A Stepwise Monolayer Protocol for Kidney Organoid Differentiation: Applications in Disease Modeling and Drug Development
This article provides a comprehensive guide to the stepwise monolayer protocol for differentiating human pluripotent stem cells into kidney organoids.
A Stepwise Monolayer Protocol for Kidney Organoid Differentiation: Applications in Disease Modeling and Drug Development
Abstract
This article provides a comprehensive guide to the stepwise monolayer protocol for differentiating human pluripotent stem cells into kidney organoids. Tailored for researchers and drug development professionals, it covers the foundational principles of kidney development that inform the protocol, detailed methodological steps, and key applications in disease modeling and nephrotoxicity screening. It further addresses common challenges and optimization strategies, including novel approaches to enhance differentiation efficiency and reduce off-target cells. Finally, it explores validation techniques using single-cell transcriptomics and comparative analyses with other differentiation methods, offering a holistic resource for implementing and advancing this powerful in vitro model system.
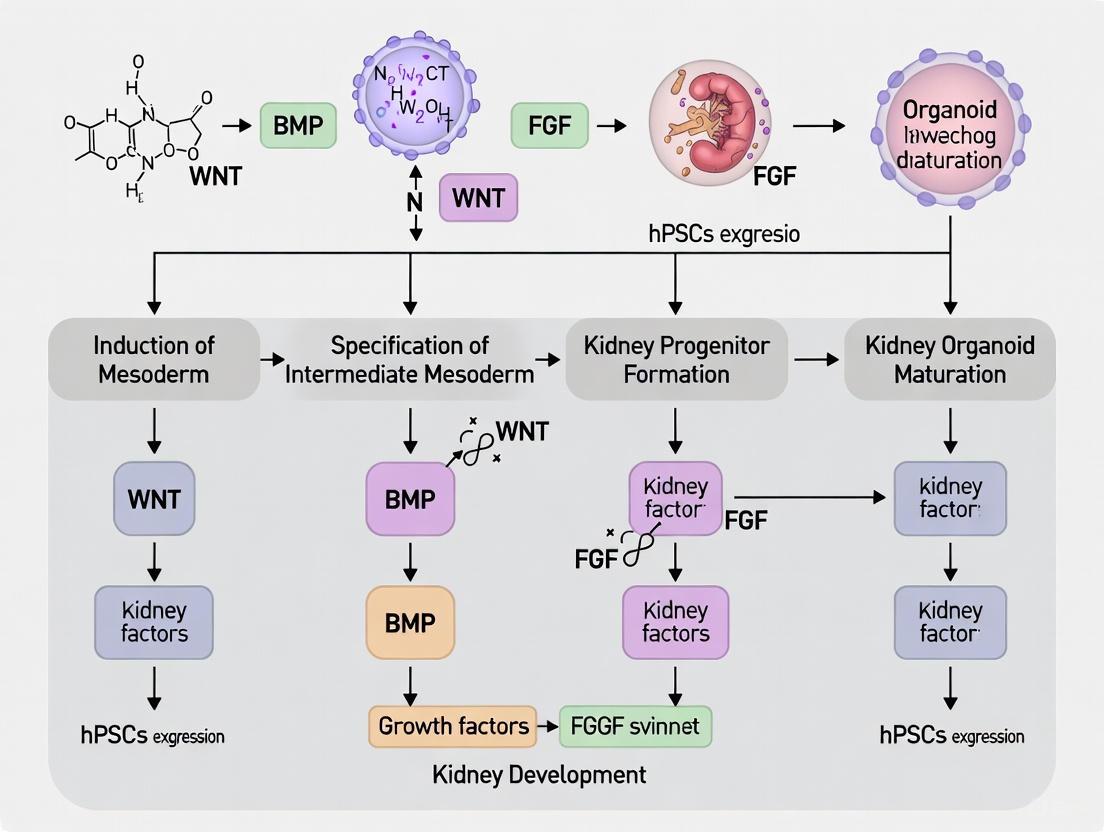
The Blueprint of the Kidney: How Developmental Biology Informs Organoid Differentiation
The in vitro differentiation of pluripotent stem cells (PSCs) into kidney organoids requires the precise recapitulation of embryonic developmental stages. This process initiates with the formation of the primitive streak, which gives rise to the three germ layers, followed by the specification of the intermediate mesoderm (IM)—the embryonic precursor to the entire urogenital system [1] [2]. The IM subsequently patterns into the metanephric mesenchyme and ureteric bud, which through reciprocal signaling, generate the complex architecture of the kidney [2]. Mastering the trajectory from primitive streak to IM is therefore a critical, foundational step in protocols for generating kidney organoids for disease modeling, drug screening, and regenerative medicine [1] [2]. This Application Note details the key signaling pathways, provides a optimized, quantitative protocol, and lists essential reagents for the efficient and reproducible derivation of IM from human induced pluripotent stem cells (hiPSCs) in a monolayer culture system.
Key Signaling Pathways in Mesoderm Patterning
The stepwise differentiation from pluripotency to IM is orchestrated by the precise modulation of several conserved signaling pathways, primarily Nodal, WNT, and BMP [1]. The role of these pathways is hierarchical and concentration-dependent.
Nodal Signaling: Nodal, a member of the TGF-β superfamily, is fundamental for mesendoderm formation. Conventional models posit a morphogen gradient where high Nodal activity promotes definitive endoderm, while lower activity specifies mesoderm [1]. Recent protocol optimizations suggest that suppressing Nodal signaling during the mesoderm induction step can enhance the fidelity of IM differentiation [1].
WNT Signaling: WNT signaling is indispensable for the initial induction of the primitive streak and the subsequent formation of mesoderm progenitors [1] [2]. The GSK3β inhibitor CHIR99021 is commonly used to activate canonical WNT signaling. Its concentration and duration of application must be carefully optimized, as it also plays a role in maintaining posterior mesodermal progenitors [1].
BMP Signaling: Bone Morphogenetic Protein (BMP) signaling acts as a critical patterning cue. During IM specification, lower levels of BMP activity favor IM fate, while higher levels drive cells toward lateral plate mesoderm [1]. The concentration of BMP4 is therefore a key variable in protocol efficiency.
The following diagram illustrates the sequential activation and interaction of these pathways during the transition from pluripotent stem cells to intermediate mesoderm.
Quantitative Comparison of Published IM Induction Protocols
Substantial variability exists in published protocols for generating IM cells from hiPSCs, particularly in the choice of morphogens, small molecules, and their concentrations [1]. The table below summarizes and compares key parameters from several established methods, highlighting the optimized condition.
Table 1: Comparison of Intermediate Mesoderm Induction Protocols
| Protocol Reference | Primitive Streak / Mesoderm Induction (~48-96h) | Intermediate Mesoderm Induction (~48-72h) | Key IM Markers Analyzed |
|---|---|---|---|
| Optimized Protocol [1] | 3 μM CHIR99021 | 3 μM CHIR99021 + 4 ng/mL BMP4 | OSR1, GATA3, PAX2 |
| Yucer et al., 2017 [1] | 100 ng/mL Activin A + 3 μM CHIR99021 | 100 ng/mL BMP4 + 3 μM CHIR99021 | OSR1, GATA3, PAX2 |
| Knarston et al., 2020 [1] | 3 μM CHIR99021 (96h) | 10 ng/mL BMP4 + 1 μg/mL Heparin + 200 ng/mL FGF9 (72h) | OSR1, LHX1, PAX2 |
| Bejoy et al., 2022 [1] | 100 ng/mL Activin A + 3 μM CHIR99021 | 8 μM CHIR99021 (72h) | PAX8 |
| Gong et al., 2022 [1] | 5 μM CHIR99021 (36h) | 100 ng/mL bFGF + 10 nM Retinoic Acid (72h) | OSR1, PAX2, LHX1 |
The optimized protocol featured in this note demonstrates that a simplified, reproducible system using 3 μM CHIR99021 for mesoderm progenitor induction, followed by a combination of 3 μM CHIR99021 and a low concentration of BMP4 (4 ng/mL) for IM specification, efficiently generates cells expressing the canonical IM marker triad: OSR1, GATA3, and PAX2 [1]. This protocol effectively suppresses high Nodal signaling during the mesoderm step, which more faithfully recapitulates in vivo molecular features [1].
Stepwise Monolayer Protocol for IM Differentiation
This section provides a detailed methodology for the efficient and reproducible differentiation of hiPSCs into IM cells, adapted from the optimized protocol [1].
Materials and Pre-Culture Preparation
- hiPSC Line: UCSD167i-99-1 (or a well-characterated alternative) [1].
- Base Medium: mTeSR1 or mTeSR Plus medium [1].
- Matrigel: hPSC-qualified Matrigel for coating culture vessels [1].
- Small Molecules and Growth Factors:
- CHIR99021 (Tocris), reconstituted in DMSO.
- Recombinant Human BMP4 (R&D Systems), reconstituted as per manufacturer's instructions.
- Equipment: Standard humidified cell culture incubator (37°C, 5% CO2), 6-well Nunclon Delta surface plates [1].
Pre-Culture Preparation: Maintain hiPSCs in an undifferentiated state in feeder-free conditions on Matrigel-coated plates in mTeSR1 or mTeSR Plus medium. Culture medium should be replaced daily, and cells should be passaged every 4-6 days at a confluence of 70-80% using a gentle cell dissociation reagent. Ensure cells have a high viability and show no signs of spontaneous differentiation before starting the protocol [1].
Detailed Differentiation Procedure
Day 0: Mesoderm Induction Initiation
- Passage hiPSCs as a single-cell suspension and seed them onto a Matrigel-coated 6-well plate at an optimized density (e.g., 0.5 x 10^6 cells per well) in mTeSR Plus medium supplemented with a ROCK inhibitor (e.g., Y-27632).
- Allow cells to attach for 24 hours. The target confluency at the start of differentiation should be approximately 90-95%.
Day 1-2: Primitive Streak / Mesoderm Progenitor Specification
- Aspirate the mTeSR Plus medium and replace it with fresh medium containing 3 μM CHIR99021.
- Incubate the cells for 48 hours. During this period, cells should undergo morphological changes and rapidly proliferate, transitioning into TBXT+/MIXL1+ mesoderm progenitors [1].
Day 3-4: Intermediate Mesoderm Specification
- On the morning of Day 3, carefully aspirate the medium containing CHIR99021.
- Replace it with fresh medium supplemented with 3 μM CHIR99021 and 4 ng/mL BMP4.
- Incubate the cells for a further 48 hours [1].
Day 5: Harvest and Analysis
- By Day 5, the cells are ready for harvest and analysis. The differentiated population should express key IM markers (OSR1, GATA3, PAX2) as confirmed by RT-qPCR and immunofluorescence staining [1].
Expected Outcomes and Quality Control
- Morphology: Cells will transition from compact, pluripotent colonies to a more uniform, proliferative monolayer with a distinct mesenchymal appearance.
- Molecular Characterization: Successful differentiation should be confirmed by analyzing the expression of marker genes.
- Downregulation: Pluripotency markers (OCT3/4, NANOG).
- Upregulation: Mesoderm progenitor markers (TBXT, MIXL1) followed by intermediate mesoderm markers (OSR1, GATA3, PAX2).
- Immunofluorescence: Staining should reveal nuclear expression of OSR1, GATA3, and PAX2 proteins in a high percentage of the cell population.
The following diagram provides a simplified overview of this experimental workflow.
The Scientist's Toolkit: Essential Research Reagents
A robust and reproducible differentiation protocol relies on high-quality, well-defined reagents. The table below lists the essential materials required for the successful execution of the IM differentiation protocol described herein.
Table 2: Key Research Reagent Solutions for IM Differentiation
| Item | Function / Role in Protocol | Example / Source |
|---|---|---|
| CHIR99021 | A GSK3β inhibitor that activates canonical WNT signaling. Critical for inducing primitive streak and mesoderm progenitors, and for maintaining posterior mesoderm during IM specification. [1] | Tocris Bioscience |
| Recombinant Human BMP4 | A morphogen belonging to the TGF-β family. Used at low concentration to pattern mesoderm progenitors towards an intermediate mesoderm fate. [1] | R&D Systems |
| mTeSR1 / Plus Medium | A defined, serum-free culture medium optimized for the maintenance and growth of human pluripotent stem cells. Serves as the base medium for the differentiation protocol. [1] | StemCell Technologies |
| hPSC-qualified Matrigel | A basement membrane matrix extracted from mouse tumors. Used to coat culture vessels to provide a substrate that supports the attachment and growth of hiPSCs in a feeder-free system. [1] | Corning |
| Anti-OSR1 / GATA3 / PAX2 Antibodies | Validated antibodies for immunofluorescence staining and flow cytometry. Essential for the molecular characterization and validation of successfully differentiated IM cells. [1] | Various suppliers (e.g., Abcam, R&D Systems) |
Troubleshooting and Protocol Validation
Common challenges during IM differentiation include low efficiency, high cell death, and contamination with off-target cell types. Low efficiency can often be attributed to suboptimal hiPSC quality or passage number; therefore, starting with healthy, high-viability cultures is paramount. Inconsistent WNT activation due to improper CHIR99021 reconstitution or storage can also lead to poor outcomes. High cell death during the initial days can be mitigated by using a ROCK inhibitor during cell passaging and ensuring gentle medium changes.
To validate a successful differentiation, researchers should employ a multi-faceted approach:
- RT-qPCR: Confirm the downregulation of pluripotency markers (OCT4, NANOG) and the sequential upregulation of TBXT/MIXL1 (mesoderm) followed by OSR1, GATA3, and PAX2 (IM) [1].
- Immunofluorescence: Demonstrate protein-level co-expression of OSR1, GATA3, and PAX2 in a significant proportion of the cell population [1].
- Flow Cytometry: If specific antibodies are available, quantify the percentage of cells positive for IM markers to provide a quantitative measure of protocol efficiency and reproducibility.
For advanced quality control, single-cell RNA sequencing (scRNA-seq) can be employed to comprehensively assess the transcriptional profile of the differentiated population and identify any contaminating off-target cell types. Computational tools like DevKidCC, a classifier trained on human fetal kidney data, can be used to robustly assign cell identity in scRNA-seq datasets and benchmark in vitro-derived IM cells against their in vivo counterparts [3].
The development of the mammalian kidney is orchestrated by a complex, sequential interplay of signaling pathways that guide the differentiation of pluripotent stem cells into specialized renal structures. Understanding the precise roles of WNT, FGF, and BMP signaling is crucial for advancing kidney organoid research, particularly in the context of stepwise monolayer differentiation protocols. These pathways regulate key developmental processes including progenitor cell maintenance, mesenchymal-to-epithelial transition (MET), and nephron patterning [2]. Recapitulating these signaling events in vitro has enabled the generation of kidney organoids from human pluripotent stem cells (hPSCs), providing powerful models for studying renal development, disease modeling, and drug screening [4] [2]. This application note details the specific roles and experimental manipulation of these pathways in renal patterning, with a focus on practical protocols for kidney organoid differentiation.
Pathway Mechanisms and Functions
WNT Signaling Pathway
The WNT signaling pathway is a phylogenetically conserved system crucial for kidney development, functioning through both canonical (β-catenin-dependent) and non-canonical branches [5] [6]. The canonical pathway initiates when WNT ligands bind to Frizzled (Fzd) receptors and LRP5/6 co-receptors, disrupting the β-catenin destruction complex (comprising Axin, APC, GSK3β, and CK1α). This stabilization allows β-catenin to accumulate and translocate to the nucleus, where it associates with TCF/LEF transcription factors to activate target genes governing cell fate, proliferation, and differentiation [5]. In contrast, non-canonical pathways (WNT/PCP and WNT/Ca²⁺) regulate cell polarity and migration independently of β-catenin [5].
During kidney development, WNT signaling plays multiple, stage-specific roles. WNT9b and WNT4 are particularly vital for nephron formation, with WNT9b from the ureteric bud inducing nephron progenitor cells in the metanephric mesenchyme, and WNT4 driving the subsequent mesenchymal-to-epithelial transition (MET) to form renal vesicles [6] [2]. The pathway's activity must be precisely controlled, as its dysregulation is implicated in kidney disease and fibrosis, wherein sustained activation promotes a reactive process leading to functional decline [7] [6].
FGF Signaling Pathway
The Fibroblast Growth Factor (FGF) signaling pathway is fundamental to kidney development, primarily regulating survival, proliferation, and branching morphogenesis. Signaling is initiated when FGF ligands bind to FGF receptors (FGFRs), triggering receptor dimerization and autophosphorylation. This activates downstream cascades, including the MAPK/ERK, PI3K/AKT, and PLCγ pathways, which coordinate cellular responses such as proliferation, differentiation, and survival [8].
In the developing kidney, FGF signaling exhibits distinct spatial and functional roles. FGF9 and FGF8 are particularly crucial; FGF9, often combined with heparin, supports the survival and maintenance of nephron progenitor cells in the metanephric mesenchyme [4] [2]. Meanwhile, FGF8 promotes the differentiation of these progenitors into renal vesicles [2]. Furthermore, FGF signaling, in concert with GDNF from the metanephric mesenchyme, promotes the repetitive branching of the ureteric bud, which is essential for forming the collecting duct system [2]. In urine-derived renal progenitor cells, FGF2 drives the TGFβ-SMAD2/3 pathway to maintain self-renewal, highlighting its role in progenitor cell maintenance [8].
BMP Signaling Pathway
The Bone Morphogenetic Protein (BMP) pathway, a subset of the TGFβ superfamily, signals through serine/threonine kinase receptors and intracellular SMAD transcription factors (primarily SMAD1/5/8). Ligand binding induces receptor complex formation, phosphorylating SMADs which then complex with SMAD4 and translocate to the nucleus to regulate target gene expression [2].
BMPs are critical for early kidney development, with BMP7 playing a particularly prominent role. It promotes the survival and proliferation of metanephric mesenchyme and nephron progenitor cells, preventing apoptosis [2] [7]. Beyond survival, BMP signaling also influences nephron patterning and segmentation. In adult-derived rat kidney stem cells, BMP7 is part of a defined cocktail that enables self-organization into 3D tubular organoids [2]. The pathway's activity is finely balanced, as it crosstalks with other key pathways like WNT and FGF to coordinate overall kidney morphogenesis.
Table 1: Key Signaling Pathways in Renal Patterning
| Pathway | Key Ligands | Receptors/Components | Primary Functions in Kidney Development |
|---|---|---|---|
| WNT | WNT9b, WNT4, WNT11 | Frizzled, LRP5/6, β-catenin, GSK3β | Nephron progenitor induction, MET, tubulogenesis, axis patterning [6] [2] |
| FGF | FGF9, FGF8, FGF2 | FGFR1-4, Heparin | Nephron progenitor maintenance, UB branching, cell survival, proliferation [8] [2] |
| BMP | BMP7, BMP4 | BMPR1/2, SMAD1/5/8 | Metanephric mesenchyme survival, proliferation, nephron patterning [2] |
Experimental Protocols for Kidney Organoid Differentiation
Stepwise Monolayer Protocol for Kidney Organoid Differentiation
The generation of kidney organoids via a stepwise monolayer protocol efficiently recapitulates kidney development by directing hPSCs through intermediate mesoderm and metanephric mesenchyme stages. The following protocol, adapted from Morizane et al. and subsequent refinements, is designed for a 24-well plate format [9] [4].
