Optimizing Sucrose in Embryo Warming: From Foundational Science to Clinical Protocols
This article synthesizes the latest research on the critical role of sucrose concentration in embryo warming solutions for assisted reproductive technology (ART).
Optimizing Sucrose in Embryo Warming: From Foundational Science to Clinical Protocols
Abstract
This article synthesizes the latest research on the critical role of sucrose concentration in embryo warming solutions for assisted reproductive technology (ART). It explores the foundational science of sucrose as a non-permeating cryoprotectant, examines the emergence of simplified one-step warming methodologies, and provides evidence-based guidance for protocol optimization across different embryo types and patient factors. Drawing from recent clinical studies and preclinical models, the content validates the safety and efficacy of optimized protocols, highlighting their significant advantages in laboratory workflow efficiency without compromising embryology or clinical outcomes such as survival, implantation, and live birth rates. This resource is tailored for researchers, scientists, and drug development professionals seeking to refine cryopreservation techniques.
The Science of Sucrose: Understanding Its Role as a Cryoprotectant in Vitrification
Sucrose, a non-penetrating disaccharide, is a critical component in cryopreservation solutions for embryos and other cellular systems. Unlike penetrating cryoprotectants like dimethyl sulfoxide (DMSO) or ethylene glycol (EG) that enter cells, sucrose remains in the extracellular space and exerts its protective effects through well-defined physicochemical mechanisms [1]. Its primary functions are to counteract osmotic shock during the addition and removal of other cryoprotectants and to inhibit damaging ice crystal formation during the freezing and warming processes [2] [3]. Understanding these mechanisms is essential for optimizing cryopreservation protocols in reproductive medicine, regenerative medicine, and biopharmaceutical development.
Detailed Mechanisms of Action
Prevention of Osmotic Shock
During cryopreservation, cells are exposed to highly concentrated solutions of penetrating cryoprotectants. While these agents are necessary for intracellular protection, their introduction and subsequent removal create substantial osmotic gradients across the cell membrane. Sucrose mitigates the associated stress through its action as a non-penetrating osmotic balancer.
- Mechanism During Cryoprotectant Addition: When a cell is placed in a solution containing both a penetrating cryoprotectant (e.g., EG) and sucrose, a two-stage osmotic response occurs. First, the high overall osmolality of the external solution causes water to rapidly flow out of the cell, leading to controlled shrinkage. This dehydration is beneficial as it reduces the amount of intracellular water available to form ice. Sucrose, because it cannot cross the membrane, sustains this osmotic drive, ensuring sufficient dehydration occurs before cooling [3] [1].
- Mechanism During Cryoprotectant Removal (Warming): This is a particularly critical phase. After warming, the cell contains high concentrations of the penetrating cryoprotectant. If placed directly into an isotonic solution, the large osmotic difference would cause water to rush into the cell much faster than the cryoprotectant can diffuse out. This leads to excessive swelling, which can rupture the plasma membrane—a phenomenon known as osmotic shock or "osmotic swelling" [3]. The inclusion of sucrose in the warming solution provides a counterbalancing osmotic pressure. It draws water out of the cell gradually, allowing the penetrating cryoprotectant to diffuse out in a controlled manner without the cell swelling beyond its safe volume limits. The stepwise dilution through solutions with decreasing sucrose concentrations (e.g., from 1.0 M to 0.5 M, then 0.25 M, and finally to zero) allows for a gentle return to isotonic conditions, minimizing osmotic stress and maximizing cell survival [4] [3] [5].
The following diagram illustrates the protective role of sucrose during the warming and dilution phase of cryopreservation.
Inhibition of Ice Crystallization
The formation of ice crystals, both inside and outside the cell, is a primary cause of cryoinjury. Sucrose contributes to the prevention of ice formation through several interrelated mechanisms:
- Colligative Action and Vitrification: Sucrose dissolves in the aqueous solution and, through colligative effects, reduces the freezing point of water. More importantly, it increases the overall solute concentration of the solution. During cooling, this leads to a greater degree of "supercooling" and dramatically increases the solution's viscosity. At a critical cooling rate, this viscous solution solidifies into an amorphous, glassy state rather than forming an organized, crystalline ice lattice. This process is known as vitrification, and it is essential for preventing the mechanical damage caused by ice crystals [2] [6] [1]. While penetrating cryoprotectants are the primary drivers of intracellular vitrification, sucrose significantly contributes to extracellular vitrification.
