Mastering Whole-Mount Immunofluorescence for Cardiac Crescent Stage Embryos: A Complete Guide for Developmental Biology Research
This comprehensive guide details the application of whole-mount immunofluorescence (WMIF) for analyzing cardiac progenitor populations during the critical cardiac crescent stage of mouse embryonic development.
Mastering Whole-Mount Immunofluorescence for Cardiac Crescent Stage Embryos: A Complete Guide for Developmental Biology Research
Abstract
This comprehensive guide details the application of whole-mount immunofluorescence (WMIF) for analyzing cardiac progenitor populations during the critical cardiac crescent stage of mouse embryonic development. Covering foundational principles through advanced optimization, we explore the significance of the cardiac crescent in early heart formation, provide a step-by-step protocol for volumetric imaging and 3D reconstruction, address common troubleshooting scenarios with evidence-based solutions, and validate the technique through comparisons with modern single-cell and spatial transcriptomics approaches. Designed for researchers and drug development professionals, this resource enables precise quantitative analysis of cardiac progenitor localization and organization, facilitating deeper investigation into congenital heart defects and regenerative strategies.
Understanding Cardiac Crescent Formation: Developmental Principles and Significance in Heart Organogenesis
The Cardiac Crescent as the Developmental Precursor to the Heart Tube
Application Note: Analyzing Cardiac Crescent Morphogenesis
The cardiac crescent (CC) stage represents a pivotal morphological event in early mammalian cardiogenesis, where bilateral cardiac progenitors reorganize to form the primitive linear heart tube (HT) [1]. This process involves highly coordinated tissue deformation and cell movements, which, if disrupted, can lead to congenital heart defects [2]. Understanding the morphogenetic trajectory from the cardiac crescent to the heart tube is therefore fundamental for developmental biology and cardiac disease modeling. This application note details integrated methodologies for the quantitative analysis of cardiac crescent morphogenesis, combining whole-mount immunofluorescence, live imaging, and computational modeling to provide a multiscale understanding of this critical developmental transition.
Key Findings and Quantitative Data
Recent quantitative analyses have revealed strongly compartmentalized tissue deformation patterns underlying mammalian heart tube formation [3]. The table below summarizes the core quantitative findings related to the morphogenetic process from the cardiac crescent to the early heart tube.
Table 1: Key Quantitative Findings in Cardiac Crescent to Heart Tube Morphogenesis
| Parameter | Finding | Experimental Model | Significance |
|---|---|---|---|
| Tissue Deformation Analysis | Strong spatio-temporal compartmentalization of strain and growth patterns [3] | Mouse embryo explants (E7.75-E8.5) | Reveals harnessed, regionalized tissue remodeling rather than uniform growth. |
| Cell Tracking Validation | Computational motion estimation validated against >9,000 manual cell tracks [3] | Nkx2.5-GFP mouse embryos with sparse labeling | Confirms accuracy of displacement tensors for high-resolution tissue deformation analysis. |
| Developmental Time Window | Primary heart tube formation occurs rapidly, between ~E7.75 and E8.5 in mouse [1] | Mouse embryo (in vivo & ex vivo culture) | Defines the narrow, critical period for observing CC-to-HT transition. |
| Progenitor Contribution | Mesp1+ precursor cells contribute approximately 70% of cells to the heart [1] | Mouse lineage tracing studies | Establishes the major source of cardiac progenitors during gastrulation. |
Experimental Workflow
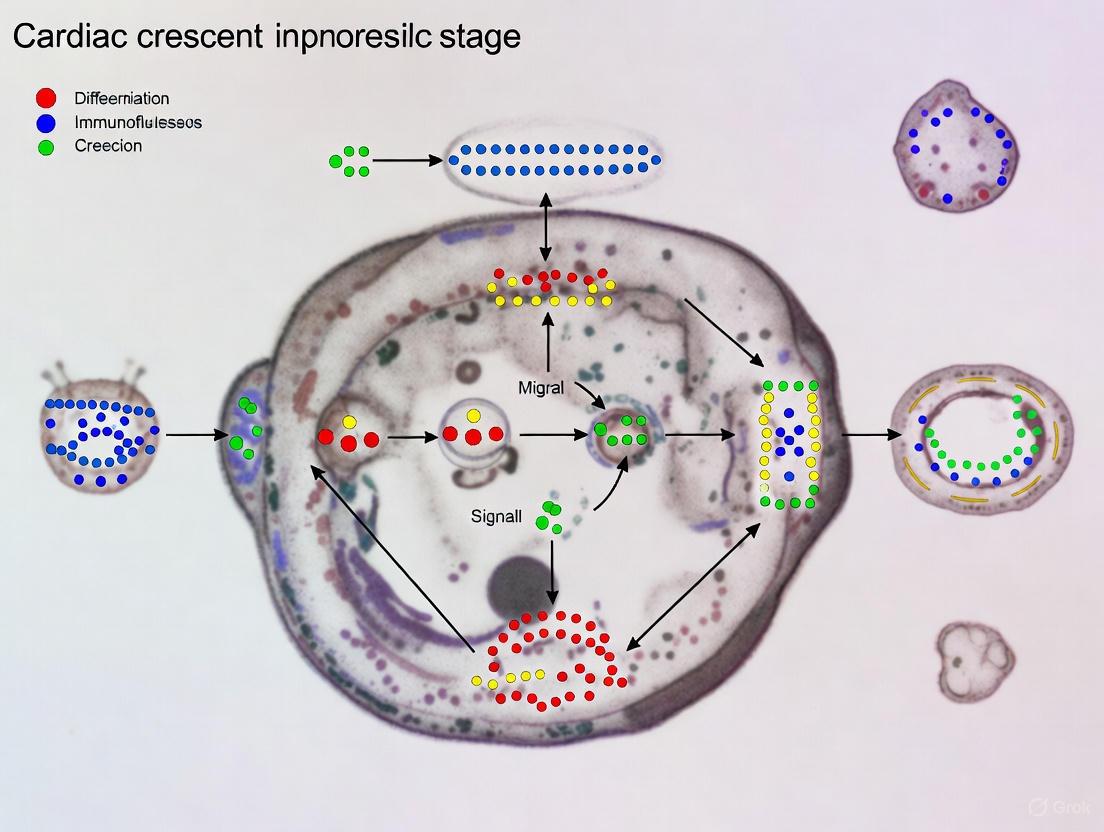
The comprehensive analysis of cardiac crescent morphogenesis requires a multi-step workflow that integrates specimen preparation, imaging, and computational analysis, as visualized below.
Protocols
Protocol 1: Whole-Mount Immunofluorescence with Autofluorescence Reduction for Cardiac Crescent Staged Embryos
This protocol is optimized for high-signal-to-noise imaging of cardiac crescent staged mouse embryos, incorporating oxidation-mediated autofluorescence reduction (OMAR) to minimize background [4].
Reagents and Materials
- Mouse Embryos: Dissected at E7.5-E8.5 from timed pregnancies.
- Fixative: 4% Paraformaldehyde (PFA) in PBS.
- OMAR Solution: 2.5 mM CuSO~4~, 25 mM Ammonium Acetate, 2.5% Triton X-100 in PBS.
- Permeabilization Solution: PBS with 2.5% Triton X-100.
- Blocking Solution: PBS with 10% heat-inactivated lamb serum and 2.5% Triton X-100.
- Primary Antibodies: e.g., Anti-NKX2-5 (rabbit), Anti-GATA4 (mouse).
- Secondary Antibodies: Fluorescently conjugated (e.g., Alexa Fluor 488, 568).
- Mounting Medium: Vectashield or equivalent antifading medium.
Procedure
- Embryo Collection and Fixation: Dissect embryos in cold PBS, maintaining extra-embryonic membranes for orientation. Fix in 4% PFA for 2 hours at 4°C on a rotator. Wash 3x with PBS.
- Oxidation-Mediated Autofluorescence Reduction (OMAR): Incubate embryos in OMAR solution under bright fluorescent light (e.g., 100W mercury arc lamp) for 2 hours at room temperature. This photochemical bleaching step quits endogenous fluorophores [4].
- Permeabilization and Blocking: Wash embryos 3x with PBS. Permeabilize with Permeabilization Solution for 1 hour. Replace solution with Blocking Solution and incubate for 4 hours at 4°C.
- Antibody Staining: Incubate with primary antibodies diluted in Blocking Solution for 48-72 hours at 4°C. Wash 6x over 24 hours with PBS containing 0.1% Tween-20 (PBS-T). Incubate with secondary antibodies diluted in Blocking Solution for 24-48 hours at 4°C, protected from light. Wash 6x over 24 hours with PBS-T.
- Clearing and Mounting: Clear embryos using a mild clearing agent (e.g., FocusClear or 50% Glycerol in PBS). Mount on a glass-bottom dish for 3D confocal or light-sheet microscopy.
Protocol 2: Live Imaging and Computational Analysis of Tissue Deformation
This protocol outlines the procedure for capturing and quantifying the dynamic tissue remodeling during the CC to HT transition [3].
Reagents and Materials
- Live Embryo Explants: Embryos (E7.5) from transgenic reporter lines (e.g., Nkx2.5-GFP [3] or Mesp1-Cre;Ai14).
- Ex Vivo Culture Media: DMEM/F12 supplemented with serum replacement.
- Imaging Setup: Confocal or light-sheet microscope with environmental chamber (37°C, 5% CO~2~).
- Computational Tools: Medical Image Registration Toolbox (MIRT) [3], custom scripts for strain analysis (Raiola et al., 2025b).
Procedure
- Embryo Explant Preparation and Mounting: Dissect E7.5 embryos with cardiac crescents intact. Place the explant on a membrane filter or in a glass-bottom dish with culture media to immobilize for live imaging [3] [1].
- Time-Lapse Imaging: Acquire 3D image stacks every 5-15 minutes for 12-24 hours using a long-working-distance objective to capture the entire morphogenetic sequence from CC to early HT.
- Image Registration and Staging: Segment the myocardial tissue from time-lapse data to create "Live-Shapes." Register each specimen to a standardized 3D+t developmental Atlas using a morphometric staging system [3].
- Computational Motion Estimation: Apply the MIRT algorithm to the raw 3D time-lapse images to compute displacement tensors for each point in the tissue over time [3].
- Deformation Map Calculation: Calculate local tissue deformation parameters (growth rate
J, anisotropyθ, magnitude of deformationε) between consecutive time points. Generate cumulative maps of tissue strain and the Strain Agreement Index (φ) to identify regions of coordinated versus chaotic deformation [3].
Table 2: Key Research Reagent Solutions for Cardiac Crescent Studies
| Item | Function/Application | Example Reagents/Tools |
|---|---|---|
| Transgenic Mouse Lines | Lineage tracing and live imaging of cardiac progenitors. | Nkx2.5-GFP [3], Mesp1-Cre [3] [1], Islet1-Cre [3]. |
| Key Antibodies | Marker analysis for cardiac progenitors and differentiated cells via immunofluorescence. | Anti-NKX2-5 [2], Anti-GATA4 [2], Anti-MEF2C. |
| Computational Tools | Quantifying tissue deformation, motion estimation, and atlas registration. | Medical Image Registration Toolbox (MIRT) [3], Custom pipelines for strain analysis [3]. |
| 3D+t Developmental Atlas | Spatio-temporal reference framework for aligning and comparing multiple specimens. | Pseudo-dynamic Atlas of mouse heart morphogenesis [3]. |
Signaling Pathways in Cardiac Crescent Development
The formation and maturation of the cardiac crescent are regulated by a network of conserved signaling pathways and transcription factors. The diagram below summarizes the core interactions.
Expected Results and Data Interpretation
Successful application of these protocols will yield several key outcomes, including high-contrast 3D reconstructions of the cardiac crescent's cellular architecture, a quantitative description of tissue strain patterns showing compartmentalized deformation, and virtual fate maps predicting the contribution of each CC region to the nascent heart tube [3]. The strain analysis is expected to reveal a harnessed expansion at the future outer curvature, constrained by belts at the arterial and venous poles, providing a new model for heart tube formation [3]. Integration of data into the 3D+t Atlas allows for direct comparison between wild-type and mutant embryos or under different pharmacological treatments, facilitating the identification of subtle morphogenetic defects that may underlie congenital heart conditions.
The mammalian heart, a vital organ for embryonic survival, arises from the sophisticated spatiotemporal coordination of distinct progenitor populations during cardiogenesis. As the first functional organ to form, the heart's development is a rapid and precise process, with key decisions about cell fate occurring early in gestation [5]. Disruptions to this process are a leading cause of congenital birth defects, underscoring the critical need to understand its underlying mechanisms [5]. The cardiac crescent, the first morphologically recognizable heart structure, emerges at approximately embryonic day (E) 8.0 in mice and day 20 of gestation in humans [5]. This arc of immature cardiomyocytes forms from the coordinated integration of multiple progenitor sources that have undergone different specification pathways [5]. Among these, the First Heart Field (FHF) and Second Heart Field (SHF) represent the two principal populations of cardiac progenitors, which are the focus of intense research within developmental biology and whole mount immunofluorescence studies [6].
Defining the Heart Fields: Characteristics and Markers
Cardiac progenitor populations are anatomically and molecularly defined regions within the embryo that contribute cells to the forming heart. While traditionally viewed as distinct lineages, recent high-resolution studies suggest a more complex continuum of progenitor states [7].
Table 1: Key Characteristics of First and Second Heart Fields
| Feature | First Heart Field (FHF) | Second Heart Field (SHF) |
|---|---|---|
| Primary Contribution | Left ventricle, parts of atria [8] | Right ventricle, outflow tract, most of atria [8] |
| Differentiation Timing | Early; differentiates rapidly to form the cardiac crescent and linear heart tube [8] | Later; maintains proliferative, undifferentiated state while being added to the heart tube [9] [8] |
| Key Molecular Markers | Tbx5 [5], Myl2 [10], Fhl2 [10] | Islet1 (Isl1) [5], Tbx1 [5], Fgf10 [5] |
| Spatial Location in Crescent | Forms the core of the cardiac crescent [9] | Located dorsal and medial to the crescent; a proliferative progenitor pool [5] |
It is crucial to note that marker expression is dynamic. For instance, Islet1, often considered an SHF marker, is broadly expressed in all cardiac progenitors prior to cardiac crescent formation but is rapidly downregulated upon cardiomyocyte differentiation [5] [8]. Furthermore, the SHF can be subdivided into anterior (aSHF) and posterior (pSHF) domains, giving rise to the outflow tract/right ventricle and atria, respectively, and are patterned by factors like retinoic acid [10].
Whole Mount Immunofluorescence for Cardiac Crescent Analysis
Whole mount immunofluorescence (IF) enables three-dimensional spatial reconstruction of progenitor populations within the intact cardiac crescent, providing both cell- and tissue-level quantitative information that is lost in traditional sectioning methods [6].
Protocol: Harvesting and Processing Cardiac Crescent Stage Embryos
The following protocol, adapted from Bardot et al., details the steps for harvesting and preparing mouse embryos for whole mount IF analysis [6].
- Embryo Collection: Sacrifice a pregnant dam at E8.25 (plug day = E0.5). Exact timing can be strain-dependent and should be determined empirically by embryo morphology [6].
- Uterine Dissection: Remove the entire uterine horn and place it in phosphate-buffered saline (PBS). Sub-dissect the uterus to isolate individual decidua, which contain the embryos [6].
- Embryo Dissection: Under a dissection microscope, use fine forceps (#5) to carefully remove the uterine and decidual tissue to reveal the embryo. Gently pull the embryo out and dissect away extraembryonic tissues without damaging embryonic morphology [6].
- Fixation: Transfer embryos to a tube and fix with 4% paraformaldehyde (PFA) in PBS for 1 hour at room temperature (or overnight at 4°C). Rinse three times with PBS after fixation. Embryos can be stored in PBS at 4°C for several weeks at this point [6].
Protocol: Immunofluorescence Staining and Imaging
This section details the staining and imaging procedures to visualize specific progenitor populations [6].
- Permeabilization and Blocking: Remove PBS and incubate embryos in blocking buffer (0.5% saponin, 1% BSA in PBS) for at least 4 hours at room temperature to permeabilize tissues and prevent non-specific antibody binding [6].
- Primary Antibody Incubation: Incubate embryos in a primary antibody mixture diluted in blocking buffer overnight at 4°C.
- Washing: Remove primary antibodies and wash the embryos three times for 1 hour each with 0.1% Triton in PBS [6].
- Secondary Antibody Incubation: Incubate with fluorescently conjugated secondary antibodies diluted in blocking buffer for 3 hours at room temperature (or overnight at 4°C) [6].
- Counterstaining and Final Washes: Counterstain with DAPI to label nuclei. Perform two final 5-minute washes with 0.1% Triton in PBS [6].
- Mounting and Imaging: Suspend embryos in an anti-fade mounting medium. Mount on a microscope slide using double-stick tape or silicone spacers to create a chamber that prevents embryo crushing. Image using a confocal microscope to generate high-resolution z-stacks for 3D reconstruction and quantitative analysis [6].
The Scientist's Toolkit: Essential Research Reagents
The table below lists critical reagents used in the featured whole mount immunofluorescence protocol for studying cardiac progenitors [6].
Table 2: Key Research Reagent Solutions
| Reagent | Function / Application |
|---|---|
| Anti-Nkx2-5 Antibody | Reference stain for the entire cardiac crescent; essential for tissue segmentation and quantitative analysis of progenitor zones [6]. |
| Saponin | Detergent used in blocking and antibody buffers to permeabilize cell membranes, allowing antibodies to access intracellular targets [6]. |
| Bovine Serum Albumin (BSA) | Used as a blocking agent to reduce non-specific binding of antibodies, thereby lowering background signal [6]. |
| Anti-Foxa2Cre:YFP | Example of a genetic lineage tracer used to mark and track the fate of specific progenitor populations [6]. |
| n-Propyl Gallate (nPG) in Glycerol | Anti-fade mounting medium that reduces photobleaching of fluorescent signals during prolonged confocal microscopy imaging [6]. |
Signaling Pathways Governing Progenitor Dynamics
The specification and patterning of FHF and SHF progenitors are controlled by an evolutionarily conserved network of signaling pathways. The diagram below illustrates the key pathways and their interactions.
Diagram: Signaling in Cardiac Progenitor Specification. Pathways like Wnt inhibition, BMP, and FGF promote cardiogenesis. RA posteriorizes the SHF, inhibiting aSHF and promoting pSHF fate.
Advanced Concepts and Recent Paradigms
Recent technological advances are refining our understanding of heart field dynamics, moving beyond the classical binary model.
The Continuum Model: High-resolution single-cell and live-imaging studies suggest that FHF and SHF progenitors may not represent strictly predetermined lineages but rather a continuum of cardiogenic cells derived from the lateral head mesoderm. Cell recruitment into the heart appears to depend on cell position, morphogenetic movements, and the breakdown of tissue bridges, rather than a rigid lineage boundary [7].
Novel Progenitor Populations: Beyond FHF and SHF, a distinct population called the Juxta Cardiac Field (JCF) has been identified. The JCF resides adjacent to the forming cardiac crescent and gives rise to both myocardial and epicardial cells, highlighting an unexpected lineage relationship [5] [10].
Mechanics of Morphogenesis: The SHF functions as an atypical epithelium, and its morphogenesis is driven by patterned mechanical forces. Single-cell morphometric analyses reveal that transcription factors like Tbx1 and Tbx5 are required to orient cell shape and establish epithelial tension, directly linking genetic programs to the cellular mechanics of heart tube elongation [11].
Application Notes for Drug Development and Disease Modeling
Understanding heart field dynamics has direct translational applications for disease modeling and regenerative medicine.
In Vitro Modeling of Congenital Disease: The ability to direct human pluripotent stem cells (hPSCs) into specific heart field fates (FHF, aSHF, pSHF) by modulating pathways like retinoic acid signaling provides a powerful platform for modeling congenital heart diseases. For example, this approach has identified specific transcriptional dysregulation in FHF and SHF progenitors derived from patients with hypoplastic left heart syndrome (HLHS) [10].
Blueprint for Regeneration: A detailed understanding of how distinct cardiomyocyte subtypes are generated during embryogenesis provides a blueprint for developing regenerative therapies. This knowledge can inform strategies to differentiate stem cells into specific cardiac cell types for cell replacement therapy or to stimulate endogenous repair mechanisms in the adult heart after injury, such as a myocardial infarction [5].
The precise identification and isolation of cardiac progenitor populations are fundamental to understanding the molecular and cellular events that orchestrate heart development. These progenitor cells give rise to the diverse cellular components of the mature heart, and errors in their specification, migration, or differentiation underlie many congenital heart defects. The integration of advanced techniques, particularly whole-mount immunofluorescence, with the use of specific molecular markers now enables the qualitative and quantitative three-dimensional analysis of these progenitors within their native architectural context. This Application Note details the essential molecular signatures for identifying key cardiac progenitor populations and provides a standardized protocol for their volumetric analysis in mouse embryos at the cardiac crescent stage, a critical period in early heart morphogenesis. Framed within the context of whole-mount immunofluorescence research, this guide provides researchers with the methodologies to move beyond two-dimensional analysis and achieve a comprehensive spatial understanding of cardiac progenitor organization.
Essential Molecular Signatures of Cardiac Progenitors
Cardiac progenitors can be distinguished by their unique spatiotemporal expression of specific transcription factors and surface markers. The following table summarizes the primary markers essential for identifying major progenitor populations during early cardiogenesis.
Table 1: Key Molecular Markers for Identifying Cardiac Progenitor Populations
| Marker | Progenitor Population | Expression Pattern / Role | Key Findings from Lineage Tracing |
|---|---|---|---|
| Nkx2-5 | First Heart Field (FHF), Second Heart Field (SHF) | Early marker for cardiac crescent; key reference stain for image segmentation and analysis [12] [13]. | Labels SHF-derived smooth muscle in the aorta, distributed to the adventitial side of the aortic media, revealing a boundary with neural crest-derived cells [13]. |
| Foxa2 | Ventricular-Specified Cardiac Progenitors (Foxa2-vCPs) | Transiently expressed during gastrulation; labels progenitors for ventricular cardiomyocytes and epicardial cells [14]. | Foxa2+ cells at gastrulation contribute primarily to both ventricular chambers; later Foxa2 expression is excluded from differentiated cardiovascular lineages [14]. |
| Isl1 | Second Heart Field (SHF) | Marks SHF progenitors that give rise to the right ventricle, outflow tract, and parts of the atria [14]. | - |
| Mesp1 | Early Pre-cardiac Mesoderm | Transiently expressed in the pre-cardiac mesoderm during early gastrulation [13]. | Labels early progenitors that contribute to SHF-derived smooth muscle on the adventitial side of the aorta [13]. |
| GFRA2 | Multipotent Cardiac Progenitors (CPs) | Surface marker that specifically identifies cardiac progenitors among mesodermal cells, enabling isolation without genetic modification [15]. | Facilitates the isolation of multipotent or unipotent CPs from mouse and human pluripotent stem cells; vital for cardiomyocyte differentiation [15]. |
| PrP (CD230) | Atypically-shaped Cardiomyocytes (ACMs) | Surface marker for isolating cardiac progenitors; co-expressed with cardiac Troponin T (cTnT) in native ACMs [16]. | PrP+ cTnT+ cells are present in the border of necrotic tissue in myocardial infarction, suggesting ischemic resistance [16]. |
Research Reagent Solutions
The following table catalogs essential reagents and materials required for the successful execution of whole-mount immunofluorescence and the analysis of cardiac progenitors.
Table 2: Key Research Reagent Solutions for Cardiac Progenitor Analysis
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| Foxa2Cre:YFP Mouse Line | Genetic lineage tracing of Foxa2-expressing ventricular progenitors. | Foxa2T2AiCre (Foxa2Cre) crossed with Rosa26-YFP or Rosa26-tdTomato reporter mice [14]. |
| Nkx2-5 Antibody | Reference immunofluorescence stain for delineating the cardiac crescent structure. | Used for whole-mount immunofluorescence; key for downstream image segmentation [12]. |
| Cardiac Troponin T (cTnT) Antibody | Immunofluorescence marker for cardiomyocytes and committed cardiac progenitors. | Used to identify mature cardiomyocytes and PrP+ cTnT+ ACMs [16]. |
| sm22α & smMHC Antibodies | Markers for smooth muscle cell lineage in outflow tract and great vessels. | sm22α used in embryonic stages with cTnT counterstain; smMHC for mature smooth muscle [13]. |
| CHIR99021 | Small molecule GSK3β inhibitor; activates WNT signaling to direct pluripotent stem cells toward mesoderm. | Used in "WNT Switch" and "2i+LIF" protocols for efficient cardiac differentiation of mESCs [17] [18]. |
| XAV939 | Small molecule tankyrase inhibitor; inhibits WNT signaling to commit mesodermal cells to cardiomyocytes. | Used in sequence with CHIR99021 in the "WNT Switch" method for mESC cardiomyocyte differentiation [17]. |
| Anti-fade Mounting Media | Preserves fluorescence signal during microscopy and prevents photobleaching. | Formulation with 2% w/v n-Propyl gallate (nPG), 90% glycerol, 1x PBS [12]. |
Whole-Mount Immunofluorescence Protocol for Cardiac Crescent Analysis
This protocol is adapted from established methodologies [12] and is designed for the volumetric analysis of cardiac progenitor populations in E8.25 mouse embryos.
The following diagram outlines the major stages of the protocol, from embryo collection to final quantitative analysis.
Detailed Experimental Methodology
Part I: Harvesting and Processing Cardiac Crescent Stage Embryos (E8.25)
- Embryo Dissection: Sacrifice a pregnant dam at E8.25, where noon of the day of a vaginal plug is considered E0.5 [12]. Remove the uterine horn and dissect individual decidua in cold phosphate-buffered saline (PBS). Under a dissection microscope, use fine forceps (#5) to remove uterine and decidual tissues, followed by careful removal of extraembryonic membranes to reveal the embryo without damaging its morphology.
- Fixation: Transfer embryos to a 1.5 mL tube using a transfer pipette. Fix embryos in 4% paraformaldehyde (PFA) in PBS for 1 hour at room temperature (RT) or overnight at 4°C.
- Storage: Rinse embryos three times with PBS after fixation. Embryos can be stored in PBS at 4°C for several weeks at this point.
Part II: Whole-Mount Immunofluorescence Staining
- Blocking: Remove PBS and add 1 mL of blocking buffer (0.5% saponin, 1% bovine serum albumin (BSA) in PBS). Incubate for at least 4 hours at RT or overnight at 4°C with gentle shaking or rocking.
- Primary Antibody Incubation: Prepare primary antibody mixture in blocking buffer. The use of a reference antibody such as Nkx2-5 is critical for defining the cardiac crescent [12]. Incubate embryos with the primary antibody mixture overnight at 4°C.
- Note: Antibody dilutions should be determined empirically.
- Washing: Remove the primary antibody by aspiration. Wash the embryos three times for 1 hour each with 0.1% Triton X-100 in PBS.
- Secondary Antibody Incubation: Remove the wash and add a secondary antibody mixture diluted in blocking buffer. Incubate for 3 hours at RT or overnight at 4°C.
- Counterstaining and Final Washes: Counterstain nuclei with DAPI (e.g., 10 minutes in PBS). Perform two final 5-minute washes with 0.1% Triton in PBS.
Part III: Mounting and Imaging
- Mounting: Suspend embryos slowly in an anti-fade mounting medium (e.g., 2% w/v n-propyl gallate, 90% glycerol, 1x PBS). Allow embryos to equilibrate for at least 1 hour before mounting.
- Slide Preparation: Prepare microscope slides using double-stick tape or silicone spacers to create a chamber that prevents crushing the embryo. Position the embryo in the chamber and carefully cover with a coverslip.
- Confocal Microscopy: Image the mounted embryos using a confocal microscope. Acquire z-stacks with sufficient resolution and step size to enable accurate three-dimensional reconstruction of the cardiac crescent.
Part IV: Image Analysis and Quantification
- 3D Reconstruction: Use image processing software (e.g., Imaris, Volocity, or open-source alternatives like Fiji/ImageJ with 3D plugins) to reconstruct the z-stack images into a volumetric model.
- Segmentation and Masking: Use the reference stain (e.g., Nkx2-5) to create a mask that defines the boundaries of the cardiac crescent.
- Quantitative Measurements: Within the defined mask, quantify the volume, spatial distribution, and signal intensity of the experimental marker (e.g., Foxa2Cre:YFP). This allows for the analysis of the localization and organization of specific progenitor populations within the cardiac crescent [12].
Signaling Pathways in Cardiac Progenitor Specification
The differentiation of cardiac progenitors from pluripotent stem cells is a tightly regulated process. The "WNT Switch" protocol, which temporally controls WNT signaling, is a prime example of harnessing these pathways for efficient cardiomyocyte generation [17]. The following diagram illustrates this core signaling logic and its application.
