Tissue Permeability in Biomedical Research: Mechanisms, Assessment, and Impact on Drug Development
This article provides a comprehensive analysis of the critical role tissue permeability plays in physiological function, disease pathogenesis, and therapeutic development.
Tissue Permeability in Biomedical Research: Mechanisms, Assessment, and Impact on Drug Development
Abstract
This article provides a comprehensive analysis of the critical role tissue permeability plays in physiological function, disease pathogenesis, and therapeutic development. We explore foundational concepts of paracellular and transcellular transport mechanisms across different tissue barriers, including intestinal and vascular endothelium. The content details state-of-the-art methodologies for assessing permeability in research and clinical settings, addresses common challenges in permeability modulation, and examines regulatory considerations for permeability-targeting therapies. Designed for researchers, scientists, and drug development professionals, this review synthesizes current evidence and emerging trends to inform research design and therapeutic innovation in this rapidly evolving field.
Fundamental Principles of Tissue Permeability: From Cellular Mechanisms to Systemic Impact
Tissue permeability refers to the regulated movement of substances—including fluids, ions, nutrients, and pharmaceuticals—across biological barriers formed by cellular layers. These semi-permeable barriers, primarily constituted by endothelial and epithelial cell linings, separate distinctive physiological compartments and maintain compartment-specific homeostasis [1]. The controlled passage of materials occurs through two principal pathways: the paracellular route (between adjacent cells) and the transcellular route (through the cells themselves) [2] [3]. The permeability of a tissue barrier is not a static property but is dynamically regulated by complex molecular mechanisms and can be disrupted in various disease states, leading to pathological conditions such as edema (in the case of vascular endothelium) or compromised drug absorption (in the case of intestinal epithelium) [1] [2].
The study of tissue permeability is fundamental to multiple scientific and clinical disciplines. In drug development, understanding and predicting intestinal permeability is critical for estimating the oral bioavailability of active pharmaceutical ingredients (APIs) [4] [5]. In toxicology and physiology, the breakdown of barrier function in organs like the lung or gut is a key event in inflammatory diseases [6] [2]. Consequently, accurate assessment and a deep mechanistic understanding of tissue permeability are prerequisites for advances in therapeutics and disease management.
Core Concepts and Pathways of Transport
The Paracellular Pathway
The paracellular pathway is a major route for the passive movement of water, solutes, and immune cells through the intercellular space between adjacent endothelial or epithelial cells [2]. This pathway is governed by specialized junctional complexes that bridge the cells, which together form a selectively permeable "gate" in the paracellular space [6].
- Tight Junctions (TJs): These are the most apical component of the junctional complex and represent the primary determinant of paracellular permeability. TJs are multimolecular structures composed of proteins such as claudins and occludins, which create a seal that can be tuned to allow selective passage based on size and charge [6] [3].
- Adherens Junctions (AJs): Located just below the tight junctions, AJs are crucial for initiating and maintaining cell-cell adhesion, primarily through E-cadherin proteins. They provide structural integrity to the epithelial layer and are connected to the actin cytoskeleton, playing a supportive role in barrier regulation [6].
- The Perijunctional Actomyosin Ring (PAMR): This is a contractile ring of actin and myosin filaments that is intimately associated with the TJs and AJs. The equilibrium between contractile forces generated by the PAMR and the tethering forces of the junctional complexes determines the tightness of the paracellular gate. An increase in PAMR tension, often mediated by the phosphorylation of myosin light chain (MLC), leads to junctional opening and increased permeability [2] [3].
The permeability conferred by this pathway can be experimentally enhanced by agents like ethylenediaminetetraacetic acid (EDTA), which acts as a chelator of divalent cations (e.g., Ca²âº). By sequestering these ions, EDTA disrupts the integrity of tight junctions, leading to a "bulging" of the enterocyte apex and a pronounced increase in the paracellular flux of both polar and lipophilic probes [3].
The Transcellular Pathway
The transcellular pathway involves the movement of substances directly across the cell's membrane and cytoplasm. This pathway can be passive or active and is highly dependent on the physicochemical properties of the permeating molecule [2] [3].
- Passive Diffusion: Small, nonpolar molecules can diffuse freely through the lipid bilayer of the cell membrane. The rate of this passive transcellular transport is governed by the molecule's size, lipophilicity, and polarity [7].
- Transporter-Mediated Uptake: Numerous nutrients and drugs rely on specific membrane transporters (e.g., for amino acids, sugars) to facilitate their entry into cells.
- Transcytosis: This is an active process for transporting larger molecules (such as albumin) or even entire complexes across the cell. It involves vesicle formation at one cell membrane, transport of the vesicle through the cytoplasm, and exocytosis at the opposite membrane. A key structure involved in transcytosis is the caveolae, a type of lipid raft plasma membrane microdomain enriched with the scaffolding protein caveolin-1 [2].
The transcellular pathway can be compromised by surfactants like sodium dodecyl sulfate (SDS). SDS inserts into the outer leaflet of the plasma membrane, increasing its fluidity and compromising its integrity. At the ultrastructural level, this leads to the formation of vacuoles and vesicle-like structures, which increases passive transcellular leakage and can also block constitutive endocytosis from the brush border [3].
Selective Permeability and Membrane Permeability Coefficients
The concept of selective permeability describes the ability of a biological membrane to differentiate between different types of molecules, allowing some to pass while blocking others [7]. This selectivity stems from both the intrinsic physicochemical properties of the membrane's lipid bilayer and the activity of various protein-based channels and transporters.
The permeability of a substance across a membrane can be quantified experimentally and reported as a Membrane Permeability Coefficient (MPC), typically in units of cm/s. The MPC is proportional to the molecule's partition coefficient and inversely proportional to the membrane thickness. The table below summarizes the vast range of MPCs for different types of compounds, illustrating the basis for selective permeability [7].
Table 1: Membrane Permeability Coefficients for Various Compounds
| Compound | Membrane Permeability Coefficient (cm/s) | Relative Permeability |
|---|---|---|
| Hexanoic Acid | 0.9 | Very High |
| Acetic Acid | 0.01 - 0.001 | Moderate |
| Water | 0.01 - 0.001 | Moderate |
| Ethanol | 0.01 - 0.001 | Moderate |
| Sodium Ion (Naâº) | 10â»Â¹Â² | Very Low |
Quantitative Assessment of Tissue Permeability
Key Quantitative Parameters
The permeability of tissue barriers is characterized using specific, measurable parameters that allow for the comparison of different barriers, substances, and experimental or pathological conditions.
Table 2: Key Quantitative Parameters in Tissue Permeability Studies
| Parameter | Description | Typical Units | Application & Significance |
|---|---|---|---|
| Membrane Permeability Coefficient (MPC) | The rate of simple diffusion of a solute across a membrane. | cm/s | A fundamental biophysical property used to compare intrinsic permeability of different molecules [7]. |
| Apparent Permeability (P_app) | The measured permeability of a compound across a cellular barrier (e.g., Caco-2 monolayer). Often reported as log P_app. | cm/s | A standard metric in drug development for predicting human intestinal absorption [4]. |
| Human Intestinal Absorption (HIA) | The percentage of an orally administered dose that is absorbed through the intestinal wall. | % | A direct physiological and clinical endpoint; compounds with >85% HIA are classified as highly permeable [4]. |
| Elimination Half-Life | The time required for the plasma concentration of a substance to reduce by half. | hours (h) | A key pharmacokinetic parameter indicating the persistence of a compound in the body, influenced by its distribution and clearance [8]. |
| Volume of Distribution (Vd) | A theoretical volume that a drug would need to occupy to achieve the current blood concentration. | L/kg | Reflects the extent of a drug's distribution into tissues; a high Vd suggests extensive tissue penetration beyond the plasma compartment [8]. |
In Vivo Pharmacokinetic and Tissue Distribution Studies
In vivo studies provide the most physiologically relevant data on tissue permeability and barrier penetration. These studies involve administering a compound to a live animal and then measuring its concentration over time in the blood (pharmacokinetics) and in various harvested tissues (tissue distribution).
A recent study on Ginsenoside Rh3 (GRh3) in rats provides a clear example. Researchers used a validated LC-MS/MS method to quantify GRh3 after oral administration. The study revealed that GRh3 had a prolonged elimination half-life of 14.7 ± 1.7 hours and a high volume of distribution of 280.4 ± 109.3 L/kg, indicating extensive tissue penetration. The tissue distribution analysis at the time of peak plasma concentration (T~max~) showed the highest levels in the intestine, stomach, and liver. Critically, it demonstrated that GRh3 could cross the blood-brain barrier, with significant accumulation in the hippocampus (520.0 ng/g), suggesting potential for central nervous system activity [8].
Table 3: Tissue Distribution of Ginsenoside Rh3 in Rats Following Oral Administration (100 mg/kg)
| Tissue | Concentration (ng/g) |
|---|---|
| Intestine | 15445.2 |
| Stomach | 2906.7 |
| Liver | 1930.8 |
| Hippocampus | 520.0 |
| Other Tissues (e.g., kidney, lung, heart, spleen) | Analyzed, specific values not listed in excerpt |
Experimental Models and Methodologies
In Vitro and Ex Vivo Models
A variety of models are employed to study tissue permeability in a controlled setting, each with its own advantages and limitations.
- Cell-Based Monolayers:
- Caco-2: A human colorectal adenocarcinoma cell line that, upon differentiation, forms a monolayer with morphology and functionality similar to human enterocytes. It is the most widely used in vitro model for predicting human intestinal permeability and is recommended by regulatory agencies [4] [5].
- MDCK & LLC-PK1: Canine and porcine kidney epithelial cell lines, respectively, also used for permeability screening [4].
- Parallel Artificial Membrane Permeability Assay (PAMPA): This is a non-cell-based, high-throughput assay that uses an artificial membrane to measure passive transcellular permeability [4].
- Mucosal Explant Systems: Cultured intestinal mucosal tissues, as used in studies with SDS and EDTA, offer a more in-vivo-like environment than simple cell lines while remaining simpler than whole-animal models. They allow for easy visualization of probe uptake and differentiation between paracellular and transcellular mechanisms [3].
- Membrane Insert Systems with Engineered Tissues: Advanced systems cultivate skin or other tissue models on permeable membrane inserts. A specific protocol uses 96-well or 12-well Transwell systems to determine permeability coefficients for fluorescently-labeled substances directly in the insert, providing a compact and cost-effective alternative to larger systems like the Franz diffusion cell [9].
Key Experimental Protocols
Protocol: Permeability Measurement in Membrane Insert Systems
This protocol, adapted from a 2018 study, details a method for determining permeability coefficients in small membrane-insert systems, suitable for engineered skin or mucosal models [9].
- Sample Preparation:
- For a collagen gel barrier, mix 125 µL of HBSS with 1 mL of 0.4% collagen R solution on ice.
- Titrate with ~6 µL of 1 M NaOH until the color of phenol red changes from yellow to red.
- Add 125 µL of DMEM + 10% FCS and mix carefully.
- Apply 28.6 µL of the collagen gel to the membrane of a 96-well membrane insert system (4.26 mm diameter).
- Incubate at 37°C, 5% CO₂ for 30 min to allow polymerization.
- Permeation Experiment:
- Apply the donor substance (e.g., fluorescent tracer like sodium fluorescein) in solution to the top (apical side) of the sample.
- Ensure the bottom (basolateral) chamber is filled with an appropriate acceptor medium.
- Incubate the system at a constant temperature (e.g., 37°C).
- Sample Collection and Analysis:
- At predetermined time points, measure the concentration of the permeated substance in the acceptor chamber using a method suitable for the tracer (e.g., fluorescence plate reader).
- Data Calculation:
- The permeability coefficient can be calculated from the time-dependent concentration change in the acceptor compartment. Supporting simulations using computational fluid dynamics can be used to fit the experimental data and determine the diffusion coefficient [9].
Protocol: Differentiating Paracellular vs. Transcellular Pathways in Mucosal Explants
This protocol uses fluorescent probes to visually distinguish the mechanism of action of permeation enhancers in a porcine jejunal mucosal explant system [3].
- Tissue Preparation:
- Surgically remove segments of porcine jejunum and place in ice-cold RPMI medium.
- Excise small mucosal specimens (~0.1 g) and transfer them to metal grids in organ culture dishes with 1 mL of RPMI medium.
- Treatment and Incubation:
- Pre-incubate explants for 15 minutes at 37°C.
- Add the permeation enhancer (e.g., 0.05% SDS for transcellular study, 0.05% EDTA for paracellular study) along with fluorescent probes to the culture medium.
- Key Probes: Lucifer Yellow (small polar), Texas Red-conjugated dextrans of varying sizes (3kDa, 70kDa), and lipophilic FM dyes (e.g., FM 1–43).
- Culture the explants with probes for 1 hour at 37°C.
- Post-Incubation Processing:
- Rinse explants carefully in fresh medium.
- Fix overnight in 4% paraformaldehyde at 4°C.
- Cryoprotect by immersing in 25% sucrose overnight, then embed and section (~7 µm thickness) using a cryostat.
- Visualization and Analysis:
- Analyze sections using fluorescence microscopy.
- Expected Outcomes:
- EDTA (Paracellular): Increased paracellular flux is visualized as distinct stripy lateral staining of enterocytes and accumulation of probes (including larger dextrans) in the lamina propria. It may also cause a loss of cell polarity.
- SDS (Transcellular): Renders cell membranes leaky to small polar tracers and conspicuously blocks constitutive endocytosis. It causes vacuolization at the ultrastructural level.
In Silico and AI-Based Prediction Models
Computational approaches are increasingly important for predicting permeability, especially in early drug discovery. Quantitative Structure-Permeability Relationship (QSPR) models use machine learning to predict permeability based on molecular descriptors derived from a compound's chemical structure [4].
A recent advanced approach used an Artificial Intelligence (AI)-based system—a hierarchical combination of classification and regression models—to predict Human Intestinal Absorption (HIA) for compounds with serotonergic activity. This system widened the space of molecules classified as highly permeable with high accuracy and, in external validation, correctly selected 38% of highly permeable molecules without any false positives. Such AI-based tools represent a promising strategy for in silico screening of oral drug candidates at early development stages [4].
Molecular Regulation and Signaling Pathways
The permeability of tissue barriers is dynamically regulated by a complex interplay of signaling pathways that control the cytoskeleton and intercellular junctions.
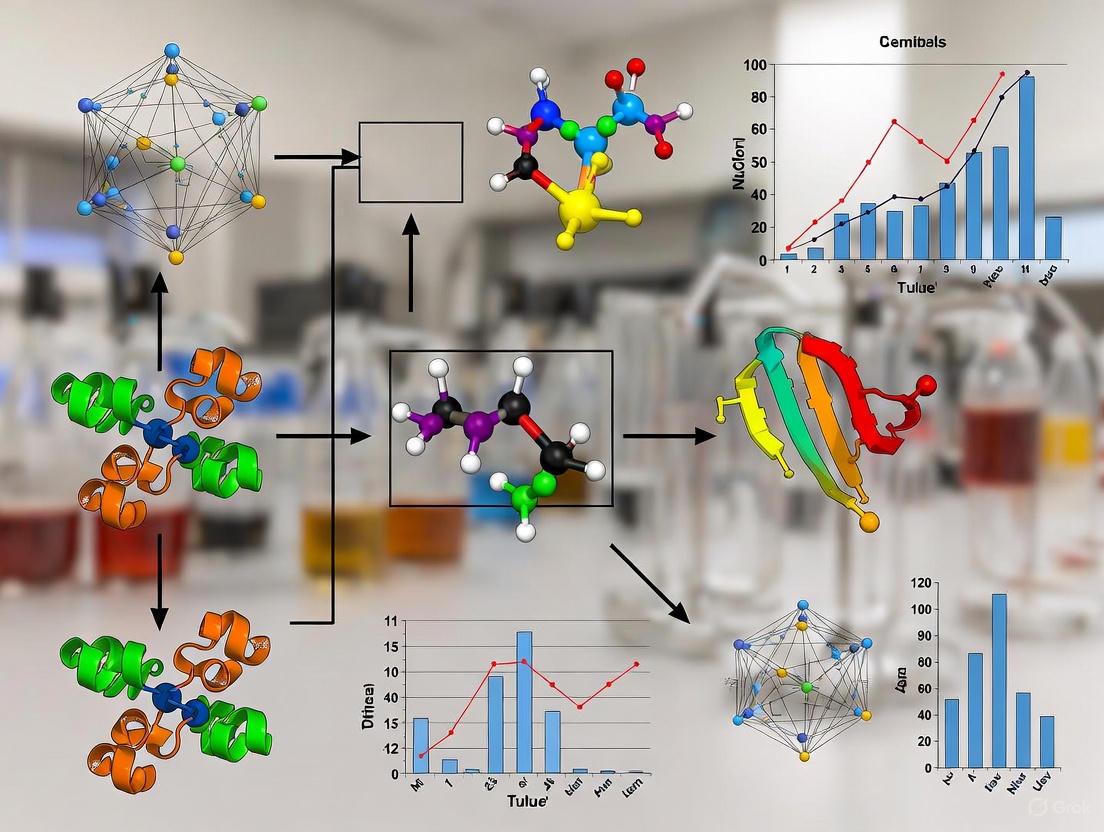
Diagram Title: Signaling Pathways in Endothelial Barrier Regulation
The diagram above illustrates the core signaling pathways that regulate endothelial permeability, particularly in the context of conditions like Acute Lung Injury (ALI) [2].
Barrier-Disruptive Signaling (Red):
- Edemagenic Agonists such as thrombin, lipopolysaccharide (LPS), or tumor necrosis factor-α (TNF-α) trigger the pathway.
- They lead to microtubule (MT) destabilization, either directly or through activation of histone deacetylase 6 (HDAC6), which deacetylates tubulin.
- Microtubule disassembly releases the Rho-specific guanine nucleotide exchange factor GEF-H1.
- GEF-H1 activates the small GTPase RhoA, which in turn activates its effector ROCK (Rho-associated protein kinase).
- ROCK promotes the phosphorylation of Myosin Light Chain (MLC), which increases the tension of the Perijunctional Actomyosin Ring (PAMR).
- This contraction pulls apart the tight and adherens junctions, resulting in increased paracellular permeability [2].
Barrier-Protective Signaling (Green):
- Conversely, microtubule stabilization (e.g., by the drug paclitaxel or by tubulin acetylation) promotes activation of the small GTPase Rac1.
- Rac1 activation generally opposes RhoA signaling and promotes barrier enhancement and restoration. Factors that increase cAMP or inhibit HSP90 and p38 MAPK also exert their barrier-protective effects partly through MT stabilization [2].
The Scientist's Toolkit: Key Research Reagents and Models
Table 4: Essential Reagents and Models for Tissue Permeability Research
| Tool Name | Type | Function & Application |
|---|---|---|
| Caco-2 Cell Line | In Vitro Model | Gold-standard human cell line for predicting intestinal drug permeability and absorption studies [4] [5]. |
| Transwell / Membrane Insert Systems | Experimental Apparatus | Permeable supports for cultivating cell monolayers or tissue models to study directional solute flux (e.g., apical-to-basolateral) [9]. |
| Sodium Dodecyl Sulfate (SDS) | Transcellular Permeation Enhancer | Surfactant used to investigate transcellular transport pathways by perturbing plasma membrane integrity [3]. |
| Ethylenediaminetetraacetate (EDTA) | Paracellular Permeation Enhancer | Chelator of divalent cations used to disrupt tight junctions and study the paracellular transport pathway [3]. |
| Fluorescent Tracers (e.g., Lucifer Yellow, FITC-Dextrans) | Research Reagents | A suite of probes of varying size and charge used to visualize and quantify permeability across biological barriers and determine pore sizes [9] [3]. |
| LC-MS/MS (Liquid Chromatography-Tandem Mass Spectrometry) | Analytical Instrument | Highly sensitive and specific technology for quantifying drug concentrations in complex biological matrices (e.g., plasma, tissue homogenates) for pharmacokinetic and tissue distribution studies [8]. |
| GEF-H1, RhoA/ROCK, MLC Pathway Inhibitors | Pharmacological/Signaling Tools | Chemical inhibitors (e.g., ROCK inhibitor Y-27632) used to dissect the molecular mechanisms controlling actomyosin-based contraction and paracellular permeability [2]. |
| HDAC6 Inhibitors (e.g., Tubastatin A) | Pharmacological/Signaling Tools | Used to investigate the role of microtubule acetylation and stability in maintaining endothelial barrier function; potential therapeutic agents for ALI/ARDS [2]. |
| Rat CGRP-(8-37) | Rat CGRP-(8-37), MF:C138H224N42O41, MW:3127.5 g/mol | Chemical Reagent |
| 1-Monomyristin | 1-Monomyristin, CAS:27214-38-6, MF:C17H34O4, MW:302.4 g/mol | Chemical Reagent |
The permeation of substances across cellular barriers is a fundamental process in physiology and drug development. Two primary pathways facilitate this movement: the paracellular and transcellular routes. The paracellular pathway involves the transport of substances between adjacent cells, passing through intercellular spaces sealed by tight junctions [10] [11]. In contrast, the transcellular pathway involves the transport of substances through the cell, requiring translocation across both the apical and basolateral membranes [12] [13]. The distinct structural components, regulatory mechanisms, and functional characteristics of these pathways collectively define the permeability of biological tissues, a critical parameter in therapeutic agent absorption and distribution. Within the context of WISH background research, a precise understanding of these pathways is paramount for predicting drug bioavailability and designing novel delivery strategies that can navigate or modulate biological barriers.
Core Structural and Mechanistic Distinctions
The paracellular and transcellular pathways are distinguished by their unique architectural designs and the physical forces that govern solute movement.
The Paracellular Pathway
This is a passive, energy-independent process where solutes move diffusively through the intercellular space, driven by concentration, osmotic, or electrochemical gradients [10] [11]. The rate-limiting step is passage through the tight junction (TJ), a multi-protein complex that forms a selective seal at the most apical part of the intercellular space [12] [11]. The TJ's barrier and pore functions are defined by specific transmembrane proteins, primarily claudins and occludin, which form a branching network of strands [10] [11]. These strands are anchored intracellularly to the actin cytoskeleton via plaque proteins like ZO-1, allowing for dynamic regulation [11]. The paracellular pathway is generally size-selective and charge-selective. It is most relevant for small, hydrophilic molecules (typically under 0.6 kDa) and demonstrates a preference for cations over anions due to the net negative charge of the tight junctions [10] [11].
The Transcellular Pathway
This pathway entails solute traversal across the cell's membrane structures. Transcellular transport can occur via several mechanisms, which can be either passive or active [13] [14]:
- Passive Transcellular Diffusion: A passive process where lipophilic solutes dissolve into and diffuse across the lipid bilayer of the cell membrane, moving down their concentration gradient [13].
- Carrier-Mediated Transport: An active, energy-dependent process that utilizes specific membrane-bound transporters to move solutes, often against a concentration gradient [13] [14].
- Transcytosis: A process where large molecules, such as proteins or nanoparticles, are engulfed by the cell via endocytosis, transported across the cytoplasm in vesicles, and expelled on the opposite side via exocytosis [13] [14].
A prerequisite for vectorial transcellular transport is cell polarity, the asymmetric distribution of transporters, channels, and enzymes between the apical and basolateral membranes, which is maintained by the fence function of the tight junctions [12].
Table 1: Core Characteristics of Paracellular and Transcellular Transport Pathways
| Feature | Paracellular Transport | Transcellular Transport |
|---|---|---|
| Route | Between adjacent cells (through tight junctions) [10] [11] | Through the cell body (across apical and basolateral membranes) [12] [13] |
| Energy Requirement | Passive (no energy required) [10] | Can be passive or active (energy-requiring) [13] [14] |
| Primary Driving Force | Concentration, osmotic, or electrochemical gradients [10] [11] | Concentration gradient (passive) or ATP (active) [13] |
| Key Molecular Structures | Tight junction proteins (claudins, occludin, ZO proteins) [10] [11] | Membrane lipids, channels, carriers, and endocytic machinery [13] |
| Typical Solutes | Small, hydrophilic molecules and ions (e.g., acyclovir) [10] [15] | Lipophilic molecules (passive); specific nutrients/drugs (carrier-mediated); macromolecules (transcytosis) [13] [15] |
| Saturability | Generally non-saturable [10] | Carrier-mediated transport is saturable [13] |
| Influencing Factors | Tight junction integrity and dynamic regulation [11] | Solute lipophilicity, molecular size, and affinity for specific transporters [13] |
Diagram 1: Overview of Transport Pathways
Molecular Architecture and Regulation
The functional distinction between the two pathways is rooted in their unique molecular architectures.
Tight Junctions: Gatekeepers of the Paracellular Route
The tight junction is not a static seal but a dynamic, regulated structure. Its core transmembrane components are:
- Claudins: A large family of proteins that form the primary seal and create charge- and size-selective pores within the tight junction strands [10]. Different claudin isoforms determine the specific permeability properties of a given tissue [10].
- Occludin: A regulatory protein that contributes to the barrier function and is involved in the response to various physiological stimuli [11].
- Junctional Adhesion Molecules (JAMs): These proteins play a role in the initial formation of tight junctions and in cell-cell adhesion [12].
Intracellularly, these proteins are linked to the actin cytoskeleton by scaffolding proteins like zonula occludens (ZO-1, -2, -3) [11]. This connection is crucial, as it allows the cell to rapidly modulate paracellular permeability in response to physiological demands; for instance, the phosphorylation of myosin light chains can trigger actin-myosin contraction and open the junctions [12].
Cellular Machinery for Transcellular Transport
The transcellular route relies on the polarized distribution of various transport systems across the cell:
- Lipid Bilayer: Serves as the conduit for passive diffusion of lipophilic solutes [13].
- Transport Proteins: Include channels, carriers, and pumps that facilitate the movement of specific solutes. For example, the Na-K-ATPase pump on the basolateral membrane actively maintains the sodium gradient that drives many secondary active transporters on the apical membrane [12].
- Endocytic and Exocytic Machinery: A complex system of vesicles, receptors, and cytoskeletal elements that facilitates transcytosis, enabling the transport of nanoparticles and macromolecules [13] [16].
Diagram 2: Molecular Architecture of Transport Pathways
Experimental Methods for Assessing Pathway Permeability
Distinguishing the contribution of each pathway and measuring tissue permeability are essential in research and development. The following are established methodologies.
In Vitro Barrier Models and Permeability Studies
A common approach involves using cell monolayers grown on permeable transwell inserts. The apparent permeability coefficient (Papp) of a solute is calculated from its rate of transport from the donor to the acceptor compartment [17].
Protocol 1: Standard Permeability Assay Using Transwell Inserts
- Cell Culture: Seed relevant epithelial cells (e.g., Caco-2 for intestine, Calu-3 for lung) on porous membrane inserts and culture until a fully differentiated, confluent monolayer with high transepithelial electrical resistance (TEER) is formed [17].
- TEER Measurement: Measure TEER before the experiment to verify monolayer integrity. TEER is a sensitive indicator of tight junction integrity and thus paracellular permeability [12].
- Dosing and Sampling: Apply the test compound in buffer to the donor compartment (e.g., apical side). Collect samples from the acceptor compartment (e.g., basolateral side) at predetermined time points over the course of several hours [15] [17].
- Analytical Quantification: Analyze samples using a suitable method (e.g., HPLC, MS, fluorescence spectroscopy) to determine the concentration of the transported compound.
- Papp Calculation: Calculate the apparent permeability coefficient using the formula:
Papp = (dQ/dt) / (A * C0), where dQ/dt is the steady-state flux, A is the membrane surface area, and C0 is the initial donor concentration [17].
Pharmacological Modulation of Pathways
Specific inhibitors or manipulative techniques can be used to delineate the contribution of each pathway.
Protocol 2: Pathway Differentiation Using Inhibitors and Osmotic Manipulation
- Inhibiting Transcellular Transport:
- Modulating Paracellular Transport:
- Osmotic Manipulation: Pre-treat barriers with hypo-osmotic solutions. This can cause swelling of cells or vesicles, physically altering the intercellular spaces and increasing paracellular flux of hydrophilic markers, as demonstrated in PermeaPad models [15].
- TJ Modulators: Use agents that directly affect tight junctions, such as calcium chelators (EGTA) or specific peptides targeting claudins.
Advanced Microphysiological Systems (MPS)
More complex in vitro models, such as organ-on-a-chip systems, incorporate fluid flow and multiple cell types to better recapitulate in vivo physiology. For instance, a small airway MPS with primary human lung epithelial and endothelial cells has been used to study the permeability of inhaled drugs like albuterol and formoterol [17]. These systems allow for real-time monitoring of solute transport in a more physiologically relevant context.
Table 2: Experimental Reagents for Pathway Analysis
| Reagent / Tool | Function / Target | Experimental Purpose |
|---|---|---|
| Dynasore [16] | Inhibitor of dynamin, a GTPase | Blocks clathrin- and caveolin-mediated endocytosis; used to inhibit transcellular transport via endocytosis. |
| Amiloride [16] | Inhibitor of Na+/H+ exchange | Blocks macropinocytosis, a form of fluid-phase endocytosis; used to study transcellular particle uptake. |
| EGTA (Ca2+ Chelator) | Depletes extracellular calcium | Disrupts calcium-dependent cell adhesion, leading to the opening of tight junctions; used to probe paracellular pathway. |
| Hypo-/Hyper-osmotic Solutions [15] | Alters cellular and vesicular volume via osmosis | Modifies the width of paracellular water channels; used to manipulate paracellular permeability. |
| TEER Measurement [12] | Measures electrical resistance across a monolayer | A non-invasive, quantitative readout of tight junction integrity and paracellular permeability. |
| Fluorescent Tracers (e.g., Calcein, FD-4) | Inert, detectable molecules | Serve as markers for paracellular (small/charged) or transcellular (lipophilic) transport. |
Diagram 3: Permeability Experiment Workflow
Implications for Drug Delivery and Permeability Research
The strategic exploitation of these pathways is central to modern drug delivery, particularly within the WISH research framework focused on tissue permeability.
Designing Molecules for Targeted Pathways
- Transcellular Route Optimization: For drugs with low oral bioavailability, chemical modification to increase lipophilicity (e.g., prodrug approaches) can enhance passive transcellular diffusion [13]. Alternatively, designing molecules to be substrates for active transporters expressed in the target tissue can facilitate efficient uptake [13].
- Paracellular Route Considerations: The paracellular route is particularly important for hydrophilic, charged drugs that poorly cross cell membranes (e.g., acyclovir, atenolol) [10] [11]. However, its utility is limited by molecular size and the restricted surface area of the intercellular space. Strategies to safely and transiently enhance paracellular permeability using permeation enhancers (e.g., medium-chain fatty acids, chitosan) are an active area of research [10].
Nanoparticle Delivery Systems
Nanoparticles (NPs) can be engineered to exploit specific transport mechanisms. Their size, surface charge, and coating dictate their pathway.
- Transcellular Dominance: Most nanoparticles are taken up by lymphatic endothelial cells and other barriers primarily via transcellular mechanisms such as micropinocytosis and macropinocytosis [16]. PEGylation of nanoparticles can steer their transport toward these mechanisms [16].
- Paracellular Potential: Smaller nanoparticles with positive surface charges may more readily undergo paracellular transport by interacting with the negatively charged tight junction proteins [11]. Computational kinetic modeling, using systems of differential equations, can help deconvolute the contributions of para- and transcellular mechanisms to overall NP transport [16].
The paracellular and transcellular routes represent two structurally and functionally distinct biological systems for solute transport. The paracellular pathway is a passive conduit between cells, rigorously governed by the dynamic tight junction complex, while the transcellular pathway is a multifaceted cellular traversal system capable of both passive and active transport. The distinction is not merely academic; it provides a critical framework for understanding tissue permeability, predicting drug absorption, and innovating drug delivery platforms. For WISH background research, a deep and nuanced grasp of these pathways, their interactions, and the methods to study them is indispensable for advancing therapeutic efficacy and navigating the complex landscape of biological barriers.
Tight junctions (TJs) represent the primary determinant of paracellular permeability, forming selective seals between epithelial and endothelial cells that control the passage of ions, molecules, and cells across tissue compartments [18]. These dynamic structures function not merely as static barriers but as sophisticated signaling hubs that integrate environmental cues, microbial signals, and metabolic information to regulate tissue homeostasis [19]. The molecular architecture of TJs encompasses multiple protein families including claudins, zonula occludens (ZO) proteins, occludin, and regulatory mediators like zonulin [20] [21]. Within the context of tissue permeability research, understanding the precise mechanisms governing these key molecular regulators provides critical insights into numerous pathological conditions including inflammatory disorders, autoimmune diseases, cancer metastasis, and infectious diseases [22] [19]. This technical guide comprehensively examines the structure, function, and experimental methodologies for investigating these crucial molecular determinants of barrier function.
Molecular Architecture of Tight Junctions
Core Protein Components and Their Functions
The tight junction complex comprises transmembrane proteins, cytoplasmic plaque proteins, and cytoskeletal linkers that collectively regulate paracellular permeability [20] [21].
Table 1: Core Protein Components of Tight Junctions
| Protein Category | Key Members | Primary Functions | Structural Features |
|---|---|---|---|
| Transmembrane Proteins | Claudin family (27 members) | Forms paracellular barrier & selective pores; determines ion selectivity [18] | Tetraspan proteins with 2 extracellular loops, short N-terminus, long C-terminal cytoplasmic domain [18] |
| Occludin | TJ regulation & stabilization; modulates leak pathway [21] | Tetraspan protein with 2 extracellular loops, C-terminal OCEL domain [21] | |
| Junctional Adhesion Molecules (JAMs) | Cell-cell adhesion; immune cell migration [23] | Immunoglobulin-like fold with single transmembrane domain [23] | |
| Cytoplasmic Plaque Proteins | Zonula Occludens (ZO-1, ZO-2, ZO-3) | Scaffolding proteins linking transmembrane proteins to actin cytoskeleton [21] | PDZ domains, SH3 domain, guanylate kinase domain, actin-binding region [21] |
| Regulatory Mediators | Zonulin | Reversibly regulates intestinal permeability by modulating intercellular TJs [24] [25] | Serum protein that activates PAR-2/EGFR signaling leading to actin rearrangement [26] |
Claudin Family: Masters of Paracellular Selectivity
The claudin (CLDN) protein family represents the fundamental building blocks of tight junction strands, with at least 27 members identified in mammals [18]. These four-pass transmembrane proteins create the characteristic tight junction strands observed via freeze-fracture microscopy and establish the paracellular charge and size selectivity [18]. Several structural features dictate claudin functionality:
- Extracellular Loop 1 (ECL1): This larger extracellular domain contains critical conserved amino acid motifs that directly determine ion selectivity and paracellular permeability. The distribution pattern of acidic and basic amino acids in ECL1 creates charge-selective channels [18].
- Extracellular Loop 2 (ECL2): The smaller second extracellular loop contributes to strand organization and barrier integrity [18].
- C-terminal PDZ-binding domain: This cytoplasmic domain interacts with scaffold proteins of the ZO family and MUPP1, enabling connection to the actin cytoskeleton and facilitating intracellular signaling [18].