- Reduction of "Solution Effects" Injury: As a solution freezes, pure water forms ice crystals, which excludes solutes. The remaining unfrozen fraction becomes increasingly concentrated with salts and other solutes. Cells exposed to this hypertonic environment can suffer "solution effects" injury, which includes protein denaturation and membrane damage [2] [1]. By being a major component of the solute pool, sucrose dilutes the concentration of these more harmful electrolytes (e.g., sodium chloride) in the unfrozen fraction, thereby reducing the severity of this type of chemical damage.
- Stabilization of Biomembranes and Proteins: There is evidence that sugars, including sucrose, can directly stabilize phospholipid bilayers and proteins in a dehydrated state. By forming hydrogen bonds with polar head groups of membrane lipids and the surface of proteins, sucrose can effectively "replace" water molecules, helping to maintain structural integrity during the dehydration that accompanies freezing [1]. This mechanism is analogous to the one used by many anhydrobiotic (desiccation-tolerant) organisms.
Optimizing Sucrose Concentration: Key Experimental Data
Optimizing the concentration of sucrose in warming solutions is critical for balancing its protective benefits against potential osmotic stress from over-shooting. The following table summarizes quantitative findings from key studies on sucrose concentration optimization.
Table 1: Experimental Data on Sucrose Concentration Optimization in Warming Solutions
| Species/Cell Type | Sucrose Concentrations Tested | Key Findings | Citation |
|---|---|---|---|
| Rat Zygotes (IVF) | 0 M, 0.05 M, 0.1 M, 0.2 M, 0.3 M | 0.1 M sucrose yielded the highest rates of survival and development to two-cell embryos. Lower (0.05 M) and higher (0.2 M, 0.3 M) concentrations resulted in reduced success. | [5] |
| Human Blastocysts | Stepwise dilution: 1.0 M → 0.5 M → 0.25 M → 0 M | This standard multi-step protocol, which includes sucrose, resulted in high survival rates and significantly improved implantation rates (up to 59.7%) compared to non-treated controls. | [4] |
| General Principle | Varies by protocol | Sucrose is included in cryopreservation solutions to promote cell shrinkage before freezing and to prevent osmotic swelling during dilution, counteracting the inflow of water. | [3] |
Frequently Asked Questions (FAQs)
Q1: Why is sucrose used instead of a penetrating cryoprotectant like DMSO for preventing osmotic shock? Sucrose is effective precisely because it is non-penetrating. Its inability to cross the cell membrane allows it to create a stable, persistent osmotic gradient that reliably draws water out of the cell during CPA removal. If a penetrating agent were used for this purpose, it would eventually enter the cell and negate the osmotic differential, failing to prevent the damaging influx of water [1] [7].
Q2: Can I use a simple isotonic solution without sucrose to warm and dilute my cryopreserved embryos? This is not recommended. Directly placing a cell laden with penetrating CPAs into an isotonic solution would cause a rapid and massive influx of water, leading to lethal osmotic swelling and cell membrane rupture. The use of a sucrose-containing hypertonic solution is a mandatory step to control this process and ensure high survival rates [3] [5].
Q3: What are the consequences of using a sucrose concentration that is too high or too low? Using a concentration that is too low provides insufficient osmotic protection, leading to osmotic swelling and reduced survival during warming. Conversely, a concentration that is too high can cause excessive cellular dehydration and shrinkage, which can be equally damaging due to "osmotic shrinkage" injury and concentration of intracellular solutes [3] [5]. The optimal concentration, as shown in Table 1, must be determined empirically for specific cell types.
Q4: Is sucrose the only non-penetrating cryoprotectant available? No, other non-penetrating cryoprotectants exist, including polymers like polyvinylpyrrolidone (PVP), hydroxyethyl starch (HES), and Ficoll [2] [1]. These larger molecules also act extracellularly and are sometimes used in combination with sugars. However, sucrose remains a popular choice due to its well-characterized effects, low toxicity, and historical success in clinical and research applications.
Troubleshooting Common Sucrose-Related Issues
Problem: Low survival rates after warming.