This protocol, leveraging sequential WNT activation and inhibition, provides a robust and simplified system for generating cardiomyocytes from mESCs, making it an excellent tool for assessing the role of specific genes or factors in cardiac differentiation [17] [18]. The efficiency of this system can be tracked using surface markers like PDGFRα or specific fluorescent reporter lines [18].
The combination of well-defined molecular signatures and sophisticated whole-mount immunofluorescence techniques provides an powerful framework for analyzing cardiac progenitor populations in unprecedented detail. The application notes and detailed protocols outlined here, centered on markers like NKX2-5 and Foxa2, provide researchers with a reliable path to quantitatively assess the three-dimensional organization of progenitors during the critical cardiac crescent stage. This approach is not only essential for advancing our fundamental understanding of heart development but also provides a critical methodological foundation for modeling congenital heart diseases and for developing targeted regenerative strategies.
The journey from a primitive streak to a cardiac crescent represents a foundational period in mammalian embryogenesis, during which the blueprint for the heart is first established. This process involves the precise spatial organization and temporal coordination of progenitor cell populations, culminating in the formation of the cardiac crescent—the earliest embryonic structure with clear cardiac identity [12]. Understanding these dynamic morphogenetic events is crucial not only for fundamental developmental biology but also for elucidating the origins of congenital heart diseases and advancing regenerative medicine strategies [2].
Recent technological advances in whole-mount immunofluorescence, live imaging, and computational analysis have transformed our ability to visualize and quantify these early developmental processes in unprecedented detail [12] [19]. This Application Note provides detailed methodologies and analytical frameworks for investigating the spatiotemporal organization of cardiac progenitor cells from primitive streak migration through cardiac crescent formation, with particular emphasis on whole-mount immunofluorescence approaches compatible with subsequent volumetric analysis.
Biological Background
Developmental Timeline of Early Cardiogenesis
Cardiac development initiates during gastrulation as mesodermal cells migrate through the primitive streak [2]. The heart, as the first functional organ in the fetus, undergoes a complex developmental process starting from the differentiation of mesodermal cells during gastrulation [2]. This process involves three main regions with cardiac precursor cells: the cardiogenic mesoderm, the proepicardium, and the cardiac neural crest [2].
Through coordinated regulation of various signaling pathways, heart development begins with the migration of mesodermal cells from the primitive streak, moving to both sides of the embryonic midline formatting two heart-forming regions (HFRs), each consisting of the first heart field (FHF) on the anterior lateral side and the secondary heart field (SHF) on the anterior medial side [2]. The HFRs then merge to form the cardiac crescent, from which cells of the FHF eventually fold to form the primitive heart tube, initiating subsequent pulsation [2].
Table: Key Developmental Stages in Early Mouse Cardiogenesis
| Developmental Stage | Approximate Timing | Major Morphological Events | Key Molecular Markers |
|---|---|---|---|
| Primitive Streak | E6.5-E7.5 | Mesoderm formation and migration | Brachyury, Wnt3 [20] |
| Heart-Forming Regions | E7.5-E8.0 | Bilateral fields of cardiac progenitors | NKX2-5, GATA4 [2] |
| Cardiac Crescent | E8.0-E8.5 | Fusion of heart fields at anterior midline | NKX2-5, Foxa2Cre:YFP [12] |
| Early Heart Tube | E8.5-E9.0 | Tube formation and initiation of beating | NKX2-5, MEF2 [2] |
Signaling Pathways and Molecular Regulation
The formation of the cardiac crescent is regulated by an intricate network of signaling pathways and transcription factors. The determination process begins with the formation of the primary heart field from mesodermal cells at the embryo's anterior, which differentiate into cardiac progenitor cells [21]. At the site of gastrulation, Wnt growth factors block differentiation of the mesodermal cells. As these cells migrate anteriorly, they leave the Wnt expression domain and enter a domain of active Wnt inhibition, gaining the capacity to enter the cardiac lineage [21].
The transcription factor NKX2-5 is a marker of cardiac precursor cells that regulates the proliferation and differentiation of these cells in the early phases of cardiac development [2]. Another important transcription factor for cardiac development, GATA4, has been found to interact with NKX2-5 through its zinc finger structure and specific residues in the C-terminal extension, while bone morphogenetic protein (BMP) 4, one of the growth factors essential for embryonic heart development, has been suggested to regulate NKX2-5 expression via GATA4 [2].
The following diagram illustrates the key signaling pathways and transcriptional regulators involved in cardiac crescent formation:
Experimental Workflow for Whole-Mount Immunofluorescence
The following comprehensive protocol enables qualitative and quantitative analysis of cardiac progenitor cell populations within the developing cardiac crescent, providing both cell- and tissue-level information through confocal microscopy and three-dimensional spatial reconstruction [12].
Embryo Collection and Fixation
Materials:
- Pregnant dam mice (E8.25, with plug detection considered E0.5) [12]
- Phosphate buffered saline (PBS, pH 7.4)
- 4% paraformaldehyde (PFA) in PBS
- Fine forceps (#5)
- Dissection microscope
Protocol:
- Sacrifice the pregnant dam by CO2 inhalation or according to local and institutional regulations on the morning of E8.25 [12].
- Expose the viscera through an abdominal incision and locate the uterus [12].
- Remove the entire uterine horn by cutting above the oviducts and through the cervix [12].
- Place the uterus in a 10 cm dish with PBS to wash away excess blood [12].
- Sub-dissect the uterus by cutting the mesometrium between each deciduum containing embryos [12].
- Under a dissection microscope, use fine forceps to remove uterine tissue from the decidual tissue [12].
- Carefully slice the tip of the embryonic half of the deciduum to reveal the embryo and pinch the deciduum to push the embryo out [12].
- Dissect away extraembryonic tissues as much as possible without damaging embryo morphology [12].
- Transfer embryos to a 1.5 mL tube with fresh PBS and place on ice [12].
- Fix embryos with 4% PFA in PBS for 1 hour at room temperature (or overnight at 4°C) [12].
- Rinse three times with PBS and store at 4°C until ready for immunofluorescence (embryos can be stored for several weeks) [12].
Critical Considerations:
- Exact timing can be strain dependent and should be determined empirically by morphology [12].
- Plugs should be checked for in the morning, as they are lost throughout the day [12].
- Manual removal of solutions is recommended at all steps to avoid loss of embryos [12].
Whole-Mount Immunofluorescence Staining
Materials:
- Blocking buffer (0.5% saponin, 1% BSA in PBS) [12]
- Primary antibodies (e.g., anti-NKX2-5, anti-YFP for Foxa2Cre:YFP) [12]
- Secondary antibodies conjugated to fluorophores
- Wash buffer (0.1% Triton X-100 in PBS) [12]
- DAPI (4',6-diamidino-2-phenylindole) for nuclear counterstaining
- Anti-fade mounting media (2% w/v n-Propyl gallate, 90% glycerol, 1x PBS) [12]
Protocol:
- Remove PBS and add 1 mL of blocking buffer [12].
- Incubate for at least 4 hours at room temperature (or overnight at 4°C) [12].
- Remove blocking buffer and add primary antibody mixture diluted in blocking buffer [12].
- Incubate overnight at 4°C [12].
- Note: Antibody dilutions should be determined empirically. The use of Nkx2-5 as a reference stain for the cardiac crescent is recommended, and is key to downstream image segmentation and analysis steps [12].
- Remove primary antibodies by aspiration [12].
- Wash 3 times for 1 hour each with 0.1% Triton in PBS [12].
- Remove wash and add secondary antibody mixture diluted in blocking buffer [12].
- Incubate for 3 hours at room temperature (or overnight at 4°C) [12].
- Wash 3 times for 1 hour each with 0.1% Triton in PBS (can be done overnight at 4°C) [12].
- Counterstain with DAPI in PBS for 10 minutes [12].
- Note: This counterstain can be performed simultaneously with secondary antibody [12].
- Wash 2 times for 5 minutes each with 0.1% Triton in PBS [12].
- Slowly suspend embryos in anti-fade mounting media and allow to equilibrate for at least 1 hour before mounting [12].
- Note: Embryos can be stored for several days in anti-fade solution until ready to mount and image [12].
The following workflow diagram summarizes the key experimental steps:
Mounting and Imaging
Materials:
- Microscope slides with double-stick tape or silicone spacers [12]
- Confocal microscope with appropriate laser lines and filters
Protocol:
- Prepare microscope slides for mounting using either double-stick tape or silicone spacers [12].
- If using double-stick tape, make two parallel stacks of 5-6 layers about 15-20 mm apart to create a space for embryos and secure the coverslip [12].
- Transfer embryos to the mounting chamber in anti-fade media.
- Carefully position embryos to optimize orientation for imaging.
- Seal coverslip with clear nail polish or commercial sealant.
- Image using confocal microscopy with appropriate laser lines and filter sets for the fluorophores used.
- Acquire z-stacks with sufficient resolution for subsequent three-dimensional reconstruction.
Image Acquisition Parameters:
- Resolution: 1024 × 1024 or higher depending on objective
- Z-step size: 0.5-1.0 μm depending on embryo size and resolution requirements
- Laser power and gain settings optimized to maximize signal-to-noise ratio while avoiding saturation and photobleaching
Quantitative Analysis and Computational Approaches
Image Processing and Volumetric Analysis
Recent advances in both confocal microscopy and 3D image analysis allow for high-resolution and high-throughput algorithmic reconstructions of cells and structures in situ with relative ease, thus paving the way for detailed studies of complex cellular structures [12]. With the increase of computational power and the development of big-data managing algorithms, both necessary to handle the exponential increase of the size of imaging data-sets, analyses can now be fully automated [12].
The quantitative analysis pipeline typically includes:
- Image Pre-processing: Background subtraction, noise reduction, and channel alignment [12].
- Segmentation: Identification of the cardiac crescent using reference markers (e.g., NKX2-5) [12].
- Masking: Successive masking of specific progenitor populations within the cardiac crescent [12].
- Quantitative Measurement: Calculation of volumes, positions, and spatial relationships between different progenitor populations [12].
Computational Analysis of Tissue Deformation
For dynamic analysis of morphogenetic processes, computational frameworks can extract regional and temporal patterns of tissue deformation. One recently developed workflow includes [19]:
- Individual time-lapse analysis to capture myocardial geometry [19].
- Integration of multiple time-lapse datasets through spatiotemporal registration [19].
- Quantification of cardiac spatiotemporal deformation patterns [19].
- In-silico fate mapping to investigate how different cardiac crescent regions contribute to the forming heart tube [19].
Table: Parameters for Quantitative Analysis of Cardiac Crescent Morphogenesis
| Parameter | Description | Calculation Method | Biological Significance |
|---|---|---|---|
| Tissue Growth Rate (J) | Local rate of tissue expansion | Computed from deformation of mesh triangles between consecutive time points [19] | Identifies regions of active proliferation |
| Tissue Anisotropy (θ) | Directionality of tissue deformation | Calculated from strain tensors [19] | Reveals patterned tissue remodeling |
| Strain Agreement Index (φ) | Local coordination of strain directions | Quantifies coordination between neighboring regions [19] | Distinguishes ordered vs. chaotic deformation |
| Progenitor Population Volume | Volume occupied by specific progenitor cells | 3D reconstruction from segmented immunofluorescence images [12] | Quantifies contribution of different heart fields |
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Whole-Mount Immunofluorescence of Cardiac Crescent Stage Embryos
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Fixatives | 4% Paraformaldehyde (PFA) [12] | Preserves cellular structure by crosslinking proteins | Standard fixation; avoid over-fixation to prevent epitope masking [22] |
| Permeabilization Agents | 0.1% Triton X-100 [12], Saponin [22] | Disrupts membranes allowing antibody penetration | Saponin is gentler, better for surface antigens [22] |
| Blocking Agents | 1% BSA [12], Animal serums (e.g., goat serum) [22] | Reduces non-specific antibody binding | Use serum from secondary antibody host species for best results [22] |
| Primary Antibodies | Anti-NKX2-5 [12], Anti-YFP (for Foxa2Cre:YFP) [12] | Binds specific antigens of interest | Validate for whole-mount applications; determine optimal dilution empirically [12] |
| Secondary Antibodies | Fluorophore-conjugated anti-species antibodies [23] | Binds primary antibodies with fluorescent detection | Choose fluorophores compatible with microscope filters; consider spectral overlap [22] |
| Nuclear Counterstains | DAPI [12] | Labels all nuclei for spatial reference | Can be performed simultaneously with secondary antibody [12] |
| Mounting Media | Anti-fade media with n-Propyl gallate [12] | Preserves fluorescence and enables imaging | Prevents photobleaching during imaging [12] |
Troubleshooting and Technical Considerations
Antibody Validation and Optimization
The selection of the primary antibody and its incubation conditions is the most critical step of an immunofluorescence staining protocol [24]. Most antibody manufacturers do not do extensive antibody validation, and so it falls on the end user to make sure that the chosen antibody works for their application [22]. Ideal validation includes:
- Testing against tissues or cells with known expression (positive control) [22].
- Testing against tissues or cells with no expression (negative control) [22].
- Including a secondary antibody-only control to assess non-specific binding [22].
- Performing antibody titration to determine optimal concentration [22].
Multiplexing Considerations
For multicolor stainings, different specific primary antibodies for the parallel detection of several antigens in the same sample must be produced in different hosts, in order to avoid cross-reactivity [24]. When building a panel, it is best to use antibodies that come from different host species, however this isn't always possible as mouse or rabbit may be the only option available [22]. In such cases, many mouse antibodies can be paired together, as long as they have different isotypes (e.g., IgG, IgG1, IgG2a) and care is taken when choosing secondary antibodies and when to apply them [22].
Fixation and Permeabilization Optimization
The goal of fixation is to preserve the structure of cells or tissues so that they can be labeled and visualized post-experiment [22]. Both under-fixing (not allowing enough time in the fixative) and over-fixing (too much time in the fixative) can cause issues with downstream labeling [22]. Under-fixing is more of an issue in 3D samples where not enough time is allowed for the fixative to diffuse through the entire sample, leaving a center section unfixed which results in cell decay in that area [22]. Over-fixation can occur with any sample and typically results in the masking of antibody epitopes and thus poor labeling [22].
For intracellular targets, permeabilization is required which disrupts the cell membrane, allowing for passage of antibodies into the cell [22]. Permeabilization can be done using a detergent (e.g., Triton X-100) or even through fixation, such as with methanol [22]. If the target is on the cell surface, a permeabilization step may not be necessary [22]. However, combining cell surface targets with internal targets often requires making sure that the permeabilization step doesn't disrupt the cell surface target [22].
The integration of whole-mount immunofluorescence with advanced computational analysis provides a powerful framework for investigating the spatiotemporal organization of cardiac progenitor cells during the critical developmental window from primitive streak migration to cardiac crescent formation. The protocols and methodologies outlined in this Application Note enable researchers to capture both qualitative and quantitative information about the dynamic morphogenetic processes that establish the foundation for heart development.
As technological advances in imaging, tissue clearing, and computational analysis continue to evolve, so too will our ability to resolve the intricate cellular behaviors and molecular interactions that guide early cardiogenesis. These approaches not only advance fundamental developmental biology but also provide critical insights into the origins of congenital heart diseases, potentially informing new diagnostic and therapeutic strategies in the future.
In the study of embryogenesis, particularly during critical phases such as the cardiac crescent stage, understanding the precise spatial organization of progenitor cells is paramount. Whole-mount imaging has emerged as a groundbreaking technique that allows scientists to gain comprehensive insights into tissue organization and cellular interactions without disrupting the native tissue architecture [25]. This approach is indispensable for research focused on cardiac crescent stage embryos, as it enables the three-dimensional spatial reconstruction of this key structure, thereby providing the ability to analyze the localization and organization of specific progenitor populations [26] [27]. By preserving the overall architecture of the tissue, whole-mount imaging facilitates the study of relationships between cells and their microenvironment, revealing crucial insights into developmental processes and disease mechanisms [25].
Technical Advantages: A Quantitative Comparison
The critical advantage of whole-mount imaging over traditional sectioning methods lies in its ability to preserve intact three-dimensional spatial relationships. The table below summarizes the key technical benefits quantified through established protocols.
Table 1: Quantitative Advantages of Whole-Mount Imaging for 3D Analysis
| Technical Feature | Traditional Sectioning Method | Whole-Mount Imaging Approach | Quantitative Impact on Cardiac Crescent Analysis |
|---|---|---|---|
| Spatial Context | 2D slices; spatial relationships between sections are inferred and modeled. | Direct 3D visualization of entire structure in its native state [25]. | Enables quantitative 3D spatial reconstruction of the cardiac crescent for analyzing progenitor population organization [26]. |
| Data Integrity | Physical sectioning introduces tissue loss, compression, and folding artifacts. | No physical sectioning; architecture remains pristine [25]. | Eliminates reconstruction artifacts, allowing for reliable successive masking and quantitative measurements within the crescent [26]. |
| Cell-Level Information | Risk of losing rare progenitor cells during section processing. | All cells within the volume are captured and can be localized [26]. | Provides both cell- and tissue-level information, crucial for fate mapping and genetic lineage tracing in the developing heart [26] [27]. |
| Throughput & Efficiency | Labor-intensive serial sectioning and staining required for 3D data. | Single-sample processing, staining, and imaging workflow [25]. | Protocol is designed for comprehensive analysis and is adaptable to most organ systems in the gastrula to early somite stage mouse embryo [26]. |
Detailed Experimental Protocol for Cardiac Crescent Analysis
The following protocol is adapted from the quantitative whole-mount immunofluorescence method established for visualizing cardiac progenitor populations in mouse embryos [26].
Sample Preparation and Fixation
- Dissection: Carefully isolate gastrula to early somite stage mouse embryos in fresh phosphate-buffered saline (PBS). The dissection of the cardiac crescent must be performed with precision to preserve its delicate structure.
- Fixation: Immerse embryos in freshly prepared 4% Paraformaldehyde (PFA) in PBS. Fixation time must be optimized for embryo size and stage to ensure adequate penetration while preserving antigenicity for subsequent immunolabeling.
Whole-Mount Immunofluorescence Staining
- Permeabilization and Blocking: Incubate fixed embryos in a permeabilization/blocking buffer (e.g., PBS containing 0.3% Triton X-100, 0.3% BSA, and 3% goat serum) for several hours to overnight. This step is critical for antibody penetration into the intact tissue and for reducing non-specific background staining [28].
- Antibody Incubation: Incubate embryos with primary antibodies specific to cardiac progenitor cell markers (e.g., Nkx2-5, Isl1) diluted in blocking buffer. This is followed by extensive washing and subsequent incubation with fluorophore-conjugated secondary antibodies. The use of reference antibodies allows for successive masking of the cardiac crescent structure during analysis [26].
Sample Mounting and Imaging
- Microscopy: Image the stained, whole-mount embryos using a laser-scanning confocal microscope. Use objectives with high numerical aperture (NA) for optimal resolution (e.g., 40x oil objective, NA=1.3) [28].
- Z-Stack Acquisition: Capture image Z-stacks with a pinhole set to 1 Airy Unit to ensure optimal optical section thickness. This step is fundamental for generating high-quality 3D volumetric data for subsequent reconstruction and quantification of the cardiac crescent [26] [28].
Workflow Visualization: From Sample to 3D Reconstruction
The following diagram illustrates the integrated experimental and computational pipeline for whole-mount imaging, highlighting the steps that preserve 3D architecture.
Research Reagent Solutions for Whole-Mount Imaging
Successful implementation of whole-mount imaging relies on a specific set of reagents and tools. The table below details essential materials and their functions, with a focus on cardiac crescent analysis.
Table 2: Essential Research Reagents for Whole-Mount Immunofluorescence
| Reagent / Material | Function / Application | Specific Example / Note |
|---|---|---|
| Primary Antibodies | Label specific cardiac progenitor cell markers and reference proteins for spatial mapping and masking [26]. | Antibodies against Nkx2-5, Isl1; reference antibodies for delineating the cardiac crescent structure. |
| Fluorophore-Conjugated Secondaries | Enable multiplexed visualization of different progenitor populations within the same intact sample. | Use antibodies conjugated to distinct fluorophores (e.g., Alexa Fluor 488, 568, 647). |
| Permeabilization Agent | Creates pores in cell membranes to allow antibody penetration into the thick, intact tissue. | Triton X-100, typically used at 0.1-0.5% in buffer [28]. |
| Blocking Serum | Reduces non-specific antibody binding, lowering background signal and improving image quality. | Normal goat or donkey serum, used at 1-5% in conjunction with BSA [28]. |
| Mounting Medium | Immobilizes the sample for imaging. Optimal mediums can clear tissue to enhance imaging depth [29]. | 80% Glycerol (for clearing); ProLong Gold; or specialized optical gels. |
| Confocal Microscope | High-resolution 3D image acquisition; uses a pinhole to reject out-of-focus light [25]. | Equipped with high-NA oil objectives (40x, 63x) and multiple laser lines for multiplexing [28]. |
Whole-mount imaging is not merely an alternative technique but a fundamental methodology for research requiring accurate 3D spatial information, such as the analysis of cardiac progenitor populations in mouse embryos. Its capacity to preserve the intact three-dimensional architecture of delicate structures like the cardiac crescent allows for quantitative insights into morphogenetic events, cell organization, and lineage relationships that are otherwise lost or distorted with traditional sectioning methods [26] [27]. As imaging technologies and computational analysis continue to evolve, whole-mount imaging will remain a critical tool for elucidating the complex mechanisms that govern embryonic development and organogenesis.
A Step-by-Step Protocol: From Embryo Dissection to 3D Quantitative Analysis of the Cardiac Crescent
The stages of embryonic day 8.0 to 8.25 (E8.0-E8.25) in the mouse represent a critical developmental window encompassing late gastrulation and the initiation of early organogenesis. During this brief 6-hour period, the embryo undergoes rapid morphological transformations, including the formation of the cardiac crescent, the precursor to the heart. The precision in harvesting embryos at this stage is paramount for research focused on early heart development and the analysis of cardiac progenitor populations [26] [27]. The cardiac crescent, a key structure formed during heart development, contains the progenitor cells that will give rise to the future heart [30]. Contemporary studies leverage advanced single-cell genomic technologies to profile millions of cells across temporal and spatial dimensions, providing unprecedented resolution of developmental processes [31] [32]. These approaches rely fundamentally on the accurate morphological staging of embryos, as gestational age alone is an insufficient proxy for developmental progression due to natural stochastic variations [31]. This protocol details the methods for the precise harvesting, staging, and processing of mouse embryos at E8.0-E8.25, specifically framed within the context of whole-mount immunofluorescence analysis of the cardiac crescent.
Key Morphological Staging Criteria at E8.0-E8.25
At E8.0-E8.25, embryonic development is highly ordered and reproducible, making morphological criteria the gold standard for staging. The following table summarizes the key features used for precise staging during this period.
Table 1: Morphological Staging Criteria for Mouse Embryos from E8.0 to E8.25
| Developmental Timepoint | Somite Number | Key Morphological Landmarks | Cardiac Crescent Development |
|---|---|---|---|
| E8.0 (~0-2 somites) | 0 - 2 pairs | Initiation of somitogenesis; emergence of head folds; presence of a defined primitive streak [31]. | Cardiac progenitor cells begin to coalesce at the myocardial plate [30]. |
| E8.25 (~3-6 somites) | 3 - 6 pairs | Progressive formation of somites; advancing head fold development; early neural plate/fold formation [31]. | Progenitor populations form the distinct crescent-shaped structure at the anterior lateral plate [26] [27]. |
The transition through these stages occurs over a period of just 2-6 hours, underscoring the need for meticulous examination [31]. The following diagram illustrates the logical relationship between developmental timing, morphological checkpoints, and the subsequent analytical workflow.
Protocol: Embryo Harvesting and Staging
Materials and Reagents
Table 2: Research Reagent Solutions for Embryo Harvesting and Staging
| Item | Function/Application | Specifications/Alternatives |
|---|---|---|
| Timed-pregnant mice | Source of embryos. Noon of vaginal plug discovery is designated E0.5 [33]. | C57BL/6J is commonly used; ensure IACUC-approved protocols are followed. |
| Ice-cold Phosphate-Buffered Saline (PBS) | Washing and temporary storage of dissected embryos. Preserves tissue integrity [33]. | Must be calcium- and magnesium-free to prevent premature tissue adhesion. |
| Sharp surgical scissors & fine forceps | Dissection of uterine horn and embryonic tissues [33]. | Dumont #5 forceps are ideal for fine manipulation of embryonic tissues. |
| Dissecting microscope with fiber optic illuminator | Visualization of embryos for accurate dissection and staging [26] [33]. | A magnification range of 0.63x to 18.9x is suitable [33]. |
| Transfer pipettes | Gentle handling and transfer of embryos between solutions [33]. | Flame-polish tips to prevent damaging the embryonic tissues. |
Step-by-Step Harvesting and Staging Procedure
Embryo Collection:
- Euthanize the timed-pregnant dam at the desired gestational window (E8.0-E8.25) using a method approved by your institutional animal care and use committee (e.g., CO₂ inhalation followed by cervical dislocation) [33].
- Open the abdominal cavity to locate and dissect the entire uterine horn. Place the uterus in a Petri dish containing ice-cold PBS.
- Under a dissecting microscope, carefully separate the individual amniotic sacs from the uterine horn using sharp surgical scissors and fine forceps.
- Gently open each amniotic sac and expose the embryo by cutting the umbilical cord. Transfer each embryo to a separate well of a multi-well plate filled with ice-cold PBS using a transfer pipette [33].
Morphological Staging:
- Under the dissecting microscope, meticulously trim away extra-embryonic tissues without damaging the embryo itself.
- Identify and count the number of somite pairs. This is the most precise and reliable criterion for staging embryos within the E8.0-E8.25 window [31].
- Confirm the developmental stage by examining complementary landmarks: the development of head folds and the presence of a cardiac crescent at the anterior lateral plate [31] [26].
- Embryos matching the desired somite count and morphological criteria can now be processed for downstream applications. A small tissue sample (e.g., the embryonic head) should be collected for genotyping, if required [33].
Protocol: Whole-Mount Immunofluorescence for Cardiac Crescent
Workflow for 3D Analysis
This section adapts a published whole-mount immunofluorescence approach for the specific analysis of cardiac progenitor populations within the cardiac crescent [26] [27]. The following diagram outlines the core workflow from fixed embryo to quantitative 3D analysis.
Detailed Methodology
Fixation and Permeabilization: Fix the staged embryos in 4% paraformaldehyde (PFA) for 2-4 hours at 4°C. Following PBS washes, permeabilize the tissue by incubating in a solution containing 0.5% Triton X-100 for several hours to allow antibody penetration [26].
Antibody Staining:
- Blocking: Incubate embryos in a blocking solution (e.g., 5% normal serum, 1% bovine serum albumin (BSA), 0.1% Triton X-100 in PBS) for several hours or overnight at 4°C to reduce non-specific binding.
- Primary Antibodies: Prepare a cocktail of primary antibodies in blocking solution. For cardiac progenitors, this may include antibodies against transcription factors like Nkx2-5 or Isl1 [33]. Critically, include reference antibodies that mark the entire cardiac crescent structure (e.g., Phalloidin for F-actin) to enable subsequent masking and quantification [26] [27].
- Washing and Secondary Antibodies: After incubation for 2-3 days at 4°C, wash the embryos extensively. Then incubate with fluorophore-conjugated secondary antibodies and, optionally, DAPI for nuclear staining, for 1-2 days at 4°C [26].
Imaging and Quantitative Analysis:
- Confocal Microscopy: Mount the stained embryos and image using a confocal microscope. Acquire Z-stacks through the entire cardiac crescent region to generate 3D volumetric data [26] [27].
- Image Processing: Use image analysis software (e.g., Imaris, Fiji/ImageJ) to create a 3D reconstruction of the cardiac crescent.
- Quantitative Measurement: Leveraging the reference stain, create a mask of the entire cardiac crescent. Subsequently, apply this mask to quantify the area, volume, and fluorescence intensity of specific progenitor populations (e.g., Nkx2-5+ cells) within the defined structure [26] [27]. This allows for both cell- and tissue-level information to be obtained.
Integration with Advanced Analytical Techniques
The precisely staged embryos harvested using this protocol are perfectly suited for integration with cutting-edge spatial and genomic techniques. Recent studies have profiled serial sections from E7.5-E8.0 embryos to generate full spatiotemporal transcriptome maps at single-cell resolution, reconstructing so-called "digital embryos" [34]. Furthermore, computational frameworks like multi-omics single-cell optimal transport (moscot) can be applied to reconstruct developmental trajectories and map cells across both temporal and spatial dimensions, providing deep insight into the dynamics of cell fate acquisition during this critical window [32] [35]. The staging precision outlined here is the critical first step that ensures the validity and power of these advanced downstream analyses.