Claudins can be functionally categorized as "barrier-forming" (e.g., claudin-1, -3, -4, -5, -8, -11) or "pore-forming" (e.g., claudin-2, -10, -15, -16), with the specific claudin composition of a tissue determining its paracellular transport properties [18] [26]. The expression balance between sealing and pore-forming claudins is dynamically regulated in physiological and pathological states; inflammation typically decreases sealing claudins while increasing pore-forming claudins like claudin-2, disrupting barrier function [26].
Quantitative Assessment of Tight Junction Regulators
Recent clinical studies have established the diagnostic and prognostic value of specific tight junction proteins as serum biomarkers for barrier dysfunction.
Table 2: Diagnostic Performance of TJ Protein Biomarkers in Clinical Studies
| Biomarker | Condition Assessed | Population | Key Findings | Diagnostic Performance (AUC) |
|---|---|---|---|---|
| Claudin-3 | Post-abdominal surgery intestinal barrier dysfunction [24] | Patients undergoing abdominal surgery | Significantly increased at 24h post-operation; positively correlated with intestinal injury severity [24] | AUC = 0.934 [24] |
| Zonulin | Post-abdominal surgery intestinal barrier dysfunction [24] | Patients undergoing abdominal surgery | Significantly increased at 24h post-operation; peaks at 24h post-reperfusion [24] | AUC = 0.826 [24] |
| Occludin | Inflammatory Bowel Disease [26] | IBD patients (UC & CD) | Decreased serum levels compared to healthy controls; improved with anti-TNF-α treatment [26] | UC: AUC = 0.959; CD: AUC = 0.948 [26] |
| Claudin-2 | Inflammatory Bowel Disease [26] | IBD patients (UC & CD) | Increased serum levels compared to healthy controls [26] | UC: AUC = 0.864; CD: AUC = 0.896 [26] |
| Zonulin | Crohn's Disease [26] | CD patients | Increased concentration compared to control group [26] | AUC = 0.74 [26] |
Signaling Pathways and Molecular Interactions
Zonulin Signaling Pathway
Zonulin serves as a key physiological regulator of intestinal permeability through its reversible modulation of intercellular tight junctions [24] [25]. The zonulin signaling cascade involves:
- Receptor Binding: Zonulin binds to specific apical membrane receptors on enterocytes [22]
- Intracellular Activation: Triggers activation of protease-activated receptor-2 (PAR-2) and epidermal growth factor receptor (EGFR) signaling [26]
- Cytoskeletal Rearrangement: Leads to protein kinase C (PKC)-dependent phosphorylation and subsequent actin polymerization and contraction [22]
- Tight Junction Disassembly: Causes dislocation of zonula occludens-1 and rearrangement of TJ proteins, increasing paracellular permeability [26]
This pathway is physiologically upregulated in response to bacterial exposure and intestinal dysbiosis, highlighting its role in host-microbe interactions [26]. In pathological states, zonulin upregulation is associated with increased intestinal permeability in autoimmune, inflammatory, and neoplastic diseases [22] [20].
Claudin Cross-Regulation and Signaling
Claudin proteins participate in complex regulatory networks, including cross-regulation between family members. A significant mechanistic insight reveals that one claudin can influence the ability of another claudin to interact with the tight junction scaffold [27]. For instance:
- Claudin-5 and Claudin-18 Interaction: In alveolar epithelial cells, alcohol exposure upregulates claudin-5 expression, which impairs barrier function by displacing claudin-18 from ZO-1 interactions [27]. This claudin-5 mediated disruption is both necessary and sufficient for barrier compromise.
- Scaffold Protein Competition: Claudins compete for binding sites on ZO proteins; phosphorylation events regulate these interactions and consequently affect paracellular permeability [27] [21].
- Signaling Pathway Integration: Claudins modulate critical signaling pathways including:
- PI3K/AKT: Regulates cell survival and proliferation
- Wnt/β-catenin: Influences cell polarity and differentiation
- Small GTPases (Rac1/RhoA): Controls cytoskeletal reorganization
- Notch and Hippo pathways: Potential roles in proliferation and junction organization [18]
Experimental Methodologies and Protocols
Assessment of Intestinal Barrier Function in Animal Models
Intestinal Ischemia-Reperfusion (I/R) Injury Model [24] [25]
Objective: To establish a reproducible model of intestinal barrier dysfunction for evaluating TJ protein dynamics.
Materials:
- Sprague-Dawley rats (6-8 weeks, 180-220g)
- Anesthetic: 10% chloral hydrate solution
- Surgical instruments: microvascular clamps, sutures
- Sample collection: tubes for serum, 4% paraformaldehyde for tissue fixation
Procedure:
- Anesthetize rats with intraperitoneal chloral hydrate (0.3 ml/100g)
- Perform midline laparotomy (4cm incision) and exteriorize small intestine
- Identify superior mesenteric artery (SMA) and apply microvascular clamp for 40 minutes
- Confirm ischemia by pale intestinal coloration
- Remove clamp and confirm reperfusion by return of bright red color
- Close abdomen in layers
- Collect blood samples at predetermined timepoints (6h, 24h, 48h, 72h post-reperfusion)
- Euthanize animals and collect intestinal tissue samples 6cm from cecum
- Process samples for H&E staining and serum biomarker analysis
Assessment Parameters:
- Chiu's scoring system for intestinal mucosal injury: 0 (normal) to 5 (complete destruction with hemorrhage) [24] [25]
- Serum claudin-3 and zonulin levels via ELISA
- Peripheral blood E. coli 16sDNA detection via qPCR as translocation marker
Measurement of Serum Tight Junction Proteins by ELISA
Principle: Quantitative detection of soluble TJ proteins in serum samples using sandwich enzyme-linked immunosorbent assay [24] [26].
Reagents:
- Pre-coated capture antibody plates
- Detection antibodies conjugated to horseradish peroxidase (HRP)
- Protein standards for calibration curves
- Substrate solution (TMB or similar)
- Stop solution
Procedure:
- Coat wells with capture antibodies specific to target protein (claudin-3, zonulin, or occludin)
- Block remaining protein-binding sites
- Add serum samples and standards in duplicate
- Incubate with detection antibody (HRP-conjugated)
- Develop with substrate solution for 15-30 minutes
- Stop reaction and measure absorbance at appropriate wavelength
- Calculate concentrations from standard curve
Technical Notes:
- Optimal sample collection at 24h post-injury for peak biomarker levels [24]
- Centrifuge blood samples at 3500 rpm for 10 minutes for serum separation
- Store serum at -80°C until analysis to prevent protein degradation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Tight Junction Studies
| Reagent/Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Animal Models | Rat intestinal I/R model [24] | Studying dynamic changes in TJ proteins post-injury | Peak TJ protein release at 24h post-reperfusion; monitor via Chiu's scoring [24] |
| Cell Culture Models | Primary alveolar epithelial cells [27] | Mechanistic studies of claudin interactions | Alcohol exposure model demonstrates claudin-5/18 cross-regulation [27] |
| Detection Antibodies | Claudin-3, zonulin, occludin ELISA kits [24] [26] | Quantifying serum biomarkers of barrier dysfunction | Commercial kits available; validate with spike-recovery experiments [24] |
| Molecular Tools | Claudin-5 shRNA [27], YFP-claudin constructs [27] | Manipulating specific claudin expression | shRNA reverses alcohol-induced barrier defects; overexpression studies [27] |
| Permeability Assays | Transepithelial electrical resistance (TER) [27], paracellular flux markers [27] | Functional assessment of barrier integrity | Use multiple probe sizes (0.6-10 kDa) for comprehensive assessment [27] |
| Therapeutic Modulators | Claudin-5 peptide mimetic [27], anti-TNF-α [26] | Testing barrier-restoring interventions | Peptide mimetic reverses alcohol-induced dysfunction; anti-TNF-α improves occludin [27] [26] |
| Eupalinolide B | Eupalinolide B, CAS:877822-40-7, MF:C₂₄H₃₀O₉, MW:462.49 | Chemical Reagent | Bench Chemicals |
| Larsucosterol Sodium | Larsucosterol Sodium, CAS:1174047-40-5, MF:C27H45NaO5S, MW:504.7 g/mol | Chemical Reagent | Bench Chemicals |
The molecular regulators of tight junctions—claudins, zonulin, and associated scaffolding proteins—represent sophisticated determinants of tissue permeability with far-reaching implications for human health and disease. The experimental methodologies outlined herein enable rigorous investigation of these regulatory systems, while the emerging toolkit of targeted modulators offers promising therapeutic avenues. Future research directions should prioritize the development of claudin-specific modulators, exploration of tissue-specific TJ protein isoforms, and translation of serum TJ biomarkers into clinical diagnostics for barrier-related pathologies. As our understanding of these key molecular regulators deepens, so too does our capacity to manipulate tissue permeability for therapeutic benefit across a spectrum of diseases.
Physiological Roles in Nutrient Absorption, Immune Surveillance, and Homeostasis
Tissue permeability is a fundamental biological property that governs the selective movement of molecules, fluids, and cells across biological barriers. This selective transport plays a critical role in maintaining organismal health by enabling nutrient absorption, facilitating immune surveillance, and ensuring tissue homeostasis. The controlled exchange between compartments allows for the delivery of essential nutrients, immune cell trafficking for pathogen detection, and communication signals for tissue repair and regeneration. Disruption of these finely tuned permeability barriers contributes significantly to disease pathogenesis, including inflammatory disorders, metabolic syndromes, and cancer. This whitepaper examines the physiological roles of tissue permeability through the lens of its core functions, integrating current scientific understanding with methodological approaches for research and drug development.
Tissue Barrier Structures and Permeability Fundamentals
Biological barriers throughout the body maintain compartmentalization while permitting selective exchange. These barriers share common design principles but exhibit specialized adaptations suited to their specific physiological contexts.
Structural Components of Major Biological Barriers
The intestinal barrier exemplifies a complex selective interface between the external environment and internal milieus. It consists of multiple integrated layers: a mucous layer containing commensal microbiota, a single layer of specialized epithelial cells, and the underlying lamina propria rich in immune cells [28]. The mucous layer itself is subdivided into an inner stratum firmly attached to the epithelium and an outer layer colonized by microorganisms [29]. This structural organization allows for nutrient processing while maintaining defense functions.
The blood-brain barrier (BBB) represents a highly specialized vascular interface that protects the central nervous system (CNS). The BBB is formed by specialized microvascular endothelial cells connected by complex tight junctions, an underlying basement membrane containing pericytes, and the glia limitans composed of astrocyte end-feet [30]. This multi-layered structure strictly limits paracellular transport while regulating transcellular passage of substances.
Pathways of Molecular and Cellular Transport
The transport of substances across biological barriers occurs through several distinct pathways:
- Paracellular pathway: Small hydrophilic compounds (400 Da to 10-20 kDa) pass between epithelial cells through tight junction complexes [29]
- Transcellular pathway: Small lipophilic compounds cross directly through the plasma membrane of epithelial cells [29]
- Transporter-mediated uptake: Nutrients including amino acids, vitamins, and sugars use specialized epithelial transporters [29]
- Endocytic pathways: Larger peptides, proteins, and bacteria cross via vesicular transport mechanisms [29]
Table 1: Transport Pathways Across Biological Barriers
| Pathway | Mechanism | Substances Transported |
|---|---|---|
| Paracellular | Movement between cells through tight junctions | Small hydrophilic compounds (400 Da - 20 kDa), ions, water |
| Transcellular | Passive diffusion through cell membranes | Small lipophilic compounds |
| Transporter-mediated | Active transport via membrane proteins | Nutrients (amino acids, sugars, vitamins) |
| Endocytic | Vesicular uptake and transcytosis | Large peptides, proteins, bacteria |
Nutrient Absorption and the Gastrointestinal Barrier
The gastrointestinal tract represents the primary interface for nutrient absorption, with its permeability tightly regulated to allow uptake of dietary components while excluding potential harmful substances.
Intestinal Architecture for Selective Permeability
The intestinal epithelium contains several specialized cell types that collectively mediate its absorptive and barrier functions. Enterocytes, the most abundant epithelial cells, are primarily responsible for nutrient absorption and form an effective physical barrier [29]. Goblet cells (approximately 10% of epithelial cells) secrete gel-forming mucins that generate the protective mucous layer [29] [28]. Paneth cells located at the crypt bases produce antimicrobial compounds, while enteroendocrine cells secrete gastrointestinal hormones and peptides [29]. Microfold (M) cells overlying Peyer's patches play important roles in intestinal immune sampling [29].
The tight junction complexes between epithelial cells constitute the primary determinant of paracellular permeability. Historically first described in 1976 as "occluding zonules" in gallbladder epithelium, these protein complexes create a selective seal that polarizes the intestinal epithelium and allows regulated passage of ions and molecules [29].
Regional Specialization for Nutrient Processing
The gastrointestinal tract exhibits remarkable regional specialization for nutrient processing and absorption:
- Stomach: Functions in food storage, acidification, and initial enzymatic digestion with antibacterial properties [29]
- Duodenum: Continues digestion with bile and pancreatic juices for nutrient preparation [29]
- Jejunum: Absorbs water, amino acids, sugars, and fatty acids [29]
- Ileum: Absorbs remaining digestion products (e.g., vitamin B12) and contains important immune structures (Peyer's patches) [29]
- Colon: Reabsorbs remaining water and prepares luminal content for elimination [29]
This functional specialization is reflected in varying pH gradients along the GI tract, from highly acidic in the stomach (pH 1.4-4.6) to nearly neutral in the distal small intestine (pH 7.4-7.8) and variable in the colon (pH 5-8) [29]. These chemical gradients significantly influence microbial distribution, enzyme activity, and nutrient absorption efficiency.
Regulation of Absorption Processes
Nutrient absorption is precisely regulated by multiple factors, including gastrointestinal hormones, neural signals, and local cellular responses. The presence of nutrients in the intestinal lumen stimulates the release of hormones such as cholecystokinin (CCK), glucagon-like peptides (GLP-1 and GLP-2), and peptide YY, which collectively regulate digestion and absorption processes [31]. GLP-2 specifically enhances nutrient absorption and has been shown to improve lean body mass in patients with functional short-bowel syndrome [31].
The rate of gastric emptying represents a primary determinant of absorption kinetics, particularly for compounds like alcohol that require no digestion and are absorbed passively [31]. Food in the stomach generally slows gastric emptying and consequently delays absorption, while strong alcoholic beverages can irritate the stomach and cause pyloric sphincter closure, further complicating absorption predictability [31].
Immune Surveillance and Tissue-Resident Immunity
The immune system maintains continuous monitoring of tissues through specialized resident cell populations that interface with permeability barriers to detect and respond to potential threats.
Tissue-Resident Immune Cells (TRICs)
Tissue-resident immune cells constitute a heterogeneous population of immune cells that reside in lymphoid or peripheral tissues without recirculation, endowed with distinct capabilities not shared by their circulating counterparts [32]. These cells include tissue-resident memory T cells (T~RM~), tissue-resident macrophages, tissue-resident innate lymphoid cells (ILCs), tissue-resident natural killer (trNK) cells, and tissue-resident memory B cells (B~RM~) [32].
TRICs are defined by their origins, phenotypic markers, and transcriptional profiles. Some TRICs, including tissue-resident macrophages and mast cells, acquire tissue-resident properties during embryogenesis, while others such as T~RM~ cells establish residency during effector stages postnatally [32]. Common phenotypic markers include CD69, CD103, and CD49a, though expression patterns vary significantly across different tissues [32].
Table 2: Major Tissue-Resident Immune Cell Populations and Functions
| Cell Type | Primary Markers | Main Functions | Tissue Distribution |
|---|---|---|---|
| Tissue-resident memory T cells (T~RM~) | CD69, CD103, CD49a | Local pathogen protection, immune surveillance | Mucosal sites, skin, various organs |
| Tissue-resident macrophages | F4/80, CD64, MerTK | Phagocytosis, homeostasis, tissue repair | All tissues, tissue-specific subtypes |
| Tissue-resident innate lymphoid cells (ILCs) | CD127, varying receptors | Barrier immunity, tissue remodeling, homeostasis | Mucosal barriers, various tissues |
| Tissue-resident natural killer (trNK) cells | CD49a, CXCR6 | Viral defense, antitumor immunity | Liver, uterus, salivary glands |
| Tissue-resident memory B cells (B~RM~) | CD69, CD80, CD73 | Local antibody production, antigen presentation | Mucosal tissues, lymphoid organs |
Immune Surveillance of Barrier Tissues
At barrier sites such as the skin and intestinal mucosa, immune surveillance involves close interaction between TRICs and the local tissue environment. Dendritic cells in tissue-draining lymph nodes process microenvironmental signals, including food-derived vitamin A in the gut and ultraviolet-induced vitamin D3 in the skin, to imprint tissue-specific homing programs in naïve lymphocytes [30]. This process ensures that immune cells are programmed to return to the specific tissue sites where they initially encountered antigens.
In the central nervous system, immune surveillance occurs despite the protective blood-brain barrier. Under physiological conditions, the BBB restricts immune cell trafficking primarily to activated T cells, which can reach the cerebrospinal fluid-filled compartments to perform CNS immune surveillance [30]. The CNS parenchyma itself maintains immune privilege, prioritizing neuronal function over robust immune responses, while the ventricular spaces and border compartments (subarachnoid and perivascular spaces) are dedicated to CNS immunity [30].
Immunosurveillance as a Homeostatic Mechanism
Beyond pathogen defense, immune surveillance plays crucial roles in tissue homeostasis by eliminating damaged, senescent, and potentially malignant cells [33]. This homeostatic immunosurveillance involves recognition of stress-induced ligands on compromised cells, followed by their removal through various immune mechanisms. Defects in these surveillance mechanisms accelerate the development of pathological conditions including cancer, fibrosis, post-ischemic tissue damage, and neurodegenerative diseases [33].
The immune system employs multiple recognition strategies for detecting aberrant cells:
- MHC-I-associated peptides that reflect intracellular alterations [33]
- Stress-induced ligands such as NKG2D ligands recognized by natural killer cells [33]
- Damage-associated molecular patterns (DAMPs) released during cellular stress [33]
Tissue Homeostasis and Permeability Regulation
Tissue homeostasis involves the maintenance of microenvironmental variables within narrow ranges despite constant internal and external challenges. Permeability regulation represents a crucial aspect of this homeostatic maintenance across multiple tissue types.
Core Principles of Tissue Homeostasis
While cellular and organismal homeostasis are relatively well-understood, tissue homeostasis remains less comprehensively characterized [34]. Tissue homeostasis involves maintaining critical microenvironmental variables including oxygen and nutrient levels, cell number and composition, extracellular matrix composition and mechanical properties, and interstitial fluid characteristics (volume, pH, osmolarity) [34].
The maintenance of these variables depends on regulated processes including local blood perfusion, angiogenesis, cell proliferation and death, ECM production and degradation, vascular permeability, and lymphatic drainage [34]. The minimal composition of most vertebrate tissues comprises four core cell types: functional cells specific to the tissue (e.g., hepatocytes in liver, neurons in brain), microvascular endothelial cells, fibroblast-like stromal cells, and tissue-resident macrophages [34].
Cellular Circuits in Homeostatic Maintenance
Homeostatic regulation often involves reciprocal communication circuits between different cell types. A prime example is the macrophage-fibroblast two-cell circuit where fibroblasts produce colony stimulating factor-1 (CSF-1) for macrophages, and macrophages synthesize platelet-derived growth factor (PDGF) for fibroblasts [34]. This reciprocal exchange establishes a stable regulatory circuit that maintains appropriate cellular composition within tissues.
The cellular division of labor in tissues follows several organizational principles:
- Independent specialization: Different cell types perform distinct functions independently
- Collaborative function: Multiple cell types contribute to the same function
- Support relationships: One cell type performs primary functions while others provide essential support [34]
Impact of Permeability Dysregulation on Homeostasis
Disruption of normal tissue permeability barriers contributes significantly to disease pathogenesis. In the intestinal barrier, increased permeability permits translocation of luminal bacteria and microbial components such as lipopolysaccharides (LPS) into the portal bloodstream [28]. This triggers metabolic endotoxemia characterized by chronic low-grade inflammation, which can promote atherosclerosis and thrombotic diseases through activation of Toll-like receptor 4 (TLR4) on leukocytes and endothelial cells [28].
In the central nervous system, breaching of the glia limitans allows immune cells to access the CNS parenchyma, contributing to neuroinflammatory conditions such as multiple sclerosis [30]. The unique anatomical relationship between the brain barriers and the immune system creates compartments with differing accessibility to immune mediators, with the CNS parenchyma maintaining immune privilege while the ventricular and border compartments facilitate immune interactions [30].
Experimental Methods for Assessing Tissue Permeability
Accurate measurement of tissue permeability is essential for both basic research and drug development. Multiple experimental approaches have been developed to assess barrier function in various biological systems.
In Vivo Permeability Assessment
In vivo methods provide physiologically relevant data by preserving the complex interactions between different cell types and tissues. These approaches typically involve administering tracer substances and measuring their distribution across biological barriers [1]. Common methodologies include:
- Vascular permeability assays: Measuring leakage of intravenous tracers into tissues
- Intestinal permeability tests: Using non-metabolizable markers to assess gut barrier function
- Blood-brain barrier permeability evaluations: Quantifying CNS penetration of specific compounds
These in vivo approaches complement molecular findings and help establish the physiological significance of experimental observations [1]. The interaction of multiple cell types and tissues present in mammalian models allows for comprehensive testing of hypotheses regarding barrier function.
Ex Vivo and In Vitro Models
Reductionist systems provide controlled environments for mechanistic studies of permeability regulation:
- Using chamber systems: Measure transepithelial electrical resistance (TEER) and molecular flux across epithelial barriers
- Cell culture models: Recreate simplified barrier systems using endothelial or epithelial cell monolayers
- Tissue explants: Maintain native tissue architecture while permitting controlled experimental manipulation
Specific Permeability Measurement Techniques
Different tissue types require specialized methodological approaches:
- Intestinal permeability: Lactose absorption tests, hydrogen breath tests, and sugar permeability assays [31]
- Vascular permeability: Tracer leakage assays using Evans blue or fluorescent dextrans [35]
- Blood-brain barrier permeability: In situ brain perfusion techniques, microdialysis
Table 3: Experimental Methods for Assessing Tissue Permeability
| Method Type | Specific Techniques | Measured Parameters | Applications |
|---|---|---|---|
| In vivo approaches | Vascular tracer leakage, intestinal permeability tests, BBB penetration assays | Leakage rate, absorption kinetics, distribution volume | Physiological relevance, therapeutic screening |
| Ex vivo systems | Using chamber experiments, tissue explant models | Transepithelial resistance, molecular flux, permeability coefficients | Mechanism investigation, toxin testing |
| Cellular assays | Cell monolayer permeability, transwell migration assays | Paracellular flux, transcellular transport, tight junction integrity | High-throughput screening, molecular studies |
| Clinical tests | Lactose tolerance tests, hydrogen breath tests | Blood glucose changes, expired hydrogen concentrations | Diagnostic applications, patient stratification |
The Scientist's Toolkit: Key Research Reagents and Materials
This section details essential research tools for investigating tissue permeability, barrier function, and related physiological processes.
Table 4: Essential Research Reagents for Tissue Permeability Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Tight junction markers | Identify and quantify junctional complexes | Antibodies against ZO-1, occludin, claudin family proteins |
| Tracer molecules | Assess permeability in various systems | Fluorescent dextrans, Evans blue, HRP, sucrose isotopes |
| Cytokine and growth factors | Modulate barrier function experimentally | TNF-α, IFN-γ, TGF-β, VEGF for permeability manipulation |
| Immune cell markers | Characterize tissue-resident immune populations | Anti-CD69, CD103, CD49a for TRM cells; F4/80 for macrophages |
| TLR4 pathway reagents | Study innate immune activation by barrier disruption | LPS, TLR4 antagonists, MyD88/TRIF pathway inhibitors |
| Parabiosis setup | Distinguish tissue-resident vs. circulating cells | Surgical equipment for parabolic pairing, flow cytometry analysis |
| Intravascular labeling antibodies | Differentiate blood-borne and tissue-resident cells | Anti-CD45, CD3 antibodies administered intravenously |
| scRNA-seq reagents | Transcriptional profiling of tissue-resident cells | 10x Genomics platforms, droplet-based sequencing reagents |
| Guaiacol-d4 | Guaiacol-d4, MF:C7H8O2, MW:128.16 g/mol | Chemical Reagent |
| (R)-Methotrexate-d3 | (R)-Methotrexate-d3, CAS:432545-63-6, MF:C20H22N8O5, MW:457.5 g/mol | Chemical Reagent |
Tissue permeability serves as a master regulator of physiological processes spanning nutrient absorption, immune surveillance, and tissue homeostasis. The intricate balance of selective barrier function enables organisms to maintain compartmentalization while permitting essential exchange processes. Understanding the molecular mechanisms governing permeability regulation across different tissue barriers provides critical insights for therapeutic development across a spectrum of diseases, including inflammatory disorders, metabolic syndromes, and cancer. Continued advancement in imaging technologies, single-cell analysis methods, and sophisticated experimental models will further elucidate the complex interplay between barrier function and physiological regulation, opening new avenues for targeted therapeutic interventions.
The regulation of molecular and cellular traffic across biological barriers is a cornerstone of physiological homeostasis and a critical consideration in drug development. Intestinal, vascular, and cutaneous barriers employ specialized structures and mechanisms to selectively control permeability. Disruption of this delicate balance is implicated in numerous disease states, from inflammatory conditions to metabolic disorders. This whitepaper provides a technical analysis of permeability regulation across these three fundamental tissue types, framing the discussion within research on barrier function assessment and its implications for therapeutic development. We synthesize contemporary research methodologies, quantitative permeability data, and experimental protocols to offer a consolidated resource for scientists and drug development professionals.
Intestinal Barrier Permeability
The intestinal epithelium forms a dynamic, selective barrier that facilitates nutrient absorption while preventing the translocation of pathogens, toxins, and undigested antigens. Its permeability is governed by complex cellular architectures and molecular systems.
Structure and Permeability Pathways
The intestinal barrier consists of a single layer of epithelial cells interconnected by tight junction (TJ) complexes, which are the primary regulators of paracellular permeability [36]. These TJs are composed of proteins including claudins, occludins, and zonula occludens (ZO) [37]. The transcellular pathway allows for the controlled transport of molecules through the epithelial cells themselves, via mechanisms such as carrier-mediated transport or transcytosis [37].
Advanced in vitro models have revealed significant segment-specific differences in human intestinal physiology. Enteroid-derived cells from human jejunum (J2) and duodenum (D109) demonstrate more physiologically relevant morphology and higher transepithelial electrical resistance (TEER) compared to the traditional Caco-2 cell line (derived from colon adenocarcinoma) [36]. The EpiIntestinalTM model, a commercial engineered tissue, exhibits thicker, more uneven structures with lower TEER and correspondingly higher passive permeability [36].
Assessment Methods and Quantitative Data
The lactulose:mannitol (L:M) test is a widely used clinical and research method for assessing intestinal permeability in humans [37]. In this test, participants ingest a solution containing these two non-metabolized sugar molecules. Lactulose (larger molecule, ~0.62 nm) primarily crosses the intestinal barrier via the paracellular pathway, while mannitol (smaller molecule) primarily uses the transcellular pathway. Urinary excretion is measured over a 5-hour period, and the ratio of the two provides an indicator of barrier integrity, with a higher ratio suggesting increased paracellular permeability [37].
Table 1: Intestinal Permeability Assessment in an Elderly Population via L:M Test
| Parameter | Overall Population (n=54) | L:M ≤ P50 (n=27) | L:M > P50 (n=27) | P-value |
|---|---|---|---|---|
| Median L:M Ratio | 0.037 (IQR: 0.014-0.060) | ≤0.037 | >0.037 | - |
| Hip Circumference (cm) | 99.00 (95.00-106.75) | 101.00 (97.00-108.00) | 96.50 (93.00-104.00) | 0.041 |
| Serum Retinol (mmol/L) | 1.19 (0.91-1.45) | 1.33 (1.19-1.52) | 0.95 (0.60-1.16) | <0.001 |
| Diabetes Prevalence | 25.9% | 22.2% | 29.6% | 0.75 |
| Hypertension Prevalence | 53.7% | 48.1% | 59.3% | 0.58 |
A study of an elderly population found the median L:M ratio was 0.037, and an L:M ratio above the 50th percentile was significantly associated with lower hip circumference and lower serum retinol levels, suggesting a link between intestinal hyperpermeability and nutritional status [37].
In vitro models provide comparative data for drug permeability assessment. The permeability of model small molecules like caffeine, propranolol, and indomethacin varies significantly across different intestinal models. Research shows that integrating data from traditional Caco-2 models with corrections from more physiologically relevant enteroid-derived cells can improve the accuracy of predicting human oral bioavailability using tools like the Physiologically based Gut Absorption Model (PECAT) [36].
Experimental Protocol: Lactulose:Mannitol Test
Purpose: To assess in vivo human intestinal permeability, specifically differentiating paracellular and transcellular absorption [37]. Materials:
- Lactulose and Mannitol Solution: 5.0 g lactulose and 1.0 g mannitol dissolved in 20 mL of water.
- Collection Supplies: Urine collection containers, 2.35% chlorhexidine solution for preservation.
- Analysis Equipment: High-performance liquid chromatography with pulsed amperometric detection (HPLC-PAD). Procedure:
- Participants fast for a minimum of 2 hours and empty their bladder completely.
- Administer the oral lactulose/mannitol solution.
- Maintain fasting for an additional hour post-administration.
- Collect total urine output for a 5-hour period.
- Add 1 drop of 2.35% chlorhexidine per 50 mL of urine for preservation.
- Record total urine volume and store samples at -80°C until analysis.
- Analyze lactulose and mannitol concentrations using HPLC-PAD. Data Analysis: Calculate the percentage of the administered dose of each sugar recovered in the urine. The primary outcome is the lactulose-to-mannitol ratio (L:M ratio). A higher ratio indicates increased paracellular permeability.
Vascular Barrier Permeability
Vascular endothelial barriers control the exchange of fluids, solutes, and cells between the bloodstream and tissues. Their permeability characteristics are highly specialized according to organ-specific requirements.
Structural Classification and Barrier Mechanisms
Blood vessels are structurally classified into three main types with distinct permeability properties [38]:
- Continuous Capillaries: Feature non-fenestrated endothelial cells with tight junctions and a continuous basement membrane (e.g., in skin, muscle, brain). They present the tightest barrier.
- Fenestrated Capillaries: Contain diaphragmed pores (fenestrae) that enhance permeability to small molecules and fluids (e.g., in endocrine glands, intestinal mucosa, kidney peritubular capillaries).
- Sinusoidal Capillaries: Have discontinuous endothelium with large intercellular gaps and an incomplete basement membrane, allowing passage of large proteins and even cells (e.g., in liver, spleen, bone marrow).
The vascular permeability barrier is maintained by two primary systems [38]:
- Size Barrier: Dictated by Interendothelial Junctions (IEJs) comprising adherens junctions (AJs, primarily VE-cadherin) and tight junctions (TJs, including claudins and occludin). The specific composition of these junctions determines the physical space available for paracellular transport.
- Charge Barrier: Formed by the glycocalyx, a negatively charged mesh of proteoglycans and glycosaminoglycans on the endothelial luminal surface. This layer repels anionic molecules in the plasma.
Table 2: Vascular Barrier Types and Their Permeability Properties
| Vessel Type | Endothelial Characteristics | Junctional Complexes | Representative Organs | Estimated Size Limit (Paracellular) |
|---|---|---|---|---|
| Continuous (non-fenestrated) | Continuous basement membrane, no fenestrae | Tight Junctions (TJs) & Adherens Junctions (AJs) | Brain, Retina, Spinal Cord | <1 nm [38] |
| Continuous (non-fenestrated) | Continuous basement membrane, no fenestrae | Adherens Junctions (AJs predominate) | Skin, Muscle, Heart, Lung | <5 nm [38] |
| Fenestrated | Fenestrations with diaphragm | Specialized diaphragms | Exocrine/Endocrine Glands, Intestinal Mucosa, Kidney (peritubular) | 6-12 nm [38] |
| Sinusoidal (Discontinuous) | Discontinuous basement membrane, large fenestrations | Few, loose junctions | Liver, Spleen | 50-280 nm (species-dependent) [38] |
Assessment and Pathophysiological Dynamics
Vascular permeability is dynamically regulated and increases significantly during inflammation. Histamine is a potent mediator of this response, and its effects are highly tissue-specific. A classic study demonstrated that after intravenous histamine injection, albumin permeation increased most dramatically in the cecum (4-fold), followed by the pancreas and small intestine, while skin permeability remained unchanged unless histamine was injected locally [39].
In the central nervous system, the Blood-Brain Barrier (BBB) is a highly specialized vascular barrier. Its integrity can be severely compromised after ischemic stroke. Research shows that vascular recanalization (reperfusion), while therapeutic, can exacerbate BBB disruption. This is characterized by a significant downregulation of TJ proteins occludin and ZO-1 (impairing the paracellular pathway) and an increase in the Caveolin-1/MFSD2a ratio (indicating enhanced transcytosis) [40]. This leads to increased leakage of IgG and FITC-dextran into brain tissue, worsening outcomes like hemorrhagic transformation [40].
Experimental Protocol: In Vivo Vascular Permeability Assay (Miles Assay)
Purpose: To assess changes in vascular permeability in response to vasoactive agents or inflammatory stimuli in an animal model [38] [39]. Materials:
- Tracers: Evans Blue dye (which binds to serum albumin) or fluorescent conjugates like FITC-dextran.
- Test Substances: Vasoactive agents (e.g., histamine).
- Equipment: Microinjection equipment, spectrophotometer or fluorescence microscope. Procedure:
- Administer the tracer (e.g., Evans Blue) intravenously to the animal.
- Inject the test substance (e.g., histamine) intradermally or subcutaneously at defined sites on the skin. A control site should be injected with vehicle alone.
- Allow circulation for a predetermined period (e.g., 20-30 minutes).
- Euthanize the animal and perfuse with saline to remove intravascular tracer.
- Excise the skin from the injection sites and control areas.
- Extract the Evans Blue dye from the tissue using formamide and quantify it spectrophotometrically. For fluorescent tracers, visualize and quantify leakage using fluorescence microscopy. Data Analysis: The amount of tracer extravasated at the test site is compared to the control site. A significant increase indicates induced vascular hyperpermeability.
Cutaneous Barrier Permeability
The skin is the body's outermost barrier, providing formidable protection against environmental insults and preventing water loss. Overcoming this barrier is a principal challenge for transdermal drug delivery.
Skin Architecture and Permeation Pathways
Human skin comprises three primary layers [41]:
- Epidermis: The outermost layer, containing the stratum corneum (SC), which is the rate-limiting barrier for most molecular permeation. The SC consists of cornified keratinocytes (corneocytes) embedded in a lipid matrix, often described as a "brick-and-mortar" structure.
- Dermis: A vascularized connective tissue layer housing nerves, hair follicles, and sweat glands.
- Hypodermis: The underlying adipose tissue.