Days -4 to -1: Intermediate Mesoderm Induction
- Seed hPS cells at 1–2 × 10^5 viable cells per well on vitronectin-coated 24-well plates in Essential 8 medium.
- The next day (designated day -4), replace the medium with Advanced RPMI 1640 containing 8 μM CHIR99021 (a GSK3β inhibitor that activates WNT signaling).
- Incubate for 3 days, changing the CHIR99021 medium daily, to induce primitive streak and posterior intermediate mesoderm fates.
Day -1: Metanephric Mesenchyme Patterning
- Replace the medium with Advanced RPMI 1640 containing 200 ng/mL FGF9 and 1 μg/mL heparin. Some protocols include 10 ng/mL Activin A at this stage [4].
- Incubate for 24 hours to pattern the cells toward a metanephric mesenchyme identity.
Day 0: 3D Aggregation and Nephron Induction
- On day 0, treat the monolayer cultures with 5 μM CHIR99021 for 1 hour while maintaining FGF9 and heparin.
- Dissociate the cells into single cells and seed them in V-bottom 96-well plates to promote 3D spheroid formation. Cell seeding numbers can be optimized (e.g., 500 to 250,000 cells/well) to influence final organoid composition [4].
- Maintain the 3D spheroids in free-floating culture with continued FGF9 and heparin until day 7 to promote renal vesicle formation.
Days 7-16: Maturation
- From day 7 onwards, culture the organoids in basal medium without growth factors to allow spontaneous differentiation and maturation into various nephron segments [4].
- The organoids should develop visible glomerular-like (PODXL+/WT1+) and tubular-like (LTL+/ECAD+) structures by day 16.
Protocol for Generating Proximal-Biased Kidney Organoids
Recent advances enable the generation of proximal-biased kidney organoids with enhanced maturation of proximal tubule cells, which are crucial for modeling renal reabsorption and nephrotoxicity [10].
- Follow the standard stepwise monolayer protocol through the 3D aggregation stage (Days -4 to 0).
- During early nephrogenesis (e.g., days 1-3 post-aggregation), add a PI3K inhibitor (e.g., LY294002) to the culture medium. This manipulation activates Notch signaling, shifting nephron axial differentiation toward proximal tubule fates.
- Continue culture until maturation (up to day 16). These proximal-biased organoids will exhibit expanded populations of HNF4A⁺/HNF1B⁺ proximal tubule precursor cells and show higher expression of solute carriers (e.g., organic cation and anion transporters). They demonstrate improved functional responses to nephrotoxic injury, including upregulation of injury markers KIM1/HAVCR1 and SOX9, and downregulation of HNF4A [10].
Table 2: Essential Research Reagents for Kidney Organoid Differentiation
| Reagent Category | Specific Examples | Function/Application | Typical Working Concentration |
|---|---|---|---|
| WNT Pathway Agonists | CHIR99021 | GSK3β inhibitor; activates canonical WNT signaling to induce mesoderm and nephron progenitors [4] | 5-8 μM [4] |
| FGF Signaling Ligands | FGF9, FGF2, FGF8 | Maintains nephron progenitors; promotes UB branching and differentiation [8] [2] | 200 ng/mL [4] |
| BMP Signaling Ligands | BMP7, BMP4 | Supports survival and proliferation of metanephric mesenchyme [2] | Protocol-dependent |
| Enzymatic Dissociation Reagents | Trypsin/EDTA, Accutase | Dissociates monolayer cells for 3D aggregation into spheroids | Cell line-specific |
| Extracellular Matrix | Vitronectin, Matrigel | Provides substrate for monolayer culture and cell attachment | Manufacturer-recommended |
| Basal Media | Advanced RPMI 1640, Essential 8 | Base medium for differentiation and pluripotency maintenance | N/A |
| Signaling Inhibitors | PI3K inhibitors (e.g., LY294002) | Shifts differentiation toward proximal tubule fates in specific protocols [10] | Protocol-dependent |
The precise manipulation of WNT, FGF, and BMP signaling pathways is fundamental to generating kidney organoids that faithfully recapitulate human renal development. The protocols detailed herein provide a foundation for the stepwise differentiation of hPSCs into kidney organoids with emerging cellular complexity and function. Current research focuses on enhancing the maturation and vascularization of these organoids, reducing batch-to-batch variability, and achieving more complete nephron segmentation. Future directions include the integration of these organoids with microfluidic systems to create organ-on-a-chip models, which will further improve their physiological relevance and utility in disease modeling and drug nephrotoxicity screening [2]. As the field progresses, the continued refinement of these signaling manipulations will be paramount for realizing the full translational potential of kidney organoids in regenerative medicine.
Nephron progenitor cells (NPCs) represent a foundational population in kidney development, responsible for generating all the epithelial cells of the nephron, the functional unit of the kidney [11]. These self-renewing cells balance proliferation with differentiation during organogenesis, with their availability being a major determinant of final nephron number at birth [12]. In recent years, the field has made significant advances in deriving induced nephron progenitor-like cells (iNPCs) from human pluripotent stem cells (hPSCs), creating powerful platforms for studying human kidney development, disease modeling, and drug screening [11] [2]. This Application Note details current protocols and mechanistic insights for the efficient generation, expansion, and differentiation of NPCs within the context of kidney organoid research, providing researchers with practical methodologies for leveraging these cells in renal studies.
Nephron Progenitor Cell Fundamentals
NPCs, also known as cap mesenchyme, reside in a specialized niche during kidney development where they receive signals from the ureteric bud and surrounding stroma [12]. They are characterized by the expression of key transcription factors including SIX2, WT1, PAX2, OSR1, and CITED1 [12] [2]. The balance between NPC self-renewal and differentiation is tightly regulated by both signaling pathways and metabolic processes.
- Developmental Significance: NPCs undergo mesenchymal-to-epithelial transition (MET) to form all nephron segments except the collecting duct [2]. Their gradual recruitment into forming nephrons follows a stereotyped developmental program [10].
- Metabolic Regulation: Young NPCs (embryonic day 13.5 in mice) demonstrate significantly higher glycolytic flux compared to older NPCs (postnatal day 0), with this high glycolysis rate supporting self-renewal, while inhibition of glycolysis stimulates differentiation [12].
- Transcriptional Control: SIX2 acts as a master regulator maintaining the progenitor state, while a Cited1+/Six2+ subpopulation remains refractory to differentiation signals compared to Cited1-/Six2+ cells that are poised to differentiate [12].
Protocols for NPC Generation and Differentiation
Expansion of hPSC-Derived Induced Nephron Progenitor Cells
Recent protocols have enabled the purification and expansion of hPSC-derived induced nephron progenitor-like cells (iNPCs) in monolayer culture [11].
Table 1: Key Reagents for iNPC Expansion and Differentiation
| Reagent Category | Specific Components | Function | Protocol Reference |
|---|---|---|---|
| Pluripotency Maintenance | mTeSRplus medium, Geltrex | Maintains hiPSCs in primed pluripotent state | [13] |
| Initial Differentiation | CHIR99021 (GSK3β inhibitor) | Activates WNT signaling; induces posterior primitive streak | [4] |
| Progenitor Patterning | FGF9, Heparin, Activin A | Patterns cells toward intermediate mesoderm | [4] |
| iNPC Expansion Medium | Chemically defined "hNPSR-v2" | Supports long-term iNPC self-renewal and expansion | [11] |
| Nephron Differentiation | Air-liquid interface culture | Promotes 3D nephron organoid formation from iNPCs | [11] |
Stepwise Protocol:
- hPSC Culture: Maintain hiPSCs in essential 8 medium on vitronectin-coated plates [4].
- Primitive Streak Induction: Treat with 8μM CHIR99021 in Advanced RPMI 1640 for 3 days [4].
- Intermediate Mesoderm Commitment: Switch to media containing 200ng/ml FGF9, 1μg/ml heparin, and 10ng/ml activin A for 24 hours [4].
- iNPC Expansion: Purify and expand iNPCs in specialized hNPSR-v2 medium in monolayer culture [11].
- Nephron Organoid Differentiation: Transfer iNPCs to air-liquid interface culture for 21 days to generate nephron organoids with enhanced podocyte maturity and minimal off-target cell types [11].
DMSO Pre-conditioning for Enhanced Differentiation
Pre-treatment of hiPSCs with low-dose dimethyl sulfoxide (DMSO) enhances subsequent kidney organoid differentiation efficiency [9] [13].
Protocol Details:
- Pre-treatment: Culture hiPSCs in mTeSRplus medium supplemented with 1-2% DMSO for 24 hours prior to differentiation induction [13].
- Mechanism: DMSO alters the expression of pluripotency transcription factors, modifies the epigenetic landscape, and affects colony morphology, priming cells for more efficient differentiation [13].
- Outcome: Treated cells show enhanced expression of the key nephron progenitor marker SIX2 after 9 days of kidney organoid differentiation and improved tubular organoid development [9].
Generating Proximal-Biased Kidney Organoids
Controlling nephron precursor differentiation toward proximal tubule lineages creates organoids with enhanced functionality for disease modeling and toxicity testing [10].
Key Intervention:
- Transient PI3K inhibition during early nephrogenesis activates Notch signaling, shifting nephron axial differentiation toward proximal precursor states [10].
- This protocol generates HNF4A+ proximal tubule precursors that mature to express solute carriers including organic cation and organic anion transporters [10].
- These "proximal-biased" organoids demonstrate improved physiological function and better mimic in vivo injury responses to nephrotoxic compounds [10].
Signaling Pathways Regulating NPC Fate
The balance between NPC self-renewal and differentiation is governed by an intricate network of signaling pathways and metabolic processes.
Table 2: Metabolic and Signaling Regulation of NPC Fate
| Regulatory Mechanism | Effect on NPCs | Experimental Evidence |
|---|---|---|
| High Glycolytic Flux | Supports self-renewal; younger NPCs have 30% higher ATP levels | Inhibition with YN1 (5-25μM) enhances nephrogenesis in cultured embryonic kidneys [12] |
| FGF/PI3K/Akt Signaling | Maintains progenitor state and proliferation | Inhibition decreases glycolytic flux and promotes differentiation [12] |
| Notch Signaling | Promotes proximal tubule specification | Activated by PI3K inhibition; drives HNF4A+ proximal precursor formation [10] |
| WNT/β-catenin | Regulates balance between self-renewal and differentiation | Required for NPC maintenance and MET induction [2] |
Applications and Validation Models
Nephrotoxicity and Disease Modeling
Kidney organoids derived from NPCs have been widely applied for modeling genetic kidney diseases, nephrotoxicity screening, and studying disease mechanisms [2].
- Cisplatin Toxicity Modeling: Chimeric nephrons generated from progenitor cells demonstrate dose-dependent increases in kidney injury molecule-1 (KIM1/HAVCR1) expression in proximal tubule cells upon cisplatin exposure, mirroring in vivo injury responses [14].
- Genetic Disease Modeling: Organoids enable study of polycystic kidney disease, congenital anomalies of the kidney and urinary tract, and other genetic disorders using patient-specific iPSCs [2].
- Functional Assessment: Mature organoids exhibit filtration and reabsorption capabilities, with systemically administered fluorescent dextran observed around podocytes and on apical surfaces of proximal tubule cells [14].
In Vivo Integration Models
Neonatal niche injection represents a promising approach for generating long-term viable chimeric nephrons with host urinary tract integration [14].
Protocol Overview:
- Donor Cell Preparation: Isolate renal progenitor cells from E14.5 fetal mice or differentiate from hiPSCs [14].
- Host Preparation: Expose kidneys of neonatal (P0.5-P1.5) mice through a small back incision [14].
- Cell Injection: Inject donor cells under the renal capsule using a 34G Hamilton syringe [14].
- Integration Assessment: Donor cells integrate into host cap mesenchyme within 2 days and form chimeric glomeruli and tubules within 2 weeks [14].
This method achieves 85% survival rate with P1.5 neonates and generates chimeric nephrons that remain viable for over 4 months, with functional filtration and reabsorption capacity [14].
Research Reagent Solutions
Table 3: Essential Research Reagents for NPC Studies
| Reagent/Cell Line | Specification | Application | Reference |
|---|---|---|---|
| hiPSC Lines | LUMCi004-C (female, urine-derived); TISSUi001-A (male, PBMC) | Protocol optimization and differentiation studies | [13] |
| CHIR99021 | 5-8μM in Advanced RPMI 1640 | GSK3β inhibitor for WNT activation and primitive streak induction | [4] |
| FGF9 | 200ng/ml with 1μg/ml heparin | Intermediate mesoderm patterning and nephron progenitor maintenance | [4] |
| DMSO | 1-2% in mTeSRplus for 24h | hiPSC pre-conditioning for enhanced differentiation efficiency | [9] [13] |
| hNPSR-v2 Medium | Chemically defined formulation | Expansion and maintenance of hPSC-derived iNPCs in monolayer | [11] |
| Y-27632 | 10μM | ROCK inhibitor for improving cell survival after passaging | [13] |
NPCs serve as the fundamental building blocks for nephron formation, both in development and in engineered kidney organoids. The protocols detailed in this Application Note provide researchers with robust methodologies for generating, expanding, and differentiating these cells into kidney structures with enhanced maturity and functionality. Recent advances in metabolic conditioning, signaling manipulation, and in vivo integration models have significantly improved the physiological relevance of NPC-derived tissues. As the field continues to evolve, further refinement of these protocols will enable more precise modeling of kidney diseases, more accurate nephrotoxicity screening, and ultimately, progress toward regenerative therapies for kidney disease.
Cellular Composition of a Mature Kidney Organoid
Within the field of regenerative nephrology, the generation of kidney organoids from human pluripotent stem cells (hPSCs) represents a transformative approach for modeling development, disease, and drug response. A critical benchmark for the success of this technology is the achievement of a mature cellular composition that closely mirrors the complexity of the native kidney. This Application Note details the characteristic cellular makeup of a mature kidney organoid, provides a detailed protocol for its generation via a stepwise monolayer method, and outlines essential quality control measures to validate organoid fidelity for research and drug development applications.
Cellular Census of a Mature Kidney Organoid
A mature kidney organoid is a complex, multi-lineage structure. Single-cell RNA sequencing (scRNA-seq) has been instrumental in providing a high-resolution census of the cell types present, revealing both on-target renal cells and common off-target populations.
Table 1: Characteristic Cellular Composition of a Mature hPSC-Derived Kidney Organoid
| Cell Type | Key Marker Genes | Approximate Frequency in D29 Organoids | Functional & Structural Characteristics |
|---|---|---|---|
| Podocyte-like | NPHS1, NPHS2, WT1, PODXL, SYNPO |
14–29% [15] [16] | Forms glomerular-like structures with immature foot processes and apico-basal polarity [17]. |
| Proximal Tubule-like | LTL, LRP2, SLC3A1, CUBN |
Varies by protocol [15] | Exhibits functional uptake capabilities (e.g., albumin endocytosis); expresses injury markers like KIM1 [2] [17]. |
| Distal Tubule-like | ECAD, SLC12A1, GATA3 |
Varies by protocol [15] [16] | Includes thick ascending limb (TAL) characteristics; distinct distal convoluted tubule (DCT) segment is often absent [16]. |
| Nephron Progenitor-like | SIX2, PAX2, OSR1, CITED1 |
Present [9] [16] | Population of progenitor cells maintained in an undifferentiated state, supporting ongoing nephrogenesis. |
| Stromal/Interstitial-like | FOXD1, PDGFRβ, SULT1E1, DKK1 |
Present (Multiple subsets) [4] [16] | Includes mesenchymal, fibroblast, and pericyte-like populations. |
| Endothelial-like | CD31, PECAM1 |
Rare (Sparse and unorganized) [2] [16] | Observed within organoids but typically requires co-culture or in vivo transplantation for maturation and organization. |
| Collecting Duct-like | AQP2, ECAD, GATA3 |
Typically absent unless co-differentiated [18] | Not generated in standard protocols; requires integration of ureteric bud (UB) progenitors for formation [18]. |
| Off-Target Non-Renal | SOX2, STMN2 (Neuronal), MYOG (Muscle), PMEL (Melanocyte) |
10–21% [15] [16] | Undesired cell types reflecting incomplete lineage specification; can be reduced through protocol refinement or transplantation [16]. |
The maturity and transcriptional profile of these organoid cell types are most similar to first and second-trimester human fetal kidney, highlighting an opportunity for further maturation [15] [16]. A key structural limitation of most protocols is the absence of a functional collecting system, though recent advances in co-culturing nephron progenitors with ureteric bud progenitors have successfully generated organoids with integrated, patent collecting ducts [18].
Experimental Protocol: Stepwise Monolayer Differentiation
The following detailed protocol, adapted from established methods [4], directs the differentiation of hPSCs into kidney organoids with a mature cellular composition.
Materials and Reagents
Table 2: Essential Research Reagent Solutions for Kidney Organoid Differentiation
| Reagent | Function in Protocol | Key Signaling Pathway Modulated |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor; induces primitive streak and posterior intermediate mesoderm. | WNT Activation [4] [2] |
| FGF9 | Supports survival and expansion of nephron progenitor populations. | FGF Signaling [4] [2] |
| Heparin | Co-factor that enhances FGF signaling activity. | FGF Signaling [4] |
| Activin A | Contributes to mesoderm patterning and induction. | TGF-β Signaling [4] |
| Vitronectin | Extracellular matrix coating for monolayer cell culture. | Cell Adhesion & Survival |
| Advanced RPMI 1640 | Basal medium for the initial differentiation phases. | N/A |
Step-by-Step Procedure
Part 1: Monolayer Differentiation to Posterior Intermediate Mesoderm (Days -4 to 0)
- Day -4: Seed hPSCs as a monolayer on vitronectin-coated plates in Essential 8 medium.
- Days -4 to -1: Induce primitive streak and IM commitment by replacing the medium with Advanced RPMI 1640 containing 8 µM CHIR99021. Incubate for 72 hours.
- Days -1 to 0: Pattern the IM by treating with Advanced RPMI 1640 containing 200 ng/mL FGF9 and 1 µg/mL heparin. Some protocols also include 10 ng/mL Activin A at this stage [4]. Incubate for 24 hours.
The following diagram illustrates the key signaling pathway interactions during this initial differentiation phase:
Part 2: 3D Spheroid Aggregation and Organoid Maturation (Days 0 to 16)
- Day 0: Pre-treat the PIM-committed monolayer cultures with 5 µM CHIR99021 for 1 hour while maintaining FGF9 and heparin.
- Dissociate the cells into a single-cell suspension.
- Aggregation: Seed the cells into a low-adhesion U-bottom 96-well plate to promote 3D spheroid formation. The number of cells per spheroid (e.g., 8,000) influences the final organoid composition and maturity, with lower numbers often promoting more differentiated structures [4].
- Days 0 to 7: Culture the 3D spheroids in free-floating conditions in medium containing FGF9 and heparin to promote renal vesicle formation.
- Days 7 to 16: Withdraw growth factors to allow for spontaneous differentiation into segmented nephron structures. Maintain organoids in free-floating culture with regular medium changes.
The overall workflow from monolayer to mature organoid is summarized below:
Quality Control and Validation
Rigorous validation of the final organoid's cellular composition is essential for ensuring experimental reproducibility and relevance.
- scRNA-seq Census: Profiling a representative organoid batch via scRNA-seq is the gold standard for comprehensively identifying all cell types, their proportions, and transcriptional maturity compared to human fetal and adult kidney datasets [15] [16].
