Optimizing Foster Mother Selection in Embryo Transfer: Strategies for Enhanced Reproductive Outcomes in Biomedical Research
This comprehensive review examines evidence-based strategies for optimizing foster mother selection in embryo transfer protocols, a critical factor in reproductive science and genetically engineered animal model production.
Optimizing Foster Mother Selection in Embryo Transfer: Strategies for Enhanced Reproductive Outcomes in Biomedical Research
Abstract
This comprehensive review examines evidence-based strategies for optimizing foster mother selection in embryo transfer protocols, a critical factor in reproductive science and genetically engineered animal model production. We analyze foundational principles of maternal influence on pregnancy success, methodological frameworks for foster mother assessment, troubleshooting approaches for common challenges, and validation techniques for protocol optimization. Drawing from recent advances in reproductive technology, including germ-free mouse production and assisted reproduction, this article provides researchers and drug development professionals with practical guidance to improve experimental reproducibility, enhance offspring viability, and accelerate biomedical discovery through refined embryo transfer methodologies.
The Biological Basis of Maternal Influence in Embryo Transfer Success
Defining the Foster Mother Role in Experimental Reproduction
Frequently Asked Questions
What is the primary role of a foster mother in embryo transfer experiments? The foster mother provides only a womb and postnatal care to manipulated embryos; she does not contribute her genomic material to the resulting offspring. Her key functions are to maintain pregnancy and provide optimal maternal care until weaning [1].
Which mouse strains are recommended as foster mothers for optimal reproductive performance? F1 hybrids between standard inbred strains (such as [B6 x CBA]) are recommended for their optimal reproductive fitness and mothering characteristics. Commercially available outbred strains like CD-1 or Swiss Webster are also excellent choices, particularly useful when a coat color difference (e.g., albino vs. pigmented) is needed to distinguish fostered offspring [1].
My foster mothers are not maintaining pregnancies consistently. What could be wrong? Ensure the foster mothers are in the correct physiological state—they must be pseudopregnant. This condition is induced by mating with a vasectomized or genetically sterile male. Sufficient sexual stimulation is required to create a uterine environment receptive to implantation [1].
The weaning rates for my germ-free C57BL/6J foster mothers are low. Is this typical? Yes, this is a documented issue. One study found that germ-free C57BL/6J foster mothers had the lowest weaning success among the strains tested. Consider using BALB/c or NSG strains as germ-free foster mothers, as they demonstrated superior nursing and weaning success in research [2].
Could the strain of the foster mother affect my experimental offspring's phenotype? Yes. Studies show that the foster mother's strain and the resulting maternal care can significantly influence the emotional behavior and stress physiology of the offspring. This effect occurs even when the foster mother is of the same strain as the biological mother (intrastrain-fostering) [3].
Experimental Protocols & Workflows
Key Protocol: Preparation of Pseudopregnant Foster Mothers
The following workflow outlines the critical steps for preparing a receptive foster mother for embryo transfer.
Detailed Methodology:
- Strain Selection: Choose females from a strain known for good reproductive fitness and mothering abilities (e.g., outbred CD-1, Swiss Webster, or F1 hybrids like [B6 x CBA]) [1].
- Mating for Pseudopregnancy: Place a single sexually mature female (2-8 months old) with a proven vasectomized or genetically sterile male. House in pairs (one male, one female) for optimal results [1].
- Confirmation of Mating: The morning after mating, check for the presence of a vaginal plug. The discovery of a plug confirms successful mating and is designated as Gestation Day 0.5 [2] [1].
- Timing of Embryo Transfer: The transferred embryos must be developmentally synchronized with the pseudopregnant recipient's uterine state. Blastocyst-stage embryos are typically transferred into a recipient on day 2.5 or 3.5 of pseudopregnancy [4].
Strain Selection Data for Foster Mothers
The choice of foster mother strain is a critical experimental variable. The table below summarizes quantitative performance data and key considerations.
| Strain / Genotype | Key Maternal Characteristics | Weaning Rate (Germ-Free Study) | Recommended Application |
|---|---|---|---|
| Outbred (e.g., CD-1, Swiss Webster) | High reproductive fitness, good mothering, readily available [1] | Not Specified | General embryo transfer; useful when albino coat color is needed for identification [1] |
| F1 Hybrid (e.g., [B6 x CBA]) | Optimal reproductive fitness and hybrid vigor [1] | Not Specified | For high-value embryos where maximum survival is critical [1] |
| BALB/c (Inbred) | Exhibited superior nursing and weaning success as a germ-free foster mother [2] | Superior | Germ-free mouse production; situations requiring a defined inbred background [2] |
| NSG (Inbred) | Exhibited superior nursing and weaning success as a germ-free foster mother [2] | Superior | Germ-free mouse production; immunodeficient research models [2] |
| C57BL/6J (Inbred) | Lowest weaning rate as a germ-free foster mother; active maternal behavior in SPF conditions [2] | Lowest | Not recommended as a germ-free foster mother; common genetic background for donor embryos [2] |
| NMRI (Outbred) | Good nursing, solid maternal care, commonly used as foster dams in breeding facilities [3] | Not Specified | "Foster saving" of compromised pups; noted to alter emotional phenotype of C57BL/6 offspring [3] |
The Scientist's Toolkit: Essential Research Reagents
This table lists key materials and reagents used in foster mother preparation and embryo transfer protocols.
| Item Name | Function / Purpose | Technical Notes |
|---|---|---|
| Vasectomized Male | Induces pseudopregnancy in the female foster mother via mating without producing viable embryos [1]. | Use males with proven sterility and mating performance. Allow 2-3 days of rest between mating sessions [1]. |
| Pregnant Mare Serum Gonadotropin (PMSG) | A gonadotropin used in superovulation protocols to stimulate follicle development in donor females [5]. | Often used in conjunction with hCG. Doses and timing are strain-dependent [5]. |
| Human Chorionic Gonadotropin (hCG) | A gonadotropin used to trigger ovulation in superovulated donor females [5]. | Administered after PMSG to finalize oocyte maturation and induce ovulation [5]. |
| M2 Medium | A handling medium used for flushing, manipulating, and temporarily holding embryos outside the incubator [5]. | Used for procedures such as embryo collection and transfer. Pre-warm to 37°C before use [5]. |
| KSOM / M16 Media | Specialized media for the in vitro culture of preimplantation embryos [5]. | KSOM may support development to the 8-cell stage in some species, while M16 can support blastocyst formation [5]. |
| Pseudopregnant Foster Mother | The ultimate "reagent"; provides the in vivo environment for transferred embryos to develop to term [1]. | Select based on strain performance, health status, and synchronization with the embryonic developmental stage [1]. |
Advanced Troubleshooting Guide
Problem: Poor Implantation or Pregnancy Failure After Transfer
- Potential Cause 1: Lack of Synchronization. The developmental stage of the transferred embryos is not synchronized with the pseudopregnant recipient's uterine receptivity window [1].
- Solution: Precisely time the recipient's pseudopregnancy (via plug check) and coordinate with the in vitro development of your embryos.
- Potential Cause 2: Suboptimal Maternal Environment. The chosen foster mother strain may have inherent reproductive challenges or the female may be too young/old [2] [1].
- Solution: Use proven, high-performance foster strains like outbred mice or F1 hybrids. Select females between 2 and 8 months of age that have successfully carried a litter before [1].
Problem: Foster Mother Neglects or Cannibalizes Pups
- Potential Cause 1: Stress from Environmental Disturbance. The foster mother may be disturbed by noise, light, or cage movement shortly after birth [3].
- Solution: Provide a quiet, low-stress environment. Minimize cage disturbances for at least 5-7 days post-partum. Ensure the nest is not disrupted during health checks.
- Potential Cause 2: Inherent Strain-Specific Maternal Behavior. Some inbred strains (like C57BL/6J under germ-free conditions) are documented to have lower maternal care efficiency [2].
- Solution: Cross-foster pups to a strain known for strong maternal instincts, such as NMRI or BALB/c (in germ-free settings). This is a standard practice in many facilities [2] [3].
Problem: Unexpected Phenotype in Experimental Offspring
- Potential Cause: Cross-Fostering Artifact. The foster mother's strain and the quality of maternal care she provides can have long-term programming effects on the offspring's emotionality, stress response, and behavior [3].
- Solution: Always report the strain of the foster mother and the fostering procedure in your methods. For highly sensitive behavioral studies, consider using foster mothers of the same genetic background as the embryo donors to minimize this confound [3].
Critical Uterine and Systemic Factors Affecting Implantation
Troubleshooting Guide: Common Implantation Failure Scenarios
This guide assists researchers in diagnosing and addressing the primary causes of implantation failure in experimental models.
Problem 1: Recurrent Implantation Failure (RIF) despite high-quality embryo transfer.
- Potential Cause: Displaced Window of Implantation (WOI) leading to embryo-endometrium asynchrony [6].
- Diagnostic Approach:
- Perform Endometrial Receptivity Analysis (ERA): A molecular diagnostic tool that analyzes the expression of 238 genes to determine endometrial receptivity status and pinpoint the precise WOI [7] [6].
- Experimental Protocol for ERA:
- Endometrial Preparation: Prepare the endometrium using a Hormone Replacement Therapy (HRT) protocol. Administer estrogen for approximately 16 days from the third day of menstruation [6].
- Progesterone Administration: Once endometrial thickness exceeds 6mm, administer progesterone (P). The first day of progesterone supplementation is designated as P+0 [6].
- Endometrial Biopsy: Perform an endometrial biopsy on P+5 in a mock cycle [6].
- Analysis: Analyze the biopsy sample using a customized gene array. Computational analysis predicts whether the endometrium is receptive ("Receptive") or non-receptive ("Pre-receptive," "Post-receptive") [6].
- Solution: Implement personalized Embryo Transfer (pET), where the embryo transfer timing is adjusted based on the ERA results. Studies show this significantly improves clinical pregnancy and live birth rates in subjects with a history of failed transfers [6].
Problem 2: Suboptimal uterine environment and immune rejection.
- Potential Cause: Dysregulated maternal immune response and inadequate embryo-maternal cross-talk [8].
- Diagnostic Approach:
- Analyze the population and phenotype of uterine immune cells, particularly uterine Natural Killer (uNK) cells and decidual macrophages [8].
- Evaluate expression levels of key tolerance-promoting factors like HLA-G on trophoblasts and Progestagen-associated Endometrial Protein (PAEP) in the endometrium [8].
- Solution: Consider immunomodulatory strategies aimed at optimizing the uterine immune environment. Further research is needed to develop targeted therapies, but understanding these pathways is critical for troubleshooting [9] [8].
Problem 3: Poor selection of recipient (foster) mothers leading to low pup survival.
- Potential Cause: Inadequate maternal care and nursing capabilities of the selected foster strain [2].
- Diagnostic Approach: Systematically compare the weaning success rates and maternal behaviors of different germ-free (GF) foster strains.
- Solution: Select foster strains with demonstrated superior nursing capabilities. Research indicates that BALB/c and NSG GF mice exhibit superior nursing and weaning success compared to C57BL/6J strains in germ-free rederivation experiments [2].
Frequently Asked Questions (FAQs) for Researchers
Q1: What are the most critical, non-embryonic factors dictating implantation success?
Based on clinical and AI-based studies, the key factors are [10]:
- Endometrial Receptivity: The status of the endometrium is a critical determinant [7] [6].
- Maternal Age: Age is positively correlated with an increased rate of a displaced WOI [10] [6].
- Endometrial Thickness: A key variable influencing clinical pregnancy rates in euploid embryo transfers [10].
- Previous Failed Cycles: The number of prior failed embryo transfer cycles is linked to a higher probability of a displaced WOI [6].
- Hormonal Environment: The estrogen-to-progesterone (E2/P) ratio during the secretory phase is crucial; either too high or too low can negatively impact receptivity [6].
Q2: How can machine learning (ML) optimize implantation research and foster mother selection?
ML algorithms can analyze complex datasets to identify non-linear relationships between variables that may be missed by conventional statistics.
- Prediction Models: ML models like XGBoost can effectively predict clinical pregnancy outcomes by weighing factors such as maternal age, AMH levels, and endometrial thickness [10].
- Factor Ranking: Ensemble algorithms can rank the influence of various clinical features, identifying "Therapeutic Interventions" (e.g., ovarian stimulation protocols) as the most significant group affecting live birth rates [11].
- Strain Selection: While not explicitly shown in the results, the principles of ML can be applied to analyze historical data on pup survival, maternal behavior, and weaning rates to build predictive models for optimal foster mother strain selection.
Q3: What is the single most important technique for assessing endometrial receptivity at the molecular level?
The Endometrial Receptivity Array (ERA) is a leading molecular technique. It transforms assessment from static morphological evaluation to a dynamic analysis of the transcriptomic signature of the endometrium, allowing for precise identification of the Window of Implantation (WOI) [7] [6].
Q4: How does the maternal immune system support implantation rather than reject the semi-allogeneic embryo?
The maternal immune system undergoes unique adaptation:
- Specialized Immune Cells: Uterine Natural Killer (uNK) cells, which are distinct from peripheral NK cells, expand and become the dominant immune population. They facilitate trophoblast invasion and vascular remodeling by releasing cytokines (e.g., VEGF, CSF1) rather than executing cytotoxic functions [8].
- Immune Tolerance: Interactions such as HLA-G (on the trophoblast) with inhibitory receptors on maternal immune cells help suppress destructive immunity [8].
- Controlled Inflammation: Implantation itself is a pro-inflammatory event, followed by an anti-inflammatory phase for fetal development, all tightly regulated by immune cells and their secretions [8].
Table 1: Impact of Personalized Embryo Transfer (pET) guided by ERA on Pregnancy Outcomes
| Patient Group | Transfer Type | Clinical Pregnancy Rate | Live Birth Rate | Early Abortion Rate |
|---|---|---|---|---|
| Non-RIF Patients | pET (ERA-guided) | 64.5% [6] | 57.1% [6] | 8.2% [6] |
| Non-RIF Patients | npET (Standard timing) | 58.3% [6] | 48.3% [6] | 13.0% [6] |
| RIF Patients | pET (ERA-guided) | 62.7% [6] | 52.5% [6] | Not Specified |
| RIF Patients | npET (Standard timing) | 49.3% [6] | 40.4% [6] | Not Specified |
Table 2: Key Factors Correlated with a Displaced Window of Implantation (WOI) [6]
| Factor | Correlation with Displaced WOI | Notes |
|---|---|---|
| Age | Positive Correlation | Displaced WOI rate increases with age. |
| Number of Previous Failed ET Cycles | Positive Correlation | More failed cycles correlate with higher displaced WOI rate. |
| Serum E2/P Ratio | Non-linear (Optimal Range) | A median E2/P ratio (4.46 - 10.39 pg/ng) was associated with the lowest rate of displaced WOI. |
Table 3: Success Rates of Different Germ-Free Foster Mouse Strains [2]
| Foster Mother Strain | Weaning Success | Maternal Care Characteristics |
|---|---|---|
| BALB/c | Superior | Exhibited superior nursing and weaning success. |
| NSG | Superior | Exhibited superior nursing and weaning success. |
| KM (Outbred) | Intermediate | Not specified in results. |
| C57BL/6J | Lowest | Had the lowest weaning rate in the germ-free context. |
Experimental Protocol: Optimizing Germ-Free Mouse Production via Cesarean Section
This detailed protocol is derived from research aimed at improving the efficiency of generating germ-free (GF) mouse models, a critical step for embryo transfer research without microbiome interference [2].
Objective: To obtain GF pups via sterile cesarean section with high survival rates through optimized surgical technique, donor selection, and foster mother strain choice.
Materials:
- Specific Pathogen-Free (SPF) pregnant donor mice (e.g., C57BL/6).
- Germ-free (GF) foster mother mice (recommended: BALB/c or NSG strains).
- Surgical instruments (autoclaved).
- PVC isolators or flexible film isolators for GF housing.
- Clidox-S disinfectant (1:3:1 dilution, activated for 15 min).
- Heating pad.
Methodology:
- Donor Preparation:
- Option A (Natural Mating): House SPF donor females with males and check for vaginal plugs to confirm mating (designated as G0.5). Monitor for natural delivery from G18 [2].
- Option B (In Vitro Fertilization - IVF): Use IVF-derived embryos transferred to recipient females to precisely control the delivery date, enhancing experimental reproducibility [2].
- Cesarean Section Technique:
- Euthanize the donor female at term.
- Perform the Female Reproductive Tract Preserved C-section (FRT-CS). This technique involves placing a clamp only at the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, cervix), which has been shown to significantly improve fetal survival rates compared to the traditional method [2].
- Transfer the intact uterus rapidly into a disinfectant solution (e.g., Clidox-S) and then into a sterile isolator. The entire procedure from euthanasia to transfer should be completed within 5 minutes to maintain sterility and pup viability [2].
- Pup Extraction and Foster Introduction:
- Inside the isolator, incise the uterine sac and amniotic membrane to expose the pup.
- Wipe away amniotic fluid with a sterile swab until spontaneous breathing is noted [2].
- Immediately present the pups to a proven GF foster mother that has recently given birth (to ensure she is lactating) and has demonstrated good maternal care [2].
Signaling Pathways and Experimental Workflows
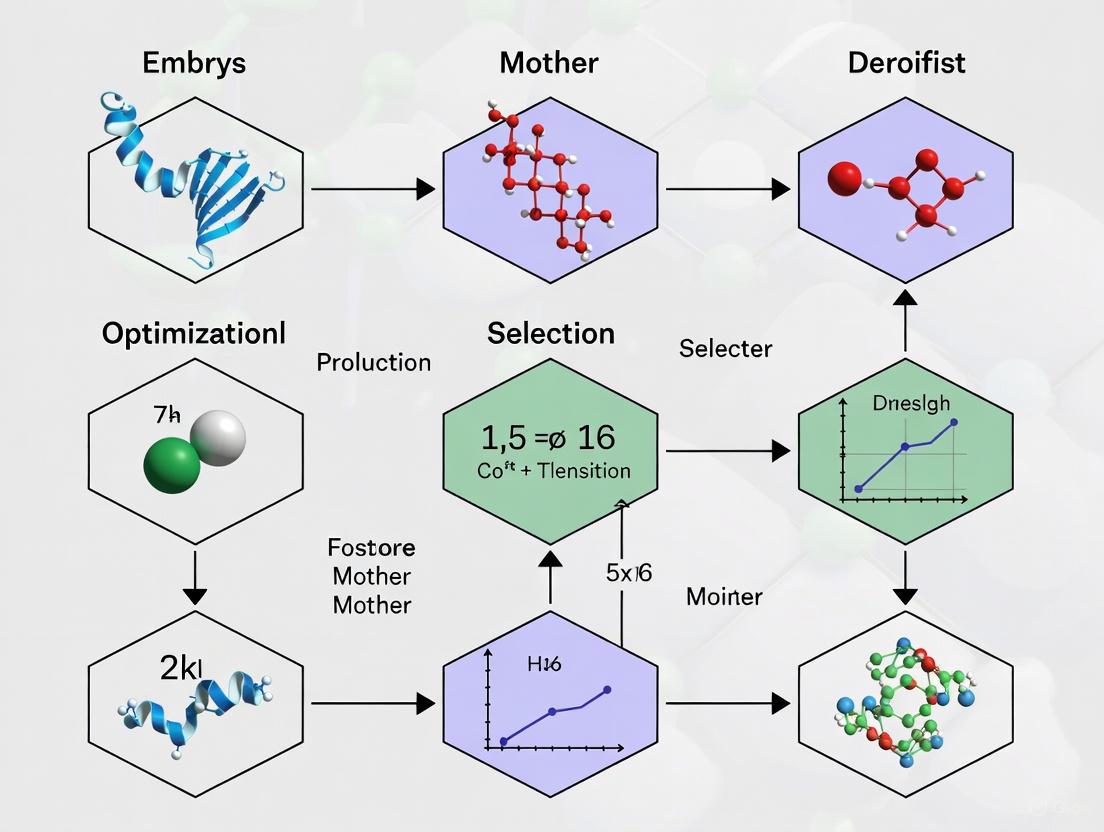
Diagram 1: GF Mouse Production Workflow
Diagram 2: Embryo-Maternal Cross-Talk
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Research Reagent Solutions for Implantation Studies
| Item | Function/Application in Research | Example/Notes |
|---|---|---|
| Endometrial Receptivity Array (ERA) | Molecular diagnostic tool to identify the Window of Implantation (WOI) by analyzing 238 gene expressions [7] [6]. | Customized gene array; used for personalized embryo transfer timing. |
| Preimplantation Genetic Testing for Aneuploidy (PGT-A) | Screens embryos for chromosomal abnormalities, significantly increasing implantation odds by selecting euploid embryos [9]. | Critical for controlling embryo quality factor in experiments. |
| Hormone Replacement Therapy (HRT) Drugs | Prepares the endometrium in a controlled, synchronous manner for experiments like ERA or embryo transfer [6]. | Includes estrogen (oral/transdermal) and progesterone (injection/vaginal). |
| Clidox-S | Chlorine dioxide disinfectant used for sterilizing tissue samples and surfaces before introduction into germ-free isolators [2]. | Used in a 1:3:1 dilution, activated for 15 minutes prior to use. |
| Germ-Free Isolators | Polyvinyl chloride (PVC) isolators provide a sterile barrier environment for housing and breeding germ-free animals [2]. | Essential for studying implantation without microbiome influence. |
Strain-Specific Variations in Reproductive Efficiency and Maternal Care
Troubleshooting Guide & FAQs
Frequently Asked Questions
Q1: Which mouse strain should I select as a foster mother for embryo transfer to ensure the best pup survival?
