Best Practices for Storing Fixed Embryos for Whole-Mount Immunofluorescence: A Guide to Preserving Antigenicity and Tissue Integrity
This article provides a comprehensive guide for researchers and drug development professionals on the critical aspects of storing fixed embryos for whole-mount immunofluorescence (WM-IF).
Best Practices for Storing Fixed Embryos for Whole-Mount Immunofluorescence: A Guide to Preserving Antigenicity and Tissue Integrity
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical aspects of storing fixed embryos for whole-mount immunofluorescence (WM-IF). It covers foundational principles of how storage conditions impact antigen preservation and tissue morphology, detailed protocols for short and long-term storage of various model organisms, advanced troubleshooting strategies for common issues like high background and signal loss, and validation techniques to ensure staining reproducibility. By synthesizing current methodologies and optimization strategies, this resource aims to empower scientists to achieve consistent, high-quality results in their developmental biology and biomedical research.
The Science of Specimen Preservation: How Storage Impacts Immunofluorescence Outcomes
The Critical Link Between Fixation, Storage, and Epitope Integrity
Troubleshooting Guides
Guide 1: Troubleshooting Poor Signal and Background Issues
This guide addresses the most common challenges researchers face when storing fixed embryos for whole-mount immunofluorescence.
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Weak or No Staining | Over-fixation (epitope masking) [1] [2] [3] | Reduce fixation duration; employ antigen retrieval (HIER) [4]. |
| Inadequate permeabilization [1] [2] | Use methanol/acetone or add a detergent like 0.1-0.5% Triton X-100 [5] [2]. | |
| Protein degradation due to under-fixation or delayed fixation [6] [4] | Ensure rapid and adequate fixation; use fresh fixative [6]. | |
| Antigen loss during long-term storage [1] | Use freshly prepared slides; image shortly after processing [1]. | |
| High Background Staining | Insufficient blocking [1] [2] [3] | Increase blocking incubation time; use serum from the secondary antibody host [1] [3]. |
| Antibody concentration too high [1] [2] | Titrate primary and/or secondary antibody to optimal dilution [1]. | |
| Sample autofluorescence [1] [2] [3] | Use unstained controls; avoid glutaraldehyde; use fresh formaldehyde [1]. | |
| Insufficient washing [1] [2] | Increase wash duration and volume between staining steps [1]. |
Guide 2: Troubleshooting Morphology and Preservation Issues
This guide focuses on problems related to the preservation of tissue architecture during fixation and storage.
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Poor Tissue Morphology | Fixative penetration issues [6] [4] | Ensure tissue is thin (<10 mm); use fixative volume 50-100x tissue volume [6]. |
| Use of inappropriate fixative for target [7] [5] | Choose cross-linking (e.g., PFA) for structure; precipitating (e.g., TCA) for some epitopes [5]. | |
| Tissue degradation before fixation [4] | Minimize delay between dissection and fixation; consider perfusion fixation [6]. | |
| Loss of Delicate Structures | Over-digestion with protease (e.g., Proteinase K) [8] | Optimize or omit protease digestion; use gentler acid-based permeabilization [8]. |
| Physical damage from harsh processing [8] | Use tailored protocols (e.g., NAFA) for fragile tissues like blastemas [8]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental impact of fixation on epitope integrity? Fixation is a balancing act. Its primary goal is to preserve tissue morphology and prevent proteolytic degradation by stabilizing biomolecules [7] [6]. However, the process itself can chemically alter proteins. Under-fixation fails to protect antigens, leading to their loss [6] [4]. Conversely, over-fixation, particularly with cross-linking fixatives like formaldehyde, can create excessive molecular cross-links that physically mask the epitope, preventing antibody binding [7] [6] [4].
Q2: How does the choice between PFA and TCA fixatives affect my experiment? The choice significantly impacts your results. Paraformaldehyde (PFA) is a cross-linking fixative that excellently preserves tissue architecture and is optimal for nuclear antigens [7] [5]. Trichloroacetic acid (TCA) is a precipitating fixative that denatures and aggregates proteins. It can alter the appearance of subcellular localization and sometimes reveal epitopes that are inaccessible with PFA, making it potentially better for some cytoskeletal or membrane proteins [5]. TCA fixation has been shown to result in larger, more circular nuclei compared to PFA [5].
Q3: What are the best practices for storing fixed embryos before immunostaining? To preserve epitope integrity, fixed samples should be stored in buffered solutions like PBS or TBS, often at 4°C [5]. For long-term storage, transferring fixed tissues to 70% alcohol until processing can help maintain antigenicity [4]. It is crucial to avoid prolonged storage of fixed samples, as antigenicity can fade over time. Samples should be processed and imaged as soon as possible after staining, mounting them with an anti-fade reagent [1].
Q4: How can I "rescue" an epitope that has been masked by over-fixation? Antigen retrieval techniques are designed to reverse the epitope masking caused by fixation. The most common method is Heat-Induced Epitope Retrieval (HIER), which involves heating tissue sections in a buffer (e.g., citrate pH 6.0 or EDTA pH 8.0) to break cross-links and unwind proteins [4] [9]. An alternative method is Enzymatic-Induced Epitope Retrieval (EIER), which uses proteases like trypsin to digest proteins and expose epitopes [4]. The optimal method and buffer must be determined empirically for each target.
Q5: Why is standardization of fixation protocols so important? Variability in fixation protocols between institutions is a major source of inconsistent and unreliable results [7] [4]. Factors such as fixation time, temperature, pH, and fixative concentration can dramatically affect epitope integrity and staining outcomes. Standardizing these parameters, along with the use of robust positive and negative controls, is essential for achieving reproducible data, especially in clinical and multi-center research settings [7] [4].
Experimental Protocol: Comparing Fixatives for Whole-Mount Immunofluorescence
The following detailed protocol, adapted from a 2024 preprint, allows for the systematic comparison of PFA and TCA fixation on chicken embryos [5].
1. Sample Preparation
- Incubate fertilized chicken eggs at 37°C to the desired Hamburger and Hamilton (HH) stage.
- Dissect embryos and place them onto filter paper in Ringer's Solution.
2. Fixation Methods
- Paraformaldehyde (PFA) Fixation:
- Fix embryos in 4% PFA in 0.2M phosphate buffer for 20 minutes at room temperature [5].
- Post-fixation, wash in Tris-Buffered Saline or Phosphate-Buffered Saline containing 0.1–0.5% Triton X-100 (TBST or PBST).
- Trichloroacetic Acid (TCA) Fixation:
- Fix embryos in 2% TCA in PBS for 1–3 hours at room temperature [5].
- Wash in TBST or PBST after fixation.
3. Immunostaining
- Blocking: Incubate embryos in PBST or TBST containing 10% donkey serum for 1 hour at room temperature or overnight at 4°C.
- Primary Antibody Incubation: Incubate in diluted primary antibody (see Table 2 in the preprint for examples) for 72–96 hours at 4°C [5].
- Washing: Wash embryos thoroughly in PBST or TBST.
- Secondary Antibody Incubation: Incubate with fluorophore-conjugated secondary antibodies (e.g., AlexaFluor, diluted 1:500) overnight at 4°C.
- Final Wash: Wash embryos in buffer.
- Post-fixation (for PFA-only): PFA-fixed embryos may be post-fixed with PFA for 1 hour at room temperature to stabilize the signal [5].
4. Mounting and Imaging
- Mount samples in an anti-fade mounting medium.
- Image immediately for optimal results [1].
The table below summarizes quantitative findings from a study comparing PFA and TCA fixation in chicken embryos [5].
| Fixative Type | Fixation Duration | Nuclear Morphology | Optimal For Epitope Localization | Key Considerations |
|---|---|---|---|---|
| 4% PFA (Cross-linking) | 20 minutes | Smaller, less circular [5] | Nuclear transcription factors (e.g., SOX9, PAX7) [5] | Excellent tissue preservation; may mask some epitopes requiring antigen retrieval [5] [4]. |
| 2% TCA (Precipitating) | 1-3 hours | Larger, more circular [5] | Cytoskeletal (e.g., Tubulin) & membrane proteins (e.g., Cadherin) [5] | Can alter subcellular localization; may damage delicate structures [5]. |
Research Reagent Solutions
This table lists key reagents essential for successful fixation and staining, along with their primary functions.
| Reagent | Function | Example Use Case |
|---|---|---|
| Paraformaldehyde (PFA) | Cross-linking fixative; preserves tissue architecture by forming methylene bridges between proteins [7] [6]. | Standard fixation for whole-mount embryos; optimal for nuclear antigens [5]. |
| Trichloroacetic Acid (TCA) | Precipitating fixative; denatures and aggregates proteins via acid-induced coagulation [5]. | Accessing hidden epitopes in cytosolic and membrane proteins [5]. |
| Triton X-100 | Non-ionic detergent; permeabilizes cell membranes to allow antibody penetration [5] [2]. | Added to wash buffers (0.1-0.5%) after aldehyde fixation to permeabilize cells [5]. |
| Donkey Serum | Blocking agent; reduces non-specific background staining by saturating reactive sites [5] [3]. | Used at 10% concentration in buffer to block embryos before antibody incubation [5]. |
| Sodium Borohydride | Reducing agent; quenches free aldehyde groups to reduce autofluorescence [2]. | Wash with 0.1% in PBS after aldehyde fixation to lower background [2]. |
| Citrate/EDTA Buffer | Antigen retrieval buffer; reverses formaldehyde-induced cross-links under heat [4] [9]. | Heat-induced epitope retrieval (HIER) for over-fixed, paraffin-embedded samples [4] [9]. |
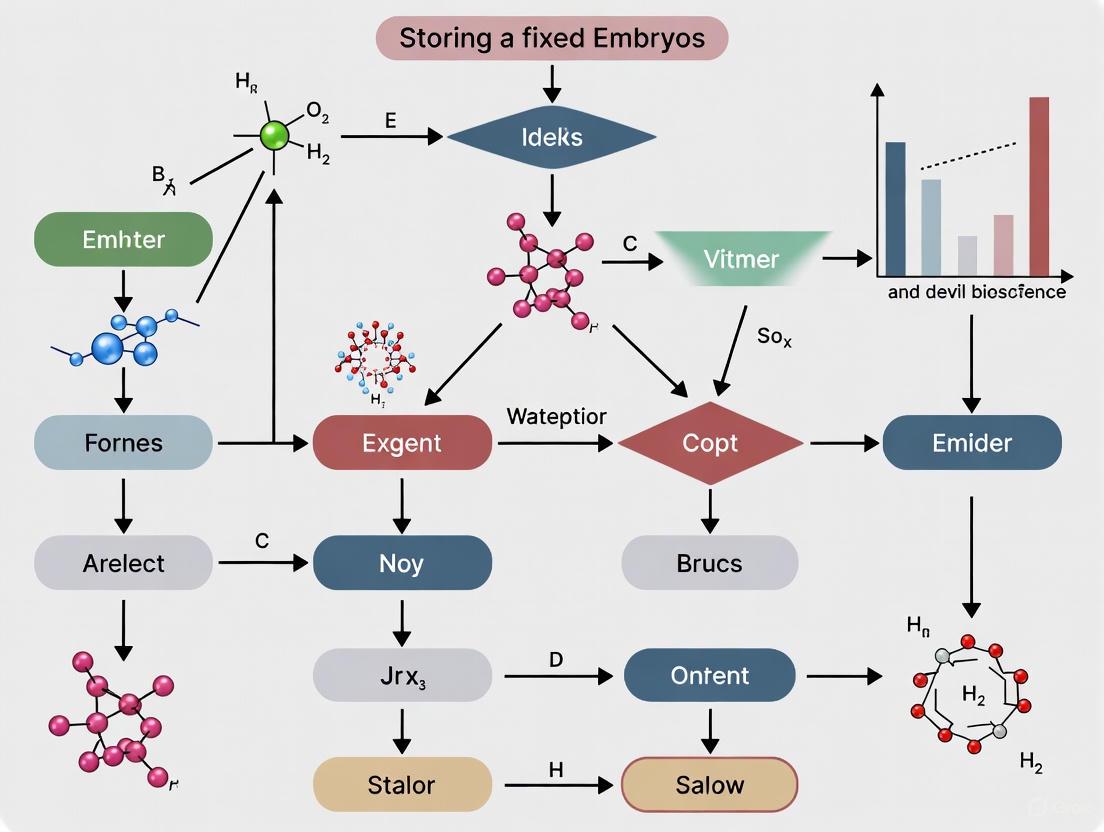
Workflow and Relationship Diagrams
Fixation and Storage Impact on Epitopes
Fixation Selection Decision Guide
For researchers conducting whole mount immunofluorescence on fixed embryos, proper storage is not merely a matter of sample preservation but a critical determinant of experimental success. Improperly stored samples are susceptible to two primary, interconnected issues that can compromise data integrity: the degradation of protein epitopes and the induction of autofluorescence. Epitope degradation diminishes the specific antibody signal, while autofluorescence increases background noise, collectively destroying the signal-to-noise ratio essential for high-quality imaging. This guide provides troubleshooting and best practices to help you safeguard your samples and ensure the reliability of your research outcomes.
Troubleshooting Guide: Common Storage-Related Issues
Q1: My immunofluorescence images have high background noise, making specific signal difficult to distinguish. Could this be related to how my fixed embryos are stored?
Yes, high background is a frequent consequence of improper storage. A primary cause is autofluorescence, which can be induced or exacerbated by several storage-related factors:
- Fixative-Related Autofluorescence: Using aldehydes like paraformaldehyde (PFA) is standard, but the chemical reactions between aldehydes and amines in proteins can generate fluorescent products. This is particularly problematic with over-fixation or if a "quenching" step is omitted after fixation [10].
- Storage Buffer and Duration: Prolonged storage, especially in buffers containing certain salts or at non-optimal pH, can increase background fluorescence over time. While specific studies on embryo storage duration are limited, the principles of protein and tissue integrity dictate that long-term storage should be approached with caution and validated.
How to Fix It:
- Quenching: After aldehyde fixation, incubate your samples with reagents that quench the unreacted aldehyde groups. Common quenching agents include 100mM glycine or 1% sodium borohydride in PBS [10].
- Optimized Storage Buffer: Store fixed samples in a neutral, isotonic buffer like PBS at 4°C. The addition of a preservative like 0.01% sodium azide can prevent microbial growth. For long-term storage, consider freezing at -20°C in an antifreeze solution, but be aware that freeze-thaw cycles can damage tissue morphology.
- Use Appropriate Controls: Always include a control sample stained only with the secondary antibody. This will help you determine the threshold of background signal specific to your storage conditions [10].
Q2: I am getting a weak or absent specific signal despite using a validated antibody. Could epitope degradation during storage be the cause?
Absolutely. A weak or absent signal often points to epitope degradation or masking. Epitopes are the specific regions on antigens recognized by antibodies. During storage, several processes can negatively impact them:
- Protein Denaturation and Modification: Over time, even fixed proteins can undergo subtle conformational changes or chemical modifications that destroy the antibody-binding site. Inadequate fixation can allow proteolytic enzymes to remain active, gradually degrading the target protein [10].
- Epitope Masking: The fixation process itself can cross-link proteins, potentially burying the epitope and making it inaccessible to the antibody. This is more likely with over-fixation.
How to Fix It:
- Optimize Fixation Protocol: Ensure fixation is sufficient but not excessive. A typical protocol is 10-20 minutes at room temperature with 2%-4% PFA for cell cultures, though tissues like embryos may require longer [10]. Test different fixation times for your specific antigen.
- Antigen Retrieval: For masked epitopes, employ antigen retrieval techniques after storage. This typically involves heating the samples in a buffered solution (e.g., citrate buffer) or using enzymatic digestion (e.g., proteinase K) to break cross-links and reveal hidden epitopes.
- Ensure Proper Permeabilization: If your target is intracellular, antibodies cannot access it without permeabilization. After storage and before staining, permeabilize your embryos with a detergent like 0.1%-0.2% Triton X-100 in PBS for 10 minutes at room temperature [10].
Frequently Asked Questions (FAQs)
Q: What is the best temperature for storing fixed embryos for long-term immunofluorescence studies? A: For short-term storage (days to a few weeks), fixed embryos can typically be kept in PBS at 4°C. For long-term storage (months to years), freezing at -20°C is recommended. However, the optimal protocol can be antigen-dependent. Freezing can cause ice crystal formation that disrupts morphology, so using a cryoprotectant solution is advised. You must empirically test the stability of your specific antigens under your chosen storage conditions.
Q: How does the choice of fixative influence long-term storage and autofluorescence? A: The fixative choice is a critical initial decision that impacts long-term sample quality.
- Aldehydes (PFA/Glutaraldehyde): Provide excellent structural preservation but are a major cause of chemical-induced autofluorescence, which can intensify with storage time. Quenching is essential [10].
- Organic Solvents (Methanol/Acetone): Precipitate proteins and are less likely to cause the same type of autofluorescence as aldehydes. They also permeabilize cells, eliminating the need for a separate permeabilization step. However, they may not preserve certain epitopes or cellular structures as well as PFA and can extract lipid-soluble components [10].
Q: Can I store my stained embryos and re-image them later? What are the risks? A: Yes, but with precautions. Mounted samples should be sealed with nail polish to prevent drying and stored in the dark at -20°C or +4°C [10]. The primary risks are fluorophore bleaching and potential sample degradation over time. For quantitative comparisons, it is best to image all samples within a single experiment using the same imaging settings to minimize variability.
Experimental Protocols for Validation
Protocol 1: Assessing Autofluorescence in Stored Samples
Purpose: To quantify and identify the level of autofluorescence in fixed embryo samples after different storage conditions.
Materials:
- Fixed embryo samples (stored under various conditions: e.g., 4°C vs. -20°C, different buffers)
- Phosphate-Buffered Saline (PBS)
- Mounting medium with anti-fading agents
- Microscope slides and coverslips
- Confocal or fluorescence microscope
Method:
- Sample Preparation: Take a subset of fixed embryos from each storage condition. Do not stain them with any primary or secondary antibodies.
- Mounting: Mount the unstained samples on slides using an anti-fade mounting medium.
- Imaging: Image the samples using the exact same laser lines and detection settings you would use for your actual immunofluorescence experiment.
- Analysis: The signal detected in these unstained samples is the autofluorescence. Compare the intensity and distribution across different storage conditions. This will establish a baseline background for your experiment.
Protocol 2: Validating Epitope Integrity After Storage
Purpose: To confirm that a specific antigen of interest remains detectable and produces a strong signal after a period of storage.
Materials:
- Fixed embryo samples (freshly fixed vs. stored)
- Validated primary antibody against your target
- Fluorophore-conjugated secondary antibody
- Blocking buffer (e.g., 1-5% BSA in PBS)
- Permeabilization buffer (e.g., 0.1-0.2% Triton X-100 in PBS)
- Washing buffer (e.g., PBS Tween-20)
- Counterstain (e.g., DAPI)
- Mounting medium
Method:
- Parallel Staining: Process a freshly fixed embryo and a stored embryo for immunofluorescence simultaneously, using the same antibody solutions and incubation times.
- Standard Staining Procedure:
- Permeabilize and block samples.
- Incubate with primary antibody (diluted in blocking buffer) for 1-2 hours at room temperature or overnight at 4°C [10].
- Wash extensively with a buffer like PBS Tween-20 to reduce unspecific binding [10] [11].
- Incubate with fluorophore-conjugated secondary antibody.
- Wash extensively again.
- Counterstain with DAPI and mount.
- Analysis: Image both samples with identical microscope settings. A significant reduction in specific signal intensity in the stored sample compared to the fresh control indicates a loss of epitope integrity due to storage.
