Modified vs. Conventional Warming Protocols in ART: Impact on Embryo Viability and Clinical Outcomes
This article synthesizes current evidence on warming protocols for vitrified oocytes and embryos in Assisted Reproductive Technology (ART).
Modified vs. Conventional Warming Protocols in ART: Impact on Embryo Viability and Clinical Outcomes
Abstract
This article synthesizes current evidence on warming protocols for vitrified oocytes and embryos in Assisted Reproductive Technology (ART). It explores the foundational principles of cryopreservation, details the methodological shifts from conventional multi-step to simplified one-step warming, and analyzes troubleshooting for cell-type-specific sensitivities. A critical comparative analysis validates the non-inferiority or superiority of modified protocols, highlighting significant improvements in blastocyst formation and ongoing pregnancy rates for oocytes, while demonstrating maintained efficacy with enhanced efficiency for embryos. This review provides researchers, scientists, and drug development professionals with a comprehensive evidence base to inform laboratory practice and the development of standardized, optimized warming strategies.
The Science of Vitrification and Warming: Principles and Evolution in ART
Core Principles of Vitrification and the Critical Warming Phase
Vitrification has revolutionized the cryopreservation of oocytes, embryos, and reproductive tissues by achieving a glass-like state that avoids damaging ice crystal formation. While the core principles of vitrification are well-established, recent research has focused on optimizing the warming phase—a critical determinant of cryopreservation success. This review examines the fundamental biophysical principles governing vitrification and warming, with particular emphasis on emerging evidence comparing conventional and modified warming protocols. We analyze experimental data from recent clinical studies evaluating warming rate impacts on survival, blastocyst formation, and pregnancy outcomes, providing researchers and clinicians with evidence-based guidance for protocol selection and implementation.
Fundamental Principles of Vitrification and Warming
Vitrification represents a fundamental advancement in cryopreservation technology, enabling the preservation of oocytes, embryos, and reproductive tissues through the formation of a glass-like amorphous solid rather than crystalline ice [1]. This process depends on four critical variables: cooling rate, warming rate, viscosity, and sample volume [1]. Successful vitrification requires cooling rates typically exceeding -10,000°C/min when using open microvolume devices, rapidly solidifying the cell so that intracellular water does not form damaging ice crystals [1].
The warming phase is equally, if not more, critical than the cooling phase for cell survival and function [1]. During warming, the critical warming rate (CWR) must be achieved to prevent devitrification—the formation of ice crystals during the warming process from the glassy state [2]. The CWR is often one to two orders of magnitude higher than the critical cooling rate (CCR) for the same cryoprotective agent (CPA) solution [2]. For example, while the CCR for VS55 (8.4 M CPA cocktail) is 2.5°C/min, its CWR is 50°C/min [2]. This differential exists because slow warming provides time for small ice crystals to grow through recrystallization, causing irreversible cellular damage [1].
The relationship between CPA concentration and required warming rates follows a predictable pattern: lower CPA concentrations require significantly higher warming rates to avoid ice formation [2]. This presents a particular challenge for tissue and organ cryopreservation, where CPAs may not fully equilibrate throughout the sample, creating regions with effectively lower CPA concentrations that demand exceptionally high warming rates [2].
Conventional vs. Modified Warming Protocols: Experimental Comparisons
Protocol Methodologies
Conventional Warming Protocol (CWP) typically involves a multi-step dilution process after rapid warming to 37°C. In oocyte cryopreservation, this includes:
- Thawing Solution (TS): 1 minute incubation at 37°C to prevent ice formation and maintain structural integrity
- Dilution Solution (DS): 3-minute incubation at room temperature
- Wash Solution (WS): 5-6 minute incubation at room temperature This gradient dilution approach aims to minimize osmotic stress during cryoprotectant removal [3].
Modified Warming Protocol (MWP) simplifies this process into an ultrafast, single-step approach:
- Elimination of DS and WS steps
- Single incubation in TS for 1 minute at 37°C
- Direct transfer to culture media This protocol significantly reduces total warming time and potential osmotic stress [3].
Universal Warming Protocol (UWP) represents a further development, designed to be compatible with different devitrification media from various suppliers, allowing flexibility in laboratory workflows while maintaining efficacy [4] [5].
Comparative Experimental Data
Table 1: Outcomes of Conventional vs. Modified Warming Protocols for Vitrified Oocytes
| Parameter | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Control Group |
|---|---|---|---|
| Survival Rate | 93.7% (7967/8506) | 93.9% (920/980) | - |
| Degeneration Rate (post-ICSI) | 3.4% (268/7967) | 2.7% (25/920) | 2.8% (60/2106) |
| Normal Fertilization | 79.5% | 79.6% | 83.0% |
| Blastocyst Formation | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | - |
Data adapted from [3]
Recent multicenter studies have further validated the universal warming approach. When applied to vitrified donor oocytes across three centers using different devitrification media, survival rates ranged from 85-94%, with no statistically significant differences in fertilization rates (73-77%), cleavage rates (80-83%), blastulation rates (52-58%), or clinical pregnancy rates (13-60% depending on transfer day) between media types [4].
Statistical Analysis
Multivariate analysis of the comparative data demonstrates a significant positive association between MWP and key outcome parameters. For usable blastocyst formation, the adjusted incidence rate ratio was 1.423 (95% CI = 1.268 to 1.597, P < 0.001), while for ongoing pregnancy/live birth, the adjusted odds ratio was 1.899 (95% CI = 1.002 to 3.6, P < 0.05) [3]. These results indicate that the modified warming protocol provides statistically significant improvements in both laboratory and clinical outcomes compared to conventional approaches.
Measurement Techniques for Critical Warming Rates
Determining critical warming rates requires sophisticated instrumentation capable of both achieving rapid temperature changes and detecting ice formation. The following table summarizes the primary methods used in contemporary research:
Table 2: Techniques for Measuring Critical Warming Rates in Vitrification Research
| Method | Maximum Achievable Rates | Ice Formation Detection | Applications |
|---|---|---|---|
| Differential Scanning Calorimetry (DSC) | 160°C/min (2.67°C/s) | Calorimetry measurements | Quantifying heat of ice crystallization dynamically |
| Plunge Cooling/Warming | 10ⵠ°C/s | Visual inspection, X-ray diffraction | Assessing glass/crystal transition |
| Fast Scanning Calorimetry | 10âµ~10ⶠ°C/s | Calorimetry measurements | Ultra-rapid warming rate studies |
| Laser Calorimetry | Cooling: 10ⵠ°C/s; Heating: 10ⷠ°C/s | High-speed video microscopy | Precise warming rate control via laser absorption |
Data compiled from [2]
The definition of CWR varies slightly between measurement techniques. In DSC studies, the CWR is typically defined as the warming rate required to confine crystallization to approximately 0.2-0.5% of the sample mass, often corresponding to Tm/Td = 1.05 (where Tm is melting temperature and Td is devitrification temperature) [2]. For plunge warming studies with visual inspection, CWR represents the minimum rate at which samples remain transparent without opacification indicating ice formation [2].
Research Reagent Solutions and Materials
Table 3: Essential Research Materials for Vitrification and Warming Studies
| Category | Specific Examples | Function |
|---|---|---|
| Vitrification Media | Kitazato media (Japan), Irvine media (Fujifilm Irvine Scientific, USA), RapidWarm Omni media (Vitrolife, Sweden) | Provide cryoprotectant solutions for vitrification process |
| Permeable Cryoprotectants | Ethylene glycol, DMSO, PROH (1,2-propanediol) | Penetrate cell membrane, depress freezing point |
| Non-Permeable Cryoprotectants | Sucrose, trehalose | Create osmotic gradient, promote dehydration |
| Cryopreservation Devices | Cryotop, Open Pulled Straw (OPS), Cryoloop, microSecure | Enable ultra-rapid cooling through minimal volume design |
| Warming Solutions | Thawing Solution (TS), Dilution Solution (DS), Wash Solution (WS) | Remove cryoprotectants while minimizing osmotic shock |
Information compiled from [4] [1] [5]
Conceptual Framework and Experimental Workflows
Critical Warming Rate Determination Workflow
Protocol Comparison and Outcomes Relationship
The critical warming phase represents a pivotal determinant of success in vitrification-based cryopreservation. While conventional warming protocols have established a foundation for safe and effective cryopreservation, emerging evidence demonstrates that modified and universal warming protocols offer significant advantages in both laboratory efficiency and clinical outcomes. The simplified, rapid warming approaches achieve comparable survival rates while significantly enhancing blastocyst formation potential and ongoing pregnancy rates.
The development of universal warming protocols that maintain efficacy across different media systems provides laboratories with unprecedented flexibility and standardization potential. As the field advances, further research is needed to optimize warming protocols for specialized applications such as ovarian tissue and organ cryopreservation, where CPA equilibration challenges may demand even more sophisticated warming strategies. The consistent demonstration that simplified, rapid warming protocols yield superior outcomes suggests that the field is moving toward a new standard that prioritizes both practical efficiency and enhanced clinical results.
The field of assisted reproductive technology (ART) has undergone a significant evolution in cryopreservation techniques, particularly in the warming protocols used for vitrified oocytes and embryos. For years, conventional multi-step warming protocols represented the standard of care, employing sequential dilution steps at specific temperatures to remove cryoprotectants while minimizing osmotic stress. These protocols, while effective, were complex and time-intensive, requiring precise laboratory execution [3].
Recent research has focused on simplifying these procedures into modified, faster protocols that reduce processing time while aiming to maintain or even improve developmental outcomes. This transition from conventional to simplified warming represents a paradigm shift in ART laboratory practice, driven by both clinical outcomes and workflow efficiency considerations. The modified protocols challenge traditional assumptions about the necessity of gradual cryoprotectant dilution, particularly for blastocysts which were historically considered less susceptible to osmotic stress than oocytes [3].
This comparison guide examines the historical context and experimental evidence supporting this transition, providing researchers and clinicians with objective data on the performance of conventional versus modified warming protocols across different cell types and developmental stages.
Comparative Analysis of Warming Protocol Outcomes
Quantitative Comparison of Oocyte Outcomes
Table 1: Laboratory and clinical outcomes of fresh and vitrified-warmed oocytes using different warming protocols
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | - |
| Degeneration Rate Post-ICSI | 3.4% | 2.7% | 2.8% |
| Normal Fertilization | 79.5% | 79.6% | 83.0% |
| Abnormal Fertilization | 10.1% | 9.1% | 3.3% |
| Blastocyst Formation | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | - |
Data adapted from a retrospective cohort study of 13,103 donor oocytes (Lee Women's Hospital, Taiwan, 2019-2024) [3]
The data demonstrates that the modified warming protocol yields significantly improved outcomes for blastocyst formation (77.3% vs. 57.5%) and usable blastocyst formation (51.4% vs. 35.4%) compared to conventional protocols. Multivariate analysis confirmed a positive association between MWP and usable blastocyst formation (adjusted incidence rate ratio = 1.423, 95% CI = 1.268 to 1.597, P < 0.001) as well as ongoing pregnancy/live birth (adjusted odds ratio = 1.899, 95% CI = 1.002 to 3.6, P < 0.05) [3].
Quantitative Comparison of Blastocyst Outcomes
Table 2: Comparative outcomes of different warming protocols for vitrified-warmed blastocysts
| Outcome Measure | Conventional Warming Protocol | Simplified One-Step Protocol |
|---|---|---|
| Survival Rate | 96.1% (Kit 1) | 97.3% (Kit 2) |
| Clinical Pregnancy Rate | 35.4% | 34.1% |
| Live Birth Rate | 30.9% | 30.5% |
| Singleton Birth Weight | 3413 ± 571 g | 3410 ± 528 g |
| Gestational Age | 38.8 ± 2.5 weeks | 38.8 ± 2.0 weeks |
| Day 5 Blastocyst Live Birth Rate | 36.1% | 36.1% |
| Day 6 Blastocyst Live Birth Rate | 25.4% | 23.5% |
Data adapted from comparative studies of vitrification kits with different warming protocols [6] [7]
Studies comparing blastocyst outcomes between conventional and simplified warming protocols show comparable results across all key metrics. A prospective cohort study of 802 cycles found no significant differences in survival, pregnancy, implantation, ongoing pregnancy, or live birth rates between standard warming and one-step fast-warming protocols [6]. Similarly, research comparing different commercial kits with varying warming procedures demonstrated no statistically significant differences in clinical outcomes, suggesting that blastocysts may adapt well to simplified warming approaches [7].
Experimental Protocols and Methodologies
Conventional Warming Protocol (CWP) for Oocytes
The conventional warming protocol follows a multi-step dilution process designed to minimize osmotic shock. The process begins with rapid warming to 37°C in a thawing solution (TS) for approximately 1 minute to prevent ice crystal formation and maintain the structural integrity of the glass-like state [3].
This is followed by a gradient dilution approach involving incubation in dilution solution (DS) for 3 minutes and wash solution (WS) for 5-6 minutes at room temperature. This gradual process aims to ensure uniform rehydration of oocytes while mitigating the risk of membrane rupture [3]. The step-by-step methodology includes:
- Preparation: Equilibrate all solutions to specified temperatures (TS at 37°C, DS and WS at room temperature)
- Thawing: Transfer vitrified oocytes to TS at 37°C for 1 minute
- Dilution: Move oocytes to DS for 3 minutes at room temperature
- Washing: Transfer oocytes through two drops of WS for 5-6 minutes total at room temperature
- Recovery: Culture oocytes in appropriate medium for subsequent procedures
This protocol requires precise timing and temperature control at each step, with total processing time typically exceeding 10 minutes per batch of oocytes [3].
Modified Warming Protocol (MWP) for Oocytes
The modified warming protocol simplifies the process into an ultrafast, single-step approach that eliminates the need for DS and WS. This method builds on research demonstrating that embryos may be less susceptible to osmotic stress than previously assumed [3].
The MWP procedure involves:
- Preparation: Pre-warm TS to 37°C
- Thawing: Incubate vitrified oocytes in TS for 1 minute at 37°C
- Completion: Directly transfer to culture medium without additional dilution steps
This simplified approach reduces the warming time approximately 80% compared to conventional protocols (1 minute versus 10+ minutes), significantly streamlining laboratory workflow while reducing potential procedural variability [3].
Blastocyst Warming Protocols
For blastocysts, studies have evaluated both conventional sequential dilution methods and simplified one-step approaches. The one-step fast-warming protocol for blastocysts similarly reduces the process to a single warming solution step, taking advantage of the greater resilience of blastocyst-stage embryos to osmotic stress [6].
Validation studies for blastocyst warming protocols typically assess immediate morphological survival based on membrane intactness without extensive cellular degeneration, with acceptance criteria set at 70% for competence level and 95% for benchmark, as suggested by the Alpha consensus meeting [7]. Additional functional parameters include re-expansion within 2-4 hours post-warming (minimum 70%) and continued development until 24 hours post-warming (minimum 80%) [7].
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents and materials for warming protocol implementation
| Reagent/Material | Function | Protocol Application |
|---|---|---|
| Thawing Solution (TS) | Initial dilution of cryoprotectants at elevated temperature | Both CWP and MWP |
| Dilution Solution (DS) | Gradual reduction of cryoprotectant concentration | Conventional protocol only |
| Wash Solution (WS) | Final removal of cryoprotectants prior to culture | Conventional protocol only |
| Vitrification Carrier Devices | Physical support during vitrification/warming | Both protocols (Open vs. Closed systems) |
| Holding Medium (e.g., G-MOPS PLUS) | Maintain physiological conditions during handling | Both protocols |
| Culture Media (e.g., G-TL, G-2 PLUS) | Support continued development post-warming | Both protocols |
| Laser Blastocyst Collapsing System | Artificial reduction of blastocoel fluid prior to vitrification | Primarily for blastocysts |
| Carboplatin | Carboplatin for Cancer Research|Platinum-Based Compound | High-purity Carboplatin for research applications. This platinum-based alkylating agent is for Research Use Only (RUO). Not for human or veterinary use. |
| SB-431542 | SB-431542, CAS:301836-41-9, MF:C22H16N4O3, MW:384.4 g/mol | Chemical Reagent |
Essential materials adapted from described methodologies [3] [7]
The selection between open and closed carrier systems represents a critical consideration, with open systems allowing direct contact with liquid nitrogen and closed systems preventing this contact to minimize contamination risk. Studies have validated both approaches, with the move toward closed systems often driven by regulatory requirements [7].
Laser-assisted collapsing of expanded blastocysts prior to vitrification has been shown to optimize survival rates by reducing the volume of intracellular fluid and minimizing ice crystal formation potential [7].
The transition from conventional multi-step to simplified warming protocols represents a significant advancement in reproductive cryopreservation. Experimental evidence demonstrates that modified warming protocols not only reduce processing time and technical complexity but also improve key outcomes including blastocyst formation rates and ongoing pregnancy outcomes for vitrified-warmed oocytes [3]. For blastocysts, simplified one-step protocols achieve comparable outcomes to conventional methods while offering practical advantages through reduced procedural time [6].
The historical context of this evolution reflects a growing understanding of cellular responses to cryoprotectant exposure and removal, challenging previous assumptions about the necessity of gradual dilution steps. This paradigm shift toward simplified protocols aligns with broader trends in ART toward standardization, efficiency, and improved reproducibility while maintaining or enhancing clinical outcomes.
Future research directions include further optimization of warming solutions, exploration of protocol adaptations for specific patient populations, and long-term follow-up of children born from simplified warming techniques. As the field continues to evolve, the historical progression from conventional multi-step to simplified protocols provides a framework for evaluating future technological innovations in reproductive cryopreservation.