Fixation and Permeabilization Strategies for Maximum Antibody Penetration
Whole mount immunofluorescence of cardiac crescent stage embryos presents unique technical challenges for developmental biologists. At embryonic day (E) 8.25 in mouse development, the cardiac crescent represents a critical morphological stage in heart development where progenitor cell populations, including the First and Second Heart Fields, are established and can be distinguished by unique molecular markers [6]. The three-dimensional architecture of these embryos necessitates optimized fixation and permeabilization strategies to ensure complete antibody penetration while preserving delicate tissue morphology and antigen integrity. The theoretical immunostaining route is frequently hampered by roadblocks including masked epitopes, poor antibody penetration, background signal, and protein relocalization [36]. This application note provides detailed methodologies and strategic frameworks to overcome these challenges, enabling precise spatial reconstruction of progenitor populations within the developing cardiac crescent.
Strategic Comparison of Fixation and Permeabilization Methods
Fixation Agents: Balancing Preservation and Accessibility
Fixation preserves cellular morphology and integrity by preventing proteolytic degradation and maintaining the native architecture of tissues. The choice of fixative is critical as it directly impacts epitope preservation and antibody accessibility [37].
Table 1: Comparison of Common Fixation Agents for Cardiac Crescent Embryos
| Fixative Type | Mechanism of Action | Concentration & Incubation | Major Advantages | Major Disadvantages |
|---|---|---|---|---|
| Paraformaldehyde (PFA) | Cross-links proteins via amine groups, creating molecular bridges [37] [38] | 4% in PBS for 1 hour at RT or O/N at 4°C [6] | Ideal for preserving morphology; universal fixative; recommended for membrane proteins [37] | Excessive cross-linking may mask epitopes and reduce signal [36] [37] |
| Methanol | Precipitates cellular proteins through dehydration [37] [38] | 100% ice-cold for 10 minutes [39] [37] | Serves as both fixative and permeabilizer; good for phosphorylated and nuclear antigens [39] | Can denature protein-based fluorophores; may damage cell membranes and microtubules [39] [37] |
| Acetone | Precipitates proteins through dehydration [37] | 100% for 10 minutes [37] | Milder than methanol; suitable for alcohol-sensitive epitopes [37] | Highly volatile; not suitable for over-expressed fluorescent proteins [37] |
For cardiac crescent stage embryos, 4% PFA fixation is widely employed. The standard protocol involves fixing dissected embryos with 4% paraformaldehyde (PFA) in PBS for 1 hour at room temperature, which can be extended to overnight at 4°C [6]. Crosslinking fixatives like PFA are often preferable for studying intracellular signaling and post-translational modifications such as phosphorylation, as they preserve these modifications better than alcohol-based fixatives [39].
Permeabilization Agents: Enabling Intracellular Access
Permeabilization disrupts cellular membranes to allow antibodies access to intracellular targets. The selection of permeabilization agent should be guided by the subcellular localization of the target antigen and the compatibility with specific antibodies [38].
Table 2: Comparison of Permeabilization Strategies for Embryonic Tissues
| Permeabilization Agent | Mechanism of Action | Concentration & Incubation | Target Compatibility | Considerations for Cardiac Crescent Embryos |
|---|---|---|---|---|
| Triton X-100 | Non-ionic detergent that non-selectively solubilizes lipid bilayers [37] [38] | 0.1-0.3% in PBS for 10 minutes at RT [39] | Most intracellular targets; use after PFA fixation [39] | Strong permeabilization; may be harsh for delicate embryonic tissues [37] |
| Saponin | Mild detergent that selectively permeabilizes membranes based on cholesterol content [37] [38] | 0.1-0.5% in PBS for 10 minutes at RT; must be included in all subsequent buffers [39] | Cytosolic targets; not ideal for nuclear stains [39] | Reversible action; preserves native epitope structure; recommended for whole mount immunofluorescence [6] [39] |
| Methanol | Precipitates lipids and proteins, disrupting membranes [39] [38] | 90% ice-cold for 15 minutes on ice [39] | Nuclear and organelle targets; good for phospho-markers [39] | Denatures protein-based fluorophores (e.g., PE, APC); can be used as standalone fixative/permeabilizer [39] |
For whole mount immunofluorescence of cardiac crescent embryos, saponin is particularly valuable. The protocol typically involves using blocking buffer containing 0.5% saponin and 1% bovine serum albumin (BSA) in PBS, with incubation for at least 4 hours at room temperature or overnight at 4°C [6]. The reversible nature of saponin permeabilization necessitates its inclusion in all subsequent wash and antibody incubation buffers to maintain intracellular access [39].
Integrated Protocols for Cardiac Crescent Stage Embryos
Comprehensive Whole Mount Immunofluorescence Workflow
The following diagram illustrates the complete experimental workflow for processing cardiac crescent stage embryos:
Workflow for Whole Mount Immunofluorescence
Detailed Step-by-Step Protocol
Embryo Harvest and Dissection:
- Sacrifice pregnant dam at E8.25 (approximately 8th day post-conception) and extract uterine horn [6].
- Carefully remove uterine and decidual tissues to expose embryos using fine forceps (#5) under a dissection microscope [6].
- Dissect away extraembryonic tissues without damaging embryonic morphology [6].
Fixation:
Blocking and Permeabilization:
Antibody Incubations:
- Incubate with primary antibody mixture diluted in blocking buffer overnight at 4°C [6].
- Recommended reference antibodies for cardiac crescent: Nkx2-5 for cardiac crescent demarcation [6].
- Wash 3 times for 1 hour each with 0.1% Triton X-100 in PBS [6].
- Incubate with secondary antibody mixture diluted in blocking buffer for 3 hours at room temperature or overnight at 4°C [6].
Counterstaining and Mounting:
- Counterstain with DAPI (4',6-diamidino-2-phenylindole) in PBS for 10 minutes [6].
- Wash twice for 5 minutes each with 0.1% Triton X-100 in PBS [6].
- Slowly suspend embryos in anti-fade mounting media (2% w/v n-Propyl gallate, 90% glycerol, 1× PBS) and allow to equilibrate for at least 1 hour before mounting [6].
Fixation and Permeabilization Decision Framework
The selection of optimal fixation and permeabilization strategies depends on multiple experimental factors, as illustrated in the following decision diagram:
Fixation and Permeabilization Decision Guide
The Scientist's Toolkit: Essential Reagents for Cardiac Crescent Immunolabeling
Table 3: Essential Research Reagents for Whole Mount Cardiac Crescent Immunolabeling
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Fixatives | 4% Paraformaldehyde (PFA) in PBS [6] | Preserves tissue architecture through protein cross-linking; standard for cardiac crescent embryos |
| Permeabilization Agents | Saponin (0.1-0.5%) [6] [39], Triton X-100 (0.1-0.3%) [39] | Enables antibody access to intracellular targets; saponin preferred for delicate embryonic tissues |
| Blocking Agents | Bovine Serum Albumin (BSA, 1%) [6] | Reduces non-specific antibody binding; typically combined with permeabilization agents |
| Primary Antibodies | Nkx2-5 (cardiac crescent reference) [6], Foxa2Cre:YFP (progenitor populations) [6] | Identify specific cardiac progenitor populations; reference antibodies crucial for spatial orientation |
| Secondary Antibodies | Fluorochrome-conjugated species-specific antibodies [6] | Amplify signal through indirect detection; compatible with chosen fixation method |
| Counterstains | DAPI (nuclear stain) [6] | Provides structural context by labeling all nuclei |
| Mounting Media | Anti-fade media (n-Propyl gallate in glycerol/PBS) [6] | Preserves fluorescence during storage and imaging |
Troubleshooting and Optimization Strategies
Addressing Common Challenges in Embryonic Immunolabeling
- Low Signal Intensity: Extend permeabilization time or increase saponin concentration to 0.5%; validate antibody compatibility with PFA fixation [36] [39].
- High Background Staining: Increase BSA concentration to 2-5% in blocking buffer; include additional washes with 0.1% Triton X-100; consider using quenching reagents like copper sulfate or Sudan black B [36].
- Poor Antibody Penetration: For thicker tissues, extend permeabilization incubation times; consider combination approaches with mild detergents; ensure adequate tissue clearing [36] [40].
- Epitope Masking: For formaldehyde-sensitive epitopes, try methanol or acetone fixation; optimize fixation duration to balance preservation versus accessibility [37] [38].
- Morphological Damage: Always handle embryos gently with transfer pipettes; ensure fixative is fresh and properly prepared; avoid excessive vortexing during processing steps [6].
Sequential Staining for Complex Antigen Detection
When detecting both extracellular and intracellular targets, sequential staining often yields superior results:
- First, stain live cells with cell-surface marker antibodies validated for use on unfixed cells [39].
- Then fix with 4% PFA and permeabilize with saponin (not methanol, which denatures protein-based fluorophores) [39].
- Finally, stain intracellular targets with validated antibodies [39]. Always verify antibody compatibility with chosen fixation and permeabilization methods through pilot experiments [39].
Optimized fixation and permeabilization strategies are fundamental to successful whole mount immunofluorescence of cardiac crescent stage embryos. The 4% PFA fixation followed by saponin permeabilization provides an excellent balance between morphological preservation and antibody accessibility for most applications in early heart development research. By implementing the detailed protocols and strategic frameworks presented in this application note, researchers can achieve maximum antibody penetration while maintaining tissue integrity, enabling precise quantitative analysis of progenitor cell populations during this critical phase of cardiac morphogenesis.
The precise identification and isolation of cardiac progenitor cells (CPCs) is a cornerstone of cardiovascular developmental biology and regenerative medicine. The design of a specific antibody panel is critical for the reliable characterization of these transient cell populations, particularly in complex three-dimensional structures like the cardiac crescent stage embryo. The cardiac crescent, a key structure in early heart development, contains multipotent progenitor cells that give rise to the major lineages of the mature heart. This application note provides a detailed framework for the construction of an antibody panel for the identification of cardiac progenitors, with specific methodologies optimized for whole-mount immunofluorescence analysis of mouse embryos. The protocols and reagents described herein are designed to be integrated within a broader thesis research project, enabling the spatial quantification of progenitor populations during this critical developmental window. A major advancement in the field is the discovery that certain glycosylated residues on known proteins serve as highly specific markers for progenitor populations, a fact that must be considered during antibody selection [41].
Marker Selection for Antibody Panel Design
The selection of markers should strategically target cell surface and intracellular antigens that define the cardinal properties of progenitor cells, including multipotency, proliferation, and early lineage commitment. The panel should enable the distinction of cardiac progenitors from surrounding mesoderm and other cell types within the embryo.
Reference Marker Categories
Table 1: Core Marker Panel for Cardiac Progenitor Characterization
| Marker | Type/Location | Expression in Cardiac Progenitors | Function | Application Notes for Whole-Mount IF |
|---|---|---|---|---|
| Transcription Factors | ||||
| Nkx2.5 | Nuclear | Early cardiac mesoderm, marks first heart-forming cells [42] | Key transcription factor for heart tube formation and cardiomyocyte differentiation | Requires high-quality antigen retrieval and permeabilization. |
| SOX2 | Nuclear | Pluripotency-associated factor in progenitor cells [43] | Maintains progenitor state in multipotent cells | Useful for identifying less-committed populations. |
| Cell Surface & Cytoplasmic Proteins | ||||
| PECAM1 (CD31) | Cell Surface (Glycosylated) | Endothelial and hematopoietic lineages; specific glycosylated forms mark progenitors [41] | Cell adhesion, migration; glycosylated forms are key | C1096 mAb recognizes a glycosylated epitope on PECAM1 [41]. |
| GRP78 | Cell Surface (Glycosylated) | Stress response chaperone; specific glycosylated forms mark progenitors [41] | Protein folding and processing; cell surface form is a marker | C19 mAb recognizes a glycosylated epitope on GRP78 [41]. |
| Flk1 (KDR) | Cell Surface | Multipotent cardiovascular progenitor cells [42] | Receptor for VEGF, crucial for cardiovascular development | Requires specific growth factor cocktails during differentiation for robust detection. |
| Structural Proteins | ||||
| Nestin | Cytoplasmic (Intermediate Filament) | Neural progenitors; also expressed in some cardiac progenitors [43] | Cytoskeletal protein associated with immature, dividing cells | A good marker of a progenitor state, though not entirely cardiac-specific. |
| Vimentin | Cytoplasmic (Intermediate Filament) | Mesenchymal cells, including early cardiac mesoderm [43] | Maintains cell shape and cytoskeletal integrity | A broad mesodermal marker useful for outlining the cardiac crescent structure. |
Experimental and Emerging Markers
Table 2: Quantitative Data and Validation for Selected Markers
| Marker | Typical Assay | Detection Timing in Mouse Embryos (≈) | Key Validation Data | Significance in Cardiac Crescent |
|---|---|---|---|---|
| Nkx2.5 | IF, FACS (with GFP reporter) | Earliest GFP+ at E7.5-8.0 (Day 5-6 in vitro) [42] | Gives rise to cardiomyocytes and smooth muscle in vivo/in vitro [42] | Demarcates the primary heart field within the cardiac crescent. |
| PECAM1 (C1096 mAb) | IF, FACS | Fetal and adult human heart [41] | Recognizes multipotent progenitor population; binding abolished by de-N-glycosylation [41] | Labels a progenitor subpopulation; glycosylation state is critical. |
| Flk1 | FACS | Depends on differentiation protocol (e.g., with BMP4) [42] | Isolates multipotent cardiovascular progenitors (cardiomyocytes, endothelial, vascular SMC) [42] | Marks a population with broader developmental potential. |
The data in Table 2 underscores the importance of validating antibodies not just for the target protein, but for specific post-translational modifications. The finding that mAb C1096 and C19 binding is "significantly abolished" by de-N-glycosylation highlights that an antibody's effectiveness can depend on the specific glycosylation state of its epitope, which may be unique to progenitor cells [41]. Furthermore, the use of transgenic reporters, such as Nkx2.5-eGFP, provides a powerful tool for isolating live progenitor cells for downstream functional characterization [42].
Whole-Mount Immunofluorescence Protocol for Cardiac Crescent Stage Embryos
This protocol is adapted from established methods for the whole-mount immunofluorescence analysis of cardiac progenitor populations in mouse embryos, allowing for 3D spatial reconstruction and quantification [26].
Materials and Reagents
The Scientist's Toolkit: Essential Research Reagents
| Item | Function/Description | Example/Note |
|---|---|---|
| Primary Antibodies | Antigen-specific immunoglobulins that bind to target markers. | See Table 1 for specificities. Use antibodies validated for IF on embryonic tissue. |
| Fluorophore-conjugated Secondary Antibodies | Bind to primary antibodies to provide a detectable signal. | Use highly cross-adsorbed antibodies to minimize non-specific binding. |
| Permeabilization Solution | Creates pores in cell membranes to allow antibody entry. | 0.1% Triton X-100 in PBS is standard [43]. |
| Blocking Solution | Reduces non-specific antibody binding to tissue. | 1% BSA / 10% normal goat serum / 0.3M glycine in 0.1% PBS-Tween [43]. |
| Fixative | Preserves tissue architecture and antigenicity. | 4% Paraformaldehyde (PFA) in PBS [43]. |
| Mounting Medium with DAPI | Preserves fluorescence and stains nuclei for reference. | Essential for defining cellular context within the whole-mount. |
| Reference Antibodies | Antibodies against known structural components. | Used for successive masking of the cardiac crescent for quantitative analysis [26]. |
Step-by-Step Procedural Workflow
Day 1: Embryo Dissection and Fixation
- Dissect mouse embryos at the cardiac crescent stage (e.g., E7.5-E8.0) in cold PBS.
- Immediately transfer embryos to ice-cold 4% PFA. Fix for 2-4 hours at 4°C on a rocking platform. Critical: Avoid over-fixation to prevent epitope masking.
- Wash embryos 3 x 15 minutes in PBS at 4°C to remove all traces of PFA.
Day 2: Permeabilization and Blocking
- Permeabilize embryos by incubating in 0.1% Triton X-100 in PBS (PBT) for 1-2 hours at room temperature on a rocker.
- Prepare blocking solution (1% BSA, 10% normal serum, 0.3M glycine in PBT).
- Incubate embryos in blocking solution for a minimum of 4 hours or overnight at 4°C to block non-specific sites.
Day 3: Primary Antibody Incubation
- Prepare primary antibodies diluted in fresh blocking solution.
- Incubate embryos in the primary antibody solution for 48-72 hours at 4°C under constant gentle agitation. Note: Extended incubation times are often necessary for adequate antibody penetration in whole-mount specimens.
Day 5-6: Secondary Antibody Incubation and Mounting
- Wash embryos extensively with PBT over 8-12 hours (e.g., 6-8 changes of wash buffer) to remove unbound primary antibody.
- Prepare fluorophore-conjugated secondary antibodies diluted in blocking solution. Critical: From this step onward, protect samples from light to prevent fluorophore photobleaching.
- Incubate embryos in secondary antibody solution for 24-48 hours at 4°C.
- Perform a final series of washes with PBT over 8-12 hours.
- Counterstain nuclei with DAPI (if not included in the mountant) by incubating for 1 hour.
- Wash briefly in PBS and mount embryos in a suitable anti-fade mounting medium on a depression slide or using spacers to prevent crushing.
Day 7: Imaging and Analysis
- Image the stained embryos using confocal microscopy, acquiring Z-stacks that encompass the entire cardiac crescent structure.
- Use image processing software for 3D reconstruction and quantitative measurements of the progenitor populations, guided by reference antibodies to define the region of interest [26].
Experimental Workflow and Data Analysis Visualization
The following diagram outlines the complete experimental pipeline from embryo preparation to quantitative analysis, as described in the protocol.
Critical Considerations for Panel Design and Validation
- Multiplexing and Controls: When designing a multiplex panel, verify the compatibility of primary antibodies from different host species and select secondary antibodies with minimal cross-reactivity. Include controls essential for whole-mount immunofluorescence: no-primary antibody controls for autofluorescence and secondary antibody specificity, and biological controls using known positive and negative tissue sections.
- Spatial Quantification: The power of this whole-mount approach lies in its ability to provide three-dimensional spatial data on progenitor localization. Using reference markers to mask the cardiac crescent allows for quantitative measurements of the area, density, and positional relationships of different progenitor populations, moving beyond simple detection to meaningful morphogenetic analysis [26].
- Integration with Live Cell Isolation: The markers identified via immunofluorescence can be translated into protocols for the isolation of live cardiac progenitors. For instance, the Nkx2.5-eGFP reporter system enables the derivation and fluorescence-activated cell sorting (FACS) of cardiac progenitors from differentiated pluripotent stem cells using the hanging-droplet method, providing a source of cells for functional experimentation [42].
Mounting and Orientation Techniques for Optimal Volumetric Imaging
Whole-mount immunofluorescence (WMIF) represents a powerful technique for the three-dimensional analysis of embryonic development, preserving spatial relationships that are critical for understanding organogenesis. This application note details a optimized protocol for mounting and orienting cardiac crescent stage mouse embryos (approximately E8.25) to facilitate high-resolution volumetric imaging and subsequent quantitative analysis [6]. The cardiac crescent, a key structure in early heart development, contains progenitor populations that will form the future heart, and understanding their 3D organization provides crucial insights into normal and abnormal cardiogenesis [6] [44]. Proper mounting and orientation are critical technical steps that directly impact image quality, resolution, and the accuracy of 3D reconstructions.
Key Principles of Volumetric Imaging for Whole-Mount Embryos
Successful volumetric imaging of whole-mount specimens depends on several interconnected principles. Specimen clarity must be achieved through methods that minimize light scattering; while this protocol uses refractive index matching with mounting media, advanced optical clearing techniques like LIMPID can further enhance transparency for thicker samples [45]. Optimal orientation requires stabilizing the embryo to position the region of interest (e.g., cardiac crescent) perpendicular to the imaging axis while considering the working distance of the objective lens [6]. Photostability is maintained using anti-fade agents such as n-propyl gallate to preserve fluorescence signal throughout extended imaging sessions [6]. Finally, refractive index homogeneity throughout the light path—from objective lens through mounting medium to specimen—is essential for minimizing spherical aberration and maintaining resolution at depth [45].
Materials and Reagents
Research Reagent Solutions
Table: Essential Reagents for Whole-Mount Immunofluorescence and Imaging
| Reagent | Function | Application Notes |
|---|---|---|
| Anti-fade Mounting Medium (2% n-propyl gallate, 90% glycerol, 1× PBS) | Prevents photobleaching during imaging | Equilibrate embryos for ≥1 hour; provides refractive index ~1.45 [6] |
| Phosphate Buffered Saline (PBS) | Washing and buffer base | Maintains physiological pH and osmolarity [6] |
| Blocking Buffer (0.5% saponin, 1% BSA in PBS) | Reduces non-specific antibody binding | Can be extended to 3% BSA with 5% donkey serum for challenging antibodies [6] [46] |
| 4% Paraformaldehyde (PFA) | Tissue fixation | Preserves tissue architecture and antigenicity; fix for 1h at RT or overnight at 4°C [6] [47] |
| Primary Antibodies (e.g., Nkx2-5) | Reference structure labeling | Enables downstream image segmentation; cardiac crescent marker [6] |
| Secondary Antibodies (Fluorophore-conjugated) | Target detection | Allows multiplexing; choose fluorophores with minimal spectral overlap [6] |
| 4',6-diamidino-2-phenylindole (DAPI) | Nuclear counterstain | Provides structural context; use concurrently with secondary antibodies [6] |
| LIMPID Clearing Solution | Refractive index matching | Aqueous-based clearing; compatible with FISH and IHC; enhances imaging depth [45] |
Protocol: Mounting and Orientation for Cardiac Crescent Stage Embryos
Specimen Preparation Timeline
Table: Experimental Workflow and Timing
| Stage | Duration | Critical Parameters |
|---|---|---|
| Embryo Harvesting (E8.25) | 1-2 hours | Strain-dependent timing; minimize damage during deciduum removal [6] |
| Fixation (4% PFA) | 1 hour at RT or O/N at 4°C | Optimal cross-linking preserves structure and antigenicity [6] [47] |
| Immunofluorescence | 2-3 days | Permeabilization with 0.1% Triton X-100; antibody concentrations require empirical determination [6] |
| Equilibration in Mounting Medium | ≥1 hour | Gentle flicking periodically helps embryos settle [6] |
| Mounting and Orientation | 30-45 minutes | Critical step for optimal imaging plane [6] |
| Volumetric Imaging | Variable | Dependent on embryo size and resolution requirements [6] |
Mounting Procedure
The following protocol describes the mounting of immunofluorescently stained cardiac crescent stage embryos for optimal volumetric imaging [6]:
Slide Preparation: Create parallel supports on a microscope slide using either:
- Double-stick tape stacks (5-6 layers high, 15-20mm apart)
- Silicone spacers of equivalent height
Medium Application: Place a 15μL drop of anti-fade mounting medium between the supports.
Embryo Transfer: Carefully transfer one embryo to the mounting medium using a transfer pipette. For multiple embryos, ensure sufficient spacing to avoid interference during orientation and imaging.
Orientation: Using fine forceps or a hair loop, manipulate the embryo to position the cardiac crescent (identified by its anterior position and Nkx2-5 staining) perpendicular to the intended imaging axis. The cardiac crescent appears as a horseshoe-shaped structure at the anterior region of the embryo.
Coverslip Placement: Gently lower a coverslip onto the supports, allowing the mounting medium to spread evenly without creating bubbles. Avoid excessive pressure that may compress the embryo.
Sealing: Seal the coverslip edges with clear nail polish or commercial sealant to prevent medium evaporation and specimen movement during imaging.
Orientation Strategies for Cardiac Crescent Visualization
Proper orientation of the cardiac crescent stage embryo is essential for comprehensive analysis of progenitor cell populations. The following approaches facilitate optimal imaging:
Dorsal View Orientation: Position the embryo with the dorsal surface facing the coverslip to visualize the cardiac crescent in the anterior region as a continuous horseshoe-shaped structure [6] [44].
Lateral View Orientation: Rotate the embryo 90 degrees to analyze the anterior-posterior distribution of progenitor populations within the crescent.
Reference Antibody Guidance: Utilize Nkx2-5 immunostaining as a reference marker to identify the cardiac crescent boundaries during orientation [6].
Multi-position Imaging: For complete analysis, consider imaging the same embryo from multiple orientations, though remounting may be necessary.
Imaging Parameters for Volumetric Reconstruction
Table: Confocal Microscopy Parameters for Cardiac Crescent Imaging
| Parameter | Recommended Setting | Rationale |
|---|---|---|
| Objective Lens | 20× (NA ≥0.8) or 40× (NA ≥1.2) water immersion | Balance between resolution and working distance [6] |
| Z-step Size | 0.5-2.0 μm | Nyquist sampling for 3D reconstruction; adjust based on objective NA [6] |
| Image Format | 1024 × 1024 pixels | Adequate sampling without excessive acquisition time [6] |
| Pinhole Size | 1 Airy unit | Optimal sectioning with sufficient signal [6] |
| Laser Power | Minimal to avoid photobleaching | Use signal amplification if needed [6] [45] |
| Digital Zoom | 1.0-2.0× | Balance field of view and resolution [6] |
Advanced Techniques: Integration with Optical Clearing
For enhanced imaging depth, particularly with larger embryos or dense tissues, consider integrating optical clearing methods:
LIMPID Technique: An aqueous-based clearing method that preserves lipids and fluorescent signals while significantly improving tissue transparency [45]. LIMPID uses saline-sodium citrate, urea, and iohexol to match refractive indices.
Compatibility: The LIMPID approach is compatible with both immunofluorescence and fluorescence in situ hybridization (FISH), enabling multimodal imaging [45].
Implementation: Post-immunostaining, equilibrate embryos in LIMPID solution (refractive index ~1.46) for 24-48 hours before mounting in the same solution for imaging [45].
Troubleshooting Common Challenges
Table: Troubleshooting Mounting and Imaging Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor penetration of antibodies | Inadequate permeabilization | Increase Triton X-100 concentration to 0.3-0.5% or extend permeabilization time [6] [47] |
| High background fluorescence | Insufficient blocking | Increase BSA to 3% and add 5% serum from secondary antibody host [46] |
| Specimen movement during imaging | Incomplete sealing of coverslip | Ensure complete seal with nail polish; allow to fully dry before imaging [6] |
| Weak signal | Antibody concentration too low | Perform antibody titration; extend primary incubation to 48-72 hours [6] [47] |
| Non-specific staining | Cross-reactivity | Include species-appropriate controls; validate antibodies in knockout tissue if available [47] |
Applications in Cardiac Development Research
The mounting and orientation techniques described herein enable sophisticated analysis of cardiac progenitor populations during the critical period of heart development. When properly implemented, this approach facilitates:
Quantitative 3D Analysis: Precisely measure the volume, position, and organization of progenitor populations within the cardiac crescent [6].
Fate Mapping Studies: Track progenitor cell distributions in genetic lineage tracing experiments [44].
Phenotypic Characterization: Analyze structural defects in mutant embryos with cell-level resolution [6] [44].
Multimodal Integration: Correlate protein expression (via immunofluorescence) with gene expression patterns (via FISH) in the same specimen [45].
These applications provide powerful insights into the fundamental processes governing heart development and the origins of congenital heart defects.
In the study of early heart development, particularly during the formation of the cardiac crescent in mouse embryos, three-dimensional (3D) reconstruction via confocal microscopy is indispensable. This stage, crucial for the analysis of progenitor cell populations like the first and second heart fields, presents significant challenges for high-quality imaging due to the embryo's small size and complex 3D architecture [26] [8]. Obtaining quantifiable, high-resolution data requires meticulous configuration of the microscope to ensure that all optical information is captured without aliasing or loss of detail [48]. This application note details the essential acquisition parameters, with a focus on the Nyquist-Shannon sampling theorem, to guide researchers in configuring a confocal microscope for optimal 3D reconstruction of whole-mount immunofluorescence samples in cardiac development research.
Theoretical Foundation: Nyquist-Shannon Sampling in Microscopy
The Nyquist-Shannon sampling theorem states that to perfectly reconstruct a signal, the sampling frequency must be greater than twice the highest frequency contained in that signal [48]. In microscopy, this translates to a requirement for the digital sampling distance (pixel size in x-y, z-step in z) to be small enough to capture the finest details the optics can resolve.
- Undersampling: When the sampling distance is larger than the Nyquist distance, information is permanently lost, and aliasing artifacts (e.g., jagged edges or moiré patterns) can appear in the image, severely compromising 3D reconstruction [48].
- Oversampling: Sampling at intervals smaller than the Nyquist distance captures all information. While this increases data size and acquisition time, it is harmless and can sometimes benefit subsequent image restoration processes like deconvolution [48] [49].
