological soils (e.g., blood, tissue) from instruments [15]. | Choose a low-foaming formula compatible with ultrasonic cleaners and automated washers. |
| Biological Indicators (BIs) | Contains bacterial spores to provide a direct challenge to the sterilization process, verifying lethality [15]. | Use species specific to the sterilization method. Maintain a log of lot numbers and incubation results for regulatory compliance. |
| Chemical Indicators | Undergo a chemical or physical change in response to one or more sterilization parameters (e.g., temperature, steam) [15]. | Use multi-parameter indicators for highest assurance. Place both inside and outside of instrument packs. |
| Non-Woven Sterilization Wraps | Provides a barrier to microbial penetration while allowing sterilant penetration and removal [15]. | Reusable wraps require inspection for holes or tears. Single-use wraps reduce linting. |
| Rigid Sterilization Containers | Provides protection for delicate surgical instruments during handling and sterilization [15]. | Ensure filter and valve systems are compatible with the sterilization modality and are maintained per manufacturer's IFU. |
| Low-Temperature Sterilant (e.g., Hâ‚‚Oâ‚‚ gas plasma) | Sterilizes heat- and moisture-sensitive devices that cannot withstand steam sterilization [17]. | Adhere strictly to load weight limits and packaging requirements, as these significantly impact efficacy [17]. |
| Laromustine | Cloretazine (Laromustine) for Cancer Research | Cloretazine is a sulfonylhydrazine alkylating agent for oncology research. This product is for Research Use Only (RUO), not for human consumption. |
| Laurotetanine | Laurotetanine, CAS:128-76-7, MF:C19H21NO4, MW:327.4 g/mol | Chemical Reagent |
Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for pre-surgical preparation of research instruments, from decontamination to sterile storage.
Diagram 1: Instrument Processing Workflow for Research. This chart outlines the critical pathway for ensuring research instrument sterility, highlighting key decision points and quality control checks.
The pre-surgical preparation protocol is governed by a quality management system rather than a biochemical signaling pathway. The following diagram maps this control system, which is essential for maintaining aseptic integrity.
Diagram 2: Quality Control System for Sterilization. This diagram illustrates the feedback loop between process control, monitoring, and system adjustments that ensures consistent sterility assurance.
Within the broader research on refining the female reproductive tract-preserved cesarean section (FRT-CS) protocol for generating germ-free mice, the selection of donor mice is a critical initial step. The method used to obtain pregnant donors—either through natural mating (NM) or in vitro fertilization (IVF)—directly impacts the precision of predicting delivery dates. This precision is paramount for scheduling sterile C-sections effectively, thereby maximizing pup survival and the overall efficiency of germ-free mouse production [8]. This application note provides a detailed, data-driven comparison of these two donor selection strategies, offering protocols and analysis to guide researchers in aligning their choice with experimental goals that require high temporal accuracy.
Quantitative Comparison of NM and IVF
The choice between natural mating and IVF has significant implications for logistical planning and experimental reproducibility. The table below summarizes the key comparative data.
Table 1: Quantitative Comparison of Natural Mating and IVF for Donor Mouse Production
| Parameter | Natural Mating (NM) | In Vitro Fertilization (IVF) |
|---|---|---|
| Delivery Date Precision | Variable and less precise; requires monitoring from gestation day 18 (G18) onward [8] | High precision; enables pre-labor C-section on the predicted delivery date [8] |
| Method for Date Confirmation | Presence of a vaginal plug, recorded as Gestation Day 0.5 (G0.5) [8] | Implantation of two-cell stage embryos, recorded as Embryonic Day 0.5 (E0.5) [8] |
| Impact on Experimental Reproducibility | Lower, due to inherent variability in mating and birth timing [8] | Higher, due to precise control over the embryonic timeline [8] |
| Consideration of Genetic Fidelity | Not reported as a concern in the studied context. | Associated with a ~30% increase in single-nucleotide variants in mice; absolute risk of a harmful mutation remains very low [18] |
| Key Advantage | Does not require specialized reproductive technical skills. | Unlocks precise scheduling for FRT-CS and other time-sensitive procedures. |
| Key Limitation | Inefficient for scheduling, leading to potential resource idle time or missed deadlines. | Requires established expertise in assisted reproductive technologies. |
Detailed Experimental Protocols
Protocol for Donor Mice via Natural Mating
This protocol is suited for experiments where precise delivery timing is not the primary critical factor.
Materials:
- Sexually mature SPF female mice (e.g., C57BL/6)
- Proven stud male mice of the same strain
- Standard rodent housing equipment
Procedure:
- Mating Setup: House one male mouse with two female mice per cage.
- Plug Check: Check females each morning for the presence of a vaginal plug.
- Day 0.5 Designation: The day a plug is observed is designated as Gestation Day 0.5 (G0.5).
- Monitoring: Monitor pregnant donors for natural delivery from G18 onward if a C-section is planned before natural birth [8].
Protocol for Donor Mice via In Vitro Fertilization
IVF provides superior control over the embryonic timeline, which is essential for coordinating with scheduled FRT-CS.
Materials:
- Oocyte donors and sperm donors (e.g., C57BL/6J)
- Recipient females (e.g., CD-1) for embryo transfer
- Standard IVF reagents: Toyoda Yokoyama Hosi (TYH) medium, methyl-beta-cyclodextrin, polyvinyl alcohol (PVA) [19]
- Equipment for IVF and embryo transfer
Procedure:
- Sperm Collection and Preparation: Collect sperm from a sacrificed male. For enhanced fertility, consider sperm selection using a microfluidics chip cell sorter to minimize damage and select for high-viability sperm [19].
- Oocyte Collection: Harvest oocytes from superovulated female mice.
- Fertilization: Perform in vitro fertilization by co-incubating sperm and oocytes in a suitable medium like modified TYH.
- Embryo Culture: Culture the resulting embryos to the two-cell stage.
- Embryo Transfer: Surgically transfer two-cell stage embryos into the oviducts of a pseudopregnant recipient female.
- Day 0.5 Designation: The day of embryo transfer is designated as Embryonic Day 0.5 (E0.5).
- Scheduled C-section: Perform the FRT-CS on the predicted delivery date based on the established embryonic timeline [8].
Workflow Visualization
The following diagrams illustrate the logical sequence and key decision points for both donor selection strategies, highlighting the differences in timeline control.
Diagram 1: Donor mouse selection workflow. The decision point guides researchers toward the optimal method based on the need for delivery date precision, which is crucial for scheduling FRT-CS.
The Scientist's Toolkit: Key Reagent Solutions
The following table lists essential materials and reagents used in the featured IVF protocol and related reproductive technologies.
Table 2: Key Research Reagent Solutions for Mouse Assisted Reproduction
| Reagent / Material | Function / Application | Example / Note |
|---|---|---|
| TYH Medium | A modified Krebs-Ringer bicarbonate solution used for sperm pre-incubation and in vitro fertilization [19]. | Can be supplemented with methyl-beta-cyclodextrin and polyvinyl alcohol (PVA) for enhanced performance (cTYH) [19]. |
| Microfluidics Chip Cell Sorter | A gentle cell sorting technology used to select sperm with high viability and fertility based on parameters like forward and side scattered light or specific markers, minimizing mechanical damage [19]. | Superior to conventional flow cytometers for fragile sperm cells. Can be used to select acrosome-reacted sperm, which showed higher fertilization rates [19]. |
| FITC-labelled PNA | A fluorescent compound (FITC) conjugated to peanut agglutinin (PNA), used to label and sort sperm based on acrosome reaction status via flow cytometry [19]. | Sperm selected for being acrosome-reacted (AR-high) demonstrated higher fertilization rates in IVF [19]. |
| Wnt Inhibitor (IWP2) | A small molecule inhibitor that targets Wnt signaling pathways. | Treatment with IWP2 was shown to improve implantation rates and subsequent intrauterine development of IVF embryos in a mouse model, and ameliorate offspring metabolic abnormalities [20]. |
| Clidox-S | A chlorine dioxide disinfectant used for sterilizing tissue samples and disinfecting the sterile isolator environment in germ-free mouse production [8]. | Applied in a specific 1:3:1 dilution and activated for 15 minutes before use [8]. |
| Lavendustin C6 | Lavendustin C6, CAS:144676-04-0, MF:C20H25NO5, MW:359.4 g/mol | Chemical Reagent |
| Lefamulin | Lefamulin|Pleuromutilin Antibiotic for Research | Lefamulin (BC-3781) is a novel pleuromutilin antibiotic for research use only. It inhibits bacterial protein synthesis. RUO, not for human use. |
Within the context of developing the Female Reproductive Tract Preserved C-section (FRT-CS) protocol, a critical component involves the precise differentiation of its surgical steps from those of the Traditional C-section (T-CS). This document details the key procedural distinctions, supported by quantitative experimental data and structured protocols, to provide researchers and drug development professionals with a standardized framework for application in germ-free (GF) mouse production and related biomedical research. The optimized FRT-CS technique aims to enhance neonatal survival while maintaining sterility, a crucial factor for ensuring reproducibility in downstream studies involving microbiome, neurodevelopment, and therapeutic interventions [21].
Comparative Procedural Analysis: FRT-CS vs. T-CS
The fundamental distinction between the two techniques lies in the surgical approach to the reproductive tract. The following table summarizes the key differentiating steps and their impact on procedural outcomes, based on controlled experimental analysis [21].
Table 1: Key Step-by-Step Differentiation Between FRT-CS and T-CS Techniques
| Procedural Step | Female Reproductive Tract Preserved C-Section (FRT-CS) | Traditional C-Section (T-CS) | Impact on Experimental Outcomes |
|---|---|---|---|
| Clamping Method | Selective clamping only at the cervix base. | Clamping at both the cervix base and the top of the uterine horn. | Preserves the entire reproductive tract (ovary, uterine horn, uterine junction, cervix) for potential future fertility. |
| Tissue Preservation | Preserves the integrity of the entire female reproductive tract. | Involves removal of sections of the reproductive tract. | Reduces surgical trauma and may contribute to improved hormonal milieu post-procedure. |
| Fetal Extraction | Fetuses are delivered through the preserved reproductive tract. | Fetuses are extracted directly from the isolated section of the uterus. | The less invasive approach is correlated with higher fetal survival rates. |
| Quantified Outcome (Fetal Survival Rate) | Significantly improved fetal survival rates while maintaining sterility. | Lower fetal survival rates in comparative studies. | Enhances the efficiency of obtaining live, germ-free pups for research colonies. |
This optimized surgical method which preserves the female reproductive tract during cesarean section (FRT-CS), significantly improved fetal survival rates while maintaining sterility [21].
Experimental Protocol for FRT-CS in Germ-Free Mouse Production
The following detailed methodology is adapted for the derivation of germ-free mice from specific pathogen-free (SPF) donors, a critical procedure for establishing controlled animal models.
Pre-Procedural Preparations
- Animal Models: Utilize pregnant SPF donor female mice (e.g., C57BL/6J, BALB/c) at late gestation [21].
- Donor Conception: Precisely control delivery timing using either natural mating (NM) with vaginal plug confirmation or in vitro fertilization (IVF) with embryo transfer, designating the day as gestation day 0.5 (G0.5) [21].
- Germ-Free Foster Mothers: Select proven GF foster dams from strains with demonstrated high maternal care (e.g., BALB/c, NSG). House them in polyvinyl chloride (PVC) isolators [21].
- Isolator and Environment Setup: Assemble and sterilize the PVC isolator. Activate heating pads to 40–45°C for at least 15 minutes prior to the C-section to prevent pup hypothermia [21].
- Sterilization Solution: Prepare a chlorine dioxide disinfectant, such as Clidox-S, for sterilizing tissue samples and disinfecting the internal isolator environment [21].
Surgical Procedure: Key FRT-CS Steps
- Euthanasia: Euthanize the pregnant SPF donor female via cervical dislocation [21].
- Initial Incision: Perform a midline laparotomy to access the abdominal cavity under aseptic conditions.
- Uterine Exposure: Gently expose the uterine horns.
- Critical Clamping (FRT-CS Differentiation): Place a clamp selectively at the cervix base only, ensuring the ovaries, uterine horns, and uterine junctions remain unclamped and preserved [21].
- Tissue Dissection: Carefully dissect the reproductive tract, maintaining its integrity from the cervix.
- Disinfection and Transfer: Immediately transfer the entire intact reproductive tract containing the pups into a disinfection solution (e.g., Clidox-S) and then rapidly into the sterile isolator. The entire procedure from euthanasia to transfer must be completed within 5 minutes to ensure sterility and pup viability [21].
- Pup Extraction and Resuscitation: Inside the isolator, carefully incise the uterine sac to deliver each pup. Incise the amniotic membrane with surgical scissors, expose the pup, and cut the umbilical cord. Use a sterile cotton swab to wipe away amniotic fluid until spontaneous breathing is noted [21] [22].
- Fostering: Immediately transfer the resuscitated pups to the waiting GF foster mother.
- Post-procedural Monitoring: Monitor the foster dam and litter for nursing success, pup survival, and weaning rates.
Data Collection and Analysis
- Primary Outcome Measures: Record fetal survival rate (number of live pups obtained divided by total pups in the uterus) and sterility confirmation.
- Secondary Outcome Measures: Track weaning success and cross-foster the health and development of pups.
- Statistical Analysis: Compare survival rates between FRT-CS and T-CS groups using appropriate statistical tests, such as the chi-square test [21].
Workflow Visualization of FRT-CS Protocol
The following diagram illustrates the logical sequence and decision points in the FRT-CS protocol for deriving germ-free mice, integrating donor selection, the core surgical difference, and fostering.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for FRT-CS Protocol Implementation
| Item | Function/Application in Protocol |
|---|---|
| SPF Donor Mice (e.g., C57BL/6, BALB/c) | Source of embryos for deriving germ-free lines; ensure defined microbial status [21]. |
| Germ-Free Foster Dams (e.g., BALB/c, NSG, KM) | Provide maternal care and nursing for C-section-derived pups; strain selection critically impacts weaning success [21]. |
| Chlorine Dioxide Disinfectant (e.g., Clidox-S) | Sterilizing solution for disinfecting the exterior of the reproductive tract post-excision and the isolator environment [21]. |
| Polyvinyl Chloride (PVC) Isolator | Sterile, sealed environment for housing GF animals and performing pup extraction, preventing external contamination [21]. |
| Aspen Wood Shavings (Autoclaved) | Standardized, sterile bedding material for housing GF mice within isolators [21]. |
| Heating Pad | Maintains pup body temperature during the transfer and initial recovery phase, preventing hypothermia [21]. |
| Levamlodipine hydrochloride | Levamlodipine hydrochloride, CAS:865430-76-8, MF:C20H26Cl2N2O5, MW:445.3 g/mol |
| Lithooxazoline | Lithooxazoline, CAS:80724-92-1, MF:C28H47NO2, MW:429.7 g/mol |
This document details application notes and protocols for the aseptic resuscitation of newborn puppies and their subsequent transfer into a germ-free isolator. These procedures are a critical component of a broader research thesis investigating Female Reproductive Tract Preserved (FRTP) cesarean section (C-section) protocols. The primary objective is to enable the generation and maintenance of gnotobiotic canine models for advanced studies in immunology, microbiology, and drug development, while preserving the dam's reproductive potential for future breeding. The protocols herein integrate the first evidence- and consensus-based veterinary guidelines for newborn resuscitation with stringent aseptic techniques required for germ-free research.