The optimal strain depends on your specific requirements, but several studies have identified high-performing candidates. BALB/c and NSG strains have demonstrated superior nursing capabilities and higher weaning success in germ-free (GF) production settings [12]. Furthermore, F1 hybrids (e.g., B6 x CBA) are highly recommended for their excellent reproductive fitness and mothering characteristics, as they often exhibit hybrid vigor [1]. The C57BL/6 strain is a common choice and shows good results in embryo transfer with live pup development [13]. It is generally advised to avoid using C57BL/6J as a GF foster mother, as it has shown the lowest weaning rate in comparative studies [12].
Q2: Our superovulation yields are low. Is this strain-dependent, and which strains respond best?
Yes, the response to superovulation is highly strain-dependent [13]. The table below summarizes the performance of common inbred strains.
| Strain | Avg. Normal Oocytes per Female | In Vitro Fertilization Rate (%) | Live Pups from Fresh Embryo Transfer (%) |
|---|---|---|---|
| 129S1/SvImJ | 40 ± 3 | 24 | 45 (from thawed embryos) |
| C57BL/6J | 28 ± 2 | 76 | 53 |
| BALB/cByJ | 21 ± 2 | 90 | 18 (from thawed embryos) |
| DBA/2J | 19 ± 1 | 93 | 33 |
| FVB/NJ | 19 ± 1 | 84 | 44 |
| A/J | 5 ± 1 | 93 | 5 |
Data adapted from Sztein et al. (2006) [13].
Q3: We observe significant differences in maternal behavior between strains. What are the key behavioral components to monitor?
Strain-specific variations in maternal care are well-documented. Key behaviors to observe include [14] [15] [16]:
- Nursing Postures: Arched-back, blanket, and supine nursing.
- Pup Licking: Anogenital and body licking.
- Nest Building: Quality and frequency of nest construction.
- Neglecting Behaviors: Pups found outside the nest.
For example, one study found that C57BL/6 and CBA/Ca dams showed more active licking and grooming, while BALB/c dams were generally less vigorous in their maternal care [15]. These differences can significantly impact pup development.
Q4: Why is the genetic background of a strain so important, and how can it confound my results?
The genetic background can dramatically influence phenotypic outcomes. Residual genetic elements from embryonic stem (ES) cell donors (like the 129 strain) can be mistaken for the effect of a genetic modification if not properly controlled [17]. For instance, a study on Band3-modified mice found that a contaminating 129 genetic region on chromosome 1, and not the Band3 mutation itself, was responsible for observed differences in red blood cell storage [17]. Always backcross GA mice onto a defined genetic background for at least 10 generations and use appropriate littermate controls to mitigate this issue [18].
Experimental Protocols
Protocol 1: Assessing Strain-Specific Maternal Behavior
This protocol is adapted from detailed behavioral observations used to characterize differences between inbred strains [15] [16].
- Subject Preparation: Use primiparous female mice. House them individually with ad libitum access to food and water in a 12-hour light/dark cycle.
- Behavioral Recording: Videotape home cages during both light and dark phases for 1-hour periods on postpartum days 2, 4, 6, and 8.
- Behavioral Coding: Using scan sampling, record behaviors every 3 minutes during each observation period. Catalog the following:
- Caring Behaviors: Licking/grooming (anogenital and body), active nursing (upright arched posture), passive nursing (lying immobile on pups), nest building.
- Self-Maintenance: Self-grooming, eating/drinking.
- Neglecting Behaviors: Pups out of the nest, climbing/digging while away from the litter [14].
- Data Analysis: Sum the scans for each behavior and relate them to the total number of recorded scans. Compare the frequencies and patterns across different strains.
Protocol 2: Evaluating Reproductive Efficiency via Assisted Reproductive Technologies (ARTs)
This standardized protocol allows for direct comparison of superovulation response, in vitro fertilization (IVF) success, and embryo transfer efficiency across strains [13].
- Superovulation: Administer 5.0 IU of eCG (equine chorionic gonadotropin) to 3-week-old female mice, followed by 5.0 IU of hCG (human chorionic gonadotropin) 48 hours later.
- In Vitro Fertilization: Collect oocytes after hCG administration. Fertilize them in Human Tubal Fluid (HTF) medium with sperm from the same strain.
- Embryo Culture & Transfer: The following day, collect two-cell embryos. Transfer fresh two-cell embryos into the oviducts of pseudopregnant recipient females (e.g., outbred CD-1 or Swiss Webster). Alternatively, cryopreserve embryos for later transfer.
- Outcome Measures:
- Superovulation Response: Count the number of normal oocytes per female.
- Fertilization Rate: Calculate the proportion of oocytes that develop into two-cell embryos.
- Embryo Transfer Efficiency: Record the proportion of transferred two-cell embryos that develop into live pups.
The Scientist's Toolkit
Research Reagent Solutions
| Item | Function & Application |
|---|---|
| FVB/N Strain | Ideal for transgenic production due to large, prominent pronuclei in fertilized eggs and high survival rates of injected embryos [1]. |
| C57BL/6 Strain | The most common genetic background for experimentation; performs well in embryo transfer with high rates of live pup development [13]. |
| B6D2F1 Hybrid | A common F1 hybrid used for somatic cell nuclear transfer (SCNT) studies as a source of donor cells [19]. |
| CD-1 or Swiss Webster | Outbred strains frequently used as pseudopregnant recipients for embryo transfer due to their good reproductive fitness and mothering traits [12] [1]. |
| KSOM/HTF Medium | Specialized culture media used for in vitro fertilization and embryo culture [13]. |
| 2i/LIF Culture System | A culture system containing differentiation inhibitors used to establish and maintain naive embryonic stem cells (ESCs) and nuclear transfer ES cells (ntESCs) [19]. |
Technical Diagrams
Foster Mother Selection Workflow
Strain Performance Comparison
Impact of Maternal Physiology on Offspring Development and Viability
Frequently Asked Questions (FAQs)
FAQ 1: How does the genetic strain of a foster mother impact the success of embryo transfer? The genetic background of the foster mother is a critical factor for successful pup weaning. Research evaluating different germ-free (GF) foster strains has shown significant variation in weaning success. For example, BALB/c and NSG strains exhibit superior nursing capabilities and higher weaning rates. In contrast, the C57BL/6J strain demonstrates the lowest weaning success in a germ-free environment, a finding that contrasts with its maternal performance under specific pathogen-free (SPF) conditions [12]. Therefore, strain selection should be based on empirical data of maternal care within your specific facility environment.
FAQ 2: Why is precise timing critical for Cesarean section (C-section) in embryo transfer experiments, and how can it be improved? The timing of the C-section is vital for fetal survival. In natural mating (NM), predicting the exact delivery date is challenging, leading to variability. Using in vitro fertilization (IVF) to generate donor embryos allows for precise control over the fertilization timeline. This method enables researchers to schedule pre-labor C-sections on the predicted delivery date, significantly enhancing experimental reproducibility and fetal survival rates [12].
FAQ 3: What surgical technique improves fetal survival during sterile C-section? Optimizing the surgical method can significantly improve outcomes. The Female Reproductive Tract-Preserving C-section (FRT-CS), which selectively clamps only the cervix base and preserves the entire reproductive tract, has been shown to improve fetal survival rates while maintaining sterility compared to traditional C-section (T-CS) techniques [12].
FAQ 4: How does maternal age affect reproductive outcomes, even when using donor oocytes? Maternal age directly impacts uterine receptivity. A large-scale retrospective study found that even when using donor oocytes from young women (≤35 years), the recipient's uterine age affects outcomes. The risk of implantation failure increases by 4.2% per year after age 40, and the risk of pregnancy loss increases by 3.2% per year. Live birth rates begin to decrease significantly from age 40 [20]. This indicates that uterine aging is an independent factor affecting embryo implantation and development.
Troubleshooting Guides
Problem: Low Weaning Rate of Fostered Pups
Possible Causes and Solutions:
- Cause: Suboptimal foster strain selection.
- Solution: Select a foster strain with documented high maternal care. Based on experimental data, prioritize BALB/c or NSG strains over C57BL/6J for germ-free fostering [12]. See Table 1 for comparative data.
- Cause: Inexperienced foster mother.
- Solution: Use foster mothers that are approximately four months old and have had at least one successful prior pregnancy. This ensures they have experience in nursing and caring for pups [12].
- Cause: Hypothermia in newborns.
- Solution: Ensure the sterile isolator or receiving environment is pre-warmed. Use a heating pad set to 40–45°C for at least 15 minutes before the C-section procedure begins to prevent pup loss due to low body temperature [12].
Problem: High Rate of Implantation Failure or Pregnancy Loss
Possible Causes and Solutions:
- Cause: Advanced maternal age of the recipient.
- Solution: When possible, use younger recipient females. For critical experiments requiring high success rates, consider the use of recipients under 40 years of age, as the risk of implantation failure and pregnancy loss increases markedly after this age [20].
- Cause: Non-euploid or poor-quality embryos.
- Solution: Prioritize the transfer of high-quality, euploid embryos. In frozen-thawed embryo transfer cycles, the number of high-quality embryos transferred is significantly higher in pregnancy groups compared to non-pregnancy groups [21].
- Cause: Suboptimal number of embryos transferred.
- Solution: Adhere to evidence-based guidelines on the number of embryos to transfer. A higher number of transferred embryos is associated with significantly increased clinical pregnancy and live birth rates. However, balance this with the risk of multiple gestations [21].
Table 1: Weaning Success of Pups by Germ-Free Foster Mother Strain
Data derived from evaluation of different GF foster strains, all four months old with prior birthing experience [12].
| Foster Mother Strain | Strain Type | Weaning Success | Key Characteristics |
|---|---|---|---|
| BALB/c | Inbred | Superior | Exhibits superior nursing capabilities and weaning success. |
| NSG | Inbred | Superior | Shows high weaning success suitable for germ-free conditions. |
| KM | Outbred | Moderate | -- |
| C57BL/6J | Inbred | Lowest | Weaning rate is lowest, contrary to its performance in SPF environments. |
Table 2: Impact of Maternal Age on Reproductive Outcomes with Donor Oocytes
Data from a retrospective study of 33,141 single euploid embryo transfers using donor oocytes [20].
| Outcome Metric | Age at Significant Worsening | Annual Increase in Risk After 40 (Relative Risk) |
|---|---|---|
| Implantation Failure | 39 years | 4.2% per year (RR=1.042) |
| Live Birth Rate | 40 years | -- |
| Pregnancy Loss | 43 years | 3.2% per year (RR=1.032) |
Table 3: Influence of Embryo Transfer Parameters on Pregnancy Outcomes
Data from a retrospective cohort study of 1,031 frozen-thawed embryo transfer cycles [21].
| Parameter | Pregnant Group (Mean ± SE) | Non-Pregnant Group (Mean ± SE) | P-value |
|---|---|---|---|
| Maternal Age (years) | 30.89 ± 0.22 | 31.61 ± 0.22 | < 0.05 |
| Number of Embryos Transferred | 2.12 ± 0.02 | 2.00 ± 0.02 | < 0.0001 |
| Number of High-Quality Embryos | 1.90 ± 0.03 | 1.66 ± 0.03 | < 0.0001 |
Experimental Protocols
Detailed Protocol: Optimized Sterile Cesarean Section and Fostering
Purpose: To obtain germ-free pups from specific pathogen-free (SPF) donor mice via a sterile C-section and successfully foster them to a germ-free recipient mother.
Key Materials:
- Pregnant SPF donor female (e.g., C57BL/6 from a commercial breeder) [12]
- Germ-free foster mother (e.g., BALB/c or NSG strain, ~4 months old, with prior birthing experience) [12]
- Sterile isolator or appropriate surgical setup [12]
- Heating pad
- Surgical tools (autoclaved)
- Clidox-S or other approved disinfectant [12]
Methodology:
- Donor Preparation: Time mating of SPF donors either by natural mating or, for better precision, via IVF. If using natural mating, confirm a vaginal plug and designate that day as gestation day 0.5 (G0.5) [12].
- Foster Preparation: Mate the GF foster mother with a vasectomized GF male to induce a state of pseudopregnancy, synchronizing her receptivity with the donor's delivery date [1].
- C-Section Procedure: Euthanize the SPF donor female on the predicted delivery date (e.g., G18-G19 for natural mating). Perform the Female Reproductive Tract-Preserving C-section (FRT-CS) under aseptic conditions [12].
- FRT-CS Technique: Selectively clamp only the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, and cervix). Excise the uterus.
- Disinfection and Pup Retrieval: Transfer the intact uterus to a sterile transfer port and disinfect by submersion in a chlorine dioxide solution (e.g., Clidox-S) for a validated contact time. Move the uterus into the sterile isolator [12].
- Pup Processing: Inside the isolator, carefully incise the uterine sac and amniotic membrane to expose each pup. Wipe away amniotic fluid with a sterile swab until spontaneous breathing is noted. Cut the umbilical cord [12].
- Fostering: Immediately place the viable, breathing pups with the prepared GF foster mother. The entire procedure from donor euthanasia to fostering should be completed within 5 minutes to maximize pup survival [12].
- Post-Procedure Monitoring: Monitor the foster mother and pups regularly for nursing behavior and pup growth until weaning.
Detailed Protocol: Evaluating Foster Mother Maternal Care
Purpose: To systematically assess and compare the nursing capabilities and weaning success of different germ-free mouse strains as foster mothers.
Key Materials:
- Multiple strains of GF female mice (e.g., C57BL/6J, BALB/c, NSG, KM) [12]
- Litters of pups for fostering (e.g., from C-section derivation)
- Standard GF housing (e.g., PVC isolators) with aspen wood shavings [12]
Methodology:
- Subject Selection: Select GF foster mothers of the strains to be evaluated. Standardize critical variables: age (e.g., four months old) and prior experience (e.g., all have given birth once before) [12].
- Housing and Mating: House the females individually. Mate them with a vasectomized male of the same GF strain to induce pseudopregnancy [1].
- Fostering: On the day of the C-section, assign a standardized number of viable newborn pups to each foster mother.
- Data Collection: Record observations daily. Key metrics include:
- Nursing Success: Observation of pups nursing.
- Pup Retrieval: Mother's behavior in gathering pups.
- Pup Survival: Number of pups alive at designated time points (e.g., 7 days, 21 days).
- Weaning Rate: The primary outcome, calculated as the number of pups successfully weaned per number fostered [12].
- Data Analysis: Compare the weaning rates and other maternal behavior metrics between the different GF foster strains using appropriate statistical tests.
Workflow and Pathway Diagrams
Foster Mother Selection Workflow
Maternal Age Impact Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Embryo Transfer Research
| Item | Function / Application | Example / Note |
|---|---|---|
| FVB/N Mice | Ideal egg donors for pronuclear injection. | Produces eggs with large, prominent pronuclei, facilitating DNA microinjection [1]. |
| Germ-Free (GF) Foster Strains | Rearing pups derived via sterile C-section. | BALB/c and NSG strains show superior weaning success in GF conditions [12]. |
| Superovulation Reagents | Increase egg yield from donor females. | Commercially available gonadotropins; effectiveness is highly strain-dependent [1]. |
| SPF Stud Males | For mating with superovulated females to produce zygotes. | Use healthy, proven males (2-8 months old) of the same genotype as the female [1]. |
| Vasectomized Males | Induce pseudopregnancy in recipient females. | Crucial for preparing the uterine environment of the foster mother for embryo implantation [1]. |
| Sterile Isolators | Provide a germ-free environment for housing GF animals and performing procedures. | Often made of PVC; requires strict sterilization protocols [12]. |
| Chlorine Dioxide Disinfectant | Surface sterilization of the uterus during C-section derivation. | Clidox-S is used to disinfect the tissue sample before entry into the sterile isolator [12]. |
The 'Sterile Womb' Hypothesis and Germ-Free Animal Production Foundations
Foundational Concepts FAQ
Q1: What is the "Sterile Womb" hypothesis and why is it fundamental to germ-free animal production?
The "Sterile Womb" hypothesis, also known as the "sterile womb paradigm," posits that the fetal environment—including the placenta, amniotic fluid, and uterus—is free of viable microorganisms in healthy pregnancies. According to this dogma, microbial colonization of mammals begins during and after birth, rather than in utero [22] [23]. This concept is critically important because it forms the foundational principle for producing germ-free (GF) animal models via sterile cesarean section. If the fetus develops in a sterile environment, transferring it via hysterectomy to a sterile isolator prevents microbial colonization, enabling derivation of GF research animals [2].
Q2: What is the competing "in utero colonization" hypothesis and what is the current scientific consensus?
The "in utero colonization" hypothesis suggests that microbial colonization begins before birth, challenging the traditional sterile womb paradigm. Proponents point to studies using molecular techniques that have detected bacterial DNA in placental tissue, amniotic fluid, and meconium [22] [23]. However, a comprehensive critical assessment reveals that evidence supporting this hypothesis remains extremely weak. These studies often suffer from methodological limitations, including insufficient detection limits for low-biomass samples, inadequate contamination controls, and failure to demonstrate bacterial viability [22]. The ability to reliably derive axenic (germ-free) animals via cesarean sections strongly supports the sterility of the fetal environment in mammals [22] [23]. Most international experts thus maintain that current evidence does not support the existence of microbiomes within the healthy fetal milieu [22] [23] [24].
Q3: How does the sterile womb hypothesis practically impact foster mother selection in embryo transfer research?
The sterile womb hypothesis directly informs foster mother selection because GF pups derived via cesarean section must be reared by a foster mother that is also germ-free. Selecting the optimal GF foster strain is crucial for pup survival and successful colonization studies. Research demonstrates significant strain-dependent variation in maternal care capabilities among GF foster mothers [2]. This contrasts with findings in specific pathogen-free (SPF) environments, highlighting that conventional behavioral data cannot directly predict GF foster mother performance.
Technical Troubleshooting Guide
Problem: Low Neonatal Survival After Cesarean Derivation
Potential Causes and Solutions:
Cause 1: Suboptimal surgical technique
- Solution: Implement the female reproductive tract preserved C-section (FRT-CS) technique. This method selectively clamps only the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, and cervix), which has been shown to significantly improve fetal survival rates while maintaining sterility compared to traditional C-section (T-CS) [2].