The system's Bandwidth is determined by the Point Spread Function (PSF), and the ideal sampling rate is defined to capture this full bandwidth. The Nyquist rate in cycles per unit distance is calculated as F_Nyquist = 1 / (2 * Δ), where Δ is the critical sampling distance [48].
Determining Critical Sampling Distances
The ideal sampling density is not arbitrary but is derived from the optical properties of the microscope. The following equations and subsequent tables provide the foundation for calculating these critical parameters.
Fundamental Equations
The calculations depend on the microscope type (widefield, confocal, or multi-photon), the numerical aperture (NA) of the objective, the emission or excitation wavelength (λ), and the refractive index (n) of the immersion medium. The half-aperture angle (α) is calculated as α = arcsin(NA / n) [48].
Table 1: Nyquist Critical Sampling Distance Equations for Different Microscopy Modalities
| Microscopy Modality | Lateral Sampling Distance (Δx) | Axial Sampling Distance (Δz) | Key Wavelength Consideration |
|---|---|---|---|
| Widefield | ( \Deltax = \frac{\lambda{em}}{4 n \sin(\alpha)} ) | ( \Deltaz = \frac{\lambda{em}}{ 2 n (1-\cos(\alpha))} ) | Uses emission wavelength (λem). |
| Confocal | ( \Deltax = \frac{\lambda{ex}}{8 n \sin(\alpha)} ) | ( \Deltaz = \frac{\lambda{ex}}{4 n (1-\cos(\alpha))} ) | Uses excitation wavelength (λex). |
| Multi-photon (k-photon) | ( \Deltax = \frac{\lambda{ex}}{4 k n \sin(\alpha)} ) | ( \Deltaz = \frac{\lambda{ex}}{2 k n (1-\cos(\alpha))} ) | Uses excitation wavelength (λex) divided by photon count (k). |
For a confocal microscope, the sampling distances are half those of a widefield microscope because the effective system bandwidth is doubled [48]. In practice, with a typical confocal pinhole diameter of 1 Airy disk, the lateral critical sampling distance may be increased by up to 50% without significant information loss [48].
Practical Sampling Table for Cardiac Crescent Imaging
Based on the equations and the context of cardiac development (e.g., using common fluorophores like tdTomato and GFP) [33] [8], the following table provides calculated sampling parameters for a high-NA oil immersion objective, assuming a refractive index of 1.51 and an excitation wavelength of 488 nm for confocal (e.g., for GFP), 561 nm for confocal (e.g., for tdTomato), and 920 nm for two-photon (e.g., for GFP).
Table 2: Practical Nyquist Sampling Guide for Cardiac Crescent Imaging
| Objective & NA | Modality | Excitation λ (nm) | Lateral Δx (nm) | Axial Δz (nm) | Rationale & Application Note |
|---|---|---|---|---|---|
| 40x/1.3 Oil | Confocal | 488 | ~59 nm | ~236 nm | High lateral resolution for discerning individual progenitor cells in the crescent [48]. |
| 40x/1.3 Oil | Confocal | 561 | ~68 nm | ~271 nm | Suitable for tdTomato reporters (e.g., MLC-2v-tdTomato) in ventricular specification studies [33]. |
| 63x/1.4 Oil | Confocal | 488 | ~55 nm | ~219 nm | For maximum resolution of subcellular structures and precise cell boundary delineation [48] [49]. |
| 63x/1.4 Oil | Two-photon | 920 | ~82 nm | ~327 nm | Superior penetration for thicker whole-mount embryos; reduced photobleaching in live imaging [48] [8]. |
Experimental Protocol: 3D Confocal Acquisition of Cardiac Crescent Embryos
This protocol is adapted from established methods for whole-mount immunofluorescence and live imaging of mouse embryos at the cardiac crescent stage (approximately E7.5-E8.5) [26] [33] [8].
Sample Preparation and Mounting
- Mouse Embryo Dissection: Dissect mouse embryos at E7.5-E8.5 in ice-cold PBS. For fixed samples, perform whole-mount immunofluorescence using validated primary antibodies (e.g., against cTnnT) and Alexa Fluor-conjugated secondary antibodies [26] [8].
- Mounting: For fixed samples, mount embryos in a proprietary clearing agent or an anti-fading mounting medium. For live imaging, use embryos from reporter lines (e.g., Nkx2.5eGFP, MLC-2v-tdTomato) and mount in a glass-bottom dish with pre-warmed culture medium [33] [8].
- Orientation: Position the embryo to ensure the cardiac crescent/developing heart tube is unobstructed and facing the objective. Use a vacuum grease or agarose well to stabilize the embryo during imaging.
Microscope Setup and Image Acquisition
- Objective Selection: Choose a high-numerical aperture (NA > 1.2) oil-immersion objective. A 40x objective provides a good field of view, while a 63x objective offers higher resolution for cellular details.
- Define Imaging Volume: Use the microscope software to set the top and bottom limits of the z-stack, ensuring the entire volume of the cardiac crescent is included.
- Calculate and Set Sampling Parameters:
- Enter the optical parameters (NA, magnification, λex, λem, refractive index) into the microscope's "Optimal" or "Nyquist" function, if available.
- Alternatively, manually calculate the required pixel size and z-step using the formulas in Table 1 or values from Table 2 as a guide. Set these values in the acquisition software.
- Pixel Size: The software often derives this from the zoom factor and scan area. The "Optimal" button typically sets this to a value between 2-3 times smaller than the theoretical resolution [50].
- Z-step Size: Manually input the calculated axial sampling distance (Δz) from Table 2.
- Optimize Detection:
- Set the pinhole diameter to 1 Airy Unit (AU) for an optimal balance between optical sectioning and signal intensity [51].
- Adjust laser power and detector gain/high voltage to achieve a strong signal without saturation or excessive photobleaching. Use the histogram tool to ensure pixel intensities are within the dynamic range.
- Acquire Z-stack: Start the acquisition of the 3D z-stack. For live imaging, set the appropriate time intervals to capture morphogenetic movements [8].
Post-Acquisition and 3D Reconstruction
- Data Verification: Check the acquired stack for signs of undersampling (aliasing) or excessive bleaching.
- Deconvolution: Apply deconvolution algorithms to reduce out-of-focus light and improve resolution and contrast. Densely sampled images (at or beyond Nyquist) yield the best deconvolution results [48] [49].
- 3D Reconstruction and Analysis: Use image analysis software (e.g., Imaris, FIJI/ImageJ) to create 3D renderings, segment specific progenitor populations (e.g., using reference antibodies for masking), and perform quantitative measurements of volume, position, and signal intensity within the cardiac crescent [26] [49].
Visual Guide to the Sampling Workflow
The following diagram illustrates the logical workflow and key decision points for applying Nyquist criteria to confocal microscopy setup.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Whole-Mount Imaging of Cardiac Crescent
| Item | Function / Application in Protocol | Example / Specification |
|---|---|---|
| Reporter Mouse Line | Genetically labels specific cardiac progenitor populations for live or fixed imaging. | MLC-2v-tdTomato (ventricular chamber) [33], Nkx2.5eGFP (differentiated cardiomyocytes) [8]. |
| Primary Antibodies | Immunofluorescence labeling of specific proteins in fixed whole-mount embryos. | Cardiac Troponin T (cTnnT) for differentiated cardiomyocytes [8]. |
| Secondary Antibodies | fluorescently-labeled detection of primary antibodies. | Alexa Fluor 488, 568, or 647 conjugates [26]. |
| Mounting Medium | Preserves fluorescence and allows optical clearing for deep imaging. | Proprietary anti-fade mounting media (e.g., Vectashield) or clearing agents [26]. |
| Glass-Bottom Dish | High-quality imaging substrate for high-NA objectives. | No. 1.5 thickness (0.16-0.19 mm) coverslip glass [49]. |
| Confocal Microscope | Instrument for optical sectioning and 3D data collection. | Laser Scanning Confocal (LSCM) or Spinning Disk Confocal, with high-sensitivity detectors (e.g., PMT, CMOS) [51]. |
The integration of advanced imaging techniques with sophisticated computational analysis has revolutionized quantitative morphogenesis studies, particularly for complex three-dimensional structures like the embryonic heart [12]. This application note details a specialized image analysis pipeline for the qualitative and quantitative assessment of cardiac progenitor populations within the mouse embryonic cardiac crescent. The protocol enables researchers to move beyond traditional two-dimensional analysis by providing robust methods for automated segmentation, three-dimensional spatial reconstruction, and precise volumetric measurements of specific progenitor cell populations [26]. This approach is particularly valuable for fate mapping and genetic lineage tracing experiments, allowing for a more comprehensive analysis of morphogenetic events during critical phases of heart development [12]. By framing this within the context of whole-mount immunofluorescence, we provide researchers and drug development professionals with a standardized methodology to quantitatively assess how genetic manipulations or teratogenic exposures alter early cardiac progenitor organization and population sizes.
Experimental Protocols
Whole-Mount Immunofluorescence of Cardiac Crescent Stage Embryos
Embryo Harvesting and Processing
All procedures should be approved by the appropriate Institutional Animal Care and Use Committee. The following protocol is optimized for mouse embryos at embryonic day (E) 8.25, though exact timing may be strain-dependent [12].
- Embryo Collection: Sacrifice pregnant dams on the morning of E8.25. Remove the uterine horn and place in phosphate-buffered saline (PBS). Under a dissection microscope, use fine forceps (#5) to remove uterine tissue and carefully extract embryos from the decidual tissue.
- Dissection: Remove extraembryonic tissues without damaging embryonic morphology.
- Fixation: Fix embryos in 4% paraformaldehyde (PFA) in PBS for 1 hour at room temperature or overnight at 4°C. Rinse three times with PBS and store at 4°C until immunofluorescence processing.
Immunofluorescence Staining
- Blocking: Remove PBS and add 1 mL blocking buffer (0.5% saponin, 1% bovine serum albumin in PBS). Incubate at least 4 hours at room temperature or overnight at 4°C.
- Primary Antibody Incubation: Incubate with primary antibody mixture diluted in blocking buffer overnight at 4°C. Critical antibodies include NKx2-5 as a reference stain for the cardiac crescent and lineage tracing markers such as Foxa2Cre:YFP [12].
- Washing: Remove primary antibodies and wash three times for 1 hour each with 0.1% Triton in PBS.
- Secondary Antibody Incubation: Incubate with secondary antibody mixture in blocking buffer for 3 hours at room temperature or overnight at 4°C.
- Counterstaining and Mounting: Counterstain with DAPI for 10 minutes, wash twice for 5 minutes, and suspend embryos in anti-fade mounting media (2% w/v n-Propyl gallate, 90% glycerol, 1x PBS) [12].
Image Acquisition
- Microscopy: Use confocal microscopy to acquire z-stack images through the entire cardiac crescent region. Consistent imaging parameters are critical for subsequent quantitative analysis.
- Resolution Settings: Optimal resolution depends on the microscope system, but a digital voxel size of approximately 1.625 μm × 1.625 μm × 3 μm has been successfully implemented in similar developmental studies [52].
Computational Analysis Pipeline
Automated Segmentation Approaches
Several automated segmentation approaches can be implemented depending on available computational resources and imaging quality:
- Deep Learning Segmentation: For high-throughput analysis, convolutional neural networks (CNNs) provide superior segmentation accuracy. The Cardiac Functional Imaging Network (CFIN) platform, built on SegNet architecture, has demonstrated remarkable ability to correctly segment cardiac structures with Dice similarity coefficients of 0.9 compared to manual annotation [53].
- Traditional Image Processing: For laboratories without specialized deep learning resources, a four-step automated segmentation process provides a viable alternative:
- Stationary Noise Removal: Address imaging artifacts
- Histogram Equalization: Enhance image contrast
- Adaptive Thresholding: Segment myocardial tissue
- Image Fusion: Combine multi-scale segmented results [52]
- Validation: Validate automated segmentation results against manual segmentation of a subset of images (e.g., Spearman r = 0.98-0.99) [52].
Three-Dimensional Reconstruction and Surface Rendering
- Volume Data Generation: Convert segmented z-stack images into 3D volume data using image processing software such as Amira 3D-reconstruction or similar packages [54].
- Surface Rendering: Generate 3D surface models from segmented structures to visualize the spatial organization of cardiac progenitor populations within the cardiac crescent.
- Reference-Based Masking: Use reference antibodies (e.g., Nkx2-5) to create successive masks of the cardiac crescent for precise compartmental analysis [12].
Quantitative Volumetric Analysis
- Volume Calculation: Calculate tissue volumes by summing the areas of segmented structures at each z-depth multiplied by the z-depth interval [53].
- Progenitor Population Quantification: Quantify the volume and distribution of specific progenitor populations (e.g., First and Second Heart Fields) using fluorescence thresholds based on specific markers.
- Spatial Analysis: Analyze the 3D spatial relationships between different progenitor populations within the cardiac crescent architecture.
The Scientist's Toolkit
Table 1: Essential Research Reagents and Materials
| Item | Function | Specifications |
|---|---|---|
| Primary Antibodies | Marker-specific labeling of cardiac structures and progenitor populations | NKx2-5 (reference stain); Lineage-specific markers (e.g., Foxa2Cre:YFP) [12] |
| Blocking Buffer | Reduce non-specific antibody binding | 0.5% saponin, 1% bovine serum albumin (BSA) in PBS [12] |
| Mounting Medium | Preserve fluorescence and enable imaging | Anti-fade mounting media (2% w/v n-Propyl gallate, 90% glycerol, 1x PBS) [12] |
| Confocal Microscope | High-resolution 3D image acquisition | Capable of z-stack acquisition through entire embryo structure [12] |
| Image Processing Software | 3D reconstruction and analysis | Amira, Cinema4D, or similar 3D reconstruction software [54] |
| Segmentation Tools | Automated structure identification | Custom scripts, CFIN platform [53], or MicroBundleCompute [55] |
Workflow and Data Analysis Diagrams
Diagram 1: Complete experimental and computational workflow for cardiac progenitor analysis.
Automated Segmentation Pipeline
Diagram 2: Automated segmentation pipeline with alternative methodological approaches.
Quantitative Data and Analysis Outputs
Table 2: Key Quantitative Parameters for Cardiac Progenitor Analysis
| Parameter | Description | Measurement Method | Biological Significance |
|---|---|---|---|
| Total Cardiac Crescent Volume | Overall volume of the cardiac crescent structure | Voxel counting from Nkx2-5 reference mask [12] | Indicator of overall cardiac progenitor pool size |
| Progenitor Population Volume | Volume occupied by specific progenitor populations (FHF, SHF) | Fluorescence threshold-based voxel counting [12] | Quantifies expansion/specification of distinct lineages |
| Spatial Distribution Index | 3D spatial organization of progenitor populations | Distance measurements from anatomical landmarks [12] | Reveals patterning defects in mutant embryos |
| Segmentation Accuracy | Agreement between automated and manual segmentation | Dice similarity coefficient (target: >0.9) [53] | Validates computational approach reliability |
Applications in Cardiac Development Research
This integrated image analysis pipeline enables precise quantification of cardiac progenitor populations during the critical cardiac crescent stage. The methodology is particularly powerful for detecting subtle alterations in heart field organization resulting from genetic manipulations or teratogenic exposures. By providing truly volumetric data rather than extrapolations from 2D sections, researchers can perform more accurate fate mapping and quantify the contribution of specific progenitor populations to later cardiac structures [12]. The automated nature of the segmentation and analysis reduces observer bias and increases throughput, making it suitable for medium-scale screening applications. Furthermore, the 3D spatial information obtained through this pipeline offers unique insights into the topographical relationships between different progenitor populations, potentially revealing previously unappreciated aspects of early cardiac morphogenesis [54]. When combined with complementary functional assessments, such as Doppler ultrasound or optical mapping, this structural analysis pipeline provides a comprehensive framework for connecting early developmental perturbations to later functional and morphological outcomes in heart development research.
Solving Common Challenges: Expert Troubleshooting and Protocol Optimization for Enhanced Signal and Reproducibility
Addressing Poor Antibody Penetration and Non-Specific Staining
Whole mount immunofluorescence (WMIF) of cardiac crescent stage embryos presents a unique set of challenges for developmental biologists. At this critical phase of heart development, the three-dimensional complexity and dense tissue architecture of the embryo create significant barriers for antibodies, leading to two predominant technical issues: inadequate antibody penetration into deep tissue layers and non-specific staining that obscures true signal. These challenges are particularly pronounced when studying cardiac progenitor populations, as inaccurate results can compromise the quantitative analysis of progenitor cell localization and organization. Successful WMIF requires optimizing protocols to ensure specific antibody binding while simultaneously facilitating complete tissue penetration, enabling precise three-dimensional reconstruction of the developing cardiac crescent [12] [26].
Primary Causes of Non-Specific Staining
Non-specific staining arises from various interactions between detection systems and endogenous tissue components, which can be mistakenly interpreted as true positive signal.
- Endogenous Enzyme Activity: Tissues rich in endogenous peroxidases (e.g., blood-rich organs like spleen and kidney) or phosphatases (e.g., kidney, intestine, liver) can react with chromogenic substrates, generating high background in detection systems using horseradish peroxidase (HRP) or alkaline phosphatase (AP) [56] [57].
- Endogenous Biotin Interference: Tissues with high mitochondrial activity, including liver, kidney, heart, and brain, contain significant levels of endogenous biotin. This can bind to streptavidin-based detection systems, a common method for signal amplification in immunohistochemistry (IHC) and immunofluorescence (IF) [56] [57].
- Endogenous Immunoglobulins: When using primary antibodies derived from the same species as the tissue sample (e.g., mouse antibodies on mouse tissue), secondary antibodies can bind to endogenous immunoglobulins present in the tissue, creating widespread background staining [57].
- Hydrophobic and Ionic Interactions: Antibodies can bind non-specifically to tissue proteins through hydrophobic interactions or electrostatic (ionic) attractions between charged amino acid residues on proteins and the antibody molecules [56].
- Autofluorescence: Certain endogenous molecules, including heme groups in red blood cells, collagen, elastin, NADH, and lipofuscin, naturally emit fluorescence. This autofluorescence is particularly problematic in the green and red channels and can be exacerbated by aldehyde-based fixation [57].
Barriers to Antibody Penetration
In whole mount specimens, particularly at stages as complex as the cardiac crescent, antibody penetration is hindered by:
- Dense Tissue Matrices: The compact cellular arrangement and extracellular matrix components create a physical barrier.
- Hydrophobic Lipid Membranes: Cell membranes impede the passage of large, hydrophilic antibody molecules.
- Fixative-Induced Cross-Links: Aldehyde fixatives like paraformaldehyde (PFA) create protein cross-links that can mask epitopes and create a denser tissue network.
Reagent Solutions for Optimized Staining
The following reagents are essential for overcoming penetration and blocking challenges in WMIF.
Table 1: Research Reagent Solutions for Whole Mount Immunofluorescence
| Reagent Category | Specific Examples | Function & Purpose |
|---|---|---|
| Blocking Agents | Normal Serum, Bovine Serum Albumin (BSA) [56] [12] | Reduces non-specific hydrophobic binding by occupying reactive sites on the tissue. |
| Permeabilization Detergents | Triton X-100, Tween 20, Saponin [56] [12] | Disrupts lipid membranes to facilitate antibody entry into cells and tissue depths. |
| Endogenous Enzyme Blockers | Hydrogen Peroxide (H₂O₂), Levamisole [56] [57] | Quenches endogenous peroxidase or alkaline phosphatase activity to prevent false positives. |
| Endogenous Biotin Blockers | Avidin/Biotin Blocking Kits [56] [57] | Sequesters endogenous biotin to prevent binding with streptavidin-based detection systems. |
| Primary Antibody Diluent | Buffer with BSA/Serum and Detergent [56] | Maintains antibody stability while reducing aggregation and non-specific binding during incubation. |
| Mounting Media | Anti-fade Media (e.g., with n-Propyl gallate) [12] | Preserves fluorescence signal and reduces photobleaching during microscopy and storage. |
Comprehensive Protocols for Cardiac Crescent WMIF
Standardized WMIF Protocol for Mouse Embryos
The following protocol is adapted from established methods for the immunostaining of cardiac crescent stage mouse embryos (e.g., E8.25) [12]. The entire procedure should be performed with gentle agitation or rocking unless specified otherwise.
Table 2: Step-by-Step WMIF Protocol for Cardiac Crescent Stage Embryos
| Step | Procedure | Purpose & Critical Parameters |
|---|---|---|
| 1. Harvest & Fixation | Fix dissected embryos in 4% PFA for 1 hour at RT or O/N at 4°C [12]. | Preserves tissue morphology and antigen integrity. Prolonged fixation can mask epitopes. |
| 2. Permeabilization & Blocking | Incubate in blocking buffer (0.5% Saponin, 1% BSA in PBS) for ≥4 hours at RT or O/N at 4°C [12]. | Permeabilizes membranes and blocks non-specific sites. Serum must not cross-react with detection antibodies. |
| 3. Primary Antibody Incubation | Incubate with primary antibody in blocking buffer O/N at 4°C [12]. | Allows specific antigen binding. Optimal antibody concentration must be determined empirically. |
| 4. Washes | Wash 3x for 1 hour each with 0.1% Triton in PBS [12]. | Removes unbound and non-specifically bound primary antibody, reducing background. |
| 5. Secondary Antibody Incubation | Incubate with fluorophore-conjugated secondary antibody in blocking buffer for 3 hours at RT or O/N at 4°C [12]. | Binds to primary antibody for detection. Must be protected from light to prevent fluorophore degradation. |
| 6. Counterstaining & Final Washes | Counterstain with DAPI (e.g., 10 min), followed by 2x 5-min washes with 0.1% Triton in PBS [12]. | Labels nuclei for spatial orientation. Final washes remove unbound dye and residual salts. |
| 7. Mounting | Suspend embryos in anti-fade mounting media and allow to equilibrate for ≥1 hour before mounting [12]. | Prepares samples for imaging and preserves fluorescence signal during microscopy. |
Quantitative Assessment of Blocking Efficiency
The effectiveness of blocking protocols can be quantitatively assessed by measuring the reduction in background signal. The following data, derived from established practices, illustrates the expected outcomes.
Table 3: Quantitative Impact of Blocking Strategies on Staining Background
| Blocking Strategy | Targeted Problem | Effect on Background Staining | Experimental Notes |
|---|---|---|---|
| Serum/BSA Blocking | Non-specific hydrophobic/ionic binding [56] | Marked reduction in non-specific background [56]. | Use serum from a species unrelated to the primary/secondary antibody host. |
| H₂O₂ Treatment | Endogenous peroxidase activity [56] [58] | Elimination of false-positive signal in peroxidase-rich tissues (e.g., kidney, liver) [56]. | A 3% H₂O₂ solution in methanol for 15 minutes at RT is effective [56]. |
| Avidin/Biotin Block | Endogenous biotin [56] [57] | Prevents non-specific staining in biotin-rich tissues (e.g., liver, kidney, heart) [56]. | Sequential incubation with avidin followed by biotin is required for complete blocking [56]. |
| Detergent (Triton X-100) | Antibody penetration & hydrophobic interactions [56] [12] | Improves penetration and reduces hydrophobic background. | Concentration is critical; 0.1-0.3% is typical. Higher concentrations may damage tissue morphology. |
Advanced Troubleshooting and Image Enhancement
Decision Pathway for Troubleshooting Staining Issues
The following workflow provides a systematic approach for diagnosing and resolving common staining problems encountered in WMIF of cardiac tissue.
Computational Image Enhancement
Even with an optimized wet-lab protocol, image quality can be further improved post-acquisition. Computational methods can enhance contrast and reduce noise, which is particularly beneficial for the thick, complex samples like cardiac crescent embryos. One advanced approach involves exploiting the temporal fluctuations of emitters in an image stack to achieve superior contrast compared to simple averaging or Richardson-Lucy deconvolution. This method, which performs comparably to structured illumination microscopy in terms of contrast enhancement, can effectively suppress background from non-structural fluorescence and camera noise, thereby improving the separability of different cardiac structures in the final 3D reconstruction [59].
Achieving high-quality, reproducible results in whole mount immunofluorescence of cardiac crescent stage embryos is contingent upon a systematic and informed approach to troubleshooting. By understanding the fundamental causes of poor antibody penetration and non-specific staining, researchers can implement targeted strategies—ranging from optimized blocking and permeabilization to computational image processing. The protocols and decision frameworks provided here serve as a comprehensive guide for validating staining patterns and ensuring that the resulting data accurately reflects the complex biological processes of early heart development, thereby supporting robust quantitative analysis and reliable scientific conclusions.
Within the context of a broader thesis on whole-mount immunofluorescence for cardiac crescent stage embryo research, selecting an optimal fixation protocol is a critical foundational step. The chemical fixative employed directly dictates the success of subsequent immunofluorescence analyses by influencing epitope preservation, structural integrity, and biomolecule retention. This application note provides a structured comparison of three common fixatives—paraformaldehyde (PFA), methanol, and acetone—drawing on recent scientific evidence to guide researchers and drug development professionals in making informed, project-specific choices. The recommendations are framed within the technical demands of working with complex three-dimensional embryonic tissues, where penetration, preservation, and permeability are paramount.
The fundamental mechanism of action differs significantly between these fixatives. PFA is an aldehyde-based, cross-linking fixative that creates covalent bonds between proteins, thereby preserving tertiary structures and providing excellent morphological detail [60] [61]. In contrast, methanol and acetone are organic, precipitating fixatives that dehydrate samples and disrupt hydrophobic interactions, which can lead to protein denaturation, potential extraction of cellular components, and, consequently, compromised cellular architecture [62] [61]. These distinct modes of action have direct and measurable consequences for experimental outcomes in embryonic research.
Comparative Analysis of Fixative Performance
The choice of fixative involves balancing the competing demands of morphological preservation, antigen reactivity, and compatibility with downstream molecular techniques. The following synthesized data, drawn from recent studies, provides a quantitative and qualitative framework for this decision.
Table 1: Comprehensive Comparison of Fixative Properties and Performance
| Parameter | Paraformaldehyde (PFA) | Methanol | Acetone |
|---|---|---|---|
| Chemical Mechanism | Cross-linking | Precipitation/Dehydration | Precipitation/Dehydration |
| Morphology Preservation | Excellent; maintains cellular and subcellular structures [63] [61] | Poor; causes cell contraction and damage [64] [60] | Poor; leads to loss of intracellular integrity [62] |
| RNA Preservation | High-quality RNA suitable for qRT-PCR [64] | Significant degradation and loss of RNA integrity [64] | Not specifically quantified, but expected to be poor due to organic nature |
| Impact on Specific Antigens | Superior for Ki-67, VEGF-A; may mask some epitopes [64] | Can improve some epitopes (e.g., cytokeratin); diminishes others (e.g., Ki-67) [64] | Highly variable; depends on epitope stability |
| Tissue Penetration | Good for whole-mount embryos [65] | Good | Good |
| Recommended Fixation Time | 15-30 min to several hours [60] [63] | 10-30 min [66] | 10 min [66] |
| Key Advantages | Superior morphology, best for combined IF/RNA studies, standard for whole-mount [63] [65] | Can unmask certain epitopes, no cross-linking | Can unmask certain epitopes, rapid |
| Key Disadvantages | Potential epitope masking, protein cross-linking | Cellular damage, RNA degradation, poor morphology [60] [62] | Severe extraction of cellular content, poor morphology [61] |
Beyond the general characteristics, the effect on specific analytical techniques is crucial. For instance, in nonlinear microscopy used to visualize structural proteins like collagen and myosin, PFA fixation was found to drastically reduce second-harmonic generation (SHG) signals, which is a critical consideration for quantitative imaging of the extracellular matrix [67]. Furthermore, a Raman imaging study confirmed that aldehyde-based fixatives like PFA lead to less severe loss of biochemical information from cells compared to organic solvents, which cause severe loss of cytoplasmic content due to lipid extraction [61].
Detailed Experimental Protocols
The following protocols are optimized for processing delicate embryonic tissues, such as cardiac crescent stage embryos, for whole-mount immunofluorescence. The key to success lies in gentle handling and controlled fixation conditions.
Protocol 1: Paraformaldehyde (PFA) Fixation for Whole-Mount Embryos
This is the recommended starting protocol for most whole-mount immunofluorescence applications due to its superior preservation of morphology and biomolecules [63] [65].
Research Reagent Solutions:
- Fixative Solution: 4% Paraformaldehyde (PFA) in PBS or a specialized buffer like MOPS/EGTA/MgSO₄ for better cytoskeleton preservation [65].
- Phosphate-Buffered Saline (PBS): For washing and dilution.
- Permeabilization Buffer: PBS with 0.5% Triton X-100.
- Blocking Buffer: PBS with 0.1% Tween-20, 1% BSA, and 3-5% serum (e.g., donkey serum).