Research Reagent Solutions
This table outlines key reagents used to prevent or mitigate storage-related issues in immunofluorescence.
| Reagent | Function | Example Protocol Notes |
|---|---|---|
| Paraformaldehyde (PFA) [10] | Cross-linking fixative that preserves cellular structure. | Typically used at 2-4%. Over-fixation can increase autofluorescence and mask epitopes. |
| Methanol [10] | Precipitating fixative. | Can be used cold (-20°C). Less associated with chemical autofluorescence but may not preserve all epitopes. |
| Triton X-100 [10] | Non-ionic detergent for permeabilization. | Used at 0.1-0.2% to allow antibody access to intracellular targets after storage. |
| Glycine / Sodium Borohydride [10] | Quenching agents. | Used after aldehyde fixation to reduce autofluorescence by neutralizing unreacted aldehyde groups. |
| Bovine Serum Albumin (BSA) [10] | Blocking agent. | Used at 1-5% to block non-specific antibody binding sites, reducing background. |
| Sodium Azide | Preservative. | Added to storage buffers (e.g., at 0.01%) to inhibit microbial growth during long-term storage at 4°C. |
Visualizing the Impact of Storage on Sample Quality
The following diagram illustrates the two main pathways through which improper storage compromises immunofluorescence results and the key interventions to prevent them.
FAQs: Storage Solutions for Fixed Embryos
Q1: Why is the osmolality of my embryo storage solution increasing over time, and how can I prevent it? Evaporation is a primary cause of rising osmolality, which can impair embryo development. The type of incubator and covering oil used are critical factors. Research shows that using a humidified incubator is significantly better at maintaining stable osmolality over a 7-day culture period compared to a dry incubator. Furthermore, when using a dry incubator, paraffin oil offers superior protection against evaporation for single-step media compared to mineral oil [12]. Ensuring an adequate volume of oil overlay and using culture dishes with designs that minimize evaporation are also effective strategies [13].
Q2: What pH buffer should I use in handling media for procedures outside the incubator? For procedures performed outside a CO₂ incubator, such as embryo transfer or cryopreservation, media containing only bicarbonate buffers are insufficient. Biological zwitterionic buffers, known as "Good's buffers," are essential for stabilizing pH in room air [14]. The table below summarizes common buffers and their properties.
| Buffer Name | pKa at 37°C | Notes on Use with Embryos |
|---|---|---|
| HEPES | 7.31 | Commonly used; provides effective buffering in handling media [14]. |
| MOPS | 6.93 | Appropriate for use near neutral pH [14]. |
| TAPSO | 7.39 | pKa is well-suited for embryonic culture; noted as potentially appropriate [14]. |
| Tris | 7.82 | pKa is relatively high for embryo culture; use with caution [14]. |
Q3: How can the choice of fixative and storage method affect my whole-mount immunofluorescence results? The fixation and storage process is critical for preserving antigenicity and tissue structure.
- Fixative: 4% Paraformaldehyde (PFA) is the most common fixative for whole-mount embryos. However, the protein cross-linking it causes can mask some epitopes. If staining is weak with PFA, methanol can be an alternative fixative that may improve antibody access [15].
- Storage: After fixation, embryos can be stored long-term in 100% methanol at -20°C [16]. For some embryos, such as Drosophila, storage in ethanol at -20°C is also effective [17]. Proper storage prevents degradation and preserves samples for future staining.
Q4: What are the common causes of high background in whole-mount immunofluorescence? High background staining is often due to non-specific antibody binding or tissue autofluorescence. Key solutions include [18] [3] [19]:
- Insufficient blocking: Extend the blocking time or optimize your blocking solution (e.g., using serum from the secondary antibody host).
- Antibody concentration too high: Titrate your primary and secondary antibodies to find the optimal concentration.
- Inadequate washing: Increase the duration and number of washing steps.
- Autofluorescence: Use unstained controls to check for inherent tissue fluorescence. Using fresh aldehyde fixatives and mounting media with anti-fade agents can help reduce this.
Troubleshooting Guide
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Weak or No Signal | Over-fixation with PFA leading to epitope masking. | Switch to methanol fixation or reduce PFA fixation time [15]. |
| Inadequate permeabilization preventing antibody penetration. | Optimize permeabilization agent concentration and incubation time [3]. | |
| Low antigen expression or primary antibody issues. | Use a positive control; validate antibody and increase concentration if needed [18]. | |
| Rising Osmolality | Evaporation due to low-humidity incubation. | Use a humidified incubator and ensure a proper seal on culture dishes [12] [13]. |
| Insufficient or inappropriate oil overlay. | Use paraffin oil, which is heavier and provides better evaporation protection than mineral oil [12]. | |
| High Background Signal | Non-specific antibody binding. | Optimize blocking conditions; include normal serum from the secondary antibody species [19]. |
| Endogenous enzymes or biotin activity. | Quench endogenous peroxidases with H₂O₂ or block endogenous biotin with a commercial kit [19]. |
Experimental Protocol: Fixation and Storage of Embryos for Whole-Mount Studies
This protocol, adapted from established methods, details the fixation and storage of zebrafish or similar vertebrate embryos for whole-mount immunofluorescence [16].
Materials Needed:
- Embryo wash buffer (e.g., PBS)
- 4% Paraformaldehyde (PFA) in PBS
- Phosphate-Buffered Saline (PBS), sterile
- 100% Methanol
- Embryo mesh baskets
- 50 mL conical tubes
- Platform shaker (optional)
Procedure:
- Collection and Washing: Collect embryos in a 50 mL conical tube. Remove culture water and wash embryos thoroughly with ice-cold sterile PBS.
- Fixation: Add 25 mL of ice-cold 4% PFA to the tube. Fix embryos for 24 hours at 4°C. If available, perform this step on a gentle rocker to ensure even fixation.
- Post-Fixation Wash: Carefully decant the PFA and wash the embryos three times with sterile PBS, for 7 minutes per wash.
- Dehydration and Storage: Decant the final PBS wash and add 25 mL of 100% methanol. Invert the tube several times. The embryos will sink to the bottom.
- Replace with fresh 100% methanol. Store the embryos at -20°C for up to one year [16].
Note: For immunofluorescence, re-hydrate embryos incrementally through a methanol:PBS series (e.g., 3:1, 1:1, 1:3) before proceeding to staining [16].
Research Reagent Solutions
| Item | Function | Application Notes |
|---|---|---|
| Paraformaldehyde (PFA) | Cross-linking fixative that preserves cellular structure. | Standard for morphology; may mask some epitopes. Use at 4% concentration [15] [16]. |
| Methanol | Precipitating fixative and storage medium. | An alternative to PFA; can improve antibody penetration for some targets [15]. |
| HEPES Buffer | Zwitterionic biological pH buffer. | Used in handling media to stabilize pH outside a CO₂ incubator [14]. |
| Paraffin Oil | Overlay to prevent evaporation. | Superior to mineral oil at reducing media evaporation and osmolality shifts in dry incubators [12]. |
| Bovine Serum Albumin (BSA) | Blocking agent and protein stabilizer. | Reduces non-specific antibody binding in blocking and antibody dilution buffers [19]. |
Workflow Diagram: Embryo Storage and Staining Pathway
The following diagram outlines the key decision points and steps in the process of preparing and storing embryos for whole-mount immunofluorescence.
For researchers working with fixed embryos in whole-mount immunofluorescence (IF), the integrity of your data is directly linked to your sample storage practices. A poorly stored sample can lead to diminished antigenicity, resulting in weak or false-negative signals, wasted resources, and inconclusive experiments. This guide addresses the critical, yet often overlooked, relationship between storage duration, conditions, and the preservation of antigenicity, providing evidence-based troubleshooting and protocols to safeguard your research outcomes.
FAQs on Storage and Antigenicity
Q1: What is the direct impact of long-term slide storage on immunofluorescence signal intensity?
Systematic studies have shown that while optimally fixed tissues are resilient, long-term storage of prepared slides can lead to a slight but significant decrease in IF signal intensity for certain antigens. The most critical factor is not time alone, but the primary antibody itself. Research on tissue microarrays found that four out of twelve antibodies tested showed no significant changes after one year of storage, while eight others exhibited limited decreases detectable by image analysis [20]. The subcellular localization of the antigen (nuclear vs. cytoplasmic/membranous) did not significantly influence its degradation rate [20].
Q2: What is the best way to store prepared slides to preserve antigenicity?
The storage condition plays a key role in preserving signal. The same long-term study compared different storage methods and found that refrigeration at 4°C proved to be the overall best procedure [20]. While storing slides coated with a protective layer of paraffin wax was also tested, no major advantages were found over uncoated slides when combined with optimal storage temperature [20].
Q3: How does the choice of fixative influence how I should store my samples?
The fixative fundamentally alters the tissue's chemical nature, which impacts storage strategy. Paraformaldehyde (PFA) works by creating cross-links between proteins, which generally creates a stable matrix that is resilient to long-term storage when properly prepared [5] [20]. In contrast, Trichloroacetic Acid (TCA) fixes by precipitating proteins through acid-induced denaturation and coagulation [5]. This different mechanism does not form the same stable cross-linked network, but its impact on long-term storage stability for whole-mount embryos is less defined and requires further empirical validation.
Q4: Can antigen retrieval reverse the damage caused by prolonged storage?
Yes, effectively. Heat-Induced Epitope Retrieval (HIER) is a powerful technique to restore antigenicity masked by fixation and potentially degraded by storage [20] [21]. The process of heating sections in specific buffers (e.g., citrate pH 6.0 or Tris-EDTA pH 9.0) helps break methylene cross-links formed during formalin/PFA fixation and can often recover epitopes, making them accessible to antibodies once more [21]. The success of this retrieval depends on using the correct buffer pH and heating method optimized for your specific antigen [22] [21].
Key Data and Comparisons
Comparative Analysis of Fixative Impact on Antigenicity
Table 1: Impact of common fixatives on antigen preservation and morphology in embryonic tissues.
| Fixative Agent | Mechanism of Action | Impact on Tissue Morphology | Impact on Antigenicity | Best Suited For |
|---|---|---|---|---|
| Paraformaldehyde (PFA) | Creates protein-protein cross-links [5]. | Preserves tissue architecture excellently [5]. | Good for a wide range of antigens; optimal for nuclear transcription factors (e.g., SOX9, PAX7) [5] [23]. | Nuclear proteins; general morphology studies [5] [23]. |
| Trichloroacetic Acid (TCA) | Precipitates proteins via acid denaturation [5]. | Alters morphology; results in larger, more circular nuclei [5] [23]. | Can alter/unmask epitopes; may be superior for some cytoskeletal (Tubulin) and membrane proteins (Cadherins) [5] [23]. | Hidden epitopes; specific cytosolic and membrane targets [5]. |
Impact of Storage Conditions on Signal Detection
Table 2: Effects of long-term slide storage on the detection of various biomarkers.
| Biomarker Type | Storage Duration | Key Findings | Recommendations |
|---|---|---|---|
| Proteins (IHC/IF) | Up to 1 year | Slight but significant changes for some, but not all, antibodies. No major difference between nuclear and cytoplasmic/membranous antigens [20]. | Test antibody sensitivity to storage. Store slides at 4°C. Use robust antigen retrieval [20]. |
| mRNA (In Situ Hybridization) | Up to 1 year | mRNA can be degraded over time on stored slides, making detection difficult [20]. | For mRNA studies, use freshly cut sections wherever possible. |
| DNA (FISH/CISH) | Up to 1 year | Gene copy number aberrations and chromosomal translocations remain detectable on slides stored for up to one year [20]. | Long-term storage is generally feasible for DNA-based assays. |
Experimental Protocols
Protocol: Validating Antigen Stability in Stored Samples
Purpose: To systematically test the effect of your storage conditions on the antigenicity of your target proteins in fixed whole-mount embryos.
Steps:
- Sample Preparation: Fix a batch of embryos (e.g., chicken or zebrafish) simultaneously using your standardized PFA protocol to ensure uniformity [5] [22].
- Storage Cohorts: Divide the fixed and washed embryos into several groups. For whole-mount samples, store them in PBS with 0.1% sodium azide at 4°C [22].
- Time-Points: Process a subset of embryos for whole-mount IF at defined intervals (e.g., immediately, 1 week, 1 month, 3 months, 6 months).
- Staining and Analysis: Perform IF under identical conditions for all time-points. Use consistent imaging parameters and quantify the mean fluorescence intensity of your target antigen relative to a background region.
- Include Controls: Always include a positive control (a freshly fixed and stained sample) to benchmark any signal loss.
Protocol: Heat-Induced Antigen Retrieval (HIER) for Restoring Signal
Purpose: To recover antigenicity that has been masked by fixation or diminished during storage [20] [21].
Materials:
- Sodium citrate buffer (10 mM, pH 6.0) or Tris-EDTA buffer (10 mM Tris, 1 mM EDTA, 0.05% Tween 20, pH 9.0) [21].
- Laboratory microwave, pressure cooker, or vegetable steamer.
- Coplin jars or microwaveable slide containers.
Steps:
- Deparaffinize and Rehydrate: If using paraffin-embedded sections, follow standard deparaffinization and rehydration steps.
- Choose Buffer: Select retrieval buffer based on the primary antibody's recommendation. Citrate pH 6.0 and Tris-EDTA pH 9.0 are the most common [21].
- Heat Retrieval:
- Pressure Cooker Method: Bring the buffer to a boil in a pressure cooker. Place slides in the buffer, secure the lid, and once full pressure is reached, time for 3 minutes. Cool rapidly under cold water [21].
- Microwave Method: Place slides in a container with retrieval buffer and heat in a microwave until boiling. Continue heating at a sub-boiling temperature for 20 minutes. Ensure slides do not dry out [21].
- Steamer Method: Place a container with slides and pre-heated buffer in a vegetable steamer for 20 minutes [21].
- Cooling: After heating, allow the slides to cool in the buffer for at least 20-30 minutes at room temperature.
- Wash and Proceed: Rinse slides with distilled water and proceed with your standard IF protocol [21].
Visual Workflows
The Scientist's Toolkit
Table 3: Essential reagents and materials for optimizing antigen preservation and detection.
| Reagent / Material | Function / Purpose | Key Considerations |
|---|---|---|
| Paraformaldehyde (PFA) | Cross-linking fixative for preserving tissue morphology and structural epitopes [5]. | Use freshly prepared or freshly thawed aliquots. Aged PFA adversely affects nuclear factor detection [24]. |
| Trichloroacetic Acid (TCA) | Precipitating fixative that can unmask hidden epitopes for certain proteins [5] [23]. | Alters nuclear and tissue morphology. Ineffective for mRNA visualization via HCR [23]. |
| Sodium Azide | Antimicrobial agent to prevent microbial growth in stored samples [22]. | Add to PBS (e.g., 0.1%) for long-term storage of fixed whole-mount embryos at 4°C [22]. |
| Triton X-100 / Tween-20 | Detergent for tissue permeabilization, allowing antibody penetration [5] [22]. | Increase concentration to 1% for dense tissues like whole-mount retina [22]. |
| Heat-Induced Epitope Retrieval Buffers | To break cross-links and unmask antigens lost during fixation or storage [21]. | Citrate (pH 6.0) and Tris-EDTA (pH 9.0) are most common. Optimal pH is antigen-dependent [21]. |
| Normal Donkey Serum | Component of blocking solution to reduce non-specific antibody binding [5] [24]. | Use the same species as your secondary antibody host for effective blocking. |
Practical Protocols for Optimal Short and Long-Term Embryo Storage
Purpose and Scope
This Standard Operating Procedure (SOP) outlines the protocols for the handling and initial storage of fixed embryos intended for whole-mount immunofluorescence (IF) research. Proper execution of these steps is critical for preserving tissue morphology, preventing antigen degradation, and ensuring high-quality staining outcomes. This protocol is designed for researchers working with murine and pre-implantation embryo models.
Materials and Equipment
Research Reagent Solutions
Table 1: Essential Reagents for Post-Fixation Handling and Storage
| Reagent/Material | Function | Protocol Notes |
|---|---|---|
| Paraformaldehyde (PFA) [24] [25] | Primary fixative; cross-links proteins to preserve tissue structure. | Use 1-4% solutions. Prepare fresh or use stocks <7 days old. Store at 4°C [24]. |
| Phosphate-Buffered Saline (PBS) [24] [26] | Isotonic washing and dilution buffer; removes fixative residue. | With or without Ca²⁺/Mg²⁺ as required by the protocol [24]. |
| PBS-Glycine [26] | Quenches unreacted aldehydes from PFA fixation to reduce background. | Used post-fixation before proceeding to storage or staining [26]. |
| Sucrose Solution [25] | Cryoprotectant; reduces ice crystal formation during freezing. | Tissues are incubated in sucrose (e.g., 15-30%) after fixation until they sink [25]. |
| Optimal Cutting Temperature (O.C.T.) Compound [25] | Water-soluble embedding medium for cryosectioning. | Used to embed tissues prior to snap-freezing [25]. |
| Isopentane (2-Methylbutane) [25] | Coolant for rapid snap-freezing of samples at ~-176°C. | Pre-cooled in liquid nitrogen; minimizes destructive ice crystals [25]. |
| Fructose-Glycerol Clearing Solution [26] | Mounting medium that improves tissue transparency for imaging. | An alternative to commercial mounting media; preserves fluorescence [26]. |
Procedure
Post-Fixation Quenching and Washing
- Transfer Fixed Embryos: Using fine forceps or a glass pipette, carefully transfer the fixed embryos from the fixative solution into a clean well or watch glass.
- Rinse: Wash the embryos with 1X PBS to remove the bulk of the fixative.
- Quench: Incubate the embryos in a freshly prepared PBS-Glycine solution (e.g., 0.1 M Glycine in PBS) for 15-30 minutes at room temperature to neutralize residual aldehydes [26].
- Final Washes: Perform three 5-minute washes in a sufficient volume of 1X PBS to ensure complete removal of the glycine and any trace fixative.
Initial Storage Setup
The choice of storage method depends on the subsequent experimental workflow.
A Short-Term Storage in PBS
- Application: For samples that will be processed for immunofluorescence within two weeks [27].
- Procedure:
- After the final PBS wash, transfer the embryos to a sterile vial or tube containing 1X PBS.
- Ensure the samples are completely submerged.
- Store at 4°C.
B Short-Term Storage in Ethanol
- Application: For long-term storage of fixed specimens, particularly for histological purposes [27].
- Procedure:
- Dehydrate the fixed and washed embryos through a series of graded ethanol baths (e.g., 50%, 70%, 95%).
- Store the embryos in 70% ethanol at room temperature [27].
C Cryopreservation for Sectioning or Staining
- Application: For optimal preservation of antigenicity and for samples intended for cryosectioning [25].
- Procedure:
- Cryoprotection: After washing, incubate the embryos in a 15-30% sucrose solution in PBS at 4°C until the samples sink (indicating saturation).
- Embedding:
- Place a small amount of O.C.T. compound in a labeled cryomold.
- Transfer the embryo into the O.C.T. and orient it correctly.
- Carefully top up the cryomold with more O.C.T., avoiding air bubbles.
- Snap-Freezing:
- Slowly lower the cryomold into a bath of isopentane pre-cooled by liquid nitrogen until the O.C.T. is completely frozen.
- CRITICAL: Do not submerge the sample directly into liquid nitrogen [25].
- Long-Term Storage:
- Wrap the frozen block in aluminum foil and transfer it to a -80°C freezer for long-term storage.
Workflow Diagram
The following diagram summarizes the key decision points and pathways after embryo fixation.
Troubleshooting and FAQs
Table 2: Troubleshooting Guide for Post-Fixation Issues
| Problem | Possible Cause | Recommendations |
|---|---|---|
| Weak or No Staining [28] [29] [30] | Antigen degradation due to long or improper storage. | For short-term storage in PBS, do not exceed 2 weeks [27]. For long-term, use cryopreservation at -80°C [25]. |
| High Background [28] [29] | Inadequate washing post-fixation; residual aldehydes. | Ensure thorough washing and include a quenching step with glycine after fixation [26]. |
| Poor Tissue Morphology [30] | Ice crystal damage during freezing. | Use adequate cryoprotection (sucrose) and snap-freeze in pre-cooled isopentane, not directly in liquid nitrogen [25]. |
| Tissue Autofluorescence [28] [29] | Autofluorescence induced by aldehyde fixatives. | Avoid glutaraldehyde. Use fresh PFA. A post-fixation wash with sodium borohydride (0.1% in PBS) can reduce this [28] [29]. |
| Sample Deterioration in Storage | Bacterial or enzymatic degradation. | Ensure samples are fully submerged in storage solution. Adding a very low concentration of sodium azide (NaN₃, e.g., 0.0048 μg/mL in 1X buffer) to PBS can prevent microbial growth [26]. CRITICAL: NaN₃ is highly toxic; handle with extreme care [26]. |
Frequently Asked Questions (FAQs)
1. What is the purpose of sodium azide in the PBS storage solution? Sodium azide is added to Phosphate-Buffered Saline (PBS) as a preservative to prevent microbial or bacterial growth in stored fixed samples. For tissue planned to be stored in a refrigerator (4°C) for over three weeks, the use of PBS with 0.01% sodium azide is recommended [31].