In the field of assisted reproductive technology (ART), the vitrification of oocytes and embryos is a cornerstone technique for fertility preservation. The subsequent warming process is equally critical, as it directly impacts the survival and developmental potential of these cryopreserved specimens. While conventional warming protocols (CWP) have been the long-standing standard, recent research has been focused on optimizing this process for improved efficiency and outcomes. This has led to the development of two significant variants: the Modified Warming Protocol (MWP) for oocytes and the One-Step Fast Warming protocol for blastocysts. This guide provides a detailed, objective comparison of these protocol variants, summarizing current research findings, experimental data, and methodologies for researchers and scientists in the field.
Comparative Analysis at a Glance
The table below summarizes the core objectives and key performance indicators of the three warming protocols based on recent scientific studies.
Table 1: Protocol Overview and Application
| Protocol Variant | Primary Application | Core Methodology | Key Distinguishing Feature |
|---|---|---|---|
| Conventional (CWP) | Oocytes & Embryos | Multi-step dilution at room temperature | Established baseline protocol; complex and time-intensive [3] |
| Modified (MWP) | Oocytes | Simplified into an ultrafast, single-step process | Replaces CWP for oocytes; improves developmental outcomes [3] |
| One-Step Fast Warming | Blastocysts | Single 1-minute step in 1M sucrose at 37°C | Simplified, efficient process for blastocysts; maintains clinical outcomes [6] [8] |
Comparative Experimental Outcomes
The following tables consolidate quantitative data from key studies, highlighting the performance of each protocol against critical laboratory and clinical metrics.
Table 2: Laboratory and Clinical Outcomes for Oocyte Warming (CWP vs. MWP)
| Outcome Measure | CWP Group | MWP Group | Fresh Group |
|---|---|---|---|
| Survival Rate | 93.7% (7967/8506) | 93.9% (920/980) | Not Applicable [3] |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% [3] |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% [3] |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | Not Reported [3] |
Table 3: Laboratory and Clinical Outcomes for Blastocyst Warming (CWP vs. One-Step Fast Warming)
| Outcome Measure | Conventional Multi-step Protocol | One-Step Fast Warming Protocol |
|---|---|---|
| Pregnancy Rate | 69.58% | 72.82% [8] |
| Clinical Pregnancy Rate | 57.36% | 56.86% [8] |
| Ongoing Pregnancy Rate | 51.12% | 50.62% [8] |
| Live Birth Rate | 51.12% | 49.38% [8] |
| Miscarriage Rate | 6.23% | 6.23% [8] |
Detailed Experimental Protocols
The methodologies below are drawn directly from the cited research publications.
Conventional Warming Protocol (CWP) for Oocytes
This protocol involves a gradient dilution approach at room temperature to minimize osmotic stress [3].
- Step 1 – Thawing: Cryopreserved oocytes are rapidly warmed to 37°C in a Thawing Solution (TS) for 1 minute [3].
- Step 2 – Dilution: Oocytes are incubated in a Dilution Solution (DS) for 3 minutes [3].
- Step 3 – Washing: Oocytes are transferred to a Wash Solution (WS) for 5–6 minutes to ensure uniform rehydration [3].
- Step 4 – Culture: After warming and dilution steps, oocytes are placed into culture media for subsequent procedures like Intracytoplasmic Sperm Injection (ICSI) [3].
Modified Warming Protocol (MWP) for Oocytes
This protocol simplifies CWP into an ultrafast, single-step process, eliminating the need for DS and WS [3].
- Procedure: Oocytes are incubated only in Thawing Solution (TS) for 1 minute at 37°C before being immediately placed into culture media [3].
- Objective: This modification aims to reduce total warming time, mitigate embryologist fatigue, and optimize clinical workflow while enhancing the developmental potential of vitrified-warmed oocytes [3].
One-Step Fast Warming Protocol for Blastocysts
This protocol is designed specifically for blastocysts, focusing on maximal simplification without compromising efficacy [6] [8].
- Procedure: Vitrified-warmed blastocysts are exposed to 1M sucrose solution for 1 minute at 37°C and then immediately placed into culture media where laser-assisted hatching is performed [6] [8].
- Control Protocol (Multi-step): The conventional method for blastocysts involved sequential exposure to 1M sucrose for 1 minute, 0.5M for 2 minutes, 0.25M for 2 minutes, and a washing solution for 3 minutes, all at room temperature [8].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key solutions and materials used in the described warming protocols, with their specific functions.
Table 4: Key Reagents and Materials in Warming Protocols
| Reagent/Material | Function in the Protocol |
|---|---|
| Thawing Solution (TS) | Initial solution for rapid warming; prevents ice crystallization and mitigates osmotic shock [3]. |
| Dilution Solution (DS) | Used in CWP to begin the gradient dilution and removal of cryoprotectants [3]. |
| Wash Solution (WS) | Used in CWP for the final removal of cryoprotectants and complete rehydration of cells [3]. |
| Sucrose Solutions (e.g., 1M, 0.5M) | Act as osmotic buffers to control the efflux of water and cryoprotectants from the cell during warming, preventing damaging volume shifts [6] [8]. |
| Culture Media | Provides a stable, nutrient-rich environment for oocytes/embryos after the warming process and before transfer or further culture [3] [6]. |
| BACE2-IN-1 | BACE2-IN-1, MF:C36H38F3N3O3, MW:617.7 g/mol |
| APX-115 | APX-115, CAS:1395946-75-4, MF:C17H18ClN3O, MW:315.8 g/mol |
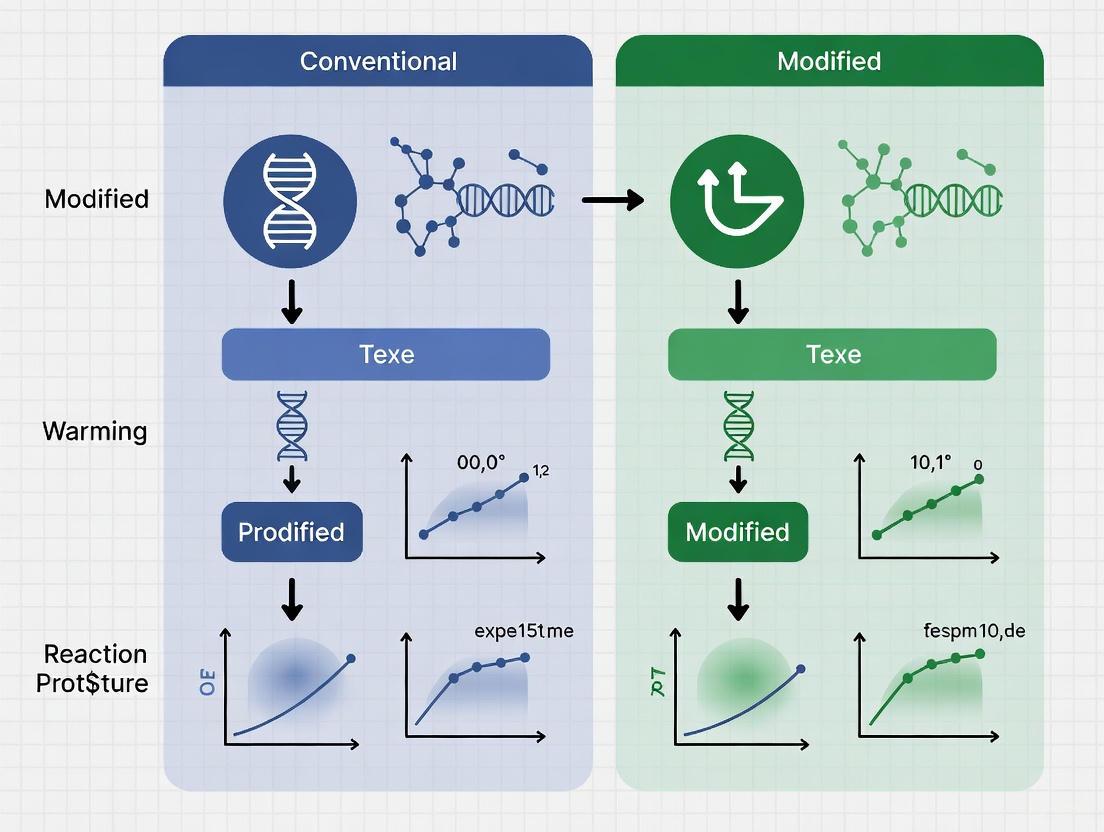
Protocol Workflow Visualization
The diagram below illustrates the fundamental procedural differences between the Conventional (CWP), Modified (MWP), and One-Step Fast Warming protocols.
Current research indicates that the optimal warming protocol variant is highly dependent on the cellular specimen. For oocytes, the Modified Warming Protocol (MWP) demonstrates superior outcomes, significantly enhancing blastocyst formation and ongoing pregnancy rates compared to the Conventional Warming Protocol (CWP) [3]. For blastocysts, the One-Step Fast Warming protocol offers a compelling alternative, providing clinical outcomes statistically comparable to conventional multi-step methods while offering significant gains in laboratory efficiency and workflow simplification [6] [8]. These findings underscore a trend in ART towards tailoring vitrification-warming strategies to specific cell types to maximize both clinical success and operational efficacy.
Embryo cryopreservation has become a cornerstone of modern assisted reproductive technology (ART), with vitrification emerging as the predominant technique due to its high efficiency and survival rates. The warming process, a critical step in frozen embryo transfer cycles, has traditionally involved a multi-step protocol to remove cryoprotectants and rehydrate embryos. However, recent research has focused on simplifying this process through modified warming protocols that reduce procedural time and complexity while aiming to maintain or even improve clinical outcomes.
This comparison guide objectively analyzes the performance of conventional versus modified warming protocols across key success metrics: survival, fertilization, blastocyst formation, and live birth rates. The data presented herein, drawn from recent clinical studies, provides researchers and clinicians with evidence-based insights to optimize laboratory protocols and enhance reproductive outcomes.
Comparative Performance Data: Conventional vs. Modified Warming Protocols
Oocyte Warming Outcomes
Recent studies have demonstrated significant differences in key performance metrics between conventional and modified warming protocols for oocytes. The data from a large retrospective cohort study comparing these protocols reveals notable variations in embryonic development and pregnancy outcomes.
Table 1: Oocyte Warming Outcomes - Conventional vs. Modified Warming Protocols
| Performance Metric | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% (7967/8506) | 93.9% (920/980) | - |
| Degeneration Rate Post-ICSI | 3.4% (268/7967) | 2.7% (25/920) | 2.8% (60/2106) |
| Normal Fertilization Rate | 79.6% | 79.5% | 83.0% |
| Abnormal Fertilization Rate | 10.1% | 9.1% | 3.3% |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | - |
The modified warming protocol shows particularly impressive results in blastocyst formation (77.3% vs. 57.5% for CWP) and usable blastocyst formation (51.4% vs. 35.4% for CWP). Multivariate analysis confirmed a positive association between MWP and usable blastocyst formation (adjusted incidence rate ratio = 1.423, 95% CI = 1.268 to 1.597, P < 0.001) as well as ongoing pregnancy/live birth (adjusted odds ratio = 1.899, 95% CI = 1.002 to 3.6, P < 0.05) [3].
Blastocyst Warming Outcomes
For vitrified-warmed blastocysts, studies have compared one-step fast warming protocols with conventional multi-step approaches, with results demonstrating comparable outcomes across multiple key metrics.
Table 2: Blastocyst Warming Outcomes - Conventional vs. Fast Warming Protocols
| Performance Metric | Conventional Warming Protocol | One-Step Fast Warming Protocol | Statistical Significance |
|---|---|---|---|
| Survival Rate | Comparable | Comparable | Not Significant |
| Pregnancy Rate | 69.58% | 72.82% | RR = 1.12, 95% CI: 1.39 |
| Clinical Pregnancy Rate | 57.36% | 56.86% | RR = 0.98, 95% CI: 0.84-1.16 |
| Ongoing Pregnancy Rate | 51.12% | 50.62% | RR = 0.99, 95% CI: 0.86-1.14 |
| Live Birth Rate | 51.12% | 49.38% | RR = 0.96, 95% CI: 0.84-1.11 |
| Miscarriage Rate | 6.23% | 6.23% | Not Significant |
The one-step fast warming protocol demonstrates comparable effectiveness to conventional warming across all measured reproductive outcomes, despite its simplified, time-efficient methodology [6] [8].
Experimental Protocols and Methodologies
Conventional Warming Protocol (CWP) for Oocytes
The conventional warming protocol follows a sequential, multi-step approach designed to gradually remove cryoprotectants and rehydrate oocytes or embryos:
Thawing Solution (TS) Incubation: Cryopreserved oocytes are rapidly warmed to 37°C in a thawing solution for 1 minute to prevent ice crystal formation and maintain structural integrity [3] [9].
Gradient Dilution Approach: Oocytes are sequentially incubated in:
Objective: This graded dilution minimizes osmotic stress, ensures uniform rehydration of oocytes, and mitigates the risk of membrane rupture [3].
Despite its effectiveness, this protocol is considered complex and time-intensive, requiring multiple solution changes and precise timing [3] [9].
Modified Warming Protocol (MWP) for Oocytes
The modified warming protocol simplifies the process into an ultrafast, single-step procedure:
Single-Step Process: Elimination of DS and WS steps, simplifying the protocol to incubation in TS for 1 minute only [3] [9].
Temperature Management: Maintains consistent temperature parameters while drastically reducing processing time.
Workflow Efficiency: This reduced warming time mitigates fatigue among embryologists, thereby optimizing clinical workflow [9].
This modified approach not only simplifies laboratory procedures but also demonstrates improved embryonic development potential, particularly for blastocyst formation [3].
One-Step Fast Warming Protocol for Blastocysts
For blastocyst warming, the one-step fast warming protocol involves:
Sucrose Solution Exposure: Embryos are exposed to 1M sucrose solution for 1 minute at 37°C [6] [8].
Direct Culture Transfer: Following sucrose exposure, embryos are immediately placed into culture media where laser-assisted hatching is performed [8].
Comparison to Conventional Blastocyst Warming: This contrasts with the conventional protocol which involves:
- 1 minute in 1M sucrose
- 2 minutes in 0.5M sucrose
- 2 minutes in 0.25M sucrose
- 3 minutes in washing solution at room temperature
- Final placement into culture media for laser-assisted hatching [8]
This simplified approach maintains embryo viability while significantly streamlining laboratory workflow.
Figure 1: Workflow Comparison of Conventional vs. Modified Warming Protocols. The modified protocol significantly simplifies the process by eliminating multiple steps while maintaining or improving outcomes [3] [9] [6].
Critical Factors Influencing Warming Success
Impact of Multiple Vitrification-Warming Cycles
Research indicates that the number of vitrification-warming cycles significantly affects blastocyst viability and live birth outcomes:
Single vs. Double Vitrification: Group BV (biopsied once, vitrified once) demonstrated superior outcomes compared to Group VBV (biopsied once, vitrified twice) across all metrics: implantation rate (55.6% vs. 37.1%, p < 0.001), clinical pregnancy rate (55.1% vs. 37.1%, p < 0.001), and live birth rate (53.6% vs. 35.7%, p = 0.01) [10].
Regression Analysis: The number of vitrification-warming cycles was the only factor significantly associated with reduced live birth rates (OR 1.95, 95% CI 1.01-3.78, p < 0.05) [10].
These findings highlight the importance of minimizing repeated warming cycles to preserve embryo viability and maximize clinical success.
Blastocyst Re-expansion as a Viability Indicator
Blastocyst re-expansion following warming serves as a critical indicator of viability and implantation potential:
Re-expanded vs. Completely Shrunken Blastocysts: Significantly higher clinical pregnancy rates (61.5% vs. 28.8%), ongoing pregnancy rates (52.9% vs. 22.1%), and live birth rates (50.0% vs. 20.2%) were observed in re-expanded blastocyst transfers compared to completely shrunken blastocysts [11].
Day of Blastocyst Formation Impact: For completely shrunken blastocysts, the clinical pregnancy rate was 3.062 times higher for day 5 blastocysts compared to day 6 blastocysts (adjusted OR 3.062, 95% CI 1.077-8.704, P = 0.036) [11].
These findings suggest that while re-expansion is a valuable viability marker, even non-re-expanded blastocysts retain implantation potential, particularly when derived from day 5 embryos.
Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Vitrification/Warming Protocols
| Reagent/Material | Function | Protocol Applications |
|---|---|---|
| Equilibration Solution (ES) | Contains permeating cryoprotectants (7.5% ethylene glycol + 7.5% DMSO) for initial cellular dehydration | Vitrification step [11] |
| Vitrification Solution (VS) | Higher concentration cryoprotectant solution (15% EG + 15% DMSO + 0.5M sucrose) for final vitrification | Vitrification step [11] |
| Thawing Solution (TS) | Initial warming solution for rapid thawing and initial cryoprotectant dilution | First step in both CWP and MWP [3] [9] |
| Dilution Solution (DS) | Reduced concentration solution for gradual cryoprotectant removal | Used in CWP only [3] [9] |
| Wash Solution (WS) | Final washing solution to remove residual cryoprotectants | Used in CWP only [3] [9] |
| 1M Sucrose Solution | Non-permeating solute for creating osmotic gradient during warming | Used in one-step blastocyst warming [6] [8] |
| Artificial Shrinkage Laser | Laser system for blastocoel collapse prior to vitrification | Blastocyst vitrification [11] |
The evidence from recent comparative studies indicates that modified warming protocols, particularly for oocytes, demonstrate significant advantages in key success metrics including blastocyst formation and ongoing pregnancy/live birth rates. The simplified one-step approach for blastocyst warming maintains comparable outcomes to conventional methods while offering improved workflow efficiency.