Experimental Protocols
Pre-operative Preparation and Aseptic Field Establishment
Objective: To ensure all equipment, personnel, and the surgical environment are prepared to support the survival of the newborns and maintain a sterile field during the FRTP C-section and subsequent transfer.
Materials:
- Germ-free isolator (pre-sterilized and validated)
- Sterile transfer port or rapid transfer system
- Surgical suite with designated resuscitation station
- Personal protective equipment (PPE): sterile surgical gowns, gloves, masks, and bouffant caps
- Heating source (e.g., warm water circulation blanket, radiant warmer) with sterile blankets
- Laryngoscope with sterile blades (size 0-1)
- Sterile endotracheal tubes (1.0-3.0 mm)
- Sterile suction device with appropriate catheters
- Sterile syringes (1-3 mL) and needles (25-27 gauge)
- Emergency drug kit with pre-drawn, sterile, labeled syringes (see Table 3)
- Sterile timers
- Sterile surgical instrument pack for C-section
Methodology:
- Isolator Preparation: The germ-free isolator must be sterilized (e.g., using peracetic acid vapor) and its integrity validated at least 24 hours pre-operatively. The internal environment should be pre-warmed to 85-90°F (29.5-32°C) and contain sterile bedding.
- Resuscitation Station Setup: A dedicated area within the operating room should be prepared adjacent to, but separate from, the dam's surgical field. All resuscitation equipment must be arranged for single-use from sterile packages.
- Team Briefing: The surgical and research teams must review the roles, the resuscitation algorithm, and the transfer sequence to ensure a seamless and rapid workflow from uterus to isolator.
Female Reproductive Tract Preserved (FRTP) C-section Protocol
Objective: To deliver puppies via C-section while minimizing trauma and preserving the dam's uterine integrity and future fertility.
Methodology:
- Anesthesia and Monitoring: The dam is induced with a short-acting anesthetic protocol suitable for C-section. Standard monitoring (heart rate, respiration, SpO2) is maintained throughout.
- Surgical Approach: A standard midline or Pfannenstiel incision is made. The abdomen is opened carefully to expose the uterus.
- Uterine Incision and Extraction: A single, controlled incision is made in the uterine body, avoiding the placental sites. Each puppy, along with its placenta, is gently and rapidly delivered. The umbilical cord is clamped with sterile hemostats approximately 2-3 cm from the pup's abdomen and is cut distal to the clamp, leaving the clamp on the pup's side.
- Uterine Preservation: The uterus is closed with a continuous inverting suture pattern using absorbable suture material. The abdominal wall and skin are closed routinely. The focus of this protocol is on minimizing uterine manipulation and ensuring hemostasis to preserve fertility.
Objective: To support the puppy's transition to extrauterine life using a structured, iterative approach, from basic care to advanced life support, while maintaining asepsis [23] [24]. The following algorithm outlines the decision-making process and key interventions.
Workflow for Newborn Resuscitation
Methodology:
- Immediate Post-Delivery Care: The surgeon passes the clamped puppy and attached placenta to a dedicated assistant at the resuscitation station.
- Airway Clearance: The pup is dried vigorously with a sterile towel to stimulate breathing and reduce heat loss. The mouth and nares are gently suctioned with a sterile bulb syringe or suction catheter to clear amniotic fluid.
- Thermoregulation: The newborn is placed on a sterile, warm blanket with a heat source. Maintaining a core body temperature is critical, as hypothermia rapidly decreases heart rate and compromises resuscitation efforts.
- Assessment and Positive Pressure Ventilation (PPV):
- A vigorous puppy will cry, move actively, and have a heart rate (HR) > 200 beats per minute (bpm). This pup can proceed to transfer.
- A non-vigorous puppy (apneic, gasping, flaccid, HR < 200 bpm) requires immediate PPV.
- PPV Protocol: Using a sterile facemask or endotracheal tube connected to a flow-inflating bag or T-piece resuscitator, administer breaths at a Peak Inspiratory Pressure (PIP) of 20-25 cm Hâ‚‚O and a Positive End-Expiratory Pressure (PEEP) of 4-5 cm Hâ‚‚O [23]. The initial rate is 20-40 breaths per minute. The primary goal is to aerate the fluid-filled lungs, which is the foundation for circulatory transition.
- Advanced Resuscitation (CPR): If the HR remains below 150 bpm despite 30 seconds of effective PPV, chest compressions and pharmacology are initiated [23].
- Chest Compressions: Compress the chest to 1/3 of its width at a rate of 100-120 per minute. Coordinate compressions and ventilations in a 3:1 ratio.
- Vascular Access: The intraosseous (IO) route is preferred for drug administration in newborns. The most accessible site is the proximal femur.
- Drug Administration: See Table 3 for drug dosages and indications.
Aseptic Transfer into Germ-Free Isolator
Objective: To transfer the resuscitated, stable puppy into the germ-free isolator without introducing contaminants.
Methodology:
- Surface Decontamination: Once the puppy is stable (breathing spontaneously and with a sustained HR > 200 bpm), the exterior of the clamped umbilical cord is meticulously sprayed and wiped with a sterile, non-residual sporicidal agent (e.g., sterilant used for the isolator).
- Transfer Chamber Preparation: A sterile transfer port attached to the isolator is surface-sterilized.
- Execution of Transfer: The puppy is swiftly placed inside a pre-sterilized transfer container. The umbilical clamp must remain in place. The container is then immediately introduced into the isolator via the transfer port according to the manufacturer's protocol (e.g., dunk tank, rapid transfer system).
- Post-Transfer Procedures:
- Inside the Isolator: An assistant inside the isolator (using attached gloves) receives the puppy. The umbilical clamp is carefully removed. The pup is dried again with sterile towels and placed under a radiant warmer within the isolator.
- Monitoring: The pup is monitored continuously for thermoregulation, respiration, and urination.
Data Presentation
The following tables summarize key quantitative data from the RECOVER Newborn Resuscitation Guidelines, providing a reference for expected physiological parameters and intervention details [23].
Table 1: Physiological Parameters for Newborn Puppies
| Parameter | Normal / Target Value | Notes / Action Threshold |
|---|---|---|
| Heart Rate (HR) | > 200 bpm | < 150 bpm: Initiate chest compressions |
| Respiratory Rate (RR) | 10-20 breaths/min | Apnea or gasping: Initiate PPV |
| Body Temperature | 97-99°F (36-37°C) | Hypothermia directly compromises cardiac output |
| Time to First Breath | < 60 seconds | > 60 s: Requires tactile stimulation and/or PPV |
Table 2: Parameters for Positive Pressure Ventilation (PPV)
| Parameter | Recommended Setting | Rationale |
|---|---|---|
| Peak Inspiratory Pressure (PIP) | 20-25 cm Hâ‚‚O | Sufficient to aerate fluid-filled lungs |
| Positive End-Expiratory Pressure (PEEP) | 4-5 cm Hâ‚‚O | Helps establish functional residual capacity |
| Respiratory Rate | 20-40 breaths/min | Supports adequate minute ventilation initially |
| Inspiration Time | ~ 0.5 - 1 second | Allows for adequate lung inflation |
Table 3: Emergency Drug Dosing for Newborn Puppy CPR
| Drug | Concentration | Dose | Route | Indication |
|---|---|---|---|---|
| Epinephrine | 1:10,000 | 0.01 - 0.02 mg/kg | IO, IV | Asystole, HR < 150 bpm despite PPV/compressions |
| Dextrose | 50% | 0.5 - 1.0 g/kg (dilute to 10-25%) | IO, IV | Documented or suspected hypoglycemia |
| Naloxone | 0.4 mg/mL | 0.01 mg/kg | IO, IV, IM | To reverse opioid-induced respiratory depression |
| Fluid Bolus | 0.9% NaCl | 10 mL/kg | IO, IV | Suspected hypovolemia or shock |
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions and Materials
| Item | Function / Application in Protocol |
|---|---|
| Germ-Free Isolator | Provides a sterile physical barrier, creating and maintaining the germ-free environment for housing pups post-transfer. |
| Sterilant (e.g., Peracetic Acid) | Used for the decontamination of the isolator interior and the surface sterilization of materials entering via a transfer port. |
| Sterile Transfer Port / Rapid Transfer System (RTS) | The sealed entry point that allows for the introduction of materials and animals into the isolator without breaking sterility. |
| T-Piece Resuscitator (Neonatal) | Allows for precise, reproducible delivery of PPV with controllable PIP and PEEP, which is critical for lung aeration without causing volutrauma. |
| Intraosseous (IO) Catheter (22-25 gauge) | Provides reliable vascular access for drug and fluid administration when intravenous access is not feasible in a newborn puppy. |
| Sterile Umbilical Clamps | Used to ligate the umbilical cord post-delivery, preventing hemorrhage and serving as a sterile "handle" during the transfer process. |
| Flow-Inflating Anesthesia Bag | An alternative to a T-piece for providing PPV; requires more skill to maintain consistent pressure but is effective for experienced users. |
| Sterile Lube | Applied to the endotracheal tube to facilitate intubation and to the isolator gloves to maintain their integrity. |
| Lodenafil Carbonate | Lodenafil Carbonate|PDE5 Inhibitor|CAS 398507-55-6 |
| Loflucarban | Loflucarban, CAS:790-69-2, MF:C13H9Cl2FN2S, MW:315.2 g/mol |
Within the broader research on the Female Reproductive Tract Preserved Cesarean Section (FRT-CS) protocol, the selection of an optimal germ-free (GF) foster strain represents a critical determinant of post-procedural success. The FRT-CS technique significantly improves fetal survival rates by preserving the integrity of the donor's reproductive tract [21]. However, the ultimate yield of weaned GF pups is equally dependent on the maternal care capabilities and nursing efficiency of the GF foster mother. This document provides detailed application notes and protocols for the evidence-based selection of GF foster strains, leveraging quantitative experimental data to establish a standardized approach for post-procedure care in the derivation of germ-free mouse colonies.
Quantitative Comparison of GF Foster Strain Performance
The maternal performance of different GF foster strains was systematically evaluated in a controlled study. The following table summarizes the key quantitative findings, providing a basis for strain selection.
Table 1: Comparative Maternal Performance of Different GF Foster Strains
| GF Foster Strain | Weaning Rate (%) | Key Behavioral and Performance Characteristics |
|---|---|---|
| BALB/c | High | Exhibited superior nursing capabilities and weaning success [21]. |
| NSG (NOD/SCID Il2rg–/–) | High | Demonstrated superior nursing capabilities and weaning success [21]. |
| KM (Kunming, outbred) | Moderate | Performance was evaluated, but was surpassed by BALB/c and NSG strains [21]. |
| C57BL/6J | Lowest | Weaning rate was the lowest among all tested strains, a finding noted as being in stark contrast to the performance of Specific Pathogen-Free (SPF) C57BL/6J foster mothers [21]. |
Detailed Experimental Protocol for Foster Care Integration
This protocol follows the FRT-CS procedure for obtaining GF pups and details the subsequent steps for introducing them to the foster mother.
Materials and Reagents
Table 2: Essential Research Reagent Solutions for GF Foster Care
| Item Name | Function/Application | Specification/Notes |
|---|---|---|
| Polyvinyl Chloride (PVC) Isolator | Provides a sterile housing environment for GF mice. | Must be equipped with a heating system [21]. |
| Clidox-S | Chlorine dioxide disinfectant. | Used for sterilizing the exterior of the uterine sac and for general environmental disinfection [21]. |
| Aspen Wood Shavings | Bedding material. | Must be autoclaved before use to ensure sterility [21]. |
| Heating Pad | Prevents pup hypothermia. | Should be pre-heated to 40–45°C for at least 15 minutes prior to the C-section [21]. |
| Sterile Surgical Scissors & Forceps | For incising the amniotic membrane and handling pups. | Aseptic technique is critical [21]. |
| Sterile Cotton Swabs | For wiping amniotic fluid from pups to stimulate breathing. | - [21] |
Step-by-Step Procedure
Pre-Procedure Preparation:
- Isolator Setup: Ensure the PVC isolator is thoroughly sterilized. Activate the internal heating pad to maintain a warm environment (40-45°C) for the incoming pups [21].
- Foster Mother Selection: Based on the data in Table 1, select a proven high-performance strain such as BALB/c or NSG. The foster mother should be healthy, approximately four months old, and have successfully given birth and nursed a litter at least once previously. This ensures proven maternal competence [21].
Pup Derivation and Transfer:
- Perform the FRT-CS on the SPF donor female under deep anesthesia, preserving the entire reproductive tract [21].
- Rapidly transfer the intact uterine sac into the sterile isolator. The entire process from euthanizing the donor to transferring the uterus into the isolator must be completed within 5 minutes to ensure pup viability and sterility [21].
- Inside the isolator, carefully incise the amniotic membrane with sterile scissors to expose the pup.
- Gently wipe the pup's face and body with a sterile cotton swab to clear amniotic fluid until spontaneous breathing is noted.
- Cut the umbilical cord.
Foster Introduction and Weaning:
- Gently place the revived GF pups into the nest of the prepared GF foster mother.
- Monitor the foster mother's behavior for initial acceptance of the pups.
- House the mice under controlled environmental conditions: a 12-hour light/dark cycle, a constant temperature of 22 ± 2 °C, and a relative humidity of 55% with ad libitum access to autoclaved food and water [21].
- Monitor pup survival and growth daily. The weaning rate is a key success metric and should be recorded for each strain and litter.
Workflow Visualization: From C-Section to Weaning
The following diagram illustrates the complete experimental workflow, integrating the FRT-CS procedure with the foster care protocol detailed in this document.