Cause 2: Inappropriate foster mother strain
- Solution: Carefully select foster mother strain based on documented maternal care performance in GF conditions. Studies show BALB/c and NSG mice exhibit superior nursing and weaning success, while C57BL/6J has the lowest weaning rate in GF conditions [2].
Cause 3: Hypothermia during transfer
- Solution: Pre-heat isolators with heating pads to 40-45°C for at least 15 minutes before C-section begins. Complete the entire transfer procedure within 5 minutes to prevent hypothermia in neonates [2].
Problem: Contamination in Germ-Free Colonies
Potential Causes and Solutions:
Cause 1: Inadequate sterility controls during derivation
Cause 2: Cross-contamination from personnel or equipment
Experimental Protocols for Validation
Protocol 1: Validating Sterility of Fetal Environment
Objective: Investigate bacterial presence in fetal samples while controlling for contamination.
Materials: Pregnant dams, sterile swabs, surgical equipment, culture media, molecular biology reagents.
Methodology:
- Perform elective cesarean sections with closed cervix to prevent ascending contamination [24]
- Collect samples from endometrium, amniotic fluid, and meconium using sterile technique
- Include multiple controls: uterine serosa, surgical tray, surgeon's gloves [25]
- Apply multi-technique approach: bacterial culture, 16S rRNA gene sequencing, and fluorescence in situ hybridization (FISH) [24] [25]
- Process controls and experimental samples identically
- Use statistical analysis to compare bacterial abundance and diversity between samples and controls
Interpretation: True fetal microbiome should show significant differences from control samples in bacterial composition and abundance [25].
Protocol 2: Optimizing Germ-Free Mouse Production
Objective: Maximize efficiency of germ-free mouse derivation through technique refinement.
Materials: SPF donor mice, GF foster mothers, sterile isolators, surgical equipment.
Methodology:
- Compare cesarean techniques: Traditional (T-CS) vs. female reproductive tract preserved (FRT-CS)
- Evaluate donor sources: Natural mating vs. in vitro fertilization (IVF) for precise timing control
- Assess maternal care across multiple GF foster strains (C57BL/6J, BALB/c, NSG, KM)
- Monitor fetal survival rates, contamination rates, and weaning success
- Maintain sterility throughout process with strict protocol adherence [2]
Table 1: Foster Strain Performance in Germ-Free Conditions
| Strain | Maternal Care Performance | Weaning Success Rate | Notes |
|---|---|---|---|
| BALB/c | Superior | High | Suitable as GF foster mothers [2] |
| NSG | Superior | High | Suitable as GF foster mothers [2] |
| C57BL/6J | Lowest performance | Lowest | Poor maternal care in GF conditions [2] |
| KM (outbred) | Moderate | Moderate | Variable performance [2] |
Table 2: Cesarean Technique Comparison
| Technique | Fetal Survival Rate | Sterility Maintenance | Key Features |
|---|---|---|---|
| Traditional C-section (T-CS) | Lower baseline | Adequate | Clamps at cervix base and top of uterine horn [2] |
| Female Reproductive Tract Preserved (FRT-CS) | Significantly improved | Maintained | Selective clamping only at cervix base [2] |
Research Reagent Solutions
Table 3: Essential Materials for Germ-Free Animal Research
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Polyvinyl chloride (PVC) isolators | Sterile housing | Maintain germ-free environment; require heating pads to prevent hypothermia [2] |
| Clidox-S | Disinfectant | Use at 1:3:1 dilution, activate for 15 min before use [2] |
| Liquid Amies Medium | Sample transport | Preserve samples for bacterial culture [24] |
| Columbia blood agar plates | Bacterial culture | Support aerobic and anaerobic growth for sterility testing [2] |
| 16S rRNA gene sequencing reagents | Bacterial detection | Identify bacterial DNA in low-biomass samples [24] [25] |
| FISH probes with fluorescent dyes | Bacterial visualization | Target 16S ribosomal bacterial RNA for spatial distribution [25] |
Experimental Workflow Visualization
Low-Biomass Microbiome Study Workflow
Germ-Free Animal Production Protocol
Protocol Development and Practical Implementation Frameworks
Standardized Criteria for Foster Mother Selection and Screening
Frequently Asked Questions (FAQs)
Q1: What are the most critical factors when selecting foster mothers for embryo transfer research? The most critical factors include the genetic strain of the foster mother, her proven maternal capability (prior successful pregnancy and weaning), age (optimally 3-4 months for mice), and health status (must be specific pathogen-free or germ-free). Research indicates that strain selection is paramount, as it significantly impacts pup survival rates, independent of the embryo's genetic background. For instance, BALB/c and NSG strains demonstrate superior nursing capabilities compared to C57BL/6J in germ-free settings [2].
Q2: Why is the genetic strain of the foster mother so important, and which strains perform best? Genetic strain directly influences maternal behavior, milk quality, and pup survival. Performance varies significantly between strains, as shown in the table below. Selecting a strain with proven high weaning success is crucial for experimental reproducibility [2].
Q3: What is the recommended protocol for preparing a foster mother to receive embryos? The key is to ensure the foster mother is pseudopregnant. This involves mating a fertile female with a vasectomized male. The successful formation of a vaginal plug confirms mating and is designated as day 0.5 of pseudopregnancy. Embryo transfer should be timed to coincide with the recipient's pseudopregnancy stage (e.g., 2.5 days post-coitus for blastocyst transfer) [2].
Q4: What are common reasons for pup loss after transfer to a foster mother, and how can they be mitigated? Common reasons include strain incompatibility, inexperienced foster mothers (first-time mothers may have higher failure rates), stress from environmental factors, and surgical stress on the donor mother during C-section. Mitigation strategies include using proven foster mothers, selecting high-performance strains like BALB/c or NSG, and minimizing environmental disturbances post-transfer [2].
Q5: How does the method of obtaining pups (e.g., natural mating vs. IVF) impact the success of fostering? Using In Vitro Fertilization (IVF) allows for precise control over the timing of embryo development and delivery date of the donor, which enhances experimental reproducibility. This is contrasted with natural mating, where predicting the exact delivery time is more challenging and can introduce variability [2].
Troubleshooting Guides
Issue: Low Pup Survival After Transfer
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Unsuitable Foster Strain | Review weaning success rates for the strain used. | Switch to a foster strain with documented high maternal performance, such as BALB/c or NSG [2]. |
| Inexperienced Foster Mother | Check the maternal history of the foster dam. | Use foster mothers that have successfully raised at least one litter previously [2]. |
| Environmental Stress | Monitor for noise, vibrations, or frequent cage disturbances. | House animals in a quiet, low-traffic area with minimal disturbances, especially in the first days post-transfer. |
| Health Status Compromise | Perform health monitoring on the foster mother colony. | Ensure all animals are specific pathogen-free (SPF) or germ-free (GF) and are housed in a controlled, sterile environment [2]. |
Issue: Inconsistent Results Across Experimental Replicates
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Variable Donor Timings | Record and compare the conception-to-delivery windows of donor dams. | Utilize IVF to generate donor embryos for precise synchronization of developmental stages with the recipient's pseudopregnancy [2]. |
| Non-Standardized Surgical Technique | Review the C-section procedure across technicians. | Implement a standardized, refined surgical method like the Female Reproductive Tract Preserved C-section (FRT-CS) to improve fetal survival rates consistently [2]. |
| Lack of Written Protocols | Check if a Standard Operating Procedure (SOP) exists and is followed. | Develop and adhere to a detailed written policy for all steps, from foster mother selection to post-operative care, to reduce operator-based bias and variability [26]. |
Experimental Data and Protocols
Quantitative Strain Performance Data
The following table summarizes key findings from a study evaluating different foster mother strains in germ-free mouse production. The weaning success rate is a critical metric of maternal capability [2].
Table 1: Comparison of Germ-Free Foster Mother Strain Performance
| Strain | Type | Weaning Success Rate | Key Maternal Characteristics |
|---|---|---|---|
| BALB/c | Inbred | Superior | Exhibited superior nursing and weaning success. |
| NSG (NOD/SCID Il2rg–/–) | Inbred | Superior | Exhibited superior nursing and weaning success. |
| KM (Kunming) | Outbred | Good | Acceptable maternal care. |
| C57BL/6J | Inbred | Lowest | Had the lowest weaning rate in germ-free conditions, contrasting with some SPF findings. |
Detailed Experimental Protocol: Optimized C-section and Fostering
This protocol is designed to maximize the efficiency of obtaining germ-free pups via C-section and fostering [2].
1. Preparation:
- Foster Mothers: Select proven 4-month-old females from a high-performing strain (e.g., BALB/c). House them individually.
- Donor Dams: Use timed-pregnant SPF females. IVF-derived donors are preferred for precise timing.
- Isolator & Environment: Sterilize the polyvinyl chloride (PVC) isolator and all supplies (food, water, bedding, instruments) via autoclaving. Pre-heat the interior to 40-45°C before the procedure. Prepare activated Clidox-S disinfectant.
2. Sterile C-section Procedure (FRT-CS method):
- Euthanize the donor dam at the predicted delivery date via cervical dislocation.
- Perform the C-section under aseptic conditions. Use the Female Reproductive Tract Preserved (FRT-CS) technique: selectively clamp only the cervix base, preserving the entire reproductive tract (ovary, uterine horn, cervix).
- Excise the uterine sac and immediately transfer it into a Clidox-S bath for disinfection.
- Quickly move the disinfected uterus into the sterile isolator. The entire procedure from euthanasia to isolator entry must be completed within 5 minutes to ensure pup viability and sterility.
3. Pup Extraction and Fostering:
- Inside the isolator, incise the amniotic membrane with sterile scissors to expose the pup.
- Wipe away amniotic fluid with a sterile cotton swab until spontaneous breathing is noted.
- Cut the umbilical cord.
- Immediately place the viable pups with the prepared foster mother. To improve acceptance, you can gently mix the scent by placing some of the foster mother's soiled bedding on the new pups.
4. Post-Operative Monitoring:
- Check for successful fostering (pups gathered in nest, milk spots visible) without causing undue stress.
- Collect fecal samples from weaned mice starting at 2 weeks post-transfer to confirm germ-free status via aerobic and anaerobic culture [2].
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials
| Item | Function/Application in Foster Studies |
|---|---|
| Inbred & Outbred Mouse Strains (e.g., BALB/c, C57BL/6, NSG, KM) | Used as foster mothers to test strain-dependent effects on pup survival and development. The strain is a key experimental variable [2]. |
| Clidox-S | A chlorine dioxide disinfectant used to sterilize the exterior of the uterine sac after C-section before introducing pups into a germ-free isolator [2]. |
| Germ-Free (GF) Isolator | A polyvinyl chloride (PVC) sterile isolator that provides a controlled, contaminant-free environment for maintaining GF foster mothers and pups post-transfer [2]. |
| Vasectomized Males | Used to induce pseudopregnancy in female foster mothers by mating. The presence of a vaginal plug confirms successful mating and timing for embryo transfer. |
| Specific Pathogen-Free (SPF) Donors | Serve as sources of embryos or pups for transfer, ensuring they are free from pathogenic viruses, bacteria, and parasites that could confound results [2]. |
Workflow and Process Diagrams
Foster Mother Selection and Screening Workflow
C-section and Fostering Experimental Setup
Comparative Analysis of Natural Mating vs. IVF for Donor Embryos
Troubleshooting Guides
FAQ 1: How do I choose between natural mating and IVF for generating donor embryos for embryo transfer studies?
Answer: The choice depends on your experimental priorities: precision in timing or maximizing natural survival rates. The table below compares the core characteristics of both methods.
| Characteristic | Natural Mating (NM) | In Vitro Fertilization (IVF) |
|---|---|---|
| Timing Control | Low. Requires monitoring for vaginal plugs (gestation day G0.5) and natural delivery from G18 [12]. | High. Allows precise scheduling of pre-labor C-section on the predicted delivery date [12]. |
| Experimental Reproducibility | Variable, due to inherent biological variance in mating and delivery timing [12]. | High. Enables precise control over donor delivery dates, enhancing reproducibility [12]. |
| Fetal Survival Rate Post-C-section | Not explicitly quantified, but implied to be the natural baseline [12]. | Comparable. No significant difference in pup survival or contamination rates after C-section was reported [12]. |
| Best Application | Studies where minimizing procedural intervention prior to C-section is a priority. | Studies requiring high synchronization of embryo/fetal ages or in experimental settings requiring precise scheduling [12]. |
FAQ 2: The fetal survival rate after sterile C-section is low. Which surgical technique can improve this?
Answer: Optimizing the cesarean technique can significantly improve fetal survival. The Female Reproductive Tract-preserving C-section (FRT-CS) method has demonstrated superior outcomes compared to the Traditional C-section (T-CS).
Experimental Protocol: Comparing C-section Techniques
- Objective: To evaluate the impact of two surgical techniques on fetal survival rates during sterile C-section derivation.
- Groups: Pregnant SPF mice are divided into two groups: T-CS and FRT-CS [12].
- T-CS Procedure: Clamps are placed at both the cervix base and the top of the uterine horn for removal [12].
- FRT-CS Procedure: Clamps are placed selectively only at the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, and cervix) [12].
- Outcome Measure: Fetal survival rate post-procedure. Results show FRT-CS significantly improves fetal survival rates while maintaining sterility [12].
FAQ 3: Which foster mother strain should I select to maximize pup weaning success in germ-free (GF) research?
Answer: Foster strain selection is critical. Maternal performance varies significantly between strains under GF conditions, sometimes contradicting data from specific pathogen-free (SPF) mice.
Experimental Protocol: Evaluating GF Foster Mother Maternal Care
- Objective: To assess the nursing capabilities and weaning success of different GF foster strains.
- Strains Tested: Three inbred (C57BL/6J, BALB/c, NSG) and one outbred (KM) strain are evaluated as GF foster mothers [12].
- Methodology: GF foster mothers (4 months old, previously parous) are presented with pups derived via C-section. Nursing behavior and weaning success are systematically recorded [12].
- Key Findings: BALB/c and NSG GF foster strains exhibited superior nursing and weaning success. C57BL/6J GF mice had the lowest weaning rate, a finding noted as being in stark contrast to the good maternal care observed in SPF C57BL/6J foster mothers [12].
Experimental Workflow Diagram
The diagram below outlines the decision pathway for selecting the donor embryo production method and foster mother strain, based on the troubleshooting guides.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists key materials and their functions for implementing the discussed methodologies.
| Item | Function / Application |
|---|---|
| SPF Donor Mice | Source of oocytes and sperm for generating embryos via Natural Mating or IVF. Common strains include C57BL/6 and BALB/c [12]. |
| GF Foster Mice | Recipient mothers for C-section-derived pups. Strains like BALB/c and NSG show superior weaning success [12]. |
| Clidox-S | A chlorine dioxide disinfectant used for sterilizing tissue samples and disinfecting the isolator environment during C-section procedures [12]. |
| Polyvinyl Chloride (PVC) Isolator | A sterile housing unit for maintaining germ-free mice, preventing external contamination [12]. |
| Heating Pad | Used to pre-warm the isolator before C-section to prevent pup hypothermia, a critical factor for survival [12]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the key advantage of using the Female Reproductive Tract-Preserving C-section (FRT-CS) over the traditional method?
The primary advantage is significantly improved fetal survival rates. The FRT-CS technique selectively clamps only the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, and cervix). This optimized surgical approach has been shown to enhance pup viability while maintaining sterility, which is critical for successful germ-free mouse production [12].
Q2: How does using In Vitro Fertilization (IVF) improve the efficiency of germ-free mouse production compared to natural mating?
IVF provides precise control over the timing of donor embryo delivery. In natural mating, predicting the exact delivery date is challenging, leading to inconsistencies. With IVF, the implantation of two-cell stage embryos is precisely timed (designated as embryonic day 0.5, or E0.5), allowing for scheduled pre-labor cesarean sections. This control enhances experimental reproducibility and planning efficiency [12].
Q3: Which germ-free mouse strain is the most suitable foster mother and why?
Among the strains evaluated, BALB/c and NSG mice exhibited superior nursing capabilities and higher weaning success rates for pups obtained via C-section. In contrast, C57BL/6J germ-free foster mothers had the lowest weaning rate. This is a critical consideration, as the performance of germ-free foster mothers can differ from their specific pathogen-free (SPF) counterparts [12].
Q4: What is the recommended timeframe for completing the entire C-section procedure to ensure pup survival?
To ensure both sterility and pup viability, the entire procedure—from euthanizing the donor female to transferring the disinfected pups to the sterile isolator—must be completed within 5 minutes. This rapid execution helps prevent hypothermia and other stress-related complications in the newborns [12].
Troubleshooting Common Issues
Issue 1: Low Post-Surgical Pup Survival Rate
- Potential Cause: Use of traditional C-section (T-CS) method or improper surgical technique.
- Solution: Adopt the Female Reproductive Tract-Preserving C-section (FRT-CS) method. Ensure the procedure is performed by trained personnel and completed within the 5-minute window. Use a heating pad pre-warmed to 40–45°C inside the isolator to prevent pup hypothermia [12].
Issue 2: Unpredictable Delivery Timing from Donor Mice
- Potential Cause: Reliance on natural mating, which leads to variability in gestation timing.
- Solution: Utilize IVF to generate donor embryos. This allows for precise scheduling of the C-section on the predicted delivery date, eliminating guesswork and improving the synchronization of pup delivery with the readiness of the GF foster mother [12].
Issue 3: Poor Acceptance and Weaning of Pups by Foster Mother
- Potential Cause: Inappropriate strain selection for foster duties.
- Solution: Select a proven GF foster strain such as BALB/c or NSG. Avoid using C57BL/6J mice as GF foster mothers due to their documented lower weaning rates. Ensure that foster mothers are experienced (have given birth once before) and are of optimal age (e.g., four months old) [12].
Issue 4: Contamination of the Germ-Free Colony
- Potential Cause: Inadequate disinfection during the transfer process or isolator integrity failure.
- Solution: Strictly follow aseptic techniques during the C-section. Use a validated disinfectant like Clidox-S for sterilizing the uterine sac and other materials entering the isolator. Regularly test the sterility of the isolator and the animals within it [12].
Summarized Data Tables
Table 1: Comparison of Cesarean Section Techniques
This table compares the two primary surgical methods for deriving germ-free mice, based on a study with 80 pregnant SPF mice (40 C57BL/6 and 40 BALB/c) [12].
| Technique | Description | Key Clamping Points | Impact on Fetal Survival |
|---|---|---|---|
| Traditional C-section (T-CS) | Standard surgical approach for fetal extraction. | Clamps placed at both the cervix base and the top of the uterine horn. | Lower fetal survival rates. |
| Female Reproductive Tract-Preserving C-section (FRT-CS) | Optimized technique that preserves the donor's reproductive anatomy. | Selectively clamps only the cervix base, preserving the ovary, uterine horn, and cervix. | Significantly improved fetal survival rates while maintaining sterility. |
Table 2: Evaluation of Germ-Free Foster Mother Strains
This table summarizes the maternal care performance of different GF mouse strains used as foster mothers, based on an evaluation of 15 females per strain [12].
| Mouse Strain | Strain Type | Maternal Care Performance | Weaning Success |
|---|---|---|---|
| BALB/c | Inbred | Superior nursing capabilities | High |
| NSG | Inbred | Superior nursing capabilities | High |
| KM | Outbred | Moderate nursing capabilities | Moderate |
| C57BL/6J | Inbred | Lowest nursing capabilities | Lowest |
Experimental Protocols
Protocol 1: Female Reproductive Tract-Preserving Cesarean Section (FRT-CS)
Objective: To aseptically derive germ-free mouse pups with high survival rates by preserving the donor female's reproductive tract during C-section [12].
