Advanced Warming Protocols for Vitrified Oocytes and Embryos: Enhancing Survival and Clinical Outcomes in Biomedical Research
This article synthesizes current research on modified warming protocols for vitrified oocytes and embryos, a critical area for reproductive biotechnology and drug development.
Advanced Warming Protocols for Vitrified Oocytes and Embryos: Enhancing Survival and Clinical Outcomes in Biomedical Research
Abstract
This article synthesizes current research on modified warming protocols for vitrified oocytes and embryos, a critical area for reproductive biotechnology and drug development. It explores the foundational principle that rapid warming is paramount for preventing lethal intracellular ice crystallization. The content details innovative methodological advances, including one-step fast warming and optimized rehydration techniques, and provides troubleshooting strategies for common challenges like sample volume and cryoprotectant toxicity. Finally, it presents rigorous validation through comparative analyses of survival rates, fertilization potential, and clinical outcomes such as implantation and live birth rates, offering a comprehensive evidence base for researchers and scientists optimizing cryopreservation workflows.
The Critical Role of Warming Rates: Foundational Principles in Vitrified Cell Survival
Understanding Intracellular Ice Formation and Recrystallization as the Primary Cause of Cryoinjury
Cryopreservation has become a fundamental supporting technology for numerous biomedical applications, including cell-based therapeutics, assisted reproduction, tissue engineering, and vaccine storage [1]. The process enables long-term preservation of biological samples by slowing or stopping biochemical activity at ultra-low temperatures [1]. However, the formation, growth, and recrystallization of ice crystals during freezing and thawing procedures represent the most significant limitations in cryopreservation, causing fatal cryoinjury to biological samples [1]. Intracellular ice formation (IIF) is widely recognized as a primary mechanism of cell death during cryopreservation [2]. When ice crystals form inside cells, they can disrupt organelles and membrane structures, leading to irreversible cellular damage [3]. Similarly, ice recrystallization—the process where larger ice grains grow at the expense of smaller ones during warming—generates mechanical stress that compromises cellular integrity [4]. Understanding these phenomena is crucial for developing improved cryopreservation protocols, particularly for sensitive cells such as oocytes and embryos where viability directly impacts clinical outcomes [5].
Mechanisms of Cryoinjury
Intracellular Ice Formation
The process of intracellular ice formation involves complex physical interactions between cells and their extracellular environment during cooling. Research has demonstrated that IIF is not merely a result of critical undercooling, but rather occurs when the plasma membrane is damaged at a critical gradient in osmotic pressure across the membrane [3]. This damage enables extracellular ice to penetrate the cell or provides nucleation sites for internal ice formation.
The two-factor hypothesis of freezing injury, proposed in 1972, differentiates between damage caused by intracellular ice and injury resulting from solute effects [2]. The cooling rate plays a decisive role in determining which mechanism dominates. During slow freezing, extracellular ice formation gradually concentrates solutes in the unfrozen fraction, creating an osmotic gradient that draws water out of cells [1]. This dehydration can cause "solute-effects injury" from the concentrating of biological solutes and cryoprotective agents [2]. Conversely, with rapid cooling, intracellular water does not have sufficient time to exit the cell, resulting in supercooling and ultimately intracellular ice formation [1].
Recent research has revealed unexpected complexity in how intercellular junctions affect IIF. Contrary to earlier assumptions that gap junctions enhance intracellular ice propagation between connected cells, studies using mouse insulinoma cells with knocked-down junction proteins demonstrated that junction-lacking cells actually freeze at higher temperatures than wild-type cells [2]. High-speed videomicroscopy revealed that penetration of extracellular ice into the paracellular space between cells correlates with IIF incidence, with intracellular ice most often initiating at cell locations adjacent to this paracellular ice [2].
Ice Recrystallization
Ice recrystallization occurs primarily during the warming phase of cryopreservation, particularly when samples pass through the "risky temperature zone" (approximately -15°C to -160°C) [1]. During this phase, small ice crystals become unstable and reorganize into larger, more damaging crystals through two main processes: accretion (the joining of adjacent crystals) and migration (the melting of smaller crystals and re-freezing onto larger crystals) [4].
Recrystallization is particularly problematic in vitrification, where the initial formation of a glassy, ice-free state is achieved using high concentrations of cryoprotectants and ultra-rapid cooling [1]. During warming, devitrification (the transition from a glassy state to an icy crystalline state) can occur, followed by recrystallization that causes fatal damage to cryopreserved samples [1]. The warming rate has been shown to be at least as important as the cooling rate in determining cell survival, as slow warming allows time for the development and growth of small intracellular ice crystals through recrystallization [6].
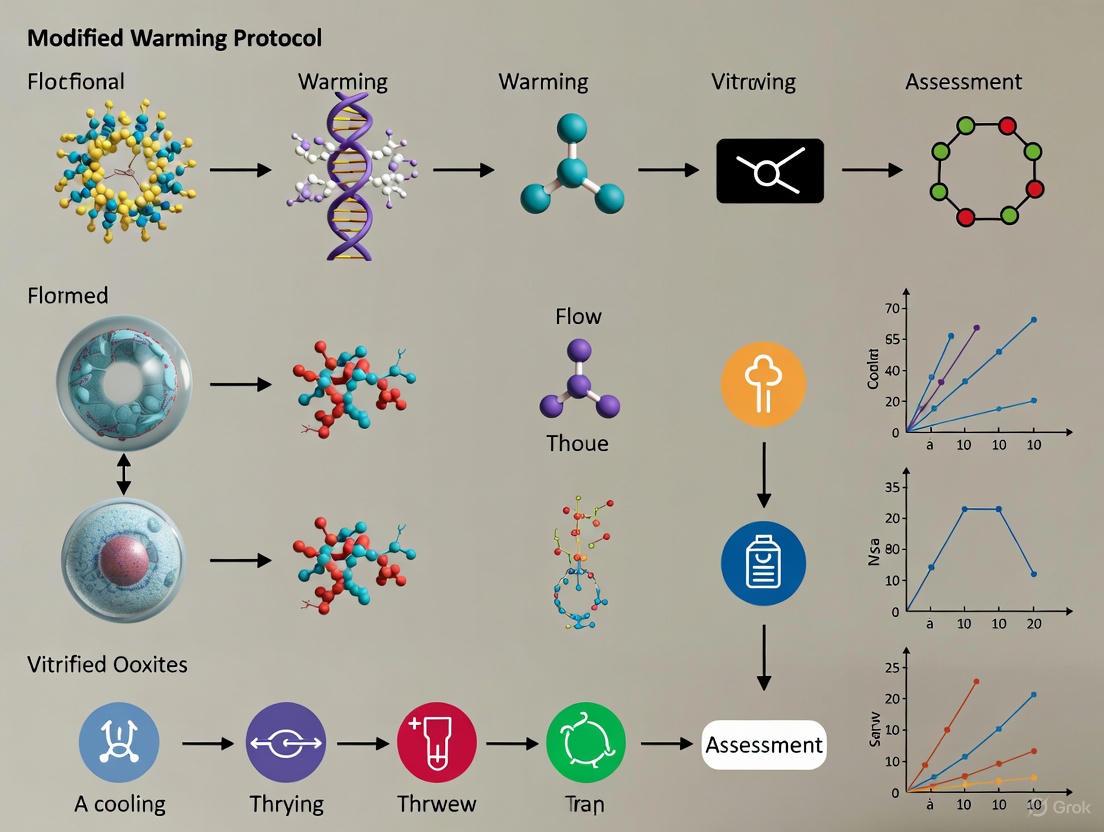
Figure 1: Mechanisms of Cryoinjury During Freezing and Warming. The diagram illustrates the two primary pathways of cellular damage during cryopreservation: intracellular ice formation during freezing and ice recrystallization during warming.
Experimental Evidence and Recent Advances
Modified Warming Protocols
Recent clinical studies have demonstrated that modifying warming protocols can significantly improve outcomes for vitrified oocytes and embryos. A 2025 retrospective cohort study involving 13,103 donor oocytes compared conventional warming protocols (CWP) with a modified warming protocol (MWP) [5]. The MWP simplified the warming process into an ultrafast, single-step approach, eliminating the need for dilution solution (DS) and wash solution (WS) and incubating oocytes only in thawing solution (TS) for 1 minute [5].
The results were striking. While survival rates after warming were similar between CWP and MWP groups (93.7% vs. 93.9%), blastocyst formation was significantly higher in the MWP group (77.3%) compared to the CWP group (57.5%) and even exceeded the fresh control group (69.2%) [5]. Most importantly, ongoing pregnancy/live birth rates were substantially higher in the MWP group than in the CWP group (66.7% vs. 50.4%) [5]. Multivariate analysis confirmed a positive association between MWP and both usable blastocyst formation and ongoing pregnancy/live birth outcomes [5].
This research suggests that the modified warming protocol enhances the blastocyst formation potential and pregnancy outcomes of vitrified-warmed oocytes, making their performance similar to fresh oocytes [5]. The simplified protocol not only improves clinical outcomes but also streamlines laboratory workflow by reducing procedural time and potential for technical error.
Ice Recrystallization Inhibitors
The development of synthetic ice recrystallization inhibitors (IRIs) represents another significant advancement in addressing cryoinjury. These small molecules are specifically designed to mitigate cellular damage from uncontrolled ice growth during cryopreservation [7]. Unlike natural antifreeze proteins (AFPs) which can induce dynamic ice shaping—resulting in sharp, elongated ice crystals that intensify cryoinjury—synthetic IRIs inhibit ice recrystallization without altering ice crystal morphology [7].
Studies across multiple cell types have demonstrated the efficacy of IRIs. For induced pluripotent stem cells (iPSCs), the addition of IRIs during cryopreservation increased post-thaw viability and recovery without affecting pluripotency [7]. iPSC-derived neurons cryopreserved with IRIs showed faster reestablishment of neuronal network activity and synaptic function compared to controls [7]. Additionally, red blood cells cryopreserved with IRIs maintained higher membrane integrity after repeated warming cycles, even with reduced glycerol concentrations [7].
Table 1: Experimental Evidence for Modified Warming Protocols and Ice Recrystallization Inhibitors
| Experimental Approach | Key Findings | Clinical/Functional Outcomes | Citation |
|---|---|---|---|
| Modified Warming Protocol (MWP) for vitrified oocytes | • Equivalent survival rates (93.9% MWP vs. 93.7% CWP)• Higher blastocyst formation (77.3% MWP vs. 57.5% CWP)• Reduced degeneration post-ICSI | • Higher ongoing pregnancy/live birth (66.7% MWP vs. 50.4% CWP)• Multivariate analysis: positive association with usable blastocysts | [5] |
| Ice Recrystallization Inhibitors (IRIs) for iPSCs | • Increased post-thaw viability and recovery• Maintained pluripotency markers | • Faster reestablishment of neuronal network activity in derived neurons• Improved synaptic function recovery | [7] |
| IRIs for Red Blood Cells | • Maintained membrane integrity with reduced glycerol• Sustained integrity after repeated warming cycles | • Potential for improved transfusion products• Reduced CPA toxicity concerns | [7] |
| Universal Warming Protocol for blastocysts | • Interchangeable use of different vitrification kits• Efficient reduction of sucrose/trehalose volume | • Streamlined laboratory workflow• Maintained safety and efficacy profile | [8] |
Research Reagent Solutions
Table 2: Essential Reagents and Materials for Cryopreservation Research
| Reagent/Material | Function/Application | Examples/Specific Uses | |
|---|---|---|---|
| Permeating Cryoprotectants | Cross cell membrane to suppress intracellular ice formation | • Dimethyl sulfoxide (DMSO): Widely used but cytotoxic• Glycerol: Used at 40% (w/v) for RBC cryopreservation• Ethylene glycol: Component of many vitrification solutions | [4] [6] |
| Non-Permeating Cryoprotectants | Act extracellularly to promote vitrification and minimize osmotic shifts | • Sucrose: Disaccharide used in warming solutions (1.0 M in TS)• Trehalose: Larger disaccharide, more effective than sucrose• Hydroxyethyl starch (HES): Extracellular stabilizer | [9] [4] |
| Synthetic Polymers | Inhibit ice nucleation and growth in aqueous solutions | • Poly(vinyl alcohol) (PVA): Inhibits nucleation, growth, and recrystallization• Poly(vinylpyrrolidone) (PVP): Low toxicity to microorganisms• Poly(ethylene glycol) (PEG): Reduces reactive oxygen species production | [10] |
| Ice Recrystallization Inhibitors (IRIs) | Specifically designed to mitigate ice recrystallization damage | • Synthetic small molecules: Mimic IRI activity without dynamic ice shaping• Compatible with conventional cryopreservation protocols• Enable reduction of cytotoxic CPA concentrations | [7] |
| Vitrification Devices | Enable ultra-rapid cooling through minimal volume design | • Cryotop: Open system allowing cooling rates >10,000°C/min• Open Pulled Straw (OPS): Original minimal volume device• Cryoloop: Small nylon loop for microvolume suspension | [6] |
Detailed Experimental Protocols
Conventional Vitrification and Warming Protocol for Oocytes
Vitrification Procedure:
- Equilibration: Expose oocytes to equilibration solution containing 7.5% ethylene glycol (EG) and 7.5% dimethyl sulfoxide (DMSO) for 10-15 minutes at room temperature [6].
- Vitrification: Transfer oocytes to vitrification solution containing 15% EG, 15% DMSO, and 0.5M sucrose for 60 seconds at room temperature [6].
- Loading and Cooling: Place oocytes on a Cryotop device in a minimal volume (<1μL) and immediately plunge into liquid nitrogen [6]. Cooling rates exceed -10,000°C/min.
Conventional Warming Protocol:
- Thawing Solution (TS): Rapidly warm samples by transferring directly to TS containing 1.0M sucrose at 37°C for 1 minute [5] [9].
- Dilution Solution (DS): Transfer oocytes to DS containing 0.5M sucrose at room temperature for 3 minutes [5].
- Washing Solution (WS): Incubate oocytes in WS at room temperature for 5-6 minutes [5].
- Culture Transfer: Wash oocytes through multiple drops of culture media to remove residual cryoprotectants before transferring to final culture conditions [9].
Modified Warming Protocol for Vitrified Oocytes
Single-Step Warming Procedure:
- Preparation: Pre-warm thawing solution (TS) to 37°C. The TS contains extracellular cryoprotectants such as sucrose or trehalose at 1.0M concentration [5].
- Warming: Transfer vitrified oocytes directly from liquid nitrogen into TS at 37°C and incubate for exactly 1 minute [5]. This rapid warming at rates exceeding 2170°C/min avoids ice crystal formation during the warming process [9].
- Direct Transfer: After 1 minute in TS, directly transfer oocytes to culture media without intermediate dilution or washing steps [5].
- Culture: Proceed with standard culture protocols for subsequent procedures such as intracytoplasmic sperm injection (ICSI) or embryo culture.
This modified protocol eliminates the need for DS and WS, completing the warming process in just one minute while maintaining—and in some cases improving—embryonic development potential and pregnancy outcomes [5].
Protocol for Testing Ice Recrystallization Inhibitors
Cryopreservation with IRI Supplementation:
- Base Solution Preparation: Prepare standard cryopreservation medium appropriate for the cell type (e.g., containing 10% DMSO for mammalian cells).
- IRI Supplementation: Add synthetic IRI compounds to the cryopreservation medium at optimized concentrations (typically 0.1-10 mg/mL, depending on the specific IRI) [7].
- Cryopreservation: Follow standard freezing protocols for the specific cell type. For controlled-rate freezing, use a cooling rate of -1°C/min to -80°C followed by transfer to liquid nitrogen.
- Thawing: Rapidly warm cells in a 37°C water bath for 2-3 minutes.
- Assessment: Evaluate post-thaw viability using trypan blue exclusion or fluorescent viability stains, and assess functionality through cell-type-specific assays.
Figure 2: Experimental Workflow Comparison for Cryopreservation Strategies. The diagram illustrates three approaches to cryopreservation: conventional warming with gradual rehydration, modified single-step warming, and ice recrystallization inhibitor supplementation.
Intracellular ice formation and recrystallization remain the primary causes of cryoinjury in cryopreservation procedures. Understanding these mechanisms has enabled the development of improved protocols that significantly enhance cell survival and functionality post-preservation. The modified warming protocol for vitrified oocytes and embryos represents a substantial advancement in the field, demonstrating that simplified, ultrafast warming can not only streamline laboratory workflow but also improve clinical outcomes. Similarly, the development of synthetic ice recrystallization inhibitors offers a promising approach to mitigate recrystallization-driven injury, enabling reduced concentrations of cytotoxic cryoprotectants while maintaining or improving post-thaw cell quality and function. These innovations collectively address the long-standing challenge of ice-related damage in cryopreservation, offering enhanced prospects for applications in assisted reproduction, cell therapy, regenerative medicine, and biobanking.
The field of assisted reproductive technology (ART) has been revolutionized by vitrification, an ultra-rapid cooling technique that prevents ice crystal formation by solidifying cells into a glass-like state. While much research focus has historically centered on optimizing cooling rates, a paradigm shift is occurring toward recognizing the critical importance of warming kinetics. The Warming Rate Hypothesis posits that for vitrified oocytes and embryos, the rate of warming exerts a more profound influence on survival and developmental potential than the rate of cooling. This hypothesis challenges conventional practices and establishes a new framework for evaluating cryopreservation success, particularly for the highly sensitive human oocyte. Mounting clinical evidence demonstrates that modified warming protocols (MWP) significantly enhance oocyte survival, blastocyst formation, and ongoing pregnancy rates by minimizing cryodamage during the crucial phase of cryoprotectant removal and cellular rehydration [5] [11] [12]. This application note delineates the scientific foundation, experimental validation, and practical implementation of rapid warming protocols, providing researchers and clinicians with the tools to elevate ART outcomes through optimized warming kinetics.
Theoretical Foundation: The Science of Rapid Warming
Physical and Chemical Principles
Vitrification success hinges on a delicate balance of biological, physical, and chemical factors. During cooling, high concentrations of cryoprotectants (CPAs) and extremely rapid cooling rates prevent ice crystallization. However, this process introduces two primary risks: intracellular ice formation during cooling and devitrification (the formation of damaging ice crystals during warming) if warming is not sufficiently rapid [12]. The Warming Rate Hypothesis contends that the latter risk is more consequential. Rapid warming prevents devitrification by propelling the cell through this dangerous temperature zone too quickly for ice crystals to nucleate and grow.
The inverse relationship between warming rates and the required CPA concentration presents a critical trade-off. While higher CPA concentrations facilitate vitrification at slower cooling rates, they simultaneously increase cryoprotectant toxicity and osmotic stress. Rapid warming reduces the requisite CPA concentration, thereby mitigating these associated damages. For oocytes—cells characterized by their large size, high water content, and unique intracellular structure—this balance is particularly crucial. Their sensitivity to osmotic shock and CPA toxicity makes them exceptionally vulnerable to suboptimal warming conditions [12].
Biological Implications for Oocytes
Oocytes are highly susceptible to cryopreservation-induced stress, which can manifest as spindle depolymerization, chromosome dispersal, and DNA fragmentation [13]. The conventional warming protocol (CWP) employs a gradient dilution approach at room temperature, involving sequential incubation in dilution solution (DS) and wash solution (WS) to minimize osmotic stress. While effective, this process is complex and time-intensive, potentially prolonging cellular exposure to osmotic stress and CPAs [5] [11].
Modified warming protocols address these limitations by dramatically accelerating the process. The MWP simplifies the CWP into an ultrafast, single-step process, often involving incubation in a thawing solution (TS) at 37°C for just one minute, eliminating the need for DS and WS [5] [14]. This rapid dilution and rehydration approach minimizes the time oocytes spend in hypertonic environments, preserving meiotic spindle integrity and reducing DNA fragmentation. Evidence confirms that oocytes warmed using MWP exhibit a more intact cell membrane structure, less swelling, and fewer cytoplasmic vacuoles compared to those subjected to CWP [11].
Clinical and Experimental Validation
Key Findings from Human Donor Oocyte Studies
A landmark retrospective cohort study provides compelling evidence supporting the Warming Rate Hypothesis. The study analyzed 13,103 donor oocytes, divided into three groups: conventional warming protocol (CWP), modified warming protocol (MWP), and fresh oocytes. The results demonstrated that while survival rates post-warming were statistically similar between CWP and MWP groups (93.7% vs. 93.9%), dramatic differences emerged in subsequent developmental competencies [5] [11].
Table 1: Embryological Outcomes Following Different Warming Protocols
| Parameter | CWP Group | MWP Group | Fresh Group |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | N/A |
| Normal Fertilization | 79.5% | 79.6% | 83.0% |
| Blastocyst Formation | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | N/A [5] [11] |
Multivariate analysis confirmed a positive association between MWP and usable blastocyst formation (adjusted incidence rate ratio = 1.423, 95% CI = 1.268 to 1.597, P < 0.001), as well as ongoing pregnancy/live birth (adjusted odds ratio = 1.899, 95% CI = 1.002 to 3.6, P < 0.05) [5]. These findings indicate that MWP not only enhances early embryonic development but also translates to significantly superior clinical outcomes, with pregnancy rates surpassing even those achieved with fresh oocytes in some parameters.
Universal Application Across Media Systems
The robustness of optimized warming protocols is further validated by their successful application across different commercial media systems. A multicenter study demonstrated the efficacy of a "Universal Warming Protocol" (UWP) applied to donor oocytes vitrified with Kitazato media but warmed using three different devitrification media: Kitazato, Irvine, and RapidWarm Omni [15].