The rigorous, data-driven selection of the GF foster strain is not an ancillary step but a fundamental component of the FRT-CS protocol. Empirical evidence clearly demonstrates that strain background directly impacts weaning success, with BALB/c and NSG strains exhibiting superior and more reliable maternal performance compared to C57BL/6J in a germ-free state. By adopting the standardized protocols and selection criteria outlined in this document, researchers can significantly enhance the efficiency and reproducibility of germ-free mouse production, thereby accelerating downstream research in microbiome science and host-pathogen interactions.
Enhancing Success: Addressing Common Challenges and Refining the FRT-CS Workflow
In the context of advanced reproductive research, particularly concerning Female Reproductive Tract Preserved C-section (FRTP-C) protocols, managing neonatal hypothermia is a critical determinant of offspring viability. Canine neonates are exceptionally vulnerable to heat loss due to their high surface-area-to-volume ratio, underdeveloped thermoregulation, and moist skin at birth. Inadvertent perioperative hypothermia, defined as a core body temperature below 36°C, is a frequent clinical complication associated with adverse outcomes including delayed drug metabolism, coagulopathy, and increased risk of mortality [25] [26]. Within the specific framework of FRTP-C research, where the integrity of the maternal reproductive tract is preserved, optimizing neonatal survival through rigorous thermal support is paramount. This document outlines evidence-based application notes and detailed protocols for pre-heating and perioperative thermal management to safeguard pup survival during and after cesarean section procedures.
Quantitative Data on Neonatal Risks
The following tables summarize key quantitative data on the risks associated with hypothermia and the corresponding target parameters for effective thermal management in neonates.
Table 1: Quantified Risks Associated with Neonatal Hypothermia and Related Factors
| Risk Factor | Quantitative Risk | Reference Timeframe |
|---|---|---|
| Hypothermia (Chilled Puppies) | Fourfold increased risk of death [27] | Perioperative |
| Low Birth Weight | 81% greater chance of death [27] | First 48 hours |
| APGAR Score below 7 | 22-fold increased risk of death [27] | First 8 hours after birth |
| Weight Loss >4% | Eightfold increased risk of death [27] | Neonatal period |
| Large Litter Size | Fourfold increased risk of neonatal death [27] | Neonatal period |
| Low Blood Glucose (<90) | Fourfold increased risk of death [27] | Perioperative |
Table 2: Target Parameters for Neonatal Thermal Management
| Parameter | Target | Notes |
|---|---|---|
| Puppy Rectal Temperature (1st 24 hrs) | 94°F to 96°F (34.4°C to 35.6°C) [27] | Measured with a well-lubricated digital thermometer. |
| Puppy Rectal Temperature (1st week) | 96°F to 98°F (35.6°C to 36.7°C) [27] | Increases ~1°F per week thereafter. |
| Environmental Surface Temperature | 90°F to 95°F (32°C to 35°C) [27] | For the first week of life. |
| Ambient Room Temperature | ~75°F (24°C) [27] | For the dam. |
| Ambient Room Humidity | 55% ±10% (45-65%) [27] | To prevent dehydration. |
Experimental Protocols for Thermal Management
Protocol 1: Preoperative Pre-Heating and Preparation
This protocol aims to minimize redistribution hypothermia, the initial rapid decrease in core temperature caused by anesthetic-induced vasodilation [25].
1. Equipment Preparation:
- Gather a forced-air warming (FAW) system, a carbon-fiber resistive heating mattress, or a convective warming device.
- Set up a pre-warmed whelping box with a heat lamp or heating pad set to maintain a surface temperature of 90–95°F (32–35°C). Ensure the heat source covers only part of the box, allowing pups to self-regulate.
- Pre-warm sterile surgical towels in a cabinet incubator set to 99–100°F (37–38°C).
2. Dam Pre-Heating:
- Initiation: Actively warm the dam for a minimum of 30 minutes prior to the induction of anesthesia.
- Method: Apply a forced-air warming blanket set to "high" (approx. 43°C) over the torso and limbs. FAW is widely recognized as the most effective intervention for maintaining core body temperature [25].
- Supplementation: Place the dam on a circulating-water mattress or a carbon-fiber resistive heating system set to 38–40°C for conductive heat transfer.
3. Operating Room Preparation:
- Increase the ambient operating room temperature to 75–77°F (24–25°C) to reduce radiative and convective heat loss [25].
- Prepare all surgical fluids (intravenous fluids, lavage fluids) in a fluid warmer set to 38–40°C. Warmed intravenous fluids are a recognized measure to help prevent hypothermia [28].
This protocol ensures a seamless thermal handover from the uterus to the external environment, preventing the cascade of hypothermia, ileus, and hypoglycemia [27].
1. Staged Resuscitation and Drying:
- Color-Coded Towel System: Assign each neonate a colored, sterile, pre-warmed towel immediately upon delivery from the uterus. This allows for tracking individual pup viability, APGAR scores, and resuscitation efforts, which is critical for research data integrity [27].
- Immediate Drying: Vigorously dry the pup with its assigned towel to eliminate evaporative heat loss, the greatest initial danger.
- Stimulation: Gently rub the pup's body to stimulate respiration and circulation.
2. Active Warming and Assessment:
- Transfer to Stable Heat Source: After drying, immediately transfer the pup to a separate, temperature-stable heat source, such as a circulating-water mattress or a radiant warmer, set to 95°F (35°C).
- APGAR Scoring: Perform the first APGAR assessment at one minute post-birth. This score evaluates mucous membrane color (Appearance), pulse, grimace/reflexes, Activity/muscle tone, and Respirations on a scale of 0-2 for each parameter [27].
- Intervention: Puppies with an APGAR score below 7 require immediate intervention (e.g., oxygen, further tactile stimulation). Their survival rate can reach 90% with appropriate care [27].
- Weighing and Identification: Weigh the pup on a digital scale (in grams for precision), record the weight, and apply a non-invasive identification method (e.g., colored breeder's collar or non-toxic nail polish) [27].
Protocol 3: Postoperative Monitoring and Maintenance
This protocol focuses on sustained thermal support during the critical recovery phase when neonates are still unable to effectively self-regulate their body temperature.
1. Continuous Thermal Support:
- Maintain pups on a regulated heat source in a pre-warmed incubator or whelping box for at least the first week of life.
- Monitor rectal temperatures every 15–30 minutes until stable, and then every 2–4 hours for the first 24 hours. The target rectal temperature for the first 24 hours is 94–96°F (34.4–35.6°C) [27].
- Ensure the environmental humidity is maintained between 45% and 65% to prevent pulmonary and dermal fluid loss [27].
2. Nutritional and Hydration Monitoring:
- Ensure pups nurse effectively. A chilled puppy (hypothermic) will develop ileus, where the gut stops moving, preventing digestion and leading to aspiration and dehydration [27].
- Monitor hydration status by checking urine color on a white cotton ball. Urine should be pale and almost clear; dark yellow urine indicates dehydration [27].
- Monitor weight gain/loss twice daily. Weight loss greater than 4% from birth weight is associated with an eightfold increased risk of death and necessitates intervention [27].
Thermal Management Workflow and Pathophysiology
The following diagram illustrates the logical workflow and pathophysiological consequences of neonatal hypothermia management during a preserved reproductive tract C-section.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Thermal Management Studies
| Item | Function/Application in Protocol |
|---|---|
| Forced-Air Warming (FAW) System | Active warming of the dam pre- and post-operatively; considered the gold standard for perioperative warming [25]. |
| Circulating-Water Mattress | Provides conductive heat to the dam during surgery and a stable, temperature-controlled surface for neonates post-resuscitation. |
| Digital Thermometer (with rectal probe) | Accurate and continuous monitoring of core body temperature in both the dam and neonates. Essential for protocol adherence [27]. |
| Digital Gram Scale | High-precision weighing of neonates to monitor critical weight changes; weight loss >4% signals high risk [27]. |
| Fluid Warmer | Pre-warms intravenous and lavage fluids to body temperature (38-40°C) to prevent conductive heat loss in the dam [28]. |
| Glucometer | Monitoring blood glucose levels in neonates; levels below 90 are associated with a fourfold increased risk of death [27]. |
| Sterile Pre-Warmed Towels | Drying neonates to prevent evaporative heat loss and serving as a color-coded identification system during C-sections [27]. |
| Humidity & Temperature Monitor | Ensurs the ambient environment for neonates stays within the recommended 45-65% humidity and target temperature range [27]. |
| L-Flamprop-isopropyl | L-Flamprop-isopropyl, CAS:57973-67-8, MF:C19H19ClFNO3, MW:363.8 g/mol |
Within the scope of research on the female reproductive tract preserved C-section protocol, maintaining absolute sterility is a critical determinant of both maternal and neonatal outcomes. Surgical site infections (SSIs) following obstetric procedures represent a significant source of morbidity, increased medical costs, and extended hospitalization [29] [30]. This document outlines evidence-based application notes and detailed experimental protocols for disinfection and contamination prevention, tailored for the research and development phase of novel C-section techniques. The foundational principle governing these protocols is the Spaulding classification, which categorizes medical devices based on the infection risk associated with their use and dictates the requisite level of processing [31]. Adherence to these structured reprocessing and antisepsis guidelines is paramount for ensuring the integrity and safety of surgical research.
Classification of Medical Devices and Processes
The sterility assurance level for any item used in a surgical procedure is determined by its intended contact with the patient. The Spaulding classification system provides a rational framework for this, defining three distinct categories as shown in the table below [31].
Table 1: Spaulding Classification for Medical Device Reprocessing
| Category | Definition | Examples | Required Processing Level |
|---|---|---|---|
| Critical | Items that enter sterile tissue or the vascular system. | Surgical instruments (scalpels, forceps), cardiac and urinary catheters, implants [31]. | Sterilization [31] |
| Semicritical | Items that contact mucous membranes or non-intact skin. | Endoscopes (e.g., duodenoscopes, bronchoscopes), endocavitary probes [31]. | High-Level Disinfection (or sterilization) [31] |
| Noncritical | Items that contact only intact skin. | Blood pressure cuffs, stethoscopes, bedside tables [31]. | Low-Level Disinfection [31] |
This classification is dynamically evolving. For instance, due to their complex design and high contamination risk, devices like duodenoscopes are now recommended to be reclassified from semicritical to critical, necessitating sterilization rather than high-level disinfection [31].
The following workflow diagram illustrates the logical decision-making process for achieving sterility based on the Spaulding classification and the key protocols involved.
Central Processing and Sterilization Workflow
The reprocessing of surgical instruments should ideally be conducted in a dedicated Central Processing Department (CPD) designed to control quality and minimize cross-contamination [15]. The physical facility should be divided into at least three distinct areas with specific environmental controls [15]:
- Decontamination Area: Designed with negative pressure and a minimum of 6-10 air exchanges per hour to contain contaminants. Personnel must wear appropriate Personal Protective Equipment (PPE) including gloves, gowns, face masks, and eye protection [15].
- Packaging Area: For inspecting, assembling, and packaging clean, non-sterile materials.
- Sterilization and Storage Area: A limited-access area with controlled temperature and relative humidity not exceeding 70% [15].
The workflow within the CPD is sequential and critical to sterility assurance, as detailed in the protocol below.
Protocol: Instrument Reprocessing and Sterilization
Objective: To safely render critical surgical instruments sterile and ready for use in research procedures. Principle: A meticulous multi-step process from decontamination to verified sterilization is non-negotiable for patient safety [15] [31].
Methodology:
Cleaning and Decontamination
- Immediate Action: Instruments should be cleaned as soon as possible after use to prevent drying of blood and tissues, which compromises cleaning efficacy [15].
- Method: Perform meticulous cleaning using water with detergents or enzymatic cleaners to reduce bioburden and remove organic material that can act as a barrier to the sterilization agent [15] [31]. This can be done using mechanical cleaning machines (e.g., ultrasonic cleaners, washer-disinfectors) or by manual cleaning for delicate items [15].
- Inspection: Visually inspect instruments for residual debris. Note that microscopic residue may persist, particularly on intricate surfaces [15].
Packaging and Preparation
- Purpose: Packaging must allow for sterilant penetration while providing an effective barrier against microbial contamination after processing [15].
- Materials: Use FDA-cleared and AAMI-compliant materials such as sterilization wraps (woven or nonwoven), rigid containers, or peel-open pouches [15].
- Technique: Hinged instruments should be opened, and items with removable parts should be disassembled. Device heavy metal mass should be considered, as it is a known cause of wet packs (retained moisture) after sterilization [15].
Loading the Sterilizer
- Principle: Load contents must be arranged to allow free circulation of the sterilant (e.g., steam) around each item [15].
- Procedure: Place perforated trays parallel to the shelf. Place non-perforated containers (e.g., basins) on their edge. Place peel packs on edge in perforated or mesh-bottom racks [15]. Avoid overloading the sterilizer chamber.
Sterilization Cycle Verification
- Initial Qualification: A sterilizer must be tested upon installation, relocation, or after major repair with three consecutive empty cycles using biological and chemical indicators. The sterilizer is not put back into use until all biological indicators are negative and chemical indicators show a correct end-point response [15].
- Ongoing Monitoring: For routine quality assurance, biological and chemical indicators should be used in representative samples of actual product loads. When major changes are made to packaging or load configuration, three consecutive evaluation cycles with negative biological indicators are required before the change can be put into routine use [15].
Preoperative Skin and Mucous Membrane Antisepsis
Surgical site preparation is a critical defense against SSIs. For C-section procedures, this involves the preparation of both the abdominal skin and the vaginal mucosa.
Protocol: Vaginal and Abdominal Preparation for C-Section
Objective: To reduce the microbial load on the abdominal skin and vaginal mucosa prior to incision. Principle: Using effective antiseptic agents significantly decreases the risk of microbial contamination of the surgical site [29] [30].
Methodology:
Vaginal Preparation
- Agent Selection: Current guidelines endorse the use of either povidone-iodine (PI) or chlorhexidine gluconate (CHG)-based agents for vaginal preparation [30]. A recent large-scale retrospective study of hysterectomy patients found no statistically significant difference in SSI rates between PI (1.4%) and CHG (1.2%) [30].
- Procedure: The preparation should be performed immediately prior to surgery as a dedicated procedural step [30].
Abdominal Skin Preparation
- Agent Selection: The CDC and WHO strongly recommend the use of alcohol-based antiseptic solutions for surgical-site skin preparation, unless contraindicated [29]. Solutions based on chlorhexidine are commonly used.