- Immunofluorescence Confirmation: Validate the presence and spatial organization of key structures using confocal microscopy with antibodies against markers listed in Table 1 (e.g., PODXL for podocytes, LTL for proximal tubules) [4] [2].
- Functional Assays:
- Refinement Strategies: To improve organoid quality:
- Inhibit Off-Target Cells: Adding inhibitors of specific pathways, such as the BDNF-NTRK2 pathway, can reduce neuronal off-target cells by up to 90% without affecting kidney differentiation [15].
- Transplantation: Transplanting organoids under the mouse kidney capsule enhances maturation and vascularization while diminishing off-target cell populations [16].
- Bioengineering: Integration with microfluidic organ-on-chip platforms can improve physiological relevance and maturation through enhanced nutrient delivery and mechanical cues [19] [20].
A Practical Guide to the Stepwise Monolayer Protocol and Its Research Applications
Kidney organoids are three-dimensional (3D) in vitro structures derived from human pluripotent stem cells (hPSCs), including both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs). These miniaturized organ models recapitulate key aspects of kidney development, architecture, and function, providing an unprecedented platform for studying renal development, disease modeling, drug screening, and regenerative medicine [21] [2]. The technology has evolved significantly since initial protocols were established in 2014-2015, with current methods enabling generation of organoids containing segmented nephron-like structures including glomerular, proximal tubule, loop of Henle, and distal tubule components [21] [2].
The fundamental principle underlying kidney organoid generation involves stepwise recapitulation of embryonic kidney development in vitro. During mammalian development, the kidney arises from the intermediate mesoderm through reciprocal interactions between two key embryonic progenitors: the metanephric mesenchyme (MM), which gives rise to nephrons, and the ureteric bud (UB), which forms the collecting system [2]. Current differentiation protocols mimic these developmental stages by precisely timing the activation and inhibition of key signaling pathways to direct hPSCs through primitive streak, intermediate mesoderm, and nephron progenitor stages before final maturation into 3D renal tissues [4] [21] [2].
Key Differentiation Protocols
Established Methodologies
Several core protocols form the foundation of kidney organoid generation, each with distinct advantages and limitations. The table below summarizes the principal established methodologies:
Table 1: Comparison of Major Kidney Organoid Differentiation Protocols
| Protocol | Cell Source | Key Signaling Factors | Efficiency of NPC Generation | Organoid Components | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Taguchi et al. [21] | Mouse ESC/hiPSCs | BMP4, Activin A, FGF2, CHIR99021, FGF9, Retinoic acid | ~62% SIX2+ NPCs | Wt1/nephrin+ glomeruli; cadherin6+ proximal tubules; E-cadherin+ distal tubules | Pioneering method for kidney reconstruction in vitro | Requires mouse embryonic spinal cord coculture; lower efficiency; immature structures |
| Morizane et al. [21] [2] | hESCs/hiPSCs | CHIR99021, Activin A, FGF9 | 80-90% SIX2+ NPCs | Multi-segmented nephrons: podocytes, proximal tubules, loops of Henle, distal tubules | Chemically defined medium; high efficiency; no coculture required | Line-to-line variability; no collecting duct system |
| Freedman et al. [21] | hESCs/hiPSCs | CHIR99021 (GSK3β inhibition only) | Not specified | Segmented nephrons with proximal tubules, podocytes, endothelial cells | Simple, low-cost, high-throughput; no FGF2/Activin/BMP | Random organoid size; non-uniform; off-target cells |
| Little's Team [21] | iPSC/hESC | CHIR99021, FGF9 | Not specified | 6-10 nephrons surrounded by endothelial and stromal populations | High cell yield (3-4x static culture); cost-effective | Immature structures |
Recent Protocol Advancements
Recent innovations have addressed several limitations of earlier methods. Scalable production approaches now enable the generation of kidney organoids from hPSCs using a reproducible and affordable system that allows differentiation into different renal cell types. This method forces cell-to-cell contact by generating 3D spheroids through self-aggregation of varying numbers of posterior intermediate mesoderm (PIM)-committed cells (from 500 to 250,000 cells), resulting in organoids with different extents of differentiation and cellular composition [4]. Single-cell RNA sequencing analysis has confirmed that this approach generates organoids containing renal endothelial-like, mesenchymal-like, proliferating, podocyte-like, and tubule-like cell populations across all tested conditions [4].
Another significant advancement addresses the integration of collecting systems. A persistent limitation of most kidney organoid protocols has been the absence of collecting ducts, which are essential for establishing a structural mechanism for distal drainage of fluid from nephrons. A recent breakthrough describes an efficient hPSC co-culture system that assembles UB progenitors with nephrogenic mesenchyme to form a network of collecting ducts structurally integrated with nephrons via fusion with the distal tubule [18]. This integration creates organoids with the most representative distribution of nephron segments, including collecting ducts, yet described, achieving a higher state of maturation across all segments [18].
Additionally, pretreatment strategies to enhance differentiation efficiency have emerged. Treatment of hiPSCs with low-dose dimethyl sulfoxide (DMSO) prior to kidney organoid differentiation using the Morizane stepwise 2D monolayer-based protocol enhances the expression of the key metanephric mesenchyme nephron progenitor marker SIX2 and improves differentiation protocol efficiency toward tubular kidney organoids [9].
Stepwise Monolayer to 3D Culture Protocol
Detailed Workflow
The following diagram illustrates the complete workflow for generating 3D kidney organoids from hPSCs, integrating multiple established protocols:
Stage-Specific Protocol Details
Stage 1: hPSC Culture and Cavitated Spheroid Formation (Days -3 to 0)
Begin with high-quality hPSCs maintained in mTeSR1 medium on Matrigel-coated plates. On Day -3, dissociate cells using ACCUTASE and seed as single cells at 30,000 cells/well in a 6-well plate in mTeSR1 supplemented with CloneR2 (1:10 dilution). After 24 hours (Day -2), overlay cells with cold mTeSR1 containing Matrigel (0.25 mg/mL protein concentration) and incubate for 24 hours. On Day -1, perform a full medium change to mTeSR1 without Matrigel. By Day 0, hPSC colonies should form round, cavitated spheroids of 50-100 µm in size [22].
Stage 2: Primitive Streak and Intermediate Mesoderm Induction (Days 0-4)
On Day 0, initiate differentiation by replacing mTeSR1 with Stage 1 Medium (STEMdiff Kidney Basal Medium + Supplement SG) or Advanced RPMI 1640 with 8 µM CHIR99021. Incubate for 36-40 hours to induce primitive streak formation. On Day 1.5, replace with Stage 2 Medium (STEMdiff Kidney Basal Medium + Supplement DM) or Advanced RPMI 1640 with 200 ng/mL FGF9, 1 µg/mL heparin, and 10 ng/mL activin A. Culture for 2 days, then refresh with fresh Stage 2 Medium and culture for an additional 3 days to promote intermediate mesoderm and early nephron progenitor formation [4] [22].
Stage 3: Nephron Progenitor Expansion (Days 4-7)
Maintain cells in Stage 2 Medium with FGF9 signaling to support nephron progenitor cell expansion. During this period, cells should express key nephron progenitor markers including SIX2, SALl1, WT1, and PAX2. Efficiency of nephron progenitor generation typically reaches 80-90% with optimized protocols [21] [2].
Stage 4: 3D Aggregation and Organoid Maturation (Days 7-16)
On Day 7, dissociate nephron progenitor cell monolayers using ACCUTASE or TrypLE Express Enzyme and aggregate into 3D spheroids. For the scalable approach, seed dissociated single cells in V-bottom 96-well plates to generate 3D spheroids by self-aggregation of 500-250,000 PIM-committed cells per well [4]. Alternatively, use AggreWell plates to generate organoids of uniform size by seeding 5,000 viable cells per microwell [22]. Maintain 3D spheroids in free-floating conditions in differentiation medium without growth factors for organoid maturation until Day 16. During this period, nephron-like structures segment into glomerular, proximal tubule, distal tubule, and loop of Henle compartments [4].
Signaling Pathways in Kidney Organoid Differentiation
The stepwise differentiation of hPSCs into kidney organoids requires precise temporal activation and inhibition of key developmental signaling pathways. The following diagram illustrates the critical pathways and their roles:
Pathway Functions and Temporal Regulation
WNT/β-catenin signaling serves as the master regulator initiating kidney organoid differentiation. Transient activation using GSK3β inhibitors such as CHIR99021 drives hPSCs toward posterior primitive streak identity, representing the first critical step in renal lineage specification. Subsequent moderate WNT signaling supports intermediate mesoderm formation and later stages of nephrogenesis, demonstrating the pathway's stage-dependent functions [2].
FGF signaling, particularly through FGF9, plays multiple essential roles throughout the differentiation process. Following primitive streak induction, FGF9 promotes patterning of the intermediate mesoderm and subsequently supports maintenance and expansion of nephron progenitor populations. Continued FGF signaling is essential for the formation of renal vesicles and the transition to epithelial structures [4] [2].
BMP signaling contributes to kidney organoid differentiation in a stage-specific manner. Early BMP signaling, particularly with BMP4, supports mesodermal induction, while later BMP7 exposure promotes metanephric mesenchyme survival and proliferation. The precise timing and concentration of BMP exposure must be carefully controlled to avoid off-target effects [21] [2].
Retinoic acid (RA) signaling contributes to anterior-posterior patterning of the intermediate mesoderm, helping to specify the metanephric kidney region versus other intermediate mesoderm derivatives. RA signaling typically occurs during intermediate mesoderm patterning stages in specific protocols [21].
Notch signaling plays a crucial role in nephron segmentation during later organoid maturation stages. This pathway influences the fate specification of different nephron segments, including proximal tubules, distal tubules, and podocytes, ensuring appropriate cellular diversity within the organoid [2].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Reagents for Kidney Organoid Differentiation
| Category | Specific Reagent | Function | Example Protocols |
|---|---|---|---|
| Basal Media | Advanced RPMI 1640; DMEM/F-12; STEMdiff Kidney Basal Medium | Foundation for differentiation media | Morizane et al.; Takasato et al.; Commercial kits |
| WNT Agonists | CHIR99021 (GSK3β inhibitor) | Induces primitive streak and posterior intermediate mesoderm | All major protocols (1-10 µM) |
| Growth Factors | FGF9; FGF2; Activin A; BMP4; BMP7 | Patterning and maintenance of nephron progenitors | Taguchi et al.; Morizane et al. |
| Enzymes for Dissociation | ACCUTASE; TrypLE Express | Gentle cell dissociation for 2D to 3D transition | Scalable protocol; Commercial kit |
| Extracellular Matrices | Matrigel; Synthetic hydrogels | Support 3D structure and provide biochemical cues | Most protocols; Vascularization studies |
| Cell Aggregation Tools | AggreWell plates; V-bottom plates | Form uniform 3D spheroids | Scalable production; Commercial kit |
| Pluripotency Media | mTeSR1; Essential 8 | Maintain hPSCs before differentiation | Initial culture; Commercial kit |
| Specialized Supplements | Heparin; Recombinant Albumin | Enhance growth factor activity and cell viability | Multiple protocols |
Applications and Future Directions
Kidney organoids have enabled significant advances in disease modeling, particularly for genetic kidney disorders such as polycystic kidney disease (PKD) and congenital anomalies of the kidney and urinary tract (CAKUT). Patient-derived iPSCs allow creation of organoids that recapitulate disease-specific phenotypes, providing platforms for studying disease mechanisms and screening therapeutic compounds [21] [2].
In drug screening and nephrotoxicity testing, kidney organoids offer a more physiologically relevant alternative to traditional 2D cell cultures. Organoids demonstrate appropriate cellular responses to nephrotoxic compounds and provide human-specific toxicity data that may improve prediction of adverse drug effects in clinical trials [23] [2]. Recent research has highlighted how the differentiation state of organoid models significantly influences their response to toxic compounds, underscoring the importance of maturation level in assay predictivity [24].
For regenerative medicine, kidney organoids represent a promising potential cell source. Transplantation studies have demonstrated engraftment of human kidney organoids into porcine kidneys during ex vivo machine perfusion, with successful in vivo integration and viability assessment [4]. The incorporation of functional collecting systems through UB organoid fusion represents a critical step toward creating organoids with potential for future therapeutic application [18].
Emerging technologies are addressing current limitations in organoid maturation, vascularization, and scalability. Microfluidic systems and bioreactors improve nutrient delivery and enhance organoid maturation and vascular network formation [21] [2]. Deep learning approaches are being developed to predict differentiation outcomes from bright-field images of organoids, potentially improving quality control and selection of optimally differentiated tissues [25]. These innovations collectively advance the field toward more physiologically relevant and clinically applicable kidney organoid technologies.
The generation of kidney organoids from human pluripotent stem cells (hPSCs) is a groundbreaking technology that recapitulates renal development in vitro, offering unprecedented opportunities for disease modeling, drug screening, and regenerative medicine [26] [27]. The fidelity of this process hinges on precisely timed manipulations of key developmental signaling pathways. This application note details the critical steps of CHIR99021-mediated priming and FGF9-driven maturation, contextualizing them within a stepwise monolayer protocol for kidney organoid differentiation. By providing explicit methodologies and quantitative benchmarks, we aim to empower researchers in reproducibly generating high-quality kidney organoids with minimized off-target cell populations.
Developmental Principles and Signaling Pathways
The directed differentiation of hPSCs into kidney organoids strategically mimics the natural process of kidney embryogenesis, which originates from the intermediate mesoderm (IM) [26]. The goal of the protocol is to first induce a posterior primitive streak population, which subsequently gives rise to the posterior intermediate mesoderm (PIM), the common precursor for both the metanephric mesenchyme (MM) and ureteric bud (UB) [4] [27]. The metanephric mesenchyme contains nephron progenitor cells (NPCs) that will differentiate into the full nephron structure—including glomeruli, proximal tubules, loops of Henle, and distal tubules—while the ureteric bud lineage forms the collecting duct system [4].
The following diagram illustrates the key signaling pathway manipulations that guide hPSCs through these developmental stages toward functional kidney organoids.
The developmental trajectory from hPSCs to kidney organoids involves two major phases. The CHIR99021 priming phase initiates differentiation by inducing a posterior primitive streak fate through WNT activation [27]. The subsequent FGF9-driven maturation phase patterns this primitive streak into posterior intermediate mesoderm and supports the expansion and subsequent differentiation of nephron progenitors [26] [4]. A critical modification to the classic Takasato protocol involves extending the FGF9 treatment to reduce the appearance of off-target chondrocytes, a common challenge in prolonged organoid cultures [28].
Experimental Workflow and Protocol Specifications
The following section outlines the complete, stepwise workflow for generating kidney organoids, from initial cell plating to mature organoid formation. The process integrates both two-dimensional monolayer differentiation and three-dimensional organoid culture.
Comprehensive Stepwise Workflow
The entire procedure, from pluripotent stem cells to mature kidney organoids, is visualized in the following workflow diagram.
Detailed Protocol Specifications
For practical implementation, the following table summarizes the key parameters from established kidney organoid differentiation protocols.
Table 1: Key Parameters in Kidney Organoid Differentiation Protocols
| Differentiation Stage | Treatment | Duration | Key Markers Induced | Protocol Variations |
|---|---|---|---|---|
| CHIR99021 Priming | 8-10 μM CHIR99021 [4] [29] | 2-4 days [26] [4] | TBX6 (Primitive Streak) [27] | Duration optimized per cell line [27] |
| FGF9-Driven Maturation | 200 ng/ml FGF9 + 1 μg/ml Heparin [4] [29] | 4 days to 1 week+ [28] [26] | OSR1, WT1, HOXD11 (IM) [27] [30] | 1-week extension reduces cartilage [28] |
| 3D Aggregation | Cell dissociation & aggregation | Day 7 [4] [29] | PAX2, LHX1 (Renal Vesicles) [4] | 500-250,000 cells/aggregate [4] |
| Growth Factor Withdrawal | Basal medium without FGF9 | From day 12-16 [4] [29] | PODXL (Podocytes), LTL (Proximal Tubules) [4] | Organoids harvested day 18-25 [28] [29] |
Critical Modifications and Optimizations
CHIR99021 Priming: Inducing Posterior Primitive Streak
The initial priming step is critical for directing hPSCs toward the appropriate mesodermal lineage. This stage requires precise optimization of CHIR99021 concentration and treatment duration, which varies between cell lines [27]. The objective is to achieve a highly efficient induction of late primitive streak cells, which express TBX6, while avoiding lateral plate mesoderm fates. This is typically accomplished using CHIR99021 at 8-10 μM in Advanced RPMI 1640 medium for 2-4 days [4] [29]. The optimal duration must be determined empirically for each hPSC line based on morphological changes and marker expression.
FGF9-Driven Maturation: Patterning and Nephron Formation
Following primitive streak induction, FGF9 signaling is applied to pattern the cells into posterior intermediate mesoderm, characterized by the expression of OSR1, WT1, and HOXD11 [27] [30]. The combination of FGF9 with heparin (200 ng/ml and 1 μg/ml, respectively) is typically maintained for approximately 4 days in the monolayer culture protocol [26] [29]. A critical protocol modification involves extending FGF9 treatment for an additional week during the subsequent 3D culture stage. This extended treatment has been demonstrated to significantly reduce the development of off-target chondrocyte populations—a common issue in prolonged organoid cultures—without adversely affecting the development of renal structures [28].
Quality Assessment and Functional Validation
Rigorous quality control is essential for generating reproducible and physiologically relevant kidney organoids. The following criteria and methods should be employed to validate successful differentiation.
Morphological and Molecular Benchmarks
Table 2: Quality Control Criteria for Kidney Organoids
| Assessment Category | Benchmark | Validation Method |
|---|---|---|
| Size & Morphology | ~200 μm or larger diameter [30] | Bright-field microscopy |
| Cell Composition | ~10-20% podocytes (PODXL+), ~40% proximal tubule cells (LTL+), ~10% distal tubule cells (CDH1+) [30] | Immunofluorescence, FACS, scRNA-seq [4] [30] |
| Nephron Segmentation | Presence of segmented nephrons: PODXL+CD31- glomeruli, LTL+ proximal tubules, ECAD+ distal tubules/loops of Henle [4] | Confocal immunofluorescence microscopy |
| Functional Transporters | Expression of PEPTs (apical) and OCTs (basolateral) [30] | qPCR, immunostaining, functional uptake assays |
| Batch Variation | Coefficient of variation <10% for size, morphology, and function between organoids [30] | Quantitative image analysis, functional assays |
Troubleshooting Common Differentiation Issues
- Low Efficiency of IM Induction: Optimize CHIR99021 exposure duration empirically for each cell line. Consider using H9 hESCs or lines maintained in ReproFF2 if persistent issues occur [27].
- Presence of Off-Target Cells: Extend FGF9 treatment during the 3D culture phase by one week to reduce chondrocyte formation [28]. Ensure growth factor concentrations are precise.
- Poor 3D Structure Formation: Confirm cell aggregation is performed using V-bottom or ultra-low attachment plates with an optimal seeding density (e.g., 8,000 cells/aggregate for RV formation) [4] [27].