There are three primary pathways for molecular penetration through the skin [41]:
- Transepidermal Pathway: Diffusion directly across the SC, which can be intercellular (through the lipid matrix) or transcellular (through corneocytes).
- Transfollicular (or Pilosebaceous) Pathway: Diffusion via hair follicles and associated sebaceous glands.
- Transglandular Pathway: Diffusion via sweat glands. The intercellular transepidermal route is considered the major pathway for the passive diffusion of most small, uncharged molecules [41].
Factors Influencing Transdermal Delivery and Enhancement Strategies
Effective transdermal delivery is highly dependent on the physicochemical properties of the drug molecule. Key parameters include [41]:
- Molecular Weight (MW): Molecules under 500 Da permeate readily; permeability decreases significantly as MW increases.
- Lipophilicity: A balanced lipophilicity (log P ~ 1-3) is ideal for partitioning into both the SC lipids and the aqueous viable epidermis.
- Melting Point: Lower melting points generally correlate with higher solubility and skin permeability.
Due to the excellent barrier function of the SC, various enhancement strategies are employed [42] [41]:
- Chemical Permeation Enhancers: Substances like ethanol, fatty acids, and terpenes that temporarily disrupt the SC lipid matrix.
- Physical Methods: Techniques like microneedles (MNs), iontophoresis, and sonophoresis that create physical microchannels or use energy to drive molecules through the skin.
- Nanotechnological Carriers: Systems like liposomes, ethosomes, and solid lipid nanoparticles (SLNs) that can encapsulate drugs and enhance their solubility and skin interaction.
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Reagents and Models for Permeability Research
| Reagent/Model Name | Type/Class | Primary Function in Research |
|---|---|---|
| Caco-2 Cell Line | In Vitro Model | Human colorectal adenocarcinoma cell line; forms polarized monolayers with TJs used as a standard model for predicting intestinal drug absorption [36]. |
| Enteroid-Derived Cells (e.g., J2, D109) | In Vitro Model | Primary human intestinal stem cell-derived cultures; offer segment-specific (jejunum, duodenum), physiologically relevant morphology and barrier function [36]. |
| EpiIntestinalTM | In Vitro Tissue Model | Commercially available reconstructed human small intestinal tissue; used for permeability and absorption studies in a ready-to-use format [36]. |
| Lactulose and Mannitol | Probe Molecules | Non-metabolized sugars used in combination (L:M test) to assess human intestinal permeability in vivo (paracellular vs. transcellular) [37]. |
| FITC-Dextran | Probe Molecule | Fluorescently-labeled polysaccharide; used to trace and quantify macromolecular permeability in vascular (e.g., BBB) and intestinal models [40]. |
| Claudin-5 Antibody | Research Antibody | Targets key tight junction protein critical for blood-tissue barrier integrity (e.g., BBB); used in WB, IF to assess junctional integrity [43] [40]. |
| Occludin & ZO-1 Antibodies | Research Antibodies | Target key tight junction proteins; used to visualize and quantify TJ integrity and distribution in endothelial and epithelial barriers via IF and WB [40]. |
| Microneedles (MNs) | Physical Enhancement | Create microscopic conduits through the stratum corneum to dramatically enhance transdermal delivery of drugs, vaccines, and macromolecules [42] [41]. |
| 15-Dihydroepioxylubimin | 15-Dihydroepioxylubimin, MF:C15H26O3, MW:254.36 g/mol | Chemical Reagent |
| (R)-CCG-1423 | (R)-CCG-1423, MF:C18H13ClF6N2O3, MW:454.7 g/mol | Chemical Reagent |
Visualizing Experimental Workflows
The following diagrams illustrate core experimental workflows and permeability pathways discussed in this whitepaper.
Intestinal Permeability Assessment Workflow
Vascular Permeability Pathways
Transdermal Drug Delivery Enhancement Strategies
Advanced Methodologies for Assessing Tissue Permeability in Research and Development
Molecular imaging represents a transformative approach in biomedical sciences, enabling the non-invasive visualization, characterization, and quantification of biological processes at the molecular and cellular levels within living organisms. This capability is particularly crucial for understanding the role of tissue permeability in whole-body in situ hybridization (WISH) background research, as it allows researchers to track how molecules traverse biological barriers in their native physiological context. Molecular imaging relies fundamentally on molecular probes and tracers—specialized detection molecules that accumulate in specific tissues or interact with particular molecular targets to generate measurable signals [44] [45]. These engineered agents provide critical insights into cellular functions, metabolic activities, and disease mechanisms that would otherwise remain inaccessible without invasive procedures.
The significance of molecular probes extends beyond basic research into drug development, where they facilitate early assessment of drug candidates' bioavailability, tissue penetration, and target engagement [46]. For WISH-related research, which traditionally localizes gene expression in fixed tissues, molecular tracers offer a dynamic complement by revealing how tissue permeability characteristics influence molecular access to potential gene targets in living systems. The development of increasingly sophisticated probes continues to expand our capability to interrogate biological systems, with recent advancements focusing on multimodal imaging approaches that combine complementary techniques to overcome the limitations of individual modalities [45] [46].
Fundamental Principles of Molecular Probes
Core Components and Design Considerations
Effective molecular probes function as targeted detection systems comprising several integrated components. Each probe typically contains a targeting moiety that confers specificity for particular molecules, cells, or physiological processes; a signaling agent that generates detectable contrast; and often a connector that links these elements while maintaining their respective functions [45] [46]. The targeting component can range from antibodies and peptides to aptamers and small molecules, each offering distinct advantages in size, affinity, stability, and immunogenicity [45]. The signaling element varies by imaging modality and may include fluorophores for optical imaging, radionuclides for nuclear medicine techniques, or nanoparticles for magnetic resonance and computed tomography applications.
The design of molecular probes must carefully balance multiple pharmacological and practical considerations. Biocompatibility remains paramount, as probes must exhibit minimal toxicity while maintaining stability in physiological environments [45]. For in vivo applications, pharmacokinetics significantly influences probe performance, including its absorption, distribution, metabolism, and excretion characteristics. Optimal probes demonstrate high target-to-background ratios, achieved through specific binding and efficient clearance from non-target tissues [47] [45]. Additionally, practical factors such as shelf stability, ease of synthesis, and cost-effectiveness profoundly impact a probe's accessibility and translational potential [45]. For tissue permeability studies specifically, molecular size and charge characteristics must be carefully matched to the research question, as these properties fundamentally influence transit across biological barriers.
Probe Characteristics and Tissue Permeability
The physicochemical properties of molecular probes directly determine their tissue permeability and distribution patterns—a consideration especially relevant for WISH background research investigating gene expression accessibility. Smaller probes typically demonstrate enhanced diffusion capabilities, while larger constructs may be limited by vascular endothelial barriers and extracellular matrix constraints [47]. The following table summarizes key probe characteristics affecting tissue permeability:
Table 1: Molecular Probe Characteristics Affecting Tissue Permeability
| Property | Impact on Tissue Permeability | Research Considerations |
|---|---|---|
| Molecular Size | Determines diffusion rates and exclusion from certain compartments; smaller probes (<1 kDa) diffuse more readily [47] | Critical for blood-brain barrier and placental transfer studies; impacts clearance kinetics |
| Charge | Influences interaction with cellular membranes and extracellular matrix; affects solubility | Cationic probes may show non-specific binding; anionic probes may be repelled by negatively charged membranes |
| Lipophilicity | Governs passive diffusion across lipid membranes; highly lipophilic compounds may accumulate in adipose tissue | Balanced hydrophilicity-lipophilicity optimizes tissue penetration while maintaining solubility |
| Stability | Resistance to metabolic degradation extends circulation time and enables imaging over longer periods [45] | Protease susceptibility particularly relevant for peptide-based probes; affects signal duration |
| Target Affinity | High affinity increases retention at target site but very high affinity may limit penetration beyond first binding site | Optimization required for sufficient signal without "binding barrier" effect |
Major Imaging Modalities and Their Tracers
Optical Imaging Techniques
Optical molecular imaging encompasses techniques that utilize light-emitting probes to visualize biological processes. Widefield fluorescence microscopy represents one of the most accessible forms, offering large fields of view and rapid acquisition times, making it ideal for initial screening applications [48]. However, this technique suffers from background fluorescence and optical artifacts, particularly in thicker samples. Confocal microscopy addresses some limitations of widefield systems by employing pinhole apertures to eliminate out-of-focus light, significantly improving image clarity through optical sectioning capabilities [48]. The point-scanning approach of traditional confocal systems, however, can be time-consuming and potentially phototoxic, leading to the development of spinning disk confocal systems that spread excitation light across thousands of pinholes scanning rapidly across the specimen, thereby reducing photodamage while maintaining resolution [49].
For deeper tissue penetration, multiphoton fluorescence microscopy utilizes near-infrared excitation light to enable optical sectioning hundreds of microns into samples with minimal photodamage outside the focal plane [48]. This technique is particularly valuable for in vivo imaging applications where tissue integrity must be preserved. Total Internal Reflection Fluorescence (TIRF) microscopy specializes in visualizing events occurring near cellular surfaces by exploiting evanescent waves that penetrate only a few hundred nanometers into samples [48]. While TIRF provides exceptional resolution for membrane-associated processes, it cannot image deeper cellular structures. The expanding repertoire of fluorescent probes—including fluorescent proteins, organic dyes, and nanocrystals—continues to enhance the capabilities of optical imaging modalities, with near-infrared fluorophores increasingly favored for reduced autofluorescence and improved signal-to-noise characteristics [48].
Nuclear Medicine and Other Modalities
Nuclear medicine imaging techniques, particularly Positron Emission Tomography (PET) and Single-Photon Emission Computed Tomography (SPECT), utilize radiolabeled compounds to provide highly sensitive, quantitative information about metabolic processes and molecular targets in vivo [44]. These approaches excel at whole-body imaging with unparalleled sensitivity, enabling detection of picomolar tracer concentrations. PET tracers such as fluorodeoxyglucose (18F-FDG) have become clinical mainstays for imaging glucose metabolism in cancer and neurological disorders [44]. The short half-lives of many radionuclides, however, necessitate specialized production facilities and limit tracer availability in resource-constrained settings [45].
Magnetic Resonance Imaging (MRI) offers exceptional soft tissue contrast and spatial resolution without ionizing radiation. Molecular MRI probes typically employ paramagnetic or superparamagnetic materials to alter relaxation times of water protons, generating contrast differences that highlight specific tissues or molecular targets [44] [45]. Recent innovations include responsive agents that change signal properties in reaction to specific physiological stimuli, such as pH or enzyme activity. Photoacoustic imaging represents an emerging modality that combines the high contrast of optical imaging with the penetration depth of ultrasound, detecting sound waves generated by light absorption in tissue [45]. This hybrid approach benefits from endogenous contrast sources like hemoglobin while accommodating exogenous probes including gold nanoparticles and organic dyes. The complementary strengths of these modalities have spurred development of multimodal imaging approaches that overcome individual limitations through combined implementation [45] [46].
Table 2: Comparison of Major Molecular Imaging Modalities
| Imaging Modality | Sensitivity | Spatial Resolution | Penetration Depth | Common Tracer Types | Key Applications |
|---|---|---|---|---|---|
| Optical Imaging | High (nM-pM) | 1-10 μm | 1-2 mm (up to cm with NIR) | Fluorescent proteins, organic dyes, nanocrystals [48] | Cellular tracking, gene expression, surgical guidance |
| PET | Very High (pM) | 3-5 mm | Unlimited | 18F-FDG, 11C-labeled compounds, 68Ga-labeled peptides [44] [45] | Metabolic imaging, receptor quantification, whole-body screening |
| SPECT | High (nM) | 5-10 mm | Unlimited | 99mTc-labeled compounds, 123I-labeled ligands | Receptor imaging, perfusion studies, infection localization |
| MRI | Low (μM-mM) | 25-100 μm | Unlimited | Gd-cheltates, iron oxide nanoparticles, hyperpolarized agents [44] [45] | Anatomical imaging, functional assessment, cell tracking |
| Photoacoustic | Moderate | 50-500 μm | 3-5 cm | Organic dyes, gold nanoparticles, carbon nanotubes [45] | Vascular imaging, tumor detection, oxygen saturation mapping |
Experimental Protocols for Tracer Studies
Live-Cell Fluorescence Imaging Methodology
Successful live-cell fluorescence imaging requires careful optimization to balance signal detection against phototoxicity concerns. The following protocol outlines key considerations for robust experimental design:
Instrument Setup and Optimization:
- Microscope Selection: Choose spinning disk confocal microscopes over laser scanning confocals for live-cell imaging when possible, as they spread excitation light over thousands of pinholes, reducing ground-state depletion and photodamage [49].
- Excitation Control: Implement hardware-triggered shutters directly controlled by the camera to minimize unnecessary light exposure. Software-controlled shutters often have significant delays (hundreds of milliseconds) that unnecessarily expose samples to light [49].
- Objective Selection: Use the lowest magnification compatible with resolution requirements, as specimen irradiance increases drastically with magnification. Select bright objectives with high numerical aperture to maximize light collection [49].
- Camera Considerations: For most live-cell applications (excluding single-molecule imaging), cooled interline CCD cameras typically provide better value than EM-CCDs, which amplify both signal and background fluorescence equally [49].
Environmental Control and Sample Preparation:
- Viability Maintenance: Maintain cells in physiological conditions (37°C, 5% CO₂) using environmental chambers throughout imaging. For tissue samples, implement appropriate perfusion systems [49].
- Probe Selection and Loading: Choose fluorescent tracers based on brightness, photostability, and compatibility with biological systems. For long-term tracking, cell-permeant tracers like CellTracker probes offer superior retention through multiple cell divisions [47].
- Phototoxicity Minimization: Reduce excitation light intensity and exposure time to the minimum required for acceptable signal-to-noise ratio. Remember that photobleaching generates free radicals that compromise cell viability [49].
Image Acquisition Parameters:
- Exposure Optimization: Begin with minimal exposure times and increase only as needed. Use camera binning to improve signal-to-noise for dim samples when high resolution isn't critical [49].
- Temporal Resolution: Balance acquisition frequency against photodamage. For slow processes, fewer time points prolong cell viability.
- Multicolor Imaging: When imaging multiple fluorophores, sequence acquisitions from longest to shortest wavelength to minimize cross-talk and photobleaching.
NanoBRET Kinase Engagement Assay Protocol
The NanoBRET (NanoLuc Binary Resonance Energy Transfer) target engagement assay enables quantitative assessment of small molecule interactions with nearly 200 full-length kinases in live cells. This protocol represents a significant workflow improvement through its use of a single tracer at four different concentrations [50]:
Plasmid Preparation (Timing: 1-10 hours):
- Obtain the library of plasmids encoding NanoLuc/kinase fusions (commercially available from Promega).
- Prepare concentrated DNA stock solutions (0.2 mg/mL) containing 0.18 mg/mL diluent DNA (Transfection Carrier DNA or cyclin DNA as specified in Table 1 of the reference) and 0.02 mg/mL kinase/Nluc fusion DNA [50].
- For day-to-day experiments, prepare 2× working DNA solutions by diluting stock solutions 1:10 into nuclease-free TE buffer to achieve 20 μg/mL final DNA concentration.
- Store DNA plates at -20°C with foil tape covers to prevent evaporation. Thaw plates by centrifugation before removing seals to minimize cross-contamination.
Cell Transfection and Tracer Incubation:
- Seed appropriate cell lines (typically HEK-293) in assay plates 24 hours before transfection to achieve 70-90% confluence at time of transfection.
- Transfect cells with the 2× working DNA solutions using preferred transfection method optimized for your cell type.
- Incubate transfected cells for 24-48 hours to allow expression of kinase-NanoLuc fusion proteins.
- Add NanoBRET Tracer K10 at four different concentrations (typically ranging from 25 nM to 250 nM depending on the specific kinase) to determine optimal assay conditions [50].
BRET Measurement and Data Analysis:
- Treat cells with kinase inhibitors at desired concentrations alongside vehicle controls.
- Measure both donor emission (460 nm) and acceptor emission (610 nm) using a compatible plate reader.
- Calculate BRET ratios as acceptor emission divided by donor emission.
- Determine target engagement by comparing BRET ratios in inhibitor-treated cells versus vehicle controls, quantifying the percentage of kinase occupancy by the inhibitor [50].
This protocol provides a live-cell context for assessing kinase inhibitor engagement, often revealing selectivity differences compared to cell-free systems, thereby offering more physiologically relevant pharmacological data [50].
Visualization of Experimental Workflows
Molecular Probe Design and Mechanism
The following diagram illustrates the core components and mechanisms of action of molecular imaging probes, highlighting their functional modules and targeting strategies:
Molecular Probe Design and Mechanism
Live-Cell Imaging Optimization Workflow
This workflow diagram outlines the critical steps for optimizing live-cell fluorescence imaging experiments to maximize data quality while preserving cell viability:
Live-Cell Imaging Optimization Workflow
Research Reagent Solutions
The following table provides a comprehensive overview of essential reagents and materials used in molecular probe development and tracer studies, serving as a practical resource for researchers designing experiments in this field:
Table 3: Essential Research Reagents for Molecular Probe Studies
| Reagent Category | Specific Examples | Primary Applications | Key Considerations |
|---|---|---|---|
| Fluorescent Tracers | CellTracker probes, Lucifer yellow, Cascade Blue hydrazide, Alexa Fluor hydrazides [47] | Long-term cell tracking, gap junction communication, cytoplasmic labeling | Membrane permeability, retention characteristics, photostability, compatibility with fixation |
| Lipophilic Membrane Labels | DiI, DiO, DiD, DiR, FM 1-43, FM 4-64 [47] | Neuronal tracing, membrane dynamics, cell association assays | Lateral diffusion rate, persistence through fixation, spectral properties |
| Nanoparticle Tracers | Qtracker Cell Labeling Kits, FluoSpheres microspheres, gold nanoparticles [47] [45] | Long-term transplantation studies, vascular tracing, photothermal applications | Size distribution, surface functionalization, potential phagocytosis, biocompatibility |
| Biotin-Based Tracers | Biocytin, biotin dextran conjugates [47] | Neuronal connectivity mapping, intracellular labeling | Requires fixation and permeabilization for detection, compatible with enzyme-based amplification |
| Protein Tracers | Cholera toxin subunit B conjugates, phycoerythrin complexes [47] | Membrane binding studies, receptor trafficking | Well-defined molecular weight, potential biological activity, immunogenicity concerns |
| Radiolabeled Compounds | 18F-FDG, 68Ga-labeled peptides, 99mTc complexes [44] [45] | PET/SPECT imaging, metabolic studies, whole-body distribution | Short half-life, specialized facilities required, quantitative capabilities |
| MRI Contrast Agents | Superparamagnetic iron oxide nanoparticles, Gd-cheltates [44] [45] | Cell tracking, anatomical imaging, functional studies | Sensitivity limitations, potential metal toxicity, complementary anatomical information |
Molecular probes and tracer methodologies continue to evolve rapidly, driven by advances in chemistry, materials science, and optical engineering. The ongoing development of multimodal probes that combine complementary imaging signals represents a particularly promising direction, enabling researchers to leverage the respective strengths of different modalities while overcoming their individual limitations [45] [46]. Similarly, the expansion of nanoparticle-based platforms offers unprecedented opportunities for creating probes with enhanced targeting capabilities, improved pharmacokinetics, and integrated therapeutic functions in theranostic applications [45].
For WISH background research specifically, molecular tracers provide invaluable tools for investigating how tissue permeability characteristics influence molecular access to gene targets—a crucial consideration often overlooked in conventional fixed-tissue analyses. The integration of molecular imaging data with transcriptomic and proteomic approaches will likely yield more comprehensive understanding of gene expression regulation in physiological and pathological contexts. However, significant challenges remain in optimizing probe specificity, reducing potential immunogenicity, and ensuring reliable clinical translation [45]. As these technical hurdles are progressively addressed through innovative probe design and rigorous validation, molecular imaging methodologies will continue to transform both basic research and clinical practice, ultimately enhancing our ability to visualize and understand complex biological systems in their native context.
The intestinal epithelial barrier serves as a critical interface, separating the internal milieu from the external environment and maintaining a symbiotic relationship with intestinal microbes. Composed of a single layer of epithelial cells linked by tight junction (TJ) protein complexes, this barrier prevents the uncontrolled passage of luminal contents, including pathogens, antigens, and other harmful agents [51] [52]. The integrity of this barrier is paramount for human health; its dysfunction, often described as "leaky gut," has been implicated in the pathogenesis of a wide range of conditions, including inflammatory bowel disease (IBD), celiac disease, cystic fibrosis, allergic respiratory diseases, and potentially colorectal cancer [51] [53] [54]. Consequently, accurate assessment of epithelial barrier function is a cornerstone of gastrointestinal, pulmonary, and pharmacological research.
Among the various techniques available for evaluating barrier integrity, the Ussing chamber system stands out as the gold standard for ex vivo investigation. Developed by Danish biologist Hans Ussing in the 1950s to study active ion transport, the system has been refined over decades into a powerful tool for quantifying permeability, ion transport, and barrier function with high physiological relevance [51] [54] [55]. This whitepaper details the principles, methodologies, and applications of the Ussing chamber, positioning it as an indispensable technology within a broader research framework investigating tissue permeability.
The Ussing Chamber System: Core Principles and Measured Parameters
The fundamental design of an Ussing chamber involves mounting a section of live epithelial tissue or a cell monolayer between two half-chambers, creating a sealed physical separation between the apical (mucosal) and basolateral (serosal) compartments. This setup allows researchers to independently control the composition of solutions on each side and perform real-time measurements of electrical and flux-based parameters [56] [54].
Key Electrical and Flux Parameters
The Ussing chamber provides simultaneous, quantitative readouts of epithelial function through electrophysiological and chemical flux measurements.
Table 1: Core Parameters Measured in an Ussing Chamber Setup
| Parameter | Abbreviation | What It Measures | Interpretation | Typical Units |
|---|---|---|---|---|
| Short-Circuit Current | I~sc~ | The net active ion transport across the epithelium. | Summation of all active ion currents (e.g., Na+ absorption, Cl- secretion). | µA/cm² |
| Transepithelial Resistance | TER (or TEER) | The electrical resistance to passive ion flow, primarily governed by tight junctions. | Indicator of paracellular barrier integrity. A low TER suggests "leaky" epithelium. | Ω·cm² |
| Potential Difference | PD | The innate voltage across the epithelium due to active ion transport. | Indicator of tissue health and viability. | mV |
| Apparent Permeability Coefficient | P~app~ | The permeability of a specific molecule (e.g., a drug or probe) across the barrier. | Quantitative measure of compound flux; used to predict drug absorption. | cm/s |
Transepithelial Electrical Resistance (TER) is a direct indicator of the integrity of the paracellular pathway, which is controlled by tight junctions. A decrease in TER is indicative of increased paracellular permeability and is often associated with the downregulation of "sealing" TJ proteins like ZO-1, occludin, and JAM-A, or the upregulation of "pore-forming" claudins such as claudin-2 [51]. Short-Circuit Current (I~sc~) represents the current required to nullify the tissue's innate potential difference, providing a real-time measurement of net active ion transport [51] [55]. Finally, Paracellular Flux studies involve adding fluorescently-labeled probes like 4 kDa FITC-dextran or lucifer yellow to one chamber and measuring their appearance in the opposite chamber over time. This provides a direct, functional assessment of macromolecular permeability [51] [57].
The synergy of these measurements allows researchers to dissect complex epithelial responses. For instance, a drop in TER with a concurrent increase in FITC-dextran flux confirms a breakdown in the physical barrier, while a change in I~sc~ can reveal the activation of specific ion channels or transporters by a drug or toxin [56].
Signaling Pathways Governing Epithelial Barrier Integrity
The molecular regulation of barrier function involves a complex interplay of signaling pathways that control the expression and localization of tight junction proteins. Key findings from recent research illustrate this complexity.
Table 2: Key Signaling Pathways and Molecular Regulators of Epithelial Barrier Function
| Regulator/Pathway | Effect on Barrier | Proposed Mechanism | Experimental Context |
|---|---|---|---|
| Aryl Hydrocarbon Receptor (AHR) | Enhancement | AHR activation upregulates zinc importers, increasing cellular zinc. Zinc then inhibits NF-κB and calpain, leading to increased tight junction protein expression [52]. | Human Caco-2 cells, ileum organoids, mouse IBD model. |
| Junctional Adhesion Molecule 1 (JAM1) | Maintenance | JAM1, a tight junction-associated protein, is critical for forming the paracellular seal. Its loss increases permeability to bacterial factors like LPS [58]. | Human gingival epithelial cells, 3D gingival tissue model. |
| HAX1 Gene | Disruption (when deficient) | HAX1 dysfunction leads to JAM1 being missorted into lysosomes for degradation, thereby disrupting the epithelial barrier [58]. | Kostmann syndrome model; human gingival epithelial cells. |
| Zinc | Enhancement | Acts as a critical co-factor for AHR-mediated barrier protection. Stabilizes tight junctions by inhibiting NF-κB and calpain activity [52]. | Human Caco-2 cells, mouse models with defined zinc diets. |
| Pro-inflammatory Cytokines (e.g., TNF-α, IFN-γ) | Disruption | Downregulate "sealing" tight junction proteins and can alter the cytoskeleton, leading to increased paracellular permeability [51] [59]. | Various in vitro and ex vivo inflammatory models. |
Diagram 1: Signaling pathways in barrier integrity and disruption. The AHR-zinc pathway (yellow/green) enhances barrier function, while HAX1 dysfunction (red) leads to breakdown.
Experimental Protocol: A Step-by-Step Guide
The following protocol, adapted from modern methodologies, provides a detailed guide for assessing intestinal permeability using the Ussing chamber system [51].
Pre-experimental Setup and Buffer Preparation
- Buffer Formulation: Prepare Krebs buffer solutions. A standard Transport Krebs buffer contains 115.6 mM NaCl, 1.3 mM CaCl₂·2H₂O, 3.7 mM KCl, 1.4 mM KH₂PO₄, 23 mM NaHCO₃, and 1.2 mM MgSO₄·7H₂O. Adjust the pH to 7.3 after oxygenation [51].
- Chamber Preparation: Clean Ussing chambers with a detergent like RBS buffer in hot water and dry thoroughly. Apply a thin, even layer of vacuum grease to the inner surfaces of the chamber halves. Place punched x-ray film squares over the chamber pins to create the aperture for the tissue. Connect the chamber halves and secure them with circlips [51].
- Electrode Preparation: Ensure Ag/AgCl electrodes are properly chlorided. Remove old AgCl coating with steel wool and immerse electrodes in household bleach for 24-48 hours before the experiment. Rinse with deionized water. Fill the electrode glass barrels with 3 M KCl electrolyte solution, ensuring no air bubbles block the ceramic junction [51].
Tissue Dissection and Mounting
- Tissue Harvesting: Following ethical approval and humane sacrifice of the animal (e.g., mouse), immediately dissect the required intestinal segment (e.g., colon, ileum). Place the tissue in ice-cold, oxygenated Transport Krebs buffer to maintain viability [51].
- Tissue Preparation: Open the intestinal segment longitudinally along the mesenteric border and flush gently with buffer to remove luminal contents. Using fine dissection tools, carefully strip away the outer muscle layers to obtain the mucosal sheet. This step reduces smooth muscle contractility that can interfere with measurements.
- Mounting: Cut the prepared mucosal tissue to an appropriate size. Gently stretch it over the pre-greased aperture of the Ussing chamber, ensuring the mucosal side faces the correct half-chamber. Clamp the tissue securely in place, taking care not to damage it. Immediately fill both half-chambers with pre-warmed, oxygenated Krebs buffer [51].
System Equilibration and Measurement
- Equilibration: Maintain the chambers at 37°C using a circulating water bath. Continuously gas the buffers with carbogen (95% O₂ / 5% CO₂) using a gas-lift system, which also serves to mix the solutions. Allow the system to equilibrate until a stable baseline for PD and I~sc~ is achieved, typically for 15-30 minutes [51] [55].
- Electrical Measurements: Using the voltage/current clamp and acquisition software, measure the baseline TER and I~sc~. TER is often calculated by applying a short pulse of voltage or current and measuring the resulting change. The system should be short-circuited (I~sc~ mode) for most of the experiment, with periodic open-circuit measurements to determine TER [55].
- Flux Measurements: To measure paracellular permeability, add a fluorescent probe like 4 kDa FITC-dextran to the mucosal chamber. Take sequential samples from the serosal chamber over time (e.g., every 30 minutes for 2 hours) and measure fluorescence using a plate reader. The apparent permeability coefficient (P~app~) can be calculated using the formula: P~app~ = (dQ/dt) / (A × C₀), where dQ/dt is the steady-state flux rate, A is the diffusion area, and C₀ is the initial donor concentration [51] [56] [57].
- Viability Controls: Monitor tissue viability throughout the experiment by ensuring stable baselines for TER and I~sc~. A progressive decline in these parameters suggests loss of tissue viability, and data collected beyond this point may be unreliable.
Advanced Applications and Validation in Research
The Ussing chamber's versatility makes it a powerful tool for investigating a wide array of research questions beyond basic barrier function.
Drug Absorption and Development
In pharmaceutical research, the Ussing chamber is pivotal for predicting oral drug absorption and optimizing formulations. It allows for the precise determination of whether a compound crosses the epithelium via passive transcellular diffusion, paracellular transport, or active carrier-mediated pathways. By adding specific transporter inhibitors (e.g., for P-glycoprotein) or modifying pH, researchers can dissect the dominant transport mechanisms. Furthermore, different drug formulations (e.g., nanoparticles, liposomes) can be tested side-by-side to evaluate their impact on permeability [56].
Host-Microbiome and Toxin Interactions
The system is ideally suited for studying the direct effects of gut microbes, their metabolites, or toxins on the epithelial barrier. For example, research has demonstrated that specific commensals like Bifidobacterium adolescentis induce a rapid increase in permeability, while others like Bacteroides fragilis do not [57]. Similarly, the microbial metabolite putrescine has been shown to induce a dose-dependent increase in FITC-dextran flux [57]. These findings can be correlated with changes in TER and TJ protein expression to provide a comprehensive view of barrier dynamics.
Disease Modeling and Therapeutic Screening
Ussing chambers are widely used to model human diseases. For instance, studying biopsies from patients with IBD or celiac disease reveals characteristic reductions in TER and alterations in ion transport compared to healthy controls [51] [55]. The system also serves as a robust platform for screening therapeutic interventions. The protective effects of AHR ligands combined with zinc, for example, were convincingly demonstrated by their ability to improve TER and reduce FITC-dextran flux in Caco-2 cells and human ileum organoids under inflammatory challenge [52].
Table 3: Key Reagents and Materials for Ussing Chamber Experiments
| Category | Item | Function / Application |
|---|---|---|
| Buffers & Solutions | Krebs Buffer | Physiological saline solution to maintain tissue viability. |
| Fluorescent Probes (e.g., 4 kDa FITC-Dextran) | Tracer molecules to quantify paracellular flux and permeability. | |
| Pharmacological Agonists/Antagonists (e.g., Amiloride, Forskolin, Bumetanide) | To probe specific ion channels and transport pathways (ENaC, CFTR, NKCC1). | |
| Tissue & Cells | Native Tissue (Mouse/Human) | Provides the most physiologically relevant model for ex vivo studies. |
| Cell Lines (e.g., Caco-2, IPEC-J2) | Form differentiated monolayers on permeable supports for in vitro studies. | |
| Organoids (e.g., Human Ileum Organoids) | Advanced 3D models that can be differentiated into monolayers. | |
| Equipment & Consumables | Ussing Chamber System (e.g., EasyMount) | Core apparatus for mounting tissue and performing measurements. |
| Voltage/Current Clamp (e.g., VCC MC8) | Instrument for applying voltage/current and measuring I~sc~ and TER. | |
| Data Acquisition Software (e.g., Acquire & Analyze) | For real-time data recording, visualization, and analysis. | |
| Ag/AgCl Electrodes & 3 M KCl Electrolyte | Essential for accurate and stable electrical measurements. |
Emerging Trends and Future Perspectives
The field of epithelial barrier research is rapidly evolving, and the Ussing chamber is being integrated with cutting-edge technologies.
- Integration with Organoid and Organ-on-a-Chip Models: There is a growing trend of combining the physiological fidelity of the Ussing chamber with the human-relevance of stem cell-derived enteroid and organoid monolayers. This synergy creates powerful models for personalized medicine and disease modeling [59] [55].
- High-Throughput and Automated Systems: Modern systems are being designed with multi-channel clamping and automated fluid handling, increasing throughput and reproducibility while reducing operator-dependent variability [55].
- Combining Transport with Metabolism: Advanced applications now seek to not only measure drug permeability but also to quantify metabolite formation during transit across the epithelium, providing valuable insights into first-pass metabolism [55].
- Novel ex vivo Assays: Techniques like the ex vivo intestinal permeability assay (X-IPA) complement the Ussing chamber by allowing real-time, live-imaging of permeability changes in intact cultured gut tissues in response to luminal stimuli like specific bacteria or metabolites [57].
The Ussing chamber system remains the undisputed gold standard for the ex vivo assessment of epithelial barrier function. Its unique ability to provide simultaneous, real-time data on active ion transport (I~sc~), paracellular integrity (TER), and molecular flux (P~app~) in a physiologically relevant context is unmatched by simpler in vitro models. As research continues to illuminate the critical role of tissue permeability in health and disease, the Ussing chamber, especially when integrated with modern models like organoids and advanced imaging, will continue to be an indispensable tool for researchers and drug development professionals aiming to decipher the complex mechanisms governing the epithelial barrier and to develop novel barrier-targeting therapeutics.
DNA barcoding has emerged as a revolutionary tool for species identification, providing a standardized, genetic method to complement traditional morphology-based taxonomy. For invasion biology, this technique offers unprecedented capabilities for tracking population dynamics and identifying invasive species, which is critical for effective biosecurity and ecosystem management [60]. The core premise of DNA barcoding involves sequencing a short, standardized genetic fragment from a specimen and comparing it to curated reference libraries to determine species identity [60]. This approach is particularly valuable for identifying morphologically indistinct life stages, cryptic species, and damaged specimens that often challenge conventional diagnostic methods [61].
The global rise in international trade and tourism has significantly increased pathways for invasive alien species (IAS), with profound economic and ecological consequences. In Japan, for instance, approximately four exotic insect species become established each year, with nearly three-quarters becoming economic pests [61]. The potential cumulative economic losses from just two species—Asian gypsy moth (Lymantria dispar) and nun moth (Lymantria monacha)—in the United States were estimated at €28–46 billion between 1990 and 2004 [61]. DNA barcoding provides a proactive framework for identifying these threats early, enabling more effective management responses and potentially saving billions in control costs and ecosystem damage.
Core DNA Barcoding Methodologies and Workflows
Standard DNA Barcoding Markers
The selection of appropriate genetic markers is fundamental to successful DNA barcoding, with standard loci established for major taxonomic groups:
- Animals: The mitochondrial cytochrome c oxidase subunit I (COI) gene serves as the primary barcode, using a 658-base pair region of the COI gene [62] [63] [60]. This region provides sufficient sequence variation to distinguish most animal species while containing conserved regions for primer binding.