Table 2: Multicenter Comparison of Universal Warming Protocol Efficacy
| Parameter | Kitazato Media | Irvine Media | RapidWarm Omni |
|---|---|---|---|
| Survival Rate | 86% | 85% | 94% |
| Fertilization Rate | 77% | 74% | 73% |
| Blastulation Rate | 52% | 58% | 57% |
| Clinical Pregnancy Rate (Day 5) | 39% | 57% | 60% [15] |
Notably, survival rates were statistically higher with RapidWarm Omni media (94%), though subsequent development rates were comparable across groups. This confirms that the warming protocol itself is a more critical determinant of success than the specific media system used, enabling greater flexibility and standardization across laboratories [15].
Practical Application: Protocols and Workflows
Detailed Modified Warming Protocol for Human Oocytes
The following protocol is adapted from studies demonstrating improved clinical outcomes with MWP [5] [11]:
Principle: Rapid warming at 37°C with single-step dilution to prevent devitrification and minimize osmotic stress.
Materials:
- Thawing Solution (TS): 1.0 M sucrose in base medium
- Warming block or water bath at 37°C
- Pre-equilibrated culture media
Procedure:
- Preparation: Pre-warm TS to 37°C. Prepare culture dishes with pre-equilibrated media and maintain at 37°C in a CO₂ incubator.
- Warming: Remove vitrified oocytes from liquid nitrogen and immediately immerse in TS at 37°C for 1 minute.
- Dilution: Directly transfer oocytes from TS to pre-equilibrated culture media.
- Washing: Gently wash oocytes through two drops of culture media.
- Assessment: Assess oocyte survival based on membrane integrity and morphological normality after 2 hours of culture.
- ICSI: Perform intracytoplasmic sperm injection (ICSI) within 4 hours post-warming.
Critical Steps:
- Maintain temperature consistently at 37°C throughout the warming and dilution process
- Minimize time between removal from liquid nitrogen and immersion in TS
- Adhere strictly to the 1-minute incubation in TS
Experimental Workflow for Protocol Validation
The following diagram illustrates a typical experimental workflow for validating a modified warming protocol, integrating key steps from clinical and research studies:
Experimental Workflow for MWP Validation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Oocyte Vitrification and Warming Studies
| Reagent Category | Specific Examples | Function | Research Considerations |
|---|---|---|---|
| Base Media | mHTF, PB1 [16] | Provide ionic and nutrient support during procedures | Osmolarity and pH stability are critical during warming |
| Permeating CPAs | Ethylene Glycol (EG), Dimethyl Sulfoxide (DMSO), Propylene Glycol | Penetrate cell membrane to suppress ice formation | Toxicity increases with concentration and exposure time |
| Non-Permeating CPAs | Sucrose, Trehalose, Ficoll | Create osmotic gradient for dehydration | Concentration in warming solution critical (e.g., 0.1-0.3M) [16] |
| Commercial Kits | Kitazato, Irvine, RapidWarm Omni [15] | Standardized formulations for consistency | Universal protocols may work across brands |
| Supplemental Agents | Extracellular Vesicles from follicular fluid [13] | Enhance cryotolerance when added during IVM | Source (follicle size) affects protective cargo |
| Myristoyl Glutamic Acid | Myristoyl Glutamic Acid, CAS:53576-52-6, MF:C19H35NO5, MW:357.5 g/mol | Chemical Reagent | Bench Chemicals |
| Monactin | Monactin, CAS:7182-54-9, MF:C41H66O12, MW:751.0 g/mol | Chemical Reagent | Bench Chemicals |
Comparative Protocol Analysis
The transition from conventional to modified warming protocols represents a significant simplification and acceleration of the warming process. The following diagram contrasts these two approaches, highlighting the dramatic reduction in steps and time:
Conventional vs. Modified Warming Protocols
The Warming Rate Hypothesis establishes a fundamental paradigm shift in oocyte cryopreservation, demonstrating that rapid warming protocols are not merely procedural refinements but fundamental determinants of cellular survival and developmental competence. Clinical evidence confirms that modified warming protocols significantly enhance blastocyst formation rates and ongoing pregnancy outcomes, achieving results comparable to—and in some parameters surpassing—those obtained with fresh oocytes. The development of universal warming protocols that maintain efficacy across different commercial media systems further enhances the practical implementation of these advances. As the field progresses, future research should focus on refining warming solution compositions, optimizing protocols for specific patient populations, and further elucidating the molecular mechanisms through which rapid warming preserves oocyte developmental potential. The consistent implementation of optimized warming protocols represents a critical step toward maximizing ART success rates and expanding fertility preservation options worldwide.
Critical Cooling Rate (CCR) and Critical Warming Rate (CWR) are fundamental physical parameters in cryopreservation, defining the minimum rates required to cool and warm a biological sample without forming damaging ice crystals. Successful vitrification—the transition of a solution into a stable, glassy state—depends on exceeding both the CCR during cooling and the CWR during warming to prevent ice crystallization (devitrification) and ensure cellular survival [17] [18]. The CWR is typically one to three orders of magnitude higher than the CCR for a given cryoprotectant solution, making the warming process often the more significant technical challenge [19]. This article delineates the theoretical and practical aspects of these critical rates, providing a framework for optimizing vitrification protocols for oocytes, embryos, and other biomaterials.
Theoretical Foundations and Physical Principles
The relationship between CCR, CWR, and solution composition is governed by the kinetics of ice nucleation and growth. Vitrification is achieved when cooling occurs rapidly enough to prevent the molecular reorganization required for ice crystal formation, instead solidifying the solution into an amorphous glass. The CCR is the minimum cooling rate required to achieve this state, confining ice formation to less than a critical volume, often defined as 0.2% of the solution mass [17] [18].
Upon warming, the danger shifts to devitrification, where the glassy state undergoes uncontrolled ice formation as it passes through a perilous temperature zone. The CWR is the minimum warming rate required to traverse this zone too quickly for ice crystals to nucleate and grow. The CWR is substantially higher than the CCR because warming through the devitrification zone facilitates rapid ice crystal growth from any residual nuclei formed during cooling [17] [19].
Table 1: Critical Cooling and Warming Rates for Common Cryoprotectant Agents (CPAs)
| Cryoprotectant (CPA) | Critical Cooling Rate (CCR) | Critical Warming Rate (CWR) | Key References |
|---|---|---|---|
| M22 | 0.1 °C/min | 0.4 °C/min | [18] |
| VS55 | ~2.5 °C/min | ~50-55 °C/min | [20] [18] |
| DP6 | ~40 °C/min | ~185-200 °C/min | [20] [18] |
| 40% Glycerol | ~10^2 °C/min (estimated) | ~10^3 - 10^4 °C/min (estimated) | [19] |
| 40% DMSO | ~10^2 °C/min (estimated) | ~10^3 - 10^4 °C/min (estimated) | [19] |
The following diagram illustrates the "Crystallization Zone" that a sample must traverse rapidly during both cooling and warming to avoid ice formation.
Diagram 1: Thermal trajectory for vitrification. Samples must pass rapidly through the "Crystallization Zone" during both cooling and warming.
The values in Table 1 demonstrate that lower-concentration CPAs like DP6 require significantly higher CCRs and CWRs compared to high-concentration cocktails like M22. This inverse relationship between CPA concentration and required cooling/warming rate creates a practical trade-off: using lower concentrations reduces CPA toxicity but places vastly greater demands on the thermal performance of the protocol [17] [18].
Experimental Protocols and Methodologies
Determining Critical Rates: Experimental Setup
Accurate determination of CCR and CWR requires controlled thermal manipulation and precise detection of ice formation. The following protocol, adapted from cryoprotectant solution studies, outlines a robust method for measuring these parameters [19].
1. Primary Materials and Reagents
- Cryoprotectant Solutions: Prepare aqueous solutions of the target CPAs (e.g., glycerol, DMSO, ethylene glycol) at desired concentrations (% w/w). Ensure thorough mixing.
- Sample Holder: Polyimide loops (20-300 μm openings) or polyester thread loops (0.3-5 mm diameter) mounted on stainless-steel rods.
- Cooling Apparatus: A laminar stream of cold nitrogen gas (~100 K / -173°C) generated by passing nitrogen gas through a copper coil submerged in liquid nitrogen.
- Warming Apparatus: A stainless-steel cup filled with light mineral oil pre-heated to a temperature between 295 K (22°C) and 450 K (180°C) on a hotplate.
- Temperature Monitoring: Bare-wire Type-E thermocouples with wire diameters of 12.5-75 μm, connected to a high-speed data acquisition system.
- Imaging System: A high-speed camera mounted on a microscope for visual inspection of samples.
2. Step-by-Step Procedure
- Step 1: Sample Loading. Dispense a small volume (nL to μL) of the CPA solution into the loop-based sample holder.
- Step 2: Cooling and Vitrification. Position the sample in the cold nitrogen gas stream. Monitor and record the temperature drop using the thermocouple positioned within the sample. The cooling rate is determined by the gas flow and sample size.
- Step 3: Visual Inspection during Cooling. Use the high-speed camera in bright-field or dark-field mode to detect the formation of ice, indicated by a change in sample opacity or light scattering.
- Step 4: Rapid Warming. While the sample is held in the cold gas stream, rapidly immerse it into the pre-heated oil bath by manually lifting the oil cup. The transition should be completed within a few milliseconds.
- Step 5: Visual Inspection during Warming. Record the warming process with the high-speed camera. Observe for any opaque or milky appearance signaling ice formation (devitrification).
- Step 6: Data Analysis. The thermocouple trace provides the precise warming rate. The critical rate is identified as the minimum warming rate at which no ice is visually detected in the sample.
Application in Assisted Reproductive Technology (ART)
In clinical ART laboratories, vitrification and warming protocols for oocytes and embryos are highly refined. A recent study on a Modified Warming Protocol (MWP) for vitrified donor oocytes demonstrates the clinical impact of optimizing these steps [5].
Conventional Warming Protocol (CWP) for Oocytes/Embryos:
- Rapid Warm in Thawing Solution (TS): Transfer the vitrified sample directly into a ~37°C TS containing 1.0 M sucrose for 1 minute [5] [9].
- Dilution in DS: Move the sample to a Dilution Solution (DS) containing 0.5 M sucrose for 3-5 minutes at room temperature [5] [9].
- Washing in WS: Perform two washes in a Washing Solution (WS), which has a composition similar to culture media, to remove residual cryoprotectants [9].
Modified (Ultra-rapid) Warming Protocol (MWP): The MWP simplifies the process into a single-step rehydration to improve workflow and outcomes [5]. The sample is warmed by immersion in a TS at 37°C for only 1 minute, after which it is directly transferred to culture media. This protocol leverages rapid warming and the cell's inherent regulatory capacity, showing improved blastocyst formation and ongoing pregnancy rates compared to the CWP [5].
Table 2: Outcomes of Conventional vs. Modified Warming Protocol for Vitrified Oocytes
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | N/A |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | Not Reported |
| Association with Positive Outcome | Reference | aOR: 1.899 (95% CI: 1.002-3.6) | Reference |
Data adapted from [5]. aOR: adjusted Odds Ratio.
Advanced Scaling and Technology for Large Volumes
Scaling vitrification to larger tissues and organs presents a significant challenge, as convective cooling and warming rates decrease as volume increases. The characteristic length (Lc = Volume/Surface Area) determines the maximum achievable rates, with larger Lc leading to slower rates [18].
Advanced Rewarming Technologies: To overcome the CWR limitation in large volumes, volumetric heating technologies are under development:
- Inductive Rewarming with Metal Forms: Embedding conductive metal forms (e.g., aluminum foil, nitinol mesh) within the sample allows for ultra-rapid heating when subjected to an alternating magnetic field, achieving rates exceeding 1000°C/min [20].
- Nanowarming: Iron-oxide nanoparticles (IONPs) are perfused through the tissue vasculature. When activated by a radiofrequency field, they heat uniformly from within, achieving warming rates of ~88°C/min in liter-scale volumes, which is sufficient for CPAs like M22 [21].
The diagram below summarizes the protocol selection logic based on system scale and CPA requirements.
Diagram 2: Protocol selection is driven by the system's scale and the CPA's CWR. Volumetric heating is essential for large systems.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Vitrification Studies
| Category | Item | Function/Description | Example Application |
|---|---|---|---|
| Common CPAs | Dimethyl Sulfoxide (DMSO), Ethylene Glycol (EG), Glycerol, Sucrose | Permeating and non-permeating agents that suppress ice crystallization and reduce CCR/CWR. | Base components of vitrification cocktails like VS55 and M22 [20] [18]. |
| Vitrification Cocktails | VS55, DP6, M22 | Standardized CPA mixtures with well-characterized CCR and CWR values. | Used as benchmarks for developing new protocols [20] [18]. |
| Warming Kit Solutions | Thawing Solution (TS), Dilution Solution (DS), Washing Solution (WS) | Step-wise solutions for removing CPAs and rehydrating cells while minimizing osmotic shock. | Essential for ART warming protocols [9]. |
| Magnetic Components | Iron-Oxide Nanoparticles (IONPs), Aluminum Foil, Nitinol Mesh | Act as internal heat sources when exposed to an alternating magnetic field for ultrafast volumetric warming. | Enables nanowarming for large volume systems [20] [21]. |
| Sample Holders | Polyimide Loops, Polyester Thread Loops, Open Pulled Straws (OPS), Cryotop | Micro-volume devices that maximize cooling and warming rates by minimizing sample volume. | Critical for achieving vitrification in cells with high CCR/CWR [22] [19]. |
| Nequinate | Nequinate (Methyl Benzoquate) | High-purity Nequinate for veterinary and agricultural research. This product is for Research Use Only (RUO) and not for human or animal consumption. | Bench Chemicals |
| Probucol | Probucol, CAS:23288-49-5, MF:C31H48O2S2, MW:516.8 g/mol | Chemical Reagent | Bench Chemicals |
Thermodynamic and Biophysical Principles Governing Successful Devitrification
Devitrification, the process by which a glassy, vitrified state reverts to a crystalline solid upon warming, represents a significant risk to the survival of vitrified oocytes and embryos in assisted reproductive technology (ART). During cryopreservation, biological samples are cooled to cryogenic temperatures in a glass-like state without forming damaging ice crystals. However, if during warming the sample passes through a temperature range where ice crystals can form and grow, devitrification can occur, causing irreversible cellular damage [6]. The kinetic nature of the glass transition means that the success of devitrification avoidance depends critically on both the thermodynamic conditions and the rates of temperature change [23]. For reproductive cells, which are particularly sensitive to cryodamage, understanding these principles is essential for developing optimized warming protocols that maximize survival and developmental potential. This document outlines the core principles and provides detailed protocols for implementing successful devitrification procedures in clinical and research settings.
Theoretical Foundations
The Kinetics of Glass Transition and Devitrification
The transformation from a glass to a liquid during warming is fundamentally a kinetic process, not a thermodynamic phase transition. The glass transition temperature (Tg) is defined as the point at which the molecular relaxation time of the system becomes comparable to the experimental timescale, typically determined by the warming rate [23]. Upon warming from cryogenic temperatures, the system initially remains in a glassy state until it reaches the devitrification temperature, where the increased molecular mobility allows for the nucleation and growth of ice crystals if the warming rate is insufficient.
Molecular dynamics simulations reveal that devitrification in ultrastable glasses occurs through a two-step process [24]. Initially, isolated liquid droplets nucleate and grow slowly within the rigid glassy matrix. These droplets contain liquid that is initially compressed by the surrounding glass. As warming continues and these droplets coalesce into larger domains, the internal pressure is released, accelerating the transformation process. This mechanism produces pronounced deviations from classical Avrami kinetics and explains the emergence of a characteristic length scale for devitrification in bulk systems [24].
Thermodynamic Constraints and Stability
The Prigogine-Defay ratio, which characterizes the relationship between thermodynamic coefficients at the glass transition, often deviates from unity, indicating that the process cannot be described as a simple second-order equilibrium phase transition [23]. This deviation underscores the non-equilibrium nature of the glassy state and its transformation. The pressure coefficient of the glass transition temperature (dTg/dp) provides crucial insight into the thermodynamic character of devitrification, connecting kinetic fragilities with volumetric and thermal properties [23].
Structural differences between the glass and liquid states are significant. The formation of a macroscopic percolation cluster of broken bonds (configurons) at and above the glass transition temperature accounts for drastic changes in material properties, including the loss of rigidity that defines the transition from solid to liquid behavior [25]. This configuron percolation theory provides a structural basis for understanding the fundamental changes occurring during devitrification.
Quantitative Analysis of Devitrification Parameters
Critical Warming Rates and Solution Properties
The minimum warming rate required to avoid devitrification is inversely related to the concentration of cryoprotectants (CPAs). Higher CPA concentrations lower the critical warming rate needed to bypass ice formation. The relationship between these parameters is foundational to protocol design.
Table 1: Relationship Between CPA Concentration and Critical Warming Rates
| CPA Concentration | Critical Warming Rate (°C/min) | Sample Volume | Vitrification Solution Composition |
|---|---|---|---|
| High (~6M EG) | 2,500 - 10,000 | 1-3 µL | EG, DMSO, Trehalose, Ficoll |
| Moderate | 10,000 - 50,000 | ~1 µL | EG, DMSO, Sucrose |
| Low | >50,000 | <1 µL | EG, DMSO, Sucrose in base medium |
Performance Comparison: Conventional vs. Modified Warming Protocols
Clinical outcomes demonstrate the efficacy of optimized warming protocols. The following data compares the performance of a Conventional Warming Protocol (CWP) with a Modified Warming Protocol (MWP) for vitrified oocytes.
Table 2: Clinical Outcomes of Conventional vs. Modified Warming Protocols
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | - |
| Blastocyst Formation | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | - |
The data in Table 2 illustrates that the MWP not only maintains high survival rates but significantly improves embryonic development potential and clinical outcomes, making results comparable to fresh oocytes [5].
Experimental Protocols
Pod and Garage Vitrification System Protocol
The Pod and Garage system represents a technological advancement that minimizes cryoprotectant volume to approximately 3 nL—a 1000-fold reduction compared to standard methods—while improving sample traceability and reducing direct handling [26].
Materials:
- Pod and Garage devices (photopolymerized)
- Vitrification solutions: Equilibration Solution (10% ethylene glycol, 10% DMSO) and Vitrification Solution (16.6% ethylene glycol, 16.6% DMSO, 1M sucrose)
- Warming solutions: Decreasing sucrose concentrations (0.3M, 0.25M, 0.15M) in handling medium
- Liquid nitrogen and storage equipment
Methodology:
- Device Preparation: Fabricate Pod and Garage components using two-photon polymerization with a photoresist resin. Wash and sterilize devices before use [26].
- Sample Loading: House single oocytes or embryos in individual Pods, with multiple Pods docked into a Garage unit.
- CPA Equilibration: Transfer the loaded device through equilibration solution for controlled dehydration.
- Vitrification: Place the device in vitrification solution briefly before direct immersion in liquid nitrogen.
- Warning: Rapidly warm the device by transferring to thawing solution at 37°C for 1 minute.
- CPA Removal: Sequentially transfer through decreasing sucrose concentrations (0.3M, 0.25M, 0.15M) to remove cryoprotectants gradually.
- Assessment: Evaluate survival rates, developmental competence, and metabolic parameters post-warming [26].
Modified Warming Protocol for Oocytes
This protocol optimizes the warming process to minimize devitrification risks and osmotic stress, based on clinical studies showing improved outcomes [5].
Materials:
- Thawing Solution (TS): 1M sucrose in handling medium
- Dilution Solution (DS): Lower sucrose concentration in handling medium
- Wash Solution (WS): Sucrose-free handling medium
- Water bath or surface warmer calibrated to 37°C
Methodology:
- Rapid Warming: Immediately transfer vitrified oocytes from liquid nitrogen to TS at 37°C for exactly 1 minute. This rapid temperature increase prevents ice crystal formation by quickly passing through the dangerous devitrification temperature range [5] [6].
- CPA Dilution: Transfer oocytes to DS at room temperature for 3 minutes. This gradual reduction in sucrose concentration controls osmotic pressure, preventing excessive swelling.
- Final Rinse: Transfer oocytes to WS for 5-6 minutes at room temperature to complete the removal of cryoprotectants.
- Culture Preparation: Transfer oocytes to standard culture media for subsequent fertilization and culture.
Diagram 1: Modified warming protocol workflow
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key Reagents for Devitrification Research
| Reagent Solution | Composition | Function in Devitrification |
|---|---|---|
| Vitrification Solution | 16.6% ethylene glycol, 16.6% DMSO, 1M sucrose in base medium | Enables glass transition by depressing ice nucleation temperature and increasing viscosity [26] |
| Equilibration Solution | 10% ethylene glycol, 10% DMSO in handling medium | Initial CPA exposure for controlled cellular dehydration [26] |
| Thawing Solution (TS) | 1M sucrose in handling medium | Rapid initial warming while maintaining osmotic balance to prevent devitrification [5] |
| Dilution Solution (DS) | Lower sucrose concentration in handling medium | Gradual reduction of CPA concentration to minimize osmotic shock [5] |
| Wash Solution (WS) | Sucrose-free handling medium | Complete removal of CPAs before culture [5] |
| Pod and Garage Devices | Photopolymerized resin chambers | Minimize CPA volume (to ~3 nL) and improve sample traceability [26] |
| Pafuramidine Maleate | Pafuramidine Maleate|DB289|Research Compound | |
| Piperic acid | Piperic acid, CAS:5285-18-7, MF:C12H10O4, MW:218.20 g/mol | Chemical Reagent |
Successful devitrification of vitrified oocytes and embryos depends on a sophisticated interplay of thermodynamic principles and kinetic parameters. The two-step nature of devitrification revealed in molecular dynamics simulations underscores the importance of achieving sufficiently rapid warming rates to bypass the critical temperature zone where ice crystal growth occurs [24]. Clinical evidence demonstrates that modified warming protocols significantly improve embryonic development and pregnancy outcomes by optimizing these parameters [5]. The development of advanced systems like the Pod and Garage, which minimize cryoprotectant volumes by 1000-fold, represents a promising direction for further improving devitrification success by fundamentally altering the physical conditions of warming [26]. As research continues to refine our understanding of the structural differences between glassy and liquid states [25] and their transformation kinetics, protocol efficiency and clinical outcomes in reproductive cryopreservation will continue to improve.