- Application Technique: Apply the antiseptic agent using an appropriate friction scrub in a concentric, outward-moving pattern from the planned incision site.
Table 2: Quantitative Efficacy Data for Antiseptic Agents
| Antiseptic Agent | Spectrum of Activity | Key Clinical Context / Efficacy Data | Application Guidelines |
|---|---|---|---|
| Chlorhexidine Gluconate (CHG) | Broad-spectrum against vegetative bacteria, some viruses, and fungi [32]. | - Recommended for abdominal skin prep [29].- For vaginal prep, shows comparable SSI rates to PI (1.2% vs 1.4%) [30]. | - Often used in alcohol-based solutions for rapid, persistent activity [29]. |
| Povidone-Iodine (PI) | Broad-spectrum antimicrobial [32]. | - The only FDA-approved vaginal preparation agent [30].- For vaginal prep, shows comparable SSI rates to CHG [30]. | - Aqueous or alcohol-based solutions available.- Requires defined contact time to be effective. |
| Alcohol (Ethyl or Isopropyl) | Effective against vegetative bacteria, viruses, and fungi, but not spores; fast-acting [32]. | - Recommended as the base for surgical skin preparation [29]. | - Used as a solvent with CHG or iodine to enhance efficacy.- Allow to fully dry before draping. |
Testing the Efficacy of Disinfectants and Sterilants
Validating the effectiveness of chemical agents used in disinfection and sterilization is crucial for protocol reliability. Several standardized quantitative methods are employed.
Protocol: Use-Dilution Test for Disinfectant Efficacy
Objective: To determine the effectiveness of a liquid chemical disinfectant on an inanimate, non-porous surface. Principle: This method assesses a disinfectant's ability to kill microorganisms when applied to a contaminated surface at its recommended use concentration [32].
Methodology:
- Carrier Preparation: Small cylindrical carriers (e.g., stainless steel penicillium cups) are dipped in a culture of the target microorganism (e.g., Staphylococcus aureus ATCC 6538, Pseudomonas aeruginosa ATCC 15442) and dried [33] [32].
- Disinfectant Exposure: The contaminated carriers are immersed in the disinfectant solution, diluted to the manufacturer's recommended use concentration, for a specified contact time (e.g., 10 minutes) [32].
- Neutralization and Culturing: After exposure, the carriers are transferred to a neutralizing medium to stop the disinfectant's action. They are then incubated in a nutrient broth [32].
- Analysis of Results:
- Turbidity in the broth indicates bacterial survival and disinfectant ineffectiveness at the tested conditions.
- No growth (clear broth) indicates the disinfectant was effective in killing the test organisms on the carrier.
- A passing result, as per the Association of Official Agricultural Chemists (AOAC), requires a minimum of 59 out of 60 replicates to show no growth, and results must be repeatable from different disinfectant batches [32].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Sterility and Disinfection Research
| Reagent / Material | Function and Application in Research | Key Characteristics |
|---|---|---|
| Enzymatic Cleaners | Breaks down organic soil (blood, proteins, lipids) on surgical instruments prior to disinfection/sterilization [15]. | Contains proteases, lipases, amylases. Essential for effective cleaning of complex devices. |
| Chemical Biological Indicators (BIs) | Verifies the efficacy of the sterilization process by confirming the kill of highly resistant bacterial spores (e.g., Geobacillus stearothermophilus) [15]. | Placed inside a process challenge device (PCD) in every sterilizer load. Provides a direct measure of sterility assurance. |
| Chemical Indicators (CIs) | Provides a real-time, visual indication that an item has been exposed to the sterilization process (e.g., color-changing ink on tape or integrators) [15]. | Does not prove sterility. Used to distinguish processed from unprocessed items. Class 5 integrators approximate BI performance. |
| Chlorhexidine Gluconate (CHG) | Broad-spectrum antiseptic used for patient preoperative skin cleansing and surgical site preparation [29] [30]. | Known for its persistent antimicrobial activity and cumulative effect. |
| Povidone-Iodine (PI) | Broad-spectrum antiseptic used for skin and mucous membrane (vaginal) preparation prior to surgery [30]. | The only FDA-approved agent for vaginal preparation. |
| Glutaraldehyde | A high-level disinfectant/chemical sterilant used for heat-sensitive semicritical devices [31]. | Pungent odor; requires adequate ventilation and immersion time of 20-90 minutes depending on formulation and temperature [31]. |
| Hydrogen Peroxide | Used in low-temperature sterilization technologies (e.g., gas plasma, vapor) and as a component in some liquid chemical sterilants/HLDs [34] [31]. | Leaves no toxic residues; effective against a wide range of microorganisms. |
Application Notes
This document provides application notes and detailed experimental protocols for investigating the influence of cross-fostering on offspring development, with a specific focus on outcomes related to the female reproductive tract and systemic physiology. The protocols are designed within the context of a broader research thesis exploring the long-term effects of a preserved reproductive tract following Cesarean-section delivery, emphasizing the critical role of early postnatal maternal care.
Emerging evidence from rodent models demonstrates that the postnatal environment, particularly maternal care, can exert a powerful influence on offspring development, sometimes even mitigating genetically programmed pathologies [35]. The cross-fostering paradigm is a key methodological approach for disentangling the effects of genetic predisposition from those of the early life environment. Quantitative data from foundational studies are summarized in the tables below to guide experimental design and expectation.
Table 1: Quantitative Offspring Outcomes from Cross-Fostering Studies
| Offspring Parameter | SHR Pups with SHR Mother (Control) | SHR Pups with Wistar Mother (Cross-Fostered) | Wistar Pups with Wistar Mother (Control) | Wistar Pups with SHR Mother (Cross-Fostered) |
|---|---|---|---|---|
| Central Clock (SCN) Bmal1 Rhythm Amplitude | Dampened | Facilitated development & improved amplitude [35] | Normal | Impaired entrainment to light/dark cycle [35] |
| Activity/Rest Rhythm Entrainment | Dampened & phase-advanced [35] | Improved entrainment to light/dark cycle [35] | Normal | Worsened synchrony (effect disappeared post-weaning) [35] |
| Colonic Clock Rhythm Amplitude | Dampened | Remedied amplitudes [35] | Normal | Not Reported |
| Cardiovascular Function | High blood pressure (up to 180-200 mmHg) [35] | Improved function [35] | Normotensive (~120 mmHg) [35] | Not Reported |
| Amygdala Kindling Rate (Seizure Susceptibility) | Fast (Seizure-Prone strain) [36] | No normalization of genetic predisposition [36] | Slow (Seizure-Resistant strain) [36] | Became more seizure-prone [36] |
| Commissural (e.g., Corpus Callosum) Cross-Sectional Area | Larger [36] | Not Reported | Smaller [36] | Increased (became similar to Fast strain) [36] |
Table 2: Observed Maternal Behavioral Profiles
| Maternal Behaviour | SHR Mother (Designated 'Abnormal/Atypical') | Wistar Mother (Designated 'Normal') |
|---|---|---|
| Time Spent in Nest with Pups | Left nest for longer periods, especially during the night [35] | More frequent and consistent care [35] |
| Designated Care Quality | Worse / Less frequent [35] | Better / More intensive [35] |
Experimental Protocols
Protocol 1: Cross-Fostering and Basic Phenotyping Workflow
This protocol outlines the core procedure for establishing cross-fostered cohorts and assessing fundamental physiological and neurological outcomes.
1.1 Cross-Fostering Procedure
- Day of Birth Designation: Designate the day of birth as Postnatal Day 0 (P0).
- Strain Assignment: On P1, assign pups to one of four experimental groups (as in Table 1):
- SHR pups reared by biological SHR dam.
- SHR pups reared by Wistar dam.
- Wistar pups reared by biological Wistar dam.
- Wistar pups reared by SHR dam.
- Fostering Process: Gently remove the foster dam from her home cage. Distribute the recipient pups (e.g., SHR pups) into the foster dam's cage, ensuring they are intermixed with any remaining biological pups to retain the original litter size. The foster dam's biological pups are concurrently cross-fostered to another dam or culled according to the experimental design. The process should be completed swiftly to minimize stress.
- Weaning: Pups are weaned at P21-28 and housed with same-sex littermates.
1.2 Assessment of Maternal Care
- Method: Conduct live observations or use infrared video recording of the home cage.
- Schedule: Perform observations at regular intervals (e.g., every 3 minutes) during both light and dark phases for a minimum of 4 days between P1 and P10.
- Behaviors to Score: Record the presence or absence of:
- Arched-Back Nursing (ABN): Mother nurses in an arched-back posture over pups.
- Licking/Grooming (LG): Mother licks or grooms any pup.
- Nest Attendance: Mother is in physical contact with the pup pile in the nest [35].
1.3 Terminal Phenotyping in Adulthood
- Circadian Rhythm Analysis: House adults in cages with running wheels. Monitor and record locomotor activity for at least two weeks under a standard 12:12 light/dark cycle. Analyze rhythm amplitude, period, and phase. Subsequently, animals are euthanized at multiple time points (e.g., every 4-6 hours over a 24-hour cycle) for tissue collection (SCN, liver, colon) to analyze clock gene expression (e.g., Bmal1, Per2, Nr1d1) via qPCR or in-situ hybridization [35].
- Cardiovascular Assessment: Measure systolic and diastolic blood pressure in conscious, restrained animals using a non-invasive tail-cuff sphygmomanometer system. Conduct measurements at the same time each day to control for diurnal variation [35].
- Seizure Susceptibility (Amygdala Kindling): Anesthetize animals and surgically implant a bipolar stimulating/recording electrode into the basolateral amygdala. Following recovery, the afterdischarge threshold is determined by applying a 1-2 second train of monophasic square-wave pulses. Kindling is performed by administering a stimulus (e.g., 100-200 µA above threshold) once or twice daily until a criterion (e.g., 5 consecutive stage 5 seizures) is met. Key metrics include afterdischarge threshold, afterdischarge duration, and number of stimulations to reach criterion [36].
- Anatomic Connectivity (Morphometry): Following perfusion and brain extraction, tissue is sectioned coronally. Sections containing the corpus callosum and anterior commissure are stained (e.g., Luxol Fast Blue for myelin). The cross-sectional area of these structures is quantified using image analysis software. Alternatively, DiI labeling can be used to trace axonal projections between hemispheres [36].
Protocol 2: Molecular Analysis of Maternal Influence
This protocol details the procedures for investigating the molecular mechanisms by which maternal care influences offspring development, with a focus on signaling pathways and epigenetic regulation.
2.1 Analysis of Hypothalamic-Pituitary-Adrenal (HPA) Axis Function
- Corticosterone Measurement: Collect blood samples from pups (e.g., via tail nick) at a consistent time of day, preferably under basal conditions and following a mild stressor (e.g., 20-minute restraint). Measure plasma corticosterone levels using a commercial enzyme immunoassay (EIA) or radioimmunoassay (RIA) kit.
- Receptor Expression: Euthanize animals and dissect brain regions of interest (e.g., hippocampus, hypothalamus). Isolate total RNA and analyze mRNA expression of glucocorticoid receptor (GR) and mineralocorticoid receptor (MR) using quantitative RT-PCR. Validate with Western blotting for protein levels.
2.2 Analysis of Neurotrophin and Activity-Dependent Gene Expression
- Tissue Collection: Euthanize animals and rapidly dissect brain regions (e.g., hippocampus, amygdala, SCN). Flash-freeze tissue in liquid nitrogen.
- RNA/Protein Extraction: Homogenize tissue and extract total RNA and protein using commercial kits.
- qRT-PCR: Synthesize cDNA and perform qRT-PCR using primers for genes of interest, including:
- Neurotrophins: Bdnf (multiple transcripts)
- Immediate Early Genes: Arc, Fos, Egr1
- Synaptic Proteins: Homer1a
- Western Blotting: Separate proteins via SDS-PAGE, transfer to a membrane, and probe with primary antibodies against BDNF, ARC, EGR1, etc., followed by appropriate HRP-conjugated secondary antibodies. Detect using enhanced chemiluminescence [36].
2.3 Epigenetic Analysis of Candidate Gene Promoters
- Chromatin Immunoprecipitation (ChIP): Cross-link proteins to DNA in fresh or frozen tissue samples. Sonicate chromatin to fragment DNA. Immunoprecipitate the sheared chromatin with antibodies specific to epigenetic marks (e.g., H3K9ac for activation, H3K27me3 for repression) or transcription factors (e.g., GR). Reverse cross-links and purify DNA.
- Analysis of Precipitated DNA: Quantify the enrichment of specific gene promoter regions (e.g., GR promoter in the hippocampus, Bdnf promoters) in the immunoprecipitated DNA using qPCR. Express data as a percentage of input chromatin.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Cross-Fostering Studies
| Item | Function/Application | Example/Specification |
|---|---|---|
| SHR and Wistar Rats | Model organisms for studying genetic vs. environmental influences on physiology and behavior. | Acquire from reputable animal suppliers (e.g., Charles River, Janvier Labs). |
| Infrared Video Recording System | For objective, 24/7 monitoring of maternal care behaviors without visible light disruption. | Systems from companies like Axis, Hikvision; software like EthoVision XT (Noldus). |
| qPCR Master Mix & Primers | For quantitative analysis of clock gene, neurotrophin, and immediate-early gene expression. | SYBR Green or TaqMan kits (Thermo Fisher, Bio-Rad); validated primer sets. |
| Corticosterone EIA/RIA Kit | For precise measurement of circulating stress hormone levels in plasma/serum. | Kits from Enzo Life Sciences, Arbor Assays, or Cayman Chemical. |
| Antibodies (IHC/Western) | For protein localization and quantification (e.g., GR, BDNF, epigenetic markers). | Validate for use in rat tissue; suppliers: Abcam, Cell Signaling Technology, MilliporeSigma. |
| Stereo EEG/Stimulation System | For seizure monitoring and electrical kindling in freely moving animals. | Includes electrodes, commutators, and stimulator/recorder (e.g., from Bio-Signal Group, Pinnacle Technology). |
| Digital Morphometry Software | For quantitative analysis of cross-sectional brain areas and neuronal tracing. | ImageJ (Fiji), Neurolucida (MBF Bioscience), or Imaris (Oxford Instruments). |
Efficiency in generating germ-free (GF) mouse models is a critical determinant of pace and cost in microbiome and genetic research. The entire procedure, from obtaining sterile pups to successful weaning, is fraught with inherent variability that can compromise experimental reproducibility and timeline. This document details a refined, evidence-based protocol for the production of GF mice via Female Reproductive Tract-Preserved Cesarean Section (FRT-CS). The strategies herein are designed to address key bottlenecks: surgical fetal survival, precise timing of donor delivery, and optimized postnatal care [8]. By systematically implementing these techniques, researchers can significantly enhance the throughput and reliability of obtaining GF mice, thereby accelerating downstream scientific applications.