- Land Plants: The core plant barcode consists of two plastid genes, rbcL and matK, which together provide broad amplification success and discriminatory power [60]. The nuclear ITS or ITS2 regions are often added as supplemental markers for increased resolution in closely related species [60].
- Fungi and Algae: The Internal Transcribed Spacer (ITS/ITS2) regions of ribosomal DNA serve as the primary barcode due to their high variability and discriminatory power across fungal taxa [60].
Laboratory Workflow for Specimen Processing
The standard DNA barcoding protocol involves multiple stages from specimen collection to sequence analysis:
Sampling and Documentation: Assign unique identifiers to each specimen and record comprehensive metadata including collection date, location, habitat, and morphological notes. Preserve tissues in 95-100% ethanol or silica gel to maintain DNA integrity [60].
DNA Extraction: Use validated extraction methods appropriate for the sample type (e.g., Nucleospin Tissue kit). Include negative controls to detect contamination and positive controls to verify protocol performance [63] [60].
PCR Amplification: Amplify the target barcode region using group-specific primers. For Lepidoptera and other insects, the LepF1 (5'-ATTCAACCAATCATAAAGATATTGG-3') and LepR1 (5'-TAAACTTCTGGATGTCCAAAAAATCA-3') primers target the COI Folmer region [63]. Reaction conditions typically include: initial denaturation at 95°C for 5 minutes; 35 cycles of 94°C for 40s, 51°C for 1 minute, 72°C for 30s; final extension at 72°C for 5 minutes [63].
Sequencing: Utilize Sanger sequencing for individual specimens or next-generation sequencing (NGS) platforms for high-throughput applications. For 454 pyrosequencing, design unique 10-mer oligonucleotide tags (Multiple Identifiers - MIDs) attached to PCR primers to multiplex hundreds of specimens in a single run [63].
Data Analysis: Process raw sequences through quality control, trim low-quality bases, and compare to reference databases such as the Barcode of Life Data System (BOLD) and GenBank [62] [60].
Reference Databases and Species Delimitation
The Barcode of Life Data System (BOLD) serves as the central informatics platform for DNA barcoding, providing a cloud-based data storage and analysis environment [62]. For species delimitation, BOLD employs the Refined Single Linkage (RESL) algorithm which clusters sequences below a 2.2% divergence threshold into Operational Taxonomic Units (OTUs) assigned unique Barcode Index Numbers (BINs) [62]. These BINs provide a standardized system for tracking genetic diversity and identifying potentially cryptic taxa, which is particularly valuable for invasion tracking where species boundaries may be unclear.
Figure 1: Comprehensive workflow for DNA barcoding in invasion biology applications, spanning from field collection to data analysis.
Advanced Applications for Tracking Invasion Dynamics
Environmental DNA (eDNA) Metabarcoding
Recent advances in eDNA metabarcoding enable large-scale monitoring of invasive species in aquatic and terrestrial ecosystems without direct specimen collection. In large river systems, where conventional surveys are logistically challenging, eDNA metabarcoding can simultaneously detect aquatic vegetation, invasive species, and land-use indicators from water samples [64]. A 2025 study on the Upper Rhine River demonstrated the effectiveness of this approach, recovering 24 aquatic plant species (18% of sequence reads) and detecting 16 exotic species, highlighting its potential for catchment-wide invasion monitoring and management [64].
Biosecurity and Border Interception
DNA barcoding has proven particularly valuable for biosecurity applications at national borders, where rapid and accurate identification of intercepted specimens is critical. Comparative studies have demonstrated superior performance of DNA barcoding over previous molecular methods. When New Zealand border interceptions of tussock moths and fruit flies were reanalyzed using COI barcoding, species identification agreement with previous PCR-RFLP methods was 90% and 96%, respectively, with additional resolution of previously unidentifiable specimens and species complex differentiation [61].
Table 1: Comparison of DNA Barcoding with Traditional Molecular Methods for Biosecurity
| Parameter | PCR-RFLP Methods | DNA Barcoding |
|---|---|---|
| Taxonomic Range | Limited to predetermined species (typically <50) | Virtually unlimited; adaptable to any species |
| Method Transferability | Low; protocols rarely transferable between labs | High; standardized protocols and data sharing |
| Data Comparability | Limited; different gene regions and methods used | High; standardized COI region enables global comparisons |
| Unpredicted Taxa Handling | Poor; difficult to modify for new species | Excellent; sequences can be compared to growing reference databases |
| Resolution | Limited to known polymorphisms | High; complete sequence data enables complex resolution |
Population Dynamics and Source Tracking
The application of DNA barcoding extends beyond simple species identification to elucidating complex population dynamics and invasion pathways. By analyzing spatial and temporal patterns of genetic variation within and among populations, researchers can infer introduction routes, source populations, and demographic changes during invasion [62]. The Barcode Index Number (BIN) system allows for tracking population-level genetic diversity through time, providing insights into founder effects, genetic bottlenecks, and adaptive changes that occur during range expansion [62].
Technical Considerations and Limitations
Methodological Challenges
Despite its power, DNA barcoding faces several technical challenges that must be considered in invasion tracking studies:
- Incomplete Reference Databases: Many taxa, particularly from undersampled regions, lack comprehensive reference sequences, potentially leading to misidentifications or inability to assign species names to specimens [60].
- Biological Complications: Nuclear mitochondrial pseudogenes (numts), heteroplasmy, hybridization, and introgression can confound mitochondrial barcoding results, requiring additional verification [63] [60].
- Diagnostic Gaps: In some recently diverged species complexes or taxa with incomplete lineage sorting, the standard "barcoding gap" (the difference between intra- and interspecific variation) may be insufficient for reliable discrimination [62].
Analytical Frameworks
Proper interpretation of barcode data requires careful analytical consideration. Key aspects include:
- Multi-Marker Approaches: For problematic groups, combining standard barcodes with supplemental markers (e.g., nuclear genes for COI-based animal barcoding) improves resolution and confidence [60].
- Threshold-Based Delimitation: The RESL algorithm in BOLD uses a 2.2% divergence threshold for initial cluster formation, but subsequent refinement incorporates additional criteria [62].
- Integration with Traditional Taxonomy: DNA barcoding should complement, not replace, traditional morphological identification, especially for voucher specimens and type material [62] [61].
Table 2: DNA Barcode Markers for Major Taxonomic Groups in Invasion Tracking
| Taxonomic Group | Primary Marker(s) | Secondary Marker(s) | Key Applications |
|---|---|---|---|
| Animals | COI (658 bp Folmer region) | - | Border interceptions, cryptic species detection, life stage association |
| Land Plants | rbcL + matK | ITS/ITS2 | Aquatic weed monitoring, riparian invasion tracking |
| Fungi | ITS/ITS2 | - | Plant pathogen tracking, ecosystem engineer identification |
| Freshwater Organisms | COI, 18S rRNA | - | Aquatic invasion monitoring via eDNA |
Integration with Tissue Permeability Research in WISH Context
The connection between DNA barcoding and tissue permeability research in Whole Organism In Situ Hybridization (WISH) backgrounds lies in their shared reliance on molecular permeability for biological assessment. While DNA barcoding identifies organisms through genetic sequence analysis, tissue permeability studies examine how molecules traverse biological barriers—a critical consideration for both WISH protocols and environmental DNA (eDNA) detection.
In WISH methodologies, controlled tissue permeability enables hybridization probes to access intracellular targets, similar to how eDNA fragments permeate through aquatic environments and cellular membranes to become detectable in environmental samples [64]. This permeability principle enables non-invasive detection of invasive species through aquatic eDNA sampling, where genetic material permeates from organisms into surrounding ecosystems [64]. Understanding these permeability dynamics enhances both DNA barcode detection efficiency and the spatial interpretation of detection results in invasion monitoring.
Essential Research Reagents and Materials
Table 3: Essential Research Reagents for DNA Barcoding workflows
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| DNA Extraction Kits | Nucleospin Tissue kit, DNeasy Blood & Tissue Kit | High-quality DNA extraction from various sample types |
| PCR Primers | LepF1/LepR1 (insects), rbcL-a-F/matK-1R (plants) | Amplification of standardized barcode regions |
| DNA Polymerases | Platinum Taq DNA Polymerase, Q5 High-Fidelity | Robust amplification with low error rates |
| Sequencing Platforms | ABI 3730XL (Sanger), 454 GS FLX+ (Pyrosequencing) | Sequence generation with different throughput needs |
| Quality Control Tools | Bioanalyzer, TapeStation, Sequence Scanner Software | Assessment of DNA quality and sequence reliability |
| Reference Databases | BOLD Systems, GenBank, Barcode Index Number (BIN) | Species identification and sequence validation |
Figure 2: Integration of DNA barcode data into comprehensive invasion species management frameworks.
DNA barcoding technologies continue to evolve, with significant advances in sequencing platforms and data analysis methods. The transition from Sanger sequencing to high-throughput platforms (Oxford Nanopore Technologies, Pacific Biosciences) has reduced costs by up to two orders of magnitude while increasing data output [62]. These advances enable more comprehensive monitoring programs and faster response times for incursion events.
The integration of DNA barcoding with emerging technologies like satellite monitoring, automated image recognition, and ecological modeling creates powerful synergies for invasion forecasting and management. As reference databases expand and analytical methods refine, DNA barcoding will play an increasingly central role in global efforts to understand and mitigate the impacts of biological invasions on ecosystems, economies, and human well-being.
For researchers in both invasion biology and tissue permeability fields, DNA barcoding offers a standardized, reproducible framework for species identification that transcends taxonomic expertise limitations and enables large-scale comparative studies. The continued refinement of these methodologies will further enhance their utility for tracking population dynamics and biological invasions in an increasingly interconnected world.
The integrity of biological barriers is a critical determinant of human health, with intestinal barrier function serving as a primary interface between the internal milieu and external environment. The identification and validation of circulating biomarkers for barrier integrity has emerged as a pivotal research area, particularly for investigating tissue permeability in therapeutic development. This technical guide provides a comprehensive analysis of established and emerging biomarkers—with particular focus on zonulin and intestinal fatty acid-binding protein (I-FABP)—detailing their biological functions, measurement methodologies, and application in research and clinical contexts. We synthesize current evidence on their roles in various disease states and provide standardized experimental protocols for reliable assessment of barrier function, offering researchers a foundational framework for integrating these biomarkers into systemic permeability investigations.
Biological barriers represent sophisticated interfaces that maintain physiological homeostasis through selective permeability, protecting internal compartments from environmental challenges while facilitating essential molecular transport. The gastrointestinal barrier constitutes one of the most extensive and clinically significant barriers, with its dysfunction implicated in diverse pathological states spanning gastrointestinal, metabolic, autoimmune, and neuropsychiatric domains [65] [28] [66].
The conceptualization of "leaky gut" or increased intestinal permeability has evolved from a contested notion to a recognized pathological feature in numerous disease processes. Intestinal permeability refers to the measurable passage of solutes, fluids, and molecules across the intestinal epithelium via paracellular (between cells) and transcellular (through cells) routes [66]. In health, this permeability is tightly regulated, but disruption of this balance can facilitate translocation of luminal contents—including bacteria, microbial components, and dietary antigens—into systemic circulation, potentially triggering local and systemic inflammatory responses [28] [66].
Circulating biomarkers offer a minimally invasive approach to assess barrier integrity in research and clinical settings. Unlike functional permeability tests requiring specialized protocols, blood-based biomarkers can be readily integrated into standard laboratory workflows, enabling broader application in longitudinal studies and therapeutic trials [67] [66]. This whitepaper focuses specifically on zonulin and I-FABP as key circulating indicators with distinct biological significance, while contextualizing them within the broader landscape of barrier integrity assessment.
Biomarker Profiles and Pathophysiological Significance
Zonulin: Regulator of Paracellular Permeability
Zonulin stands as the only known physiological modulator of intercellular tight junctions discovered in humans to date [65]. Identified as pre-haptoglobin2 (pre-HP2), this protein exists in two functionally distinct forms: the intact single-chain protein (zonulin) that regulates intestinal permeability, and the cleaved two-chain form that functions as a hemoglobin scavenger [65].
Biological Function and Mechanism: Zonulin modulates tight junction permeability primarily through proteinase-activated receptor 2 (PAR2) transactivation of epidermal growth factor receptor (EGFR) [65]. This signaling cascade leads to reversible disengagement of zonula occludens (ZO-1) from tight junction complexes, increasing paracellular flux [65]. Under physiological conditions, this mechanism facilitates innate immune responses by flushing out intestinal pathogens and regulates nutrient absorption [65].
Regulatory Triggers: Two primary stimuli for zonulin release have been identified: intestinal exposure to bacteria and gliadin (a wheat-derived protein) [65]. Bacterial-induced zonulin secretion occurs independently of microbial virulence and is restricted to the luminal aspect of the intestinal mucosa [65]. Gliadin activates zonulin release by engaging the chemokine receptor CXCR3, which recruits the adapter protein MyD88—a pathway notably overexpressed in celiac disease patients [65].
Clinical and Research Significance: Elevated zonulin levels correlate with increased intestinal permeability in numerous conditions. Approximately 50% of type 1 diabetes patients demonstrate elevated serum zonulin that precedes disease onset [65]. In celiac disease, zonulin up-regulation represents an initial step in pathogenesis, with levels normalizing following gluten elimination [65]. Recent research also implicates zonulin in obesity-associated insulin resistance, potentially mediated through IL-6 stimulation of zonulin gene expression via STAT3 activation [65]. Beyond gastrointestinal and metabolic conditions, zonulin elevation has been documented in neuropsychiatric disorders including depression, bipolar disorder, and neurodegenerative conditions [67] [68] [66].
Intestinal Fatty Acid-Binding Protein (I-FABP): Indicator of Enterocyte Damage
I-FABP represents a highly specific marker of enterocyte injury. This small (15 kDa) cytosolic protein is predominantly expressed in mature enterocytes of the small intestinal villi, with minimal expression in colonic epithelium [67] [66].
Biological Function and Mechanism: I-FABP facilitates intracellular transport of long-chain fatty acids and participates in lipid metabolism within enterocytes [67] [66]. Following epithelial cell damage, I-FABP rapidly releases into circulation due to its cytosolic localization and low molecular weight, providing a sensitive indicator of intestinal epithelial integrity compromise [67] [66].
Clinical and Research Significance: Elevated circulating I-FABP reflects ongoing enterocyte damage or necrosis, making it particularly valuable for assessing acute intestinal injury in conditions like ischemia, inflammatory bowel disease, and critical illness [67] [66]. In psychiatric research, I-FABP elevation has been reported in depression and bipolar disorder, suggesting subtle intestinal epithelial compromise in these populations [67] [68]. Unlike zonulin, which reflects functional permeability regulation, I-FABP serves as a direct marker of structural epithelial damage [67].
Additional Circulating Indicators
Lipopolysaccharide (LPS) and Related Proteins: LPS, a component of Gram-negative bacterial membranes, translocates across compromised intestinal barriers, triggering immune responses [67] [28]. LPS-binding protein (LBP) facilitates LPS binding to immune cells, while soluble CD14 (sCD14) mediates cellular responses to LPS, providing complementary markers of microbial translocation and immune activation [67].
Claudin-3: As a core structural component of tight junctions, claudin-3 enters circulation upon junctional complex disintegration [69]. Recent surgical research indicates claudin-3 may outperform zonulin in diagnosing postoperative intestinal barrier dysfunction, with area under curve values of 0.934 versus 0.826, respectively [69].
Table 1: Core Biomarkers of Intestinal Barrier Integrity
| Biomarker | Biological Role | What Elevated Levels Indicate | Primary Origin |
|---|---|---|---|
| Zonulin | Physiological regulator of tight junctions | Increased intestinal permeability | Intestinal epithelium |
| I-FABP | Cytosolic fatty acid transporter | Enterocyte damage/necrosis | Small intestinal enterocytes |
| LPS | Bacterial endotoxin | Microbial translocation | Gut microbiota |
| LBP | Binds and facilitates LPS signaling | Increased LPS exposure | Liver (in response to LPS) |
| sCD14 | Soluble receptor for LPS signaling | Immune activation | Monocytes, macrophages |
| Claudin-3 | Structural tight junction protein | Junctional complex disintegration | Intestinal epithelium |
Table 2: Biomarker Associations in Disease States
| Condition | Zonulin | I-FABP | LPS/LBP/sCD14 | Key Research Findings |
|---|---|---|---|---|
| Celiac Disease | ↑↑↑ | ↑ | ↑ | Zonulin upregulation initiates pathogenesis; normalizes with gluten withdrawal [65] |
| Type 1 Diabetes | ↑↑ | ↑ | ↑ | Zonulin elevation precedes clinical onset; 70% diabetes reduction with zonulin inhibition in animal models [65] |
| Bipolar Disorder | ↑↑ | ↑↑ | - | Significant correlations between zonulin and cognitive performance [68] |
| Major Depression | ↑ | ↑ | ↑ | Association with disease severity and treatment resistance [67] |
| Obesity/Insulin Resistance | ↑↑ | - | ↑↑ | Zonulin correlates with BMI, IL-6, and insulin resistance [65] |
| Abdominal Surgery | ↑↑ | - | - | Claudin-3 demonstrates superior diagnostic accuracy vs. zonulin [69] |
Experimental Protocols and Methodological Considerations
Biomarker Measurement Techniques
Sample Collection and Processing: For circulating biomarkers, venous blood collection in serum separator tubes followed by centrifugation (3000×g for 15 minutes at 4°C) represents the standard approach. Serum aliquots should be stored at -80°C until analysis to maintain biomarker stability [67] [68] [66].
Analytical Methods:
- Zonulin Quantification: Commercial ELISA kits provide the most widely utilized methodology, with measurements typically reported in ng/mL. Methodological consistency is crucial as inter-assay variability represents a significant challenge in zonulin measurement [65] [67].
- I-FABP Measurement: Enzyme-linked immunosorbent assay (ELISA) constitutes the primary detection method, with concentrations conventionally expressed in pg/mL [67] [66].
- LPS/LBP/sCD14 Assessment: ELISA platforms similarly predominate for these biomarkers, though LPS activity assays provide functional assessment of endotoxin exposure [67] [28].
Complementary Permeability Assessments: While circulating biomarkers offer practical advantages, traditional permeability tests utilizing probe molecules (lactulose, mannitol, sucralose) with urinary measurement remain valuable for functional barrier assessment [67] [70] [66]. These approaches directly measure paracellular and transcellular solute passage, providing functional correlation for biomarker findings [70] [66].
Stimulation Protocols for Barrier Function Research
Gliadin Exposure Model: To investigate zonulin-mediated permeability pathways, researchers can utilize gliadin stimulation protocols. In vitro, intestinal cell lines or biopsy specimens are exposed to gliadin peptides (1 mg/mL for 2-4 hours), followed by zonulin measurement in supernatant and assessment of transepithelial electrical resistance (TEER) [65]. In human challenge studies, oral gluten administration (10-20g) with serial blood sampling at baseline, 1, 2, and 4 hours enables evaluation of acute zonulin response and permeability changes [65].
High-Fat/High-Carbohydrate Meal Challenge: Standardized nutrient challenges (e.g., 900-1000 kcal meals with 50-60% fat content) effectively assess diet-induced permeability changes [28] [71]. Blood collection at baseline, 1, 2, 3, and 4 hours post-prandially permits characterization of temporal biomarker patterns, particularly for LPS, zonulin, and I-FABP [28] [71].
Corticotropin-Releasing Hormone (CRH) Administration: Exogenous CRH infusion (1 μg/kg or 100 μg fixed dose) models stress-induced permeability alterations, with biomarker assessment at 30-minute intervals for 2-3 hours post-administration [71]. This approach specifically investigates neuroendocrine pathways in barrier regulation.
Diagram 1: Zonulin Signaling Pathway. This diagram illustrates the established mechanisms of zonulin release and tight junction regulation triggered by bacterial exposure and gliadin.
Research Reagent Solutions
Table 3: Essential Research Reagents for Barrier Integrity Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Zonulin ELISA Kits | Commercial human zonulin ELISA | Quantification of serum/plasma zonulin | Multiple vendors available; cross-comparison recommended |
| I-FABP Detection Assays | Human I-FABP/FABP2 ELISA | Measurement of enterocyte damage | Multiple validated platforms available |
| Endotoxin Detection | LAL assay, LPS ELISA | Direct LPS quantification | Functional vs. immunometric approaches available |
| LBP/sCD14 Kits | Commercial ELISAs | Assessment of immune activation to LPS | Standardized kits widely available |
| Permeability Probes | Lactulose, Mannitol, Sucralose | Functional in vivo permeability testing | HPLC or MS detection required |
| Cell Culture Models | Caco-2 cells, T84 cells | In vitro barrier function assessment | TEER measurements essential |
| Stimulation Reagents | Gliadin peptides, CRH, LPS | Controlled induction of permeability | Dose-response characterization needed |
Methodological Workflow Integration
Diagram 2: Experimental Workflow for Barrier Assessment. This diagram outlines a comprehensive approach integrating circulating biomarkers with functional permeability measures.
Circulating biomarkers of barrier integrity, particularly zonulin and I-FABP, provide valuable tools for investigating tissue permeability in research contexts. Their distinct biological roles—zonulin as a physiological regulator of paracellular permeability and I-FABP as an indicator of structural epithelial damage—offer complementary insights into barrier function. Standardized methodological approaches, including controlled stimulation protocols and multimodal assessment strategies, enhance the reliability and interpretability of research findings. As investigation into tissue permeability advances, these biomarkers present promising avenues for understanding disease mechanisms, stratifying patient populations, and evaluating therapeutic interventions targeting barrier function.
Integrating Permeability Assessment into Preclinical Drug Development Pipelines
Permeability assessment stands as a critical determinant of success in preclinical drug development, directly influencing a compound's absorption, distribution, and eventual efficacy. The high attrition rates in drug development, with over 90% of candidates failing at the preclinical stage, underscore the necessity for accurate, predictive permeability models early in the development pipeline [72]. The recent regulatory reforms, including the FDA Modernization Acts of 2022 and 2024, have accelerated the adoption of advanced human-relevant models by relaxing mandatory animal testing requirements, creating an urgent need for robust, standardized permeability assessment methodologies [72]. This paradigm shift recognizes the fundamental limitations of traditional animal models, which often misrepresent human physiology and safety, leading to both false negatives and positives in drug screening.
The integration of reliable permeability assessment enables pharmaceutical scientists to forecast a drug's behavior in humans, optimizing candidate selection and reducing late-stage failures. Permeability influences bioavailability for nearly all administration routes—oral, transdermal, pulmonary, and buccal—making its accurate quantification essential for rational drug design [73] [17] [74]. This technical guide provides a comprehensive framework for implementing modern permeability assessment strategies within preclinical development pipelines, focusing on technologically advanced models, standardized protocols, and emerging microphysiological systems that collectively enhance the predictive power of early-stage drug screening.
Foundational Principles of Drug Permeability
Key Parameters and Mathematical Definitions
Drug permeability is quantified through several key parameters that describe the rate and extent of compound transfer across biological barriers. The apparent permeability coefficient (Papp) serves as the primary metric for in vitro systems, calculated from the rate of solute appearance in the receiver compartment [73] [17]. The permeability coefficient (Kp) specifically applies to transdermal and mucosal routes, representing steady-state permeation under standardized conditions [75]. For fluid and solute dynamics, the hydraulic conductivity (Lp) and solute permeability coefficient (Ps) provide specialized measurements of convective and diffusive transport, respectively [76].
The fundamental relationship between permeability and extent of absorption enables these in vitro measurements to predict in vivo performance. For oral drugs, this relationship is formalized in the Biopharmaceutics Classification System (BCS), which categorizes compounds based on permeability and solubility [73]. Similarly, an inhaled Biopharmaceutics Classification System (iBCS) has been proposed for pulmonary drugs, demonstrating the universal importance of permeability assessment across administration routes [17].
Method Suitability and Standardization
The concept of method suitability provides a generalized framework for standardizing and validating permeability models within individual laboratories [73]. This approach encompasses three critical stages: method development (optimizing and standardizing assay parameters), demonstrating assay suitability (establishing rank-order relationship between experimental permeability values and human intestinal absorption), and permeability classification of new drugs [73]. Implementation of method suitability requires setting strict acceptance criteria, using standard compounds for quality control, and selecting appropriate high-permeability internal standards (HP-IS) with permeability values near the high/low class boundary to facilitate consistent classification decisions [73].
Table 1: Standard Compounds for Permeability Model Validation
| Compound | Permeability Class | Primary Transport Mechanism | Application in Quality Control |
|---|---|---|---|
| Propranolol | High | Transcellular | Barrier functionality verification |
| Lucifer Yellow | Low | Paracellular | Tight junction integrity assessment |
| Metoprolol | High | Passive transcellular | High permeability benchmark |
| Atenolol | Low | Paracellular | Low permeability benchmark |
| Ketoprofen | High | Passive transcellular | Performance standardization |
Advanced Models for Permeability Assessment
Microphysiological Systems (Organs-on-Chips)
Microphysiological systems (MPS) represent a transformative advancement in permeability assessment, recapitulating functional features of human tissues through three-dimensional architecture, dynamic fluid flow, and relevant human cells [17]. These systems improve upon conventional in vitro models by incorporating physiological cues such as shear stress, mechanical stretching, and air-liquid interfaces that significantly influence barrier function and drug transport [17].
A notable advancement includes a single-compartment skin-on-chip (SoC) model featuring 3D co-culture of human dermal fibroblasts and keratinocytes under dynamic perfusion for 11 days [72]. This system demonstrated robust barrier formation with transepithelial electrical resistance (TEER) values comparable to native skin, consistent drug permeability patterns for compounds of varying lipophilicities (caffeine, hydrocortisone, salicylic acid, clotrimazole), and mechanical properties resembling human tissue [72]. Similarly, a small airway MPS recapitulating the pulmonary air-liquid interface with primary epithelial and vascular endothelial cell layers has shown promise for predicting inhaled drug permeability, successfully categorizing albuterol sulfate and formoterol fumarate as highly permeable and olodaterol HCl as low permeability [17].
Figure 1: MPS Permeability Assessment Workflow. This standardized protocol ensures reliable permeability classification through systematic barrier validation and quantitative analysis.
Traditional and Specialized Permeability Models
Despite the emergence of sophisticated MPS, traditional permeability models remain relevant when properly validated. These include in situ intestinal perfusions, ex vivo tissue diffusion systems (everted intestinal sacs, diffusion chambers), and in vitro cell monolayers (Caco-2, MDCK) [73] [5]. Each model offers distinct advantages and limitations regarding physiological relevance, throughput, and mechanistic insight.
For specialized administration routes, optimized models have been developed. Oral cavity permeability assessment utilizes human-derived sublingual (HO-1-u-1) and buccal (EpiOral) tissue models, which have demonstrated significant variations in permeability for drugs like asenapine (Papp = 2.72 ± 0.06 × 10â»âµ cm/s) and naloxone (Papp = 6.21 ± 2.60 × 10â»âµ cm/s) in sublingual tissue, while buccal tissue showed greater discrimination with values ranging from 3.31 ± 0.83 × 10â»â· cm/s for acyclovir to 2.56 ± 0.68 × 10â»âµ cm/s for sufentanil [74]. These route-specific models account for unique anatomical features such as keratinization status, mucus presence, and region-specific transporter expression.
Table 2: Comparison of Permeability Assessment Platforms
| Model Type | Throughput | Physiological Relevance | Key Applications | Limitations |
|---|---|---|---|---|
| Artificial Membranes | High | Low | Early screening of passive diffusion | Lacks biological transport mechanisms |
| Cell Monolayers (Caco-2) | Medium | Medium | Mechanistic studies, transporter evaluation | Inter-laboratory variability, limited expression of some transporters |
| Ex Vivo Tissues | Low | High | Regional differences, human or animal tissue | Limited tissue viability, suboptimal stirring conditions |
| Microphysiological Systems | Medium-High | High | Human-relevant prediction, disease modeling, personalized medicine | Technical complexity, higher cost, standardization ongoing |
| In Situ Perfusion | Low | High | Intact anatomy with blood flow and innervation | Animal usage, not suitable for screening |
Experimental Protocols and Methodological Standards
Skin-on-Chip Permeability Assessment Protocol
The development of a robust skin-on-chip model involves precise fabrication and validation steps. The microfluidic chip is designed using Autodesk Fusion 360 and fabricated via soft lithography with PDMS, supporting dynamic perfusion co-culture of human dermal fibroblasts and epidermal keratinocytes within Matrigel for extracellular matrix remodeling [72]. The protocol proceeds as follows:
- Device Preparation: Fabricate PDMS chips via soft lithography, sterilize, and coat with extracellular matrix proteins.
- Cell Seeding: Seed primary human dermal fibroblasts into the matrix and allow attachment, followed by seeding of epidermal keratinocytes.
- Perfusion Culture: Maintain dynamic perfusion for 11 days with specialized media to promote stratified epidermal differentiation.
- Barrier Validation: Measure TEER values and assess 4 kDa FITC-dextran permeability to confirm barrier integrity.
- Morphological Characterization: Perform high-resolution imaging (confocal and scanning microscopy) of thick (>500 µm) tissue constructs to verify native-like architecture.
- Drug Permeation Studies: Apply model drugs with varying polarities (caffeine, hydrocortisone, salicylic acid, clotrimazole) to the apical surface and quantify permeation using HPLC.
- Biomechanical Analysis: Conduct rheological amplitude and frequency sweep tests to quantify viscoelastic properties [72].
This comprehensive approach combines high-content imaging, biomechanical analysis, barrier validation, and sensitive drug quantification to establish a predictive model benchmarked against international guidelines like OECD 428 [72].
Method Suitability Implementation for Regulatory Compliance
Implementing method suitability ensures permeability data meets regulatory standards for decision-making. The process involves:
- Assay Optimization: Define and control critical parameters including pH, temperature, stirring, dosing concentration, and sample analysis method.
- Acceptance Criteria Establishment: Set specifications for barrier integrity markers (TEER, LY flux), standard compound permeability ranges, and intra-assay variability.
- Rank-Order Relationship Demonstration: Establish correlation between experimental permeability values and human extent of absorption using model drugs representing absorption ranges of <50%, 50-89%, and ≥90%.
- Classification Boundary Determination: Select a high-permeability internal standard (HP-IS) with permeability near the high/low boundary based on reference data.
- Ongoing Quality Control: Regularly test reference standards to monitor assay performance and ensure classification accuracy over time [73].
This systematic validation approach accounts for inter-laboratory variability, allows technology improvements, and applies across various tissue types, cell lines, and membrane systems [73].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Permeability Assessment
| Reagent/Material | Function | Application Examples | Technical Considerations |
|---|---|---|---|
| Polydimethylsiloxane (PDMS) | Microfluidic device fabrication | Skin-on-chip, airway MPS | Prone to drug binding; surface treatment may be required |
| Matrigel | Extracellular matrix simulation | 3D cell culture in MPS | Lot-to-lot variability; contains growth factors |
| Primary Human Cells | Physiological relevance | Epithelial/endothelial co-culture | Donor variability; limited lifespan |
| Transwell Inserts | Barrier function assessment | Caco-2, buccal/sublingual models | Standardized surface area; various pore sizes |
| Lucifer Yellow | Paracellular integrity marker | Tight junction assessment | Low permeability; minimal cellular uptake |
| Propranolol | Transcellular permeability marker | Barrier functionality verification | High permeability; passive diffusion |
| HPLC Systems | Drug quantification | Permeation kinetics | Sensitivity to low concentrations; method validation required |
| TEER Electrodes | Barrier integrity monitoring | Real-time epithelial quality | Temperature and calibration sensitivity |
| Agathadiol diacetate | Agathadiol diacetate, MF:C24H38O4, MW:390.6 g/mol | Chemical Reagent | Bench Chemicals |
| Chamaejasmenin B | Chamaejasmenin B | Chamaejasmenin B is a biflavonoid for cancer research, shown to inhibit tumor metastasis and cell invasion. This product is for Research Use Only (RUO). Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
Computational and Predictive Approaches
Quantitative Structure-Permeability Relationships
Computational prediction of permeability continues to evolve as a complementary approach to experimental assessment. The HuskinDB database, containing human skin permeation values for 253 compounds, has enabled development of predictive models based on physicochemical properties [75]. Successful quantitative structure-permeability relationships (QSPRs) typically incorporate key molecular descriptors including lipophilicity (logP), molecular weight, hydrogen bonding capacity, polar surface area, and solubility parameters.
For skin permeability, the Potts and Guy equation represents a foundational QSPR: logKp = 0.71·logP - 0.0061·MW - 6.3, though more sophisticated models have demonstrated improved accuracy by incorporating additional descriptors and training on larger datasets [75]. Recent analysis of HuskinDB data has yielded scenario-specific models with varying predictive power (R² values from 0.16 to 0.99), highlighting the significant influence of experimental conditions like skin source, temperature, and donor concentration on permeability outcomes [75].
Statistical Learning and Microstructural Analysis
For porous materials and tissue constructs, statistical learning approaches applied to microstructural information have shown remarkable success in predicting permeability. Traditional Kozeny-Carman equations relating permeability to porosity and specific surface area (k = φ³/cs²) suffer from limitations as the constant c varies across different systems and depends on porosity itself [77].
Advanced approaches incorporate higher-order microstructural descriptors including two-point surface-surface, surface-void, and void-void correlation functions, along with geodesic tortuosity [77]. Studies comparing prediction methods have found that artificial neural networks outperform conventional regression techniques, particularly when combining all three two-point correlation functions with tortuosity, with the void-void correlation function emerging as the most informative individual descriptor [77]. These data-driven methodologies benefit from large virtual microstructure datasets (30,000+ samples) spanning diverse structural types including granular and continuous solid phases [77].
Figure 2: Computational Permeability Prediction Framework. This integrated approach combines structural descriptors with experimental parameters to generate predictive models validated against experimental data.
Regulatory Considerations and Future Perspectives
The regulatory landscape for permeability assessment is evolving toward greater acceptance of human-relevant models. The FDA Modernization Act 2.0 has rendered animal testing optional, accelerating the validation and adoption of advanced models like organ-on-chip systems [72]. This shift necessitates robust validation frameworks demonstrating functional equivalence between new methodologies and traditional references.
For regulatory applications, permeability models must satisfy key criteria including reproducibility, predictive capacity, and relevance to human physiology. The alignment with international guidelines such as OECD TG 428 for skin permeability provides important validation benchmarks [72]. Additionally, quality control attributes including cellular composition verification, barrier integrity monitoring, and assessment of non-specific binding to materials (particularly relevant for PDMS chips) establish model credibility [17].
Future advancements will focus on enhancing model complexity through multi-organ systems, integrating patient-specific cells for personalized medicine applications, and establishing stronger in vitro-in vivo correlations through mechanistic modeling. The combination of advanced MPS with sophisticated computational approaches represents the most promising path toward predictive, human-relevant permeability assessment that accelerates drug development while reducing reliance on animal models.