2. Why is a 30% sucrose solution used prior to freezing samples? Sucrose is used as a cryoprotectant. It helps to protect against freezing artifacts by displacing water within the tissue, which reduces the formation of damaging ice crystals during the freezing process. Specimens are equilibrated in the sucrose solution until they sink to the bottom of the container, indicating full penetration [32] [33].
3. Can I store my fixed embryos directly in PBS, and for how long? Yes, fixed samples can be stored in PBS or PBS-T (PBS with Tween 20) at 2-8°C for extended periods. One protocol specifies storing fixed organoids in PBS-T at 2-8°C for up to one week [33]. Another source indicates that PBS with 0.01% sodium azide should be used for tissue stored for over three weeks at 4°C [31].
4. My immunofluorescence background is high. What could be the cause? High background can result from several factors:
- Inadequate Blocking: Ensure you are using an appropriate blocking buffer, such as one containing 5% serum from the same species as your secondary antibody host, for a sufficient time (30 minutes to 2 hours at room temperature or overnight at 4°C) [34] [33].
- Insufficient Washing: Perform multiple thorough washes (e.g., 3x for 10-15 minutes each) with a wash buffer like PBS-T after each antibody incubation step [32] [34].
- Over-fixation: Excessive fixation can mask epitopes and increase non-specific background staining [32].
5. My sample morphology is poor after sectioning. How can I improve this? Poor morphology can often be traced to the fixation and cryoprotection steps:
- Fixation: Use freshly prepared paraformaldehyde (PFA) for optimal results. Under-fixation can lead to poor structural preservation [33].
- Cryoprotection: Ensure complete equilibration in the 30% sucrose solution before attempting to freeze the sample. The tissue should no longer float in the sucrose solution [33].
- Freezing Method: Snap-freezing the sample rapidly helps prevent the formation of ice crystals that disrupt cellular architecture. This can be done using a dry ice/ethanol slurry or isopentane chilled with liquid nitrogen [32] [33].
Troubleshooting Guide
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| Microbial Contamination | Storage solution lacks preservative. | Add 0.01% sodium azide to PBS for long-term storage (>3 weeks) [31]. |
| High Background Staining | Non-specific antibody binding or insufficient washing. | Optimize blocking conditions (e.g., 5% serum); Increase wash frequency/duration; Titrate primary antibody concentration [32] [34]. |
| Poor Tissue Morphology | Incomplete cryoprotection; Slow freezing. | Equilibrate in 30% sucrose until tissue sinks; Use a snap-freezing method (dry ice/ethanol slurry) [33]. |
| Weak or No Signal | Epitope masked by over-fixation. | Perform antigen retrieval (e.g., heat-induced epitope retrieval with citrate buffer) [32] [33]. |
| Tissue Damage/Loss | Sample not adequately adhered to slide; Rough handling. | Use gelatin-coated slides for better adhesion; Handle samples gently with cut pipette tips [32] [33]. |
Research Reagent Solutions
The table below lists key reagents used in the short-term storage and processing of fixed embryos for whole-mount immunofluorescence.
| Reagent | Function | Example Formulation & Notes |
|---|---|---|
| Paraformaldehyde (PFA) | Fixative: Cross-links proteins to preserve tissue structure and antigenicity. | 2-4% in PBS. For best results, use freshly prepared from powder or frozen aliquots [33] [26]. |
| PBS with Azide | Storage Buffer: Provides an isotonic environment for storage; azide inhibits microbial growth. | 1X PBS with 0.01% sodium azide. Ideal for refrigerated storage for several weeks [31]. |
| Sucrose | Cryoprotectant: Penetrates tissue and reduces ice crystal formation during freezing. | 30% (w/v) in PBS. Specimens are equilibrated until they sink [33]. |
| Triton X-100 | Detergent / Permeabilization Agent: Creates pores in cell membranes to allow antibody penetration. | Typically used at 0.1-0.5% in blocking or wash buffers [32] [26]. |
| Serum Albumin (BSA) | Blocking Agent: Used to block non-specific binding sites to reduce background. | Used at 1-5% in incubation buffers [32] [26]. |
| Normal Serum | Blocking Agent: Serum from the host species of the secondary antibody further reduces background. | Commonly used at 1-10% in blocking buffers [32] [34] [33]. |
| Tween 20 | Detergent / Wash Buffer Additive: A mild detergent used in wash buffers to reduce non-specific binding. | Typically used at 0.1% in PBS (PBS-T) for washing steps [33]. |
Experimental Workflow for Embryo Storage & Processing
The following diagram outlines the key steps for the short-term storage, processing, and staining of fixed embryos for whole-mount immunofluorescence.
Cryopreservation is a fundamental technique that uses low temperatures to preserve the structural integrity of living cells and tissues, effectively suspending their metabolic activity for long-term storage. For researchers working with fixed embryos for whole mount immunofluorescence, a robust cryopreservation strategy is essential for maintaining antigen accessibility, cellular morphology, and experimental reproducibility over months to years. This process involves carefully controlled cooling to very low temperatures (typically -80°C to -196°C) to dramatically reduce all biological and chemical reactions. The success of long-term storage depends on three critical factors: the composition of the freezing media, the cooling and warming rates employed, and the optimization of storage temperatures. By implementing proper cryopreservation protocols, researchers can preserve valuable embryonic specimens for future immunofluorescence analyses while minimizing changes to cellular genetics or morphology that might occur with continuous passaging or inadequate storage conditions.
Fundamental Principles of Cryopreservation
The Role of Cryoprotective Agents (CPAs)
Cryoprotective agents are essential components of any freezing media, functioning to protect cells from damage during the freezing process. The primary mechanism of protection involves preventing the formation of intracellular ice crystals that can pierce cell membranes and cause structural damage [35]. CPAs work by replacing water within cells and creating a protective environment that minimizes ice crystal formation. The permeability of embryos to different CPAs varies significantly, which directly influences how these compounds are taken up by cells and ultimately determines their protective efficacy [36]. Commonly used permeable CPAs include:
- Dimethyl sulfoxide (DMSO): A highly permeable CPA that readily crosses cell membranes but exhibits higher toxicity, particularly at suprazero temperatures [37].
- Ethylene glycol (EG): Demonstrates lower CPA toxicity and often provides higher post-cryopreservation survival compared to DMSO at the same concentration [37].
- Propylene glycol (PG): Another permeable CPA option with intermediate properties.
Non-permeable CPAs include sugars such as sucrose, sorbitol, and trehalose, which function primarily by creating an osmotic gradient that facilitates dehydration before freezing [37]. Research indicates that combinations of permeable and non-permeable CPAs often provide superior post-cryopreservation survival compared to permeable CPAs alone at the same total osmolarity, as they reduce overall CPA toxicity while maintaining protection against lethal ice formation [37].
Temperature Optimization and Rate Changes
The temperatures and rate changes employed during cryopreservation are critical variables that significantly impact specimen survival. The cooling rate determines how water exits cells and ice forms, while the warming rate affects the reversal of these processes. For most cell types, a controlled cooling rate of approximately -1°C/minute is ideal for freezing [38]. However, the warming rate is at least as important, if not more important, in determining ultimate survival of cryopreserved specimens [36]. Rapid warming helps reduce exposure time to the solutes present in freezing media and minimizes damage from ice recrystallization [38].
Storage temperature selection directly affects long-term viability. For optimal long-term performance, storage at liquid nitrogen temperatures (-135°C to -196°C) is recommended [39] [38]. While short-term storage (<1 month) at -80°C may be acceptable, cells kept at this temperature will degrade over time due to transient warming events during freezer access and thermal cycling [38]. This decline in viability is cell-type dependent but inevitable at these higher storage temperatures.
Figure 1: Cryopreservation Workflow for Embryo Storage. This diagram outlines the key stages in the long-term cryopreservation process, from initial preparation through to viability assessment after thawing.
Cryopreservation Protocols for Fixed Embryos
Pre-processing and Fixation Considerations
Proper tissue preparation before cryopreservation is crucial for maintaining specimen quality, particularly for fixed embryos intended for whole mount immunofluorescence. The quality of your starting tissue fundamentally impacts staining results, so always use the freshest tissue possible or ensure appropriate storage conditions for downstream applications [40]. Fixation should be performed with freshly prepared or freshly thawed 4% paraformaldehyde (PFA) to achieve optimal results. For consistent fixation, incubate embryos in fixative overnight at 4°C on a gentle shaker to ensure homogeneous reaction across the tissue [40].
For embryos destined for frozen tissue sections, post-fixation processing includes incubation in 30% sucrose solution, which acts as a cryoprotectant. This step should be conducted for at least overnight in the refrigerator before embedding in a cryomatrix [40]. It's important to note that tissue should not be stored in sucrose for longer than one week to prevent bacterial or fungal growth and degradation of proteins of interest [40]. For long-term storage of fixed tissue before sectioning, frozen tissue blocks or cryosections should be stored at -20°C or -80°C.
Vitrification Protocol for Embryos
Vitrification represents an advanced cryopreservation method that utilizes high concentrations of CPAs and ultra-rapid cooling to transform cellular solutions into a glassy, non-crystalline state. This technique has proven highly effective for embryo cryopreservation, with studies demonstrating that embryos resulting from vitrified eggs have similar developmental competence as those from fresh eggs when optimized protocols are used [41].
Table 1: Comparative Analysis of Vitrification Protocol Variables
| Protocol Variable | Short Protocol (45 sec) | Long Protocol (90 sec) | Impact on Outcome |
|---|---|---|---|
| VS Exposure Time | 45 seconds | 90 seconds | Affects CPA penetration and potential toxicity |
| Blastocyst Formation | 26.5% | 50.8% | Significantly higher with longer exposure [41] |
| Survival Rate | No significant difference | No significant difference | Both protocols showed similar survival |
| Clinical Pregnancy | No significant difference | No significant difference | Comparable outcomes after transfer |
| Recommended Use | Suboptimal for blastocyst development | Preferred for improved blastocyst formation | Long protocol provides better developmental outcomes |
A standardized vitrification protocol for embryos involves the following key steps:
Equilibration: Transfer embryos through a series of equilibration solutions containing increasing concentrations of CPAs. A typical approach involves:
- Basic solution for 1 minute
- Equilibration solution (7.5% ethylene glycol + 7.5% DMSO) for 2 minutes
- Second equilibration solution for another 2 minutes
- Fresh equilibration solution for 5 minutes [41]
Vitrification Solution Exposure: Transfer embryos to vitrification solution (typically 15% EG + 15% DMSO + 0.5M sucrose) in three drops of 10-20 seconds each [41]. Research indicates that longer exposure times (90 seconds total) significantly improve blastocyst formation rates compared to shorter exposures (45 seconds) without compromising survival, fertilization, or pregnancy rates [41].
Loading and Cooling: Load embryos onto specialized vitrification devices (e.g., cryotop, cryomesh) and immediately plunge into liquid nitrogen. The "CPA solution free" method, which involves wicking away excess solution before vitrification, significantly improves cooling and warming rates and enhances post-cryopreservation survival [37].
Slow Freezing Protocol
While vitrification has gained popularity for many applications, controlled slow freezing remains a valuable approach, particularly for certain embryo types. The slow freezing method involves:
CPA Exposure: Embryos are exposed to lower concentrations of CPAs compared to vitrification, typically through a step-wise addition to minimize osmotic shock.
Controlled Cooling: Using a programmable freezer or freezing container, embryos are cooled at a controlled rate of approximately -1°C/minute to between -30°C and -80°C before transfer to liquid nitrogen for storage [38] [35].
Seeding: During the cooling process, the solution is intentionally seeded to initiate extracellular ice crystal formation at a specific temperature, which helps control dehydration.
This method allows for gradual dehydration of cells as extracellular ice forms, minimizing intracellular ice crystal formation. However, comparisons between slow freezing and vitrification generally show superior survival rates with vitrification for most embryo types [41].
Research Reagent Solutions
Table 2: Essential Reagents for Embryo Cryopreservation
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Permeable CPAs | Ethylene Glycol (EG), Dimethyl Sulfoxide (DMSO), Propylene Glycol (PG) | Penetrate cell membranes to protect against intracellular ice formation; EG shows lower toxicity [37] |
| Non-permeable CPAs | Sucrose, Sorbitol, Trehalose | Create osmotic gradient for controlled dehydration; reduce required concentration of permeable CPAs [37] |
| Commercial Media | CryoStor CS10, mFreSR, STEMdiff | Pre-formulated, serum-free options providing consistent performance; some are GMP-manufactured for regulatory compliance [38] |
| Permeabilization Agents | D-limonene and heptane mixture | Remove waxy layers for improved CPA penetration; critical for some embryo types [37] |
| Cryoprotective Additives | Fetal Bovine Serum (FBS), Bovine Serum Albumin (BSA) | Provide additional membrane protection in home-made freezing media; FBS raises concerns about lot-to-lot variability [38] |
Troubleshooting Common Cryopreservation Issues
Low Post-Thaw Survival Rates
Inadequate survival rates following thawing indicate issues with one or more aspects of the cryopreservation process:
Problem: Ice crystal formation during freezing or thawing.
Problem: CPA toxicity evidenced by damaged cellular structures.
- Solution: Optimize CPA exposure times and concentrations. Consider using less toxic CPAs like ethylene glycol instead of DMSO. Implement combination strategies using both permeable and non-permeable CPAs to reduce overall toxic load [37].
Problem: Incomplete permeabilization preventing CPA entry.
- Solution: For challenging specimens, implement permeabilization steps such as brief treatment with D-limonene and heptane mixtures to remove waxy layers [37].
Poor Morphology or Antigen Preservation in Fixed Specimens
When cryopreserved fixed embryos show degraded morphology or poor antigen recognition in immunofluorescence:
Problem: Inadequate or inconsistent fixation before cryopreservation.
- Solution: Use freshly prepared 4% PFA and ensure consistent fixation conditions with gentle agitation. Standardize fixation times across experiments [40].
Problem: Ice crystal damage during freezing disrupting cellular architecture.
- Solution: Implement proper cryoprotection with sucrose infiltration (e.g., 30% sucrose overnight) before freezing for specimens intended for sectioning [40].
Problem: Antigen masking during the freezing process.
- Solution: Incorporate antigen retrieval methods after thawing, such as heating in acidic (sodium citrate, pH 6) or basic buffer (Tris-HCl, pH 9) for 15-20 minutes [40].
Contamination and Storage Failures
Maintaining specimen integrity throughout the storage period is essential for long-term projects:
Problem: Microbial contamination in stored specimens.
- Solution: Include antimicrobial agents like sodium azide in PBS for temporary storage of fixed specimens before freezing. Avoid long-term storage in sucrose solutions which promote microbial growth [40].
Problem: Temperature fluctuations during storage compromising viability.
- Solution: Use temperature monitoring systems with alarms for storage tanks. Ensure proper maintenance of liquid nitrogen levels in storage dewars. For critical samples, consider duplicate storage in separate tanks [39].
Problem: Sample identification errors or mix-ups.
- Solution: Implement comprehensive labeling systems using alcohol- and liquid nitrogen-resistant markers or printed cryo labels. Maintain detailed inventory records of banked specimens [38].
Frequently Asked Questions (FAQs)
Q1: How long can embryos remain in cryostorage without significant degradation? Embryos can theoretically remain viable indefinitely when stored at proper liquid nitrogen temperatures (-135°C to -196°C), as all metabolic activity is effectively suspended at these temperatures [39]. However, practical storage limits may be influenced by factors such as storage tank maintenance, potential for temperature fluctuations, and legal constraints on storage duration which can extend up to 55 years in some jurisdictions with proper consent [42].
Q2: What concentration of cryoprotectant should I use for embryo cryopreservation? Optimal CPA concentration depends on the specific embryo type and cryopreservation method. For vitrification, final concentrations of 15% EG + 15% DMSO + 0.5M sucrose have been used successfully [41]. However, research indicates that combinations of 39% EG with 9% sorbitol can provide excellent protection with reduced toxicity [37]. Empirical testing is recommended to determine the ideal concentration for specific embryo types.
Q3: Why do some embryos survive cryopreservation while others do not, even from the same batch? Embryo viability post-cryopreservation depends on multiple factors including developmental stage, morphological quality, and genetic background [39] [37]. At the time of freezing, embryos are evaluated for potential viability based on morphology and structural features. Even with careful selection, some embryos may not survive the freezing process due to subtle differences in membrane composition, metabolic state, or structural integrity [39].
Q4: What is the recommended cooling rate for embryo cryopreservation? For slow freezing methods, a controlled rate of approximately -1°C/minute is generally ideal for most cell types [38]. However, for vitrification, ultra-rapid cooling is essential to achieve the glassy state without ice crystal formation. This requires specialized devices or direct plunging into liquid nitrogen after proper CPA equilibration [41] [37].
Q5: How can I improve antibody penetration in cryopreserved fixed embryos for whole mount immunofluorescence? For whole mount immunostaining of cryopreserved embryos, several strategies can enhance antibody penetration: (1) Increase detergent concentration (e.g., 1% Triton-X or Tween-20) during permeabilization; (2) Implement antigen retrieval using heated buffers (70°C for 15 minutes) in Tris-HCl pH 9 or sodium citrate pH 6; (3) For challenging specimens, include a 20-minute treatment with ice-cold acetone at -20°C before antibody incubation [40].
Q6: What quality control measures should I implement for long-term cryostorage? Robust quality control for cryostorage includes: (1) Daily monitoring of storage tank temperatures with alarm systems that alert staff if temperatures rise even a single degree above requirements [39]; (2) Proper labeling systems using liquid nitrogen-resistant markers; (3) Detailed inventory management tracking all samples entering and leaving storage; (4) Regular tank maintenance and backup systems for critical storage units [39] [38].
Implementing optimized long-term cryopreservation strategies for fixed embryos requires careful attention to multiple interdependent factors: the composition and formulation of freezing media, controlled manipulation of temperature rates during cooling and warming, and maintenance of stable ultra-low storage temperatures. The protocols and troubleshooting guides presented here provide a foundation for researchers to preserve embryonic specimens effectively for whole mount immunofluorescence and other downstream applications. By understanding the fundamental principles of cryobiology and applying systematic approaches to protocol optimization and problem-solving, scientists can ensure the long-term viability and experimental utility of valuable embryonic research specimens for months to years, thereby enhancing research reproducibility and enabling longitudinal studies that would otherwise be impossible.
Frequently Asked Questions (FAQs)
1. What is the most critical factor for successful long-term storage of fixed embryos? The quality of the initial fixation is paramount. Always use fresh, high-quality fixative (e.g., freshly prepared or thawed 4% PFA) and ensure the fixation time is appropriate for your embryo's size and stage. Poor fixation cannot be reversed and will compromise all downstream applications, including long-term storage [43].
2. I need to pause my experiment after fixation. What is the best way to store my zebrafish embryos? For zebrafish embryos, you can store them in phosphate-buffered saline (PBS) with 0.1% sodium azide at 4°C for up to two weeks. The sodium azide prevents bacterial and fungal growth. For longer storage, consider proceeding with cryoprotection and freezing. [43]
3. Can I store my fixed mouse embryos in the sucrose solution used for cryoprotection? While embryos must be incubated in sucrose (e.g., 30%) for cryoprotection, you should not store them in this solution for extended periods. Do not exceed one week of storage in sucrose at 4°C, as this can promote microbial growth and degradation of your proteins of interest. For long-term storage, freeze the prepared tissue blocks or cryosections at -20°C or -80°C. [43]
4. My antibody signal is weak after storing my chick embryos. What could have happened? Weak signal can result from epitope degradation during storage. Ensure that the embryos were thoroughly washed after fixation to remove all PFA residues before storage. Also, verify that your storage temperature is consistent and that the embryos were not subjected to multiple freeze-thaw cycles if they were frozen. For some antigens, the fixation method itself (e.g., PFA vs. TCA) can impact accessibility [5].