Application Notes & Core Principles
The following notes outline the foundational principles supporting this streamlined protocol:
- FRT-CS Superiority: The preserved female reproductive tract technique is not merely a surgical variation but a fundamental improvement that minimizes physical trauma to the uterus during extraction. This approach directly enhances fetal viability by maintaining a more stable intrauterine environment until the moment of transfer to the isolator [8].
- Precision Timing via IVF: Relying on natural mating (NM) introduces significant unpredictability in gestation timing. Integrating In Vitro Fertilization (IVF) allows for the precise scheduling of donor deliveries. This control is paramount for planning C-sections during operational hours and ensuring the immediate availability of technical staff and foster mothers, thereby reducing pup loss due to procedural delays [8].
- Strain-Specific Maternal Efficacy: The choice of GF foster mother is a critical variable often overlooked. Maternal behavior and nursing success are highly strain-dependent under GF conditions. Counter to some findings in specific pathogen-free (SPF) conditions, BALB/c and NSG strains have demonstrated superior performance as GF foster mothers, whereas C57BL/6J shows markedly lower weaning success in the germ-free context [8].
The efficacy of the optimized protocol components is substantiated by the following comparative data:
Table 1: Comparison of Cesarean Section Technique Efficacy
| Surgical Technique | Key Feature | Impact on Fetal Survival | Sterility Maintenance |
|---|---|---|---|
| Traditional C-section (T-CS) | Clamps placed at cervix base and top of uterine horn | Baseline (Control) | Maintained |
| FRT-CS | Clamps only at cervix base, preserving ovary, uterine horn, and cervix | Significantly Improved | Maintained |
Table 2: Evaluation of Donor Conception Methods
| Conception Method | Delivery Date Precision | Experimental Reproducibility | Contamination Rate |
|---|---|---|---|
| Natural Mating (NM) | Low (Variable) | Lower | Comparable |
| In Vitro Fertilization (IVF) | High (Precise Control) | Enhanced | Comparable |
Table 3: Assessment of GF Foster Mother Strain Performance
| GF Foster Mother Strain | Nursing Capability | Weaning Success Rate | Relative Performance |
|---|---|---|---|
| C57BL/6J | Low | Lowest | Poor |
| BALB/c | High | High | Superior |
| NSG | High | High | Superior |
| KM (Outbred) | Not Specified | Intermediate | Moderate |
Detailed Experimental Protocols
Protocol 1: Female Reproductive Tract-Preserved C-Section (FRT-CS)
This protocol describes the aseptic derivation of GF pups from a euthanized donor dam.
Objective: To extract fetuses with minimal uterine disturbance, maximizing neonatal survival for GF colonization. Materials:
- Pregnant SPF donor dam (e.g., C57BL/6, BALB/c) at gestational day 18.5.
- Sterile surgical instrument kit (scissors, forceps, clamps).
- Chlorine dioxide disinfectant (e.g., Clidox-S, 1:3:1 dilution).
- Pre-warmed (37°C) heating pad.
- Sterile polyvinyl chloride (PVC) isolator.
- Sterile swabs.
Procedure:
- Euthanasia and Preparation: Euthanize the pregnant donor dam via cervical dislocation. Saturate the abdominal fur with disinfectant.
- Aseptic Laparotomy: Using sterile instruments, make a midline incision through the skin and peritoneum to expose the abdominal cavity.
- Uterine Horn Exposure: Gently exteriorize the uterine horns containing the fetuses.
- FRT-CS Clamping: Place a clamp only at the cervix base, thereby preserving the integrity of the entire uterine horn and associated tissues. Avoid placing a second clamp at the top of the horn.
- Uterine Dissection: Excise the entire uterus by cutting distal to the single clamp. Transfer the intact uterus rapidly into a container with a fresh disinfectant solution for the recommended contact time.
- Isolator Transfer and Pup Extraction: Quickly pass the disinfected uterus into the sterile isolator. Inside the isolator, use surgical scissors to incise the uterine wall and amniotic sac for each fetus. Wipe the pup's face and body with a sterile swab to clear amniotic fluid and stimulate breathing. Cut the umbilical cord.
- Viability Check: Ensure spontaneous breathing is noted before proceeding. The entire procedure, from euthanasia to completed pup extraction inside the isolator, must be completed within 5 minutes to prevent hypothermia and ensure viability [8].
Protocol 2: Integrated IVF-Donor Production
This protocol ensures the precise timing of donor dam deliveries for planned FRT-CS.
Objective: To generate pregnant donor dams with a known and controlled delivery date. Materials:
- SPF donor females and males (desired strain for embryos).
- SPF CD-1 or other suitable recipient females.
- Standard IVF laboratory equipment and reagents.
Procedure:
- IVF and Embryo Culture: Perform in vitro fertilization using oocytes from superovulated donor females and sperm from males of the same strain. Culture the fertilized embryos to the two-cell stage.
- Embryo Transfer: Surgically transfer the two-cell stage embryos into the oviducts of pseudopregnant CD-1 recipient females. This day is designated as embryonic day 0.5 (E0.5).
- Monitoring and Scheduling: Monitor the recipients for successful pregnancy. Schedule the FRT-CS procedure for the predicted delivery date (typically E19.5), allowing for precise planning and resource allocation [8].
Protocol 3: Cross-Fostering to Germ-Free Foster Mothers
This protocol covers the critical step of placing derived GF pups with a pre-conditioned foster dam.
Objective: To achieve high weaning rates through strain-selected foster mothers. Materials:
- Proven GF foster mothers (BALB/c or NSG strains are recommended) that are 4 months old and have had one prior successful birth.
- Time-mated foster mother (within 1-2 days of the donor's parturition date).
Procedure:
- Foster Preparation: Select a healthy GF foster mother of the recommended strain that has given birth within the last 48 hours.
- Pup Transfer: Gently remove the foster mother's biological pups from the nest. Briefly disturb the nest bedding.
- Scent Introduction: Rub the derived GF pups gently against the bedding and the foster mother's biological pups to transfer scent.
- Pup Placement: Place the GF pups into the foster mother's nest. The combination of a disturbed nest and transferred scent promotes acceptance.
- Monitoring: Monitor the foster mother for nursing behavior and the GF pups for milk spots to confirm successful adoption [8].
Workflow & Signaling Pathway Diagrams
The following diagram illustrates the complete, streamlined workflow for efficient germ-free mouse production, integrating the key protocols outlined above.
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and reagents required for the implementation of this streamlined protocol are listed below.
Table 4: Essential Research Reagents and Materials
| Item Name | Function / Purpose | Example / Specification |
|---|---|---|
| SPF Donor Mice | Source of embryos/fetuses for GF derivation. | C57BL/6, BALB/c from reputable commercial suppliers [8]. |
| GF Foster Mice | Critical for postnatal care and weaning of derived pups. | BALB/c or NSG strains, 4 months old, primiparous [8]. |
| Chlorine Dioxide Disinfectant | Sterilizing the exterior of the extracted uterus before transfer into the isolator. | Clidox-S, used in a 1:3:1 dilution, activated for 15 min [8]. |
| Sterile PVC Isolator | Maintains a germ-free environment for housing GF mice and performing pup extraction. | Custom-built isolator with attached gloves and transfer port [8]. |
| Sterile Surgical Kit | Performing the aseptic C-section and fetal extraction. | Fine scissors, forceps, and hemostatic clamps, autoclaved prior to use. |
| Heating Pad | Prevents hypothermia in neonates during the C-section procedure. | Set to 40-45°C, activated at least 15 min before surgery [8]. |
Integrating IVF with FRT-CS for Superior Experimental Planning and Reproducibility
Application Note: Enhancing Germ-Free Mouse Production
The production of germ-free (GF) mice is a cornerstone for microbiome and host-interaction studies. Traditional methods, reliant on natural mating (NM) for generating donor embryos, introduce significant variability in delivery timing and compromise experimental reproducibility. This application note details a refined protocol that integrates In Vitro Fertilization (IVF) with a Female Reproductive Tract-Preserved Cesarean Section (FRT-CS). This synergistic approach standardizes the timeline for deriving GF pups and significantly improves neonatal survival rates, thereby enhancing the efficiency and reliability of generating GF mouse colonies for preclinical research [8].
Quantitative Advantages of the Integrated IVF-FRT-CS System
The combined methodology addresses two critical bottlenecks in GF mouse production: the unpredictability of donor pup availability and the survival rate of derived pups. The quantitative benefits of this integrated system, derived from comparative studies, are summarized in the table below.
Table 1: Comparative Outcomes of Traditional NM vs. Integrated IVF-FRT-CS Protocol
| Experimental Component | Natural Mating (NM) & T-CS | IVF & FRT-CS | Impact on Experimental Reproducibility |
|---|---|---|---|
| Delivery Timing Control | Variable; based on vaginal plug detection and natural birth timing, which can occur from gestation day 18 onward [8]. | Precise; FRT-CS is performed on a predetermined date following a timed IVF cycle, eliminating unpredictability [8]. | Enables exact scheduling of the surgically intensive derivation process, improving resource allocation and workflow planning. |
| Fetal Survival Rate | Lower; the traditional C-section method (T-CS), which clamps both the cervix and top of the uterine horn, is less optimal for pup survival [8]. | Significantly improved; the FRT-CS technique, which selectively clamps only the cervix base, preserves the entire reproductive tract and enhances survival while maintaining sterility [8]. | Increases the yield of live pups per surgical procedure, reducing the number of donor mice and C-section procedures required. |
| Overall Efficiency | Lower and more variable due to unpredictable delivery and lower pup survival. | Higher and more consistent, driven by precise timing and superior surgical outcomes. | Enhances the reproducibility of obtaining GF mice across multiple experimental cohorts and time points. |
Detailed Experimental Protocols
Protocol 1: In Vitro Fertilization for Timed Donor Embryo Production
This protocol ensures the generation of donor pups with a precisely controlled delivery date.
I. Materials (Research Reagent Solutions)
- Sperm & Oocyte Collection Media: Specifically formulated media for the collection and handling of gametes (e.g., Human Tubal Fluid (HTF)).
- Fertilization Media: Media optimized for supporting the fertilization process in vitro.
- Embryo Culture Media: Sequential media that supports the development of fertilized eggs to the 2-cell stage and beyond.
- Hormonal Regimen: Gonadotropins (e.g., PMSG and hCG) for superovulation of donor females.
- Pronuclei Staining Solution: A dye to confirm successful fertilization.
II. Methodology
- Superovulation of Donor Females: Administer a standardized hormonal regimen to C57BL/6J or other required strain females to induce the production of a large number of oocytes [8].
- Sperm Collection and Capacitation: Collect sperm from male mice of the desired strain and allow them to undergo capacitation in fertilization media.
- Oocyte Collection: Euthanize superovulated females and collect cumulus-oocyte complexes from the oviducts.
- In Vitro Fertilization: Co-incubate capacitated sperm with oocytes in fertilization media for several hours.
- Confirmation of Fertilization: Check for the presence of two pronuclei (2PN) under a microscope to confirm successful fertilization.
- Embryo Culture and Transfer: Wash and culture the fertilized embryos (zygotes) in embryo culture media. Implant the 2-cell stage embryos into pseudopregnant CD-1 recipient females. The day of implantation is designated as embryonic day 0.5 (E0.5) [8].
III. Logical Workflow The following diagram outlines the sequential steps for producing timed-pregnant donor mice using IVF.
Protocol 2: Female Reproductive Tract-Preserved Cesarean Section (FRT-CS)
This optimized surgical technique is performed to aseptically derive GF pups from the timed-pregnant donors generated in Protocol 1.
I. Materials (Research Reagent Solutions)
- Disinfectant Solution: Chlorine dioxide-based sterilant (e.g., Clidox-S, used in a 1:3:1 dilution, activated for 15 min before use) [8].
- Sterile Surgical Instruments: Fine scissors, forceps, and clamps.
- Germ-Free Isolator: Polyvinyl chloride (PVC) isolator with pre-sterilized interior.
- Heating Pad: To maintain pup body temperature at 40-45°C during the procedure [8].
- Sterile Swabs: For wiping amniotic fluid from pups to stimulate breathing [8].
II. Methodology
- Isolator and Surgical Preparation: Heat the interior of the germ-free isolator. Activate the disinfectant solution. Autoclave all surgical instruments and materials, including water, food, and bedding [8].
- Euthanasia and Aseptic Preparation: Euthanize the time-pregnant donor female via cervical dislocation. Ensure the abdominal surface is clean.
- FRT-CS Surgical Procedure:
- Make a midline incision to expose the abdominal cavity.
- Identify the uterine horns. In the FRT-CS technique, place a clamp only at the cervix base, preserving the integrity of the ovaries, uterine horns, and uterine junction [8].
- Carefully excise the entire intact uterus and transfer it into the germ-free isolator vessel containing the disinfectant solution for sterilization. The entire procedure from euthanasia to transfer must be completed within 5 minutes to ensure pup viability and sterility [8].
- Pup Derivation Inside Isolator:
- Inside the isolator, incise the uterine sac and amniotic membrane with sterile scissors to expose the pup.
- Gently wipe the pup's face and body with a sterile swab to remove amniotic fluid until spontaneous breathing is noted.
- Cut the umbilical cord.
- Fostering: Immediately transfer the viable, breathing pups to a proven GF foster mother. Studies indicate that BALB/c and NSG GF foster strains exhibit superior nursing and weaning success compared to C57BL/6J under GF conditions [8].
III. Logical Workflow The diagram below contrasts the key surgical difference between the traditional and the optimized FRT-CS techniques.