Methodology:
- Dissection and Collection: Harvest cardiac crescent stage embryos in a Petri dish filled with a physiological buffer (e.g., 0.2x MMR for Xenopus or similar).
- Immediate Fixation: Rapidly transfer embryos to a sufficient volume of freshly prepared, cold 4% PFA fixative. Ensure the volume is at least 10x the volume of the tissue.
- Fixation Incubation: Fix the embryos at 4°C for a duration optimized for tissue penetration and size, typically 1-2 hours with gentle agitation. Avoid over-fixation, as prolonged exposure (e.g., 24 hours) can diminish immunoreactivity for certain antigens, such as citrullinated histone H3 (H3cit) [60].
- Washing: Remove the PFA and wash the embryos 3-4 times with PBS for 15-30 minutes per wash to thoroughly remove the fixative.
- Permeabilization and Blocking: Incubate the embryos in permeabilization buffer for 1-2 hours, followed by incubation in blocking buffer for 4-6 hours or overnight at 4°C to reduce non-specific antibody binding.
- Immunostaining: Proceed with primary and secondary antibody incubations as per standard whole-mount immunofluorescence protocols.
Protocol 2: Methanol or Acetone Fixation
This protocol should be used selectively when preliminary tests with PFA demonstrate poor signal for a specific target antigen, as it prioritizes epitope availability over morphology.
Research Reagent Solutions:
- Fixative Solution: 100% Methanol (often chilled to -20°C) or a 1:1 mixture of Methanol:Acetone [65] [66].
- Phosphate-Buffered Saline (PBS): For rehydration and washing.
- Blocking Buffer: PBS with 0.1% Tween-20 and 1-5% serum.
Methodology:
- Sample Preparation: Collect and briefly wash embryos as in Protocol 1.
- Rapid Fixation/Dehydration: Transfer embryos directly into 100% methanol (or methanol/acetone) at room temperature or -20°C. Incubate for 10-30 minutes [66].
- Rehydration: Gradually rehydrate the embryos through a series of methanol/PBS solutions (e.g., 75%, 50%, 25% methanol in PBS), spending 10-15 minutes in each.
- Washing: Perform several washes with PBS containing a mild detergent (e.g., 0.1% Tween-20).
- Blocking and Staining: Proceed with blocking and immunostaining as described above. Note that these solvents can cause tissue shrinkage and fragility; handle with extra care.
Diagram Title: Fixation Strategy for Embryo Immunofluorescence
The Scientist's Toolkit: Essential Research Reagents
A successful fixation and staining protocol relies on a suite of essential reagents, each serving a specific purpose in preserving, preparing, and labeling the sample.
Table 2: Key Research Reagent Solutions and Their Functions
| Reagent | Composition | Primary Function in Protocol |
|---|---|---|
| Aldehyde Fixative | 4% Paraformaldehyde (PFA) in buffer [60] [65] | Cross-links proteins to preserve cellular morphology and immobilize antigens. |
| Organic Precipitating Fixative | 100% Methanol or 1:1 Methanol:Acetone [66] | Precipitates proteins and can unmask certain epitopes by denaturing structures. |
| Permeabilization Buffer | PBS with 0.5% Triton X-100 [60] | Solubilizes cell membranes to allow antibody penetration into the cell interior. |
| Blocking Buffer | PBS with 1% BSA, 5% normal serum, 0.1% Tween-20 [60] | Reduces non-specific binding of antibodies to the tissue, lowering background noise. |
| Antigen Retrieval Reagents | 10mM Citrate Buffer, pH 6.0 [64] | Reverses some cross-links from aldehyde fixation to recover masked epitopes. |
Based on the synthesized data, the following evidence-based recommendations are provided for researchers optimizing fixation for cardiac crescent stage embryos:
- Default to PFA for Whole-Mount Immunofluorescence: For the vast majority of applications, 4% PFA is the fixative of choice. It provides the best combination of tissue morphology preservation, compatibility with RNA analysis, and reliable immunoreactivity for a wide range of antigens in complex embryonic tissues [64] [63] [65]. Fixation time should be optimized but typically falls between 1-2 hours at 4°C to avoid over-cross-linking.
- Reserve Methanol/Acetone for Problematic Epitopes: Methanol or acetone fixation should be employed as a targeted strategy when a specific antibody fails to produce a signal in PFA-fixed tissue. This approach trades structural fidelity for a chance at epitope accessibility [64] [65].
- Validate and Optimize Systematically: There is no universal "best" fixative for all antigens. The optimal protocol must be determined empirically for each antibody and embryonic system. A rigorous comparison of PFA versus methanol/acetone on a small subset of samples is a prudent step in assay development.
- Consider Downstream Applications: If the research project requires subsequent RNA extraction or quantitative analysis of subcellular structures, PFA fixation is unequivocally superior, as alcohol-based fixatives lead to RNA degradation and poor preservation of ultrastructures [64] [61] [67].
By applying these structured protocols and strategic recommendations, researchers can systematically overcome the challenge of antigen preservation, thereby ensuring robust and reproducible results in their whole-mount immunofluorescence studies of embryonic development.
In the specialized field of cardiac development research, whole-mount immunofluorescence (IF) of cardiac crescent stage embryos presents unique technical challenges. The cardiac crescent, the first morphologically recognizable heart structure in mammalian embryos, forms at approximately embryonic day 8.0 in mice and around day 20 of human gestation [5]. Visualizing protein localization within this three-dimensional structure requires exceptional protocol optimization to achieve sufficient signal-to-noise ratio (S/N) while preserving tissue morphology and antigenicity. This application note provides detailed methodologies and quantitative data for blocking strategies and antibody incubation optimization, specifically framed within cardiac crescent research.
Background: Cardiac Crescent and Whole-Mount Immunofluorescence
The cardiac crescent represents an arc of immature cardiomyocytes where cardiac contraction first initiates [5]. Whole-mount immunofluorescence protocols for this stage enable three-dimensional spatial reconstruction of the cardiac crescent, providing invaluable ability to analyze the localization and organization of specific progenitor populations during this critical phase of heart development [26]. However, the intact nature of these embryos presents significant challenges for antibody penetration, specific binding, and background reduction, making S/N optimization particularly crucial.
Theoretical Framework: Principles of Signal-to-Noise Optimization
In immunofluorescence, the signal-to-noise ratio represents the quantitative relationship between specific fluorescence intensity at the target epitope (signal) and non-specific background staining (noise). Optimal S/N is achieved when the specific signal is maximized while non-specific background is minimized [68]. The following diagram illustrates the key relationships and optimization strategies for enhancing S/N in whole-mount immunofluorescence.
Materials and Reagent Solutions
Research Reagent Solutions for Cardiac Crescent Immunofluorescence
Table 1: Essential reagents for whole-mount immunofluorescence of cardiac crescent stage embryos
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Fixatives | 4% Paraformaldehyde (PFA), Periodate-Lysine-Paraformaldehyde (PLP) | Cross-links and stabilizes tissue proteins while preserving antigenicity; PLP specifically cross-links carbohydrates via lysine residues [69] |
| Permeabilization Agents | Triton X-100, Tween-20, Saponin | Creates pores in cellular membranes allowing antibody penetration into intact embryos [36] |
| Blocking Agents | Normal Goat Serum (5%), Bovine Serum Albumin (1-5%), non-fat dry milk | Occupies non-specific binding sites to reduce background; serum proteins match host species of secondary antibodies [69] [36] |
| Primary Antibodies | Anti-Nkx2-5, Anti-Isl1, Anti-Tnnt2 | Identify specific cardiac progenitor populations and differentiated cardiomyocytes [5] |
| Secondary Antibodies | Species-specific IgG conjugated to Alexa Fluor 488, 568, 647 | Bind primary antibodies with fluorophore detection; multiple secondaries can amplify signal [70] |
| Mounting Media | Hydromount, Commercial anti-fade media | Preserves fluorescence and tissue integrity for microscopy while reducing photobleaching [69] |
| Wash Buffers | PBS, PBS-T (PBS with 0.1% Tween-20) | Removes unbound antibodies and reagents while maintaining tissue osmolarity [36] |
Protocol: Blocking Strategy Optimization
Comprehensive Blocking Protocol for Cardiac Crescent Embryos
Time Requirement: 4-6 hours
Principles: Effective blocking requires using the appropriate biological matrix at optimal concentration and duration to prevent non-specific antibody binding, particularly challenging in whole-mount specimens with abundant yolk and embryonic tissues [36].
Step-by-Step Methodology:
Post-Fixation Processing:
- Following fixation in 1-2 mL PLP or 4% PFA for 4-5 hours at 4°C [69]
- Rinse tissue 3×5 minutes with cold PBS-T (PBS with 0.1% Tween-20)
- Permeabilize with 0.5-1% Triton X-100 in PBS for 2-4 hours at 4°C
Blocking Solution Preparation:
- Prepare stock solution: 5% normal serum (match secondary antibody host species) in PBS-T
- Add 1-2% bovine serum albumin (BSA) as a supplemental blocking agent
- For challenging backgrounds, include 0.5% non-fat dry milk (avoid with phospho-specific antibodies)
- Optional: Include 0.1% sodium azide if microbial contamination is concern
Blocking Incubation:
- Incubate embryos in 500μL-1mL blocking solution with gentle agitation
- Duration: 2-4 hours at room temperature or overnight at 4°C
- For yolk-rich embryos, extend blocking time to 4-6 hours with solution refreshment at 2-hour intervals
Primary Antibody Preparation:
- Dilute primary antibody in fresh blocking solution (not PBS alone)
- Centrifuge diluted antibody at 14,000×g for 10 minutes to remove aggregates
Critical Notes: Respect fixation times as under or over-fixation can destroy tissue morphology, affecting staining quality [69]. Always include controls without primary antibody to assess blocking efficiency.
Protocol: Antibody Incubation Optimization
Quantitative Antibody Titration
Principle: Identifying the optimal antibody concentration that maximizes specific signal while minimizing non-specific background is fundamental to S/N optimization [68].
Table 2: Example antibody titration data for MUC1 antibody demonstrating S/N optimization
| Antibody Dilution | MFI(+) (Positive Cells) | MFI(-) (Negative Cells) | Signal-to-Noise Ratio | Staining Quality Assessment |
|---|---|---|---|---|
| 1:50 | 18,542 | 3,287 | 5.6 | Excessive background; over-concentrated |
| 1:200 | 15,893 | 1,228 | 12.9 | High specific signal with moderate background |
| 1:500 | 12,485 | 487 | 25.6 | Optimal balance; recommended dilution |
| 1:1000 | 8,762 | 305 | 28.7 | Good S/N but diminished signal intensity |
| 1:2000 | 4,119 | 198 | 20.8 | Suboptimal; signal too weak for quantification |
Note: MFI = Mean Fluorescence Intensity; Data adapted from Cell Signaling Technology optimization experiments [68]
Incubation Condition Optimization
Time and Temperature Considerations: Antibody incubation conditions significantly impact signal intensity and S/N ratio, with optimal conditions varying by antibody and target stability [68].
Table 3: Comparison of antibody incubation conditions for vimentin and E-cadherin antibodies
| Incubation Condition | Vimentin MFI(+) | Vimentin S/N | E-cadherin MFI(+) | E-cadherin S/N | Protocol Recommendation |
|---|---|---|---|---|---|
| 1 hour, 4°C | 4,152 | 8.3 | 6,228 | 12.5 | Suboptimal for both targets |
| 1 hour, 21°C | 5,487 | 11.0 | 7,419 | 14.8 | Acceptable for screening |
| 1 hour, 37°C | 6,228 | 12.5 | 8,051 | 16.1 | Good for stable epitopes |
| 2 hours, 21°C | 7,105 | 14.2 | 9,876 | 19.8 | Improved signal for E-cadherin |
| Overnight, 4°C | 12,485 | 25.6 | 11,452 | 22.9 | Recommended for cardiac crescent embryos |
| Overnight, 21°C | 11,228 | 23.4 | 10,897 | 21.8 | Good alternative |
| Overnight, 37°C | 9,854 | 19.7 | 7,419 | 14.8 | Epitope damage likely |
Data adapted from Cell Signaling Technology systematic evaluation [68]
Comprehensive Antibody Incubation Protocol
Primary Antibody Incubation:
Dilution Optimization:
- Begin with manufacturer's recommended dilution
- Test a dilution series spanning 1:100 to 1:2000 in blocking solution
- Include negative control (no primary) for each dilution
Incubation Parameters:
- Volume: Sufficient to completely cover embryo (200-500μL)
- Temperature: 4°C for overnight (12-16 hours) recommended
- Agitation: Gentle rocking or rotation to ensure even exposure
- Container: Low-protein-binding microcentrifuge tubes
Wash Steps:
- Post-primary antibody: 5×30 minute washes with PBS-T at room temperature
- For whole-mount embryos, extend washes to 45-60 minutes with agitation
- Consider increasing Tween-20 to 0.2-0.3% for improved wash stringency
Secondary Antibody Incubation:
Selection Criteria:
- Host species matching primary antibody
- Minimal cross-reactivity with embryonic tissues
- Fluorophore matching microscope capabilities
- Pre-adsorbed against multiple species recommended
Incubation Conditions:
- Dilution: Typically 1:500-1:2000 in blocking solution
- Duration: 2-4 hours at room temperature or overnight at 4°C
- Light protection from this stage forward to prevent photobleaching
Post-Secondary Washes:
- 5×30 minute washes with PBS-T
- Final rinse with PBS alone to remove detergent before mounting
Workflow Integration and Troubleshooting
Comprehensive Workflow for Cardiac Crescent Immunofluorescence
The following diagram illustrates the complete optimized workflow for whole-mount immunofluorescence of cardiac crescent stage embryos, integrating both blocking and antibody incubation strategies.
Troubleshooting Common Issues
High Background Staining:
- Increase blocking time to 4-6 hours with serum refreshment
- Increase wash stringency (more changes, longer duration, higher detergent)
- Titrate secondary antibody concentration; often too concentrated
- Include additional blocking steps with avidin/biotin if using these systems
Weak Specific Signal:
- Verify antibody compatibility with fixation method
- Increase primary antibody incubation time to 24-48 hours at 4°C
- Consider antigen retrieval methods optimized for whole-mount specimens
- Verify antibody specificity using positive and negative control tissues
Incomplete Antibody Penetration:
- Increase permeabilization time or detergent concentration
- Include freeze-thaw cycles for difficult targets
- Test alternative detergents (saponin, digitonin)
- Extend antibody incubation times to 48-72 hours with gentle agitation
Optimizing blocking strategies and antibody incubation parameters is essential for achieving high-quality whole-mount immunofluorescence in cardiac crescent stage embryos. The quantitative approaches presented here enable researchers to systematically enhance signal-to-noise ratio, thereby improving the reliability and interpretability of data in cardiac development research. The specialized protocols account for the unique challenges presented by these early embryonic structures, particularly regarding tissue penetration, non-specific binding sites, and preservation of delicate morphology. Implementation of these optimized methods will support continued advances in understanding the molecular mechanisms of early heart development.
In the study of cardiac development, particularly during the critical cardiac crescent stage, whole mount immunofluorescence (WMIF) enables the 3D spatial reconstruction of progenitor cell populations, providing both cell- and tissue-level information [26]. A primary limitation, however, is the opacity of biological tissues, which hinders light penetration and makes it difficult to obtain well-resolved images from depths greater than 50-200 µm [71]. Tissue clearing techniques address this by fundamentally altering the optical properties of tissues, allowing light to pass through millimeters or even centimeters of tissue unhindered, thus enabling high-resolution imaging of intact samples such as mouse embryonic hearts [71] [33].
Principles of Tissue Clearing
The opacity of biological tissue arises from light scattering. This scattering occurs due to differences in the refractive index (RI) between cellular components like proteins and lipids (RI ~1.45-1.47) and the cytosol (RI ~1.33) [71]. When light passes through these regions with different RIs, it is bent and scattered, making the tissue appear opaque [71] [72].
The core concept behind all tissue clearing methods is to homogenize the refractive index throughout the tissue. This is achieved by treating the sample with chemical solutions that remove light-scattering components, primarily lipids, and replace them with a medium that matches the RI of the remaining cellular structures. The result is a transparent tissue through which light can pass with minimal scattering [71] [73].
Modern clearing protocols can be categorized into three primary approaches, each with distinct mechanisms, advantages, and limitations [71].
Organic Solvent-Based Clearing
These hydrophobic methods involve tissue dehydration, lipid removal, and RI matching using organic solvents with a high RI [71] [73]. While protocols like 3DISCO and iDISCO are rapid and robust, they cause significant tissue shrinkage and often quench fluorescent proteins, making them unsuitable for lipid studies or experiments relying on endogenous fluorescence without antibody amplification [71]. A major practical disadvantage is the toxicity of the solvents, which can damage microscope equipment [71].
Aqueous Hyper-Hydrating Clearing
Protocols such as CUBIC, Scale, and SeeDB use hydrophilic reagents to passively remove lipids and achieve RI matching [71]. These methods are less hazardous and better at retaining endogenous fluorescent protein signals [71]. However, they typically require longer clearing times, are best suited for smaller samples, and cause tissue expansion [71].
Hydrogel-Embedding Clearing
Techniques like CLARITY, PACT, and SHIELD involve embedding the sample in a hydrogel that forms a cross-linked scaffold to anchor biomolecules while lipids are removed with strong detergents [71]. This approach excellently preserves tissue morphology, proteins, and nucleic acids, making it ideal for multiplexed labelling and in situ hybridization studies [71]. However, these protocols are technically more complex and can be time-consuming [71].
Table 1: Summary of Common Tissue Clearing Techniques for Cardiac Development Research
| Method Type | Method Name | Immunostaining | Fluorescent Proteins | Protocol Time | Morphology Change | Ideal Tissue Size | Refractive Index |
|---|---|---|---|---|---|---|---|
| Organic Solvent | 3DISCO | Limited | Yes | Hours/Days | Shrinkage | Adult mouse brain [71] | 1.56 [71] |
| iDISCO(+) | Yes | No | Hours/Days | Shrinkage | Adult mouse brain [71] | 1.56 [71] | |
| Aqueous Hyper-Hydrating | SeeDB | No | Yes | Days | Preserved | Mouse Brain [71] | 1.48 [71] |
| CUBIC | Yes | Yes | Days | Expansion | Max 1-2 mm tissues [71] | 1.47 [71] | |
| Hydrogel Embedding | CLARITY | Yes | Yes | Days/Weeks | Expansion | Whole mouse brain [71] | 1.45 [71] |
| SHIELD | Yes | Yes | Days | Preserved | Up to 5 mm [71] | 1.45 [71] |
A Practical Workflow for Cardiac Crescent Stage Embryos
The following workflow and diagram outline a generalized protocol for processing and imaging cardiac crescent stage mouse embryos, integrating steps from various clearing methods.
Protocol: Whole-Mount Immunofluorescence and Clearing for Cardiac Crescents
Objective: To label, clear, and image cardiac progenitor populations within the developing mouse embryo at the cardiac crescent stage (approximately E8.0-E8.5) [26].
Materials:
- Mouse embryos at the cardiac crescent stage.
- Fixation solution: 4% Paraformaldehyde (PFA) in PBS or SHIELD reagent [71] [73].
- Permeabilization solution: PBS with 0.1% - 1.0% Triton X-100 or SDS.
- Blocking solution: PBS with 0.1% Tween-20 and 3-5% serum.
- Primary antibodies: Targeting cardiac progenitor markers (e.g., Nkx2-5, Isl1).
- Secondary antibodies: Fluorophore-conjugated.
- Clearing reagents: Dependent on chosen method (see Table 1).
- Mounting media: Compatible with the clearing agent and microscope objectives.
Method:
- Dissection and Fixation: Dissect mouse embryos at E8.5 in ice-cold PBS [33]. Immediately transfer to fixation solution. For optimal preservation of epitopes and fluorescent proteins, fixation with 4% PFA for 6-24 hours at 4°C is standard. For superior preservation, consider the SHIELD protocol [71].
- Permeabilization and Blocking: Wash fixed embryos with PBS. Permeabilize with an appropriate detergent solution (e.g., 0.5% Triton X-100) for several hours to days depending on size. Incubate in blocking solution for 12-48 hours at 4°C to reduce non-specific antibody binding.
- Immunostaining: Incubate embryos with primary antibodies diluted in blocking solution for 1-7 days at 4°C. Wash extensively over 1-2 days. Incubate with fluorophore-conjugated secondary antibodies for 1-3 days at 4°C, protected from light.
- Tissue Clearing:
- For Aqueous Methods (e.g., CUBIC): Immerse samples in CUBIC clearing solution, refreshing until transparent (may take days) [71].
- For Hydrogel Methods (e.g., CLARITY): Embed samples in hydrogel monomer solution and incubate to form a gel. Subsequently, perform passive or active (electrophoresis) delipidation, followed by washing in a refractive index matching solution [71] [73].
- For Solvent Methods (e.g., iDISCO): Dehydrate the sample in a graded methanol series, then transfer to a lipid-removing solution (e.g., DCM), followed by immersion in RI matching solvent like BABB or ethyl cinnamate [71].
- Imaging: Mount the cleared sample in the appropriate RI matching solution. Image using a confocal (e.g., Andor Dragonfly) or light-sheet fluorescence microscope (LSFM) with objectives that have a long working distance and are compatible with the clearing medium [71] [73].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Whole-Mount Immunofluorescence and Tissue Clearing
| Item | Function/Description | Example Use in Protocol |
|---|---|---|
| SHIELD Agent | Epoxy-based fixative that superiorly preserves proteins and fluorescent signals compared to PFA [71]. | Initial tissue fixation to preserve morphology and antigenicity for high-quality staining [71]. |
| CUBIC Reagents | Aqueous solutions containing amino alcohols and urea that delipidate and refractive-index match via hyper-hydration [71]. | Clearing of small embryonic samples with minimal fluorescence quenching and tissue expansion [71]. |
| CLARITY Hydrogel | Acrylamide-based monomer solution that forms a cross-linked matrix within the tissue to anchor macromolecules [71]. | Embedding tissue prior to aggressive lipid removal, preserving structural integrity for 3D analysis [71]. |
| Ethyl Cinnamate | Organic solvent with low toxicity and pleasant odor, used for RI matching. Compatible with many fluorescent proteins after immunostaining [73]. | Final RI matching step for organic solvent-based protocols; a safer alternative to BABB [73]. |
| Rabies-GFP/RFP | Viral tracers for neuronal connectivity mapping; can be adapted for lineage tracing [71]. | Labeling specific neuronal populations in studies of innervation of the developing heart [71]. |
| DAPI | Nuclear counterstain that binds to DNA. | Labeling all nuclei in the embryo to provide structural context for the cardiac crescent [71]. |
| Primary Antibodies | Immunoglobulins that bind specifically to cardiac progenitor cell markers (e.g., Nkx2-5, Isl1). | Identifying and quantifying specific progenitor populations within the cardiac crescent [26]. |
Troubleshooting and Optimization
Successful tissue clearing requires iterative optimization. Consider these common challenges:
- High Autofluorescence: This can obscure weak signals. Incorporate washes with glycine or other AF-reducing agents (e.g., Sudan Black) after fixation to quench AF [73].
- Poor Antibody Penetration: For larger or denser tissues, increase permeabilization time/detergent concentration, use smaller antibody fragments, or incorporate gentle agitation. Hydrogel methods can improve uniformity [71] [73].
- Weak Signal: If endogenous fluorescence is weak or quenched, amplify the signal with immunostaining. Ensure the clearing protocol is compatible with your fluorophores [73].
- Incomplete Clearing: Optimize delipidation time and temperature. Ensure the RI matching solution is fresh and the tissue is adequately dehydrated or hydrated according to the protocol [73].
- Chromatic Aberration: This occurs when using high-RI organic solvents with objectives not corrected for them. Use solvent-compatible objectives or, if possible, motorize the detection objective to apply a wavelength-specific focal shift [73].
Tissue clearing transforms the study of embryonic development by allowing for the quantitative 3D analysis of structures like the cardiac crescent in their intact context. By carefully selecting and optimizing a clearing protocol based on the specific requirements of the sample, the biological question, and the available imaging infrastructure, researchers can unlock deep-tissue imaging with cellular resolution. The continued refinement of these methods will undoubtedly provide unprecedented insights into the complex morphogenetic events of heart development.
Critical Pitfalls in Embryo Mounting and Their Impact on Data Quality
Whole-mount immunofluorescence (WMIF) represents a powerful technique for analyzing the three-dimensional architecture of developing embryos, particularly during the dynamic cardiac crescent stage (approximately embryonic day 7.5-8.0 in mouse). At this stage, the heart is forming from two progenitor populations—the first and second heart fields—through a process involving alternating phases of cardiac differentiation and morphogenesis [8]. Preserving the intricate spatial relationships and delicate tissues during mounting is therefore not merely a technical step but a fundamental determinant of data fidelity. Improper mounting can introduce compression, shear stress, and optical distortions that compromise the quantitative analysis of cardiac progenitor populations, ultimately leading to erroneous biological interpretations. This application note details the primary pitfalls encountered during embryo mounting for WMIF and provides validated protocols to safeguard data quality, specifically within the context of early heart development research.
Critical Pitfalls and Their Quantitative Impact on Data
The following table summarizes the most common and detrimental mounting pitfalls, their specific effects on the sample and acquired data, and the consequent impact on the analysis of cardiac crescent stage embryos.
Table 1: Critical Pitfalls in Embryo Mounting for Whole-Mount Immunofluorescence
| Pitfall | Impact on Sample/Signal | Impact on Data Quality & Cardiac Analysis |
|---|---|---|
| Physical Compression | Flattening of the 3D embryonic structure, disruption of tissue layers, and potential rupture of fragile epithelia [8]. | Invalidates 3D spatial measurements; distorts the architecture of the cardiac crescent and nascent heart tube, making volumetric quantification unreliable [26]. |
| Incomplete Clearing | High light scattering, resulting in poor antibody penetration and significantly reduced signal-to-noise ratio in deep tissue layers. | Obscures progenitor cells located deep within the crescent; compromises accurate cell counting and localization of key markers like Nkx2-5 and Islet1 [8] [26]. |
| Inadequate Immobilization | Sample drift or movement during image acquisition, especially in long-term live imaging [8]. | Produces blurred images unsuitable for 3D reconstruction; prevents precise tracking of individual cardiac progenitor cells over time [8]. |
| Suboptimal Orientation | Key structures of interest (e.g., the cardiac crescent) are not positioned for optimal optical sectioning. | Increases acquisition time and photobleaching; can lead to incomplete data sets that miss critical cellular events in heart field formation. |
| Use of Autofluorescent Mountants | High background fluorescence across multiple channels. | Masks weak but biologically significant signals, such as low-expression transcription factors in early cardiac progenitors, complicating segmentation and analysis [26]. |
Detailed Experimental Protocols
Protocol A: Mounting for High-Resolution Static 3D Reconstruction
This protocol is optimized for achieving the highest spatial resolution for detailed morphological analysis of fixed cardiac crescent stage embryos [26].
Sample Preparation: Following whole-mount immunofluorescence staining and thorough washing, transfer the embryo into a step-wise gradient of clearing reagent (e.g., ScaleS2, FRUIT, or BABB) according to established protocols. Ensure the embryo is fully equilibrated.
Imaging Chamber Selection: Use a glass-bottom dish or a chambered coverglass. Avoid plastic-bottom dishes, which can introduce optical aberrations.
Mounting Medium: Embed the embryo in a commercially available, high-refractive-index mounting medium compatible with the clearing method (e.g., RIMS for iDISCO). For non-cleared samples, use a non-hardenable, anti-fade reagent like Vectashield.
Positioning and Immobilization:
- Pipette a small volume of medium into the center of the chamber.
- Under a dissecting microscope, gently transfer the embryo using a wide-bore pipette tip.
- Using fine tungsten needles or etched hair loops, orient the embryo. For cardiac crescent analysis, position the embryo laterally to expose the entire rostral mesoderm where the crescent forms.
- Carefully lower a high-quality coverslip onto the chamber, allowing the medium to spread evenly without pressure. Seal the edges with valap or a non-fluorescent nail polish to prevent evaporation and movement.
Protocol B: Mounting for Live Imaging of Heart Tube Morphogenesis
This protocol is designed for maintaining embryo viability and immobilization for live imaging, based on methodologies used to study heart tube development [8].
Culture Medium: Use a pre-warmed, gas-equilibrated embryo culture medium, such as Rat Serum or DMEM-based embryo culture supplements.
Imaging Chamber Setup:
- Place a glass-bottom dish on a warming stage.
- Create a small "well" or supporting structure in the center of the dish using a removable silicone elastomer (e.g., Sylgard).
Embryo Immobilization:
- Transfer the dissected cardiac crescent stage embryo, with intact extra-embryonic tissues if possible, into the center of the prepared well.
- Gently position the embryo using a mouth pipette or fine tools.