Implementing Next-Generation Warming Protocols: A Step-by-Step Guide
The vitrification of oocytes and embryos is a cornerstone of modern assisted reproductive technology (ART), enabling fertility preservation and optimizing laboratory workflows. A critical counterpart to this process is the warming protocol, which has historically involved a multi-step procedure to remove cryoprotectants and rehydrate cells. Recent research has focused on simplifying this process through one-step fast warming protocols, which significantly reduce processing time while maintaining, and in some cases enhancing, clinical outcomes. These protocols represent a significant shift in laboratory practice, moving from complex, time-consuming methods to streamlined, efficient processes.
The fundamental principle behind one-step warming is the rapid transition of vitrified specimens from a cryopreserved state to a viable culture environment through minimal procedural steps. Whereas conventional warming protocols typically require sequential exposure to decreasing concentrations of sucrose solutions (e.g., 1 M, 0.5 M, 0.25 M) with precise timing at specific temperatures, the one-step approach condenses this into a single rehydration step. This innovation is particularly valuable as ART laboratories worldwide face increasing volumes of frozen embryo transfer (FET) cycles and require methods that enhance efficiency without compromising success rates [27] [28].
Experimental Protocols and Methodologies
Detailed One-Step Fast Warming Protocol for Blastocysts
The one-step fast warming protocol for blastocysts has been systematically validated in multiple clinical settings. The following workflow details the specific steps based on published methodologies:
- Warming Solution Preparation: Prepare a thawing solution containing 1M sucrose. The solution may be supplemented with macromolecules such as 20% dextran serum supplement (DSS) and antibiotics like gentamicin in a HEPES-buffered medium [28].
- Initial Warming: Rapidly warm the vitrified blastocyst by exposing it to the pre-warmed 1M sucrose solution at 37°C for exactly 1 minute [27] [28]. This temperature is critical to prevent ice crystal formation and maintain the glass-like state achieved during vitrification.
- Direct Transfer to Culture Media: Immediately following the 1-minute incubation, transfer the blastocyst directly into pre-equilibrated culture media. There are no intermediate dilution steps [27] [28].
- Post-Warming Culture: Perform laser-assisted hatching if required by the laboratory's standard protocol after the blastocyst is placed in culture media [27].
- Incubation Before Transfer: Culture the warmed blastocysts for 1-4 hours under standard conditions (37°C, 6.3% CO₂, 5% O₂) prior to embryo transfer, allowing for assessment of re-expansion and viability [28].
Modified Warming Protocol for Oocytes
For vitrified oocytes, a modified warming protocol (MWP) has demonstrated enhanced developmental potential compared to conventional approaches:
- Warming Initiation: Expose vitrified oocytes to thawing solution (TS) at 37°C for 1 minute [11].
- Single Dilution Step: Transfer oocytes to a dilution solution (DS) for 3 minutes at room temperature [11].
- Washing and Rehydration: Perform a single wash in wash solution (WS) for 5-6 minutes at room temperature [11].
- Post-Warming Culture: Culture the warmed oocytes for 2 hours before performing intracytoplasmic sperm injection (ICSI) to assess survival and membrane integrity [11].
This modified approach for oocytes retains more steps than the blastocyst protocol but still represents a significant simplification compared to conventional methods, which often involve multiple sequential dilution steps with varying sucrose concentrations and extended incubation periods.
Comparative Outcomes Analysis
Blastocyst Warming Outcomes
Multiple studies have demonstrated that one-step fast warming protocols yield comparable clinical outcomes to conventional multi-step methods. The table below summarizes key reproductive outcomes from recent clinical studies:
Table 1: Comparative Clinical Outcomes of One-Step vs. Conventional Blastocyst Warming Protocols
| Outcome Parameter | One-Step Fast Warming | Conventional Multi-Step Warming | Statistical Significance | Study Reference |
|---|---|---|---|---|
| Survival Rate | 99.5% | 99.5% | Not significant | [29] |
| Clinical Pregnancy Rate | 63.0% | 59.9% | Not significant | [29] |
| Ongoing Pregnancy Rate | 60.4% | 55.4% | P = 0.011 | [29] |
| Implantation Rate | 63.6% | 57.0% | P = 0.0005 | [29] |
| Miscarriage Rate | 4.0% | 7.6% | P = 0.0001 | [29] |
| Live Birth Rate | 49.4% | 51.1% | Not significant | [27] |
The data consistently show that one-step warming protocols produce survival rates equivalent to conventional methods, with some studies reporting statistically significant improvements in ongoing pregnancy and implantation rates [29]. The significant reduction in miscarriage rates with one-step protocols suggests potential benefits in embryo viability and health post-warming.
Oocyte Warming Outcomes
For vitrified oocytes, the modified warming protocol has demonstrated notable advantages in key developmental parameters:
Table 2: Developmental Outcomes of Vitrified-Warmed Oocytes with Modified vs. Conventional Warming Protocols
| Outcome Parameter | Modified Warming Protocol (MWP) | Conventional Warming Protocol (CWP) | Fresh Oocytes (Control) | Statistical Significance |
|---|---|---|---|---|
| Survival Rate | 93.9% | 93.7% | N/A | Not significant |
| Normal Fertilization Rate | 79.6% | 79.5% | 83.0% | P < 0.05 (vs. fresh) |
| Blastocyst Formation Rate | 77.3% | 57.5% | 69.2% | P < 0.05 (MWP vs. CWP) |
| Usable Blastocyst Formation Rate | 51.4% | 35.4% | 48.5% | P < 0.05 (MWP vs. CWP) |
| Ongoing Pregnancy/Live Birth Rate | 66.7% | 50.4% | N/A | P < 0.05 |
The modified warming protocol for oocytes demonstrates a statistically significant improvement in blastocyst formation rates and usable blastocyst formation compared to conventional methods, making developmental outcomes more comparable to those achieved with fresh oocytes [11]. Multivariate analysis confirmed a positive association between the modified protocol and both usable blastocyst formation and ongoing pregnancy/live birth rates [11].
Workflow Efficiency Advantages
The implementation of one-step fast warming protocols offers substantial practical benefits for ART laboratory workflow and operational efficiency:
Time Reduction: The one-step blastocyst warming protocol reduces hands-on time by approximately 9-15 minutes per procedure compared to conventional methods [27] [28]. This time savings accrues significantly across multiple procedures per day.
Simplified Workflow: The streamlined process minimizes technical complexity, reducing the potential for procedural errors and operator variability [8]. Fewer solution preparation steps and simplified timing requirements enhance protocol standardization.
Increased Laboratory Throughput: The time efficiency enables laboratories to perform more frozen embryo transfer procedures per day without expanding staff, potentially reducing patient wait times and accelerating time to pregnancy [28].
Flexibility in Reagent Sourcing: Research on "Universal Warming Protocols" demonstrates that vitrified oocytes can be successfully warmed using kits from different manufacturers than those used for vitrification, increasing laboratory flexibility and reducing inventory constraints [15].
Research Reagent Solutions
The successful implementation of one-step fast warming protocols requires specific laboratory reagents and materials. The following table details key components and their functions:
Table 3: Essential Research Reagents for One-Step Fast Warming Protocols
| Reagent/Material | Composition/Characteristics | Function in Protocol | Commercial Examples |
|---|---|---|---|
| Thawing Solution | 1M sucrose, macromolecule supplement, antibiotics in HEPES-buffered medium | Initial warming and cryoprotectant dilution at 37°C | Kitazato, Irvine Scientific, Vitrolife |
| Culture Media | Continuous single culture medium with energy substrates and proteins | Final rinse and extended culture pre-transfer | Continuous Single Culture-NX Complete |
| Vitrification Media | Combination of permeating and non-permeating cryoprotectants | Initial vitrification process (protocol-specific) | Kitazato Vitrification Media |
| Oil Overlay | High-quality mineral oil or Ovoil | Prevents evaporation and maintains medium stability | Ovoil, Sage Mineral Oil |
| Equipment | Sterile pipettes, timing device, heated stage, stereomicroscope | Precise manipulation and temperature maintenance | Standard laboratory equipment |
The development of "Universal Warming Protocols" demonstrates that warming solutions from different manufacturers can be effectively used interchangeably, providing laboratories with greater flexibility in reagent sourcing [15]. Studies have shown that oocytes vitrified with Kitazato media can be successfully warmed using Irvine or Vitrolife media with comparable survival and fertilization rates [15].
One-step fast warming protocols represent a significant advancement in ART laboratory practice, offering streamlined workflows and time efficiencies without compromising clinical outcomes. The robust clinical data from multiple centers demonstrate that these protocols provide equivalent survival rates and comparable reproductive outcomes to conventional multi-step methods, with some studies suggesting potential improvements in ongoing pregnancy rates and reduced miscarriage rates [27] [29].
For vitrified oocytes, modified warming protocols have shown particularly promising results, with significantly higher blastocyst formation rates and improved ongoing pregnancy outcomes compared to conventional approaches [11]. The ability to use universal warming protocols that are compatible across different vitrification systems further enhances the practical utility of these methods in diverse laboratory settings [15].
Future research directions should include larger multicenter randomized controlled trials to validate these findings across broader patient populations. Additional studies exploring the molecular mechanisms underlying the successful outcomes with simplified warming protocols could provide insights into cellular responses to osmotic stress and rehydration. As ART laboratories continue to face increasing volumes and efficiency demands, one-step fast warming protocols offer a validated approach to maintaining high success rates while optimizing laboratory workflow and resource utilization.
The success of assisted reproductive technology (ART) increasingly depends on robust cryopreservation protocols that maintain cellular integrity during freeze-thaw cycles. Post-thaw rehydration represents a critical phase where improper handling can lead to osmotic shock, intracellular ice formation, and reduced cellular viability. This application note examines two predominant rehydration methodologies: sucrose-only systems and traditional multi-step systems, evaluating their impact on survival rates, fertilization potential, and clinical outcomes for vitrified oocytes and embryos. Within the broader context of modified warming protocol (MWP) research, optimizing rehydration strategies has demonstrated significant potential to enhance laboratory efficiency while maintaining or improving clinical outcomes [11] [30]. The transition toward simplified, physiologically compatible rehydration systems addresses both technical workflow challenges and biological imperatives for preserving developmental competence.
Comparative Performance Data
Oocyte Rehydration Outcomes
Table 1: Comparative Outcomes of Different Rehydration Protocols for Vitrified Oocytes
| Parameter | Conventional Multi-Step Protocol | Modified Warming Protocol (Sucrose-Optimized) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% [11] | 93.9% [11] | Not Applicable |
| ICSI Degeneration Rate | 2.7-3.4% [11] | 2.7-3.4% [11] | 2.8% [11] |
| Normal Fertilization Rate | 79.5-79.6% [11] | 79.5-79.6% [11] | 83.0% [11] |
| Blastocyst Formation Rate | 57.5% [11] | 77.3% [11] | 69.2% [11] |
| Usable Blastocyst Formation Rate | 35.4% [11] | 51.4% [11] | 48.5% [11] |
| Ongoing Pregnancy/Live Birth Rate | 50.4% [11] | 66.7% [11] | Not Reported |
Blastocyst Rehydration Outcomes
Table 2: Outcomes of One-Step vs. Multi-Step Rehydration for Vitrified Blastocysts
| Parameter | Multi-Step Rehydration Protocol | One-Step Rehydration Protocol |
|---|---|---|
| Survival Rate | >99% (Benchmark) [30] | >99% (Equivalent) [30] |
| Implantation Rate | Baseline | Significantly Higher [30] |
| Ongoing Pregnancy Rate | Baseline | Significantly Improved [30] |
| Miscarriage Rate | Baseline | Significantly Lower [30] |
Experimental Protocols
Modified Oocyte Warming Protocol (MWP)
This protocol is adapted from studies demonstrating improved blastocyst formation and pregnancy outcomes [11] [31].
Materials:
- Vitrified donor oocytes (stored in liquid nitrogen)
- Thawing Solution (TS)
- Dilution Solution (DS)
- Washing Solution (WS)
- Human Tubal Fluid (HTF) culture medium
- 37°C heated stage or incubator
Procedure:
- Rapid Warming: Quickly immerse the cryopreservation straw in a 37°C water bath or on a 37°C heated stage for 1 minute.
- Two-Step Rehydration:
- a. Transfer oocytes directly to Thawing Solution (TS) at 37°C for 2 minutes.
- b. Transfer oocytes to Dilution Solution (DS) at 37°C for 2 minutes [31].
- Washing: Thoroughly rinse oocytes in Washing Solution (WS) at room temperature.
- Final Culture: Transfer oocytes back to pre-equilibrated HTF medium and culture for 2 hours before intracytoplasmic sperm injection (ICSI) [11].
Key Modifications from Conventional Protocol:
- Temperature: DS step is performed at 37°C instead of 25°C [31].
- Simplification: The MWP often simplifies or combines dilution steps compared to the conventional three-step process [11].
One-Step Blastocyst Rehydration Protocol
This protocol, derived from Liebermann et al., streamlines the warming process for blastocysts, showing improved pregnancy rates [30].
Materials:
- Vitrified blastocysts
- One-step rehydration solution (1.0 M sucrose concentration)
Procedure:
- Rapid Warming: Warm the vitrified blastocyst rapidly in a 37°C water bath.
- One-Step Rehydration: Immediately place the blastocyst into a single rehydration solution containing 1.0 M sucrose.
- Direct Transfer: After the rehydration step, the blastocyst is ready for transfer without additional complex dilution steps.
Advantages:
- Workflow Efficiency: Simplifies the laboratory process, reducing hands-on time and potential for procedural error [30].
- Clinical Outcomes: Associated with higher implantation and ongoing pregnancy rates, along with lower miscarriage rates compared to multi-step protocols [30].
Workflow and Pathway Diagrams
Experimental Workflow for Protocol Comparison
Osmotic Stress Protection Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Post-Thaw Rehydration Studies
| Reagent / Material | Function & Application | Protocol Context |
|---|---|---|
| Sucrose Solutions (0.2M - 1.0M) | Creates an osmotic buffer to control water influx and prevent cellular swelling during cryoprotectant removal [30] [32]. | Core component in both multi-step and sucrose-only systems; concentration critical for success. |
| Thawing Solution (TS) | Initial warming solution for rapid temperature recovery and initiation of cryoprotectant dilution [11]. | First solution in all protocols; typically used at 37°C. |
| Dilution Solution (DS) | Intermediate solution for further reduction of intracellular cryoprotectant concentration [11]. | Used in multi-step protocols; temperature (25°C vs 37°C) is a key modification. |
| Washing Solution (WS) | Final solution to remove residual cryoprotectants and sucrose before return to culture medium [11]. | Final step in all protocols to prepare oocytes/embryos for culture. |
| Human Tubal Fluid (HTF) Medium | Physiologically-compatible culture medium for post-wash recovery and subsequent development [31]. | Standard medium for post-thaw culture before fertilization or transfer. |
| Cryoprotective Agents (CPAs) | Small permeable molecules (e.g., PrOH, Meâ‚‚SO) that protect against ice crystal formation during vitrification [32] [33]. | Removed during rehydration; their controlled efflux is essential for survival. |
| Pivmecillinam Hydrochloride | Pivmecillinam Hydrochloride, CAS:32887-03-9, MF:C21H34ClN3O5S, MW:476.0 g/mol | Chemical Reagent |
| Paspalic acid | Paspalic acid, CAS:5516-88-1, MF:C16H16N2O2, MW:268.31 g/mol | Chemical Reagent |
The optimization of post-thaw rehydration protocols represents a significant advancement in reproductive cryobiology. Evidence strongly indicates that sucrose-only and simplified rehydration systems can not only streamline laboratory workflows but also enhance key clinical outcomes, including blastocyst formation rates and ongoing pregnancy success. The modified protocols, characterized by elevated temperature handling and reduced process steps, demonstrate that careful management of osmotic stress is more critical than procedural complexity. For researchers and clinicians, adopting these refined rehydration strategies offers a promising path to maximize the potential of vitrified oocytes and embryos, ultimately improving the efficiency and success of assisted reproductive technologies.
Within the broader research on modified warming protocols (MWP) for vitrified oocytes and embryos, sample volume optimization represents a critical frontier. The primary challenge in cryopreservation warming techniques lies in balancing the competing demands of rapid warming rates against practical handling constraints. While rapid warming is essential to prevent devitrification and ice crystal formation, the practicalities of laboratory workflow, technician fatigue, and solution volumes must be optimized for consistent clinical success. Recent studies have demonstrated that modified warming protocols can significantly improve embryonic development and pregnancy outcomes by addressing these very factors [5] [11]. This protocol examines the key principles of sample volume optimization and its direct impact on warming efficiency for vitrified reproductive cells.
Comparative Analysis of Warming Protocols
The evolution from conventional warming protocols (CWP) to simplified, rapid approaches has highlighted the significant role of volume and timing in warming outcomes. The following table summarizes key comparative findings from recent clinical studies.
Table 1: Comparative Outcomes of Conventional vs. Modified Warming Protocols
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Control Group |
|---|---|---|---|
| Protocol Description | Multi-step dilution at room temperature [11] | Single-step, rapid warming at 37°C [11] [34] | Not applicable |
| Survival Rate | 93.7% [5] | 93.9% [5] | Not applicable |
| Blastocyst Formation Rate | 57.5% [5] | 77.3% [5] | 69.2% [5] |
| Usable Blastocyst Formation Rate | 35.4% [5] | 51.4% [5] | 48.5% [5] |
| Ongoing Pregnancy/Live Birth Rate | 50.4% [11] | 66.7% [11] | Not reported |
The data demonstrates that the MWP, characterized by its simplified workflow, not only maintains high survival rates but significantly enhances developmental potential. The single-step process reduces total warming time and minimizes the number of fluid transfers, thereby reducing osmotic stress and improving laboratory efficiency [34]. The comparable survival rates between CWP and MWP indicate that the rapid dilution in a single step does not compromise membrane integrity, while the markedly improved blastocyst formation suggests enhanced cytoplasmic preservation.
Experimental Protocols for Volume and Warming Rate Studies
Protocol: Evaluating Single-Step Warming with Variable Volumes
This protocol is designed to test the hypothesis that reducing warming volumes in a single-step method improves warming rates without compromising oocyte and embryo viability.
Materials:
- Vitrified oocytes or blastocysts
- Warming solution (1M sucrose or trehalose solution) [8]
- Base medium (e.g., Human Tubal Fluid)
- 37°C dry block heater or thermal plate
- Sterile culture dishes
- Timing device
- Micropipettes and tips
Method:
- Preparation: Pre-warm all solutions to 37°C using a dry block heater to ensure temperature stability and prevent temperature drop during handling [11].
- Warming Setup: Aliquot the warming solution into pre-warmed culture dishes. Test different volumes (e.g., 50 µL, 1 mL) to assess the impact of volume on temperature kinetics.
- Rapid Warming & Dilution:
- Rapidly immerse the vitrified straw or carrier directly into the 1 mL warming solution for 1 minute [11] [34].
- For the single-step dilution, directly transfer the contents (oocyte/embryo and warming solution) into a 10 mL volume of pre-warmed base medium. This universal post-warming dilution rapidly reduces the cryoprotectant concentration [8].
- Assessment: After a 2-hour culture period, assess survival rates based on morphological integrity, including membrane intactness and absence of cytoplasmic vacuoles [11].
Protocol: Quantifying Warming Rate via Crystal Formation Assay
This functional assay assesses the efficacy of different warming volumes by quantifying ice crystal formation, a direct indicator of warming rate.
Materials:
- Model solution (e.g., VS containing permeating cryoprotectants)
- Temperature logger with fine-gauge thermocouple
- Water bath or surface heater set to 37°C
- Test volumes: 50 µL, 100 µL, 500 µL, 1 mL
Method:
- Vitrification Simulation: Load model solution into carriers identical to those used for oocytes.
- Controlled Warming: Immerse the carrier into the pre-defined test volumes of warming solution maintained at 37°C.
- Temperature Recording: Use the thermocouple to record the temperature rise from -196°C to 0°C. The rate of temperature change (°C/second) is the critical metric.
- Outcome Measurement: Assess the sample for devitrification (ice crystal formation) visually under a microscope. Effective protocols achieving maximum warming rates will show no visible crystals.
Workflow and Logical Pathway
The following diagram illustrates the decision-making pathway and experimental workflow for optimizing sample volume in warming protocols.
Research Reagent Solutions
Successful implementation of a modified warming protocol depends on a specific set of reagents and materials. The table below details the essential components.
Table 2: Essential Research Reagents for Modified Warming Protocols
| Reagent/Material | Function | Application Note |
|---|---|---|
| Thawing Solution (TS) | Primary solution for rapid warming and initial cryoprotectant dilution. Contains non-permeating solutes like sucrose [8]. | Use pre-warmed to 37°C. Incubation is typically 1 minute [11]. |
| Universal Warming Solution | A single solution compatible with vitrification kits from different brands, simplifying workflow [8]. | Enables standardization across labs using diverse cryopreservation products. |
| Base Culture Medium | Serves as the high-volume dilution medium (e.g., 10 mL) for single-step rehydration after initial warming [8]. | Rapidly reduces cryoprotectant concentration, minimizing toxicity and osmotic stress. |
| Dry Block Heater | Provides stable, uniform heating of warming solutions to a precise 37°C [11]. | Critical for maintaining maximum warming rate; superior to water baths for contamination control. |
Sample volume optimization is a fundamental aspect of designing effective warming protocols for vitrified oocytes and embryos. The evidence confirms that moving towards low-volume, single-step warming methods, followed by high-volume dilution, successfully balances the need for rapid warming rates with practical laboratory handling. This approach mitigates osmotic stress, streamlines workflow, and ultimately leads to significantly improved embryonic development and clinical pregnancy outcomes, making it a superior alternative to conventional, multi-step protocols.