Materials:
- Pregnant SPF donor mouse (at term)
- Surgical instruments (autoclaved)
- Clidox-S disinfectant
- Sterile polyvinyl chloride (PVC) isolator
- Heating pad
- Sterile swabs and surgical scissors
Methodology:
- Preparation: Euthanize the pregnant donor female via cervical dislocation. Pre-heat the isolator to 40-45°C using a heating pad.
- Surgery: Perform the C-section under aseptic conditions. Instead of clamping both ends of the uterus, place a clamp only at the cervix base. This preserves the integrity of the entire reproductive tract (ovaries, uterine horns).
- Extraction and Disinfection: Excise the uterus and immediately transfer it into the sterile isolator, disinfecting the exterior with Clidox-S.
- Pup Delivery: Inside the isolator, carefully incise the uterine sac and amniotic membrane with sterile scissors to expose the pup.
- Post-delivery Care: Gently wipe away amniotic fluid with a sterile cotton swab until spontaneous breathing is noted. Cut the umbilical cord.
- Timing: Ensure the entire process, from donor euthanasia to pup transfer into the isolator, is completed within 5 minutes to ensure viability and sterility.
Protocol 2: Utilizing IVF-Derived Donors for Timed Pregnancies
Objective: To achieve precise control over the delivery date of donor embryos for C-section, thereby enhancing experimental reproducibility [12].
Materials:
- SPF donor mice (oocyte and sperm donors)
- CD-1 female mice (embryo transfer recipients)
- IVF laboratory equipment
Methodology:
- IVF and Embryo Transfer: Perform in vitro fertilization using gametes from the desired SPF donor strain (e.g., C57BL/6J). Transfer the resulting two-cell stage embryos into pseudopregnant CD-1 recipient females.
- Date Designation: Designate the day of embryo implantation as embryonic day 0.5 (E0.5).
- Scheduling: Schedule the FRT-CS procedure for the predicted delivery date (typically around E19.5), based on the precisely known E0.5. This replaces the need to monitor naturally mated donors for vague signs of impending labor from gestation day 18 (G18) onward.
Experimental Workflow and Decision Pathway
Foster Mother Selection Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Germ-Free Mouse Production
| Item | Function/Brief Explanation |
|---|---|
| Clidox-S | A chlorine dioxide-based disinfectant used for sterilizing the exterior of the uterine sac and other materials before entry into the sterile isolator [12]. |
| Polyvinyl Chloride (PVC) Isolator | A sterile, sealed environment for housing germ-free mice after derivation. It acts as a barrier against external contaminants [12]. |
| SPF Donor Mice (e.g., C57BL/6, BALB/c) | Provide the embryos or term fetuses for rederivation. They are maintained under specific pathogen-free conditions to ensure health status is known before creating a germ-free line [12]. |
| GF Foster Mothers (e.g., BALB/c, NSG) | Lactating germ-free females that receive and nurse the pups derived via C-section. Their strain can critically impact the success of weaning [12]. |
| CD-1 Recipient Mice | A robust outbred strain often used as recipients for embryo transfer in IVF protocols to carry the donor embryos to term [12]. |
Troubleshooting Guide: Common Challenges in Endometrial Preparation
Q1: For a researcher using an ovulatory animal model, which endometrial preparation protocol should be prioritized to improve live birth rates and reduce complications?
A: In ovulatory models, natural cycle (NC) protocols should be prioritized. Recent high-quality evidence from randomized controlled trials demonstrates that NC leads to superior live birth rates and reduced obstetric complications compared to programmed (hormone replacement therapy, or HRT) cycles [27] [28].
- Evidence: A large RCT (n=902) found that NC resulted in a significantly higher live birth rate (54.0%) compared to HRT (43.0%), an absolute difference of 11.1 percentage points [27]. Another multicentre RCT (n=4,376) confirmed comparable live birth rates between NC (51.2%) and programmed cycles (50.1%), but found NC was associated with significantly lower risks of clinical pregnancy loss, hypertensive disorders, and postpartum haemorrhage [28].
- Troubleshooting Tip: If your model has intact ovarian function and regular cycles, defaulting to an HRT protocol may be suboptimal. NC creates a more physiologic endocrine environment, including the presence of a corpus luteum, which is absent in HRT cycles and is thought to be crucial for reducing maternal complications [27] [29].
Q2: How does the choice of endometrial protocol impact maternal safety outcomes in a research setting?
A: The choice of protocol has a significant impact on maternal safety profiles. Natural cycles are consistently associated with a lower risk of serious obstetric complications compared to artificial cycles [28] [27].
- Evidence: Compared to programmed cycles, NC protocols demonstrate:
- Troubleshooting Tip: When studying interventions where maternal vascular health is a key endpoint, selecting an NC protocol can minimize background rates of hypertension-related complications, providing a clearer signal of the intervention's effect.
Q3: In what scenarios is a programmed (HRT) cycle still the necessary protocol?
A: Programmed cycles remain essential for specific model conditions where ovarian function is absent or inadequate [29].
- Primary Indications:
- Troubleshooting Tip: For researchers using HRT cycles, pay close attention to luteal phase support. Evidence is conflicting on whether monitoring serum progesterone and adding intramuscular supplementation improves outcomes, but some trials show a benefit [28].
Q4: For subjects at high risk of Ovarian Hyperstimulation Syndrome (OHSS), which protocols are most effective?
A: For high-risk OHSS models, both Natural Cycle (NC) and Ovarian Stimulation (OS) protocols show superior pregnancy outcomes compared to HRT [31].
- Evidence: A propensity score-matched study in high-OHSS-risk patients found:
- Troubleshooting Tip: If an HRT cycle must be used in a high-OHSS-risk model, be vigilant for suboptimal pregnancy outcomes. Where possible, consider switching to an NC or mild OS protocol to improve success rates.
Quantitative Data Comparison
Table 1: Comparative Pregnancy Outcomes from Key Recent Studies
| Study/Group | Live Birth Rate | Clinical Pregnancy Rate | Miscarriage Rate | Key Maternal Safety Findings |
|---|---|---|---|---|
| COMPETE RCT (NC vs. HRT) [27] | NC: 54.0%HRT: 43.0% | Not specified | NC: Lower(RR 0.61) | NC group had lower rates of antepartum hemorrhage. |
| Multicentre RCT (Natural vs. Programmed) [28] | Natural: 51.2%Programmed: 50.1% | Not specified | Natural: 14.0%Programmed: 17.0% | Natural cycle had significantly lower risks of hypertensive disorders and postpartum haemorrhage. |
| High-OHSS Risk (NC vs. HRT) [31] | NC: Higher(aOR 1.50) | Not significantly different | Not significantly different | NC associated with a lower cesarean delivery rate. |
| High-OHSS Risk (OS vs. HRT) [31] | OS: Higher(aOR 2.53) | OS: Higher(aOR 1.86) | OS: Lower(aOR 0.29) | Not specified |
Table 2: Protocol Selection Guide Based on Model Characteristics
| Model Characteristic | Recommended Protocol | Rationale & Technical Notes |
|---|---|---|
| Regular Ovulation | Natural Cycle (NC) | Higher live birth rate, superior maternal safety profile. Requires monitoring of follicular growth and LH surge [27] [29]. |
| Anovulation / POI | Programmed Cycle (HRT) | Only viable option. Requires exogenous estrogen and progesterone [29]. |
| High OHSS Risk | NC or Ovarian Stimulation (OS) | Both superior to HRT for live birth. OS uses letrozole ± gonadotropins [31]. |
| Need for Scheduling Flexibility | Programmed Cycle (HRT) | Offers greater control over the timing of embryo transfer [30]. |
| Recurrent Implantation Failure (RIF) | Consider Adjuncts (e.g., PRP) | Intrauterine PRP infusion shows promise in improving pregnancy and live birth rates in RIF models [28]. |
Detailed Experimental Protocols
Protocol 1: Natural Cycle (NC) Endometrial Preparation
- Objective: To achieve endometrial receptivity by leveraging the model's natural hormonal cycle.
- Methodology:
- Initiation: Monitoring begins on day 5 of the spontaneous menstrual cycle.
- Follicular Monitoring: Serial transvaginal ultrasounds are performed to track the growth of the dominant follicle.
- Ovulation Trigger: When the dominant follicle reaches ≥17 mm in diameter, ovulation is triggered either by the endogenous LH surge (serum LH > 20 IU/L) or by administration of exogenous hCG (e.g., 10,000 IU) [27] [31].
- Timing of Transfer: Embryo transfer is scheduled based on the day of ovulation (+3 days for cleavage-stage embryos; +5 days for blastocysts) and the developmental stage of the embryo [27].
- Luteal Support: Vaginal micronized progesterone (e.g., 200 mg thrice daily) is initiated from the day of ovulation [27].
Protocol 2: Programmed Cycle (HRT) Endometrial Preparation
- Objective: To create a fully controlled, artificial endometrial environment using exogenous hormones.
- Methodology:
- Estrogen Priming: Oral estradiol valerate (6 mg/day) is started on day 5 of the menstrual cycle (induced or natural) [27] [31].
- Endometrial Assessment: After 10-12 days of estrogen, transvaginal ultrasound is used to assess endometrial thickness. A thickness of ≥7-8 mm is generally considered adequate. The estrogen dose can be increased if the response is suboptimal [30] [27].
- Endometrial Transformation: Once the endometrium is ready, endometrial transformation is initiated with intramuscular progesterone (e.g., 60 mg/day). This marks the first day of progesterone administration [31].
- Timing of Transfer: Embryo transfer is performed on the 4th day of progesterone for cleavage-stage embryos, or the 6th day for blastocysts [31].
- Luteal Support: Progesterone and estrogen support are continued until pregnancy testing and, if successful, until 10-12 weeks of gestation [30].
Signaling Pathways and Experimental Workflow
Protocol Selection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Endometrial Preparation Protocols
| Reagent / Material | Function / Application | Example in Protocol |
|---|---|---|
| Estradiol Valerate | Synthetic estrogen for endometrial proliferation in programmed cycles. | Used in HRT protocol for 10-12 days to build the endometrial lining [27] [31]. |
| Micronized Progesterone | Provides luteal phase support; prepares endometrium for implantation. | Used in both NC and HRT cycles after ovulation or for endometrial transformation [27] [28]. |
| Human Chorionic Gonadotropin (hCG) | Triggers final oocyte maturation and ovulation in natural or stimulated cycles. | Administered when dominant follicle is mature (e.g., >17mm) to induce ovulation [31]. |
| Letrozole | Aromatase inhibitor used for mild ovarian stimulation in OS protocols. | Administered on cycle days 3-5 in OS protocols for patients at high OHSS risk [31]. |
| Human Menopausal Gonadotropin (HMG) | Contains FSH and LH; used for controlled ovarian stimulation. | Used in OS protocols after letrozole priming to support follicular growth [31]. |
| GnRH Agonist (GnRHa) | Suppresses endogenous hormone activity before HRT. | Used in GnRHa+HRT protocol for pituitary down-regulation, often in models with endometriosis [30]. |
Environmental and Housing Considerations for Optimal Outcomes
This technical support guide outlines the critical environmental and housing parameters for optimizing foster mother selection in embryo transfer research. Consistent application of these protocols ensures animal welfare, maximizes reproductive outcomes, and enhances experimental reproducibility. The following sections provide detailed troubleshooting guidance and frequently asked questions to address common challenges.
Research Reagent & Material Solutions
Table 1: Essential materials and reagents for embryo transfer and housing.
| Item | Function | Technical Specifications |
|---|---|---|
| Polyvinyl Chloride (PVC) Isolators | Provides a sterile germ-free (GF) housing environment for foster mothers and pups post-cesarean derivation [2]. | - |
| Aspen Wood Shavings | Autoclaved bedding material changed weekly to maintain hygiene and environmental enrichment [2]. | Autoclaved at 121°C before use [2]. |
| Clidox-S | Chlorine dioxide disinfectant for sterilizing tissue samples and the external surface of items entering the isolator [2]. | Applied in a 1:3:1 dilution, activated for 15 minutes before use [2]. |
| Heating Pad | Prevents hypothermia in neonates during the cesarean section procedure and immediately after transfer [2]. | Pre-heated to 40–45°C for at least 15 minutes before the procedure begins [2]. |
| Columbia Blood Agar Plates | Used for aerobic and anaerobic culturing of fecal samples to routinely confirm sterility of GF colonies [2]. | - |
| Ham's F-10 Medium with EDTA | A culture medium used for in vitro fertilization that has been shown to support high fetal developmental potential in mouse models [32]. | 100 µM EDTA concentration improved fetal developmental potential to that of in vivo derived embryos [32]. |
Experimental Workflow & Housing Environment
The following diagram illustrates the logical workflow from foster mother preparation to weaning, highlighting key environmental control points.
Detailed Experimental Protocols
Germ-Free Isolator Preparation and Sterilization
Purpose: To establish and maintain a sterile environment for housing germ-free (GF) foster mothers and derived pups [2].
Methodology:
- Isolator Setup: Assemble polyvinyl chloride (PVC) isolators according to manufacturer specifications [2].
- Sterilization of Supplies: All life supplements, including food, water, bedding, and surgical instruments, must be autoclaved at 121°C for a minimum of 1200 seconds (20 minutes) before introduction into the isolator [2].
- Entry Protocol: A chemical dunk tank or rapid transfer port is used to introduce sterile supplies. Items are surface-sterilized with a chlorine dioxide solution (e.g., Clidox-S in a 1:3:1 dilution, activated for 15 minutes) before transfer [2].
- Environmental Control: Due to the heat insulation of PVC, use a heating pad set to 40–45°C for at least 15 minutes prior to any C-section procedure inside the isolator to prevent neonatal hypothermia [2].
Cesarean Section for Germ-Free Pup Derivation
Purpose: To aseptically derive germ-free pups from a donor mother and transfer them to a pseudopregnant GF foster mother [2].
Methodology:
- Donor Euthanasia: Euthanize the pregnant donor female via cervical dislocation [2].
- Surgical Techniques: Two primary methods can be compared:
- Traditional C-section (T-CS): Clamps are placed at both the cervix base and the top of the uterine horn.
- Female Reproductive Tract Preserved C-section (FRT-CS): Selectively clamps only the cervix base, preserving the entire reproductive tract. This method has been shown to significantly improve fetal survival rates [2].
- Fetal Extraction and Resuscitation: The uterine sac is transferred to a disinfectant bath (Clidox-S) and then into the sterile isolator. The amniotic membrane is incised, the pup is exposed, and the umbilical cord is cut. A sterile cotton swab is used to wipe away amniotic fluid until spontaneous breathing is noted [2].
- Time Constraint: The entire procedure, from donor euthanasia to pup transfer, must be completed within 5 minutes to ensure sterility and pup viability [2].
Frequently Asked Questions (FAQs)
Q1: Which mouse strain is most effective as a germ-free foster mother? A: Strain selection significantly impacts weaning success. Quantitative data demonstrates that BALB/c and NSG strains exhibit superior nursing and weaning success. In contrast, C57BL/6J GF foster mothers have the lowest weaning rate, which is a critical finding given their common use in research [2]. See Table 2 for comparative data.
Q2: What is the optimal technique for cesarean section in embryo transfer research? A: The Female Reproductive Tract Preserved C-section (FRT-CS) technique is recommended. Compared to the traditional method, FRT-CS, which involves clamping only the cervix base, has been shown to significantly improve fetal survival rates while maintaining sterility [2].
Q3: What are the critical environmental parameters for housing foster mothers? A: Precise environmental control is non-negotiable for reproductive success. The established standards are [2]:
- Light Cycle: 12-hour light/12-hour dark cycle (lights on at 08:00).
- Temperature: 22 ± 2°C.
- Relative Humidity: 55%. Housing should use sterile aspen wood shavings as bedding, changed weekly, with unrestricted access to autoclaved food and water.
Q4: How can we precisely control the delivery timing of donor mice for C-section? A: Utilizing in vitro fertilization (IVF) for obtaining donor embryos provides superior control over timing compared to natural mating. IVF enables precise scheduling of embryo implantation in recipient mice, allowing for accurate prediction of the delivery date and enhancing experimental reproducibility [2].
Troubleshooting Guides
Table 2: Troubleshooting common issues in foster mother studies.
| Problem | Potential Cause | Solution |
|---|---|---|
| Low Weaning Success | Suboptimal foster mother strain; C57BL/6J GF mothers show poor maternal care [2]. | Switch to a proven GF foster strain like BALB/c or NSG [2]. |
| Poor Fetal Survival Post-C-Section | Use of traumatic surgical technique or prolonged procedure time. | Adopt the FRT-CS technique and ensure the entire C-section is completed within 5 minutes [2]. |
| Inconsistent Donor Delivery Dates | Reliance on natural mating, which introduces variability in conception timing [2]. | Use IVF to generate donor embryos, allowing for precise control over the embryo transfer date and subsequent predicted delivery [2]. |
| Contamination of Germ-Free Colony | Breach in sterile protocol during isolator entry or C-section. | Strictly adhere to autoclaving and Clidox-S disinfection protocols. Routinely test sterility by culturing fecal samples on Columbia blood agar plates under both aerobic and anaerobic conditions [2]. |
Table 3: Comparative weaning success of different germ-free foster mother strains [2].
| Foster Mother Strain | Strain Type | Reported Weaning Success |
|---|---|---|
| BALB/c | Inbred | Superior |
| NSG | Inbred | Superior |
| KM | Outbred | Moderate |
| C57BL/6J | Inbred | Lowest |
Table 4: Standardized environmental housing parameters for rodent foster mothers [2].
| Parameter | Optimal Setting | Purpose |
|---|---|---|
| Light/Dark Cycle | 12 hours/12 hours | Regulates circadian rhythms and reproductive cycles. |
| Temperature | 22 ± 2°C | Prevents thermal stress. |
| Relative Humidity | ~55% | Maintains respiratory health and prevents dehydration. |
| Bedding | Sterile aspen wood shavings | Provides comfort, enrichment, and absorbs waste. |
| Cage Change Frequency | Once per week | Maintains hygiene and prevents ammonia buildup. |
Addressing Common Challenges and Enhancing Efficiency
Identifying and Mitigating Causes of Implantation Failure
Troubleshooting Guides
Guide 1: Troubleshooting Embryonic Causes of Implantation Failure
Issue: Embryos fail to implant despite normal morphological appearance.
Background: Embryo quality is the most significant factor affecting implantation, with even morphologically good-quality embryos potentially possessing undetectable abnormalities that prevent successful implantation [33] [34].
- Troubleshooting Table: Embryonic Factors
| Potential Cause | Diagnostic Method | Mitigation Strategy | Key References |
|---|---|---|---|
| Chromosomal Aneuploidy | Preimplantation Genetic Testing for Aneuploidy (PGT-A) [35] [9]. | Transfer of euploid embryos. PGT-A significantly increases implantation rates [9] [36]. | |
| Embryo Arrest/Developmental Competence | Extended culture to blastocyst stage (Day 5/6) allows for natural selection [37]. | Blastocyst transfer improves synchronization with endometrium and increases implantation rates [37]. | |
| Zona Pellucida Hardening | Observation during assisted hatching procedure [35]. | Laser-assisted hatching of the zona pellucida prior to transfer [35]. | |
| Impaired Cell Adhesion | Evaluation of blastocyst morphology, specifically the Trophectoderm (TE) and Inner Cell Mass (ICM) [37]. | Use of hyaluronan-enriched embryo transfer medium to facilitate embryo-endometrial interaction [35]. |
Experimental Protocol: Blastocyst Morphology Assessment
- Method: Morphological grading system per Gardner and Schoolcraft [37].
- Procedure:
- Assess degree of blastocoel expansion and hatching status (Score 1-6).
- Evaluate Inner Cell Mass (ICM): Grade A (tightly packed, many cells) to C (few cells).