- Lack of Functional Maturation: Allow sufficient maturation time (up to day 25) after growth factor withdrawal. Consider incorporating flow-induced shear stress or more complex culture conditions to enhance maturation [4].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Kidney Organoid Differentiation
| Reagent | Function | Specification |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor; induces WNT signaling to direct hPSCs toward posterior primitive streak fate. [4] [27] | 8-10 μM in Advanced RPMI [4] [29] |
| FGF9 (Fibroblast Growth Factor 9) | Patterns posterior intermediate mesoderm; supports nephron progenitor expansion and inhibits off-target chondrogenesis. [28] [26] | 200 ng/ml with 1 μg/ml Heparin [4] [29] |
| Heparin | Sulfated glycosaminoglycan; enhances FGF9 signaling stability and efficacy. [26] [29] | 1 μg/ml, used concurrently with FGF9 [4] [29] |
| Vitronectin | Recombinant attachment matrix for coating culture vessels; supports hPSC maintenance and monolayer differentiation. | Used for coating plates before hPSC seeding [4] |
| APEL/Advanced RPMI 1640 | Chemically defined, serum-free medium; used as the basal medium for differentiation steps to ensure reproducibility. [29] | Used throughout differentiation protocol [4] [29] |
The precise execution of CHIR99021 priming and FGF9-driven maturation is fundamental to generating high-fidelity kidney organoids from hPSCs. The initial WNT activation establishes the developmental trajectory toward kidney lineages, while sustained FGF9 signaling ensures proper patterning, minimizes off-target differentiation, and promotes the development of complex, segmented nephron structures. By adhering to the detailed protocols, quality controls, and reagent specifications outlined in this application note, researchers can reliably produce kidney organoids suitable for advanced applications in disease modeling, nephrotoxicity screening, and ultimately, regenerative medicine approaches. The continued refinement of these critical steps, particularly regarding prolonged maturation and vascular integration, remains a vital focus for the field.
Within the rapidly advancing field of kidney organoid research, the precise characterization of differentiated nephron segments—podocytes, proximal tubules, and distal segments—stands as a critical benchmark for success. This application note provides a detailed framework for the identification and validation of these essential cell types within kidney organoids generated via stepwise monolayer protocols. By integrating contemporary molecular markers, functional assays, and advanced analytical techniques, researchers can rigorously assess the cellular composition and maturity of their renal models, thereby enhancing the reliability of data generated for developmental studies, disease modeling, and nephrotoxicity screening.
The protocol is framed within a broader thesis on kidney organoid differentiation, which emphasizes recapitulating human kidney development in vitro [31]. This involves the sequential induction of posterior primitive streak, intermediate mesoderm, and ultimately, self-organizing kidney organoids containing multiple renal progenitor populations [31] [27]. The accurate characterization of the resulting nephron segments is paramount for validating this differentiation approach and for its application in translational research.
Molecular Marker Tables for Nephron Segments
Podocyte Markers
Podocytes, highly specialized cells of the glomerular filtration barrier, can be identified using a combination of structural and molecular markers. Recent single-cell RNA sequencing studies have further refined our understanding of podocyte heterogeneity in health and disease.
Table 1: Key Molecular Markers for Podocyte Characterization
| Marker | Type | Expression/Location | Significance in Characterization |
|---|---|---|---|
| ARHGEF26 | Protein/Gene | Significantly downregulated in Diabetic Kidney Disease (DKD) [32] | Novel potential diagnostic biomarker; decreased expression indicates podocyte injury in DKD [32] |
| Slit Diaphragm Proteins | Protein Complex | Foot processes of podocytes [33] | Key component of the glomerular filter; essential for selective permeability [33] |
| WT1 | Transcription Factor | Podocyte nucleus [27] | Marks podocyte identity and is a critical regulator of podocyte function. |
| SYNPO | Cytoskeletal Protein | Podocyte cell body and foot processes | A structural marker of podocyte maturity and integrity. |
The detection of these markers can be achieved through standard immunofluorescence staining and RNA analysis techniques. Furthermore, functional assessment of podocytes can involve evaluating their response to mechanical stress and molecular signals from their microenvironment, which is crucial for maintaining glomerular health [33].
Proximal Tubule Markers
The proximal tubule is responsible for the reabsorption of the majority of filtrate and is a primary site of drug-induced nephrotoxicity. Its cells possess distinct transport capabilities.
Table 2: Key Molecular Markers for Proximal Tubule Characterization
| Marker | Type | Expression/Location | Significance in Characterization |
|---|---|---|---|
| AQP1 | Channel Protein | Apical/Basolateral Membranes [34] | Facilitates water reabsorption; expressed in proximal tubule and thin descending limb [34] |
| Megalin & Cubilin | Endocytic Receptors | Apical Membrane [31] | Mediate endocytosis of proteins and ligands; evidence of functional maturity in organoids [31] |
| HNF4A | Transcription Factor | Nucleus [34] | Master regulator of proximal tubule cell formation and maturation; essential for AQP1 expression [34] |
| SLC34A1 | Transporter | Apical Membrane | Encodes the sodium-phosphate cotransporter NaPi-IIa; a specific marker for proximal tubule identity. |
A critical demonstration of functional maturity in kidney organoids is the presence of megalin- and cubilin-mediated endocytosis in the proximal tubules [31]. Additionally, the expression of transporters like organic cation transporter 2 (OCT2) and copper transporter 1 (CTR1) allows these cells to uptake nephrotoxicants such as cisplatin, leading to specific cell death—a vital assay for nephrotoxicity testing [31].
Distal Nephron Segments
The distal nephron, including the thick ascending limb (TAL), distal convoluted tubule (DCT), and collecting duct, is crucial for fine-tuning electrolyte balance and urine concentration.
Table 3: Key Markers for Distal Nephron Segments
| Segment | Marker | Type | Expression/Location |
|---|---|---|---|
| Thin Descending Limb | AQP1 [34] | Channel Protein | Apical Membrane |
| Bst1 [34] | Surface Protein | Cell Membrane | |
| Thick Ascending Limb | UMOD | Protein | Apical Membrane/Cytoplasm |
| Distal Convoluted Tubule | NCC | Transporter | Apical Membrane |
| Collecting Duct | AQP2 [27] | Channel Protein | Apical Membrane |
| CDH1 [27] | Adhesion Protein | Basolateral Membrane |
A key developmental insight is the origin of the thin descending limb. Lineage tracing using a Slc34a1eGFPCre line (a proximal tubule marker) has demonstrated that a subset of thin descending limb cells are descendants of proximal tubule cells [34]. This finding is crucial for understanding nephron patterning in organoids.
Experimental Protocols for Characterization
Immunofluorescence Characterization of Podocytes
Objective: To confirm the presence and structural organization of podocytes within kidney organoids. Materials: Fixed kidney organoid cryosections, blocking buffer (e.g., 5% BSA in PBS), primary antibodies (e.g., against WT1, ARHGEF26, SYNPO), fluorescently-labeled secondary antibodies, DAPI, and mounting medium. Workflow:
- Fixation & Sectioning: Fix organoids in 4% PFA for 15-20 minutes at room temperature. Embed in OCT compound and section at 5-10 μm thickness using a cryostat.
- Permeabilization & Blocking: Permeabilize sections with 0.1% Triton X-100 in PBS for 10 minutes. Incubate with blocking buffer for 1 hour to reduce non-specific binding.
- Antibody Incubation: Incubate sections with primary antibodies diluted in blocking buffer overnight at 4°C. The following day, wash with PBS and incubate with appropriate secondary antibodies for 1 hour at room temperature, protected from light.
- Imaging & Analysis: Wash thoroughly, counterstain nuclei with DAPI, and mount. Analyze using a confocal microscope. Co-localization of nuclear WT1 with cytoplasmic markers like SYNPO confirms podocyte identity. Notably, reduced ARHGEF26 signal may indicate a diseased state [32].
Functional Assay for Proximal Tubule Maturity
Objective: To validate the functional maturity of proximal tubule cells in organoids by assessing receptor-mediated endocytosis. Materials: Kidney organoids, fluorescently-labeled dextran or albumin (e.g., 10-70 kDa), cell culture medium, live-cell imaging setup or flow cytometer. Workflow:
- Preparation: Transfer organoids to a suitable imaging dish with fresh medium. Allow them to equilibrate in a 37°C incubator for at least 30 minutes.
- Uptake Assay: Add the fluorescent ligand (e.g., 50 μg/mL dextran) to the medium. Incubate for a defined period (e.g., 30-120 minutes) at 37°C.
- Control: Include control organoids incubated at 4°C to inhibit active endocytosis, or pre-treated with a endocytic inhibitor.
- Termination & Analysis:
- For imaging: Wash organoids extensively with cold PBS to remove surface-bound ligand. Fix with 4% PFA and image using confocal microscopy. Co-localization of the fluorescent signal with a proximal tubule marker (e.g., LRP2/megalin) confirms specific uptake [31].
- For flow cytometry: Dissociate organoids into single cells after uptake, wash, and analyze intracellular fluorescence immediately using a flow cytometer. A rightward shift in fluorescence intensity compared to the 4°C control indicates active endocytosis.
Gene Expression Analysis via RT-qPCR
Objective: To quantitatively assess the expression levels of key segment-specific markers. Materials: RNA extraction kit (e.g., TRIzol), DNase I, reverse transcription kit, SYBR Green qPCR master mix, gene-specific primers (e.g., for SIX2, SLC34A1, AQP2, UMOD, etc.), and a real-time PCR instrument. Workflow:
- RNA Extraction: Homogenize pooled organoids or micro-dissected regions in TRIzol. Extract total RNA according to the manufacturer's protocol. Treat with DNase I to remove genomic DNA contamination.
- cDNA Synthesis: Use 0.5-1 μg of total RNA for reverse transcription using a high-capacity cDNA synthesis kit.
- qPCR Setup: Prepare reactions with SYBR Green master mix, gene-specific primers (validated for efficiency), and cDNA template. Run in technical duplicates/triplicates.
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method. Normalize to stable housekeeping genes (e.g., GAPDH, HPRT1). Compare expression across different batches of organoids or against control samples. For instance, validation of ARHGEF26 as a podocyte marker was confirmed using RT-qPCR [32].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Kidney Organoid Characterization
| Reagent/Cell Line | Function/Application | Key Details |
|---|---|---|
| Human Pluripotent Stem Cells (hPSCs) | Starting material for organoid generation | Both ESCs and iPSCs can be used; line-specific differentiation efficiency varies [27]. |
| Slc34a1eGFPCre Mouse Line | Lineage tracing of proximal tubule and its derivatives | Used to demonstrate that thin descending limb cells originate from proximal tubule cells [34]. |
| CHIR99021 | GSK-3β inhibitor; activates Wnt signaling | Used in initial primitive streak induction and later to trigger nephrogenesis from NPCs [27]. |
| FGF9 | Growth Factor | Directs differentiation of primitive streak to intermediate mesoderm [31]. |
| Microfluidic Chip System | Creates a proximal tubule-on-chip model | Enhances transporter expression and polarization for improved nephrotoxicity and drug transport assays [35]. |
| Anti-ARHGEF26 Antibody | Detects a novel podocyte injury marker | Validated via Western blot and immunofluorescence; shows significant downregulation in DKD [32]. |
Workflow Visualization: From Pluripotency to Characterized Organoids
The entire process, from stem cell differentiation to the final characterization of nephron segments, can be summarized in the following workflow. This integrates the differentiation protocol with the specific characterization techniques outlined in this note.
The systematic characterization of podocytes, proximal tubules, and distal segments is indispensable for validating the success of kidney organoid differentiation protocols. By employing the panel of molecular markers, functional assays, and detailed methodologies described in this application note, researchers can robustly quantify the identity, maturity, and functionality of the nephron segments within their models. This rigorous approach not only strengthens the fidelity of in vitro organoids as models of human kidney biology and disease but also paves the way for their standardized application in drug development and regenerative medicine strategies. The integration of novel biomarkers, such as ARHGEF26 for podocytes, and advanced culture systems, like tubule-on-chip models, continues to push the boundaries of what can be achieved with these complex tissues.
The advent of three-dimensional kidney organoid technology represents a paradigm shift in nephrological research, offering an unprecedented in vitro platform that recapitulates key aspects of human kidney development, structure, and function. Derived from human pluripotent stem cells (hPSCs), including both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), these self-organizing structures provide a versatile tool for investigating disease mechanisms, performing high-throughput drug screening, and exploring regenerative medicine applications [2]. The field has progressed significantly since the initial establishment of protocols that direct hPSCs through stages mimicking embryonic kidney development, culminating in organoids containing segmented nephrons with glomerular and tubular structures [2] [36].
The "bench to bedside" translation of this technology is particularly relevant for drug nephrotoxicity screening, which remains a significant challenge in pharmaceutical development. Kidney organoids offer a human-specific, physiologically relevant model that can potentially overcome the limitations of traditional animal models and two-dimensional cell cultures [2]. This Application Note details current methodologies and applications of kidney organoids, with a specific focus on their implementation within drug development pipelines for nephrotoxicity assessment and their use in modeling hereditary kidney diseases, providing researchers with detailed protocols and analytical frameworks to advance their translational research.
Kidney Organoid Differentiation: Core Principles and Protocols
Developmental Biology Informing Differentiation Strategies
The differentiation of hPSCs into kidney organoids strategically recapitulates key stages of embryonic kidney development. The mammalian kidney, the metanephros, arises from the intermediate mesoderm (IM) through reciprocal inductive signaling between two key embryonic tissues: the ureteric bud (UB) and the metanephric mesenchyme (MM) [2]. The UB evolves into the collecting duct system, while the MM contains self-renewing nephron progenitor cells (NPCs) that differentiate into all the epithelial components of the nephron—including the glomerulus, proximal tubule, loop of Henle, and distal tubule—through a mesenchymal-to-epithelial transition (MET) process [2] [36]. This developmental cascade is orchestrated by precisely timed signaling pathways, with WNT, FGF, and BMP playing particularly critical roles [2].
Table 1: Key Signaling Pathways in Kidney Development and Their In Vitro Recapitulation
| Signaling Pathway | Role in Kidney Development | Commonly Used Agonists/Antagonists in Differentiation |
|---|---|---|
| WNT/β-catenin | Induction of posterior primitive streak; MET initiation | CHIR99021 (GSK3β inhibitor) [2] [4] |
| FGF | NPC proliferation and survival; UB branching | FGF9 [2] [4] |
| BMP | MM survival and proliferation | BMP7 [2] |
| RA | Patterning of the IM | Retinoic Acid |
Established Monolayer-Based Differentiation Protocols
The stepwise 2D monolayer-based protocol, as pioneered by Morizane et al. (2015), provides a robust framework for generating kidney organoids with reduced variability and improved reproducibility [9] [2]. This approach involves directing a confluent monolayer of hPSCs through defined developmental stages by sequential activation and inhibition of key signaling pathways.
Figure 1: Workflow of a stepwise monolayer-based kidney organoid differentiation protocol.
A critical refinement to this protocol involves the pretreatment of hPSCs with low-dose (1-2%) dimethyl sulfoxide (DMSO) prior to differentiation induction. This preconditioning step has been shown to alter the expression of pluripotency transcription factors, modify the epigenetic landscape, and enhance the differentiation efficiency toward nephron progenitor cells, ultimately resulting in kidney organoids with improved tubular formation [9]. The treated cells demonstrate enhanced expression of the key nephron progenitor marker SIX2 after nine days of differentiation [9].
The Scientist's Toolkit: Essential Reagents for Organoid Differentiation
Table 2: Key Research Reagent Solutions for Kidney Organoid Differentiation
| Reagent/Category | Specific Example | Function in Protocol |
|---|---|---|
| Base Medium | Advanced RPMI 1640 | Chemically defined basal medium for differentiation [4] |
| WNT Agonist | CHIR99021 (8 µM initial; 5 µM later) | GSK3β inhibitor inducing primitive streak and IM [2] [4] |
| Growth Factors | FGF9 (200 ng/mL) | Supports MM patterning and NPC expansion [2] [4] |
| Chemical Modifier | Dimethyl Sulfoxide (DMSO 1-2%) | Pretreatment to enhance differentiation efficiency [9] |
| Extracellular Matrix | Vitronectin | Coating substrate for initial hPSC monolayer culture [4] |
Advanced Technological Innovations in Kidney Organoid Systems
Integration of a Collecting System
A significant limitation of earlier kidney organoid protocols was the absence of a functional collecting system, which is crucial for establishing a patent luminal conduit for fluid drainage. A groundbreaking advancement addresses this by combining UB progenitors with NM in a co-culture system [18]. This protocol involves generating UB spheroids from hPSCs that express RET and GATA3, then combining them with dissociated SIX2-positive NM cells [18]. The assembled organoids demonstrate successful fusion between distal nephron segments and CD-like structures, creating a more physiologically relevant model with improved maturation and organization across all nephron segments [18].
Scalable Production and Transplantation Models
For therapeutic applications, scalable and reproducible production of kidney organoids is essential. Recent work has established a free-floating culture method that allows for the systematic production of hPSC-derived kidney organoids (hPSC-kidney organoids) by varying the number of intermediate mesoderm-committed cells during the 3D spheroid formation stage [4]. This research demonstrated that infusion of these organoids into porcine kidneys undergoing ex vivo normothermic machine perfusion (NMP) led to successful engraftment, providing a foundation for future cell-based therapies and clinical trials [4].
Application in Drug Nephrotoxicity Screening
The Need for Improved Nephrotoxicity Models
Drug-induced kidney injury is a major cause of pipeline attrition in drug development and a significant clinical concern. The kidneys are particularly vulnerable to toxic injury due to their high blood flow, concentration of drugs and metabolites, and extensive active transport processes [37]. Traditional preclinical models, including animal studies and 2D cell cultures, often fail to accurately predict human-specific nephrotoxicity, highlighting the critical need for more physiologically relevant human in vitro models [2] [37].
Implementing Organoids for Toxicity Screening
Kidney organoids contain multiple, integrated renal cell types, enabling the detection of cell-type-specific toxicities and complex tissue-level responses that cannot be modeled in simpler systems. Proximal tubule cells in organoids express functional transporters and demonstrate uptake capabilities, making them particularly suitable for assessing compound toxicity [2]. The application of kidney organoids in toxicity screening typically involves exposing mature organoids (day 18-25 of differentiation) to the compound of interest for 24-72 hours, followed by multiparametric endpoint analysis.
Table 3: Quantitative Endpoints for Nephrotoxicity Assessment in Organoids
| Endpoint Category | Specific Assay/Marker | Application in Toxicity Screening |
|---|---|---|
| Cell Viability Lactate Dehydrogenase (LDH) Release | Quantifies necrotic cell death [2] | |
| Apoptosis | Caspase-3/7 Activation | Measures apoptotic cell death [2] |
| Proximal Tubule Injury | LTL+ Area, KIM-1 Expression | Specific marker for proximal tubule damage [2] |
| Podocyte Injury | WT1+ Cell Count, NEPHRIN Expression | Assesses glomerular compartment toxicity [2] |
| Oxidative Stress | γH2AX, Metallothionein Expression | Indicators of DNA damage and cellular stress [4] |
Integration with Organ-on-Chip and AI Technologies
Microfluidic "kidney-on-a-chip" platforms that incorporate kidney organoids are redefining nephrotoxicity screening by introducing physiological cues such as fluid flow and shear stress [38]. These systems reproduce nephron-relevant structure, fluid flow, and molecular transport, enabling more mechanistic interrogation of drug-induced kidney injury and revealing patient-to-patient variability in susceptibility [38]. Case studies have demonstrated concordance with known nephrotoxins and enabled detection of off-target effects and cardio-renal complications [38].