For clinical applications and future research, the following considerations emerge as critical:
Protocol Selection: Modified warming protocols present a viable, efficient alternative to conventional methods without compromising outcomes.
Multiple Warming Cycles: The significant reduction in live birth rates associated with double vitrification-warming cycles warrants careful consideration in PGT-A and embryo management strategies.
Viability Assessment: Blastocyst re-expansion remains a valuable viability indicator, though even non-re-expanded blastocysts retain implantation potential under specific conditions.
These findings support the continued refinement of warming protocols to optimize both laboratory efficiency and clinical outcomes in assisted reproduction.
Protocol in Practice: A Step-by-Step Guide to Modern Warming Techniques
In the field of assisted reproductive technology (ART), cryopreservation has revolutionized treatment by enabling the preservation of oocytes and embryos. The warming process is equally critical, as improper thawing can induce osmotic shock, ice crystal formation, and cellular damage, compromising developmental potential. The Conventional Warming Protocol (CWP) represents a meticulous, multi-step approach designed to mitigate these risks through gradual cryoprotectant removal. Recent research has focused on developing simplified modified warming protocols (MWPs) that reduce procedural time while maintaining, and in some cases enhancing, clinical outcomes. This guide deconstructs the established CWP and objectively compares its performance against emerging MWPs, providing researchers and clinicians with evidence-based insights to inform laboratory practices.
Experimental Protocols and Methodologies
The comparative data presented in this guide are synthesized from recent prospective and retrospective cohort studies. The following outlines the key methodological frameworks employed by these investigations.
Study Populations and Design: A 2025 prospective cohort study at Embryolab Fertility Clinic (Thessaloniki, Greece) analyzed 802 cycles, prospectively comparing a one-step fast-warming protocol to the CWP for vitrified blastocysts, with strict controls on maternal age, embryo quality, and number transferred [6]. Concurrently, a large-scale retrospective cohort study from Lee Women’s Hospital (Taiwan) analyzed 13,103 donor oocytes from cycles conducted between 2019 and 2024, comparing outcomes between CWP, MWP, and fresh oocyte groups [3] [9]. A separate 2024 retrospective analysis of 752 frozen embryo transfers (FETs) at a Boston academic fertility clinic compared single-step warming to standard warming, using generalized estimated equation models to account for confounders [12].
Cryopreservation and Warming Techniques: Across studies, oocytes or blastocysts were vitrified using standard methods and devices (e.g., Cryolock). The core comparison lay in the warming methodology. The CWP adhered to manufacturer guidelines, typically involving sequential immersion in Thaw Solution (TS), Dilution Solution (DS), and Wash Solution (WS) at specific temperatures and durations [3] [12] [9]. In contrast, the MWP often eliminated the DS and WS steps, involving only a brief immersion in TS followed by direct transfer to culture media [12].
Outcome Measures: Key performance indicators included:
- Cellular Survival: Rate of oocyte or blastocyst survival post-warming.
- Developmental Competence: For oocytes, this included normal fertilization, blastocyst formation, and usable blastocyst rates. For blastocysts, re-expansion rate was measured.
- Clinical Endpoints: Implantation, clinical pregnancy, ongoing pregnancy, and live birth rates.
- Laboratory Efficiency: Total time required for the warming procedure.
Anatomizing the Conventional Warming Protocol (CWP)
The CWP is a carefully orchestrated procedure to safely remove cryoprotectants and rehydrate cells.
Step-by-Step Process and Reagents
Table 1: Steps and Reagents in a Typical Conventional Warming Protocol
| Step Sequence | Solution | Duration | Temperature | Primary Function |
|---|---|---|---|---|
| Step 1 | Thaw Solution (TS) | 1 minute | 37°C | Rapid warming and initial dilution of cryoprotectants [12] |
| Step 2 | Dilution Solution (DS) | 3-4 minutes | Room Temperature | Further dilution of cryoprotectants to mitigate osmotic shock [3] [12] [9] |
| Step 3 | Wash Solution (WS) | 5-8 minutes (one or two rinses) | Room Temperature | Complete removal of cryoprotectants and gradual cell rehydration [3] [12] [9] |
| Step 4 | Culture Media | 1-4 hours before transfer | 37°C (in incubator) | Final equilibrium and assessment of survival/re-expansion [12] |
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Reagents in the Conventional Warming Protocol
| Reagent Solution | Typical Composition | Critical Function in the Protocol |
|---|---|---|
| Thaw Solution (TS) | 1.0 M Sucrose, 20% DSS (Defined Supplement Solution), Gentamicin in a HEPES-buffered medium [12]. | Creates a high osmotic pressure to draw cryoprotectants out of the cell gradually upon warming, preventing lethal osmotic swelling. |
| Dilution Solution (DS) | 0.5 M Sucrose, 20% DSS, Gentamicin [12]. | Provides an intermediate osmotic step to safely further reduce cryoprotectant concentration. |
| Wash Solution (WS) | 20% DSS, Gentamicin in a HEPES-buffered medium [12]. | A sucrose-free solution used for the final rinse, allowing the cell to fully rehydrate in an isotonic environment. |
| Mezigdomide | Mezigdomide, CAS:2259648-80-9, MF:C32H30FN5O4, MW:567.6 g/mol | Chemical Reagent |
| Sulfopin | Sulfopin|Covalent Pin1 Inhibitor|For Research | Sulfopin is a potent, selective covalent Pin1 inhibitor for cancer research. Blocks Myc-driven tumors. For Research Use Only. Not for human use. |
Diagram 1: Sequential workflow of the Conventional Warming Protocol (CWP), illustrating the multi-step process with specific solutions, durations, and temperatures.
Performance Comparison: CWP vs. Modified Warming Protocols
Recent studies provide quantitative data to compare the efficacy of CWP against faster, simplified MWPs.
Outcomes for Vitrified Oocytes
Table 3: Oocyte Warming Outcomes: CWP vs. MWP vs. Fresh
| Outcome Metric | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Reference) | P-Value |
|---|---|---|---|---|
| Oocyte Survival Rate | 93.7% (7967/8506) [3] [9] | 93.9% (920/980) [3] [9] | Not Applicable | > 0.05 |
| Normal Fertilization (ICSI) | 79.5-79.6% [3] [9] | 79.5-79.6% [3] [9] | 83.0% [3] [9] | < 0.05 (vs. Fresh) |
| Blastocyst Formation Rate | 57.5% [3] [9] | 77.3% [3] [9] | 69.2% [3] [9] | < 0.05 (CWP vs. MWP/Fresh) |
| Usable Blastocyst Formation Rate | 35.4% [3] [9] | 51.4% [3] [9] | 48.5% [3] [9] | < 0.05 (CWP vs. MWP) |
| Ongoing Pregnancy/Live Birth Rate | 50.4% [3] [9] | 66.7% [3] [9] | Not Reported | < 0.05 |
The data demonstrates that while oocyte survival and initial fertilization are comparable between CWP and MWP, the MWP leads to a statistically significant improvement in key developmental metrics. The blastocyst formation rate with MWP was superior to CWP and even exceeded the rate in the fresh oocyte reference group. This enhanced developmental competence translated to a significantly higher ongoing pregnancy/live birth rate in the MWP group (66.7% vs. 50.4%) [3] [9].
Outcomes for Vitrified Blastocysts
Table 4: Blastocyst Warming Outcomes: Standard Warming (SW) vs. Single-Step (SS) Warming
| Outcome Metric | Standard Warming (SW) Protocol | Single-Step (SS) Warming Protocol | P-Value |
|---|---|---|---|
| Blastocyst Survival Rate | 100% (Safety Study, n= embryos) [12] | 100% (Safety Study, n= embryos) [12] | Not Significant |
| Blastocyst Re-expansion Rate | No significant difference [12] | No significant difference [12] | Not Significant |
| Clinical Pregnancy Rate | No significant difference [6] [12] | No significant difference [6] [12] | Not Significant |
| Live Birth Rate | No significant difference [6] [12] | No significant difference [6] [12] | Not Significant |
| Multiple Gestation Rate | Baseline [12] | Increased [AdjOR 1.06] [12] | 0.019 |
For blastocysts, the evidence suggests clinical equivalence between the complex SW and the simplified SS warming protocol in terms of survival, pregnancy, and live birth outcomes [6] [12]. A notable finding was a slightly increased odds of multiple gestation with the SS protocol, even after adjusting for the number of embryos transferred, the clinical significance of which requires further study [12]. A critical distinction is the dramatic reduction in warming time; the SS protocol completes in approximately 1 minute, compared to the 14-minute SW protocol, offering substantial gains in laboratory workflow efficiency [12].
Diagram 2: Protocol efficiency comparison, highlighting the significant reduction in laboratory processing time achieved by the Modified Warming Protocol.
Discussion and Research Implications
The collective evidence indicates a paradigm shift in warming protocols. For oocytes, the MWP is not just equivalent but appears superior to the CWP, yielding significantly better blastocyst development and pregnancy outcomes [3] [9]. This challenges the long-held belief that the gradual, multi-step dilution of CWP is indispensable for the sensitive oocyte. For blastocysts, the single-step warming protocol presents a compelling alternative, offering clinical parity with the standard protocol while maximizing laboratory efficiency [6] [12].
However, one experimental study sounded a note of caution, indicating that a shortened warming protocol could induce transient over-rehydration-induced cell necrosis in blastocysts, though this did not ultimately impact their outgrowth competence in that model [13]. This underscores the need for careful internal validation when implementing any new protocol. The drive towards simplification is also evident in ovarian tissue cryopreservation, where research is exploring universal rapid warming protocols to standardize practice for both slow-frozen and vitrified tissue [14].
The Conventional Warming Protocol, with its sequential use of Thaw, Dilution, and Wash solutions, has been a cornerstone of ART, providing a safe and effective method for reviving vitrified cells. However, rigorous comparative research demonstrates that modern Modified Warming Protocols achieve comparable or superior clinical outcomes while offering significant advantages in laboratory workflow efficiency through drastically reduced procedure times. The optimal protocol may depend on the cell type (oocyte vs. blastocyst) and specific laboratory conditions. Nevertheless, the evidence strongly supports the adoption of simplified MWPs as a new standard for optimizing outcomes in donor oocyte cycles and enhancing efficiency in blastocyst warming programs.
Cryopreservation has revolutionized assisted reproductive technology (ART), with vitrification becoming a cornerstone for preserving oocytes and embryos. While conventional warming protocols (CWP) have established effectiveness, they are complex and time-intensive laboratory procedures. Recent research has focused on simplifying these processes, leading to the development of modified warming protocols (MWP) and one-step warming protocols that aim to enhance laboratory efficiency while maintaining or even improving clinical outcomes.
The fundamental challenge in warming vitrified cells lies in rapidly transitioning them from -196°C while safely removing cryoprotectants to prevent osmotic shock and cellular damage. Conventional protocols typically employ a gradient dilution approach with multiple solutions and steps. Emerging evidence now demonstrates that simplified protocols can reduce procedural time and potential stressors on delicate reproductive cells. This guide provides a detailed comparison of these protocol variations, presenting experimental data and methodologies to inform researchers and clinical laboratories in their protocol selection and optimization.
Experimental Protocols and Methodologies
Conventional Warming Protocol (CWP) for Oocytes
The CWP serves as the established baseline against which modified protocols are compared. The process involves sequential exposure to solutions with decreasing concentrations of cryoprotectants:
- Thawing Solution (TS): Oocytes are rapidly warmed to 37°C in TS for 1 minute to prevent ice crystal formation and maintain structural integrity [3] [9].
- Dilution Solution (DS): Cells are then incubated in DS at room temperature for 3 minutes to initiate cryoprotectant dilution [3] [9].
- Wash Solution (WS): A final incubation in WS at room temperature for 5-6 minutes ensures complete removal of cryoprotectants, minimizing osmotic stress and ensuring uniform rehydration [3] [9].
This multi-step, multi-temperature process, while effective, is complex and contributes significantly to embryologist workload [3] [9].
Modified Warming Protocol (MWP) for Oocytes
The MWP simplifies the process into an ultrafast, single-step procedure, eliminating the need for DS and WS [3] [9]. The key modification is:
- Single-Step Warming: Vitrified oocytes are placed directly in a Thawing Solution (TS) and incubated for 1 minute at 37°C [15]. This streamlined approach significantly reduces total warming time and minimizes cell manipulation.
One-Step Warming Protocol for Embryos
A similar simplification has been successfully applied to embryo warming, demonstrating the broader applicability of this concept. This protocol is used for both cleavage-stage (day 3) and blastocyst-stage (day 5 or 6) embryos [16].
- Short Rehydration: The one-step protocol employs a significantly shortened rehydration process compared to conventional methods for embryos [16]. The exact duration, while shortened, must be optimized for specific media and embryo stages.
The Universal Warming Protocol (UWP) Concept
Addressing practical challenges in clinics, the Universal Warming Protocol (UWP) investigates the feasibility of using warming media from a different manufacturer than the vitrification media. In one multicenter study, oocytes vitrified with a Kitazato kit were successfully warmed using three different devitrification media: Kitazato, Irvine, and RapidWarm Omni, following their respective manufacturer protocols [17]. This approach offers flexibility and can reduce costs for laboratories that work with oocytes vitrified elsewhere or with multiple kit systems.
Comparative Experimental Outcomes
The following tables summarize key quantitative outcomes from studies comparing these protocols for oocytes and embryos.
Table 1: Oocyte Warming and Subsequent Embryo Development Outcomes [3] [9]
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Oocyte Survival Rate | 93.7% | 93.9% | Not Applicable |
| Normal Fertilization Rate | 79.5% | 79.6% | 83.0% |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | Not Reported |
Table 2: One-Step vs. Long Warming Protocol for Embryos [16]
| Outcome Measure | Long Warming Protocol (Control) | One-Step/Short Warming Protocol |
|---|---|---|
| Clinical Pregnancy Rate (Blastocysts) | ~50% | ~62% |
| Miscarriage Rate | ~17% | ~8% |
| Ongoing Pregnancy Rate (≥26 weeks) | ~41% | ~54% |
Table 3: Universal Warming Protocol with Different Media [17]
| Outcome Measure | Group A: Vitrified & Warmed with Kitazato | Group B: Vitrified with Kitazato, Warmed with Irvine | Group C: Vitrified with Kitazato, Warmed with RapidWarm Omni |
|---|---|---|---|
| Oocyte Survival Rate | 86% | 85% | 94% |
| Blastulation Rate | 52% | 58% | 57% |
| Clinical Pregnancy Rate (Day 5 Transfer) | 39% | 57% | 60% |
Statistical and Clinical Significance
Multivariate analysis of the oocyte MWP data revealed a strong positive association between the modified protocol and key outcomes. The adjusted incidence rate ratio for usable blastocyst formation was 1.423 (95% CI: 1.268-1.597, P < 0.001), and the adjusted odds ratio for ongoing pregnancy/live birth was 1.899 (95% CI: 1.002-3.6, P < 0.05), indicating that the MWP is a significant independent factor for improving success rates [3] [9].
Workflow and Signaling Pathways
The diagrams below illustrate the procedural workflow of the different protocols and the logical relationship between protocol choices and cellular outcomes.
Oocyte Warming Protocol Workflow
Protocol Impact on Cell Viability
The Scientist's Toolkit: Key Research Reagents and Materials
Table 4: Essential Reagents for Vitrification and Warming Protocols
| Reagent Category | Specific Examples | Function in Protocol |
|---|---|---|
| Vitrification Media Kits | Kitazato Vitrification Media (Japan) | Provides cryoprotectants and solutions for the freezing process [17]. |
| Devitrification/Warming Media Kits | Kitazato, Irvine (Fujifilm), RapidWarm Omni (Vitrolife) | Provides solutions for thawing, diluting, and removing cryoprotectants during warming [17]. |
| Cryoprotectant Agents (CPA) | Dimethyl Sulfoxide (DMSO), Ethylene Glycol, Sucrose | Permeate (DMSO, EG) or non-permeate (Sucrose) the cell to prevent ice crystal formation but pose toxicity risks [16]. |
| Thawing Solution (TS) | Component of warming kits | First solution for rapid warming and initial cryoprotectant dilution [3] [9]. |
| Dilution Solution (DS) | Component of conventional warming kits | Further dilutes cryoprotectant concentration in a controlled manner (omitted in MWP) [3] [9]. |
| Wash Solution (WS) | Component of warming kits | Final solution for complete cryoprotectant removal and cell rehydration [3] [9]. |
| KRAS inhibitor-9 | KRAS inhibitor-9, MF:C13H9ClN2S2, MW:292.8 g/mol | Chemical Reagent |
| GSK-25 | GSK-25, CAS:874119-56-9, MF:C24H16Cl2F2N6O, MW:513.33 | Chemical Reagent |
The experimental data compellingly demonstrates that simplified warming protocols—whether MWP for oocytes or one-step methods for embryos—can not only enhance laboratory efficiency but also significantly improve key clinical outcomes, including blastocyst formation and ongoing pregnancy rates. The concept of a Universal Warming Protocol further adds a layer of practicality, offering clinics flexibility in reagent selection without compromising success.
Future research directions should focus on standardizing these simplified protocols across different patient populations and vitrification systems. Larger multicenter trials and further investigation into the underlying cellular mechanisms, particularly how reduced osmotic stress translates to improved developmental potential, will solidify the position of these streamlined protocols as the new standard in assisted reproductive technology.
