Beyond Animal Models: Validating Organoid Systems for Predictive Human Development and Disease Research
This article provides a comprehensive framework for researchers and drug development professionals on validating organoid models against in vivo development.
Beyond Animal Models: Validating Organoid Systems for Predictive Human Development and Disease Research
Abstract
This article provides a comprehensive framework for researchers and drug development professionals on validating organoid models against in vivo development. It explores the foundational principles establishing organoids as physiologically relevant systems, details advanced methodological applications from disease modeling to drug screening, addresses key troubleshooting and optimization challenges including reproducibility and maturation, and presents rigorous comparative analyses with traditional models. By synthesizing current evidence and standardization initiatives, this resource aims to guide the confident adoption of organoid technology to enhance the translational predictive power of preclinical research.
Establishing the Basis: Why Organoids Offer a Physiologically Relevant Platform
In the evolving landscape of biological research, organoids have emerged as a transformative technology that bridges the gap between traditional two-dimensional cell cultures and complex in vivo models. These three-dimensional (3D) multicellular, microtissues are derived from stem cells and are designed to closely mimic the complex structure and functionality of human organs like the lung, liver, or brain [1]. Organoids represent a paradigm shift in in vitro modeling, affording researchers a much more physiologically relevant system than traditional two-dimensional cell cultures [2]. The defining characteristics of organoids include their 3D architecture, presence of multiple cell types, representation of the complexity and organization of native tissue, and resemblance of at least some aspects of tissue functionality [1].
The significance of organoid technology is reflected in its growing market impact. According to a report by The Insight Partners, the organoid market is expected to reach $15.01 billion in 2031, a compound annual growth rate (CAGR) of 22.1% from 2023's $3.03 billion [3]. This growth is fueled by increasing recognition of organoids' potential in disease modeling, drug discovery, and personalized medicine. The passing of the FDA Modernization Act 2.0 has further empowered researchers to use innovative non-animal methods, including organoids, for drug testing, potentially transforming the speed and success of bringing safe and effective treatments to market [3].
Stem Cells: The Foundation of Organoid Technology
Pluripotent Stem Cells and Their Differentiation Potential
Organoids can be generated from various stem cell sources, each offering distinct advantages for specific research applications. Pluripotent stem cells (PSCs), including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), possess the remarkable capacity to differentiate into any cell type present in an embryo or adult [4]. Takahashi and Yamanaka's groundbreaking 2006 discovery demonstrated that somatic cells could be reprogrammed into iPSCs through the ectopic expression of four transcription factors (OCT4, SOX2, KLF4, and MYC), opening new avenues for patient-specific disease modeling [4].
When PSCs are exposed to the right combination of growth factors and signals and provided with a 3D scaffold, they can differentiate into various cell types and self-organize into organoids. This approach has successfully generated organoids resembling multiple tissues, including brain, eyes, kidney, lung, stomach, intestine, inner ear, skin, thyroid, and liver [4]. The differentiation process is guided by specific growth factor combinations that mimic embryonic development. For example, intestinal organoid formation requires signals mediated by the Wnt (WNT) and fibroblast growth factor (FGF) protein families to induce posterior endoderm patterning, hindgut, and intestinal morphogenesis [5]. Similarly, brain organoids require factors that promote neural induction and regional specification.
Adult Stem Cells and Tissue-Specific Organoids
In contrast to pluripotent stem cells, adult stem cells (ASCs) are tissue-resident, multipotent cells responsible for maintaining homeostasis in specific organs throughout postnatal life [4]. These cells can only differentiate into cell types from their organ of origin, making them ideal for generating tissue-specific organoids. ASCs reside in specialized microenvironments known as stem cell niches, which regulate their cellular fate through secreted molecules, cell-cell interactions, and physical contact with the extracellular matrix [4].
The first protocol for generating organoids from ASCs was developed using intestinal tissue, where the molecular mechanisms regulating intestinal stem cell turnover are well understood [5]. The Wnt signaling pathway emerged as a key driver of epithelial ASC growth, inducing the secretion of R-spondin-1 protein (RSPO1), the ligand of the leucine-rich repeat-containing G protein-coupled receptor 5 (LGR5) expressed in most ASCs [5]. This breakthrough enabled the generation of patient-derived organoids (PDOs) from various tissues, including pancreas, prostate, esophagus, ovary, liver, kidney, and breast [5]. Organoids generated from ASCs or adult tissue fragments more closely resemble the homeostatic and regenerative capacity of the tissue of origin than PSC-derived organoids, making them valuable models for studying diseases such as cancer or neurodegenerative disorders [4].
Table 1: Comparison of Stem Cell Sources for Organoid Generation
| Characteristic | Pluripotent Stem Cells (PSCs) | Adult Stem Cells (ASCs) |
|---|---|---|
| Origin | Embryonic stem cells (ESCs) or induced pluripotent stem cells (iPSCs) | Tissue-specific stem cells |
| Differentiation Potential | Can differentiate into all cell types from three germ layers | Limited to cell types of their organ of origin |
| Resemblance to Native Tissue | More closely resembles fetal tissue stage [4] | Closely resembles homeostatic and regenerative adult tissue [4] |
| Genetic Stability | Lower genetic stability [4] | Higher genetic stability [4] |
| Primary Applications | Developmental studies, disease modeling, organogenesis [4] | Disease modeling, personalized medicine, cancer research [6] |
| Examples | Brain, kidney, lung organoids [4] | Intestinal, pancreatic, prostate organoids [5] |
Validating Organoid Models Against In Vivo Physiology
Methodological Framework for Physiological Validation
A critical challenge in organoid research is establishing the physiological fidelity of these in vitro models against their in vivo counterparts. A systematic framework for validation utilizes massively parallel single-cell RNA sequencing (scRNA-seq) to compare cell types and states found in vivo with those of in vitro organoid models [7]. This approach enables researchers to identify discrepancies and implement molecular interventions to rationally improve physiological fidelity.
In a landmark study, researchers used scRNA-seq to compare Paneth cells—specialized epithelial cells of the small intestine that support the stem cell niche and produce antimicrobial peptides—in conventional intestinal organoids against their in vivo counterparts [7]. This comparison revealed fundamental gene expression differences in lineage-defining genes, enabling the researchers to nominate and test molecular interventions to enhance Paneth cell physiology in organoids. The resulting improved model demonstrated enhanced antimicrobial activity and niche support function, key characteristics of in vivo Paneth cells [7].
Functional and Structural Validation Approaches
Beyond transcriptomic profiling, comprehensive validation of organoid models requires multidisciplinary approaches including histopathological analysis, functional assays, and drug response testing. Histological comparison involves examining organoid sections through hematoxylin and eosin (H&E) staining and immunohistochemistry for tissue-specific markers to assess architectural resemblance to native tissue [8]. For example, pancreatic ductal adenocarcinoma (PDAC) tumor organoids show strong correlation of histopathological features with matched patient-derived xenograft (PDX) models, with tumor cells in both systems expressing cytokeratin 19, a marker of pancreatic epithelial differentiation [8].
Functional validation includes assessing organoid capabilities that mirror in vivo tissue functions, such as nutrient absorption in intestinal organoids, metabolic activity in hepatic organoids, or synaptic connectivity in brain organoids. For specialized cells like Paneth cells, functional validation involves testing antimicrobial activity through bacterial killing assays and evaluating niche support capability through stem cell maintenance assays [7]. Drug response profiling represents another critical validation parameter, particularly for cancer organoids. Studies have demonstrated a specific relationship between area under the curve values of organoid drug dose response and in vivo tumor growth, irrespective of the drug treatment [8].
Table 2: Multi-Modal Validation of Organoid Physiological Fidelity
| Validation Method | Key Parameters Assessed | Experimental Techniques | Representative Findings |
|---|---|---|---|
| Transcriptomic Profiling | Gene expression patterns, cell type representation | Single-cell RNA sequencing (scRNA-seq), bulk RNA-seq | Identification of gene expression differences in Paneth cells between in vivo and organoid models [7] |
| Histopathological Analysis | Tissue architecture, cellular organization, marker expression | H&E staining, immunohistochemistry, immunofluorescence | PDAC organoids maintain glandular structures and cytokeratin 19 expression seen in PDX models [8] |
| Functional Assays | Cell-specific functions, metabolic activity, secretory profile | Antimicrobial assays, nutrient absorption tests, metabolite profiling | Enhanced Paneth cells in improved organoid models show increased antimicrobial activity [7] |
| Drug Response Testing | Therapeutic sensitivity, resistance mechanisms, predictive value | Dose-response curves, high-throughput screening | Concordance between PXO and PDX responses to therapeutic drugs observed in pancreatic cancer models [8] |
| Glycomic Analysis | Glycosylation patterns, post-translational modifications | Mass spectrometry, lectin arrays | PXO cultures retain complex glycosylation changes observed in PDX models [8] |
Experimental Protocols for Organoid Generation and Validation
Standardized Workflow for Organoid Culture
The general workflow for organoid culturing and analysis involves multiple standardized steps that ensure reproducibility and physiological relevance. The process begins with 2D preculture, where organoids are derived from either primary cells or induced pluripotent stem cells [1]. The cells are then premixed with an extracellular matrix (ECM) substitute, most commonly Matrigel, and droplets are placed into multi-well plates at room temperature. The plates are transferred to an incubator to form a solid droplet dome, after which media is added for seven or more days to promote cell growth and differentiation into specific tissues [1].
Organoid culture is a long process that may include several steps with different media formulations. During this process, cell health needs to be monitored regularly through imaging to ensure proper development [1]. Before experiments are conducted, organoids require comprehensive characterization to verify appropriate tissue structure and differentiation. High-content imaging allows for monitoring and visualizing organoid growth and differentiation, 3D reconstruction of structures, complex analysis of organoid architecture, cell morphology and viability, and expression of different cell markers [1]. Confocal imaging and 3D analysis of organoids enable visualization and quantitation of the organoids and their constituent cells, with characterization of multiple quantitative descriptors used for studying disease phenotypes and compound effects [1].
Key Signaling Pathways and Growth Factors
Successful organoid culture depends on precise activation or inhibition of key signaling pathways through specific growth factors and inhibitors in the culture medium. The Wnt signaling pathway is fundamental for maintaining stemness and promoting proliferation in many organoid types. Activation is typically achieved through recombinant WNT3A or small molecule inhibitors of GSK3, combined with R-spondin 1 (RSPO1), which enhances Wnt signaling by binding to LGR5 receptors on stem cells [5] [2]. Bone Morphogenetic Protein (BMP) signaling must often be inhibited to prevent differentiation, typically using Noggin, which binds to various BMPs including BMP4 and BMP7, limiting their inhibitory activity on stem cell maintenance [2].
The EGF signaling pathway drives proliferation in many epithelial organoid systems. Epidermal growth factor (EGF) induces proliferative signaling cascades by binding to its receptor EGFR, supporting self-renewal and expansion of adult stem cell populations within organoids [2]. Research has shown that inhibiting EGFR signaling pharmacologically or through EGF depletion can significantly impair organoid proliferation and induce cellular quiescence and differentiation [2]. Additional factors like FGF10, FGF2, and Activin A are employed in specific organoid systems to direct differentiation toward particular lineages [2].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Organoid Research and Their Functions
| Reagent Category | Specific Examples | Function in Organoid Culture | Validation Parameters |
|---|---|---|---|
| Extracellular Matrices | Matrigel, Geltrex, synthetic hydrogels | Provides 3D structural support, mechanical cues, and biochemical signals for cell growth and organization | Batch-to-batch consistency, growth factor content, polymerization properties [1] |
| Growth Factors & Cytokines | R-spondin 1, Noggin, EGF, FGF10, WNT3A | Activates specific signaling pathways for stem cell maintenance, proliferation, and differentiation | Purity, bioactivity, endotoxin levels, performance in organoid growth assays [2] |
| Small Molecule Inhibitors | CHIR99021 (GSK3 inhibitor), Y-27632 (ROCK inhibitor), A83-01 (TGF-β inhibitor) | Modulates signaling pathways to enhance stem cell survival, growth, and direct differentiation | Specificity, potency, cytotoxicity, effects on target pathway activity [5] [8] |
| Basal Media Components | Advanced DMEM/F12, B27 supplement, N2 supplement, N-acetylcysteine | Provides nutritional support, hormones, and antioxidants for cell viability and function | Osmolality, pH stability, nutrient composition, support of long-term culture [8] |
| Dissociation Reagents | TrypLE, Accutase, collagenase, dispase | Enables organoid passaging and single-cell isolation for expansion and analysis | Enzymatic activity, cell viability post-dissociation, recovery efficiency [9] |
Current Limitations and Engineering Solutions
Addressing Structural and Functional Gaps
Despite their significant advantages, organoid models face several limitations that affect their physiological relevance and scalability. A primary constraint is the lack of vascularization, which limits organoid size due to inadequate nutrient and oxygen diffusion, leading to necrotic core development when organoids exceed approximately 500 micrometers in diameter [10] [3]. This absence of vascular networks also prevents recapitulation of crucial endothelial cell interactions and blood-tissue barriers present in vivo. Additionally, most organoid protocols are limited to epithelial cells, lacking the full complexity of the tumor microenvironment (TME) including immune cells, fibroblasts, and neural cells [5].
The fetal phenotype of many PSC-derived organoids presents another limitation, as they may not fully represent adult tissue characteristics or adult-onset diseases [3]. This is particularly relevant for disease modeling of conditions that manifest in mature tissues. Issues with reproducibility and standardization also persist, with variability in organoid shape, size, and cell type composition between batches and protocols [3]. A 2023 survey by Molecular Devices revealed that nearly 40% of scientists rely on complex human-relevant models like organoids, with reproducibility and batch-to-batch consistency identified as significant challenges [3].
Engineering Advances for Enhanced Physiological Relevance
Multiple engineering approaches are being developed to address these limitations and enhance organoid functionality. Vascularization strategies include co-culture with endothelial cells, incorporation of mesenchymal cells, and use of microfluidic devices to create perfusable networks [3] [10]. The chick chorioallantoic membrane (CAM) model provides an alternative in vivo system for vascularizing organoids, where inoculation onto the highly vascularized, non-innervated CAM results in extensively vascularized xenografts that maintain histomorphological similarity to original patient tissue [9].
Organoid-on-chip systems combine organoids with microfluidic technology to create dynamic microenvironments that better recapitulate physiologic conditions [10]. These systems incorporate fluid flow, mechanical forces, and electrical stimulation to enhance cellular differentiation and tissue functionality. For example, fluid shear stress in renal organoid-on-chip systems leads to tissue maturation and morphogenesis, including formation of proximal tubule and glomerular compartments [10]. 3D bioprinting and biofabrication techniques enable precise control over organoid size, shape, and cellular composition, allowing creation of more complex and reproducible models [10]. These approaches facilitate the generation of multi-tissue interfaces and incorporation of stromal and immune cells to better mimic native tissue environments.
Organoid technology represents one of the most promising advancements in biomedical research, offering unprecedented opportunities for studying human development, disease mechanisms, and therapeutic interventions. The validation of organoid models against in vivo physiology remains crucial for realizing their full potential in basic and translational research. As systematic validation frameworks using single-cell genomics and other multi-omics approaches become more widespread, the physiological fidelity of organoid models continues to improve [7].
Future developments in organoid technology will likely focus on enhancing complexity through the incorporation of immune and vascular components, improving maturation to adult tissue phenotypes, and increasing scalability and reproducibility through automation and standardization [3] [10]. The integration of organoids with organ-on-chip technology and 3D bioprinting will further advance their applications in drug discovery and personalized medicine [3]. As these technologies evolve, organoids are poised to become indispensable tools for modeling human biology and disease, ultimately accelerating the development of safer and more effective therapies.
Organoid technology represents a transformative advancement in biomedical research, offering in vitro models that closely mimic human physiology. For researchers and drug development professionals, the value of these three-dimensional structures lies in their core capabilities: faithfully preserving native tissue architecture, maintaining cellular diversity, and retaining patient-specific genetics. These advantages position organoids as superior tools for disease modeling, drug discovery, and personalized medicine approaches, effectively bridging the gap between traditional two-dimensional cell cultures and in vivo models [11] [12] [13]. This review systematically examines the experimental evidence validating organoid models against in vivo development and disease processes, providing critical insights for scientists selecting model systems for preclinical research.
Experimental Validation of Tissue Architecture Preservation
The capacity of organoids to recapitulate the complex three-dimensional architecture of native tissues represents a fundamental advantage over traditional two-dimensional cultures. This structural fidelity enables more physiologically relevant studies of cellular behavior, drug penetration, and tissue organization.
Histological and Morphological Evidence
Multiple studies have demonstrated that patient-derived organoids (PDOs) maintain histological features remarkably similar to their tissue of origin. Research on colorectal cancer organoids revealed conservation of characteristic pathological features, including the CK20+/CK7- immunophenotype found in most primary colorectal tumors [14]. Similarly, gliosarcoma organoids (GSOs) preserved the biphasic architecture of original tumors, containing both glial and mesenchymal elements characteristic of this rare glioblastoma variant [15].
Table 1: Quantitative Assessment of Architectural Features in Cancer Organoids
| Organoid Type | Architectural Feature | Similarity to Primary Tissue | Assessment Method |
|---|---|---|---|
| Colorectal Cancer PDOs | Crypt-villus-like structures | High (96% mutation concordance) | Whole exome sequencing, immunohistochemistry [14] |
| Gliosarcoma Organoids (GSOs) | Biphasic glial and sarcomatous histology | High (key features preserved) | H&E staining, Masson's trichrome, reticulin stains [15] |
| Breast Cancer Organoids | Glandular organization | Moderate to high (variable by subtype) | Histological analysis, drug response profiling [11] |
| Lung Organoids | Airway and alveolar sac structures | High (mimics distinct lung regions) | Air-liquid interface culture, immunofluorescence [12] |
Protocol for Evaluating Architectural Integrity
Standardized methodologies have emerged to quantitatively assess architectural preservation in organoid models:
- Tissue Processing: For gliosarcoma organoids, researchers mechanically minced fresh tumor tissue into approximately 1mm³ pieces without enzymatic digestion to preserve native tissue integrity and cellular composition [15].
- Matrix Embedding: Samples are embedded in appropriate extracellular matrices (e.g., Matrigel, BME, or synthetic hydrogels) to support 3D growth [13].
- Histological Analysis: Organoids are fixed, sectioned, and stained using H&E, Masson's trichrome, or immunohistochemistry for cell-type-specific markers [15].
- Imaging and Quantification: High-resolution confocal microscopy followed by digital image analysis quantifies structural parameters including size, lumen formation, and spatial organization [15].
Conservation of Cellular Diversity
Organoids maintain the heterogeneous cellular composition of their source tissues, encompassing multiple cell types and states present in vivo. This diversity enables more comprehensive studies of cell-cell interactions, differentiation pathways, and disease mechanisms.
Single-Cell Transcriptomic Validation
Single-cell RNA sequencing (scRNA-seq) has provided unprecedented resolution for validating cellular heterogeneity in organoid models. Comparative analysis of gliosarcoma organoids (GSOs) versus glioblastoma organoids (GBOs) revealed distinct transcriptional programs: GSOs were enriched for fibroblast-like and oligodendrocyte progenitor-like states, while GBOs displayed astrocyte-like differentiation patterns, faithfully reflecting differences in their parent tumors [15].
Brain organoids similarly demonstrate remarkable cellular diversity, containing radial glial cells, intermediate progenitors, deep- and superficial-layer neurons, and in some cases, microglia and other glial cell types [16]. These systems recapitulate the ordered temporal generation of different neuronal subclasses observed in vivo, although the precise laminar organization of the mammalian cortex is not fully replicated [16].
Table 2: Cellular Composition Across Organoid Systems
| Organoid Type | Key Cell Types Identified | Validation Method | Clinical Relevance |
|---|---|---|---|
| Brain Organoids | Radial glial cells, neurons, astrocytes, oligodendrocytes, microglia | scRNA-seq, immunofluorescence, functional assays | Neurodevelopment, disease modeling, drug screening [16] |
| Airway Organoids | Basal cells, ciliated cells, goblet cells, neuroendocrine cells | ALI culture, immunofluorescence, electrophysiology | Respiratory disease modeling, host-pathogen interactions, toxicity testing [17] |
| Intestinal Organoids | Intestinal stem cells, enterocytes, goblet cells, Paneth cells | Histology, mRNA sequencing, functional transport assays | Personalized medicine, regenerative medicine, infection biology [12] [13] |
| Tumor PDOs | Cancer stem cells, differentiated cancer cells, some stromal elements | Flow cytometry, immunohistochemistry, drug response | Cancer biology, drug screening, personalized therapy [14] [13] |
Protocol for scRNA-seq of Organoids
The standard workflow for single-cell transcriptomic analysis of organoids includes:
- Organoid Dissociation: Enzymatic (e.g., trypsin, accutase) and/or mechanical dissociation of organoids into single-cell suspensions [15].
- Cell Viability Assessment: Using viability dyes or automated cell counters to ensure >80% viability.
- Single-Cell Partitioning: Loading cells into appropriate scRNA-seq platforms (10X Genomics, Drop-seq, etc.).
- Library Preparation and Sequencing: Following manufacturer protocols for cDNA synthesis, amplification, and library preparation.
- Bioinformatic Analysis: Cell clustering, trajectory inference, and differential expression analysis using tools like Seurat, Scanpy, or Monocle [15].
Maintenance of Patient-Specific Genetics
Perhaps the most significant advantage of patient-derived organoids is their capacity to maintain the genetic landscape of the source tissue, enabling personalized disease modeling and drug response prediction.
Genomic and Transcriptomic Concordance
Comprehensive genomic analyses have demonstrated high concordance between PDOs and their corresponding patient tumors. Whole exome sequencing of colorectal cancer PDOs revealed approximately 96% similarity in mutations of key driver genes when compared to primary tumors [14]. Similarly, patient-derived tumor organoids (PDTOs) recapitulate the genetic diversity among patients, with quantitative mass-spectrometry-based proteome profiles resembling original tumors [11].
In oncology, this genetic fidelity translates to predictive power for treatment response. Studies report approximately 76% accuracy in organoids predicting patient response, with a sensitivity of 0.79 and specificity of 0.75, making PDOs suitable for guiding selection of effective therapeutic approaches personalized to each patient [14].
Table 3: Multi-Omics Validation of Patient-Specific Genetics in Organoids
| Analysis Type | Genetic Feature Preserved | Experimental Evidence | Application |
|---|---|---|---|
| Genomics | Somatic mutations, copy number variations | 96% mutation concordance in CRC PDOs [14] | Disease modeling, driver gene identification |
| Transcriptomics | Gene expression signatures, subtype classification | Conservation of CMS subtypes in CRC PDOs [14] | Drug response prediction, biomarker discovery |
| Proteomics | Protein expression patterns, signaling pathway activation | MS-based proteomics recapitulated tumor diversity [11] | Targeted therapy validation, signaling studies |
| Epigenomics | DNA methylation patterns, chromatin accessibility | Maintenance of segmental DNA methylation during differentiation [11] | Aging studies, developmental biology |
Protocol for Genomic Validation of PDOs
Standardized protocols for genomic validation include:
- DNA/RNA Extraction: Using commercial kits to obtain high-quality nucleic acids from both source tissue and derived organoids.
- Sequencing Library Preparation: Following established protocols for whole genome, whole exome, or transcriptome sequencing.
- Bioinformatic Analysis: Variant calling using established pipelines (GATK, VarScan) and comparison between tissue and organoid samples.
- Statistical Validation: Calculating concordance rates for mutations, copy number alterations, and gene expression profiles.
The Scientist's Toolkit: Essential Research Reagents
Successful organoid culture requires carefully optimized reagents and materials. The table below details key solutions used in establishing and maintaining organoid cultures.
Table 4: Essential Research Reagents for Organoid Culture
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Extracellular Matrices | Matrigel, BME, synthetic PEG hydrogels | Provides 3D scaffold for growth, mechanical cues | Batch variability, composition definition, clinical translation limitations [13] |
| Growth Factors & Cytokines | EGF, Noggin, R-spondin, Wnt3a, FGF10 | Directs differentiation, maintains stemness | Tissue-specific requirements, concentration optimization [13] [17] |
| Pathway Inhibitors/Agonists | Y-27632 (ROCK inhibitor), CHIR99021 (Wnt activator) | Enhances viability, modulates signaling pathways | Concentration-dependent effects, temporal application critical [15] |
| Medium Formulations | Intestinal, cerebral, airway-specific media | Provides nutritional support, hormonal cues | Component stability, osmolarity, pH buffering [13] [17] |
| Dissociation Reagents | Trypsin, accutase, collagenase | Organoid passage, single-cell isolation | Duration optimization, viability impact [13] |
Signaling Pathways in Organoid Development and Culture
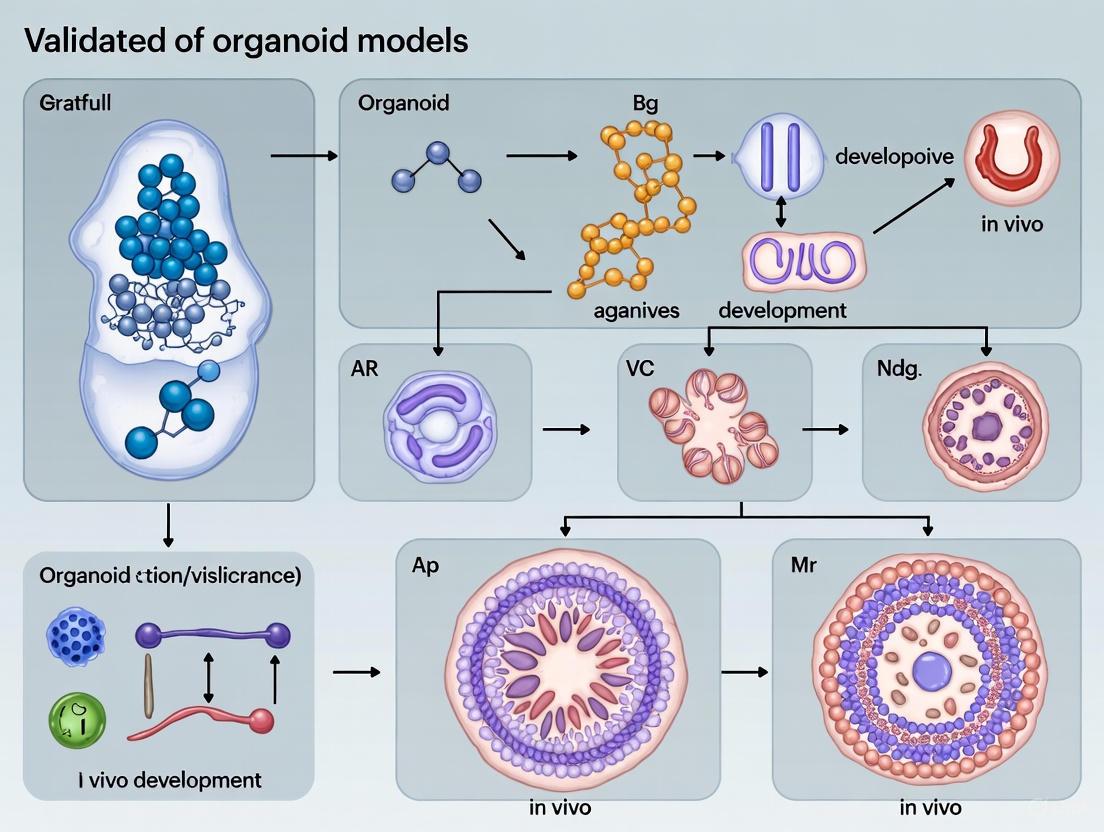
The successful establishment and maintenance of organoids depend on recapitulating key developmental signaling pathways. The diagram below illustrates the core pathways involved in organoid formation and maintenance, particularly for epithelial-derived organoids.
Key Signaling Pathways in Organoid Culture
The Wnt pathway is particularly crucial, with activation through R-spondin and Wnt3a supplementation supporting LGR5+ stem cell maintenance [13]. Interestingly, colorectal cancers with Wnt pathway mutations often grow without requiring exogenous Wnt activation, demonstrating how cancer organoids maintain the pathway alterations of their parent tumors [13]. Similarly, tumors with EGFR mutations can be cultured without EGF supplementation, reflecting their autonomous signaling [13].
Comparative Analysis with Alternative Models
Organoids occupy a unique position in the spectrum of preclinical models, offering advantages over both traditional 2D cultures and in vivo models while having their own limitations.
Table 5: Model System Comparison for Drug Development Applications
| Model Characteristic | 2D Cell Cultures | Organoid Models | In Vivo Models |
|---|---|---|---|
| Architectural Complexity | Low (monolayer) | High (3D structure) | High (native context) |
| Cellular Diversity | Limited (often single cell type) | Moderate to high (multiple cell types) | Complete (all native cells) |
| Genetic Fidelity | Low (genetic drift) | High (maintains patient genetics) | High (patient-derived xenografts) |
| Throughput | High | Moderate to high | Low |
| Cost | Low | Moderate | High |
| Human Relevance | Variable | High (human-derived) | Limited (species differences) |
| Regulatory Acceptance | Established | Growing | Established |
| Personalization Potential | Low | High | Moderate |
Organoid technology has firmly established itself as an indispensable tool for biomedical research, offering unprecedented preservation of tissue architecture, cellular diversity, and patient-specific genetics. The experimental data summarized in this review demonstrates that organoids provide a robust platform for modeling human development and disease, drug screening, and advancing personalized medicine. While challenges remain in standardizing protocols, incorporating complete tumor microenvironments, and improving reproducibility, the core advantages of organoid models position them as transformative tools that effectively bridge the gap between traditional in vitro systems and clinical research. For drug development professionals and researchers, organoids offer a physiologically relevant, human-derived model system that accelerates the translation of basic research findings into clinical applications.