5. Is it possible to store embryos after a whole-mount nuclear stain for later imaging? Yes, one advantage of whole-mount nuclear staining techniques is that they have minimal impact on the specimen. Embryos stained with dyes like DAPI and imaged in an aqueous buffer can subsequently be processed for paraffin or frozen sectioning and histological staining, making them available for multiple assays. [44]
Troubleshooting Guides
Problem: Poor Tissue Morphology After Storage
| Possible Cause | Solution | Applicable Model Organisms |
|---|---|---|
| Incomplete or uneven fixation | Ensure fixation is performed on a gentle shaker for homogeneity. Always use fresh PFA. | Zebrafish, Mouse, Chick [43] |
| Microbial contamination during storage | Add 0.1% sodium azide to aqueous storage buffers (e.g., PBS). Avoid long-term storage in sucrose solutions. | Zebrafish, Mouse, Chick [43] |
| Improper cryoprotection before freezing | Infiltrate tissue thoroughly with 30% sucrose until the tissue sinks before embedding and freezing. | Zebrafish, Mouse, Chick [43] |
| Freezer burn or dehydration | Ensure tissue blocks or samples are well-sealed in optimal cutting temperature (OCT) compound or storage containers to prevent air exposure. | Zebrafish, Mouse, Chick |
Problem: Loss of Antigenicity (Weak or No Antibody Signal) After Storage
| Possible Cause | Solution | Applicable Model Organisms |
|---|---|---|
| Over-fixation | Standardize fixation time and temperature. For zebrafish, test lighter fixation (e.g., 1% PFA) if deyolking is required [45]. For chicken embryos, 20 mins-1 hour at room temperature may be sufficient [46]. | All, but specific timing varies [43] [46] [45] |
| Protein degradation during storage | For fixed samples stored in PBS at 4°C, do not exceed 2 weeks. For long-term storage, use -20°C or -80°C. | Zebrafish, Mouse, Chick [43] |
| Epitope masking by cross-linking | If using PFA, consider optimizing an antigen retrieval step before immunostaining. For whole-mount samples, this can be done by heating in sodium citrate (pH 6) or Tris-HCl (pH 9) buffer [43]. | All |
| Incompatible fixative for the target epitope | If PFA gives poor results, validate an alternative fixative like methanol or Trichloroacetic Acid (TCA). TCA can be particularly effective for some cytoskeletal and membrane proteins [5] [15]. | All, studied in Chick [5] |
Embryo Storage Parameters Table
The following table summarizes key storage parameters for fixed embryos of different model organisms based on experimental goals.
| Organism | Fixation Protocol (for Storage) | Short-Term Storage (Post-Fixation) | Long-Term Storage (Processed Samples) | Special Considerations |
|---|---|---|---|---|
| Zebrafish | 4% PFA, overnight at 4°C on gentle shaker [43]. For deyolking protocols: 1% PFA, 2h at RT or overnight at 4°C [45]. | PBS + 0.1% Sodium Azide at 4°C for up to 2 weeks [43]. | Cryosections or tissue blocks at -20°C or -80°C [43]. De-yolked embryos can be stored in methanol at -20°C [45]. | Permeabilization is critical. For whole-mount, detergent concentration may be increased to 1% [43]. The yolk can hinder imaging and storage; deyolking is an option [45]. |
| Chick | 4% PFA for 20 minutes to 1 hour at room temperature [46]. | In PBS or PBT (PBS with Triton) at 4°C. | Similar to mouse and zebrafish; embedded blocks or sections at -80°C. | For whole-mount, embryos older than ~6 days are too large for effective reagent penetration and should be dissected [15]. |
| Mouse | 4% PFA, time varies with embryo size (e.g., 1-2 hours for E9.5 to overnight for E15.5). | PBS at 4°C. | Cryosections or tissue blocks at -20°C or -80°C. | Nuclear stain penetration in whole mounts is effective through E15.5; skin maturation thereafter reduces permeability [44]. |
Experimental Workflow: From Fixation to Storage
The diagram below outlines the core decision-making process for handling and storing fixed embryos to ensure sample quality for future immunofluorescence analysis.
Fixation Method Decision Guide
Choosing the correct fixative is a critical first step that influences all subsequent storage and staining outcomes. The following diagram helps guide this decision based on the target protein's localization.
Research Reagent Solutions
This table lists essential reagents for the fixation and storage of embryos, along with their primary functions.
| Reagent | Function in Protocol | Key Considerations |
|---|---|---|
| Paraformaldehyde (PFA) | Cross-linking fixative that preserves tissue architecture by creating stable bonds between proteins. | Use freshly prepared or freshly thawed aliquots. Avoid multiple freeze-thaw cycles. Standard concentration is 4% [43]. |
| Trichloroacetic Acid (TCA) | Precipitating fixative that denatures and aggregates proteins via acid-induced coagulation. | Can provide better access to some epitopes hidden by PFA cross-linking, especially for cytoskeletal proteins [5]. |
| Sucrose | Cryoprotectant that displaces water in tissues to prevent ice crystal formation during freezing. | Incubate until tissue sinks (often overnight). Do not store tissues in sucrose for >1 week to prevent degradation [43]. |
| Sodium Azide | Antimicrobial agent that inhibits bacterial and fungal growth in aqueous storage buffers. | Use at 0.1% concentration in PBS for short-term storage of fixed samples at 4°C [43]. Handle with care as it is toxic. |
| Triton X-100 or Tween-20 | Detergent used for permeabilization of cell membranes to allow antibody penetration. | For thick whole-mount samples like retina, concentration may be increased to 1% for better penetration [43]. |
| Donkey Serum or BSA | Component of blocking buffer to reduce non-specific antibody binding. | Used at 1-10% in PBS with detergent. Serum should match the species in which the secondary antibody was raised [15] [46]. |
For researchers storing fixed embryos for whole mount immunofluorescence, implementing rigorous quality control (QC) checkpoints is crucial for experimental success. A quality control plan provides a documented framework of specific procedures and standards to ensure consistent and reliable results [47]. Within this framework, visual inspection and pre-staining assessments serve as fundamental, non-destructive testing methods to identify issues before they compromise your data [48] [49]. This guide provides targeted troubleshooting and FAQs to help you maintain the integrity of your fixed embryo samples from storage through to staining.
Troubleshooting Guides & FAQs
Pre-Staining Visual Inspection of Fixed Embryos
User Issue: "How do I know if my fixed embryos are still healthy for staining after storage?"
A systematic visual inspection of fixed embryos before proceeding to staining is the first critical defense against experimental failure.
Inspection Procedure:
- Environment Setup: Use a dissection microscope in a clean, well-lit area. Ensure proper lighting (500-1000 lux is often recommended for visual tasks) and a dark background to enhance contrast and visibility of the embryos [49] [50].
- Direct Visual Inspection: Examine the embryos with the naked eye or using magnifying tools for any obvious signs of degradation [48].
- Documentation: Record the appearance of the embryos, including any noted issues, using a standardized checklist to maintain consistency and track sample quality over time [47] [50].
Common Defects & Corrective Actions:
Observed Issue Potential Cause Corrective Action Embryos appear shrunken or crumpled Over-fixation or improper storage solution [51]. For future samples, reduce fixation time. For current samples, proceed with caution as antigenicity may be reduced. Embryos are discolored (brown/yellow) Oxidation or bacterial/fungal contamination during storage. Discard the sample. Ensure fixed embryos are stored in adequate PBS at 4°C and that equipment is sterile [52]. Embryos are fragmented Physical damage during dissection or handling post-fixation. Use gentle pipetting with wide-bore tips. Fixed embryos can be sticky; using PBT (PBS with Triton X-100) during washes can help reduce sticking [53]. Precipitates or crystals on surface Salt precipitation from evaporation of storage buffer. Ensure samples are fully submerged in PBS during storage. Rinse embryos thoroughly with fresh PBS before proceeding [51].
Troubleshooting Weak or No Staining
User Issue: "I followed the protocol, but my signal is weak or non-existent."
This is a common challenge often rooted in sample preparation, antibody handling, or staining conditions.
- Systematic Troubleshooting Table:
Potential Cause Investigation & Solution Inadequate Permeabilization The antibody cannot access intracellular targets. Solution: Increase incubation time with permeabilization agent (e.g., ice-cold methanol or Triton X-100) or increase the detergent concentration in the permeabilization buffer [53] [51]. Antigen Masking from Fixation Over-fixation can cross-link and hide epitopes. Solution: Reduce fixation time or perform an antigen retrieval step. For example, incubate samples in a pre-heated antigen retrieval buffer (e.g., 100 mM Tris, 5% urea, pH 9.5) at 95°C for 10 minutes [51]. Inactive Antibodies Antibodies may have degraded due to improper storage or repeated freeze-thaw cycles. Solution: Aliquot antibodies and store at -20°C or below. Use a new batch or run a positive control to verify antibody activity [51] [54]. Low Antigen Abundance The target protein is not present or is in very low amounts. Solution: Increase sensitivity by increasing primary antibody concentration or incubation time (e.g., overnight at 4°C). Consider using signal amplification systems like tyramide (TSA) [51] [54]. Improper Blocking Non-specific sites are not effectively blocked, leading to high background that obscures signal. Solution: Increase blocking time (up to 1 hour) or change the blocking agent. Common blockers include 1-5% BSA or 10% normal serum from the host species of the secondary antibody [51] [54].
Addressing High Background and Non-Specific Staining
User Issue: "My staining has so much background noise that I can't distinguish the specific signal."
High background often stems from non-specific interactions between the antibodies and the sample.
- Systematic Troubleshooting Table:
Potential Cause Investigation & Solution Insufficient Washing Unbound antibodies or fixative remains in the sample. Solution: Wash samples at least 3 times with PBT (PBS with 0.1% Triton X-100) between steps, with gentle agitation for 1 hour per wash [53] [54]. Ineffective Blocking Non-specific binding sites are not saturated. Solution: Extend the blocking incubation period and consider using a different blocking agent, such as a combination of normal serum and BSA [51] [54]. Antibody Concentration Too High The antibody is binding non-specifically. Solution: Titrate the primary and secondary antibodies to find the optimal dilution. Incubating for longer periods with a more dilute antibody can sometimes improve the signal-to-noise ratio [54]. Secondary Antibody Cross-Reactivity The secondary antibody binds non-specifically to the sample. Solution: Always run a secondary-only control (no primary antibody). Use secondary antibodies that are pre-adsorbed against the serum proteins of your sample species [51] [54]. Autofluorescence from Aldehyde Fixatives Residual aldehyde groups can cause background glow. Solution: After fixation and washing, treat samples with a fresh 1% sodium borohydride (NaBH4) solution in PBS to reduce these groups [51].
The Scientist's Toolkit: Research Reagent Solutions
The following reagents are essential for successful whole mount immunofluorescence and its associated quality control. Proper preparation and understanding of their function are key.
| Reagent / Solution | Function & Rationale |
|---|---|
| Phosphate-Buffered Saline (PBS) | An isotonic, pH-balanced salt solution used for washing tissues and as a base for other solutions. It maintains osmotic balance to prevent damage to the embryos [53] [52]. |
| 4% Paraformaldehyde (PFA) | A cross-linking fixative that preserves tissue architecture and immobilizes antigens by creating chemical bonds between proteins. Fixation time and temperature should be optimized for your specific antigen [53] [52]. |
| PBT (PBS + 0.1% Triton X-100) | A standard wash and dilution buffer. Triton X-100 is a non-ionic detergent that permeabilizes cell membranes, allowing antibodies to enter, and helps reduce stickiness of fixed embryos [53] [52]. |
| Blocking Buffer | A solution containing a protein or serum (e.g., 1-5% BSA or 10% normal serum) used to occupy non-specific binding sites on the tissue, thereby reducing background staining [53] [52] [54]. |
| Antigen Retrieval Buffer | A solution (e.g., 100 mM Tris, 5% Urea, pH 9.5) used to break cross-links formed by aldehyde fixation, thereby "unmasking" epitopes and restoring antibody binding. Typically used with heat [51]. |
| Antifade Mounting Medium | A medium containing agents like n-Propyl gallate that retards photobleaching of fluorescent signals. It is used to mount samples under a coverslip for microscopy preservation [52]. |
Quality Control Workflow Diagram
The diagram below outlines the key quality control checkpoints in the whole mount immunofluorescence process, from embryo collection to imaging, highlighting the critical pre-staining assessment phase.
Solving Storage-Related Staining Problems: Autofluorescence, Signal Loss and Background Issues
Core Concepts: Understanding Storage-Induced Autofluorescence
What is autofluorescence and why does it increase with storage? Autofluorescence is the non-specific, background fluorescence emitted naturally by biological tissues or induced by chemical processes. It is a significant source of noise in fluorescence microscopy, as its broad emission spectrum can obscure the specific signal from fluorescent reporters like antibodies [55] [56] [57]. During storage of fixed embryos, autofluorescence can intensify due to the formation of irreversible fluorescent complexes, particularly from aldehyde-based fixatives like paraformaldehyde. Over time, these fixatives form fluorescent Schiff bases, and this fluorescence can be further exacerbated by the oxidation of molecules like lipofuscin and flavins within the tissue [55] [56] [58].
What are the common endogenous sources of autofluorescence in stored embryos? In fixed embryonic tissue, the key contributors to autofluorescence are:
- Red Blood Cells (RBCs): Hemoglobin in RBCs fluoresces across multiple wavelengths, interfering with many common fluorescent reporters. This is a major challenge in non-perfused embryonic tissue [55].
- Lipofuscin: This granular pigment accumulates in lysosomes and is highly fluorescent across multiple wavelengths. Its presence can increase with cell age or stress [55].
- Extracellular Matrix Components: Collagen and elastin are naturally fluorescent [56].
- Flavins and NADH: These cellular metabolites are intrinsic fluorophores [56].
How can I quickly confirm that the signal I'm seeing is autofluorescence? Run an unstained control. By imaging a fixed embryo that has not been treated with any fluorescent antibodies or probes, you can directly observe the level and pattern of background autofluorescence. This control is essential for diagnosing the problem and setting a baseline for background subtraction in image analysis software [56].
Troubleshooting Guide & FAQs
Frequently Asked Questions (FAQs)
Q1: My fixed embryo autofluorescence is too high after long-term storage. What is the first thing I should check? The first and most critical step is to review your fixation and storage conditions. Aldehyde-based fixatives are a primary cause of storage-induced autofluorescence. Ensure you are using high-purity reagents, that fixation times are not excessively long, and that fixed samples are stored in the dark at 4°C or -20°C to slow down oxidative processes that enhance background [56] [55].
Q2: Can I perform antigen retrieval on stored whole-mount embryos to reduce autofluorescence? Generally, no. Standard heat-induced antigen retrieval methods used on paraffin sections are typically not feasible for fragile whole-mount embryos, as the heating process can destroy the sample's structural integrity [15]. Focus instead on chemical quenching or computational methods detailed below.
Q3: I am multiplexing. Will the autofluorescence quencher affect my far-red channel signal? This depends on the quencher. Traditional Sudan Black B is known to increase background fluorescence at high red wavelengths, which could interfere with far-red signals. In contrast, TrueBlack Lipofuscin Autofluorescence Quencher has been reported to work efficiently across red and green wavelengths without introducing background staining, making it more suitable for multiplexing experiments [55].
Troubleshooting Flowchart
The following diagram outlines a logical pathway for diagnosing and addressing storage-induced autofluorescence.
Quantitative Data & Reagent Solutions
Comparison of Autofluorescence Quenching Reagents
The table below summarizes key chemical agents used to quench autofluorescence in fixed tissues.
| Reagent Name | Mechanism of Action | Effective Against | Key Advantages | Key Limitations/Disadvantages |
|---|---|---|---|---|
| TrueBlack Lipofuscin Autofluorescence Quencher [55] | Lipophilic dye that binds to autofluorescent pigments like lipofuscin. | Red blood cells, lipofuscin across red and green wavelengths. | Efficient quenching; Does not mask antibody signal; Can be reused; Low background staining. | Commercial reagent (cost). |
| Sudan Black B [55] [59] | Lipophilic dye that binds to lipofuscin granules. | Lipofuscin. | Widely used, established protocol. | Can introduce background fluorescence at high red wavelengths; May not efficiently quench RBC autofluorescence. |
| Sodium Borohydride [55] [56] | Reduces fluorescent Schiff bases formed by aldehyde fixation. | Aldehyde-induced autofluorescence. | Targets a primary cause of storage-induced fluorescence. | Can be caustic; May damage tissue integrity; Can reduce specific antibody signal. |
| Ammonium Ethanol [56] | Not fully specified in literature, but used as a bleaching agent. | Broad-spectrum autofluorescence. | Can attenuate autofluorescence signals. | May require careful optimization. |
The Researcher's Toolkit: Key Reagents for Quenching
- TrueBlack Lipofuscin Autofluorescence Quencher (Biotium #23007): A ready-to-use alternative to Sudan Black B for effectively quenching red blood cell and lipofuscin autofluorescence without compromising signal intensity [55].
- Sudan Black B: A traditional, cost-effective dye for reducing lipofuscin-type autofluorescence. Must be prepared in 70% ethanol [59].
- Sodium Borohydride (NaBH₄): A reducing agent used to treat aldehyde-induced fluorescence specifically. Use with caution as it can damage tissue [55] [56].
- Alexa Fluor, Dylight, or Atto Dyes: Modern, bright, and stable fluorophores with narrow emission bands. Choosing far-red variants helps avoid the common blue-green autofluorescence spectrum [56].
Detailed Experimental Protocols
Protocol 1: Quenching with TrueBlack Lipofuscin Autofluorescence Quencher
This protocol is adapted for fixed whole-mount embryonic tissue and is based on a method proven to quench red blood cell autofluorescence effectively [55].
Materials:
- Fixed whole-mount embryos.
- 20X TrueBlack Lipofuscin Autofluorescence Quencher in DMF (Biotium, Cat# 23007).
- Phosphate-Buffered Saline (PBS).
- Staining boxes or plates.
Method:
- After immunofluorescence staining and final PBS washes, prepare a working solution of 1X TrueBlack by diluting the 20X stock in PBS.
- Incubate the stained embryos in the TrueBlack solution for 30 seconds to 2 minutes. Note: Longer incubations (e.g., 5-30 minutes) may be used for thicker tissues, but optimization is required [55].
- Wash the embryos thoroughly twice with PBS to remove any residual quencher.
- Proceed to clearing, mounting, or imaging. The quenched samples can be stored in the dark at 4°C.
Technical Notes:
- The TrueBlack solution can be reused for multiple staining sessions [55].
- This method is compatible with various mounting media, including Vectashield with DAPI [55].
Protocol 2: Quenching with Sudan Black B
A standard protocol for reducing lipofuscin autofluorescence, commonly used in tissue sections and applicable to whole-mount samples with extended incubation [59].
Materials:
- Fixed whole-mount embryos.
- Sudan Black B powder.
- 70% ethanol.
Method:
- Prepare a 0.1% Sudan Black B solution in 70% ethanol. Filter if necessary.
- Incubate the embryos in the Sudan Black B solution for 20 minutes at room temperature.
- Rinse the embryos thoroughly with PBS until no more color leaches from the tissue.
- Continue with subsequent imaging steps.
Protocol 3: Computational Removal Using a Moving Median Filter
For super-resolution techniques like STORM, where autofluorescence appears as a constant background, a moving median filter can effectively separate the specific signal. This method is highly effective for highly autofluorescent cells like lung macrophages [58].
Principle: In single-molecule localization microscopy (SMLM), true signal appears as stochastic blinking events, while storage-induced autofluorescence is relatively stable over time. The moving median filter identifies and subtracts this constant background [58].
Workflow:
- Acquire STORM Data: Collect a long sequence of frames (e.g., >9,000 frames) of the blinking fluorophores.
- Apply Moving Median Filter: Process the data with a filter that calculates the median pixel value across a rolling window of frames (e.g., 21 frames). This generates a background model.