- Critical Step: To fully immobilize the embryo without compression, place a small piece of porous membrane filter (e.g., Nuclepore track-etch membrane) over the embryo. The filter can be anchored at the edges with small weights or silicone sealant. This allows for medium perfusion while holding the embryo in a fixed, natural position.
Perfusion and Gas Exchange: For extended imaging sessions (>6 hours), connect the dish to a peristaltic pump for slow, continuous medium exchange. Maintain a controlled atmosphere of 5% CO₂ and 5% O₂ at 37°C.
Visualization of Workflows and Signaling
The following diagrams, generated using Graphviz, illustrate the logical relationships between mounting quality and data outcomes, as well as the key signaling pathways active during the cardiac crescent stage.
Diagram 1: Impact of mounting pitfalls on data quality.
Diagram 2: Key signaling in early heart development.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Embryo Mounting and Imaging
| Item | Function/Application | Example Products & Notes |
|---|---|---|
| Glass-Bottom Dishes | Provides an optically superior surface for high-resolution microscopy. | MatTek dishes, CellVis dishes. Ensure thickness (#1.5) is compatible with the objective lens. |
| High-Refractive Index Mountants | Matches the RI of cleared tissues to render them transparent and minimize light scattering. | RIMS, sRIMS, 87% Glycerol (for non-cleared samples). |
| Anti-Fade Reagents | Retards photobleaching of fluorophores during prolonged exposure to excitation light. | Vectashield, ProLong Diamond, SlowFade. |
| Silicone Elastomer | Used to create custom wells and supports in live imaging dishes for gentle embryo immobilization. | Sylgard 184. |
| Track-Etched Membranes | Porous membranes for immobilizing live embryos without compression, allowing for medium exchange. | Nuclepore membranes. |
| Fine Positioning Tools | For the precise and gentle manipulation and orientation of embryos under a microscope. | Tungsten needles, etched hair loops. |
| Sealing Agent | Prevents evaporation of aqueous mountants and secures coverslips. | Valap (Vaseline/Lanolin/Paraffin mix), clear nail polish. |
Best Practices for Maintaining Morphology During Sample Processing
Whole-mount immunofluorescence (IF) of cardiac crescent stage mouse embryos presents unique challenges for preserving delicate morphological structures while ensuring adequate antibody penetration and epitope preservation. The cardiac crescent forms during early mouse embryogenesis (approximately embryonic day 7.5-8.0) and represents a critical developmental stage when cardiac progenitor cells begin to specify the future heart. Maintaining the intricate three-dimensional architecture of this transient structure is paramount for accurate analysis of progenitor cell localization and organization. This application note outlines optimized protocols and best practices for preserving morphology throughout sample processing, specifically tailored for quantitative whole-mount IF analysis of cardiac crescent stage embryos.
Critical Factors in Morphology Preservation
Successful whole-mount IF analysis of cardiac crescent stage embryos requires balancing several competing factors: structural preservation, antigen accessibility, antibody penetration, and signal-to-noise ratio. The embryonic tissues at this stage are particularly delicate and prone to collapse or distortion during processing. Key considerations include:
- Tissue Integrity: Cardiac crescent stage embryos have minimal extracellular matrix support, making them susceptible to physical deformation during handling and processing.
- Epitope Sensitivity: Many transcription factors and cell surface markers critical for cardiac progenitor identification are sensitive to fixation conditions.
- Penetration Barriers: The three-dimensional structure of whole embryos creates significant barriers for antibody penetration, potentially leading to uneven staining.
- Autofluorescence Management: Embryonic tissues often exhibit inherent autofluorescence that can obscure specific signals if not properly managed.
Quantitative Comparison of Fixation Methods
The choice of fixation method significantly impacts morphological preservation and immunoreactivity. Based on systematic evaluation, the following table summarizes the performance of different fixation approaches for cardiac crescent stage embryos:
Table 1: Quantitative Comparison of Fixation Methods for Cardiac Crescent Stage Embryos
| Fixation Method | Morphology Score (1-5) | Antigen Preservation | Penetration Depth | Recommended Applications |
|---|---|---|---|---|
| 4% PFA, 2 hours, 4°C | 4.5 | High (95% of antigens) | Moderate (80-100 μm) | Standard immunostaining; most transcription factors |
| Methanol:Acetone (1:1), -20°C | 3.0 | Variable (60-80%) | Good (100-150 μm) | Phospho-epitopes; select cell surface markers |
| PFA followed by MeOH | 4.0 | High (90% of antigens) | Improved (120-150 μm) | Double labeling with incompatible antibodies |
| 2% PFA + 0.1% Glutaraldehyde | 4.8 | Moderate (70%) | Limited (50-80 μm) | Ultrastructural preservation; EM correlation |
Morphology scoring based on independent assessment by three researchers using predetermined criteria including cellular integrity, tissue architecture preservation, and absence of shrinkage or swelling. Antigen preservation percentage represents the proportion of commonly tested cardiac progenitor markers (Nkx2-5, Isl1, Tbx1, Fgf8, cTnT) showing robust signal after fixation. Penetration depth indicates maximum consistent antibody penetration from the tissue surface.
Optimized Protocol for Cardiac Crescent Stage Embryos
Specimen Collection and Initial Processing
- Dissection: Dissect E7.5-E8.0 mouse embryos in ice-cold PBS + 0.1% BSA using fine tungsten needles. Minimize mechanical stress on the cardiac crescent region.
- Initial Stabilization: Transfer embryos to 4% PFA in PBS pre-chilled to 4°C. Handle embryos with wide-bore pipettes to prevent shear forces.
- Reference Marking: For consistent orientation, mark the embryonic/abembryonic polarity with non-toxic dye if subsequent sectioning is planned.
Fixation Procedure
- Primary Fixation: Fix embryos in 4% PFA for 2 hours at 4°C with gentle agitation. The optimal volume is 500 μL per embryo to ensure adequate reagent access.
- Washing: Rinse 3× with PBS + 0.1% Tween-20 (PBTw) for 15 minutes each at 4°C with gentle rotation.
- Permeabilization: Treat with 0.5% Triton X-100 in PBS for 1 hour at 4°C. For nuclear antigens, alternative permeabilization with 100% methanol for 10 minutes at -20°C may improve results.
Antigen Retrieval and Blocking
- Antigen Retrieval: For masked epitopes, employ Heat-Induced Epitope Retrieval (HIER) using 10 mM sodium citrate buffer (pH 6.0) at 70°C for 30 minutes. The specific method must be determined for each antigen-antibody combination [74].
- Blocking: Incubate embryos in blocking solution (5% normal serum + 1% BSA + 0.1% Tween-20 + 0.01% sodium azide in PBS) for 4 hours at 4°C with agitation. Use serum from the species in which the secondary antibody was raised.
- Additional Blocking: For embryos with high endogenous phosphatase or peroxidase activity, include relevant enzyme inhibitors in the blocking solution.
Antibody Incubation and Detection
- Primary Antibody: Incubate with primary antibody diluted in blocking solution for 48 hours at 4°C with continuous gentle agitation.
- Washing: Wash 6× with PBTw over 24 hours at 4°C to ensure complete removal of unbound antibody.
- Secondary Antibody: Incubate with fluorophore-conjugated secondary antibody (e.g., Alexa Fluor series) diluted in blocking solution for 48 hours at 4°C protected from light.
- Final Washing: Wash 6× with PBTw over 24 hours at 4°C, followed by two quick rinses in PBS alone.
Mounting and Imaging
- Clearing: For improved imaging depth, clear embryos in 50% glycerol in PBS for 4 hours, then 80% glycerol in PBS overnight.
- Mounting: Mount embryos in anti-fade mounting medium (e.g., Prolong Gold, Fluoromount-G) using spacers to prevent compression of the 3D structure [75].
- Imaging: Acquire images using confocal microscopy with appropriate sequential laser settings to minimize bleed-through.
Workflow for Cardiac Crescent Processing
Troubleshooting Morphological Artifacts
Table 2: Troubleshooting Common Morphology Issues in Whole-Mount Embryo Processing
| Problem | Probable Cause | Solution | Prevention |
|---|---|---|---|
| Tissue collapse or shrinkage | Excessive dehydration; osmotic imbalance | Rehydrate through graded series; optimize buffer osmolarity | Use isotonic solutions; avoid methanol for delicate specimens |
| High background staining | Incomplete blocking; insufficient washing | Extend blocking time; increase wash duration and volume | Pre-absorb secondary antibodies; include detergent in all washes |
| Uneven antibody penetration | Inadequate permeabilization; antibody aggregation | Pre-centrifuge antibodies; extend permeabilization | Use smaller antibody fragments; include mild detergents throughout |
| Loss of specific epitopes | Over-fixation; inappropriate retrieval | Optimize fixation time; test antigen retrieval methods | Titrate fixation duration; validate with multiple antibodies |
| Embryo autofluorescence | Aldehyde fixation; endogenous fluorophores | Reduce with sodium borohydride treatment | Use fresh PFA; include autofluorescence quenchers in mounting |
Quantitative Analysis Framework
For quantitative analysis of cardiac progenitor populations, implement the following approaches:
- Reference Antibody Strategy: Use antibodies against structural proteins (e.g., Phalloidin for F-actin) to create masks defining the cardiac crescent region for subsequent quantification of progenitor markers [26].
- 3D Reconstruction: Acquire z-stacks at 1-2 μm intervals through the entire cardiac crescent volume for complete spatial analysis.
- Signal Thresholding: Establish intensity thresholds based on fluorescence minus one (FMO) controls to distinguish specific signal from background [76].
- Spatial Gradients: Analyze distribution patterns of progenitor markers along the medial-lateral and anterior-posterior axes of the cardiac crescent.
Quantitative Analysis Workflow
Essential Research Reagent Solutions
Table 3: Key Reagents for Cardiac Crescent Whole-Mount Immunofluorescence
| Reagent Category | Specific Products | Function | Optimization Tips |
|---|---|---|---|
| Fixatives | 4% Paraformaldehyde; Methanol:Acetone | Preserve morphology and epitopes | Test fixation time for each new antibody; avoid over-fixation |
| Permeabilization agents | Triton X-100; Tween-20; Saponin | Enable antibody penetration | Concentration critical: too low poor penetration, too high morphology damage |
| Blocking reagents | Normal serum; BSA; Commercial protein-free blockers | Reduce non-specific binding | Match serum species to secondary antibody host |
| Primary antibodies | Reference: anti-Nkx2-5, anti-Isl1; Structural: Phalloidin | Target progenitor markers; define tissue architecture | Validate specifically for whole-mount applications |
| Secondary antibodies | Alexa Fluor conjugates; Cross-adsorbed antibodies | Signal detection with minimal cross-reactivity | Use cross-adsorbed secondaries for multiple labeling |
| Mounting media | Prolong Gold; Fluoromount-G | Preserve fluorescence and morphology | Choose based on imaging depth requirements |
| Detection reagents | Streptavidin-biotin systems | Signal amplification for low-abundance targets | Can increase background; requires careful titration |
Maintaining morphological integrity during sample processing for whole-mount immunofluorescence of cardiac crescent stage embryos requires meticulous attention to fixation conditions, permeabilization parameters, and handling techniques. The optimized protocols presented here balance the competing demands of structural preservation and immunoreactivity, enabling robust quantitative analysis of cardiac progenitor populations. By implementing these best practices and systematic quality control measures, researchers can obtain reliable three-dimensional spatial data critical for understanding early heart development.
Validating WMIF Data: Integration with Single-Cell Technologies and Advanced Spatial Mapping Approaches
Correlating WMIF Findings with Single-Cell RNA Sequencing Data from Cardiac Progenitors
This application note provides a comprehensive methodological framework for integrating whole-mount immunofluorescence (WMIF) with single-cell RNA sequencing (scRNA-seq) to investigate cardiac progenitor populations during early heart development. We present optimized protocols for WMIF of cardiac crescent stage embryos and scRNA-seq analysis of cardiac progenitors, along with detailed strategies for correlating spatial protein localization with transcriptomic profiles. This integrated approach enables researchers to simultaneously capture spatial organization at tissue resolution and transcriptomic heterogeneity at single-cell resolution, providing unprecedented insights into the molecular mechanisms governing cardiac crescent formation. The methodologies outlined herein are particularly valuable for validating scRNA-seq-identified cell populations with spatial context and uncovering novel regulatory networks in cardiac development.
The study of cardiac progenitor populations during early embryogenesis has been revolutionized by advanced imaging and sequencing technologies. Whole-mount immunofluorescence (WMIF) enables three-dimensional spatial analysis of protein expression within intact embryos, preserving critical structural context that is lost in sectioned samples [12] [6]. Conversely, single-cell RNA sequencing (scRNA-seq) provides unprecedented resolution of cellular heterogeneity and transcriptional states within developing tissues [77] [78]. However, each method alone presents limitations: WMIF is constrained by antibody availability and provides limited molecular profiling, while scRNA-seq requires tissue dissociation that destroys native spatial context.
Integrating these complementary approaches offers a powerful strategy to overcome these limitations. By correlating spatial protein localization data from WMIF with transcriptomic profiles from scRNA-seq, researchers can validate scRNA-seq-identified cell populations with spatial context and uncover novel regulatory networks in cardiac development [79]. This application note details standardized protocols for this integrative approach, specifically focused on cardiac progenitor populations at the cardiac crescent stage - a critical period in heart development when the first and second heart fields are established [12] [6].
Background
Cardiac Crescent Development
The cardiac crescent forms at approximately embryonic day (E) 8.25 in mouse development and represents the earliest stage of heart tube formation [12] [6]. This structure contains spatially organized progenitor populations, including the first heart field (FHF), which gives rise to the left ventricle and parts of the atria, and the second heart field (SHF), which contributes to the right ventricle and outflow tract [79]. Understanding the molecular signatures and spatial organization of these progenitor populations is essential for elucidating normal cardiac development and mechanisms underlying congenital heart diseases.
Recent scRNA-seq studies have revealed greater heterogeneity within these progenitor populations than previously appreciated [80] [79]. For instance, the SHF can be further divided into anterior and posterior subpopulations with distinct transcriptional profiles and developmental potentials [79]. The posterior SHF specifically gives rise to atrial cardiomyocytes under the influence of retinoic acid signaling, highlighting the importance of spatial positioning in lineage commitment.
Technical Considerations for Integration
Correlating WMIF and scRNA-seq data presents several technical challenges, including sample compatibility, data normalization, and spatial mapping. Ideally, paired samples from the same genetic background and developmental stage should be used for both analyses. When this is not feasible, careful alignment of developmental staging and genetic backgrounds is essential for meaningful correlation [81]. The protocols presented herein address these challenges through standardized sample preparation and cross-referencing with established marker genes.
Materials and Methods
Whole-Mount Immunofluorescence for Cardiac Crescent Stage Embryos
Embryo Collection and Fixation
- Timed Mating: House mice under standard conditions with a 12-hour light/dark cycle. Set up matings in the evening and check for vaginal plugs the following morning; noon on the day of plug detection is designated E0.5 [12] [6].
- Embryo Harvest: Sacrifice pregnant dams at E8.25 by CO₂ inhalation or according to institutional guidelines. Spray the abdomen with 70% ethanol before opening the body cavity to maintain sterility [6].
- Uterine Dissection: Remove the entire uterine horn and transfer to a 10 cm dish containing phosphate-buffered saline (PBS, pH 7.4). Sub-dissect the uterus by cutting the mesometrium between each deciduum [6].
- Embryo Isolation: Under a dissection microscope, use fine forceps (#5) to remove uterine tissue from the decidual tissue. Carefully slice the tip of the embryonic half of the deciduum and gently pinch to push the embryo out [12].
- Tissue Preparation: Dissect away extraembryonic tissues without damaging embryonic morphology. Transfer embryos to a 1.5 mL tube with fresh PBS and keep on ice [6].
- Fixation: Aspirate PBS and fix embryos with 4% paraformaldehyde (PFA) in PBS for 1 hour at room temperature. Embryos can be fixed overnight at 4°C for convenience [12].
Table 1: Key Reagents for Whole-Mount Immunofluorescence
| Reagent | Function | Concentration/Type |
|---|---|---|
| Paraformaldehyde (PFA) | Tissue fixation | 4% in PBS |
| Saponin | Permeabilization | 0.5% in blocking buffer |
| Bovine Serum Albumin (BSA) | Blocking non-specific binding | 1% in PBS |
| Triton X-100 | Wash solution component | 0.1% in PBS |
| n-Propyl gallate (nPG) | Anti-fade agent | 2% w/v in mounting media |
| Primary Antibodies | Target protein detection | Optimized dilution |
Immunofluorescence Staining
- Permeabilization and Blocking: Remove PBS and add 1 mL blocking buffer (0.5% saponin, 1% BSA in PBS). Incubate for at least 4 hours at room temperature or overnight at 4°C [6].
- Primary Antibody Incubation: Replace blocking buffer with primary antibody mixture diluted in blocking buffer. Incubate overnight at 4°C with gentle shaking [12]. Critical antibodies for cardiac crescent analysis include:
- Washing: Remove primary antibody and wash 3 times for 1 hour each with 0.1% Triton in PBS [6].
- Secondary Antibody Incubation: Add secondary antibodies diluted in blocking buffer. Incubate for 3 hours at room temperature or overnight at 4°C [12].
- Counterstaining: Incubate with DAPI (4',6-diamidino-2-phenylindole) in PBS for 10 minutes to label nuclei [6].
- Final Washes: Wash 2 times for 5 minutes each with 0.1% Triton in PBS [12].
Mounting and Imaging
- Mounting Preparation: Prepare microscope slides using double-stick tape or silicone spacers to create a chamber approximately 15-20 mm wide [6].
- Embryo Equilibration: Transfer embryos to anti-fade mounting media (2% w/v nPG, 90% glycerol, 1× PBS) and allow to equilibrate for at least 1 hour [12].
- Slide Preparation: Place a 15 μL drop of anti-fade media on the slide between tape spacers. Carefully transfer one embryo to the slide and orient appropriately [6].
- Coverslip Sealing: Gently lower a coverslip onto the spacers, avoiding bubble formation. Seal edges with clear nail polish to prevent drying [12].
- Confocal Microscopy: Image using a confocal microscope with appropriate laser lines for each fluorophore. Acquire z-stacks with sufficient resolution for three-dimensional reconstruction (typically 1-2 μm intervals) [6].
Single-Cell RNA Sequencing of Cardiac Progenitors
Single-Cell Dissociation
- Tissue Collection: Dissect cardiac crescent regions from E8.25 embryos under a stereomicroscope. Pool tissues from multiple embryos to ensure sufficient cell numbers [81].
- Tissue Dissociation: Minced tissues into small pieces (3×3×3 mm³ to 5×5×5 mm³) using fine scissors. Digest for 1 hour in DS-LT buffer (0.2 mg/ml CaCl₂, 5 μM MgCl₂, 0.2% BSA, 0.2 mg/ml Liberase in HBSS) at 37°C [81].
- Reaction Termination: Stop digestion by adding 3 mL fetal bovine serum (FBS) [81].
- Cell Strainer Filtration: Filter cell suspension through a 40-μm cell strainer to remove debris [81].
- Centrifugation: Centrifuge at 500 × g for 5 minutes at 4°C to pellet cells [81].
- Viability Assessment: Assess cell viability using Trypan Blue exclusion staining. Proceed only if viability exceeds 80% [81].
- Cell Resuspension: Resuspend cells in cell resuspension buffer (0.04% BSA in PBS) at appropriate concentration for scRNA-seq platform [81].
scRNA-seq Library Preparation
Several scRNA-seq platforms are available, each with advantages and limitations:
Plate-based Methods (Smart-seq2):
- Isolate single cells into 96-well or 384-well plates containing lysis buffer
- Perform reverse transcription and cDNA amplification in individual wells
- Advantages: Full-length transcript coverage, high sensitivity
- Disadvantages: Lower throughput, higher cost [77]
Droplet-based Methods (10× Genomics Chromium):
Microfluidic-based Methods (Fluidigm C1):
- Capture cells in integrated fluidic circuit chips
- Perform all reactions within microfluidic chambers
- Advantages: Visual confirmation of single cells, small reaction volumes
- Disadvantages: Limited to specific cell sizes, medium throughput [77]
For cardiac progenitors, we recommend either plate-based methods for comprehensive transcript coverage or droplet-based methods for larger cell numbers and population heterogeneity studies.
Sequencing and Data Processing
- Library Sequencing: Sequence libraries on an appropriate platform (Illumina, DNBSEQ-T7, etc.) with sufficient depth (typically 50,000 reads/cell) [81] [82].
- Quality Control: Process raw sequencing data through:
- Data Filtering: Apply quality control filters:
- Data Integration and Normalization: Use Seurat package in R for:
Correlative Analysis Framework
Marker Gene Correlation
- Identify Cluster Markers: For each scRNA-seq cluster, identify significantly enriched marker genes using Wilcoxon rank sum test [82].
- Protein-Gene Alignment: Compare WMIF protein expression patterns with expression of corresponding genes from scRNA-seq.
- Spatial Validation: Use WMIF to validate the spatial distribution of cell populations identified through scRNA-seq clustering.
Trajectory Analysis
- Pseudotemporal Ordering: Use Monocle 3 or similar tools to reconstruct differentiation trajectories [82] [79].
- Spatial Mapping: Correlate trajectory positions with spatial locations from WMIF.
- Lineage Validation: Confirm predicted lineage relationships through WMIF co-localization studies.
Signaling Pathway Analysis
- Ligand-Receptor Pair Identification: Predict active cell-cell communication using ligand-receptor pairing algorithms [83].
- Spatial Validation: Confirm predicted interactions through proximity analysis in WMIF data.
- Pathway Activity Mapping: Integrate pathway activity scores from scRNA-seq with spatial protein expression patterns.
Diagram 1: Experimental workflow for correlative WMIF and scRNA-seq analysis. The integrated approach enables spatial validation of transcriptomically-defined cell populations.
Expected Results and Data Interpretation
Spatial Mapping of Cardiac Progenitor Populations
When successfully integrated, WMIF and scRNA-seq data should enable precise spatial mapping of distinct cardiac progenitor populations. For example, scRNA-seq typically identifies separate clusters corresponding to FHF progenitors (characterized by Hcn4, Tbx5 expression) and SHF progenitors (characterized by Isl1, Fgf10 expression) [79]. WMIF validation should show spatially distinct localization of these populations within the cardiac crescent, with FHF progenitors typically located medially and SHF progenitors located laterally [6].
Table 2: Key Cardiac Progenitor Markers for Correlation Studies
| Cell Population | Transcriptomic Markers | Protein Markers | Spatial Location |
|---|---|---|---|
| First Heart Field (FHF) | Hcn4, Tbx5, Nppa | Nkx2-5, Tbx5 | Medial cardiac crescent |
| Second Heart Field (SHF) | Isl1, Fgf10, Tbx1 | Isl1, Fgf10 | Lateral cardiac crescent |
| Anterior SHF | Tbx1, Fgf8 | Tbx1, Fgf8 | Anterior region |
| Posterior SHF | Hoxb1, Ret | Hoxb1, Ret | Posterior region |
Validation of Novel Cell States
scRNA-seq frequently identifies novel or transient cell states that were previously unrecognized. For example, recent studies have identified a distinct population of Ndrg1-expressing myeloid dendritic cells and Cdkn1c-expressing dendritic cells that correlate with specific immune responses [84]. WMIF enables validation of such populations by confirming their spatial distribution and relative abundance within tissues. When correlating these findings, consider both the presence of marker genes and the overall transcriptional similarity to established populations.
Trajectory Analysis and Lineage Relationships
Pseudotemporal ordering of scRNA-seq data can reconstruct differentiation trajectories and predict lineage relationships [82] [79]. For cardiac progenitors, this typically reveals progression from mesodermal precursors to committed cardiomyocytes, with branching points corresponding to atrial/ventricular or FHF/SHF lineage decisions [79]. WMIF can validate these trajectories by showing spatial arrangement consistent with predicted developmental sequences and co-expression of markers from connected trajectory points.
Diagram 2: Retinoic acid signaling pathway in cardiac lineage commitment, showing key regulatory interactions identified through integrated analysis.
Troubleshooting and Optimization
WMIF-Specific Challenges
Poor Antibody Penetration:
- Problem: Incomplete staining in thick specimens
- Solution: Increase permeabilization time; use saponin instead of Triton X-100; extend antibody incubation times [6]
High Background Fluorescence:
- Problem: Non-specific antibody binding
- Solution: Optimize blocking conditions; titrate antibodies; increase wash stringency [12]
Photobleaching:
- Problem: Signal loss during imaging
- Solution: Use fresh anti-fade mounting media; minimize light exposure; image promptly after staining [6]
scRNA-seq-Specific Challenges
Low Cell Viability:
- Problem: Excessive cell death during dissociation
- Solution: Optimize enzyme concentration and digestion time; include viability-enhancing reagents [81]
Doublet Formation:
- Problem: Multiple cells in single partitions
- Solution: Optimize cell concentration; use doublet detection algorithms; employ doublet removal kits [81]
Batch Effects:
- Problem: Technical variation between samples
- Solution: Include batch correction in analysis; process samples in parallel; use multiplexing technologies [82]
Integration Challenges
Marker Discrepancies:
- Problem: Poor correlation between protein and RNA detection
- Solution: Consider post-transcriptional regulation; validate multiple markers per population; use RNAscope for spatial transcriptomics
Spatial Mapping Difficulties:
- Problem: Difficulty aligning scRNA-seq clusters with spatial locations
- Solution: Use computational spatial mapping tools; analyze continuous gradients rather than discrete clusters; incorporate multiple spatial landmarks
Applications in Drug Development and Disease Modeling
The integrated WMIF and scRNA-seq approach has significant applications in pharmaceutical development and disease modeling:
Congenital Heart Disease Modeling: By comparing wild-type and mutant embryos, researchers can identify specific alterations in progenitor population composition, spatial organization, and differentiation trajectories [81]. For example, studies of Cyp26b1 knockout mice have revealed altered retinoic acid signaling and disrupted ventricular compaction, modeling left ventricular non-compaction cardiomyopathy [81].
Drug Teratogenicity Screening: This approach can identify specific progenitor populations and developmental processes affected by teratogenic compounds, providing mechanistic insights beyond simple phenotypic assessment.
Stem Cell-Derived Cardiomyocyte Validation: For cardiac differentiation protocols using human pluripotent stem cells, integrated analysis can assess how closely in vitro-derived populations recapitulate in vivo development [79]. This is particularly valuable for optimizing differentiation protocols for regenerative medicine applications.
Personalized Medicine Approaches: Single-cell analysis of patient-derived cardiac cells can identify subpopulations with enhanced therapeutic potential [82]. For example, versican (VCAN) and integrin alpha 2 (ITGA2) have been identified as markers of a fibrotic subpopulation in cardiac-derived stromal cells with reduced reparative capacity [82].
The integration of WMIF and scRNA-seq provides a powerful multidimensional approach to investigate cardiac progenitor biology during early heart development. By combining spatial protein localization with comprehensive transcriptomic profiling, researchers can validate novel cell states, reconstruct lineage relationships, and uncover molecular mechanisms governing cardiac development and disease. The protocols outlined in this application note provide a standardized framework for implementing this integrated approach, with specific optimization for the unique challenges of cardiac crescent stage embryos. As both imaging and sequencing technologies continue to advance, this correlative methodology will become increasingly accessible and informative for basic research and therapeutic development.
Cross-Validation with Genetic Lineage Tracing and Fate Mapping Studies
Genetic lineage tracing and fate mapping are cornerstone techniques in developmental biology, enabling researchers to track the descendants of specific progenitor cells over time. In cardiac development research, these methods have been instrumental in elucidating the origins of diverse cardiac structures from distinct progenitor pools. However, the complexity of these biological systems and the technical challenges inherent in these approaches necessitate rigorous validation strategies. Cross-validation, a concept widely employed in statistical modeling and machine learning, provides a powerful framework for enhancing the reliability and interpretation of lineage tracing data. This application note details how cross-validation methodologies can be integrated with experimental techniques such as whole mount immunofluorescence (WMIF) to strengthen conclusions about cardiac lineage commitment, particularly during the critical cardiac crescent stage.
Quantitative Data from Key Lineage Tracing Studies
The following tables summarize quantitative findings from recent fate mapping studies that investigate the behavior and potential of cardiac progenitors. These data provide a benchmark for validating new observations and for understanding the expected contributions of different progenitor populations.