Organoids, which are three-dimensional (3D) cell cultures derived from pluripotent or adult stem cells, have emerged as revolutionary tools in biomedical research for their ability to recapitulate the cellular heterogeneity, structure, and function of human organs [18]. These microstructures provide an invaluable platform for studying human biology, offering a more physiologically relevant system than traditional two-dimensional (2D) cell cultures while retaining human genetic material that animal models lack [19]. The capacity of organoids to mimic in vivo conditions has garnered significant attention from regulatory bodies, including the FDA, which has recently approved organoids for drug testing to reduce reliance on animal models [2]. As the organoid market is expected to grow substantially from $3.03 billion in 2023 to $15.01 billion in 2031, reflecting a compound annual growth rate of 22.1%, these models are increasingly positioned to bridge the translational gap between basic research and clinical application [3].
However, despite their promising features, organoids remain rudimentary and inherently artificial compared to intact living systems [20]. A significant translational gap persists between in vitro studies and in vivo applications, largely attributed to limitations in current organoid technologies [21]. The critical challenge lies in validating these models against in vivo development to ensure they faithfully replicate the complex biological processes of human organs. Without rigorous validation standards, organoid-based research and drug screening may yield misleading results, ultimately hindering their potential in disease modeling, drug discovery, and personalized medicine. This guide systematically compares organoid performance against traditional models, provides experimental validation protocols, and details essential reagent solutions to support researchers in bridging the in vitro-in vivo gap.
Comparative Analysis: Organoids Versus Traditional Research Models
Performance Metrics Across Model Systems
To objectively evaluate organoids as research tools, it is essential to compare their performance against traditional models—specifically 2D cell lines and patient-derived xenografts (PDX). The table below summarizes key quantitative and qualitative metrics across these systems, highlighting the relative advantages and limitations of each approach for biomedical research and drug development applications.
Table 1: Comparative Analysis of Research Models for Biomedical Applications
| Performance Metric | 2D Cell Lines | Patient-Derived Xenografts (PDX) | Organoid Models |
|---|---|---|---|
| Physiological Relevance | Low: Single cell type, lacks tissue structure and cell-cell interactions [19] | Moderate: Maintains 3D structure and some tumor microenvironment elements, but human stroma is replaced by mouse cells over time [19] | High: Retains 3D architecture, cellular heterogeneity, and genetic profile of original tissue [19] [18] |
| Success Rate/Establishment Time | High (Nearly 100%), days [19] | Low to moderate (Variable), months [19] | Moderate to high (Varies by organ system), weeks [19] |
| Cost Efficiency | Low cost [19] | High cost: Expensive to maintain and requires ethical oversight [19] | Moderate cost: More affordable than PDX but requires specialized matrices and factors [19] |
| Genetic Stability | Poor: Develops heterogeneity and drifts from original tissue over time [19] | Moderate: Loses primitive heterogeneity with passages; mouse stroma replaces human cells [19] | High: Faithfully maintains genetic and phenotypic heterogeneity of original tissue across passages [19] [18] |
| Scalability/Throughput | High: Suitable for high-throughput drug screening [19] | Low: Time-consuming, low throughput [19] | Moderate to high: Improving toward high-throughput applications with automation [3] |
| Personalized Medicine Application | Limited: Represents only a subgroup of original tissue [19] | Moderate: Maintains some patient-specific characteristics but affected by mouse microenvironment [19] | High: Patient-derived organoids (PDOs) enable personalized drug testing and treatment prediction [22] [23] |
| Validation Status | Well-established with known limitations | Established but with recognized species-specific limitations | Emerging: Requires further validation against in vivo biology [20] |
Key Advantages of Organoid Models
The comparative analysis reveals several distinct advantages of organoid models that position them as transformative tools in biomedical research. Organoids retain the 3D structure of original tissues, faithfully summarizing the genetic and phenotypic heterogeneity that is often lost in traditional 2D cell cultures [19]. This structural and functional fidelity enables more accurate modeling of human physiology and disease states. Furthermore, organoids provide a human-specific experimental platform that avoids the species-specific limitations inherent in animal models, thereby offering more clinically relevant insights for drug development and disease modeling [19] [3].
Another significant advantage lies in their application for personalized medicine. Patient-derived organoids (PDOs) can be utilized to examine the efficacy of various drugs, specifically tailoring treatments to individual genetic backgrounds and disease profiles [2] [22]. This more personalized approach helps improve treatment effectiveness while minimizing unwanted side effects. The technology also supports gene editing applications through techniques like CRISPR-Cas9, providing opportunities to study tumor gene mutations and disease mechanisms in a human-relevant context [19]. Additionally, organoids can be used to construct comprehensive biobanks, preserving diverse cellular models for research and therapeutic development [19].
Critical Validation Challenges and Experimental Solutions
Key Limitations in Current Organoid Models
Despite their promising applications, organoids face several significant challenges that limit their fidelity and reliability as experimental models. The diagram below illustrates the primary validation challenges and the corresponding experimental solutions being developed to address them.
The core challenges highlighted in the diagram manifest in specific ways that compromise organoid utility. Regarding cell type specification, while organoids contain broad cell types present in native tissues, they demonstrate impaired specification programs. Single-cell RNA sequencing analyses reveal that organoid-derived cells lack refined gene networks observed in endogenous development and show decreased expression of type-defining marker genes across multiple organoid protocols [20]. This suggests pervasive impairment in cell type specification that current protocols cannot fully overcome.
Structural and maturation limitations present another significant hurdle. Organoids typically exhibit a simplified version of native tissue architecture, such as forming ventricular zone-like rosettes instead of proper laminar sheets in neural organoids [20]. Furthermore, organoids often retain a fetal-like phenotype rather than maturing into adult tissue equivalents, limiting their utility for studying adult-onset diseases [3]. The lack of vascularization compounds these issues by restricting nutrient and oxygen diffusion, leading to hypoxic cores and necrosis in larger organoids [20] [3].
Experimental Validation Protocols
To address these challenges and bridge the in vitro-in vivo gap, researchers have developed sophisticated validation methodologies. The table below summarizes key experimental protocols for validating organoid models against in vivo standards, including the specific experimental setup, validation metrics, and purpose for each approach.
Table 2: Experimental Protocols for Organoid Model Validation
| Validation Method | Experimental Setup | Key Validation Metrics | Purpose/Application |
|---|---|---|---|
| Single-Cell RNA Sequencing (scRNA-seq) | Single-cell dissociation of organoids followed by RNA sequencing; comparison to primary tissue reference datasets [20] | Cell type diversity, expression of type-defining marker genes, identification of aberrant gene expression patterns [20] | Assessing fidelity of cell type specification; identifying atypical cellular states |
| Machine Learning Morphology Prediction | Convolutional neural networks trained on phase-contrast images from early organoid development to predict later differentiation outcomes [24] | Prediction accuracy (e.g., 79% accuracy for pituitary differentiation at day 40 using day 9 images); Grad-CAM visualization of decisive morphological features [24] | Non-invasive quality assessment; early prediction of organoid developmental potential |
| Immunofluorescence & Spatial Transcriptomics | Antibody staining for cell type-specific markers; spatial transcriptomics to map gene expression in organizational contexts [20] | Presence and distribution of key protein markers; correlation of spatial gene expression with native tissue architecture | Validating structural organization and cellular positioning within organoids |
| Electrophysiological Functional Assays | Multi-electrode arrays or patch clamping to record electrical activity in neural organoids [20] | Neural activity patterns, synaptic function, network synchronization | Assessing functional maturation and physiological relevance of neuronal organoids |
| Vascularization & Perfusion Models | Co-culture with endothelial cells; integration with microfluidic organ-on-chip platforms [3] [23] | Formation of endothelial networks; improved nutrient perfusion; reduction in hypoxic cores | Enhancing organoid size, maturity, and physiological relevance |
The application of these validation protocols has yielded critical insights into organoid biology. For instance, machine learning approaches have demonstrated that surface morphology features such as budding patterns and texture in early organoid development can predict successful differentiation with 79% accuracy, outperforming human assessment particularly at early stages (day 9) [24]. Successful organoids typically show small budding areas with slightly rough surfaces, while failed organoids exhibit smooth or irregularly rough textures often associated with mislocalized neural or retinal cells [24].
Similarly, single-cell RNA sequencing validation has revealed that organoids chronically express cellular stress genes across all cell types, indicating metabolic stress, endoplasmic reticulum stress, and electron transport dysfunction not typically observed in normal neural development [20]. This chronic stress response may interfere with proper developmental programs, highlighting a critical area for protocol improvement.
Essential Research Reagent Solutions for Organoid Validation
The successful culture and validation of organoids depends critically on a suite of specialized research reagents that support their development and mimic native tissue microenvironments. The table below details essential reagent solutions, their specific functions, and examples of their application in organoid research.
Table 3: Essential Research Reagent Solutions for Organoid Culture and Validation
| Research Reagent | Function in Organoid Culture | Specific Application Examples |
|---|---|---|
| R-spondin 1 | Activates Wnt/β-catenin signaling by binding Lgr5 receptor; supports stem cell self-renewal and proliferation [2] | Essential for long-term expansion of intestinal, mammary, and hepatic organoids; cooperates with Noggin to maintain Lgr5+ stem cell populations [2] |
| Noggin | BMP signaling pathway inhibitor; modulates cell differentiation and coordinates Wnt signaling to activate stem cells [2] | Required for liver organoid culture where BMP suppression is crucial; enables expansion by inhibiting differentiation-promoting BMP signals [2] |
| Epidermal Growth Factor (EGF) | Binds EGFR to induce proliferative signaling cascades; supports self-renewal and expansion of adult stem cell populations [2] | Critical for liver, thyroid, gastrointestinal, and brain organoids; depletion leads to cellular quiescence and differentiation rather than proliferation [2] |
| Extracellular Matrix (ECM) | Provides 3D structural support mimicking basal membrane; enables self-organization and polarization of cells [19] [18] | Standard requirement for most organoid cultures; Matrigel is commonly used but research focuses on defined, GMP-grade alternatives [3] |
| Wnt Agonists | Enhance Wnt pathway activation crucial for stem cell maintenance and proliferation in various epithelial tissues [2] | Particularly important for intestinal and colon organoids; required alongside R-spondin for optimal stem cell activity [2] |
| FGF10 & FGF2 | Support branching morphogenesis and proliferation in various organ systems; particularly important for foregut-derived organs [2] | Used in gastric organoid culture alongside EGF, Noggin, and R-spondin 1 to support growth across multiple passages [2] |
The critical importance of these reagents is demonstrated through functional validation assays. For example, bioactivity testing shows that recombinant human R-Spondin 1 induces TCF reporter activity in HEK293 cells with an EC50 of 0.0138-0.0163 µg/mL, while EGF stimulates EGFR reporter cells with approximately 56-fold induction [2]. These quantitative potency measurements are essential for standardizing organoid culture conditions across different laboratories and applications.
Furthermore, proper combination of these factors enables successful establishment of diverse organoid types. Experimental data demonstrates that EGF, Noggin, and R-spondin 1 together maintain intestinal, gastric, and colonic organoid growth through multiple passages and long-term culture processes [2]. The functional synergy between these components—where R-spondin activates Wnt signaling and Noggin inhibits BMP signaling—creates a balanced environment that supports stem cell maintenance while permitting appropriate differentiation.
Organoid technology represents a transformative approach in biomedical research, offering unprecedented opportunities to model human development and disease in a physiologically relevant context. However, realizing the full potential of these models requires rigorous validation against in vivo benchmarks to ensure they faithfully recapitulate the complex cellular, structural, and functional properties of native tissues. The comparative data presented in this guide demonstrates that while organoids already surpass traditional 2D cultures and animal models in several key metrics—particularly in maintaining human genetic and phenotypic heterogeneity—significant challenges remain in achieving complete physiological fidelity.
The future of organoid validation will likely involve increased integration of advanced technologies such as artificial intelligence for quality assessment and prediction [24] [23], multi-omics characterization for comprehensive profiling [20] [23], microfluidic systems for enhanced physiological relevance [3] [23], and automated platforms for improved reproducibility [3]. Additionally, efforts to vascularize organoids and incorporate immune components will be crucial for creating more complete tissue models that better bridge the in vitro-in vivo gap [3] [23]. As these advancements converge, validated organoid models will increasingly accelerate drug discovery, enable more accurate disease modeling, and advance personalized medicine approaches—ultimately fulfilling their promise as transformative tools in biomedical research.
Organoids represent a groundbreaking advancement in biomedical research, offering three-dimensional (3D) in vitro models that remarkably recapitulate the architecture and functionality of human organs. These self-organizing structures, derived from stem cells or tissue-specific progenitors, have emerged as powerful tools bridging the gap between traditional two-dimensional cell cultures and complex in vivo models [25]. The development of organoid technology has revolutionized our approach to studying human development, disease mechanisms, and drug responses, providing unprecedented insights into organ-specific physiology and pathology.
According to a consensus definition endorsed by the hepatic, pancreatic, and biliary Organoid Consortium, organoids are "three-dimensional structures derived from pluripotent stem cells, progenitor, and/or differentiated cells that self-organize through cell-cell and cell-matrix interactions to recapitulate aspects of the native tissue architecture and function in vitro" [26]. This definition highlights the key characteristics that distinguish organoids from other 3D culture systems: their self-organization capacity and ability to mimic native tissue functionality.
The significance of organoid technology was recognized when Nature Methods named it "Method of the Year 2017," reflecting the excitement and promise of this rapidly evolving field [26]. Since the pioneering work on intestinal organoids in 2009, the field has expanded to include models for numerous organs, including brain, liver, kidney, lung, and many others [25] [27]. This guide provides a comprehensive comparison of brain, intestinal, liver, and cancer organoid systems, focusing on their validation against in vivo development and their applications in biomedical research.
Comparative Analysis of Organoid Systems
Brain Organoids
Generation Strategies and Key Features: Brain organoids are typically generated from human pluripotent stem cells (hPSCs), including both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) [28]. These organoids mimic various regions of the developing human brain, such as the cortex, midbrain, hippocampus, and cerebellum, through self-organization principles that recapitulate in vivo neurodevelopment [28]. Recent advancements include the development of multi-region brain organoids (MRBOs) that contain interconnected tissues from different brain regions, representing a significant leap forward in modeling the complex organization of the entire brain [29].
The generation of brain organoids typically involves embryoid body formation followed by neural induction and maturation in 3D culture conditions. These structures develop various neuronal subtypes, glial cells, and demonstrate functional neural network activity. Notably, recent models have even shown the formation of rudimentary blood-brain barrier components, enhancing their physiological relevance [29]. One key advantage of brain organoids is their ability to model human-specific aspects of brain development and disorders that cannot be adequately studied in animal models [25].
Validation Against In Vivo Development: Transcriptomic analyses have demonstrated that brain organoids recapitulate key aspects of human fetal brain development, with some models exhibiting up to 80% of the cell type diversity found in early human fetal brains [29]. These organoids have been shown to follow similar developmental trajectories as the human brain, with sequential emergence of specific neuronal subtypes and glial cells. Furthermore, brain organoids have successfully modeled the effects of genetic mutations associated with neurodevelopmental disorders, reproducing pathological features observed in patient brains [28].
Table: Brain Organoid Validation Metrics
| Validation Parameter | Findings | Significance |
|---|---|---|
| Cell Type Diversity | 80% of range of cell types in early fetal brain development [29] | Recapitulates cellular complexity of developing brain |
| Developmental Stage | Resembles 40-day-old human fetal brain [29] | Models early neurodevelopment events |
| Functional Maturation | Production of electrical activity and network responses [29] | Demonstrates functional neuronal properties |
| Blood-Brain Barrier | Early blood-brain barrier formation observed [29] | Includes critical neurovascular components |
| Disease Modeling | Recapitulates features of Alzheimer's, Parkinson's, Huntington's disease [28] | Validates pathological relevance for neurodegenerative disorders |
Intestinal Organoids
Generation Strategies and Key Features: Intestinal organoids were among the first successfully established organoid systems and represent a well-characterized model for epithelial biology. These organoids can be generated from two main sources: intestinal stem cells isolated from biopsy tissues or pluripotent stem cells directed toward intestinal differentiation [30]. The breakthrough in intestinal organoid culture came with the identification of Lgr5+ stem cells at the base of intestinal crypts and the development of culture conditions containing essential niche factors like EGF, Noggin, and R-spondin [31].
Intestinal organoids form intricate crypt-villus structures containing all the major epithelial cell types found in the native intestine, including enterocytes, goblet cells, Paneth cells, and enteroendocrine cells [30]. These organoids exhibit key intestinal functions such as nutrient absorption, mucus secretion, and response to microbial signals. The ability to culture intestinal organoids from human tissue has been particularly valuable for studying patient-specific intestinal diseases and host-microbe interactions.
Validation Against In Vivo Development: Intestinal organoids closely mirror the cellular composition and organization of the native intestinal epithelium. Single-cell RNA sequencing analyses have confirmed that these organoids contain all the expected intestinal epithelial cell lineages with transcriptomic profiles similar to their in vivo counterparts [30]. Importantly, human intestinal organoids have been shown to contain certain cell types, such as motilin+ enteroendocrine cells and BEST4+/OTOP2+ cells, that are found in humans but not in mice, highlighting their value for studying human-specific intestinal biology [31].
Functional validation studies have demonstrated that intestinal organoids respond appropriately to key signaling pathways that regulate intestinal stem cell behavior in vivo, including Wnt, Notch, and BMP signaling [31]. When transplanted into mice, human intestinal organoids form tissue structures that closely resemble human intestinal epithelium, maintaining appropriate regional specificity (small intestinal vs. colonic characteristics) [31].
Liver Organoids
Generation Strategies and Key Features: Liver organoids can be generated through multiple approaches, including from tissue-derived liver cells (hepatocytes or cholangiocytes) or via differentiation of pluripotent stem cells [26]. Early liver organoid systems primarily utilized cholangiocyte organoids derived from biliary epithelial cells, which could be expanded long-term and differentiated toward hepatocyte-like cells [26]. More recent advances have enabled the direct expansion of primary hepatocytes as organoids, better maintaining their mature functional characteristics [26].
Liver organoids typically exhibit key hepatic functions, including albumin secretion, urea production, drug metabolism, and bile acid synthesis [26]. Advanced culture conditions incorporating factors like triiodothyronine (T3) have enabled the generation of more mature hepatocyte organoids (MHOs) with enhanced metabolic capabilities that more closely resemble adult human liver [26]. These improvements have significantly increased the utility of liver organoids for modeling liver diseases, drug screening, and studying liver regeneration.
Validation Against In Vivo Development: Liver organoids derived from adult tissue maintain the genetic and functional characteristics of their tissue of origin, including disease-specific phenotypes when generated from patients with genetic liver disorders [26]. For example, organoids from patients with alpha 1-antitrypsin deficiency or Alagille syndrome successfully mirror the pathological features observed in these patients [26].
Transcriptomic analyses have demonstrated that advanced liver organoid models closely match the gene expression profiles of primary human hepatocytes, particularly for genes involved in key metabolic pathways [26]. Functional validation studies have shown that liver organoids can perform essential hepatocyte functions at levels comparable to primary hepatocytes, including cytochrome P450 activity, albumin secretion, and LDL uptake [26]. When transplanted into mouse models of liver disease, liver organoids have been shown to integrate into the host liver and provide functional improvement, further validating their physiological relevance [26].
Table: Liver Organoid Functional Validation
| Functional Parameter | Validation Results | Physiological Relevance |
|---|---|---|
| Albumin Secretion | Only 2-4 folds lower than primary human hepatocytes [26] | Maintains key synthetic function of hepatocytes |
| Drug Metabolism | CYP450 activity demonstrated [26] | Capable of pharmaceutical compound processing |
| Maturation State | Transcriptome similar to adult liver with T3 supplementation [26] | Recapitulates mature hepatocyte phenotype |
| Disease Modeling | Mirrors pathology of A1AT deficiency and Alagille syndrome [26] | Preserves patient-specific disease phenotypes |
| In Vivo Function | Engraftment and functional improvement in mouse models [26] | Demonstrates physiological relevance |
Cancer Organoids
Generation Strategies and Key Features: Cancer organoids, particularly patient-derived organoids (PDOs), have emerged as powerful tools for modeling tumor biology and advancing precision oncology. These organoids are generated directly from patient tumor samples and can be expanded while preserving the genetic and phenotypic characteristics of the original tumor [32] [5]. Cancer organoids have been successfully established from various cancer types, including colorectal, pancreatic, liver, breast, and prostate cancers [32] [33].
Cancer organoids maintain the histological architecture, genetic heterogeneity, and drug response profiles of the tumors from which they are derived [5]. They can be used to model tumor-stroma interactions, particularly when co-cultured with cancer-associated fibroblasts (CAFs) or immune cells [33]. Recent advances have enabled high-throughput drug screening using cancer organoids, allowing for the identification of patient-specific therapeutic responses and resistance mechanisms [32].
Validation Against In Vivo Development: Extensive genomic analyses have confirmed that cancer PDOs retain the mutational profiles, copy number variations, and gene expression patterns of their parent tumors, even after extended in vitro culture [5]. This genetic stability makes them valuable models for studying tumor evolution and clonal dynamics.
Multiple studies have demonstrated strong correlation between drug responses in cancer organoids and clinical outcomes in patients, validating their predictive value for treatment selection [32]. For example, in colorectal cancer, organoid drug sensitivity testing has shown high concordance with patient responses to chemotherapy, targeted therapies, and immunotherapies [5]. Cancer organoids have also been shown to maintain tumor-specific features such as hypoxia gradients, metabolic profiles, and stem cell hierarchies that resemble in vivo tumors [33].
Experimental Protocols for Organoid Generation
Brain Organoid Generation Protocol
The generation of multi-region brain organoids (MRBOs) involves a sophisticated multi-step process [29]:
Neural Induction: hPSCs are aggregated into embryoid bodies in low-attachment plates using neural induction media containing TGF-β/NODAL and WNT inhibitors to promote neural ectoderm formation.
Regional Specification: Neural progenitors are patterned toward specific brain regions using region-specific morphogens:
- Forebrain: Combined treatment with WNT and SHH inhibitors
- Midbrain: FGF8 and SHH activation
- Hindbrain: WNT and FGF activation
- Cortical: Sequential treatment with WNT and BMP inhibitors
3D Matrigel Embedding: Patterned neural progenitors are embedded in Matrigel droplets to support 3D organization and expansion.
Tissue Fusion: Separately generated region-specific organoids are combined using biological adhesives to create multi-region complexes that establish functional connections.
Maturation: Fused organoids are maintained in spinning bioreactors or agitated cultures with optimized media to promote neuronal differentiation, synaptogenesis, and network formation over 8-16 weeks.
The entire process takes approximately 10-20 weeks, resulting in organoids containing 6-7 million neurons with emerging regional identities, electrophysiological activity, and rudimentary blood-brain barrier formation [29].
Liver Organoid Generation Protocol
Liver organoids can be generated from either primary tissues or pluripotent stem cells using distinct protocols [26]:
Tissue-Derived Liver Organoids:
- Tissue Dissociation: Human liver biopsies are enzymatically digested to single cells or small clusters using collagenase-based solutions.
Epithelial Cell Enrichment: Hepatocytes or cholangiocytes are isolated using density centrifugation or magnetic-activated cell sorting (for EpCAM+ cells).
3D Culture Setup: Isolated liver cells are embedded in growth factor-reduced Matrigel and cultured in expansion media containing:
- Essential niche factors: EGF, HGF, FGF, R-spondin
- TGF-β pathway inhibition (A83-01)
- cAMP activation (forskolin)
- Wnt pathway activation
Organoid Expansion: Cultures are maintained with weekly passaging, with organoids typically appearing within 1-2 weeks and expanding for several months.
Hepatocyte Differentiation: For cholangiocyte-derived organoids, hepatocyte differentiation is induced by modifying media to include BMP, FGF, and HGF while withdrawing Wnt agonists [26].
PSC-Derived Liver Organoids:
- Definitive Endoderm Induction: hPSCs are directed toward definitive endoderm using Activin A with Wnt3a for 3 days.
Hepatic Endoderm Specification: Cells are treated with BMP4 and FGF2 to induce hepatic endoderm formation (5-7 days).
Hepatoblast Expansion: Hepatic endoderm cells are expanded as 3D organoids in media containing HGF, FGF, and niche factors.
Hepatocyte Maturation: Organoids are matured using advanced media supplements including T3, dexamethasone, and maturation factors to enhance functional characteristics [26].
Signaling Pathways in Organoid Development
The successful generation and maintenance of organoids require precise recapitulation of key developmental signaling pathways. These pathways regulate stem cell self-renewal, lineage specification, and tissue patterning in organoid cultures, mirroring their roles in vivo.
Key Signaling Pathways in Organoid Development
This diagram illustrates the essential signaling pathways active across different organoid systems and their primary functions in organoid development and maintenance. The conservation of these pathways across organoid types highlights their fundamental roles in tissue development and homeostasis.
Research Reagent Solutions for Organoid Culture
Table: Essential Reagents for Organoid Research
| Reagent Category | Specific Examples | Function in Organoid Culture |
|---|---|---|
| Basal Media | Advanced DMEM/F12, B-27 Supplement, N-2 Supplement | Provides nutritional base and essential factors for stem cell maintenance |
| Growth Factors | EGF, FGF, HGF, R-spondin, Noggin, Wnt3a | Mimics niche signaling for proliferation and patterning |
| Extracellular Matrix | Matrigel, Collagen I, Laminin, dECM scaffolds | Provides 3D structural support and biochemical cues |
| Signaling Inhibitors A83-01 (TGF-β inhibitor), CHIR99021 (GSK3 inhibitor), LDN193189 (BMP inhibitor) | Controls differentiation and maintains stemness | |
| Differentiation Factors | Activin A, BMP4, FGF4, FGF10, Retinoic Acid | Directs lineage specification and tissue maturation |
| Metabolic Supplements | N-acetylcysteine, B27, N2, Lipid concentrates | Supports energy metabolism and specialized functions |
| Antibiotics | Primocin, Penicillin-Streptomycin, Normocin | Prevents microbial contamination in long-term cultures |
| Dissociation Reagents | Accutase, TrypLE, Dispase, Collagenase | Enables organoid passaging and single-cell applications |
The selection and optimization of culture reagents are critical for successful organoid generation and maintenance. Different organoid types require specific combinations of growth factors and signaling modulators to recapitulate their respective tissue niches [26] [5] [30]. For example, intestinal organoids require Wnt agonists, R-spondin, and Noggin for long-term expansion, while brain organoids need neural induction factors and patterning morphogens [31] [28]. Recent advances include the development of chemically defined matrices as alternatives to animal-derived Matrigel, improving reproducibility and translational potential [5].
Applications in Disease Modeling and Drug Development
Organoid technology has transformed biomedical research by providing human-relevant models for studying disease mechanisms and therapeutic interventions. The applications span basic research, drug discovery, and personalized medicine approaches.
Disease Modeling: Organoids have been particularly valuable for modeling human genetic disorders, infectious diseases, and cancer. Brain organoids have successfully recapitulated key pathological features of neurodegenerative diseases like Alzheimer's, Parkinson's, and Huntington's disease, including protein aggregation, neuronal loss, and synaptic dysfunction [28]. Similarly, liver organoids from patients with genetic metabolic disorders have mirrored disease-specific phenotypes, enabling study of disease mechanisms and drug testing [26]. Cancer PDOs have proven exceptional tools for investigating tumor heterogeneity, drug resistance mechanisms, and tumor-microenvironment interactions [32] [33].
Drug Development and Screening: Organoids have significantly impacted the drug development pipeline by providing more predictive models for efficacy and toxicity testing. The high failure rate of neuropsychiatric drugs (approximately 96% in Phase 1 clinical trials) underscores the limitations of animal models for predicting human responses [29]. Brain organoids offer a human-based system for evaluating neurotoxicity and blood-brain barrier penetration early in drug development. Similarly, liver organoids provide platforms for predicting drug-induced liver injury, a major cause of drug attrition [26]. The capacity for high-throughput screening using organoid arrays has accelerated compound screening and lead optimization processes [32] [5].
Personalized Medicine: Cancer PDOs have emerged as powerful tools for personalized oncology, enabling functional testing of therapeutic responses in patient-specific models. Clinical studies have demonstrated that PDO drug sensitivity testing can predict patient responses to chemotherapy, targeted therapies, and immunotherapies with high accuracy [32]. This approach holds promise for guiding treatment selection and identifying resistance mechanisms in individual patients. Similarly, organoids from patients with genetic disorders allow for personalized drug testing and therapeutic optimization [26] [28].