- Subtract Background: Subtract the generated background model from each original frame in the sequence.
- Reconstruct Image: Proceed with standard STORM reconstruction algorithms on the background-corrected frames to obtain a clean, high-resolution image [58].
This correction technique allows for quantitative nanoscale analysis of membrane structures and extracellular secretions even in challenging, autofluorescent samples [58].
FAQs: Signal Attenuation in Fixed Embryos
Q1: What are the primary causes of weak or lost staining in stored fixed embryos for whole-mount immunofluorescence? Weak or lost staining typically stems from three main areas: inadequate tissue permeabilization preventing antibody access, autofluorescence masking specific signal, and epitope masking caused by the fixation process itself, particularly with cross-linking fixatives like PFA [60] [5]. For stored samples, improper fixation or storage conditions can exacerbate these issues over time.
Q2: How can I recover a signal that was lost after my embryos were in storage? Recovery often involves revisiting the permeabilization and antigen accessibility steps. Implementing a more robust detergent-based permeabilization protocol (e.g., using 0.5% saponin) can help [52]. Furthermore, switching to or including a acid-based fixation method like Trichloroacetic Acid (TCA) for future experiments can better expose certain epitopes that PFA cross-links may hide [5].
Q3: My background autofluorescence is overwhelming my specific signal. What can I do? A protocol called Oxidation-Mediated Autofluorescence Reduction (OMAR) can be applied. This photochemical bleaching method maximally suppresses tissue autofluorescence prior to staining, eliminating the need for digital post-processing to remove background and thereby enhancing the specific signal-to-noise ratio [60].
Q4: Does the choice of fixative genuinely affect the final signal strength? Yes, significantly. The fixative choice creates a fundamental trade-off between tissue preservation and antibody access. Paraformaldehyde (PFA) works by creating protein cross-links, which excellently preserve morphology but can bury epitopes. Trichloroacetic Acid (TCA) fixes by precipitating proteins, which can better expose some epitopes but may alter tissue morphology more [5]. The optimal fixative depends on your target protein.
Troubleshooting Guide: Quantitative Analysis of Common Issues
The table below summarizes the core problems and their evidence-based solutions, with quantitative data where available.
Table 1: Troubleshooting Weak or Lost Staining in Whole-Mount Immunofluorescence
| Problem | Primary Cause | Recommended Solution | Experimental Evidence |
|---|---|---|---|
| High Background Autofluorescence | Endogenous fluorophores in tissues [60] | OMAR (Oxidation-Mediated Autofluorescence Reduction): A photochemical bleaching step during sample preparation [60]. | Protocol provides "maximal suppression of autofluorescence," suitable for whole-mount RNA-FISH and immunofluorescence on mouse embryos [60]. |
| Weak Specific Signal | Inadequate tissue permeabilization; epitope masked by cross-linking [52] [5] | Optimized Permeabilization: Use 0.5% saponin in blocking buffer [52].Alternative Fixation: Use 2% TCA in PBS for 1-3 hours instead of PFA [5]. | Saponin-based buffer used for successful whole-mount immunofluorescence in mouse embryos [52]. TCA fixation altered fluorescence intensity and revealed protein domains inaccessible with PFA [5]. |
| Inconsistent Staining Between Experiments | Non-specific antibody binding; variable staining conditions [61] | Optimized Blocking: Use 1% BSA with species-appropriate serum in blocking buffer. Antibody Titration: Systematically titrate all antibodies for high-parameter assays [61]. | Judicious use of blocking reagents improves assay specificity and sensitivity by reducing non-specific binding in flow cytometry, a principle applicable to immunofluorescence [61]. |
Detailed Experimental Protocols for Signal Recovery
Protocol 1: Oxidation-Mediated Autofluorescence Reduction (OMAR)
This protocol is adapted for whole-mount samples following fixation and prior to immunostaining [60].
- Sample Preparation: After fixation and several washes in PBS, transfer embryos to a suitable dish for bleaching.
- OMAR Treatment: Expose the fixed samples to the OMAR photochemical bleaching solution as described. The process involves oxidation that minimizes endogenous fluorescence.
- Wash and Proceed: Thoroughly rinse the samples with PBS after bleaching. The samples are now ready for standard permeabilization and immunostaining protocols. This method has been validated to allow for high-quality 2D and 3D image analysis without digital background subtraction [60].
Protocol 2: Whole-Mount Immunofluorescence with Enhanced Permeabilization
This is a generalized protocol for cardiac crescent stage mouse embryos, highlighting key steps for robust staining [52].
- Fixation: Fix embryos with 4% Paraformaldehyde (PFA) in PBS for 1 hour at room temperature or overnight at 4°C.
- Permeabilization and Blocking: Remove PBS and incubate embryos in blocking buffer (0.5% saponin, 1% BSA in PBS) for at least 4 hours at room temperature. This critical step permeabilizes membranes and blocks non-specific binding.
- Primary Antibody Incubation: Incubate with primary antibody diluted in blocking buffer overnight at 4°C.
- Washing: Remove primary antibody and wash 3 times for 1 hour each with 0.1% Triton X-100 in PBS.
- Secondary Antibody Incubation: Incubate with fluorescent secondary antibody diluted in blocking buffer for 3 hours at room temperature or overnight at 4°C.
- Final Washes and Mounting: Wash 3 times for 1 hour each with 0.1% Triton X-100 in PBS. Counterstain with DAPI if desired, and mount in an anti-fade mounting medium for imaging [52].
Experimental Workflow and Fixative Mechanism Diagrams
Diagram 1: A systematic workflow for diagnosing and addressing common staining problems.
Diagram 2: A comparison of fixation mechanisms, highlighting the trade-offs between PFA and TCA [5].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Addressing Signal Attenuation
| Reagent | Function/Application | Example Usage in Protocol |
|---|---|---|
| Saponin | Detergent for permeabilizing cell membranes in fixed tissue. Preserves membrane structure better than Triton X-100 for some epitopes. | Used at 0.5% in blocking buffer for whole-mount immunofluorescence [52]. |
| Trichloroacetic Acid (TCA) | Acid-based fixative that precipitates proteins. Can expose epitopes that are masked by PFA cross-linking. | Used at 2% in PBS for 1-3 hours for fixing chicken embryos [5]. |
| Bovine Serum Albumin (BSA) | Blocking agent used to reduce non-specific binding of antibodies to the tissue. | Used at 1% in combination with serum in blocking buffers [52] [61]. |
| n-Propyl Gallate (nPG) | Anti-fade agent that reduces photobleaching of fluorescent signals during storage and microscopy. | Component of anti-fade mounting media (e.g., 2% w/v in glycerol/PBS) [52]. |
| OMAR Reagents | Chemical oxidizers for photochemical bleaching to reduce tissue autofluorescence. | Applied after fixation and before immunostaining on mouse embryonic limb buds [60]. |
FAQs and Troubleshooting Guide
Q1: After long-term storage, my fixed embryos show weak or no intracellular fluorescence signal. What should I check first?
Weak signal in archived samples often stems from inadequate permeabilization, which can be exacerbated by extended fixation or storage. We recommend the following checks and actions [62]:
- Review Your Permeabilization Reagent: The choice of detergent is critical. For nuclear or mitochondrial targets, Triton X-100 is effective, but it can dissolve membranes and is not ideal for preserving membrane-bound structures. For these, Saponin is a preferable alternative [63].
- Re-optimize Permeabilization Time and Concentration: The standard permeabilization duration may be insufficient for long-term fixed embryos. Consider increasing the incubation time or the concentration of the detergent [63].
- Confirm Antibody Compatibility: Ensure your primary and secondary antibodies are compatible and that the antibody has been validated for use on fixed, permeabilized samples in their native conformation [63].
- Check for Epitope Masking: Over-fixation can cross-link epitopes, making them inaccessible. You may need to use antigen retrieval methods or test a shorter fixation time on a new batch of samples [63].
Q2: I am getting high background staining in my archived embryo samples. How can I reduce it?
High background is frequently caused by non-specific antibody binding or incomplete washing. To resolve this [62] [63]:
- Titrate Your Antibodies: The optimal antibody concentration for fresh samples may be too high for archived samples. Perform a dilution series to find the concentration that maximizes signal-to-noise.
- Enhance Blocking: Increase the incubation time or the concentration of serum in your blocking buffer. Using the same serum host species as your secondary antibody can improve blocking efficiency.
- Increase Wash Stringency: Add more wash steps between antibody incubations. You can also increase the concentration of Tween in your PBS-T (e.g., from 0.1% to 0.2%) and include very gentle agitation during washes.
- Include a Secondary Antibody-Only Control: Perform your staining protocol without the primary antibody to determine if the background is originating from non-specific binding of your secondary antibody.
Q3: The morphology of my embryos appears damaged after the permeabilization step. What could be the cause?
Rapid immersion into a hypotonic permeabilization solution like methanol can damage cellular structures. To prevent this, always chill your cells (or embryos) on ice prior to adding ice-cold methanol and introduce the methanol drop-wise to the cell pellet while gently vortexing to ensure homogeneous permeabilization [62].
Quantitative Comparison of Permeabilization Agents
The table below summarizes key characteristics of common permeabilization agents to help you select the right one for your target and sample type [62] [63].
Table 1: Permeabilization Reagent Properties and Applications
| Permeabilization Agent | Mechanism of Action | Ideal For | Considerations for Archived Samples |
|---|---|---|---|
| Saponin | Forms pores in cholesterol-rich membranes, which are reversible. | Preserving membrane integrity; staining of membrane-bound organelles. | The reversible nature may require including saponin in antibody incubation buffers. Less disruptive for delicate morphologies. |
| Triton X-100 | Dissolves lipid membranes through surfactant action. | Strong, irreversible permeabilization; robust staining of nuclear and cytoplasmic targets. | Can over-permeabilize and damage subcellular structures. Overuse can increase background. |
| Methanol | Precipitates proteins and dissolves lipids (acts as a fixative and permeabilizer). | Staining of nuclear targets like transcription factors or for cell cycle analysis. | Can be harsh. Must be added drop-wise to ice-cold samples to prevent hypotonic shock and morphological damage [62]. |
| Tween-20 | Mild, non-ionic detergent. | Gentle washing and low-stringency permeabilization. | Often too mild for effective intracellular penetration in fixed, archived embryos. Best used as a wash buffer additive. |
Experimental Protocol: Optimized Permeabilization for Archived Embryos
This protocol is designed to systematically troubleshoot and optimize permeabilization for embryos that have been in long-term storage.
Materials Needed:
- Archived, fixed embryo samples
- Permeabilization buffer (e.g., PBS with 0.1-0.5% Triton X-100, or 0.1% Saponin)
- Blocking buffer (e.g., PBS with 1-5% BSA or serum from the secondary antibody host species)
- Primary and secondary antibodies
- Wash buffer (PBS with 0.1% Tween-20)
Methodology:
- Rehydration and Washing: Gently wash the archived embryos three times in PBS to remove any residual storage solution.
- Permeabilization Optimization Test: Divide your samples into several aliquots. Treat each aliquot with a different permeabilization condition. We recommend testing:
- Condition A: Standard protocol (e.g., 0.1% Triton X-100 for 15 minutes at room temperature).
- Condition B: Increased concentration (e.g., 0.3% Triton X-100 for 15 minutes).
- Condition C: Increased time (e.g., 0.1% Triton X-100 for 30 minutes).
- Condition D: Alternative reagent (e.g., 0.1% Saponin for 30 minutes, with Saponin included in all subsequent buffers).
- Blocking: Incubate all samples in blocking buffer for 1-2 hours at room temperature to reduce non-specific binding.
- Antibody Incubation: Incubate with primary antibody (diluted in blocking buffer) overnight at 4°C. The following day, wash the samples 3-5 times with wash buffer. Then, incubate with fluorophore-conjugated secondary antibody for 1-2 hours at room temperature, protected from light.
- Imaging and Analysis: After final washes, image the samples using a fluorescence microscope. Compare the signal intensity and background levels across the different permeabilization conditions to determine the optimal protocol.
The following workflow diagrams the logical process for diagnosing and resolving permeabilization issues:
Research Reagent Solutions
Table 2: Essential Materials for Permeabilization Optimization
| Item | Function | Example / Key Consideration |
|---|---|---|
| Triton X-100 | Non-ionic detergent for strong, irreversible permeabilization of lipid membranes. | Effective for robust intracellular staining, but can damage membrane structures [62]. |
| Saponin | Mild, cholesterol-specific detergent for reversible permeabilization. | Ideal for preserving membrane-bound organelles; must be included in all antibody buffers [63]. |
| Methanol | Acts as both a fixative and permeabilizing agent. | Must be ice-cold and added drop-wise while vortexing to prevent cell damage [62]. |
| Bovine Serum Albumin (BSA) | Blocking agent to reduce non-specific antibody binding. | Using 1-5% BSA in blocking and antibody buffers helps lower background [62] [63]. |
| Normal Serum | Blocking agent specific to the host species of the secondary antibody. | More effective than BSA for blocking; matches the secondary antibody species for best results [62]. |
| Tween-20 | Mild detergent used in wash buffers to reduce non-specific binding. | Critical for effective washing between steps to minimize background staining [63]. |
Mitigating Background Fluorescence and Non-Specific Binding in Long-Stored Specimens
Troubleshooting Guide: Common Issues and Solutions
Weak or No Specific Signal
- Problem: After storing fixed embryo samples, the expected fluorescent signal is faint or absent.
- Potential Causes and Solutions:
- Loss of Antigenicity: Prolonged storage, especially beyond recommended timeframes, can degrade the target epitopes.
- Solution: Use freshly prepared slides where possible. For long-term storage, validate the maximum storage duration for your specific antigen [64].
- Inadequate Fixation: Over-fixation can mask epitopes, while under-fixation leads to poor preservation.
- Antibody Concentration: The antibody may be too dilute.
- Fluorophore Bleaching: The fluorescent tag may have degraded due to light exposure.
- Loss of Antigenicity: Prolonged storage, especially beyond recommended timeframes, can degrade the target epitopes.
High Background Fluorescence
- Problem: The sample shows high levels of non-specific fluorescence, obscuring the specific signal.
- Potential Causes and Solutions:
- Autofluorescence: This is a common issue in fixed and long-stored tissues, caused by endogenous molecules like lipofuscin or aldehyde cross-links.
- Insufficient Blocking: Non-specific sites are available for antibody binding.
- Solution: Extend the blocking incubation time and use a robust blocking agent. A solution of 1-5% normal serum from the secondary antibody host species or 1-5% BSA is commonly effective [70].
- Antibody Concentration Too High: Excess antibody leads to non-specific binding.
- Incomplete Washing: Unbound antibodies and reagents remain in the sample.
Non-Specific Antibody Binding
- Problem: Antibodies bind to sites other than the intended target antigen.
- Potential Causes and Solutions:
- Fc Receptor Binding: Antibodies may bind to Fc receptors on immune cells via their Fc region.
- Non-viable Cells: Dead cells are "sticky" and prone to non-specific binding.
- Solution: Include a viability dye to exclude dead cells during analysis. Ensure tissue is fixed promptly after dissection [71].
- Charge or Hydrophobic Interactions: Antibodies can bind non-specifically via non-immunological forces.
Frequently Asked Questions (FAQs)
Q1: What is the best fixative for long-term storage of embryos for whole-mount immunofluorescence? A: Research indicates that a combination fixative of 0.4% glutaraldehyde and 4% formaldehyde in a suitable buffer provides a good balance. It offers excellent ultrastructural preservation for extended periods (up to two weeks for reliable fluorescence) while maintaining antigenicity better than glutaraldehyde alone [65] [66].
Q2: How long can I store fixed embryo samples before processing? A: The acceptable storage duration depends on the fixative and temperature. The table below summarizes findings from a controlled study on tissue storage:
| Fixative Solution | Storage Temperature | Max Duration for Reliable Fluorescence | Max Duration for Ultrastructure |
|---|---|---|---|
| 0.4% GA + 4% FA | 4°C | ~14 days [65] [66] | Several years [65] [66] |
| 4% Formaldehyde | 4°C | Data not specified | ~28 days [65] [66] |
| 1.5% Glutaraldehyde | 4°C | Not recommended | ~28 days [65] [66] |
GA: Glutaraldehyde; FA: Formaldehyde
Q3: My samples were stored for a very long time and now have high background. How can I salvage them? A: Samples stored for years often lose fluorescent labeling capacity and develop autofluorescence [65] [66]. You can try:
- Photobleaching: Irradiate the sample with a strong, broad-spectrum white LED light for 24-48 hours at 4°C in a buffered solution to bleach endogenous fluorophores [69].
- Chemical Quenching: Treat sections with Sudan Black B or similar reagents to suppress lipofuscin and aldehyde-induced autofluorescence [69] [68].
Q4: How can I prevent non-specific binding of my secondary antibody? A: Non-specific secondary antibody binding is a common cause of background.
- Optimize Concentration: Always titrate your secondary antibody. High concentrations are a primary cause of background [67].
- Use a Secondary-Only Control: Always run a control stained only with the secondary antibody to identify non-specific binding [68].
- Ensure Complete Blocking: Block with a protein-rich solution (e.g., BSA or serum) for a sufficient duration [70] [67].
Experimental Protocols for Mitigation
Protocol 1: Photobleaching to Reduce Autofluorescence
This protocol uses a white LED lamp to chemically bleach autofluorescence in fixed tissue sections before immunostaining [69].
- Construct the Apparatus: Use a desk lamp with a white phosphor LED. Remove any diffusers. Build a scaffold to hold a slide chamber (e.g., a 100 mm square petri dish) above the LED. Cover the setup with a reflective dome (e.g., a foil-lined box).
- Prepare Bleaching Solution: Prepare a solution of 0.05% sodium azide in Tris-buffered saline (TBS).
- Treat Sections: Place slide-mounted tissue sections in the chamber, submerge in the azide-TBS solution, and cover with the dome.
- Bleach: Turn on the LED lamp and incubate the sections for 48 hours at 4°C.
- Proceed with Staining: After bleaching, wash the slides with TBS and continue with your standard immunofluorescence protocol.
Protocol 2: Optimized Blocking and Antibody Incubation
A rigorous blocking and antibody incubation protocol is crucial for minimizing background in stored specimens.
- Blocking:
- After permeabilization and washing, incubate the sample in a blocking buffer for 2 hours at room temperature (or overnight at 4°C for enhanced blocking).
- Blocking Buffer Recommendation: 1-5% normal serum from the species of the secondary antibody, supplemented with 1% Bovine Serum Albumin (BSA) in PBS with a mild detergent (e.g., 0.025% Triton X-100) [70].
- Primary Antibody Incubation:
- Dilute the primary antibody in the same blocking buffer.
- Incubate at 4°C overnight for maximum specific binding and minimal background [64].
- Washing:
- Wash the sample thoroughly with PBS-Triton (or your chosen wash buffer) 3 times for 10 minutes each, followed by 3 washes for 1 hour each to remove all unbound antibody [46].
- Secondary Antibody Incubation:
- Use a fluorophore-conjugated secondary antibody, pre-centrifuged to remove aggregates.
- Dilute the secondary antibody in blocking buffer at the optimized concentration (determined by titration) and incubate for 2 hours at room temperature in the dark [68].
Visualization of Workflows
Experimental Strategy for Long-Term Storage
Key Mitigation Techniques Relationship
The Scientist's Toolkit: Research Reagent Solutions
| Reagent | Function/Benefit | Key Consideration |
|---|---|---|
| Aldehyde Mixture Fixative (0.4% Glutaraldehyde + 4% Formaldehyde) | Provides strong cross-linking for long-term ultrastructure preservation while maintaining some antigenicity for fluorescence [65] [66]. | Superior to glutaraldehyde alone for fluorescence applications in stored samples. |
| Bovine Serum Albumin (BSA) | A versatile blocking agent that competes for non-specific protein-binding sites on tissues and membranes [70]. | A fundamental component of most blocking and antibody dilution buffers. |
| Normal Serum | Contains antibodies that bind to non-specific sites, particularly effective at preventing secondary antibody cross-reactivity [70]. | Must be from the same species as the secondary antibody host. |
| Sodium Azide | A preservative used in photobleaching and storage buffers to inhibit microbial growth [69]. | Handle with care: Toxic. |
| Sudan Black B | A chemical dye that quenches lipofuscin and other endogenous autofluorescence [69] [68]. | Effective for reducing broad-spectrum autofluorescence in aged and fixed tissues. |
| Anti-Fade Mounting Medium | Preserves fluorophore signal by reducing photobleaching during microscopy and storage [64]. | Essential for imaging and for any samples that will not be imaged immediately. |
Rescue Protocols for Suboptimally Stored Historical Samples
This technical support center provides targeted troubleshooting guides for researchers working with fixed embryos for whole-mount immunofluorescence. A significant challenge in this field is managing historical samples that have been suboptimally stored, leading to degradation and poor experimental outcomes. The following FAQs and protocols offer evidence-based solutions to rescue these valuable specimens, ensuring their viability for critical research in developmental biology and drug discovery.