Furthermore, artificial intelligence approaches are being leveraged to predict drug-induced nephrotoxicity. Deep learning algorithms trained on molecular fingerprint data can accurately predict the nephrotoxic potential of various compounds, providing a valuable complementary approach to empirical organoid-based testing [37]. This computational framework allows for early prioritization or deprioritization of compounds before they enter more resource-intensive experimental screening phases [37].
Figure 2: Integrated workflow combining AI-based prediction and organoid-based experimental validation for nephrotoxicity screening.
Application in Disease Modeling
Modeling Genetic Kidney Diseases
Kidney organoids have proven particularly valuable for modeling monogenic kidney diseases, offering insights into disease pathophysiology and enabling therapeutic screening. Successful models have been established for various hereditary disorders, including:
- Polycystic Kidney Disease (PKD): Organoids with PKD-associated mutations develop cyst-like structures that can be quantified over time, serving as a platform for evaluating potential therapeutic interventions [2] [36].
- Congenital Anomalies of the Kidney and Urinary Tract (CAKUT): These complex developmental disorders can be modeled using patient-derived iPSCs or through CRISPR/Cas9 engineering of specific genetic mutations in wild-type hPSCs [2].
The combination of kidney organoid technology with CRISPR/Cas9 gene editing has been especially powerful, allowing researchers to introduce specific disease-causing mutations into control lines or to correct mutations in patient-derived iPSCs, creating isogenic control lines that are crucial for distinguishing phenotype from background genetic variation [36].
Protocol: Disease Modeling Using CRISPR/Cas9-Engineered Organoids
- Target Selection: Identify the genetic target based on human genetic evidence (e.g., PKD1, PKD2 for polycystic kidney disease).
- gRNA Design and Validation: Design guide RNAs (gRNAs) with high on-target efficiency and minimal off-target effects. Validate editing efficiency in the hPSC line of choice.
- hPSC Engineering: Introduce CRISPR/Cas9 components into hPSCs via electroporation or nucleofection. For disease modeling, deliver Cas9 protein with gRNA and a donor DNA template containing the desired mutation to enhance efficiency and reduce off-target effects.
- Clone Isolation and Validation: Isolve single-cell-derived clones, expand them, and validate the introduction of the specific mutation via Sanger sequencing, next-generation sequencing, or other appropriate genomic analyses.
- Organoid Differentiation: Differentiate the validated mutant and isogenic control hPSC lines into kidney organoids using the stepwise monolayer protocol.
- Phenotypic Analysis: Compare mutant and control organoids for disease-relevant phenotypes using microscopy (cyst formation, structural abnormalities), immunofluorescence (cell type-specific markers, protein localization), and transcriptomic profiling (bulk or single-cell RNA-seq).
Kidney organoid technology has rapidly evolved from a novel discovery tool to a robust platform with significant translational applications in disease modeling and drug safety assessment. The continued refinement of differentiation protocols—including DMSO preconditioning for enhanced efficiency [9] and the integration of collecting systems for improved physiological relevance [18]—is steadily addressing initial limitations related to maturation, variability, and structural complexity.
For drug development professionals, kidney organoids integrated with organ-on-chip technologies offer a human-specific, physiologically complex model that can enhance the prediction of nephrotoxicity earlier in the drug development pipeline, potentially reducing late-stage attrition and improving patient safety [38] [2]. For researchers investigating kidney diseases, the combination of organoids with CRISPR/Cas9 gene editing provides an unprecedented opportunity to study disease mechanisms in a human cellular context and perform high-throughput screening of therapeutic candidates [36].
As the field advances, key areas for development include further enhancing organoid vascularization and maturation, standardizing protocols across different laboratory settings, and establishing validated, quantitative endpoints for high-content screening. The ongoing integration of bioengineering approaches, such of microfluidic systems and 3D bioprinting, with single-cell omics technologies promises to further bridge the gap between in vitro models and human kidney physiology, accelerating the journey from bench to bedside.
Enhancing Efficiency and Maturity: Solving Common Challenges in Organoid Generation
Within the broader context of optimizing stepwise monolayer protocols for kidney organoid differentiation, addressing the challenge of functional immaturity is a pivotal research frontier. Current differentiation protocols successfully generate organoids with nephron-like structures; however, these tissues often exhibit a transcriptional and functional profile reminiscent of first-trimester fetal kidney, limiting their direct application in modeling adult-onset diseases and high-fidelity drug screening [2] [15]. This Application Note details validated, experimentally-grounded strategies to overcome this developmental arrest, focusing on enhancing the structural and functional maturity of kidney organoids derived from human pluripotent stem cells (hPSCs).
Strategic Approaches to Enhance Maturation
Several innovative strategies have emerged to drive kidney organoids toward a more mature state. The table below summarizes the core approaches, their mechanistic basis, and key experimental findings.
Table 1: Strategies for Promoting Kidney Organoid Maturation
| Strategy | Mechanistic Basis | Key Experimental Findings |
|---|---|---|
| Metabolic & Signaling Modulation | Transient activation of key maturation pathways (e.g., AMPK, ERR) to induce metabolic switching and transcriptional maturation [39]. | Pharmacological activation of AMPK and ERR in cardiac organoids increased expression of mature sarcomeric proteins (cTnI) and enhanced oxidative phosphorylation capacity [39]. |
| Pre-conditioning of hPSCs | Pre-differentiation exposure to low-dose Dimethyl Sulfoxide (DMSO) to alter the epigenetic landscape and pluripotency state of the starting cell population [9]. | Treating hPSCs with 1-2% DMSO altered colony morphology and gene expression, leading to enhanced expression of the nephron progenitor marker SIX2 and improved tubular kidney organoid development [9]. |
| Optimized Cellular Aggregation | Controlling initial cell-to-cell contact and spheroid size in 3D culture to better mimic developmental cues and reduce stromal cell abundance, a hallmark of maturation [4]. | scRNA-seq revealed that organoids derived from smaller spheroids (500-8,000 cells) showed a higher degree of differentiation, with a larger proportion of podocyte- and tubular-like cells and less stromal cells compared to larger aggregates [4]. |
| Bioengineering & Microenvironment Tuning | Using microfluidic devices, bioreactors, or 3D bioprinting to improve nutrient delivery, reduce hypoxia-induced necrosis, and provide mechanical cues [40] [41]. | In brain organoids, extended culture exacerbates central necrosis; integrating vascularization and microfluidics was identified as a key strategy to support long-term culture and maturation [40]. |
Detailed Experimental Protocols
Protocol 1: DMSO Pre-conditioning of hPSCs for Enhanced Nephron Progenitor Differentiation
This protocol is adapted from a 2025 study demonstrating that pre-treating hPSCs with low-dose DMSO enhances their subsequent differentiation into nephron progenitors and kidney organoids [9].
Research Reagent Solutions
Table 2: Essential Reagents for DMSO Pre-conditioning Protocol
| Reagent / Material | Function | Example Catalog # |
|---|---|---|
| hPSCs (e.g., hiPSCs) | The starting cell population for organoid differentiation. | LUMCi004-C, TISSUi001-A [9] |
| Dimethyl Sulfoxide (DMSO) | Pre-conditioning agent to modulate pluripotency and epigenetic state. | - |
| Essential 8 Medium (E8) | Maintenance medium for hPSCs prior to differentiation. | - |
| Advanced RPMI 1640 | Basal medium for the initial differentiation steps. | - |
| CHIR99021 (GSK3β inhibitor) | Small molecule to activate WNT signaling and induce primitive streak. | - |
| FGF9 & Heparin | Growth factors for patterning and maintaining nephron progenitors. | - |
| Activin A | Signaling molecule involved in mesodermal patterning. | - |
Workflow Diagram
Step-by-Step Methodology
- Culture hPSCs: Maintain high-quality hPSCs in Essential 8 medium on a suitable substrate (e.g., Matrigel). Ensure cultures are free of excessive differentiation (<5%) before starting [22].
- DMSO Pre-conditioning: Add filter-sterilized DMSO to the culture medium to a final concentration of 1-2%. Incubate cells for 24-48 hours. Monitor cell morphology for changes indicative of altered pluripotency [9].
- Initiate Differentiation: Following pre-conditioning, begin a standard stepwise monolayer differentiation protocol.
- Day 0: Replace medium with Advanced RPMI 1640 containing 8 μM CHIR99021 to induce primitive streak formation. Incubate for 3 days [2].
- Pattern Nephron Progenitors:
- Day 3: Switch to a medium containing 200 ng/mL FGF9, 1 μg/mL heparin, and 10 ng/mL Activin A to pattern the cells into the metanephric mesenchyme. Incubate for 24 hours [4].
- Form 3D Organoids:
- Day 4: Dissociate the monolayer into single cells using ACCUTASE [22].
- Seed the cells into low-attachment plates (e.g., AggreWell) at an optimized density (e.g., 5,000 cells per microwell) to form uniform 3D spheroids [4] [22].
- Continue culture with FGF9 and heparin for several more days to promote renal vesicle formation.
- Final Differentiation: Maintain the free-floating organoids in culture for up to 16-18 days total, allowing for the development of segmented nephron structures (glomeruli, proximal tubules, distal tubules) [4].
- Analysis: Assess the outcome by quantifying the expression of the key nephron progenitor marker SIX2 at day 9 of differentiation via immunostaining or qPCR, comparing pre-conditioned and control organoids [9].
Protocol 2: Optimized Aggregation for Improved Organoid Composition
This protocol leverages the controlled formation of 3D spheroids to enhance the fidelity and maturity of the resulting kidney organoids, as demonstrated by single-cell RNA sequencing (scRNA-seq) analysis [4].
Workflow Diagram
Step-by-Step Methodology
- Generate PIM-committed Cells: Differentiate hPSCs in a monolayer towards posterior intermediate mesoderm (PIM) using established protocols involving CHIR99021 and FGF9/Activin A signaling [4].
- Dissociate and Aggregate:
- On the day of aggregation (typically day 4-5 of differentiation), dissociate the monolayer into a single-cell suspension.
- Seed the cells into non-adherent V-bottom 96-well plates to promote forced aggregation. It is critical to test a range of cell seeding numbers per spheroid (e.g., 500, 8,000, 100,000, and 250,000 cells) to optimize for specific cell lines and protocols [4].
- Differentiate Organoids: Culture the resulting 3D spheroids under free-floating conditions for a total differentiation period of 16 days, maintaining FGF9 signaling from days 0 to 7 to promote renal vesicle formation [4].
- Quality Control and Analysis:
- At day 7, assess the formation of renal vesicles by immunostaining for PAX2 and LHX1. Spheroids derived from lower cell numbers (500-8,000) typically develop more PAX2+LHX1+ structures [4].
- At day 16, use scRNA-seq to comprehensively evaluate the cellular composition. Benchmark against fetal and adult human kidney datasets to assess maturity and purity. Expect organoids from smaller spheroids to show a higher abundance of podocyte- and tubular-like cells and a lower proportion of stromal cells [4] [15].
Discussion and Future Perspectives
The protocols outlined herein provide a tangible pathway to enhance the maturity of kidney organoids. The DMSO pre-conditioning strategy operates by priming the epigenetic and transcriptional state of the starting hPSCs, making them more amenable to renal differentiation [9]. Meanwhile, the aggregation control protocol demonstrates that the initial physical conditions of 3D culture profoundly influence lineage specification and the resultant organoid's cellular architecture, with smaller spheroids favoring a more differentiated renal state [4].
A critical consideration for any maturation strategy is the rigorous assessment of outcomes. As highlighted in brain organoid research, the field requires standardized, multidimensional maturity metrics [40]. For kidney organoids, this should include:
- Molecular Profiling: scRNA-seq to benchmark against human fetal and adult kidney atlases [4] [15].
- Structural Analysis: Confocal microscopy for complex structures (e.g., laminated glomeruli with mature podocytes) and electron microscopy to visualize ultrastructural details like mature slit diaphragms and tubular brush borders [2].
- Functional Assays: Uptake assays for proximal tubules (e.g., albumin endocytosis) and drug response testing to validate physiological relevance [4] [2].
Future directions will likely involve combining these strategies—for instance, using pre-conditioned cells in optimized aggregation systems—along with integrating bioengineering advances such as vascularization [4] [41] and electrical or mechanical stimulation [40] [39] to create the next generation of physiologically relevant kidney organoids for disease modeling and therapeutic discovery.
The differentiation of human pluripotent stem cells (hPSCs) into kidney organoids represents a transformative technology for researching development, disease modeling, and drug screening. However, a significant limiting phenomenon in this field is high variability, where technical variation across experiments and laboratories can surpass variation caused by genotypic effects of induced pluripotent stem cell (iPSC) lines [42]. This variability manifests in differences in organoid size, cellular composition, and structural maturity, ultimately compromising experimental reproducibility and translational potential. Common sources of this variability include the choice of differentiation protocol, specific iPSC lines used, culture conditions, and initial cell seeding densities [42] [2]. This Application Note details evidence-based strategies and optimized protocols to combat these challenges, enhance differentiation efficiency, and improve the reliability of kidney organoid generation.
Understanding the relative impact of different factors is crucial for targeted improvement. The following table summarizes key variables and their quantified effects on kidney organoid differentiation, as revealed by recent studies.
Table 1: Factors Influencing Kidney Organoid Differentiation Efficiency and Variability
| Factor | Impact on Differentiation | Quantitative Effect | Reference |
|---|---|---|---|
| Culture Approach | Significant association with glomerular and tubular structure development | High-content screening showed culture method is a major variable | [42] |
| iPSC Line | Affects success rate and final organoid composition | Not all lines differentiate with equal efficiency; patient-specific lines (e.g., GRACILE syndrome) can be used | [42] |
| Initial Cell Number in 3D Spheroid | Determines progenitor cell interactions and final organoid composition | 500-8,000 cells/spheroid generated more PAX2+LHX1+ renal vesicles than 100,000-250,000 cell spheroids | [4] |
| Experimental Replication | Contributes to technical variation | Identified as a significant factor in multiple linear models | [42] |
| Integrated Model | Explains a major portion of observable variability | Culture approach, iPSC line, replication, and cell number explained 35-77% of variability in nephrin/ECAD+ structures | [42] |
Optimized Protocols for Enhanced Reproducibility
High-Throughput Microplate-Based Approach
To combat organoid size variability and enable scalable production, an original air-medium interface (AMI) protocol was adapted for microplate-based high-throughput culture [42].
Key Methodology:
- Base Protocol: The protocol begins with a 2D monolayer differentiation of hPSCs on vitronectin-coated plates in defined media (e.g., Essential 8) [42] [4].
- Primitive Streak & Intermediate Mesoderm Induction: Cells are treated with a GSK3β inhibitor (CHIR99021, typically 8 μM) in Advanced RPMI 1640 for 3 days to induce posterior primitive streak, followed by patterning into intermediate mesoderm using FGF9 (200 ng/mL) and heparin (1 μg/mL) for 1-4 days [26] [4].
- 3D Spheroid Formation: On differentiation day 0, the IM-committed monolayer is dissociated into single cells and seeded in V-bottom 96-well plates. Critical parameter: seeding density. Optimal results were achieved with 500 to 8,000 cells per spheroid, which promoted efficient formation of renal vesicle-like structures [4].
- Renal Vesicle and Organoid Culture: Spheroids are treated with a pulse of CHIR99021 (5 μM) for 1 hour while maintaining FGF9 signaling. They are then cultured in free-floating conditions with FGF9 for 7 days to form renal vesicles, followed by maturation without growth factors until day 16 [4].
Advantages: This method effectively controls organoid size variability and is compatible with quantitative high-content screening, allowing for better distinction between technical and biological variation [42].
Agitation-Based Suspension Culture
Building on successes in cardiac differentiation, stirred suspension systems offer a pathway for scalable and reproducible kidney organoid production [43].
Key Methodology:
- Stirred Bioreactor/Spinner Flasks: Cells are differentiated in a controlled suspension culture system that maintains consistent temperature, O2, CO2, and pH [43].
- Cell Aggregation: hiPSCs spontaneously form embryoid bodies (EBs) in suspension. A critical quality control point is initiating differentiation with a Wnt activator (CHIR99021) only when the average EB diameter reaches ~100 μm. EBs larger than 300 μm differentiate less efficiently due to diffusion limits [43].
- Directed Differentiation: A precise sequence of Wnt activation (24 hours with CHIR) followed by a gap and then Wnt inhibition (48 hours with IWR-1) drives efficient and consistent mesoderm patterning [43].
Advantages: This system eliminates local heterogeneity in cell seeding and microenvironment found in static monolayer cultures, resulting in improved batch-to-batch consistency and functional properties [43].
Pre-Conditioning with Dimethyl Sulfoxide (DMSO)
A novel pre-conditioning strategy has been shown to enhance the efficiency of subsequent kidney organoid differentiation.
Key Methodology:
- Pre-Treatment: hiPSCs are treated with a low dose (1-2%) of DMSO while in the pluripotent state [9].
- Mechanism of Action: DMSO conditioning affects the gene expression of pluripotency transcription factors and the epigenetic landscape of the cells, potentially priming them for differentiation [9].
- Outcome: Treated hiPSCs show enhanced expression of the key nephron progenitor marker SIX2 after 9 days of kidney organoid differentiation, indicating improved protocol efficiency toward tubular kidney organoids [9].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Kidney Organoid Differentiation
| Reagent/Category | Specific Examples | Function in Protocol |
|---|---|---|
| GSK3β Inhibitor (Wnt activator) | CHIR99021 | Induces primitive streak and posterior intermediate mesoderm; used as a pulse for renal vesicle induction [26] [4] |
| Growth Factors | FGF9, FGF2, BMP7 | Patterns intermediate mesoderm and supports survival/expansion of nephron progenitors [26] [2] |
| Extracellular Matrix | Matrigel, Vitronectin, Geltrex | Provides a scaffold for 2D monolayer differentiation and supports pluripotent stem cell growth [42] [44] |
| Cell Culture Media | Advanced RPMI 1640, Essential 8, Essential 6 | Defined, serum-free media used as a base for differentiation or pluripotent cell culture [42] [4] |
| Small Molecule Inhibitors/Activators | IWR-1 (Wnt inhibitor), Y-27632 (ROCK inhibitor), Purmorphamine (Shh activator) | IWR-1 promotes cardiac mesoderm; ROCK inhibitor improves cell survival after passaging [44] [43] |
| Pluripotent Stem Cell Conditioner | Dimethyl Sulfoxide (DMSO) | Pre-conditions hiPSCs to enhance subsequent differentiation into nephron progenitors [9] |
Signaling Pathways and Workflow Visualization
The stepwise differentiation of kidney organoids meticulously recapitulates developmental stages by activating and inhibiting key signaling pathways. The logical progression from pluripotent stem cells to a mature kidney organoid, including critical branching points and quality control checkpoints, is summarized in the workflow below.
Combating variability in kidney organoid differentiation requires a multi-faceted approach that addresses key technical and biological sources of inconsistency. As demonstrated, employing high-throughput microplate formats, transitioning to controlled agitation-based suspension systems, and exploring novel pre-conditioning strategies with molecules like DMSO can significantly enhance the efficiency, reproducibility, and scalability of kidney organoid generation. The quantitative frameworks and optimized protocols detailed in this Application Note provide researchers with a solid foundation to standardize their workflows, thereby increasing the reliability of data generated from kidney organoid models and accelerating their application in disease modeling and drug development.