- Evaluate Trophectoderm (TE): Grade A (many cells, cohesive epithelium) to C (few large cells).
- Application: High-quality blastocysts (e.g., 3AA, 4AB) are selected for transfer. The quality of the TE is critical for implantation, as it forms the placenta [37].
Guide 2: Troubleshooting Uterine and Maternal Causes of Implantation Failure
Issue: Failure of euploid embryos to implant, suggesting a uterine or maternal factor.
Background: The uterine environment must be receptive during the Window of Implantation (WOI). Imbalances can lead to rejection of even genetically normal embryos [35] [38].
- Troubleshooting Table: Uterine & Maternal Factors
| Potential Cause | Diagnostic Method | Mitigation Strategy | Key References |
|---|---|---|---|
| Chronic Endometritis (CE) | Hysteroscopy and endometrial biopsy with CD138 immunohistochemistry [35]. | Broad-spectrum antibiotics (e.g., Doxycycline); hysteroscopic surgery for CE linked to structural issues [35]. | |
| Anatomical Abnormalities | Hysteroscopy, Saline Infusion Sonography (SIS) [38]. | Hysteroscopic resection of submucosal fibroids, polyps, or uterine septum [38]. | |
| Thin Endometrium | Transvaginal ultrasound to measure endometrial thickness [38]. | Estradiol treatment; investigational therapies like intrauterine Platelet-Rich Plasma (PRP) or G-CSF [35]. | |
| Altered Window of Implantation (WOI) | Endometrial Receptivity Array (ERA) to detect displaced WOI [35] [39]. | Personalized Embryo Transfer (pET) based on diagnostic results [35]. | |
| Hydrosalpinx | Hysterosalpingogram (HSG) or laparoscopy [38]. | Laparoscopic salpingectomy or proximal tubal occlusion before IVF [38]. | |
| Vitamin D Deficiency | Serum 25-hydroxyvitamin D3 testing [35]. | Vitamin D supplementation to improve immune tolerance [35]. | |
| Thrombophilia | Thrombophilia screening (e.g., for Antiphospholipid Syndrome) [35]. | Low-dose aspirin, sometimes with low-molecular-weight heparin, starting post-implantation [35]. |
Experimental Protocol: Optimization of Foster Mother Selection
- Objective: To select foster mothers with optimal reproductive fitness and maternal characteristics to maximize pup survival and weaning rates in embryo transfer research [2].
- Strain Selection Criteria:
- Reproductive Fitness: Select strains with proven high fecundity and litter sizes.
- Maternal Behavior: Choose strains known for strong nursing capabilities and low pup rejection rates. Data shows BALB/c and NSG strains exhibit superior nursing and weaning success as germ-free foster mothers, while C57BL/6J had the lowest weaning rate in a germ-free environment [2].
- Genetic Background: Use F1 hybrids (e.g., [BALB/cByJ x C57BL/6]) or outbred strains (e.g., CD-1, Swiss Webster) for hybrid vigor, which often provides hardier pups and better maternal care [1] [2].
- Procedure:
- Preparation: Mate foster mothers with vasectomized males to induce pseudopregnancy.
- Timing: Perform embryo transfer on the appropriate day of pseudopregnancy.
- Monitoring: Continuously monitor for maternal behavior, pup retrieval, and nursing after birth.
Frequently Asked Questions (FAQs)
Q1: What is the definition of Recurrent Implantation Failure (RIF) in a clinical context? A: There is no universal definition, but one commonly used clinical definition is the failure to achieve a clinical pregnancy after the transfer of at least four good-quality embryos in a minimum of three fresh or frozen cycles in a woman under the age of 40 [38].
Q2: Does maternal age impact embryo quality independently of the uterus? A: Yes. Data from embryo donations to gestational carriers shows that the age of the embryo donor (oocyte source) is the primary factor determining success. Older women experience reduced embryo implantation even as gestational carriers, highlighting the dominant role of embryonic age over the uterine environment [9] [34].
Q3: What lifestyle factors can influence implantation success? A: Smoking, excessive alcohol consumption, and high body mass index (BMI) are associated with lower implantation rates. Smoking negatively affects egg quality and endometrial receptivity. High BMI can disrupt hormonal balance and is correlated with poorer blastocyst development [38] [36] [37]. Managing blood sugar levels is also crucial as high levels can create an adverse uterine environment [39].
Q4: Is surrogacy always the solution after repeated implantation failure? A: No. Research from egg donation cycles indicates that embryo quality, particularly egg health, is the biggest factor in implantation success. Switching to a surrogate may not improve success rates if the primary issue is embryo aneuploidy. Investigations should focus on improving embryo quality or using donor eggs before considering surrogacy [33].
Data Presentation
Table 1: Impact of Maternal Age on Embryo Implantation Potential
| Maternal Age | Approximate Implantation Rate per Embryo Transfer [33] | Likelihood of Embryo Chromosomal Abnormalities [33] |
|---|---|---|
| < 35 years | ~43% | Lower, begins to rise in early 30s |
| 41-42 years | ~9% | Over 75% |
Table 2: Comparison of Germ-Free Foster Mouse Strains for Maternal Care
| Mouse Strain | Weaning Success Rate | Key Maternal Characteristics |
|---|---|---|
| BALB/c | Superior [2] | Exhibits strong nursing capabilities and contributes significantly to pup weight gain. |
| NSG | Superior [2] | Excellent nursing capabilities observed in a germ-free environment. |
| KM (Outbred) | Not specified | Often used for hybrid vigor; requires empirical validation for specific conditions. |
| C57BL/6J | Lowest [2] | Contrasts with findings in Specific Pathogen-Free (SPF) conditions; performance is context-dependent. |
Visualizations
Diagram 1: Implantation Failure Diagnostic Workflow
Diagram 2: Foster Mother Selection Logic
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Experiment |
|---|---|
| Hybrid Strain Females (e.g., B6CBAF1/J) | Used as foster mothers for their documented hybrid vigor, excellent reproductive fitness, and strong maternal instincts, leading to higher pup survival rates [1] [2]. |
| Blastocyst Culture Media | Specialized sequential media systems that support embryo development from the cleavage stage to the blastocyst stage in vitro, enabling better embryo selection [37]. |
| Hyaluronan-Enriched Transfer Medium | A embryo transfer medium supplemented with hyaluronan, which is believed to improve embryo-endometrial interactions and adhesion during the implantation process [35]. |
| Gonadotropins (e.g., recombinant FSH) | Used for controlled ovarian stimulation in superovulation protocols to obtain a large number of oocytes or embryos from donor females for experimental use [1] [37]. |
| Clidox-S Disinfectant | A chlorine dioxide-based disinfectant used to sterilize the exterior of the uterine sac during sterile cesarean section procedures for deriving germ-free pups [2]. |
| CD138 Antibodies | Used for immunohistochemical staining of endometrial biopsy samples to identify plasma cells, which is the gold standard for diagnosing Chronic Endometritis (CE) [35]. |
Optimizing Surgical Techniques for Improved Fetal Survival Rates
Frequently Asked Questions (FAQs)
Q1: What are the primary surgical approaches for prenatal repair of open spina bifida, and how do they impact gestational age at birth?
Several surgical techniques exist for prenatal repair of open spina bifida, each with different outcomes for gestational age at delivery [40].
- Open Repair: Involves a laparotomy and a larger uterine hysterotomy (approximately 8 cm) to directly access and repair the fetus [41] [40].
- Mini-Hysterotomy: A modified open approach using a smaller uterine incision of 2.5–3.5 cm [40].
- Laparotomy-assisted Fetoscopic Repair: Requires a maternal laparotomy and uterine exteriorization, with the fetoscope introduced through ports for repair [40].
- Percutaneous Fetoscopic Repair: A minimally invasive technique using trocars placed percutaneously into the uterine cavity without a laparotomy [40].
A meta-analysis comparing these techniques found that the choice of surgical approach can influence the gestational age at delivery, which is a critical factor for fetal survival and development [40].
Table 1: Comparison of Surgical Techniques for Open Spina Bifida Repair
| Surgical Technique | Description | Reported Mean Gestational Age at Birth (weeks) |
|---|---|---|
| Laparotomy-assisted Fetoscopic | Laparotomy with fetoscopic ports for repair [40] | 35+3 to 35.62 [40] |
| Mini-Hysterotomy | Small uterine incision (2.5-3.5 cm) [40] | 34+2 [40] |
| Open Repair | Standard open hysterotomy [41] [40] | 34+1 [40] |
| Percutaneous Fetoscopic | Fully percutaneous, minimally invasive approach [40] | 32+3 to 32.36 [40] |
Q2: How does the selection of a germ-free (GF) foster mother strain impact the success of cesarean derivation in mouse models?
The genetic strain of the GF foster mother is a critical variable that significantly affects the weaning success of pups following cesarean derivation. Performance varies considerably between strains [12].
Table 2: Weaning Success Rates by GF Foster Mother Strain
| Foster Mother Strain | Strain Type | Weaning Success Rate | Key Characteristics |
|---|---|---|---|
| BALB/c | Inbred | Superior | Exhibits superior nursing and weaning success [12]. |
| NSG (NOD/SCID Il2rg–/–) | Inbred | Superior | Exhibits superior nursing and weaning success [12]. |
| KM (Kunming) | Outbred | Moderate | -- |
| C57BL/6J | Inbred | Lowest | Lowest weaning rate, contrary to its good maternal performance in SPF conditions [12]. |
Q3: What optimized cesarean technique can improve fetal survival rates in mouse models?
Research indicates that modifying the surgical technique during cesarean section can significantly impact fetal survival. The Female Reproductive Tract Preserved C-section (FRT-CS) technique has been shown to be superior to the traditional method [12].
- Traditional C-section (T-CS): Involves placing clamps at both the cervix base and the top of the uterine horn.
- FRT-CS Technique: Selectively clamps only the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, and cervix) [12].
Experimental results demonstrate that the FRT-CS technique significantly improves fetal survival rates while maintaining sterility, making it a recommended method for obtaining germ-free pups [12].
Troubleshooting Guides
Problem: Low weaning success of pups after surgical derivation and transfer to a foster mother.
Potential Causes and Solutions:
Suboptimal Foster Mother Strain:
- Cause: The genetic background of the foster mother can profoundly affect her maternal care and nursing capabilities.
- Solution: Carefully select the foster mother strain based on empirical evidence. As shown in Table 2, BALB/c and NSG strains are superior choices for GF foster mothers compared to C57BL/6J [12].
Traumatic or Inefficient Surgical Technique:
- Cause: The traditional C-section method may cause more tissue damage or stress, reducing pup viability.
- Solution: Implement the FRT-CS (Female Reproductive Tract Preserved C-section) technique. This method minimizes trauma by preserving the integrity of the uterus and associated structures, which has been proven to enhance fetal survival rates [12].
Inconsistent Donor Mother Delivery Timing:
- Cause: Relying on natural mating (NM) alone leads to variability in predicting exact delivery dates, making it difficult to schedule the C-section at the optimal time.
- Solution: Utilize In Vitro Fertilization (IVF) to generate donor mothers. IVF allows for precise control over the timing of embryo implantation, enabling accurate prediction of the delivery date and facilitating a planned pre-labor C-section, which improves experimental reproducibility and outcomes [12].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Germ-Free Mouse Derivation
| Item | Function/Description |
|---|---|
| PVC Isolators | Sterile housing units for maintaining germ-free animals after derivation [12]. |
| Clidox-S | A chlorine dioxide disinfectant used for sterilizing tissue samples and disinfecting the surgical and isolator environment [12]. |
| Heating Pad | Critical for maintaining pup body temperature during and immediately after the C-section procedure, as PVC isolators provide heat insulation [12]. |
| SPF Donor Mice | Specific pathogen-free animals used as sources of embryos or for timed pregnancies via natural mating or IVF [12]. |
| GF Foster Mice | Germ-free female mice of a selected strain (e.g., BALB/c, NSG) that have proven maternal success, used to nurse and wean the derived pups [12]. |
Experimental Workflow and Protocol
Detailed Methodology: Optimized Cesarean Derivation for Germ-Free Mouse Production
This protocol integrates the key optimized techniques discussed to maximize pup survival [12].
1. Pre-Surgical Preparation:
- Isolator Setup: Assemble and sterilize the polyvinyl chloride (PVC) isolator using a chlorine dioxide disinfectant like Clidox-S. Activate the heating pad inside the isolator to 40–45°C at least 15 minutes before the procedure to prevent pup hypothermia [12].
- Donor Selection: Use SPF donor females. For precise timing, utilize IVF-derived recipients, designating the day of two-cell stage embryo transfer as embryonic day 0.5 (E0.5). Schedule the C-section for the predicted delivery date [12].
- Foster Mother Preparation: Select a proven GF foster mother strain, such as BALB/c or NSG. The foster should be healthy, approximately four months old, and have prior successful birthing and nursing experience [12].
2. Surgical Procedure (FRT-CS Technique):
- Euthanize the pregnant donor female via cervical dislocation.
- Perform the C-section under strict aseptic conditions.
- Instead of the traditional method, employ the FRT-CS technique: clamp only the cervix base, preserving the entire reproductive tract (ovary, uterine horn, uterine junction, and cervix) [12].
- Quickly transfer the intact uterine sac to a container for disinfection with Clidox-S.
3. Post-Surgical Pup Recovery and Transfer:
- Immediately move the disinfected uterine sac into the pre-warmed sterile isolator.
- Carefully incise the amniotic membrane with surgical scissors to expose the pup.
- Cut the umbilical cord and use a sterile cotton swab to gently wipe away amniotic fluid until spontaneous breathing is observed.
- The entire procedure, from donor euthanasia to initiating pup breathing, must be completed within 5 minutes to ensure sterility and viability [12].
- Promptly present the viable pups to the prepared GF foster mother within the isolator.
Strategies for Precise Timing and Synchronization of Transfers
Troubleshooting Guides & FAQs
This technical support resource addresses common challenges in embryo transfer synchronization for research, providing evidence-based protocols to optimize the selection and use of foster mothers in germ-free animal production.
FAQ: Foster Mother Selection and Management
Q: What are the most critical factors in selecting an optimal foster mother strain for embryo transfer research?
A: The choice of foster mother strain significantly impacts pup survival and weaning success. Key factors include the strain's inherent maternal care capabilities, reproductive fitness, and genetic background relative to the transferred embryos.
- Maternal Care Capabilities: Different strains exhibit varying nursing abilities. Research indicates BALB/c and NSG strains demonstrate superior nursing and weaning success as germ-free foster mothers, while C57BL/6J showed the lowest weaning rates in germ-free conditions [2].
- Reproductive Fitness: F1 hybrids between two standard inbred strains (like C57BL/6 x CBA) are recommended for optimal reproductive fitness and mothering characteristics [1].
- Genetic Distinguishability: When using pseudopregnant females, select foster mothers with coat color differences (e.g., albino vs. pigmented) from the expected embryos to distinguish naturally-born pups from fostered ones [1].
Q: How can I precisely synchronize embryo development with the foster mother's receptive state?
A: Precise synchronization requires controlling both embryonic development stage and the foster mother's pseudopregnancy status.
- Embryo Stage Control: Utilize in vitro fertilization (IVF) to precisely control donor embryo delivery dates, enhancing experimental reproducibility compared to natural mating [2].
- Pseudopregnancy Induction: Mate sexually mature females with vasectomized males; the presence of a vaginal plug indicates successful mating and induction of pseudopregnancy, typically 2.5-3.5 days post-coitus [1].
- Hormonal Monitoring: In clinical models, serum progesterone tracking enables accurate transfer timing with fewer monitoring visits and lower cancellation rates [42].
Troubleshooting Common Synchronization Issues
Problem: Poor pup survival following transfer to foster mothers
Potential Causes and Solutions:
- Suboptimal Strain Selection: Replace with proven maternal care strains like BALB/c or NSG for germ-free models [2].
- Surgical Technique: Implement female reproductive tract-preserving cesarean section (FRT-CS), which significantly improves fetal survival rates while maintaining sterility compared to traditional methods [2].
- Procedure Timing: Complete entire transfer procedure within 5 minutes under sterile conditions to maximize viability [2].
Problem: Inconsistent receptivity in foster mothers
Potential Causes and Solutions:
- Variable Pseudopregnancy Induction: Use proven fertile stud males (2-8 months old) with successful mating records; provide 2-3 days rest between mating sessions [1].
- Environmental Stressors: Maintain controlled environmental conditions (12-hour light/dark cycle, 22 ± 2°C temperature, 55% relative humidity) [2].
- Health Status: Ensure foster mothers are healthy, parasite-free, and previously proven fertile [1].
Experimental Protocols & Workflows
Detailed Protocol: Optimized Foster Mother Preparation
Objective: Generate reproducibly pseudopregnant foster mothers with synchronized receptivity for embryo transfer.
Materials:
- Sexually mature female mice (8-12 weeks old) of selected strain
- Vasectomized proven male mice (2-8 months old)
- Sterile cages, bedding, and housing equipment
- Light cycle-controlled animal facility
Methodology:
- Strain Selection: Select F1 hybrid females (e.g., [BALB/cByJ x B6] or [B6 x CBA/CaJ]) for optimal superovulation response and maternal characteristics [1].
- Environment Synchronization: Acclimate females to controlled conditions (12-hour light/dark cycle, 22 ± 2°C, 55% humidity) for at least 7 days prior to mating [2].
- Mating Setup: Place 2 females with 1 vasectomized male per cage at the beginning of the dark cycle.
- Receptivity Confirmation: Check for vaginal plugs each morning; consider females with visible plugs as Day 0.5 of pseudopregnancy.
- Pre-Transfer Housing: House successfully mated females individually from late gestation through transfer to facilitate accurate monitoring [2].
Quantitative Data on Strain Performance
Table 1: Comparative Maternal Performance of Germ-Free Foster Mother Strains
| Strain | Nursing Capability | Weaning Success Rate | Recommended Application |
|---|---|---|---|
| BALB/c | Superior | High | Germ-free mouse production |
| NSG | Superior | High | Germ-free mouse production |
| KM (Outbred) | Moderate | Moderate | General research applications |
| C57BL/6J | Lowest | Lowest | Avoid for germ-free foster mothers [2] |
Table 2: Embryo Transfer Synchronization Strategies Comparison
| Strategy | Precision | Advantages | Limitations |
|---|---|---|---|
| Natural Mating | Variable | Physiological receptivity | Difficult timing prediction [2] |
| IVF + Timed Transfer | High | Precise delivery control | Requires technical expertise [2] |
| Serum Progesterone Monitoring | High | Fewer monitoring visits | Requires hormone testing [42] |
| LH Surge/Follicle Collapse | Moderate | Established protocol | Higher cancellation rates [42] |
Research Reagent Solutions
Table 3: Essential Materials for Embryo Transfer Synchronization
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Gonadotropins (PMSG/hCG) | Superovulation induction | Strain-dependent response; B6, BALB/cByJ, 129/SvJ are high responders [1] |
| Culture Media (G-IVF, G-1) | Embryo development support | Maintain at 37°C with 6% CO₂, 5% O₂ [43] |
| Progesterone Assays | Receptivity monitoring | Center-specific P4 thresholds enable accurate transfer timing [42] |
| Clidox-S | Surface disinfection | 1:3:1 dilution, activate 15 min before use [2] |
| Sterile PVC Isolators | Germ-free maintenance | Pre-heat to 40-45°C before C-section to prevent hypothermia [2] |
Experimental Workflow Visualization
Foster Mother Optimization Workflow
Transfer Synchronization Pathways
Managing Strain-Specific Limitations in Maternal Capability
Strain Performance Comparison Table
The table below summarizes the key quantitative findings from comparative studies on the maternal capabilities of different mouse strains used as germ-free foster mothers.
| Mouse Strain | Strain Type | Weaning Success Rate | Key Maternal Characteristics | Recommended Application |
|---|---|---|---|---|
| BALB/c | Inbred | Superior [12] | Exhibits superior nursing capabilities; milk contributes significantly to pup weight gain [12] | High-priority candidate for reliable foster mother selection |
| NSG (NOD/SCID Il2rg–/–) | Inbred | Superior [12] | Demonstrated excellent nursing and weaning success [12] | High-priority candidate for reliable foster mother selection |
| KM (Kunming) | Outbred | Good (Study Included) [12] | Evaluated for nursing capabilities alongside inbred strains [12] | Viable alternative when inbred foster mothers are unavailable |
| C57BL/6J | Inbred | Lowest Weaning Rate [12] | Poor nursing performance as a germ-free foster mother, contrary to its behavior under SPF conditions [12] | Not recommended for use as a germ-free foster mother |
Troubleshooting FAQ
Q1: Our C57BL/6J germ-free foster mothers are consistently showing low weaning success. Is this a common issue and what are our alternatives?