Frequently Asked Questions (FAQs)
Q1: What are the primary signs of degradation in historical fixed embryo samples? Historical samples often show DNA degradation through several mechanisms: oxidation (from heat or UV exposure), hydrolysis (water breaking DNA bonds), enzymatic breakdown (nuclease activity), and excessive DNA shearing from overly aggressive mechanical processing [72]. For immunofluorescence, this manifests as poor antibody binding, high background noise, and weak or absent specific signal.
Q2: My historical samples were stored at -80°C but experienced a thaw event. Can they be rescued? Yes, samples that underwent a thaw event can often be rescued, but the protocol depends on the extent of degradation. Begin by re-fixing the tissue with fresh 4% Paraformaldehyde (PFA) to re-stabilize protein epitopes [73]. Implement an enhanced antigen retrieval step, testing both acidic (sodium citrate, pH 6) and basic (Tris-HCl, pH 9) buffers to maximize antigen availability [73]. Increase permeabilization and blocking times to mitigate higher background.
Q3: For samples stored in inadequate fixative or for too long, what are the rescue options? Samples fixed for too long or in suboptimal fixatives can become over-crosslinked, masking antigenic sites. The key rescue strategy is robust antigen retrieval. We recommend a combination of heat-induced epitope retrieval (HIER) and a 20-minute treatment with ice-cold acetone at -20°C, which has been shown to drastically improve staining quality in challenging zebrafish tissues [73].
Q4: What is the most critical step when processing limited or irreplaceable historical samples? The most critical step is rigorous quality control before committing to a full protocol. For precious samples, always run a pilot test on a small subset or a single embryo. Use fragment analysis to assess DNA integrity and perform a test staining with a well-characterized antibody to evaluate protein preservation [72]. This prevents the irreversible loss of unique material.
Troubleshooting Guides
Problem 1: High Background and Non-Specific Staining
- Potential Cause: Inadequate blocking or non-specific antibody binding, often exacerbated by sample degradation.
- Solution:
- Optimize Blocking Solution: Increase the concentration of serum (e.g., to 10% goat serum) and add 1% Bovine Serum Albumin (BSA) [73].
- Increase Wash Stringency: Add a mild detergent like 0.1% Triton-X or Tween-20 to all wash buffers and increase wash frequency and duration [73]. For whole-mount samples, consider increasing detergent concentration to 1% [73].
- Titrate Antibodies: Re-titrate primary and secondary antibodies on a compromised sample, as degraded samples often require lower antibody concentrations than fresh tissue.
Problem 2: Weak or Absent Specific Signal
- Potential Cause: Antigen degradation or masking due to improper fixation and long-term storage.
- Solution:
- Systematic Antigen Retrieval: Test different antigen retrieval methods on a control sample. As a rule of thumb, compare sodium citrate (pH 6), Tris-HCl (pH 9), and no retrieval to identify the optimal condition for your specific antigen [73].
- Enhanced Permeabilization: For whole-mount embryos, extend permeabilization times and ensure the use of an effective detergent like Triton-X.
- Signal Amplification: Consider using a tyramide signal amplification (TSA) kit to enhance a weak signal, though this may compromise some spatial resolution.
Problem 3: Physical Damage and Loss of Morphology
- Potential Cause: Ice crystal formation from improper freezing or mechanical stress during handling.
- Solution:
- Cryoprotection: For frozen samples, ensure proper infiltration with 30% sucrose as a cryoprotectant before embedding and freezing. Avoid storing tissue in sucrose for longer than a week to prevent microbial growth [73].
- Gentle Handling: When applying solutions to slides, pipette liquid between sections, not directly onto them, as delicate larval sections can easily detach [73].
Experimental Rescue Protocols & Data
Protocol 1: Antigen Retrieval Optimization for Fixed Embryos
This protocol is critical for recovering signal from over-fixed or poorly stored samples [73].
- Deparaffinize and Rehydrate sections if needed.
- Antigen Retrieval Buffer: Choose either:
- Sodium citrate buffer (10 mM, pH 6.0)
- Tris-EDTA buffer (10 mM, pH 9.0)
- Heating: Place slides in buffer and heat using a water bath, steamer, or rice cooker at 70-95°C for 15-20 minutes.
- Cooling: Allow slides to cool in the buffer for 20-30 minutes at room temperature.
- Acetone Treatment (for whole-mount): Incubate samples in 100% ice-cold acetone at -20°C for 20 minutes. Wash extensively with PBST afterward [73].
- Proceed with standard immunofluorescence blocking and staining steps.
Protocol 2: Whole-Mount Immunostaining for Degraded Embryos
An optimized protocol for challenging whole-mount samples, such as zebrafish retinae [73].
- Fixation: Use fresh 4% PFA overnight at 4°C on a gentle shaker.
- Permeabilization: Wash and permeabilize with 1% PBST (PBS with 1% Triton-X-100) for extended periods (multiple hours to overnight).
- Blocking: Incubate in blocking solution (10% serum, 1% BSA, 0.1% Triton-X) for at least 2 hours at room temperature on a shaker.
- Antibody Incubation: Incubate with primary antibody in blocking solution for at least 48 hours at 4°C. For secondary antibodies, incubate for 2 hours at room temperature, protected from light.
- Washing: Perform extensive washes with 0.1% PBST (3-5 times, 20-60 minutes each) after each antibody step.
Table 1: Comparison of Antigen Retrieval Methods for Suboptimal Samples
| Method | Buffer | Best For | Pros | Cons |
|---|---|---|---|---|
| Heat-Induced (HIER) | Sodium Citrate, pH 6.0 | Most common epitopes | Widely used, effective for many targets | May not work for all antibodies |
| Heat-Induced (HIER) | Tris-EDTA, pH 9.0 | More resistant epitopes | Can retrieve targets citrate cannot | Higher pH can damage some tissues |
| Proteolytic (Enzyme) | Trypsin or Proteinase K | Formalin-fixed, paraffin-embedded | Can break cross-links | Can easily destroy morphology and antigens if overdone |
| Solvent-Based | Ice-cold Acetone | Whole-mount samples, membrane proteins | Drastically improves penetration in thick tissues [73] | Requires post-treatment washing |
Workflow Visualization
The following diagram outlines the logical decision-making process for rescuing suboptimal samples.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Rescuing Historical Samples
| Reagent / Material | Function | Application Note |
|---|---|---|
| Paraformaldehyde (PFA) | Protein cross-linking fixative | Always use fresh 4% PFA for initial fixation or re-fixation steps [73]. |
| Triton-X-100 / Tween-20 | Detergent for permeabilization | Critical for antibody penetration. Use 0.1-1.0% concentration; higher for whole-mount [73]. |
| Goat Serum & BSA | Blocking agents | Reduces non-specific antibody binding. Use 10% serum + 1% BSA in blocking buffer [73]. |
| Sucrose | Cryoprotectant | Prevents ice crystal damage in frozen samples. Use 30% solution for infiltration [73]. |
| Sodium Citrate / Tris-EDTA | Antigen retrieval buffers | Unmask hidden epitopes. Test both pH 6 and pH 9 for optimal results [73]. |
| Acetone | Solvent for permeabilization | Effective for whole-mount samples; use ice-cold at -20°C for 20 mins [73]. |
| DNA Preservation Polymers | Room-temperature DNA storage | Emerging technology for stabilizing nucleic acids in degraded samples, eliminating cold chain failures [74]. |
Ensuring Reproducibility: Validation Methods and Comparative Analysis of Storage Techniques
This technical support center provides troubleshooting guides and FAQs for researchers validating storage protocols for fixed embryos used in whole-mount immunofluorescence.
Troubleshooting Guides & FAQs
Issue: High Background Fluorescence After Storage
- Q: After retrieving my fixed embryos from long-term storage, I am experiencing high, non-specific background fluorescence. What could be the cause?
- A: High background is often linked to incomplete washing or inadequate blocking. Ensure embryos are washed thoroughly after fixation and after incubation with the primary and secondary antibodies to remove unbound reagents. Verify that your blocking solution is fresh and that you are using the correct serum. Additionally, consider testing different fixation methods, as some (like TCA) can alter fluorescence intensity and background [5].
Issue: Loss of Antigenicity (Weak or No Signal)
- Q: My stained embryos show a very weak signal, even with antibodies that have worked previously. Could my storage solution be degrading my samples?
- A: Yes, this is a common issue. The primary culprits are often the storage temperature and the composition of the storage buffer. Fixed samples stored long-term should be kept at 4°C in a buffered solution with a preservative like 0.01% sodium azide to prevent microbial growth. Furthermore, the choice of fixative itself can impact long-term antigen preservation. Some epitopes are better preserved with PFA fixation, while others may be more accessible with TCA fixation [5]. Re-optimizing your fixation protocol for your specific target antigen may be necessary.
Issue: Poor Tissue Morphology and Preservation
- Q: The tissue architecture of my stored embryos appears damaged or shrunken. How can I improve morphological preservation?
- A: This typically points to a problem with the initial fixation or post-fixation handling. Ensure the fixation time is optimized for your embryo size and stage; over-fixation can make tissues brittle. The osmolarity and pH of your fixation and storage buffers are also critical. Always use freshly prepared fixative, as old PFA can degrade and become acidic, damaging tissues [5]. For some tissues, alternative fixatives like glyoxal can offer superior morphology preservation [75].
Issue: Inconsistent Staining Across Batches
- Q: I am getting inconsistent staining results between different batches of embryos stored using the same protocol. What should I investigate?
- A: Inconsistency can stem from genetic variability in your model organism or slight variations in sample handling. When using zebrafish, for example, remember that laboratory strains are genetically heterogeneous [76]. To control for this, ensure your experimental design includes adequate sample sizes and, if possible, use embryos from the same clutch for direct comparisons. Meticulous documentation of fixation times, storage durations, and reagent lot numbers is essential for identifying the source of variation.
Experimental Protocols & Data
Comparison of Fixation Methods for Long-Term Storage
The choice of fixative fundamentally impacts tissue morphology and antigen preservation, which is critical for storage validity. The table below summarizes key findings from a comparison of Paraformaldehyde (PFA) and Trichloroacetic Acid (TCA) fixation [5].
| Parameter | PFA Fixation | TCA Fixation |
|---|---|---|
| Primary Mechanism | Protein cross-linking [5] | Protein denaturation and precipitation [5] |
| Nuclear Morphology | Standard size and shape [5] | Larger, more circular nuclei [5] |
| Optimal For | Nuclear transcription factors (e.g., SOX9, PAX7); general use [5] | Cytoskeletal (e.g., Tubulin) and membrane proteins (e.g., Cadherin) [5] |
| Impact on Fluorescence | Adequate signal strength for proteins in nucleus, cytoplasm, and membrane [5] | Can alter fluorescence intensity and reveal hidden protein domains [5] |
| Typical Fixation Time | 20 minutes (for chicken embryos) [5] | 1-3 hours (for chicken embryos) [5] |
Detailed Protocol: Validating Storage with PFA-fixed Embryos
This protocol is adapted from whole-mount immunofluorescence procedures for adult zebrafish spinal cord and chicken embryos [77] [5].
Fixation:
- Dissect embryos and immediately place into freshly prepared 4% Paraformaldehyde (PFA) in 0.2M Phosphate Buffer.
- Fix at room temperature for 20 minutes to 1 hour, with gentle agitation. Note: Duration depends on embryo size and stage.
- Wash embryos 3 x 10 minutes in 1X PBS with 0.1% Triton X-100 (PBST) to remove all PFA.
Long-Term Storage:
- Transfer embryos to 1X PBS containing 0.01% sodium azide to inhibit microbial growth.
- Store at 4°C. For best practices, document the storage date and buffer composition.
Immunofluorescence Staining (Post-Storage Validation):
- Blocking: Incubate embryos in PBST containing 10% normal donkey serum (or serum matching your secondary antibody) for 1 hour at room temperature or overnight at 4°C [5].
- Primary Antibody: Incubate with primary antibody diluted in blocking solution for 48-72 hours at 4°C with agitation [77].
- Washing: Wash embryos 4-6 times over 12-24 hours with PBST to reduce background [77].
- Secondary Antibody: Incubate with fluorescently-labeled secondary antibody (e.g., AlexaFluor conjugates) diluted in blocking solution for 24 hours at 4°C, protected from light [78].
- Final Wash: Perform extensive final washes in PBST (e.g., 6 x 1 hour) before imaging [77].
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Solution | Function & Rationale |
|---|---|
| Paraformaldehyde (PFA) | A cross-linking fixative that preserves tissue architecture by creating covalent bonds between proteins. Ideal for general morphology and many nuclear antigens [5]. |
| Trichloroacetic Acid (TCA) | A precipitating fixative that denatures proteins. Can be superior for preserving certain cytoskeletal and membrane protein epitopes that are cross-linked and hidden by PFA [5]. |
| Glyoxal | An alternative dialdehyde fixative that cross-links tissues faster than formaldehyde and may retain higher antigenicity for some targets. Considered less hazardous [75]. |
| Triton X-100 | A non-ionic detergent used in washing and blocking buffers (e.g., PBST) to permeabilize cell membranes, allowing antibodies to access intracellular epitopes [5]. |
| Donkey Serum | Used as a blocking agent to bind to non-specific sites and prevent non-specific binding of antibodies, thereby reducing background fluorescence [5]. |
| Sodium Azide | A preservative added to storage and antibody buffers (typically at 0.01-0.02%) to prevent bacterial and fungal growth during long-term storage at 4°C [5]. |
Workflow Diagrams
Storage Protocol Validation Workflow
Troubleshooting Logic Flow
The table below summarizes quantitative data on the performance of different mounting and clearing media for deep imaging of fixed embryo samples, based on empirical measurements.
| Storage/Mounting Medium | Key Performance Metrics | Quantitative Improvement Over PBS | Best Use Case |
|---|---|---|---|
| 80% Glycerol [79] | 3-fold reduction in intensity decay at 100 µm; 8-fold reduction at 200 µm [79]. 1.5x and 3x improvement in information content (FRC-QE) at 100 µm and 200 µm, respectively [79]. | High | Optimal clearing for immunostained gastruloids; enables reliable cell detection up to 200 µm depth [79]. |
| Scale S4 Solution [80] | Provides tissue clearing and refractive index matching for light-sheet imaging [80]. Contains D-sorbitol, urea, glycerol, Triton X-100, and DMSO [80]. | Not specified | Recommended clearing/immersion solution for whole-mount zebrafish spinal cords and similar tissues [80]. |
| ProLong Gold Antifade [79] | Performance inferior to 80% Glycerol in reducing signal intensity decay with depth [79]. | Low | General antifade mounting; less effective for deep imaging in dense tissues [79]. |
| Optiprep [79] | Live-cell compatible; performance inferior to 80% Glycerol for reducing signal decay [79]. | Low | Situations requiring compatibility with live samples, but with compromised clearing [79]. |
The Scientist's Toolkit: Essential Research Reagents
This table details key reagents used in protocols for storing and preparing fixed embryos for whole-mount immunofluorescence.
| Reagent | Function | Protocol Example & Specification |
|---|---|---|
| Paraformaldehyde (PFA) [15] | Fixative; preserves tissue architecture and antigenicity by cross-linking proteins [15]. | Typically used at 4% concentration; incubation from 30 min at room temperature to overnight at 4°C [15]. |
| Triton X-100 [80] [81] [15] | Detergent; permeabilizes cell membranes to allow antibody penetration into the tissue [15]. | Used in various concentrations (e.g., 0.1% - 1%) in wash and blocking buffers [80] [81]. |
| Bovine Serum Albumin (BSA) [80] [15] | Blocking agent; reduces non-specific antibody binding to minimize background signal [15]. | Used in blocking buffers, often at 1% (w/v) concentration [80]. |
| Dimethyl Sulfoxide (DMSO) [80] | Penetration enhancer; helps facilitate the penetration of antibodies and other reagents into thick tissues [80]. | Included in washing and clearing solutions (e.g., Scale S4) for whole-mount samples [80]. |
| Glycerol [79] [80] | Clearing agent and mounting medium; reduces light scattering by matching the refractive index of the tissue [79]. | Used at high concentrations (e.g., 80%) for effective clearing and as a component of Scale solutions [79] [80]. |
| DAPI [80] [15] | Nuclear counterstain; fluorescent dye that binds to DNA to label all nuclei in the sample [15]. | Added during mounting to visualize nuclear location and density [80]. |
Experimental Protocols: Key Methodologies
Protocol 1: Whole-Mount Sample Preparation, Clearing, and Imaging for Spinal Cord
This protocol is adapted for adult zebrafish spinal cords and outlines a robust method for storage, clearing, and imaging [80].
- Fixation: Fix dissected samples in 4% Paraformaldehyde (PFA) at room temperature [80].
- Washing and Blocking: Wash samples with a solution of 1X PBS containing DMSO and Triton X-100. Subsequently, block using a buffer such as PBS with 1% BSA, 0.2% non-fat dry milk powder, and 0.3% Triton X-100 [80].
- Antibody Incubation: Incubate with primary antibody diluted in blocking buffer overnight at 4°C with gentle rocking. Follow with extensive washing and incubation with fluorescent-conjugated secondary antibodies [80].
- Clearing and Storage for Imaging: Clear samples using Scale S4 solution (containing urea, D-sorbitol, glycerol, Triton X-100, and DMSO). The cleared samples can be stored in this solution and are ready for imaging via light-sheet or confocal microscopy [80].
Protocol 2: Whole-Mount Immunofluorescence for Cultured Embryonic Tissues
This protocol is designed for mouse embryonic tissues, such as Wolffian ducts, cultured ex vivo [81].
- Fixation: Fix cultured tissues with 4% PFA overnight at 4°C or for 1 hour at room temperature [81].
- Permeabilization and Dehydration: Wash tissues with PBS-T (PBS + 1% Triton X-100). Dehydrate through a graded ethanol series (25%, 50%, 75%, 100%), then rehydrate through a reverse series. This step enhances antibody penetration [81].
- Blocking and Staining: Block tissues for 1 hour at room temperature. Incubate with primary antibody diluted in blocking buffer overnight at 4°C [81].
- Post-Staining Storage and Imaging: After staining and final washes, samples can be stored in mounting media or buffer for imaging. For 3D visualization, image using confocal microscopy [81].
Troubleshooting Guides and FAQs
Q1: My antibody signal is weak in the deep regions of my fixed embryo sample. What can I optimize? A1: Weak deep-tissue signal is often related to inadequate clearing or antibody penetration.
- Optimize Clearing: Test different clearing media. Empirical data shows 80% Glycerol can significantly reduce signal decay (3-fold at 100 µm) compared to PBS or other media like ProLong Gold [79].
- Enhance Permeabilization: Ensure your protocol includes a permeabilization step with detergents like Triton X-100 (e.g., 0.3-1%) in all wash and blocking buffers [81] [15].
- Extend Incubation Times: For whole-mount samples, incubations with antibodies and washing steps need to be much longer than for sections to allow for diffusion into the center of the sample [15].
Q2: What is the recommended maximum size or age for embryos to be successfully processed with whole-mount immunofluorescence? A2: The feasibility of whole-mount staining depends on tissue permeability.
- General Guidelines: For untreated whole embryos, chicken embryos are typically manageable up to 6 days, and mouse embryos up to 12 days [15].