Challenges and Strategies for Modulating Tissue Permeability in Therapeutic Contexts
The integrity of biological barriers, particularly the intestinal epithelium, is paramount for maintaining systemic homeostasis. This whitepaper examines three primary factors compromising barrier function: psychological stress, inflammatory signaling pathways, and dietary components. Evidence from translational studies demonstrates that psychosocial stress activates the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous system, leading to mast cell-dependent barrier disruption [78] [79]. Concurrently, inflammatory mediators including TNF-α, IL-1β, and IL-6 activate transcriptional programs through NF-κB, MAPK, and JAK-STAT pathways that reorganize tight junction complexes [80]. Furthermore, specific dietary components directly modulate barrier integrity, with fructose increasing permeability while prebiotics and probiotics demonstrate protective effects [81] [82]. Understanding these interconnected mechanisms provides critical insights for developing therapeutic strategies targeting tissue permeability in pathological conditions.
The Intestinal Barrier: Structure and Function
The intestinal barrier constitutes a complex, multi-layered system comprising both physical and functional components [78].
Physical Barrier Components
- Cellular Structure: A single layer of intestinal epithelial cells joined by intercellular junctions including tight junctions, adherens junctions, and desmosomes
- Mucus Layer: A gel-forming mucin secretion creating a physical separation between luminal contents and epithelial surface
- Stromal Elements: Underlying connective tissue supporting epithelial structure and function
Functional Barrier Components
- Digestive Secretions: Gastric acid, bile, enzymes, and antimicrobial peptides
- Immunological Factors: Secreted immunoglobulins (sIgA), cytokines, and chemokines
- Neural and Endocrine Elements: Enteric nervous system signaling and gut hormone release
Barrier function is quantitatively assessed through intestinal permeability, which reflects the measurable passage of defined molecules across the intestinal wall [78]. This permeability occurs via two primary routes:
- Paracellular Pathway: Transport between cells regulated by tight junction complexes
- Transcellular Pathway: Transport through cells via active transport, passive diffusion, or endocytosis
Stress-Induced Barrier Dysfunction
Neuroendocrine Mechanisms
Psychosocial stress activates two core endocrine systems: the HPA axis and sympathetic-adrenal-medullary (SAM) system [78] [79]. Prolonged activation of these systems exerts deleterious effects on gastrointestinal barrier function through several mechanisms:
- Corticotropin-Releasing Hormone (CRH): Directly increases intestinal permeability via mast cell activation [78]
- Cortisol: Sustained elevation disrupts tight junction protein expression
- Catecholamines: Norepinephrine and epinephrine alter mucosal blood flow and epithelial cell function
Preclinical models demonstrate that stress hormones including norepinephrine can stimulate the growth of pathogenic bacteria (e.g., Escherichia coli) while reducing beneficial microbes (e.g., Lactobacillus), creating a dysbiotic environment that further compromises barrier integrity [79].
Mast Cell Activation
Stress induces mast cell degranulation via CRH-dependent mechanisms, releasing:
- Proteases that directly cleave tight junction proteins
- Histamine and serotonin altering epithelial fluid secretion
- Cytokines (TNF-α, IL-6) promoting inflammatory cascades
These mediators increase paracellular permeability primarily through the "leak pathway" mediated by myosin light chain kinase (MLCK) phosphorylation and subsequent cytoskeletal contraction [78].
Clinical Evidence
Human studies present conflicting evidence regarding stress-induced permeability changes, with methodological challenges complicating translation from animal models [78]. However, clinical observations confirm that stress triggers flare-ups in inflammatory bowel disease (IBD) patients, with prospective evidence showing perceived stress, negative affect, and major life events predict disease exacerbation [79].
Inflammatory Pathways in Barrier Disruption
Key Signaling Pathways
Inflammation disrupts barrier function through activation of specific intracellular signaling cascades that reorganize tight junction complexes and induce apoptotic pathways in epithelial cells [80].
NF-κB Pathway
- Activation: Triggered by pro-inflammatory cytokines (TNF-α, IL-1β), pathogen-associated molecular patterns (PAMPs), and damage-associated molecular patterns (DAMPs) through pattern recognition receptors (PRRs) including Toll-like receptors (TLRs)
- Mechanism: IκB kinase (IKK) activation leads to IκB phosphorylation and degradation, releasing NF-κB for nuclear translocation
- Outcome: Transcriptional upregulation of additional pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) creating an amplification loop
MAPK Pathway
- Activation: Inflammatory cytokines and cellular stressors activate MAPK kinases (MKKs)
- Branches: ERK1/2 (mitogens/differentiation), JNK and p38 (stress/inflammation)
- Outcome: Phosphorylation of transcription factors (AP-1, ATF-2) regulating inflammatory gene expression
JAK-STAT Pathway
- Activation: Cytokine binding (e.g., IL-6 family) to cell surface receptors activates receptor-associated Janus kinases (JAKs)
- Mechanism: JAKs phosphorylate STAT transcription factors, promoting dimerization and nuclear translocation
- Outcome: Direct transcriptional regulation of inflammatory response genes
Cytokine-Mediated Barrier Disruption
Pro-inflammatory cytokines directly compromise barrier function through multiple mechanisms:
- TNF-α: Upregulates myosin light chain kinase (MLCK) expression, inducing tight junction strand disruption and increasing claudin-2 expression that enhances the pore pathway [78]
- IL-1β and IL-6: Synergize with TNF-α to amplify inflammatory signaling and promote immune cell recruitment
- IFN-γ: Reduces barrier function by downregulating occludin and ZO-1 expression while enhancing endosomal recycling of junctional proteins
Table 1: Inflammatory Mediators in Barrier Dysfunction
| Mediator | Primary Sources | Mechanism of Barrier Disruption | Downstream Effects |
|---|---|---|---|
| TNF-α | Macrophages, monocytes, T cells | Upregulates MLCK expression; Alters claudin-2 | Increased paracellular permeability; Apoptosis |
| IL-1β | Macrophages, monocytes | Activates NF-κB pathway | Amplification of inflammation; Neutrophil recruitment |
| IL-6 | Macrophages, T cells, adipocytes | JAK-STAT signaling; B cell differentiation | Acute phase protein production; Adaptive immunity activation |
| IFN-γ | T cells, NK cells | Downregulates occludin & ZO-1; Junctional protein internalization | MHC class II upregulation; Macrophage activation |
Dietary Modulation of Barrier Function
Dietary Components That Compromise Barrier Integrity
Specific dietary factors have been demonstrated to increase intestinal permeability:
- Fructose: Consumption significantly increases intestinal permeability in adults, with a very low GRADE level of evidence [81]
- Western Diet Pattern: Characterized by high saturated fat, refined carbohydrates, and food additives promotes pro-inflammatory microbiota shifts and barrier dysfunction
- Alcohol: Directly damages epithelial cells and increases paracellular permeability
Protective Dietary Components
Certain dietary interventions demonstrate protective effects on barrier function:
- Chicory Inulin: A prebiotic fiber that reduces intestinal permeability in healthy adults (moderate GRADE evidence) [81]
- Probiotics: Specific strains (e.g., Lactobacillus, Bifidobacterium) reinforce barrier function through competitive exclusion, antimicrobial production, and enhanced junctional protein expression [81]
- Mediterranean Diet: Rich in polyphenols, omega-3 fatty acids, and fermentable fibers demonstrates anti-inflammatory effects and promotes barrier integrity [83]
- Fermented Foods: Support microbial diversity and enhance barrier function through bioactive metabolites [83]
Table 2: Efficacy of Dietary Interventions on Barrier Function and Inflammation
| Dietary Intervention | Effect on CRP | Effect on Albumin | Effect on Intestinal Permeability | Clinical Evidence |
|---|---|---|---|---|
| Low FODMAP Diet + Enteral Nutrition (LFD + EN) | MD = -5.21 mg/L vs. LRD [84] | MD = 3.64 g/L vs. EN [84] | Not specifically measured | Highest ranking for reducing systemic inflammation [84] |
| Chicory Inulin | Not reported | Not reported | Reduced permeability [81] | Moderate GRADE evidence [81] |
| Probiotics | Not reported | Not reported | Reduced permeability [81] | Moderate GRADE evidence [81] |
| Fructose | Not reported | Not reported | Increased permeability [81] | Very low GRADE evidence [81] |
| Mediterranean Diet + Fermented Foods | Secondary outcome in ongoing trial [83] | Secondary outcome in ongoing trial [83] | Change in lactulose/mannitol ratio (secondary outcome) [83] | Ongoing TASTY trial (NCT06758817) [83] |
Experimental Models and Assessment Methodologies
Intestinal Permeability Measurement Techniques
Accurate assessment of barrier function employs multiple complementary approaches:
In Vivo Permeability Tests
- Sugar Absorption Tests: Orally administered probe combinations (lactulose/mannitol, sucralose) with urinary recovery measurement
- Lactulose/Mannitol Ratio: Assesses small intestinal permeability (lactulose: leak pathway; mannitol: pore pathway)
- Sucralose: Resistant to bacterial degradation, assesses whole gut permeability
- Chromium-51 EDTA: Radioactive tracer measuring paracellular permeability
Serum Biomarkers
- Lipopolysaccharide-Binding Protein (LBP): Marker of bacterial translocation and intestinal permeability [85]
- Zonulin: Regulator of tight junctions; elevated levels associate with increased permeability [85]
- Intestinal Fatty-Acid Binding Protein (I-FABP): Marker of enterocyte damage
- Soluble CD14 (sCD14): Marker of monocyte activation in response to bacterial translocation
Limitations of Current Assessment Methods
Important methodological considerations complicate barrier function assessment:
- Regional Specificity: Different intestinal segments demonstrate varying permeability characteristics
- Probe Metabolism: Bacterial degradation of certain probes (e.g., lactulose, mannitol) in the colon limits regional assessment [78]
- Confounding Factors: Intestinal motility, renal function, and systemic inflammation influence probe excretion and biomarker levels [78]
- Technical Challenges: LPS detection in peripheral blood presents analytical difficulties [78]
Table 3: Research Reagent Solutions for Barrier Function Assessment
| Research Tool | Application | Mechanism/Function | Considerations |
|---|---|---|---|
| Lactulose/Mannitol Test | Small intestinal permeability assessment | Differential urinary recovery: Mannitol (pore pathway), Lactulose (leak pathway) | Degraded by colonic bacteria; requires controlled renal function [78] |
| Sucralose | Whole gut/colonic permeability | Sugar probe resistant to bacterial degradation | Reflects combined small and large intestinal permeability [78] |
| 51Cr-EDTA | Paracellular permeability assessment | Radioactive tracer measuring paracellular flux | Radiation exposure limits repeated use; no regional differentiation [78] |
| Lipopolysaccharide-Binding Protein (LBP) | Serum biomarker of bacterial translocation | Binds LPS and enhances immune response to endotoxins | Acute phase reactant; not specific to intestinal permeability [85] |
| Zonulin | Serum biomarker of tight junction regulation | Modulator of intercellular tight junctions | Limited validation in non-GI disorders [85] |
| USsing Chamber | Ex vivo permeability measurement | Electrophysiological assessment of tissue permeability | Requires fresh tissue; measures combined para/transcellular flux [78] |
Integrated Pathophysiological Model
Barrier dysfunction emerges from the interplay between psychological stress, inflammatory activation, and dietary factors through a feed-forward cycle:
- Initial Insult: Psychological stress or dietary triggers activate neuroendocrine and inflammatory pathways
- Epithelial Signaling: CRH and inflammatory cytokines (TNF-α, IL-1β, IL-6) directly compromise tight junction integrity
- Microbial Translocation: Increased permeability permits bacterial product translocation (LPS, peptidoglycan) into circulation
- Systemic Immune Activation: Pattern recognition receptors (TLR4, TLR2) detect bacterial products, amplifying inflammatory cascades
- Sustained Barrier Dysfunction: Chronic inflammation and continued stress maintain barrier defects, creating a self-perpetuating cycle
This model is supported by clinical evidence demonstrating increased serum LBP in Graves' orbitopathy patients, correlating with aggravated orbital inflammation and myofibroblast accumulation [85]. Similarly, rheumatoid arthritis patients exhibit gut dysbiosis and increased intestinal permeability that may contribute to joint inflammation [83].
Therapeutic Implications and Future Directions
Understanding these mechanisms reveals multiple therapeutic targets for restoring barrier function:
- Stress Reduction Interventions: Mindfulness-based stress reduction, cognitive behavioral therapy
- Anti-inflammatory Approaches: TNF-α antagonists, JAK inhibitors, MAPK pathway modulators
- Dietary Interventions: Personalized nutrition with prebiotics, probiotics, and anti-inflammatory dietary patterns
- Microbiome-Targeted Therapies: Fecal microbiota transplantation, precision probiotics
Ongoing clinical trials like the TASTY trial (NCT06758817) are investigating whether a Mediterranean Diet enriched with fermented foods can modulate gut microbiota, intestinal permeability, and disease activity in rheumatoid arthritis [83]. Similar approaches show promise for other permeability-associated conditions.
Future research should prioritize:
- Development of more specific and region-targeted permeability assessments
- Elucidation of genetic susceptibility factors for barrier dysfunction
- Randomized controlled trials examining combined interventions targeting multiple barrier-compromising factors simultaneously
- Advanced organoid and microphysiological systems for modeling human-specific barrier function
The intestinal barrier represents a critical interface whose dysfunction has far-reaching consequences for systemic health and disease. Psychological stress, inflammation, and dietary factors interact through complex, overlapping pathways to compromise barrier integrity. A comprehensive understanding of these mechanisms provides the foundation for developing targeted interventions to restore barrier function across multiple disease contexts. As research methodologies advance, particularly in the realm of personalized nutrition and microbiome modulation, novel approaches to maintaining barrier integrity promise to impact numerous inflammatory and autoimmune conditions where tissue permeability plays a fundamental pathogenic role.
Population Bottlenecks and Genetic Diversity in Pathogen-Host Interactions
Population bottlenecks represent critical constraints that sharply reduce pathogen population size during host invasion, fundamentally shaping the genetic diversity and evolutionary trajectory of infectious agents [86]. In the context of host-pathogen interactions, these bottlenecks occur when physical and immune barriers restrict the number of successful invaders that found the subsequent infection population. The permeability of host tissues at the initial infection site serves as a primary determinant of bottleneck stringency, directly influencing whether selective forces or stochastic processes dominate pathogen population assembly [87] [88]. Understanding these dynamics is crucial for predicting pathogen evolution, designing effective interventions, and developing novel therapeutic strategies that account for the complex interplay between host barriers and pathogen population genetics.
Quantitative Impact of Tissue Permeability on Pathogen Populations
Bottleneck Size Across Infection Routes
Recent research utilizing barcoded pathogen populations has quantified how tissue permeability governs bottleneck size during infection. The following table summarizes experimental findings from studies using 90 isogenic barcoded Ralstonia solanacearum strains inoculated through routes of varying permeability in tomato plants [87].
Table 1: Population Bottleneck Sizes Under Different Infection Routes
| Infection Route | Bottleneck Size (Nâ‚‘) - Resistant Cultivar | Bottleneck Size (Nâ‚‘) - Susceptible Cultivar | Fold Change vs. Intact Roots |
|---|---|---|---|
| Intact Roots (Least Permeable) | 4.96 | 1.60 | 1x (Reference) |
| Wounded Roots | 51.15 | 194.80 | 10.31x (R), 121.75x (S) |
| Direct Xylem Inoculation (Most Permeable) | 141.69 | 205.84 | 28.57x (R), 128.65x (S) |
Genetic Diversity Metrics Across Infection Routes
The permeability of host tissues directly correlates with maintained pathogen genetic diversity, as measured by standard population genetics metrics [87].
Table 2: Genetic Diversity Metrics in Establishing Pathogen Populations
| Diversity Metric | Intact Roots | Wounded Roots | Direct Xylem Inoculation |
|---|---|---|---|
| Shannon Diversity Index | 0.15 ± 0.08 | 0.89 ± 0.11 | 0.94 ± 0.05 |
| Simpson Dominance Index | 0.91 ± 0.05 | 0.24 ± 0.07 | 0.12 ± 0.03 |
| Lineage Composition | 1-2 dominant lineages (>75% abundance) | No single lineage >25% abundance | All lineages at relatively equal proportions |
Experimental Models and Methodologies
Barcoded Pathogen Model System
The application of barcoded pathogen populations represents a cutting-edge methodology for quantifying bottleneck dynamics in host-pathogen interactions [87] [86].
Experimental Workflow for Barcoded Pathogen Studies
Protocol: Generating and Validating Barcoded Pathogen Libraries
Barcode Design and Insertion:
- Design 8-12bp unique random DNA sequences as barcodes
- Insert barcodes into neutral chromosomal loci via homologous recombination
- Verify single insertion events and absence of fitness effects through growth curve analyses (measuring maximum growth rates, biomass, lag phase, and area under the curve) [87]
Library Validation:
- Culture individual barcoded strains separately, then combine in equal proportions
- Sequence barcode representation to confirm even distribution in initial inoculum
- Verify virulence equivalence to wild-type through parallel infection assays
- Confirm no significant differences in expression of key pathogenicity factors (e.g., cell wall-degrading enzymes, type 3 effectors) [87]
Inoculation and Sampling:
- Prepare inoculum with pre-defined barcode diversity (e.g., 90 strains)
- Apply through routes of varying permeability (intact roots, wounded roots, direct xylem injection)
- Sample establishing pathogen populations at defined time points post-infection
- Extract genomic DNA and amplify barcode regions for sequencing [87]
Bottleneck Size Calculation Methods
Multiple analytical approaches enable quantification of bottleneck sizes from barcode frequency data:
Probabilistic Methods: Analyze stochastic loss of tagged strains based on presence/absence data [86]
Population Genetic Approaches: Compare allele frequency changes before and after bottlenecks using formulas such as:
- F-statistics: Measuring reduction in heterozygosity
- Variance-based estimators: Using changes in barcode frequency variances [86]
Mathematical Modeling: Incorporate pathogen migration patterns and replication dynamics within host compartments to estimate population sizes [86]
Mechanisms and Consequences of Population Bottlenecks
Host Barriers as Bottleneck Determinants
Host organisms deploy multiple barrier types that restrict pathogen population sizes during infection:
Host Barriers Determining Population Bottlenecks
Evolutionary Consequences of Bottlenecks
The stringency of population bottlenecks profoundly influences pathogen evolutionary dynamics:
Genetic Drift vs. Selection:
- Stringent bottlenecks (intact roots): Increase effects of genetic drift, where random lineage loss dominates population assembly
- Permeable barriers (direct xylem inoculation): Enable selective processes to dominate, maintaining adaptive lineages [87]
Virulence Evolution:
Founder Effects:
- The limited number of surviving organisms determines genetic composition of subsequent generations
- Founder effects can drive specialized adaptation to local host environments [86]
Research Toolkit: Essential Reagents and Methodologies
Table 3: Key Research Reagents for Bottleneck Studies
| Reagent/Method | Function | Application Example |
|---|---|---|
| Isogenic Barcoded Strains | Neutral genetic tags for lineage tracking | 90 uniquely barcoded Ralstonia solanacearum strains [87] |
| High-Throughput Sequencing | Quantification of barcode frequencies | Amplicon sequencing of barcode regions from infected tissues [87] |
| Controlled Inoculation Methods | Varying tissue permeability | Intact roots vs. wounded roots vs. direct xylem inoculation [87] |
| Host Genotype Panels | Testing host genetic diversity effects | Arabidopsis thaliana ecotypes with differential susceptibility [89] |
| Population Genetics Algorithms | Bottleneck size calculation | F-statistics, variance-based estimators from barcode frequency changes [86] |
| GO-203 TFA | GO-203 TFA, CAS:1222186-26-6, MF:C89H171F3N52O21S2, MW:2426.8 g/mol | Chemical Reagent |
| Alstonic acid B | Alstonic acid B, MF:C30H46O3, MW:454.7 g/mol | Chemical Reagent |
Implications for Therapeutic Development
Understanding population bottlenecks in pathogen-host interactions provides crucial insights for therapeutic strategies:
Antimicrobial Dosing:
Vaccine Design:
- Accounting for transmission bottlenecks may improve vaccine efficacy by targeting conserved epitopes maintained through bottleneck events
- Understanding antigenic variation mechanisms helps counter pathogen immune evasion [91]
Resistance Management:
- Bottlenecks increase fixation rates of resistance mutations, necessitating combination therapies
- Host heterogeneity can be leveraged to slow resistance evolution [89]
Population bottlenecks imposed by host tissue permeability serve as critical determinants of pathogen genetic diversity and evolutionary trajectory during infection. The integration of barcoded pathogen libraries with high-throughput sequencing and computational modeling has enabled precise quantification of these fundamental processes, revealing how physical and immune barriers shape the balance between selective and stochastic forces in pathogen population assembly. This understanding provides a foundation for developing novel intervention strategies that specifically target bottleneck points in disease establishment and progression, potentially leading to more effective approaches for managing infectious diseases in both agricultural and medical contexts.
The intestinal barrier serves as a critical defense system, and its dysfunction, often characterized by increased permeability or "leaky gut," is a significant upstream event in the pathogenesis of diverse inflammatory, autoimmune, and metabolic diseases [92] [20] [93]. This whitepaper examines pharmacological strategies designed to restore and protect intestinal barrier integrity, with a specific focus on zonulin antagonists and a range of barrier-enhancing agents. Within the context of the WISH research framework on tissue permeability, understanding these interventions is paramount for developing novel therapeutics for conditions driven by barrier dysfunction. We provide a detailed analysis of molecular mechanisms, summarize key experimental data, and offer standardized protocols for evaluating barrier function in research settings, presenting this complex information through structured tables and pathway diagrams to aid the drug development community.
The Intestinal Barrier System and the Role of Zonulin
The intestinal mucosal barrier is a complex, multi-layered system essential for maintaining physiological homeostasis. Its functions extend beyond simple absorption to include sophisticated immune surveillance and the maintenance of a critical boundary with the external environment [20].
Components of the Intestinal Barrier
The barrier consists of several coordinated layers:
- Physical Barrier: This is primarily formed by a single layer of intestinal epithelial cells interconnected by tight junctions (TJs) and adherens junctions (AJs). TJs, comprising proteins such as claudins, occludin, and Zonula Occludens-1 (ZO-1), are the apical-most complexes that seal the paracellular space and regulate selective permeability [20] [93]. The epithelium is further protected by a mucus layer secreted by goblet cells.
- Chemical Barrier: This includes gastric acid, bile, digestive enzymes, and antimicrobial peptides (e.g., defensins) secreted by Paneth cells, which create a hostile environment for pathogens [20].
- Immune Barrier: The gut-associated lymphoid tissue (GALT) and secreted immunoglobulin A (sIgA) provide adaptive and innate immune responses, distinguishing between commensal bacteria and pathogenic invaders [20] [94].
- Microbial Barrier: The commensal gut microbiota competes with pathogens for nutrients and space, and produces beneficial metabolites like short-chain fatty acids (SCFAs) that are crucial for barrier integrity [20] [94].
Zonulin as a Master Regulator of Permeability
Zonulin is a physiological modulator of intercellular TJs and is the only known human protein that reversibly regulates intestinal permeability [92]. It functions as a "biological door opener" by triggering a cascade of intracellular signals that lead to the disassembly of TJs, thereby increasing paracellular permeability. This process is typically a physiological response to certain luminal stimuli, facilitating the absorption of nutrients and the movement of immune cells. However, dysregulation of the zonulin pathway—often driven by genetic predisposition and environmental triggers—can lead to a pathologically "leaky gut." This allows the translocation of non-self antigens, microorganisms, and their toxins into the systemic circulation, which can trigger inflammatory and autoimmune responses in susceptible individuals [92] [20]. The discovery of zonulin has provided a mechanistic link between intestinal barrier dysfunction and a wide array of local and systemic diseases.
Pharmacological Interventions: Mechanisms and Agents
Targeting the pathways that control barrier function offers a promising therapeutic strategy. The two primary approaches involve antagonizing the zonulin pathway and directly enhancing barrier components.
Zonulin Antagonists: Larazotide Acetate
Larazotide Acetate (LA), also known as AT1001, is a synthetic octapeptide (H-Gly-Gly-Val-Leu-Val-Gln-Pro-Gly-OH) that functions as a zonulin receptor antagonist [95]. It is the most advanced therapeutic candidate in this class, primarily developed for celiac disease but with potential applicability in other barrier dysfunction-related conditions.
The following diagram illustrates the core mechanism of action of zonulin and its antagonist, Larazotide Acetate.
Figure 1: Mechanism of Zonulin and Larazotide Acetate. Zonulin binding triggers the ROCK pathway, leading to MLC-2 phosphorylation and tight junction disassembly. Larazotide acetate antagonizes this pathway, promoting junctional stability.
Recent mechanistic studies from 2025 have elucidated novel functions of LA beyond zonulin antagonism. In cellular models of anoxia/reoxygenation (A/R) injury, LA pretreatment:
- Significantly increased transepithelial electrical resistance (TEER), a key indicator of barrier integrity [95].
- Preserved the organization of TJ proteins (ZO-1, occludin) at the cell membrane [95].
- Markedly reduced phosphorylation of myosin light chain-2 (MLC-2), a key event in actomyosin contraction and increased permeability, likely through modulation of the ROCK pathway [95].
- Enhanced cellular proliferation, potentially via the Wnt and Notch signaling pathways, as predicted by transcriptomic analysis [95].
These findings position LA as a multi-functional barrier-protective agent that stabilizes TJs, modulates cytoskeletal contraction, and promotes epithelial repair.
Barrier-Enhancing Agents
A diverse array of naturally occurring and synthetic molecules can directly enhance endothelial and epithelial barrier function. Their mechanisms are distinct from, but potentially complementary to, zonulin antagonism.
Table 1: Key Barrier-Enhancing Agents and Their Mechanisms
| Agent Class | Representative Molecules | Primary Mechanism of Action | Key Signaling Pathways | Research/Clinical Context |
|---|---|---|---|---|
| Prostanoids | PGDâ‚‚, PGEâ‚‚, PGIâ‚‚ (Iloprost, Beraprost) | Agonism of DP1/EP4/IP receptors; increases intracellular cAMP [96]. | cAMP/PKA, Tiam1/Rac1 [96]. | Explored in models of acute lung injury (ALI); promotes endothelial barrier restoration [96]. |
| Sphingolipids | Sphingosine-1-Phosphate (S1P) | Agonism of S1P receptors (S1P1–5) [96]. | Rac1, cortical actin formation [96]. | Plasma S1P decreased in sepsis; infusion offers protection in injury models [96]. |
| Growth Factors | Hepatocyte Growth Factor (HGF) | Binding to c-Met receptor [96]. | Interaction of actin-cortactin and α/β catenin-VE-cadherin [96]. | Elevated in early sepsis, suggesting a role in tissue protection and regeneration [96]. |
| Oxidized Phospholipids | POVPC, PGPC | Potential binding to LRP6 receptor [96]. | Rac1, promotion of cortical actin cytoskeleton [96]. | Generated during inflammation; demonstrated barrier-protective effects in studies [96]. |
| Nutraceuticals | Short-Chain Fatty Acids (e.g., Butyrate) | Metabolites from gut microbiota; activation of GPCRs (e.g., GPR41/43) [94]. | AMPK pathway activation [94]. | Dietary intervention; crucial for colonic epithelium energy metabolism and barrier integrity [94]. |
Quantitative Assessment of Barrier Function in Research
Robust and reproducible assessment of barrier integrity is fundamental to pharmacological development in this field. The following section outlines standard biomarkers and experimental methodologies.
Biomarkers of Intestinal Barrier Integrity
Serum biomarkers provide a non-invasive means to assess different aspects of barrier dysfunction in clinical and preclinical research.
Table 2: Serum Biomarkers for Assessing Intestinal Barrier Function
| Biomarker | Molecular Weight | Physiological Role | Significance of Elevation | Associated Clinical Findings |
|---|---|---|---|---|
| Diamine Oxidase (DAO) | ~250 kDa | Intracellular enzyme in mature enterocytes [97]. | Indicator of mucosal epithelial cell damage and shedding [97]. | Highest positivity rate post-digestive surgery; reflects mucosal injury [97]. |
| D-Lactate (D-Lac) | 90 Da | Bacterial fermentation byproduct [97]. | Direct marker of increased intestinal permeability [97]. | Positively correlated with systemic inflammation markers (CRP, PCT) [97]. |
| Lipopolysaccharide (LPS) | 10-20 kDa | Component of gram-negative bacterial membrane [97]. | Indicator of microbial translocation [97]. | Least frequently elevated; triggers systemic inflammation [97]. |
A 2025 clinical study on postoperative patients demonstrated that the severity of barrier impairment, as defined by the positivity of all three biomarkers (DAO > 10 U/L, D-lac > 15 mg/L, LPS > 20 U/L), was strongly correlated with progressively worsening nutritional status and escalating systemic inflammation [97].
Standard Experimental Models and Protocols
In Vitro Model: Anoxia/Reoxygenation (A/R) Injury
Application: This model simulates ischemia/reperfusion injury, a common pathophysiological event in gastrointestinal disorders, to study barrier dysfunction and test protective agents [95].
Detailed Protocol:
- Cell Culture: Utilize human intestinal Caco-2BBe1 or porcine IPEC-J2 cell lines. Culture on 0.4 µm pore-sized permeable supports until fully differentiated (TEER > 400 Ω·cm² for Caco-2BBe1 or > 30 Ω·cm² for IPEC-J2) [95].
- Agent Pretreatment: Apically pretreat cell monolayers with the investigational compound (e.g., 10 µM Larazotide Acetate) for a specified period prior to injury induction [95].
- Anoxia Induction: Place cells in a modular incubator chamber. Flush with 95% N₂ / 5% CO₂ for 5 minutes to displace oxygen. Seal the chamber airtight and incubate at 37°C for 2 hours [95].
- Reoxygenation: Remove cells from the chamber and return them to a normoxic incubator (21% Oâ‚‚, 5% COâ‚‚) for up to 4 hours [95].
- Endpoint Analysis:
- Transepithelial Electrical Resistance (TEER): Measure using a chopstick electrode and volt-ohm meter. Record triplicate readings per monolayer and subtract the blank insert value [95].
- Immunofluorescence: Fix cells and stain for TJ proteins (ZO-1, occludin) to assess localization and organization.
- Western Blotting: Analyze protein expression and phosphorylation status (e.g., pMLC-2, TJ proteins) in membrane and cytosolic fractions [95].
- Transcriptomics: Conduct RNA sequencing to identify differentially expressed genes and affected pathways (e.g., small GTPase signaling, proliferation) [95].
The Scientist's Toolkit: Essential Research Reagents
This section catalogs critical reagents and models used in barrier function research, providing a quick reference for experimental design.
Table 3: Research Reagent Solutions for Barrier Function Studies
| Reagent / Model | Specifications / Source | Primary Research Application |
|---|---|---|
| Larazotide Acetate (AT1001) | >99% purity by HPLC/MS; obtained as acetate salt [95]. | Zonulin antagonist; positive control for barrier protection studies. |
| Caco-2BBe1 Cell Line | Human intestinal epithelial cell line; derived from Caco-2 [95]. | Standard in vitro model for forming polarized, high-TEER monolayers. |
| Leaky IPEC-J2 Model | Porcine jejunal epithelial cell line cultured in crypt-enriched media (e.g., with Wnt-3a, R-Spondin, Noggin) for >5 passages [95]. | Model of inherently permeable epithelium for studying barrier closure. |
| Fasudil | ROCK inhibitor (e.g., from STEMCELL Technologies) [95]. | Tool to inhibit ROCK-mediated MLC-2 phosphorylation and permeability. |
| Peptide 18 | MLCK inhibitor (e.g., from Tocris Bioscience) [95]. | Tool to inhibit MLCK-mediated MLC-2 phosphorylation. |
| JY-DLT System | (Beijing Zhongsheng Jinyu Diagnostic Technology) [97]. | Automated system for quantifying serum DAO, D-lactate, and LPS. |
| Diosbulbin L | Diosbulbin L | Diosbulbin L is a high-purity natural product compound provided For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Integrated View: Signaling Pathways in Barrier Regulation
The following diagram synthesizes the key signaling pathways involved in barrier regulation, integrating the actions of zonulin, larazotide, and other barrier-enhancing agents, providing a comprehensive view for the WISH research context.
Figure 2: Integrated Signaling in Barrier Regulation. This map illustrates the balance between permeability-promoting signals (red) initiated by zonulin and barrier-enhancing, protective signals (green) activated by agents like larazotide, SCFAs, prostanoids, S1P, and HGF. Larazotide acetate acts as a key node by antagonizing the zonulin-triggered pathway while promoting stabilizing and reparative processes.
The integrity of biological barriers, particularly the intestinal barrier, is a fundamental determinant of systemic health. Compromised barrier function, often described as "leaky gut," is characterized by increased tissue permeability and allows for the translocation of microbes, their structural components, and other luminal pro-inflammatory substances into systemic circulation. This process can initiate and perpetuate local and systemic inflammatory responses, which are implicated in a wide spectrum of diseases, from gastrointestinal and metabolic disorders to neurological and autoimmune conditions [98]. This whitepaper provides an in-depth technical examination of non-pharmacological strategies, specifically probiotics, prebiotics, and targeted dietary modifications, for reinforcing intestinal barrier function and managing tissue permeability. Aimed at researchers and drug development professionals, this guide synthesizes current evidence, details mechanistic pathways, and outlines standardized experimental protocols for investigating these interventions within the context of the gut-brain axis and broader systemic health.
The intestinal barrier is a complex, multi-layered system that selectively allows the absorption of nutrients, electrolytes, and water while preventing the passage of harmful entities such as pathogens, toxins, and immunogenic molecules. Its functional state is described as intestinal permeability [99] [98]. A breach in this barrier's integrity is a recognized factor in the pathophysiology of numerous diseases.
The "leaky gut hypothesis" posits that increased intestinal permeability facilitates the translocation of gut-derived microbial products, notably lipopolysaccharide (LPS) from Gram-negative bacteria, into the portal circulation and subsequently into systemic circulation. This triggers a low-grade, chronic inflammatory state known as metabolic endotoxemia, which is believed to be a key driver in the development and progression of various local and systemic disorders [99] [98]. The table below summarizes the clinical evidence linking increased intestinal permeability to a range of conditions.
Table 1: Clinical Evidence of Increased Intestinal Permeability in Various Diseases
| Disease Category | Specific Conditions | Evidence of Increased Permeability & Inflammation |
|---|---|---|
| Gastrointestinal | Inflammatory Bowel Disease (IBD) [98], Irritable Bowel Syndrome (IBS) [98] | Increased lactulose/mannitol test results; decreased expression of ZO-1/occludin; systemic endotoxemia and elevated pro-inflammatory cytokines (TNF-α, IL-6, IL-1β). |
| Hepatic | Alcoholic Liver Disease [98], Non-Alcoholic Steatohepatitis (NASH) [98], Liver Cirrhosis [98] | Elevated circulating endotoxin; reduced expression of tight junction proteins (claudin-1, ZO-1); correlation with systemic TNF-α levels. |
| Metabolic | Type 1 & Type 2 Diabetes [98] | Documentated increase in intestinal permeability. |
| Neurological/Psychiatric | Depression [98], Alzheimer's Disease (AD) [100], Parkinson's Disease (PD) [101] | Presence of anti-lipid A antibodies (Depression); unique microbiome phenotypes and secondary bile acid profiles associated with disease (AD) [100]; systemic inflammatory components. |
| Autoimmune | Rheumatoid Arthritis, Ankylosing Spondylitis, Type 1 Diabetes, Multiple Sclerosis [102] | Clinical association with increased intestinal permeability. |
Mechanisms of Action: How Interventions Modulate Permeability
Non-pharmacological approaches target the pathways that regulate intestinal barrier integrity. Their mechanisms are multifaceted and often interdependent.