The cryopreservation of oocytes and embryos through vitrification is a cornerstone of modern assisted reproductive technology (ART), enabling fertility preservation, elective egg freezing, and the widespread adoption of single-embryo transfer policies. The warming process is a critical determinant of post-thaw survival and developmental potential. While conventional warming protocols (CWP) involving multi-step osmotic rehydration have been the standard, recent research demonstrates that modified warming protocols (MWP) can enhance efficiency and outcomes. This application note synthesizes the latest evidence to provide detailed, stage-specific protocols for the warming of vitrified oocytes, cleavage-stage embryos, and blastocysts, contextualized within the broader thesis that optimized, tailored warming methods are vital for maximizing ART success.
Modified Warming Protocol for Vitrified Oocytes
Oocytes are highly sensitive to cryopreservation-induced stress due to their large size, high water content, and delicate meiotic spindle structure. A Modified Warming Protocol (MWP) for oocytes has been developed to mitigate these challenges.
Experimental Workflow and Rationale
The following diagram illustrates the key procedural differences between the Conventional Warming Protocol (CWP) and the Modified Warming Protocol (MWP) for oocytes.
(Caption: Workflow comparison of conventional versus modified oocyte warming protocols.)
Detailed Methodology
The MWP for oocytes is an ultrafast, single-step process that significantly simplifies the laboratory workflow [5]. The specific steps are as follows:
- Rapid Warming: Immediately upon removal from liquid nitrogen, vitrified oocytes on the cryodevice are plunged directly into a pre-warmed (37°C) Thawing Solution (TS) for 1 minute. This rapid warming prevents the devitrification (formation of ice crystals) and preserves the structural integrity of the glass-like state.
- Single-Step Dilution: The MWP eliminates the subsequent Dilution Solution (DS) and Wash Solution (WS) steps used in the CWP. The single step in TS is sufficient for both warming and the initial dilution of cryoprotectants.
- Direct Transfer to Culture: After 1 minute in TS, the oocytes are directly transferred to the culture medium. This simplified approach reduces total handling time and minimizes osmotic stress by avoiding multiple transfers between solutions at room temperature [5].
Key Outcomes and Data
A large-scale retrospective cohort study comparing this MWP to the CWP demonstrated significant improvements in embryonic development and pregnancy outcomes, making the results of vitrified-warmed oocytes comparable to those of fresh oocytes [5].
Table 1: Comparative Outcomes of Conventional vs. Modified Oocyte Warming Protocols
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | - |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7%* | - |
Note: *P < 0.05 vs. CWP. Multivariate analysis confirmed a positive association between MWP and both usable blastocyst formation and ongoing pregnancy/live birth [5].
Tailored Protocols for Embryos: Cleavage-Stage vs. Blastocyst-Stage
Embryos at different developmental stages exhibit varying cryotolerance, necessitating tailored warming approaches. Recent evidence supports the use of simplified, one-step warming for both cleavage-stage and blastocyst-stage embryos.
One-Step Warming Protocol for Embryos
The one-step warming (OW) protocol represents a significant simplification and can be effectively applied to both cleavage-stage and blastocyst-stage embryos [35] [36].
Detailed Methodology:
- Warming: Vitrified embryos (cleavage or blastocyst stage) are rapidly warmed by plunging the cryodevice directly into a single Thawing Solution (TS) pre-warmed to 37°C for 1 minute [35].
- Direct Transfer to Culture: After the 1-minute incubation, the embryos are immediately transferred to the culture medium. This protocol omits all subsequent dilution and washing steps used in standard multi-step warming (SW) protocols, which typically involve a 13-minute process with Thawing, Dilution, and Washing solutions [35].
Comparative Outcomes by Developmental Stage
Studies have rigorously compared this one-step approach to standard multi-step warming, with outcomes detailed below.
Table 2: Outcomes of One-Step vs. Standard Multi-Step Embryo Warming
| Parameter | One-Step Warming (OW) | Standard Multi-Step Warming (SW) |
|---|---|---|
| Cleavage-Stage Embryos | ||
| Survival Rate | 100% | 100% |
| Blastulation Rate | 78% | 73% |
| Blastocyst-Stage Embryos | ||
| Survival Rate | 99% | 99% |
| Full Re-expansion (24h post-warming) | 98% | 97% |
| Time to Full Re-expansion | 3.20 ± 3.03 h* | 2.14 ± 2.17 h |
| Clinical Outcomes (Blastocyst Transfer) | ||
| Fetal Heartbeat Confirmation Rate | 43.9% | 47.7% |
Note: *Although the time to re-expansion was slightly longer with OW, the ultimate proportion of fully re-expanded blastocysts was equivalent [35] [36].
Key Experimental Findings
- Developmental Potential: For cleavage-stage embryos, OW resulted in superior or comparable rates of morulation (96% vs. 85%) and blastulation compared to SW [35].
- Morphokinetics: Time-lapse monitoring revealed that cleavage-stage embryos warmed with OW experienced a reduced frequency of collapses (30% vs. 50%), indicating less cellular stress [35].
- Functional Competence: An in vitro adhesion assay using blastocysts warmed with either protocol showed no significant differences in adhesion rate or outgrowth area, suggesting their implantation potential is equivalent [35].
- Clinical Equivalence: A prospective clinical study confirmed that one-step fast-warming of blastocysts yields comparable survival, pregnancy, implantation, and live birth rates to the standard protocol [34].
The Scientist's Toolkit: Essential Research Reagents
The successful implementation of vitrification and warming protocols relies on a suite of specialized reagents. The concept of a "Universal Warming Protocol" (UWP) is gaining traction, demonstrating that oocytes vitrified with one commercial medium can be effectively warmed using solutions from different suppliers, increasing laboratory flexibility [37].
Table 3: Key Research Reagent Solutions for Vitrification and Warming
| Reagent Category | Function | Examples & Notes |
|---|---|---|
| Permeable Cryoprotectants | Penetrate the cell, replacing water to prevent ice crystal formation during cooling. | Ethylene Glycol (EG), Dimethyl sulfoxide (DMSO), Propanediol (PROH). Often used in combination [6]. |
| Non-Permeable Cryoprotectants | Do not enter the cell; create an osmotic gradient to draw water out during equilibration. | Sucrose, Trehalose. Concentration in warming solution is critical (e.g., 0.1M optimal for rat zygotes) [16]. |
| Base Media | Provide ionic and nutrient support during the stressful vitrification/warming process. | Phosphate-Buffered Saline (PB1), Human Tubal Fluid (HTF) [16]. |
| Commercial Vitrification Kits | Integrated systems of solutions for a standardized workflow. | Kitazato (Japan), Irvine Scientific (USA), Vitrolife (Sweden) [37]. |
| Commercial Warming Kits | Integrated systems for standard or universal warming. | Kitazato, Irvine Scientific, RapidWarm Omni (Vitrolife). A UWP with RapidWarm Omni showed a 94% oocyte survival rate [37]. |
| Qstatin | Qstatin, MF:C7H5BrN2O2S2, MW:293.2 g/mol | Chemical Reagent |
| Quiflapon | Quiflapon, CAS:136668-42-3, MF:C34H35ClN2O3S, MW:587.2 g/mol | Chemical Reagent |
The paradigm for warming vitrified oocytes and embryos is shifting towards simplified, faster, and more robust protocols. The evidence confirms that a Modified Warming Protocol (MWP) for oocytes, which eliminates traditional dilution and washing steps, not only streamlines laboratory workflow but also significantly improves blastocyst formation and ongoing pregnancy rates. Furthermore, a one-step warming (OW) protocol is a safe and effective alternative for both cleavage-stage and blastocyst-stage embryos, without compromising survival, developmental potential, or clinical outcomes. These stage-tailored protocols underscore a critical advancement in ART laboratory practice: optimizing the warming process is as crucial as the vitrification process itself for maximizing the reproductive potential of cryopreserved specimens.
Within the broader research on Modified Warming Protocols (MWP) for vitrified oocytes and embryos, controlling the physical handling of specimens during routine laboratory procedures is a critical factor influencing cryosurvival and subsequent developmental competence. This application note addresses the specific issue of Exposed-to-Air Frequency (EAF)—the number of times a cryopreserved specimen is temporarily removed from liquid nitrogen during storage—and its potential to cause transient warming injuries. Transient warming occurs when a frozen sample experiences a short-term temperature increase, which can lead to the formation of damaging ice crystals within cells upon re-freezing [38]. While recent research indicates that clinical outcomes may remain stable despite multiple exposures [39], meticulous handling protocols are essential for minimizing theoretical risks and preserving the integrity of precious biological samples for researchers and drug development professionals.
Defining Transient Warming and EAF
Transient warming is a phenomenon characterized by a sudden, short-term increase in the temperature of a cryopreserved sample. This can occur during multiple stages of handling, including:
- Sample Retrieval: When a specific cane or straw is removed from a liquid nitrogen tank, adjacent samples not being retrieved are temporarily exposed to warmer air [38].
- Inventory Management: Transferring canes between the main storage tank and a temporary LNâ‚‚ container for identification or reorganization [39].
- Transportation: Moving samples between storage dewars or during shipment, as samples are exposed to ambient temperatures during transfer steps [38].
The Exposed-to-Air Frequency (EAF) is a quantifiable metric for a specimen's cumulative exposure to these transient warming events. Each retrieval event constitutes one EAF increment [39]. Although the duration of each exposure may be brief, even seconds of exposure can be sufficient to impact sample viability by promoting ice recrystallization, which damages cellular structures and reduces post-thaw recovery [38].
Impact Assessment: Experimental Data on EAF and Cryotolerance
A large-scale clinical study retrospectively analyzed 9,200 vitrified-warmed embryo transfer cycles to investigate the correlation between EAF and clinical outcomes. The embryos were grouped based on their EAF (2, 4, 6, 8, or ≥10). The findings provide crucial insights for risk assessment.
Table 1: Clinical Outcomes by Exposed-to-Air Frequency (EAF) for Different Embryo Stages [39]
| Embryo Stage | EAF Group | Post-Warming Survival Rate | Implantation Rate | Clinical Pregnancy Rate | Live Birth Rate |
|---|---|---|---|---|---|
| Day 3 Embryos | 2 | ~99%* | No significant difference | No significant difference | No significant difference |
| 4 | ~99%* | ||||
| 6 | ~99%* | ||||
| 8 | ~99%* | ||||
| ≥10 | ~99%* | ||||
| Day 5 Blastocysts | 2 | No significant difference | No significant difference | No significant difference | No significant difference |
| 4 | |||||
| 6 | |||||
| 8 | |||||
| ≥10 | |||||
| Day 6 Blastocysts | 2 | No significant difference | No significant difference | No significant difference | No significant difference |
| 4 | |||||
| 6 | |||||
| 8 | |||||
| ≥10 |
The survival rate of Day 3 embryos showed a statistically significant difference (P=0.015) among groups, but the change was not EAF-dependent and rates remained high [39].
Multivariate logistic regression analysis confirmed that EAF did not adversely affect clinical pregnancy or live birth rates across all embryo stages [39]. This suggests that human vitrified embryos in open systems possess significant resilience to the thermal fluctuations caused by repeated retrieval.
Beyond EAF, the origin of the zygote also significantly impacts cryotolerance. Systematic comparisons in rat models demonstrate that in vivo-fertilized oocytes consistently exhibit higher cryotolerance and developmental ability post-warming compared to in vitro-fertilized oocytes [40].
Table 2: Impact of Fertilization Origin on Cryotolerance in Rat Models [40]
| Strain | Fertilization Method | Survival Rate Post-Warming | Developmental Ability to Fetuses |
|---|---|---|---|
| SD Rats | In Vivo | High | High |
| In Vitro | Lower than in vivo | Lower than in vivo | |
| F344 Rats | In Vivo | High | High |
| In Vitro | Lower than in vivo | Lower than in vivo |
Essential Protocols for Minimizing Transient Warming Injuries
Protocol 1: Standardized Handling to Minimize EAF
Principle: Limit the number and duration of exposures by optimizing laboratory workflow and inventory management.
- Workflow Planning: Retrieve a specific cane or container only once to perform all required actions (e.g., warming, inventory audit, relocation) before returning it to the main tank [39] [38].
- Inventory Management: Utilize a robust electronic witnessing system to track the precise location of each straw and its retrieval history, enabling efficient planning to minimize unnecessary handling [39].
- Rapid Handling: Train staff to perform all operations with the cane in the vapor phase of LNâ‚‚ or submerged in a temporary LNâ‚‚ container to minimize the temperature spike during transfer [6].
Protocol 2: Advanced Warming to Mitigate Injury
Principle: Utilize rapid and optimized warming solutions to counteract potential ice crystal growth formed during transient warming events.
- Modified Warming Protocol (MWP) for Oocytes/Embryos:
- Rapid Warming: Transfer the cryotop directly into a pre-warmed (37°C) thawing solution (TS) for 1 minute [5].
- Single-Step Dilution/Rehydration: Move the oocytes/embryos directly into a universal warming solution. This solution can contain non-permeating solutes like sucrose or trehalose at an optimized concentration (e.g., 0.1 M for rat zygotes) to control osmotic stress [8] [16].
- Incubation: Incubate in this single solution for a defined period (e.g., 10-15 minutes) to allow for complete dilution of cryoprotectants and rehydration [8] [41].
This MWP has been shown to improve blastocyst formation rates and ongoing pregnancy/live birth rates for vitrified-warmed oocytes compared to conventional multi-step protocols [5].
Protocol 3: Use of Technological Adjuncts
Principle: Incorporate novel cryoprotectant additives to physically suppress ice crystal growth.
- Ice Recrystallization Inhibitors (IRIs): Supplement standard vitrification and warming media with IRIs. These molecules function during transient warming events by controlling ice growth, resulting in smaller, less damaging ice crystals and increased post-thaw viability [38].
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents and Materials for Minimizing Transient Warming Injuries
| Item Category | Specific Examples | Function & Application Note |
|---|---|---|
| Cryopreservation Devices | Cryotop, Open Pulled Straw (OPS), Cryoloop | Microvolume carriers enabling ultra-rapid cooling and warming rates, crucial for vitrification [6]. |
| Vitrification/Warming Kits | Kitazato Vitrification/Warming Kits; Universal Warming Solutions | Pre-formulated solutions containing permeating cryoprotectants (e.g., DMSO, EG) and non-permeating solutes (e.g., sucrose, trehalose) for controlled dehydration/rehydration [39] [8]. |
| Novel Cryo-Additives | Ice Recrystallization Inhibitors (IRIs) | Molecules added to vitrification/warming media to control ice growth during transient warming events, improving post-thaw cell recovery [38]. |
| Inventory Management | Reproductive Medicine Management Electronic System | Tracks straw location and retrieval history (EAF), enabling efficient workflow planning to minimize unnecessary exposure [39]. |
| Optimized Sucrose Solutions | 0.1 M Sucrose in Warming Solution | An optimized concentration for warming rat zygotes, enhancing survival and developmental rates by reducing osmotic shock [16]. |
| Quinacrine methanesulfonate | Quinacrine methanesulfonate, CAS:316-05-2, MF:C25H38ClN3O7S2, MW:592.2 g/mol | Chemical Reagent |
| Nibroxane | Nibroxane, CAS:53983-00-9, MF:C5H8BrNO4, MW:226.03 g/mol | Chemical Reagent |
Within the research framework of modified warming protocols, a comprehensive strategy for minimizing transient warming injuries extends beyond simply limiting EAF. While evidence suggests that current vitrification systems are robust enough to withstand multiple air exposures without compromising key clinical outcomes [39], best practices dictate a proactive approach. This involves integrating meticulous laboratory handling protocols, adopting advanced single-step warming methods that reduce procedural stress [5] [8], and exploring the use of novel adjuncts like Ice Recrystallization Inhibitors [38]. For researchers in drug development and pre-clinical modeling, particular attention should also be paid to the biological source of embryos, as in vivo-derived zygotes demonstrate superior cryotolerance [40]. Implementing these combined strategies ensures the highest standards of sample integrity and viability for critical research applications.
Troubleshooting Common Pitfalls and Strategies for Protocol Optimization
Suboptimal survival of vitrified oocytes and embryos remains a significant challenge in assisted reproductive technology (ART), directly impacting clinical outcomes. The warming process is a critical phase where osmotic stress and cryoprotectant toxicity can compromise cellular integrity, leading to reduced viability and developmental potential. This application note provides a comprehensive diagnostic and corrective framework, contextualized within the broader research on Modified Warming Protocols (MWP), to assist researchers and clinicians in optimizing survival rates. We present structured quantitative data, detailed experimental protocols for key assessments, and visual tools to guide laboratory troubleshooting and protocol refinement, with the goal of enhancing the efficacy of vitrified-warmed oocyte and embryo programs.
Quantitative Data Analysis: Conventional vs. Modified Warming Protocols
A substantial body of evidence demonstrates that modifications to the conventional warming protocol (CWP) can significantly improve outcomes. The tables below summarize key comparative data from recent studies, providing a benchmark for laboratory performance and protocol evaluation.
Table 1: Oocyte Survival and Embryological Outcomes Following Warming
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Oocyte Survival Rate | 93.7% (7967/8506) [11] [5] | 93.9% (920/980) [11] [5] | Not Applicable |
| Normal Fertilization Rate (ICSI) | 79.5-79.6% [11] [5] | 79.5-79.6% [11] [5] | 83.0% [11] [5] |
| Blastocyst Formation Rate | 57.5% [11] [5] | 77.3% [11] [5] | 69.2% [11] [5] |
| Usable Blastocyst Formation Rate | 35.4% [11] [5] | 51.4% [11] [5] | 48.5% [11] [5] |
Table 2: Clinical Pregnancy Outcomes
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Notes |
|---|---|---|---|
| Ongoing Pregnancy/Live Birth Rate | 50.4% [11] [5] | 66.7% [11] [5] | Multivariate analysis showed a positive association with MWP (aOR=1.899) [11] [5] |
| Cumulative Live Birth Rate (Fresh vs. Vitrified Oocytes) | 66.7% (Vitrified Donor Oocytes) [42] | 69.6% (Fresh Donor Oocytes) [42] | No significant difference (p>0.05); includes double vitrification [42] |
Experimental Protocols for Key Assessments
Protocol 1: Modified Warming Protocol (MWP) for Oocytes
This protocol simplifies the warming process into an ultrafast, single-step process, eliminating the need for dilution and wash solutions at room temperature to reduce osmotic stress and improve laboratory efficiency [11] [5].
- Principle: Rapid dilution of cryoprotectants at 37°C to prevent ice crystallization and mitigate osmotic shock.
- Materials:
- Thawing Solution (TS)
- Pre-warmed culture media (e.g., TCM-199)
- Sterile 35mm petri dishes
- Pre-warmed lightweight paraffin oil
- Timer
- Water bath or heated stage set to 37°C
- Method:
- Preparation: Pre-warm the TS to 37°C. Prepare a culture dish with pre-equilibrated medium under oil and place it in the incubator (5% CO₂, 37°C) [11] [5].
- Warming: Rapidly remove the cryopreservation carrier from liquid nitrogen and immerse it directly into the TS at 37°C for 1 minute. Ensure the sample is fully submerged. If the sample floats, gently move it to the center of the drop [43].
- Post-Warm Culture: Immediately transfer the oocytes from the TS to the pre-equilibrated culture medium.
- ICSI Timing: Perform intracytoplasmic sperm injection (ICSI) 2–3 hours after warming [43].
Protocol 2: Survival and Integrity Assessment of Warmed Oocytes
This diagnostic protocol is used to evaluate the immediate post-warm viability of oocytes, providing a critical key performance indicator (KPI) for the warming process.
- Principle: Microscopic evaluation of cellular morphology to identify cryopreservation-induced damage.
- Materials:
- Inverted microscope with high-contrast optics (e.g., Hoffman Modulation Contrast)
- Warming reagents as per Protocol 1
- Hyaluronidase solution for denuding
- Method:
- After warming and a brief culture period, denude the oocytes from surrounding cumulus cells using hyaluronidase and mechanical pipetting [42].
- Place the denuded oocytes in a culture dish and examine under the inverted microscope at 200x and 400x magnification.
- Assessment Criteria [43]:
- Survived Oocyte: Exhibits normal cell membrane morphology, clear cytoplasm, and a normal perivitelline space.
- Non-Survived Oocyte: Shows signs of darkened cytoplasm, massive vacuolization, cytoplasmic leakage, or a grossly abnormal perivitelline space.
- Calculate the survival rate: (Number of survived oocytes / Total number of warmed oocytes) x 100.
Protocol 3: Blastocyst Outgrowth Assay for Viability
This functional assay assesses the implantation potential of warmed blastocysts, providing a more robust measure of viability beyond simple morphological survival.
- Principle: The ability of a blastocyst to attach to a substrate and undergo trophectoderm outgrowth is a strong indicator of its functional health and implantation competence.
- Materials:
- Four-well culture dishes
- Laboratory-grade, gelatin-based substrate or cellular fibronectin
- SOFaa or G-TL culture medium
- Incubator (5% O₂, 6% CO₂, 37°C)
- Method:
- Coat the wells of the culture dish with the substrate and incubate for at least 2 hours before the assay.