- For Larger Samples: If working with larger tissues (e.g., late-stage embryos or organoids), dissection into smaller segments may be necessary for effective antibody penetration [79] [15]. Removing surrounding dense tissue, like muscle and skin, can also facilitate staining [15].
Q3: How long can fixed samples be stored before staining, and what are the best conditions? A3: Proper fixation is key to long-term storage.
- Short-Term: Fixed samples can be stored in PBS or 75% ethanol at 4°C for a period before proceeding with staining [81].
- Long-Term: For extended storage, fixed samples should be kept at -20°C to preserve antigenicity. Ensure samples are protected from drying out [15].
Workflow Diagram: Fixed Embryo Storage & Processing
The diagram below outlines the key decision points and steps in a generalized workflow for storing and processing fixed embryos for whole-mount immunofluorescence.
We hope this technical support center provides valuable guidance for your research. For specific antibody-related issues, always refer to the manufacturer's datasheet for validated protocols.
Leveraging Automated Imaging and Analysis for Objective Storage Quality Assessment
For researchers conducting whole-mount immunofluorescence on fixed embryos, preserving specimen integrity throughout storage is paramount to experimental success and data reliability. The quality of fixed embryo storage directly impacts key experimental outcomes, including antigen preservation, structural integrity, and reduction of storage-induced autofluorescence. Traditional quality assessment methods rely on subjective visual inspection, which introduces variability and potential bias. This technical support center outlines how automated imaging and analysis technologies provide objective, quantitative, and standardized assessment of fixed embryo storage quality. By implementing these approaches, researchers can establish robust quality control benchmarks, troubleshoot storage issues systematically, and ensure the consistency required for high-impact publications and drug development applications.
Automated imaging systems, including quantitative phase imaging and computational specificity techniques, now enable non-destructive measurement of intrinsic biomarkers that correlate with embryo viability and structural preservation. These label-free methods are particularly valuable for long-term storage monitoring as they avoid additional processing or damage to precious samples. Furthermore, machine learning algorithms can integrate multiple quantitative parameters to generate standardized health assessments, eliminating inter-observer variability and establishing objective quality metrics for fixed embryo repositories [82].
Technical Foundations: Imaging Principles for Quality Assessment
Core Imaging Technologies
Table 1: Automated Imaging Modalities for Fixed Embryo Quality Assessment
| Imaging Technology | Primary Applications in Quality Assessment | Key Advantages | Technical Requirements |
|---|---|---|---|
| Quantitative Phase Imaging (QPI) | Dry mass measurement, structural integrity assessment [82] | Label-free, non-destructive; quantitative structural data | Specialized optical systems (e.g., GLIM modules); phase reconstruction software |
| Artificial Confocal Microscopy (ACM) | Computational specificity, subcellular feature prediction [82] | No physical staining required; confocal-quality data from phase images | Laser-scanning system; trained deep learning models |
| Fluorescence Microscopy | Antigen preservation verification, autofluorescence quantification [60] | Direct visualization of epitope integrity; standard in most core facilities | Appropriate filter sets; sensitive detectors |
| Brightfield/Time-Lapse Imaging | Morphological assessment, documentation of degradation [83] | Widely accessible; minimal sample preparation | Basic microscope with camera; time-lapse capability |
Quantitative Biomarkers for Storage Quality
Table 2: Objective Biomarkers for Fixed Embryo Storage Quality
| Biomarker Category | Specific Measurable Parameters | Correlation with Storage Quality | Measurement Technique |
|---|---|---|---|
| Structural Integrity | Nuclear shape descriptors, embryo volume, cell boundary clarity [82] | Poor preservation shows nuclear fragmentation, membrane blebbing | ACM, QPI with segmentation |
| Compositional Integrity | Dry mass density, protein concentration distribution [82] | Protein aggregation indicates degradation; uniform distribution indicates good preservation | QPI dry mass calculation |
| Autofluorescence | Background intensity, signal-to-noise ratio [60] | Increased autofluorescence suggests improper fixation or storage conditions | OMAR protocol with fluorescence imaging |
| Morphological Consistency | Size uniformity across batches, shape descriptors | High variability indicates inconsistent processing or storage | Automated morphological analysis |
Troubleshooting Guides: Addressing Common Storage Quality Issues
FAQ 1: How can I objectively monitor fixed embryo degradation during long-term storage without destructive sampling?
Issue: Researchers need non-destructive methods to monitor fixed embryo quality over extended storage periods without consuming valuable samples.
Solution: Implement quantitative phase imaging (QPI) for routine quality control checks. QPI techniques like Gradient Light Interference Microscopy (GLIM) measure optical phase delays to calculate dry mass and dry mass density - intrinsic biomarkers that reflect overall macromolecular integrity. These measurements are particularly valuable because they:
- Require no labels or additional processing, preserving specimens for future experiments
- Provide quantitative data on protein density and distribution within the embryo
- Detect subtle changes in structural integrity before they become visually apparent
- Generate objective metrics that can be tracked over time to establish storage stability profiles [82]
Protocol for QPI-Based Quality Monitoring:
- At predetermined intervals (e.g., monthly, quarterly), remove a representative subset of stored embryos from storage conditions
- Image embryos using QPI system with consistent settings (magnification, resolution)
- Calculate whole-embryo dry mass and dry mass density using established formulas based on optical phase measurements
- Segment individual nuclei to extract nuclear shape descriptors and dry mass distribution
- Compare values to baseline measurements taken immediately after fixation
- Document any significant deviations (>15% from baseline) as potential indicators of degradation [82]
FAQ 2: What automated approach can reduce subjectivity when assessing fixed embryo quality across multiple research personnel?
Issue: Multiple laboratory personnel assessing embryo quality introduces inter-observer variability, compromising experimental consistency.
Solution: Deploy machine learning-assisted classification systems that standardize quality assessment across users and time. The EVATOM (Embryo Viability Assessment Tool) framework demonstrates how machine learning can classify embryo health based on quantitative features, achieving high reproducibility (weighted F1 scores of 0.9-0.95 in validation studies) [82].
Implementation Workflow:
- Feature Extraction: Utilize automated image analysis to extract quantitative features from embryo images:
- Nuclear count and spatial distribution
- Nuclear volume and sphericity
- Dry mass distribution uniformity
- Texture features indicating structural preservation
Model Training: Train a classifier on expert-annotated embryos representing "optimal," "acceptable," and "compromised" storage outcomes
Validation: Establish ground truth through correlation with experimental outcomes like immunofluorescence success rates
Deployment: Implement the trained model for standardized quality scoring of all stored embryos [82]
FAQ 3: How can I minimize storage-induced autofluorescence that interferes with whole-mount immunofluorescence signals?
Issue: Autofluorescence that develops during storage masks specific immunofluorescence signals and increases background noise.
Solution: Implement the Oxidation-Mediated Autofluorescence Reduction (OMAR) protocol, which uses photochemical bleaching to suppress tissue autofluorescence before proceeding with immunofluorescence staining. This method is particularly effective for stored embryos as it addresses autofluorescence that develops over time during storage [60].
OMAR Protocol for Fixed Embryos:
- Reagent Preparation:
- Prepare freshly diluted hydrogen peroxide (concentration optimized for embryo type)
- Prepare appropriate buffer (e.g., PBS, 0.1M Tris-HCl) at correct pH
Bleaching Process:
- Transfer fixed embryos to OMAR working solution
- Expose to bright light source (LED or fluorescent lamp) for optimized duration
- Monitor autofluorescence reduction with control samples
Post-Treatment Processing:
- Rinse thoroughly with buffer to remove residual hydrogen peroxide
- Proceed with standard immunofluorescence protocol [60]
Critical Optimization Parameters:
- Hydrogen peroxide concentration (typically 0.5-5%)
- Buffer composition and pH
- Light source intensity and spectral characteristics
- Treatment duration (balance between autofluorescence reduction and epitope preservation)
FAQ 4: How do I establish quantitative acceptance criteria for fixed embryo quality before proceeding with expensive immunofluorescence experiments?
Issue: Researchers need objective thresholds to determine when stored embryos remain suitable for experiments.
Solution: Develop laboratory-specific quality benchmarks based on correlation between quantitative imaging parameters and experimental success rates.
Benchmark Establishment Protocol:
- Baseline Characterization: Image embryos immediately after fixation and processing to establish reference values for:
- Nuclear count and distribution
- Dry mass values and distribution
- Background autofluorescence intensity
Performance Tracking: Record immunofluorescence outcomes for each embryo, including:
- Signal-to-noise ratio for target antigens
- Non-specific background staining
- Structural preservation in final images
Correlation Analysis: Statistically relate initial quality metrics to experimental outcomes to determine predictive thresholds
Threshold Implementation: Establish go/no-go criteria such as:
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Fixed Embryo Quality Assessment and Storage
| Reagent/Category | Primary Function in Quality Assessment | Application Notes | Quality Control Parameters |
|---|---|---|---|
| OMAR Solutions [60] | Suppression of storage-induced autofluorescence | Hydrogen peroxide-based; concentration must be optimized for embryo type | Fresh preparation required; efficacy verification with control samples |
| Mounting Media with Anti-fade Agents | Preservation of signal during imaging and storage | Compatible with whole-mount specimens; various refractive indices | pH stability; hardening properties; fluorescence compatibility |
| Proteinase K & Antigen Retrieval Reagents | Epitope exposure for validation staining | Concentration and timing critical for embryo integrity | Titration required for each fixation protocol; batch-to-batch consistency |
| Validation Antibodies | Positive control for antigen preservation | Housekeeping proteins; structural markers | Specificity validation; consistent lot performance |
| Blocking Buffers | Reduction of non-specific background | Protein-based (BSA, serum) or commercial formulations | Optimization for autofluorescence reduction; compatibility with detection systems |
| Nuclear Stains | Structural integrity assessment | DAPI, Hoechst, SYTOX dyes; concentration titration | Signal intensity; photostability; compatibility with fixation |
Advanced Implementation: Integrated Quality Assessment Workflow
For comprehensive quality management, implement an integrated pipeline that combines multiple assessment technologies. This approach leverages the complementary strengths of different imaging modalities to create a robust quality assessment system:
Workflow Integration Protocol:
- Baseline Assessment: Within 24 hours of fixation, perform comprehensive imaging using QPI, brightfield, and fluorescence microscopy to establish reference values for all quality parameters
Structured Storage Monitoring: Implement a scheduled assessment protocol where representative samples are periodically evaluated using rapid QPI scans, with full assessment reserved for when changes are detected
Multi-parameter Scoring System: Develop a weighted quality score that incorporates:
- Structural integrity metrics (40% weight)
- Compositional consistency (30% weight)
- Autofluorescence levels (20% weight)
- Morphological stability (10% weight)
Decision Tree Implementation: Establish clear protocols for different quality classifications:
This integrated approach enables researchers to objectively track storage quality, make data-driven decisions about experimental use of stored embryos, and systematically identify storage condition issues before they compromise entire sample collections.
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary cause of high background fluorescence in stored fixed embryos, and how can it be mitigated? High background, or autofluorescence, in stored fixed embryos often results from the fixative itself or from prolonged storage. Old aldehyde-based fixatives, particularly glutaraldehyde, are known to induce high autofluorescence [84] [85] [3]. To mitigate this, use fresh formaldehyde stocks and prepare fresh dilutions for fixation [84] [3]. For samples already fixed, a photochemical bleaching technique like Oxidation-Mediated Autofluorescence Reduction (OMAR) can be applied to suppress autofluorescence without the need for digital post-processing [60].
FAQ 2: How does the choice of fixative impact the long-term storage and antigenicity of embryos for whole-mount studies? The fixative choice is critical for preserving both morphology and antigenicity during storage. Paraformaldehyde (PFA) is a common crosslinking fixative that preserves structure but can mask epitopes over time, especially with prolonged fixation [86] [85]. Methanol, a precipitating fixative, is a good alternative for some antigens sensitive to PFA cross-linking and can help with permeabilization [86] [15]. A study on neutrophil extracellular traps (NETs) found that fixation with 100% methanol resulted in visible cellular damage, while PFA fixation for 24 hours decreased the signal intensity for certain markers, recommending a 15–30 minute PFA fixation for optimal results [85].
FAQ 3: What are the recommended storage conditions for fixed embryos prior to whole-mount staining? After fixation and dehydration, embryos can be stored long-term in 100% methanol at -20°C for up to eight months or longer [87]. This method is frequently used in whole-mount in situ hybridization protocols to preserve samples. For shorter-term storage, fixed samples can be kept in phosphate-buffered saline (PBS) at 4°C [15] [87].
FAQ 4: Why might my stained embryo show weak or no signal, and how is this related to sample storage? Weak or no signal can stem from over-fixation and epitope masking due to extensive cross-linking from aldehydes like PFA, especially if fixation occurs over long periods [84] [88] [3]. This can be exacerbated during storage. Additionally, inadequate permeabilization during the staining protocol can prevent antibody access to internal antigens, a step that is even more critical in thick whole-mount samples [84] [15] [88]. Signal may also fade if fluorophores are exposed to light during storage or processing; therefore, samples should be stored and incubated in the dark [84].
Troubleshooting Guides
Troubleshooting Storage and Staining Issues
Table 1: Common issues linking storage conditions to staining reproducibility.
| Problem | Potential Cause Linked to Storage | Recommended Solution | Expected Outcome |
|---|---|---|---|
| High Background Autofluorescence | Use of glutaraldehyde or old, oxidized formaldehyde fixatives [84] [85]. | Use fresh PFA; avoid glutaraldehyde; treat samples with OMAR photochemical bleaching or 0.1% sodium borohydride [60] [84] [88]. | Clean background, reducing the need for image post-processing and improving publication quality [60]. |
| Weak or No Specific Signal | Over-fixation (too long in PFA) leading to epitope masking; degradation of antigens during improper storage [84] [85] [3]. | Optimize fixation time (e.g., 15-30 min for cells [85]); store fixed samples in methanol at -20°C; validate antibody on a positive control [15] [87] [3]. | Strong, specific signal with a high signal-to-noise ratio, allowing for clear interpretation of results. |
| Non-Specific Staining & High Background | Insufficient blocking of non-specific binding sites due to rushed protocol after storage; cross-reactivity of secondary antibodies [84] [3]. | Extend blocking time (at least 2.5 hours); use serum from the secondary antibody host; include controls to check for secondary antibody cross-reactivity [84] [87] [3]. | Clean, specific staining with minimal non-specific background, ensuring data reliability. |
| Physical Damage to Embryos | Freezing artifacts from snap-freezing without adequate cryoprotection; damage during long-term storage in methanol if not properly handled. | For frozen sections, embed in OCT compound before snap-freezing [86] [89]. Handle stored embryos gently during washing steps. | Preservation of intact tissue morphology and architecture, which is crucial for 3D analysis. |
Experimental Protocol: Validating Fixation and Storage Conditions
To ensure staining reproducibility, systematically validate your fixation and storage pipeline using the following protocol.
Aim: To determine the optimal fixation time and storage condition for preserving antigenicity of a specific target in mouse embryos for whole-mount immunofluorescence.
Materials:
- Mouse embryos (E10.5-E12.5 recommended) [15]
- 4% Paraformaldehyde (PFA) in PBS (freshly prepared from PFA powder or from frozen aliquots of a stock solution) [86] [90]
- Phosphate-Buffered Saline (PBS)
- 100% Methanol
- Permeabilization buffer (e.g., PBS with 0.1% Triton X-100)
- Blocking buffer (e.g., PBS with 1% BSA, 5% normal serum, and 0.05% Tween-20) [87] [90]
- Primary antibody and fluorescently conjugated secondary antibody, validated for whole-mount staining [15]
- Mounting medium with anti-fade agent [84]
Methodology:
- Fixation Time Course: Collect mouse embryos and divide them into groups. Fix all groups in 4% PFA at 4°C with gentle agitation. Use different fixation times for each group (e.g., 30 minutes, 2 hours, overnight).
- Post-Fixation Processing: After fixation, wash embryos 3 times in PBS for 5 minutes each.
- Storage Conditions: For each fixation time group, subdivide embryos into two storage conditions:
- Condition A: Dehydrate in a methanol series (25%, 50%, 75% in PBS) and store in 100% methanol at -20°C [87].
- Condition B: Store in PBS at 4°C.
- Staining: After a predetermined storage period (e.g., 1 week, 1 month), process all samples for whole-mount immunofluorescence simultaneously using an identical protocol [15]. This includes:
- Rehydration (for methanol-stored samples) through a reverse methanol series.
- Permeabilization.
- Blocking.
- Incubation with primary antibody.
- Washing.
- Incubation with secondary antibody.
- Final washing.
- Imaging and Analysis: Mount all embryos and image using consistent microscope settings (e.g., laser power, gain, exposure time) [84]. Quantify the signal-to-noise ratio for each condition.
Table 2: Key research reagents for whole-mount embryo staining and storage.
| Reagent / Material | Function / Explanation |
|---|---|
| Paraformaldehyde (PFA) | A cross-linking fixative that preserves tissue architecture and antigenicity by creating methylene bridges between proteins [86]. |
| Methanol | A precipitating fixative and storage medium; denatures proteins and can be used as an alternative to PFA for some antigens. Also permeabilizes cells [86] [15]. |
| Triton X-100 | A non-ionic detergent used in permeabilization buffers to dissolve cellular membranes, allowing antibodies to access intracellular targets [88] [90]. |
| Bovine Serum Albumin (BSA) / Normal Serum | Used in blocking buffers to adsorb to and "block" non-specific binding sites on the tissue, thereby reducing background staining [87] [90]. |
| Sodium Borohydride | A chemical reducing agent that can quench free aldehyde groups from PFA/glutaraldehyde fixation, reducing autofluorescence [88]. |
| Anti-fade Mounting Medium | Preserves fluorescence by reducing photobleaching during microscopy and storage, crucial for publication-quality images [84]. |
Workflow and Relationship Diagrams
The following diagram illustrates the critical decision points and their impacts on staining quality within a standard workflow for processing fixed embryos.
Benchmarking Against Fresh Tissue Standards and Establishing Acceptance Criteria
For researchers using whole mount immunofluorescence (WMIF) to study embryonic development, the fixation and storage of samples are critical steps that directly impact data quality and reproducibility. Properly benchmarking stored fixed embryos against fresh tissue standards ensures that antigenicity and morphology are preserved, enabling accurate biological interpretation. This guide provides essential troubleshooting and methodological support for establishing robust acceptance criteria for your fixed embryo repository.
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: What are the primary factors that cause degradation of immunofluorescence signal in stored fixed embryos? A: The primary factors include the choice of fixative, storage buffer composition, storage temperature, and fixation duration. In particular, the fixation method significantly impacts tissue morphology and the visualization of proteins and mRNA [91] [23]. Inadequate fixation or storage can lead to increased autofluorescence, antigen degradation, and morphological artifacts, making benchmarks against fresh tissue essential.
Q: Why should I benchmark my fixed samples against fresh tissue, and what are the key acceptance criteria? A: Benchmarking is the only way to verify that your storage protocol does not introduce analytical artifacts. Key acceptance criteria should include [91] [23] [92]:
- Nuclear and Tissue Morphology: Nuclei and tissue structures (e.g., neural tubes) should show consistent size, shape, and architecture without swelling or shrinkage.
- Fluorescence Signal Intensity: Signal intensity for your target antigens should be comparable, with a high signal-to-noise ratio.
- Antigen Preservation: The ability to detect a range of antigen types (e.g., transcription factors, cytoskeletal proteins) should be maintained.
- Background Levels: Background fluorescence and non-specific staining should be low and consistent.
Q: A common problem is high background fluorescence. How can I resolve this? A: High background often stems from incomplete washing, non-specific antibody binding, or residual fixative. To resolve this [26]:
- Increase Washing: Implement more frequent and longer washes with a specialized IF-Wash buffer (containing Triton X-100 and Tween-20) after fixation and after each antibody incubation step.
- Optimize Blocking: Use a blocking solution containing 0.1-1% Bovine Serum Albumin (BSA) and 5-10% normal serum from the host species of your secondary antibody.
- Check Fixative: Ensure unreacted paraformaldehyde (PFA) is quenched with a PBS-glycine solution after fixation [26].