Organoid technology represents a paradigm shift in biomedical research, providing unprecedented opportunities to study human biology and disease in physiologically relevant models. The comparative analysis presented in this guide demonstrates that brain, intestinal, liver, and cancer organoids each offer unique advantages while sharing the common ability to recapitulate key aspects of their corresponding in vivo tissues. Validation studies across multiple organoid systems have consistently shown that these models maintain tissue-specific architecture, cellular heterogeneity, and functional capabilities that closely mirror their native counterparts.
While significant progress has been made in organoid technology, challenges remain in achieving full physiological maturity, incorporating all relevant cell types (particularly vascular and immune components), and enhancing reproducibility across laboratories. Ongoing advances in bioengineering, including organ-on-a-chip platforms, 3D bioprinting, and improved biomaterials, are addressing these limitations and pushing the boundaries of organoid complexity and functionality [32] [5].
As organoid technology continues to evolve, these models are poised to play an increasingly central role in basic research, drug development, and clinical medicine. Their ability to bridge the gap between traditional cell culture and animal models makes them invaluable tools for understanding human biology and disease, ultimately accelerating the development of more effective and personalized therapies.
From Theory to Practice: Advanced Applications in Disease Modeling and Drug Development
Patient-Derived Organoids (PDOs) for Personalized Therapy Selection
The high failure rate of anticancer drugs in clinical trials, exceeding 85% in some estimates, underscores a critical gap between traditional preclinical models and human pathophysiology [3]. Patient-derived organoids (PDOs) have emerged as transformative three-dimensional (3D) ex vivo models that bridge this translational gap by faithfully retaining the genetic, phenotypic, and functional characteristics of original patient tumors [14] [34]. This guide provides a comparative analysis of PDO performance against established models, detailing experimental protocols and validation data that position PDOs as essential tools for therapy selection within precision oncology frameworks.
The fundamental strength of PDOs lies in their ability to mimic in vivo development and disease states. By conserving the cellular composition and architecture of native tissues, they provide a physiologically relevant platform for assessing drug sensitivity and resistance mechanisms [34]. For drug development professionals, this translates to improved clinical predictivity at the preclinical stage, enabling more reliable go/no-go decisions and reducing late-stage attrition.
Model Comparison: PDOs Versus Alternative Preclinical Platforms
Performance Metrics Across Model Types
Different preclinical models offer varying advantages and limitations for drug development applications. The table below provides a systematic comparison of key performance characteristics.
Table 1: Comparative analysis of preclinical cancer models
| Model Characteristic | 2D Cell Cultures | Patient-Derived Xenografts (PDXs) | Patient-Derived Organoids (PDOs) |
|---|---|---|---|
| Architectural Complexity | Low (monolayer) [35] | High (in vivo context) [36] | Moderate to High (3D structure) [14] [37] |
| Genetic Stability | Low (clonal selection) [34] | High [36] | High (long-term culture) [36] [34] |
| Tumor Microenvironment | Absent or limited | Preserved (murine stroma) | Modifiable (co-culture possible) [14] [34] |
| Throughput Capacity | High | Low (costly, time-consuming) [36] [37] | Medium to High [36] |
| Timeline for Establishment | Weeks | 6+ months [38] | 2-3 weeks [38] |
| Clinical Predictive Value | Variable, often poor [34] | High (>90% correlation) [36] | High (76% accuracy) [14] |
| Cost Efficiency | High | Low | Medium [36] |
Validation Against Clinical Responses
The validation of PDOs against actual patient outcomes provides the most compelling evidence for their clinical relevance. The following table summarizes quantitative data from multiple studies across different cancer types.
Table 2: PDO predictive performance across cancer types
| Cancer Type | Therapeutic Class | Correlation with Patient Response | Key Metrics | Citation |
|---|---|---|---|---|
| Colorectal Cancer (CRC) | Chemotherapy, Targeted therapy | 76% overall accuracy | Sensitivity: 0.79, Specificity: 0.75 | [14] |
| Metastatic CRC | Irinotecan-based chemotherapy | >80% predictive accuracy | Prevented misclassification of potential responders | [35] |
| Pancreatic Ductal Adenocarcinoma (PDAC) | 111 FDA-approved drugs | High PDO-PDOX concordance | Correlation with clinical outcomes | [39] |
| Ovarian Cancer | Platinum-based therapy | Reliably reflected patient sensitivity | Distinguished sensitive/resistant/refractory cases | [37] |
| Multiple Cancers | Various (PDX-derived organoids) | >90% biological equivalency | High correlation with matched PDX drug response | [36] |
Experimental Protocols for PDO-Based Therapeutic Screening
Core Methodology for PDO Establishment and Drug Screening
The standard workflow for generating and utilizing PDOs in therapy selection involves multiple critical stages, each requiring specific technical expertise and quality control measures.
Tissue Processing and Digestion: Surgical specimens or biopsy materials are washed with PBS and subjected to enzymatic digestion using specialized kits (e.g., human tumor dissociation kit from Miltenyi Biotec) [39]. The resulting cell suspension is filtered through 100-micron strainers to remove large fragments, and viable cells are counted.
Matrix Embedding and Culture: Dissociated cells are embedded in ice-cold extracellular matrix (ECM) substitutes like Matrigel (Corning) or other gelatinous protein mixtures [39] [37]. After polymerization at 37°C, the matrix is overlaid with organoid-specific culture medium. The precise composition varies by cancer type but typically includes:
- Advanced DMEM/F12 as basal medium
- Wnt pathway agonists (e.g., Wnt3A-conditioned medium)
- R-spondin-1 (ligand for LGR5 receptor)
- Noggin (BMP pathway inhibitor)
- Epidermal Growth Factor (EGF)
- N-acetylcysteine (antioxidant)
- A83-01 (TGF-β inhibitor)
- Y-27632 (ROCK inhibitor, prevents anoikis) [39] [34]
Expansion and Biobanking: Organoids are typically passaged every 1-2 weeks using enzymatic or mechanical dissociation [39]. For long-term storage, organoids are cryopreserved in medium containing 90% FBS and 10% DMSO, maintaining viability and characteristics in liquid nitrogen [39].
Advanced Functional Drug Screening Protocols
High-Throughput Screening Platforms: For comprehensive drug profiling, PDOs are seeded in standardized sizes (350-450μm) into multi-well plates for systematic exposure to therapeutic agents [14]. The Therapeutically-Guided Multidrug Optimization (TGMO) platform enables efficient screening of single agents and combination therapies across concentration gradients [14].
Viability and Response Assessment:
- CellTiter-Glo 3D Assay: Measures ATP content as a viability indicator, with strong correlation to cell numbers (R² = 0.988) [40]
- High-Content Imaging: Automated microscopy coupled with AI-based analysis tools like OrgaExtractor quantifies morphological changes [40]
- Immunohistochemical Analysis: Marker expression (Ki67, CA19-9, CEA, PD-L1) evaluated in formalin-fixed paraffin-embedded organoid sections [39]
Combination Therapy Evaluation: PDOs enable systematic optimization of multi-drug regimens. For example, the TGMO platform has been applied to screen combinations of tyrosine kinase inhibitors (e.g., regorafenib, vemurafenib, palbociclib, lapatinib) at low doses, achieving up to 88% reduction in PDO viability [14].
The Researcher's Toolkit: Essential Reagents and Technologies
Table 3: Essential research reagents and platforms for PDO applications
| Reagent/Technology Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Extracellular Matrices | Matrigel (Corning) [39] | Provides 3D structural support for organoid growth | Lot-to-lot variability requires quality control |
| Culture Medium Additives | Wnt3A, R-spondin-1, Noggin [34], N-acetylcysteine [39] | Maintain stemness and support proliferation | Conditioned media or recombinant proteins |
| Dissociation Reagents | TrypLE (Gibco) [37], Tumor Dissociation Kits (Miltenyi) [39] | Break down organoids for passaging or analysis | Enzymatic composition varies by tissue type |
| Viability Assays | CellTiter-Glo 3D [40] | Quantify metabolic activity/cell viability | Optimized for 3D structures |
| Imaging & Analysis | OrgaExtractor (AI tool) [40], Two-photon microscopy [41] | Automated organoid segmentation and analysis | Enables high-content screening |
| Specialized Media | Advanced DMEM/F12 [39], B-27 Supplement [39] | Base nutrient medium | Formulations specific to organoid cultures |
Key Signaling Pathways in PDO Biology and Therapeutic Targeting
The maintenance and drug response of PDOs are governed by critical signaling pathways that represent both therapeutic targets and essential culture requirements.
Wnt/β-catenin Pathway: Serves as a master regulator of stem cell maintenance. In colorectal cancer PDOs, Wnt signaling is essential for long-term culture, often provided via Wnt3A-conditioned medium [34]. Therapeutic targeting of this pathway demonstrates differential effects based on mutational status.
EGFR Signaling: Epidermal Growth Factor receptor signaling drives proliferation in many epithelial cancers. PDOs retain expression of EGFR family members, making them responsive to targeted inhibitors like lapatinib [14].
BMP/TGF-β Pathways: Bone Morphogenetic Protein signaling is typically inhibited in PDO cultures (via Noggin) to prevent differentiation [34]. TGF-β inhibition (using A83-01) helps maintain proliferation in certain cancer types.
MAPK and PI3K Pathways: Critical for growth and survival signaling, these pathways are frequently dysregulated in cancers. PDOs have been instrumental in validating combination therapies targeting MEK and PI3K in tumors with relevant mutations [14].
Future Directions and Implementation Challenges
Current Limitations and Developing Solutions
Despite their promise, PDO implementation faces several challenges that active research seeks to address:
Tumor Microenvironment Complexity: Early PDO cultures primarily contained epithelial components, lacking full immune and stromal context. Newer co-culture systems now incorporate cancer-associated fibroblasts, immune cells (PBMCs), and engineered immune cells (CAR-T, CAR-M) to better model immunotherapy responses [39] [34].
Standardization and Scalability: Organoid culture variability presents challenges for reproducible drug screening. Emerging solutions include:
- Automated platforms with AI-driven image analysis (e.g., OrgaExtractor) [40] [3]
- Microfluidic organ-on-chip technologies that enhance physiological relevance and reproducibility [3]
- Vascularization strategies to improve nutrient delivery and mimic metastatic processes [3]
Clinical Integration Timelines: While PDO establishment requires approximately 2-3 weeks—significantly faster than PDX models (6+ months)—this timeline still presents challenges for immediate treatment decisions in aggressive cancers [38]. Ongoing efforts focus on protocol optimization to further reduce this timeframe.
Emerging Applications and Concluding Outlook
The evolution of PDO technology continues to open new applications in personalized oncology:
- Functional precision medicine platforms that complement genomic profiling
- Living organoid biobanks representing diverse patient populations for population-level drug discovery [34]
- Radiation sensitivity testing using specialized organoid culture protocols [35]
- Microenvironment engineering to study metastasis and therapy resistance mechanisms
As the field addresses current limitations through technological innovation, PDOs are poised to become increasingly central in preclinical drug development and clinical therapy selection. Their demonstrated ability to recapitulate patient-specific treatment responses positions them as invaluable tools for realizing the promise of precision oncology, ultimately helping to match the right therapies with the right patients.
The pursuit of physiologically relevant in vitro models has long been a challenge in biomedical research. Traditional two-dimensional cell cultures and animal models have significant limitations in recapitulating human-specific disease processes, creating a translational gap between preclinical studies and clinical outcomes. The emergence of three-dimensional organoid technology represents a paradigm shift in disease modeling, offering unprecedented opportunities to mirror human organ development and pathology in a controlled laboratory environment. Organoids are three-dimensional structures derived from stem cells that self-organize to mimic key aspects of human tissue architecture, cellular heterogeneity, and functionality [42] [43]. This review provides a comprehensive comparison of organoid models across disease categories, with particular focus on their validation against in vivo developmental processes and their growing impact on drug discovery and personalized medicine.
The validation of organoid models against in vivo development remains a crucial endeavor. Research demonstrates that human brain organoids feature transcriptional profiles and neurodevelopmental trajectories that closely resemble fetal brain development, providing a powerful tool for studying patterning and specification of various neuronal and glial cell types [42]. Similarly, intestinal organoids develop crypt-villus structures, and cerebral organoids form neuroepithelial units resembling developing ventricles, producing their own cells and morphogen gradients [42] [44]. This faithful recapitulation of developmental processes provides the foundation for their application in disease modeling, where pathological processes often represent aberrations of normal development or homeostasis.
Comparative Analysis of Organoid Models Across Disease Categories
Neurodegenerative Disease Modeling
Brain organoids have emerged as particularly valuable for studying neurodegenerative disorders like Alzheimer's disease (AD) and Parkinson's disease (PD), conditions notoriously difficult to model in non-human systems due to their human-specific pathophysiology. Compared to animal models, brain organoids provide more physiologically relevant data, capturing key cellular and molecular aspects of these diseases [42]. Studies using iPSC-derived cortical neurons from AD patients have demonstrated increased Aβ42:40 ratios and distinct signatures for Aβ43, Aβ38, and other Aβ fragments in both 2D and 3D cultures [43]. Similarly, dopaminergic neurons derived from PD patients' iPSCs reveal disease-related phenotypes including impaired mitochondrial function, increased oxidative stress, enhanced apoptosis, and α-synuclein accumulation [43].
Table 1: Performance Metrics of Brain Organoid Models for Neurodegenerative Disease Research
| Model Characteristic | Traditional 2D Models | Animal Models | Organoid Models |
|---|---|---|---|
| Recapitulation of human pathology | Limited cellular complexity | Species-specific differences | Closely mimics human fetal brain development [42] |
| Cellular diversity | Primarily homogeneous populations | Complete but non-human system | Multiple neural and glial cell types [42] |
| Drug screening predictive value | ~5% clinical translation [42] | ~5% regulatory approval rate [42] | Improved physiological relevance for preclinical research [42] |
| Model variability | Low | Moderate | High, but improving with protocol standardization [3] |
| Aβ pathology modeling | Basic Aβ production | Limited human Aβ specificity | Patient-specific Aβ profiles [43] |
| α-synuclein accumulation | Overexpression artifacts | Species-specific processing | Native human protein handling [43] |
Cancer Modeling
Patient-derived cancer organoids (PDOs) have transformed oncological research by preserving the genetic and phenotypic heterogeneity of original tumors. In cholangiocarcinoma, organoids retain the expression profiles, genetic mutations, and histological features of individual patients, demonstrating remarkable heterogeneity that mirrors the clinical variability observed in patients [45]. Drug response testing on patient-derived liver cancer organoid lines has revealed significant inter-patient functional heterogeneity, with similar variability found in organoids derived from different regions of the same cancer resection, highlighting their capacity to capture intra-tumoral heterogeneity [45]. This fidelity makes cancer organoids particularly valuable for personalized therapeutic screening, as they can predict individual patient responses to chemotherapeutic agents.
Table 2: Cancer Organoid Model Applications and Validation
| Cancer Type | Organoid Characteristics | Drug Screening Applications | Validation Against Clinical Response |
|---|---|---|---|
| Cholangiocarcinoma | Retains patient-specific mutations and histology [45] | Personalized treatment testing [45] | High inter- and intra-patient heterogeneity recapitulation [45] |
| Liver Cancer | Multiple phenotypes: hollow spheres, compact structures, irregular cysts [45] | 129 chemotherapeutic compounds tested [45] | Functional heterogeneity matching clinical variability [45] |
| Pancreatic Cancer | Brightfield/phase-contrast compatible for automated imaging [46] | Dose-response experiments with morphology readouts [46] | Automated analysis correlates with manual quantification (97% size agreement) [46] |
| Lung, Colon, Adenoid Carcinoma | Cross-tissue type applicability [46] | High-throughput screening compatible | Validation across multiple organ systems without parameter adjustment [46] |
Infectious Disease Modeling
While the search results provided limited specific examples of infectious disease modeling, organoids have shown significant promise for studying host-pathogen interactions, particularly for pathogens that exhibit human-specific tropism. The capacity of organoids to emulate human tissue architecture and cellular composition provides an ideal platform for investigating infectious mechanisms that cannot be adequately studied in animal models or traditional cell cultures. The integration of organoids with organ-on-chip technology further advances infection modeling by incorporating fluidic flow and mechanical cues that enhance cellular differentiation and polarized architecture, critical for studying entry mechanisms of pathogens [3].
Advanced Methodologies in Organoid Research
Experimental Protocols for Organoid Generation and Analysis
Protocol 1: Cerebral Organoid Generation from iPSCs
The generation of cerebral organoids follows a sequential differentiation protocol that mimics in vivo neurodevelopment [42] [44]:
- iPSC Maintenance: Human iPSCs are maintained in essential 8 medium on Matrigel-coated plates until 80-90% confluent.
- Embryoid Body Formation: iPSCs are dissociated with Accutase and transferred to low-attachment plates in embryoid body medium (DMEM/F12, 20% KOSR, 2-mercaptoethanol, non-essential amino acids).
- Neural Induction: After 5 days, embryoid bodies are transferred to neural induction medium (DMEM/F12, 1% N2 supplement, heparin) for 7 days.
- Matrix Embedding: Neural ectoderm structures are embedded in Matrigel droplets and allowed to solidify at 37°C.
- Organoid Maturation: Embedded structures are transferred to organoid differentiation medium (DMEM/F12, 1% B27 supplement, insulin) in spinning bioreactors for extended culture (up to several months).
- Medium Supplementation: For enhanced neuronal maturation, BDNF is added after day 40 of culture [44].
Protocol 2: Whole-Organoid Immunostaining and Clearing
Comprehensive organoid analysis requires specialized tissue processing to overcome light scattering in thick tissues [44]:
- Fixation: Organoids are fixed in 4% PFA for 30-60 minutes at room temperature.
- SHIELD Processing: Samples are treated with poly-epoxide crosslinker (SHIELD reagent) to preserve tissue architecture and biomolecules during delipidation.
- Permeabilization: Organoids are permeabilized with 0.5% Triton X-100 for 24-48 hours.
- Antibody Staining: Primary antibodies (e.g., SOX2, TBR1, MAP2) are applied for 48-72 hours, followed by secondary antibodies for 24-48 hours.
- Optical Clearing: Samples are immersed in PROTOS-based solution (histodenz in TDE) for refractive index matching.
- Imaging: Cleared organoids are imaged using light-sheet fluorescence microscopy with axially sweeping acquisition at 0.65 × 0.65 × 2.00 µm voxel size.
Protocol 3: Automated Organoid Imaging and Analysis
High-throughput organoid screening requires automated imaging and analysis pipelines [46] [44]:
- Image Acquisition: Brightfield/phase-contrast or fluorescence images acquired at regular intervals (15 min - 24 hours).
- OrganoID Processing: Convolutional neural network (U-Net architecture) detects organoids pixel-by-pixel.
- Single-Organoid Tracking: Identification module resolves contours to label individual organoids; tracking module follows organoids over time.
- Morphometric Analysis: Quantification of organoid count, size, circularity, solidity, and eccentricity.
- Dose-Response Analysis: Morphological changes are correlated with treatment conditions.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Organoid Technology
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| Matrigel | Extracellular matrix providing structural support and signaling cues | Intestinal, cerebral, and pancreatic organoid culture [42] |
| mTeSR1/Essential 8 | iPSC maintenance media | Pluripotent stem cell culture for organoid initiation [42] |
| Dual SMAD Inhibitors | Neural induction by inhibiting BMP and TGF-β pathways | Cerebral organoid patterning [44] |
| SHIELD Reagent | Tissue clearing and preservation | Whole-organoid immunostaining and imaging [44] |
| OrganoID | Automated image analysis platform | High-throughput organoid quantification and tracking [46] |
| 3DCellScope | 3D segmentation and analysis software | Multiscale phenotyping of organoid morphology [47] |
| Z1-FEP Cuvette | Specialized sample holder for light-sheet microscopy | Long-term live imaging of organoids [45] |
Analytical Frameworks and Computational Tools
The complexity of organoid systems demands sophisticated computational approaches for data extraction and interpretation. Several platforms have been developed to address the challenges of 3D data analysis:
SCOUT (Single-cell and Cytoarchitecture analysis of Organoids using Unbiased Techniques): This computational pipeline enables automated multiscale phenotyping of intact cerebral organoids, extracting hundreds of features characterizing molecular, cellular, spatial, cytoarchitectural, and organoid-wide properties from fluorescence microscopy datasets [44]. The platform employs curvature-based seeded watershed algorithms for nuclear detection (90% accuracy) and proximity scoring to quantify spatial relationships between different cell types.
OrganoID: A robust image analysis platform that automatically recognizes, labels, and tracks single organoids in brightfield and phase-contrast microscopy experiments [46]. The system uses a modified U-Net convolutional neural network with 98% fewer parameters than the original implementation, achieving 95% agreement with manual organoid count and 97% agreement with manual size measurements without parameter adjustments.
MultiOrg Dataset: A comprehensive resource for benchmarking organoid detection algorithms, comprising over 400 high-resolution microscopy images with curated annotations of more than 60,000 organoids [48]. The dataset includes three label sets independently annotated by two experts at different time points, enabling quantification of annotation uncertainty and label noise.
The following diagram illustrates the integrated workflow for multiscale organoid analysis, from sample preparation to computational phenotyping:
Workflow for Multiscale Organoid Analysis
Current Limitations and Future Directions
Despite their significant promise, organoid technologies face several challenges that must be addressed to fully realize their potential. Key limitations include:
Technical Challenges: Organoids exhibit considerable variability in size, shape, and cellular composition between batches, complicating experimental reproducibility [3]. The lack of vascularization limits nutrient diffusion, leading to necrotic cores in larger organoids and restricting their size and maturity [42] [3]. Most cerebral organoids exhibit a fetal phenotype, which may not fully capture adult disease processes [3].
Standardization and Scaling: The labor-intensive nature of organoid culture and analysis has hindered high-throughput applications. However, advances in automation and AI are addressing these limitations. Nearly 40% of scientists currently use complex models like organoids, with usage expected to double by 2028 [3]. Integrated platforms combining automated culture systems with AI-powered image analysis are improving reproducibility and scalability.
Future Developments: The field is moving toward enhanced physiological relevance through vascularization, immune component integration, and multi-tissue systems. The integration of organoids with organ-on-chip technology provides microenvironments with fluidic flow and mechanical cues that enhance cellular differentiation and function [3]. Assay-ready, validated organoid models that undergo rigorous testing and characterization are becoming increasingly available, providing researchers with more standardized and reliable tools [3].
The following diagram illustrates the key signaling pathways and cellular interactions involved in organoid development and disease modeling:
Signaling Pathways in Organoid Development and Disease
Organoid technology has fundamentally transformed our approach to modeling complex human diseases, providing an unprecedented window into human-specific biological processes. The validation of these models against in vivo development has strengthened their utility for studying disease mechanisms, screening therapeutic compounds, and advancing personalized medicine. While challenges remain in standardization, vascularization, and maturation, ongoing innovations in bioengineering, computational analysis, and multi-system integration are rapidly addressing these limitations. As the field continues to evolve, organoid models are poised to bridge the critical gap between traditional preclinical models and human clinical trials, ultimately accelerating the development of effective therapies for neurodegenerative disorders, cancer, and infectious diseases. The continued refinement and validation of organoid systems against in vivo biology will ensure their growing impact on biomedical research and therapeutic development.
High-Throughput Drug Screening and Toxicity Assessment
High-throughput screening (HTS) represents a foundational approach in modern drug discovery, enabling the rapid testing of thousands of chemical compounds against biological targets to identify potential therapeutic candidates [49]. Traditionally applied to simplified two-dimensional (2D) cell cultures and biochemical assays, HTS has significantly accelerated early drug discovery phases by leveraging robotics, detectors, and sophisticated software to conduct extensive analyses in remarkably short timeframes [49]. The implementation of automation has elevated screening capabilities to extraordinary levels, with ultra-high-throughput screening (UHTS) platforms now capable of processing up to 100,000 compounds daily [49]. This technological evolution has been characterized by progressive miniaturization, transitioning from 96-well plates to 384-well, 1536-well, and even 3456-well formats with working volumes as low as 1-2 μL, dramatically reducing reagent costs and compound requirements [49].
Despite these advancements, traditional HTS approaches face significant limitations in predictive accuracy, particularly concerning human-specific toxicological responses and complex tissue-level dynamics. The pharmaceutical industry continues to contend with high clinical trial failure rates exceeding 85%, often due to safety and efficacy concerns that remain undetected in conventional models [3]. This predictive gap has stimulated the development of more physiologically relevant models, notably three-dimensional (3D) organoid systems that better mimic the structural and functional properties of human organs [50] [3]. This guide provides a comprehensive comparison of established and emerging HTS platforms for toxicity assessment, with particular emphasis on the validation of organoid models against in vivo development research—a critical frontier in improving the predictive accuracy of preclinical safety assessment.
Comparative Analysis of Screening Platforms
Technical Specifications and Performance Metrics
Table 1: Comparative analysis of high-throughput screening platforms for toxicity assessment
| Platform Characteristic | Traditional 2D HTS | Organoid-Based Screening | In Vivo Models |
|---|---|---|---|
| Throughput Capacity | 10,000-100,000 compounds/day [49] | Medium throughput, improving with automation [3] | Very low throughput |
| Physiological Relevance | Limited cell-to-cell contacts, lacks tissue architecture [51] | Recapitulates tissue architecture and cellular composition [51] | High physiological relevance, but species differences exist [50] |
| Human Specificity | Variable (cell line-dependent) | High, especially with patient-derived organoids [3] | Limited due to interspecies differences [50] |
| Toxicity Prediction Accuracy | Moderate, often misses organ-specific toxicity [49] | Emerging evidence for improved prediction [51] | Variable predictive value for human toxicity [50] |
| Compound Requirement | 1-3 mg for toxicity studies [49] | Similar minimal requirements | Significantly higher compound amounts needed |
| Cost Considerations | Lower per compound, but high overall due to false positives | Moderate, decreasing with technology improvements [3] | Very high, including ethical considerations |
| Regulatory Acceptance | Well-established for early screening | Increasing acceptance with FDA Modernization Act 2.0 [3] | Gold standard for regulatory submissions |
| Multiparameter Readouts | Limited in standard formats | Excellent for complex phenotypic assessment [52] | Comprehensive but requires multiple animals |
Applications in Toxicity Assessment
Each platform offers distinct advantages for specific toxicity assessment applications. Traditional HTS excels in identifying modulators of drug-metabolizing enzymes, evaluating genotoxicity, and screening against channel and receptor targets [49]. Its robust automation and standardized protocols make it ideal for primary screening campaigns where throughput is paramount. However, its simplified biological systems often fail to detect complex toxicological responses manifesting at tissue or organ levels.
Organoid-based screening platforms address this limitation by preserving tissue architecture and cellular heterogeneity, enabling more accurate prediction of human-specific toxicities [50]. Recent advances have demonstrated particular utility in neurotoxicity assessment, where the complex cellular organization of the central nervous system presents unique challenges for traditional models [50]. Neural organoids replicate structural and functional properties of human brain tissue, providing unprecedented opportunities to evaluate developmental neurotoxicity—a endpoint particularly difficult to assess in animal models due to interspecies differences in brain development [50].
Table 2: Toxicity assessment capabilities across platform types
| Toxicity Type | Traditional HTS | Organoid-Based Screening | In Vivo Models |
|---|---|---|---|
| Cytotoxicity | Strong capability with high reproducibility | Excellent, with tissue context [51] | Comprehensive but requires terminal endpoints |
| Organ-Specific Toxicity | Limited to cellular mechanisms | High for modeled organs [50] [3] | Comprehensive but species-specific |
| Developmental Toxicity | Limited relevance | Promising for neurodevelopment [50] | Established standard with species limitations |
| Genotoxicity | Well-established assays [49] | Emerging capabilities | Comprehensive but indirect measures |
| Metabolic Toxicity | Hepatic cell lines available | Improved with hepatocyte organoids [49] | Physiologically relevant but species-specific |
| Cardiotoxicity | hERG channel screening standard | Emerging with cardiac organoids | ECG in whole animals |
Experimental Protocols for Platform Validation
Standard HTS Protocol for Toxicity Screening
Traditional high-throughput screening for toxicity assessment follows a well-established workflow [49]:
- Target Identification: Selection of biologically relevant targets implicated in toxicological responses.
- Reagent Preparation: Optimization and validation of assay components, including enzymes, cell lines, and detection reagents.
- Compound Management: Preparation of compound libraries in appropriate solvent systems compatible with screening formats.
- Assay Development: Optimization of assay parameters including cell density, incubation times, and reagent concentrations using statistical design of experiments.
- Primary Screening: Implementation of automated screening protocols in microtiter plates (96- to 1536-well formats) with appropriate controls.
- Hit Identification: Selection of compounds showing significant activity based on predetermined thresholds.
- Secondary Screening: Concentration-response studies to determine IC50 values and confirmatory assays in more physiologically relevant systems.
- Data Analysis: Normalization, quality control assessment, and cheminformatic analysis of screening results.
This process typically employs either heterogeneous assays (involving multiple steps like filtration, centrifugation, and fluid addition) or homogeneous assays (simpler, single-step procedures), with each format offering distinct advantages in sensitivity versus convenience [49].