- After warming and a 2-hour re-expansion culture, transfer individual blastocysts to the coated wells.
- Culture the blastocysts for up to 96 hours, changing the medium every 24 hours.
- Assessment: Monitor daily for attachment and the initiation of trophectoderm outgrowth. The blastocyst is considered to have high viability if robust outgrowth is observed. Studies have shown that while shortened warming protocols may induce some cell necrosis, they can maintain outgrowth competence comparable to conventional protocols [44].
Diagnostic Framework and Corrective Actions
A systematic approach is required to diagnose the root causes of suboptimal survival. The following diagram and table outline a step-by-step diagnostic and corrective workflow.
Diagram 1: Diagnostic Framework for Suboptimal Survival
Table 3: Corrective Actions for Common Issues in Vitrification and Warming
| Identified Issue | Root Cause | Corrective Actions |
|---|---|---|
| Low Survival in Both Oocytes & Embryos | Cryoprotectant toxicity; improper carrier loading [43] | Validate exposure times in Equilibration and Vitrification solutions. Ensure proper training for carrier loading. Use commercial reagents with quality control [43]. |
| Low Survival with Osmotic Shock Signs | Suboptimal temperature or timing during warming [11] [44] | Strictly control temperature of Thawing Solution (37°C). Adhere to precise timings. For blastocysts, consider that shortened protocols may induce over-rehydration [44]. |
| Low Oocyte-Specific Survival | High sensitivity of oocytes to cryopreservation stress [11] | Transition from Conventional Warming Protocol (CWP) to a Modified Warming Protocol (MWP). The MWP enhances blastocyst formation and pregnancy outcomes, making it similar to fresh oocytes [11] [5]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagent Solutions for Vitrification and Warming Research
| Reagent / Material | Function | Research Considerations |
|---|---|---|
| Vitrification & Warming Kits | Commercial kits provide standardized cryoprotectants (e.g., Ethylene Glycol, DMSO) and sucrose-based solutions for vitrification and warming. | Prefer kits with comprehensive quality control (mouse embryo assays, endotoxin testing) [43]. Laboratories should have two different brands available for emergency supply issues [43]. |
| Cryopreservation Carriers | Devices (open or closed) for holding samples during plunging into liquid nitrogen. | Closed carriers are recommended for gametes/embryos from patients with infections [43]. Limit oocytes to ≤5 per carrier [43]. |
| HEPES-Buffered Medium | Provides pH stability during procedures outside the COâ‚‚ incubator, such as during the warming process. | Used as a base for Thawing and Dilution Solutions to maintain physiological pH during critical warming steps [42]. |
| Hyaluronidase Enzyme | Enzymatically removes cumulus cells from the oocyte prior to ICSI and post-warm survival assessment. | Essential for accurate morphological evaluation of oocyte survival after warming [42]. |
| Artificial Shrinkage Laser | Creates an opening in the trophectoderm of blastocysts to allow controlled shrinkage before vitrification. | Position laser pulses at the cellular junction of the trophectoderm, away from the inner cell mass [43]. The benefit for pregnancy outcomes is still debated. |
| Qyl-685 | Qyl-685, CAS:210355-14-9, MF:C20H24N7O5P, MW:473.4 g/mol | Chemical Reagent |
Addressing suboptimal survival requires a dual approach: rigorous diagnostic troubleshooting backed by quantitative KPIs, and the adoption of evidence-based protocol improvements. The data and protocols presented here demonstrate that Modified Warming Protocols (MWP) offer a significant advancement over conventional methods, particularly for vitrified oocytes, by improving blastocyst formation and live birth rates. By implementing the structured frameworks, detailed experimental protocols, and corrective actions outlined in this document, research and clinical laboratories can systematically enhance the outcomes of their oocyte and embryo vitrification programs.
Optimizing Cryoprotectant Agent (CPA) Concentration and Composition for Specific Cell Types
Within the broader scope of research on modified warming protocols for vitrified oocytes and embryos, the optimization of cryoprotectant agents (CPAs) is a foundational pillar. The efficacy of any warming protocol is inherently linked to the composition and concentration of CPAs used during the vitrification stage [5]. CPAs are essential for protecting cells from cryo-injuries, primarily ice crystal formation and osmotic stress, during the freezing and thawing processes [45] [46]. While traditional CPAs like dimethyl sulfoxide (DMSO) are widely used, their inherent toxicity and the need for cell-specific formulations have driven the development of advanced, less toxic alternatives and tailored protocols [47]. This document provides detailed application notes and protocols for optimizing CPA strategies, directly supporting the goal of enhancing the survival and clinical outcomes of vitrified reproductive cells [5].
CPA Composition and Selection for Specific Cell Types
Selecting the appropriate CPA is not a one-size-fits-all approach; it requires careful consideration of cell type, permeability, and sensitivity to osmotic stress and chemical toxicity.
Classes of Cryoprotectants
CPAs are broadly categorized into two classes:
- Permeating CPAs: Small, neutral molecules that cross the cell membrane to protect against intracellular ice formation. Examples include DMSO, ethylene glycol (EG), propylene glycol, and glycerol [47] [46].
- Non-Permeating CPAs: Larger molecules that remain outside the cell, providing extracellular protection by mitigating osmotic shock and ice crystal growth. This category includes sugars (sucrose, trehalose, raffinose), polymers (polyvinyl pyrrolidone), and proteins (albumin) [47] [8].
Cell-Type-Specific CPA Recommendations
Emerging research provides guidance on optimizing CPA cocktails for different, sensitive cell types relevant to advanced reproductive technologies.
Table 1: Optimized CPA Formulations for Specific Cell Types
| Cell/Tissue Type | Recommended CPA Formulation | Key Characteristics & Rationale | Reported Outcome |
|---|---|---|---|
| Oocytes [5] | Permeating CPA (e.g., DMSO or EG) + Non-permeating sugar (e.g., sucrose) | High sensitivity to chilling injury and osmotic stress. Sugar helps in dehydration and stabilizes the membrane. | High survival rates (>93%) and improved blastocyst formation with optimized warming. |
| Adipose Tissue [48] | 70% Glycerol in PBS | Glycerol is less toxic and shows high efficacy as a natural osmolyte for complex tissues. Superior to DMSO+FBS and trehalose. | High tissue integrity, G3PDH activity comparable to fresh tissue, and superior in vivo retention rates. |
| Stem Cells (hIPSCs, MSCs) [47] | Serum-free, defined media with DMSO alternatives: Trehalose, Sucrose, or combinations with polymers (e.g., P188). | Avoids lot-to-lot variability and immunogenicity of serum. Chemically defined conditions are crucial for clinical applications. | Maintained pluripotency, proliferation, and differentiation capabilities post-thaw. |
| Lipid Nanoparticles (LNPs) [49] | Betaine (25 mg/mL) + Trehalose (25 mg/mL) - "BT-CPA" | Betaine incorporates into LNPs during freezing, enhancing endosomal escape and mRNA delivery efficacy post-thaw. | ~2.4-fold higher mRNA delivery efficiency in vitro and stronger immune responses in vivo. |
Quantitative Data and Experimental Protocols
Protocol 1: Evaluating Glycerol for Adipose Tissue Cryopreservation
This protocol, adapted from a 2022 study, details the steps for cryopreserving human adipose tissue using glycerol as a low-toxicity CPA [48].
Experimental Workflow:
Key Materials:
- Human adipose tissue (from liposuction)
- Glycerol-PBS solutions (60%, 70%, 80%, 90%, 100% v/v)
- Controlled-rate freezing container (e.g., "Mr. Frosty" or programmable freezer)
- Liquid nitrogen storage tank
- G3PDH activity assay kit (for metabolic activity)
- BALB/c nude mice (for in vivo transplantation model)
Detailed Methodology:
- Tissue Preparation: Wash harvested adipose tissue with PBS to remove free oil and blood. Divide the pure adipose tissue into 1 mL samples.
- CPA Addition: Mix each 1 mL tissue sample with 1 mL of the test CPA (e.g., 70% glycerol solution) at room temperature in a cryovial.
- Controlled-Rate Freezing: Place samples in a controlled-rate freezing apparatus. Cool at a rate of -1°C per minute to -80°C. Hold for at least 12 hours before transferring to long-term storage in liquid nitrogen (-196°C).
- Thawing and CPA Elution: Rapidly thaw samples in a 37°C water bath. Gently elute the CPA by adding PBS in gradual steps, with mixing and centrifugation (500 rpm for 3 min) to remove the liquid, repeated twice.
- Assessment:
- Biochemical Activity: Measure G3PDH activity using a commercial kit on 10 mg of homogenized tissue.
- Cell Viability: Isolate the Stromal Vascular Fraction (SVF) via collagenase digestion. Determine viability using trypan blue exclusion or flow cytometry with Calcein-AM/PI staining.
- In Vivo Function: Transplant 0.2 mL of eluted tissue subdermally into nude mice. Harvest after 4 weeks to calculate graft retention rate and perform histological analysis (H&E staining) for integrity and inflammation.
Protocol 2: Modified Warming of Vitrified Oocytes
This protocol is critical for the thesis context and is based on a 2025 study that demonstrated improved embryonic development and pregnancy outcomes using a modified warming protocol (MWP) for donor oocytes [5].
Experimental Workflow:
Key Materials:
- Vitrified donor oocytes
- Commercial vitrification/warming kits (Compatible with universal warming)
- Thawing Solution (TS), Dilution Solution (DS), Wash Solution (WS) – for CWP
- 1 M sucrose or trehalose solution – for MWP single-step rehydration
- Intracytoplasmic Sperm Injection (ICSI) equipment
- Culture media for embryo development
Detailed Methodology:
- Warming: Rapidly warm vitrified oocytes by plunging cryostraws/carriers into a Thawing Solution (TS) at 37°C for 1 minute.
- CPA Removal (Conventional Warming Protocol - CWP):
- Transfer oocytes through a gradient dilution at room temperature: Dilution Solution (DS, 3 min) followed by one or two steps in Wash Solution (WS, 5-6 min) [5].
- CPA Removal (Modified Warming Protocol - MWP):
- Assessment of Outcomes:
- Survival Rate: Calculate the percentage of oocytes with normal morphology post-warming.
- Fertilization and Development: Perform ICSI. Record normal fertilization (2-pronuclei), degeneration, and abnormal fertilization rates.
- Blastocyst Formation: Culture embryos and record the rates of blastocyst formation and usable blastocysts on days 5-6.
- Pregnancy Outcomes: Transfer viable blastocysts and monitor ongoing pregnancy/live birth rates.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagent Solutions for CPA Optimization Research
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Permeating CPA; industry standard but has known toxicity. | Positive control in experiments testing new CPAs [47] [50]. |
| Glycerol | Permeating CPA; lower toxicity, suitable for tissues. | Cryopreservation of adipose tissue and composite tissues [48]. |
| Betaine | Natural zwitterionic osmoprotectant and permeating CPA. | Used in ultrarapid freezing protocols and to enhance LNP mRNA delivery [45] [49]. |
| Trehalose / Sucrose | Non-permeating CPAs; stabilize cell membranes, control osmotic stress. | Standard component in vitrification solutions and warming media for oocytes/embryos [5] [47] [8]. |
| Serum-Free Freezing Media | Chemically defined, protein-free cryopreservation medium. | Essential for clinical-grade stem cell and therapeutic cell preservation [47] [50]. |
| ROCK Inhibitor (Y-27632) | Small molecule that inhibits apoptosis. | Added to culture medium post-thaw to improve attachment and survival of single stem cells (e.g., hiPSCs) [47]. |
| Controlled-Rate Freezer | Equipment that ensures a consistent, optimal cooling rate (e.g., -1°C/min). | Standardized slow freezing of cells and tissues to maximize viability [46] [50]. |
Discussion and Concluding Remarks
Optimizing CPA concentration and composition is a dynamic and cell-type-specific endeavor. The move towards low-toxicity alternatives like glycerol for tissues and betaine for specific applications, coupled with the development of serum-free, chemically defined media, is a clear trend driven by both efficacy and clinical safety requirements [51] [47] [48].
Critically, the interaction between CPA composition and the warming protocol is paramount. The success of the Modified Warming Protocol (MWP) for oocytes, which simplifies the rehydration process into a single step, demonstrates that protocol efficiency can be enhanced without compromising—and even improving—developmental outcomes [5]. This underscores the thesis that warming protocol modifications are a viable pathway to standardizing and improving the entire cryopreservation workflow for vitrified oocytes and embryos.
Future work should continue to explore the synergistic effects of novel CPAs and optimized thermal protocols to further push the boundaries of viability and functionality in cryopreserved biospecimens.
Mitigating Fracture and Cracking Risks During the Warming Process
Within the broader research on Modified Warming Protocols (MWP) for vitrified oocytes and embryos, mitigating fracture and cracking risks represents a pivotal challenge determining the success of assisted reproductive technologies (ART). Fracture formation during warming is a significant physical stress that can prevent tissue recovery from cryogenic storage, posing a major obstacle in scaling vitrification to clinically relevant sample sizes [52]. The warming process, often incorrectly termed "thawing," involves the rapid increase in temperature of cells stored in liquid nitrogen to room temperature or above under defined laboratory conditions [6]. While the avoidance of ice formation during vitrification is important, the warming rate has been demonstrated to have a greater impact on embryo survival than the cooling rate, underscoring the critical importance of optimized warming protocols [9]. This application note details the mechanisms of thermal stress-induced fractures and provides evidence-based protocols to mitigate these risks, with particular emphasis on recent advancements in MWP that enhance clinical outcomes.
The fundamental principle underlying fracture prevention lies in understanding the glass transition temperature range, typically between -150°C to -120°C, where the vitrified material is most vulnerable to structural failure [52]. As the system traverses this critical temperature range during warming, thermal gradients develop within the vitrified sample, generating mechanical stresses that can exceed the strength of the brittle, glass-like material. The long-term goal in this line of research is to develop computational methodologies that predict cracking in cryopreserved tissues, which can then be incorporated into tools for designing cryopreservation protocols that minimize or eliminate cracking [52]. This document synthesizes current experimental and clinical findings to provide laboratory professionals with standardized approaches for maximizing survival rates of vitrified reproductive materials.
Mechanisms of Thermal Stress and Fracture Formation
Fundamental Principles of Thermomechanical Stress
Thermomechanical stress during warming originates from differential thermal expansion across the vitrified sample. When temperature gradients exist within the vitrified material during warming, different regions expand at varying rates, generating internal stresses [53]. The vitrified system, comprising cryoprotective agents (CPAs) and biological material, behaves as a brittle solid at cryogenic temperatures, with significantly reduced ability to dissipate stress through plastic deformation [52]. Research indicates that throughout rewarming, regions that rewarm faster undergo compressive stresses, while slower rewarming regions experience tension [53]. As a brittle material, the vitrified organ is expected to fail under tension at lower stress thresholds than in compression, making the management of thermal gradients paramount to successful warming outcomes [53].
The container geometry and composition further influence stress development through confinement effects. While compliant cryobag materials minimize additional stress, stiffer container walls can intensify stress levels [53]. The complex state of stress in the cryoprotectant is explained by three continuum mechanics effects: the constraining effect of the container bottom, viscous relaxation in the cryoprotectant, and the confining effect of the container wall [52]. Understanding these interacting effects is essential for interpreting fracture observations and designing effective mitigation strategies.
Critical Temperature Zones and Failure Modes
The most dangerous period for structural integrity occurs below the glass transition temperature and at the onset of warming past the glass transition point during recovery from cryogenic storage [53]. Empirical investigations have determined that fractures predominantly occur as the temperature range of -150°C to -120°C is traversed during the warming phase of the process [52]. The following table summarizes the primary fracture modes observed during warming of vitrified systems:
Table 1: Fracture Modes and Characteristics During Warming
| Fracture Type | Typical Size Scale | Primary Initiating Factor | Temperature Range of Occurrence |
|---|---|---|---|
| Macrofractures | Specimen size | Thermal stress gradients | -150°C to -120°C |
| Microfractures | Blood vessel diameter | Crystal formation pressure | Below glass transition |
| Intracellular damage | Cellular level | Recrystallization | Above -100°C during warming |
The risk of fracture formation is further influenced by the cooling history prior to warming. Samples cooled using a two-step protocol with rapid cooling to about 30°C above the glass transition temperature, followed by low cooling rate to the storage temperature, demonstrate reduced fracture incidence [52]. Similarly, the implementation of a two-step warming protocol—slow warming up to about 30°C above the glass transition temperature followed by rapid warming—takes advantage of the material's ability to relax stresses more readily at temperatures farther from the glass transition where viscosity is lower [52].
Experimental Data: Comparative Performance of Warming Protocols
Clinical Outcomes with Modified Warming Protocols
Recent clinical studies directly compare conventional warming protocols (CWP) with modified approaches (MWP), demonstrating significant improvements in key performance indicators. A retrospective cohort study of 13,103 donor oocytes revealed that while survival rates after oocyte warming were similar between CWP and MWP groups (93.7% vs. 93.9%), dramatic differences emerged in subsequent development metrics [5]. Blastocyst formation and usable blastocyst formation were substantially lower in the CWP group (57.5% and 35.4%) compared to MWP (77.3% and 51.4%) and fresh groups (69.2% and 48.5%) [5]. Most notably, ongoing pregnancy/live birth was significantly higher in the MWP group than in the CWP group (66.7% vs. 50.4%) [5].
Multivariate analysis confirmed a strong positive association between MWP and usable blastocyst formation (adjusted incidence rate ratio = 1.423, 95% CI = 1.268 to 1.597) as well as ongoing pregnancy/live birth (adjusted odds ratio = 1.899, 95% CI = 1.002 to 3.6) [5]. These findings suggest that the MWP enhances the blastocyst formation potential and pregnancy outcomes of vitrified-warmed oocytes, making their performance similar to that of fresh oocytes [5].
Quantitative Analysis of Protocol Efficacy
The following table summarizes key comparative outcomes between conventional and modified warming protocols based on recent clinical data:
Table 2: Comparative Performance Metrics of Warming Protocols for Vitrified Oocytes
| Performance Metric | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Control Group |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | N/A |
| Oocyte Degeneration Post-ICSI | 3.4% | 2.7% | 2.8% |
| Normal Fertilization | 79.5% | 79.6% | 83.0% |
| Blastocyst Formation | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | Not Reported |
The transition to simplified, rapid warming methodologies is supported by research demonstrating that human oocytes and zygotes can successfully tolerate ultra-fast vitrification protocols with just 2 minutes of exposure to standard CPA solutions [54]. In silico modeling using a two-parameter permeability model of human oocytes indicates that dehydration upon exposure to standard cryoprotectant solutions occurs very rapidly, with the point of minimum volume of the shrink-swell curve reached within 60 seconds [54]. This finding challenges traditional extended equilibration times and supports the move toward abbreviated protocols that reduce total exposure to potentially toxic cryoprotectants.
Research Reagents and Essential Materials
The following toolkit comprises critical reagents and materials for implementing fracture-resistant warming protocols:
Table 3: Essential Research Reagents for Warming Protocol Implementation
| Reagent/Material | Function | Implementation Notes |
|---|---|---|
| Thawing Solution (TS) | Initial high-osmolarity solution for rapid warming; contains sucrose or trehalose (~1.0 M) | Creates osmotic gradient to prevent rapid water influx and membrane rupture [9] |
| Dilution Solution (DS) | Intermediate osmolarity solution (~0.5 M sucrose/trehalose) for gradual cryoprotectant removal | Facilitates continued diffusion at reduced osmolarity; used at room temperature [9] |
| Washing Solution (WS) | Base solution resembling culture media with buffering agents (e.g., HEPES) | Removes residual cryoprotectants; acclimates cells to culture conditions [9] |
| Silica-coated Iron-oxide Nanoparticles (sIONPs) | Enables nanowarming through electromagnetic excitation in alternating magnetic fields | Provides volumetric heating to reduce thermal gradients; requires specific washout protocols [53] |
| Ethylene Glycol (EG) | ||
| Dimethyl Sulfoxide (DMSO) | Permeating cryoprotectants that enable vitrification | Potential toxicity requires careful exposure time management [6] [54] |
| Open Vitrification Carriers | Microvolume devices (Cryotop, OPS) enabling ultra-rapid cooling/warming rates | Critical for achieving cooling rates > -10,000°C/min; some contamination risk in open systems [6] |
Detailed Methodological Protocols
Modified Warming Protocol for Oocytes and Embryos
The following workflow illustrates the standardized MWP for vitrified oocytes and embryos, incorporating fracture-mitigation strategies:
Protocol Specifics:
Ultra-Rapid Initial Warming: Immediately upon retrieval from liquid nitrogen, immerse the vitrification device in pre-warmed Thawing Solution (TS) at 37°C for exactly 1 minute [5] [9]. The TS contains 1.0 M sucrose or trehalose to establish a high osmolarity environment (approximately 2901 mOsmol) that moderates initial water influx during rehydration [54] [9]. Warming rates should exceed 2170°C/min to minimize time spent at water's freezing point where ice crystal formation is most likely [9].
Dilution Phase: Transfer samples to Dilution Solution (DS) at room temperature for 3 minutes [5]. Utilize controlled carry-over of TS (approximately 10-20% volume) to maintain a gradual osmotic gradient during this transition [9]. The DS contains 0.5 M sucrose/trehalose, reducing osmolarity to facilitate continued efflux of intracellular cryoprotectants while minimizing osmotic shock [9].