- Potential Cause: Incorrect osmolarity of the sucrose warming solutions.
- Solution: Calibrate and verify the osmolarity of all sucrose solutions using an osmometer before use. Ensure accurate molarity during preparation [5].
Problem: Embryos appear shrunken and do not re-expand properly after warming.
- Potential Cause: Over-exposure to the sucrose solution or the use of a sucrose concentration that is too high.
- Solution: Optimize and strictly adhere to the recommended exposure times for each dilution step. Consider validating a slightly lower sucrose concentration for your specific cell type [3] [5].
Problem: Crystalline ice formation observed during the warming process.
- Potential Cause: Inadequate cooling or warming rates, or an insufficient overall concentration of cryoprotectants (including sucrose) to promote vitrification.
- Solution: Ensure ultra-rapid warming rates are achieved. Review the complete CPA cocktail to ensure the total solute concentration is sufficient for vitrification. Sucrose contributes to this total solute load [2] [6].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Sucrose in Cryopreservation
| Reagent / Material | Function / Explanation |
|---|---|
| Sucrose (High Purity) | The primary non-penetrating cryoprotectant under investigation. Must be of high purity (e.g., ACS grade) to avoid introducing contaminants that could affect embryos or ice nucleation. |
| Base Medium (e.g., PBS, mHTF) | The isotonic salt solution used to prepare the sucrose solutions. It provides essential ions and a buffered pH. |
| Penetrating CPAs (DMSO, EG, PG) | Used in combination with sucrose in vitrification solutions. Their toxicity and permeation kinetics are key interaction points for sucrose's osmotic action. |
| Serum Substitute Supplement (SSS) | Often added (e.g., at 20%) to cryopreservation solutions to provide macromolecules that can stabilize cell membranes and reduce mechanical stress. |
| Osmometer | A critical instrument for verifying the precise osmolarity of all prepared sucrose and cryoprotectant solutions, ensuring experimental consistency. |
| Cryodevices (e.g., Cryotop) | Ultra-thin devices that minimize the volume of the vitrification solution, enabling the ultra-fast cooling and warming rates necessary for successful vitrification. |
Experimental Protocol: Optimizing Sucrose Concentration for a New Cell Type
The following workflow outlines a systematic approach to determine the optimal sucrose concentration in a warming solution for a cell type not previously characterized.
Detailed Protocol Steps:
- Solution Preparation: Prepare a series of warming solutions with sucrose concentrations spanning a logical range (e.g., 0.05 M, 0.1 M, 0.2 M, 0.3 M) in your base medium (e.g., modified HTF-HEPES) supplemented with 20% Serum Substitute Supplement (SSS) [4] [5]. Verify the osmolarity of each.
- Vitrification: Vitrify a large, synchronized batch of the target cells (e.g., zygotes) using a standardized and consistent protocol. Randomly assign the vitrified samples to the different experimental warming groups to eliminate bias.
- Warming and Dilution: Warm the samples rapidly. Immediately after warming, transfer them into the respective test sucrose solutions. Subsequently, perform a stepwise dilution through decreasing concentrations of sucrose (e.g., if warmed in 1.0 M, then move to the test concentration, then to 0.5 M, 0.25 M, and finally to base medium) [4].
- Assessment - Immediate Survival: Approximately 2 hours post-warming, assess immediate survival using morphological criteria. A surviving cell will typically have an intact zona pellucida, a non-lysed cytoplasm, and no signs of excessive darkening or degeneration [5].
- Assessment - Functional Capacity: For a more rigorous assessment, culture the surviving samples and record developmental rates (e.g., progression to two-cell stage, blastocyst formation rate) [5]. Alternatively, use functional assays such as mitochondrial membrane potential analysis or cell viability stains.
- Data Analysis and Optimization: Compare survival and development rates across the different sucrose concentration groups. The concentration yielding the highest rates for both immediate and functional outcomes is the optimal one for that specific cell type under your protocol conditions.
Fundamental Concepts: FAQs on Cryoprotectant Mechanisms
FAQ 1: What is the primary functional difference between permeating and non-permeating cryoprotectants?