Within the broader thesis of conventional versus modified warming protocol outcomes research, a critical technical examination of the workflow from thawing to culture is essential. The vitrification and warming of oocytes and embryos represent cornerstone techniques in assisted reproductive technology (ART), particularly for fertility preservation and egg donation programs [3] [9]. While effective, the conventional warming protocol (CWP) is recognized as a complex and time-intensive process [9]. Recent research has focused on simplifying this workflow, leading to the development of a modified warming protocol (MWP) that significantly shortens the procedure [3] [9]. This guide provides an objective, data-driven comparison of these protocols, detailing the technical workflow, experimental methodologies, and resultant clinical outcomes to inform researchers and drug development professionals.
Experimental Protocols & Methodologies
The comparative data presented in this guide are primarily derived from a substantial retrospective cohort study conducted at Lee Women’s Hospital, Taiwan [3] [9] [18]. The study analyzed outcomes from 13,103 donor oocytes, divided into three groups: a CWP group (n=8,506 oocytes), an MWP group (n=980 oocytes), and a fresh oocyte control group (n=3,617 oocytes) [3]. All vitrified oocytes were processed using the Cryotec method (Reprolife, Japan) [18].
Detailed Workflow: Conventional vs. Modified Warming
The core distinction between the two protocols lies in the sequence, temperature, and duration of the steps involved in transitioning the oocytes from the thawing solution to the final wash before culture.
Table 1: Step-by-Step Warming Protocol Comparison
| Protocol Step | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) |
|---|---|---|
| Thawing Solution (TS) | 2 minutes at 37°C [18] | 2 minutes at 37°C [18] |
| Dilution Solution (DS) | 3 minutes at 25°C (Room Temperature) [3] [9] | 2 minutes at 37°C [18] |
| Wash Solution (WS) | 5-6 minutes at 25°C (Room Temperature) [3] [9] | Omitted or integrated [9] |
| Total Estimated Time | ~10-11 minutes | ~4 minutes |
Following the warming process, oocytes from both protocols were thoroughly washed in a final wash solution and then transferred back to a human tubal fluid (HTF) medium for subsequent culture and intracytoplasmic sperm injection (ICSI) [18].
Underlying Rationale and Workflow Visualization
The CWP uses a gradient dilution approach at room temperature to minimize osmotic stress, ensuring uniform rehydration and mitigating the risk of membrane rupture [9]. In contrast, the MWP simplifies this into an ultrafast process by maintaining a consistent temperature of 37°C and eliminating or shortening specific steps, thereby reducing the total warming time and potential thermal stress [9] [18]. The logical flow of each protocol is mapped below.
Diagram 1: A comparative workflow of Conventional versus Modified Warming Protocols, highlighting differences in steps and temperature.
Comparative Outcome Data
The efficacy of the two warming protocols was evaluated based on key laboratory and clinical endpoints. The following tables summarize the quantitative outcomes from the cited study, comparing the MWP and CWP against each other and a fresh oocyte control group.
Laboratory and Embryological Outcomes
Table 2: Oocyte Survival, Fertilization, and Blastocyst Formation Rates
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate (%) | 93.7 (7967/8506) [3] [18] | 93.9 (920/980) [3] [18] | Not Applicable |
| ICSI Degeneration Rate (%) | 3.4 (268/7967) [3] | 2.7 (25/920) [3] | 2.8 (60/2106) [3] |
| Normal Fertilization Rate (%) | 79.5 [3] | 79.6 [3] | 83.0 [3] |
| Abnormal Fertilization Rate (%) | 10.1 [3] | 9.1 [3] | 3.3 [3] |
| Blastocyst Formation Rate (%) | 57.5 (3645/6337) [18] | 77.3 (566/732) [18] | 69.2 [3] |
| Usable Blastocyst Formation Rate (%) | 35.4 [3] | 51.4 [3] | 48.5 [3] |
| Day 5 Good Blastocyst Rate (%) | 17.2 (1091/6337) [18] | 27.3 (200/732) [18] | Not Specified |
Clinical Pregnancy Outcomes
Table 3: Final Clinical Endpoints
| Clinical Endpoint | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) |
|---|---|---|
| Ongoing Pregnancy / Live Birth Rate (%) | 50.4 [3] | 66.7 [3] |
| Adjusted Odds Ratio (95% CI) | Reference (1.0) | 1.899 (1.002 - 3.6) [3] |
Multivariate analysis from the primary study confirmed a statistically significant positive association between the use of the MWP and both the formation of usable blastocysts (adjusted incidence rate ratio = 1.423, 95% CI = 1.268 to 1.597, P < 0.001) and the achievement of an ongoing pregnancy or live birth (adjusted odds ratio = 1.899, 95% CI = 1.002 to 3.6, P < 0.05) [3].
The Scientist's Toolkit: Key Research Reagents
The execution of standardized warming protocols requires specific reagents and materials. The following table details the essential solutions used in the featured experiments.
Table 4: Essential Reagents for Oocyte Warming Protocols
| Research Reagent | Function in the Protocol |
|---|---|
| Vitrification Solution (VS) | A solution with high concentrations of cryoprotectants (CPAs) used during the initial freezing process to enable glass-like solidification without ice crystal formation [3] [9]. |
| Thawing Solution (TS) | The first solution used during warming, containing a high sucrose concentration to initially draw out CPAs from the cell in a controlled manner and prevent osmotic shock [3] [9]. |
| Dilution Solution (DS) | A solution with a lower sucrose concentration than the TS, used to further dilute and remove CPAs from the oocyte [3] [9]. |
| Wash Solution (WS) | A sucrose-free solution used to thoroughly wash the oocyte and remove any residual CPAs, fully restoring the cell to an isotonic condition before culture [3] [9]. |
| Human Tubal Fluid (HTF) Medium | The base culture medium to which oocytes are transferred after the completion of the warming and washing steps, preparing them for fertilization and subsequent embryo culture [18]. |
| Schisantherin E | Schisantherin E, MF:C30H34O9, MW:538.6 g/mol |
| ROCK1-IN-1 | ROCK1-IN-1, MF:C17H15N3O2S, MW:325.4 g/mol |
The empirical data from a large-scale clinical study demonstrates that the Modified Warming Protocol, despite its significantly shorter and simpler workflow, is associated with superior embryological and clinical outcomes compared to the Conventional Warming Protocol. The MWP resulted in markedly higher rates of blastocyst formation, usable blastocysts, and ongoing pregnancies/live births, effectively bridging the performance gap between vitrified-warmed and fresh oocytes [3] [9] [18]. This evidence suggests that the MWP is not merely a procedural shortcut but a technically optimized protocol that can enhance laboratory efficiency while simultaneously improving clinical success rates, positioning it as a potential new standard for optimizing donor and fertility preservation cycles.
In the field of assisted reproductive technology (ART) and biological sample storage, the vitrification of sensitive biological materials like oocytes and embryos is a cornerstone practice. A critical yet historically time-intensive part of this process is the warming protocol, which involves thawing cryopreserved samples for use. Recent research has been focused on a fundamental thesis: that modified warming protocols (MWP) can significantly enhance laboratory efficiency by reducing process times while maintaining or even improving key reproductive outcomes compared to conventional warming protocols (CWP).
This objective comparison guide analyzes the most current experimental data from recent clinical studies, providing researchers and drug development professionals with a clear, evidence-based overview of performance differences between these two approaches. The following sections detail the experimental methodologies, quantify time savings and clinical outcomes, and provide visualizations of the optimized workflows.
Experimental Protocols and Methodologies
The data supporting the comparison between conventional and modified warming protocols stems from recent, rigorous clinical studies. The methodologies are summarized below for clear comparison.
Study on Vitrified-Warmed Blastocysts (One-Step Fast Warming)
- Study Design: Prospective cohort study conducted at Embryolab Fertility Clinic, Thessaloniki, Greece, between January 2023 and June 2024 [6] [8].
- Subjects: 1,182 embryos from 802 frozen embryo transfer cycles. Both groups consisted of patients with good-quality expanded blastocysts, matched for maternal age, embryo quality, and number of embryos transferred [6].
- Exposure/Intervention:
- Fast-Warming Group: Embryos were warmed using a one-step protocol: exposure to 1M sucrose solution for 1 minute at 37°C, followed by immediate transfer to culture media for laser-assisted hatching [8].
- Control Group: Embryos were warmed using a conventional, multi-step protocol: 1 minute in 1M sucrose, 2 minutes in 0.5M sucrose, 2 minutes in 0.25M sucrose, and 3 minutes in a washing solution at room temperature, before being placed into culture media [6] [8].
- Main Outcome Measures: Survival rate, pregnancy rate, clinical pregnancy rate, ongoing pregnancy rate, implantation rate, miscarriage rate, biochemical pregnancy rate, and live birth rate [8].
Study on Vitrified Donor Oocytes (Modified Warming Protocol)
- Study Design: Retrospective cohort study conducted at Lee Women’s Hospital, Taiwan, with data collected from January 2019 to August 2024 [9] [3].
- Subjects: An analysis of 13,103 donor oocytes, divided into three groups: Conventional Warming Protocol (CWP) group (n=8,506), Modified Warming Protocol (MWP) group (n=980), and a fresh oocyte group (n=3,617) for baseline comparison [9].
- Exposure/Intervention:
- Conventional Warming Protocol (CWP): A multi-step process involving rapid warming to 37°C in a thawing solution (1 min), followed by incubation in a dilution solution (3 min) and a wash solution (5-6 min) at room temperature [9] [3].
- Modified Warming Protocol (MWP): An ultrafast, single-step process that eliminates the dilution and wash solutions, involving incubation in a thawing solution for just 1 minute [9] [3].
- Main Outcome Measures: Oocyte survival rate, degeneration rate post-ICSI, fertilization rates, blastocyst formation rates, and ongoing pregnancy/live birth rates [9].
Quantitative Data Comparison
The following tables consolidate the key quantitative findings from the cited studies, allowing for direct comparison of performance metrics.
Table 1: Comparative Warming Protocol Timings
| Process Step | Conventional Warming Protocol | One-Step / Modified Warming Protocol |
|---|---|---|
| Total Process Time | Approximately 10-12 minutes [9] [3] | Approximately 1 minute [9] [8] |
| Thawing Solution (37°C) | 1 minute [9] | 1 minute [9] [8] |
| Dilution Solution (Room Temp) | 3 minutes [9] | Eliminated |
| Wash Solution (Room Temp) | 5-6 minutes [9] | Eliminated |
| Sucrose Solution Steps | 3 steps (1M, 0.5M, 0.25M) [6] | 1 step (1M Sucrose) [8] |
Table 2: Reproductive Outcomes for Blastocysts (One-Step vs. Conventional) [6] [8]
| Outcome Measure | Conventional Warming Protocol | One-Step Fast Warming Protocol | Statistical Significance |
|---|---|---|---|
| Survival Rate | Comparable | Comparable | Not Significant (P>0.05) |
| Pregnancy Rate | 69.58% | 72.82% | Not Significant (RR=1.12, 95% CI: 1.39) |
| Clinical Pregnancy Rate | 57.36% | 56.86% | Not Significant (RR=0.98, 95% CI: 0.84-1.16) |
| Ongoing Pregnancy Rate | 51.12% | 50.62% | Not Significant (RR=0.99, 95% CI: 0.86-1.14) |
| Live Birth Rate | 51.12% | 49.38% | Not Significant (RR=0.96, 95% CI: 0.84-1.11) |
| Miscarriage Rate | 6.23% | 6.23% | Not Significant |
Table 3: Laboratory and Clinical Outcomes for Oocytes (MWP vs. CWP) [9] [3]
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Reference) |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | - |
| Normal Fertilization Rate | 79.5% | 79.6% | 83.0% |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | - |
Workflow Visualization
The fundamental difference between the two protocols lies in the simplification of the process. The following diagram illustrates the logical sequence and dramatic reduction in steps achieved by the modified protocol.
The Scientist's Toolkit: Essential Research Reagent Solutions
The experiments cited rely on specific laboratory solutions and materials to ensure the viability of biological samples during the critical warming process. The following table details key reagents and their functions.
Table 4: Key Reagents and Materials for Vitrification Warming Protocols
| Item | Function in Protocol | Application Note |
|---|---|---|
| Thawing Solution (TS) | Initial rapid warming solution at 37°C to prevent ice crystal formation and maintain structural integrity [9]. | Used in both CWP and MWP as the critical first step. |
| Dilution Solution (DS) | Gradually reduces the concentration of cryoprotectants inside the cell at room temperature, minimizing osmotic shock [9] [3]. | A key step eliminated in the MWP, contributing to major time savings. |
| Wash Solution (WS) | Further removes residual cryoprotectants and ensures uniform rehydration of the sample [9] [3]. | A key step eliminated in the MWP. |
| Sucrose Solutions (e.g., 1M, 0.5M, 0.25M) | Act as osmotic buffers. They control the efflux of water and cryoprotectants from the cell during warming, preventing damaging volume shifts [6] [8]. | The one-step protocol uses a single sucrose concentration, while the conventional method uses a descending gradient. |
| Culture Media (e.g., Human Tubal Fluid) | Provides nutrients and a stable environment for the warmed samples (oocytes/embryos) before further procedures like fertilization or transfer [6]. | Used after the completion of either warming protocol. |
| EGFR-IN-99 | EGFR-IN-99, MF:C25H22FN7O3, MW:487.5 g/mol | Chemical Reagent |
| CHR-6494 TFA | CHR-6494 TFA, CAS:1333377-65-3; 1458630-17-5, MF:C18H17F3N6O2, MW:406.369 | Chemical Reagent |
The body of evidence from recent clinical studies strongly supports the thesis that modified warming protocols offer a superior alternative to conventional methods within the context of laboratory efficiency and outcomes research.
The primary and most consistent finding is the dramatic reduction in process time, from approximately 10 minutes to just 1 minute, without compromising key metrics such as oocyte and embryo survival rates [9] [8]. Furthermore, some studies indicate that simplified protocols can lead to improved biological outcomes, including significantly higher rates of blastocyst formation and ongoing pregnancy rates for vitrified-warmed oocytes [9] [3].
For researchers, scientists, and drug development professionals, these findings highlight that streamlining complex laboratory workflows is not merely a matter of convenience. It is a strategic imperative that can yield tangible benefits in throughput, resource allocation, and potentially, the success rates of critical biological applications.
Navigating Challenges and Optimizing Outcomes Across Cell Types
In assisted reproductive technology (ART), the cryopreservation of gametes and embryos through vitrification and warming is a cornerstone practice. However, a significant challenge persists: oocytes and embryos at different developmental stages exhibit markedly different survival rates when subjected to the same osmotic stress during these procedures. This differential sensitivity to osmotic fluctuations represents a critical focus for research aimed at optimizing ART outcomes. Within the broader investigation of conventional versus modified warming protocols, understanding these fundamental biological differences is paramount for developing more physiologically attuned methods that can enhance the viability of both oocytes and embryos, ultimately improving clinical success rates.
Comparative Sensitivity: Oocytes vs. Embryos
Fundamental Differences in Osmotic Stress Response
The differential sensitivity of oocytes and embryos to osmotic stress arises from their distinct biological structures, regulatory capacities, and developmental programming. Oocytes, being single cells, lack the compensatory mechanisms that multi-cell-stage embryos possess.
Table 1: Fundamental Differences in Osmotic Stress Response
| Characteristic | Oocytes | Early Embryos |
|---|---|---|
| Cell Structure | Single large cell with meiotic spindle | Multicellular structure with blastomeres |
| Volume Regulation | Limited capacity; highly sensitive to swelling | Distributed regulatory capacity across cells |
| Membrane Properties | More susceptible to damage during volume changes [9] | Greater resilience to over-rehydration-induced necrosis [13] |
| Key Stress Pathway | Endoplasmic Reticulum (ER) Stress signaling [19] | Metabolic-epigenetic crosstalk disruption [20] |
| Developmental Competence | Compromised maturation and fertilization potential [21] | Disrupted zygotic genome activation (ZGA) [20] |
| Critical Vulnerability | Spindle integrity and cellular organization [9] | Mitochondrial-nuclear communication [20] |
Empirical Evidence from Warming Studies
Clinical and experimental observations consistently demonstrate the heightened vulnerability of oocytes to osmotic stress during warming procedures compared to embryos.
Table 2: Experimental Outcomes from Warming Studies
| Parameter | Vitrified-Warmed Oocytes (CWP) | Vitrified-Warmed Blastocysts |
|---|---|---|
| Survival Rate | 93.7-93.9% [9] | Similar survival with CWP and shortened protocols [13] |
| Normal Fertilization | 79.5-79.6% (vs. 83.0% fresh) [9] | Not applicable |
| Blastocyst Formation | 57.5% (CWP) vs. 77.3% (MWP) [9] | Outgrowth competence not adversely impacted by shortened protocol [13] |
| Developmental Compromise | Higher abnormal fertilization (9.1-10.1% vs. 3.3% fresh) [9] | Metabolic reprogramming and epigenetic dysregulation [20] |
| Key Morphological Impact | Cytoplasmic vacuoles, membrane disruption [9] | Over-rehydration-induced cell necrosis during warming [13] |
A study on donor oocytes revealed that while survival rates after warming were high (93.7-93.9%), vitrified-warmed oocytes showed significantly lower normal fertilization rates (79.5-79.6%) compared to fresh oocytes (83.0%) and higher rates of abnormal fertilization (9.1-10.1% vs. 3.3%) [9]. In contrast, blastocysts subjected to a shortened warming protocol showed maintained "outgrowth competence" despite some observed over-rehydration-induced cell necrosis, indicating their greater resilience [13].
Molecular Mechanisms of Differential Sensitivity
Signaling Pathways in Osmotic Stress Response
The molecular responses to osmotic stress differ fundamentally between oocytes and embryos, engaging distinct cellular machinery and stress pathways.