Within kidney organoid research, a significant challenge remains the efficient differentiation of human induced pluripotent stem cells (hiPSCs) into specific renal lineages, particularly nephron progenitor cells (NPCs), which are crucial for generating functional kidney tissues [9] [2]. Current stepwise monolayer protocols, while established, often exhibit variable efficiencies and limitations in generating complex structures with multiple cell types [9] [21]. This application note explores a novel pre-conditioning strategy using low-dose dimethyl sulfoxide (DMSO) to enhance the yield of nephron progenitors, thereby improving the robustness and effectiveness of kidney organoid differentiation.
Mechanistic Basis of DMSO Action
DMSO, a polar aprotic solvent, influences hiPSC biology through several key mechanisms. Treatment with low concentrations (1-2%) of DMSO alters the gene expression of core pluripotency transcription factors and modifies the epigenetic landscape of hiPSCs [9] [13]. Research indicates that DMSO prevents the phosphorylation of retinoblastoma protein, arresting cells in the G1 phase of the cell cycle via alterations in PI3K pathway signalling [13]. This halt in the cell cycle is associated with regulating early transitory states of hiPSCs toward differentiation.
Furthermore, DMSO treatment significantly affects genes involved in cytoskeletal dynamics, cilium assembly, and cell adhesion—processes integral to cell shape, migration, and ultimately, organogenesis [13]. These changes prime the cells for a more efficient response to subsequent differentiation signals, particularly towards a nephron progenitor fate, by enhancing the expression of key markers such as SIX2, a critical transcription factor for metanephric mesenchyme maintenance [9] [13].
Table 1: Key Cellular Effects of DMSO Pre-conditioning
| Affected Process | Observed Effect | Downstream Outcome |
|---|---|---|
| Cell Cycle Regulation | Prevents retinoblastoma phosphorylation; G1 phase arrest [13] | Promotes a state conducive to differentiation |
| Gene Expression | Alters expression of pluripotency factors (OCT3/4, SOX2) and cytoskeletal genes [13] | Primes cells for lineage specification |
| Signaling Pathways | Modulates PI3K signaling [13] | Regulates early transitional states of hiPSCs |
| Nephron Progenitor Markers | Enhances expression of SIX2 protein [9] [13] | Increases yield of metanephric mesenchyme NPCs |
Detailed Experimental Protocol
Materials and Reagent Solutions
Table 2: Essential Research Reagents and Materials
| Item | Specification/Function | Example/Catalog |
|---|---|---|
| hiPSC Lines | Human induced pluripotent stem cells | LUMCi004-C, HUMIMC101, HUMIMC107 [13] |
| Basal Medium | Maintenance of hiPSC pluripotency | mTeSRplus [13] |
| DMSO | Pre-conditioning agent; alters cell state | Cell culture grade, sterile filtered [9] [13] |
| Coating Matrix | Provides adhesion substrate for monolayer culture | 1% Geltrex [13] |
| Dissociation Reagent | Generates single-cell suspension for seeding | Accutase [13] |
| Rho Kinase (ROCK) Inhibitor | Enhances survival of dissociated hiPSCs | Y-27632 (10 µM) [13] |
| Differentiation Basal Medium | For subsequent kidney differentiation | Advanced RPMI 1640 or APEL medium [4] [13] |
Step-by-Step Pre-conditioning Workflow
The following workflow integrates DMSO pre-conditioning into the established stepwise monolayer differentiation protocol for kidney organoids. The process from hiPSC culture to the emergence of nephron progenitors takes approximately 10 days.
hiPSC Culture and Maintenance:
- Maintain hiPSC colonies (e.g., LUMCi004-C, HUMIMC101, HUMIMC107) on 1% Geltrex-coated plates in mTeSRplus medium [13].
- Culture cells at 37°C with 5% CO₂, passaging with gentle cell dissociation reagent when colony edges become rounded.
Seeding hiPSCs for Differentiation (Day -3):
- Dissociate hiPSCs with Accutase to create a single-cell suspension [13].
- Resuspend cells in mTeSRplus medium supplemented with 10 µM Y-27632 (ROCK inhibitor).
- Seed cells at optimized densities onto Geltrex-coated plates:
Pre-differentiation Culture (Day -2):
- After 24 hours, remove the medium and replace it with fresh mTeSRplus without ROCK inhibitor. Incubate for another 24 hours [13].
DMSO Pre-conditioning (Day -1):
Initiation of Kidney Differentiation (Day 0):
Quantitative Outcomes and Analysis
Efficacy of DMSO Pre-conditioning
The success of the pre-conditioning protocol should be evaluated by assessing changes in pluripotency markers immediately after DMSO treatment and the subsequent enhancement of nephron progenitor markers during differentiation.
Table 3: Quantitative Effects of DMSO Pre-conditioning on Marker Expression
| Parameter | Control (No DMSO) | 1% DMSO | 2% DMSO | Measurement Method |
|---|---|---|---|---|
| Pluripotency Markers (after 24h) | High expression of TRA-1-60, TRA-1-81, SSEA3, SSEA4 [13] | Reduced expression [13] | Further reduced expression [13] | Flow Cytometry [13] |
| NPC Marker SIX2 (Day 9 of Diff.) | Baseline expression [9] | Enhanced expression [9] [13] | Enhanced expression [9] [13] | Immunofluorescence, Flow Cytometry [13] |
| Differentiation Efficiency | Standard efficiency towards tubular kidney organoids [9] | Improved efficiency [9] | Improved efficiency [9] | Morphological assessment, marker quantification |
Applications in Kidney Research
The implementation of DMSO pre-conditioning directly addresses the critical challenge of differentiation efficiency in kidney organoid generation [9] [21]. By reliably increasing the yield of SIX2-positive nephron progenitors, this protocol enhances the robustness of models for:
- Drug Nephrotoxicity Screening: Improved proximal tubule differentiation creates more physiologically relevant models for predicting drug-induced kidney injury [2] [21].
- Disease Modeling: Generating more consistent and representative organoids facilitates the study of genetic kidney diseases like polycystic kidney disease and CAKUT [2] [21].
- Regenerative Medicine: A higher fidelity in vitro model of nephron development provides a better foundation for exploring future cell-based therapies [4] [2].
Troubleshooting and Protocol Notes
- Cell Density is Critical: Adherence to the specified cell seeding densities for different hiPSC lines is vital for achieving optimal colony confluence and subsequent response to DMSO [13].
- DMSO Concentration: A 1-2% DMSO concentration range is effective. Higher concentrations may induce excessive cytotoxicity [9] [13].
- hiPSC Line Variability: Response to differentiation cues can vary between hiPSC lines. Testing multiple lines or pre-selecting lines with high differentiation potential is recommended [42] [21].
- Quality Control: Regularly monitor hiPSC morphology before DMSO treatment. The use of mycoplasma-free cultures and high-quality reagents is essential for reproducible results [42].
The presence of off-target, non-renal cell populations remains a significant challenge in the differentiation of kidney organoids from human pluripotent stem cells (hPSCs). Single-cell RNA sequencing (scRNA-seq) analyses have revealed that 10–20% of cells in typical kidney organoids are non-renal, primarily comprising neuronal clusters, muscle cells, and chondrocytes [15]. These off-target populations arise during differentiation despite adherence to established protocols, indicating incomplete lineage specification that can impact organoid maturation, functionality, and experimental reproducibility [15] [28]. This application note details the identification and minimization of these populations within the context of a stepwise monolayer protocol for kidney organoid differentiation, providing actionable strategies for quality improvement.
Identification and Characterization of Off-Target Cells
Comprehensive characterization of off-target populations is a prerequisite for their reduction. Single-cell transcriptomics serves as the gold standard for identifying the diversity and proportion of non-renal cells.
Common Off-Target Cell Types and Their Markers
The table below summarizes the primary off-target cell types identified in kidney organoids and their characteristic markers [15] [28].
Table 1: Common Off-Target Cell Types in Kidney Organoids
| Off-Target Cell Type | Characteristic Markers | Typical Proportion | Protocols Where Observed |
|---|---|---|---|
| Neuronal Cells | CRABP1 |
1-4 distinct clusters [15] | Takasato, Morizane [15] |
| Muscle Cells | MYLPF, MYOG |
Variable | Morizane (hESC & iPSC) [15] |
| Chondrocytes | SOX9, COL2A1, ACAN |
Increases with prolonged culture [28] | Takasato (especially after day 18) [28] |
| Melanocytes | MLANA, PMEL |
Rare/Protocol-specific | Takasato [15] |
Quantitative Analysis via scRNA-seq
Unsupervised clustering of scRNA-seq data from 83,130 cells derived from 65 organoids has been instrumental in defining these populations. Studies comparing protocols have found that while the Takasato protocol may generate up to 21% off-target cells, the Morizane protocol yields approximately 11%, though this varies between hESC and iPSC lines [15]. Pseudotemporal reconstruction of lineage relationships from this data can further identify key transcription factor networks and signaling pathways associated with fate decisions, revealing potential targets for intervention [15].
Experimental Protocols for Reduction of Off-Target Populations
Based on the molecular understanding of off-target origins, specific protocol modifications have been developed to suppress their development.
Protocol 1: Inhibition of the BDNF/NTRK2 Pathway to Reduce Neuronal Populations
Principle: During organoid differentiation, the brain-derived neurotrophic factor (BDNF) and its receptor NTRK2 are expressed in neuronal lineages. Inhibiting this pathway selectively reduces neuronal off-targets without affecting kidney differentiation [15].
Detailed Methodology:
- Organoid Differentiation: Differentiate kidney organoids from hPSCs (e.g., H9 hESC or BJFF.6 iPSC) using your preferred stepwise monolayer protocol (e.g., Takasato or Morizane) [15].
- Pharmacological Inhibition: At the stage where nephron progenitor patterns emerge (typically after 3D aggregation), add a selective NTRK2 inhibitor to the culture medium.
- Inhibitor Example: AFTAB (2-[(3-{[(2S)-2-aminopropy]]
- Working Concentration: 1 µM (optimization of dose and timing is recommended based on the specific protocol and cell line) [15].
- Treatment Duration: Maintain the inhibitor in the culture medium for 96 hours.
- Validation and Analysis:
- Immunofluorescence (IF): Stain organoids for neuronal markers (e.g., β-III-TUBULIN) and renal markers (e.g., NPHS1 for podocytes, LTL for proximal tubules) to confirm reduction of neurons and preservation of renal structures.
- scRNA-seq: Perform single-cell RNA sequencing on treated vs. control organoids. Analyze clusters for reduction in neuronal marker expression (
CRABP1) and calculate the percentage of remaining neuronal cells [15].
Expected Outcome: This treatment can lead to a ~90% reduction in neuronal cell populations within the organoids [15].
Protocol 2: Extended FGF9 Treatment to Reduce Chondrocytes
Principle: Chondrocyte formation is linked to sustained expression of the transcription factor SOX9. Extending exposure to FGF9, a key growth factor in kidney development, has been shown to suppress the chondrogenic pathway and prevent cartilage formation [28].
Detailed Methodology:
- Baseline Organoid Differentiation: Initiate kidney organoid differentiation from iPSCs using a standard Takasato-based protocol with CHIR99021 and FGF9 [28].
- Protocol Modification (Extended FGF9):
- Control Protocol: FGF9 supplementation is typically stopped at day 5 of the 3D differentiation phase (denoted as day 7+5).
- Modified Protocol: Continue supplementation with 200 ng/mL FGF9 for an additional week, until day 7+12 [28].
- Validation and Analysis:
- Histological Staining: Perform Alcian blue staining on organoid cryosections at day 7+25 to detect cartilage matrix. The modified protocol should show a clear reduction or absence of blue-stained cartilage nodules.
- Gene Expression Analysis: Conduct qPCR on organoids for chondrocyte markers
SOX9,COL2A1,ACAN,COL1A1, andCOL10A1. Expect a significant reduction in these transcripts in the FGF9-treated group. - Western Blot: Quantify protein levels of SOX9 and COL2A1, which should remain stable or show a reduced increase compared to controls.
- Immunofluorescence: Confirm that renal structures (NPHS1+ glomeruli, LTL+ proximal tubules, SLC12A1+ loops of Henle) are intact and unaffected by the extended treatment [28].
Expected Outcome: Organoids treated with extended FGF9 show a significant reduction in Alcian blue-positive cartilage areas and downregulation of chondrocyte markers at later time points (day 7+25), while maintaining robust renal differentiation [28].
The Scientist's Toolkit: Essential Research Reagents
The following reagents are critical for implementing the protocols described in this note.
Table 2: Key Research Reagents for Off-Target Cell Reduction
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| NTRK2 Inhibitor (e.g., AFTAB) | Selective inhibition of the BDNF/NTRK2 signaling pathway | Reduction of neuronal off-target cells in kidney organoids [15] |
| Recombinant Human FGF9 | Growth factor signaling to promote renal progenitor maintenance and suppress chondrogenesis | Extended treatment to prevent cartilage formation [28] |
| CHIR99021 | GSK3β inhibitor for canonical WNT pathway activation; induces posterior primitive streak | Initial step in directed differentiation of hPSCs to kidney organoids [4] [2] |
| Single-Cell RNA Sequencing (scRNA-seq) | Comprehensive characterization of cell populations and identification of off-target clusters | Quality control and validation of off-target reduction strategies [15] [4] |
| Antibody Panels (IF) | Validation of specific renal (NPHS1, LTL) and off-target (β-III-TUBULIN, COL2A1) cell types | Microscopic assessment of organoid composition and structure [15] [28] |
Schematic Workflows
Logical Workflow for Addressing Off-Target Cells
This diagram outlines the systematic approach to identifying and mitigating non-renal populations in kidney organoid cultures.
Extended FGF9 Treatment Experimental Timeline
This diagram illustrates the specific timeline for the protocol modification used to reduce chondrocyte formation.
The systematic reduction of off-target cells is essential for advancing the fidelity and translational potential of kidney organoid technology. By integrating scRNA-seq for rigorous characterization and implementing targeted protocol modifications—such as BDNF/NTRK2 pathway inhibition to curb neuronal populations and extended FGF9 treatment to prevent chondrogenesis—researchers can significantly improve the purity and quality of their renal models. These refined protocols provide a robust framework for generating more reliable systems for disease modeling, drug screening, and future regenerative medicine applications.
Benchmarking and Future Directions: Validating and Advancing Kidney Organoid Technology
The Power of Single-Cell RNA Sequencing for Cellular Validation
In the field of kidney organoid research, the stepwise monolayer differentiation of human pluripotent stem cells (hPSCs) into complex, three-dimensional tissues has emerged as a transformative approach for studying renal development, disease, and drug toxicity. However, the inherent cellular heterogeneity of these organoids presents a significant validation challenge. Single-cell RNA sequencing (scRNA-seq) has become an indispensable technology that provides unprecedented resolution for characterizing and validating the cellular composition of kidney organoids, ensuring that differentiation protocols yield the intended target populations and enabling rigorous quality control for downstream applications.
Kidney Organoid Generation via Monolayer Differentiation
The generation of kidney organoids from hPSCs relies on meticulously timed protocols that recapitulate key stages of embryonic kidney development. These protocols typically guide cells through intermediate mesoderm and metanephric mesoderm stages to form nephron progenitor cells (NPCs), which subsequently self-organize into organoids containing various renal structures [45] [27].
Core Differentiation Protocol
A foundational high-efficiency protocol generates NPCs within 9 days of monolayer differentiation from hPSCs with 80-90% efficiency [27]. The key stages are:
- Primitive Streak Induction (Days 1-3): Treatment with a GSK-3β inhibitor (CHIR99201) induces late primitive streak, preferentially directing differentiation toward posterior intermediate mesoderm [27].
- Intermediate Mesoderm Specification (Days 4-6): Cells express markers of intermediate mesoderm (PAX2, OSR1) [46].
- Nephron Progenitor Cell Formation (Days 7-9): High efficiency induction of SIX2+SALL1+WT1+PAX2+EYA1+ NPCs occurs [27].
- Kidney Organoid Maturation (Days 10-25): NPCs form renal vesicles that self-pattern into nephron structures containing podocytes, proximal tubules, loops of Henle, and distal tubules [45] [27].
Advanced Protocol for Proximal Tubule Biasing
Recent advancements enable the generation of "proximal-biased" kidney organoids with enhanced maturation of proximal tubule cells, which are crucial for nephrotoxicity testing [10]:
- PI3K Inhibition: Transient PI3K inhibition during early nephrogenesis activates Notch signaling.
- Axial Patterning Shift: This shifts nephron axial differentiation toward epithelial and proximal precursor states.
- Functional Maturation: Resulting proximal convoluted tubule cells broadly express solute carriers, including organic cation and organic anion transporters [10].
Table 1: Key Growth Factors and Small Molecules in Kidney Organoid Differentiation
| Component | Function | Protocol Stage | Concentration |
|---|---|---|---|
| CHIR99201 (GSK-3β inhibitor) | Induces primitive streak formation; specifies posterior intermediate mesoderm | Days 1-3 | Concentration varies by cell line (e.g., 3-12 μM) [27] |
| FGF9 | Promotes nephron progenitor cell expansion and maintenance | Days 4+ | Lower doses can be financially advantageous [27] |
| PI3K inhibitor | Shifts differentiation toward proximal tubule fates; activates Notch signaling | Early nephrogenesis | Varies by specific inhibitor [10] |
| BIO (GSK-3β inhibitor) | Alternative WNT activator for primitive streak induction | Days 1-3 | Used in two-step protocols [46] |
Single-Cell RNA Sequencing for Cellular Validation
scRNA-seq provides an unbiased, comprehensive method for validating the cell types present in kidney organoids, overcoming the limitations of traditional techniques like immunostaining and bulk RNA sequencing, which can only measure a few markers or provide averaged expression profiles [45].
scRNA-seq Wet Lab Workflow
The standard scRNA-seq workflow involves several critical steps [47]:
- Single-Cell/Nuclei Suspension: Preparation of high-quality, viable single-cell or single-nuclei suspensions from day 20-25 organoids. For difficult-to-dissociate tissues, single-nuclei RNA-seq (snRNA-seq) is advantageous [48] [47].
- Cell Capture and Barcoding: Using droplet-based microfluidics (e.g., 10x Genomics) or combinatorial indexing approaches to isolate individual cells and label their mRNA with cell-specific barcodes [48] [47].
- Library Preparation and Sequencing: Reverse transcription, amplification, and preparation of sequencing libraries, followed by high-throughput sequencing [45].
Table 2: Comparison of Key scRNA-seq Technologies for Organoid Validation
| Technology | Cell Isolation | Transcript Coverage | UMI | Amplification Method | Throughput | Best for Organoid Validation |
|---|---|---|---|---|---|---|
| Drop-Seq [48] | Droplet-based | 3'-end | Yes | PCR | High | High-throughput cell type inventory |
| inDrop [48] | Droplet-based | 3'-end | Yes | IVT | High | Cost-effective projects |
| Smart-Seq2 [48] | FACS | Full-length | No | PCR | Low | Detecting low-abundance transcripts, isoform analysis |
| Seq-Well [48] | Droplet-based | 3'-only | Yes | PCR | Portable | Applications requiring portability |
| SPLiT-Seq [48] | Not required | 3'-only | Yes | PCR | Very High (millions) | Fixed samples or extremely large cell numbers |
Dry Lab Data Analysis Pipeline
Following sequencing, data analysis typically proceeds through these steps [47]:
- Quality Control and Filtering: Removal of low-quality cells, doublets, and cells with high mitochondrial RNA content.