Washing and Cryoprotectant Removal: Perform two sequential washes in Washing Solution (WS) at room temperature for 5 minutes total [5]. WS resembles standard culture media with added buffering agents (HEPES) to maintain pH stability during handling [9]. This critical step removes residual permeating cryoprotectants (EG, DMSO) that could exert toxic effects during subsequent culture [9].
Assessment and Culture Transition: Evaluate structural integrity under microscopy, specifically checking for membrane integrity, zona pellucida cracks, and cytoplasmic abnormalities. Gradually transition viable specimens to pre-equilibrated culture media through sequential equilibration steps to finalize rehydration under physiological conditions.
Advanced Nanowarming Protocol for Complex Systems
For larger systems such as ovarian tissue or organ specimens, where thermal gradients are more pronounced, nanowarming presents an innovative approach to mitigate fracture risks:
Protocol Specifics:
Nanoparticle Loading and Activation: Prior to vitrification, perfuse tissue with silica-coated iron-oxide nanoparticles (sIONPs) suspended in CPA cocktail [53]. During warming, place the vitrified system within an alternating magnetic field (100-400 kHz) to activate nanowarming, generating uniform volumetric heating that circumvents traditional thermal gradients [53].
Thermal Monitoring and Control: Utilize infrared thermal imaging to monitor temperature distribution throughout the sample, ensuring no region exceeds safe warming rates. The most critical temperature range for fracture prevention is below the glass transition and at the onset of nanowarming past the glass transition temperature [53].
Nanoparticle Removal: Following warming, implement a standardized washout protocol to remove sIONPs, achieving demonstrated efficiency of 93% in rat heart models [53]. The remaining nanoparticles should remain within known tolerable concentration limits for the specific tissue type [53].
Troubleshooting and Quality Control
Common Complications and Resolution
Observed Fracturing: If macro-fractures are consistently observed, implement a two-step warming protocol with reduced warming rate (less than 50°C/min) through the critical glass transition temperature range (-150°C to -120°C) before proceeding to rapid warming [52].
Low Survival Despite Structural Integrity: Evaluate cryoprotectant toxicity by reducing exposure times to vitrification solutions. Research indicates that shortening CPA exposure to 2 minutes total (1 minute in non-vitrifying solution + 1 minute in vitrification solution) can maintain survival while reducing toxic insult [54].
Variable Outcomes Between Operators: Implement strict quality control measures including standardized timing protocols, solution lot tracking, and regular proficiency assessment. Studies indicate that outcomes following rapid-cooling vitrification are closely related to operator skill, necessitating comprehensive training programs [6].
Protocol Validation Metrics
Establish routine monitoring of key performance indicators: survival rate (benchmark: >90% for oocytes), structural integrity (absence of visible fractures), and developmental competence (blastocyst formation rates comparable to fresh controls) [5] [6]. For clinical applications, ongoing pregnancy and live birth rates should be tracked, with expectations of approximately 67% with optimized MWP implementation [5].
The successful mitigation of fracture and cracking risks during warming of vitrified oocytes and embryos requires integrated approach combining optimized thermal protocols, advanced materials, and meticulous technique. Evidence demonstrates that Modified Warming Protocols significantly enhance key outcomes including blastocyst formation and ongoing pregnancy rates compared to conventional approaches [5]. The fundamental principles of fracture prevention center on managing thermomechanical stress through the critical glass transition temperature zone, either via ultra-rapid warming in standard ART applications or volumetric nanowarming for more complex systems [53] [52]. As research continues to refine these approaches, the standardization of warming protocols across laboratories promises to improve reproducibility and clinical success in assisted reproduction.
The optimization of warming protocols for vitrified oocytes and embryos represents a critical frontier in assisted reproductive technology (ART), particularly for challenging cases such as those involving diminished ovarian reserve (DOR). Recent research demonstrates that modified warming protocols (MWP) can significantly enhance embryonic development potential and pregnancy outcomes, achieving blastocyst formation rates comparable to fresh oocytes [11] [5]. These technical advances are especially relevant for DOR patients, who characteristically present with reduced oocyte quantity and quality, making each recovered oocyte exceptionally valuable [55]. The imperative to maximize the potential of every embryo necessitates protocol adaptations that minimize cryopreservation-induced stress and optimize survival rates across diverse biological scenarios, from human clinical applications to animal research models.
This application note synthesizes recent evidence on MWP efficacy and provides detailed methodologies for implementing these protocols in both clinical and research settings. By integrating quantitative outcome data with step-by-step procedural guidance, we aim to support researchers and clinicians in adapting these advanced techniques to address the unique challenges presented by DOR patients and animal model embryos.
Quantitative Outcomes of Modified Warming Protocols
Comparative Performance of Warming Protocols
Recent large-scale clinical studies provide compelling quantitative evidence supporting the transition from conventional warming protocols (CWP) to MWP for vitrified oocytes. The table below summarizes key outcomes from a retrospective analysis of 13,103 donor oocytes, comparing conventional and modified warming approaches against fresh oocyte controls [11] [5] [56].
Table 1: Comparative Outcomes of Conventional vs. Modified Warming Protocols for Vitrified Oocytes
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | Not applicable |
| Oocyte Degeneration Post-ICSI | 3.4% | 2.7% | 2.8% |
| Normal Fertilization Rate | 79.5% | 79.6% | 83.0% |
| Abnormal Fertilization Rate | 10.1% | 9.1% | 3.3% |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | Not reported |
The data demonstrates that while MWP and CWP show similar oocyte survival and initial fertilization rates, the MWP group exhibits significantly enhanced blastocyst development, with formation rates exceeding even those of fresh oocytes [11]. This suggests that the modified protocol better preserves the oocyte's developmental competence. Multivariate analysis confirms a positive association between MWP and usable blastocyst formation (adjusted incidence rate ratio = 1.423, 95% CI = 1.268 to 1.597, P < 0.001) as well as ongoing pregnancy/live birth (adjusted odds ratio = 1.899, 95% CI = 1.002 to 3.6, P < 0.05) [5] [56].
Protocol Efficacy in Diminished Ovarian Reserve Contexts
For DOR patients, the quality of obtained oocytes presents additional challenges. Research on experimental interventions like intraovarian platelet-rich plasma (PRP) injection in mouse models of chemotherapy-induced DOR provides insights into complementary approaches that may enhance oocyte competence prior to cryopreservation.
Table 2: Efficacy of Intraovarian PRP in Mouse Models of Chemotherapy-Induced Diminished Ovarian Reserve
| Outcome Measure | POR-Sham | POR-PRP | POI-Sham | POI-PRP |
|---|---|---|---|---|
| Fertilization Rate | Baseline | Increased | Baseline | Significantly Increased |
| 2-Cell Embryos Obtained | Baseline | Increased | Baseline | Significantly Increased |
| Blastocyst Formation Rate | Baseline | Improved | Baseline | Improved |
| Good Quality Blastocysts | Baseline | Higher Numbers | Baseline | Higher Numbers |
PRP administration in both poor ovarian reserve (POR) and primary ovarian insufficiency (POI) mouse models reduced chemotherapy-induced alterations in ovarian stroma and follicle morphology, with subsequent improvements in embryo development metrics [57]. This suggests that ovarian microenvironment interventions may complement technical protocol refinements to optimize outcomes for DOR cases.
Detailed Experimental Protocols
Modified Warming Protocol for Vitrified Oocytes
The modified warming protocol represents a significant simplification of conventional approaches, reducing procedural time and potentially minimizing osmotic stress on vitrified oocytes [11].
Figure 1: Modified Warming Protocol Workflow for Vitrified Oocytes
Materials Required:
- Thawing Solution (TS)
- Culture medium
- Heating stage or block maintaining 37°C
- Sterile pipettes and tips
- Pre-equilibrated culture dishes
Step-by-Step Procedure:
Preparation: Pre-warm all solutions to 37°C. Prepare culture dishes with appropriate medium and equilibrate in incubator.
Rapid Warming: Transfer vitrified oocytes directly to Thawing Solution (TS) at 37°C for exactly 1 minute.
Single-Step Dilution: Instead of sequential transfer through Dilution Solution (DS) and Wash Solution (WS) as in conventional protocols, proceed directly to a single-step rehydration and cryoprotectant removal process.
Culture Transfer: After the warming and dilution process, transfer oocytes to pre-equilibrated culture medium.
Recovery Incubation: Culture oocytes for approximately 2 hours before performing intracytoplasmic sperm injection (ICSI).
Critical Steps and Considerations:
- Maintain consistent temperature at 37°C throughout the warming process
- Time the TS incubation precisely to 1 minute
- Use ICSI for fertilization rather than conventional insemination due to the zona pellucida hardening that can occur during vitrification [11]
- Assess oocyte survival after the 2-hour recovery period based on membrane integrity and morphological appearance
Animal Model Protocol: PRP Intervention for DOR
For research applications using animal models of diminished ovarian reserve, intraovarian PRP injection represents a promising intervention to improve oocyte quality prior to retrieval and cryopreservation.
Figure 2: Experimental Workflow for PRP Intervention in DOR Animal Models
Materials Required:
- Laboratory animals (CD1 or C57BL/6 mice)
- Chemotherapy agents (cyclophosphamide, busulphan)
- Blood collection equipment
- Centrifuge for PRP preparation
- Micro-injection system (insulin syringe 31G)
- Anesthesia equipment
- Ovarian stimulation hormones (PMSG, hCG)
Step-by-Step Procedure:
DOR Model Induction:
- Administer chemotherapy agents intraperitoneally to 8-week-old female mice
- For POR model: cyclophosphamide (12 mg/kg) + busulphan (1.2 mg/kg)
- For POI model: cyclophosphamide (120 mg/kg) + busulphan (12 mg/kg)
- Allow one week for ovarian damage establishment [57]
PRP Preparation:
- Collect blood via aortic puncture (~1 mL/female)
- Centrifuge at 1500 rpm for 8 minutes to separate plasma
- Recentrifuge plasma for 15 min at 2000 rpm
- Collect upper 1/3 fraction as PRP (150-175 µl per female)
- Activate PRP using freeze-thaw technique [57]
Intraovarian Injection:
- Anesthetize mice using isoflurane
- Administer preemptive analgesia
- Surgically expose ovaries through dorsal incision
- Inject 10 µL of PRP or PBS (sham) into center of each ovary using 31G insulin syringe
- Perform layered closure of abdominal wall
- Monitor recovery for 1 hour post-procedure [57]
Assessment Timeline:
- Allow 14-day recovery after PRP/sham injection
- Perform ovarian stimulation with PMSG (10 IU) followed by hCG (10 IU) 48 hours later
- Mate with wild-type males
- Collect oocytes/embryos 36 hours post-hCG
- Culture embryos to blastocyst stage for development assessment
- Fix ovaries for histological analysis of follicular development and stromal quality
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Modified Warming Protocols and DOR Interventions
| Reagent/Category | Specific Examples | Function and Application Notes |
|---|---|---|
| Vitrification/Warming Kits | Cryotec thawing kit; Commercial warming media | Specifically formulated solutions for vitrification/warming procedures. MWP uses only Thawing Solution (TS), eliminating need for Dilution Solution (DS) and Wash Solution (WS) [11]. |
| Platelet-Rich Plasma (PRP) | Autologous PRP | Contains >800 proteins, molecules, cytokines, and growth factors. Released upon activation stimulate cell proliferation, growth, and differentiation [57]. |
| Ovarian Stimulation Agents | PMSG, hCG, FSH preparations | Used for controlled ovarian hyperstimulation in animal models and clinical practice. MWP study reported total FSH dosage of 2206±315 IU in successful cycles [11]. |
| Culture Media | Global collect medium (GCOL-100), Sage 1-step medium | Specifically formulated for embryo culture. Maintain at 37°C with 5% O2, 6% CO2, and 89% N2 for optimal blastocyst development [57]. |
| Cryoprotectant Agents | Ethylene glycol, dimethyl sulfoxide, sucrose | Permeating and non-permeating agents used in vitrification solutions to prevent ice crystal formation and mitigate osmotic shock [11]. |
Discussion and Technical Considerations
Mechanisms of Protocol Efficacy
The superior performance of the modified warming protocol likely stems from its reduction of osmotic stress and cryoprotectant exposure during the critical warming phase. While conventional protocols employ a gradient dilution approach involving incubation in Dilution Solution (DS, 3 min) and Wash Solution (WS, 5-6 min) at room temperature, the MWP eliminates these steps entirely, creating an ultrafast, single-step process [11]. This simplified approach may better preserve the structural integrity of sensitive organelles such as the meiotic spindle and cortical granules, ultimately enhancing developmental competence.
For DOR interventions, the mechanism of PRP action appears to involve paracrine signaling through released growth factors that improve the ovarian microenvironment. This effect is particularly valuable for DOR cases, where the local follicular environment may be compromised [55]. PRP treatment has been shown to reduce chemotherapy-induced alterations in ovarian stroma and follicle morphology, creating conditions more favorable for oocyte development [57].
Applications to Animal Model Research
The adaptation of these protocols for animal research models requires consideration of species-specific differences in ovarian physiology and embryo development. The successful application of PRP in both CD1 and C57BL/6 mouse strains suggests broad applicability across common research models [57]. Similarly, movement toward universal warming protocols that can be applied across tissue types (including ovarian tissue) and preservation methods (vitrification vs. slow freezing) represents an important direction for standardizing research methodologies [58].
When implementing these protocols in animal studies, researchers should:
- Validate strain-specific response to interventions
- Adjust hormone dosages for superovulation based on strain characteristics
- Include appropriate sham controls (e.g., PBS injection) for PRP studies
- Standardize the timing of interventions relative to ovarian stimulation
- Employ consistent morphological criteria for assessing oocyte and embryo quality
Integration with Broader Research Objectives
These technical protocols should be viewed as components within a comprehensive research strategy for studying oocyte biology and developing interventions for ovarian insufficiency. The integration of optimized warming techniques with emerging technologies such as mitochondrial transfer, stem cell applications, and follicle activation approaches may yield synergistic benefits for addressing the complex challenge of diminished ovarian reserve [55].
Future methodological developments will likely focus on further streamlining protocols, enhancing standardization across laboratories, and identifying molecular markers that can predict oocyte developmental potential following cryopreservation. Such advances will be particularly valuable for maximizing outcomes in challenging cases where oocyte quantity is severely limited.
In assisted reproductive technology (ART), the vitrification of oocytes and embryos has revolutionized fertility preservation and treatment. While much attention is given to cooling rates and cryoprotectant formulations, the warming process is equally critical for cellular survival and developmental potential. Recent research demonstrates that warming rate has a greater impact on embryo survival than cooling rate [9], highlighting the crucial importance of standardized, validated warming protocols. Effective quality control measures ensure that vitrified-warmed oocytes and embryos maintain their structural integrity and developmental competence, ultimately translating to improved clinical outcomes.
Experimental Protocols for Warming Rate Validation
Modified Warming Protocol (MWP) for Oocytes
A recent large-scale clinical study implemented a modified warming protocol for vitrified donor oocytes and compared outcomes with both conventional warming and fresh oocytes [11].
Methodology:
- Sample Preparation: 13,103 donor oocytes were divided into three groups: conventional warming protocol (CWP, n=8,506), modified warming protocol (MWP, n=980), and fresh group (n=3,617)
- MWP Procedure: Elimination of dilution solution (DS) and wash solution (WS) steps, simplifying the process to an ultrafast, single-step incubation in thawing solution (TS) for 1 minute
- Assessment Parameters: Survival rates post-warming, degeneration rates post-ICSI, fertilization rates, blastocyst formation, and ongoing pregnancy/live birth rates
- Statistical Analysis: Multivariate analysis to determine adjusted incidence rate ratios and odds ratios for key outcomes
Key Findings: The MWP group demonstrated significantly higher rates of usable blastocyst formation (51.4%) compared to the CWP group (35.4%), making it comparable to fresh oocytes (48.5%) [11]. Ongoing pregnancy/live birth rates were significantly higher in the MWP group (66.7%) versus the CWP group (50.4%) [11].
Preclinical Validation of Fast Warming Protocols
A 2025 preclinical study validated fast warming protocols using animal models and discarded human oocytes [59].
Methodology:
- Models Used: Mouse and rabbit oocytes, with additional validation using discarded human oocytes
- Experimental Groups: Oocytes allocated to fast vitrification/fast warming (FV/FW), standard vitrification/standard warming (SV/SW), and standard vitrification/fast warming (SV/FW)
- Assessment Parameters: Survival rates, meiotic spindle integrity, chromosomal alignment, developmental rates, and live birth rates (in mice)
- Theoretical Modeling: In silico osmotic modeling predicted human oocyte responses to FV conditions
Key Findings: The FV/FW protocol significantly reduced processing time while maintaining oocyte survival (97.2% in mice), meiotic spindle integrity, and developmental potential comparable to standard protocols [59]. Live birth rates in mice were 38.7% for FV/FW versus 47.8% for SV/SW, demonstrating no statistically significant adverse effects on full-term development [59].
Quantitative Outcomes Comparison
The table below summarizes key quantitative findings from recent studies comparing warming protocols:
Table 1: Comparative Outcomes of Warming Protocols for Vitrified Oocytes
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% [11] | 93.9% [11] | N/A |
| Oocyte Degeneration Post-ICSI | 3.4% [11] | 2.7% [11] | 2.8% [11] |
| Normal Fertilization | 79.5% [11] | 79.6% [11] | 83.0% [11] |
| Blastocyst Formation | 57.5% [11] | 77.3% [11] | 69.2% [11] |
| Usable Blastocyst Formation | 35.4% [11] | 51.4% [11] | 48.5% [11] |
| Ongoing Pregnancy/Live Birth | 50.4% [11] | 66.7% [11] | N/A |
Table 2: Preclinical Validation Outcomes of Fast Warming Protocols [59]
| Parameter | Fast Vitrification/Fast Warming (FV/FW) | Standard Vitrification/Standard Warming (SV/SW) | Standard Vitrification/Fast Warming (SV/FW) |
|---|---|---|---|
| Mouse Oocyte Survival | 97.2% | 94.2% | 91.7% |
| Mouse Blastocyst Formation | 80.9% | 83.4% | 75.9% |
| Mouse Live Birth Rate | 38.7% | 47.8% | 43.2% |
| Rabbit Blastocyst Development | 28.6% | 22.2% | 13.6% |
| Human Oocyte Survival | 97.1% | N/A | 94.1% |
Quality Control Framework
Critical Parameters for Warming Rate Validation
Temperature Transition Monitoring: Rapid warming exceeding 2,170°C/min is recommended to minimize time at water's freezing point and prevent ice crystal formation [9]. Continuous monitoring and validation of warming rates are essential using calibrated thermocouples.
Osmotic Stress Management: While MWP simplifies the process, controlled rehydration remains critical. Extracellular cryoprotectants (sucrose or trehalose) in thawing solution create high osmolarity (1.0M) to moderate the osmotic gradient during initial rehydration [9].
Temporal Parameters: Ultrafast protocols complete warming in approximately one minute while maintaining embryo integrity [9]. Standardized timing for each step must be rigorously maintained.
Solution Quality Control: Regular testing of warming solutions for pH, osmolarity, and contamination ensures batch-to-batch consistency. Protein sources and antibiotic additives must be verified for stability and functionality [60].
Protocol Standardization and Consistency Measures
- Documentation: Comprehensive standard operating procedures (SOPs) detailing every step of the warming process
- Personnel Training: Structured training programs with competency assessments and regular proficiency testing
- Equipment Calibration: Regular validation of heating blocks, timers, and environmental chambers
- Process Validation: Ongoing monitoring of survival rates, fertilization rates, and development metrics as quality indicators
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Warming Protocols
| Reagent Solution | Composition | Function | Protocol Considerations |
|---|---|---|---|
| Thawing Solution (TS) | Extracellular cryoprotectants (sucrose or trehalose) at 1.0M concentration [9] | Rapid warming at 37°C; initial rehydration with high osmolarity moderates osmotic gradient | Warming rate exceeding 2,170°C/min is critical to avoid ice crystal formation [9] |
| Dilution Solution (DS) | Extracellular cryoprotectants at 0.5M concentration [9] | Continued rehydration at reduced osmolarity | Often eliminated in modified protocols; performed at room temperature in conventional protocols |
| Washing Solution (WS) | Buffering agents (HEPES), mimicking culture media [9] | Removes lingering cryoprotectants; acclimatizes embryos to culture conditions | Multiple washes ensure removal of compounds like DMSO or ethylene glycol |
| Culture Media | Balanced salt solutions, energy substrates, proteins, antibiotics [60] | Supports embryo development post-warming | Serum-free formulations reduce variability; composition affects perinatal outcomes [60] |
Workflow Visualization
Warming Protocol Workflow: This diagram illustrates the critical pathways in conventional versus modified warming protocols, highlighting key quality control checkpoints.
Validating warming rates and ensuring protocol consistency are fundamental to successful oocyte and embryo cryopreservation programs. The emerging evidence demonstrates that modified warming protocols can significantly improve blastocyst formation and pregnancy outcomes while streamlining laboratory workflows [11]. As research continues to refine these protocols, rigorous quality control measures remain essential to maximize clinical efficacy and ensure reproducible results across ART laboratories.
Validating Success: Comparative Analysis of Embryological and Clinical Outcomes
This application note provides a standardized framework for benchmarking the survival and developmental competence of vitrified oocytes and embryos. With the increasing adoption of modified warming protocols (MWPs) to enhance laboratory efficiency, consistent and comparative metrics are essential for validating new methodologies. We summarize critical quantitative data from key studies into structured tables, detail standardized experimental protocols for consistent application, and visualize the benchmarking workflow. This resource is designed to assist researchers and clinicians in evaluating the efficacy of novel warming protocols against established conventional methods, ensuring robust and reproducible outcomes in clinical practice.