Figure 1: Distinct Signaling Pathways in Oocyte and Embryo Osmotic Stress Responses
Oocytes primarily activate Endoplasmic Reticulum (ER) Stress signaling when confronted with osmotic stress [19]. This initiates the Unfolded Protein Response (UPR) through PERK, ATF6, and IRE1 pathways, leading to translation inhibition, cell cycle arrest, and potentially apoptosis under severe stress [19]. This pathway is particularly detrimental to oocytes due to their reliance on maternal mRNA stores for developmental competence.
In contrast, early embryos exhibit a more complex metabolic-epigenetic stress response [20]. Osmotic stress disrupts cell volume homeostasis, triggering mitochondria to act as osmotic stress sensors. This leads to PDH inactivation via S293 phosphorylation, blocking pyruvate-to-acetyl-CoA conversion and disrupting metabolic-epigenetic crosstalk [20]. The resulting reduction in H3K4me3 and H3K27ac histone modifications compromises zygotic genome activation (ZGA), inducing developmental arrest [20].
Volume Regulation Mechanisms
The capacity for cell volume regulation represents another fundamental difference between oocytes and embryos. Oocytes possess limited volume regulatory mechanisms compared to embryos. While both utilize organic osmolyte transporters (e.g., GLYT1 for glycine, SIT1 for betaine), embryos demonstrate more robust regulatory capacity [20] [21].
Porcine oocytes benefit significantly from glycine supplementation (1 mM) during in vitro maturation, with stage-dependent adjustment of medium osmolality (290 mOsM for first 22h, then 320 mOsM) improving maturation rates, mitochondrial function, and subsequent embryonic developmental ability [21]. This highlights the critical importance of staged osmotic environments for oocyte competence.
Embryos, particularly at later stages, distribute regulatory capacity across multiple cells. In porcine embryos, physiological-range hyperosmolarity (330 mOsM) under organic osmolyte deficiency triggers developmental arrest at the S phase of the four-cell stage, coinciding with aberrant maternal-to-zygotic transition [20]. This arrest can be rescued by restoring volume homeostasis with organic osmolytes or reactivating PDH via dichloroacetate (DCA) treatment [20].
Experimental Models and Methodologies
Key Research Models and Protocols
Table 3: Experimental Models for Osmotic Stress Research
| Model System | Application | Key Findings | Reference |
|---|---|---|---|
| Porcine Two-Cell Embryo Arrest Model | Hyperosmotic stress (330 mOsM) with organic osmolyte deficiency | Identified mitochondrial role as osmotic stress sensors; metabolic-epigenetic disruption | [20] |
| Donor Oocyte Clinical Trial | Compare conventional vs. modified warming protocols | MWP improved blastocyst formation (77.3% vs. 57.5%) and pregnancy outcomes | [9] |
| Porcine Oocyte IVM Model | Stage-dependent osmolality adjustment (290→320 mOsM) with glycine | Enhanced maturation quality, mitochondrial function, and developmental competence | [21] |
| Mouse Embryonic Stem Cells (ESC) | Pan-stress transcriptomic analysis | Identified conserved stress response pathways across diverse environmental insults | [22] |
| Human Blastocyst Warming | Compare shortened vs. conventional warming protocols | Shortened protocol induced over-rehydration but maintained outgrowth competence | [13] |
Detailed Methodological Approaches
Porcine Embryo Hyperosmotic Stress Model: Researchers established a physiological-range hyperosmotic stress (330 mOsM) model using organic osmolyte-deficient NCSU-23 medium on two-cell porcine embryos [20]. Through single-embryo RNA-seq, RT-qPCR, immunofluorescence (H3K4me3/H3K27ac/H3K9me3/m6A/BrdU), mitochondrial assays (MitoTracker Red, ROS staining), and metabolic analysis (PDH activity, fatty acid oxidation), they identified hyperosmosis-induced developmental impairments [20]. Rescue experiments via organic osmolyte supplementation, PDH modulation, and epigenetic interventions defined the molecular basis of arrest.
Modified Warming Protocol for Oocytes: The modified warming protocol (MWP) applied to vitrified oocytes involves simplified procedures compared to the conventional warming protocol (CWP) [9]. While CWP uses a gradient dilution approach with incubation in dilution solution (DS, 3 min) and wash solution (WS, 5-6 min) at room temperature, the MWP eliminates DS and WS, creating an ultrafast, single-step process with incubation in thawing solution (TS) for 1 minute [9]. This reduced warming time mitigates osmotic stress and improves developmental outcomes.
Stage-Dependent Oocyte Maturation System: For porcine oocyte in vitro maturation, researchers implemented a two-stage system with the first 22 hours at 290 mOsM and the subsequent 22 hours at 320 mOsM, supplemented with 1 mM glycine in PZM-3 medium [21]. Oocytes were assessed for maturation rate, mitochondrial distribution and activity (MitoTracker), transcript levels of glycolysis genes in granulosa cells, and subsequent embryonic developmental ability with ROS measurement after parthenogenetic activation [21].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Osmotic Stress Studies
| Reagent/Chemical | Function in Research | Application Examples |
|---|---|---|
| Raffinose | Non-metabolized osmolyte for precise osmolarity adjustment | Creating hyperosmotic conditions (330 mOsM) in embryo culture [20] [21] |
| Glycine | Organic osmolyte for cell volume regulation | Supplementation (1 mM) in oocyte IVM media to enhance volume homeostasis [21] |
| Dichloroacetate (DCA) | PDH activator, reactivates mitochondrial metabolism | Rescue of hyperosmotic stress-induced developmental arrest in embryos [20] |
| MitoTracker Red | Mitochondrial membrane potential and mass indicator | Assessment of mitochondrial function in stressed oocytes/embryos [20] [21] |
| Betaine | Organic osmolyte, regulates cell volume without ionic disruption | Replacement of inorganic ions to maintain intracellular osmolarity [20] |
| PDH Antibody (p-S293) | Detection of inactive phosphorylated PDH | Monitoring metabolic stress response in embryos [20] |
| H3K4me3/H3K27ac Antibodies | Epigenetic modification markers | Assessment of histone modification changes under osmotic stress [20] |
| RDR 03785 | RDR 03785, MF:C19H18F3NO4, MW:381.3 g/mol | Chemical Reagent |
| EMI56 | EMI56, MF:C21H20N2O3, MW:348.4 g/mol | Chemical Reagent |
The differential sensitivity of oocytes and embryos to osmotic stress stems from fundamental biological distinctions in their stress response pathways, volume regulation mechanisms, and developmental programming. Oocytes predominantly activate ER stress signaling pathways that disrupt protein homeostasis and cell cycle progression, while embryos exhibit more complex metabolic-epigenetic disruptions that compromise mitochondrial function and zygotic genome activation. These differences necessitate stage-specific approaches to osmotic management during ART procedures, particularly in the context of warming protocol optimization. The development of modified warming protocols that account for these distinct biological needs represents a promising avenue for improving oocyte and embryo viability, potentially bridging the current gap in survival and developmental competence between these critical stages of early development.
Cryopreservation has become an indispensable technique in assisted reproductive technology (ART) and fertility preservation. However, the process of warming cryopreserved cells and tissues is equally as critical as the freezing process itself. Suboptimal warming can lead to cryodamage, compromising cellular viability and developmental potential. This guide provides a comprehensive comparison of conventional and modified warming protocols, focusing on their impact on morphological integrity and key indicators of post-warming health. Recent research demonstrates that modified warming protocols (MWP) can significantly enhance outcomes by reducing procedural complexity and mitigating cryodamage, offering promising alternatives to traditional approaches [3].
The assessment of cryodamage requires sophisticated morphological evaluation at both macroscopic and ultrastructural levels. Studies utilizing transmission electron microscopy (TEM) have revealed that even with apparently good survival, cryopreserved oocytes may exhibit subtle cellular alterations including vacuolization, redistribution of organelles, and premature cortical granule exocytosis, which can impair developmental competence [23] [24]. Understanding these indicators is essential for researchers and clinicians aiming to optimize warming protocols for various biological materials.
Conventional vs. Modified Warming Protocols: A Technical Comparison
Fundamental Protocol Differences
Conventional warming protocols (CWP) typically employ a multi-step dilution approach involving sequential exposure to decreasing concentrations of cryoprotectants at room temperature. This method aims to minimize osmotic shock by gradually removing permeating cryoprotectants from cells. A standard CWP for oocytes involves initial rapid warming to 37°C in a thawing solution (approximately 1 minute), followed by incubation in dilution solution (3 minutes) and wash solution (5-6 minutes) at room temperature [3]. This sequential process ensures gradual rehydration and cryoprotectant removal, but extends the total warming time to approximately 10-15 minutes.
In contrast, modified warming protocols represent a paradigm shift toward simplification and efficiency. The MWP evaluated in recent research eliminates the dilution and wash steps, condensing the warming process into an ultrafast, single-step procedure with incubation in thawing solution for just 1 minute at 37°C [3]. This streamlined approach significantly reduces total warming time to approximately 1 minute, potentially minimizing cellular stress during the critical phase transition from vitrified to liquid state.
Impact on Laboratory Workflow
The practical implications of these protocol differences extend beyond cellular outcomes to laboratory efficiency. Conventional protocols require multiple solutions and precise timing adjustments, increasing procedural complexity and potential for technical error. Modified protocols minimize hands-on time and reduce the cognitive load on embryologists, potentially decreasing fatigue and improving overall workflow efficiency [3]. This advantage is particularly valuable in high-throughput ART laboratories where multiple warming procedures may be performed simultaneously.
Table 1: Technical Comparison of Conventional and Modified Warming Protocols
| Parameter | Conventional Warming Protocol | Modified Warming Protocol |
|---|---|---|
| Process Steps | Multiple steps (thawing, dilution, washing) | Single-step process |
| Temperature Management | Varies (room temperature and 37°C) | Consistent 37°C |
| Total Time | ~10-15 minutes | ~1 minute |
| Solution Requirements | Multiple specialized solutions | Simplified solution system |
| Technical Complexity | Higher (multiple transitions) | Lower (minimal transitions) |
Quantitative Outcomes Comparison
Oocyte and Embryo Development Parameters
Recent large-scale comparative analyses provide compelling evidence regarding the efficacy of modified warming protocols. A retrospective cohort study evaluating 13,103 donor oocytes demonstrated that while survival rates were similar between CWP and MWP groups (93.7% vs. 93.9%), significant differences emerged in subsequent development parameters [3]. The blastocyst formation rate was substantially higher in the MWP group (77.3%) compared to the CWP group (57.5%), approaching the rate observed in fresh oocytes (69.2%). Similarly, usable blastocyst formation was significantly enhanced with MWP (51.4%) versus CWP (35.4%) [3].
Fertilization parameters also showed notable differences between protocols. Vitrified-warmed oocytes from both groups exhibited lower normal fertilization rates (79.5-79.6%) compared to fresh oocytes (83.0%), along with higher abnormal fertilization rates (9.1-10.1% vs. 3.3%) [3]. These findings suggest that while cryopreservation itself impacts fertilization competence, the warming protocol can modulate developmental trajectory post-fertilization.
Clinical Outcomes Assessment
The most clinically significant differences between protocols emerge in pregnancy and live birth outcomes. Multivariate analysis of the donor oocyte data revealed a positive association between MWP and ongoing pregnancy/live birth, with an adjusted odds ratio of 1.899 (95% CI: 1.002-3.6) [3]. The ongoing pregnancy/live birth rate was significantly higher in the MWP group (66.7%) compared to the CWP group (50.4%), demonstrating the translational impact of protocol modifications on ultimate success metrics [3].
For blastocyst warming, a prospective cohort study found that a one-step fast warming protocol yielded comparable outcomes to standard warming in terms of survival, pregnancy, implantation, ongoing pregnancy, and live birth rates [6]. This suggests that the advantages of simplified protocols may extend across different developmental stages while maintaining clinical efficacy.
Table 2: Comparative Performance Metrics for Oocyte Warming Protocols
| Outcome Measure | Conventional Warming Protocol | Modified Warming Protocol | Fresh Oocytes (Reference) |
|---|---|---|---|
| Survival Rate | 93.7% | 93.9% | - |
| Blastocyst Formation | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | - |
| Normal Fertilization | 79.5% | 79.6% | 83.0% |
Morphological Indicators of Cryodamage
Ultrastructural Assessment Techniques
Comprehensive morphological assessment of post-warming health requires evaluation beyond light microscopy. Transmission electron microscopy (TEM) studies have revealed subtle but critical indicators of cryodamage in human mature oocytes. These investigations show that properly vitrified and warmed oocytes generally maintain normal organelle distribution, with mitochondria-smooth endoplasmic reticulum (M-SER) aggregates and small mitochondria-vesicle (MV) complexes representing the most numerous cytoplasmic structures [23] [24].
The integrity of cortical granules (CG) serves as a particularly sensitive indicator of cryodamage. Studies comparing slow-frozen/thawed oocytes (SFO) and vitrified/warmed oocytes (VO) have demonstrated abnormally reduced amount and density of cortical granules in both groups compared to fresh controls, irrespective of the protocol applied [23]. This reduction may contribute to zona pellucida hardening through premature exocytosis, potentially impairing fertilization capacity.
Protocol-Specific Morphological Alterations
Different warming protocols induce distinct morphological alterations that correlate with functional outcomes. Slow freezing protocols are associated with slight to moderate vacuolization in the cytoplasm, while vitrification with closed devices produces only slight vacuolization [23]. These vacuoles represent membrane-bound spaces that may disrupt cytoplasmic organization and organelle function.
Prolonged post-warming culture activates intracellular membrane "recycling" that causes abnormal transformation of the membranes of small MV complexes and smooth endoplasmic reticulum into larger rounded vesicles [23]. This phenomenon appears more pronounced in cryopreserved oocytes compared to fresh controls, suggesting compromised membrane stability following warming procedures. The dynamic reorganization of cytoplasmic organelles during extended culture may therefore serve as an indicator of sublethal cryodamage with implications for developmental competence.
Experimental Workflow for Protocol Comparison
Detailed Methodological Approach
The experimental workflow for comparing warming protocols begins with careful oocyte selection and randomization. Studies typically utilize mature metaphase II (MII) oocytes from donor cycles to control for variable oocyte quality [3]. Following protocol assignment, conventional warming employs a multi-step process: rapid warming to 37°C in thawing solution (1 minute), followed by gradient dilution through incubation in dilution solution (3 minutes) and wash solution (5-6 minutes) at room temperature [3]. The modified protocol simplifies this to a single-step process with incubation in thawing solution for 1 minute at 37°C [3].
Post-warming assessment includes immediate survival evaluation based on membrane integrity and morphological normality, followed by fertilization via intracytoplasmic sperm injection (ICSI) [3]. Subsequent embryo culture to blastocyst stage under standardized conditions (37°C, 6.3% CO2, 5% O2) enables comparison of developmental kinetics and blastocyst formation rates [3] [6]. For ultrastructural analysis, samples are prepared for light and transmission electron microscopy using standard fixation, dehydration, and embedding protocols [23].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Warming Protocol Studies
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Cryoprotectant Agents | Ethylene Glycol (EG), Dimethyl Sulfoxide (DMSO), Propanediol (PrOH) | Permeating cryoprotectants that prevent ice crystal formation |
| Non-Permeating Cryoprotectants | Sucrose, Trehalose | Osmotic regulators that facilitate dehydration |
| Base Media | Dulbecco's Modified Eagle Medium (DMEM), Human Tubal Fluid (HTF) | Foundation for preparation of vitrification/warming solutions |
| Protein Supplements | Synthetic Serum Supplement (SSS), Human Serum Albumin (HSA) | Membrane stabilizers and antioxidants in solutions |
| Vitrification/Warming Kits | CryoTouch, Cryotop, CryoTip | Commercial systems providing standardized solutions and devices |
| Viability Assessment Reagents | Hyaluronidase, Methylene Blue | Enzymatic denudation and perfusion tracking |
The comparison between conventional and modified warming protocols reveals a significant evolution in cryopreservation methodology. Modified protocols offer compelling advantages through streamlined processes that reduce technical complexity while maintaining or improving key outcomes including blastocyst formation and ongoing pregnancy rates [3]. The morphological assessment of post-warming health provides critical insights into the subtle manifestations of cryodamage that may not be apparent through conventional survival metrics alone [23] [24].
For researchers and clinicians, the evidence supports consideration of modified warming protocols as viable alternatives to conventional approaches, particularly for oocyte warming where the benefits appear most pronounced. Future protocol development should continue to address the persistent challenges of abnormal fertilization and cytoplasmic alterations observed even with optimized vitrification and warming systems. Through continued refinement of warming techniques and comprehensive morphological assessment, the field can advance toward the ultimate goal of cryopreservation outcomes that mirror fresh specimen performance.
In assisted reproductive technology (ART), the choice of warming protocol for vitrified specimens is not a one-size-fits-all decision. The unique biological and structural characteristics of oocytes and blastocysts demand tailored approaches to post-thaw processing. While recent innovations have introduced simplified, efficient "fast-warming" methods, their impact varies significantly between these two cell types. This guide objectively compares the performance of conventional and modified warming protocols for oocytes and blastocysts, providing researchers and clinicians with evidence-based data to optimize laboratory protocols for each specific cell type.