Organoid-Based Screening Protocol
The establishment of robust organoid screening platforms requires specialized methodologies to maintain 3D architecture while enabling reproducible high-content analysis [51]:
Organoid Culture Protocol [50] [51]:
- Stem Cell Expansion: Maintain human pluripotent stem cells (hPSCs), including embryonic stem cells (hESCs) or induced pluripotent stem cells (hiPSCs), in defined culture conditions.
- 3D Differentiation: Embed stem cell aggregates in extracellular matrix (Matrigel) and initiate differentiation using specific patterning factors. For neural organoids, this typically begins with dual SMAD inhibition to induce neuroectodermal fate [50].
- Regional Patterning: Apply specific morphogens to direct regional identity along anterior-posterior and dorsal-ventral axes. For example, forebrain organoids utilize WNT inhibition, while midbrain organoids require WNT activation and SHH signaling [50].
- Maturation Culture: Maintain organoids for extended periods (weeks to months) with appropriate trophic support (BDNF, NT-3) to promote neuronal maturation and circuit formation [50].
- Quality Control: Implement rigorous batch validation through morphological assessment, viability staining, and transcriptomic analysis to ensure reproducibility.
Screening Implementation [51]:
- Organoid Seeding: Transfer size-matched organoids to 96- or 384-well plates in minimal Matrigel volumes (4-10μL) at standardized densities (50-100 organoids/well).
- Compound Treatment: Apply test compounds across concentration ranges (typically 1nM-100μM) with appropriate vehicle controls.
- Viability Assessment: After treatment period (typically 3-10 days), stain with fluorescent viability indicators:
- Calcein-AM: Cell-permeable dye converted to fluorescent calcein by esterase activity in living cells (ex/em: 495/515nm) [51].
- Propidium Iodide: DNA-binding dye excluded by intact plasma membranes, selectively staining dead cells (ex/em: 535/617nm).
- Optional: Include nuclear counterstain (Hoechst 33342) for total cell quantification.
- Image Acquisition: Implement Z-stack imaging to capture entire organoid volume throughout Matrigel, typically acquiring 10-30 focal planes at 10-50μm intervals [51].
- Image Analysis: Utilize automated algorithms for organoid counting, size measurement, and fluorescence quantification. Maximum intensity projections of Z-stacks enable accurate assessment of total organoid viability.
Advanced Computational Analysis with compaRe
The complexity of multiparameter data generated from HTS, particularly in organoid systems, necessitates advanced computational tools. The compaRe toolkit addresses this challenge by providing [52]:
- Quality Control Modules: Identification and correction of technical artifacts including edge effects, signal drift, and cell viability drift.
- Mass-Aware Gridding Algorithm: Measures similarity between samples by dividing high-dimensional space into hypercubes and comparing data point distributions.
- Clustering Module: Identifies samples with similar response profiles using graph-based algorithms that prune false positive edges based on negative controls.
- Visualization Tools: Enables intuitive exploration of complex multiparameter datasets and clustering results.
compaRe demonstrates particular utility in analyzing high-throughput flow cytometry data from drug-treated samples, robustly identifying both dramatic and subtle phenotypic response patterns that might escape conventional analysis methods [52].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential research reagents for high-throughput screening and toxicity assessment
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Extracellular Matrices | Matrigel, Collagen I, Synthetic hydrogels | Provides 3D scaffolding for organoid growth and polarization [51] |
| Patterning Factors | BMP4, CHIR99021 (WNT activator), SHH, FGFs, Retinoic acid | Directs regional specification of organoids along body axes [50] |
| Cell Viability Indicators | Calcein-AM, Propidium Iodide, CFDA SE, Neutral Red | Distinguishes live/dead cells and quantifies viability in 2D and 3D cultures [51] |
| Cell Line Sources | Immortalized lines (2D), hPSCs, hESCs, hiPSCs, Patient-derived organoids | Provides biologically relevant screening platforms [50] [3] |
| Detection Reagents | Fluorescent antibodies, Aptamers, Enzyme substrates | Enables multiplexed parameter readouts in HTS [49] |
| Culture Supplements | B27, N2, Growth factors (EGF, Noggin, R-spondin) | Supports stem cell maintenance and directed differentiation [51] |
| Computational Tools | compaRe toolkit, ImageJ macros, Urban Institute R packages | Analyzes complex multiparameter screening data [52] [53] |
Signaling Pathways in Neural Organoid Development
The development of region-specific neural organoids requires precise manipulation of evolutionarily conserved signaling pathways that pattern the embryonic nervous system. Understanding these pathways is essential for generating physiologically relevant models for neurotoxicity assessment [50].
Key Pathway Manipulations [50]:
- Dual SMAD Inhibition: Simultaneous inhibition of TGF-β and BMP signaling directs cells toward default anterior neuroectodermal fate, forming the foundation for most neural organoid protocols.
- Anterior-Posterior Patterning: WNT signaling levels determine positional identity along the anterior-posterior axis, with low WNT promoting forebrain fate and progressively higher WNT signaling inducing midbrain, hindbrain, and spinal cord identities.
- Dorsal-Ventral Patterning: BMP signaling promotes dorsal characteristics while sonic hedgehog (SHH) signaling induces ventral fates. The precise concentration and timing of these morphogens generate specific neuronal subtypes.
- Neuromesodermal Progenitors: For spinal cord organoids, induction of NMPs rather than neuroectoderm is required, followed by posteriorization with FGF and retinoic acid signaling [50].
These pathway manipulations enable generation of region-specific neural organoids that recapitulate fundamental aspects of human brain development, providing unprecedented models for assessing developmental neurotoxicity.
The evolving landscape of high-throughput screening for toxicity assessment reflects a strategic shift toward more physiologically relevant models that better predict human responses. While traditional HTS remains invaluable for primary screening campaigns due to its unparalleled throughput and reproducibility, organoid-based platforms offer transformative potential for secondary screening and mechanistic toxicology studies. The validation of these models against in vivo development data represents a critical research priority, with emerging evidence supporting their improved predictive accuracy for human-specific toxicities [50] [3].
Future directions point toward increased integration of organoid systems with advanced engineering platforms such as organ-on-chip technologies, which provide dynamic microenvironments and multi-tissue interactions [3]. Additionally, the incorporation of immune cells, vascularization, and broader representation of human genetic diversity through patient-derived organoids will further enhance the physiological relevance and predictive power of these systems [3]. As computational tools like compaRe continue to evolve in parallel with these biological advances [52], the field moves closer to a comprehensive framework for toxicity assessment that combines the throughput of traditional HTS with the physiological relevance of organoid systems and the contextual understanding of in vivo studies—ultimately accelerating the development of safer, more effective therapeutics.
The pursuit of physiologically relevant in vitro models is a central goal in modern cancer research, driving the need for robust validation against in vivo development. Traditional tumor organoids have revolutionized the field by mimicking structural and genetic features of primary tumors, but their lack of a complex tumor microenvironment (TIME) has limited their predictive power [54]. The TIME is a critical determinant of tumor behavior, treatment response, and immune evasion, composed of immune cells, cancer-associated fibroblasts (CAFs), vascular networks, and extracellular matrix (ECM) components [55] [56]. To bridge this gap, innovative co-culture systems that integrate immune cells with tumor organoids have emerged as transformative tools. These systems aim to recapitulate the dynamic interplay between tumors and the immune system, providing a more accurate platform for studying immunotherapy mechanisms, drug screening, and personalized treatment strategies [54] [57]. This guide objectively compares the performance of leading co-culture platforms, detailing their experimental protocols, analytical outputs, and utility in validating findings against in vivo biology.
Co-Culture Platform Comparison
Researchers can select from several established platforms to build co-culture models, each with distinct advantages and limitations. The table below summarizes the key characteristics of the most prominent systems.
Table 1: Performance Comparison of Co-Culture Model Platforms
| Platform Type | Key Features | Model System | Primary Applications | Technical Complexity |
|---|---|---|---|---|
| Matrix-Based Direct Co-culture | Cells co-embedded in ECM scaffolds (e.g., Matrigel, BME); enables direct cell-cell contact [54]. | Tumor organoids + T cells [54]. | Study of immune cell infiltration, cytotoxicity, and immunotherapy evaluation [54]. | Medium |
| Microfluidic "Organ-on-a-Chip" | Micro-channels simulate fluid flow, mechanical stress, and nutrient gradients; allows for multi-tissue integration [57] [58]. | Immune System-on-a-Chip (ISOC) [57]. | Analysis of immune cell trafficking, metastatic cascades, and systemic drug responses [57]. | High |
| Scaffold-Free Spheroid Co-culture | Cells aggregate without ECM support via forced floating techniques; forms nutrient/oxygen gradients [55]. | Multicellular Tumor Spheroids (MCTS) with stromal cells [55]. | Drug penetration studies, hypoxia research, and basic cell-cell interaction analysis [55]. | Low-Medium |
| Gel-Liquid Interface Co-culture | Organoids embedded in gel interfacing with liquid medium containing immune cells; uses specialized chips [54]. | Lung cancer organoids + T cells on superhydrophobic microwell array chips [54]. | Precision immunotherapy diagnostics and mechanistic studies of immune activation [54]. | High |
Experimental Protocols for Key Co-Culture Applications
Protocol 1: Establishing a Direct Tumor Organoid-T Cell Co-Culture
This protocol is adapted from studies involving cholangiocarcinoma and pancreatic ductal adenocarcinoma organoids, designed to assess T-cell mediated cytotoxicity [54].
Workflow Diagram: Direct Tumor Organoid-T Cell Co-Culture
Materials & Reagents:
- Tumor tissue sample: Minimally necrotic tissue from tumor margin is optimal [54].
- Extracellular Matrix (ECM): Growth Factor Reduced Matrigel or Basement Membrane Extract (BME) [54] [55].
- Digestion enzymes: Collagenase or Dispase for tissue dissociation.
- Basal medium: Advanced DMEM/F12.
- Essential growth factors:
- T-cell culture supplements: IL-2, anti-CD3/CD28 antibodies for activation.
Procedure:
- Tumor Organoid Generation:
- Mechanically dissociate and enzymatically digest the tumor sample to create a single-cell suspension [54].
- Seed the cell suspension onto pre-chilled ECM and polymerize at 37°C.
- Overlay with organoid culture medium supplemented with growth factors (e.g., Wnt3A, R-spondin-1, Noggin, EGF). Refresh medium every 2-3 days [54].
- Allow organoids to mature for 1-2 weeks, with passaging every 7-14 days.
Immune Cell Preparation:
- Isolate Peripheral Blood Mononuclear Cells (PBMCs) from donor blood via density gradient centrifugation.
- Isolate T cells from PBMCs using negative selection kits.
- Activate T cells using plate-bound anti-CD3/anti-CD28 antibodies and expand in culture medium containing IL-2 (100 IU/mL) for 5-7 days [54].
Co-culture Establishment and Analysis:
- Harvest mature tumor organoids, gently dissociate if needed, and mix with activated T cells at a predetermined effector-to-target ratio (e.g., 10:1).
- Seed the co-culture in a fresh ECM droplet or a low-attachment plate.
- Monitor the culture for 3-7 days, analyzing outcomes via:
Protocol 2: Microfluidic Immune-Tumor Co-Culture Platform
This protocol leverages microfluidic technology to create dynamic, physiologically relevant models for studying systemic interactions [57].
Workflow Diagram: Microfluidic Immune-Tumor Co-Culture
Materials & Reagents:
- Microfluidic device: Commercially available or custom-fabricated ISOC platform [57].
- Peristaltic or syringe pump: For generating controlled fluid flow.
- Specialized medium: For simultaneous support of tumor and immune cells.
- Live-cell imaging setup: For real-time monitoring.
Procedure:
- Device Priming:
- Sterilize the microfluidic device (e.g., UV light, ethanol).
- Prime the device channels with PBS to remove air bubbles.
- Coat the tumor chamber with ECM and allow to polymerize.
Cell Loading and System Initiation:
- Load pre-formed tumor organoids into the ECM-coated main chamber.
- Load fluorescently labeled immune cells (e.g., T cells, monocytes) into the designated inlet chamber.
- Connect the device to the perfusion system and initiate flow at a physiologically low rate (e.g., 0.1-1 µL/min).
Monitoring and Analysis:
- Maintain the system for up to several weeks, periodically collecting effluent for analysis.
- Use time-lapse microscopy to track immune cell migration toward and within the tumor compartment.
- Analyze effluent for cytokine secretion (e.g., IFN-γ, IL-6) via ELISA or multiplex assays.
- At endpoint, fix and stain the entire device for confocal imaging to assess immune cell infiltration and spatial relationships.
Analytical Techniques for Model Validation
Robust validation is crucial to confirm that co-culture models faithfully replicate in vivo biology. The following table outlines key analytical methods and their applications.
Table 2: Key Analytical Techniques for Co-Culture Model Validation
| Analytical Technique | Primary Application in Co-Culture | Measurable Outputs | Compatibility with Platform |
|---|---|---|---|
| Flow Cytometry | Immunophenotyping, viability assessment, checkpoint receptor expression [54]. | Percentage of immune cell subsets, apoptosis (Annexin V), activation markers (CD69, CD25) [54]. | All platforms. |
| Confocal/Time-Lapse Imaging | Visualizing spatial interactions, tracking cell motility, and verifying infiltration [54]. | 3D reconstructions of immune-tumor contacts, killer cell velocity, organoid degradation over time [54]. | Matrix-based, Microfluidic. |
| Cytokine Profiling (ELISA/MSD) | Quantifying secreted immune signals and chemokines [54] [59]. | Concentration of IFN-γ, TNF-α, IL-6, IL-10, etc., in supernatant [54]. | All platforms. |
| ATP-based Viability Assays | High-throughput assessment of tumor cell killing [54]. | Luminescence values correlating with viable tumor cell mass [54]. | All platforms, best for endpoint. |
| RNA Sequencing (scRNA-seq) | Uncovering transcriptomic changes and heterogeneity in tumor and immune cells [54] [56]. | Differential gene expression, pathway analysis (e.g., exhaustion, inflammation) [56]. | All platforms (requires cell sorting). |
| Mass Spectrometry (MS) Imaging | Spatial mapping of protein distributions within the 3D model [55]. | Relative abundance and location of key proteins (e.g., PD-L1, granzymes) [55]. | Matrix-based spheroids/organoids. |
Signaling Pathways in the Engineered TIME
Co-culture systems recapitulate critical in vivo signaling pathways that govern immune cell function and tumor survival. Understanding these pathways is essential for interpreting experimental results.
Pathway Diagram: Key Immune-Tumor Interactions in Co-Culture
The diagram above illustrates the major signaling axes operating in a co-culture system:
- Cytotoxic Killing: Successful T-cell recognition of tumor antigen via the TCR-MHC interaction leads to IFN-γ release and tumor cell death [59].
- Immunosuppressive Checkpoint: Tumor cell upregulation of PD-L1 engages PD-1 on T cells, transmitting an inhibitory signal that leads to T-cell exhaustion and loss of effector function [56] [59]. Suppressive cytokines like TGF-β further dampen the immune response.
- Metabolic Reprogramming: Tumor-derived lactate creates localized acidosis, while enzymes like ARG1 from myeloid cells deplete essential nutrients, collectively impairing T-cell function and proliferation [56] [60].
The Scientist's Toolkit: Essential Research Reagents
Successful establishment and maintenance of complex co-culture models rely on a defined set of high-quality reagents.
Table 3: Essential Reagents for Tumor-Immune Co-Culture Research
| Reagent Category | Specific Examples | Critical Function | Validation Tip |
|---|---|---|---|
| Growth Factors & Cytokines | R-spondin 1, Noggin, EGF, FGF10, Wnt3A [54] [2]. | Maintain stem cell niche and support organoid growth and viability [2]. | Verify bioactivity via reporter assays (e.g., TCF for R-spondin 1) [2]. |
| Extracellular Matrices (ECM) | Growth Factor Reduced Matrigel, Basement Membrane Extract (BME), Collagen I [54] [55]. | Provide 3D structural support and biochemical cues mimicking the in vivo basement membrane [54] [55]. | Be aware of lot-to-lay variability; perform pilot experiments with new lots. |
| Immune Cell Activators | Recombinant IL-2, anti-human CD3/CD28 antibodies [54]. | Activate and expand T cells ex vivo prior to co-culture, enhancing their cytotoxic potential. | Titrate antibodies and cytokines to avoid over-activation and activation-induced cell death. |
| Cell Culture Media | Advanced DMEM/F12 base, supplemented with B27, N2, N-Acetylcysteine [54]. | Provide nutritional and hormonal support for both epithelial and immune cell components. | Use dedicated medium for organoid growth and immune cell growth, optimizing for co-culture. |
| Analysis Reagents | Fluorescent antibodies for flow cytometry, cell viability assay kits (ATP), cytokine ELISA kits [54]. | Enable quantitative assessment of model outcomes (killing, exhaustion, activation). | Use validated antibody panels and include isotype controls for accurate phenotyping. |
The integration of immune cells into tumor organoid models via advanced co-culture systems represents a significant leap forward in our ability to model human cancer in vitro. As detailed in this guide, platforms ranging from simple matrix-based co-cultures to sophisticated microfluidic chips offer complementary strengths for validating biological mechanisms against in vivo benchmarks. The critical signaling pathways, such as immune checkpoint activation and metabolic crosstalk, can be effectively modeled and quantified using these systems. While challenges remain—including standardization, scalability, and the full recapitulation of TIME cellular diversity [3]—these innovative models are already enhancing the predictive accuracy of drug screening and are paving the way for more effective, personalized immunotherapies. The ongoing refinement of these protocols, coupled with rigorous analytical validation, ensures their growing centrality in translational cancer research.
Organoid Biobanking and the Push for Standardization
Organoid technology has emerged as a transformative tool in biomedical research, creating three-dimensional structures that replicate the architecture and functionality of human tissues. These sophisticated models have become indispensable for disease modeling, drug discovery, and personalized medicine [61]. However, the complex nature of organoids presents unique challenges for consistent production and reliable experimentation. Unlike traditional cell culture methods, organoids exhibit complex structures, cellular diversity, and functional resemblance to native tissues, creating a pressing need for standardized biobanking practices to ensure quality, reproducibility, and ethical use [61].
The absence of standardized protocols has led to significant challenges in the field, including variability in sample quality, regulatory and ethical concerns, limited interoperability and data sharing, and barriers to clinical translation [61]. Recognizing these challenges, the International Standard for Organoid Biobanking (ISoOR-ISOB) was officially released in 2025 as the first global framework dedicated to ensuring consistency, reproducibility, and quality in organoid biobanking [61]. This standardization initiative lays a solid foundation for advancing organoid research and therapeutic development, addressing key challenges that have historically hindered reproducibility and compromised data reliability.
Within the context of validating organoid models against in vivo development research, standardization becomes particularly crucial. As the field moves toward using organoids as predictive models for human physiology and drug response, establishing standardized biobanking practices ensures that results obtained from organoid studies can be reliably correlated with in vivo outcomes. This alignment is essential for building scientific confidence in organoid technology and accelerating its translation from basic research to clinical applications.
The Standardization Landscape: Frameworks and Initiatives
International Standard for Organoid Biobanking (ISoOR-ISOB)
The ISoOR-ISOB represents a groundbreaking effort to establish a unified global framework for organoid biobanking. Released during the ISoOR 2025 Annual Meeting in Shanghai, this comprehensive standard defines best practices for the entire organoid biobanking workflow, including sample collection, processing, storage, quality control, traceability, and ethical considerations [61]. By harmonizing biobanking practices worldwide, this framework enhances data comparability, supports regulatory compliance, and fosters global collaboration among researchers, clinicians, and industry partners [61].
The rationale for developing ISoOR-ISOB stems from the rapid advancement of organoid technology over the past decade and the concomitant need for standardized practices. Maintaining organoid viability requires specialized handling, precise storage conditions, and rigorous characterization protocols that traditional cell culture methods cannot provide [61]. Without standardized procedures, discrepancies in cultivation, preservation, and quality control inevitably arise, leading to variations in research outcomes that hinder reproducibility and slow the translation of organoid-based discoveries into clinical applications [61].
Current Implementation Status and Market Growth
The implementation of standardized organoid biobanking practices is progressing at a rapid pace, with significant growth in both academic and commercial sectors. The biobank organoids market was valued at $126.9 million in 2024 and is projected to reach $220.6 million by 2032, reflecting a steady expansion across research and clinical sectors [62]. This growth is driven by increasing recognition of organoids' value in drug screening and disease modeling, particularly tissue-derived organoids that currently dominate the market due to their high biological fidelity [62].
Regionally, North America has maintained the largest share of the biobank organoids market, supported by advanced research infrastructure, high R&D investment, and strong pharmaceutical industry presence [62]. Key players in the market include Merck KGaA, HUB Organoids, Crown Bioscience, Thermo Fisher Scientific, and STEMCELL Technologies, all of which are actively engaged in strategic acquisitions and service development to advance standardized organoid biobanking [62].
Table: Global Organoid Biobank Initiatives and Their Specializations
| Institution/Initiative | Biobank Specialization | Scale and Key Features |
|---|---|---|
| Hubrecht Institute/UMC Utrecht | Comprehensive multi-organ biobank [63] | 1,000+ organoids from various organs and diseases [63] |
| Hans Clevers' Team | Colorectal cancer organoids [63] | 90% success rate; >80% post-resuscitation survival [63] |
| Vlachogiannis et al. | Metastatic gastrointestinal cancers [63] | 110 tissues from 71 patients; works with low tumor/stromal ratio [63] |
| Yao et al. | Locally advanced rectal cancer [63] | Predicts response to chemoradiotherapy (84.43% accuracy) [63] |
| Various Academic Groups | Breast cancer organoids [64] | Multiple biobanks ranging from 33 to 100 patients [64] |
Experimental Validation: Protocols for Quality Assessment
Standardized Protocols for Organoid Construction and Culture
Standardized operation and management in all steps of organoid construction is crucial for ensuring high-quality products [65]. The process begins with sample acquisition through enzymatic and mechanical dissociation of fresh tumor tissues or stem cell sources, followed by embedding in specialized matrices that support three-dimensional growth [64]. Essential soluble factors must be carefully controlled, with R-spondin 1, Noggin, and Epidermal Growth Factor (EGF) representing critical components for maintaining stem cell proliferation and preventing differentiation in various organoid types [2].
The integration of automation and artificial intelligence has emerged as a powerful approach to address reproducibility challenges in organoid culture. Recent surveys indicate that nearly 40% of scientists currently rely on complex human-relevant models like organoids, with usage expected to double by 2028 [3]. Solutions combining automation and AI can standardize protocols to reduce variability and remove human bias from decision-making, ensuring cells receive precisely what they need to consistently mature into reliable models [3]. This technological advancement is particularly valuable for creating assay-ready, validated models that have undergone rigorous testing and characterization to confirm they accurately mimic biological processes, behaviors, and responses of cells in living organisms [3].
Quantitative Assessment of Drug Response
Validating organoid models against in vivo development requires robust quantitative assessment methods. For drug screening applications, several parameters are routinely measured to evaluate treatment efficacy. These include comparative analysis of organoid surface area, live cell counts, and volume-based growth rates under different treatment conditions [64]. Additionally, evaluation of three-dimensional morphological changes, particularly sphericity and ellipticity parameters, provides fundamental insights into drug response mechanisms [64].
ATP-based cell viability assays offer a standardized approach for quantifying treatment effects across different organoid types. Studies have demonstrated that using highly validated growth factors including EGF, Noggin, and R-spondin 1 significantly improves cell viability measurements compared to non-optimized media formulations [2]. This enhanced viability directly impacts the reliability of drug screening results, strengthening the correlation between organoid-based predictions and in vivo outcomes.
Table: Standardized Viability and Bioactivity Assessment of Critical Growth Factors
| Growth Factor | Validated Function in Organoid Culture | Quantitative Bioactivity (EC50) | Key Signaling Pathways |
|---|---|---|---|
| R-spondin 1 | Activates Wnt/β-catenin signaling; essential for stem cell maintenance [2] | 0.0138-0.0163 µg/mL (TCF reporter assay) [2] | Wnt/β-catenin signaling [2] |
| Epidermal Growth Factor (EGF) | Induces proliferative signaling; supports self-renewal [2] | ~56-fold induction (EGFR reporter assay) [2] | EGFR signaling cascade [2] |
| Noggin | Inhibits BMP signaling; prevents differentiation [2] | Essential for Lgr5 stem cell marker expression [2] | BMP signaling inhibition [2] |
Technical Workflows and Signaling Pathways
Core Signaling Pathways in Organoid Culture Maintenance
The maintenance of organoid cultures relies on precisely balanced signaling pathways that control the delicate equilibrium between stem cell self-renewal and differentiation. The diagram below illustrates the core signaling network that must be carefully regulated in standardized organoid culture systems.
This intricate signaling network highlights the critical molecular pathways that standardized culture protocols must maintain. R-spondin 1 enhances Wnt signaling by binding to LGR5 receptors and stabilizing β-catenin, which activates TCF/LEF-mediated transcription of genes responsible for stem cell self-renewal [2]. Simultaneously, Noggin inhibits BMP signaling by forming complexes with BMP ligands, preventing SMAD phosphorylation and subsequent differentiation signals [2]. Epidermal Growth Factor activates its receptor to initiate the RAS-MAPK cascade, driving cellular proliferation essential for organoid expansion [2]. The precise coordination of these pathways enables the long-term maintenance of organoids that faithfully recapitulate tissue physiology.
Standardized Workflow for Organoid Biobanking and Validation
A standardized workflow for establishing and validating organoid biobanks is essential for ensuring consistency across research institutions and commercial entities. The following diagram outlines key stages in this process, from sample acquisition to functional validation.
This standardized workflow encompasses three critical phases that ensure the establishment of high-quality, validated organoid biobanks. The sample processing phase begins with enzymatic and mechanical dissociation of source tissue, followed by embedding in specialized matrices and culture with standardized growth factors essential for three-dimensional growth [2] [64]. The quality control phase involves comprehensive assessment including morphological analysis, genomic characterization, and viability testing to confirm that organoids retain key features of parental tumors [63] [64]. Finally, the validation phase employs drug screening assays and correlation with in vivo outcomes to establish predictive value, completing the cycle that connects in vitro models to physiological relevance [64] [6].
Essential Research Reagents and Solutions
The successful implementation of standardized organoid biobanking relies on a carefully selected toolkit of research reagents and solutions. These components must meet stringent quality criteria to ensure batch-to-batch consistency and experimental reproducibility. The following table details essential materials required for establishing and maintaining high-quality organoid cultures.
Table: Essential Research Reagent Solutions for Organoid Biobanking
| Reagent Category | Specific Examples | Function in Organoid Culture | Validation Parameters |
|---|---|---|---|
| Critical Growth Factors | R-spondin 1, Noggin, EGF [2] | Maintain stemness, inhibit differentiation, promote proliferation [2] | Bioactivity (EC50), purity, endotoxin levels [2] |
| Specialized Matrices | Basement membrane extracts, synthetic hydrogels | Provide 3D scaffolding for organoid development | Lot-to-lot consistency, mechanical properties |
| Cell Sources | Tissue-derived stem cells, induced pluripotent stem cells (iPSCs) [63] | Source material for organoid generation | Viability, differentiation potential, marker expression |
| Quality Assessment Tools ATP-based assays, genomic analysis kits | Quantify viability, validate genetic fidelity | Sensitivity, reproducibility, accuracy |
These research reagents form the foundation of reliable organoid biobanking operations. Growth factors like R-spondin 1, Noggin, and EGF require rigorous validation for bioactivity, with established EC50 values of 0.0138-0.0163 µg/mL for R-spondin 1 in TCF reporter assays and approximately 56-fold induction for EGF in EGFR reporter assays [2]. The sourcing of these reagents from suppliers that provide consistently high purity, high bioactivity, and ultra-low endotoxin levels is critical for maintaining long-term organoid cultures across multiple passages [2]. Additionally, specialized matrices must demonstrate lot-to-lot consistency to ensure reproducible three-dimensional growth environments, while cell sources require thorough characterization of viability, differentiation potential, and marker expression to guarantee faithful recapitulation of tissue physiology.
The push for standardization in organoid biobanking represents a critical evolutionary step in the maturation of this transformative technology. The establishment of international standards like ISoOR-ISOB, coupled with rigorous validation protocols and essential reagent characterization, provides a solid foundation for advancing biomedical research and therapeutic development [61]. As the field continues to evolve, several key areas will demand focused attention, including the incorporation of immune components and vasculature, enhancement of scalability and automation, and the development of more sophisticated correlation studies with in vivo outcomes.
The successful implementation of standardized organoid biobanking practices will ultimately accelerate the translation of basic research findings into clinical applications. By ensuring consistency, reproducibility, and quality across institutions, researchers can more confidently utilize organoid models for disease modeling, drug screening, and personalized medicine approaches. The continued refinement of standardization protocols will strengthen the validation of organoid models against in vivo development, bridging the gap between experimental models and human physiology to advance biomedical discovery and therapeutic innovation.