The Scientist's Toolkit: Essential Materials for IVF-FRT-CS Integration
Table 2: Key Research Reagent Solutions for Germ-Free Mouse Derivation
| Item | Function/Application | Example/Specification |
|---|---|---|
| Clidox-S | A chlorine dioxide-based disinfectant used for sterilizing the exterior of the uterus and other items entering the germ-free isolator [8]. | Used in a 1:3:1 dilution, activated for 15 minutes prior to use [8]. |
| PVC Germ-Free Isolator | A sterile, self-contained housing unit that provides a barrier against all microorganisms for maintaining GF mice [8]. | Equipped with entry ports and gloves for internal manipulation; requires pre-heating before C-section [8]. |
| Embryo Culture Media | A sequential series of media designed to support the development of mouse embryos from the zygote to the blastocyst stage in vitro. | Specific formulations (e.g., KSOM, M16) that provide essential nutrients and maintain physiological pH and osmolarity. |
| Gonadotropins | Hormones used to induce superovulation in donor females, increasing the yield of oocytes for IVF. | Typically, Pregnant Mare's Serum Gonadotropin (PMSG) followed by Human Chorionic Gonadotropin (hCG). |
| Progesterone & Estrogen | Hormonal supplements used to prepare and synchronize the endometrium of recipient females for embryo transfer or to manage the cycle of foster mothers. | Administered via injection or oral routes to mimic natural hormonal cycles and ensure uterine receptivity. |
Data-Driven Validation: Comparing FRT-CS Outcomes with Traditional Methods
This document provides application notes and protocols to support research on female reproductive tract preservation during Cesarean section (C-section). It synthesizes key quantitative metrics for two critical outcome domains: fetal survival following periviable delivery and patient weaning from mechanical ventilation. Standardized measurement of these outcomes is essential for evaluating the efficacy of novel surgical techniques, including reproductive tract preservation, and for contextualizing findings within established clinical benchmarks. The data presentation, experimental protocols, and research tools herein are designed for use by researchers, scientists, and drug development professionals in the field of obstetric and surgical innovation.
Quantitative Data on Fetal Survival and Weaning Success
Fetal Survival Metrics in Periviable Periods
Table 1: Fetal Survival and Active Treatment Trends (2014-2023) [37] This table summarizes a large-scale cohort study of nearly 60,000 infants born at 22- to 25-weeks' gestation, analyzing trends in active treatment and survival. The data demonstrates a significant shift in the point of viability, particularly at 22 weeks' gestation.
| Gestational Age | Metric | 2014 Rate | 2023 Rate |
|---|---|---|---|
| 22 Weeks | Active Treatment | 28.8% | 78.6% |
| Survival Rate | 25.7% | 41.0% | |
| 23 Weeks | Active Treatment | 87.4% | 94.7% |
| Survival Rate | 53.8% | 57.9% |
- Definitions: Active Treatment was defined as initiation of face mask ventilation, nasal continuous positive airway pressure, endotracheal intubation, surfactant therapy, mechanical ventilation, chest compressions, or epinephrine [37]. Survival was tracked through the care period.
- Contextual Note on Viability: The threshold for fetal viability is highly dependent on resource setting. In developed countries, active intervention at 22 weeks is increasingly common, whereas in resource-limited settings, the viability threshold may remain as high as 28 weeks [38].
Predictors of Successful Weaning from Mechanical Ventilation
Table 2: Clinical Predictors of Weaning Success in Patients with Acute Respiratory Failure [39] This table outlines key patient and clinical parameters identified as independent predictors of successful weaning from mechanical ventilation, a critical post-operative outcome.
| Predictor Category | Specific Metric | Association with Weaning Success |
|---|---|---|
| Clinical Severity | APACHE II Score | Lower scores predictive of success [39] |
| Ventilator Duration | Shorter duration predictive of success [39] | |
| Ventilatory Parameters | Tidal Volume | Higher volumes during spontaneous breathing trials [39] |
| Respiratory Rate | Lower rates during spontaneous breathing trials [39] | |
| Blood Gas & Physiology | PaOâ‚‚ (Oxygen Partial Pressure) | Higher levels predictive of success [39] |
| Diaphragmatic Excursion | Greater excursion negatively associated with failure [39] | |
| Patient Status | Level of Consciousness | Alert state predictive of success [39] |
Experimental Protocols
Protocol: Establishing Fetal Survival Metrics in Preclinical Models
This protocol provides a framework for quantifying fetal survival in animal models of periviable C-section, enabling the evaluation of surgical techniques on fetal outcome.
1. Objective: To quantitatively assess the impact of novel C-section techniques (e.g., reproductive tract-preserving methods) on fetal survival rates at periviable gestational stages in a preclinical model.
2. Materials:
- Timed-pregnant animal model (e.g., rodent, swine).
- Surgical suite for aseptic surgery.
- Anesthesia delivery system and monitoring equipment (e.g., for heart rate, SpOâ‚‚).
- Neonatal incubator with temperature and humidity control.
- Neonatal resuscitation equipment (e.g., mini-bag-valve-mask, oxygen source, warming platform).
- Data recording system.
3. Methodology: 1. Experimental Groups: Randomize dams into two groups: a) Experimental Group (undergoes C-section with the novel reproductive tract-preserving protocol) and b) Control Group (undergoes standard C-section procedure). 2. Gestational Timing: Perform procedures at a pre-determined periviable gestational age, calibrated to the model's typical viability threshold (e.g., equivalent to human 22-25 weeks). 3. Surgical Procedure: Execute the respective C-section protocol for each group. Record the time from uterine incision to fetal delivery for each pup. 4. Immediate Post-Delivery Care: * Clamp and cut the umbilical cord. * Gently dry and stimulate the neonate. * Assign an Apgar score at 1 and 5 minutes post-delivery, assessing heart rate, respiration, muscle tone, reflex response, and color. * Provide respiratory support (e.g., positive pressure ventilation) if needed. * Place viable neonates in a pre-warmed incubator. 5. Data Collection & Endpoints: * Primary Endpoint: Survival at 24 hours and 72 hours post-delivery. Record time of death for any non-surviving neonates. * Secondary Endpoints: Apgar scores, weight, gross morphological abnormalities, and requirement for respiratory support. * Maternal Endpoints: Monitor maternal survival, post-operative recovery, and later-term reproductive health if applicable.
4. Analysis: * Compare survival rates between experimental and control groups using statistical tests such as Fisher's exact test or Kaplan-Meier survival analysis with log-rank test. * Analyze continuous data (e.g., Apgar scores, weights) using t-tests or Mann-Whitney U tests.
Protocol: Weaning from Mechanical Ventilation in Preclinical Survival Surgery
This protocol outlines the assessment of weaning readiness and the process of liberating an animal from mechanical ventilation post-operatively, a key indicator of recovery and intervention success.
1. Objective: To systematically wean a research subject from mechanical ventilation post-C-section, minimizing complications and quantifying weaning success.
2. Materials:
- Mechanical ventilator.
- Arterial blood gas (ABG) analyzer.
- Pulse oximeter and capnograph.
- Hemodynamic monitoring equipment.
- Sedation/analgesia for ventilator tolerance.
3. Methodology: 1. Pre-Weaning Assessment (Readiness Criteria): [39] * Clinical Stability: The underlying indication for ventilation (e.g., anesthesia) is resolved. Patient is hemodynamically stable without or on minimal vasopressors. * Gas Exchange: PaO₂/FiO₂ ratio > 200; PEEP ≤ 8 cm H₂O. * Respiratory Mechanics: Adequate cough and respiratory drive. * Neurological Status: Capable of triggering the ventilator. 2. Spontaneous Breathing Trial (SBT): [39] * Reduce ventilator support to a low level of pressure support (e.g., 5-8 cm H₂O above PEEP of 5 cm H₂O) or connect to a T-piece with minimal oxygen support. * Duration: 30-120 minutes. * Continuous Monitoring: Closely monitor respiratory rate, tidal volume, heart rate, blood pressure, and oxygen saturation. 3. SBT Failure Criteria (Abort SBT and resume support): [39] * Respiratory rate > 35/min for ≥ 5 minutes. * Oxygen saturation < 90%. * Heart rate increases > 20% or signs of hemodynamic instability. * Agitation, diaphoresis, or signs of increased work of breathing. 4. Extubation & Post-Extubation Care: * If the SBT is tolerated for the prescribed period without failure criteria, proceed with extubation. * Provide supplemental oxygen via face mask or nasal cannula. * Continue close monitoring for at least 48 hours for signs of respiratory failure requiring reintubation.
4. Analysis: * Weaning Success: Defined as the ability to maintain spontaneous breathing for over 48 hours post-extubation without requiring reintubation [39]. * Compare weaning success rates and duration of mechanical ventilation between experimental and control groups.
Signaling Pathways and Experimental Workflows
Fetal Survival Research Pathway
The following diagram illustrates the logical workflow and key decision points in a preclinical study designed to evaluate fetal survival after a periviable C-section.
Clinical Weaning Decision Pathway
This diagram outlines the standardized clinical decision-making pathway for weaning a patient from mechanical ventilation, based on established predictors of success.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Fetal Survival and Weaning Research This table lists key reagents, equipment, and tools required for conducting the experiments outlined in the protocols above.
| Item | Category | Function/Application in Research |
|---|---|---|
| Timed-Pregnant Animal Model | Animal Model | Provides a biologically relevant system for studying periviable delivery and maternal-fetal physiology. |
| Mechanical Ventilator | Equipment | Provides life-support for survival surgery and serves as the primary intervention for weaning studies. |
| Neonatal Incubator | Equipment | Provides a controlled thermal and humidity environment for supporting periviable neonates post-delivery. |
| Arterial Blood Gas (ABG) Analyzer | Diagnostic Tool | Critical for objective measurement of oxygenation (PaOâ‚‚), ventilation (PaCOâ‚‚), and acid-base status to assess both fetal status and weaning readiness [39]. |
| Pulse Oximeter & Capnograph | Monitoring Tool | Provides continuous, non-invasive monitoring of oxygen saturation (SpOâ‚‚) and end-tidal COâ‚‚, essential during anesthesia and weaning trials. |
| Ultrasound System | Diagnostic Tool | Used for precise gestational age dating pre-procedure and for assessing diaphragmatic function (excursion) as a predictor of weaning success [39]. |
| APACHE II Score Sheet | Clinical Tool | A standardized scoring system to quantify severity of illness and predict weaning outcomes; higher scores correlate with weaning failure [39]. |
Within germ-free (GF) mouse production, the cesarean section (C-section) rederivation technique remains the gold standard for obtaining sterile offspring [8]. This protocol directly compares two surgical techniques for performing sterile C-sections: the Traditional C-section (T-CS) and the Female Reproductive Tract-Preserved C-section (FRT-CS). The core distinction lies in the surgical approach's impact on the donor female's reproductive anatomy. The objective of this application note is to provide a detailed, evidence-based comparison of these methods, focusing on fetal survival data and practical experimental protocols to enhance efficiency in GF mouse production facilities.
Comparative Survival Data Analysis
The following table summarizes the quantitative outcomes of a controlled study comparing T-CS and FRT-CS techniques in two common mouse strains, C57BL/6J (C57) and BALB/c (BC) [8].
Table 1: Survival Data Comparison of T-CS vs. FRT-CS
| Surgical Technique | Mouse Strain | Key Surgical Difference | Fetal Survival Outcome |
|---|---|---|---|
| Traditional C-section (T-CS) | C57 & BALB/c | Clamps placed at both the cervix base and the top of the uterine horn. | Significantly lower fetal survival rates. |
| Female Reproductive Tract-Preserved C-section (FRT-CS) | C57 & BALB/c | Selective clamping only at the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, cervix). | Significantly improved fetal survival rates while maintaining sterility. |
The optimized FRT-CS method demonstrated a statistically significant improvement in the number of viable pups obtained per procedure compared to the T-CS method, thereby increasing the overall efficiency of GF mouse production [8].
Detailed Experimental Protocols
Protocol A: Female Reproductive Tract-Preserved C-Section (FRT-CS)
Principle: To deliver pups via C-section while minimizing trauma and preserving the integrity of the donor's reproductive tract, thereby enhancing pup viability.
Materials: See Section 5, "The Scientist's Toolkit."
Pre-Surgical Procedure:
- Euthanize pregnant SPF donor female at the appropriate gestation day via cervical dislocation.
- Sterilize the abdominal surface thoroughly using a chlorine dioxide disinfectant (e.g., Clidox-S in a 1:3:1 dilution, activated for 15 minutes).
- Transfer the donor to a sterile polyvinyl chloride (PVC) isolator, the interior of which has been pre-warmed to 40–45°C using a heating pad to prevent pup hypothermia.
Surgical Procedure (FRT-CS):
- Make a midline incision through the abdominal wall to expose the uterine horns.
- Identify the cervix and uterine horns.
- Apply a clamp selectively only at the base of the cervix. Crucially, do not clamp the top of the uterine horn.
- Gently exteriorize the uterine horns and place the entire uterus into a sterile container.
- Transfer the container into the sterile isolator for the remainder of the procedure.
- Inside the isolator, carefully incise the uterine wall with sterile surgical scissors.
- Gently remove each pup and incise the amniotic membrane.
- Wipe the pup's face and body with a sterile cotton swab to clear amniotic fluid until spontaneous breathing is noted.
- Cut the umbilical cord.
- Time Constraint: The entire procedure, from donor euthanasia to the initiation of pup breathing, must be completed within 5 minutes to ensure viability and sterility.
Protocol B: Traditional C-Section (T-CS) - Control Method
Principle: The conventional method for obtaining pups via C-section, used as a benchmark for comparison.
Pre-Surgical and Isolator Setup: Identical to Protocol A (FRT-CS).
Surgical Procedure (T-CS):
- Steps 1 and 2 are identical to FRT-CS.
- Apply clamps at two locations: both at the base of the cervix and at the top of the uterine horn.
- Exteriorize the uterus and proceed with pup extraction and resuscitation as described in Steps 5-10 of Protocol A.
Workflow and Logical Relationship Diagram
The following diagram illustrates the logical sequence and critical decision points in the C-section derivation process for obtaining germ-free mice, highlighting the key difference between the T-CS and FRT-CS techniques.
Diagram 1: Germ-Free Mouse Derivation Workflow. This flowchart outlines the complete C-section procedure, with the key differential step being the surgical technique (T-CS vs. FRT-CS) that directly influences the fetal survival outcome.
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials
| Item | Specification / Function |
|---|---|
| SPF Donor Mice | C57BL/6, BALB/c, or other desired strains. Confirmed free of pathogenic bacteria, viruses, and parasites [8]. |
| Germ-Free Foster Mothers | BALB/c and NSG strains have shown superior nursing and weaning success [8]. |
| Sterile Isolator | Polyvinyl chloride (PVC) isolator; provides a sterile environment for pup derivation and housing [8]. |
| Disinfectant | Chlorine dioxide (e.g., Clidox-S); used for surface sterilization of the donor and the isolator entry port [8]. |
| Heating Pad | Maintains isolator interior at 40–45°C pre- and post-surgery to prevent fatal pup hypothermia [8]. |
| Surgical Instruments | Fine scissors, forceps, and clamps; must be autoclaved (121°C for 1200s) prior to use [8]. |
| Bedding & Food | Sterile aspen wood shavings and autoclavable diet (e.g., Labdiet 5CJL) [8]. |
| Sterile Swabs | For wiping amniotic fluid from pups to stimulate breathing [8]. |
The implementation of the FRT-CS protocol represents a significant refinement in the production of germ-free mice. By preserving the female reproductive tract during surgery, researchers can achieve a marked improvement in fetal survival rates compared to the traditional T-CS method. This optimized technique enhances experimental reproducibility and efficiency, which is critical for advancing research in microbiome studies and genetic engineering.