Table of Comparative Outcomes: Oocytes vs. Blastocysts
The table below summarizes key performance metrics for conventional and modified warming protocols when applied to oocytes and blastocysts, based on recent clinical studies.
| Performance Metric | Oocytes (Conventional Warming) | Oocytes (Modified Warming) | Blastocysts (Conventional Warming) | Blastocysts (One-Step Fast Warming) |
|---|---|---|---|---|
| Survival Rate | 93.7% [3] [9] | 93.9% [3] [9] | 94.2% (Mouse Model) [25] | 97.2% (Mouse Model) [25] |
| Blastocyst Formation Rate | 57.5% [3] [9] | 77.3% [3] [9] | 83.4% (Mouse Model) [25] | 80.9% (Mouse Model) [25] |
| Usable Blastocyst Rate | 35.4% [3] [9] | 51.4% [3] [9] | Information Not Specified | Information Not Specified |
| Ongoing Pregnancy/Live Birth Rate | 50.4% [3] [9] | 66.7% [3] [9] | Comparable to standard [6] | Comparable to standard [6] |
| Protocol Efficiency | Multi-step, time-intensive [3] [9] | Simplified, single-step (1 min in TS) [3] [9] | Multi-step [6] | One-step, significantly shorter duration [6] |
Detailed Experimental Protocols and Data
Oocyte Warming: A Case for the Modified Protocol
A large-scale retrospective cohort study provides robust data on oocyte warming outcomes. The research analyzed 13,103 donor oocytes, comparing a Conventional Warming Protocol (CWP) against a Modified Warming Protocol (MWP) and a fresh oocyte control group [3] [9].
Methodology: Vitrified mature oocytes were warmed using either CWP or MWP. The CWP involved a gradient dilution approach, incubating oocytes in a thawing solution (TS) at 37°C for 1 minute, followed by dilution solution (DS) for 3 minutes and wash solution (WS) for 5-6 minutes at room temperature. The MWP simplified this into an ultrafast, single-step process, eliminating the DS and WS steps and involving incubation in TS only for 1 minute [3] [9]. All warmed oocytes and fresh controls were fertilized via Intracytoplasmic Sperm Injection (ICSI) and cultured to the blastocyst stage.
Key Findings: While survival rates were equivalent, the developmental outcomes diverged significantly. The MWP group showed a dramatically higher blastocyst formation rate (77.3%) and usable blastocyst rate (51.4%) compared to the CWP group (57.5% and 35.4%, respectively). Notably, the MWP outcomes were comparable to those of fresh oocytes (69.2% and 48.5%). Most critically, the ongoing pregnancy/live birth rate was significantly higher in the MWP group (66.7%) than in the CWP group (50.4%) [3] [9]. Multivariate analysis confirmed a positive association between MWP and superior usable blastocyst formation and clinical outcomes [3] [9].
Blastocyst Warming: Where Efficiency Meets Equivalence
Research on blastocyst warming presents a different narrative, where simplification aims to enhance workflow without compromising established clinical outcomes.
Methodology: A prospective cohort study compared a standard warming protocol to a one-step fast-warming protocol for vitrified blastocysts. The study design controlled for variables including maternal age, oocyte origin (donor vs. autologous), number of embryos transferred, and embryo quality [6].
Key Findings: The study concluded that the one-step fast-warming protocol yielded comparable outcomes to the standard protocol across all measured endpoints, including survival, pregnancy, implantation, ongoing pregnancy, and live birth rates [6]. The primary advantage of the fast-warming protocol was practical: a significantly shorter warming duration that enhances laboratory workflow efficiency without adversely affecting clinical results [6]. Preclinical data from animal models further supports that fast warming maintains high blastocyst developmental potential post-warming [25].
Experimental Workflow: Protocol Selection
The following diagram illustrates the decision-making workflow for selecting an appropriate warming protocol based on the cell type and desired outcomes.
The Scientist's Toolkit: Key Research Reagents
The following table details essential reagents used in the warming protocols discussed, along with their critical functions in the process.
| Reagent Solution | Function in Protocol |
|---|---|
| Thawing Solution (TS) | Initial solution for rapid warming to 37°C; prevents ice crystal formation and re-crystallization during the phase transition from vitrified to liquid state [3] [9]. |
| Dilution Solution (DS) | Contains a lower concentration of cryoprotectants; osmotically draws and dilutes cryoprotectants out of the cell to mitigate toxicity, used in multi-step protocols [3] [9]. |
| Wash Solution (WS) | A cryoprotectant-free solution; used for final rinsing to ensure complete removal of cryoprotectants and to fully rehydrate the cell in multi-step protocols [3] [9]. |
| Sucrose | A non-permeating sugar; added to warming solutions to create an osmotic buffer, preventing excessive water influx and potential cell rupture (osmotic shock) during cryoprotectant removal [3] [9]. |
The evidence clearly demonstrates that optimal warming protocol selection is inherently cell-type specific. For oocytes, which are highly sensitive to cryopreservation-induced stress, the modified warming protocol (MWP) is superior. It not only simplifies the laboratory process but also significantly enhances key developmental metrics, including blastocyst formation and ongoing pregnancy rates, making its outcomes comparable to those of fresh oocytes. In contrast, for blastocysts, the one-step fast-warming protocol serves as a highly efficient and safe alternative to conventional methods. It achieves equivalent clinical outcomes while offering significant gains in laboratory workflow efficiency. This comparative analysis underscores the importance of tailoring ART laboratory protocols to the unique biological demands of each cell type to maximize success.
The Role of Post-Warming Culture Duration and Embryo Selection Criteria
Within the realm of assisted reproductive technology (ART), the vitrification and warming of embryos and oocytes have become standard practice, contributing significantly to the cumulative success rates of in vitro fertilization (IVF). The post-warming phase is a critical window, during which cryopreserved cells must recover their metabolic activity and developmental competence. This guide objectively compares two central laboratory strategies: the adjustment of post-warming culture duration and the implementation of modified warming protocols. The conventional paradigm often involved extended culture periods and multi-step warming procedures. However, emerging research is refining these practices, investigating whether shortened culture and simplified, rapid warming protocols can yield equivalent or superior outcomes. This analysis synthesizes current experimental data to compare these approaches, providing researchers and clinicians with evidence-based insights to optimize laboratory protocols and embryo selection criteria.
Comparative Analysis of Post-Warming Culture Durations
The duration for which embryos are cultured in vitro after warming is a subject of ongoing investigation. The central question is whether a prolonged culture, allowing for extended recovery and development, offers advantages over a shorter culture that minimizes ex vivo manipulation.
Key Experiments and Methodologies
Experiment 1: Blastocyst-Stage Transfers A 2020 study compared long-term (20-24 hours) and short-term (2-4 hours) culture of vitrified-warmed blastocysts [26].
- Methodology: This retrospective study analyzed 369 single vitrified-warmed blastocyst transfer (VBT) cycles. Embryo morphology was assessed using a time-lapse monitoring system (Embryoscope; Vitrolife) to track specific morphokinetic parameters, particularly the time to start (tRE) and complete (tCRE) blastocyst re-expansion. Propensity score matching was employed to adjust for confounding factors such as maternal age and endometrial thickness [26].
- Outcome Measures: Primary outcomes were implantation rate (IR) and ongoing pregnancy rate (OPR). Embryo development was graded using a modified Gardner system post-warming [26].
Experiment 2: Cleavage-Stage Transfers A 2023 study evaluated the impact of culture time on vitrified-warmed cleavage-stage embryos [27].
- Methodology: This retrospective cohort study included 777 cycles where day-3 embryos were thawed. Embryos were divided into a long-term culture group (18-20 hours) and a short-term culture group (2-4 hours). Embryo quality was assessed on day 3 based on blastomere number, regularity, and fragmentation. The study used propensity score matching to balance patient characteristics and multivariate logistic regression to identify factors affecting clinical pregnancy [27].
- Outcome Measures: The primary outcome was clinical pregnancy rate. Secondary outcomes included implantation rate, miscarriage rate, and ongoing pregnancy rate [27].
Table 1: Clinical Outcomes of Long-Term vs. Short-Term Post-Warming Culture
| Outcome Measure | Blastocyst-Stage (Long-term: 20-24h) | Blastocyst-Stage (Short-term: 2-4h) | P-value | Cleavage-Stage (Long-term: 18-20h) | Cleavage-Stage (Short-term: 2-4h) | P-value |
|---|---|---|---|---|---|---|
| Implantation Rate | 56.3% | 67.9% | 0.182 [26] | 25.46% | 23.98% | N/S [27] |
| Ongoing Pregnancy Rate | 47.3% | 53.6% | 0.513 [26] | 76.2%* | 77.15%* | N/S [27] |
| Clinical Pregnancy Rate | Not Reported | Not Reported | - | 35.74% | 29.79% | N/S [27] |
| Miscarriage Rate | Not Reported | Not Reported | - | 25.0% | 22.85% | N/S [27] |
Note: N/S = Not Statistically Significant; *Ongoing Pregnancy Rate in the cleavage-stage study was calculated as a percentage of clinical pregnancies [27].
Critical Analysis of Findings
The data from both blastocyst and cleavage-stage studies consistently demonstrate that prolonging post-warming culture does not significantly enhance key clinical outcomes such as implantation, clinical pregnancy, or ongoing pregnancy rates [26] [27]. This suggests that the critical events determining an embryo's implantation potential may occur within the first few hours after warming.
A pivotal finding from the blastocyst study is the importance of early re-expansion. The research revealed that the time to complete re-expansion (tCRE) was significantly shorter in women who achieved pregnancy, regardless of their assigned culture group (long-term: 2.19±0.63 vs. 4.11±0.81 hours, p=0.003; short-term: 1.17±0.29 vs. 1.94±0.76 hours, p=0.018) [26]. This positions rapid re-expansion, observable within 3-4 hours, as a potent and non-invasive selection marker superior to culture duration. For cleavage-stage embryos, extended culture allowed for the identification of embryos that continued to develop (e.g., reaching the morula stage), which was associated with higher implantation and clinical pregnancy rates within the long-term group [27]. This indicates that the utility of long-term culture may lie more in its prognostic value for identifying embryos with higher developmental potential, rather than in actively improving outcomes for all embryos.
Comparative Analysis of Conventional vs. Modified Warming Protocols
Beyond culture duration, the technical protocol used for warming itself is a critical variable. Conventional warming protocols (CWP) are multi-step processes designed to minimize osmotic shock. In contrast, modified warming protocols (MWP) streamline these procedures, significantly reducing processing time.
Key Experiments and Methodologies
Experiment 1: Oocyte Warming and Donor Cycles A 2025 study investigated the impact of an MWP on the developmental potential of vitrified donor oocytes [3].
- Methodology: This retrospective cohort study analyzed over 13,000 donor oocytes, divided into CWP, MWP, and fresh control groups. The MWP simplified the process by eliminating the dilution solution (DS) and wash solution (WS) steps, effectively creating an ultrafast, single-step process. Key metrics included survival, fertilization, blastocyst formation, and ongoing pregnancy/live birth rates [3].
- Outcome Measures: Primary outcomes were blastocyst formation rate and ongoing pregnancy/live birth rate [3].
Experiment 2: One-Step Fast Blastocyst Warming A 2025 prospective cohort study directly compared a one-step fast-warming protocol to a standard protocol for vitrified-warmed blastocysts [6].
- Methodology: The study included 802 cycles, with strict controls for maternal age, oocyte source (donor/autologous), and embryo quality. The one-step protocol reduced the warming procedure to a single solution and a drastically shorter time. The control group underwent the clinic's standard multi-step warming protocol [6].
- Outcome Measures: Outcomes included survival rate, pregnancy rate, clinical pregnancy rate, implantation rate, and live birth rate [6].
Experiment 3: Multi-Center Cleavage and Blastocyst Warming A 2025 multi-center study compared a fast one-step warming protocol with a long protocol for both cleavage-stage and blastocyst-stage embryos [28].
- Methodology: This study compared a new fast protocol (Group 2, n=413) against a conventional long protocol (Group 1, n=486) across two IVF centers. The primary outcome was the total pregnancy rate, with secondary outcomes including survival, miscarriage, and the mean time required for the warming procedure [28].
- Outcome Measures: Total pregnancy rate, clinical pregnancy rate, miscarriage rate, and procedure time [28].
Table 2: Laboratory and Clinical Outcomes of Conventional vs. Modified Warming Protocols
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | P-value | Fresh Control |
|---|---|---|---|---|
| Oocyte Survival Rate | 93.7% | 93.9% | >0.05 [3] | - |
| Usable Blastocyst Formation | 35.4% | 51.4% | <0.05 [3] | 48.5% |
| Ongoing Pregnancy/Live Birth | 50.4% | 66.7% | <0.05 [3] | Not Reported |
| Blastocyst Survival Rate | 97.6% [6] | 98.3% [6] | N/S [6] | - |
| Live Birth Rate | 29.8% [6] | 28.3% [6] | N/S [6] | - |
| Miscarriage Rate | 32.3% [28] | 18.0% [28] | 0.009 [28] | - |
Note: N/S = Not Statistically Significant.
Critical Analysis of Findings
The evidence indicates that modified warming protocols are, at a minimum, equivalent to conventional protocols in terms of survival and key pregnancy outcomes, while offering significant practical advantages [6] [28]. In some cases, MWPs may even yield superior embryological and clinical results. For oocytes, the MWP led to significantly higher rates of usable blastocyst formation and ongoing pregnancy/live birth, bringing the outcomes to a level comparable with fresh oocytes [3]. This challenges the notion that oocytes are too sensitive for simplified protocols.
A critical finding across studies is the significant reduction in miscarriage rates associated with faster warming protocols. One study reported a miscarriage rate of 18.0% for the fast protocol versus 32.3% for the conventional protocol (p=0.009) [28]. This suggests that reducing procedural time and handling may enhance embryonic health and endometrial synchronicity, potentially leading to more robust pregnancies. Furthermore, the dramatic reduction in warming procedure time is a consistent and crucial benefit, reducing technical workload and potential for error [28].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials used in the cited experiments, which are essential for conducting research in embryo vitrification and warming.
Table 3: Key Research Reagent Solutions and Their Functions
| Reagent/Material | Function in Protocol | Example from Literature |
|---|---|---|
| Equilibration Solution (ES) | Initial exposure to lower concentrations of cryoprotectants (CPAs) to permit partial cellular dehydration and CPA penetration. | HEPES medium with 20% HSA, 7.5% EG, and 7.5% DMSO [26]. |
| Vitrification Solution (VS) | Final solution with high CPA concentrations; embryos are loaded onto a device and plunged into LNâ‚‚ for glass-like solidification. | Solution with 15% EG, 15% DMSO, and 0.5 M sucrose [26]. Kitazato Cryotop Safety Kit [27]. |
| Thawing Solution (TS) | First warming solution with high sucrose concentration to initially remove CPAs while controlling rehydration. | Sucrose-based solution (1.0 M) [27] [6]. |
| Dilution Solution (DS) | Solution with lower sucrose concentration for further CPA removal and gradual rehydration. | Sucrose-based solution (0.5 M) [27]. |
| Wash Solution (WS) | CPA-free solution to finalize washing and prepare the embryo for culture. | Sucrose-free medium [27]. |
| Culture Media (G-1/G-2 Plus) | Sequential media used to support embryo development in vitro post-warming. | G-1 Plus and G-2 Plus media (Vitrolife) [27]. |
| Time-Lapse Incubator | Provides continuous, uninterrupted culture environment and allows for morphokinetic analysis without disturbing embryos. | Embryoscope (Vitrolife) [26]. |
| Vitrification Device | Physical carrier (e.g., grid, straw, top) for holding the embryo during ultra-rapid cooling in LNâ‚‚. | EM Grid (SPI Supplies) [26] or Cryotop (Kitazato) [27]. |
Visualizing Experimental Workflows and Decision Pathways
Comparative Workflow: Conventional vs. Modified Warming Protocol
The following diagram illustrates the key procedural differences between conventional multi-step and simplified one-step warming protocols, highlighting where time savings are achieved.
Embryo Selection Pathway Post-Warming
This decision pathway outlines the critical criteria for selecting embryos with high implantation potential based on post-warming observations, integrating findings from the cited research.
The synthesis of current research indicates a paradigm shift in laboratory strategies for frozen embryo transfer. The evidence strongly suggests that prolonged post-warming culture does not inherently improve clinical outcomes for blastocysts or cleavage-stage embryos [26] [27]. Instead, the focus should be on dynamic, early morphological assessment, such as the timing of blastocyst re-expansion, which serves as a more powerful, non-invasive selection marker [26]. Concurrently, modified, one-step warming protocols have demonstrated equivalence to conventional methods in survival and live birth rates for blastocysts [6], with some studies showing superior blastocyst formation and reduced miscarriage rates [3] [28]. For oocytes, MWPs can produce results on par with fresh cycles [3].
The convergence of these two strands of research points to a future of more efficient and potentially more effective ART laboratory practices. The combination of a fast, simplified warming protocol that minimizes cellular stress, followed by a short but intensive observation period to identify embryos with rapid re-expansion, represents a data-driven strategy. This approach not only aligns with positive clinical outcomes but also enhances laboratory workflow efficiency by reducing both procedure time and the total culture period before transfer. For researchers and clinicians, the imperative is to look beyond static morphological grading and standardized long cultures, and to instead integrate these dynamic assessments and optimized protocols to fully leverage the potential of vitrified-warmed embryos.
Data-Driven Validation: Comparative Analysis of Laboratory and Clinical Outcomes
Oocyte vitrification is a cornerstone of modern assisted reproductive technology (ART), crucial for fertility preservation and egg donation programs. [3] The warming process is a critical step, with conventional protocols being complex and time-intensive. Recent research focuses on modifying these protocols to enhance laboratory efficiency without compromising clinical outcomes. This guide provides a comparative analysis of a Modified Warming Protocol (MWP) against the Conventional Warming Protocol (CWP), presenting objective experimental data to highlight significant improvements in blastocyst formation and pregnancy rates.