Yes, this is a documented and significant issue. Research has found that the C57BL/6J strain has the lowest weaning rate when used as a germ-free foster mother, which is in stark contrast to its active maternal care behavior under Specific Pathogen-Free (SPF) conditions [12].
- Recommended Action: Switch to a strain with proven maternal capabilities in a germ-free environment. The data indicates that BALB/c and NSG strains exhibit superior nursing and weaning success and should be prioritized as alternatives [12].
Q2: How can we achieve more precise timing for cesarean sections to improve pup viability?
Reliance on natural mating (NM) of donor mice introduces variability in predicting delivery dates. To address this, integrate In Vitro Fertilization (IVF) into your workflow [12].
- Solution: Using IVF-derived embryos allows for precise control over the timing of embryo transfer. You can designate this day as embryonic day 0.5 (E0.5), enabling the scheduling of pre-labor cesarean sections on the predicted delivery date with high accuracy, thereby enhancing experimental reproducibility and fetal survival [12].
Q3: What surgical technique can improve fetal survival rates during sterile C-section?
The surgical method for cesarean section significantly impacts outcomes. The traditional C-section (T-CS) involves clamping both the cervix base and the top of the uterine horn.
- Optimized Protocol: Implement the Female Reproductive Tract Preserved C-section (FRT-CS). This technique selectively clamps only the cervix base, preserving the entire reproductive tract. Studies have shown that FRT-CS significantly improves fetal survival rates while maintaining sterility [12].
Experimental Protocols for Optimization
Protocol 1: Female Reproductive Tract Preserved Cesarean Section (FRT-CS)
Objective: To extract fetuses aseptically while maximizing neonatal survival for germ-free mouse production [12].
Methodology:
- Euthanize the pregnant SPF donor female via cervical dislocation.
- Perform the C-section under strict aseptic conditions.
- Instead of clamping both the cervix and the top of the uterine horn (as in T-CS), place clamps only at the cervix base.
- Carefully preserve the entire reproductive tract, including the ovary, uterine horn, uterine junction, and cervix.
- Excise the uterine sac and transfer it to a disinfectant solution (e.g., Clidox-S) for sterilization.
- Rapidly transfer the disinfected uterine sac into a sterile polyvinyl chloride (PVC) isolator.
- Inside the isolator, incise the amniotic membrane with surgical scissors to expose the pup.
- Cut the umbilical cord and use a sterile cotton swab to wipe away amniotic fluid until spontaneous breathing is noted.
- The entire procedure, from the start of the C-section to the transfer of pups into the isolator, must be completed within 5 minutes to ensure pup viability and sterility [12].
Protocol 2: Integrating IVF with C-Section for Timed Pregnancies
Objective: To precisely control the delivery date of donor embryos, eliminating the variability of natural mating [12].
Methodology:
- Obtain donor embryos via In Vitro Fertilization (IVF) using gametes from the desired donor strain (e.g., C57BL/6J).
- Transfer the resulting two-cell stage embryos into a recipient female. The day of implantation is designated as embryonic day 0.5 (E0.5).
- Use these IVF-derived females as your donor mothers. Schedule the pre-labor FRT-CS for the predicted delivery date with high accuracy.
- This approach decouples the genetic background of the embryo from the maternal environment of the donor, allowing for precise scheduling and improved reproducibility [12].
The Scientist's Toolkit: Essential Research Reagents
| Item / Reagent | Function / Application |
|---|---|
| Germ-Free Foster Strains (BALB/c, NSG) | Providing optimal maternal care and nursing for cesarean-derived germ-free pups [12] |
| Clidox-S | Chlorine dioxide-based disinfectant used for sterilizing tissue samples and disinfecting the isolator environment [12] |
| Polyvinyl Chloride (PVC) Isolator | Sterile barrier facility for housing germ-free mice and performing post-C-section pup handling [12] |
| Aspergillus shavings | Autoclaved bedding material for germ-free mouse housing [12] |
| Heating Pad | Critical for maintaining pup body temperature during the C-section procedure; should be pre-heated to 40–45°C [12] |
Workflow and Decision Diagrams
DOT Script: Foster Mother Selection
DOT Script: Optimized GF Mouse Production
Luteal Phase Support and Progesterone Monitoring Protocols
Troubleshooting Guides
Guide 1: Addressing Low Serum Progesterone in Hormone Replacement Therapy-Frozen Embryo Transfer (HRT-FET) Cycles
Problem: Despite progesterone supplementation, serum progesterone levels remain below the target threshold on the day of embryo transfer, potentially compromising live birth rates.
Solution: Implement a combined progesterone protocol using vaginal and injectable routes.
- Recommended Protocols: Based on a randomized controlled trial, the following two protocols were most effective for women with serum progesterone <10 ng/mL [44]:
- Protocol A: 600 mg vaginal progesterone + 50 mg intramuscular (IM) progesterone daily.
- Protocol B: 600 mg vaginal progesterone + 25 mg subcutaneous (SC) progesterone daily.
- Expected Outcomes: These combined protocols achieved [44]:
- Significantly higher serum progesterone levels.
- Clinical pregnancy rates of 70% and 68%, respectively.
- Live birth rates of 83% and 84%, respectively.
- Lower rates of early pregnancy loss.
Application in Foster Mother Selection: For embryo transfer research, ensure recipient females have adequate luteal support. Monitor serum progesterone on the day of transfer and consider a combined supplementation protocol if levels are low to optimize the uterine environment for embryo implantation and development.
Guide 2: Optimizing Luteal Support for Frozen Embryo Transfer (FET) Cycles
Problem: Identifying the most effective luteal support strategy to improve key reproductive outcomes like clinical pregnancy in FET cycles.
Solution: Supplement a standard vaginal progesterone regimen with a GnRH agonist.
- Recommended Protocol: Add 0.1 mg of a subcutaneous GnRH agonist (such as leuprolide) in a single (on Day 3 post-embryo transfer) or double dose (on Day 3 and Day 6 post-embryo transfer) schedule [45].
- Supporting Evidence: A network meta-analysis found that adding a GnRH agonist to vaginal progesterone significantly improved clinical pregnancy rates (Risk Ratio 1.86) compared to vaginal progesterone alone [45]. Luteal support should be continued until Week 12 of pregnancy.
Research Context: While directly applicable to clinical IVF, this protocol underscores the importance of robust luteal phase manipulation. In rodent models, the principles of hormonal support to synchronize embryo development with the uterine environment are equally critical. The choice of an F1 hybrid or outbred foster mother with proven maternal instincts provides the physiological basis upon which these hormonal protocols act [1].
Frequently Asked Questions (FAQs)
FAQ 1: What is the target serum progesterone level on the day of frozen embryo transfer?
Answer: Monitoring serum progesterone is recommended. One prospective cohort study in HRT-FET cycles found a positive association between serum progesterone levels on transfer day and live birth rates. The research suggested a threshold of 26.95 ng/ml was significant for live birth, with a sensitivity of 82% and specificity of 43% [46]. Another study observed significantly lower clinical pregnancy rates when progesterone levels were in the lowest quartile (≤23.84 ng/ml) [46].
FAQ 2: Does the stage of embryo development affect how progesterone levels impact outcomes?
Answer: Yes, the impact of elevated progesterone (P) at the end of the stimulation phase (ovulation trigger) varies. In fresh IVF cycles, elevated progesterone at trigger is associated with a lower live birth rate for Day 3 (cleavage-stage) embryo transfers but not for Day 5 (blastocyst-stage) transfers [47]. This highlights the differing synchronization requirements between embryos and the endometrium based on developmental stage.
FAQ 3: What are the key characteristics of an ideal foster mother for embryo transfer in research?
Answer: The primary considerations are reproductive fitness and strong maternal instincts. For mouse models, the recommended choices are [1]:
- F1 hybrids (e.g., from a cross between C57BL/6 and CBA strains).
- Outbred strains (e.g., CD-1 or Swiss Webster). These strains generally exhibit excellent maternal care and reproductive performance. A recent study on germ-free mouse production also found that BALB/c and NSG strains showed superior nursing and weaning success as foster mothers [12].
Data Presentation: Progesterone Protocol Outcomes
Table 1: Comparison of Luteal Support Protocols in Frozen Embryo Transfer (FET) Cycles
| Protocol | Clinical Pregnancy Rate | Live Birth Rate | Key Findings |
|---|---|---|---|
| VP + GnRH agonist (Single/Dose) [45] | Significantly improved (RR 1.86) | Not Specified | Single (Day 3) or double (Day 3 & 6) dose upon VP regimen. |
| 600 mg VP + 50 mg IM P4 [44] | 70% | 83% | Highest clinical pregnancy and live birth rates. |
| 600 mg VP + 25 mg SC P4 [44] | 68% | 84% | Comparable to IM protocol; less invasive. |
| 800 mg VP (Monotherapy) [44] | Lower than combined protocols | Lower than combined protocols | Vaginal progesterone alone was less effective. |
| VP + 30 mg Oral P4 [44] | Lower than combined protocols | Lower than combined protocols | Least effective protocol in the study. |
Table 2: Impact of Progesterone Levels on FET Outcomes
| Progesterone Metric | Threshold Level | Associated Outcome | Study Details |
|---|---|---|---|
| Live Birth Threshold [46] | 26.95 ng/ml | AUC 0.64; Sensitivity 82%, Specificity 43% | Measured on FET day with VP+IM supplementation. |
| Low Prognosis Quartile [46] | ≤ 23.84 ng/ml | Significantly lower clinical pregnancy rate | Lowest quartile of serum progesterone levels. |
Experimental Protocols
Protocol 1: Combined Progesterone Support for HRT-FET
Objective: To achieve optimal serum progesterone levels and pregnancy outcomes in women with low progesterone (<10 ng/mL) undergoing HRT-FET [44].
Methodology:
- Population: Women under 35 with unexplained infertility.
- Endometrial Preparation: Administer 6 mg of oestradiol valerate orally daily.
- Luteal Phase Support: Once the endometrial lining is ready, initiate one of the following progesterone protocols until pregnancy test or beyond:
- Group 1 (Control): 600 mg vaginal progesterone daily.
- Group 2 (Control): 800 mg vaginal progesterone daily.
- Group 3 (Experimental): 600 mg vaginal progesterone + 50 mg intramuscular progesterone daily.
- Group 4 (Experimental): 600 mg vaginal progesterone + 25 mg subcutaneous progesterone daily.
- Group 5 (Control): 600 mg vaginal progesterone + 30 mg oral progesterone daily.
- Measurement: Assess serum progesterone levels on the day of embryo transfer.
- Primary Outcomes: Live birth rate and clinical pregnancy rate.
Protocol 2: GnRH Agonist Adjuvant for Luteal Support
Objective: To enhance clinical pregnancy rates in frozen embryo transfer cycles by adding a GnRH agonist to standard vaginal progesterone support [45].
Methodology:
- Population: Women undergoing frozen embryo transfer.
- Standard Support: Administer vaginal progesterone regimen.
- Intervention: Add 0.1 mg of a subcutaneous GnRH agonist (e.g., leuprolide).
- Single Dose: Administer on Day 3 after embryo transfer.
- Double Dose: Administer on Day 3 and Day 6 after embryo transfer.
- Support Duration: Continue all luteal support until the 12th week of gestation.
- Primary Outcome: Clinical pregnancy rate.
Signaling Pathways and Workflows
Luteal Support Decision Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Luteal Phase Support Research
| Reagent / Material | Function / Application | Research Context & Considerations |
|---|---|---|
| Micronized Progesterone (Vaginal) | Standard luteal phase support; prepares and maintains endometrial receptivity. | The base of most protocols. Dose typically 600-800 mg daily [44]. |
| Progesterone for Injection (IM/SC) | Rapidly increases systemic serum progesterone levels. | Used in combination therapy (e.g., 50 mg IM, 25 mg SC) to overcome low levels [44]. |
| GnRH Agonist (e.g., Leuprolide) | Adjuvant to progesterone support; may improve endometrial receptivity. | Low dose (0.1 mg) administered subcutaneously post-embryo transfer [45]. |
| Estradiol Valerate | Prepares the endometrial lining in HRT-FET cycles prior to progesterone initiation. | Typically administered orally (e.g., 6 mg daily) for endometrial priming [46]. |
| F1 Hybrid or Outbred Foster Mice | Provides the in vivo uterine environment for embryo development. | Selected for optimal reproductive fitness and maternal instincts (e.g., B6xCBA F1, CD-1) [1]. Superior nursing by BALB/c & NSG strains noted [12]. |
Assessment Metrics and Outcome Validation Approaches
Quantitative Metrics for Evaluating Foster Mother Performance
This technical support resource provides troubleshooting guides and FAQs to assist researchers in selecting and evaluating foster mothers for embryo transfer research, a critical step in generating germ-free (GF) animal models.
Frequently Asked Questions
What are the key quantitative metrics for evaluating foster mother performance? The primary quantitative metrics are pup survival rates at key developmental stages and the weaning success rate. These metrics are used to objectively compare the performance of different foster mother strains [2].
Which foster mother strain has the best weaning success rate for germ-free pups? Studies show significant variation between strains. BALB/c and NSG GF foster mothers demonstrated superior nursing capabilities and higher weaning success rates. In contrast, C57BL/6J GF foster mothers had the lowest weaning rate, a finding that differs from their performance under specific pathogen-free (SPF) conditions [2].
How can I control the timing of donor mother delivery for my C-section experiment? Using in vitro fertilization (IVF) to generate donor embryos allows for precise control over the delivery date, enhancing experimental reproducibility. This method is superior to relying on the variable timing of natural mating [2].
Does the cesarean section technique impact pup survival? Yes, the surgical technique is critical. The Female Reproductive Tract Preserved C-section (FRT-CS) method, which selectively clamps only the cervix base, has been shown to significantly improve fetal survival rates compared to the traditional C-section technique [2].
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| Low pup survival after transfer | Suboptimal foster mother strain; inadequate maternal care. | Select a proven strain like BALB/c or NSG as the GF foster mother [2]. |
| Inconsistent delivery timing | Reliance on natural mating of donor mothers. | Use IVF to generate donor embryos for precise control over the pregnancy timeline [2]. |
| Low fetal survival post C-section | Use of a traumatic surgical technique. | Implement the FRT-CS method to preserve the reproductive tract and improve neonatal survival [2]. |
| Pup hypothermia | Inadequate temperature control during procedure. | Pre-heat the isolator with a heating pad to 40–45 °C for at least 15 minutes before the C-section begins [2]. |
Experimental Protocols & Data
Comparative Performance of Germ-Free Foster Mother Strains
The following table summarizes quantitative weaning success data from a study evaluating different strains as GF foster mothers [2].
| Foster Mother Strain | Strain Type | Maternal Care Performance | Weaning Success Rate |
|---|---|---|---|
| BALB/c | Inbred | Superior | High |
| NSG | Inbred | Superior | High |
| KM | Outbred | Not Specified | Intermediate |
| C57BL/6J | Inbred | Lowest | Low |
Optimized Workflow for Germ-Free Mouse Generation
The diagram below illustrates the integrated experimental workflow, combining optimized techniques from donor preparation to foster mother selection.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Experiment |
|---|---|
| PVC Isolator | Provides a sterile environment for housing GF mice and performing C-sections [2]. |
| Clidox-S | A chlorine dioxide disinfectant used to sterilize tissue samples and disinfect the isolator environment [2]. |
| Aspen Wood Shavings | Autoclaved bedding material for GF mouse cages, changed weekly [2]. |
| Heating Pad | Used to pre-heat the isolator to 40-45°C to prevent pup hypothermia during the C-section procedure [2]. |
Comparative Analysis of Inbred and Outbred Strain Efficacy
This technical support guide provides a comparative analysis of inbred and outbred mouse strains to assist researchers in optimizing experimental designs, particularly within the context of foster mother selection for embryo transfer research. The longstanding assumption in biomedical research has been that inbred strains, due to their genetic uniformity, yield more consistent and reproducible data than their outbred counterparts. However, contemporary research challenges this paradigm, demonstrating that outbred stocks often display comparable or even superior phenotypic stability while offering greater genetic diversity that may better model human populations [48] [49]. This resource addresses specific experimental issues through troubleshooting guides and FAQs, supported by quantitative data and detailed protocols.
Strain Selection Guide
Key Definitions and Characteristics
- Inbred Strains: Produced by a minimum of 20 consecutive generations of brother-sister mating, resulting in animals that are genetically nearly identical (isogenic) and homozygous at most loci [50] [51]. Examples include C57BL/6, BALB/c, and FVB/N.
- Outbred Stocks: Maintained as closed, randomly-mating populations to maintain high levels of genetic heterogeneity. Examples include CD-1, ICR, and Swiss Webster [52] [51].
Comparative Performance Tables
Table 1: General Characteristics of Inbred vs. Outbred Mice [48] [50] [53]
| Characteristic | Inbred Strains | Outbred Stocks |
|---|---|---|
| Genetic Uniformity | High (Isogenic) | Heterogeneous |
| Homozygosity | ~98.6% or higher [53] | Variable |
| Phenotypic Variability | Not consistently lower than outbred [48] | Comparable to or lower than inbred in some measures [48] |
| Average Litter Size | Smaller (e.g., 3-9 pups) [48] | Larger (e.g., ~12 pups in CD-1) [48] |
| Average Weight (70-day male) | ~25.4 g [48] | ~34.7 g [48] |
| Cost-Effectiveness | Lower fecundity can increase cost | Higher fecundity often reduces cost per animal |
| Preferred Research Applications | Immunological studies, genetic mapping, molecular genetic studies, defined disease models [48] | Toxicology, infectious disease, behavioral studies, generalizable research [48] [54] |
Table 2: Foster Mother Performance of Different Strains in Germ-Free Rederivation [2]
| Strain | Strain Type | Weaning Success Rate | Key Maternal Behaviors |
|---|---|---|---|
| BALB/c | Inbred | Superior | Exhibits superior nursing; milk contributes significantly to pup weight gain. |
| NSG | Inbred | Superior | Excellent nursing capabilities. |
| KM | Outbred | Moderate | Adequate maternal care. |
| C57BL/6J | Inbred | Lowest (in GF conditions) | Lower weaning success in germ-free conditions, contrary to SPF findings. |
Table 3: Behavioral and Physiological Comparisons (C57BL/6 vs. CD1) [53]
| Parameter | C57BL/6 (Inbred) | CD1 (Outbred) |
|---|---|---|
| Locomotor Activity | Lower | Higher |
| Breakpoint (Motivation in PR schedule) | Lower | Higher |
| Impulsivity (MPR model) | Lower | Higher |
| Aggression (Males) | Less aggressive | More aggressive [53] |
| Spatial Memory Performance | Better in Barnes Maze, Multiple T-maze | Better in Morris Water Maze [53] |
Troubleshooting Guides
Problem: High Pup Mortality in Germ-Free Rederivation
Issue: Poor survival of pups following sterile C-section and transfer to foster mothers.