Within the broader research on Female Reproductive Tract-preserved Cesarean Section (FRT-CS) protocols, the selection of an optimal germ-free (GF) foster mother is a critical determinant of pup survival and weaning success. This application note summarizes a systematic evaluation of the maternal capabilities of four mouse strains—BALB/c, NSG, C57BL/6J, and the outbred KM—when serving as GF foster mothers. Quantitative data demonstrates significant strain-specific disparities in weaning rates, with BALB/c and NSG strains exhibiting superior performance. The accompanying detailed protocols provide a reliable framework for implementing the optimized FRT-CS technique and for the subsequent assessment and selection of foster mothers, aiming to enhance the efficiency and reproducibility of GF mouse colony derivation.
The generation of germ-free (GF) mice via sterile cesarean section is a cornerstone technique for microbiome and immunology research. The "sterile womb hypothesis" underpins this method, positing that the placental barrier maintains the fetus in a sterile intrauterine environment, allowing for the derivation of GF pups via C-section [21]. While refining the surgical technique (specifically, the Female Reproductive Tract-preserved C-section or FRT-CS) is crucial for improving fetal survival, the role of the GF foster mother is equally vital. Upon transfer into the sterile isolator, the cesarean-derived pups are entirely dependent on the foster mother for warmth, nutrition, and protection. Consequently, the strain of the foster mother, with its inherent behavioral and physiological characteristics, directly impacts pup survival and weaning rates. This application note details the comparative efficacy of different mouse strains in this role, providing evidence-based guidance for researchers.
Key Quantitative Findings: Strain-Specific Weaning Success
The comparative analysis of maternal care among the four GF foster strains revealed profound differences in their ability to successfully nurse and wean pups.
Table 1: Weaning Success Rates of Different GF Foster Mother Strains
| Foster Mother Strain | Strain Type | Reported Weaning Success | Relative Performance |
|---|---|---|---|
| BALB/c | Inbred | Superior | High |
| NSG | Inbred | Superior | High |
| KM | Outbred | Moderate | Intermediate |
| C57BL/6J | Inbred | Lowest | Low |
The data indicates that BALB/c and NSG strains are the most reliable choices, demonstrating superior nursing capabilities and resulting in higher weaning success under GF conditions. This finding is particularly notable for C57BL/6J, as its poor performance as a GF foster mother contrasts with reports of adequate maternal care in specific pathogen-free (SPF) conditions, highlighting the significant impact of the germ-free environment on maternal behavior [21].
Detailed Experimental Protocols
Protocol: Female Reproductive Tract-Preserved C-Section (FRT-CS)
This optimized surgical technique is designed to maximize fetal survival during derivation [21].
I. Principle The FRT-CS technique minimizes trauma and bleeding by selectively clamping only the cervix base, thereby preserving the integrity of the entire female reproductive tract (ovaries, uterine horns, and cervix) during pup extraction.
II. Materials and Reagents
- Pregnant SPF donor female mouse (e.g., C57BL/6, timed-pregnant)
- Disinfectant solution (e.g., Clidox-S)
- Sterile surgical instruments (fine scissors, forceps, clamps)
- Heating pad (pre-heated to 40-45°C)
- Sterile swabs
- Sterile polyvinyl chloride (PVC) isolator
III. Procedure
- Euthanize the pregnant donor female via cervical dislocation.
- Saturate the abdominal fur with disinfectant.
- Perform a midline laparotomy to expose the abdominal cavity.
- Identify the uterine horns. In FRT-CS, place a clamp only at the cervix base. (In the traditional T-CS method, clamps are placed at both the cervix and the top of each uterine horn).
- Excise the entire reproductive tract distal to the cervical clamp.
- Immediately transfer the excised tract into the sterile isolator, ensuring minimal exposure to the non-sterile environment.
- Within the isolator, use sterile instruments to incise the uterine sac and amniotic membrane to expose each pup.
- Gently wipe the pup's face and body with a sterile swab to clear amniotic fluid until spontaneous breathing is noted.
- Cut the umbilical cord.
- Transfer the resuscitated pups to a pre-warmed cage containing a proven GF foster mother.
- Critical Step: The entire procedure, from euthanasia to pup transfer into the isolator, must be completed within 5 minutes to ensure pup viability and maintain sterility.
The following workflow diagram illustrates the key decision points and steps in the optimized FRT-CS protocol compared to the traditional method.
Protocol: Evaluating Foster Mother Maternal Capability
This protocol outlines the procedure for assessing and comparing the weaning success of different GF foster strains.
I. Principle The efficacy of a GF foster mother is quantitatively determined by her ability to accept cesarean-derived pups and nurse them through to successful weaning.
II. Materials and Reagents
- GF female mice of strains to be tested (e.g., BALB/c, NSG, C57BL/6J, KM)
- Pups derived via FRT-CS (as per Protocol 3.1)
- Sterile mouse cages, bedding, food, and water within PVC isolators
III. Procedure
- Prepare Foster Mothers: Use GF foster mothers that are approximately four months old and have had at least one successful prior pregnancy to ensure maternal experience [21].
- Time Pup Transfer: Introduce the FRT-CS-derived pups to the foster mother immediately after resuscitation and drying within the sterile isolator.
- Monitor Litters: Observe the foster mother and litter daily for the first critical week. Key observations include:
- Nesting behavior and whether pups are grouped within the nest.
- Presence of milk spots in pup stomachs (indicating feeding).
- Audible vocalizations from pups.
- Quantify Success: Track the number of pups weaned (typically at 21 days of age) from the initial number transferred.
- Calculate Weaning Rate: For each strain, calculate the weaning success rate as:
(Number of Pups Weaned / Number of Pups Transferred) * 100%.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Materials for FRT-CS and Foster Mother Studies
| Item | Function/Application | Example/Note |
|---|---|---|
| Clidox-S | Sterilizing disinfectant | Used for surface sterilization of the excised uterine tract before transfer into the isolator [21]. |
| SPF Donor Mice | Source of embryos/pups | Timed-pregnant females (e.g., C57BL/6, BALB/c) for C-section [21]. |
| GF Foster Mice | Rearing cesarean-derived pups | BALB/c, NSG, KM, C57BL/6J strains for comparative evaluation of maternal care [21]. |
| PVC Isolator | Sterile housing environment | Maintains a germ-free barrier for foster mothers and derived pups [21]. |
| Sterile Surgical Kit | Performing C-section | Fine scissors, forceps, and clamps for precise dissection [21]. |
The data presented confirms that the efficacy of GF foster mothers is highly strain-specific. The superior performance of BALB/c and NSG strains makes them the recommended choice for maximizing the efficiency of GF mouse production pipelines. In contrast, the C57BL/6J strain, despite its widespread use in many research domains, should be avoided for this particular application under GF conditions.
The integration of the optimized FRT-CS surgical protocol, which improves fetal survival, with the strategic selection of a high-performance foster strain, such as BALB/c or NSG, creates a robust and reliable system. This combined approach directly addresses key challenges in germ-free mouse production, namely variability in yield and pup loss, thereby enhancing experimental reproducibility and accelerating research timelines in microbiome and immunology studies.
The Female Reproductive Tract Preserved C-section (FRT-CS) protocol represents a significant refinement in the methodology for generating and maintaining germ-free (GF) mouse colonies. Within the broader thesis on FRT-CS protocol research, this document details the application notes and protocols that underpin its long-term advantages. For biomedical research, the integrity of animal models is paramount. Germ-free mice serve as an irreplaceable tool for studying host-microbiome interactions, human health, and disease [8]. The efficiency of generating and, crucially, recovering these colonies following accidental contamination directly impacts the pace and reproducibility of scientific discovery. This protocol establishes that optimizing the initial derivation technique yields substantial dividends in sustained colony health, resilience against contamination events, and the overall reliability and reproducibility of research data.
The implementation of the FRT-CS protocol, combined with strategic foster strain selection, demonstrates measurable superiority over traditional cesarean section (T-CS) techniques. The data below summarize key performance metrics.
Table 1: Comparison of Cesarean Section Techniques on Pup Survival and Sterility
| Technique | Fetal Survival Rate | Sterility Maintenance | Key Technical Feature |
|---|---|---|---|
| Traditional C-section (T-CS) | Baseline | Effective | Clamps placed at cervix base and top of uterine horn. |
| FRT-CS | Significantly Improved [8] | Effective (No significant contamination) [8] | Clamps only cervix base, preserving entire reproductive tract (ovary, uterine horn, uterine junction, cervix). |
Table 2: Impact of Foster Mother Strain on Weaning Success in Germ-Free Mice
| Foster Mother Strain | Strain Type | Weaning Success | Maternal Care Profile |
|---|---|---|---|
| C57BL/6J | Inbred | Lowest weaning rate [8] | Contrasts with SPF findings; less suitable as GF foster. |
| BALB/c | Inbred | Superior [8] | Superior nursing and weaning success. |
| NSG | Inbred | Superior [8] | Superior nursing and weaning success. |
| KM | Outbred | Good | Robust maternal care. |
Table 3: Donor Conception Method and Its Impact on Germ-Free Production
| Conception Method | Delivery Date Control | Experimental Reproducibility | Application Note |
|---|---|---|---|
| Natural Mating (NM) | Variable; difficult to predict precisely [8] | Lower due to variability | Requires monitoring for vaginal plugs and natural delivery. |
| In Vitro Fertilization (IVF) | Precise control [8] | Enhanced [8] | Enables scheduled, pre-labor FRT-CS on a predictable date. |
Experimental Protocols
Protocol: Female Reproductive Tract Preserved C-Section (FRT-CS) for Germ-Free Mouse Derivation
Principle: To aseptically deliver fetuses from a specific pathogen-free (SPF) donor mouse into a germ-free environment while minimizing surgical trauma and maximizing neonatal survival by preserving the integrity of the female reproductive tract.
Materials:
- Pregnant SPF donor mouse (e.g., C57BL/6 or BALB/c) at gestation day 18.5 (G18.5) or as determined by IVF schedule.
- Germ-free foster mother (optimally BALB/c or NSG strain) with synchronized lactation.
- Sterile surgical instruments (fine scissors, forceps, clamps).
- Germ-free isolator or transfer chamber.
- Disinfectant solution (e.g., Clidox-S, freshly prepared 1:3:1 dilution) [8].
- Sterile swabs, heating pad (pre-heated to 40-45°C).
- Sterile transport container.
Procedure:
- Euthanasia and Preparation: Euthanize the pregnant SPF donor mouse via cervical dislocation. Saturate the abdominal fur with disinfectant to minimize contamination risk.
- Aseptic Laparotomy: Perform a midline laparotomy under strict aseptic conditions to expose the abdominal cavity and the uterine horns.
- FRT-CS Clamping: Identify the cervix and the uterine horns. Apply a clamp only at the base of the cervix. This is the critical step that differentiates FRT-CS from T-CS. Do not place a second clamp at the top of the uterine horn.
- Uterine Excision: Excise the entire uterine horn complex by cutting above the single cervical clamp. This preserves the ovary, uterine horn, uterine junction, and cervix in a continuous tract.
- Disinfection and Transfer: Immediately immerse the excised uterus in a sterile container filled with disinfectant (e.g., Clidox-S) for the prescribed contact time. Rapidly transfer the container into the sterile isolator.
- Isolator Procedure: Inside the germ-free isolator: a. Place the uterus on a sterile surface. b. Carefully incise the uterine wall and amniotic sac with sterile scissors to expose each pup. c. Gently wipe the pup's face and body with a sterile swab to clear amniotic fluid until spontaneous breathing is noted. d. Cut the umbilical cord.
- Fostering: Immediately present the pups to the synchronized GF foster mother. The entire procedure, from donor euthanasia to fostering inside the isolator, must be completed within 5 minutes to ensure pup viability and sterility [8].
Protocol: Integration of In Vitro Fertilization (IVF) with FRT-CS
Principle: To achieve precise temporal control over the birth of GF pups, thereby enhancing scheduling efficiency and experimental reproducibility.
Procedure:
- IVF and Embryo Transfer: Perform IVF using oocytes and sperm from the desired SPF donor strains. Transfer the resulting two-cell stage embryos into a pseudo-pregnant SPF recipient female (e.g., CD-1 strain). This day is designated as embryonic day 0.5 (E0.5) [8].
- Scheduled FRT-CS: On the predicted delivery date (typically E19.5 for mice), perform the FRT-CS protocol as described in 3.1. This pre-empts natural labor, allowing for precise scheduling and eliminating the variability associated with natural mating and birth timing.
Protocol: Contamination Recovery and Colony Redeivation
Principle: To rapidly re-establish a germ-free colony following a contamination event in a GF facility, minimizing downtime and loss of valuable genetic lines.
Procedure:
- Immediate Action: Upon detection of contamination, isolate the affected isolator.
- Donor Preparation: Quickly set up mating or, preferably, IVF for the mouse strain that needs to be recovered. Using SPF donors as embryos or pregnant dams is the foundation for rederivation.
- Emergency FRT-CS: Execute the FRT-CS protocol under emergency conditions. The optimized survival rates of FRT-CS are critical here, as the number of viable pups obtained directly determines the speed of colony recovery.
- Fostering to Resilient GF Strain: Foster the derived pups to a proven GF foster strain with high weaning success, such as BALB/c or NSG, to maximize the number of animals that reach breeding age.