Navigating Challenges: Strategies to Enhance Organoid Reproducibility and Complexity
Addressing Batch-to-Batch Variability and Scalability Issues
In the pursuit of validating organoid models against in vivo development, two of the most significant technical hurdles researchers face are batch-to-batch variability and limited scalability. These challenges impact experimental reproducibility, data reliability, and the translational potential of organoid technology. This guide objectively compares the performance of emerging technological solutions against conventional methods, providing a structured framework for selecting appropriate platforms based on specific research requirements.
Comparative Analysis of Scalability and Variability in Organoid Culture Platforms
The table below summarizes quantitative and qualitative performance metrics for established and emerging organoid culture platforms, highlighting their respective capabilities in addressing scalability and variability.
Table 1: Performance Comparison of Organoid Culture Platforms
| Platform Type | Scalability (Throughput Potential) | Reported Variability (Batch-to-Batch) | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Traditional Static Culture [66] [3] | Low to Medium | High | Low cost, technical simplicity, widely accessible [67] | High variability, diffusion-limited growth, manual intensive [66] [3] [68] |
| Stirred-Tank Bioreactors [3] [69] | High | Medium | Improved nutrient/waste exchange, bulk production capability [3] [69] | Shear stress on organoids, potential for aggregation, size consistency challenges [3] |
| Organoids-on-Chip [66] [69] | Medium to High | Low (with automation) | Precise microenvironment control, incorporation of physiological cues (e.g., flow, pressure) [66] | Higher initial cost, technical complexity, device-specific expertise [66] |
| Automated & AI-Integrated Platforms [3] [69] | High | Very Low | Protocol standardization, reduced human bias, real-time monitoring and adjustment [3] | Highest infrastructure investment, requires data science expertise [3] |
Experimental Protocols for Validation
To objectively compare these platforms, researchers must implement standardized validation protocols. The following sections detail key experimental workflows for assessing scalability and variability.
Protocol for Quantifying Batch-to-Batch Variability
This protocol is designed to generate quantitative data on the consistency of organoid morphology and key phenotypic markers across multiple production batches [5] [67].
1. Sample Preparation:
- Generate a minimum of three independent organoid batches per experimental platform being tested [67].
- Use a consistent cell source (e.g., same donor iPSC line or primary tissue sample) across all batches and platforms.
- Embed organoids in a standardized extracellular matrix (ECM) such as Matrigel, BME, or a defined synthetic hydrogel [67] [70].
2. Culture and Harvest:
- Culture all batches under their platform-specific optimal conditions but for a fixed duration (e.g., 21 days).
- Harvest organoids at a predetermined time point for analysis.
3. Data Acquisition and Analysis:
- Imaging: Capture high-resolution bright-field and confocal microscopy images of at least 30 organoids per batch.
- Morphometric Analysis: Use image analysis software (e.g., ImageJ) to quantify organoid diameter, circularity, and lumen formation.
- Immunofluorescence (IF): Stain sections for organoid-specific markers (e.g., LGR5 for intestinal stem cells, β-III-tubulin for neurons) [5].
- Quantification: Use IF image analysis to quantify the percentage of positive cells and the intensity of marker expression across batches.
- Statistical Analysis: Calculate the coefficient of variation (CV) for each morphometric and IF parameter across the batches for each platform. A lower CV indicates higher consistency and lower batch-to-batch variability.
Protocol for Assessing Scalability and Long-Term Expansion
This protocol evaluates the ability of a platform to support the large-scale, sustained growth of organoids, crucial for high-throughput screening [3] [69] [70].
1. Inoculation and Expansion:
- Start cultures from a defined, low cell number (e.g., 10,000 cells) across all platforms.
- Culture organoids over multiple passages (e.g., 5 passages or 60 days, whichever is longer).
2. Longitudinal Monitoring and Data Collection:
- Growth Kinetics: At each passage, quantify the total organoid yield and calculate the population doubling time.
- Viability Assessment: Use live/dead staining assays to quantify the percentage of viable cells within organoids over time, monitoring for necrotic core development [66] [71].
- Genomic Stability: Perform karyotype analysis or whole-genome sequencing at the beginning and end of the expansion period to assess the acquisition of genetic abnormalities [70]. Studies show adult stem cell-derived organoids can maintain genomic stability over long-term culture, a key advantage for scalability [70].
3. Functional Output Assay:
- At the endpoint, subject organoids from each platform to a standardized functional assay relevant to the organ type (e.g., albumin ELISA for liver organoids, calcium imaging for neuronal organoids).
- The throughput (number of organoids processed per unit time) and success rate of the assay serve as final scalability metrics.
Signaling Pathways in Guided Organoid Maturation
The reproducible differentiation of pluripotent stem cells into specific organoid types relies on the precise manipulation of key evolutionary signaling pathways. The diagram below illustrates the core pathways that must be controlled to reduce variability and ensure consistent lineage commitment.
Figure 1: Signaling Pathway Control for Neural Organoid Patterning. This diagram outlines the key developmental pathways manipulated in vitro to guide PSCs toward specific neural fates, a process critical for reducing heterogeneity in brain organoid generation [71]. Precise temporal control of these signals is a major differentiator between platform consistencies.
The Scientist's Toolkit: Essential Research Reagents
The consistent production of high-quality organoids is dependent on a standardized set of reagents and materials. The table below details critical components for robust organoid culture.
Table 2: Essential Reagents for Reproducible Organoid Research
| Reagent Category | Specific Examples | Function in Culture | Considerations for Reducing Variability |
|---|---|---|---|
| Extracellular Matrix (ECM) | Matrigel, BME, Geltrex, synthetic hydrogels [67] [70] | Provides 3D structural support, presents biochemical cues for cell polarization and organization. | Major source of batch effects. Mitigate by using GMP-grade or synthetic, defined matrices [69] [70]. |
| Growth Factors & Cytokines | R-spondin-1 (WNT agonist), Noggin (BMP inhibitor), EGF, FGF [5] [71] | Mimics the stem cell niche, directs lineage specification and maintains stemness. | Use recombinant proteins at standardized concentrations; pre-test new lots for activity. |
| Small Molecule Inhibitors/Activators | CHIR99021 (GSK3 inhibitor), Y-27632 (ROCK inhibitor), Forskolin [5] [70] | Precisely activates or inhibits key signaling pathways (e.g., WNT), enhances cell survival after passaging. | Preferred for stability and cost over recombinant proteins; validate concentration ranges. |
| Cell Dissociation Agents | TrypLE, Accutase, collagenase/hyaluronidase mixes [67] | Gentle enzymatic digestion for organoid passaging and single-cell isolation. | Optimize incubation time and concentration to minimize cell stress and death. |
| Basal Media Formulations | Advanced DMEM/F12, organ-specific differentiation media [67] [69] | Nutrient foundation, tailored to support metabolic needs of specific organoids. | Use chemically defined media without serum to improve reproducibility [69] [70]. |
Integrated Workflow for Reproducible Organoid Generation
Combining the elements above into a standardized workflow is key to success. The following diagram maps the integrated process from initiation to analysis, highlighting critical control points for minimizing variability.
Figure 2: Integrated Workflow for Reduced-Variability Organoid Culture. This workflow emphasizes iterative quality control (QC) at a critical checkpoint to ensure only cultures meeting predefined criteria for viability and marker expression proceed to differentiation, thereby enhancing final model consistency [67] [69].
Organoid technology represents a paradigm shift in biomedical research, providing unprecedented in vitro models of human development and disease. These three-dimensional structures are derived from stem cells and can recapitulate key architectural and functional aspects of their in vivo counterparts. However, a significant limitation persists: many organoids exhibit a fetal-like phenotype rather than maturing into fully adult tissues. This immaturity hampers their utility for studying adult-onset diseases and accurately predicting drug responses. The persistent fetal molecular signature, incomplete functional maturation, and lack of tissue-scale complexity present critical barriers that the field must overcome to realize the full potential of organoid technology. This guide examines the current state of organoid maturation research, comparing strategic approaches and their experimental validation to address this fundamental challenge.
The fetal phenotype in organoids manifests through multiple dimensions. Transcriptomic analyses often reveal gene expression patterns resembling first or second-trimester fetal development rather than adult tissues [72]. Physiologically, organoids may lack the coordinated functionality of mature organs, such as proper electrical signaling in neural organoids or metabolic competence in hepatic models. Structurally, the absence of key cell types, particularly vascular networks and immune cells, further perpetuates their immature state [3]. Overcoming these limitations requires sophisticated culture techniques that more accurately mimic the in vivo microenvironment and developmental cues.
Comparative Analysis of Organoid Maturation Strategies
Strategic Approaches to Enhance Organoid Maturity
Multiple innovative approaches are being developed to drive organoid maturation, each with distinct mechanisms, advantages, and limitations. The table below provides a comprehensive comparison of these strategies based on current research findings.
Table 1: Comparison of Organoid Maturation Strategies
| Strategy | Mechanism of Action | Key Experimental Findings | Maturation Markers Enhanced | Limitations |
|---|---|---|---|---|
| Extended Culture Duration | Allows natural developmental processes over time | Cerebral organoids show increased neural, glial, and vascular gene expression over 2-month differentiation [72] | Action potentials, multiple channel activities, drug response to propofol [72] | May never reach full maturity; necrosis in core [3] |
| Vascularization | Co-culture with endothelial cells; fluid flow exposure | Enhanced nutrient delivery; enables larger organoid size [3] | Improved gas exchange; reduced necrosis [3] | Technical complexity; immune component often missing [3] |
| Organoid-Organ-Chip Integration | Provides mechanical cues, fluid flow, and tissue-tissue interfaces | Enables well-polarized cell architecture; enhances cellular differentiation [3] | Functional tissue responses; drug absorption capability [3] | High cost; requires specialized equipment [3] |
| Bioreactor Systems | Dynamic culture with improved nutrient/waste exchange | Stirred bioreactors improve diffusion and scale up production [3] | Increased organoid size and uniformity [3] | Shear stress on cells; requires optimization [3] |
| Patient-Derived Cells | Uses tissue-specific stem cells rather than iPSCs | Amniotic fluid-derived epithelial progenitors form tissue-specific organoids [73] | Transcriptomic, protein expression, and functional features of native tissue [73] | Limited starting material; lower throughput [3] |
| CRISPR-based Genetic Engineering | Introduces specific genetic modifications to induce maturation | Used to introduce disease phenotypes into patient-derived organoids [3] | Disease-relevant pathological features [3] | Potential off-target effects; may not reflect natural maturation |
Quantitative Assessment of Maturation Outcomes
The effectiveness of maturation strategies can be quantified through multiple experimental parameters. The following table synthesizes key metrics from recent studies that demonstrate successful progression toward adult phenotypes.
Table 2: Quantitative Metrics for Assessing Organoid Maturation
| Maturation Parameter | Measurement Technique | Fetal Phenotype Signature | Mature Phenotype Achievement | Study Reference |
|---|---|---|---|---|
| Transcriptomic Profile | Bulk RNA sequencing; Single-cell RNA sequencing | Similar distance to fetal and adult brain tissues [72] | Colocalization with adult tissue-derived controls [73] | [72] [73] |
| Electrophysiological Function | Multi-electrode arrays; Patch clamping | Limited action potential generation [72] | Multiple channel activities; functional drug response [72] | [72] |
| Structural Organization | Immunofluorescence; X-ray phase-contrast CT | Crypt-like structures without full polarization [73] | Apical-basal polarization; tight junction formation [73] | [73] |
| Metabolic Capacity | Metabolic flux analysis; CYP activity assays | Limited drug metabolism functionality | Adult-like metabolic enzyme expression | [3] |
| Long-term Expansion | Passaging capacity; Cryopreservation success | Limited self-renewal (≤5 passages) | Expansion up to passage 20 [73] | [73] |
| Tissue-Specific Function | Tissue-specific functional assays | Immature functional responses | Organ-level functionality (e.g., nutrient absorption, filtration) [73] | [73] |
Experimental Protocols for Maturation Studies
Integrated Workflow for Organoid Maturation and Validation
The following diagram illustrates a comprehensive experimental workflow for generating mature organoids and validating their adult-like properties, integrating multiple strategies from the comparative analysis.
Experimental Workflow for Organoid Maturation and Validation
Detailed Methodologies for Key Maturation Techniques
Cerebral Organoid Culture and Electrophysiological Validation
The following protocol for generating and validating cerebral organoids demonstrates how extended culture duration contributes to functional maturation:
iPSC Culture and Initial Differentiation:
- Maintain human iPSCs on Matrigel-coated plates in mTESR1 medium under hypoxic conditions (4% O₂) at 37°C [72]
- Upon reaching 80% confluency, passage cells with Versene solution
- For embryoid body formation, singularize iPSCs and resuspend in mTeSR1 medium
- Plate 12,000 cells per well (150 μL suspension) in 96-well ultra-low attachment plates
- Culture in normoxic conditions (21% O₂) at 37°C, changing media every other day for 6 days [72]
Organoid Maturation and Differentiation:
- On day 6, transfer embryoid bodies to 24-well low attachment plates
- Culture in neuroepithelial media (DMEM/F12, 1% N₂ Supplement, 1% glutamine, 1% nonessential amino acids, 1 μg/mL Heparin) for 5 days
- On day 11, embed neuroepithelial tissues in Matrigel droplets
- Plate on 100 mm plates in cerebral organoid differentiation media (DMEM/F12, Neurobasal media, 0.5% N₂ Supplement, 1% Glutamine, 0.5% nonessential amino acids, 1% penicillin/streptomycin, 1% B27 without vitamin A, 0.025% Insulin, 0.035% mercaptoethanol) for 5 days [72]
- On day 16, transfer to spinner flasks with cerebral organoid differentiation media supplemented with vitamin A
- Culture organoids for up to 2 months with regular media changes [72]
Functional Validation of Maturation:
- Analyze action potentials and channel activities using patch clamp electrophysiology
- Test functional electrophysiological responses to pharmacological agents such as propofol
- Validate neural, glial, and vascular-related gene expression increases over the 2-month differentiation course using qRT-PCR and RNA sequencing [72]
Amniotic Fluid-Derived Organoid Generation and Characterization
This protocol demonstrates an alternative approach using patient-derived cells that may exhibit more mature characteristics:
Sample Collection and Cell Isolation:
- Collect amniotic fluid (AF) from pregnancies (16-34 weeks gestational age)
- Isolate viable nucleated cells with intact cell membranes using fluorescence-activated cell sorting (FACS) [73]
- For single-cell RNA sequencing, process cells using 3' sequencing protocols
- Generate unsupervised Uniform Manifold Approximation and Projection (UMAP) using Seurat v.4 for cellular characterization [73]
Organoid Derivation and Clonal Expansion:
- Seed viable AF cells in Matrigel droplets using generic epithelial medium without tissue-specific signals
- Culture for 2 weeks until 3D organoids become visible
- For clonal lines, pick individual organoids, dissociate into single cells, and replate [73]
- Expand organoids up to passage 20 with cryopreservation at various passages
- Confirm clonal origin through single-cell AF epithelial cell culture [73]
Maturation Validation:
- Image distinct organoid morphologies through X-ray phase-contrast computed tomography (PC-CT)
- Confirm cell proliferation (Ki67 staining) and absence of apoptosis (cleaved caspase 3 staining)
- Validate epithelial identity (EpCAM, ECAD, pan-cytokeratin) and polarization (basolateral integrin β4, apical F-actin, ZO-1-positive tight junctions) [73]
- Conduct bulk RNA sequencing and principal component analysis to confirm tissue identity colocalization with control organoids
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful organoid maturation requires specific reagents and materials optimized for three-dimensional culture systems. The following table details essential components for establishing robust organoid maturation protocols.
Table 3: Essential Research Reagents for Organoid Maturation Studies
| Reagent/Material | Function | Example Application | Validation Requirement |
|---|---|---|---|
| Matrigel | Extracellular matrix substitute providing structural support | Organoid embedding; provides basement membrane components for polarization [72] [73] | Batch-to-batch consistency testing; growth factor content characterization |
| mTeSR1 Medium | Maintenance of pluripotent stem cells | Culture of iPSCs prior to organoid differentiation [72] | Pluripotency marker validation (OCT4, Nanog) |
| B-27 Supplement | Serum-free supplement for neural cultures | Cerebral organoid differentiation [72] | With/without vitamin A depending on differentiation stage |
| N-2 Supplement | Defined supplement for neural stem cell growth | Neuroepithelial specification phase [72] | Testing optimal concentration for specific cell lines |
| Y-27632 (ROCK inhibitor) | Prevents apoptosis in dissociated cells | Used during passaging of organoids [73] | Concentration optimization for specific organoid types |
| Recombinant Growth Factors | Direct lineage specification and maturation | EGF, FGF, Wnt agonists for patterning [73] | Dose-response validation for each organoid system |
| Organ-Chip Devices | Microfluidic platforms for physiological culture | Integration with organoids for enhanced maturation [3] | Compatibility testing with specific organoid types |
| Bioreactor Systems | Dynamic culture with improved gas/nutrient exchange | Scaling organoid production and maturation [3] | Shear stress optimization; oxygenation validation |
Signaling Pathways in Organoid Maturation
The following diagram illustrates key signaling pathways that must be properly regulated to overcome the fetal phenotype and drive organoid maturation, based on transcriptomic analyses of developing organoids.
Key Signaling Pathways in Organoid Maturation
Bioinformatics analyses comparing cerebral organoids with fetal and adult brain tissues have identified specific signaling pathways that are differentially regulated. Calcium signaling, cAMP response element-binding protein (CREB) signaling in neurons, glutamate receptor signaling, and synaptogenesis signaling are predicted to be downregulated in cerebral organoids relative to fetal samples [72]. Nearly all cerebral organoid and fetal pathway phenotypes are predicted to be downregulated compared with adult tissue, highlighting specific molecular pathways that must be targeted to achieve full maturation.
The pursuit of mature organoids that faithfully recapitulate adult human tissue functionality remains an active frontier in biomedical research. Current evidence suggests that integrated approaches combining extended culture duration, vascularization, organ-chip integration, and patient-derived cells show the most promise for overcoming the fetal phenotype. The validation of these strategies through transcriptomic, functional, and structural analyses provides a roadmap for researchers seeking to implement these techniques.
As the field progresses, key challenges including standardization, scalability, and the incorporation of immune components must be addressed [3]. The emergence of automated platforms and artificial intelligence for quality control promises to enhance reproducibility across laboratories [3]. Furthermore, the integration of organoids with organ-on-chip technologies presents an exciting avenue for introducing physiological cues that drive maturation [3]. These advances, coupled with the development of comprehensive maturation biomarkers, will ultimately strengthen the utility of organoids in disease modeling, drug development, and personalized medicine applications.
The field of organoid research has revolutionized biomedical science by providing three-dimensional (3D), self-organizing cellular structures that mimic key aspects of human organs [66]. These stem-cell derived tissues recapitulate structural and functional characteristics of their in vivo counterparts, enabling unprecedented opportunities for studying human development, disease mechanisms, and drug responses [42]. However, conventional organoid models face significant limitations in replicating the full complexity of living systems, particularly regarding the incorporation of vascular networks, neural connections, and multi-tissue interactions [3]. These missing elements represent critical barriers to advancing organoid technology from simplified models to truly physiologically relevant systems.
The validation of organoid models against in vivo development remains a central challenge in the field. While organoids demonstrate remarkable ability to self-organize and exhibit organ-specific functions, they often resemble fetal rather than adult tissues and lack the integrated systems necessary for long-term maturation and homeostasis [74]. This comparison guide examines current strategies for engineering greater complexity in organoid models, directly evaluating their performance against traditional in vivo research systems and highlighting the experimental evidence supporting their validation.
Model System Comparisons: Capabilities and Limitations
Comparative Analysis of Model Systems
Table 1: Comparative analysis of model systems for biomedical research
| Feature | 2D Models | Organoids | Animal Models |
|---|---|---|---|
| Architectural Complexity | Low (monolayer) | Moderate to High (3D structures) | High (native tissue context) |
| Cellular Diversity | Limited | Moderate (multiple cell types) | Complete (all native cells) |
| Vascularization | Absent | Limited (emerging techniques) | Complete (functional circulatory system) |
| Innervation | Absent | Limited (emerging techniques) | Complete (functional nervous system) |
| Inter-tissue Signaling | Limited | Moderate (co-culture systems) | Complete (systemic signaling) |
| Throughput | High | Moderate to High | Low |
| Human Genetic Relevance | Moderate (human cells) | High (human-derived) | Low (species differences) |
| Cost | Low | Moderate | High |
| Regulatory Considerations | Standard cell culture | Ethical committee approval | Animal committee approval [31] |
Performance Metrics for Vascularization and Innervation
Table 2: Quantitative assessment of vascularization and innervation capabilities across model systems
| Parameter | In Vivo (Human) | Animal Models | Advanced Organoids | Measurement Techniques |
|---|---|---|---|---|
| Vessel Density | 1000-2000 mm/mm³ (tissue-dependent) | Species-dependent | 100-500 mm/mm³ (in developing systems) | CD31/CD34 immunostaining, lectin perfusion [75] |
| Oxygen Diffusion Limit | Overcome by perfusion | Overcome by perfusion | 150-200 μm (limit without perfusion) | Oxygen microsensors, hypoxia markers [66] |
| Perfusion Efficiency | 100% (by definition) | 100% (by definition) | 10-30% (in perfused systems) | Fluorescent bead tracking, computational modeling |
| Neural Density | Tissue-specific | Species-specific | Emerging (minimal quantification) | β-III-tubulin, MAP2 staining, electrophysiology |
| Functional Connectivity | Complete neural circuits | Complete neural circuits | Limited synaptic networks | Calcium imaging, multi-electrode arrays |
| Drug Penetration | Physiological barriers | Species-specific barriers | Limited by diffusion | Mass spectrometry, fluorescence imaging |
Engineering Vascularization: Strategies and Experimental Validation
Vascularization Techniques and Performance Metrics
The establishment of functional vascular networks represents one of the most critical challenges in organoid engineering. In vivo tissues depend on vascular access for oxygen and nutrient delivery, with inadequate perfusion leading to central hypoxia and necrosis in organoids exceeding diffusion limits [75]. Multiple strategies have emerged to address this limitation, each with distinct advantages and experimental validation approaches.
Self-assembly vasculogenesis involves co-culturing organoid-forming cells with endothelial cells (such as human pluripotent stem cell-derived endothelial cells) and supporting pericytes or fibroblasts in 3D matrices. This approach leverages the innate ability of endothelial cells to form capillary-like networks when provided with appropriate angiogenic cues like VEGF, FGF2, and angiopoietins [75] [74]. Experimental validation typically includes immunostaining for endothelial markers (CD31, VE-cadherin), perfusion assays with fluorescently labeled lectins or dextrans, and assessment of barrier function through molecular tracer exclusion [75]. Quantitative analysis demonstrates that self-assembled networks can achieve vessel densities of 100-500 mm/mm³ in optimal conditions, though these often lack the hierarchical organization and perfusion capacity of native vasculature [74].
Organ-on-chip technology provides a complementary approach by incorporating microfluidic channels that can be lined with endothelial cells to create perfusable vascular networks [66] [76]. These systems enable precise control over flow conditions, shear stress, and pressure parameters that influence vascular maturation and function. The technology typically involves fabricating microfluidic devices using photolithography or 3D printing, seeding endothelial cells in patterned channels, and establishing physiologically relevant flow conditions using pump systems [76]. Experimental validation of these models includes measuring solute transport across endothelial barriers, assessing vascular responsiveness to pharmacological agents, and quantifying the expression of mechanosensitive genes in response to fluid shear stress [66].
In vivo transplantation represents a third approach, where organoids are implanted into immunocompromised animal models (commonly mouse anterior chamber, kidney capsule, or subcutaneous sites) to enable host-derived vascularization [31]. This method leverages the host's intact angiogenic capacity to infiltrate the organoid with functional blood vessels. Validation involves histological analysis of human-mouse chimeric vessels using species-specific antibodies, perfusion assays with intravenous tracers, and demonstration of improved organoid survival and maturation compared to in vitro cultures [31].
Vascularization Strategies and Validation
Vascularization Protocol: hPSC-Derived Vascular Organoids
Objective: Generate quantitative vascular organoids from human pluripotent stem cells (hPSCs) for angiogenesis modeling and drug screening.
Materials:
- PECAM1-mRuby3-secNluc; ACTA2-EGFP dual reporter hPSC line
- Defined ECM (such as Matrigel or synthetic hydrogel)
- Vascular differentiation media: RPMI 1640 with B27 supplement
- Growth factors: CHIR99021 (Wnt activator), VEGF-165, FGF2, BMP4
- Small molecules: IWP-2 (Wnt inhibitor), SB431542 (TGF-β inhibitor)
Methodology:
- hPSC Maintenance: Culture reporter hPSCs in mTeSR Plus medium on growth factor-reduced Matrigel-coated plates.
- Mesoderm Induction: Dissociate hPSCs to single cells and seed in ultra-low attachment plates in differentiation media with 6-8 μM CHIR99021 for 24 hours.
- Vascular Progenitor Specification: At day 2, switch to media containing 200 ng/mL VEGF-165 and 100 ng/mL FGF2 for 4 days, forming vascular embryoid bodies.
- 3D Matrix Embedding: Transfer day 6 embryoid bodies to defined ECM and culture for additional 7-14 days with vascular maturation media (VEGF-165 reduced to 50 ng/mL, addition of 50 ng/mL FGF2).
- Quantitative Assessment: Monitor vascular network formation via mRuby3 fluorescence, measure angiogenic responses using bioluminescence readouts, and quantify smooth muscle association via EGFP signal [77].
Validation Data: This protocol generates organoids exhibiting extensive branching networks with average vessel length of 350±42 μm and branch points of 28±6 per organoid. The model demonstrates dose-dependent inhibition of angiogenesis with VEGFR inhibitors (IC50 12.3 nM for sunitinib) and has identified several novel anti-angiogenic candidates through high-throughput screening [77].
Recapitulating Innervation: Current Capabilities and Experimental Approaches
Neural Integration Strategies
Innervation remains a more nascent area of organoid engineering compared to vascularization, though several promising approaches have emerged. The complex, multidirectional signaling between tissues and neural networks presents particular challenges for in vitro recapitulation.
Assembloid approaches involve fusing region-specific neural organoids with target tissue organoids to establish neural connections. For example, spinal cord organoids have been combined with skeletal muscle organoids to create functional neuromuscular junctions, demonstrated by calcium flux in muscle cells following optogenetic stimulation of motor neurons [42]. The methodology typically involves generating separate organoids from neural and target lineages, bringing them into proximity in low-adhesion plates, and allowing axonal penetration between tissues over 2-4 weeks. Validation includes immunohistochemistry for pre- and post-synaptic markers (such as SV2 and acetylcholine receptors), electrophysiological recording of signal transmission, and demonstration of target tissue responses to neural stimulation.
Neural crest incorporation provides an alternative strategy, particularly for modeling autonomic innervation of visceral organs. Neural crest cells, which give rise to the peripheral nervous system, can be co-cultured with developing organoids to enable spontaneous innervation [42]. The protocol involves differentiating hPSCs to neural crest progenitors using small molecule inhibitors of BMP and TGF-β signaling, then combining these cells with target organoids at specific developmental timepoints. Successful innervation is validated by tracking neural crest migration into organoids (often using Wnt1-Cre reporter lines), demonstration of neurotransmitter expression (such as tyrosine hydroxylase for adrenergic neurons), and functional assays showing neural-mediated physiological responses.
Organ-on-chip innervation leverages microfluidic platforms to guide axonal projections from separate neural compartments into target tissues [76]. These systems use microfabricated channels that physically constrain axonal growth while allowing fluidic isolation of different cell populations. The experimental setup typically involves seeding neural spheroids in one compartment and target organoids in another, connected by microchannels of specific dimensions (typically 5-15 μm wide, 100-500 μm long) that permit axonal penetration while restricting cell migration. Validation includes time-lapse imaging of axon progression, demonstration of action potential propagation between compartments, and quantification of neurotransmitter release in target chambers.
Multi-tissue Interactions: Engineering Physiological Complexity
System-Level Integration Approaches
The ultimate validation of organoid physiological relevance comes from their ability to recapitulate complex, multi-tissue interactions observed in vivo. Several advanced platforms now enable the study of these system-level relationships.
Multi-organoids-on-chip platforms connect distinct organoid types through microfluidic circulatory systems, enabling the study of inter-organ signaling and metabolic interactions [66] [76]. These systems recapitulate organ-organ communication critical during development and adult physiology. For example, liver-intestine axis chips have demonstrated first-pass metabolism effects, while brain-liver systems have modeled the impact of hepatic function on blood-brain barrier permeability [76]. The experimental methodology involves housing individual organoids in separate chambers connected by microfluidic channels with endothelialized surfaces, establishing controlled flow rates matching physiological perfusion (typically 0.1-10 μL/min), and incorporating sensors for real-time monitoring of metabolic parameters. Validation includes demonstration of tissue-specific responses to circulating metabolites, pharmacokinetic profiling of drugs across multiple tissues, and comparison of organoid responses to known in vivo tissue crosstalk pathways.