Solutions:
- Optimize Surgical Technique: Implement the Female Reproductive Tract Preserving C-section (FRT-CS) method. This technique, which involves clamping only the cervix base rather than both the cervix and the top of the uterine horn, has been shown to significantly improve fetal survival rates while maintaining sterility [2].
- Select an Optimal Foster Strain: Do not assume the most common inbred strain is the best foster mother. Data indicates that under germ-free conditions, BALB/c and NSG strains are superior foster mothers compared to C57BL/6J, which had the lowest weaning rate [2].
- Control Donor Delivery Precisely: Utilize in vitro fertilization (IVF) to generate donor embryos. This allows for precise scheduling of donor delivery dates, reducing unpredictability and improving the coordination of C-section with the readiness of the foster mother [2].
Problem: High Phenotypic Variability Skewing Results
Issue: Unexpectedly high variability in experimental results, assumed to be lower when using inbred strains.
Solutions:
- Re-evaluate Strain Choice: The assumption that inbred strains always yield less variable data is not universally true. A systematic review found no significant difference in phenotypic variability between inbred and outbred mice for many traits [48] [49]. Consider whether an outbred stock with a larger effective population size might provide more robust and generalizable results for your specific assay.
- Increase Sample Size Cautiously: If using an outbred stock, a moderate increase in sample size may be necessary to account for genetic heterogeneity, though this is not always the case [54].
- Verify Strain Purity: Inbred mice are not perfectly isogenic. Genetic drift can occur in production colonies away from the colony nucleus, introducing genetic variation [55]. Source animals from reputable suppliers with transparent breeding practices.
Problem: Poor Translation of Inbred Mouse Findings to Human Relevance
Issue: Promising results in an inbred mouse model fail to hold up in later stages of drug development or human trials.
Solutions:
- Incorporate Genetic Diversity Early: Use outbred stocks like the Diversity Outbred (DO) mice for preclinical validation. These populations incorporate a wider range of genetic variation, making them better at identifying genotype-dependent toxicity and efficacy, similar to the genetic heterogeneity found in human populations [48] [54] [49].
- Use a Multi-Strain Approach: If outbred stocks are not feasible, validate key findings across multiple inbred strains to ensure the effect is not strain-specific.
Frequently Asked Questions (FAQs)
Q1: I always use inbred mice to minimize variability. Is this practice incorrect? A: It is not incorrect, but it may not be optimal for all research questions. While inbred strains are essential for studies requiring genetic standardization (e.g., immunology, genetic engineering), evidence shows that for many traits, outbred mice are not more variable. Furthermore, the genetic diversity in outbred stocks can provide a more robust test of an intervention's efficacy across different genetic backgrounds, potentially enhancing the translatability of your findings [48] [49].
Q2: Why would I choose an outbred foster mother over an inbred one? A: Outbred females, such as the KM strain or CD-1, are often hardier, have larger litters, and exhibit strong maternal instincts. However, the choice is context-dependent. For germ-free rederivation, data shows specific inbred strains like BALB/c can be superior [2]. The optimal choice should be based on empirical data for your specific procedure and environmental conditions.
Q3: Are commercially available outbred mice truly "outbred"? A: While more genetically diverse than inbred strains, common outbred stocks like Swiss Webster and CD1 descend from a limited founder population. They are less diverse than wild mice, and some heterozygosity is lost over time due to the finite size of breeding colonies [52] [54]. However, they remain a highly useful source of genetic heterogeneity for research.
Q4: My results in C57BL/6 mice were not replicated in CD1 mice. What does this mean? A: This is a common experience. C57BL/6 and CD1 mice differ profoundly in their baseline physiology and behavior, as shown in Table 3. A treatment effect observed in one genetic background may be absent, diminished, or even reversed in another. This does not invalidate your initial finding but highlights its genetic specificity. This outcome underscores the importance of genetic background as a biological variable [53].
Essential Experimental Protocols
Objective: To aseptically derive germ-free pups with high survival rates. Applications: Generation of germ-free mouse lines, health monitoring, and microbiome studies.
Materials:
- Pregnant donor dam (timed-pregnant, SPF)
- Anesthetic and euthanasia equipment
- Surgical instruments (autoclaved)
- Clidox-S disinfectant or equivalent
- Sterile isolator or biosafety cabinet
- Pre-warmed heating pad (40-45°C)
- Germ-free foster mother (e.g., BALB/c or NSG)
Method:
- Preparation: Euthanize the pregnant donor dam at the appropriate gestational stage. Ensure the sterile isolator is heated and all instruments are disinfected.
- Exposure: Place the donor on its back and wet the abdomen with disinfectant. Make a midline incision to expose the uterine horns.
- Clamping: Identify the cervix. In FRT-CS, place a clamp only at the base of the cervix, preserving the integrity of the entire uterine horn and ovaries.
- Excision: Transect the tissue above the clamp to free the uterus. Transfer the entire uterus rapidly into the sterile isolator.
- Pup Extraction: Inside the isolator, incise the uterine wall and amniotic sac to deliver each pup. Wipe away amniotic fluid with a sterile swab until spontaneous breathing is noted.
- Transfer: Once pups are breathing normally, transfer them to the cage of a proven germ-free foster mother. The entire procedure from euthanasia to transfer should be completed within 5 minutes to maximize survival.
Objective: To quantitatively estimate the incentive motivation of mice for a reward (e.g., food, water, drug). Applications: Behavioral neuroscience, pharmacology, and psychiatrics.
Materials:
- Operant conditioning chambers (with lever or nose-poke operandum)
- Software for controlling PR schedules and data collection
- Water- or food-restricted mice (e.g., C57BL/6 and CD1 for comparison)
Method:
- Habituation & Training: Water or food restrict mice to approximately 85-90% of free-feeding body weight to ensure motivation. Train mice to reliably press a lever or nose-poke for a reward on a fixed-ratio 1 (FR1) schedule.
- Progressive Ratio Schedule: Once trained, switch to a PR schedule (e.g., PR3). In this schedule, the response requirement to earn each subsequent reward increases according to a predetermined formula (e.g., 1, 4, 7, 10, 13...).
- Testing: Run daily sessions. A session typically ends when the mouse fails to complete a ratio requirement within a set time (e.g., 10 minutes).
- Data Collection: The primary outcome measure is the breakpoint—the highest completed ratio in a session. This represents the maximum effort the animal is willing to expend for a single reward.
- Advanced Analysis: Apply the Mathematical Principles of Reinforcement (MPR) model to the data (response rates, latencies) to dissect the performance into underlying components: motivation, impulsivity, and motor skill [53].
Research Reagent Solutions
Table 4: Essential Materials for Comparative Strain Studies
| Reagent/Material | Function | Example Strains & Applications |
|---|---|---|
| Inbred Strains | Provide a genetically defined background for mechanistic studies. | C57BL/6J: General purpose, background for transgenics. BALB/c: Immunology, monoclonal antibody production. FVB/N: Transgenic production (large pronuclei) [50]. |
| Outbred Stocks | Model genetic diversity for generalizable or toxicology studies. | CD-1 (ICR): High fecundity, foster mothers, behavioral studies. Swiss Webster [48] [52]. |
| Diversity Outbred (DO) Mice | High-resolution genetic mapping and population-level studies. | J:DO (Jackson Laboratory): High genetic diversity for association studies, mimics human genetic variation [48] [49]. |
| Germ-Free Isolators | Maintain a sterile environment for microbiome and gnotobiotic research. | PVC Isolators: Used for housing germ-free mice derived via sterile C-section [2]. |
| Operant Conditioning Chambers | Assess learning, motivation, and cognition in behavioral phenotyping. | Standard Mouse Chambers: Used for Progressive Ratio scheduling to measure breakpoint and motivation [53]. |
Visual Workflows and Diagrams
Diagram 1: Decision Framework for Selecting Mouse Strains
Diagram 2: Experimental Workflow for Foster Mother Assessment
Machine Learning and Predictive Modeling for Outcome Forecasting
FAQs: Machine Learning for Embryo Selection and Outcome Prediction
Q1: What is the key difference between training a model for embryo implantation prediction versus embryo ranking? Training a model for implantation prediction and using the same model for embryo ranking within a cohort can lead to suboptimal results. While including clinical, cohort-related features (e.g., oocyte age) can improve overall implantation prediction, it can deteriorate the model's ability to correctly rank embryos from the same cohort. For optimal ranking, models should focus exclusively on embryo-intrinsic visual or morphokinetic features [56].
Q2: How can label ambiguity in failed implantations be addressed to improve model performance? A significant challenge is the ambiguous label of embryos that failed to implant, as it's unknown if the failure was due to embryo quality or other factors. A practical solution is to include data from discarded embryos (those excluded for poor visual appearance) in the training set. Although these are trivially poor, their definitive negative labels help reduce overall dataset ambiguity and can enhance both embryo ranking and implantation prediction accuracy [56].
Q3: Which machine learning models have shown the best performance in predicting live birth outcomes after fresh embryo transfer? In a large-scale study analyzing over 11,000 records, Random Forest (RF) demonstrated the best predictive performance for live birth, with an Area Under the Curve (AUC) exceeding 0.8. Other top-performing models included eXtreme Gradient Boosting (XGBoost) and Light Gradient Boosting Machine (LightGBM) [57]. Another study focusing on patients with endometriosis found that the XGBoost model was superior, with an AUC of 0.852 in the test set [58].
Q4: What are the most critical features for predicting live birth in a standard IVF population? Feature importance analysis from high-performing models consistently identifies several key predictors [57]:
- Female Age
- Grades of Transferred Embryos
- Number of Usable Embryos
- Endometrial Thickness
Q5: Can AI assist when only poor-quality embryos are available for transfer? Yes. Research on an AI system (EMBRYOLY) shows that it can significantly aid embryologists in these difficult scenarios. The AI's ranking of poor-quality embryos was correlated with clinical pregnancies and live births. Its adjunct use could potentially reduce the number of cycles to pregnancy by 19% and increase the first-cycle pregnancy rate by 65% in such cases [59].
Q6: What features are most important for predicting blastocyst development? A machine learning framework identified a feature signature for embryos that successfully reach the expanded blastocyst stage. The key features and their cut-offs are summarized below [60]:
| Feature | Description / Cut-off | Association with Blastocyst Development |
|---|---|---|
| t8-tSB | Duration between 8-cell and start of blastulation | Shorter time is favorable |
| t5 | Time to 5-cell stage | Specific timing windows are predictive |
| t8-t7 | Duration between 7-cell and 8-cell stage | Shorter time is favorable |
| t3 | Time to 3-cell stage | Specific timing windows are predictive |
| t8 | Time to 8-cell stage | Specific timing windows are predictive |
| tSC | Time to start of compaction | Earlier start is favorable |
| t4 | Time to 4-cell stage | Specific timing windows are predictive |
| t9-t8 | Duration between 8-cell and 9-cell stage | Shorter time is favorable |
Experimental Protocols for Key Predictive Modeling Tasks
Protocol 1: Developing a Live Birth Prediction Model for Fresh Embryo Transfer
This protocol is based on a large retrospective study that developed a model using 11,728 records with 55 pre-pregnancy features [57].
1. Data Collection and Preprocessing:
- Data Source: Collect de-identified records from patients undergoing fresh embryo transfer, including demographic, clinical, and embryonic data.
- Inclusion/Exclusion Criteria: Apply criteria such as female age (<55 years), use of husband's sperm, and cleavage-stage embryo transfer to refine the cohort.
- Data Cleaning: Handle missing values using a non-parametric imputation method like
missForest, which is efficient for mixed-type data. - Outcome Definition: The primary outcome is a live birth, confirmed by follow-up.
2. Feature Selection and Model Training:
- Feature Selection: Implement a tiered protocol combining data-driven criteria (e.g., p-value < 0.05 or top-20 feature importance) with validation by clinical experts to eliminate biologically irrelevant variables.
- Model Selection: Train and compare multiple machine learning models. The study used [57]:
- Random Forest (RF)
- eXtreme Gradient Boosting (XGBoost)
- Gradient Boosting Machines (GBM)
- Adaptive Boosting (AdaBoost)
- Light Gradient Boosting Machine (LightGBM)
- Artificial Neural Network (ANN)
- Hyperparameter Tuning: Use a grid search approach with 5-fold cross-validation on the training set, optimizing for AUC.
- Model Evaluation: Retrain the best model on the full training set and evaluate its performance on a held-out test set using AUC, accuracy, sensitivity, specificity, and F1 score.
3. Model Interpretation and Deployment:
- Interpretation: Use techniques like partial dependence plots and accumulated local profiles to understand the marginal effect of key features on the predictions.
- Deployment: Develop a web tool to allow clinicians to input patient data and receive a live birth probability, aiding in personalized treatment planning.
Protocol 2: A Machine Learning Framework for Predicting Blastocyst Development
This protocol outlines the steps for a rule-based ML framework to identify embryos with high developmental competence [60].
1. Data Annotation and Cohort Definition:
- Cohort: Collect morphokinetic data from embryos cultured in a time-lapse system (e.g., Geri plus).
- Groups: Divide embryos into two groups: those that reached expanded blastocyst stage on day 5 (BL Group) and those that did not (nBL Group).
- Annotation: Manually annotate morphokinetic parameters (e.g., tPNa, tPNf, t2, t3, t4, t5, t8, tSC) from the time-lapse videos, following standardized guidelines.
2. The EmbryoMLSelection Framework: The framework involves a four-step process to create an interpretable model [60]:
- Step 1: Feature Selection. Use statistical tests (e.g., Mann-Whitney U test) and correlation analysis to filter the initial set of morphokinetic and morphological variables, retaining only the most significant and non-redundant features.
- Step 2: Rules Extraction. Apply a supervised machine learning algorithm (e.g., Decision Tree) to the selected features to generate a set of "if-then" rules that distinguish between the BL and nBL groups.
- Step 3: Rules Selection. Refine the extracted rules by merging redundant ones and selecting those with the highest performance metrics (e.g., F1-score).
- Step 4: Rules Evaluation. Validate the final set of rules on an independent cohort of embryos. Evaluate the model's performance using AUC, accuracy, precision, and recall.
Research Reagent Solutions for Embryo Assessment and ML
The following table details key materials and technologies used in the featured experiments [2] [61] [60].
| Item | Function in Research | Example Use Case |
|---|---|---|
| Time-Lapse System (TLS) | Provides uninterrupted, real-time imaging of embryo development for morphokinetic annotation. | Geri plus (Genea Biomedx); EmbryoScope (Vitrolife) [60] [61]. |
| Culture Media | Supports embryo development in vitro from cleavage to blastocyst stage. | Sequential media (e.g., Quinn's Advantage series) or single-step media (e.g., Sage 1-Step) [61]. |
| Hyaluronidase | Enzyme used to remove cumulus cells from oocytes for Intracytoplasmic Sperm Injection (ICSI). | Synvitro Hyadase (Origio Medicult) [60]. |
| Gonadotropins | Recombinant hormones used for controlled ovarian stimulation to induce follicle growth. | Gonal-F (recombinant FSH) [60]. |
| Trigger Medication | Used to induce final oocyte maturation prior to retrieval. | Human Chorionic Gonadotropin (hCG), e.g., Gonasi HP [60]. |
| Machine Learning Platform | Software environment for developing, training, and validating predictive models. | R (with caret, xgboost, bonsai packages) or Python (with scikit-learn, PyTorch) [57] [61]. |
Visualization of Key Workflows
EmbryoMLSelection Framework
ML Model Development for Live Birth Prediction
Optimizing Foster Mother Selection
Integrating Ultrasound Radiomics with Clinical Parameters for Prediction
Troubleshooting Guides and FAQs
This technical support center provides targeted guidance for researchers integrating ultrasound radiomics with clinical parameters, specifically framed within embryo transfer and foster mother selection studies.
Frequently Asked Questions
Q: What is the primary value of integrating radiomics with clinical features? A: Combining ultrasound radiomics with clinical parameters creates models that significantly outperform approaches using either data type alone. This integration provides a more comprehensive, non-invasive method for predictive analysis, such as assessing Ki-67 status in breast carcinoma or predicting survival outcomes in triple-negative breast cancer (TNBC) [62] [63].
Q: How can researchers ensure the reproducibility of extracted radiomics features? A: Reproducibility is validated through Interclass Correlation Coefficient (ICC) analysis. Have multiple sonographers independently delineate regions of interest (ROIs) on a subset of images and extract features. An ICC value greater than 0.70 indicates good inter-observer consistency and reliable features for downstream analysis [62].
Q: What are the key steps for building a robust radiomics model? A: The core workflow involves: 1) Image acquisition and ROI segmentation, 2) High-throughput feature extraction, 3) Feature selection using algorithms like LASSO or ElasticNet to avoid overfitting, 4) Model training with various classifiers (e.g., SVM, Logistic Regression), and 5) Validation on independent test sets [62] [64].
Q: Which machine learning classifiers perform best for radiomics models? A: Performance varies by dataset. One study comparing six classifiers found Logistic Regression achieved the best performance (AUC 0.786), while XGBoost performed the worst (AUC 0.615). Systematically compare multiple algorithms on your validation set to identify the optimal classifier for your specific data [62].
Q: How can experimental reproducibility be improved in embryo transfer studies? A: Utilizing in vitro fertilization (IVF) for generating donor embryos provides precise control over delivery timing, which enhances experimental reproducibility compared to natural mating where predicting exact birth timing is challenging [2].
Troubleshooting Common Experimental Issues
Table 1: Troubleshooting Common Radiomics and Experimental Issues
| Problem Area | Specific Issue | Potential Cause | Solution |
|---|---|---|---|
| Data Quality | Poor feature reproducibility (low ICC) | Inconsistent ROI segmentation between users | Implement standardized segmentation protocols and training [62] |
| Limited model generalizability | Overfitting to training data; small cohort size | Use multicenter datasets for external validation [64] [63] | |
| Model Performance | Suboptimal predictive accuracy | Using radiomics or clinical features in isolation | Develop integrated nomograms combining Rad-Score and clinical factors [62] [63] |
| Unstable feature selection | High dimensionality and multicollinearity of features | Apply dimensionality reduction (e.g., LASSO, ElasticNet regression) [62] [64] | |
| Experimental Workflow | Low pup survival post C-section | Surgical technique stress | Optimize cesarean method (e.g., FRT-CS technique) to improve fetal survival [2] |
| Inconsistent maternal care | Unsuitable foster mother strain | Select foster strains with proven nursing capabilities (e.g., BALB/c, NSG) [2] |
Experimental Protocols
Detailed Methodology for Radiomics Analysis
This protocol is adapted from established radiomics studies for predictive modeling in medical research [62] [63].
1. Patient Cohort and Image Acquisition
- Cohort Selection: Define clear inclusion/exclusion criteria. Example: Patients with confirmed pathology, single mass-like tumors, ultrasound performed within a specific timeframe before intervention, and available clinical data [62] [63].
- Image Acquisition: Use standardized ultrasound systems and probes. Store images in Digital Imaging and Communications in Medicine (DICOM) format to preserve data integrity [62].
2. Region of Interest (ROI) Segmentation
- Manual Method: A trained sonographer, blinded to histological findings, delineates a 2D ROI covering the entire lesion on the image slice showing the largest tumor cross-section using software like ITK-SNAP [62].
- Deep Learning Method: For higher throughput, use an automated segmentation model (e.g., based on YOLO V3 algorithm). All automatically generated ROIs must be reviewed and manually corrected by an experienced radiologist to ensure accuracy [63].
3. Radiomics Feature Extraction
- Utilize an open-source library like
PyRadiomics(Python) to extract a large set of features. - Standard feature categories include:
- Shape-based features: Describe the 3D size and shape of the ROI.
- First-order statistics: Describe the distribution of voxel intensities within the ROI (e.g., entropy, kurtosis).
- Texture features: Describe the spatial relationships between voxels (e.g., from Gray-Level Co-occurrence Matrix - GLCM, Gray-Level Run-Length Matrix - GLRLM) [62] [63].