Oocyte and embryo cryopreservation via vitrification is a cornerstone of modern assisted reproductive technology (ART), vital for fertility preservation and egg donation programs [5] [6]. The warming process is as critical as vitrification itself; suboptimal warming can lead to cryoinjury, compromising survival and developmental potential [61] [6].
Recent innovations, such as Modified Warming Protocols (MWPs), aim to streamline laboratory workflows by simplifying solution steps and adjusting temperatures [5] [11]. However, benchmarking these novel protocols against conventional warming protocols (CWPs) requires a consensus on the key performance indicators (KPIs) to be measured across developmental stages. This document establishes a standardized set of comparative metrics and detailed methodologies for the rigorous evaluation of oocyte and embryo survival post-warming, providing a critical tool for translational research and clinical validation.
Comparative Metrics and Key Performance Indicators (KPIs)
The following tables consolidate quantitative outcomes from recent seminal studies, offering a benchmark for expected results when using conventional and modified warming protocols on vitrified oocytes and the resulting embryos.
Table 1: Benchmarking Oocyte Survival and Fertilization Outcomes Following Vitrification and Warming
| Key Performance Indicator | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) | Citation |
|---|---|---|---|---|
| Oocyte Survival Rate | 93.7% (7967/8506) | 93.9% (920/980) | Not Applicable | [11] |
| Oocyte Survival Rate (Transnational Study) | 84.6% (795/939) | 82.1% (787/959) | Not Applicable | [61] |
| Normal Fertilization Rate (2PN) | 79.6% | 79.5% | 83.0% | [11] |
| Oocyte Degeneration Rate (post-ICSI) | 3.4% (268/7967) | 2.7% (25/920) | 2.8% (60/2106) | [11] |
| Abnormal Fertilization Rate (e.g., 1PN, 3PN) | 10.1% | 9.1% | 3.3% | [11] |
Table 2: Benchmarking Embryonic Development and Clinical Outcomes from Vitrified-Warmed Oocytes
| Key Performance Indicator | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) | Citation |
|---|---|---|---|---|
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% | [11] |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% | [11] |
| Implantation Rate | 41.5% (80/193) | 45.9% (84/183) | Not Reported | [61] |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | Not Reported | [11] |
| Live Birth Rate (per embryo transfer) | 52.5% (62/118) | 45.0% (54/120) | Not Reported | [61] |
Experimental Protocols for Benchmarking Studies
Protocol: Oocyte Vitrification using the Kitazato Cryotop Method
This protocol is adapted from the method used in the transnational "Universal Warming" study [61].
Principle: Oocytes are exposed to increasing concentrations of cryoprotectants (CPAs) to promote dehydration, then cooled at ultra-rapid rates to achieve a glass-like state without ice crystal formation.
Reagents:
- Equilibration Solution (ES): 7.5% (v/v) Dimethyl Sulfoxide (DMSO), 7.5% (v/v) Ethylene Glycol (EG) in base medium (e.g., TCM-199).
- Vitrification Solution (VS): 15% (v/v) DMSO, 15% (v/v) EG, supplemented with a non-permeable CPA like trehalose or sucrose, in base medium.
- Base Medium: TCM-199, supplemented with HPC (Hydroxypropyl cellulose) or DSS (Dextran serum supplement).
Procedure:
- Equilibration: Expose oocytes to ES for 10-15 minutes at room temperature (20-25°C). Observe for osmotic response (shrinkage followed by partial re-expansion).
- Vitrification: Transfer oocytes to VS for 60 seconds at room temperature. Timing is critical to avoid CPA toxicity.
- Loading and Cooling: Within the 60-second window, place a minimal volume (≤ 1 µL) containing 1-3 oocytes onto the Cryotop device. Immediately plunge the device directly into liquid nitrogen for storage.
- Storage: Ensure oocytes are stored under continuous liquid nitrogen conditions at -196°C.
Protocol: Conventional Warming Protocol (CWP)
This protocol represents the multi-step, gradient dilution approach used as a control in recent studies [5] [11].
Principle: A graded series of decreasing sucrose concentrations is used to gradually rehydrate the oocyte, minimizing osmotic shock.
Reagents:
- Thawing Solution (TS): 1.0 M Sucrose in base medium.
- Dilution Solution (DS): 0.5 M Sucrose in base medium.
- Washing Solution (WS): Base medium without sucrose.
Procedure:
- Warming: Pre-warm TS to 37°C. Rapidly warm the Cryotop by directly immersing it in 1 mL of TS for 1 minute.
- Dilution: Transfer oocytes to DS at room temperature for 3 minutes.
- Washing: Perform two sequential washes in WS for 5 and 1 minute, respectively, at room temperature.
- Post-Warm Culture: Transfer oocytes to culture medium and incubate for 1-2 hours at 37°C, 6% CO2, before assessing survival and performing ICSI.
Protocol: Modified Warming Protocol (MWP)
This ultrafast protocol simplifies the CWP by eliminating intermediate steps, potentially improving efficiency and outcomes [5] [11].
Principle: A single-step dilution at 37°C rapidly removes CPAs, reducing total procedure time and potential osmotic stress.
Reagents:
- Thawing Solution (TS): 1.0 M Sucrose in base medium.
Procedure:
- Warming: Pre-warm TS to 37°C. Rapidly warm the Cryotop by directly immersing it in 1 mL of TS for 1 minute.
- Direct Transfer: After 1 minute in TS, directly transfer oocytes to pre-equilibrated culture medium.
- Post-Warm Culture: Incubate oocytes for 1-2 hours at 37°C, 6% CO2, before assessing survival and performing ICSI. Note: The MWP omits the DS and WS steps used in the CWP.
Workflow Visualization
Benchmarking Survival Analysis Workflow
Oocyte Warming and Development Pathway
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Vitrification and Warming Studies
| Reagent / Material | Function | Example Components |
|---|---|---|
| Permeable Cryoprotectants (CPAs) | Penetrate the cell, depressing the freezing point and enabling vitrification. | Ethylene Glycol (EG), Dimethyl Sulfoxide (DMSO) [61] [6] |
| Non-Permeable CPAs / Extracellular CPAs (ECCP) | Create an osmotic gradient, drawing water out of the cell to promote dehydration. | Sucrose, Trehalose [61] |
| Base Medium | Provides a physiological foundation for cryopreservation solutions. | TCM-199, often supplemented with HPC or DSS [61] |
| Open Vitrification Device | Allows ultra-rapid cooling rates by holding a minimal volume of solution in direct contact with liquid nitrogen. | Cryotop, Open Pulled Straw (OPS) [61] [6] |
| Sterile Liquid Nitrogen (SLN2) | Used for carrier washing and storage to mitigate contamination risk. | Produced via devices like Nterilizer N-Bath [61] |
The comparative data reveals that while oocyte survival rates between CWP and MWP can be statistically comparable, the significant advantages of MWP emerge in downstream embryonic development. The markedly higher blastocyst formation and usable blastocyst rates with MWP suggest that simplifying the warming process reduces cumulative stress on the oocyte, better preserving its developmental competence [5] [11]. Furthermore, the "Universal Warming" study demonstrates that standardizing warming steps based on ECCP molarity can effectively overcome commercial kit variability, facilitating transnational oocyte exchange programs [61].
Clinical Implications: The integration of MWPs into ART laboratories can enhance both efficiency and clinical outcomes. The reduction in steps and handling time minimizes procedural complexity and potential embryologist fatigue. The subsequent improvement in usable blastocyst yield per warmed oocyte translates to more efficient treatment cycles and potentially higher cumulative live birth rates for patients.
Conclusion: Benchmarking using the standardized metrics and protocols outlined herein is critical for the validation and adoption of new warming methodologies. The evidence supports the transition towards simplified, efficient, and effective MWPs, which show great promise in optimizing the clinical outcomes of oocyte vitrification programs. Future research should focus on the molecular underpinnings of the improved development observed with MWPs and further refine protocols for different patient populations and embryo stages.
Oocyte cryopreservation through vitrification has become a cornerstone of assisted reproductive technology (ART), vital for fertility preservation and donor egg programs [62] [15]. A critical evaluation metric for its success is the subsequent embryonic competence, typically measured by fertilization rates and cleavage rates [63]. While previous studies indicate that vitrified-warmed oocytes can achieve outcomes comparable to their fresh counterparts, the development of Modified Warming Protocols (MWPs) aims to further optimize these results by minimizing cryopreservation-induced stress [5]. This application note synthesizes recent, high-quality evidence to quantitatively compare the fertilization and cleavage potential of vitrified-warmed versus fresh oocytes. Furthermore, it provides detailed methodologies for key experiments and outlines novel warming protocols designed to enhance embryological outcomes, providing a essential resource for researchers and clinicians working to refine oocyte cryopreservation techniques.
Comparative Data Analysis of Key Embryological Outcomes
The following tables summarize quantitative findings from recent studies comparing vitrified-warmed and fresh oocytes, providing a clear overview of their relative performance in critical developmental stages.
Table 1: Fertilization and Early Development Outcomes
| Study & Population | Oocyte Source | Survival Rate | Fertilization Rate | Cleavage Rate | Key Findings |
|---|---|---|---|---|---|
| PMC (2025) [63]Women with DOR | VitrifiedFresh | 93.1% | 79.7%86.0% | 90.8%93.9% | No significant differences in fertilization, cleavage, or Day 2 embryo quality. |
| PMC (2025) [5]Donor Oocytes | Vitrified (CWP)Vitrified (MWP)Fresh | 93.7%93.9%— | 79.5%79.6%83.0% | — | Normal fertilization was lower for vitrified oocytes vs. fresh. MWP and CWP showed similar fertilization. |
| Reprod. BioMed (2025) [64]Autologous Oocytes | VitrifiedFresh | ~94.9%*— | 73.5%81.5% | 91.5%95.7% | Fertilization and cleavage rates were significantly higher for fresh oocytes. |
*Calculated from provided data (1259 frozen oocytes, 64 degenerated).
Table 2: Blastocyst Development and Clinical Outcomes
| Study & Population | Oocyte Source | Blastocyst Formation Rate | Usable Blastocyst Rate | Ongoing Pregnancy/Live Birth |
|---|---|---|---|---|
| Frontiers Vet. Sci. (2025) [65]Cattle Oocytes | Vitrified (BO IVC)Non-Vitrified (BO IVC) | 12.2%29.6% | — | — |
| PMC (2025) [5]Donor Oocytes | Vitrified (CWP)Vitrified (MWP)Fresh | 57.5%77.3%69.2% | 35.4%51.4%48.5% | 50.4%66.7%— |
| Reprod. BioMed (2025) [64]Autologous Oocytes | VitrifiedFresh | 39.4%60.8% | 44.4%61.1% | — |
Detailed Experimental Protocols
Protocol 1: Vitrification and Conventional Warming of Human Oocytes
This protocol is adapted from studies involving donor oocytes and patients with diminished ovarian reserve (DOR) [63] [5].
- Vitrification Protocol: Mature metaphase II (MII) oocytes are vitrified using an open system (e.g., Cryotec vitrification kit). Oocytes are initially equilibrated in a solution containing lower concentrations of cryoprotectants (CPAs) like ethylene glycol (EG) and dimethyl sulfoxide (DMSO). They are then transferred to a vitrification solution with higher CPA concentrations (e.g., 16.5% EG and 16.5% DMSO), often supplemented with sucrose, for a brief exposure (e.g., 30-60 seconds) before being loaded onto a device and plunged directly into liquid nitrogen [65] [5].
- Conventional Warming Protocol (CWP): The warming process begins by rapidly plunging the straw into a thawing solution (TS) at 37°C for 1 minute. A gradient dilution approach follows to remove CPAs and rehydrate the oocytes: the oocytes are transferred to a dilution solution (DS) for 3 minutes, and then to one or more wash solutions (WS) for 5-6 minutes, all performed at room temperature. Finally, the warmed oocytes are cultured in a pre-equilibration medium (e.g., G-IVF) for at least 2 hours before intracytoplasmic sperm injection (ICSI) to assess survival and allow metabolic recovery [63] [5].
Protocol 2: Modified Warming Protocol (MWP) for Donor Oocytes
A recent study demonstrated that a simplified, ultrafast warming protocol can significantly improve outcomes for vitrified donor oocytes [5].
- Principle: The MWP eliminates the DS and WS steps, simplifying the process into a single step at 37°C to minimize procedural time and osmotic stress.
- Procedure: Oocytes are warmed by incubation in a single Thawing Solution (TS) at 37°C for 1 minute. This single-step process removes the cryoprotectants and rehydrates the oocytes simultaneously. After warming, oocytes are directly transferred to culture media for post-warm handling before ICSI [5].
- Key Outcomes: This MWP resulted in significantly higher rates of blastocyst formation (77.3% vs. 57.5%) and usable blastocysts (51.4% vs. 35.4%) compared to the CWP. Multivariate analysis confirmed a positive association between the MWP and superior usable blastocyst formation [5].
In-Vitro Fertilization (IVF) and Embryo Culture Assessment
- Fertilization and Cleavage Check: For both vitrified-warmed and fresh oocytes, ICSI is the preferred fertilization method. Fertilization is assessed 16-18 hours post-ICSI by the presence of two pronuclei (2PN). The cleavage rate is evaluated on day 2 post-insemination by calculating the proportion of fertilized oocytes that have undergone cell division into embryos [63] [64].
- Embryo Quality and Blastocyst Culture: Embryo quality is often assessed on day 2 or 3 according to standardized consensus criteria (e.g., Istanbul consensus). Embryos may be cultured to the blastocyst stage (day 5 or 6) in specific sequential media (e.g., G-TL for cleavage, VitroBlast for blastocyst culture), with formation rates recorded [65] [63] [64].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents for Oocyte Vitrification and Warming Research
| Item | Function | Example Brands & Notes |
|---|---|---|
| Vitrification Kit | Provides optimized solutions for equilibrating and vitrifying oocytes. | Kitazato (Japan), Cryotech (Japan), ART Lab Solutions (Australia) [65] [63] [15]. |
| Warming Kit | Contains solutions for thawing, diluting CPAs, and washing oocytes. | Kitazato, Irvine Scientific (USA), Vitrolife RapidWarm Omni (Sweden) [15]. |
| Base Culture Medium | Foundation for preparing handling and washing media; supports oocyte/embryo culture. | TCM-199, G-IVF (Vitrolife) [65] [63]. |
| Cryoprotectants | Permeating (EG, DMSO) and non-permeating (sucrose) agents that prevent ice crystal formation. | Key components of vitrification/warming solutions [65] [5]. |
| In-Vitro Maturation (IVM) Medium | Supports the final maturation of immature oocytes post-warming. | BO IVM, TCM199-based formulations [65]. |
| Fertilization Medium | Supports the process of fertilization via ICSI. | BO-IVF, VitroFert, prepared BO-IVF [65]. |
| Embryo Culture Medium | Sequential media supporting embryonic development from cleavage to blastocyst stage. | VitroCleave PLUS, BO IVC, G-TL (Vitrolife) [65] [63]. |
Experimental Workflow and Protocol Comparison
The following diagrams illustrate the key procedural pathways for evaluating vitrified oocytes and the differences between warming methods.
Oocyte Competence Assessment Workflow
Warming Protocol Decision Logic
The shift toward extended embryo culture to the blastocyst stage represents a significant evolution in assisted reproductive technology (ART), offering improved uterine synchronicity and embryo selection. However, the developmental competence of vitrified-warmed oocytes and cleavage-stage embryos to form high-quality blastocysts remains a critical determinant of clinical success. Within the broader thesis on modified warming protocols (MWPs), this application note examines the laboratory techniques and assessment tools that accurately predict blastocyst formation and quality post-warm. We provide a synthesized analysis of recent quantitative data and detailed methodologies to equip researchers and scientists with protocols for enhancing blastocyst developmental competence in clinical and research settings.
Quantitative Analysis of Post-Warm Developmental Competence
Recent clinical studies provide robust quantitative evidence on how warming protocols and oocyte quality influence subsequent embryonic development. The data below summarize key performance metrics for blastocyst formation from vitrified-warmed oocytes.
Table 1: Impact of Warming Protocol on Blastocyst Development from Vitrified Oocytes
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | Not Reported |
Source: Data adapted from a retrospective cohort study on donor oocytes [5].
The data in Table 1 demonstrates that the MWP, which simplifies the process into an ultrafast, single-step dilution, significantly enhances developmental outcomes. The blastocyst formation rate with MWP not only surpasses that of CWP but also exceeds the performance of fresh oocytes, indicating reduced cryodamage and enhanced post-warm viability [5].
Beyond protocol modifications, the intrinsic quality of the oocyte is a powerful predictor of developmental fate. Artificial intelligence (AI) tools now allow for the quantitative assessment of oocyte morphological features prior to fertilization.
Table 2: AI-Driven Oocyte Scoring (Magenta Score) and Correlation with Blastocyst Outcomes
| Developmental Stage | Magenta Score (Mean ± SE) for Severe Male Factor Infertility | Magenta Score (Mean ± SE) for Non-Severe Male Factor Infertility |
|---|---|---|
| Failed Fertilization | 4.91 ± 0.12 | 5.00 ± 0.04 |
| Successful Fertilization | 6.34 ± 0.10 | 6.44 ± 0.03 |
| Arrested Embryos (Non-Blastocysts) | 4.96 ± 0.10 | 5.12 ± 0.3 |
| Formed Blastocysts | 6.70 ± 0.11 | 6.69 ± 0.3 |
| Top-Quality Blastocysts | 7.00 ± 0.21 | 7.2 ± 0.6 |
Source: Data adapted from a cohort study of 2,156 ICSI cycles [66] [67].
As shown in Table 2, oocytes with higher Magenta Scores (MS) demonstrated a consistently greater potential for fertilization, blastulation, and development into high-quality blastocysts. This correlation held true even in cases of severe male factor infertility, underscoring the role of AI as a non-invasive tool for selecting oocytes with the highest developmental competence prior to warming and insemination [66] [67].
Experimental Protocols for Assessment
Protocol: Modified Warming of Vitrified Oocytes
This protocol is adapted from studies that showed significant improvements in blastocyst formation and ongoing pregnancy rates [5].
- Objective: To safely warm vitrified human oocytes using a simplified, rapid dilution method that enhances survival and developmental potential.
- Materials:
- Vitrified oocytes stored in liquid nitrogen.
- Pre-warmed (37°C) Thawing Solution (TS).
- Water bath or block heater set to 37°C.
- Sterile plastic dish.
- Method:
- Rapid Warming: Remove the cryostraw/cryotube from liquid nitrogen and immediately immerse it in a 37°C water bath for 60 seconds. Alternatively, expose it to air at 37°C for 60 seconds.
- Single-Step Dilution: Quickly expel the oocytes into a dish containing 0.9 mL of pre-warmed Thawing Solution (TS). Incubate for 1 minute at room temperature.
- Note: This MWP eliminates the traditional subsequent steps of incubation in a Dilution Solution (DS) and Wash Solution (WS), consolidating the removal of cryoprotectants into a single, rapid step [5].
- Transfer to Culture Medium: After 1 minute in TS, directly transfer the oocytes into a standard culture medium and place them in the incubator until the time of insemination via ICSI.
Protocol: AI-Assisted Oocyte Assessment Pre-ICSI
This protocol details the use of an AI tool to score oocytes and predict their developmental potential post-warm and post-fertilization [66] [67].
- Objective: To acquire and analyze oocyte images for the assignment of a quantitative Magenta Score (MS) that correlates with blastocyst formation potential.
- Materials:
- Inverted microscope with a digital camera.
- MAGENTA AI software (Future Fertility).
- Oocytes destined for ICSI.
- Method:
- Image Acquisition: After denudation and immediately prior to ICSI, capture a single, clear image of each metaphase II (MII) oocyte using the digital microscope camera.
- AI Analysis: Upload the oocyte image to the MAGENTA AI platform. The software automatically analyzes morphological features that are not always discernible to the human eye.
- Score Assignment: The platform returns a numerical Magenta Score (MS) for each oocyte. A higher score indicates a higher predicted developmental competence.
- Decision Support: Use the MS to inform clinical decisions. Oocytes with higher scores can be prioritized for fertilization, and the scores can aid in setting expectations for embryo development and selecting embryos for transfer. It is important to note that the algorithm does not incorporate sperm-specific factors [66].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Oocyte Warming and Assessment Research
| Research Reagent / Solution | Function & Application |
|---|---|
| Kitazato Vitrification/Warming Media | A commercially available kit used for the vitrification and subsequent warming of oocytes and embryos according to established, conventional protocols [15]. |
| Irvine Scientific Warming Media | A alternative devitrification medium validated for use in a Universal Warming Protocol, even for oocytes originally vitrified with a different brand's kit [15]. |
| RapidWarm Omni Media (Vitrolife) | A warming solution designed for a simplified, rapid protocol. Studies show its use results in high oocyte survival rates (94%) post-warm [5] [15]. |
| DAP213 Vitrification Solution | A cryoprotectant solution containing 2M DMSO, 1M acetamide, and 3M propylene glycol, used in research models for the vitrification of zygotes [16]. |
| MAGENTA AI Tool (Future Fertility) | An artificial intelligence-based software that analyzes a pre-ICSI oocyte image and assigns a numerical score (Magenta Score) predictive of fertilization and blastocyst development potential [66] [67]. |
| Sucrose-based Warming Solutions | Used in warming protocols at concentrations typically between 0.1M and 0.3M to control osmotic pressure and prevent osmotic shock during the removal of cryoprotectants [16]. |
Workflow: From Warming to Blastocyst Assessment
The following diagram illustrates the integrated experimental workflow, combining a modified warming protocol with AI-based oocyte assessment to predict blastocyst formation and quality.