Q: My antibody worked on fresh tissue but gives a weak or no signal on stored fixed embryos. What should I do? A: This indicates potential antigen masking or degradation. You can [91] [23]:
- Retrieve Antigens: Perform an antigen retrieval step. This often involves heating the sample in a citrate-based or EDTA-based buffer, even for whole mounts.
- Re-validate Antibodies: The staining efficacy can be highly dependent on the fixation method. An antibody validated for PFA-fixed samples may not work for TCA-fixed samples and vice versa [91].
- Check Storage Conditions: Ensure samples are stored in an appropriate, pH-buffered solution at 4°C to slow degradation.
Troubleshooting Common Experimental Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Weak or No Signal | Antigen degradation during storage; antibody incompatibility with fixative; insufficient permeabilization. | Re-optimize fixation and storage duration; validate antibody for your specific fixative [91]; increase detergent concentration (e.g., Triton X-100) in wash buffer [26]. |
| High Background Noise | Incomplete washing; non-specific antibody binding; residual fixative. | Increase wash frequency/duration; optimize blocking serum concentration; use a glycine wash to quench PFA [26]. |
| Poor Morphology (Swollen/Shrunken Tissues) | Osmolarity imbalance in fixation or storage buffers; over-fixation. | Prepare fresh fixative with correct pH and osmolarity; avoid prolonged fixation times; benchmark against fresh tissue [92]. |
| Inconsistent Staining Between Batches | Variable fixation or storage times; slight differences in buffer preparation. | Establish and strictly adhere to Standard Operating Procedures (SOPs) for all steps; use freshly prepared buffers. |
Experimental Protocols and Benchmarking Data
Detailed Protocol: Whole-Mount Immunofluorescence for Fixed Embryos
The following protocol is adapted for gel-embedded or fragile embryonic samples, focusing on preserving morphology [26].
1. Sample Fixation and Washing
- Fixation: Immerse samples in pre-warmed 2-4% Paraformaldehyde (PFA) for 15-60 minutes at room temperature. Critical: PFA is toxic; use under a fume hood. [26]
- Washing: Remove PFA and wash samples 2-3 times with a pre-warmed PBS-Glycine solution to quench unreacted aldehyde groups. Follow with several washes with a pre-warmed IF-Wash Buffer (1X PBS, 0.1% BSA, 0.1% Triton X-100, 0.05% Tween-20, 0.0048% NaN₃) to permeabilize the tissue and reduce background [26].
2. Blocking and Antibody Incubation
- Blocking: Incubate samples in IF-Wash Buffer supplemented with 5-10% normal serum for 2-4 hours at room temperature or overnight at 4°C.
- Primary Antibody: Incubate with the primary antibody diluted in IF-Wash Buffer for 24-48 hours at 4°C with gentle agitation.
- Washing: Wash samples 3-5 times over 6-8 hours with IF-Wash Buffer to remove unbound antibody.
- Secondary Antibody: Incubate with fluorophore-conjugated secondary antibody (diluted in IF-Wash Buffer) for 24 hours at 4°C, protected from light.
3. Mounting and Imaging
- Final Washes: Perform extensive washing with IF-Wash Buffer, then PBS.
- Mounting: Mount samples using a clearing solution like fructose-glycerol to improve transparency and preserve fluorescence signals. For long-term storage, seal samples well and store at 4°C in the dark [26].
Quantitative Benchmarking: Fixative Impact on Signal Quality
The choice of fixative is a major variable. The table below summarizes a comparative analysis of Paraformaldehyde (PFA) and Trichloroacetic Acid (TCA) fixation in avian embryos, providing a model for your benchmarking studies [91] [23].
Table 1: Comparative Analysis of PFA vs. TCA Fixation for Embryonic Tissues
| Parameter | PFA Fixation | TCA Fixation | Implication for Benchmarking |
|---|---|---|---|
| Nuclear Morphology | Standard size and shape | Larger, more circular nuclei | TCA alters baseline morphology; not suitable for morphometric studies. |
| mRNA Detection (HCR) | Effective | Ineffective | PFA is mandatory for in situ hybridization or mRNA detection. |
| Protein Detection (IHC) | Effective for most targets | Alters intensity; can reveal proteins inaccessible to PFA | TCA may enhance signal for certain proteins (e.g., cadherins, tubulin) [91] [23]. |
| Tissue Architecture | Preserved standard anatomy | Altered neural tube shape | PFA is superior for preserving gross tissue architecture. |
Establishing Numerical Acceptance Criteria
When benchmarking your stored samples, define quantitative thresholds for acceptance. The following table suggests metrics based on imaging analysis.
Table 2: Proposed Acceptance Criteria for Fixed Embryo Storage Quality
| Benchmarking Metric | Measurement Method | Acceptance Criterion (Example) |
|---|---|---|
| Signal-to-Noise Ratio (SNR) | (Mean signal intensity - Mean background intensity) / Standard deviation of background. | SNR ≥ 5 for key target antigens. |
| Nuclear Size & Circularity | Segmentation and measurement of DAPI-stained nuclei (e.g., using Mesmer, Cellpose [93]). | Deviation < 10% from fresh tissue control. |
| Antigen Intensity Preservation | Mean fluorescence intensity of a stable reference antigen (e.g., Tubulin). | Intensity ≥ 80% of fresh tissue control. |
| Background Fluorescence Level | Mean intensity in a non-stained region of the embryo. | Intensity ≤ 2x the level of fresh tissue control. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Whole-Mount Immunofluorescence of Fixed Embryos
| Reagent / Material | Function | Example / Note |
|---|---|---|
| Paraformaldehyde (PFA) | Crosslinking fixative that preserves tissue architecture and antigenicity. | Typically used at 2-4% in PBS. The gold-standard for combined morphology and mRNA detection [91] [26]. |
| Trichloroacetic Acid (TCA) | Precipitating fixative. | Can enhance protein signal for some targets (e.g., cadherins) but is unsuitable for mRNA studies [91] [23]. |
| IF-Wash Buffer | Permeabilizes membranes, reduces non-specific binding, and preserves sample during washes. | Contains Triton X-100, Tween-20, and BSA. Sodium Azide (NaN₃) is added to prevent microbial growth [26]. |
| PBS-Glycine Solution | Quenches unreacted aldehyde groups from PFA fixation to reduce background fluorescence. | A critical step after PFA fixation [26]. |
| Fructose-Glycerol Clearing Solution | Mounting medium that reduces light scattering, improving image clarity and depth penetration. | Used as an alternative to commercial mounting media for better transparency [26]. |
| Normal Serum | Blocks non-specific binding sites to minimize background. | Should be from the species in which the secondary antibody was raised. |
| DAPI (4′,6-diamidino-2-phenylindole) | Nuclear counterstain. | Allows for segmentation and analysis of nuclear morphology [93]. |
Experimental and Analytical Workflows
Diagram 1: Fixation and Storage Benchmarking Workflow
Diagram 2: Nuclear Segmentation Analysis Pathway
Conclusion
Proper storage of fixed embryos is not merely a preliminary step but a critical determinant of success in whole-mount immunofluorescence. This synthesis demonstrates that meticulous attention to storage conditions—including fixation quality, storage duration, temperature control, and appropriate buffers—directly preserves epitope integrity, minimizes autofluorescence, and ensures experimental reproducibility. The integration of robust validation methods and troubleshooting protocols provides researchers with a framework for maintaining specimen quality across diverse experimental timelines. As imaging technologies advance toward higher multiplexing and quantification, standardized, optimized storage practices will become increasingly vital for generating reliable data in developmental biology, disease modeling, and drug development applications. Future directions should focus on establishing universal quality metrics for stored specimens and developing novel preservation technologies that further enhance antigen stability for long-term archival.
References
- 1. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOopiJ9Yto0_D9bx2XxXNL_o0a2zA8SyFeRQygNEBjqJvptN9syJS]
- 2. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOoqqlxWdyAdjYLmB3ChrFvx87YvNLhrNNgvxQjbmt6u_bd1FIAly]
- 3. Troubleshooting - Immunofluorescence Assays [https://ibidi.com/content/366--troubleshooting]
- 4. Effects of Fixation and Tissue Processing on ... [https://www.leicabiosystems.com/us/knowledge-pathway/effects-of-fixation-and-tissue-processing-on-immunocytochemistry/]
- 5. Effectiveness of fixation methods for wholemount ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10996528/]
- 6. Appropriate Fixation of IHC/ICC Samples [https://www.rndsystems.com/resources/protocols/appropriate-fixation-ihcicc-samples]
- 7. Reflections on the Principles of Fixation in Histochemistry and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173635/]
- 8. A powerful and versatile new fixation protocol for ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-024-02052-3]
- 9. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOootTZh2voPyB-un5mCeBI8dfZBY9yvHa-jsgUV8qB7Lt64eqLsn]
- 10. 9 Tips to optimize your IF experiments [https://www.ptglab.com/news/blog/9-tips-to-optimize-your-if-experiments/?srsltid=AfmBOorvtViBgQYxJ2cJ_6lhHMWc9xMPxejgeELFtjJEAHQSrOgFwg50]
- 11. Mouse on mouse (MOM) staining protocol [https://www.abcam.com/en-us/technical-resources/protocols/mouse-on-mouse-staining]
- 12. How to optimize culture media osmolality during Assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10065773/]
- 13. Factors of the human embryo culture system that may affect ... [https://pubmed.ncbi.nlm.nih.gov/33458748/]
- 14. Biological pH buffers in IVF: help or hindrance to success - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3170115/]
- 15. IHC staining protocol for whole mount samples [https://www.abcam.com/en-us/technical-resources/protocols/wholemount-staining-for-ihc]
- 16. Fixation and storage of embryos and fry for whole-mount in ... [https://kingsley.stanford.edu/Lab%20Protocols-WEB%202003/Fish%20Methods/Fixation.htm]
- 17. Embryo Fixation [https://people.biology.ucsd.edu/davek/fixation.html]
- 18. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoqH4kdUn1uED-UUKb7vqcFQeAFmXi5PblqgsVuWLBUb16vtEGPy]
- 19. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 20. Effects of Long-Term Storage on the Detection of Proteins, DNA, and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3283084/]
- 21. IHC antigen retrieval protocol | Abcam [https://www.abcam.cn/technical-resources/protocols/ihc-antigen-retrieval]
- 22. Immunofluorescence techniques in zebrafish retina [https://www.ptglab.com/news/blog/immunofluorescence-techniques-in-zebrafish-retina/?srsltid=AfmBOoqKRod27ygu6rVLR30B8uTj_Jq_NjIZPZpkTR2MPZWAMBUf9lg5]
- 23. Comparative analysis of fixation techniques for signal ... [https://www.sciencedirect.com/science/article/pii/S0012160624002276]
- 24. Protocol for immunofluorescence detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12156156/]
- 25. Protocol for immunofluorescence staining of murine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10322902/]
- 26. Protocol for whole-mount immunofluorescence staining of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11227007/]
- 27. Fixation Protocols | Comparative Pathology Research Core [https://medicine.yale.edu/compmed/mrp/fixationprotocols/]
- 28. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOooqC6mUodFuWuh9oxhnTBDyS-LHsI3OXUdmRmqKaRmSMcfRKg7K]
- 29. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOopqQFPuNGLLFTlMs78cMzvracBqbOaBpvc4iFOZ9zubME3z5Wlo]
- 30. Troubleshooting Guide: Immunohistochemistry [https://www.rndsystems.com/resources/technical/troubleshooting-guide-immunohistochemistry]
- 31. Fixation Methods and Perfusion Solutions [https://www.neuroscienceassociates.com/fixation-method/]
- 32. Frozen Tissue Preparation & IHC Cryosection Staining ... [https://www.rndsystems.com/resources/protocols/protocol-preparation-and-fluorescent-ihc-staining-frozen-tissue-sections]
- 33. Neural Organoid Cryopreservation and Immunofluorescence [https://www.stemcell.com/cerebral-organoid-cryosectioning-immunofluorescence.html]
- 34. Protocol Guide: Immunofluorescent Staining of Whole ... [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/3d-cell-culture/organoid-antibody-staining?srsltid=AfmBOooa14O_kEppDLyB1-0weYBYiYKXx4mHcHYEnPKKjxD-PUd2N_oV]
- 35. IVF Cryopreservation and Safe Handling Practices [https://www.pureairemonitoring.com/ivf-cryopreservation-and-safe-handling-practices/?srsltid=AfmBOop9BOfUEDeFVIhOfyZYJ0kqc97tLgjQMNbXa1BzKLO3UQMqOjZE]
- 36. The principal variables of cryopreservation: solutions, ... [https://www.sciencedirect.com/science/article/pii/S0015028211010429]
- 37. Cryopreservation method for Drosophila melanogaster ... [https://www.nature.com/articles/s41467-021-22694-z]
- 38. Protocols and Best Practices for Freezing Cells [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 39. Embryo Cryopreservation FAQ [https://fertility.womenandinfants.org/blog/cryopreservation-faq]
- 40. Immunofluorescence techniques in zebrafish retina [https://www.ptglab.com/news/blog/immunofluorescence-techniques-in-zebrafish-retina/?srsltid=AfmBOorMByeB2DwZcHzDJY0cd2bXMoEFRGQ2ujAUeRCTmTTRNAg5ozSE]
- 41. Optimized protocol for cryopreservation of human eggs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3577428/]
- 42. Embryo Cryopreservation – Information for Patients [https://www.cuh.nhs.uk/patient-information/embryo-cryopreservation-information-for-patients/]
- 43. Immunofluorescence techniques in zebrafish retina [https://www.ptglab.com/news/blog/immunofluorescence-techniques-in-zebrafish-retina/?srsltid=AfmBOop4wmR9MDMcGcZ3B0TPYkZXbLuVrNyBoMFz3jaYGi7JBNSYhhZL]
- 44. Whole mount nuclear fluorescent imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC3504639/]
- 45. Flat mount preparation for whole-mount fluorescent imaging of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10373579/]
- 46. Method for Whole Mount Antibody Staining in Chick - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2783013/]
- 47. How to Create an Effective Quality Control Plan ... [https://www.6sigma.us/six-sigma-in-focus/quality-control-plan/]
- 48. Visual Inspection: An In-Depth Guide [New for 2025] [https://mfe-is.com/visual-inspection/]
- 49. Using Visual Inspection for Quality Control in 2025 [https://averroes.ai/blog/visual-inspection-quality-control]
- 50. Visual Inspection Tips for 2025 Quality Checks [https://www.tradeaiders.com/visual-inspection-tips-for-2025-quality-checks.html]
- 51. ICC/IF Troubleshooting [https://www.antibodies.com/applications/immunofluorescence/immunofluorescence-troubleshooting]
- 52. Quantitative Whole - mount Analysis of Cardiac... Immunofluorescence [https://pmc.ncbi.nlm.nih.gov/articles/PMC6475905/]
- 53. microscopy of mouse... Whole mount immunofluorescence [https://bio-protocol.org/exchange/preprintdetail?id=543&type=3]
- 54. Troubleshooting Immunofluorescence [https://www.hycultbiotech.com/immuno-fluorescence/troubleshooting/]
- 55. Suppression of Red Blood Cell Autofluorescence for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5657453/]
- 56. Learn how to Remove Autofluorescence from your ... [https://www.leica-microsystems.com/science-lab/life-science/learn-how-to-remove-autofluorescence-from-your-confocal-images/]
- 57. Autofluorescence in Microscopy Literature References [https://www.microscopyu.com/references/autofluorescence]
- 58. Corrected Super-Resolution Microscopy Enables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7822748/]
- 59. Comprehensive Immunofluorescence Protocols: IF Protocol Hub [https://ifprotocol.org/]
- 60. Optimized protocol for whole-mount RNA fluorescent in situ ... [https://www.sciencedirect.com/science/article/pii/S2666166723005701]
- 61. Optimization of the Blocking and Signal Preservation ... [https://pubmed.ncbi.nlm.nih.gov/40996492/]
- 62. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOor4EK4Zlc6QYsvaQHKVvCRYIUlj99RaIaIBCi0m7sJMSby8rxAw]
- 63. Immunocytochemistry Troubleshooting: ICC Help & ... [https://www.bio-techne.com/applications/imaging/immunocytochemistry/troubleshooting]
- 64. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoo6VSfgAJ7WO3fjeTGGl8xVQ1c8xZWjv7nRvUm74znryFMacC60]
- 65. On the long-term storage of tissue for fluorescence and ... [https://link.springer.com/article/10.1007/s00418-024-02334-5]
- 66. On the long-term storage of tissue for fluorescence and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11602835/]
- 67. How to Minimize Non Specific Binding of Secondary ... [https://precisionbiosystems.com/how-to-minimize-non-specific-binding-of-secondary-antibody-during-western-blotting/]
- 68. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOopQwnffRHcMZm7Zb-gjAaZMzq4ac1Hws2O1ncN_g-e1NLvNzVGo]
- 69. Simple Elimination of Background Fluorescence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5614400/]
- 70. Blocking Strategies for IHC [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/blocking-strategies-ihc.html]
- 71. What causes non-specific antibody binding and how can it ... [https://www.cytometry.org/web/q_view.php?id=153&filter=Analysis%20Techniques]
- 72. How to Work with Challenging or Limited Genomic ... [https://blog.omni-inc.com/blog/how-to-work-with-challenging-or-limited-genomic-samples-updated-for-2025]
- 73. Immunofluorescence techniques in zebrafish retina [https://www.ptglab.com/news/blog/immunofluorescence-techniques-in-zebrafish-retina/?srsltid=AfmBOoq6ojCszwb9V2FEJdzGHRMf1TRAJoaNvJkSsexQu_axPUkllZ5-]
- 74. This MIT spinout is taking biomolecule storage out of the ... [https://news.mit.edu/2025/mit-spinout-cache-dna-takes-biomolecule-storage-out-freezer-0912]
- 75. Protocol Glyoxal-based fixation of Drosophila embryos for ... [https://www.sciencedirect.com/science/article/pii/S2666166723003520]
- 76. Zebrafishology, study design guidelines for rigorous and ... [https://www.nature.com/articles/s42003-025-07496-z]
- 77. Protocol for whole-mount preparation, clearing, and ... [https://www.sciencedirect.com/science/article/pii/S2666166724006567]
- 78. A quick, cheap, and reliable protocol for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9876944/]
- 79. A quantitative pipeline for whole-mount deep imaging and ... [https://elifesciences.org/reviewed-preprints/107154]
- 80. Protocol for whole-mount preparation, clearing, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11683226/]
- 81. Organ Culture and Whole Mount Immunofluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5352256/]
- 82. EVATOM: an optical, label-free, machine learning assisted ... [https://www.nature.com/articles/s42003-024-05960-w]
- 83. Semiautomated analysis of embryoscope : Using localized... images [https://pubmed.ncbi.nlm.nih.gov/25614363/]
- 84. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOop2nYcnpel0ddrFAFE2VY7XTwgx8d3gdHSRcByciApCd8N7ow9u]
- 85. The effect of chemical fixation with paraformaldehyde ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11837135/]
- 86. Fixation Strategies and Formulations Used in IHC Staining [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/fixation-strategies-formulations.html]
- 87. Whole Mount in Situ Hybridization of E8.5 to E11.5 Mouse ... [https://www.jove.com/v/2797/whole-mount-in-situ-hybridization-of-e85-to-e115-mouse-embryos]
- 88. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOor1L8hED9x_gOoVVgXuz4WFRlC2W5GvoJ53E3oWo2AUVDPYnzwX]
- 89. The Art of Frozen Tissue Sectioning [https://www.leicabiosystems.com/us/knowledge-pathway/the-art-of-embedding-tissue-for-frozen-section/]
- 90. Immunofluorescence Staining of Paraffin Sections Step by ... [https://www.frontiersin.org/journals/neuroanatomy/articles/10.3389/fnana.2020.582218/full]
- 91. Comparative analysis of fixation techniques for signal ... [https://pubmed.ncbi.nlm.nih.gov/39245159/]
- 92. Comparative study of pre- and post-mortem perfusion ... [https://www.nature.com/articles/s41684-025-01633-1]
- 93. Quantitative benchmarking of nuclear segmentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125308/]