Table 1: Spatiotemporal Origins and Contributions of Cardiac Progenitors
| Progenitor Type | Origin/Timing | Key Molecular Markers | Major Cardiac Contributions | Reference |
|---|---|---|---|---|
| Early Uni-fated Progenitors | Early proximal mesoderm (E6 +7h) | Mesp1+, T/Bra+ | Predominantly left ventricle (LV) and atrioventricular canal (AVC) myocytes; forms cardiac crescent. | [85] |
| Late Uni-fated Progenitors | Late proximal mesoderm (E6 +21h) | T/Bra+ (downregulated in advanced stages) | Atrial myocytes; establishes the heart tube's Nr2f2+ inflow tract. | [85] |
| Multipotent Progenitors | Gastrulating mesoderm | Mesp1+, Hand1+ (at embryonic/extraembryonic boundary) | LV/AVC myocytes, pericardium, epicardium, and extraembryonic tissues. | [85] |
| Endocardial Progenitors | Gastrulating mesoderm | Mesp1+, Notch1+ | Endocardial lining of the mature heart. | [86] |
| Sca1+ Progenitor Cells | Adult mouse heart | Sca1+ | Involved in cardiac homeostasis and response to injury; potential role in regeneration. | [87] |
Table 2: Cell Behavior and Lineage Analysis from Live Imaging
| Cell Behavior / Lineage Metric | Experimental Finding | Implication for Cardiac Morphogenesis | Reference |
|---|---|---|---|
| Migration Coordination (Uni-fated Progeny) | Sister cell pairs from uni-fated progenitors showed more coordinated migration paths. | Suggests early fate restriction is associated with more deterministic cell movements. | [85] |
| Migration Dispersion (Multipotent Progeny) | Descendants of multipotent progenitors displayed greater dispersion and diverse migratory trajectories. | Highlights developmental plasticity and responsiveness to local environmental cues. | [85] |
| Migration Speed (ExEm Progenitors) | Progenitors for extraembryonic mesoderm (ExEm) exhibited the fastest and most dispersed migrations. | Indicates distinct migratory programs for different mesodermal lineages. | [85] |
| Regional Cell-Cycle Activity | In adult hearts, ~80% of cycling cardiomyocytes were located in the subendocardial muscle of the left ventricle. | Reveals a non-stochastic, regionally enriched pattern of cardiomyocyte turnover. | [88] |
| Clonal Analysis of Cycling Cardiomyocytes | A subset (~13%) of traced cycling cardiomyocytes in the ProTracer system underwent cell division. | Confirms that cell-cycle activity can lead to the generation of new cardiomyocytes in specific niches. | [88] |
Integrated Experimental & Computational Workflow
The reliability of fate mapping conclusions is significantly enhanced by integrating robust experimental protocols with computational cross-validation. The diagram below illustrates this synergistic workflow for validating lineage relationships in cardiac crescent stage embryos.
Detailed Experimental Protocols
Protocol: Whole-Mount Immunofluorescence for Cardiac Crescent Stage Embryos
This protocol is adapted for the quantitative analysis of progenitor cell populations within the cardiac crescent, allowing for 3D spatial reconstruction and fate mapping validation [26].
Sample Collection and Fixation:
- Dissect mouse embryos at E7.5-E8.0 (1-7 somites) in cold PBS.
- Fix embryos immediately in 4% Paraformaldehyde (PFA) in PBS for 30-45 minutes on ice.
- Wash 3 x 15 minutes in PBS at 4°C. Embryos can be stored in PBS with 0.02% Sodium Azide at 4°C for short-term storage.
Permeabilization and Blocking:
- Permeabilize embryos in 0.5% Triton X-100 in PBS (PBTx) for 30 minutes at room temperature (RT).
- Block non-specific antibody binding by incubating in a blocking solution (e.g., 10% normal serum from the secondary antibody host, 1% BSA, 0.1% PBTx) for 2-4 hours at RT or overnight at 4°C.
Antibody Staining:
- Incubate with primary antibodies diluted in blocking solution for 48-72 hours at 4°C with gentle agitation.
- Wash 6 x 1 hour in 0.1% PBTx at 4°C.
- Incubate with fluorophore-conjugated secondary antibodies (e.g., Alexa Fluor 488, 555, 647) and DAPI (for nuclear staining) diluted in blocking solution for 48 hours at 4°C in the dark.
- Wash 6 x 1 hour in 0.1% PBTx at 4°C in the dark. Perform a final wash in PBS overnight.
Imaging and 3D Reconstruction:
- Clear embryos using a compatible clearing agent (e.g., ScaleA2, FRUIT) if required for deeper imaging.
- Image using a confocal or light-sheet microscope. Acquire z-stacks with sufficient resolution to encompass the entire cardiac crescent.
- Use image analysis software (e.g., Imaris, Fiji/ImageJ) to create 3D reconstructions. Apply reference antibody channels (e.g., cTnnT) to mask the cardiac crescent structure for subsequent quantitative measurements of progenitor locations and intensities [26].
Protocol: K-Fold Cross-Validation for Lineage Data Analysis
This protocol provides a framework for applying cross-validation to quantitative data extracted from fate mapping experiments, such as cell counts and spatial positions, to test the robustness of a lineage classification model [89].
Data Preparation:
- From your 3D reconstructed images, compile a dataset where each row (record) represents a single tracked or quantified cell.
- Crucial Consideration: For subject-wise (embryo-wise) validation, ensure all cells from a single embryo are kept together in the same fold to prevent data leakage and over-optimistic performance estimates [89].
- Define features (X): spatial coordinates (X, Y, Z), fluorescence intensity values, progenitor marker expression levels, etc.
- Define the target (Y): the assigned fate or lineage (e.g., LVMyocyte, AtrialMyocyte, Endocardium).
Stratified K-Fold Splitting:
- Choose a value for K (commonly 5 or 10). Given the typical sample size in embryological studies (n=5-15 embryos), K=5 is a reasonable starting point.
- Randomly partition the embryos (not individual cells) into K folds of roughly equal size. Use stratified splitting to ensure that the proportion of each lineage fate (Y) is approximately equal across all folds, which is vital for rare lineages [89].
Model Training and Validation Loop:
- For each of the K iterations:
- Designate one fold as the validation set (also called test fold).
- Designate the remaining K-1 folds as the training set.
- Train your predictive model (e.g., Random Forest, Support Vector Machine) on the training set.
- Use the trained model to predict cell fates for the validation set.
- Calculate performance metrics (e.g., Accuracy, F1-Score) for that iteration.
- After K iterations, every embryo has been used for validation exactly once.
- For each of the K iterations:
Performance Estimation and Model Finalization:
- Aggregate the performance metrics from all K iterations to produce a robust estimate of model performance (e.g., mean ± standard deviation of accuracy).
- This performance estimate reflects how your model is expected to generalize to new, unseen embryonic samples.
- To create a final model for interpretation and hypothesis generation, train the model on the entire dataset.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Cardiac Lineage Tracing and Validation
| Reagent / Tool | Function / Application | Example Use in Context |
|---|---|---|
| Inducible Cre-lox System (e.g., CreERT2) | Enables temporal control over genetic recombination for fate mapping. | Tamoxifen administration at E6+7h vs. E6+21h to label early vs. late cardiac progenitors [85]. |
| Fluorescent Reporter Mice (e.g., cTnnT-2a-eGFP) | Labels specific cell lineages for live imaging and endpoint analysis. | Tracking cardiomyocyte differentiation and formation of the cardiac crescent in live embryos [85]. |
| AAV9 with Cell-Type Specific Tropism | Enables highly efficient and specific gene delivery to target cells in vivo. | Used to deliver Dre recombinase specifically to cardiomyocytes for the ProTracer system [88]. |
| Proliferation Tracing System (ProTracer) | Allows seamless, long-term genetic recording of cell-cycle activity in a specific lineage. | Fate mapping cycling cardiomyocytes in adult homeostasis and after injury [88]. |
| Reference Antibodies (e.g., cTnnT, DAPI) | Provides structural context and enables spatial normalization in quantitative WMIF. | Used to mask the cardiac crescent for quantitative measurements of progenitor locations [26]. |
| Light-Sheet Fluorescence Microscopy (LSFM) | Enables high-resolution, long-term live imaging of thick samples with low phototoxicity. | Tracking mesodermal cell migrations for up to 40 hours from gastrulation to heart tube formation [85]. |
Benchmarking Against Traditional Section-Based Immunofluorescence Methods
Within the context of whole mount immunofluorescence (IF) for cardiac crescent stage embryo research, benchmarking against traditional section-based methods is essential for advancing our understanding of early cardiac development. The cardiac crescent stage, occurring around embryonic day (E)7.5-E8.0 in mouse models, represents a critical period in early organogenesis characterized by the formation of mesoderm and endoderm lineages that contribute to heart development [34]. Traditional section-based IF has long been the standard for protein localization studies, but emerging whole mount approaches offer significant advantages for three-dimensional structural analysis. This application note provides a quantitative comparison of these methodologies, detailed protocols for implementation, and specific considerations for cardiac crescent stage research.
Performance Benchmarking: Quantitative Comparison
Technical Specifications and Performance Metrics
Table 1: Comparative analysis of section-based versus whole mount immunofluorescence for cardiac development studies
| Parameter | Section-Based IF | Whole Mount IF |
|---|---|---|
| Spatial Context | 2D visualization with potential for reconstruction | Native 3D architecture preservation |
| Tissue Processing | Thin sections (5-10µm) after embedding [74] | Complete embryo clearing required [90] |
| Compatibility with Cardiac Tissue | Standard protocols established | Requires specialized clearing methods [90] |
| Antibody Penetration | Complete with proper permeabilization | Limited by tissue size; requires extended incubation |
| Imaging Depth | Limited to section thickness | Hundreds of microns to millimeters with clearing |
| Multiplexing Capacity | High with sequential staining [91] | Moderate, limited by antibody penetration |
| Quantitative Potential | Linear correlation with mass spectrometry demonstrated (R²=0.88) [92] | Emerging, requires validation |
| Throughput | High for 2D analysis | Lower due to extended processing and imaging times |
| Cardiac Crescent Stage Applicability | Disrupts 3D spatial relationships | Preserves intact embryonic architecture [34] |
Algorithm Performance for Nuclear Segmentation
Accurate cell identification is crucial for analyzing cardiac development. Recent benchmarking of nuclear segmentation tools reveals significant performance differences:
Table 2: Performance benchmarking of nuclear segmentation algorithms for embryonic tissue analysis
| Algorithm | F1-Score at IoU 0.5 | Tissue Type Performance | Computational Requirements |
|---|---|---|---|
| Mesmer | 0.67 [93] | Consistent across tissue types | High, requires GPU for optimal performance |
| Cellpose | 0.65 [93] | Excellent for tonsil, variable elsewhere | Moderate, CPU/GPU compatible |
| StarDist | 0.63 [93] | Struggles in dense nuclear regions | Low, ~12x faster on CPU than Mesmer |
| QuPath | ~0.55 (estimated) [93] | Moderate across tissue types | Low, user-friendly interface |
| CellProfiler | ~0.45 (estimated) [93] | Limited accuracy | Low, pipeline-based |
Deep learning models consistently outperform classical algorithms, with Mesmer recommended for highest accuracy and StarDist for limited computational resources [93]. For cardiac crescent stage embryos, where nuclear density varies significantly across germ layers, these performance characteristics are particularly relevant.
Experimental Protocols
Traditional Section-Based Immunofluorescence Protocol
Fixation and Sectioning:
- Fix cardiac crescent stage embryos (E7.5-E8.0) in 4% paraformaldehyde for 2-4 hours at 4°C
- Dehydrate through ethanol series and embed in paraffin [74]
- Section at 5µm thickness using a microtome and mount on charged slides
- Deparaffinize with xylene (2 × 20 minutes) and rehydrate through graded ethanol to water [92]
Antigen Retrieval:
- Perform Heat-Induced Epitope Retrieval (HIER) using EDTA buffer (pH 8.0) at 97°C for 20 minutes [92]
- Cool slides for 30 minutes at room temperature
- Alternative: Protease-Induced Epitope Retrieval (PIER) using Proteinase K (1-10 µg/mL) for 5-15 minutes at 37°C [74]
Immunostaining:
- Block with 0.3% bovine serum albumin in Tris-buffered saline with 0.05% Tween for 30 minutes [92]
- Incubate with primary antibody cocktail overnight at 4°C
- Apply species-appropriate secondary antibodies conjugated to Alexa Fluor dyes (1:100 dilution) for 1 hour at room temperature [92]
- Counterstain with DAPI (0.5-1 µg/mL) and mount with anti-fade medium
Whole Mount Immunofluorescence Protocol for Cardiac Crescent Stage Embryos
Tissue Clearing and Preparation:
- Fix embryos in 4% PFA for 12-24 hours at 4°C with gentle agitation
- Select appropriate clearing method based on imaging requirements:
Immunostaining:
- Permeabilize with 0.5-1% Triton X-100 for 24-48 hours
- Block with 5% normal serum matching secondary antibody host species for 24 hours
- Incubate with primary antibodies for 3-7 days at 4°C with agitation
- Wash extensively (3-5 days with multiple buffer changes)
- Incubate with fluorophore-conjugated secondary antibodies for 3-5 days
- Clear using chosen method (CUBIC recommended for cardiac tissue) [90]
Imaging:
- Mount in clearing solution-matched imaging chambers
- Image with light-sheet or confocal microscope with long working distance objectives
Visualization and Signaling Pathways
The following diagram illustrates the key methodological decision points and their implications for cardiac crescent stage analysis:
Method Selection Workflow for Cardiac Crescent Stage Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential reagents and materials for cardiac crescent stage immunofluorescence
| Reagent/Material | Function | Specific Application Notes |
|---|---|---|
| D38B1 EGFR Antibody [92] | Target protein detection | Validated for quantitative IF; use at 1:100-1:500 dilution |
| Alexa Fluor-conjugated Secondaries [92] | Signal amplification | High quantum yield; minimal photobleaching |
| CUBIC Clearing Reagents [90] | Tissue transparency | 4M urea/50% sucrose; optimal for cardiac tissue |
| Cyanine 5-Tyramide [92] | Signal amplification | 1:50 dilution for 10 minutes; high sensitivity |
| ProLong Gold with DAPI [92] | Nuclear counterstain/mounting | Preserves fluorescence; anti-fade properties |
| ArgoFluor Dyes [91] | Multiplex panels | 18-plex capability; stable for >5 years at -20°C |
| Proteinase K [74] | Antigen retrieval | 1-10 µg/mL for 5-15 minutes; tissue-dependent |
| Bovine Serum Albumin [92] | Blocking agent | 0.3% in TBS-T; reduces non-specific binding |
Discussion and Implementation Recommendations
For cardiac crescent stage research, the choice between section-based and whole mount IF depends heavily on the specific research questions. Section-based methods provide superior quantitative capabilities and established workflows, with demonstrated linear correlation to mass spectrometry standards (R²=0.88 for EGFR) [92]. Whole mount approaches preserve the three-dimensional architecture essential for understanding spatial relationships in developing cardiac primordia.
Recent advances in tissue clearing methods, particularly hydrogel-based techniques like CLARITY and PACT, show promise for cardiac tissue [90]. However, solvent-based methods may be suboptimal due to high autofluorescence in heart tissue [90]. For segmentation and analysis, deep learning models like Mesmer provide the highest accuracy (F1-score 0.67) [93], essential for precise cell identification in dense embryonic tissues.
Implementation should consider the trade-off between spatial context preservation and quantitative rigor. For studies focusing on primordium determination zone characterization [34] or cross-germ-layer signaling [94], whole mount methods provide irreplaceable insights. For quantitative analysis of protein expression or high-plex subtyping, section-based approaches remain superior.
The emerging Orion platform, which combines high-plex IF with traditional H&E imaging on the same section [91], represents a promising intermediate approach, though its application to embryonic tissues requires further validation. As cardiac development research increasingly focuses on subtle gene dosage effects [94] and complex signaling networks [34], the appropriate selection and implementation of these benchmarking methods becomes increasingly critical.
Leveraging Digital Embryo Reconstructions for Spatial Context and Validation
The study of early organogenesis, particularly at the cardiac crescent stage, represents a critical phase in understanding embryonic development and congenital defects. Whole mount immunofluorescence (WMIF) has long been a cornerstone technique for visualizing progenitor cell populations within three-dimensional embryonic structures. However, traditional WMIF approaches, while providing exceptional cellular resolution, face inherent limitations in achieving comprehensive quantitative analysis of morphogenetic events across entire embryos. The emergence of spatial transcriptomic technologies and sophisticated computational reconstruction methods now enables the creation of full "digital embryos" at single-cell resolution, providing an unprecedented framework for spatial validation and contextual analysis. This protocol details the integration of traditional whole mount immunofluorescence with cutting-edge digital reconstruction platforms to establish a rigorous workflow for spatial investigation of cardiac crescent formation, offering researchers a powerful validation pipeline that bridges cellular visualization with transcriptome-wide spatial mapping.
Experimental Protocols
Whole Mount Immunofluorescence for Cardiac Crescent Stage Embryos
The following protocol, adapted from a detailed JoVE methodology, describes the essential steps for preparing, staining, and imaging cardiac crescent stage embryos (approximately E8.25) to visualize specific progenitor populations with minimal morphological disruption [12].
Day 1: Embryo Dissection and Fixation
- Timed Mating: Establish timed matings, designating noon on the day of vaginal plug detection as embryonic day (E) 0.5 [12].
- Embryo Harvest: Sacrifice the pregnant dam on the morning of E8.25 by CO2 inhalation or according to institutional regulations. Exact timing can be strain-dependent and should be determined empirically by morphology [12].
- Uterine Dissection: Remove the entire uterine horn and transfer to phosphate-buffered saline (PBS). Sub-dissect the uterus by cutting the mesometrium between each deciduum [12].
- Embryo Isolation: Under a dissection microscope, use fine forceps (#5) to remove uterine tissue and carefully extract embryos from the decidual tissue. Dissect away extraembryonic tissues as completely as possible without damaging embryonic morphology [12].
- Fixation: Transfer embryos to a 1.5 mL tube and fix with 4% paraformaldehyde (PFA) in PBS for 1 hour at room temperature. Embryos can alternatively be fixed overnight at 4°C [12].
- Storage: Rinse embryos three times with PBS and store at 4°C until immunofluorescence staining. Embryos can be safely stored in PBS at 4°C for several weeks [12].
Day 2: Immunofluorescence Staining
- Blocking: Remove PBS and add 1 mL of blocking buffer (0.5% saponin, 1% bovine serum albumin in PBS). Incubate for at least 4 hours at room temperature or overnight at 4°C [12].
- Primary Antibody Incubation: Replace blocking buffer with primary antibody mixture diluted in blocking buffer. Incubate overnight at 4°C. Critical antibodies for cardiac crescent analysis include NKX2-5 (reference stain) and lineage-specific markers such as FOXA2Cre:YFP [12].
- Washing: Remove primary antibodies and wash three times for 1 hour each with 0.1% Triton in PBS [12].
- Secondary Antibody Incubation: Apply secondary antibody mixture diluted in blocking buffer. Incubate for 3 hours at room temperature or overnight at 4°C [12].
- Counterstaining and Final Washes: Counterstain with DAPI in PBS for 10 minutes. Perform two final 5-minute washes with 0.1% Triton in PBS [12].
- Mounting Preparation: Suspend embryos slowly in anti-fade mounting media and allow to equilibrate for at least 1 hour before mounting [12].
Day 3: Mounting and Imaging
- Slide Preparation: Prepare microscope slides using double-stick tape or silicone spacers to create a chamber that protects embryo morphology during imaging [12].
- Embryo Orientation: Carefully position embryos in the mounting chamber to optimize exposure of the cardiac crescent region during confocal microscopy.
- Confocal Microscopy: Acquire high-resolution z-stack images using a confocal microscope. Ensure sufficient overlap between optical sections for accurate three-dimensional reconstruction [12].
Spatial Transcriptomics and 3D Digital Reconstruction
The following methodology outlines the process for generating spatial transcriptomic maps and reconstructing digital embryos, based on recent advances in the field [34] [95].
Tissue Processing and Sequencing
- Embryo Sectioning: Process E8.5-E9.0 embryos into serial sagittal sections (10-μm thickness) with approximately 20-30μm intervals between sections [95].
- Slide-seq Application: Utilize Slide-seq technology to generate transcriptome-wide gene expression data at 10-μm spatial resolution across all sections [95].
- Bead Sequencing: Recover high-quality beads with a median of approximately 1,800 transcripts and 1,200 genes per bead for sufficient spatial transcriptome coverage [95].
Computational Reconstruction and Analysis
- Cell State Mapping: Computationally map spatial transcriptomic beads to established single-cell references to assign cell states with spatial coordinates [95].
- 3D Reconstruction with sc3D: Apply the sc3D computational method to align individual spatial transcriptomic arrays into a coherent three-dimensional "virtual embryo" [95].
- Virtual In Situ Hybridization (vISH): Perform quantitative vISH analysis for over 27,000 genes across the reconstructed embryo, enabling investigation of gradient gene expression along any embryonic axis [95].
- Spatial Trajectory Analysis: Implement unsupervised spatial RNA velocity to map differentiation trajectories and identify progenitor field domains within the spatial context [95].
Spatial Transcriptomics Data Yield
Table 1: Spatial transcriptomic data characteristics from representative studies
| Parameter | E8.5 Embryo 1 | E8.5 Embryo 2 | E9.0 Embryo | Measurement Unit |
|---|---|---|---|---|
| Sections Analyzed | 15 | 17 | 26 | Sections per embryo |
| Section Interval | 30 | 30 | 20 | μm |
| High-Quality Beads | ~150,000 | ~170,000 | ~210,000 | Beads per embryo |
| Median Transcripts per Bead | 1,798 | 1,801 | 1,795 | Transcripts |
| Median Genes per Bead | 1,224 | 1,226 | 1,222 | Genes |
Tissue Volume Measurements in Reconstructed Embryos
Table 2: Quantitative tissue volume measurements from 3D digital reconstructions
| Tissue Structure | Volume Range | Developmental Stage | Reconstruction Method |
|---|---|---|---|
| Cardiac Crescent | 250-39,264 | E8.5-E9.0 | sc3D |
| Neural Tube | 15,200-28,450 | E8.5-E9.0 | sc3D |
| Somites | 8,150-12,680 | E8.5-E9.0 | sc3D |
| Forebrain Vesicle | 5,420-9,860 | E8.5-E9.0 | sc3D |
Signaling Pathway Visualization
Integrated Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Critical research reagents for integrated WMIF and spatial transcriptomics
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| NKX2-5 Antibody | Reference stain for cardiac crescent identification; essential for image segmentation | Recommended dilution: 1:200-1:500 in blocking buffer [12] |
| FOXA2Cre:YFP Reporter | Lineage tracing of cardiac progenitor populations | Enables fate mapping of specific cardiac lineages [12] |
| Saponin-based Blocking Buffer | Permeabilization and blocking for whole mount immunofluorescence | 0.5% saponin, 1% BSA in PBS [12] |
| Slide-seq Beads | Spatial transcriptomics capture; barcoded location identification | 10μm resolution, transcriptome-wide coverage [95] |
| sc3D Software | 3D reconstruction of serial spatial transcriptomic sections | Enables virtual embryo creation and vISH analysis [95] |
| Anti-fade Mounting Media | Preservation of fluorescence during imaging | 2% w/v n-Propyl gallate, 90% glycerol, 1x PBS [12] |
Advanced Analytical Applications
Primordium Determination Zone Characterization
Recent spatial transcriptomic analyses have identified a critical primordium determination zone (PDZ) that forms along the anterior embryonic-extraembryonic interface at E7.75 [34]. This specialized region serves as a signaling hub where coordinated cross-germ-layer communications contribute to cardiac primordium formation. The PDZ represents a previously uncharacterized regulatory domain that can be precisely mapped using digital embryo reconstructions, providing new insights into the earliest stages of heart field specification. Researchers can leverage this finding to investigate defective PDZ establishment in models of congenital heart disease, using the integrated WMIF and spatial transcriptomics workflow described herein to correlate cellular localization with transcriptional identity during cardiac crescent formation.
Spatial Gene Expression Localization Analysis
Digital embryo platforms enable quantitative assessment of regionalized gene expression through localization scoring, which computes genome-wide correlations between tissue volumes and densities of expressing cells [95]. This analytical approach identifies tissue-specific, regionalized genes with precise spatial restriction patterns. For cardiac development research, this has revealed genes such as Nppa, Tdgf1, Cck, and Sfrp5 that exhibit highly localized expression domains within the developing heart tube, marking specific developmental axes (anterior-posterior, dorsoventral, right-left) and delineating presumptive anatomical structures including primitive ventricles, atria, and outflow tract regions [95]. The integration of WMIF with these spatial transcriptomic maps allows direct visualization of protein localization alongside transcriptional activity, creating a comprehensive picture of cardiac crescent patterning.
The identification of the Juxta-Cardiac Field (JCF) represents a significant advancement in our understanding of mammalian heart development, moving beyond the classical first and second heart field (FHF, SHF) paradigm [96]. This progenitor population, marked by the expression of the basic helix-loop-helix transcription factor HAND1, contributes cells to both the heart (cardiomyocytes and epicardial cells) and the extraembryonic mesoderm [96]. The study of such novel niches is crucial for comprehending the full spectrum of congenital heart diseases and for advancing regenerative medicine strategies.
This Application Note details how whole-mount immunofluorescence (IF) microscopy, applied to cardiac crescent stage embryos, serves as a powerful tool for identifying and characterizing the JCF. We provide a consolidated protocol adapted from established methodologies [26] and contextualize it within a broader research framework that includes recent single-cell genomic insights, enabling researchers to visualize and quantify these multipotent progenitor populations within their native three-dimensional architecture.
Background: The Juxta-Cardiac Field in Context
Historical and Conceptual Framework of Cardiac Progenitor Fields
Heart development begins with the formation of the cardiac crescent, the first morphologically recognizable heart structure, at approximately embryonic day (E) 8.0 in the mouse (around day 20 post-fertilization in humans) [97]. The classical model describes two major progenitor populations:
- First Heart Field (FHF): Differentiates rapidly to form the initial linear heart tube, contributing predominantly to the left ventricle [97] [8].
- Second Heart Field (SHF): Remains proliferative and is added to the heart tube over time, contributing to the right ventricle, atria, and outflow tract [97] [8].
Recent high-resolution single-cell transcriptomic studies have revealed a more complex substructure within these broad fields, leading to the identification of the JCF [96]. This population overlaps the FHF and is characterized by a unique HAND1-low transcriptional signature that confers multipotency, enabling differentiation into both cardiomyocytes and epicardial cells [96].
Key Biological Insights and Functional Significance
The JCF is defined by a transcription factor network where the level of HAND1 expression acts as a fate switch:
- HAND1-low expression promotes development toward multipotent JCF progenitors capable of generating cardiomyocytes and epicardial cells [96].
- HAND1-high expression drives commitment toward extraembryonic mesoderm lineages [96].
This concentration-dependent mechanism highlights the critical role of precise transcriptional regulation in early lineage segregation. Furthermore, the JCF gives rise to the epicardium, the mesothelial envelope of the heart that is a essential source of cardiac fibroblasts, mural cells, and signals for myocardial growth [98]. Errors in these early fate decisions are implicated in congenital heart disease, underscoring the importance of robust models for studying these processes [96].
Integrated Experimental Protocol: Whole-Mount IF for JCF Analysis in Mouse Embryos
The following protocol is synthesized and adapted from published methodologies for the specific purpose of analyzing the JCF at the cardiac crescent stage [26].
Primary Reagents and Equipment
Table 1: Essential Reagents and Equipment for Whole-Mount IF
| Category | Specific Item | Function/Application |
|---|---|---|
| Fixation | 4% Paraformaldehyde (PFA) | Tissue preservation and antigen immobilization |
| Permeabilization | Phosphate-Buffered Saline (PBS) with 0.1% Triton X-100 (PBTx) | Enables antibody penetration into cells |
| Blocking | PBTx with 10% normal serum (species matches secondary antibody) | Reduces non-specific antibody binding |
| Primary Antibodies | Anti-HAND1 [96], Anti-cTnnT (Cardiac Troponin T) [97] [8], Anti-WT1 (Epicardial Marker) [98] | Label specific progenitor and differentiated cell populations |
| Secondary Antibodies | Fluorescently-labeled (e.g., Alexa Fluor) antibodies | Detection of primary antibodies |
| Mounting & Imaging | Confocal microscope with high-resolution objectives, Mounting medium with DAPI | 3D visualization and nuclear counterstaining |
Detailed Step-by-Step Procedure
Embryo Dissection and Staging (E7.5-E8.0):
- Sacrifice timed-pregnant mice according to institutional ethical guidelines. Noon on the day of a vaginal plug is considered E0.5 [33].
- Dissect uterine horns and transfer to ice-cold PBS. Carefully isolate individual embryos in cold PBS [33].
- Critical Step: Accurately stage embryos using morphological criteria such as head-fold progression and cardiac crescent height-to-width ratio [97]. This ensures analysis of precisely comparable developmental time points.