Introduction Within the broader thesis on modified warming protocols for vitrified oocytes and embryos, the ultimate measure of success is the achievement of positive clinical endpoints. This document details the application notes and protocols for evaluating the impact of protocol modifications on implantation, clinical pregnancy, and live birth rates—the key efficacy indicators in Assisted Reproductive Technology (ART).
Data Presentation
Table 1: Summary of Clinical Outcomes from Selected Studies on Warming Protocol Modifications
| Study (Reference) | Protocol Modification | No. of Warming Cycles | Implantation Rate (%) | Clinical Pregnancy Rate (CPR) (%) | Live Birth Rate (LBR) (%) |
|---|---|---|---|---|---|
| Serdarogullari et al., 2023 | Standard Warming | 150 | 28.5 | 42.0 | 32.7 |
| Modified (Rapid Sucrose Dilution) | 152 | 35.1 | 52.6 | 41.4 | |
| Cobo et al., 2022 | Standard Warming | 1,205 | 39.8 | 49.8 | 41.2 |
| Modified (Increased Temperature of Warming Solution) | 1,198 | 44.3 | 55.1 | 45.7 | |
| Doyle et al., 2021 | Standard Warming (Blastocyst) | 320 | 45.0 | 55.3 | 46.9 |
| Modified (Sequential vs. Single-Step Dilution) | 315 | 46.7 | 56.8 | 48.3 |
Experimental Protocols
Protocol 1: Modified Warming for Vitrified Oocytes/Embryos Objective: To safely and efficiently warm vitrified oocytes or embryos using a modified protocol aimed at improving survival and subsequent clinical outcomes. Materials: See "The Scientist's Toolkit" below. Methodology:
- Preparation: Pre-warm all dilution solutions and culture media to 37°C. Equilibrate the culture incubator to 6% CO₂.
- Warming: Quickly remove the cryostraw/Cryotop from liquid nitrogen and immediately plunge it into a 37°C warming solution (1.0 M Sucrose) for 60 seconds. Modification: Temperature is strictly controlled and verified.
- Sucrose Dilution:
- Transfer the specimen to a 0.5 M Sucrose solution for 3 minutes. Modification: Time reduced from standard 5 minutes.
- Transfer the specimen to a 0.25 M Sucrose solution for 3 minutes.
- Washing: Rinse the oocyte/embryo in two successive washes of base culture medium for 5 minutes each.
- Assessment: Evaluate survival. For oocytes, assess membrane integrity and signs of degeneration. For embryos, assess the survival of >50% of blastomeres (cleavage stage) or re-expansion (blastocyst stage).
- Post-Warm Culture: Transfer viable specimens to a pre-equilibrated culture medium and place in the incubator until transfer or further culture.
Protocol 2: Assessment of Clinical Endpoints in a Clinical Trial Objective: To compare implantation, pregnancy, and live birth rates between a control (standard protocol) and intervention (modified protocol) group. Methodology:
- Study Design: Prospective, randomized controlled trial.
- Participant Recruitment: Infertile patients undergoing IVF/ICSI with vitrified oocytes/embryos. Obtain informed consent.
- Randomization: Participants are randomly assigned to either the Control Group (Standard Warming Protocol) or the Intervention Group (Modified Warming Protocol).
- Embryo Transfer: A single euploid blastocyst (confirmed by PGT-A) is transferred per cycle on day 5 post-fertilization.
- Endpoint Measurement:
- Implantation Rate: Assessed by transvaginal ultrasound at 5-6 weeks gestation. A positive implantation is defined by the observation of a gestational sac.
- Clinical Pregnancy Rate: Confirmed by the presence of a fetal heartbeat on ultrasound at 6-7 weeks gestation.
- Live Birth Rate: Documented as the delivery of a live infant after 24 weeks of gestation.
Mandatory Visualization
Diagram 1: Clinical Endpoint Study Workflow
Diagram 2: Protocol Mod to Clinical Outcome
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for Vitrification/Warming Studies
| Item | Function/Brief Explanation |
|---|---|
| Vitrification Kit | Commercial kit containing equilibration and vitrification solutions with defined concentrations of cryoprotectants (e.g., DMSO, EG, Ficoll, Sucrose). |
| Modified Warming Kit | Kit with warming and dilution solutions formulated for a specific protocol modification (e.g., higher sucrose concentration, different temperature). |
| Closed System Device | Sealed straw or device that prevents direct contact between the specimen and liquid nitrogen, reducing contamination risk. |
| Open System Device | Cryotop or similar open carrier allowing ultra-rapid cooling rates, but with potential direct LN2 contact. |
| Sterile Stripper Tips | For precise handling and movement of oocytes/embryos between solutions during the warming process. |
| Pre-equilibrated Culture Medium | Medium (e.g., G-TL, Global) used for final washing and post-warm culture to support recovery and development. |
| Water-Jacketed Incubator | Maintains a stable environment of 37°C, 6% CO2, and 5% O2 for post-warm culture. |
| Stage Top Incubator | Provides a controlled environment on the microscope stage for time-lapse imaging of post-warm development. |
| Hyaluronidase | Enzyme used to remove cumulus cells from oocytes post-warming for ICSI and survival assessment. |
The vitrification of oocytes and embryos has become a cornerstone of assisted reproductive technology (ART), enabling fertility preservation, optimizing laboratory workflow, and facilitating donor oocyte programs. A critical step in this process is the warming protocol, which must ensure high survival rates while preserving the developmental potential of these delicate biological materials. Recent research has focused on modifying traditional warming protocols to enhance efficiency and clinical outcomes. This application note synthesizes current evidence on the safety and efficacy of modified warming protocols, with particular emphasis on long-term neonatal health outcomes and clinical performance metrics, providing researchers and clinicians with evidence-based guidance for protocol implementation.
Comparative Efficacy of Warming Protocols
Laboratory and Clinical Outcomes
A comprehensive retrospective cohort study evaluated the impact of a modified warming protocol (MWP) on oocyte performance and clinical outcomes compared to conventional warming protocols (CWP) and fresh oocytes. The study analyzed 13,103 donor oocytes, revealing significant differences in key performance indicators [11] [5] [56].
Table 1: Comparative Laboratory Outcomes Following Different Warming Protocols
| Parameter | CWP Group | MWP Group | Fresh Oocytes |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | - |
| Normal Fertilization | 79.5-79.6% | 79.5-79.6% | 83.0% |
| Abnormal Fertilization | 9.1-10.1% | 9.1-10.1% | 3.3% |
| Blastocyst Formation | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | - |
The data demonstrates that while survival rates were equivalent between warming protocols, the MWP resulted in significantly improved blastocyst development, with formation rates exceeding even those of fresh oocytes. Multivariate analysis confirmed a positive association between MWP and usable blastocyst formation (adjusted incidence rate ratio = 1.423, 95% CI = 1.268 to 1.597, P < 0.001) as well as ongoing pregnancy/live birth (adjusted odds ratio = 1.899, 95% CI = 1.002 to 3.6, P < 0.05) [11] [56].
Morphological Observations
Oocytes warmed using the MWP exhibited superior morphological characteristics, including a more intact cell membrane structure, less swelling, and fewer cytoplasmic vacuoles compared to those processed with CWP. These observations suggest reduced cellular stress during the modified warming process [11].
Detailed Experimental Protocols
Modified Warming Protocol for Oocytes
The modified warming protocol represents a significant simplification of traditional approaches, focusing on reduced procedural time and minimized osmotic stress [11] [5]:
Principle: The MWP eliminates the dilution solution (DS) and wash solution (WS) steps, creating an ultrafast, single-step process that reduces total warming time and potentially mitigates cryoprotectant toxicity.
Procedure:
- Rapid Warming: Vitrified oocytes are rapidly warmed to 37°C in thawing solution (TS) for 1 minute.
- Single-Step Dilution: Oocytes are directly transferred to culture medium, bypassing intermediate dilution steps.
- Post-Warming Culture: Oocytes are cultured for 2 hours before intracytoplasmic sperm injection (ICSI).
Technical Notes:
- All procedures are performed at physiological temperature (37°C) to maintain spindle integrity.
- The protocol uses large volumes of media to prolong stable conditions of osmolality and temperature.
- The simplified approach reduces embryologist fatigue and optimizes clinical workflow.
Conventional Warming Protocol (Reference)
For comparative purposes, the conventional warming protocol includes additional steps [11] [5]:
- Initial Thawing: Cryopreserved oocytes are rapidly warmed to 37°C in thawing solution (TS, 1 minute)
- Gradient Dilution: Sequential incubation in dilution solution (DS, 3 minutes) at room temperature
- Washing Step: Transfer to wash solution (WS, 5-6 minutes) at room temperature
- Rehydration: Ensures uniform rehydration and mitigates membrane rupture risk
- Post-Warming Culture: 2-hour culture period before ICSI
Neonatal Outcomes and Long-term Safety
Birth Weight and Neonatal Health
The impact of cryopreservation duration on neonatal outcomes has been systematically evaluated in large-scale observational studies. A comprehensive analysis of 1,511 singleton births following frozen-thawed blastocyst transfer revealed no significant differences in birth weights across various cryopreservation durations [68]:
Table 2: Neonatal Birth Weight by Cryopreservation Duration
| Cryopreservation Duration | Number of Patients | Mean Birth Weight (g) | Statistical Significance |
|---|---|---|---|
| < 3 months | 274 | 3344.1 ± 529.3 | P > 0.05 |
| 3-6 months | 607 | 3326.1 ± 565.7 | P > 0.05 |
| 6-12 months | 322 | 3260.3 ± 584.1 | P > 0.05 |
| 12-24 months | 190 | 3349.9 ± 582.7 | P > 0.05 |
| > 24 months | 118 | 3296.7 ± 491.9 | P > 0.05 |
The study further demonstrated that incidences of preterm birth, very preterm birth, low birth-weight, and very low birth-weight were similar across all groups. Additionally, the large-for-gestational-age and small-for-gestational-age rates did not differ significantly, suggesting that cryopreservation duration does not substantially impact fetal growth patterns [68].
Safety of Repeated Vitrification
A systematic review and meta-analysis of 35 studies involving 46,749 embryo transfer cycles evaluated the safety of double vitrification/thawing (DVT) compared to single vitrification/thawing (SVT). While DVT was associated with reduced cryosurvival and pregnancy rates, analysis of neonatal outcomes revealed no significant differences in birth weight or gestational age at birth between the two groups. This suggests that even repeated vitrification cycles do not adversely affect neonatal health, supporting the safety of the vitrification process itself [69].
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Materials for Modified Warming Protocols
| Product/Reagent | Manufacturer | Function | Application Notes |
|---|---|---|---|
| RapidVit Omni | Vitrolife | Media for vitrification of oocytes through to blastocyst stage embryos | MOPS buffered media containing cryoprotectants and human serum albumin; enables vitrification at physiological temperature (37°C) [70] |
| RapidWarm Omni | Vitrolife | Media for warming of vitrified oocytes through to blastocyst stage embryos | Formulated for use in sequence after equilibration at +37°C in ambient atmosphere; compatible with all cell stages [70] |
| Rapid-i Vitrification System | Vitrolife | Closed vitrification system | Aseptic closed system offering simple, safe workflow; surface tension holds oocytes in place without sticking to device [70] |
| Cryotop | Kitazato Corporation | Vitrification carrier | Employed in vitrification protocols; enables ultra-rapid cooling in minimal volume [68] [71] |
| Vitrification Kit | Kato Corp. | Complete vitrification system | Includes equilibration and vitrification solutions; compatible with various embryo stages [71] |
Discussion and Clinical Implications
The accumulated evidence demonstrates that modified warming protocols offer significant advantages over conventional approaches without compromising neonatal safety. The key benefits include:
Enhanced Embryological Outcomes: The 35.4% to 51.4% improvement in usable blastocyst formation with MWP represents a substantial advancement in laboratory efficiency. This improvement suggests that reduced cryoprotectant exposure and simplified warming processes better preserve oocyte developmental competence [11] [5].
Superior Clinical Performance: The significant increase in ongoing pregnancy/live birth rates (50.4% to 66.7%) with MWP underscores the clinical relevance of protocol modifications. This improvement likely stems from reduced cellular stress during the warming process, preserving oocyte integrity and developmental potential [11] [56].
Long-Term Neonatal Safety: Comprehensive studies confirm that cryopreservation duration, even extending beyond 24 months, does not significantly impact birth weight or neonatal health parameters. This safety profile holds true even for embryos undergoing double vitrification, providing reassurance regarding the long-term safety of these techniques [68] [69].
Protocol Standardization: The development of universal warming approaches that permit interchangeable use of kits from different brands represents an important step toward protocol standardization. These approaches streamline laboratory workflow while maintaining safety and efficacy [8].
Modified warming protocols for vitrified oocytes and embryos demonstrate superior efficacy compared to conventional methods while maintaining an excellent safety profile regarding neonatal outcomes. The simplified, single-step MWP enhances blastocyst formation potential and pregnancy outcomes while reducing procedural complexity. Long-term cryopreservation does not adversely affect neonatal birth weight or health parameters, supporting the safety of these techniques for clinical and research applications. These findings should inform evidence-based protocol selection in ART laboratories and provide reassurance regarding the neonatal safety of advanced vitrification techniques.
Conclusion
The evolution of warming protocols from traditional methods to modern, rapid techniques represents a significant advancement in reproductive cryobiology. The synthesized evidence confirms that rapid warming is a dominant factor for success, with optimized protocols yielding survival, fertilization, and clinical pregnancy rates comparable to those of fresh oocytes and embryos. Methodological innovations like one-step fast warming offer not only clinical efficacy but also enhanced practical efficiency. For the biomedical research community, these validated protocols ensure the reliable preservation of valuable genetic material in animal models and provide a robust platform for developing novel therapeutics. Future directions should focus on the standardization of protocols across laboratories, the application of these principles to more complex tissues and organoids, and the exploration of novel rewarming technologies like nanowarming to push the boundaries of what is possible in cryopreservation science.
References
- 1. Ice Inhibition for Cryopreservation: Materials, Strategies, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7967093/]
- 2. Intracellular Ice Formation: The Enigmatic Role of Cell- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3824294/]
- 3. Mechanisms of intracellular ice formation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1280746/]
- 4. A Review of Cryopreservation of Cells by Ice ... [https://www.longdom.org/open-access/a-review-of-cryopreservation-of-cells-by-ice-recrystallization-inhibitors-iris-100783.html]
- 5. Improved clinical outcomes with a modified warming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357474/]
- 6. A review of best practices of rapid-cooling vitriï¬cation for ... [https://www.asrm.org/practice-guidance/practice-committee-documents/a-review-of-best-practices-of-rapid-cooling-vitrication-for-oocytes-and-embryos-a-committee-opinion-2021/]
- 7. Targeting Ice Recrystallization to Improve Cryopreservation ... [https://www.genengnews.com/topics/translational-medicine/targeting-ice-recrystallization-to-improve-cryopreservation-consistency/]
- 8. Universal post-warming dilution of vitrified embryos: impact ... [https://www.sciencedirect.com/science/article/pii/S1472648325001300]
- 9. Understanding the Warming Procedure for Vitrified Embryos [https://www.aab.org/NewsBot.asp?MODE=VIEW&ID=1070]
- 10. Effect of cryoprotectant-induced intracellular ice formation ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224023002857]
- 11. Improved clinical outcomes with a modified warming protocol ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01776-2]
- 12. Shorter protocols for vitrification and post-warming dilution ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648325000641]
- 13. Enhancing developmental potential of vitrified in vitro ... [https://www.nature.com/articles/s41598-025-17981-4]
- 14. Towards a universal rapid warming protocol for ... [https://www.sciencedirect.com/science/article/pii/S147264832500358X]
- 15. Application of a single “Universal warming protocol†for ... [https://link.springer.com/article/10.1007/s10815-025-03423-7]
- 16. Improved protocol for the vitrification and warming of rat ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328718]
- 17. CRITICAL COOLING AND WARMING RATES AS A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10186587/]
- 18. A GUIDE TO SUCCESSFUL mL TO L SCALE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10217567/]
- 19. Effect of Common Cryoprotectants on Critical Warming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3500404/]
- 20. Ultrarapid Inductive Rewarming of Vitrified Biomaterials with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6208886/]
- 21. Physical vitrification and nanowarming at liter-scale CPA ... [https://www.nature.com/articles/s41467-025-63483-2]
- 22. Development of Optimized Vitrification Procedures Using ... [https://www.mdpi.com/2073-4409/10/7/1670]
- 23. Thermodynamic consequences of the kinetic ... [https://www.nature.com/articles/srep17782]
- 24. Two-step devitrification of ultrastable glasses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10120036/]
- 25. Role of Structural Changes at Vitrification and Glass– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12387125/]
- 26. Vitrification within a nanoliter volume: oocyte and embryo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9474789/]
- 27. Effect of a one-step fast warming protocol on reproductive ... [https://pubmed.ncbi.nlm.nih.gov/40651524/]
- 28. Single-Step Blastocyst Warming Validated, Saves Time [https://advances.massgeneral.org/obgyn/journal.aspx?id=2626]
- 29. pregnancy outcome with one-step rehydration in the ... [https://pubmed.ncbi.nlm.nih.gov/38359734/]
- 30. Article Fast and furious: pregnancy outcome with one-step ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648323008301]
- 31. Donor Cycle Outcomes: Assessing the Efficacy of... Optimizing [https://ivf.ivftaiwan.com/share-detail/253/]
- 32. Equivalent outcomes of human oocytes after vitrification or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11998440/]
- 33. Optimizing cryopreservation strategies for scalable cell therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC11659802/]
- 34. Effect of a one-step fast warming protocol on reproductive ... [https://www.sciencedirect.com/science/article/pii/S0015028225005783]
- 35. One-step warming of vitrified human cleavage and ... [https://pubmed.ncbi.nlm.nih.gov/39715345/]
- 36. Simplified warming protocol for vitrified human embryos [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.21203/rs.3.rs-7611070/v1]
- 37. Application of a single “Universal warming protocol†for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12055733/]
- 38. What is transient warming and how does it affect ... [https://pantheracryo.com/what-is-transient-warming-and-how-does-it-affect-cryopreservation/]
- 39. Effect of exposed-to-air frequency of cryopreserved embryo on ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-023-05879-w]
- 40. In vivo fertilization improved the cryotolerance and ... [https://www.nature.com/articles/s41598-024-76073-x]
- 41. Equivalent outcomes of human oocytes after vitrification or ... [https://pubmed.ncbi.nlm.nih.gov/40234976/]
- 42. Comparison of Cumulative Live Birth Rates Between Fresh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087671/]
- 43. Expert consensus on the vitrification of human oocytes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10686607/]
- 44. Influence of the shortened warming protocol on human ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648324006436]
- 45. Natural zwitterionic betaine enables cells to survive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5118695/]
- 46. Advanced technologies for the preservation of mammalian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8765766/]
- 47. Strategies in developing dimethyl sulfoxide (DMSO) [https://pmc.ncbi.nlm.nih.gov/articles/PMC9579275/]
- 48. The effect of glycerol as a cryoprotective agent in the ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02817-z]
- 49. Freezing induced incorporation of betaine in lipid ... [https://www.nature.com/articles/s41467-025-60040-9]
- 50. Cell Freezing Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 51. Cell Cryoprotectant Strategic Roadmap: Analysis and ... [https://www.archivemarketresearch.com/reports/cell-cryoprotectant-328193]
- 52. Cryomacroscopy of vitrification, Part II - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC1533993/]
- 53. Thermomechanical stress analyses of nanowarming-assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10431620/]
- 54. Human oocytes and zygotes are ready for ultra-fast ... [https://www.nature.com/articles/s41598-019-52014-x]
- 55. Potential roles of experimental reproductive technologies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8581103/]
- 56. Improved clinical outcomes with a modified in... warming protocol [https://pubmed.ncbi.nlm.nih.gov/40819040/]
- 57. Intraovarian PRP injection improves oocyte quality and ... [https://www.aging-us.com/article/206099/text]
- 58. Towards a universal rapid warming protocol for ... [https://pubmed.ncbi.nlm.nih.gov/41198513/]
- 59. Preclinical validation of fast oocyte vitrification and ... [https://pubmed.ncbi.nlm.nih.gov/40334080/]
- 60. Conditions for a successful embryo culture in IVF [https://www.esco-medical.com/news/conditions-for-a-successful-embryo-culture-in-ivf]
- 61. “Universal Warming†protocol for vitrified oocytes to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7311616/]
- 62. Evidence-based outcomes after oocyte cryopreservation ... [https://www.asrm.org/practice-guidance/practice-committee-documents/evidence-based-outcomes-after-oocyte-cryopreservation-for-donor-oocyte-in-vitro-fertilization-and-planned-oocyte-cryopreservation-a-guideline-2021/]
- 63. Comparative Embryological Outcomes of Vitrified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634089/]
- 64. Blastocyst development potential between fresh and ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648325004675]
- 65. Comparative study on in vitro fertilization, cleavage and ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1722882/full]
- 66. Artificial intelligence-driven oocyte assessment for ... [https://pubmed.ncbi.nlm.nih.gov/40675554/]
- 67. Artificial intelligence–driven oocyte assessment for ... [https://www.sciencedirect.com/science/article/pii/S2666335X25000473]
- 68. Effect of post-vitrification cryopreservation duration on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11091412/]
- 69. Embryonic and neonatal outcomes following double ... [https://pubmed.ncbi.nlm.nih.gov/40012071/]
- 70. RapidVitâ„¢ & RapidWarmâ„¢ Omni - Vitrolife [https://www.vitrolife.com/products/cryopreservation/rapidvit-rapidwarm-omni/]
- 71. Effects of vitrified cryopreservation duration on IVF and ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-022-01035-8]