Probiotics
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. They support barrier function through several direct and indirect mechanisms:
- Reinforcement of Tight Junctions: Specific probiotic strains upregulate the expression of key tight junction proteins such as ZO-1, occludin, and claudins, thereby strengthening the paracellular seal between epithelial cells [98].
- Modulation of Microbiota Composition: Probiotics compete with pathobionts for nutrients and adhesion sites, produce antimicrobial compounds (bacteriocins), and help restore a healthy microbial balance, reducing the population of barrier-disrupting organisms [103].
- Immunomodulation: They interact with intestinal immune cells to promote anti-inflammatory responses, such as enhancing regulatory T-cell function and reducing the secretion of pro-inflammatory cytokines like TNF-α and IFN-γ, which are known to disrupt tight junctions [101].
- Production of Beneficial Metabolites: Certain probiotics are involved in the production of short-chain fatty acids (SCFAs) and other bioactive molecules that are crucial for barrier maintenance [103].
Prebiotics
Prebiotics are indigestible food ingredients (e.g., dietary fibers) that selectively stimulate the growth and/or activity of beneficial gut bacteria [103]. Their primary mechanism is indirect:
- Selective Fermentation: Prebiotics serve as substrates for beneficial commensal bacteria, such as Bifidobacterium and Lactobacillus, promoting their proliferation.
- SCFA Production: The fermentation of prebiotics by gut microbiota yields SCFAs, most notably butyrate, acetate, and propionate. Butyrate is a primary energy source for colonocytes and is essential for maintaining epithelial integrity. It plays a pivotal role in the assembly of tight junctions and enhances mucus production [102] [103].
- Stabilization of the Gut Ecosystem: By promoting a healthy and diverse microbiota, prebiotics help crowd out pathobionts and stabilize the gut environment against dysbiosis.
Dietary Modifications
Overall dietary patterns directly influence the gut environment and barrier function:
- Western Diet vs. High-Fiber Diet: Diets rich in saturated fats and refined sugars (Western diet) are strongly associated with increased intestinal permeability and metabolic endotoxemia. Conversely, diets high in fiber and polyphenols support a diverse microbiota and SCFA production [99] [102].
- Micronutrient Supplementation: Vitamins A and D are critical for barrier maintenance. Vitamin A deficiency is linked to altered commensal bacteria and compromised barrier, while Vitamin D receptor signaling helps maintain the integrity of the intestinal mucosal barrier [102].
Table 2: Mechanisms of Action for Non-Pharmacological Interventions
| Intervention | Primary Mechanism | Key Effectors | Molecular/Cellular Outcome |
|---|---|---|---|
| Probiotics | Direct interaction with epithelium and immune system | Specific strains (e.g., Lactobacillus, Bifidobacterium) | Upregulation of ZO-1, occludin; secretion of bacteriocins; reduction of pro-inflammatory cytokines (TNF-α, IL-6). |
| Prebiotics | Selective stimulation of beneficial microbiota | Dietary fibers (e.g., FOS, GOS), resistant starch | Increased production of SCFAs (butyrate); expansion of SCFA-producing bacteria (e.g., Faecalibacterium). |
| Dietary Modifications | Global alteration of the gut milieu | High-fiber diets, vitamin A & D, low-fat diets | Enhanced microbial diversity; reduced circulating LPS; improved mucus layer thickness; stabilization of tight junctions. |
Signaling Pathways in Barrier Regulation and the Gut-Brain Axis
The communication between the gut and other organs, particularly the brain, is facilitated by the microbiota-gut-brain axis (MGBA). Increased intestinal permeability and microbial translocation can influence distal organs through neural, endocrine, and immune pathways [104] [101]. The following diagram illustrates the key signaling pathways involved in this communication, particularly following a breach in the intestinal barrier.
Diagram Title: Signaling Pathways Activated by Gut Permeability
Experimental Protocols for Assessing Intestinal Permeability
Robust and standardized methodologies are essential for evaluating the efficacy of interventions on tissue permeability. Below are detailed protocols for common in vivo and ex vivo assessments.
In Vivo Intestinal Permeability Test (Lactulose/Mannitol Test)
This is a non-invasive, functional clinical test that measures the urinary excretion of two non-metabolizable sugar molecules with different absorption pathways.
- Primary Objective: To assess the functional integrity of the intestinal paracellular pathway.
- Reagents:
- Lactulose: A disaccharide (Mr ~342 Da) that is minimally absorbed via the paracellular pathway in a healthy intestine. Increased absorption indicates a "leaky" tight junction complex.
- Mannitol: A monosaccharide (Mr ~182 Da) that is readily absorbed via the transcellular pathway. It serves as an internal control for gastric emptying, intestinal transit, and renal function.
- Procedure:
- Patient Preparation: The subject fasts for 8-12 hours overnight.
- Baseline Urine Collection: Upon waking, the subject completely empties their bladder (this sample is discarded).
- Sugar Administration: The subject ingests a pre-mixed solution containing 10g lactulose and 5g mannitol in 100-200 mL of water.
- Restrictions: No food or liquid is allowed for the first hour post-ingestion.
- Total Urine Collection: All urine produced over a precise 5-hour period is collected in a graduated container kept refrigerated.
- Sample Handling: After the 5-hour collection, the total urine volume is recorded and homogenized. A 10 mL aliquot is sent to the laboratory for analysis.
- Analysis: Urinary concentrations of lactulose and mannitol are quantified, typically by high-performance liquid chromatography (HPLC) or enzymatic assays. The result is expressed as the Lactulose:Mannitol (L:M) Excretion Ratio. A higher L:M ratio indicates increased paracellular intestinal permeability [102] [98].
Ex Vivo Analysis of Tight Junction Proteins in Intestinal Biopsies
This protocol allows for the direct molecular assessment of the epithelial barrier structure.
- Primary Objective: To quantify and localize the expression of tight junction proteins (TJPs) in intestinal epithelial tissue.
- Reagents:
- Primary Antibodies: Rabbit or mouse monoclonal antibodies against human ZO-1, Occludin, Claudin-1, -2, -3, -4, -5, -7, -8, -14, -15, -18, etc.
- Secondary Antibodies: Fluorescently labeled (e.g., Alexa Fluor 488, 594) or enzyme-conjugated (e.g., HRP) antibodies specific to the primary antibody host species.
- Other Reagents: Phosphate-buffered saline (PBS), paraformaldehyde (PFA) for fixation, Triton X-100 for permeabilization, blocking serum (e.g., normal goat serum), and mounting medium with DAPI.
- Procedure (Immunofluorescence):
- Tissue Acquisition: Intestinal biopsies are obtained via endoscopy (e.g., from terminal ileum or colon).
- Fixation: Biopsies are fixed in 4% PFA for 4-24 hours at 4°C.
- Sectioning: Fixed tissue is embedded in paraffin or optimal cutting temperature (OCT) compound and sectioned into 4-5 µm thick slices using a microtome or cryostat.
- Staining:
- Deparaffinization/Rehydration: (If using paraffin-embedded sections).
- Antigen Retrieval: Using a citrate-based buffer.
- Permeabilization: Incubate with 0.1-0.5% Triton X-100 in PBS.
- Blocking: Incubate with 5-10% normal serum for 1 hour.
- Primary Antibody Incubation: Apply diluted primary antibody and incubate overnight at 4°C.
- Washing: Wash with PBS 3 times for 5 minutes each.
- Secondary Antibody Incubation: Apply fluorescent secondary antibody and incubate for 1-2 hours at room temperature in the dark.
- Washing: Wash with PBS 3 times for 5 minutes in the dark.
- Mounting: Mount slides with a medium containing DAPI to stain cell nuclei.
- Imaging & Analysis: Images are acquired using a confocal or fluorescence microscope. Analysis includes assessing the fluorescence intensity and cellular localization (e.g., continuous vs. discontinuous membrane staining) of TJPs using image analysis software (e.g., ImageJ) [98].
Table 3: The Scientist's Toolkit: Key Research Reagents for Permeability Studies
| Reagent / Assay | Function / Target | Application in Research |
|---|---|---|
| Lactulose & Mannitol | Inert sugar probes for paracellular and transcellular pathways. | In vivo functional assessment of intestinal permeability (L:M test). |
| Anti-ZO-1 Antibody | Primary antibody targeting the tight junction protein ZO-1. | Immunofluorescence/Immunohistochemistry to visualize and quantify TJP expression in tissue sections. |
| Anti-Occludin Antibody | Primary antibody targeting the tight junction protein Occludin. | Evaluating the integrity and protein levels of the tight junction complex. |
| Lipopolysaccharide (LPS) ELISA Kit | Quantifies circulating bacterial endotoxin. | Measuring metabolic endotoxemia as a systemic consequence of increased intestinal permeability. |
| Cytokine Multiplex Assay (e.g., TNF-α, IL-6, IL-1β) | Quantifies multiple pro-inflammatory cytokines. | Assessing the systemic inflammatory response triggered by microbial translocation. |
| SCFA Analysis Kit (GC/MS) | Quantifies short-chain fatty acids (butyrate, acetate, propionate). | Measuring the metabolic output of the gut microbiota in response to prebiotic/probiotic interventions. |
Application in Disease Contexts and Research Outlook
The therapeutic potential of targeting the gut barrier is being explored across numerous disease domains.
- Aging and Neurodegeneration: The concept of "biome-aging" describes the cumulative, detrimental changes in the gut microbiome and barrier function with age, which is linked to "inflammaging" – a chronic, low-grade inflammatory state that drives age-related diseases [100]. Microbiome-based therapeutics are being investigated to promote healthier aging. For instance, centenarians exhibit a unique microbiome phenotype capable of producing specific secondary bile acids with antimicrobial properties that promote intestinal homeostasis [100].
- Stroke and Cardiovascular Disease: Dysbiosis is linked to an elevated risk of stroke and unfavorable outcomes post-stroke. The MGBA modulates immune function and metabolite production (e.g., TMAO, SCFAs), which can intensify neuroinflammation or promote repair. Strategies like probiotics, prebiotics, and fecal microbiota transplantation (FMT) are being explored to reduce stroke risk and improve recovery [104].
- Neurological and Psychiatric Disorders: The MGBA significantly influences brain structure and function, including neurogenesis, myelination, and microglia activity. Preclinical models (e.g., germ-free animals, antibiotic-induced dysbiosis) demonstrate that microbiota manipulations can lead to structural brain changes and altered behavior, offering potential avenues for microbial-based interventions in conditions like Alzheimer's, Parkinson's, and depression [105] [101].
Future research must focus on moving from association studies to elucidating cause-and-effect relationships. Key challenges include the high individual variability of gut microbiota, ensuring the stability and safety of interventions, and standardizing methodologies for human studies to build a validated evidence base for clinical application [104] [101].
Within the context of Wish (Water-Insoluble and Super-High permeability) compound research, the strategic enhancement of tissue permeability is a cornerstone of developing effective oral drug delivery systems. The oral route, while preferred for its non-invasiveness and patient compliance, presents a significant biopharmaceutical challenge: the intestinal epithelium is a formidable barrier to drug absorption [106]. A drug's journey from the gastrointestinal (GI) lumen to systemic circulation is governed by its aqueous solubility, stability in the GI environment, and most critically, its permeability across the intestinal membrane [5]. For Wish compounds, which inherently possess high permeability but poor solubility, the formulation focus often shifts towards solubilization. However, a vast number of new chemical entities (NCEs) and macromolecular therapeutics exhibit less-than-ideal permeability, limiting their therapeutic potential.
This is where absorption-modifying excipients (AMEs) transition from inert components to active enablers of drug delivery. Also known as permeation enhancers, these are critical pharmaceutical excipients that temporarily and reversibly alter the integrity of the intestinal epithelial cell membrane to facilitate drug absorption [107]. Their application is particularly vital for overcoming the permeability barrier, thereby increasing the bioavailability of drugs that would otherwise be poorly absorbed. The utility of AMEs extends beyond conventional small molecules to the burgeoning field of biologics, including peptides, proteins, and nucleic acids, where they can be the differentiating factor between a failed and a successful delivery system [108]. This whitepaper provides an in-depth technical guide to the mechanisms, evaluation, and strategic application of AMEs, framing their use within the essential paradigm of optimizing tissue permeability for advanced drug delivery.
Mechanisms of Action: How Absorption-Modifying Excipients Work
AMEs enhance drug permeability through a variety of biological mechanisms, each targeting specific components of the intestinal barrier. Understanding these mechanisms is prerequisite for their rational selection and application in formulation design.
The primary barrier to oral drug absorption is the intestinal epithelium, a single layer of cells joined at their apical surfaces by tight junctions (TJs) [106]. Drug transport occurs via the transcellular (across cells) or paracellular (between cells) pathways. The transcellular route is favored by lipophilic, low-molecular-weight drugs, while the paracellular route is the only option for hydrophilic compounds. AMEs are classified based on their interaction with these pathways and cellular components.
- Tight Junction Modulation: Many AMEs, such as sodium caprate and certain chitosan derivatives, function primarily by modulating the TJs. They can induce intracellular signaling pathways (e.g., involving phospholipase C, protein kinase C, and myosin light-chain kinase) that lead to the contraction of the perijunctional actin-myosin ring. This contraction causes the TJ strands to separate, physically widening the paracellular pores and allowing the passage of hydrophilic molecules [109]. This effect is generally transient and reversible.
- Membrane Fluidization: Surfactant-based AMEs like sodium dodecyl sulfate (SDS) can interact with and disrupt the phospholipid bilayer of cell membranes. By solubilizing membrane lipids or proteins, they increase membrane fluidity and create transient pores, thereby enhancing the transcellular transport of drugs [107] [110].
- Mucoadhesion and Mucus Interaction: Cationic polymers like chitosan not only affect TJs but also exhibit mucoadhesive properties. They can interact with and potentially disrupt the negatively charged mucus layer, increasing the contact time between the drug and the epithelial surface and facilitating direct access to the underlying absorptive cells [107].
- Inhibition of Efflux Transporters: Some excipients can inhibit efflux pumps like P-glycoprotein (P-gp), which actively pump certain drugs back into the intestinal lumen. While not a direct permeability enhancement mechanism, this inhibition effectively increases the net absorption of susceptible drugs, working synergistically with other enhancement strategies [106].
The following diagram illustrates the primary cellular pathways and mechanisms through which AMEs exert their effects.
The efficacy of an AME is not universal; it depends heavily on the physicochemical properties of the drug and the specific region of the GI tract. For instance, studies in rat intestine have shown that the permeability-enhancing effects of excipients like methyl-β-cyclodextrin and certain disintegrants can be significantly more pronounced in the jejunum compared to the ileum, highlighting the regional heterogeneity of the intestinal barrier [109].
Quantitative Assessment of Absorption-Modifying Excipients
The evaluation of AME efficacy requires robust quantitative data from validated models. The absorption-enhancing effects are typically reported as an increase in the membrane permeability coefficient (Papp) or a relative increase in the fraction of drug absorbed. However, it is critical to note that the observed enhancement is highly dependent on the experimental model used, as transit time, fluid volume, and membrane integrity can vary significantly between systems.
Table 1: Quantitative Effects of Selected AMEs in Various Preclinical Models
| AME | Model Compound | Experimental Model | Key Quantitative Result | Notes | Reference |
|---|---|---|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Multiple Model Compounds | Rat SPIP Model | Substantial enhancement effect observed | Effect was substantially lower in rat and dog bolus models. | [107] |
| Rat & Dog Bolus Models | Absorption-enhancing effect confirmed | [107] | |||
| Chitosan | Multiple Model Compounds | Rat SPIP Model | Substantial enhancement effect observed | Effect was substantially lower in rat and dog bolus models. | [107] |
| Rat & Dog Bolus Models | Absorption-enhancing effect confirmed | [107] | |||
| Sodium Caprate | Multiple Model Compounds | Rat SPIP Model | Substantial enhancement effect observed | [107] | |
| Methyl-β-cyclodextrin | 5(6)-carboxyfluorescein | Rat Jejunum Sac | Significantly increased membrane permeability | No significant change observed in the ileum. | [109] |
| Disintegrants (e.g., CCS, CMS-Na) | 5(6)-carboxyfluorescein | Rat Jejunum Sac | Significantly increased membrane permeability | Effect was region-dependent (jejunum vs. ileum). | [109] |
A critical insight from comparative studies is that data from transit-independent, pre-clinical permeability models like the single-pass intestinal perfusion (SPIP) model can overestimate the in vivo enhancement effect. For example, while SDS and chitosan showed substantial effects in the rat SPIP model, their efficacy was "substantially lower" in more physiologically relevant rat and dog intraintestinal bolus models [107]. This underscores the complexity of AME effects and indicates that additional GI physiological factors, such as luminal contents, mucus, and transit time, must be considered for a predictive evaluation. Therefore, it is recommended that initial AME screening data be verified in animal models that better simulate in vivo conditions at multiple excipient concentrations [107].
Experimental Protocols for Evaluating AMEs
To ensure reliable and reproducible data, standardized experimental protocols are essential. Below are detailed methodologies for two key assays used in the assessment of AME activity.
In Vitro Sac Method for Assessing Regional Intestinal Permeability
This ex vivo protocol is designed to evaluate the effects of excipients on the membrane permeability of model compounds, specifically in different regions of the small intestine [109].
- 1. Tissue Preparation: Sacrifice the rat and immediately excise the small intestine. Gently flush the intestinal lumen with ice-cold, oxygenated Krebs-Ringer buffer (or equivalent) to remove intestinal contents. Carefully isolate specific segments (e.g., jejunum and ileum) and cut them into sacs of a standardized length (e.g., 4-5 cm).
- 2. Excipient Exposure: Ligate one end of each intestinal sac and fill the serosal side with an appropriate buffer. The mucosal side is then filled with a buffer solution containing the model compound (e.g., 5(6)-carboxyfluorescein (5-CF) at a specified concentration) and the test excipient at the desired concentration. The contralateral end is then ligated to create a closed sac.
- 3. Incubation and Sampling: Place the prepared sacs in an incubation medium (oxygenated buffer at 37°C) for a predetermined period (e.g., 30-60 minutes). Maintain continuous oxygenation and gentle agitation to mimic physiological conditions.
- 4. Analytical Measurement: At the end of the incubation period, sample the serosal fluid inside the sac. The concentration of the model compound that has permeated from the mucosal to the serosal side is quantified using a suitable analytical method, such as fluorescence spectroscopy for 5-CF or HPLC for other compounds.
- 5. Data Calculation: Calculate the apparent membrane permeability (Papp) of the model compound. Compare the Papp values in the presence and absence of the excipient to determine the enhancement ratio. Statistical analysis (e.g., Student's t-test) should be performed to confirm significance.
Single-Pass Intestinal Perfusion (SPIP) Model
The SPIP model offers a more dynamic and transit-dependent system for evaluating permeability and the effects of AMEs [107].
- 1. Surgical Procedure: Anesthetize the rat and perform a midline abdominal incision to externalize a specific segment of the small intestine (e.g., jejunum). Cannulate both ends of the isolated intestinal segment.
- 2. Perfusion and Dosing: Perfuse the intestinal segment with a warmed (37°C), oxygenated buffer solution at a constant flow rate using a peristaltic pump. The perfusion buffer contains the drug candidate and the AME at the target concentration.
- 3. Sample Collection: Collect the perfusate exiting the segment at regular time intervals until steady-state conditions are achieved. The difference between the inlet and outlet drug concentrations is used to determine the fraction of drug absorbed.
- 4. Data Analysis: Calculate the effective permeability (Peff) coefficient based on the disappearance of the drug from the perfusate, taking into account water transport. The enhancement effect of the AME is quantified by the increase in Peff relative to a control perfusion (drug without AME).
The workflow for these key experiments, from design to data interpretation, is summarized in the following diagram.
The Scientist's Toolkit: Key Research Reagent Solutions
The effective study and application of AMEs require a suite of specialized reagents and materials. The following table details essential items for a research laboratory working in this field.
Table 2: Essential Research Reagents for AME Investigation
| Category / Reagent Name | Function & Application in AME Research | Key Considerations |
|---|---|---|
| Model Permeants | ||
| 5(6)-Carboxyfluorescein (5-CF) | A hydrophilic, fluorescent marker for assessing paracellular permeability enhancement [109]. | Easy to quantify via fluorescence; serves as a model for water-soluble, poorly permeable compounds. |
| Absorption-Modifying Excipients | ||
| Chitosan (and derivatives) | A cationic polymer that modulates tight junctions and exhibits mucoadhesive properties [107]. | Molecular weight and degree of deacetylation significantly influence its efficacy and toxicity. |
| Sodium Caprate (C10) | A medium-chain fatty acid salt that acts as a tight junction modulator via intracellular signaling [107]. | Concentration-dependent effect; well-studied safety profile. |
| Sodium Dodecyl Sulfate (SDS) | An anionic surfactant that enhances transcellular permeability via membrane fluidization [107]. | Can be cytotoxic at higher concentrations; requires careful concentration optimization. |
| Methyl-β-cyclodextrin | Used to enhance solubility and membrane permeability, primarily by cholesterol complexation/extraction [109]. | Can significantly alter membrane properties; effects can be region-specific in the intestine. |
| Specialized Excipients | ||
| Super Refined Poloxamer 188 | A high-purity, low-peroxide surfactant used to stabilize formulations (e.g., proteins) without introducing oxidative degradation [108]. | Ultra-low impurity levels are critical for sensitive biologics and for minimizing excipient-induced instability. |
| Analytical & Formulation Tools | ||
| ZoomLab (BASF) | A virtual formulation assistant providing algorithm-based analysis and science-backed formulation guidance [108]. | Useful for pre-screening excipient combinations and assessing risks like nitrosamine formation. |
| Nitrite-Tested Polymer Grades | Grades of polymers (e.g., povidone, copovidone) with validated low nitrite levels to mitigate nitrosamine risk [108]. | A critical quality attribute for regulatory compliance and patient safety. |
Strategic Application and Future Perspectives in Drug Development
The strategic deployment of AMEs in drug development requires a balanced consideration of efficacy, safety, and regulatory factors. A patient-centric approach, often implemented via an "Excipient Exclusion Filter," is increasingly important. This involves proactively screening and eliminating potentially problematic excipients based on the target patient population (e.g., lactose-free for the lactose-intolerant, PEG-free for those with PEG hypersensitivity) to de-risk development and enhance patient safety and compliance [111].
Future perspectives in the field are being shaped by several key trends:
- Advanced and Natural Excipients: There is a growing demand for novel, multifunctional excipients, including those derived from natural and plant-based sources, which are perceived to have fewer side effects [108].
- Personalized Medicine: The shift towards tailored therapies is driving the need for equally precise excipient systems that support route-specific delivery and enhanced bioavailability for specific patient subpopulations [108].
- Nanotechnology: The rise of nanoparticle delivery systems (e.g., lipid nanoparticles for mRNA) necessitates novel excipients that can act as lipid carriers, surface modifiers, and polymeric stabilizers to preserve nanoparticle integrity and improve intracellular delivery [108] [110].
In conclusion, absorption-modifying excipients represent a powerful tool for overcoming the fundamental biological barrier of low intestinal permeability. Their rational use, grounded in a deep understanding of their mechanisms, a critical interpretation of preclinical data, and a strategic, patient-centric formulation approach, is indispensable for advancing the oral delivery of challenging drug candidates within the WISH research landscape and beyond.
Validation Frameworks and Comparative Analysis of Permeability-Targeting Therapies
The development of therapies for rare diseases presents profound challenges, including small patient populations, difficulty conducting traditional randomized controlled trials, and the urgent, unmet medical needs of patients. In response, the U.S. Food and Drug Administration (FDA) has introduced innovative regulatory frameworks designed to provide greater speed and predictability while maintaining rigorous standards for safety and efficacy. The Rare Disease Evidence Principles (RDEP) and the "Plausible Mechanism" Pathway (PM Pathway) represent significant evolutions in the regulatory landscape for rare disease therapies [112] [113]. These pathways acknowledge the impracticality of traditional clinical trial designs for many rare conditions and create more flexible, evidence-based approaches for demonstrating therapeutic effectiveness.
For researchers focused on tissue permeability—particularly in the context of the WISH research background—these new frameworks offer opportunities to leverage advanced in vitro models, biomarker data, and mechanistic studies as substantial components of regulatory submissions. The explicit recognition of alternative evidence types within these pathways aligns with the scientific community's growing understanding of disease mechanisms and the critical role of biological barriers in therapeutic effectiveness [114] [17]. This guide provides a comprehensive technical analysis of these regulatory pathways, their eligibility requirements, evidence standards, and practical implementation strategies for research and development professionals.
The Rare Disease Evidence Principles (RDEP) Framework
The RDEP is a joint initiative between FDA's Center for Drug Evaluation and Research (CDER) and Center for Biologics Evaluation and Research (CBER) that provides a structured process for reviewing therapies targeting rare diseases with very small patient populations and significant unmet medical needs [112] [115]. Announced in September 2025, this framework addresses the fundamental challenge that generating substantial evidence of safety and efficacy using traditional clinical trials is often difficult or impossible for rare diseases [115]. The RDEP operates within existing statutory authorities, maintaining the requirement for substantial evidence of effectiveness under Section 505(d) of the FD&C Act, while providing greater clarity on the types of evidence that can fulfill this standard [115].
Eligibility Criteria
To qualify for the RDEP process, investigative therapies must meet specific eligibility criteria designed to identify those conditions where traditional development approaches are most challenging and where the benefit-risk profile may support alternative evidence generation strategies [115]:
- Population Size: The drug must target a very small, rare disease population or subpopulation, generally fewer than 1,000 persons in the United States [112] [115].
- Disease Mechanism: The condition must be caused by a known, in-born genetic defect that is the major driver of the pathophysiology [115].
- Disease Course: The clinical course must involve progressive deterioration in function leading to rapid and/or significant disability or death in a relatively short period [115].
- Unmet Need: There must be no adequate alternative therapies that alter the course of the disease [115].
- Therapeutic Specificity: The investigative therapy must be specific to the correction of the genetic defect in question, either by correcting the gene itself or replacing an essential physiological protein that is deficient due to the gene defect [115].
Table: RDEP Eligibility Requirements and Evidence Standards
| Criterion | Requirement | Potential Evidence |
|---|---|---|
| Population Size | Generally <1,000 patients in U.S. | Epidemiological studies, registry data, genetic prevalence models |
| Disease Mechanism | Known in-born genetic defect as major pathophysiology driver | Genetic sequencing, functional validation studies, biomarker data |
| Disease Course | Progressive deterioration leading to significant disability/death | Natural history studies, clinical records, patient registry data |
| Unmet Need | No adequate alternative disease-modifying therapies | Literature review, clinical guidelines, expert statements |
| Therapeutic Specificity | Direct correction of genetic defect or replacement of deficient protein | Mechanism of action studies, preclinical models, biomarker data |
Evidence Standards and Confirmatory Evidence
Under the RDEP, substantial evidence of effectiveness may generally be established based on one adequate and well-controlled study (which may be a single-arm trial) together with robust confirmatory evidence of the drug's treatment effect [115] [116]. The FDA has outlined several categories of acceptable confirmatory evidence:
- Evidence of the drug's treatment effect on direct pathophysiology: This may include demonstration of target engagement, modulation of disease-relevant pathways, or correction of physiological abnormalities [115].
- Evidence from relevant non-clinical models: This encompasses data from animal models, organ-on-chip systems, or other in vitro models that recapitulate key aspects of the human disease [112] [115].
- Therapeutically relevant clinical pharmacodynamic data: Measures of biological activity in human subjects that demonstrate engagement with the intended target and downstream effects [115] [116].
- Other clinical data: Including case reports, expanded access data, and natural history studies that provide context for interpreting treatment effects [112] [116].
The RDEP also explicitly acknowledges that external controls or natural history studies may serve as appropriate confirmatory evidence when properly characterized and matched to the treatment population [115]. This approach is particularly relevant for diseases with predictable progression patterns or well-documented natural history.
Application Process and Timeline
Sponsors may apply for the RDEP process at any time prior to the launch of a pivotal trial [115]. The request should be submitted to the existing Investigational New Drug (IND) application and must include reasonable evidence that the eligibility criteria are met and that safety and efficacy can be demonstrated by one adequate and well-controlled study with confirmatory evidence [115]. If no IND exists, FDA will assign a pre-IND number to facilitate discussions about the overall development plan [115]. Each request should address only one protocol, and the relevant center review team will issue a decision on acceptance following consultation with the CDER/CBER Rare Disease Policy and Portfolio Council (RDPPC) [115].
The "Plausible Mechanism" Pathway
Conceptual Framework and Background
The "Plausible Mechanism" Pathway (PM Pathway), introduced by FDA Commissioner Marty Makary and CBER Director Vinay Prasad in a November 2025 New England Journal of Medicine article, represents a more radical approach to regulating bespoke, personalized therapies [117] [113] [118]. This pathway is designed specifically for situations where randomized trials are not feasible, particularly for individualized therapies targeting unique genetic mutations [117]. The PM Pathway uses an operational model that begins with treating consecutive patients with bespoke therapies, with the "Baby K.J." case—a newborn with a rare genetic disorder treated with a personalized gene editing therapy—serving as an illustrative example [117] [113].
Core Eligibility Elements
The PM Pathway is defined by five key characteristics that determine eligibility [117] [113] [119]:
Identification of a specific molecular or cellular abnormality: The pathway is limited to conditions with a known and clear molecular or cellular abnormality with a direct causal link between the specific alteration and the disease presentation, as opposed to diseases defined by a range of diagnostic criteria or genome-wide associations.
Targeting the underlying biological alteration: Eligible interventions must target the underlying or proximate biological alteration by acting on the molecular or cellular abnormality itself, rather than acting broadly on the affected system or on downstream components.
Use of natural history data: There must be well-characterized natural history data for the disease in the untreated population to provide context for interpreting treatment effects.
Evidence of successful target engagement or editing: There must be confirmatory evidence showing that the product has successfully engaged or edited the target, which may come from animal models, non-animal models, or clinical biopsies.
Demonstration of clinical improvement: There must be evidence of durable improvements in clinical outcomes consistent with disease biology, such as prolonged periods of disease remission in relapsing conditions or consistent improvement in progressive disorders.
Table: PM Pathway Core Elements and Implementation Considerations
| Core Element | Technical Requirements | Implementation Examples |
|---|---|---|
| Specific Abnormality | Clear causal link between genetic alteration and disease | Single-gene disorders with established pathogenicity |
| Targeting Mechanism | Direct action on underlying biological defect | Gene correction, protein replacement, precise gene editing |
| Natural History | Well-characterized disease progression without treatment | Patient registries, retrospective studies, published literature |
| Target Engagement | Confirmatory evidence of successful targeting | Biopsy data, functional imaging, specific biomarker changes |
| Clinical Improvement | Durable improvement consistent with disease biology | Objective functional measures, survival data, quality of life |
Approval Process and Postmarketing Requirements
Under the PM Pathway, after a manufacturer has demonstrated success with several consecutive patients with different bespoke therapies, FDA will "move towards" granting marketing authorization [117] [113]. This approach allows sponsors to leverage clinical efficacy and safety data from the platform to support marketing approval for similar personalized products in other conditions [117]. Marketing authorization can be pursued through either accelerated or traditional approval pathways, depending on the strength of evidence in the product application [117] [113].
A critical component of the PM Pathway is the requirement for postmarketing evidence collection [117] [113] [119]. Sponsors must collect real-world evidence to demonstrate durability of effect, check for off-target edits, monitor for safety signals, and study the effect of early treatment on childhood growth and development [117] [113]. The specific requirements will vary based on feasibility and the product's risk-benefit profile, and FDA may alter product labeling, indications, or concomitant medication requirements as safety and effectiveness data mature [117].
Advanced Permeability Models in Regulatory Submissions
Tissue-Engineered Blood-Air Barrier Model
For researchers working in the context of WISH background research, advanced permeability models represent particularly relevant forms of confirmatory evidence under both the RDEP and PM Pathway frameworks. A 2025 study by Ozdemir et al. describes the development and functional characterization of a tissue-engineered blood-air barrier (BAB) model for in vitro applications [114]. This model replicates the structural and functional properties of the pulmonary alveolar-capillary interface, which is critical for gas exchange and protection against external insults [114].
The BAB model consists of alveolar epithelial (A549) and primary endothelial (pHUVEC) cells seeded on opposite sides of a thin (11 ± 4 μm) electrospun poly(ε-caprolactone) mesh of nanofibers (140-800 nm) representing the basal membrane and interstitial matrix of the native BAB when coated with collagen type I, fibronectin, and laminin 511 proteins [114]. The dense, nanofibrous architecture enables formation of cellular monolayers on opposite sides, allowing gas and nutrient exchange for 14 days at air-liquid interface [114].
Key functional measurements from this model include:
- TEER (Transepithelial Electrical Resistance): 44 ± 5.0 Ω·cm²
- Permeability coefficient (Papp): 2-5 × 10â»â¶ cm/s against fluorescein
- Tight junction formation: Demonstrated by ZO-1 and CD31 expression
- Structural integrity: Maintained over 14-day culture period
This physiologically relevant in vitro BAB model provides a robust platform for evaluating therapeutic permeability and barrier function in respiratory research, offering potential applications in regulatory submissions as non-clinical evidence of mechanism and tissue engagement [114].
Small Airway Microphysiological System for Drug Permeability
Another advanced model with significant regulatory relevance is the small airway microphysiological system (MPS) evaluated by Geiger et al. (2025) for assessing drug permeability of inhaled compounds [17]. This system recapitulates the pulmonary air-liquid interface (ALI) with primary epithelial and vascular endothelial cell layers, providing a more physiologically relevant environment for measuring drug permeability than simpler two-dimensional in vitro cell culture platforms [17].
The experimental protocol involves:
- Seeding primary human lung epithelial cells onto the top channel of the chip
- Culture for 14 days at ALI to promote monolayer differentiation
- Addition of endothelial cells into the bottom channel
- Evaluation of drug permeability by passing each compound (10 µM) through the top channel and measuring permeation into the bottom channel over 30, 60, 120, and 180 minutes
The system demonstrated appropriate cellular composition with tight junctions, basal, goblet, and ciliated cells in the top channel and endothelial attachment in the bottom channel [17]. Permeability studies estimated apparent permeability (Papp) values of:
- Albuterol sulfate: 1.02 × 10â»â¶ cm/s (highly permeable)
- Formoterol fumarate: 2.44 × 10â»â¶ cm/s (highly permeable)
- Olodaterol HCl: 0.0813 × 10â»â¶ cm/s (low permeability)
This small airway MPS represents the type of sophisticated in vitro model that may serve as confirmatory evidence under the RDEP framework, particularly for therapies targeting respiratory conditions where tissue permeability is a critical factor in therapeutic effectiveness [17].