- Normalization and Dimensionality Reduction: Normalizing counts and using PCA for dimensionality reduction.
- Clustering and Cell Type Annotation: Unsupervised clustering (e.g., Louvain, Leiden) and annotation of cell types using known marker genes [49].
- Advanced Analyses:
- Differential Expression: Identifying genes significantly different between conditions or clusters.
- Trajectory Inference: Reconstructing developmental lineages and cellular differentiation paths.
- Ligand-Receptor Analysis: Identifying potential cell-cell communication events.
Diagram 1: Organoid Differentiation & scRNA-seq Validation Workflow (Width: 760px)
Key Applications of scRNA-seq in Kidney Organoid Research
Identifying and Eliminating Off-Target Cells
A critical application of scRNA-seq is identifying non-renal "off-target" cells, such as neurons and melanocytes, which frequently arise in organoids regardless of the protocol used [45]. In one case study:
- Analysis: scRNA-seq with pseudo-temporal ordering revealed strong expression of brain-derived neurotrophic factor (BDNF) and its receptor NTRK2 specifically in off-target neuronal populations [45].
- Intervention: Adding an NTRK2 inhibitor (K252a) to the differentiation protocol reduced off-target neurons by 90% [45].
- Impact: This demonstrates how scRNA-seq data can directly guide protocol improvements to enhance purity.
Assessing Cellular Maturation States
scRNA-seq enables direct comparison of organoid cells to human fetal and adult kidney reference datasets, objectively evaluating maturation status [45] [10]. Studies consistently show that conventional organoids (day 20-25) exhibit gene expression patterns comparable to first-trimester fetal kidneys rather than adult tissue, highlighting a key limitation and target for improvement [45].
Validating Disease Modeling and Nephrotoxicity Platforms
scRNA-seq confirms that organoids respond to injury in a segment-specific manner, validating their use for disease modeling and toxicology studies [45] [10]. For example:
- Proximal Tubule Injury: Treatment with cisplatin induces both HAVCR1/KIM1 (proximal tubule marker) and NGAL (expressed in thick ascending limbs and collecting ducts) in more advanced organoid models [45].
- Segment-Specific Validation: scRNA-seq verifies that HAVCR1 protein localizes apically in LTL-positive proximal tubules, while NGAL is specifically induced in ECAD-positive distal tubules, confirming a physiologically relevant injury response [45].
Diagram 2: scRNA-seq Data Analysis Pipeline (Width: 760px)
The Scientist's Toolkit: Essential Reagents and Solutions
Table 3: Research Reagent Solutions for Kidney Organoid scRNA-seq
| Category | Specific Product/Kit | Function in Workflow |
|---|---|---|
| Cell Dissociation | Collagenase IV, Trypsin-EDTA, Accumax | Enzymatic digestion of organoids into single-cell suspensions [47] |
| Viability Staining | Propidium Iodide, DAPI, Calcein AM | Distinguishing live vs. dead cells for FACS sorting [47] |
| scRNA-seq Library Prep | 10x Genomics Chromium Single Cell 3' Reagent Kit | Droplet-based single cell capture, barcoding, and library preparation [48] [47] |
| Nuclei Isolation | SNUC-13 Nuclei Isolation Kit (custom protocols also used) | Preparation of nuclei suspensions for snRNA-seq from frozen tissue [48] |
| Cell Culture | Recombinant FGF9, CHIR99201, BIO | Key signaling molecules directing differentiation to kidney lineage [27] [46] |
| Cell Sorting | Anti-KSP (Cadherin 16) Antibody | Purification of kidney tubular cells via FACS for specialized applications [46] |
Single-cell RNA sequencing has revolutionized quality control and validation in kidney organoid research by providing an unbiased, high-resolution platform for comprehensive cellular characterization. Its integration with stepwise monolayer differentiation protocols enables researchers to precisely identify cellular composition, assess maturation status, eliminate off-target populations, and validate disease models with unprecedented accuracy. As kidney organoids continue to advance toward more mature and complex structures, scRNA-seq will remain an essential tool for driving protocol improvements and ensuring the reliability of these powerful models for developmental biology, disease modeling, and drug discovery applications.
Within stem cell and regenerative medicine research, the differentiation of pluripotent stem cells (PSCs) into kidney organoids represents a significant advancement for modeling development, disease, and nephrotoxicity. A critical factor determining the success of these applications is the initial differentiation methodology. This application note provides a comparative analysis of the stepwise monolayer protocol against other common differentiation methods, with a specific focus on scalability, reproducibility, and functional outcomes in kidney organoid research. The stepwise monolayer protocol directs human pluripotent stem cells through a two-dimensional (2D) differentiation sequence that recapitulates key developmental stages—primitive streak, intermediate mesoderm, and metanephric mesenchyme—before transitioning to three-dimensional (3D) culture for nephron formation [4] [2]. We present structured quantitative data, detailed experimental protocols, and signaling pathway visualizations to guide researchers in selecting and optimizing differentiation strategies for their specific projects.
Tabular Comparison of Differentiation Methods
The following table summarizes the core characteristics, advantages, and limitations of the major kidney organoid differentiation protocols.
Table 1: Comparative Overview of Kidney Organoid Differentiation Methods
| Method Feature | Stepwise Monolayer Protocol | 3D Aggregate Differentiation | Adult Progenitor-Based |
|---|---|---|---|
| Principle | Sequential 2D differentiation followed by 3D aggregation [2] | Direct 3D aggregation of PSCs with staged biochemical cues [4] | Expansion and self-organization of tissue-resident renal stem cells [2] |
| Key Steps | 1. 2D monolayer differentiation2. Dissociation & 3D spheroid formation3. Free-floating culture [4] | 1. 3D spheroid formation from PSCs2. Direct differentiation in suspension [4] | 1. Isolation of kidney stem cells2. 3D culture with growth factor cocktail [2] |
| Differentiation Fidelity | High, due to controlled, sequential patterning [2] | Moderate, can exhibit higher variability [4] | High for tubular structures, limited for glomeruli |
| Scalability | High, amenable to large-scale production [4] [50] | Moderate, limited by aggregation efficiency | Lower, dependent on primary cell availability |
| Reproducibility | High, offers uniform cell-to-cell contact [4] | Variable, influenced by initial spheroid size and homogeneity [4] | Moderate |
| Relative Cost | Moderate | Moderate | Low |
| Typical Maturation Level | Develops segmented nephrons; requires further maturation for adult phenotypes [2] | Develops nephron-like structures; can be immature [4] | Generates tubular organoids; limited nephron segmentation |
Quantitative Data from Key Studies
The methodological choice significantly impacts the cellular composition and transcriptional profile of the resulting organoids. Systematic studies comparing different initial seeding conditions within a monolayer-based approach reveal critical quantitative differences.
Table 2: Impact of Initial Seeding Density on Organoid Composition
| Analysis Parameter | 500-Cell Spheroids | 8,000-Cell Spheroids | 100,000-Cell Spheroids | 250,000-Cell Spheroids |
|---|---|---|---|---|
| PAX2+LHX1+ Renal Vesicles | Higher number [4] | Higher number [4] | Reduced number [4] | Reduced number [4] |
| Podocyte Marker Expression (TCF21, NPHS2, MAFB) | Increased [4] | Intermediate | Reduced | Reduced |
| Proportion of Stromal-like Cells | Less abundant [4] | Less abundant [4] | More abundant [4] | More abundant [4] |
| Metallothionein Expression in Tubular Cells | Increased [4] | Intermediate | Reduced | Reduced |
| Transcriptional Variety (per scRNA-seq) | High, with distinct renal lineages [4] | High, with distinct renal lineages [4] | High, with distinct renal lineages [4] | High, with distinct renal lineages [4] |
Detailed Experimental Protocols
Stepwise Monolayer Protocol for Kidney Organoid Differentiation
The following protocol, adapted from recent literature, details the generation of kidney organoids via a stepwise monolayer system [4] [2].
Key Research Reagent Solutions:
- Basal Medium: Advanced RPMI 1640
- Small Molecule Inhibitor: CHIR99021 (a GSK3β inhibitor activating WNT signaling)
- Growth Factors: FGF9, Activin A
- Cell Dissociation Reagent: Trypsin/EDTA or a gentle cell dissociation enzyme
- Coating Matrix: Vitronectin or a comparable extracellular matrix protein
Procedure:
- Culture and Maintenance of hPSCs: Maintain human PSCs (e.g., iPSCs or ESCs) in a feeder-free culture on vitronectin-coated plates using Essential 8 medium. Ensure cells are in a state of active, undifferentiated proliferation before initiating differentiation.
- Primitive Streak and IM Induction (Day -4 to Day 0):
- On day -4, seed hPSCs as a single-cell suspension at a density of 1–2 × 10^5 viable cells per well of a vitronectin-coated 24-well plate.
- The next day (day -3), initiate differentiation by replacing the medium with Advanced RPMI 1640 containing 8 μM CHIR99021 to direct cells toward a posterior primitive streak fate.
- Refresh the CHIR99021-containing medium daily for three days.
- On day -1, switch the medium to Advanced RPMI 1640 supplemented with 200 ng/mL FGF9, 1 μg/mL heparin, and 10 ng/mL Activin A to pattern the cells into intermediate mesoderm. Culture for 24 hours.
- 3D Spheroid Formation (Day 0):
- On day 0, treat the IM-committed monolayer cultures with 5 μM CHIR99021 for 1 hour while maintaining FGF9 signaling.
- Dissociate the cells into a single-cell suspension using a cell dissociation reagent.
- Seed the cells into V-bottom 96-well plates to promote self-aggregation. Critical parameter: The seeding density per well can be optimized (e.g., 500 to 250,000 cells) to influence final organoid composition, as shown in Table 2 [4].
- Renal Vesicle and Nephron Patterning (Day 0 to Day 7):
- Maintain the 3D spheroids in free-floating culture in medium containing FGF9 for 7 days to promote the formation of renal vesicles (RVs). This stage should yield spheroids with numerous PAX2+ and LHX1+ RVs.
- Terminal Differentiation (Day 7 to Day 16):
- From day 7 to day 16, culture the organoids in basal Advanced RPMI 1640 medium without additional growth factors to allow for terminal differentiation into nephron-like structures.
- The resulting organoids should contain segmented structures, including podocyte-like cells (PODXL+, WT1+), proximal tubule-like structures (LTL+), distal tubule-like structures (ECAD+), and endothelial-like cells (CD31+) [4].
Protocol for Functional Analysis: ALP Release Electrochemical Detection
Alkaline phosphatase (ALP) activity is a functional marker for certain renal cell types and can be quantified sensitively using electrochemical detection [51].
Key Research Reagent Solutions:
- Graphite Screen-Printed Electrodes (graphite-SPE): For electrochemical measurements.
- Assay Buffer: Diethanolamine (DEA) 1 M, MgCl₂ 8 mM, NaCl 50 mM, KCl 100 mM, pH 9.5.
- Enzyme Substrate: para-Aminophenyl Phosphate (p-APP).
- Cell Culture Media: Appropriate for cell line (e.g., DMEM, MEME).
Procedure:
- Cell Culture and ALP Release:
- Culture relevant cells (e.g., embryonic or carcinoma cell lines) as a monolayer in 48-well plates until confluent (e.g., 4 days), changing media every two days [51].
- Wash the cell monolayer twice with Hank's Balanced Salt Solution (HBSS).
- Incubate the cells with the assay buffer (70 μL is sufficient) to release ALP.
- Electrode Preparation:
- Clean graphite screen-printed electrodes (graphite-SPE) using a plasma cleaner for 20 minutes to enhance performance.
- Electrochemical Measurement:
- Mix 30 μL of the sample (released ALP) with 100 μM of p-APP substrate in the assay buffer.
- Incubate for 10 minutes at room temperature to allow the enzymatic reaction to proceed, producing the electroactive product p-aminophenol (p-AP).
- Place a 70 μL droplet of the reaction mixture onto the prepared graphite-SPE.
- Perform Linear Sweep Voltammetry (LSV) with a potential range from -1.2 V to 1.5 V (vs. Ag/AgCl reference) at a scan rate of 100 mV/s.
- The measured current is proportional to the p-AP concentration, which in turn reflects ALP activity. This method offers a high dynamic range (1.5 to 1500 U/L) and is ideal for small-volume samples [51].
Signaling Pathways in Kidney Organoid Differentiation
The stepwise monolayer protocol meticulously recapitulates key developmental signaling cascades. The following diagram illustrates the core pathways activated during directed differentiation.
Diagram 1: Signaling in Kidney Organoid Differentiation.
This workflow is governed by specific molecular pathways whose precise activation is critical for successful differentiation [2]:
- WNT/β-catenin signaling: Initially activated using CHIR99021, it drives the formation of the primitive streak and posterior fate. Later, endogenous WNT signaling (e.g., WNT9b, WNT4) is crucial for the mesenchymal-to-epithelial transition (MET) that forms renal vesicles [2].
- FGF signaling: FGF9 is a key factor for patterning the intermediate mesoderm and supporting the survival and expansion of nephron progenitor cells within the metanephric mesenchyme [2].
- Activin/Nodal and BMP signaling: These pathways support the specification and maturation of the intermediate mesoderm. BMP7 is sometimes included in protocols to enhance this process and mimic developmental cues [2].
- Notch signaling: This pathway plays a critical role later in differentiation, guiding the segmentation of the nephron into distinct segments such as proximal and distal tubules [2].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Kidney Organoid Differentiation and Characterization
| Reagent Category | Specific Example | Function in Protocol |
|---|---|---|
| Small Molecule Agonists/Antagonists | CHIR99021 | GSK3β inhibitor; activates WNT signaling to induce primitive streak and IM [4] [2]. |
| Recombinant Growth Factors | FGF9, Activin A, BMP7 | Patterns IM; maintains nephron progenitors; supports mesodermal induction [4] [2]. |
| Extracellular Matrix & Culture Aids | Vitronectin, V-bottom plates | Provides adhesion surface for 2D monolayer; forces cell aggregation for 3D spheroid formation [4]. |
| Cell Characterization & Isolation | Anti-PAX2, Anti-LHX1, Anti-LTL, Anti-PODXL | Immunofluorescence markers for identifying renal vesicles, proximal tubules, and podocytes [4]. |
| Advanced Analysis Tools | Single-cell RNA sequencing | Deep phenotypic analysis of cellular heterogeneity and transcriptional maturity in organoids [4]. |
| Functional Assay Reagents | p-APP (para-Aminophenyl Phosphate) | Enzyme substrate for electrochemical detection of Alkaline Phosphatase (ALP) activity [51]. |
Within the context of kidney organoid differentiation research using stepwise monolayer protocols, functional assays are indispensable for validating the maturity and physiological relevance of the generated tissues. The directed differentiation of human pluripotent stem cells (hPSCs) into kidney organoids recapitulates developmental processes, resulting in complex structures containing segmented nephrons, collecting ducts, renal interstitial cells, and endothelial networks [31]. For researchers and drug development professionals, confirming that these organoids possess functional transporter activity and appropriate barrier function is crucial for applications in disease modeling, nephrotoxicity testing, and regenerative medicine. This application note details established methodologies for evaluating these key functional parameters, with a specific focus on transporter activity assessment and barrier integrity validation.
Kidney Organoid Differentiation: A Foundational Protocol
The generation of kidney organoids via a stepwise monolayer protocol provides the essential foundation for subsequent functional assays. This methodology simultaneously induces four progenitor populations—nephron progenitors, ureteric epithelial progenitors, renal interstitial progenitors, and endothelial progenitors—to generate kidney organoids with segmented nephrons connected to collecting ducts [31].
Core Differentiation Workflow
The standard protocol consists of two main phases [31]:
- Days 1-7: Monolayer Culture for Mesoderm Induction: 7 days of monolayer culture for intermediate mesoderm induction.
- Days 8-25: Three-Dimensional Culture: 18 days of three-dimensional culture to facilitate self-organizing renogenic events leading to organoid formation.
Recent methodological advancements demonstrate that pretreatment of human induced pluripotent stem cells (hiPSCs) with low-dose dimethyl sulfoxide (1-2% DMSO) can enhance the expression of the key metanephric mesenchyme nephron progenitor marker SIX2 after 9 days of kidney organoid differentiation, thereby improving protocol efficiency [9].
Key Signaling Pathways in Kidney Organoid Differentiation
The differentiation process meticulously recapitulates kidney development through sequential modulation of key signaling pathways. The following diagram illustrates the core signaling pathway involved in the early stages of kidney organoid differentiation:
Figure 1: Signaling Pathway in Kidney Organoid Differentiation. The stepwise differentiation from hPSCs to kidney organoids requires precise temporal activation of key signaling pathways, including WNT, BMP, and FGF signaling.
Transporter Activity Assays
Solute carrier (SLC) transporters represent the largest family of membrane transporters in the human genome, with over 400 members divided into more than 60 families [52] [53]. These transporters are responsible for the cellular uptake and efflux of a wide spectrum of molecules including nutrients, metabolites, ions, and pharmaceutical compounds. In the kidney, SLC transporters play critical roles in reabsorption and secretion processes, making their functional assessment essential in kidney organoid research.
Fundamentals of SLC Transporter Biology
SLC transporters operate through two primary mechanisms [52]:
- Facilitative transport: Movement of compounds along their concentration gradient
- Secondary active transport: Coupling substrate movement to ion gradients (typically Na+, H+, or Cl-)
This transport mechanism diversity necessitates different assay approaches, particularly for electrogenic versus electroneutral transporters.
SLC Transporter Assay Technologies
The table below summarizes the primary assay technologies available for evaluating SLC transporter function in cellular systems, including kidney organoids:
Table 1: SLC Transporter Assay Technologies for Functional Analysis
| Assay Type | Measured Parameter | Compatible Transporter Types | Key Applications in Kidney Research |
|---|---|---|---|
| Sodium-Dependent Assay | Sodium flux using fluorescent indicators (e.g., ING-2 AM) | Electrogenic and electroneutral Na+-coupled transporters (SLC1, SLC5, SLC6 families) | Nutrient reabsorption, neurotransmitter transport |
| Membrane Potential Assay | Changes in membrane potential | Electrogenic transporters only | High-throughput screening of modulator compounds |
| Thallium Flux Assay | Thallium flux as chloride surrogate | SLC12 family (cation-chloride cotransporters) | Cell volume regulation, salt transport |
| Intracellular pH Assay | pH changes using ratiometric indicators (e.g., BCECF AM) | Proton-coupled transporters (SLC15, SLC2 families) | Peptide transport, sugar alcohol transport |
| Endocytosis Assay | Uptake of fluorescent substrates (e.g., albumin-megalin mediated) | Endocytic receptors in proximal tubules | Protein reabsorption function |
Nephrotoxicity Assessment via Transporter Function
A key application of transporter assays in kidney organoid research is nephrotoxicity assessment. Cisplatin-induced toxicity serves as a validated model for evaluating proximal tubule maturity and function in kidney organoids. The following workflow illustrates the cisplatin nephrotoxicity assay:
Figure 2: Cisplatin Nephrotoxicity Assay Workflow. This assay validates proximal tubule function in kidney organoids by demonstrating cisplatin uptake through basolateral organic cation transporter 2 (OCT2) and copper transporter 1 (CTR1), leading to apoptosis.