Immune-organoid co-culture systems incorporate immune components to model inflammatory processes and immune-mediated tissue responses [78]. These approaches range from simple incorporation of peripheral blood mononuclear cells into organoid cultures to more complex systems preserving tissue-resident immune populations. The "innate immune microenvironment" model leverages organoids derived from intact tumor tissues that naturally retain tumor-infiltrating lymphocytes, enabling study of endogenous immune responses [78]. Alternatively, "immune reconstitution" models introduce specific immune cell populations into established organoids to study particular immune interactions. Experimental validation includes quantification of immune cell infiltration, measurement of cytokine secretion profiles, demonstration of immune-mediated tissue remodeling, and assessment of checkpoint inhibitor responses in tumor organoids.
Body-axis chips represent the most ambitious approach to multi-tissue integration, seeking to recapitulate interactions along defined physiological axes such as the gut-brain axis or gut-liver-kidney axis [76]. These systems typically incorporate 3-5 organoid types connected in physiological relevant sequences, with circulating medium composition and flow rates designed to mimic blood circulation. The gut-brain axis model, for instance, has demonstrated neural responses to gut metabolites and microbial products, reproducing findings previously only observable in vivo [76]. Validation strategies include comparison of multi-organoid responses to known systemic challenges, demonstration of tissue-specific transcriptomic changes following inter-organ signaling, and correlation of drug distribution patterns with clinical pharmacokinetic data.
Organoid Engineering and Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key research reagents and platforms for engineering complex organoids
| Category | Specific Products/Platforms | Function | Application Examples |
|---|---|---|---|
| Stem Cell Sources | Human induced pluripotent stem cells (hiPSCs), Human embryonic stem cells (hESCs), Adult stem cells (ASCs) | Foundation for organoid generation | Patient-specific disease modeling, Developmental studies [42] |
| Extracellular Matrices | Matrigel, Collagen I, Fibrin, Synthetic hydrogels (PEG, GelMA) | Provide 3D structural support and biochemical cues | Organoid self-organization, Mechanical signaling [75] |
| Growth Factors | EGF, Noggin, R-spondin, FGF, VEGF, BMP4, Wnt agonists/antagonists | Direct cell differentiation and tissue patterning | Stem cell maintenance, Vascular induction [74] |
| Small Molecules | CHIR99021 (Wnt activator), IWP-2/IWR-1 (Wnt inhibitors), Y-27632 (ROCK inhibitor) | Precisely control signaling pathways | Directed differentiation, Enhanced viability [74] |
| Microfluidic Platforms | Organ-on-chip devices, Micropatterned surfaces, Perfusion bioreactors | Provide dynamic culture environments | Vascular perfusion, Multi-organ integration [66] |
| Reporter Systems | Fluorescent proteins (GFP, mRuby3), Luciferase, Calcium indicators | Enable real-time monitoring and quantification | Lineage tracing, Functional assessment [77] |
| Characterization Tools | scRNA-seq, Immunostaining, Multi-electrode arrays, Mass spectrometry | Validate molecular and functional properties | Comparison to in vivo benchmarks [78] |
The engineering of vascularization, innervation, and multi-tissue interactions in organoid models has progressed substantially, yet significant gaps remain when compared to in vivo systems. Current vascularization strategies successfully establish primitive networks that improve nutrient delivery and extend organoid viability, but these engineered vasculature lacks the hierarchical branching patterns and regulatory sophistication of native circulatory systems. Similarly, innervation approaches demonstrate preliminary synaptic connections and functional neural signaling, but fall short of recapitulating the complex neural circuits that orchestrate tissue function in vivo.
The validation of these enhanced organoid models against native development requires multifaceted assessment spanning molecular, structural, functional, and systemic dimensions. While transcriptomic analyses show that advanced organoids more closely resemble their in vivo counterparts than simpler 2D cultures, discrepancies in maturation state and cellular diversity persist. Functional assessments demonstrate tissue-specific capabilities such as cardiac contraction or neuronal firing, but often at reduced efficiency compared to native tissues.
As the field advances, the integration of organoids with organ-on-chip technologies, the development of more physiological matrices, and the incorporation of immune and microbial components will further narrow the gap between in vitro models and in vivo reality. These enhanced systems promise to transform biomedical research by providing more predictive platforms for studying human development, disease mechanisms, and therapeutic interventions, potentially reducing the current reliance on animal models that often poorly translate to human physiology. The ongoing validation of these complex organoid systems against gold-standard in vivo data remains essential for establishing their appropriate roles in basic research and drug development pipelines.
The high failure rate of drug candidates in clinical trials, despite promising preclinical results from animal models, highlights a critical inadequacy in traditional testing methods [79]. This discrepancy, stemming from interspecies physiological differences and the oversimplification of two-dimensional (2D) cell cultures, has driven the demand for more human-relevant in vitro models [80] [81]. Within this context, validating organoid models against in vivo development has become a central thesis in biomedical research. Advanced culture technologies have emerged to address the limitations of organoids—such as structural variability, lack of vascularization, and inadequate maturation—by providing precise environmental control [80] [82]. This guide objectively compares three pivotal technologies—Organ-on-a-Chip (OoC), 3D Bioprinting, and Synthetic Matrices—based on their performance in supporting the development and validation of physiologically faithful organoids.
Organ-on-a-Chip, 3D Bioprinting, and Synthetic Matrices are not mutually exclusive technologies. Instead, they are increasingly integrated to create robust, validated organoid models, as their strengths are highly complementary [80] [83].
Table 1: Core Characteristics of Advanced Culture Technologies
| Technology | Primary Function | Key Strengths | Inherent Limitations |
|---|---|---|---|
| Organ-on-a-Chip (OoC) | Provides a dynamic, perfusable microenvironment with physiological cues [80] [79]. | Precise control over biochemical & mechanical cues (e.g., fluid shear stress, cyclic stretch) [80] [83]. Enables real-time monitoring and integration of multiple tissue interfaces [84]. | Limited initial structural complexity. Fabrication can be complex and low-throughput [84]. |
| 3D Bioprinting | Enables automated, precise spatial patterning of cells and matrices into 3D structures [85] [86]. | High architectural control and automation [85] [87]. Facilitates creation of complex, heterotypic tissues and vascular networks [84]. | Print-induced shear stress can affect cell viability [87]. Resolution limits may restrict capillary-level detail [81]. |
| Synthetic Matrices | Defined biomaterials that mimic the native extracellular matrix (ECM) for 3D cell support [82]. | High batch-to-batch consistency, tunable biochemical & mechanical properties [82]. Reduces variability from animal-derived matrices. | May lack the full complexity of natural ECM. Requires extensive optimization for each cell type [82]. |
Table 2: Quantitative Performance Comparison for Organoid Validation
| Performance Metric | Organ-on-a-Chip | 3D Bioprinting | Synthetic Matrices |
|---|---|---|---|
| Enhancement of Organoid Function (e.g., Liver-specific Albumin Production) | Significantly enhanced metabolic function under perfusion [80]. | Demonstrated significantly enhanced liver function [85]. | Improved and more consistent function due to tunable cues [82]. |
| Reduction in Organoid Batch Variability | Medium-High (through environmental control) [79]. | High (through automation and precision) [85] [86]. | Very High (through defined composition) [82]. |
| Maturation to Adult-like Phenotypes | Promotes maturation via mechanical and perfusion cues [80]. | Can direct structure formation, but maturity can vary [82]. | Supports maturation via presentation of specific adhesive ligands [82]. |
| Throughput for Drug Screening | Medium (evolving towards automated systems) [79]. | Potentially High (automation compatible) [86]. | High (compatible with standard multi-well formats) [82]. |
| Support for Complex Multi-cellularity | High (designed for multiple cell type integration) [83]. | Very High (precise multi-cellular patterning) [84] [87]. | Medium (dependent on initial cell seeding mix) [82]. |
The convergence of these technologies creates a powerful synergistic effect. 3D bioprinting can fabricate complex organoid structures directly within OoC devices, which are then perfused and matured under dynamic conditions, all supported by a synthetic matrix that provides a consistent and tunable microenvironment [80] [84] [83]. This integration is key to generating organoids that faithfully recapitulate in vivo physiology.
Experimental Protocols for Model Validation
To validate these advanced organoid models against in vivo development, standardized experimental protocols are essential. Below are detailed methodologies for key validation experiments.
Protocol 1: Validating Barrier Function in a Bioprinted Intestinal Organoid-on-a-Chip
This protocol assesses the formation and functionality of a critical intestinal barrier, a key indicator of physiological relevance [80] [84].
- Chip Fabrication & Bioprinting: Fabricate a microfluidic chip from PDMS or a 3D-printed polymer featuring a central tissue chamber (∼2 mm width) flanked by two parallel perfusion channels [84] [87].
- Bioink Preparation & Printing: Prepare a bioink composed of intestinal organoid fragments (derived from human induced pluripotent stem cells - iPSCs) mixed with a synthetic PEG-based hydrogel supplemented with cell-adhesive peptides (e.g., RGD) [84] [82]. Using a micro-extrusion bioprinter, deposit the bioink directly into the tissue chamber of the chip, creating a tubular structure interfacing with the perfusion channels [85] [87].
- Perfusion Culture: Connect the chip to a pneumatic or peristaltic pump system. Culture the bioprinted tissue under continuous perfusion (∼50-100 µL/h flow rate) with intestinal differentiation medium for 14-21 days [80] [79].
- Transepithelial Electrical Resistance (TEER) Measurement: Monitor barrier integrity in real-time using integrated or external electrodes to measure TEER. A steady increase and high final TEER value (>500 Ω·cm²) indicate tight junction formation [79].
- Permeability Assay & Imaging: At day 21, perfuse a solution of fluorescently-labeled dextran (e.g., 4 kDa FITC-dextran) through the luminal channel. Collect effluent from the basal channel and measure fluorescence to quantify apparent permeability (Papp). Subsequently, fix the tissue and perform immunostaining for ZO-1 and occludin to visualize tight junctions [79].
Protocol 2: Assessing Drug-Induced Liver Toxicity in a Perfused System
This protocol leverages the metabolic competence of liver organoids under flow to predict human-specific toxic responses [80] [81].
- Model Setup: Incorporate a 3D-bioprinted liver organoid (comprising hepatocytes, stellate, and Kupffer cells in a synthetic matrix) into an OoC device [85] [81]. Alternatively, seed pre-aggregated liver organoids into a chamber lined with a synthetic matrix.
- Perfusion & Stabilization: Perfuse the system with liver maintenance medium at a physiologically relevant flow rate for 7 days to stabilize metabolic function. Monitor albumin and urea production in the effluent as markers of functionality [80].
- Drug Exposure: After stabilization, switch the perfusion medium to one containing the drug candidate (e.g., Trovafloxacin) at a therapeutically relevant concentration. A control group should be perfused with vehicle-only medium. Run the experiment for 72 hours [81].
- Endpoint Analysis:
- Functional Metabolomics: Collect effluent samples at 0, 24, 48, and 72 hours. Quantify the levels of albumin, urea, and released lactate dehydrogenase (LDH) as a marker of cytotoxicity using colorimetric or fluorometric assays [81].
- Gene Expression Analysis: At the end of the experiment, lyse the organoids and extract RNA. Perform qRT-PCR to analyze the expression of key cytochrome P450 enzymes (e.g., CYP3A4) and apoptosis-related genes (e.g., BAX, BCL-2) [80] [81].
- Histological Analysis: Fix and section the organoids. Stain with H&E for general morphology and perform TUNEL staining to quantify apoptosis [81].
The Scientist's Toolkit: Essential Reagent Solutions
Successful implementation of these advanced models relies on a suite of key reagents and materials.
Table 3: Essential Research Reagents for Advanced Organoid Culture
| Reagent/Material | Function | Key Consideration |
|---|---|---|
| Human iPSCs or Adult Stem Cells | The cellular "seeds" for generating patient-specific organoids [80] [82]. | Quality controls for pluripotency and genetic stability are critical for reproducibility. |
| Synthetic Hydrogels (e.g., PEG, Peptide-based) | Defined, tunable extracellular matrix (ECM) mimic that provides structural support and biochemical cues [82]. | Mechanical stiffness and adhesive ligand density must be optimized for each organoid type. |
| Chemically Defined Medium | A serum-free medium containing precise growth factors and small molecules to direct organoid growth and differentiation [80]. | Eliminates batch variability of serum and allows for precise control of signaling pathways. |
| Microfluidic Chip | The physical device that houses the organoid and enables perfusion and application of mechanical forces [84] [79]. | Material (e.g., PDMS, PS) should be selected to minimize small molecule absorption. |
| Specialized Bioinks | Cell-laden materials (often hydrogel-based) designed for specific bioprinting modalities [84] [86]. | Must balance printability (viscosity, crosslinking) with cell-compatibility and bioactivity. |
The objective comparison of Organ-on-a-Chip, 3D Bioprinting, and Synthetic Matrices reveals a clear path toward overcoming the limitations of traditional organoid cultures. While each technology excels in specific areas—OoC in providing dynamic physiological cues, 3D Bioprinting in achieving architectural control and automation, and Synthetic Matrices in ensuring reproducibility—their true potential is unlocked through integration [80] [83]. The experimental data and protocols provided herein demonstrate that these convergent technologies are powerful tools for creating organoid models with enhanced physiological function, structural fidelity, and reproducibility. This technological progress is pivotal for the rigorous validation of organoids against in vivo development, ultimately accelerating the development of safer and more effective therapeutics.
The Role of AI and Machine Learning in Protocol Optimization and Image Analysis
In the field of biomedical research, the validation of organoid models against traditional in vivo development represents a critical frontier for advancing drug discovery and personalized medicine. Organoids—three-dimensional, self-organizing microtissues derived from stem cells—closely mimic the structural and functional complexity of human organs, providing a powerful in vitro platform for disease modeling and therapeutic screening [3] [88]. However, the full potential of organoid technology remains constrained by challenges in standardization, scalability, and accurate phenotypic characterization. This is where artificial intelligence (AI) and machine learning (ML) are emerging as transformative technologies, enabling researchers to optimize culture protocols and extract nuanced, quantitative data from complex organoid images with unprecedented precision and scale.
This guide objectively compares the performance of current AI-powered platforms and algorithms specifically for organoid image analysis, framing the discussion within the broader scientific imperative of validating these sophisticated in vitro models against the gold standard of in vivo development.
The AI and ML Toolkit for Organoid Research
Modern AI tools for image analysis in organoid research span from general-purpose classification models to specialized segmentation architectures. The selection of an appropriate model depends on the specific research question, whether it involves quantifying organoid growth, classifying morphological phenotypes, or segmenting sub-cellular structures.
State-of-the-Art Image Analysis Models
The table below summarizes the performance metrics of leading image classification models relevant to organoid analysis, based on benchmark evaluations.
Table 1: Performance Comparison of State-of-the-Art Image Models
| Model | Architecture Type | Reported Top-1 Accuracy (ImageNet) | Key Strengths | Computational Demand |
|---|---|---|---|---|
| CoCa | Vision Transformer + Contrastive Learning | 91.0% (fine-tuned) [89] | Exceptional zero-shot capabilities, multimodal understanding | High (2.1B parameters) |
| DaViT | Dual Attention Vision Transformer | 90.4% (fine-tuned) [89] | Captures global and local features simultaneously | Medium to High (Up to 1.4B parameters) |
| ConvNeXt V2 | Pure Convolutional | ~84-86% (reported range) [89] | High efficiency, strong performance on textured images | Medium |
| EfficientNet | Convolutional (Compound Scaling) | ~85% (reported range) [89] | Optimal accuracy/efficiency trade-off, good for deployment | Low to Medium |
| UNet Variants | Encoder-Decoder CNN | N/A (Specialized for Segmentation) | Superior for biomedical image segmentation (e.g., 99.4% accuracy for brain tumor segmentation [90]) | Low to Medium |
Specialized AI Models for Medical and Organoid Image Analysis
Beyond general-purpose models, specialized architectures have been developed to address the unique challenges of biological image analysis:
- CSM-FusionNet: A framework designed for enhanced detection of hepatocellular carcinoma from ultrasound images, achieving 97.25% accuracy and 100% sensitivity [90].
- YOLOv8: Demonstrated high performance in real-time detection tasks, such as identifying fractured endodontic instruments in radiographs with 97.4% accuracy and a rapid inference time of 14.6 ms [90].
- Mask R-CNN: While slightly slower (88.4 ms inference time), this model achieved higher 98.21% accuracy in pixel-wise segmentation tasks, making it suitable for detailed morphological analysis of organoid structures [90].
- Enhanced Super-Pixel Techniques: Used for precise brain tumor segmentation, achieving a Dice similarity coefficient of 0.91, indicating high overlap with ground truth annotations [90].
Experimental Protocols for AI-Driven Organoid Analysis
To ensure reproducible and biologically relevant results, researchers must implement standardized protocols that integrate AI tools throughout the organoid culture and analysis pipeline.
Protocol for High-Content Screening of Organoid Morphology
Objective: To quantitatively assess treatment effects on organoid size, shape, and complexity using AI-based image analysis.
Workflow:
- Organoid Culture & Treatment: Plate organoids in Matrigel or similar extracellular matrix in 96-well imaging plates. Apply experimental treatments alongside appropriate controls.
- Image Acquisition: Acquire high-resolution brightfield or fluorescence images using an automated high-content microscope. Ensure consistent magnification, lighting, and z-stack settings across all wells.
- AI-Powered Preprocessing: Use a trained model (e.g., UNet variant) to automatically identify and segment individual organoids from the background and debris.
- Feature Extraction: The AI model computes quantitative morphological descriptors (e.g., diameter, circularity, surface texture, luminal area) for each segmented organoid.
- Phenotypic Classification: Input the extracted features into a classifier (e.g., EfficientNet or a custom CNN) to assign organoids to predefined phenotypic classes (e.g., "normal," "cystic," "disorganized").
- Statistical Analysis & Validation: Compare morphological metrics across treatment groups using appropriate statistical tests. Correlate AI-derived classifications with molecular markers (e.g., immunofluorescence) to validate biological relevance.
Diagram: AI-Driven Organoid Screening Workflow
Protocol for Validating Organoid Maturity Against In Vivo Counterparts
Objective: To use AI-based image analysis to quantitatively demonstrate that organoids recapitulate key architectural features of their in vivo counterparts.
Workflow:
- Parallel Sample Preparation: Generate organoids (e.g., hepatic) using an optimized protocol [91]. Collect in vivo tissue samples (e.g., from mouse embryos at equivalent developmental stages).
- Multichannel Imaging: Perform multiplex immunofluorescence staining on both organoid and tissue sections for key cell type-specific (e.g., hepatoblasts, endothelial cells) and functional markers (e.g., Albumin).
- Co-registration & Spatial Analysis: Use a platform like Recursion's phenomics platform [92] to align and segment images based on marker expression. AI algorithms quantify the spatial distribution and co-localization of different cell types.
- Morphometric Comparison: Extract and compare quantitative features (e.g., tissue porosity, cord-like structure length, nuclear density) between organoids and in vivo tissues using a pre-trained model like DaViT, which is adept at capturing complex spatial relationships [89].
- Functional Correlation: Integrate image-based metrics with functional data (e.g., transcriptomics from single-cell RNA sequencing) to build a multi-modal validation profile.
Diagram: Organoid vs. In Vivo Validation Pipeline
Comparative Performance Data of AI Platforms
The true test of an AI model lies in its performance on specific, biologically relevant tasks. The following data, drawn from published studies, provides a basis for comparing different approaches.
Performance on Specific Organoid-Relevant Analysis Tasks
Table 2: AI Model Performance on Biomedical Image Analysis Tasks
| Analysis Task | AI Model / Platform Used | Reported Performance Metric | Biological Context |
|---|---|---|---|
| Brain Tumor Segmentation | Modified U-Net | 99.4% Global Accuracy, 90.2% Dice Score [90] | Segmentation of tumor regions in MRI; analogous to organoid structure segmentation. |
| Kidney Tumor Diagnosis | SSLSD-KTD (Masked Autoencoder) | 98.04% Accuracy (KAUH dataset) [90] | Classification of kidney tumors from images; relevant for disease modeling in renal organoids. |
| Skin Disease Detection | Fused EfficientNet-B0, B2, ResNet50 | 99.14% Accuracy [90] | Multi-class classification of skin conditions; demonstrates feasibility for complex organoid phenotypic classification. |
| Fractured Instrument Detection | YOLOv8 | 97.4% Accuracy, 14.6 ms inference time [90] | High-speed, accurate detection in radiographs; applicable for real-time quality control in organoid cultures. |
| Colorectal Abnormality Classification | Cross-Attention Multi-Scale Vision Transformer | 93.4% Accuracy, 94.46% Precision [90] | Distinguishing between five types of abnormalities; relevant for grading organoid phenotypic responses. |
Signaling Pathways in Organoid Development and Analysis
A key application of AI in organoid validation is linking morphological features, quantified through image analysis, to the underlying molecular signaling pathways that drive development and disease.
One pathway of recent interest, identified through a combination of molecular biology and single-cell RNA sequencing, involves a placenta-derived factor that promotes liver organoid growth [91]. Recapitulating such embryonic signaling is a major goal in organoid protocol optimization.
Diagram: IL1α Signaling in Liver Organoid Growth
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the aforementioned protocols relies on a suite of specialized reagents and tools. The following table details key components for AI-driven organoid research.
Table 3: Essential Research Reagent Solutions for Organoid and AI Workflows
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| Matrigel or BME | Extracellular matrix substitute providing a 3D scaffold for organoid growth. | Foundational for all 3D organoid culture protocols. |
| Placenta-Derived Factors (e.g., IL1α) | Soluble signaling molecules that promote progenitor cell expansion. | Enhancing growth and maturity of liver organoids under hypoxic conditions [91]. |
| Cell Type-Specific Antibodies | For multiplex immunofluorescence staining to identify different cell populations. | Validating cellular composition and spatial organization in organoids vs. in vivo tissue. |
| hiPSCs (Human Induced Pluripotent Stem Cells) | Starting cell source for generating patient-specific organoids. | Creating disease models and personalized therapeutic screening platforms. |
| Automated Bioreactors | Systems providing dynamic culture conditions (perfusion, mixing). | Scaling up organoid production for high-throughput screening and improving nutrient/waste exchange. |
| Organ-Chip Microfluidic Devices | Platforms that integrate organoids with dynamic fluid flow and mechanical cues. | Enhancing organoid maturity and creating multi-tissue interaction models for ADME toxicity studies [3]. |
The integration of AI and machine learning into organoid research marks a paradigm shift in how we quantify and validate these complex biological models. As the performance comparison data demonstrates, a suite of powerful models—from specialized segmentation U-Nets to large-scale vision transformers like CoCa and DaViT—now provide researchers with an unprecedented ability to extract quantitative, objective data from organoid images. This computational power, when deployed via standardized experimental protocols, directly addresses the critical challenge of reproducibility and scalability that has hampered the field.
The ultimate goal is to close the loop between in vitro modeling and in vivo reality. By using AI to rigorously compare organoid morphology, cellular spatial relationships, and functional outputs against their in vivo counterparts, researchers can iteratively refine culture protocols—for instance, by incorporating key developmental signals like placenta-derived factors. This virtuous cycle of image-driven analysis and protocol optimization, powered by AI, is accelerating the transition of organoid technology from a promising research tool to a validated platform for drug discovery and regenerative medicine.
Evidence and Efficacy: Direct Comparative Analysis with Traditional Models
The pursuit of accurate and predictive models in biomedical research represents a critical challenge in the translation of basic scientific discoveries into effective clinical therapies. Historically, drug development and disease modeling have relied on a combination of two-dimensional (2D) cell cultures and experimental animal models. However, a staggering attrition rate persists, with over 90% of drugs that demonstrate efficacy in animal trials failing during human clinical phases [93]. This disconnect underscores a fundamental limitation: traditional models often lack the specificity and physiological relevance required to accurately predict human outcomes. This review systematically compares the capabilities of 2D cell cultures, 3D organoids, and animal models, framing the analysis within the broader thesis of validating organoid technology as a more physiologically relevant platform for emulating in vivo human development and disease processes.
Defining the Model Systems
2D Cell Cultures
The two-dimensional (2D) cell culture system is a long-standing cornerstone of biological research. This method involves growing cells as a single monolayer on flat, rigid plastic or glass surfaces [94] [95]. While these systems are celebrated for their simplicity, low cost, and highly controlled conditions, they force cells into an unnatural state that lacks the complex three-dimensional architecture of living tissues. Consequently, they fail to replicate critical in vivo microenvironmental cues such as oxygen and nutrient gradients, 3D cell-to-cell interactions, and extracellular matrix (ECM) signaling [94]. This often results in altered cell shape, polarity, and function, leading to poor translation of findings to whole organisms.
3D Organoids
Organoids are defined as three-dimensional (3D), multicellular structures grown in vitro from stem cells that self-organize to mimic the micro-anatomy and functionality of specific organs [96] [4]. They can be derived from several sources:
- Tissue-derived adult stem cells (ASCs) [97] [4]
- Induced pluripotent stem cells (iPSCs) [93] [4]
- Embryonic stem cells (ESCs) [97] [4]
These miniaturized organ versions exhibit self-renewal and self-organization capabilities and can be cultured long-term [96]. They are classified based on their tissue of origin, such as cerebral, intestinal, or hepatic organoids, and represent one of the latest innovations for recapitulating physiologic processes in a human-relevant context [96].
Experimental Animal Models
Experimental animal models—typically mice, rats, zebrafish, and non-human primates—have been indispensable for strengthening biomedical and pharmaceutical research [96] [98]. They provide a whole-organism context, including systemic interactions like immune responses, hormonal regulation, and blood flow dynamics [93]. However, they are hampered by significant interspecies differences in genetics, gene expression, developmental timing, immunology, and metabolism, which limit their ability to reliably predict human clinical outcomes [96] [98] [99].
Comparative Analysis of Key Characteristics
The following tables provide a structured, quantitative comparison of the three model systems across critical parameters relevant to research and drug development.
Table 1: Overall Model System Comparison
| Feature | 2D Cell Culture [97] [94] | 3D Organoids [96] [97] | Animal Models [98] [97] |
|---|---|---|---|
| Physiological Relevance | Low | Moderate to High | High (but species-specific) |
| Structural Complexity | None (monolayer) | Mimics in vivo micro-anatomy | Fully mimics whole-organism features |
| Cost | Low | Moderate | High |
| Experimental Timelines | Short (days) | Moderate (weeks) | Long (months to years) |
| Throughput & Scalability | High | Moderate (improving with automation) | Low |
| Self-Renewal/Expansion | High (for cell lines) | High | No (requires breeding) |
| Ethical Considerations | Minimal | Minimal (uses human cells) | Significant (animal welfare concerns) |
Table 2: Performance in Drug Discovery and Disease Modeling
| Parameter | 2D Cell Culture | 3D Organoids | Animal Models |
|---|---|---|---|
| Human Specificity | Yes (if human cells) | Yes (human-cell derived) | No (interspecies differences) |
| Success Rate in Establishment | High [97] | Very High [97] | Low to Moderate [97] |
| Reproducibility | High [97] | High [97] | Moderate [97] |
| Tumor Microenvironment (TME) Fidelity | Poor [97] | Moderate to High [97] | High [97] |
| Predictive Value for Drug Efficacy | Low (high false positives/negatives) [94] | High [94] [93] | Moderate (prone to interspecies discrepancies) [99] |
| Personalized Medicine Potential | Low | High (via patient-derived organoids) [94] [93] | Low |
| Suitability for High-Throughput Screening | Excellent [94] [99] | Good (with technical optimization) [94] | Poor |
Table 3: Technical and Operational Considerations
| Aspect | 2D Cell Culture | 3D Organoids | Animal Models |
|---|---|---|---|
| Ease of Maintenance | Easy [97] | Easy to Moderate [97] | Difficult (requires specialized facilities) [97] |
| Protocol Standardization | Highly standardized | Evolving, requires optimization [94] | Standardized, but species-variable |
| Imaging & Analysis | Simple and standardized | Challenging (requires tissue clearing, confocal imaging) [95] | Complex (e.g., in vivo imaging) |
| Genetic Manipulation | Easy | Moderate (e.g., CRISPR/Cas9) [100] | Established but complex and time-consuming |
| Regulatory Acceptance | Well-established for early discovery | Growing (aided by FDA Modernization Act 2.0) [98] [93] | Traditional gold standard, but requirements are evolving [98] |
Experimental Validation: Methodologies and Key Findings
Core Protocol for Establishing Patient-Derived Tumor Organoids (PDOs)
The following workflow details a standard method for generating PDOs, a key technique for validating organoids against in vivo tumor biology [97].
- Sample Acquisition & Processing: Tumor tissue is obtained via surgical resection or biopsy. The sample is washed and subjected to enzymatic (e.g., collagenase) and/or mechanical digestion to create a single-cell suspension or small tissue fragments [97].
- 3D Culture Embedding: The resulting cell mixture is embedded in a basement membrane extract (BME) or Matrigel, which provides a scaffold mimicking the extracellular matrix [97] [4].
- Specialized Culture Media: The embedded cells are cultured in a tailored medium. Key components often include:
- R-spondin-1: A Wnt signaling agonist essential for stem cell maintenance [97] [4].
- Noggin: A BMP pathway inhibitor that prevents unwanted differentiation [97] [4].
- Epidermal Growth Factor (EGF): Supports cell proliferation.
- Other niche factors like B27, FGF, and small-molecule inhibitors (e.g., A83-01, Y27632) specific to the tumor type [97] [4].