Fixation and Permeabilization:
- Fix embryos in 4% PFA for 2 hours at 4°C.
- Wash embryos 3x in PBS.
- Permeabilize embryos by incubating in 0.1% PBTx for 1-2 hours at room temperature. The duration may be optimized based on embryo size.
Blocking and Antibody Incubation:
- Incubate embryos in blocking solution (e.g., 10% normal donkey serum in PBTx) for a minimum of 2 hours at room temperature to minimize background.
- Incubate with primary antibodies (e.g., HAND1, cTnnT, WT1) diluted in blocking solution for 48-72 hours at 4°C with gentle agitation.
- Wash extensively with PBTx over 12-24 hours, with multiple solution changes.
- Incubate with fluorophore-conjugated secondary antibodies and DAPI (if not included in the mounting medium later) diluted in blocking solution for 24-48 hours at 4°C, protected from light.
- Perform final washes with PBTx over 12-24 hours.
Mounting and Imaging:
- Carefully orient the embryo in a drop of proprietary mounting medium on a microscope slide. Use a coverslip supported by small dots of vacuum grease or silicone sealant to prevent crushing the embryo.
- Image the specimens using a confocal microscope. Acquire Z-stacks with sufficient resolution and step-size to enable subsequent 3D reconstruction and quantitative analysis [26].
Quantitative Analysis of Progenitor Populations
Following image acquisition, quantitative data can be extracted:
- 3D Reconstruction: Use image processing software (e.g., Imaris, Fiji/ImageJ) to create three-dimensional models of the cardiac crescent [26].
- Progenitor Quantification: Successive masking techniques, guided by reference antibodies, allow for the measurement of specific areas within the cardiac crescent [26]. For instance, the HAND1-positive JCF domain can be quantified relative to the total cTnnT-positive cardiac crescent area or the DAPI-positive nuclear area.
- Spatial Analysis: The 3D spatial reconstruction enables analysis of the localization and organization of the JCF relative to the FHF, SHF, and emerging pericardial mesothelium [26] [99].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Key Reagents for JCF and Cardiac Progenitor Research
| Reagent / Tool | Type | Key Function in Research | Example Application |
|---|---|---|---|
| HAND1 Antibody | Primary Antibody | Marks the JCF progenitor population [96] | Identifying and quantifying JCF cells in cardiac crescent via IF |
| cTnnT Antibody | Primary Antibody | Labels differentiated cardiomyocytes [97] [8] | Demarcating the differentiated cardiac crescent in IF |
| WT1 Antibody | Primary Antibody | Labels epicardial and mesothelial lineages [98] | Tracing one of the fate potentials of the JCF |
| Nkx2-5 Reporter Mice | Genetic Model | Labels cardiac precursors and differentiated cardiomyocytes [8] | Live imaging and fate mapping of cardiac lineages |
| hand2:EGFP; myl7:DsRed Zebrafish | Transgenic Reporter | Visualizes myocardium and lateral hand2+ cells (potential pericardial precursors) [99] | Studying heart field separation and morphogenesis |
| hPSC-derived Epicardioids | In Vitro Model | Self-organizing organoids with epicardium and myocardium [98] | Modeling human epicardial development and JCF-derived lineages in vitro |
Integrated Data Analysis and Interpretation
Correlative Single-Cell Genomics
Whole-mount IF provides spatial context, but its power is magnified when correlated with single-cell RNA sequencing (scRNA-seq) data. scRNA-seq has been instrumental in defining the transcriptional signature of the JCF, revealing that HAND1-low progenitors express a network of genes, including specific HOX targets, that underpin their multipotency [96]. When analyzing IF results, co-localization of HAND1 with markers identified by scRNA-seq (e.g., specific surface receptors) can further validate and refine the identity of the progenitor population.
Signaling Pathways Governing JCF Fate
The specification of the JCF is regulated by key signaling pathways, particularly BMP and its interplay with HAND1. The following workflow summarizes the critical regulatory mechanism:
Discussion and Future Perspectives
The application of whole-mount IF to identify niches like the JCF provides a critical spatial dimension to transcriptomic data, enabling a more complete understanding of heart development. The HAND1-level-dependent mechanism illustrates how quantitative variations in transcription factor expression can dictate fundamental lineage choices [96].
Future research directions will likely involve:
- Live Imaging: Combining HAND1 reporters with live imaging to track the dynamic morphogenesis and fate decisions of JCF cells in real-time, building on approaches used for FHF/SHF imaging [8].
- Disease Modeling: Utilizing hPSC-derived epicardioids [98] with modulated HAND1 levels to model how errors in JCF specification contribute to congenital heart diseases.
- Regenerative Applications: Exploring whether the multipotent, propagatable state of HAND1-low progenitors [96] can be harnessed for cell therapy-based heart repair.
In conclusion, the integration of detailed spatial analysis via whole-mount IF with modern genomic tools has been pivotal in discovering and characterizing novel progenitor niches such as the JCF. The protocols and insights outlined here provide a roadmap for researchers to continue dissecting the complex cellular and molecular interactions that build the mammalian heart.
Congenital heart defects (CHDs) represent the most common type of birth defect, affecting nearly 1% of—or approximately 40,000—births annually in the United States [100]. As a leading cause of birth defect-associated infant mortality, CHDs impose significant healthcare burdens, with hospital costs exceeding $9.8 billion in 2019 alone [100]. Understanding the molecular and cellular mechanisms driving normal and aberrant heart development is therefore crucial for developing improved diagnostic and therapeutic strategies.
Whole-mount immunofluorescence (IF) has emerged as a powerful technique for investigating cardiac morphogenesis, particularly during early embryonic stages such as the cardiac crescent phase. This methodology enables three-dimensional spatial reconstruction of progenitor populations within the developing heart, providing unparalleled ability to analyze the localization and organization of specific cardiac progenitor populations during this critical phase of heart development [26]. When applied to disease modeling, whole-mount IF permits researchers to visualize how genetic mutations or environmental factors disrupt normal cardiac crescent formation, thereby illuminating fundamental mechanisms underlying CHD pathogenesis.
Quantitative Analysis of Cardiac Progenitor Populations
Whole-Mount Immunofluorescence Protocol for Cardiac Crescent Analysis
The following protocol describes a specialized approach for labeling, visualizing, and quantifying progenitor cell populations within the developing cardiac crescent of mouse embryos, enabling both cell- and tissue-level information to be obtained [26].
Materials and Reagents:
- Mouse embryos at cardiac crescent stage (approximately E7.5-E8.5)
- Fixative: 4% paraformaldehyde (PFA) in phosphate-buffered saline (PBS)
- Permeabilization solution: 0.5% Triton X-100 in PBS
- Blocking solution: 5% normal serum (species-matched to secondary antibody) in PBS
- Primary antibodies: Target-specific (e.g., anti-Nkx2-5, anti-Isl1, anti-Tbx1)
- Reference antibodies: For successive masking of cardiac crescent structures
- Fluorophore-conjugated secondary antibodies
- Mounting medium with anti-fade agents
- Phosphate-buffered saline (PBS)
Methodology:
- Embryo Collection and Fixation: Dissect mouse embryos at cardiac crescent stage in cold PBS. Fix embryos in 4% PFA for 2 hours at 4°C with gentle agitation.
- Permeabilization and Blocking: Wash embryos 3× in PBS, then permeabilize with 0.5% Triton X-100 for 30 minutes. Block non-specific binding sites with 5% normal serum for 2 hours at room temperature.
- Primary Antibody Incubation: Incubate embryos with primary antibodies diluted in blocking solution for 48-72 hours at 4°C with continuous agitation.
- Secondary Antibody Incubation: Wash embryos 5× in PBS over 8 hours, then incubate with fluorophore-conjugated secondary antibodies for 24-48 hours at 4°C.
- Mounting and Imaging: Wash embryos thoroughly and mount in anti-fade mounting medium. Image using confocal microscopy with appropriate laser lines and detection filters.
Table 1: Key Research Reagent Solutions for Cardiac Crescent Whole-Mount IF
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Fixatives | 4% Paraformaldehyde | Preserves tissue morphology and immobilizes antigens | Over-fixation can mask epitopes; requires optimization |
| Permeabilization Agents | Triton X-100, Tween-20 | Enables antibody penetration by dissolving membranes | Concentration critical for balance between access and preservation |
| Blocking Reagents | Normal serum, BSA, commercial protein-free blockers | Reduces non-specific antibody binding | Should match species of secondary antibody for optimal results |
| Primary Antibodies | Anti-Nkx2-5, Anti-Isl1, Anti-Tbx1 | Binds specifically to target proteins in cardiac progenitors | Validation for whole-mount applications essential |
| Secondary Antibodies | Fluorophore-conjugated (e.g., Alexa Fluor series) | Visualizes primary antibody binding | Multiple fluorophores enable multiplexing; must target primary host species |
Workflow Visualization
Figure 1: Experimental workflow for whole-mount immunofluorescence analysis of cardiac crescent stage embryos. The process extends over 4-6 days, with critical temperature control during antibody incubation steps.
Three-Dimensional Reconstruction and Quantitative Measurements
A key advantage of this whole-mount IF approach is the ability to perform three-dimensional spatial reconstruction of the cardiac crescent. Using confocal microscopy and image processing software, researchers can obtain volumetric data on specific progenitor populations [26]. The incorporation of reference antibodies enables successive masking of the cardiac crescent and subsequent quantitative measurements of areas within this structure. This spatial information is particularly valuable for understanding how progenitor populations are disrupted in CHD models, as the relative position and abundance of different progenitor subsets can be precisely quantified.
Clinical Epidemiology of Congenital Heart Defects
To contextualize the importance of CHD research, it is essential to understand the prevalence, survival statistics, and clinical burden of these conditions. The following tables summarize key epidemiological data.
Table 2: Prevalence and Survival Statistics for Congenital Heart Defects [100]
| Epidemiological Measure | Statistic | Additional Detail |
|---|---|---|
| Overall Prevalence | Nearly 1% of births (~40,000/year) | Most common birth defect |
| Critical CHD Prevalence | 1 in 4 babies with CHD | Require surgery or procedures in first year |
| Infant Survival (Non-critical CHD) | 97% to 1 year | - |
| Infant Survival (Critical CHD) | 75% to 1 year | Improved from 67% (1979-1993) to 83% (1994-2005) |
| Adolescent Survival (Non-critical CHD) | 95% to 18 years | - |
| Adolescent Survival (Critical CHD) | 69% to 18 years | - |
| Adult Survival (Overall CHD) | 81% to 35 years | 93% survival from age 1 to 35 years |
Table 3: Comorbidities and Healthcare Burden Associated with Congenital Heart Defects [100]
| Aspect | Statistic | Comparison Population |
|---|---|---|
| Children with Special Healthcare Needs | 60% | 20% of children without heart conditions |
| Adults with Disabilities | 40% (4 in 10) | Lower in general population |
| Cognitive Disabilities in Adults | Most common type | - |
| Receipt of Special Education Services | 50% more likely | Compared to children without birth defects |
| Hospital Costs (2019) | >$9.8 billion | United States |
Technical Considerations for Whole-Mount Immunofluorescence
Antibody Selection and Validation
The choice between monoclonal and polyclonal antibodies represents a critical decision point in experimental design. Monoclonal antibodies offer superior specificity and very low cross-reactivity, resulting in reduced background noise, but typically produce lower signals as only one antibody can bind per target molecule [23]. Polyclonal antibodies, recognizing multiple epitopes, provide higher signal amplification but carry greater risk of cross-reactivity with non-target proteins [23].
For whole-mount applications, indirect immunofluorescence is generally preferred over direct methods. While direct IF (with fluorophore-conjugated primary antibodies) offers simpler and faster staining protocols, it provides limited signal strength and fewer available commercial options [23] [74]. Indirect IF (using unlabeled primary antibodies followed by fluorophore-tagged secondary antibodies) enables signal amplification as multiple secondary antibodies can bind to a single primary antibody, significantly enhancing detection sensitivity [23].
Signal Amplification Strategies
Figure 2: Signal amplification in indirect immunofluorescence. Multiple fluorophore-conjugated secondary antibodies bind to each primary antibody, significantly enhancing detection sensitivity compared to direct methods.
For challenging targets or when working with precious samples, additional signal amplification strategies can be employed. The fluorophore-labeled Streptavidin-Biotin system represents one powerful approach, where multiple biotinylated secondary antibodies recognize a single primary antibody, followed by binding of fluorophore-labeled streptavidin to each biotin molecule [74]. This cascade effect can dramatically increase the fluorescence signal relative to standard indirect IF methods.
Image Acquisition and Analysis
Confocal microscopy is essential for high-quality whole-mount IF imaging, as it enables optical sectioning of thick specimens and collection of data for three-dimensional reconstruction [26]. When imaging the cardiac crescent, particular attention should be paid to:
- Spatial Resolution: Capture data at sufficient resolution to distinguish individual cells and subcellular structures
- Spectral Separation: Carefully select filter sets to minimize bleed-through between channels in multiplex experiments
- Z-stack Sampling: Ensure adequate sampling along the z-axis to properly represent three-dimensional structures
- Signal-to-Noise Optimization: Balance laser power, detector gain, and pixel dwell time to maximize information while minimizing photobleaching
For quantitative analysis, reference antibodies enable sequential masking of specific cardiac crescent subregions, facilitating precise measurement of progenitor population sizes, distribution patterns, and spatial relationships [26].
Applications in CHD Mechanism Investigation
Modeling Genetic CHD Subtypes
Whole-mount IF analysis of cardiac crescent stage embryos provides exceptional utility for investigating the cellular basis of various CHD subtypes. The HVSMR-2.0 dataset, comprising 60 cardiovascular MR scans from CHD patients, showcases the remarkable anatomical diversity observed in these conditions, including abnormalities such as double outlet right ventricle, single ventricle, and malpositioned great vessels [101]. By applying whole-mount IF to mouse models of these specific genetic conditions, researchers can trace anatomical abnormalities back to their origins in the cardiac crescent stage.
The protocol enables classification of anatomical malformations as mild, moderate, or severe based on deviation from normal cardiac crescent morphology [101]. Mild cases may show roughly normal anatomy with minor dilation, moderate cases demonstrate abnormal connectivity or septal defects, while severe cases exhibit fundamental disruptions such as heart malposition, single ventricle, or major reconstructive surgery resulting in highly abnormal anatomy [101].
Integration with Advanced Imaging Datasets
The whole-mount IF approach complements emerging imaging resources for CHD research. The HVSMR-2.0 dataset represents the first public resource for whole-heart segmentation from cardiovascular magnetic resonance images of CHD patients, specifically designed to include diverse heart defects and prior surgical interventions [101]. Correlation of embryonic progenitor population abnormalities (identified via whole-mount IF) with resulting cardiac phenotypes in mature structures (characterized via CMR) enables more complete understanding of disease progression.
This integrated approach is particularly valuable for studying the growing population of adults with CHD, who represent an increasing clinical challenge as life expectancy improves [101]. By understanding how early embryonic disruptions manifest in mature cardiac structures, researchers can develop improved prognostic indicators and targeted interventions.
Troubleshooting and Protocol Optimization
Successful application of whole-mount IF for CHD modeling requires careful attention to potential technical challenges:
- Antigen Preservation: Balance between adequate fixation to preserve morphology and minimal fixation to maintain antigenicity; consider antigen retrieval methods if needed
- Antibody Penetration: For larger embryos, extended incubation times or mild detergent treatments may improve antibody penetration
- Background Reduction: Optimize blocking conditions and antibody concentrations to minimize non-specific signal
- Multiplexing Limitations: The number of simultaneously detectable targets may be limited by antibody host species; careful experimental design can partially overcome this constraint
- Spatial Resolution: The size of antibody complexes (~30 nm) creates a linkage error that may be significant for superresolution applications
With proper optimization and validation, whole-mount immunofluorescence analysis of cardiac crescent stage embryos provides a powerful platform for elucidating the cellular and molecular mechanisms underlying congenital heart defects, contributing to improved diagnostic and therapeutic approaches for these common and clinically significant conditions.
Conclusion
Whole-mount immunofluorescence for cardiac crescent stage embryos represents a powerful methodology that bridges classical developmental biology with modern quantitative 3D imaging. When mastered, this technique provides unparalleled insights into the spatial organization and molecular signatures of cardiac progenitor populations during a critical window of heart development. The integration of optimized WMIF protocols with cutting-edge single-cell technologies and digital reconstruction platforms creates a robust framework for validating findings and exploring new biological questions. Future directions will focus on increasing multiplexing capabilities, enhancing computational analysis for high-throughput screening, and applying these integrated approaches to human stem cell-derived models and congenital heart disease research, ultimately accelerating the development of diagnostic and therapeutic strategies for cardiac malformations.
References
- 1. Cardiac construction—Recent advances in morphological ... [https://www.sciencedirect.com/science/article/abs/pii/S0070215324000267]
- 2. The molecular mechanisms of cardiac development and ... [https://www.nature.com/articles/s41392-024-02069-8]
- 3. Quantitative computerized analysis demonstrates strongly ... [https://elifesciences.org/reviewed-preprints/108559v1]
- 4. Optimized protocol for whole-mount RNA fluorescent in situ ... [https://www.sciencedirect.com/science/article/pii/S2666166723005701]
- 5. Formation of the Heart: Defining Cardiomyocyte ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10188409/]
- 6. Quantitative Whole-mount Immunofluorescence Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6475905/]
- 7. At early stages of heart development, the first and second ... [https://www.sciencedirect.com/science/article/pii/S0012160625000211]
- 8. Live imaging of heart tube development in mouse reveals ... [https://elifesciences.org/articles/30668]
- 9. Embryonic Heart Progenitors and Cardiogenesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3784811/]
- 10. Retinoic acid signaling modulation guides in vitro ... [https://www.nature.com/articles/s41467-023-36764-x]
- 11. Single-cell morphometrics reveals T-box gene-dependent ... [https://www.nature.com/articles/s41467-024-53612-8]
- 12. Quantitative Whole-mount Immunofluorescence Analysis of ... [https://www.jove.com/t/56446/quantitative-whole-mount-immunofluorescence-analysis-cardiac]
- 13. Nkx2-5 Lineage Tracing Visualizes the Distribution of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3943338/]
- 14. Foxa2 identifies a cardiac progenitor population ... - Nature [https://www.nature.com/articles/ncomms14428]
- 15. Article GFRA2 Identifies Cardiac Progenitors and Mediates ... [https://www.sciencedirect.com/science/article/pii/S221112471630804X]
- 16. Identification of cardiac progenitors that survive in the ... [https://www.nature.com/articles/srep41318]
- 17. Cardiomyocyte Differentiation from Mouse Embryonic Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814988/]
- 18. An Optimized and Simplified System of Mouse Embryonic ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0093033]
- 19. Quantitative computerized analysis demonstrates strongly ... [https://elifesciences.org/reviewed-preprints/108559]
- 20. Primitive streak formation in mice is preceded by localized ... [https://www.sciencedirect.com/science/article/pii/S0012160605006196]
- 21. Synthetic embryology of the human heart - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11810959/]
- 22. 9 Important Things to Consider for Immunofluorescent Labels [https://visikol.com/blog/2022/10/27/9-important-things-to-consider-for-immunofluorescent-labeling/]
- 23. How Immunofluorescence (IF) labeling works! [https://abberior.rocks/knowledge-base/let-the-cells-shine/]
- 24. Immunofluorescence Staining | A Typical Workflow [https://ibidi.com/content/365-immunofluorescence-staining-a-typical-workflow]
- 25. Whole Mount Imaging [https://visikol.com/blog/2023/10/16/whole-mount-imaging/]
- 26. Quantitative Whole-mount Immunofluorescence Analysis of ... [https://pubmed.ncbi.nlm.nih.gov/29053691/]
- 27. Quantitative whole-mount immunofluorescence analysis of cardiac ... [https://scholars.mssm.edu/en/publications/quantitative-whole-mount-immunofluorescence-analysis-of-cardiac-p-2]
- 28. Whole Mount Imaging Methodology to Visualize and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11623403/]
- 29. A quantitative pipeline for whole-mount deep imaging and ... [https://elifesciences.org/reviewed-preprints/107154]
- 30. Heart Development - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/heart-development]
- 31. A single-cell time-lapse of mouse prenatal development ... [https://www.nature.com/articles/s41586-024-07069-w]
- 32. Mapping cells through time and space with moscot [https://www.nature.com/articles/s41586-024-08453-2]
- 33. Analysis of Cardiac Chamber Development During Mouse ... [https://www.jove.com/t/59413/analysis-cardiac-chamber-development-during-mouse-embryogenesis-using]
- 34. Digital reconstruction of full embryos during early mouse ... [https://www.sciencedirect.com/science/article/pii/S0092867425006221]
- 35. A single-embryo, single-cell time-resolved model for ... [https://www.sciencedirect.com/science/article/pii/S0092867421004396]
- 36. Ten Approaches That Improve Immunostaining: A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8836139/]
- 37. Fixation and Permeabilization in Immunocytochemistry [https://www.bio-techne.com/applications/imaging/immunocytochemistry/fixation-and-permeabilization-in-icc-if]
- 38. Guide to Fixation and Permeabilization [https://fluorofinder.com/guide-to-fixation-and-permeabilization/]
- 39. Intracellular Flow Cytometry Staining Protocol [https://www.ptglab.com/news/blog/intracellular-flow-cytometry-staining-protocol/?srsltid=AfmBOorT7_tcpWamkFcwEGDMLgkYleGbVN1mgi7snqx74dvnLt7BbzfC]
- 40. Tissue clearing and imaging methods for cardiovascular ... [https://www.sciencedirect.com/science/article/pii/S2589004221003552]
- 41. Glycosylated Cell Surface Markers for the Isolation of Human Cardiac ... [https://pubmed.ncbi.nlm.nih.gov/28891400/]
- 42. Isolation and Functional Characterization of Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2947085/]
- 43. Neural Progenitor Cell Marker (CXCR4, Nestin, PDGFR...) | Abcam [https://www.abcam.com/en-us/products/antibody-panels/neural-progenitor-cell-marker-cxcr4-nestin-pdgfr-sox2-vimentin-doublecortin-antibody-panel-ab263461]
- 44. Early coordination of cell migration and cardiac fate ... [https://link.springer.com/article/10.1038/s44318-025-00441-0]
- 45. A simple and fast optical clearing method for whole-mount ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342960/]
- 46. Protocol for immunofluorescent staining, high-resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212140/]
- 47. IHC staining protocol for whole mount samples [https://www.abcam.com/en-us/technical-resources/protocols/wholemount-staining-for-ihc]
- 48. NyquistRate [https://svi.nl/NyquistRate]
- 49. A pipeline for multidimensional confocal analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7052579/]
- 50. Confocal canvas size, Nyquist sampling and FOV - Microforum [https://forum.microlist.org/t/confocal-canvas-size-nyquist-sampling-and-fov/2248]
- 51. Introduction To Spinning Disk Confocal Microscopy [https://www.teledynevisionsolutions.com/learn/learning-center/scientific-imaging/introduction-to-spinning-disk-confocal-microscopy/]
- 52. Automated Segmentation of Light-Sheet Fluorescent ... [https://www.nature.com/articles/s41598-017-09152-x]
- 53. Deep learning enables automated volumetric assessments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6826023/]
- 54. A pictorial account of the human embryonic heart between ... [https://www.nature.com/articles/s42003-022-03153-x]
- 55. MicroBundleCompute: Automated segmentation, tracking, and ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0298863]
- 56. ICC/IHC Non-Specific Binding / Staining Prevention Protocol [https://www.rndsystems.com/resources/protocols/preventing-non-specific-staining]
- 57. 5 Sources Of Non-specific Staining And Background In IHC ... [https://vectorlabs.com/blog/5-sources-of-non-specific-staining-and-background-in-ihc-and-if/?srsltid=AfmBOooaeHKEUeY78TZ0-5ukvSk9HIuZL2l1sEEDt-mHmFpoSygaQNrl]
- 58. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 59. Deriving high contrast fluorescence microscopy images ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8515974/]
- 60. The effect of chemical fixation with paraformaldehyde ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11837135/]
- 61. An evaluation of fixation methods: Spatial and ... [https://www.sciencedirect.com/science/article/pii/S0924203116302995]
- 62. Effects of Acetone, Methanol, or Paraformaldehyde on ... [https://www.semanticscholar.org/paper/Effects-of-Acetone%2C-Methanol%2C-or-Paraformaldehyde-Hoetelmans-Prins/2a49856f4d59f737b94b99490d0d10036e759a9a]
- 63. Improved whole-mount immunofluorescence protocol for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11317099/]
- 64. Comparison of Fixation Methods for Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3201123/]
- 65. Preparation of developing Xenopus muscle for sarcomeric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3871942/]
- 66. Optimization of fixation methods for observation of bacterial ... [https://link.springer.com/article/10.1007/s00253-011-3551-5]
- 67. Effect of tissue fixation on the optical properties of structural ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-14-8-3988]
- 68. Immunofluorescence: Antibody Dilution and Incubation ... [https://blog.cellsignal.com/successful-immunofluorescence-antibody-dilution-and-incubation]
- 69. Optimized immunofluorescence staining protocol for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8233161/]
- 70. Antibodies 101: Introduction to Immunofluorescence [https://blog.addgene.org/introduction-to-immunofluorescence]
- 71. Tissue Clearing Methods and Applications for Fluorescence Imaging- Oxford Instruments [https://andor.oxinst.com/learning/view/article/overview-of-tissue-clearing-methods-and-applications]
- 72. Physical and chemical mechanisms of tissue optical clearing - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2589004221001462]
- 73. Tutorial: practical considerations for tissue clearing and imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10542857/]
- 74. An introduction to Performing Immunofluorescence Staining [https://pmc.ncbi.nlm.nih.gov/articles/PMC6918834/]
- 75. Introduction to Sample Preparation: Immunofluorescence [https://microscopy.duke.edu/guides/intro-sample-prep-immunofluorescence]
- 76. Principles of Advanced Flow Cytometry: A Practical Guide [https://pmc.ncbi.nlm.nih.gov/articles/PMC10802916/]
- 77. Single-cell RNA sequencing in cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7528042/]
- 78. Single Cell RNA Sequencing Approaches to Cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8434959/]
- 79. Cardiac differentiation roadmap for analysis of plasticity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960529/]
- 80. Single cell RNA sequencing approaches to cardiac ... [https://www.rna-seqblog.com/single-cell-rna-sequencing-approaches-to-cardiac-development-and-congenital-heart-disease/]
- 81. Single-cell RNA sequencing dataset of hearts from wild ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12241566/]
- 82. Single-Cell RNA Sequencing Reveals Distinct Cardiac- ... [https://www.mdpi.com/2308-3425/9/11/374]
- 83. Enhanced single-cell RNA-seq workflow reveals coronary ... [https://www.sciencedirect.com/science/article/pii/S0021915021014647]
- 84. Machine Learning-Based Single Cell and Integrative ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.690470/full]
- 85. Early coordination of cell migration and cardiac fate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170898/]
- 86. Decoding congenital heart disease: a multi-omic ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1659884/full]
- 87. Fate Mapping of Sca1+ Cardiac Progenitor Cells in the ... [https://pubmed.ncbi.nlm.nih.gov/30566021/]
- 88. Cell proliferation fate mapping reveals regional ... [https://www.nature.com/articles/s41467-021-25933-5]
- 89. Practical Considerations and Applied Examples of Cross - Validation ... [https://ai.jmir.org/2023/1/e49023/]
- 90. Tissue clearing and imaging methods for cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8086021/]
- 91. High-plex immunofluorescence imaging and traditional ... [https://www.nature.com/articles/s43018-023-00576-1]
- 92. Proof of the Quantitative Potential of Immunofluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5334147/]
- 93. Quantitative benchmarking of nuclear segmentation ... [https://www.nature.com/articles/s42003-025-08184-8]
- 94. Single-nuclei multiomics analysis identifies abnormal ... [https://www.nature.com/articles/s41467-025-62208-9]
- 95. Spatiotemporal transcriptomic maps of whole mouse ... [https://www.nature.com/articles/s41588-023-01435-6]
- 96. HAND1 level controls the specification of multipotent cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12048643/]
- 97. Early heart development: examining the dynamics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11668286/]
- 98. Epicardioid single-cell genomics uncovers principles of ... [https://www.nature.com/articles/s41587-023-01718-7]
- 99. The pericardium forms as a distinct structure during heart ... [https://www.nature.com/articles/s41467-025-63599-5]
- 100. and Statistics | Congenital Data (CHDs) | CDC Heart Defects [https://www.cdc.gov/heart-defects/data/index.html]
- 101. HVSMR-2.0: A 3D cardiovascular MR dataset for whole- heart ... [https://www.nature.com/articles/s41597-024-03469-9?error=cookies_not_supported&code=accba475-e369-482f-be30-bf1e3556ada6]