Research has demonstrated that mature kidney organoids contain proximal tubules with sufficient functional maturity to respond appropriately to cisplatin, evidenced by basolateral organic cation transporter 2 (OCT2) and copper transporter 1 (CTR1) expression that mediate cisplatin uptake, ultimately leading to apoptosis [31].
Barrier Function Assessment
Barrier function represents another critical parameter of kidney organoid maturity, particularly for modeling the selective filtration and reabsorption capabilities of native renal tissue.
Endocytic Function in Proximal Tubules
A key barrier function in renal proximal tubules is the receptor-mediated endocytosis of proteins, primarily through the megalin-cubilin system. In kidney organoids, functional proximal tubules display megalin-mediated and cubilin-mediated endocytosis, which can be assessed using fluorescently-labeled substrates such as albumin [31].
Transwell-Based Barrier Integrity Assays
For assessing epithelial barrier formation in kidney organoids, transepithelial electrical resistance (TEER) measurements and permeability assays using Transwell systems provide quantitative data on barrier integrity. The methodology involves:
- Transferring day 7 intermediate mesoderm aggregates to Transwell filters
- Culturing at air-media interface for 18 days
- Measuring TEER values using epithelial volt-ohm meters
- Performing permeability assays with fluorescent tracers of varying molecular weights
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of functional assays for kidney organoid research requires specific reagents and tools. The following table details essential components:
Table 2: Essential Research Reagents for Kidney Organoid Functional Assays
| Reagent/Category | Specific Examples | Function in Assays |
|---|---|---|
| Ion-Sensitive Fluorescent Dyes | ING-2 AM (sodium), BCECF AM (pH), Thallos AM (thallium) | Direct measurement of ion flux in SLC transporter assays |
| Membrane Potential Dyes | FMP dyes, DiBAC4(3) | Detection of changes in membrane potential in electrogenic transporters |
| SLC Transporter Substrates | Glutamate (for EAAT2/SLC1A2), Neurotransmitters (for SLC6 family) | Validation of transporter activity and inhibition studies |
| Nephrotoxicants | Cisplatin (5-20 μM), Gentamicin | Assessment of proximal tubule maturity and toxicity response |
| Endocytic Tracers | Fluorescently-labeled albumin, dextrans | Evaluation of megalin-cubilin mediated endocytosis in proximal tubules |
| Cell Viability Assays Caspase-3/7 assays, LDH release, ATP content | Quantification of apoptosis and cell death in toxicity studies | |
| SLC Modulator Compounds | Specific inhibitors/activators for target SLCs | Validation of assay specificity and mechanism of action studies |
The integration of functional assays for transporter activity and barrier function evaluation is essential for validating kidney organoids generated through stepwise monolayer protocols. These assays provide critical evidence of physiological relevance, enabling applications in disease modeling, drug screening, and nephrotoxicity assessment. The continued refinement of these functional assessment methodologies, coupled with advancements in kidney organoid differentiation protocols, will further enhance the utility of these systems in both basic research and pharmaceutical development.
The stepwise monolayer protocol for kidney organoid differentiation has established a robust foundation for generating nephron-like structures from human induced pluripotent stem cells (hiPSCs). However, conventional static culture methods often result in organoids with immaturity, limited vascularization, and functional deficiencies, restricting their translational applications. The integration of kidney organoids with microfluidic chip technologies represents a paradigm shift, addressing these limitations by providing dynamic microenvironments that enhance physiological relevance. This approach leverages biomechanical and biochemical cues to promote improved cellular differentiation, structural organization, and functional maturation, creating more predictive models for disease modeling and drug development [54] [55].
Microfluidic platforms, often termed organ-on-a-chip devices, enable precise control over the cellular microenvironment through the application of fluid shear stress, mechanical stretching, and biochemical gradients. These systems facilitate enhanced nutrient delivery, waste removal, and vascular network formation – critical factors currently limiting kidney organoid technology. Recent advances demonstrate that integrating organoids with microfluidic devices generates more physiologically relevant models for investigating renal transporter function, nephrotoxicity, drug-drug interactions, and genetic kidney diseases, thereby bridging the gap between traditional in vitro models and in vivo physiology [56] [54] [55].
Quantitative Foundation: Relationship Between Initial Conditions and Organoid Composition
The reproducibility and cellular composition of kidney organoids are significantly influenced by initial differentiation parameters. Systematic investigation of cell seeding numbers in free-floating culture conditions reveals profound effects on resulting organoid structure and composition, providing crucial quantitative guidance for protocol optimization.
Table 1: Impact of Initial Cell Seeding Number on Kidney Organoid Development
| Initial Cell Number per Spheroid | Renal Vesicle Formation (PAX2+LHX1+) | Podocyte-like Cells | Tubule-like Cells | Endothelial-like Cells | Stromal-like Cells |
|---|---|---|---|---|---|
| 500 | ++++ (Most abundant) | ++++ | ++++ | ++++ | + |
| 8,000 | +++ | +++ | +++ | +++ | ++ |
| 100,000 | ++ | ++ | ++ | ++ | +++ |
| 250,000 | + (Least abundant) | + | + | + | ++++ |
Analysis of these conditions demonstrates that intermediate cell numbers (500-8,000 cells per spheroid) promote superior development of nephron structures, including renal vesicles and segmented nephron components, while higher cell numbers (100,000-250,000) result in increased stromal cell populations and reduced epithelial differentiation [4]. Single-cell RNA sequencing confirmed that organoids derived from 500 and 8,000 cell spheroids contained higher proportions of podocyte-like, endothelial-like, and tubular-like cells, with correspondingly lower stromal cell abundance – a pattern associated with improved kidney maturation [4].
Table 2: Functional Advantages of Microfluidic Culture Systems for Kidney Organoids
| Parameter | Static Culture | Microfluidic Chip | Functional Significance |
|---|---|---|---|
| Vascularization | Limited, regressing over time | Enhanced, perfusable vessels | Improves nutrient delivery, maturation, and barrier function |
| Glucose Uptake | Baseline | 2.5-3.5 fold increase | Indicates enhanced metabolic activity |
| Transporter Expression | Low | Significantly upregulated | Improves drug transport prediction and nephrotoxicity assessment |
| Oxidative Stress Response | Moderate | Enhanced detection sensitivity | Better prediction of drug-induced injury |
| Gene Expression Markers | Variable, immature patterns | Mature fetal kidney signatures | Induces developmental maturation pathways |
The quantitative advantages of microfluidic systems are particularly evident in disease modeling applications. For Fabry disease kidney organoids, microfluidic gradient chip systems demonstrated significantly enhanced detection of therapeutic effects following enzyme replacement therapy, with improved restoration of physiological characteristics compared to static cultures [54].
Experimental Protocols: Microfluidic Integration for Enhanced Organoid Maturation
Microfluidic Gradient Chip Protocol for Kidney Organoids
This protocol establishes a method for enhancing the maturation and functionality of kidney organoids through integration with a microfluidic gradient chip system, optimized for both normal and disease modeling applications [54].
Materials:
- PDMS microfluidic chip with gradient generators
- Peristaltic or syringe pump system
- Differentiated kidney organoids (day 16-18)
- Renal epithelial cell medium
- Matrigel or collagen I hydrogel
- Fabry disease hiPSC-derived organoids (for disease modeling)
Method:
- Organoid Preparation: Differentiate kidney organoids using established stepwise monolayer protocols until day 16-18, ensuring presence of segmented nephron structures.
- Hydrogel Embedding: Mix pre-cooled Matrigel with dispersed organoid fragments at 4°C in a 3:1 ratio (Matrigel:organoid suspension).
- Chip Loading: Introduce the organoid-hydrogel mixture into the microfluidic chamber through injection ports, avoiding bubble formation.
- Gradient Establishment: Program the pump system to generate a continuous flow of 100-200 μL/hour, creating a biochemical gradient across the chamber.
- Long-term Culture: Maintain organoids under flow conditions for 10-14 days, with medium renewal every 48 hours.
- Functional Assessment: Evaluate vascularization (CD31 immunostaining), glucose uptake (fluorescence glucose analogs), and gene expression (qPCR for mature renal markers) at experimental endpoints.
Troubleshooting:
- Poor viability: Reduce flow rate to 50-100 μL/hour during initial 3 days
- Limited vascularization: Supplement with 50 ng/mL VEGF in medium
- Gradient instability: Verify pump calibration and check for chamber leaks
Proximal Tubule-on-Chip Model from hiPSC-Derived Organoids
This protocol describes the generation of a proximal tubule-on-chip model specifically designed for renal transporter analysis and nephrotoxicity assessment [56].
Materials:
- Two-channel microfluidic device (0.2-0.5 mm channel width)
- Collagen IV-coated porous membranes (5 μm pores)
- Proximal tubule cell isolation kit (CD13/CD26 magnetic beads)
- Transwell inserts (3 μm pores)
- Renal transporter substrates (fluorescently labeled)
Method:
- Proximal Tubule Cell Isolation:
- Dissociate day 18-21 kidney organoids with collagenase IV (1 mg/mL, 37°C, 15 min)
- Isolate proximal tubule cells using positive selection with CD13/CD26 magnetic beads
- Centrifuge at 300 × g for 5 min and resuspend in renal epithelial growth medium
Chip Seeding and Culture:
- Seed isolated cells (2.5 × 10^6 cells/mL) into the apical channel of the microfluidic device
- Allow cell attachment for 6 hours under static conditions
- Initiate unidirectional flow (50 μL/hour, gradually increasing to 200 μL/hour over 3 days)
- Culture for 7-10 days until confluent, polarized monolayers form
Functional Validation:
- Assess transporter function using fluorescent substrates (1 μM each)
- Measure albumin uptake (10 μg/mL FITC-albumin, 37°C, 30 min)
- Evaluate nephrotoxicity with cisplatin (50 μM, 24 hours) and measure cell viability
Validation Parameters:
- Transporter activity (≥2-fold increase over static culture)
- Albumin uptake efficiency (≥60% improvement)
- Tight junction formation (ZO-1 immunostaining)
- Apical-basal polarity (acetylated tubulin staining)
Signaling Pathways and Experimental Workflows
Diagram 1: Integrated Workflow for Kidney Organoid Differentiation and Microfluidic Maturation
Diagram 2: Signaling Pathways in Microfluidic-Induced Vascular Maturation
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for Kidney Organoid-Microfluidic Integration
| Reagent/Category | Specific Examples | Function/Application | Protocol Specifications |
|---|---|---|---|
| hiPSC Lines | LUMCi004-C, TISSUi001-A, TISSUi007-A, HEL124 (GRACILE) | Disease modeling, protocol standardization | Ethics approval: LUMC0031iCTRL08, HUS 77/E7/2007 [9] [42] |
| Differentiation Factors | CHIR99021 (GSK3β inhibitor), FGF9, Heparin, Activin A | Sequential induction of renal lineages | CHIR99021: 8μM (3 days), FGF9: 200ng/mL + Heparin: 1μg/mL + Activin A: 10ng/mL (24h) [4] |
| Microfluidic Systems | Gradient generators, Perfusion chips, Two-channel devices | Provide biomechanical cues, perfusion | Flow rate: 100-200μL/hour, 0.2-0.5mm channel width [56] [54] |
| Matrix Materials | Matrigel, Collagen I, Collagen IV | 3D structural support, polarized growth | 3:1 ratio with organoid fragments, collagen IV coating for tubules [56] [54] |
| Cell Isolation | CD13/CD26 magnetic beads, CD31 FACS sorting | Proximal tubule and endothelial cell isolation | Positive selection after collagenase IV dissociation [56] [57] |
| Functional Assays | Fluorescent albumin, Transporter substrates, Glucose analogs | Assessment of maturation and functionality | FITC-albumin: 10μg/mL, transporter substrates: 1μM [56] [54] |
The integration of kidney organoids with microfluidic chip technology represents a transformative approach that addresses critical limitations in organoid maturation, reproducibility, and functionality. By providing precisely controlled biomechanical and biochemical cues, these systems promote enhanced vascularization, improved cellular differentiation, and more physiologically relevant function. The protocols and analytical frameworks presented here provide researchers with standardized methods for implementing these advanced culture systems, enabling more predictive disease modeling and drug screening applications. As the field progresses, further innovations in multi-organ integration, sensor incorporation, and automated analysis will continue to enhance the translational potential of kidney organoid technology, ultimately bridging the gap between in vitro models and clinical applications.
Conclusion
The stepwise monolayer protocol for kidney organoid differentiation has established a robust platform for studying human kidney development, disease mechanisms, and drug-induced toxicity. By faithfully recapitulating key developmental stages, this method generates complex, multi-cellular structures that are invaluable for biomedical research. Ongoing challenges, such as achieving full functional maturity and reducing off-target cell types, are being addressed through innovative strategies like DMSO pre-conditioning and bioengineering. The integration of advanced validation tools, particularly single-cell transcriptomics, ensures the fidelity of these models. Looking ahead, the convergence of protocol refinement, biohybrid systems like organ-on-a-chip technology, and CRISPR-based genome editing will further enhance the physiological relevance of kidney organoids. This progress solidifies their role not only as powerful research tools but also as a promising foundation for future regenerative medicine therapies, ultimately bridging the gap between in vitro models and clinical applications for kidney disease.
References
- 1. Optimizing Nodal, Wnt and BMP signaling pathways for robust ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11182123/]
- 2. Kidney Organoids: Current Advances and Applications [https://www.mdpi.com/2075-1729/15/11/1680]
- 3. DevKidCC allows for robust classification and direct ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-022-01023-z]
- 4. Systematic production of human kidney organoids for ... [https://www.nature.com/articles/s41551-025-01542-1]
- 5. Wnt signaling pathways in biology and disease [https://www.nature.com/articles/s41392-025-02142-w]
- 6. Wnt signaling in kidney: the initiator or terminator? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7591426/]
- 7. Developmental signalling pathways in renal fibrosis: the roles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5529143/]
- 8. The FGF, TGFβ and WNT axis Modulate Self-renewal of ... [https://www.nature.com/articles/s41598-020-57723-2]
- 9. Dimethyl Sulfoxide Conditions Induced Pluripotent Stem ... [https://pubmed.ncbi.nlm.nih.gov/40965814/]
- 10. Controlling nephron precursor differentiation to generate ... [https://www.nature.com/articles/s41467-025-63107-9]
- 11. Expansion of human pluripotent stem cell-induced nephron ... [https://pubmed.ncbi.nlm.nih.gov/40883437/]
- 12. Regulation of Nephron Progenitor Cell Self-Renewal by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5661282/]
- 13. Dimethyl Sulfoxide Conditions Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504399/]
- 14. Long-term viable chimeric nephrons generated from ... [https://www.nature.com/articles/s42003-023-05484-9]
- 15. Comparative analysis and refinement of human PSC-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6324730/]
- 16. Single cell census of human kidney organoids shows ... [https://www.nature.com/articles/s41467-019-13382-0]
- 17. Kidney Organoids as Disease Models: Strengths, ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.563981/full]
- 18. Integrating collecting systems in human kidney organoids ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925001432]
- 19. Unlocking the full potential of human pluripotent stem cell ... [https://pubmed.ncbi.nlm.nih.gov/40280411/]
- 20. Unlocking the full potential of human pluripotent stem cell ... [https://www.sciencedirect.com/science/article/pii/S0085253825003278]
- 21. Progress of Induced Pluripotent Stem Cell-Derived Renal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11908814/]
- 22. Generate hPSC-Derived 3D Kidney Organoids [https://www.stemcell.com/generate-3d-kidney-organoids.html]
- 23. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 24. The differentiation state of small intestinal organoid models ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1508820/full]
- 25. A deep learning approach to predict differentiation ... [https://www.nature.com/articles/s42003-024-07109-1]
- 26. A strategy for generating kidney organoids: recapitulating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6186756/]
- 27. Generation of nephron progenitor cells and kidney ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5278902/]
- 28. FGF9 treatment reduces off-target chondrocytes from iPSC- ... [https://www.nature.com/articles/s41536-025-00428-9]
- 29. Generation of Kidney Organoids from hPSCs [https://www.tocris.com/resources/protocols/organoids/generation-kidney-organoids-hpscs]
- 30. Guidelines for Manufacturing and Application of Organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC11170122/]
- 31. Generating kidney organoids from human pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5113819/]
- 32. Identification of podocyte molecular markers in diabetic ... [https://pubmed.ncbi.nlm.nih.gov/40690456/]
- 33. Podocytes - Latest research and news [https://www.nature.com/subjects/podocytes]
- 34. Proximal tubule cells contribute to the thin descending limb of ... [https://pubmed.ncbi.nlm.nih.gov/39868227/]
- 35. Protocol to develop a proximal tubule-on-chip model based ... [https://www.sciencedirect.com/science/article/pii/S2666166725001832]
- 36. Assessing kidney development and disease using ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.948395/full]
- 37. Deep Learning Unveils Drug-Induced Nephrotoxicity ... [https://bioengineer.org/deep-learning-unveils-drug-induced-nephrotoxicity-predictions/]
- 38. September 19, 2025: Human Organ Chip Models for ... [https://sites.nicholas.duke.edu/envhealth/seminars-symposia/fall-2025-seminar-series/september-19-2025-human-organ-chip-models-for-nephrotoxicity-screening-and-biomedical-applications/]
- 39. Maturation of human cardiac organoids enables complex ... [https://www.nature.com/articles/s44161-025-00669-3]
- 40. Navigating Brain Organoid Maturation: From Benchmarking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383812/]
- 41. Advancements, Strategies, and Challenges in Organoid ... [https://www.sciencedirect.com/science/article/pii/S2095809925006083]
- 42. Parsing Glomerular and Tubular Structure Variability in High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566879/]
- 43. Efficient and reproducible generation of human iPSC- ... [https://www.nature.com/articles/s41467-024-50224-0]
- 44. A Monolayer System for the Efficient Generation of Motor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8151197/]
- 45. Single-cell RNA sequencing and kidney organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276109/]
- 46. Generation of kidney tubular organoids from human ... [https://www.nature.com/articles/srep38353]
- 47. Establishing single cell RNA transcriptomics: a brief guide [https://frontiersinzoology.biomedcentral.com/articles/10.1186/s12983-025-00579-x]
- 48. Navigating single-cell RNA-sequencing: protocols, tools ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085826/]
- 49. Single-cell RNA-seq reveals cell type-specific molecular ... [https://www.nature.com/articles/s41392-025-02438-x]
- 50. 自动化细胞培养 - Molecular Devices [https://www.moleculardevices.com.cn/applications/automated-cell-culture]
- 51. Electrochemical Detection and Capillary Electrophoresis [https://www.mdpi.com/2079-6374/10/8/95]
- 52. An Overview of Cell-Based Assay Platforms for the Solute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8383457/]
- 53. SLC Transporter Assay Services [https://ionbiosciences.com/services/screening-services/slc-transporter-assay-services/]
- 54. Enhancement of Maturation and Functionality of Human Fabry Disease... [https://link.springer.com/article/10.1007/s13206-024-00188-6]
- 55. Integrating organoids and... | Nature Reviews Bioengineering [https://www.nature.com/articles/s44222-024-00207-z?error=cookies_not_supported&code=5a84fcff-2b68-4742-a6d4-efbefd65c0d8]
- 56. Protocol to develop a proximal tubule-on- chip model based on... [https://pubmed.ncbi.nlm.nih.gov/40266846/]
- 57. Single cell transcriptomics of human kidney organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12216864/]