Translational Porcine Model for Intestinal Permeability
For therapies targeting gastrointestinal conditions or administered orally, translational large animal models of intestinal permeability may provide relevant preclinical data. A 2025 study developed and optimized protocols to induce and quantify intestinal permeability in pigs as a translational model [120]. This research established methods using urinary recovery of orally administered permeability markers (sucralose, erythritol, and cobalt-disodium EDTA) over 120 hours to assess intestinal barrier function [120].
Key methodological aspects include:
- Use of intestinal stressors (indomethacin for small intestinal damage, DSS for large intestinal damage and inflammation)
- Quantification of urinary excretion rates of permeability markers
- Assessment of fecal inflammatory biomarkers (S100 family proteins)
- Evaluation of histomorphometric changes in intestinal tissue
This porcine model offers significant translational value for nutritional and pharmaceutical research, with direct relevance to understanding how therapeutic interventions might modulate intestinal barrier function in human diseases [120]. The well-characterized protocol provides a template for generating robust permeability data that could support regulatory submissions under the evidence frameworks discussed.
Table: Advanced Permeability Models for Regulatory Submissions
| Model Type | Key Applications | Primary Measurements | Regulatory Utility |
|---|---|---|---|
| Blood-Air Barrier Model [114] | Respiratory therapy development, inhalation toxicology | TEER, Papp, tight junction markers | Non-clinical evidence of tissue engagement and barrier penetration |
| Small Airway MPS [17] | Inhaled drug development, permeability classification | Apparent permeability (Papp), cellular composition, non-specific binding | Mechanism evidence, pharmacokinetic prediction, replacement for animal models |
| Translational Porcine Intestinal Model [120] | Oral therapy development, GI barrier function studies | Urinary recovery of markers, histomorphometry, inflammatory biomarkers | Translational bridge between in vitro models and human studies, pathophysiology evidence |
Experimental Protocols for Permeability Assessment
Protocol 1: Blood-Air Barrier Model Development
Objective: Create a physiologically relevant in vitro model of the blood-air barrier for therapeutic permeability assessment [114].
Materials:
- Electrospun poly(ε-caprolactone) nanofiber mesh (140-800 nm diameter)
- Alveolar epithelial cells (A549 cell line)
- Primary human umbilical vein endothelial cells (pHUVEC)
- Extracellular matrix coatings (collagen type I, fibronectin, laminin 511)
- Transepithelial electrical resistance (TEER) measurement system
- Fluorescein for permeability assessment
Methodology:
- Mesh Preparation: Fabricate thin (11 ± 4 μm) electrospun PCL meshes with nanofibrous architecture.
- Surface Modification: Coat meshes with ECM proteins to improve cellular adhesion.
- Cell Seeding: Seed alveolar epithelial cells on the apical side and endothelial cells on the basolateral side.
- Air-Liquid Interface Culture: Maintain cultures for 14 days at ALI to promote differentiation.
- Functional Characterization:
- Measure TEER values daily using volt-ohm meter
- Assess permeability using fluorescein (Papp calculation)
- Evaluate tight junction formation via immunofluorescence (ZO-1, CD31)
- Validation: Confirm physiological relevance through morphological and functional comparisons to native tissue.
Regulatory Application: Data generated from this protocol can serve as non-clinical evidence of mechanism and tissue engagement for respiratory therapies submitted under RDEP or PM Pathway [114].
Protocol 2: Microphysiological System Permeability Testing
Objective: Evaluate drug permeability using a small airway microphysiological system to support regulatory submissions for inhaled therapies [17].
Materials:
- Small airway MPS chips (microfluidic circuits with porous membrane)
- Primary human small airway epithelial cells
- Lung microvascular endothelial cells
- Test compounds (albuterol sulfate, formoterol fumarate, olodaterol HCl)
- LC-MS/MS system for drug quantification
- Confocal microscope for cellular characterization
Methodology:
- Chip Preparation: Seed epithelial cells in top channel and culture at ALI for 14 days.
- Endothelial Addition: Introduce endothelial cells into bottom channel after epithelial differentiation.
- Quality Control Assessment:
- Confirm appropriate cellular composition (goblet, ciliated, basal cells)
- Verify tight junction formation
- Evaluate non-specific drug binding to PDMS components
- Permeability Studies:
- Apply test compounds (10 µM) to top channel
- Sample from bottom channel at 30, 60, 120, and 180 minutes
- Quantify drug concentrations using LC-MS/MS
- Data Analysis:
- Calculate apparent permeability (Papp) coefficients
- Classify compounds according to inhaled Biopharmaceutical Classification System (iBCS)
Regulatory Application: This protocol generates human-relevant permeability data that can support evidence of target engagement and mechanistic understanding for therapies submitted under flexible regulatory pathways [17].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Reagents for Permeability Studies and Regulatory Applications
| Reagent/Material | Function | Example Application | Regulatory Relevance |
|---|---|---|---|
| Electrospun PCL Nanofiber Meshes [114] | Synthetic basal membrane for 3D cell culture | Blood-air barrier model development | Provides physiological relevance for in vitro models used as non-clinical evidence |
| Primary Human Small Airway Epithelial Cells [17] | Recreate human-relevant tissue barriers | Small airway MPS for inhalation studies | Human-derived data strengthens regulatory submissions; reduces animal testing |
| Transepithelial Electrical Resistance (TEER) Measurement Systems [114] | Quantify barrier integrity and tight junction formation | Functional validation of barrier models | Objective quantification of tissue integrity for mechanism evidence |
| Permeability Markers (Sucralose, Erythritol, Co-EDTA) [120] | Assess intestinal barrier function in vivo | Translational porcine intestinal permeability model | Provides translational bridge between in vitro models and human applications |
| Microphysiological System (Organ-on-Chip) Platforms [17] | Recapitulate human tissue microenvironment with fluid flow and mechanical cues | Predictive permeability assessment for inhaled drugs | Advanced models acceptable as confirmatory evidence under RDEP |
| Extracellular Matrix Proteins (Collagen I, Fibronectin, Laminin) [114] | Enhance cellular adhesion and differentiation | Coating of synthetic scaffolds for improved barrier formation | Improves physiological relevance of in vitro models for regulatory submissions |
Strategic Implementation for Drug Development Professionals
Pathway Selection and Integration
For research and development professionals, strategic selection between the RDEP and PM Pathway depends on multiple factors, including the nature of the therapeutic approach, patient population characteristics, and stage of development. The RDEP framework is particularly suited for rare diseases with known genetic defects where some traditional clinical development is possible but requires flexibility in evidence generation [112] [115]. In contrast, the PM Pathway is designed for truly bespoke therapies where even small clinical trials are not feasible, and evidence must be generated from consecutive individual treatments [117] [113].
Successful implementation often involves integrating these pathways with other regulatory tools, such as:
- Orphan Drug Designation: Provides incentives for rare disease development but requires separate application [112] [115]
- Accelerated Approval Pathways: Allow approval based on surrogate endpoints with postmarketing confirmation [117] [113]
- Breakthrough Therapy Designation: Expedites development and review of promising therapies [119]
Evidence Generation Strategy
Developing a robust evidence generation strategy is essential for success under these pathways. Key considerations include:
- Natural History Studies: Invest in comprehensive natural history data collection early in development, as this forms the critical foundation for interpreting treatment effects in single-arm studies or individual cases [117] [113].
- Biomarker Development: Validate biomarkers of target engagement, pathophysiology, and clinical effect that can serve as confirmatory evidence [115] [116].
- Advanced Model Systems: Incorporate physiologically relevant in vitro and in vivo models that can provide robust mechanistic data supporting the therapeutic approach [114] [17].
- Real-World Evidence Planning: Develop systematic approaches for collecting real-world evidence both pre- and post-approval to address evidence gaps [117] [113].
For researchers with WISH background focusing on tissue permeability, these frameworks offer unprecedented opportunities to leverage sophisticated permeability models as substantial components of regulatory packages, potentially accelerating the development of transformative therapies for rare disease patients while maintaining rigorous standards for safety and effectiveness.
Clinical Endpoints and Biomarker Validation for Permeability-Targeting Interventions
Biomarkers are an integral component of both the practice of medicine and the development and approval of new therapies. In drug development, biomarkers often play an important role in the selection of the patient population to be studied, dose selection, and safety and efficacy assessments [121]. Appropriately validated biomarkers are important tools that can benefit drug development and regulatory assessments by detecting physiological changes earlier than traditional clinical signs or symptoms, potentially before significant irreversible damage occurs [121]. For drug development purposes, biomarker development involves identifying a drug development need and context of use (COU) for the biomarker, analytically validating assays, clinically validating the biomarker for the COU, and determining if the biomarker provides benefits over current methods [121].
The validation of biomarkers is a complex process where the level of evidence needed depends on the COU and the purpose for which a biomarker is applied. This principle underscores the importance of a fit-for-purpose approach to biomarker validation, where different biomarker types require varying validation approaches focusing on specific evidence characteristics based on their intended COU [121]. Regulatory acceptance pathways include early engagement with regulators, the IND process, and the Biomarker Qualification Program (BQP), which provides a structured framework for the development and regulatory acceptance of biomarkers for a specific COU [121].
Biomarker Categories and Context of Use for Permeability
The FDA defines a biomarker's COU as a concise description of the biomarker's specified use in drug development, which includes the BEST biomarker category and the biomarker's intended use [121]. The BEST Resource defines multiple categories of biomarkers relevant to permeability-targeting interventions.
Table 1: Biomarker Categories and Applications in Permeability-Targeting Interventions
| Biomarker Category | Use in Permeability Interventions | Example |
|---|---|---|
| Diagnostic Biomarker | Identify abnormal intestinal or vascular permeability | Serum markers of microbial translocation |
| Monitoring Biomarker | Assess permeability status over time | Serial measurements of zonulin levels |
| Pharmacodynamic/ Response Biomarker | Measure biological response to permeability-targeting therapy | Changes in LPS or zonulin after intervention [122] |
| Predictive Biomarker | Identify patients likely to respond to specific permeability therapies | Specific gut microbiota signatures |
| Safety Biomarker | Detect potential adverse effects during treatment | Serum creatinine for kidney safety [121] |
For permeability-focused research, several biomarker categories are particularly relevant. Susceptibility/risk biomarkers identify individuals with increased risk of developing diseases related to permeability defects, while diagnostic biomarkers can detect and categorize existing permeability abnormalities. Monitoring biomarkers are used to assess permeability status over time or in response to environmental factors [121]. Pharmacodynamic/response biomarkers are particularly valuable for measuring biological responses to permeability-targeting interventions, providing critical information on whether a therapeutic is having its intended effect on the permeability barrier [121].
Quantitative Biomarkers of Permeability: Evidence and Data
Substantial clinical evidence supports various biomarkers for assessing permeability changes in response to interventions. Recent meta-analyses have quantified the effects of different intervention types on established permeability markers.
Table 2: Quantitative Effects of Interventions on Permeability Biomarkers Based on Meta-Analyses
| Intervention Type | Biomarker | Number of Studies (Participants) | Standardized Mean Difference (95% CI) | Certainty of Evidence |
|---|---|---|---|---|
| Pro- and Synbiotics | Lipopolysaccharide (LPS) | 24 RCTs (n=1,603) | -0.54 (-1.01, -0.07) | Very Low |
| Pro- and Synbiotics | Zonulin | 13 RCTs (n=778) | -0.49 (-0.79, -0.18) | Moderate |
| Prebiotics | Lipopolysaccharide (LPS) | 16 RCTs (n=792) | -0.88 (-1.28, -0.47) | High |
The data demonstrate that prebiotic supplementation shows particularly strong effects on reducing LPS levels, a key marker of bacterial translocation resulting from increased intestinal permeability. The high certainty of evidence for prebiotics suggests consistent findings across studies, while the more moderate certainty for pro- and synbiotics on zonulin reduction indicates promising but less consistent effects [122]. These quantitative benchmarks provide essential reference points for designing new clinical trials targeting permeability improvement.
Experimental Protocols for Permeability Assessment
In Vitro Permeability Assays
In vitro permeability assays typically use cells cultured in 2D or 3D geometries to model biological barriers. The transwell assay system represents a standardized methodology for quantifying permeability across cellular monolayers [123].
Protocol: Transwell Assay for Epithelial/Endothelial Permeability
- Cell Culture: Seed appropriate cell types (Caco-2 for intestinal models, MDCK for general permeability, or brain endothelial cells for BBB models) on permeable membrane inserts at standardized densities (typically 50,000-100,000 cells/cm²).
- Barrier Formation: Culture for 7-21 days until transepithelial electrical resistance (TEER) values stabilize, indicating mature barrier formation.
- Compound Application: Add test compounds to donor compartment (apical for absorption studies, basolateral for secretion studies).
- Sampling and Analysis: Collect samples from receiver compartment at predetermined time points (e.g., 30, 60, 120 minutes) and quantify compound concentration using HPLC, MS, or fluorescence detection.
- Permeability Calculation: Calculate apparent permeability (Papp) using the formula: Papp = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial donor concentration [123].
Quality control measures include monitoring TEER throughout the experiment, assessing monolayer integrity with paracellular markers, and maintaining physiological temperature and pH conditions.
In Vivo Permeability Assessment
In vivo methods provide physiological context for permeability assessment. The in situ brain perfusion technique quantitatively measures blood-brain barrier permeability, while intestinal permeability can be assessed using orally administered probe molecules [123].
Protocol: Multiple Time-Point Regression Analysis for BBB Permeability
- Animal Preparation: Anesthetize and surgically prepare animals (typically rodents) for intracarotid perfusion.
- Perfusate Preparation: Create physiological buffer containing test compound and permeability reference markers.
- Perfusion Procedure: Cannulate common carotid artery and perfuse at constant flow rate (2.5-5 mL/min) for varying durations (15 seconds to 10 minutes).
- Tissue Collection: Terminate perfusion, decapitate animal, and rapidly remove brain regions of interest.
- Quantitative Analysis: Measure compound concentrations in brain tissue and perfusate using appropriate analytical methods. Calculate permeability-surface area product using graphical or computational methods [123].
For intestinal permeability assessment, the lactulose-mannitol test represents a standardized clinical approach where these non-metabolized sugars are orally administered and their urinary excretion ratio is measured, with higher lactulose:mannitol ratios indicating increased intestinal permeability.
Signaling Pathways in Permeability Regulation
The regulation of tissue permeability involves complex signaling networks that control intercellular junctions and barrier function. The following diagram illustrates key pathways implicated in permeability regulation across various tissue types.
Diagram 1: Signaling Pathways in Permeability Regulation
This pathway diagram illustrates the balance between barrier-disrupting signals (primarily from inflammatory stimuli) and barrier-strengthening pathways activated by therapeutic interventions. The convergence on tight junction regulation highlights critical control points for permeability-targeting therapies, with downstream effects measurable through biomarkers such as LPS and zonulin [122].
Biomarker Validation Workflow
The validation of permeability biomarkers requires a systematic approach to ensure reliability and regulatory acceptance. The following workflow outlines the key stages from biomarker identification to regulatory submission.
Diagram 2: Biomarker Validation Workflow
This validation workflow emphasizes the fit-for-purpose approach endorsed by regulatory agencies [121]. The process begins with clearly defining the drug development challenge and context of use, followed by rigorous analytical validation assessing performance characteristics such as accuracy, precision, analytical sensitivity, and specificity [121]. Clinical validation then demonstrates that the biomarker accurately identifies or predicts the clinical outcome of interest in the intended population, including assessment of sensitivity, specificity, and predictive values [121].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Permeability Studies
| Reagent/Category | Specific Examples | Function in Permeability Research |
|---|---|---|
| Cell Culture Models | Caco-2, MDCK, MDCK-MDR1, brain endothelial cells | In vitro modeling of intestinal, renal, or blood-brain barrier permeability [123] |
| Permeability Markers | Lucifer yellow, FITC-dextrans, propranolol, bupropion | Quantitative assessment of paracellular and transcellular transport [123] |
| Tight Junction Assays | Zonulin ELISA, occludin Western blot, claudin antibodies | Measurement of tight junction proteins regulating paracellular permeability |
| Microbiome Modulators | Specific probiotic strains, prebiotic fibers, synbiotic formulations | Investigational tools for modulating gut barrier function [122] |
| Analytical Instruments | HPLC-MS, plate readers, TEER measurement systems | Quantification of compound transport and barrier integrity [123] |
This toolkit encompasses the essential materials required for comprehensive permeability research, from basic barrier models to advanced analytical systems. The selection of appropriate cell models depends on the specific biological barrier being studied, with Caco-2 cells representing the intestinal epithelium and various endothelial cell types modeling vascular barriers [123]. Permeability markers enable quantitative assessment of transport mechanisms, with different molecular weight probes distinguishing paracellular versus transcellular routes. Advanced analytical instrumentation provides the sensitivity required for accurate quantification of permeability changes and biomarker levels in complex biological matrices [123].
Celiac disease is an immune-mediated disorder triggered by dietary gluten in genetically susceptible individuals, characterized by damage to the small intestinal mucosa. A pivotal aspect of its pathophysiology is increased intestinal permeability, which facilitates the translocation of immunogenic gluten peptides across the epithelial barrier into the lamina propria, thereby initiating and perpetuating a destructive immune response [124]. This case study examines larazotide acetate (LA), a first-in-class tight junction regulator peptide, as a therapeutic intervention designed to restore intestinal barrier integrity. Framed within broader research on tissue permeability, this analysis provides an in-depth technical evaluation of LA's mechanisms, efficacy, and practical application in experimental models, intended for an audience of researchers, scientists, and drug development professionals.
Background and Pathophysiology
Intestinal Permeability in Celiac Disease
The intestinal epithelium forms a selective barrier, with tight junctions (TJs) serving as the primary regulators of paracellular permeability. In celiac disease, this barrier function is compromised, allowing increased passage of gluten-derived peptides such as gliadin [125] [124]. These peptides undergo deamidation by tissue transglutaminase (tTG) in the lamina propria, enhancing their immunogenicity and triggering a T-helper cell type 1-mediated immune response that leads to mucosal inflammation and damage [126]. Notably, the "transcellular pathway" has been identified as a key route for gluten translocation, with secretory IgA potentially facilitating the rapid transport of intact gluten peptides via the transferrin receptor in a "Trojan horse" manner [125].
The regulation of TJ integrity is critically influenced by the phosphorylation state of myosin light chain-2 (MLC-2). Phosphorylated MLC-2 induces contraction of the perijunctional actomyosin ring, increasing paracellular permeability. This process is mediated by the myosin light chain kinase (MLCK) and Rho-associated coiled-coil containing protein kinase (ROCK) pathways, both of which are implicated in the barrier dysfunction observed in intestinal disorders, including celiac disease [127] [95].
Larazotide Acetate: A Therapeutic Candidate
Larazotide acetate (also known as AT1001) is a synthetic octapeptide (H-Gly-Gly-Val-Leu-Val-Gln-Pro-Gly-OH) developed as a zonulin antagonist [127] [95]. Zonulin is an endogenous modulator of intestinal tight junctions, and its dysregulation is implicated in increased gut permeability. While initially characterized as a zonulin antagonist, recent research suggests LA may exert its protective effects through additional cellular mechanisms independent of zonulin inhibition, including direct regulation of TJ proteins and the actin cytoskeleton [127] [95]. Clinical trials have demonstrated that LA is generally well-tolerated and can mitigate gluten-induced worsening of gastrointestinal symptoms in patients with celiac disease, supporting its potential as a therapeutic adjunct to a gluten-free diet [126].
Mechanisms of Action
Larazotide acetate protects intestinal epithelial integrity through multiple interconnected cellular mechanisms, as elucidated by recent transcriptomic and functional studies.
Tight Junction Stabilization and Actin Regulation
Pretreatment with LA significantly preserves the organization and cellular distribution of key TJ proteins, including ZO-1, occludin, and claudins, during injury induced by anoxia/reoxygenation (A/R) [127] [95]. This stabilization is associated with a marked reduction in the phosphorylation of myosin light chain-2 (MLC-2), a regulatory protein whose phosphorylation status directly controls the contractility of the perijunctional actomyosin ring and, consequently, paracellular permeability [127]. The reduction in MLC-2 phosphorylation is achieved through LA's modulation of the ROCK pathway, a key regulator of the cytoskeleton [127]. This mechanism helps prevent the contraction of the actomyosin ring and the subsequent opening of tight junctions, thereby maintaining a selective barrier.
Modulation of Proliferative Signaling Pathways
RNA sequencing analysis of intestinal epithelial cells treated with LA revealed significant enrichment of genes associated with barrier regulation, small GTPase signaling, and crucially, pathways controlling cellular proliferation and migration [127]. LA was found to enhance the activity of proliferative pathways, including Wnt and Notch signaling [127]. The canonical Wnt/β-catenin pathway is essential for intestinal epithelial homeostasis; it promotes the cytoplasmic and nuclear accumulation of β-catenin, which then partners with T-cell factor/lymphoid enhancer factor (TCF/LEF) to activate the transcription of target genes that drive cell proliferation, such as c-myc and cyclin D1 [128] [129]. By positively influencing these pathways, LA facilitates epithelial repair and restoration of the mucosal surface following injury.
Table 1: Core Mechanisms of Action of Larazotide Acetate
| Mechanism | Biological Effect | Experimental Outcome |
|---|---|---|
| Tight Junction Stabilization | Preserves localization of ZO-1, occludin, and claudins at the cell membrane. | Increased Transepithelial Electrical Resistance (TEER); reduced paracellular flux [127] [95]. |
| ROCK/MLC-2 Pathway Modulation | Reduces phosphorylation of Myosin Light Chain-2 (MLC-2). | Prevents perijunctional actomyosin ring contraction, stabilizing the paracellular barrier [127]. |
| Actin Cytoskeleton Rearrangement | Promotes cortical actin stabilization. | Contributes to the reinforcement of the apical junctional complex [127] [95]. |
| Activation of Proliferative Pathways | Enhances Wnt/β-catenin and Notch signaling. | Increases cellular proliferation and migration, supporting epithelial repair [127]. |
The following diagram synthesizes the primary signaling pathways modulated by Larazotide Acetate as identified from the transcriptomic and functional data.
Experimental Models and Protocols
To rigorously evaluate the efficacy and mechanism of action of LA, researchers employ standardized in vitro models of intestinal barrier injury.
Cell Culture Models
- Caco-2BBe1 Monolayers: The human intestinal epithelial cell line Caco-2BBe1, a derivative of Caco-2 cells, is plated at a density of 100,000 cells per well on 0.4 µm pore-sized permeable supports. These monolayers are cultured for 10-14 days to achieve full differentiation and a Transepithelial Electrical Resistance (TEER) value exceeding 400 Ω·cm², indicative of a mature, tight barrier [127] [95].
- Leaky IPEC-J2 Model: Porcine intestinal epithelial cells (IPEC-J2) are cultured in a specialized crypt-like medium containing 50% L-WRN (which supplies Wnt-3a, R-Spondin, and Noggin) to induce a stem-cell like, proliferative state. After at least five passages in this medium, the cells are considered a "leaky" model and are plated on permeable supports, typically forming monolayers with a baseline TEER of approximately 30 Ω·cm² [127] [95].
Induction of Barrier Injury and Treatment
- Anoxia/Reoxygenation (A/R) Injury: Differentiated Caco-2BBe1 monolayers are placed in a modular incubator chamber, flushed with 95% N₂/5% CO₂ for 5 minutes to displace oxygen, and sealed airtight for a 2-hour anoxic period at 37°C. The chamber is then opened, and cells are returned to a normoxic environment (21% O₂) for up to 4 hours of reoxygenation. This A/R insult mimics the ischemic injury found in inflammatory conditions and reliably increases paracellular permeability [127] [95].
- Larazotide Acetate Administration: LA is typically prepared in a lyophilized, >99% pure form. For experiments, it is dissolved and applied apically to the cell monolayers at varying concentrations (e.g., 0.01, 1, and 10 mM) as a pretreatment prior to the induction of A/R injury [127] [95]. Control groups may include inhibitors such as the ROCK inhibitor Fasudil (100 µM) for mechanistic comparison [127].
The workflow for a typical experiment is outlined below.
Key Analytical Assays
- Transepithelial Electrical Resistance (TEER): TEER is measured using a chopstick electrode set connected to an epithelial voltohmeter. Measurements are taken in triplicate from both apical and basal sides of the monolayer, with the resistance value from a blank insert subtracted to yield the final TEER value. This serves as a direct, real-time functional readout of barrier integrity [127] [95].
- Protein Localization and Expression: The localization and organization of TJ proteins (e.g., ZO-1, occludin) and the actin cytoskeleton are visualized via immunofluorescence (IF) staining. Protein expression and post-translational modifications (e.g., phosphorylated MLC-2) are quantified by Western blotting. Membrane and cytosolic protein fractions can be separated using commercial extraction kits for more precise analysis [127] [95].
- Transcriptomic Analysis: RNA sequencing (RNA-seq) is performed to identify global changes in gene expression. Differentially expressed genes are analyzed for enrichment in specific biological pathways (e.g., small GTPase signaling, protein phosphorylation, proliferation, migration) using bioinformatic tools, providing a systems-level view of LA's mechanism [127].
The protective effects of Larazotide Acetate are quantified through key functional and molecular metrics.
Table 2: Summary of Key Experimental Findings for Larazotide Acetate
| Experimental Model | Treatment Condition | Primary Functional Readout (TEER) | Key Molecular Findings |
|---|---|---|---|
| Caco-2BBe1 Monolayers | A/R Injury + Vehicle | Significant Decrease | Disrupted TJ protein localization; ↑ MLC-2 phosphorylation [127] [95]. |
| Caco-2BBe1 Monolayers | A/R Injury + LA Pretreatment | Significantly Increased vs. Vehicle | Preserved TJ organization; ↓ MLC-2 phosphorylation; Actin rearrangement [127] [95]. |
| Leaky IPEC-J2 Cells | Baseline (L-WRN Media) | Low Baseline (~30 Ω·cm²) | Constitutively "leaky" phenotype [127]. |
| Leaky IPEC-J2 Cells | LA Treatment | Increased vs. Baseline | Enhanced barrier function in a constitutive leak model [127]. |
| Human Celiac Disease Patients (Clinical Trial) | Gluten Challenge + Placebo | Worsened GI Symptoms | Increased gastrointestinal symptom severity [126]. |
| Human Celiac Disease Patients (Clinical Trial) | Gluten Challenge + LA (lower doses) | Limited Symptom Worsening | Prevented gluten-induced increase in GI symptom severity [126]. |
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs critical reagents and their applications for studying intestinal permeability and the effects of larazotide acetate.
Table 3: Key Research Reagent Solutions for Intestinal Permeability Studies
| Reagent / Kit | Manufacturer (Example) | Function in Research |
|---|---|---|
| Larazotide Acetate (AT1001) | Innovative Biopharmaceuticals, Inc. | The investigational peptide used to protect barrier function and regulate tight junctions in models of intestinal injury [127] [95]. |
| Caco-2BBe1 Cell Line | ATCC | A well-established human intestinal epithelial cell model that forms polarized, differentiated monolayers with high TEER, ideal for barrier function studies [127] [95]. |
| IPEC-J2 Cell Line | N/A (Academic Source) | A non-transformed porcine intestinal epithelial cell line useful for creating "leaky" barrier models, especially when cultured in L-WRN medium [127] [95]. |
| Fasudil (ROCK Inhibitor) | STEMCELL Technologies | A small-molecule inhibitor of ROCK kinase. Used as a mechanistic control to inhibit the ROCK-MLC-2 pathway and compare effects with LA [127]. |
| Peptide 18 (MLCK Inhibitor) | Tocris Bioscience | A cell-permeable inhibitor of myosin light chain kinase. Used to probe the specific role of the MLCK pathway in barrier regulation [127]. |
| Mem-PER Kit | Thermo Scientific | Used to fractionate cellular lysates into cytosolic and membrane-bound protein compartments, enabling detailed analysis of TJ protein distribution [127] [95]. |
| L-WRN Cell Line/Conditioned Medium | ATCC | Conditioned medium containing Wnt-3a, R-Spondin, and Noggin. Used to culture IPEC-J2 cells in a stem-cell promoting state, inducing a constitutive "leaky" phenotype for research [127] [95]. |
| Chopstick Electrode Set & EVOM2 Voltohmeter | World Precision Instruments (WPI) | The standard equipment for rapid, non-destructive measurement of Transepithelial Electrical Resistance (TEER) in cell culture monolayers [127] [95]. |
Larazotide acetate represents a mechanistically novel therapeutic approach for celiac disease that directly targets the underlying pathology of intestinal hyperpermeability. Evidence from preclinical models demonstrates that its efficacy extends beyond simple zonulin antagonism, involving the stabilization of tight junction proteins via modulation of the ROCK/MLC-2 axis, rearrangement of the actin cytoskeleton, and promotion of epithelial repair through the enhancement of proliferative pathways like Wnt and Notch. The experimental protocols and reagent toolkit detailed herein provide a robust framework for researchers to further investigate barrier biology and evaluate next-generation therapeutic candidates. As the understanding of tissue permeability evolves, LA continues to serve as a critical proof-of-concept, underscoring the therapeutic potential of targeting the intestinal barrier in celiac disease and other conditions characterized by "leaky gut."
The integrity of biological barriers is a cornerstone of physiological homeostasis, and its disruption is a pivotal mechanism in the pathogenesis of diverse diseases. This whitepaper provides a comparative analysis of altered permeability in celiac disease (CeD), inflammatory bowel disease (IBD), and metabolic disorders, contextualized within a broader research framework on the role of tissue permeability. For researchers and drug development professionals, understanding the distinct and shared pathways of barrier dysfunction across these conditions is critical for developing targeted therapeutic strategies. The analysis synthesizes current findings on key biomarkers, functional tests, and underlying molecular mechanisms, offering a technical foundation for further investigative and developmental work.
Pathophysiological Mechanisms and Biomarkers
The "leaky gut" phenomenon manifests through distinct yet sometimes overlapping pathways in different diseases. Table 1 summarizes the primary biomarkers and their associations.
Table 1: Key Biomarkers of Altered Permeability Across Diseases
| Disease Context | Key Biomarkers / Functional Tests | Direction of Change | Primary Biological Significance |
|---|---|---|---|
| Celiac Disease (CeD) | Serum Zonulin [130] | ↑ in non-compliant GFD | Modulator of tight junctions; indicates intestinal barrier disruption [130]. |
| Lactulose/Mannitol (L/M) Ratio [131] | ↑ | Functional measure of increased paracellular permeability [131]. | |
| Inflammatory Bowel Disease (IBD) | Lactulose/Mannitol Excretion [132] | ↑ (vs. healthy controls) | Marker of increased small intestinal and colonic permeability, present even in remission [132]. |
| Growth Differentiation Factor 15 (GDF15) [133] | ↑ (vs. healthy controls) | Marker of mitochondrial stress; reduces ZO-1 and claudin-1, increasing permeability [133]. | |
| Lipopolysaccharide-Binding Protein (LBP) [133] | ↑ | Correlates with inflammation and intestinal permeability [133]. | |
| Gluten Sensitivity (GS) | Lactulose/Mannitol (L/M) Ratio [134] | ↓ (vs. healthy controls) | Suggests a different pathophysiology from CeD, potentially with enhanced barrier integrity [134]. |
| Claudin-4 (CLDN4) Gene Expression [134] | ↑ | May contribute to observed reduction in permeability [134]. | |
| Metabolic Disorders | 24-hour Urinary Microalbumin [135] | ↑ in Metabolic Syndrome | Indicator of systemic endothelial and glomerular permeability; independently associated with MetS [135]. |
| Serum Retinol [37] | ↓ with higher L/M ratio | Inverse association with intestinal permeability in the elderly [37]. |
The pathophysiology of barrier dysfunction varies significantly between conditions. In CeD, the central event is gluten exposure in genetically susceptible individuals, which triggers the release of zonulin. Zonulin is a key regulator of tight junctions, and its upregulation leads to increased paracellular permeability, allowing gliadin peptides to cross the epithelial barrier and initiate an adaptive immune response [130]. This is quantifiable via the lactulose/mannitol test, which measures the ratio of the paracellular probe (lactulose) to the transcellular probe (mannitol) [131].
In contrast, IBD involves a more complex interplay of factors. Recent research highlights the role of mitochondrial stress. The mitochondrial unfolded protein response (UPRmt) in intestinal epithelial cells leads to the release of GDF15, which in turn decreases the expression of critical tight junction proteins like zonula occludens-1 (ZO-1) and claudin-1, compromising barrier integrity [133]. Importantly, increased intestinal permeability, measured by sugar excretion tests, is a feature of IBD even during endoscopic remission, suggesting it may be a primary defect predisposing to relapse [132].
A critical distinction is evident between CeD and Gluten Sensitivity (GS). Despite symptom overlap, GS is not associated with increased intestinal permeability. In fact, one study found permeability in GS to be significantly reduced compared to healthy controls, paralleled by increased expression of the tight junction protein claudin-4. This suggests GS is a distinct entity characterized by innate immune activation without the breakdown of the physical barrier seen in CeD [134].
In metabolic disorders, the permeability concept extends beyond the gut. Microalbuminuria (elevated albumin in urine) is a well-established marker of systemic endothelial dysfunction and glomerular capillary permeability and is independently associated with metabolic syndrome (MetS) [135]. Furthermore, systemic nutritional status, such as low serum retinol (Vitamin A), is inversely associated with increased intestinal permeability in the elderly, linking nutrition, gut barrier, and metabolic health [37].
Experimental Methodologies for Permeability Assessment
In Vivo Intestinal Permeability Assessment (Lactulose/Mannitol Test)
The lactulose/mannitol (L/M) test is a gold-standard, non-invasive method for assessing small intestinal permeability in vivo [131]. The following is a detailed protocol.
Principle: The test uses two non-metabolizable sugar probes. The small molecule mannitol (transcellular probe) is absorbed through water pores in the epithelial membrane, while the larger molecule lactulose (paracellular probe) passes through tight junctions. An increased L/M ratio in urine indicates enhanced paracellular permeability [131].
Materials:
- Lactulose (5 g) and Mannitol (2 g)
- Distilled water
- Standard urine collection containers
- Chlorhexidine (2.35%) as a urine preservative
- High-Performance Anion-Exchange Chromatography with Pulsed Amperometric Detection (HPAE-PAD) system for sugar analysis
Procedure:
- Patient Preparation: The patient undergoes an overnight fast (minimum 8 hours) [131] [132].
- Test Solution Administration: The patient drinks 100 mL of a solution containing 5 g of lactulose and 2 g of mannitol dissolved in water [131].
- Urine Collection: All urine is collected for a precisely timed 5-hour period. To prevent bacterial growth, 1 drop of 2.35% chlorhexidine is added for every 50 mL of urine collected. The total urine volume is recorded [131] [37].
- Sample Analysis: Urine samples are analyzed via HPAE-PAD to determine the concentrations of lactulose and mannitol [131].