Experimental Protocols & Methodologies
Source of Oocytes and Study Design
The primary data for this comparison is drawn from a large-scale retrospective cohort study performed at Lee Women’s Hospital, Taiwan. [3] The study analyzed 13,103 donor oocytes, divided into three distinct groups:
- CWP Group (n=8,506): Oocytes warmed using the conventional protocol.
- MWP Group (n=980): Oocytes warmed using the modified protocol.
- Fresh Group (n=3,617): A control group of fresh oocytes for baseline comparison.
All vitrified oocytes were thawed, fertilized via Intracytoplasmic Sperm Injection (ICSI), and cultured to the blastocyst stage. Blastocysts meeting morphological criteria on day 5 or 6 were selected for transfer or cryopreservation. [3]
Detailed Warming Procedures
The core difference between the two protocols lies in the simplification and optimization of the warming steps.
Conventional Warming Protocol (CWP): This method involves a gradient dilution approach. After rapid warming to 37°C in a thawing solution (TS), oocytes are incubated in a dilution solution (DS) for 3 minutes and then in a wash solution (WS) for 5-6 minutes at room temperature to mitigate osmotic stress. [3]
Modified Warming Protocol (MWP): This protocol simplifies the process into an ultrafast, single-step procedure. It eliminates the separate DS and WS steps, incubating oocytes directly in TS for 1 minute. This reduction in processing time aims to minimize laboratory handling and potential stress on the oocytes. [3]
The following workflow diagram illustrates the key procedural differences between the two protocols:
Comparative Outcome Data
The outcomes from the aforementioned study are summarized in the table below, providing a direct comparison of key performance metrics between CWP, MWP, and fresh oocytes.
Table 1: Comparative Laboratory and Clinical Outcomes of Oocyte Warming Protocols
| Outcome Measure | Conventional Warming Protocol (CWP) | Modified Warming Protocol (MWP) | Fresh Oocytes (Control) |
|---|---|---|---|
| Survival Rate | 93.7% (7967/8506) | 93.9% (920/980) | Not Applicable |
| Post-ICSI Degeneration Rate | 3.4% (268/7967) | 2.7% (25/920) | 2.8% (60/2106) |
| Normal Fertilization Rate | 79.5% | 79.6% | 83.0% |
| Blastocyst Formation Rate | 57.5% | 77.3% | 69.2% |
| Usable Blastocyst Formation Rate | 35.4% | 51.4% | 48.5% |
| Ongoing Pregnancy/Live Birth Rate | 50.4% | 66.7% | Not Reported |
Analysis of Key Findings
- Efficiency and Viability: The MWP achieved a significantly higher blastocyst formation rate (77.3%) compared to both the CWP (57.5%) and even the fresh oocyte control group (69.2%). [3]
- Clinical Success: The most critical clinical outcome, ongoing pregnancy/live birth rate, was 66.7% in the MWP group, a statistically significant improvement over the 50.4% rate in the CWP group. [3]
- Multivariate Analysis: After adjusting for confounding variables, the MWP showed a strong positive association with both usable blastocyst formation and ongoing pregnancy/live birth, with adjusted odds ratios of 1.423 and 1.899, respectively. [3]
The Scientist's Toolkit: Key Research Reagents
Successful implementation of vitrification and warming protocols depends on specific laboratory reagents. The table below details essential solutions and their functions based on the cited research.
Table 2: Essential Reagents for Oocyte Vitrification and Warming
| Reagent | Function in Protocol |
|---|---|
| Vitrification Solution (VS) | High-concentration cryoprotectant solution used during freezing to achieve a glass-like state, preventing ice crystal formation. [3] |
| Thawing Solution (TS) | Initial warming solution used to rapidly raise temperature and begin dilution of cryoprotectants. [3] |
| Dilution Solution (DS) | Used in CWP to gradually reduce cryoprotectant concentration and minimize osmotic shock. [3] |
| Wash Solution (WS) | Final solution in CWP for removing residual cryoprotectants and preparing oocytes for culture. [3] |
| Fatty Acid-Supplemented Solutions | Culture or warming solutions enriched with fatty acids; some studies suggest they may mitigate cold shock, though their advantage may be protocol-dependent. [13] |
Mechanisms and Considerations
Protocol Superiority and Potential Risks
The superior performance of the MWP is attributed to its ability to reduce procedural complexity and minimize the time oocytes are exposed to in-vitro conditions, thereby lessening cumulative stress. [3] However, it is important to consider that one in-vitro experimental study on blastocysts (not oocytes) found that a shortened warming protocol could induce over-rehydration-induced cell necrosis during the warming process. Interestingly, that same study noted that the blastocysts' ultimate ability to implant (outgrowth competence) was not adversely impacted. [13] This highlights the need for careful optimization when adapting protocols for different cell types.
Impact of External Stressors
While not directly part of the warming protocol, research into environmental stressors provides crucial context for oocyte sensitivity. Studies on heat stress in sheep demonstrate that elevated temperatures significantly compromise oocyte and cumulus cell viability, DNA integrity, mitochondrial distribution, and subsequent blastocyst quality. [29] This underscores the high sensitivity of oocytes to various physical stresses and reinforces the importance of optimizing all handling procedures, including warming.
Evidence from a large-scale clinical study demonstrates that the Modified Warming Protocol (MWP) for vitrified oocytes surpasses the Conventional Warming Protocol (CWP). The MWP not only simplifies laboratory workflow but also significantly enhances key embryological and clinical outcomes, including blastocyst formation rates and ongoing pregnancy/live birth rates. The data suggests that the MWP can achieve results comparable to, and in some aspects superior to, fresh oocyte cycles, positioning it as a new standard for optimizing outcomes in donor and fertility preservation cycles.
The vitrification of oocytes and embryos is a cornerstone of modern assisted reproductive technology (ART), essential for fertility preservation and egg donation programs. The conventional warming protocol (CWP) for these cryopreserved cells, while effective, is a complex, multi-step process designed to minimize osmotic shock and cryoprotectant (CPA) toxicity during rehydration. Recent innovations have focused on simplifying this procedure, leading to the development of one-step or modified warming protocols (MWP). These ultrafast methods significantly reduce processing time. A critical question has emerged from their adoption: can these streamlined protocols maintain, or even improve, key embryological and clinical outcomes? A growing body of research confirms that one-step warming protocols yield survival and live birth rates that are non-inferior to conventional methods, while also enhancing laboratory efficiency.
Comparative Analysis of Warming Protocol Outcomes
The following tables synthesize key quantitative findings from recent clinical studies, comparing the one-step/modified warming protocol against the conventional warming protocol across different stages of embryonic development.
Table 1: Outcomes of Oocyte Warming using Conventional vs. Modified Protocols
| Outcome Measure | Conventional Warming Protocol (CWP) | One-Step/Modified Warming Protocol (MWP) | Fresh Oocytes (Reference) |
|---|---|---|---|
| Oocyte Survival Rate | 93.7% (7967/8506) [3] [9] | 93.9% (920/980) [3] [9] | Not Applicable |
| Normal Fertilization Rate | 79.5% [3] [9] | 79.6% [3] [9] | 83.0% [3] [9] |
| Blastocyst Formation Rate | 57.5% [3] [9] | 77.3% [3] [9] | 69.2% [3] [9] |
| Usable Blastocyst Formation Rate | 35.4% [3] [9] | 51.4% [3] [9] | 48.5% [3] [9] |
| Ongoing Pregnancy/Live Birth Rate | 50.4% [3] [9] | 66.7% [3] [9] | Not Reported |
Table 2: Outcomes of Blastocyst Warming using Conventional vs. One-Step Protocols
| Outcome Measure | Conventional Multi-Step Warming | One-Step Fast Warming | Study Details |
|---|---|---|---|
| Blastocyst Survival Rate | 100% (376/376) [30] | 100% (376/376) [30] | Phase 2 Clinical Evaluation |
| Clinical Pregnancy Rate | 57.36% [8] | 56.86% [8] | Prospective Cohort (n=802 FET) |
| Ongoing Pregnancy Rate | 51.12% [8] | 50.62% [8] | Prospective Cohort (n=802 FET) |
| Live Birth Rate | 51.12% [8] | 49.38% [8] | Prospective Cohort (n=802 FET) |
| Miscarriage Rate | 32.3% [28] | 18.0% [28] | Multi-Center Study (n=899 cycles) |
Detailed Experimental Protocols
To understand the mechanistic basis for these outcomes, a detailed examination of the methodologies used in key studies is essential.
Protocol for Vitrified Oocytes
A large retrospective cohort study on vitrified donor oocytes provided the data comparing the MWP to the CWP [3] [9].
- Conventional Warming Protocol (CWP): This process involved multiple steps at different temperatures. Warmed oocytes were first placed in a Thawing Solution (TS) at 37°C for 1 minute. They were then transferred to a Dilution Solution (DS) for 3 minutes at room temperature, followed by a Wash Solution (WS) for 5-6 minutes, also at room temperature. This gradient dilution approach aimed to minimize osmotic stress during CPA removal [3] [9].
- Modified Warming Protocol (MWP): This simplified, ultrafast protocol eliminated the DS and WS steps. Oocytes were warmed by exposure only to the Thawing Solution (TS) at 37°C for 1 minute before being rinsed and placed into culture media [3] [9]. The study concluded that the MWP not only simplified the process but also significantly enhanced blastocyst formation potential and ongoing pregnancy rates, making outcomes comparable to those from fresh oocytes.
Protocol for Vitrified Blastocysts
Multiple studies have validated a one-step warming protocol for blastocysts, demonstrating non-inferior outcomes compared to the standard method.
- Standard Warming (SW) Protocol: The multi-step process included: 1 minute in 1M sucrose Thaw Solution at 37°C; 4 minutes in a 0.5M sucrose Dilution Solution at room temperature; two 4-minute rinses in a Wash Solution at room temperature; and finally, placement into culture media [30].
- Single-Step (SS) Warming Protocol: This streamlined method required only exposure to the same 1M sucrose Thaw Solution at 37°C for 1 minute, followed by a vigorous rinse through five drops of culture media before incubation [30]. External validation research from Massachusetts General Hospital confirmed that this SS protocol provided similar survival, implantation, clinical pregnancy, and live birth rates compared to SW [30]. A separate prospective cohort study further confirmed that the one-step protocol showed no significant differences in clinical pregnancy, ongoing pregnancy, or live birth rates [8].
The Scientist's Toolkit: Key Research Reagents
The execution of these warming protocols relies on a specific set of laboratory reagents and materials. The following table details essential components and their functions in the vitrification and warming processes.
Table 3: Essential Reagents for Vitrification and Warming Protocols
| Reagent / Material | Function in Protocol |
|---|---|
| Sucrose Solutions (e.g., 1M, 0.5M) | Acts as an osmotic buffer during warming; the high concentration in the Thawing Solution draws cryoprotectants out slowly to prevent osmotic shock [30]. |
| Thawing Solution (TS) | Typically contains 1M sucrose and supplements; the primary solution for the initial, rapid warming of vitrified oocytes/embryos [3] [30]. |
| Dilution Solution (DS) | Contains a lower sucrose concentration (e.g., 0.5M); used in conventional protocols for further cryoprotectant removal [3] [30]. |
| Wash Solution (WS) | Sucrose-free solution; used in the final steps of conventional protocols to fully remove cryoprotectants and rehydrate the cell [3] [30]. |
| Culture Media (e.g., Continuous Single Culture-NX Complete) | A nutrient-rich medium used to sustain the embryo after warming and during subsequent culture prior to transfer [30]. |
| Vitrification Solution (VS) | A solution with high concentrations of permeating cryoprotectants (e.g., ethylene glycol, DMSO) and sucrose, used to dehydrate cells and enable glass-like solidification during freezing [3] [9]. |
Implications for Clinical Practice and Research
The validated non-inferiority of one-step warming protocols has significant practical implications for ART laboratories. The most immediate benefit is a substantial increase in operational efficiency. The single-step protocol saves at least 15 minutes per cryothaw procedure compared to the conventional multi-step method [30]. This time saving reduces embryologist fatigue and allows a laboratory to perform more frozen embryo transfer procedures per day without expanding staff. Ultimately, this increased throughput can lead to a shorter time to pregnancy for patients, as there are fewer delays in cycle scheduling [30].
Furthermore, the improved blastocyst formation and ongoing pregnancy rates observed with the MWP for oocytes suggest that the simplified protocol may be superior in specific applications [3] [9]. The morphological analysis indicating a more intact cell membrane and less cytoplasmic swelling in MWP oocytes points to reduced cellular stress, which may underlie these enhanced developmental outcomes [9]. For neonatal outcomes, a large-scale study of 1,266 healthy infants born after one-step warming of blastocysts reported an average gestational age of 37.6 weeks and an average birth weight of 3267 grams, providing further reassurance of the protocol's safety [31]. As the demand for assisted reproduction continues to grow, the adoption of these efficient and effective warming protocols is a critical step toward optimizing laboratory workflows and maintaining high clinical success rates.
Within the field of assisted reproductive technology (ART), the vitrification of oocytes and embryos has become a cornerstone technique, particularly for fertility preservation and donor egg programs [3] [9]. The post-warming survival and subsequent developmental potential of these cryopreserved specimens are critically dependent on the warming protocol used. For years, conventional warming protocols (CWP) involving multi-step dilution of cryoprotectants have been the standard. However, these protocols are complex and time-intensive [9].
Recent research has focused on simplifying this process, leading to the development of modified warming protocols (MWP) that significantly reduce processing time. While these ultrafast methods have shown promise for embryos, their application to the more sensitive oocytes has been less clear [3] [9]. This guide provides a objective, data-driven comparison of these two approaches, analyzing key efficacy endpoints from recent clinical studies to determine the optimal warming strategy for vitrified oocytes and blastocysts.
Statistical Comparison of Efficacy Endpoints
Oocyte Warming Outcomes
The following table summarizes the primary outcomes from a large-scale retrospective cohort study comparing Conventional (CWP) and Modified Warming Protocols (MWP) for vitrified donor oocytes, with fresh oocytes included as a reference [3] [9].
| Efficacy Endpoint | CWP Group | MWP Group | Fresh Oocyte Group |
|---|---|---|---|
| Survival Rate (%) | 93.7 | 93.9 | Not Applicable |
| Oocyte Degeneration post-ICSI (%) | 3.4 | 2.7 | 2.8 |
| Normal Fertilization (%) | 79.6 | 79.5 | 83.0 |
| Abnormal Fertilization (%) | 10.1 | 9.1 | 3.3 |
| Blastocyst Formation Rate (%) | 57.5 | 77.3 | 69.2 |
| Usable Blastocyst Formation Rate (%) | 35.4 | 51.4 | 48.5 |
| Ongoing Pregnancy/Live Birth Rate (%) | 50.4 | 66.7 | Not Reported |
Note: CWP: Conventional Warming Protocol; MWP: Modified Warming Protocol; ICSI: Intracytoplasmic Sperm Injection [3] [9]
Key Findings: The data reveals that while survival and initial fertilization rates are nearly identical between the two vitrification groups, the MWP group demonstrates a statistically superior performance in key developmental metrics. The blastocyst formation rate and usable blastocyst formation rate for the MWP group (77.3% and 51.4%, respectively) not only surpass the CWP group (57.5% and 35.4%) but also closely mirror the outcomes of the fresh oocyte group (69.2% and 48.5%). This enhanced embryonic development translates to a significantly higher clinical outcome, with the ongoing pregnancy/live birth rate being 16.3% absolute higher in the MWP group (66.7% vs. 50.4%) [3] [9]. Multivariate analysis confirmed a positive association between MWP and usable blastocyst formation (aIRR=1.423, 95% CI: 1.268-1.597, P<0.001) as well as ongoing pregnancy/live birth (aOR=1.899, 95% CI: 1.002-3.6, P<0.05) [3].
Blastocyst Warming Outcomes
For vitrified blastocysts, the evidence supports the non-inferiority of simplified, fast-warming protocols. The table below compares a one-step fast-warming protocol to the standard protocol [6].
| Efficacy Endpoint | Standard Warming Protocol | One-Step Fast-Warming Protocol |
|---|---|---|
| Survival Rate | Comparable | Comparable |
| Pregnancy Rate | Comparable | Comparable |
| Clinical Pregnancy Rate | Comparable | Comparable |
| Implantation Rate | Comparable | Comparable |
| Ongoing Pregnancy Rate | Comparable | Comparable |
| Live Birth Rate | Comparable | Comparable |
| Practical Workflow | Complex, multi-step (10-12 minutes) | Simplified, single-step (~2 minutes) |
Note: The study concluded that the one-step fast-warming protocol yielded comparable outcomes across all clinical metrics while offering significant practical advantages [6].
Key Findings: A prospective cohort study by Karagianni et al. (2025) found no statistically significant differences in survival, pregnancy, implantation, ongoing pregnancy, or live birth rates between the standard and one-step fast-warming protocols for vitrified blastocysts [6]. This clinical equivalence, combined with the dramatic reduction in warming time from over 10 minutes to approximately 2 minutes, presents a compelling case for the adoption of simplified protocols for blastocyst warming [32] [6]. This efficiency gain can save 8-11 minutes per blastocyst, reducing embryologist fatigue and optimizing laboratory workflow [32].
Experimental Protocols & Methodologies
Detailed Workflow: Conventional vs. Modified Oocyte Warming
The core difference between the protocols lies in the number and duration of steps required to remove cryoprotectants and rehydrate the cell. The following diagram illustrates the key steps of the conventional multi-step method versus the simplified ultrafast approach for oocytes.