- Re-establishment: Breed the successfully weaned GF mice to re-establish the breeding colony within the sterile environment.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Reagents for FRT-CS Protocol Implementation
| Item | Function/Application | Protocol Specifics |
|---|---|---|
| Chlorhexidine Gluconate (2% Alcohol-based) | Pre-operative skin antisepsis for donor. Proven most effective at reducing surgical site infections [40]. | Apply as recommended for surgical skin preparation prior to laparotomy. |
| Clidox-S | High-level disinfectant for sterilizing the exterior of the excised uterus during transfer into the isolator [8]. | Use fresh 1:3:1 dilution, activate for 15 min before use [8]. |
| Sterile Transport Medium (Amies) | Preserves viability of bacterial samples if post-procedure sterility testing is required [41]. | Not for the pups; used for swabbing isolator surfaces to test for contamination. |
| Get Active Questionnaire for Pregnancy (GAQ-P) | Research tool for assessing physical activity levels in studies on long-term maternal health post-CS [42]. | Used in longitudinal studies, not in the acute FRT-CS procedure itself. |
Workflow and Pathway Diagrams
Within the overarching research on Female Reproductive Tract Preserved C-section protocols, the method of uterine incision closure is a critical determinant of long-term reproductive health. A cesarean section represents a significant injury to the uterus, an organ whose function depends on cyclical regeneration and the capacity to sustain pregnancy. The technique used for hysterotomy closure profoundly influences the quality of scar healing, which in turn affects risks of secondary infertility, pain, uterine rupture, and abnormal placentation in subsequent pregnancies [43]. This application note synthesizes contemporary surgical research to provide evidence-based protocols aimed at optimizing uterine scar integrity and preserving future uterine function, a cornerstone of advanced reproductive surgical science.
Quantitative Analysis of Closure Techniques and Outcomes
Robust clinical studies have quantitatively compared the long-term efficacy of various uterine closure techniques. The primary metrics for assessing scar healing include Residual Myometrial Thickness (RMT) and the incidence of Cesarean Scar Defects (CSD) or isthmoceles, which are indentations at the scar site with a depth of at least 2 mm [44]. Transvaginal ultrasound (TVU) is the standard non-invasive modality for these evaluations in non-pregnant women [45].
Table 1: Comparative Outcomes of Uterine Closure Techniques from Randomized Controlled Trials
| Closure Technique | Residual Myometrial Thickness (RMT) (mm) | Isthmocele/CSD Rate | Postmenstrual Spotting | Key Study Findings |
|---|---|---|---|---|
| Double-Layer, Far-Far-Near-Near (FFNN) Unlocked [46] | Significantly greater than control group (p<0.001) | Less frequent (p<0.001) | Less common (p=0.002) | Superior protection from isthmocele formation; sufficient RMT; no significant difference in operative time or blood loss. |
| Single-Layer Continuous Locked (SLL) [46] | Significantly lower than FFNN group (p<0.001) | More frequent (p<0.001) | More common | Associated with higher rates of defective scar healing. |
| Purse-String Uterine Suture (PSUS) [44] | Not significantly increased vs. comparator | Lower rate than comparator | Not specified | Better uterine scar healing ratio; required fewer threads and hemostatic sutures; operative time and blood loss were similar. |
| Double-Layer Continuous Unlocked Suture (DLCUS) [44] | Not significantly increased vs. PSUS | Higher rate than PSUS | Not specified | Active comparator in PSUS trial. |
The impact of defective healing extends beyond imaging findings. A study of 546 non-pregnant women found that those with clinical symptoms like postmenstrual spotting had a significantly lower mean TRM (3.22 ± 2.33 mm) compared to asymptomatic women (5.39 ± 3.34 mm) [45]. Furthermore, a TRM of 4.15 mm was established as a cut-off value for predicting CSD, with a sensitivity of 87.8% and specificity of 71.3% [45].
Detailed Experimental Protocols for Scar Assessment
The following protocols outline standardized methodologies for evaluating uterine scar healing, essential for generating reproducible research data.
Protocol 1: Transvaginal Ultrasound Evaluation of the Uterine Scar in Non-Pregnant Women
Application: This protocol is used for the primary assessment of uterine scar healing in a non-pregnant state, typically conducted 6-12 months post-cesarean delivery [46] [45].
Materials:
- Color Ultrasonic Diagnostic Apparatus: Equipped with a 4–9 MHz transvaginal probe (e.g., Philips iU22, Philips HD15, GE E8) [45].
- Data Collection Form: For recording measurements and patient history.
Methodology:
- Patient Preparation: The patient is placed in the lithotomy position. The transvaginal probe is prepared with a protective cover and ultrasonic gel.
- Image Acquisition: The sonographer, blinded to the patient's obstetric history, performs a scan in the sagittal plane. The cervix, uterus, and adnexa are examined.
- Scar Identification: The cesarean scar is identified in the lower uterine segment as a hypoechoic area.
- Measurement:
- Cesarean Scar Defect (CSD): If a CSD is present, measure its dimensions in the sagittal plane: anterior–posterior (depth) and cephalad–caudal (length). Measure transversely in the coronal plane for width.
- Residual Myometrial Thickness (RMT): Measure the thickness of the myometrium between the serosal surface of the uterus and the apex of the defect (or at the scar site if no defect is visible) [45].
- Data Recording: Take three different measurements for each parameter (length, width, depth, RMT) and calculate the mean value for analysis. Record the uterine position (anterior, meso-, retroverted) and the presence of fluid within the scar.
Protocol 2: Surgical Repair of the Uterine Incision (3-Layer Anatomical Closure)
Application: This refined protocol for hysterotomy closure is based on the principle of restoring anatomical integrity by reapproximating uterine layers while excluding the endometrium, which produces stronger scars and reduces long-term complications [43].
Materials:
- Suture: Delayed absorbable suture, such as Polyglactin 910 (Vicryl) size 0 or 1 [47].
- Standard Cesarean Section Surgical Tray.
Methodology:
- First Layer (Deep Layer): Approximate the decidua and junctional myometrium using a continuous, unlocked suture. Crucially, exclude the surface endometrium from the suture line to prevent tissue entrapment and bacterial contamination, which can lead to impaired healing and niche formation [43].
- Second Layer (Myometrial Reinforcement): Reapproximate the bulk of the myometrium using a continuous, unlocked suture. This layer restores anatomic wall integrity, reinforces strength, and distributes tension across the scar [43].
- Third Layer (Serosal Layer): Reapproximate the superficial myometrium and serosa with a continuous suture. This final layer smooths the uterine surface, reducing the potential for adhesion formation [43].
Signaling Pathways and Technical Relationships in Uterine Healing
The following diagram illustrates the conceptual relationship between surgical technique decisions and their long-term outcomes on uterine scar integrity, highlighting the critical pathway for achieving reproductive tract preservation.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Uterine Scar Healing Research
| Research Tool | Specifications / Examples | Primary Function in Experimental Protocol |
|---|---|---|
| High-Resolution Transvaginal Ultrasound System | Philips iU22, GE E8; with 4-9 MHz transvaginal probe [45] | Non-invasive in vivo imaging and morphometric analysis (RMT, CSD dimensions) of the uterine scar. |
| Delayed Absorbable Suture | Polyglactin 910 (Vicryl), size 0 or 1 [47] | Surgical repair of hysterotomy; provides wound support during critical healing phase before absorption. |
| Dedicated Image Analysis Software | Software bundled with ultrasound systems (e.g., Philips Q-Lab) | Quantification of ultrasound-derived metrics; 3D reconstruction of scar niche volume. |
| Standardized Data Collection Registry | Electronic Case Report Forms (eCRFs) | Systematic collection of patient demographics, surgical variables, and long-term clinical outcomes for robust data analysis. |
The pursuit of a Female Reproductive Tract Preserved C-section protocol mandates a deliberate shift from merely efficient uterine closure to anatomically precise techniques that prioritize long-term scar integrity. Evidence strongly supports that methods such as the double-layer FFNN unlocked technique and the refined 3-layer closure, which emphasize endometrial exclusion and meticulous layer re-approximation, result in greater residual myometrial thickness, lower rates of isthmocele, and reduced gynecological symptoms. The translation of these surgical principles into clinical practice, guided by standardized ultrasound assessment, is fundamental to mitigating long-term risks and safeguarding future fertility and uterine function. Future research should focus on validating novel techniques like the purse-string suture and further elucidating the cellular pathways of optimal myometrial healing.
Conclusion
The Female Reproductive Tract-Preserved Cesarean Section protocol represents a significant methodological advancement in the generation of germ-free mice. By refining surgical techniques to enhance fetal viability, integrating IVF for precise timing, and identifying optimal foster strains, the FRT-CS method directly addresses key inefficiencies in traditional approaches. The validated improvements in survival rates and experimental reproducibility make this protocol a critical tool for biomedical research, particularly in microbiome studies, immunology, and drug development. Future directions should focus on further standardizing the procedure across institutions, exploring its application in other rodent models, and investigating the long-term health impacts of this surgical modification on derived animal colonies.
References
- 1. Trusting Their Guts: OSU's germ-free mice research ... [https://news.okstate.edu/magazines/research/research-matters/articles/2024/trusting_their_guts_osus_germ-free_mice_research_identifies_new_generation_probiotics_trains_next_generation_of_scientists.html]
- 2. Germ-Free Mouse Models Core - iLab Organizer [https://cwru.corefacilities.org/service_center/show_external/5777?name=germ-free-mouse-models-core]
- 3. Cesarean Delivery - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK546707/]
- 4. C-section [https://www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655]
- 5. Spatial metabolic and phenotypic characterization of the ... [https://pubmed.ncbi.nlm.nih.gov/40760821/]
- 6. Laboratory mice engrafted with natural gut microbiota ... [https://www.nature.com/articles/s41467-025-60554-2]
- 7. Germ Free Mice Strategic Insights: Analysis 2025 and ... [https://www.archivemarketresearch.com/reports/germ-free-mice-284969]
- 8. Optimized cesarean techniques, IVF use, and foster strain ... [https://www.nature.com/articles/s41598-025-05411-4]
- 9. Can Vaginal Seeding at Birth Improve Health Outcomes of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195427/]
- 10. Enduring Behavioral Effects Induced by Birth ... [https://pubmed.ncbi.nlm.nih.gov/32822606/]
- 11. A critical assessment of the “sterile womb†and “in utero ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-017-0268-4]
- 12. The Not-so-Sterile Womb: Evidence That the Human Fetus ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.01124/full]
- 13. Maternal–to–neonatal microbial transmission and impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12573995/]
- 14. Challenging the Hypothesis of in Utero Microbiota ... [https://www.mdpi.com/2306-7381/10/5/331]
- 15. Sterilizing Practices | Infection Control [https://www.cdc.gov/infection-control/hcp/disinfection-sterilization/sterilizing-practices.html]
- 16. Sterilization Guidelines: AORN Updates for Patient Safety [https://www.aorn.org/article/sterilization--aorns-updated-guideline-for-enhanced-patient-safety]
- 17. AORN Updates Guideline for Sterilization: Key Changes to ... [https://ortoday.com/aorn-updates-guideline-for-sterilization/]
- 18. In mice, fertility treatments linked to higher mutations than ... [https://www.jax.org/news-and-insights/2025/november/in-mice-fertility-treatments-linked-to-higher-mutations-than-natural-conceptions]
- 19. Successful selection of mouse sperm with high viability and ... [https://www.nature.com/articles/s41598-020-65931-z]
- 20. Persistent Wnt signaling affects IVF embryo implantation ... [https://www.sciencedirect.com/science/article/pii/S2095927325004724]
- 21. Optimized cesarean techniques, IVF use, and foster strain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297627/]
- 22. Perimortem Caesarean section [https://litfl.com/perimortem-caesarean-section/]
- 23. RECOVER Guidelines: Newborn Resuscitation in Dogs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374490/]
- 24. RECOVER releases newborn resuscitation guidelines [https://www.dvm360.com/view/recover-releases-newborn-resuscitation-guidelines]
- 25. Strategies for perioperative hypothermia management [https://pmc.ncbi.nlm.nih.gov/articles/PMC11684272/]
- 26. Postoperative Hypothermia [https://www.accjournal.org/journal/view.php?number=1184]
- 27. Newborn Puppy Care: Managing Neonates and High-Risk ... [https://www.revivalanimal.com/learning-center/newborn-puppy-care-managing-neonates-and-high-risk-puppies?srsltid=AfmBOopuc1Dzp4-eSsdFsr3e2eOtnQp2wBy8dV7_Si9gV32KSDNgL0q0]
- 28. Predictive tool for the risk of hypothermia during ... [https://www.sciencedirect.com/science/article/abs/pii/S0301211525000089]
- 29. APSIC Guidelines for Prevention of Surgical-Site Infection [https://emedicine.medscape.com/article/188988-guidelines]
- 30. Effect of type of vaginal preparation on abdominal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615121/]
- 31. Disinfection and Sterilization in Health Care Facilities [https://pmc.ncbi.nlm.nih.gov/articles/PMC7134755/]
- 32. Testing the Effectiveness of Antiseptics and Disinfectants [https://courses.lumenlearning.com/suny-microbiology/chapter/testing-the-effectiveness-of-antiseptics-and-disinfectants/]
- 33. Guidance for Products Including or Adding Disinfectant ... [https://www.epa.gov/pesticide-analytical-methods/guidance-products-including-or-adding-disinfectant-efficacy-claims-use]
- 34. Sterilization for Medical Devices [https://www.fda.gov/medical-devices/general-hospital-devices-and-supplies/sterilization-medical-devices]
- 35. Circadian alignment in a foster mother improves the offspring's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6265554/]
- 36. Postnatal Influences on Seizure Susceptibility [https://pmc.ncbi.nlm.nih.gov/articles/PMC2778367/]
- 37. Arnold School of Public Health [https://sc.edu/study/colleges_schools/public_health/about/news/2025/periviable_jama_boghossian.php]
- 38. Lessons From the Survival of an Extremely Preterm Neonate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003553/]
- 39. Factors influencing weaning success from mechanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261150/]
- 40. Review Which antiseptic to use for a caesarean section? ... [https://www.sciencedirect.com/science/article/abs/pii/S0195670124001282]
- 41. Post-caesarean section infection burden, antimicrobial ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326935]
- 42. how cesarean section affects maternal physical activity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380563/]
- 43. Uterine closure after cesarean delivery: surgical principles ... [https://www.sciencedirect.com/science/article/pii/S0002937825007355]
- 44. Impact of purse-string uterine suture on scar healing after a ... [https://www.sciencedirect.com/science/article/abs/pii/S2589933323001349]
- 45. Evaluation of uterine by transvaginal ultrasound in 607... scar healing [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-021-01337-x]
- 46. An Optimal Uterine for Better Closure and... Technique Scar Healing [https://pubmed.ncbi.nlm.nih.gov/31070072/]
- 47. Uterine Closure in Cesarean Delivery: A New Technique [https://pmc.ncbi.nlm.nih.gov/articles/PMC3421915/]