- Expansion & Passaging: Organoids are typically passaged every 1-2 weeks by mechanically or enzymatically breaking down the structures and re-embedding the fragments into fresh matrix [97].
- Characterization & Validation: The resulting PDOs are validated using techniques such as:
Key Validating Findings
- Recapitulating Drug Resistance: A pivotal study comparing 2D cultures and 3D organoids in breast cancer revealed that drug resistance to temozolomide was 50% higher in 3D organoids than in 2D models. This highlights the critical role of the 3D microenvironment in developing chemoresistance, a phenomenon poorly captured by monolayer cultures [4].
- Zika Virus Modeling: Brain organoids were instrumental in uncovering the mechanism of Zika virus-induced microcephaly. Researchers found the virus preferentially targeted and killed neural progenitor cells in human brain organoids, a finding not readily observed in traditional murine models. This demonstrated the unique ability of organoids to model human-specific cellular responses to infection [93] [100].
- Personalized Therapy for Cystic Fibrosis: Intestinal organoids derived from cystic fibrosis patients have been used as a predictive platform for individual patient responses to CFTR modulator drugs. This application allows for the functional repair of CFTR using CRISPR/Cas9 in patient-derived organoids, paving the way for personalized treatment strategies, especially for those with rare mutations [93].
Visualizing Critical Signaling Pathways in Organoid Culture
The self-renewal and differentiation of stem cells within organoids are governed by precise signaling pathways, meticulously replicated in vitro through culture medium additives. The following diagram illustrates the key pathways manipulated to guide organoid development and maintain stemness.
The Scientist's Toolkit: Essential Reagents for Organoid Research
Success in organoid culture is heavily dependent on specific reagents and materials that recreate the native stem cell niche. The following table details key solutions required for establishing and maintaining these complex 3D models.
Table 4: Essential Research Reagents for Organoid Culture
| Reagent / Material | Function & Application in Organoid Culture |
|---|---|
| Basement Membrane Extract (BME)/Matrigel [97] [4] [95] | A gelatinous protein mixture that serves as a 3D scaffold, mimicking the in vivo extracellular matrix (ECM) to support cell growth, polarization, and self-organization. |
| R-spondin 1 [97] [4] | A critical growth factor that acts as a potent agonist of the Wnt signaling pathway, essential for the maintenance and expansion of Lgr5+ intestinal and other stem cells. |
| Noggin [97] [4] | A bone morphogenetic protein (BMP) inhibitor. Suppressing BMP signaling prevents stem cell differentiation, allowing for the propagation of undifferentiated progenitor cells within the organoid. |
| EGF (Epidermal Growth Factor) [97] [4] | A key mitogen that promotes the proliferation and expansion of stem and progenitor cells within the organoid structure. |
| B27 Supplement [4] | A serum-free supplement designed to support the growth and survival of neurons and other specialized cells, commonly used in neural organoid and other differentiation media. |
| Y-27632 (Rho Kinase Inhibitor) [4] | A small molecule inhibitor used to enhance cell survival, particularly after passaging or thawing, by preventing anoikis (cell death due to detachment). |
| Tissue Clearing Reagents (e.g., Corning 3D Clear, Visikol HISTO-M) [95] | Chemical solutions that reduce the opacity of 3D tissues, enabling deeper and clearer imaging of entire organoids by making them optically transparent. |
| Microwell Plates (e.g., Millicell Microwell plates) [95] | Specialized cultureware with microcavities that promote the formation of uniformly-sized, single organoids or spheroids in a single focal plane, ideal for high-throughput screening. |
The comparative analysis presented herein validates 3D organoid technology as a profoundly transformative model system that effectively bridges the long-standing gap between simplistic 2D cultures and species-divergent animal models. While 2D cultures remain invaluable for high-throughput initial screening and mechanistic studies under uniform conditions, and animal models are still necessary for studying complex systemic physiology, organoids offer an unparalleled capacity to mimic human-specific tissue architecture, disease pathology, and drug responses in vitro.
The improved physiological relevance of organoids leads to better prediction of drug efficacy and toxicity, helping to reduce the high attrition rates in clinical trials [94]. Furthermore, the advent of patient-derived organoids ushers in a new era of personalized medicine, enabling the functional testing of therapeutics on a patient's own cells [94] [93]. Despite ongoing challenges related to standardization, vascularization, and the incorporation of immune components, the trajectory of innovation—through automation, organ-on-a-chip integration, and advanced biomaterials—is rapidly addressing these limitations [94] [101]. Supported by evolving regulatory frameworks like the FDA Modernization Act 2.0 [98] [93], organoids are poised to become an indispensable tool in the biomedical research arsenal, accelerating the development of safer and more effective human therapeutics.
In the field of precision oncology, demonstrating that a preclinical model can accurately predict a patient's clinical response to therapy is the ultimate benchmark for functional validation. Patient-derived organoids (PDOs) have emerged as a powerful ex vivo platform for drug screening and biomarker discovery, bridging the gap between traditional 2D cell cultures and complex in vivo models [102] [103]. This guide objectively compares the performance of PDOs and computational models in predicting clinical drug responses, framing the analysis within the broader thesis of validating organoid models against in vivo development research. We summarize supporting experimental data, detail key methodologies, and provide resources for the research community.
Comparative Performance of Preclinical Models
The table below summarizes key comparative studies benchmarking the predictive performance of different preclinical models against clinical outcomes.
Table 1: Benchmarking Preclinical Models Against Clinical Outcomes
| Model Type | Validation Context | Key Performance Metric | Reported Outcome | Reference |
|---|---|---|---|---|
| PDO (Pancreatic Cancer) | Drug response vs. paired Patient-Derived Xenograft (PDX) | Correlation of Area Under the Curve (AUC) | Specific relationship between PDO drug dose response and in vivo tumor growth, irrespective of drug [102]. | JCI Insight, 2020 |
| PDO (Colorectal Cancer) | Meta-analysis of patient response prediction | Accuracy / Sensitivity / Specificity | On average, 76% accuracy in predicting patient response (sensitivity: 0.79, specificity: 0.75) [14]. | J Exp Clin Cancer Res, 2024 |
| Deep Learning (DrugS Model) | Drug response prediction in PDX models | Correlation of predictions with PDX response | Model predictions showed correlation with drug response data from PDX models [104]. | Sci Rep, 2025 |
| Cell Line-Based Models | Prediction of xenograft response (Erlotinib) | Correlation between prediction and observed response | Moderate accuracy (correlation ≈ 0.5) for erlotinib-treated cohort; unable to predict for gemcitabine or paclitaxel [105]. | Sci Rep, 2020 |
Detailed Experimental Protocols for Validation
A critical component of functional validation is the rigorous experimental workflow used to generate benchmark data. The following diagram outlines a standardized protocol for validating patient-derived organoid drug responses against clinical outcomes.
Diagram Title: PDO Drug Response Validation Workflow
Core Protocol Steps
- PDO Establishment and Culture: Patient-derived tissue samples are dissociated, and epithelial components are embedded in a basement membrane matrix like Matrigel [106]. The culture medium is supplemented with a specialized cocktail of growth factors to mimic the stem cell niche, which is critical for long-term expansion. Key factors often include WNT agonists (e.g., WNT3A, R-spondin-1), EGF, and Noggin (a BMP inhibitor) [14] [106].
- Drug Screening and Response Quantification: Organoids are exposed to a range of drug concentrations, often in a high-throughput format. The cell viability is measured using assays like ATP-based luminescence (CellTiter-Glo). The drug response is quantified using metrics such as the Area Under the dose-response Curve (AUC) or the half-maximal inhibitory concentration (IC50) [102] [14].
- Correlation with Clinical Outcomes: The ex vivo drug response data from PDOs are directly compared with the corresponding patient's clinical outcome or with the response in paired Patient-Derived Xenograft (PDX) models, which are considered a "gold standard" for in vivo validation [102]. A study on pancreatic cancer PDOs demonstrated a "specific relationship between AUC value of organoid drug dose response and in vivo tumor growth, irrespective of the drug treatment" [102].
Advanced Validation: Combination Therapies and Computational Integration
Beyond monotherapy, validating models for combination treatments represents a more complex, clinically relevant challenge. Furthermore, computational models are being developed to predict drug response from genomic data, which also require rigorous validation.
Validation of Combination Therapies
In colorectal cancer (CRC), PDOs have been used to validate and optimize multi-drug combinations. One innovative platform, Therapeutically-Guided Multidrug Optimization (TGMO), systematically screens combinations of tyrosine kinase inhibitors (e.g., regorafenib, vemurafenib) on PDOs from primary and metastatic CRC [14]. This approach can identify low-dose combinations that achieve high efficacy (e.g., up to 88% reduction in cell viability), providing a rational strategy to overcome drug resistance [14].
Validation of Deep Learning Models
Computational models offer a complementary approach to physical models. The DrugS deep neural network model uses gene expression data and drug chemical structures to predict cellular responses to drugs [104]. Its performance was validated by correlating its predictions with drug response data from PDX models, thereby creating a link between in silico predictions and in vivo outcomes [104]. Another model, PASO, integrates multi-omics pathway data and drug structures, and has been validated for clinical utility using data from The Cancer Genome Atlas (TCGA) [107]. The workflow for this integrated validation approach is illustrated below.
Diagram Title: Computational Model Validation Path
The Scientist's Toolkit: Essential Reagents and Models
Successful execution of these validation experiments relies on key biological and computational reagents. The following table details essential solutions for establishing a robust functional validation pipeline.
Table 2: Key Research Reagent Solutions for Drug Response Validation
| Item Name | Function / Application | Critical Features / Considerations |
|---|---|---|
| Matrigel / Basement Membrane Extract | 3D scaffold for organoid culture | Provides structural and biochemical support for stem cell growth and self-organization [106]. |
| Specialized Growth Factor Cocktails | Maintenance and expansion of PDOs | Typically includes WNT agonists (R-spondin-1), EGF, Noggin; specific to tissue type [14] [106]. |
| Patient-Derived Organoid (PDO) Biobanks | Representative disease models for screening | Preserve genetic and phenotypic characteristics of the original tumor; enable reproducible drug screens [103] [106]. |
| Patient-Derived Xenograft (PDX) Models | In vivo "gold standard" for validation | Used to benchmark PDO and computational model predictions against a complex in vivo environment [102]. |
| Decellularized ECM (dECM) Scaffolds | Advanced culture substrate | Replicates native tumor microenvironment more effectively than standard matrices, incorporating diverse cell types [106]. |
| Organoid-on-Chip Systems | Enhanced culture with physiological cues | Microfluidic chips integrate fluid flow, mechanical forces, and improved oxygenation, enhancing organoid maturity and function [108]. |
| Pre-trained Deep Learning Models (e.g., DrugS, PASO) | In silico drug response prediction | Models trained on large-scale pharmacogenomic data (e.g., GDSC, CCLE) can predict IC50/AUC for new samples [104] [107]. |
The functional validation of drug response predictions against clinical outcomes remains a cornerstone of translational cancer research. Patient-derived organoids have demonstrated significant and reproducible predictive power, with their response profiles showing a direct correlation with in vivo tumor growth in PDX models and patient outcomes. While challenges regarding standardization, scalability, and full recapitulation of the tumor microenvironment persist, PDOs, especially when integrated with advanced computational models and sophisticated culture systems like organoids-on-chip, provide a powerful and validated platform for drug discovery and personalized therapy planning [103] [3] [108]. The continued refinement of these models and validation protocols will be crucial for improving their accuracy and clinical adoption.
The pursuit of human-relevant preclinical models is a central thesis in modern biomedical research, driving the transition from traditional 2D cell cultures and animal models to more physiologically complex systems. Among these, organoid technologies have emerged as powerful tools for disease modeling and drug development. This guide objectively compares the experimental performance of organoid models against established alternatives, focusing on two key application areas: cystic fibrosis and oncology. The data and methodologies presented herein provide a framework for researchers validating organoid models against in vivo development research.
Case Study 1: Cystic Fibrosis and CFTR Modulator Testing
Cystic fibrosis (CF) research has been revolutionized by organoid models, which enable patient-specific drug response testing. The following section compares established preclinical models used for CFTR modulator drug testing.
Experimental Platforms & Quantitative Performance
Table 1: Comparison of Preclinical CFTR Modulator Testing Platforms
| Platform Feature | 2D Intestinal Organoid Monolayers (2D HIO) | 3D Intestinal Organoids (3D HIO) | Human Nasal Epithelial Cells (HNE) |
|---|---|---|---|
| Primary Assay Type | Transepithelial current measurement (Ussing chamber) | Forskolin-Induced Swelling (FIS) assay | Transepithelial current measurement (Ussing chamber) |
| CFTR Function Measurement | CFTR-dependent ΔIeq (ΔFsk-Ieq and ΔCFTRInh-172-Ieq) | Luminal fluid influx and organoid swelling | CFTR-dependent ΔIeq |
| Measurable CFTR Functional Range | Higher, with linear Fsk activation up to 10 µM [109] | Limited by physics of organoid swelling, plateaus at ~1 µM Fsk [109] | Lower than 2D HIO [109] |
| Baseline Transepithelial Resistance (Rte) | Non-CF: 634 ± 202 Ω·cm²; CF: 550 ± 342 Ω·cm² [109] | Not Applicable | Not Fully Detailed |
| Apical Membrane Accessibility | High, enables direct access for electrophysiology and compound application [109] | Low, luminal access is challenging [109] | High |
| Tissue Source | Rectal biopsy | Rectal biopsy | Nasal brush |
Detailed Experimental Protocols
Protocol A: Establishing and Using 2D Human Intestinal Organoid (2D HIO) Monolayers for Ussing Chamber Studies
- Objective: To generate polarized intestinal epithelial monolayers from 3D organoids for functional CFTR assessment via electrophysiology.
- Starting Material: 3D human intestinal organoids (HIOs), derived from patient rectal biopsies and expanded in Matrigel domes using IntestiCult organoid growth medium.
- Procedure:
- Organoid Dissociation: Harvest 3D HIOs from Matrigel and dissociate into single cells or small clusters using a gentle cell dissociation reagent.
- Monolayer Culture: Seed the dissociated cells onto permeable Transwell inserts coated with an extracellular matrix (e.g., collagen). Culture the cells with specific medium until a confluent, polarized monolayer is formed.
- Transepithelial Resistance (TEER) Monitoring: Monitor the integrity and tight junction formation of the monolayer by measuring TEER regularly.
- Ussing Chamber Assay: Once a stable, high TEER is confirmed, mount the monolayer in an Ussing chamber system. Bathe both apical and basolateral sides with physiological solutions.
- CFTR Function Measurement:
- Baseline Measurement: Record the baseline short-circuit current (Ieq).
- Forskolin Stimulation: Add forskolin (a cAMP agonist) to the basolateral side to activate CFTR. The increase in Ieq (ΔFsk-Ieq) indicates CFTR-mediated anion secretion.
- CFTR Inhibition: Apply a specific CFTR inhibitor (e.g., CFTRInh-172) to confirm the current is CFTR-dependent (ΔCFTRInh-172-Ieq).
- Drug Testing: For modulator testing, pre-incubate the monolayers with the drugs (e.g., correctors, potentiators) before performing the Ussing chamber assay to assess functional rescue of defective CFTR.
Protocol B: Forskolin-Induced Swelling (FIS) Assay in 3D Human Intestinal Organoids (3D HIO)
- Objective: To quantify CFTR function in 3D organoids by measuring cAMP-mediated fluid influx into the organoid lumen.
- Starting Material: 3D human intestinal organoids in Matrigel.
- Procedure:
- Organoid Harvesting: Mechanically harvest 3D HIOs from Matrigel and transfer them to a solution.
- Plating: Plate intact organoids into a 96-well imaging plate.
- Forskolin Stimulation: Treat the organoids with forskolin. CFTR activation leads to chloride and fluid secretion into the organoid lumen.
- Image Acquisition and Analysis: Capture bright-field images of the organoids at regular intervals (e.g., every 15-30 minutes for 60-120 minutes). Use automated image analysis software to quantify the increase in organoid cross-sectional area over time. The swelling rate or the percentage of swelling-responsive organoids serves as a metric for CFTR function.
Experimental Workflow and Signaling Pathway
The following diagram illustrates the logical workflow for establishing and testing patient-derived intestinal organoids, culminating in the assessment of CFTR function via different assay platforms.
Case Study 2: Oncology and Patient-Derived Organoids
While the provided search results offer extensive background on organoid technology and its market potential, specific case studies with quantitative clinical prediction data in oncology were not available in the searched literature. However, the general principles and applications of patient-derived organoids (PDOs) in cancer research are well-established as outlined below.
The Role of Organoids in Cancer Research
The field of oncology is leveraging organoids for personalized medicine and drug discovery. The market for organoids is expected to grow significantly, reflecting their increased adoption in research and development [3]. The primary advantages and challenges in this context include:
- Personalized Treatment: A key application is using patient-derived organoids (PDOs) to guide personalized cancer treatment. PDOs can be established from a patient's tumor tissue and used to screen a panel of therapeutics ex vivo to identify the most effective drug or combination for that specific individual [3].
- Disease Modeling: Organoids allow for the reconstruction of tumor microenvironments and can be used to study tumor development, progression, and drug resistance mechanisms. Gene editing tools like CRISPR can be used to introduce specific oncogenic mutations into organoids to model tumorigenesis [3].
- Current Limitations: Several challenges remain, including a lack of standardization and scalability, limited physiological relevance due to the frequent absence of immune cells and vasculature, and issues with reproducibility in size, shape, and cell type composition [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagent Solutions for Intestinal Organoid Research and CFTR Assays
| Item | Function/Application | Specific Examples / Notes |
|---|---|---|
| Stem Cell Source | Starting material for generating organoids. | Adult intestinal stem cells from rectal biopsies; Induced Pluripotent Stem Cells (iPSCs) [31] [3]. |
| Extracellular Matrix (ECM) | Provides a 3D scaffold to support organoid growth and polarization. | Matrigel or other GMP-grade ECM hydrogels are critical for 3D culture [3]. |
| Specialized Growth Medium | Provides essential niche factors and nutrients for stem cell maintenance and differentiation. | Combinations of growth factors (EGF), Noggin (BMP inhibitor), and R-spondin (Wnt activator) are fundamental [31]. Commercially available media like IntestiCult are also used. |
| CRISPR-Cas9 System | For precise genome editing to introduce or correct disease-associated mutations (e.g., for disease modeling). | Enables genetic lineage tracing and precise disease modeling in organoids [31] [3]. |
| CFTR Modulators | Pharmacological agents used to rescue defective CFTR function in experiments. | Corrector drugs (e.g., Tezacaftor/VX-661, Elexacaftor/VX-445); Potentiator drugs (e.g., Ivacaftor/VX-770) [109]. |
| CFTR Agonist/Inhibitor | Tools to activate and inhibit CFTR for functional assays. | Forskolin (agonist); CFTRInh-172 (specific inhibitor) [109]. |
| Permeable Supports | Physical substrate for growing polarized 2D epithelial monolayers from dissociated organoids. | Transwell inserts [109]. |
| Microfluidic Chips | Advanced culture platforms to enhance organoid maturation and enable multi-organ systems. | "Organoids-on-chip" technology provides dynamic fluid flow and mechanical cues, improving reproducibility and tissue function [108]. |
The validation of organoid models against in vivo development is an ongoing endeavor. Current trends focus on integrating organoids with organ-on-a-chip microfluidic technology to introduce dynamic fluid flow, mechanical cues, and co-culture with other cell types like endothelium and immune cells, thereby enhancing physiological relevance [108]. Furthermore, efforts are directed toward vascularization to overcome nutrient diffusion limits and prevent necrosis in larger organoids [3]. The push for standardization, automation, and AI-driven analysis is also critical to improve reproducibility and enable high-throughput screening, making organoids an even more reliable tool for clinical prediction [3].
In conclusion, the case study in cystic fibrosis provides robust, quantitative evidence that organoid models, particularly 2D monolayers, can effectively recapitulate patient-specific drug responses and show strong correlation with clinical outcomes, validating their use in preclinical research and personalized therapy. Although specific quantitative oncology case studies are not detailed here, the expanding use of PDOs in cancer research underscores the broad potential of this technology to transform drug discovery and development across diverse disease areas.
In the pursuit of precision oncology, accurately predicting patient-specific responses to therapy remains a paramount challenge. The validation of any preclinical model hinges on its demonstrable predictive power, quantitatively expressed through the fundamental metrics of sensitivity, specificity, and accuracy. These metrics provide the statistical foundation for evaluating how well a model's predictions correlate with actual clinical outcomes. Sensitivity measures the model's ability to correctly identify effective treatments (true positives), while specificity quantifies its capacity to rule out ineffective therapies (true negatives). Accuracy represents the overall proportion of correct predictions. Together, they form a crucial triad for assessing a model's translational reliability.
This guide objectively compares the predictive performance of emerging patient-derived organoid (PDO) models against established clinical tools like PET/CT imaging, framing this comparison within the broader thesis of validating in vitro organoid systems against gold-standard in vivo and clinical data. As organoids increasingly bridge the gap between traditional 2D cell cultures and complex in vivo environments, quantifying their predictive validity becomes essential for their integration into drug development pipelines and personalized treatment strategies.
Quantitative Comparison of Predictive Performance Across Models
The following tables summarize the reported performance metrics for various models used in therapy response prediction, providing a direct comparison of their predictive power.
Table 1: Predictive Performance of Clinical and Preclinical Models for Solid Tumors
| Model Type | Cancer Type | Sensitivity (%) | Specificity (%) | Accuracy (%) | Key Metric for Clinical Correlation | Reference |
|---|---|---|---|---|---|---|
| PET/CT (Hopkins Criteria) | Head & Neck SCC | 68.1 | 92.2 | 86.9 | Progression-Free Survival (PFS) & Overall Survival (OS) | [110] |
| PET/CT | Colorectal Cancer | 95.5 | 97.4 | 96.7 | Detection of Local Recurrence | [111] |
| Patient-Derived Organoids (PDOs) | Colorectal Cancer | ~85-98* | ~72-100* | Data pending | Correlation with Patient Clinical Response | [112] |
| PharmaFormer AI (Cell Line-Based) | Pan-Cancer (GDSC) | N/A | N/A | Pearson R: 0.742 | Prediction of Drug AUC in Cell Lines | [113] |
| PharmaFormer AI (Fine-Tuned on PDOs) | Colorectal Cancer | N/A | N/A | Hazard Ratio Improvement: 2.50 to 3.91* | Prediction of Patient Survival | [113] |
Range derived from multiple organoid studies; values are highly dependent on protocol and cancer type. Pearson correlation coefficient between predicted and actual drug response in cell lines. *Hazard Ratio for 5-fluorouracil prediction in TCGA patients, showing improvement after PDO fine-tuning.
Table 2: Fundamental Definitions of Key Predictive Metrics
| Metric | Definition | Clinical Interpretation | Formula |
|---|---|---|---|
| Sensitivity | Probability of a test being positive if the disease is present. | Ability to correctly identify a truly effective therapy. | TP / (TP + FN) |
| Specificity | Probability of a test being negative if the disease is absent. | Ability to correctly rule out an ineffective therapy. | TN / (TN + FP) |
| Accuracy | Overall probability that a test result is correct. | Overall rate of correct therapeutic predictions. | (TP + TN) / (TP + TN + FP + FN) |
| Positive Predictive Value (PPV) | Probability that the disease is present when the test is positive. | Probability that a predicted effective therapy will actually work. | TP / (TP + FP) |
| Negative Predictive Value (NPV) | Probability that the disease is absent when the test is negative. | Probability that a predicted ineffective therapy will truly fail. | TN / (TN + FN) |
TP = True Positive; TN = True Negative; FP = False Positive; FN = False Negative [114]
Experimental Protocols for Key Predictive Assays
PET/CT Imaging Interpretation with Hopkins Criteria
The Hopkins Criteria provide a standardized, qualitative 5-point scale for interpreting post-therapy PET/CT scans in head and neck squamous cell carcinoma (HNSCC), enabling reliable therapy response assessment.
- Objective: To validate a qualitative interpretation system for assessing therapy response and survival outcomes in HNSCC patients.
- Patient Population: 214 patients with biopsy-proven HNSCC who underwent post-therapy PET/CT between 5 and 24 weeks after treatment completion [110].
- Interpretation Protocol:
- Imaging: PET/CT studies are performed according to standard clinical protocols.
- Scoring: Three nuclear medicine physicians independently score the studies using a 5-point scale for the primary tumor, right neck, left neck, and an overall assessment.
- Dichotomization: Scores of 1, 2, and 3 are considered negative for residual tumor; scores of 4 and 5 are considered positive.
- Statistical Analysis: Inter-reader reliability is calculated using Cohen's κ coefficient. Overall survival (OS) and progression-free survival (PFS) are analyzed using Kaplan-Meier plots with log-rank tests [110].
- Key Validation: The criteria's predictive power is confirmed by significant differences in PFS and OS between patients with negative versus positive scores, particularly in HPV-positive cohorts.
High-Throughput Drug Sensitivity Testing in Patient-Derived Organoids
The mini-ring method enables automated, high-throughput drug sensitivity testing (DST) in PDOs, generating predictive data compatible with clinical decision-making timelines.
- Objective: To identify actionable drug sensitivities in patient-derived tumor organoids using a simple, high-throughput screening platform.
- Organoid Culture:
- Tissue Processing: Fresh tumor tissue is processed through mechanical and/or enzymatic digestion to create a single-cell suspension.
- Matrix Embedding: Cells are premixed with a cold extracellular matrix (e.g., Matrigel) at a 3:4 ratio.
- Mini-Ring Seeding: 10 µL of the cell-Matrigel mixture is seeded in a ring shape around the rim of 96-well plates. The ring configuration is maintained by surface tension until the matrix solidifies at 37°C [115].
- Drug Screening Protocol:
- Organoid Establishment: Organoids are cultured for 2-3 days after seeding.
- Drug Treatment: Two consecutive daily drug treatments are performed by complete medium change, pipetting directly into the center of the well to avoid disturbing the matrix ring.
- Viability Readout: After treatment, multiple endpoints can be measured:
- ATP-based Luminescence: For a metabolic readout of cell viability.
- Live-Cell Imaging: Using stains like calcein-AM (for live cells) and propidium iodide (for dead cells) [115].
- Automation: The mini-ring geometry is compatible with automated liquid handling systems, enabling screening of hundreds of compounds.
- Timeline: Results from screening 240 kinase inhibitors can be obtained within one week of surgery, a timeline compatible with therapeutic decision-making [115].
Visualizing Workflows and Relationships
PDO Drug Screening and Clinical Validation Workflow
Predictive Model Validation Logic
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Organoid-Based Therapy Response Prediction
| Reagent/Material | Function | Example Application |
|---|---|---|
| Extracellular Matrix (Matrigel) | Provides a 3D scaffold that mimics the basal membrane, supporting organoid growth and polarization. | Used for embedding dissociated tumor cells to form PDOs in the mini-ring screening protocol [115]. |
| Dispase/Collagenase | Enzymatic digestion of tumor tissue to create single-cell suspensions or fragment organoids for subculturing. | Critical for the initial processing of fresh tumor tissue to initiate organoid cultures [112]. |
| Stem Cell Factor Cocktail | A defined mixture of growth factors (e.g., EGF, Noggin, R-spondin) that maintains stemness and promotes organoid growth. | Added to the culture medium to support the long-term expansion of PDOs from various epithelial cancers [112]. |
| Calcein-AM / Propidium Iodide | Fluorescent live/dead viability stains. Calcein-AM labels live cells (green), while PI labels dead cells (red). | Used for endpoint live-cell imaging to quantify drug-induced cytotoxicity in organoid screening [115]. |
| ATP-Luminescence Assay Kits | Measures cellular ATP levels as a surrogate for metabolically active cells, enabling high-throughput viability readouts. | Provides a quantitative, automated readout of organoid viability after drug treatment in 96- or 384-well formats [115]. |
| Tumor Dissociation Kit | Optimized blends of enzymes for efficient tissue dissociation while maintaining high cell viability. | Standardizes the initial processing step of diverse tumor specimens for reproducible organoid establishment [112]. |
Discussion and Comparative Analysis
The quantitative data presented reveals a dynamic landscape in therapy response prediction. Established clinical tools like PET/CT imaging demonstrate high specificity and accuracy in detecting residual disease and predicting survival, with the Hopkins Criteria showing excellent inter-reader reliability (κ=0.69-0.86) [110]. This makes them valuable for post-therapy assessment. However, their application is largely confined to monitoring established disease rather than prospectively predicting which therapy will be effective for a given patient.
In contrast, patient-derived organoids offer a platform for prospective, personalized therapy prediction. While comprehensive sensitivity/specificity data for PDOs is still emerging, studies show they closely recapitulate patient responses to chemotherapy and radiotherapy [112]. The key advantage of PDOs lies in their functionality for high-throughput screening of therapeutic agents before treatment initiation, potentially expanding their predictive utility beyond imaging.