- Calculation:
- Fractional Excretion of Lactulose (FEL) = (Lactulose excreted in mg) / (Ingested lactulose in mg)
- Fractional Excretion of Mannitol (FEM) = (Mannitol excreted in mg) / (Ingested mannitol in mg)
- Lactulose:Mannitol Ratio (LMR) = FEL / FEM [131]
The following diagram illustrates the workflow and underlying principle of this test.
Assessment of Serum Biomarkers (Zonulin, GDF15)
Quantifying serum biomarkers like zonulin and GDF15 provides a molecular correlate to functional permeability tests.
Principle: Enzyme-linked immunosorbent assay (ELISA) uses antibodies immobilized on a plate to capture the target protein from serum. A detection antibody and enzyme reaction generate a signal proportional to the protein concentration [130] [133].
Materials:
- Venous blood sample tubes
- Centrifuge
- ELISA kits for target protein (e.g., human zonulin, GDF15)
- Microplate reader
Procedure (Summarized from Zonulin Protocol [130]):
- Sample Collection & Preparation: Collect venous blood after an 8-12 hour fast. Centrifuge to separate serum. Store aliquots at -80°C.
- ELISA Assay:
- Add serum samples to wells pre-coated with a capture antibody.
- Incubate, then wash to remove unbound substances.
- Add a biotinylated detection antibody. Incubate and wash.
- Add Horseradish Peroxidase (HRP)-avidin enzyme conjugate. Incubate and wash.
- Add tetramethylbenzidine (TMB) substrate. Enzymatic reaction produces a blue color.
- Add a stop solution to terminate the reaction, changing the color to yellow.
- Measurement & Analysis: Measure the absorbance at 450 nm. Calculate the concentration of the target protein by interpolating from a standard curve.
Research Reagent Solutions Toolkit
Table 2: Essential Research Reagents for Permeability Studies
| Reagent / Assay | Function / Application | Specific Examples / Notes |
|---|---|---|
| In Vivo Permeability Probes | Functional assessment of gut barrier in living subjects. | Lactulose & Mannitol for L/M test [131]; 13C-Mannitol for segmental analysis [132]. |
| ELISA Kits | Quantify soluble biomarkers in serum/plasma. | Zonulin [130], GDF15 [133], LBP [133] [136]. |
| Cell Culture Models | In vitro study of barrier function and molecular mechanisms. | Caco-2 cells (standard, but limited) [36]; Human jejunal (J2) & duodenal (D109) enteroid-derived cells (higher physiological relevance) [36]; Colonic organoids [133]. |
| Antibodies for Tight Junction Proteins | Visualize and quantify junctional complexes via immunohistochemistry/Western blot. | Targets: Zonula Occludens-1 (ZO-1), Claudin-1, Claudin-4, Occludin [134] [133]. |
| HPAE-PAD / HPLC Systems | Gold-standard analysis for sugar probes in urine. | Critical for accurate measurement in L/M tests [131]. |
Signaling Pathways in Barrier Dysfunction
The mechanisms by which different diseases disrupt barrier integrity involve distinct signaling cascades. The following diagram synthesizes key pathways from the literature, illustrating the divergent paths in CeD, IBD, and GS.
This analysis underscores that increased tissue permeability is a common pathogenic endpoint across CeD, IBD, and metabolic disorders, yet it arises through fundamentally distinct mechanisms. In CeD, zonulin-mediated tight junction disassembly is a direct response to an environmental trigger (gluten). In IBD, mitochondrial stress-induced GDF15 release appears to be a novel pathway eroding the barrier, with permeability persisting as a subclinical risk factor even during remission. Conversely, gluten sensitivity demonstrates that clinical symptoms can occur without, or even with reduced, permeability, highlighting the critical role of non-barrier related immune mechanisms. In metabolic disorders, systemic microalbuminuria serves as a proxy for widespread vascular permeability and endothelial dysfunction.
From a drug development perspective, these distinctions are paramount. Therapeutic strategies aimed at "sealing the leaky gut" must be disease-specific. Targeting the zonulin pathway holds promise for CeD, while mitigating mitochondrial stress and GDF15 effects may be a novel avenue for IBD. The persistence of permeability in IBD remission suggests a window for barrier-stabilizing interventions to prevent relapse. For metabolic syndrome, nutritional interventions addressing micronutrient deficiencies like vitamin A could indirectly support barrier function. Future research should prioritize the development and standardization of robust permeability biomarkers and the translation of pathway insights into targeted, disease-modifying therapies.
Conventional randomized clinical trials (RCTs), while considered the gold standard for generating clinical evidence, present significant logistical, ethical, and financial challenges, especially when studying small patient populations or complex diseases. These challenges have catalyzed the development of innovative methodological approaches that can generate robust evidence more efficiently. Externally Controlled Trials (ECTs) and Adaptive Trial Designs represent two powerful paradigms that address these constraints. ECTs can serve as a viable alternative in settings where RCTs are unfeasible, by comparing a group of subjects receiving the test treatment with a group of patients external to the study, rather than an internal control group [137]. Meanwhile, adaptive designs are "studies that include a prospectively planned opportunity for modification of one or more specified aspects of the study design and hypotheses based on analysis of (usually interim) data" [138]. When framed within research on tissue permeability—a field requiring sophisticated assessment of biomarker transport and exchange across biological barriers—these innovative designs enable more nuanced and efficient investigation of therapeutic effects, particularly in specialized or limited patient cohorts.
Externally Controlled Trials (ECTs): Leveraging Existing Data
Design Principles and Rationale
The fundamental principle of an ECT is the use of existing data to construct a control group for comparison with a prospectively enrolled treatment group, typically from a single-arm trial. This approach is particularly valuable in situations where randomization is impractical or unethical, such as in oncology, rare diseases, or conditions with high unmet medical need [137]. The US Food and Drug Administration (FDA) guidance documents acknowledge that the use of external controls is acceptable when internal controls are not feasible or ethical in certain circumstances [137]. The international Conference on Harmonization E10 guidance formally defines an ECT as a trial that "compares a group of subjects receiving the test treatment with a group of patients external to the study, rather than to an internal control group consisting of patients from the same population assigned to a different treatment" [137].
Current Methodological Practice and Gaps
A recent cross-sectional analysis of 180 ECTs published between 2010 and 2023 revealed several critical methodological shortcomings in current practice, limiting the reliability and credibility of many studies [137]. The analysis identified suboptimal practices across the design, conduct, and analysis of ECTs. The table below summarizes key quantitative findings from this analysis:
Table 1: Methodological Characteristics of 180 Published ECTs (2010-2023)
| Methodological Characteristic | Frequency | Percentage |
|---|---|---|
| Studies focused on oncology | 85 | 47.2% |
| Provided rationale for using external controls | 64 | 35.6% |
| Prespecified use of external controls in protocol | 29 | 16.1% |
| Conducted feasibility assessments of data sources | 14 | 7.8% |
| Specified handling of missing data in external controls | 13 | 7.2% |
| Used statistical methods to adjust for covariates | 60 | 33.3% |
| Performed sensitivity analyses for primary outcomes | 32 | 17.8% |
| Performed quantitative bias analyses | 2 | 1.1% |
Furthermore, the main sources of external controls were clinical (real-world) data (54.4%) and trial-derived controls (37.2%), while concurrent data collection with the treatment arm was relatively infrequent (10.0%) [137]. Among studies that used statistical adjustment, the propensity score method was the most common (58.3% of adjusted studies) [137]. These findings highlight a significant gap between methodological recommendations and their application, underscoring the need for more rigorous standards.
Experimental Protocol: Designing a Rigorous ECT
For researchers designing an ECT, the following protocol outlines key steps to minimize bias and enhance validity.
Step 1: Justify and Prespecify
- Action: Provide a clear rationale for why an ECT is necessary and why an RCT is not feasible. Prespecify the use of the external control and all analysis plans in the trial protocol and statistical analysis plan before treatment initiation [137].
- Rationale: This prevents data-driven, post-hoc decisions that inflate type I error.
Step 2: Select and Assess Data Source
- Action: Identify a potential source for the external control (e.g., historical clinical trial data, high-quality real-world data from registries). Conduct a feasibility assessment to evaluate the suitability of this data. This involves comparing the population, eligibility criteria, endpoint definitions, and data quality with the planned single-arm trial [137].
- Rationale: Ensures the external control group is fit-for-purpose and sufficiently comparable to the treatment group at baseline.
Step 3: Design and Analyze with Rigor
- Action: Use appropriate statistical methods, such as propensity score matching or weighting, to adjust for baseline imbalances between the treatment and external control arms. The specific covariates for adjustment should be selected a priori based on clinical knowledge and their known relationship with the outcome [137].
- Rationale: Statistical adjustment helps to reduce confounding bias, a major threat to validity in non-randomized studies.
Step 4: Validate with Sensitivity Analysis
- Action: Plan and execute comprehensive sensitivity analyses for the primary outcome. This tests the robustness of the findings to different assumptions and methods (e.g., different matching algorithms, inclusion of unmeasured confounding). Consider quantitative bias analysis to quantify the potential impact of residual confounding [137].
- Rationale: Sensitivity analyses assess how much the conclusions depend on specific methodological choices and strengthen the credibility of the results.
Adaptive Trial Designs: Building Flexibility into Clinical Development
Core Concepts and Classification
Adaptive clinical trial designs are flexible frameworks that allow for preplanned modifications to the trial based on interim analyses of accumulating data, without undermining the trial's scientific validity and integrity [138]. These designs contrast with traditional fixed designs, which specify all aspects (e.g., sample size, treatment arms) upfront and do not change after the trial commences [138]. The core principle is prospectively planned flexibility, which distinguishes it from ad hoc data dredging.
Table 2: Comparison of Traditional Fixed Trials and Adaptive Trial Designs
| Feature | Traditional Fixed Trial | Adaptive Trial |
|---|---|---|
| Trial Course | Fixed design; no changes after start | Prespecified interim analyses allow design changes |
| Sample Size | Set in advance; no changes | Can be re-estimated during the trial |
| Flexibility | Rigid and inflexible by design | Built-in flexibility to respond to accumulating data |
| Efficiency | Can be inefficient, with fixed resource allocation | Often more efficient; may require fewer patients |
| Ethics | May continue giving inferior treatments | Can reduce patient exposure to ineffective treatments |
| Complexity | Relatively straightforward | Statistically and operationally complex |
Types of Adaptive Designs
The landscape of adaptive designs is diverse, with different designs serving different purposes across the drug development continuum. The 2019 FDA guidance outlines several major adaptive design elements [139]:
- Group Sequential Designs: Allow for one or more prospectively planned interim analyses with prespecified criteria for stopping the trial early for efficacy, futility, or harm [139]. This is one of the most established and widely used adaptive designs.
- Sample Size Re-Estimation (SSR): Accounts for uncertainty in the assumed treatment effect by using accumulated data at an interim analysis to re-estimate the sample size needed to maintain prespecified power [139]. This can be done with the treatment assignment blinded or unblinded.
- Adaptive Enrichment: Allows the trial to adapt the patient population based on interim results, for instance, by focusing recruitment on a biomarker-defined subgroup that shows a stronger treatment response [139].
- Adaptations to Treatment Arm Selection: Enables the modification of treatment arms during the trial, such as dropping arms for futility or efficacy, or adding new arms based on emerging external evidence. This is common in platform trials, umbrella trials, and basket trials [139].
- Adaptive Randomization: Modifies the randomization probabilities to allocate more patients to the treatment arms that are showing better performance based on interim outcomes (response-adaptive randomization) or to achieve balance in baseline covariates (covariate-adaptive randomization) [139].
Experimental Protocol: Implementing a Bayesian Adaptive Platform Trial
Platform trials represent a sophisticated application of adaptive design, evaluating multiple interventions simultaneously under a master protocol. The I-SPY 2 trial in neoadjuvant breast cancer is a canonical example [140].
Step 1: Define the Master Protocol
- Action: Develop a single, overarching protocol that defines the common procedures, eligible patient population (often with biomarker strata), control arm, and the adaptive rules for the entire platform. New interventions can be added and inferior ones removed as the trial progresses [140] [139].
- Rationale: A master protocol creates an efficient, persistent infrastructure for evaluating multiple questions, as opposed to multiple standalone trials.
Step 2: Establish a Bayesian Statistical Model
- Action: Implement a Bayesian model that will update the probability of each treatment's success as patient outcome data accumulates. The model will use predictive probabilities to forecast the likelihood that a given treatment will prove superior at the final analysis [140].
- Rationale: The Bayesian framework is naturally suited for continuous learning and probabilistic decision-making throughout the trial.
Step 3: Set Adaptive Decision Rules
- Action: Prespecify decision rules based on the Bayesian model outputs. For example:
- Graduation: A treatment shows a high predictive probability of success in a specific biomarker signature and "graduates" to a confirmatory phase III trial.
- Dropping: A treatment shows a low predictive probability of success and is dropped from the platform for futility.
- Randomization: Allocate new patients adaptively, with higher probabilities of being assigned to treatments performing well in their biomarker signature [140].
- Rationale: These rules ensure the trial dynamically allocates resources to the most promising therapies.
- Action: Prespecify decision rules based on the Bayesian model outputs. For example:
Step 4: Conduct Extensive Simulation
- Action: Before the trial begins, conduct thousands of computer simulations under various scenarios (e.g., null effect, strong effect) to validate the operating characteristics of the design, including type I error rate and power [140].
- Rationale: Simulation is critical for understanding the behavior of a complex adaptive design and is a requirement for regulatory review.
Integration with Tissue Permeability Research
The Role of Permeability Assessment
In the context of WISH background research, the study of tissue permeability—particularly intestinal and capillary permeability—is crucial for understanding disease mechanisms and treatment effects. The "leaky gut," or increased intestinal permeability, is implicated in a range of gastrointestinal and non-gastrointestinal diseases, as it may allow the translocation of luminal antigens into the bloodstream, potentially triggering immune responses [141] [142]. Similarly, assessing capillary permeability is vital for understanding nutrient exchange and vascular function in tissues like the heart [143].
Methodologies for Assessing Permeability
- In Vivo Permeability Probes: A common method involves administering probe molecules, such as sugar complexes (e.g., lactulose/mannitol test), and measuring their excretion in urine or appearance in blood. This primarily assesses the paracellular pathway [141] [142].
- Ex Vivo Ussing Chambers: This is considered the gold standard for assessing epithelial barrier function. Tissue samples are mounted in chambers that measure the short-circuit current and the flux of marker molecules across the epithelium, providing a direct functional readout of permeability [141] [142].
- Circulating and Fecal Biomarkers: Biomarkers like zonulin (a regulator of tight junctions), intestinal fatty acid-binding protein (I-FABP), and lipopolysaccharides (LPS) can be measured in blood or stool as indirect indicators of barrier integrity and permeability [141] [142].
Incorporating Permeability Endpoints into Innovative Trials
Adaptive designs and ECTs are exceptionally well-suited for trials where permeability is a key biomarker or endpoint. In an adaptive trial for a drug intended to reduce intestinal permeability in a rare disease, an interim analysis could use early permeability data (e.g., from a biomarker like zonulin) to inform decisions. For example, the trial could adapt to enrich the population with patients showing high baseline permeability, or it could drop treatment arms that fail to show a signal of normalizing permeability. In an ECT for the same drug, the treatment arm's effect on permeability could be compared against the natural history of permeability changes derived from a highly characterized historical cohort, provided rigorous statistical adjustment is applied.
The diagram below illustrates a conceptual workflow integrating permeability assessment into an adaptive trial framework.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Research Reagent Solutions for Permeability and Trial Research
| Item | Function/Application |
|---|---|
| Lactulose/Mannitol Test Kit | A non-invasive in vivo probe for assessing paracellular intestinal permeability via urinary excretion measurement [141]. |
| Fluorescent Dextran Probes | Sized molecules (e.g., 4kDa, 10kDa, 70kDa FITC-Dextran) used to assess permeability in vivo (tail vein injection in mice) or ex vivo in Ussing chambers [143]. |
| ELISA Kits for Zonulin | Quantifies levels of circulating zonulin, a protein that modulates intestinal tight junctions, serving as a blood-based permeability biomarker [141] [142]. |
| Lipopolysaccharide (LPS) Assay | Measures circulating endotoxin levels (e.g., via LAL test), indicating bacterial translocation due to increased intestinal permeability [142]. |
| Ussing Chamber System | An ex vivo apparatus that is the gold standard for direct, functional measurement of ionic current and macromolecular flux across a tissue membrane [141] [142]. |
| Statistical Software (R, SAS) | Essential for complex analyses like propensity score matching (for ECTs) and Bayesian modeling/simulations (for adaptive designs) [137] [140]. |
Regulatory and Statistical Considerations
The regulatory environment for innovative trial designs is evolving. The FDA has issued final guidance on adaptive designs (2019) and is currently collaborating internationally on the ICH E20 guideline for adaptive clinical trials, a draft of which was released for comment in September 2025 [144] [139]. For ECTs, the FDA has recognized the risk of biases such as confounding, selection bias, and survivor-lead-time bias, and has provided recommendations to sponsors to mitigate these risks [137].
From a statistical perspective, controlling the type I error rate (the chance of a false positive) is a paramount concern in confirmatory adaptive trials and requires advanced techniques like alpha-spending functions [139]. The use of extensive simulation is considered essential to understand the operating characteristics of a complex design and to demonstrate control of error rates to regulators [140]. Furthermore, prospective planning and total transparency (e.g., pre-registering the protocol and analysis plan) are non-negotiable for maintaining the scientific integrity and regulatory acceptability of both adaptive trials and ECTs [137] [138].
Adaptive protocols and externally controlled trials represent a paradigm shift towards more patient-centric, efficient, and informative clinical research. While they introduce operational and statistical complexity, their potential benefits in accelerating drug development for small populations—such as those characterized by specific tissue permeability pathologies—are substantial. Success hinges on rigorous prospective planning, robust methodology including comprehensive simulation for adaptive designs and diligent bias control for ECTs, and early and continuous dialogue with regulatory agencies. As these innovative designs continue to mature through experience and harmonized guidance, they are poised to play an increasingly central role in the future of clinical investigation.
Conclusion
Tissue permeability represents a fundamental biological process with profound implications for health, disease pathogenesis, and therapeutic development. The integration of advanced assessment methodologies with a deeper understanding of molecular regulators provides unprecedented opportunities for targeting barrier dysfunction across multiple disease states. Future research directions should focus on developing standardized, validated biomarkers for clinical use, elucidating tissue-specific regulatory mechanisms, and leveraging innovative trial designs to accelerate the development of permeability-modulating therapies. As our comprehension of barrier function evolves, so too will our ability to design precision interventions that restore physiological permeability for improved patient outcomes across gastrointestinal, neurological, and metabolic disorders.
References
- 1. Methods to assess tissue permeability [https://pubmed.ncbi.nlm.nih.gov/23955735/]
- 2. Editorial: Molecular mechanisms of lung endothelial ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.976873/full]
- 3. Probing paracellular -versus transcellular tissue barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6592590/]
- 4. Artificial Intelligence-Based Quantitative Structure–Property ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10155205/]
- 5. Best practices in current models mimicking drug ... [https://www.sciencedirect.com/science/article/pii/S0928098721003997]
- 6. Tissue Barriers: Introducing an exciting new journal - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5008708/]
- 7. Membrane Transport w/Selective Permeability*# [https://bio.libretexts.org/Under_Construction/Purgatory/Core_(Britt's_page)/Membrane_Transport_w%2F%2FSelective_Permeability*%23]
- 8. Pharmacokinetics and tissue distribution analysis of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1582644/full]
- 9. A Method for Determination and Simulation of Permeability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5931342/]
- 10. Paracellular transport [https://en.wikipedia.org/wiki/Paracellular_transport]
- 11. Paracellular Transport - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/paracellular-transport]
- 12. Transcellular - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/transcellular]
- 13. Transcellular Transport - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/transcellular-transport]
- 14. Transcellular – Knowledge and References [https://taylorandfrancis.com/knowledge/Medicine_and_healthcare/Physiology/Transcellular/]
- 15. Modulation of Paracellular-like Drug Transport across an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9027509/]
- 16. Para- and Transcellular Transport Kinetics of Nanoparticles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10923144/]
- 17. Assessment of drug permeability using a small airway ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1621775/full]
- 18. Exploring claudin proteins: from sequence motifs to their ... [https://link.springer.com/article/10.1007/s00726-025-03479-w]
- 19. Tight Junction Proteins at the Crossroads of Inflammation, ... [https://www.mdpi.com/1422-0067/26/17/8115]
- 20. The Role of Intestinal Mucosal Barrier in Autoimmune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.871713/full]
- 21. Tight junction proteins occludin and ZO-1 as regulators of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9427709/]
- 22. Alterations in intestinal permeability - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1856434/]
- 23. Target specific tight junction modulators [https://www.sciencedirect.com/science/article/pii/S0169409X21000429]
- 24. Diagnostic study of serum claudin-3 and zonulin for intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620425/]
- 25. Diagnostic study of serum claudin-3 and zonulin for ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1669630/full]
- 26. Occludin, Claudin-2 and Zonulin as Biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11478261/]
- 27. Regulation of claudin/zonula occludens-1 complexes by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4962485/]
- 28. Intestinal barrier permeability: the influence of gut ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2024.1380713/full]
- 29. Intestinal Permeability, Inflammation and the Role of Nutrients [https://pmc.ncbi.nlm.nih.gov/articles/PMC7231157/]
- 30. How Does the Immune System Enter the Brain? [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.805657/full]
- 31. Nutrient Absorption - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/nutrient-absorption]
- 32. Tissue-resident immune cells: from defining characteristics ... [https://www.nature.com/articles/s41392-024-02050-5]
- 33. Immunosurveillance as a regulator of tissue homeostasis [https://www.sciencedirect.com/science/article/abs/pii/S1471490613000963]
- 34. Tissue Homeostasis, Inflammation, and Repair - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK582256/]
- 35. Permeability of technical and biological tissues - PubMed [https://pubmed.ncbi.nlm.nih.gov/19713609/]
- 36. Human Small Intestinal Tissue Models to Assess Barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384003/]
- 37. Intestinal permeability and its relation to anthropometric ... [https://www.nature.com/articles/s41598-025-08045-8]
- 38. Regulation of blood vascular permeability in the skin - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5725833/]
- 39. Tissue differences in vascular permeability changes ... [https://www.sciencedirect.com/science/article/pii/0026286285900597]
- 40. Vascular recanalization exacerbates BBB permeability ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1682748/full]
- 41. Transdermal Drug Delivery Systems: Methods for Enhancing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300492/]
- 42. Review article Transdermal drug delivery system [https://www.sciencedirect.com/science/article/pii/S2352952025000143]
- 43. Claudin 5 Across the Vascular Landscape: From Blood-Tissue ... [https://pubmed.ncbi.nlm.nih.gov/40940757/]
- 44. Progress in the application of molecular imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11996769/]
- 45. Molecular imaging using (nano)probes - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03927d]
- 46. Crafting molecular probes for multimodal imaging intended ... [https://www.sciencedirect.com/science/article/pii/S0926669025012051]
- 47. Choosing a Tracer—Section 14.1 [https://www.thermofisher.com/us/en/home/references/molecular-probes-the-handbook/fluorescent-tracers-of-cell-morphology-and-fluid-flow/choosing-a-tracer.html]
- 48. Types of Fluorescence Imaging [https://www.licorbio.com/blog/types-of-fluorescence-imaging]
- 49. Fluorescence Live Cell Imaging - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4198327/]
- 50. Single tracer-based protocol for broad-spectrum kinase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8449129/]
- 51. The Ussing chamber system for measuring intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6585111/]
- 52. Aryl hydrocarbon receptor utilises cellular zinc signals to ... [https://www.nature.com/articles/s41467-023-41168-y]
- 53. The epithelial barrier: a Janus-faced regulator in allergic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631285/]
- 54. How the Ussing Chamber System Accelerates Epithelial ... [https://physiologicinstruments.com/blogs/news/how-the-ussing-chamber-system-accelerates-epithelial-research?srsltid=AfmBOopchAvZRkXqyNAFV7VYy7E0be7JNjFg08SXC-6zzKsZ1RlhvENi]
- 55. Epithelial Transport Explained – Ussing Chamber Research [https://physiologicinstruments.com/blogs/news/epithelial-transport-explained-ussing-chamber-research?srsltid=AfmBOopZHdzIK6NNS1yOZ_NSANRDeFy9cS3yrpUa0f9rXAbe8azaMTTT]
- 56. Ussing Chambers & Drug Absorption Studies - [https://ussingchamber.com/ussing-chambers-drug-absorption-studies/]
- 57. Ex vivo intestinal permeability assay (X-IPA) for tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10318059/]
- 58. HAX1, gene responsible for Kostmann syndrome ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1624718/full]
- 59. Assessing Intestinal Health. In Vitro and Ex vivo Gut Barrier ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2021.723387/full]
- 60. DNA Barcoding 101: Definition, Steps & How It Works [https://www.cd-genomics.com/pop-genomics/pop-genomics/resources/dna-barcoding-overview.html]
- 61. DNA barcodes for biosecurity: invasive species identification [https://pmc.ncbi.nlm.nih.gov/articles/PMC1609225/]
- 62. Delimiting Species—Prospects and Challenges for DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11842946/]
- 63. Next-generation DNA barcoding [https://pmc.ncbi.nlm.nih.gov/articles/PMC4276293/]
- 64. Environmental DNA metabarcoding for catchment-scale ... [https://www.sciencedirect.com/science/article/pii/S1470160X25008738]
- 65. Intestinal Permeability and its Regulation by Zonulin [https://pmc.ncbi.nlm.nih.gov/articles/PMC3458511/]
- 66. The Intestinal Barrier and Current Techniques for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7463717/]
- 67. Intestinal Permeability and Depression—A Narrative Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563369/]
- 68. The Relation of Zonulin And Intestinal Fatty Acid Binding ... [https://www.cpn.or.kr/view.html?uid=1853&vmd=Full]
- 69. 腹部手术åŽè¡€æ¸…Claudin-3å’ŒZonulinæ°´å¹³æ£€æµ‹åœ¨è¯„ä¼°è‚ é“ ... [https://www.ebiotrade.com/newsf/2025-11/20251104000157765.htm]
- 70. Predictive Potential of Biomarkers of Intestinal Barrier ... [https://pubmed.ncbi.nlm.nih.gov/37836505/]
- 71. Peer Review History - Research journals - PLOS [https://journals.plos.org/plosone/article/peerReview?id=10.1371/journal.pone.0294918]
- 72. A 3D microfluidic model for preclinical drug permeation ... [https://www.sciencedirect.com/science/article/abs/pii/S073170852500528X]
- 73. Application of Method Suitability for Drug Permeability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2976984/]
- 74. In Vitro Oral Cavity Permeability Assessment to Enable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298201/]
- 75. Predicting skin permeability using HuskinDB - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9508232/]
- 76. Methods for Measuring Permeability - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK54124/]
- 77. Predicting permeability via statistical learning on higher- ... [https://www.nature.com/articles/s41598-020-72085-5]
- 78. Psychosocial stress-induced intestinal permeability in healthy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10569989/]
- 79. Stressed to the Core: Inflammation and Intestinal Permeability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10867428/]
- 80. Inflammatory responses and inflammation-associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5805548/]
- 81. Can Diet Alter the Intestinal Barrier Permeability in Healthy ... [https://pubmed.ncbi.nlm.nih.gov/38931225/]
- 82. Intestinal Permeability, Inflammation and the Role of Nutrients - PubMed [https://pubmed.ncbi.nlm.nih.gov/32340206/]
- 83. TASTY trial: protocol for a study on the triad of nutrition ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-025-01089-6]
- 84. a network meta-analysis of 15 interventions [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1668590/full]
- 85. Intestinal permeability is associated with aggravated ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1173481/full]
- 86. Analysis of Bottlenecks in Experimental Models of Infection [https://pmc.ncbi.nlm.nih.gov/articles/PMC4465827/]
- 87. Effects of plant tissue permeability on invasion and population ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10762237/]
- 88. Effects of plant tissue permeability on invasion and ... [https://pure.psu.edu/en/publications/effects-of-plant-tissue-permeability-on-invasion-and-population-b/]
- 89. Role of host genetic diversity for susceptibility-to-infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6863064/]
- 90. Trends in mathematical modeling of host–pathogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7010650/]
- 91. Uncovering the diversity of pathogenic invaders [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1374438/full]
- 92. Zonulin and its regulation of intestinal barrier function - PubMed [https://pubmed.ncbi.nlm.nih.gov/21248165/]
- 93. Intestinal Barrier Function: Molecular Regulation and Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4266989/]
- 94. Energy metabolism and the intestinal barrier: implications ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1515364/full]
- 95. Larazotide Acetate Protects the Intestinal Mucosal Barrier from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561949/]
- 96. Regulation of Vascular Endothelial Barrier Integrity and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK597461/]
- 97. Intestinal barrier function as a key determinant of inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446253/]
- 98. Increased Intestinal Permeability and Decreased Barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5988153/]
- 99. Intestinal barrier permeability: the influence of gut microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11260943/]
- 100. Microbiome-based therapeutics towards healthier aging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220006/]
- 101. The microbiota–gut–brain axis: pathways to better ... [https://link.springer.com/article/10.1007/s00018-021-04060-w]
- 102. Intestinal permeability: symptoms and causes - Synlab [https://www.synlab-sd.com/en/blog/health-and-wellness-en/intestinal-permeability-everything-you-need-to-know-about-the-root-of-many-diseases/]
- 103. Unveiling the role of functional foods with emphasis on ... [https://www.sciencedirect.com/science/article/pii/S1756464624003396]
- 104. Advancements in the investigation of gut microbiota-based ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1533343/full]
- 105. Exploring the microbiota-gut-brain axis: impact on ... [https://www.frontiersin.org/journals/neuroanatomy/articles/10.3389/fnana.2025.1504065/full]
- 106. Advances in Oral Drug Delivery [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.618411/full]
- 107. The effects of three absorption-modifying critical excipients ... [https://pubmed.ncbi.nlm.nih.gov/29758344/]
- 108. Excipients: Innovation in a Shifting Pharma Landscape [https://drug-dev.com/special-feature-excipients-innovation-in-a-shifting-pharma-landscape/]
- 109. Effects of pharmaceutical excipients on membrane ... [https://pubmed.ncbi.nlm.nih.gov/23742974/]
- 110. The role of excipients in promoting topical and transdermal ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2022.1049848/full]
- 111. A Strategic Guide to Risk Mitigation in Drug Development ... [https://www.drugpatentwatch.com/blog/a-strategic-guide-to-risk-mitigation-in-drug-development-using-excipient-exclusion/?srsltid=AfmBOopwuChyr8pX2VrsNxOeOsXaPceThTwnKIWdBrjdrvncJdaPrREN]
- 112. FDA Advances Rare Disease Drug Development with New ... [https://www.fda.gov/news-events/press-announcements/fda-advances-rare-disease-drug-development-new-evidence-principles]
- 113. FDA's New “Plausible Mechanism Pathway†and Other ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-plausible-mechanism-pathway-and-other-initiatives-drugs-for-ultra-rare-conditions]
- 114. Development and functional characterization of a tissue ... [https://pubmed.ncbi.nlm.nih.gov/40878769/]
- 115. CDER/CBER Rare Disease Evidence Principles (RDEP) [https://www.fda.gov/industry/fda-rare-disease-innovation-hub/cdercber-rare-disease-evidence-principles-rdep]
- 116. FDA Rare Disease Evidence Principles (RDEP) 2025 [https://www.allucent.com/resources/blog/fda-rare-disease-evidence-principles-rdep]
- 117. FDA Outlines “Plausible Mechanism†Approval Pathway for ... [https://www.ropesgray.com/en/insights/alerts/2025/11/fda-outlines-plausible-mechanism-approval-pathway-for-personalized-therapies-but-significant]
- 118. FDA Leaders Propose New Regulatory Pathway for ... [https://www.aabb.org/news-resources/news/article/2025/11/19/fda-leaders-propose-new-regulatory-pathway-for-bespoke-therapies]
- 119. FDA announces “plausible mechanism†approval pathway ... [https://www.hoganlovells.com/en/publications/fda-announces-plausible-mechanism-approval-pathway-for-certain-personalized-therapies-with-few-detai]
- 120. A translational model for in vivo intestinal permeability ... [https://www.sciencedirect.com/science/article/abs/pii/S0022316625005577]
- 121. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 122. Reinforcing gut integrity: A systematic review and meta- ... [https://www.sciencedirect.com/science/article/pii/S1043661825002051]
- 123. Permeability Benchmarking: Guidelines for Comparing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11815851/]
- 124. Coeliac disease and the intestinal barrier: mechanisms of ... [https://pubmed.ncbi.nlm.nih.gov/40579122/]
- 125. Intestinal permeability in coeliac disease: insight into ... [https://pubmed.ncbi.nlm.nih.gov/21890812/]
- 126. A randomized, double-blind study of larazotide acetate to prevent the activation of celiac disease during gluten challenge - PubMed [https://pubmed.ncbi.nlm.nih.gov/22825365/]
- 127. Larazotide Acetate Protects the Intestinal Mucosal Barrier from Anoxia/Reoxygenation Injury via Various Cellular Mechanisms [https://www.mdpi.com/2227-9059/13/10/2483]
- 128. The Roles of WNT Signaling Pathways in Skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10741662/]
- 129. Wnt/β-catenin signalling: function, biological mechanisms ... [https://www.nature.com/articles/s41392-021-00762-6]
- 130. The Investigation of Nutritional Status, Intestinal Permeability, and Quality of Life in People with Celiac Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9797792/]
- 131. Intestinal permeability assessment using lactulose and mannitol in celiac disease - ScienceDirect [https://www.sciencedirect.com/science/chapter/bookseries/abs/pii/S0091679X22001868]
- 132. Comparing intestinal barrier function in patients with ... [https://www.mayoclinic.org/medical-professionals/digestive-diseases/news/comparing-intestinal-barrier-function-in-patients-with-crohns-disease-or-ulcerative-colitis-and-healthy-controls/mac-20589041]
- 133. Growth differentiation factor 15 alters intestinal barrier and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620814/]
- 134. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity | BMC Medicine | Full Text [https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-9-23]
- 135. The association between 24-hour urinary biomarkers and ... [https://www.nature.com/articles/s41598-025-21246-5]
- 136. Biomarkers of intestinal permeability in major psychiatric ... [https://www.sciencedirect.com/science/article/pii/S0278584625001599]
- 137. Design, Conduct, and Analysis of Externally Controlled Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411980/]
- 138. Adaptive Trial Design: A Guide to Flexible Clinical Trials [https://intuitionlabs.ai/articles/adaptive-clinical-trial-design]
- 139. Recent innovations in adaptive trial designs: A review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10260347/]
- 140. Statistical innovations in clinical trial design with a focus on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627888/]
- 141. Fecal and Circulating Biomarkers for the Non-Invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10253128/]
- 142. The Role of Intestinal Permeability in Gastrointestinal ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.717925/full]
- 143. Assessment of permeability in deep tissue capillaries using ... [https://pubmed.ncbi.nlm.nih.gov/41142454/]
- 144. E20 Adaptive Designs for Clinical Trials September 2025 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e20-adaptive-designs-clinical-trials]