Protocol Steps in Detail
- Conventional Warming Protocol (CWP) for Oocytes: This is a multi-step, gradient dilution process. The oocyte is first incubated in a Thawing Solution (TS) at 37°C for 1 minute. It is then moved sequentially to a Dilution Solution (DS) for 3 minutes at room temperature, and finally through one or more Wash Solutions (WS) for 5-6 minutes, also at room temperature. This gradual process aims to minimize osmotic shock by slowly reducing the concentration of cryoprotectants inside the cell [9].
- Modified Warming Protocol (MWP) for Oocytes: This is an ultrafast, single-step process. The protocol eliminates the need for the DS and WS steps. The oocyte is warmed directly in a TS at 37°C for 1 minute, after which it is washed and placed in culture medium. This simplification reduces the total warming and rehydration time from approximately 10 minutes to just over 1 minute, thereby reducing handling and potential stress on the oocyte [3] [9].
- One-Step Fast-Warming for Blastocysts: The protocol for blastocysts follows a similar simplified principle. As commercialized in products like Ultra RapidWarm Blast, the blastocyst is placed in a single warming solution containing 0.25M sucrose at 37°C for 2 minutes. After this brief incubation, it is washed in culture medium and is ready for transfer or further culture. This represents a significant time saving compared to conventional 3-step warming protocols that can take 10-12 minutes [32] [6].
The Scientist's Toolkit: Key Research Reagents
The successful implementation of modified warming protocols relies on specific laboratory reagents and tools. The following table details essential components and their functions in the vitrification and warming workflow.
| Reagent / Tool | Primary Function | Application Note |
|---|---|---|
| Vitrification Solution (VS) | High-concentration cryoprotectant solution that enables glass-like solidification during ultra-rapid cooling, preventing ice crystal formation [9]. | Typically contains a mix of permeating (e.g., DMSO, ethylene glycol) and non-permeating (e.g., sucrose) cryoprotectants. |
| Thawing Solution (TS) | Primary warming medium used to rapidly thaw the sample and initiate cryoprotectant dilution. Serves as the sole medium in the one-step MWP [9] [32]. | In MWP, this solution is used alone. Its composition, often including a low sucrose concentration (e.g., 0.25M), is critical for reducing osmotic shock [32]. |
| Dilution Solution (DS) | Medium with an intermediate solute concentration to gradually dilute intracellular cryoprotectants. Used in CWP but omitted in MWP [9]. | Helps in the step-wise reduction of cryoprotectant concentration to prevent massive water influx and membrane rupture. |
| Wash Solution (WS) | A final solution with minimal or no cryoprotectants to fully remove residual chemicals and complete oocyte/blastocyst rehydration. Used in CWP but omitted in MWP [9]. | Ensures a clean, stable environment for the cell before being returned to culture conditions. |
| Hyaluronan-Enriched Transfer Medium | A specialized embryo transfer medium containing high concentrations of hyaluronan. | Shown to significantly increase clinical pregnancy and live birth rates. It may provide additional protection against cryodamage and improve cryo-survivability [32]. |
The statistical evidence from recent clinical studies indicates a paradigm shift in warming strategies for cryopreserved reproductive cells. For vitrified oocytes, the modified warming protocol does not merely offer a faster laboratory workflow but is associated with significantly superior biological and clinical outcomes. The data shows a marked improvement in blastocyst formation potential and ongoing pregnancy/live birth rates, making the developmental potential of vitrified-warmed oocytes comparable to that of fresh oocytes [3] [9]. This suggests that the MWP may be less stressful to the delicate oocyte, better preserving its developmental competence.
For vitrified blastocysts, the evidence consistently supports the non-inferiority of one-step fast-warming protocols compared to conventional multi-step methods across all key efficacy endpoints, including survival, implantation, and live birth rates [6]. The primary advantage here is a dramatic improvement in laboratory efficiency, saving valuable time and reducing procedural complexity without compromising clinical success [32] [6].
In conclusion, the head-to-head comparison of key efficacy endpoints strongly supports the adoption of modified, simplified warming protocols in clinical practice. For oocytes, the MWP appears to enhance outcomes and should be considered a new standard. For blastocysts, ultra-fast protocols provide equal efficacy with superior efficiency. These advancements represent a significant step forward in optimizing outcomes in assisted reproduction and fertility preservation.
Within the broader research context of conventional versus modified warming protocol outcomes, a critical layer of analysis involves understanding how these protocols perform across distinct patient and cycle characteristics. The efficacy of assisted reproductive technology (ART) is not uniform; it is significantly influenced by individual patient profiles and specific laboratory techniques. This guide provides an objective, data-driven comparison of key performance metrics, focusing on the interplay between warming protocols and crucial variables such as maternal age, embryo quality, and fertilization methods. The analysis is synthesized from recent, high-quality scientific literature to support researchers and clinicians in making evidence-based decisions and guiding future drug and protocol development. By dissecting outcomes across these subgroups, we can move towards more personalized and effective fertility treatments.
Methodological Frameworks for Comparative Analysis
Experimental Designs in Cited Literature
The data presented in this guide are drawn from robust retrospective cohort studies, which provide real-world insights into the performance of different ART techniques.
Study on Modified Warming Protocol (MWP) for Oocytes [3] [9]: This research compared a Modified Warming Protocol (MWP) against a Conventional Warming Protocol (CWP) and fresh oocyte cycles. The study involved 13,103 donor oocytes, divided into three groups: CWP (n=8,506), MWP (n=980), and fresh (n=3,617). The primary outcomes measured were oocyte survival post-warming, fertilization rates, blastocyst formation, and ongoing pregnancy/live birth rates. The use of donor oocytes helped control for variability in maternal age and ovarian reserve.
Study on Maternal Age and Embryo Quality [33]: This retrospective analysis of 1,031 frozen-thawed embryo transfer (FET) cycles investigated the effects of maternal age, the number of transferred embryos, and embryo quality on pregnancy outcomes. Cycles were categorized into pregnant and non-pregnant groups for comparison, and subgroup analyses were performed based on patient age and the quality of embryos transferred.
Study on Fertilization Methods in PGT-A Cycles [34]: This large retrospective cohort study compared conventional in vitro fertilization (c-IVF) and intracytoplasmic sperm injection (ICSI) in 578 matched PGT-A cycles for couples with non-male factor infertility. The matching criteria included maternal age, number of oocytes retrieved, and progressive motile sperm count. Key outcomes included fertilization rates, blastocyst formation, and euploidy rates.
Analytical and Statistical Approaches
The cited studies employed rigorous statistical methods to ensure the reliability of their findings. These included:
- Multivariate Analysis: Used to adjust for potential confounding factors and isolate the independent effect of the intervention (e.g., MWP) on outcomes like usable blastocyst formation and ongoing pregnancy [3] [9].
- Comparative Group Statistics: Student's t-tests, chi-square tests, and ANOVA were used to compare continuous and categorical variables between groups (e.g., pregnant vs. non-pregnant) [33].
- Regression Models: Logistic regression was utilized to calculate adjusted odds ratios, providing a measure of association that accounts for other variables [34].
Comparative Data on Critical Performance Subgroups
Performance by Warming Protocol and Embryo Quality
The choice of warming protocol exhibits a significant interaction with the quality of the embryos being warmed, particularly affecting blastocyst development and live birth outcomes.
Table 1: Impact of Warming Protocol and Embryo Quality on Outcomes
| Subgroup / Protocol | Blastocyst Formation Rate | Usable Blastocyst Formation Rate | Ongoing Pregnancy / Live Birth Rate |
|---|---|---|---|
| Donor Oocytes (MWP) [3] [9] | 77.3% | 51.4% | 66.7% |
| Donor Oocytes (CWP) [3] [9] | 57.5% | 35.4% | 50.4% |
| Donor Oocytes (Fresh) [3] [9] | 69.2% | 48.5% | Not Specified |
| Low-Quality Embryos (NC-FET) [35] | Not Specified | Not Specified | Significantly Higher (aOR: 2.57) |
| Low-Quality Embryos (HT-FET) [35] | Not Specified | Not Specified | Reference Group |
| High-Quality Embryos (HT-FET) [35] | Not Specified | Not Specified | Higher Implantation Rate (45% vs 34%) |
The data indicates that the Modified Warming Protocol (MWP) markedly improves laboratory and clinical outcomes for vitrified-warmed oocytes, bringing them to a level comparable with fresh oocytes [3] [9]. Furthermore, the endometrial preparation protocol for frozen embryo transfer should be considered in the context of embryo quality. For low-quality embryos, transfer in a natural cycle (NC-FET) was associated with a significantly higher live birth rate compared to a hormone therapy cycle (HT-FET) (adjusted Odds Ratio 2.57) [35].
Performance by Maternal Age
Maternal age remains one of the most powerful predictors of ART success, directly impacting key outcome measures.
Table 2: Impact of Maternal Age on Frozen-Thawed Embryo Transfer Outcomes [33]
| Maternal Age Group | Clinical Pregnancy Rate | Implantation Rate | Live Birth Rate |
|---|---|---|---|
| ≤ 35 years | Significantly Higher | Significantly Higher | Significantly Higher |
| > 35 years | Significantly Lower (p < 0.05) | Significantly Lower (p < 0.001) | Significantly Lower (p < 0.01) |
The study confirmed that women in the pregnant group had a significantly lower average age (30.89 years) compared to the non-pregnant group (31.61 years) [33]. This underscores the continued importance of age as a primary factor in prognostic models.
Performance by Fertilization Method
The selection of fertilization method (c-IVF vs. ICSI) has distinct effects on early embryo development and ploidy rates, particularly in non-male factor infertility cases.
Table 3: Impact of Fertilization Method on Laboratory Outcomes in PGT-A Cycles [34]
| Outcome Metric | Conventional IVF (c-IVF) | Intracytoplasmic Sperm Injection (ICSI) | P-value |
|---|---|---|---|
| 2PN Fertilization Rate | 65.88% | 78.46% | < 0.001 |
| Blastocyst Formation per 2PN Zygote | 51.54% | 48.32% | 0.008 |
| Blastocyst Available for Biopsy per 2PN Zygote | 35.60% | 29.46% | < 0.001 |
| Blastocyst Available for Biopsy per Oocyte Retrieved | 23.45% | 17.82% | < 0.001 |
| Euploidy Rate (Adjusted) | Significantly Higher (aRR=1.611) | Reference Group | 0.001 |
While ICSI achieved a higher normal fertilization rate, c-IVF resulted in a significantly better blastocyst formation yield and a higher rate of euploid embryos after genetic testing [34]. This suggests that c-IVF may be a more efficient and effective strategy for couples without male factor infertility undergoing PGT-A.
Integrated Workflows and Decision Pathways
The experimental data and subgroup analyses can be synthesized into a logical workflow for protocol selection and a decision pathway for embryo transfer. The following diagrams visualize these processes.
Oocyte Warming and Culture Assessment Workflow
Diagram 1: Oocyte Warming and Culture Assessment Workflow. This diagram outlines the experimental sequence for comparing Modified and Conventional Warming Protocols, leading to the measurement of critical outcome metrics.
Embryo Transfer Strategy Decision Pathway
Diagram 2: Embryo Transfer Strategy Decision Pathway. This chart illustrates a data-informed strategy for selecting an endometrial preparation protocol based on embryo quality to optimize clinical outcomes.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the featured experiments, highlighting their critical functions in ART research.
Table 4: Key Research Reagent Solutions and Their Functions
| Reagent / Material | Function in Research Context | Example Use Case |
|---|---|---|
| Vitrification Solutions | Cryoprotectant mixtures used to preserve oocytes/embryos in a glass-like state without ice crystal formation. | Central to comparing CWP vs. MWP; contains permeating and non-permeating cryoprotectants [3] [9]. |
| G-IVF PLUS / G1/G2 Sequential Media | Culture media designed to support fertilization and sequential stages of embryo development in vitro. | Used for c-IVF insemination and extended embryo culture to the blastocyst stage [34]. |
| Progestin-Primed Ovarian Stimulation (PPOS) Protocol | A controlled ovarian stimulation protocol using progestins to prevent premature LH surges. | Employed in donor oocyte cycles to coordinate and control ovarian response [3] [9]. |
| Thawing Solution (TS) / Dilution Solution (DS) | Solutions used during the warming process to rapidly reheat and remove cryoprotectants from vitrified oocytes/embryos. | The MWP simplifies the CWP by potentially eliminating the need for DS and WS, reducing process time [3]. |
| Preimplantation Genetic Testing for Aneuploidy (PGT-A) | A genetic testing technology to determine the chromosomal status (euploid/aneuploid) of embryos. | Used as a key outcome measure to compare the biological effects of c-IVF versus ICSI [34] [36]. |
Conclusion
The collective evidence strongly supports a paradigm shift towards simplified warming protocols in ART. For vitrified oocytes, the modified warming protocol (MWP) demonstrates clear superiority, significantly enhancing blastocyst formation potential and ongoing pregnancy rates, making outcomes comparable to those of fresh oocytes. For vitrified blastocysts, one-step fast warming protocols achieve non-inferior survival and clinical pregnancy rates while offering substantial gains in laboratory efficiency and workflow simplification. Future research should focus on the molecular mechanisms underlying these improved outcomes, the development of universal standardization, and long-term follow-up studies. For biomedical research and drug development, these findings highlight a critical avenue for innovating cryopreservation media and devices that further minimize cellular stress and maximize viability.
References
- 1. A review of best practices of rapid-cooling vitriï¬cation for ... [https://www.asrm.org/practice-guidance/practice-committee-documents/a-review-of-best-practices-of-rapid-cooling-vitrication-for-oocytes-and-embryos-a-committee-opinion-2021/]
- 2. CRITICAL COOLING AND WARMING RATES AS A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10186587/]
- 3. Improved clinical outcomes with a modified warming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357474/]
- 4. Application of a single "Universal warming protocol" for ... [https://pubmed.ncbi.nlm.nih.gov/40153246/]
- 5. Universal post-warming dilution of vitrified embryos: impact ... [https://www.sciencedirect.com/science/article/pii/S1472648325001300]
- 6. Effect of a one-step fast warming protocol on reproductive ... [https://www.sciencedirect.com/science/article/pii/S0015028225005783]
- 7. Comparative Assessment of Survival and Clinical Outcome ... [https://link.springer.com/article/10.1007/s43032-023-01281-1]
- 8. Effect of a one-step fast warming protocol on reproductive ... [https://pubmed.ncbi.nlm.nih.gov/40651524/]
- 9. Improved clinical outcomes with a modified warming protocol ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01776-2]
- 10. Double Vitrification-Warming Cycles Reduce Live Birth ... [https://bmrat.org/index.php/BMRAT/article/view/978]
- 11. The impact of completely shrunken blastocysts on clinical ... [https://www.nature.com/articles/s41598-025-17526-9]
- 12. Live birth outcomes following single-step blastocyst ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11143112/]
- 13. Influence of the shortened warming protocol on human ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648324006436]
- 14. Towards a universal rapid warming protocol for ... [https://www.sciencedirect.com/science/article/pii/S147264832500358X]
- 15. Comparing warming strategies to reduce hypothermia and ... [https://www.nature.com/articles/s41598-025-04644-7]
- 16. frozen embryo transfer outcomes with one-step warming ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648325000811]
- 17. Application of a single “Universal warming protocol†for ... [https://link.springer.com/article/10.1007/s10815-025-03423-7]
- 18. Assessing the Efficacy of a Modified Warming Protocol for ... [https://ivf.ivftaiwan.com/share-detail/253/]
- 19. Stress signaling in mammalian oocytes and embryos [https://pmc.ncbi.nlm.nih.gov/articles/PMC4561599/]
- 20. Cellular osmoregulation enhances porcine embryo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616923/]
- 21. Stage-dependent changes in culture medium osmolality ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1524749/full]
- 22. Novel kinetic and developmental transcriptomic pan-stress ... [https://www.nature.com/articles/s41598-025-06628-z]
- 23. Fine morphological of quality of human mature oocytes... assessment [https://rbej.biomedcentral.com/articles/10.1186/1477-7827-12-110]
- 24. Fine morphological of quality of human mature oocytes... assessment [https://pubmed.ncbi.nlm.nih.gov/25421073/]
- 25. Preclinical validation of fast oocyte vitrification and ... [https://pubmed.ncbi.nlm.nih.gov/40334080/]
- 26. The impact of post-warming culture duration on clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7711098/]
- 27. Impacts of different culture times on pregnancy outcomes after ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-023-06139-7]
- 28. frozen embryo transfer outcomes with one-step warming ... [https://pubmed.ncbi.nlm.nih.gov/40782787/]
- 29. Heat stress affects the functionality of the ovine cumulus- ... [https://www.nature.com/articles/s41598-025-01173-1]
- 30. Single-Step Blastocyst Warming Validated, Saves Time [https://advances.massgeneral.org/obgyn/journal.aspx?id=2626]
- 31. gestational age, birth weight and sex of 1266 healthy ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648325004456]
- 32. Ultra RapidWarmâ„¢ Blast [https://www.vitrolife.com/products/cryopreservation/ultra-rapidwarm-blast/]
- 33. Effect of maternal age, embryo number and quality on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634337/]
- 34. Conventional in vitro fertilization enhances preimplantation ... [https://www.nature.com/articles/s41598-025-10300-x]
- 35. Optimizing frozen embryo transfer for low-quality ... [https://www.sciencedirect.com/science/article/pii/S1028455925001731]
- 36. The use of preimplantation genetic testing for aneuploidy [https://www.asrm.org/practice-guidance/practice-committee-documents/the-use-of-preimplantation-genetic-testing-for-aneuploidy-a-committee-opinion-2024/]