4. Feature Selection and Model Building
- Data Preprocessing: Normalize all features using z-score normalization.
- Feature Selection: Employ a two-step process to reduce dimensionality and select the most predictive features:
- Use independent sample t-tests (or similar) to exclude features showing no significant difference between groups.
- Apply a feature selection algorithm like Least Absolute Shrinkage and Selection Operator (LASSO) or ElasticNet regression to further select non-redundant, informative features [62] [64].
- Model Training: Train multiple machine learning classifiers (e.g., Support Vector Machine (SVM), Logistic Regression (LR), Random Forest (RF)) using the selected features on a training cohort. Optimize hyperparameters via cross-validation.
- Model Validation: Evaluate the final model's performance on a held-out test set and/or external validation sets from different institutions. Report area under the curve (AUC), sensitivity, and specificity [62] [64].
Protocol for Optimizing Foster Mother Selection
This protocol outlines the evaluation of different mouse strains as suitable foster mothers for embryo transfer research, based on contemporary studies [2].
1. Subject and Housing Preparation
- Strains: Select GF female foster mothers from multiple inbred (e.g., C57BL/6J, BALB/c, NSG) and outbred (e.g., KM) strains. Use females of consistent age (e.g., four months) that have previously given birth once.
- Housing: House all mice in sterile PVC isolators. Autoclave all life supplements (food, water, bedding) and surgical instruments at 121°C for 20 minutes prior to use. Pre-heat the isolator with a heating pad to 40-45°C before the C-section to prevent pup hypothermia [2].
2. Cesarean Section and Pup Transfer
- Donor Preparation: Use pregnant SPF donor females. Euthanize via cervical dislocation immediately before the C-section.
- Surgical Technique: Perform the Female Reproductive Tract Preserved C-section (FRT-CS) technique under aseptic conditions. This method, which clamps only the cervix base, has been shown to significantly improve fetal survival rates compared to the traditional method [2].
- Pup Processing: Transfer the uterine sac to a disinfectant (e.g., Clidox-S), then quickly move it into the sterile isolator. Incise the amniotic membrane, cut the umbilical cord, and gently wipe the pup with a sterile swab until spontaneous breathing is noted. The entire procedure must be completed within 5 minutes to ensure pup viability and sterility [2].
3. Evaluation of Maternal Care
- Fostering: Introduce the recovered pups to the pre-prepared GF foster mothers.
- Data Collection: Systematically record key performance metrics for each foster strain, including:
- Number of pups successfully accepted.
- Pup survival rate at weaning.
- General nursing behavior and nest building.
- Analysis: Compare weaning success rates across the different strains to identify the most suitable foster mothers for maintaining GF colonies [2].
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function / Application | Example / Specification |
|---|---|---|
| PyRadiomics Library | Open-source Python package for standardized extraction of radiomics features from medical images. | Version 3.0.1; Extracts 100+ features including shape, first-order, and texture features [63]. |
| ITK-SNAP Software | Interactive software used for manual segmentation of structures (ROIs) in medical images. | Used for precise delineation of tumor boundaries on ultrasound images [62]. |
| LOGIC E9 / Siemens Acuson S2000 | Clinical ultrasound systems for image acquisition. | Equipped with linear array probes (e.g., 6-15L); produces DICOM images for analysis [62]. |
| Sterile PVC Isolator | Controlled environment for housing germ-free (GF) mice and performing aseptic procedures. | Maintains a sterile barrier; requires disinfection with chlorine dioxide (Clidox-S) [2]. |
| Clidox-S | Chlorine dioxide disinfectant used for sterilizing surfaces and materials entering the sterile isolator. | Used in a 1:3:1 dilution, activated for 15 minutes before use [2]. |
| FVB/N Strain | Inbred mouse strain ideal for egg production for transgenic studies due to large, prominent pronuclei. | Facilitates microinjection; high survival rate of injected embryos [1]. |
Workflow Diagrams
Radiomics-Clinical Integration Workflow
Foster Mother Optimization Pathway
Troubleshooting Guide: Foster Mother Selection and Post-Transfer Procedures
Frequently Asked Questions (FAQs)
Q1: Which foster mother strains demonstrate the highest success rates for weaning germ-free pups? Strain selection is critical for post-transfer success. Systematic evaluation of maternal care in germ-free (GF) conditions reveals significant strain-specific differences [2].
- Optimal Strains: BALB/c and NSG (NOD/SCID Il2rg–/–) GF foster mothers exhibit superior nursing capabilities and weaning success [2].
- Strain to Use with Caution: C57BL/6J GF foster mothers show the lowest weaning rates. This is a critical finding, as it contrasts with data on the maternal behavior of C57BL/6J mice under specific pathogen-free (SPF) conditions, highlighting the importance of the germ-free environment itself [2].
- Additional Strain: The outbred KM (Kunming) strain was also evaluated, but BALB/c and NSG were superior [2].
Q2: What surgical technique improves fetal survival during cesarean derivation? The surgical method for obtaining pups directly impacts viability. The female reproductive tract preserved C-section (FRT-CS) technique has been shown to significantly improve fetal survival rates while maintaining sterility compared to traditional C-section (T-CS) [2]. In FRT-CS, clamps are applied selectively at the cervix base, preserving the integrity of the entire reproductive tract, including the ovary, uterine horn, and uterine junction [2].
Q3: Does the origin of donor embryos (natural mating vs. IVF) affect experimental outcomes? Yes, the embryo source can impact the reproducibility of your timeline. Using in vitro fertilization (IVF) for obtaining donor embryos allows for precise control over the donor delivery date, which enhances experimental reproducibility and helps in planning the transfer to foster mothers [2]. This precision is more difficult to achieve with natural mating, where predicting the exact delivery time is challenging [2].
Q4: What are the key considerations for long-term health assessment of ART-conceived offspring? While most offspring conceived via Assisted Reproductive Technologies (ART) are healthy, long-term studies suggest a slightly increased risk of certain conditions, necessitating specific monitoring protocols [65] [66].
- Birth Defects: Epidemiological data confirm a small increase in birth defects with ART (3–4% vs. 2–3% in natural conception) [66].
- Cardiometabolic Health: Some studies suggest an increased risk of altered blood pressure, generalized vascular functional disorders, and metabolic disorders in children born after ART [65] [66].
- Other Considerations: Research has also indicated potential associations with a higher prevalence of malignancies and asthma, though the direct contribution of ART procedures versus underlying parental factors requires further investigation [66].
- Confounding Factors: It is essential to consider that parents requiring ART may differ from the fertile population in aspects such as age and the underlying causes of infertility, which can also influence offspring health [66].
Q5: How do in vitro culture conditions potentially affect the long-term health of embryos? The preimplantation period is highly sensitive to environmental conditions. Suboptimal in vitro culture conditions are a subject of ongoing research concerning their potential long-term effects [66] [67].
- Epigenetic Alterations: A key concern is that ART procedures, including embryo culture, may influence epigenetic reprogramming—a crucial process during early embryogenesis that can affect gene expression and disease susceptibility later in life [66] [67].
- Stress Factors: Conditions such as culture media composition, oxygen tension, temperature, and pH can impose stress on the developing embryo [67]. While advances in sequential and simplex optimization media have improved embryo viability, the artificial environment does not fully replicate the dynamic in vivo conditions [67].
Experimental Protocols for Validation
Protocol 1: Evaluating Foster Mother Maternal Capability
Objective: To systematically assess and identify the most suitable mouse strain for use as a germ-free foster mother in embryo transfer research.
Methodology:
- Strain Selection: Utilize three inbred strains (C57BL/6J, BALB/c, NSG) and one outbred strain (KM) as GF foster mothers [2].
- Standardization: Ensure all foster mothers are of the same age (e.g., four months) and have equivalent prior birthing experience (e.g., one previous litter) to control for these variables [2].
- Transfer: Introduce pups obtained via sterile C-section to the foster mothers within a sterile isolator.
- Data Collection: Record key performance metrics, including:
- Pup survival rate at 24 hours and 7 days post-transfer.
- Successful weaning rate (e.g., at 21 days).
- Qualitative observations of nursing behavior and pup retrieval.
Protocol 2: Sterile Cesarean Section for Germ-Free Pup Derivation
Objective: To obtain germ-free pups from a donor mother with high survival rates.
Methodology:
- Donor Preparation: Use either naturally mated or IVF-derived timed-pregnant donor females [2].
- Euthanasia: Euthanize the donor female via cervical dislocation at the appropriate gestational stage [2].
- Surgical Technique: Perform the Female Reproductive Tract Preserved C-section (FRT-CS) under aseptic conditions [2].
- Disinfection and Transfer:
- Excise the uterine sac and disinfect it with a chlorine dioxide solution (e.g., Clidox-S) [2].
- Rapidly transfer the uterus into a sterile isolator (the entire procedure should be completed within 5 minutes to ensure viability) [2].
- Inside the isolator, incise the amniotic membrane, wipe the pup with a sterile swab, and cut the umbilical cord [2].
- Foster Introduction: Immediately present the pups to a pre-conditioned GF foster mother.
Data Presentation
Table 1: Comparative Weaning Success of Germ-Free Foster Mother Strains
| Strain | Type | Weaning Success | Key Maternal Characteristics |
|---|---|---|---|
| BALB/c | Inbred | Superior | Exhibits superior nursing and weaning success [2]. |
| NSG | Inbred | Superior | Exhibits superior nursing and weaning success [2]. |
| KM | Outbred | Intermediate | Evaluated for maternal care capabilities [2]. |
| C57BL/6J | Inbred | Lowest | Lowest weaning rate in GF conditions [2]. |
Table 2: Long-Term Health Considerations in ART-Conceived Offspring
| Health Domain | Observed Risk/Association | Key Confounding Factors |
|---|---|---|
| Birth Defects | Slight increase (3-4% vs. 2-3% in natural conception) [66]. | Underlying parental infertility, multiple pregnancies [66]. |
| Cardiometabolic | Altered blood pressure, vascular function, metabolic disorders [65] [66]. | Parental health, genetic background. |
| Cancer | Some studies suggest a higher prevalence [66]. | More research is needed to establish a direct causal link [66]. |
| Epigenetics | Potential for alterations due to ART procedures and culture conditions [66] [67]. | Inherent sensitivity of the preimplantation embryo [67]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function/Application |
|---|---|
| Sequential Culture Media | Supports embryo development through different metabolic stages (e.g., pre- and post-genomic activation) [67]. |
| Chlorine Dioxide (Clidox-S) | A disinfectant used for sterilizing the exterior of the uterine sac during C-section derivation [2]. |
| Polyvinyl Chloride (PVC) Isolator | A sterile housing unit for maintaining germ-free mice and performing procedures [2]. |
| Hormonal Support (Progesterone/Estrogen) | Used in frozen embryo transfer cycles to prepare and thicken the uterine lining for implantation [68]. |
| Amino Acid Supplementation | Added to culture media to improve embryo growth and development to the blastocyst stage [67]. |
| Preimplantation Genetic Testing (PGT) | A suite of technologies (e.g., PGT-A, PGT-WGS) to screen embryos for chromosomal abnormalities and severe genetic diseases [69]. |
Experimental Workflow: From Embryo Transfer to Long-Term Validation
Conclusion
Optimizing foster mother selection represents a critical multidimensional approach to enhancing embryo transfer success in biomedical research. The integration of evidence-based strain selection, refined surgical techniques, precise synchronization protocols, and advanced predictive modeling significantly improves reproductive outcomes and experimental reproducibility. Future directions should focus on developing standardized, validated selection criteria across model organisms, incorporating artificial intelligence and radiomics for outcome prediction, and establishing robust databases of strain-specific performance metrics. These advancements will accelerate the production of genetically engineered animal models, particularly for microbiome and therapeutic research, while improving animal welfare and resource efficiency in scientific discovery. The continued refinement of foster mother selection protocols promises to substantially impact drug development pipelines and translational research capabilities.
References
- 1. 6.2 EMBRYO MANIPULATION: GENETIC CONSIDERATIONS [https://www.informatics.jax.org/silver/chapters/6-2.shtml]
- 2. Optimized cesarean techniques, IVF use, and foster strain ... [https://www.nature.com/articles/s41598-025-05411-4]
- 3. What makes a good mother? Implication of inter-, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0166432814005336]
- 4. Advanced strategies for single embryo selection in assisted ... [https://ecerm.org/journal/view.php?number=1349]
- 5. The biology and methodology of assisted reproduction in deer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3243791/]
- 6. The study on the clinical efficacy of endometrial receptivity ... [https://www.nature.com/articles/s41598-025-91745-y]
- 7. Advances in endometrial receptivity and embryo ... [https://www.sciencedirect.com/science/article/pii/S2950248925000355]
- 8. Embryo-maternal cross-talk: key players in successful ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548195/]
- 9. Causes of embryo implantation failure: A systematic review ... [https://pubmed.ncbi.nlm.nih.gov/40028443/]
- 10. Key factors influencing clinical pregnancy rates in frozen ... [https://www.sciencedirect.com/science/article/pii/S1472648325000677]
- 11. Critical factors influencing live birth rates in fresh embryo ... [https://www.nature.com/articles/s41598-025-88210-1]
- 12. Optimized cesarean techniques, IVF use, and foster strain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297627/]
- 13. Performance of ten inbred mouse strains following assisted ... [https://www.sciencedirect.com/science/article/abs/pii/S0093691X0500405X]
- 14. Differences in Mouse Maternal Care Behavior - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3084270/]
- 15. Maternal behavior of primiparous females in inbred strains ... [https://www.sciencedirect.com/science/article/abs/pii/S0031938406002691]
- 16. Variations in Maternal Behavior in C57BL/6J Mice [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2011.00042/full]
- 17. Mouse Background Genetics in Biomedical Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC8627118/]
- 18. The importance of background strains in GA mice [https://nc3rs.org.uk/3rs-resources/importance-background-strains-ga-mice]
- 19. Derivation of embryonic stem cells from wild ... [https://www.nature.com/articles/s41598-023-38341-0]
- 20. Advanced maternal age was associated with an annual ... [https://www.sciencedirect.com/science/article/pii/S0015028225004388]
- 21. Effect of maternal age, embryo number and quality on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634337/]
- 22. A critical assessment of the “sterile womb” and “in utero ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-017-0268-4]
- 23. A microbial symphony: a literature review of the factors that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11977369/]
- 24. Challenging the Hypothesis of in Utero Microbiota ... [https://www.mdpi.com/2306-7381/10/5/331]
- 25. Approaching the sterile womb theory in dogs and cats [https://www.sciencedirect.com/science/article/abs/pii/S0093691X24004643]
- 26. Assisted reproduction with advancing paternal and ... [https://www.asrm.org/practice-guidance/ethics-opinions/assisted-reproduction-with-advancing-paternal-and-maternal-age-an-ethics-committee-opinion-2025/]
- 27. Natural cycle versus hormone replacement therapy as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193059/]
- 28. Highlights from ESHRE 2025: Advances in Endometrial ... [https://www.emjreviews.com/reproductive-health/congress-review/highlights-from-eshre-2025-advances-in-endometrial-preparation-strategies-for-frozen-embryo-transfer-j150125/]
- 29. Cycle management in frozen embryo transfer: the best of ... [https://www.sciencedirect.com/science/article/pii/S1472648324009787]
- 30. Endometrial preparation methods prior to frozen embryo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11951573/]
- 31. Impact of different endometrial preparation protocols on ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-025-07535-x]
- 32. The developmental potential of mouse embryos conceived ... [https://www.sciencedirect.com/science/article/pii/S0015028216564152]
- 33. Implantation Failure: Why IVF Sometimes Doesn't Work | Blog [https://www.advancedfertility.com/blog/ivf-implantation-failure]
- 34. Causes of embryo implantation failure: A systematic review ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1429193/full]
- 35. Management strategies following implantation failure of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11000815/]
- 36. Overcoming IVF Implantation Failure: Failed IVF Cycles ... [https://rmanetwork.com/blog/ivf-implantation-failure-failed-ivf-cycles-explained/]
- 37. Patient selection criteria for blastocyst transfers in extended ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3528882/]
- 38. What to do when good-quality embryos repeatedly fail ... [https://www.sciencedirect.com/science/article/abs/pii/S1521693418301627]
- 39. What to do when your embryos won't “stick”? - Care Fertility [https://carefertility.com.au/blog/items/what-to-do-when-your-embryos-won-t-stick]
- 40. Gestational age at birth varies by surgical technique in ... [https://www.sciencedirect.com/science/article/pii/S0002937825000948]
- 41. Advances in Fetal Surgery: A Narrative Review of Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300766/]
- 42. Optimizing embryo transfer timing based on serum ... [https://www.sciencedirect.com/science/article/pii/S092966462500395X]
- 43. Effects of Various Transfer Strategies of Frozen-Thawed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12039847/]
- 44. Comparison of Different Progesterone Protocols for Luteal ... [https://pubmed.ncbi.nlm.nih.gov/41153770/]
- 45. Comparison of Luteal Support Protocols in Frozen IVF/ICSI ... [https://pubmed.ncbi.nlm.nih.gov/40313195/]
- 46. Predictive Value of Serum Progesterone Levels on The ... [https://pubmed.ncbi.nlm.nih.gov/40200780/]
- 47. Progesterone level in assisted reproductive technology [https://www.nature.com/articles/s41598-024-81539-z]
- 48. Comparing phenotypic variation between inbred and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6518396/]
- 49. The unexpected advantages of outbred mice in research [https://www.jax.org/news-and-insights/2018/december/the-advantages-of-outbred-mice-in-research]
- 50. Inbred Strain - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/inbred-strain]
- 51. Outbred Mouse Strain - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/outbred-mouse-strain]
- 52. Commercially Available Outbred Mice for Genome-Wide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2932682/]
- 53. Assessment of the inbred C57BL/6 and outbred CD1 ... [https://www.sciencedirect.com/science/article/abs/pii/S0031938424000301]
- 54. Inbred Versus Outbred Strains | Center for Mouse Genome ... [https://health.uconn.edu/mouse-genome-modification/resources/inbred-versus-outbred-strains/]
- 55. Inbred lab mice are not isogenic: genetic variation within ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7852876/]
- 56. Solving the “right” problems for effective machine learning ... [https://www.medrxiv.org/content/10.1101/2021.10.07.21264503v1]
- 57. Predictive models for live birth outcomes following fresh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462326/]
- 58. Development and validation of a machine learning-based ... [https://pubmed.ncbi.nlm.nih.gov/40986161/]
- 59. can artificial intelligence (AI) help embryologists when only ... [https://www.sciencedirect.com/science/article/pii/S1472648325001609]
- 60. A novel machine-learning framework based on early embryo ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-024-01376-6]
- 61. Development of a dynamic machine learning algorithm to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9250114/]
- 62. Integration of ultrasound radiomics features and clinical factors [https://pmc.ncbi.nlm.nih.gov/articles/PMC9581085/]
- 63. Integrating ultrasound radiomics and clinicopathological ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13635-w]
- 64. An Interpretable Radiomics Model Integrating Ultrasound ... [https://www.sciencedirect.com/science/article/pii/S0301562925003126]
- 65. Long-term outcomes for children conceived by assisted ... [https://www.sciencedirect.com/science/article/pii/S0015028223003072]
- 66. Long-Term Effects of ART on the Health of the Offspring [https://www.mdpi.com/1422-0067/24/17/13564]
- 67. Association Between Human Embryo Culture Conditions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298697/]
- 68. FET-IVF: Frozen Embryo Transfer Tips, Timelines and ... [https://www.pfcla.com/blog/frozen-embryo-transfer-tips]
- 69. Unlocking the Future of IVF: Navigating the Complex World ... [https://www.asrm.org/news-and-events/asrm-news/tech-talk-blogs/27-june-2025-unlocking-the-future-of-ivf-navigating-the-complex-world-of-ivf-genomics/]