The integration of AI models like PharmaFormer represents a cutting-edge approach that leverages both cell line data and PDO information. The significant improvement in hazard ratios for predicting patient survival after fine-tuning the model with PDO data (e.g., from 2.50 to 3.91 for 5-fluorouracil in colon cancer) underscores the unique value of organoid pharmacogenomic data in enhancing predictive accuracy [113]. This hybrid approach may ultimately deliver the most powerful prediction tool, combining the scalability of computational models with the biological fidelity of PDOs.
As the field progresses, standardizing organoid culture protocols and validation metrics will be crucial for translating these promising results into clinically actionable tools that reliably guide personalized therapy selection.
The FDA Modernization Act 2.0, signed into law in December 2022, represents a fundamental transformation in pharmaceutical regulatory science by ending the mandate for animal testing for every new drug development protocol [116] [117]. This legislation refutes the Federal Food, Drug, and Cosmetic Act of 1938, which had required animal testing for over eight decades [116] [118]. The act permits the use of specific alternatives to animal testing, including cell-based assays, organoids, organs-on-chips, and advanced artificial intelligence methods for assessing drug safety and effectiveness during preclinical development [118]. This shift responds to the high attrition rates in drug development, where over 90% of drugs that pass animal studies fail in human trials due to unexpected toxicity or lack of efficacy [119]. By enabling the integration of human-relevant models that more accurately mirror human physiology and disease characteristics, this regulatory evolution creates an urgent need for standardized approaches to validate these new methodologies, particularly organoid technologies, against traditional in vivo development research.
The FDA Modernization Act 2.0: Implementation and Impact
Legislative Foundation and Implementation Timeline
The FDA Modernization Act 2.0 was introduced as S.5002 in the 117th Congress with the primary purpose of "allow[ing] for alternatives to animal testing for purposes of drug and biological product applications" [120]. The bill's provisions were incorporated into the Consolidated Appropriations Act, 2023, which was signed into law on December 29, 2022 [120]. The legislative journey and key implementation milestones are detailed in Table 1.
Table 1: Timeline of FDA Modernization Act 2.0 Implementation
| Date | Regulatory Action | Significance |
|---|---|---|
| September 29, 2022 | Bill introduced in Senate [120] | Legislative process begins |
| December 29, 2022 | Enacted as part of H.R. 2617 [120] | Becomes law, allowing non-animal alternatives |
| April 10, 2025 | FDA announces phased implementation plan [121] | Concrete steps to reduce animal testing reliance |
| April 11, 2025 | FDA Modernization Act 3.0 reintroduced [121] | Aims to further accelerate transition |
The FDA's April 2025 announcement detailed a comprehensive plan to phase out animal testing requirements, emphasizing the incorporation of New Approach Methodologies (NAMs) including "AI-based computational models of toxicity and cell lines and organoid toxicity testing in a laboratory setting" [121]. This implementation strategy will initially focus on monoclonal antibodies (mAbs) and other biologics that currently require extensive animal testing for safety and efficacy evaluations, with plans to expand to other biologics and eventually new chemical entities [121]. The FDA aims to make animal studies the exception rather than the norm within three to five years, with NAMs covering all critical areas of drug safety and efficacy testing [121].
Scientific and Economic Rationale
The regulatory shift embodied in the FDA Modernization Act 2.0 addresses fundamental limitations in traditional drug development paradigms. A significant concern is the poor translatability of results from animals to humans, which contributes to the high failure rate of drugs entering clinical trials [119] [117]. Only 10.4% of potential therapeutics entering Phase I trials between 2003-2014 achieved approval, with this rate dropping to 6-7% between 2011-2017 [118]. The most common causes of termination in Phase I and II clinical trials are lack of efficacy (60%) and toxicity (30%) [118].
These translational failures stem from fundamental species differences between animal models and humans that have substantial pharmacogenomic implications [118]. Enzymes involved in drug metabolism, such as cytochrome P450, vary between species, leading to differences in how drugs are broken down and cleared from the body [118]. Additionally, the limited genetic diversity in inbred rodent models (sharing roughly 98.6% of their genome) fails to represent the vast genetic variability of human populations, where "as few as 1 in 25 people are optimal responders to common medications" [118].
Organoids as Validated Preclinical Models: Methodologies and Standardization
Organoid Generation and Culture Protocols
Organoids are three-dimensional miniature structures cultured in vitro that recapitulate the cellular heterogeneity, structure, and functions of human organs [122]. They can be generated from either human pluripotent stem cells (hPSCs), including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), or adult stem cells (AdSCs) derived from healthy individuals or patients [122]. The general workflow for generating tumor organoids, as exemplified in cancer research, involves several critical steps that require standardization for regulatory acceptance [67].
Table 2: Key Steps in Tumor Organoid Generation
| Step | Protocol Details | Variations by Tissue Type |
|---|---|---|
| Sampling | Surgical or non-surgical methods [67] | Endoscopic biopsy (esophageal), urine (bladder cancer), pleural effusions (lung cancer) [67] |
| Digestion | Enzymatic (collagenase/hyaluronidase, TrypLE Express) and mechanical disruption [67] | Incubation time (2h to overnight), use of ROCK inhibitor for sensitive tissues [67] |
| Filtration | Cell strainer filtration (70μm/100μm) [67] | Pore size determined by tumor type and desired cluster size [67] |
| ECM Embedding | Matrigel, BME, Geltrex [67] | Droplet plating (10-20μL) for low cell numbers vs. large-volume methods [67] |
| Culture | Specific cytokine cocktails [67] | Wnt3A, Noggin, R-spondin for intestine; HGF for liver organoids [78] |
The following diagram illustrates the generalized workflow for organoid generation, highlighting critical decision points that require standardization:
Critical Research Reagents and Standardization Solutions
The reproducibility of organoid models depends heavily on standardized research reagents and culture components. Variations in these essential materials represent a significant challenge in validating organoids against in vivo development research.
Table 3: Essential Research Reagents for Organoid Standardization
| Reagent Category | Key Components | Function in Culture | Standardization Challenges |
|---|---|---|---|
| Extracellular Matrix (ECM) | Matrigel, BME, Geltrex, synthetic hydrogels [67] [78] | Provides 3D structural support, regulates cell behavior [78] | Batch-to-batch variability in animal-derived matrices [78] |
| Growth Factors & Cytokines | EGF, Noggin, R-spondin, Wnt3A, B27 [67] [78] | Maintain stemness, direct differentiation [78] | Tissue-specific requirements; concentration optimization [78] |
| Digestion Enzymes | Collagenase/hyaluronidase, TrypLE Express [67] | Tissue dissociation for cell isolation [67] | Incubation time optimization; tissue-specific protocols [67] |
| Specialized Media Components | ROCK inhibitor, N2 supplement, N-acetylcysteine [67] [78] | Enhance cell viability, support growth [67] | Proprietary formulations; supplier variability |
Validation Against In Vivo Models: Key Methodological Approaches
Validating organoid models against traditional in vivo development research requires multifaceted approaches that assess how well organoids recapitulate the physiology, pathology, and drug responses of living systems. Key methodological frameworks for this validation include:
Histological and Genomic Comparison: Tumor organoids have demonstrated remarkable fidelity to parental tumors in histology and genomics, capturing their heterogeneity and drug response [67]. Studies comparing patient-derived organoids (PDOs) with original tumor tissues show retention of key morphological features, expression markers, and genetic alterations, including driver mutations and copy number variations [123] [78].
Drug Response Correlation: A critical validation approach involves comparing drug sensitivity profiles between organoids and clinical patient responses. In a landmark study, colorectal cancer PDOs were used to identify a lead bispecific antibody that reached clinical trials within 5 years from initial development, demonstrating the predictive power of properly validated organoid models [117]. Validation experiments typically involve dose-response assays, calculation of IC50 values, and correlation with clinical outcomes where available [123].
Immune Microenvironment Recapitulation: Advanced validation efforts focus on replicating complex tumor-immune interactions using organoid-immune co-culture models. These include both innate immune microenvironment models that retain tumor-infiltrating lymphocytes from original samples, and reconstituted models where immune components are added to established organoids [78]. These systems can predict responses to immunotherapies, including immune checkpoint inhibitors and CAR-T therapies [78].
The following diagram illustrates the key approaches for validating organoid models against in vivo biology:
Comparative Performance Data: Organoids vs. Traditional Models
Technical and Functional Comparisons
Rigorous comparison of organoids with traditional preclinical models provides critical data for regulatory validation and researcher adoption. The table below synthesizes quantitative and qualitative performance metrics across model systems.
Table 4: Comprehensive Model Comparison for Drug Development Applications
| Parameter | 2D Cell Cultures | Animal Models | Organoid Models |
|---|---|---|---|
| Clinical Translation Accuracy | 5-10% predictive value [119] | <10% approval rate from preclinical [118] | High correlation in validated systems [117] |
| Tumor Heterogeneity Preservation | Limited, genetic drift [67] [123] | Preserved in PDX [67] | High, maintains parental tumor diversity [67] [123] |
| Culture/Timeline | Days to weeks [123] | Months for PDX [67] [123] | 1-3 weeks establishment [67] |
| Cost Considerations | Low [67] | High (facilities, lengthy studies) [117] | Moderate, decreasing with standardization [67] |
| Genetic Manipulation | Easy [67] | Complex, time-consuming [67] | Amenable to gene editing [67] [78] |
| Throughput for Screening | High [67] [123] | Low [67] | Medium to high with optimization [123] [78] |
| TME Complexity | Limited cell-cell interactions [67] [123] | In vivo physiology but species differences [118] | Can incorporate immune, stromal components [78] |
| Success Rate Establishment | High for established lines | Variable, ~20% for PDX [123] | 70-90% for many carcinomas [67] |
Experimental Protocol for Drug Response Validation
A standardized protocol for validating organoid drug responses against clinical outcomes is essential for regulatory acceptance. The following detailed methodology is compiled from multiple established organoid screening platforms:
Organoid Drug Sensitivity Assay Protocol:
Organoid Preparation: Passage organoids at 70-80% confluence using appropriate dissociation reagents (TrypLE Express or accutase) to generate single cells or small clusters [67]. Adjust cell density based on specific organotype growth characteristics.
Plating and Recovery: Plate dissociated organoids in ECM droplets (Matrigel or BME) in 96-well plates at optimized densities (500-5000 cells/well depending on proliferation rate) [67] [123]. Culture for 3-5 days to allow recovery and formation of 3D structures before drug exposure.
Drug Treatment Preparation: Prepare drug stocks in appropriate vehicles (typically DMSO) and create serial dilutions in complete organoid media. Include vehicle controls and reference compounds where available [123].
Drug Exposure and Incubation: Add drug dilutions to organoid cultures, typically for 5-7 days with medium refreshment at day 3-4 [123]. Test a range of concentrations (typically 8-10 points in half-log or log dilutions) to generate dose-response curves.
Viability Assessment: Measure cell viability using ATP-based assays (CellTiter-Glo 3D), live-cell imaging, or immunohistochemical staining for cleavage markers [123]. Normalize values to vehicle-treated controls.
Data Analysis: Calculate IC50 values using four-parameter nonlinear regression. For clinical correlation, compare with patient response data using metrics such as sensitivity-specificity ROC analysis [123] [78].
This protocol can be adapted for specific applications, including immunotherapy assessment through co-culture with autologous immune cells [78], and combination therapy screening through factorial drug designs.
The FDA Modernization Act 2.0 has initiated a fundamental restructuring of drug development paradigms by creating a regulatory pathway for human-relevant models like organoids. The successful integration of these technologies into mainstream pharmaceutical development depends on establishing robust validation frameworks that demonstrate consistent performance against traditional in vivo models. Current evidence indicates that properly standardized organoid systems can recapitulate key aspects of human physiology and disease states, particularly in preserving tumor heterogeneity and predicting drug responses [67] [123] [117].
Significant challenges remain in achieving full standardization, particularly in areas of ECM reproducibility [78], culture protocol harmonization [67], and immune component integration [78]. However, emerging technologies including synthetic hydrogels [78], automated screening platforms [119] [123], and AI-driven analysis [78] [118] are rapidly addressing these limitations. The ongoing development of the FDA Modernization Act 3.0 [121] signals continued regulatory evolution toward human-relevant systems that may ultimately increase the efficiency and success rate of drug development while reducing reliance on animal models.
Conclusion
The validation of organoid models against in vivo development marks a paradigm shift in biomedical research, offering a more human-relevant, ethical, and personalized approach to disease modeling and drug development. While challenges in standardization, maturation, and functional complexity persist, interdisciplinary innovations in bioengineering, AI, and microfluidics are rapidly addressing these gaps. The convergence of regulatory support, such as the FDA's new roadmap, and robust comparative evidence positions organoid technology as an indispensable tool for the future. Future efforts must focus on creating fully vascularized, immune-competent systems and establishing universal standards to fully realize their potential in accelerating translational research and delivering effective precision medicines to patients.
References
- 1. Organoids, 3D Organoid Research | Molecular Devices [https://www.moleculardevices.com/applications/3d-cell-models/organoids]
- 2. Advancing organoid using highly research growth factors... validated [https://www.news-medical.net/whitepaper/20240606/Advancing-Organoid-Research-Using-Highly-Validated-Growth-Factors-and-Cytokines.aspx]
- 3. Trends: 2025 Organoids [https://www.genengnews.com/topics/genome-editing/2025-trends-organoids/]
- 4. 3D and organoid culture in research: physiology, hereditary genetic diseases and cancer | Cell & Bioscience | Full Text [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-022-00775-w]
- 5. Frontiers | Organoids technology in cancer research : from basic... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1569337/full]
- 6. New Approach Methodologies (NAMs) | Harvard Bioscience [https://www.harvardbioscience.com/applications/nams]
- 7. Harnessing single-cell genomics to improve the physiological fidelity of... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-018-0527-2]
- 8. PDX-derived organoids drug response and secrete... model in vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC7710298/]
- 9. An in tumour vivo based on the chick embryonic... organoid model [https://ejnmmires.springeropen.com/articles/10.1186/s13550-024-01151-0]
- 10. Engineering the 3D structure of organoids - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11784486/]
- 11. assessment technologies - PMC Organoid [https://pmc.ncbi.nlm.nih.gov/articles/PMC10731122/]
- 12. Organoids: A new window into disease, development and discovery | Harvard Stem Cell Institute (HSCI) [https://www.hsci.harvard.edu/organoids]
- 13. Patient-derived tumor organoids: a new avenue for preclinical research and precision medicine in oncology | Experimental & Molecular Medicine [https://www.nature.com/articles/s12276-024-01272-5]
- 14. Challenges in validation of combination treatment strategies for CRC... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-024-03173-x]
- 15. Tumor microenvironment- preserving gliosarcoma organoids as an in... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06952-y]
- 16. Brain organoid: a 3D technology for investigating cellular composition and interactions in human neurological development and disease models in vitro | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02369-8]
- 17. Airway Organoid : The Key to Deciphering Molecular... Models [https://www.dovepress.com/airway-organoid-models-as-pivotal-tools-for-unraveling-molecular-mecha-peer-reviewed-fulltext-article-TCRM]
- 18. Advances in the Development and Application of Human Organoids: Techniques, Applications, and Future Perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11775963/]
- 19. Frontiers | Research Progress, Challenges, and Breakthroughs of Organoids as Disease Models [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.740574/full]
- 20. Challenges of Organoid Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10559943/]
- 21. Immune organoids : emerging platforms for modeling and analyzing... [https://pubmed.ncbi.nlm.nih.gov/40843000/]
- 22. Frontiers | Organoid : applications and models advances in... research [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1432506/full]
- 23. Breakthroughs and challenges of organoid models for assessing cancer immunotherapy: a cutting-edge tool for advancing personalised treatments - PubMed [https://pubmed.ncbi.nlm.nih.gov/40335487/]
- 24. Machine Learning Model Predicts Organoid Quality [https://www.technologynetworks.com/cell-science/news/machine-learning-model-predicts-organoid-quality-403126]
- 25. Human organoids: model systems for human biology and medicine | Nature Reviews Molecular Cell Biology [https://www.nature.com/articles/s41580-020-0259-3]
- 26. Liver organoids: updates on generation strategies and biomedical applications | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03865-3]
- 27. Disease modelling in human organoids - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6679380/]
- 28. Frontiers | Brain model systems of neurodegenerative... organoid [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1604435/full]
- 29. Johns Hopkins scientists grow novel 'whole- brain ' organoid | Hub [https://hub.jhu.edu/2025/07/25/hopkins-researchers-develop-whole-brain-organoid/]
- 30. Advances in the Construction and Application of Research ... Intestinal [https://www.besjournal.com/en/article/doi/10.3967/bes2025.010]
- 31. Mouse Model: Which is Better Organoid Tool to... vs In Vivo Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC8593653/]
- 32. Organoid models in oncology: advancing precision cancer therapy and vaccine development | Cancer Biology & Medicine [https://www.cancerbiomed.org/content/early/2025/07/24/j.issn.2095-3941.2025.0127]
- 33. Frontiers | Organoids and spheroids: advanced in vitro models for liver cancer research [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1536854/full]
- 34. Frontiers | Patient-Derived Organoids in Precision Medicine: Drug Screening, Organoid-on-a-Chip and Living Organoid Biobank [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.762184/full]
- 35. Frontiers | Advances of Patient - Derived in Organoids ... Personalized [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.888416/full]
- 36. PDOs, PDXOs, PDOXs or PDXs? Selecting the Best Model to... [https://blog.crownbio.com/pdos-pdxos-pdoxs-or-pdxs-selecting-the-best-model-to-progress-your-patient-centric-research]
- 37. established from primary tumors and patient-derived... Organoid models [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14811-8]
- 38. Patient-derived organoids for precision oncology: a platform to facilitate clinical decision making | BMC Cancer | Full Text [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-023-11078-9]
- 39. Combining molecular characteristics and therapeutic analysis of PDOs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11863571/]
- 40. Development of a deep learning based image processing tool for enhanced organoid analysis | Scientific Reports [https://www.nature.com/articles/s41598-023-46485-2]
- 41. A quantitative pipeline for whole-mount deep imaging and analysis of multi-layered organoids across scales [https://elifesciences.org/reviewed-preprints/107154]
- 42. Frontiers | Modeling neurodegenerative diseases with brain... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1663286/full]
- 43. Revolutionizing Disease : The Emergence of Modeling in... Organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC10047824/]
- 44. Multiscale 3D phenotyping of human cerebral organoids | Scientific Reports [https://www.nature.com/articles/s41598-020-78130-7]
- 45. Long-term live imaging and multiscale analysis identify heterogeneity and core principles of epithelial organoid morphogenesis | BMC Biology | Full Text [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-021-00958-w]
- 46. : A versatile deep learning platform for tracking and analysis... OrganoID [https://pmc.ncbi.nlm.nih.gov/articles/PMC9645660/]
- 47. Digitalized organoids: integrated pipeline for high-speed 3D analysis of organoid structures using multilevel segmentation and cellular topology | Nature Methods [https://www.nature.com/articles/s41592-025-02685-4]
- 48. MultiOrg: A Multi-rater Organoid -detection Dataset [https://arxiv.org/html/2410.14612v1]
- 49. Adaptation of High - Throughput in Screening ... Drug [https://pmc.ncbi.nlm.nih.gov/articles/PMC3269696/]
- 50. Toxicity assessment using neural organoids: innovative approaches and challenges | Toxicological Research [https://link.springer.com/article/10.1007/s43188-025-00279-y]
- 51. Assay establishment and validation of a high-throughput organoid-based drug screening platform | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02902-3]
- 52. Comprehensive and unbiased multiparameter high - throughput ... [https://elifesciences.org/articles/73760]
- 53. Urban Institute Data Visualization style guide [http://urbaninstitute.github.io/graphics-styleguide/]
- 54. organoid- Tumor - immune models: exploring a new... co culture [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019369/]
- 55. Co-culturing multicellular tumor models: Modeling the tumor microenvironment and analysis techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8262778/]
- 56. Frontiers | Unraveling the immune evasion mechanisms in the tumor microenvironment of head and neck squamous cell carcinoma [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597202/full]
- 57. Advances in engineering immune – tumor ... microenvironments [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02479-4]
- 58. Cell Culture Model Evolution and Its Impact on Improving Therapy Efficiency in Lung Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10605536/]
- 59. Frontiers | Deciphering T- cell exhaustion in the tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1548234/full]
- 60. Frontiers | Research progress on mechanisms of tumor immune microenvironment and gastrointestinal resistance to immunotherapy: mini review [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1641518/full]
- 61. Introduction to the ISoOR-ISOB & Why This Standard Matters [https://www.linkedin.com/pulse/introduction-isoor-isob-why-standard-matters-isoor-tspwe]
- 62. Market Size, Share and Growth Report 2032 Biobank Organoids [https://www.credenceresearch.com/report/biobank-organoids-market]
- 63. Tumor organoid biobank-new platform for medical research | Scientific Reports [https://www.nature.com/articles/s41598-023-29065-2]
- 64. Organoid biobanks as a new tool for pre-clinical validation of candidate drug efficacy and safety - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012858/]
- 65. Living biobank: Standardization of organoid construction and challenges - PubMed [https://pubmed.ncbi.nlm.nih.gov/39663560/]
- 66. Frontiers | Organoids -on-a-chip: microfluidic technology enables... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1515340/full]
- 67. Modeling methods of different tumor organoids and their application in tumor drug resistance research [https://www.oaepublish.com/articles/cdr.2025.34]
- 68. iPSC-derived and Patient-Derived Organoids : Applications and... [https://pubmed.ncbi.nlm.nih.gov/40276485/]
- 69. Stem Cells and Organoids: A Paradigm Shift in Preclinical Models Toward Personalized Medicine [https://www.mdpi.com/1424-8247/18/7/992]
- 70. Long-term expansion, genomic stability and in safety of adult... vivo [https://bmcdevbiol.biomedcentral.com/articles/10.1186/s12861-020-0209-5]
- 71. Brain Organoids : A Revolutionary Tool for Modeling Neurological... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842775/]
- 72. Dynamic Characterization of Structural, Molecular, and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7291286/]
- 73. Single-cell guided prenatal derivation of primary fetal ... | Nature Medicine [https://www.nature.com/articles/s41591-024-02807-z?error=cookies_not_supported]
- 74. Engineering the Beating Heart: Cardiac Organoid for Models ... Tissue [https://www.intechopen.com/online-first/1227666]
- 75. Vascularised organoids: Recent advances and applications in cancer research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11882480/]
- 76. Human organoids-on-chips for biomedical research and applications [https://www.thno.org/v14p0788.htm]
- 77. A novel quantitative angiogenesis assay based on visualized vascular organoid - PubMed [https://pubmed.ncbi.nlm.nih.gov/39751990/]
- 78. Breakthroughs and challenges of organoid models for assessing cancer immunotherapy: a cutting-edge tool for advancing personalised treatments | Cell Death Discovery [https://www.nature.com/articles/s41420-025-02505-w]
- 79. Frontiers | 3D organ-on-a-chip: The convergence of microphysiological systems and organoids [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1043117/full]
- 80. From organoids to organoids-on-a-chip: Current applications and challenges in biomedical research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11970821/]
- 81. Three-dimensional bioprinting in human-relevant toxicology... [https://accscience.com/journal/IJB/articles/online_first/5167]
- 82. Advanced 3D Imaging and Organoid Bioprinting for Biomedical Research and Therapeutic Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11031334/]
- 83. Patient-Specific Organoid and Organ-on-a-Chip: 3D Cell-Culture Meets 3D Printing and Numerical Simulation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8243895/]
- 84. Bioprinting on Organ-on-Chip: Development and Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9775862/]
- 85. One-step fabrication of an organ - on - a - chip with spatial heterogeneity... [https://pubmed.ncbi.nlm.nih.gov/27302471/]
- 86. Frontiers | 3 at the Frontier of Regenerative Medicine... D Bioprinting [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2020.607648/full]
- 87. Bioprinters for Organs-On-Chips - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6756175/]
- 88. as an in vitro Organoids of human model and disease development [https://www.nature.com/articles/ncb3312?error=cookies_not_supported]
- 89. Image Classification: State-of-the-Art Models in 2025 [https://hiringnet.com/image-classification-state-of-the-art-models-in-2025]
- 90. Editorial for the Special Issue “Advances in Medical Image Processing, Segmentation, and Classification” - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071901/]
- 91. Mimicking embryonic growth to break barriers in organoid research [https://www.sciencedaily.com/releases/2025/04/250408121640.htm]
- 92. Leading AI-Driven Drug Discovery Platforms: 2025 Landscape and Global Outlook - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 93. Could Organoids Make Animal Obsolete in Research? Models [https://www.news-medical.net/health/Can-Organoids-Replace-Animal-Models-in-Human-Disease-Research.aspx]
- 94. 3D Organoids Lines in Drug Discovery & Disease vs 2 D Cell Modeling [https://www.moleculardevices.com/lab-notes/3d-biology/3d-organoids-vs-2d-cell-lines-drug-discovery]
- 95. 3 2 | FluoroFinder D vs D Cell Cultures [https://fluorofinder.com/2d-vs-3d-cell-cultures/]
- 96. (PDF) Comparative Efficacy of 3Dimensional (3 D ) Cell ... Culture [https://www.academia.edu/144456380/Comparative_Efficacy_of_3Dimensional_3D_Cell_Culture_Organoids_Vs_2Dimensional_2D_Cell_Cultures_Vs_Experimental_Animal_Models_In_Disease_modeling_Drug_development_And_Drug_Toxicity_Testing]
- 97. Tumor organoids: A review of culture methods, applications in cancer research, precision medicine, and drug development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574996/]
- 98. Replacing Animal Testing with Stem Cell-Organoids : Advantages and Limitations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319430/]
- 99. 3 2 : Choosing the Right D vs D Cell Culture Model [https://www.tempobioscience.com/2d-vs-3d-cell-culture-choosing-the-right-model-by-tempo-bioscience/]
- 100. Application of Human Brain Organoids —Opportunities and Challenges... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10420018/]
- 101. organs on chip: A Organoids Review by Elveflow VS Comparative [https://elveflow.com/microfluidic-reviews/organoids-vs-organ-on-a-chip/]
- 102. PDX-derived organoids and secrete... model in vivo drug response [https://pubmed.ncbi.nlm.nih.gov/32990680/]
- 103. Frontiers | Advances in precision oncology using patient-derived... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1670328/full]
- 104. Deep learning-driven drug response prediction and mechanistic insights in cancer genomics | Scientific Reports [https://www.nature.com/articles/s41598-025-91571-2]
- 105. Assessment of modelling strategies for drug response prediction in cell lines and xenografts | Scientific Reports [https://www.nature.com/articles/s41598-020-59656-2]
- 106. technology in cancer Organoids : from basic applications to... research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12137298/]
- 107. Anticancer drug response prediction integrating multi-omics pathway-based difference features and multiple deep learning techniques | PLOS Computational Biology [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1012905]
- 108. -on-a-chip: microfluidic technology enables culture of... Organoids [https://research.utwente.nl/en/publications/organoids-on-a-chip-microfluidic-technology-enables-culture-of-or]
- 109. -derived human intestinal monolayers for... Validating organoid [https://pmc.ncbi.nlm.nih.gov/articles/PMC10079552/]
- 110. Head and neck PET/CT: therapy interpretation criteria... response [https://pubmed.ncbi.nlm.nih.gov/24947059/]
- 111. of 18F-FDG PET/CT in monitoring Accuracy ... therapeutic response [https://ejrnm.springeropen.com/articles/10.1186/s43055-020-00151-z]
- 112. Building consensus on the application of organoid-based drug sensitivity testing in cancer precision medicine and drug development [https://www.thno.org/v14p3300.htm]
- 113. PharmaFormer predicts clinical drug responses through transfer learning guided by patient derived organoid | npj Precision Oncology [https://www.nature.com/articles/s41698-025-01082-6]
- 114. sciencedirect.com/topics/medicine-and-dentistry/ sensitivity -and... [https://www.sciencedirect.com/topics/medicine-and-dentistry/sensitivity-and-specificity]
- 115. A simple high-throughput approach identifies actionable drug sensitivities in patient-derived tumor organoids | Communications Biology [https://www.nature.com/articles/s42003-019-0305-x]
- 116. FDA Modernization Act 2.0 allows for alternatives to animal testing - PubMed [https://pubmed.ncbi.nlm.nih.gov/36762462/]
- 117. The FDA . Modernization : A patient-centric paradigm shift in... Act 2 0 [https://blog.huborganoids.nl/patient-centric-drug-development-with-organoids]
- 118. JCI - FDA . Modernization : transitioning beyond animal models... Act 2 0 [https://www.jci.org/articles/view/175824]
- 119. . FDA : What Labs Need... | Technology Networks Modernization Act 2 0 [https://www.technologynetworks.com/drug-discovery/articles/boost-fda-modernization-act-20-readiness-with-an-advanced-lims-403885]
- 120. . FDA (2022; 117th Congress...) - GovTrack.us Modernization Act 2 0 [https://www.govtrack.us/congress/bills/117/s5002]
- 121. Announces Plan to Phase Out Animal Testing Requirement FDA [https://www.hklaw.com/en/insights/publications/2025/04/fda-announces-plan-to-phase-out-animal-testing-requirement]
- 122. Human organoids in basic research and clinical applications | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-022-01024-9]
- 123. Frontiers | Advancements and challenges in culturing patient-derived cancer cells for personalized therapeutics [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2025.1663420/full]