Permeating cryoprotectants are low molecular weight compounds (typically < 100 g/mol) that can cross the cell membrane, while non-permeating cryoprotectants are larger molecules that remain in the extracellular space [2] [8]. This difference dictates their protective mechanisms: permeating agents protect against intracellular ice formation by depressing the freezing point and promoting vitrification inside the cell, whereas non-permeating agents like sucrose exert their effects extracellularly by controlling osmotic balance and increasing solution viscosity [9] [2].
FAQ 2: How does sucrose specifically protect cells during cryopreservation and warming?
Sucrose, a non-permeating disaccharide, protects cells through multiple synergistic mechanisms [8]:
- Osmotic Control: It creates a hypertonic extracellular environment that promotes controlled cellular dehydration before freezing, reducing the chance of lethal intracellular ice formation [2].
- Membrane Stabilization: It helps maintain cell membrane integrity during dehydration by lowering membrane lipid phase transition temperatures [8].
- Vitrification Enhancement: It increases the viscosity of the carrier solution, facilitating the transition to a glass-like state during cooling [9] [10].
- Ice Crystal Inhibition: Computational studies show sucrose forms strong hydrogen bonds with water molecules, disrupting the specific alignment needed for crystalline ice formation [10].
FAQ 3: Why are combinations of permeating and non-permeating cryoprotectants often used?
Mixtures of cryoprotectants confer greater protection to cell membranes with reduced toxicity compared to single agents [9] [8]. Non-permeating cryoprotectants like sucrose allow for a reduction in the required concentration of potentially toxic permeating agents (e.g., DMSO, ethylene glycol) while maintaining effective vitrification [2]. This synergistic combination protects against both intracellular and extracellular ice formation while minimizing osmotic shock and chemical toxicity [9].
Troubleshooting Sucrose-Based Protocols
Common Experimental Challenges & Solutions
Issue: Low Post-Thaw Cell Survival Rates
- Potential Cause: Excessive osmotic shock during CPA addition or removal.
- Solution: Implement a stepwise addition and removal of cryoprotectants. For warming, use lower sucrose concentrations (e.g., 0.25 M) to reduce osmotic stress and enable faster rehydration [11].
Issue: Intracellular Ice Formation
- Potential Cause: Inadequate dehydration before plunging into liquid nitrogen.
- Solution: Optimize the equilibration time in the sucrose-containing solution. Research on porcine oocytes showed that equilibration in a solution containing a lower concentration of permeating CPAs (4%) for 5-15 minutes before vitrification in a high concentration (35%) resulted in better survival than shorter equilibration with higher CPA concentrations [12].
Issue: Signs of CPA Toxicity
- Potential Cause: Excessive concentration or exposure time to permeating CPAs.
- Solution: Reduce the concentration of toxic permeating agents by leveraging the synergistic effect of sucrose. Ensure all procedures are performed at lower temperatures (e.g., on a cold plate) to mitigate toxicity, as CPA toxicity is temperature- and time-dependent [13] [8].
Optimizing Sucrose Concentration: Experimental Data
The following table summarizes key quantitative findings on sucrose concentration effects from recent research:
Table 1: Impact of Sucrose Concentration on Cryopreservation Outcomes
| Sucrose Concentration | Experimental Context | Key Outcome | Reference |
|---|---|---|---|
| 1 mmol (osmotically inactive) | Chicken sperm cryopreservation | Significantly increased motility, membrane integrity, acrosome integrity, mitochondrial function, and fertility (91% vs 86% control) of frozen-thawed sperm [14]. | |
| 0.25 M | Ultra-fast warming of human blastocysts | Faster re-expansion, higher hatching rates, reduced blebbing (5.1% vs. 10.9%), and equivalent survival/implantation rates compared to higher sucrose concentrations [11]. | |
| 0.3 M | Vitrification of porcine oocytes | Equally effective as 0.3 M trehalose in facilitating oocyte survival and subsequent embryo development after vitrification and warming [12]. | |
| 0.4 M - 1.0 M | Various warming protocols | Higher sucrose concentrations (e.g., 1 M) are associated with higher solution density, causing blastocysts to float, potentially complicating handling and standardizing protocol timing [11]. |
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Sucrose in Cryopreservation
| Reagent / Material | Function / Role in Research |
|---|---|
| Permeating CPAs (EG, DMSO, PG) | Used in combination with sucrose to create vitrification solutions. Their toxicity and permeability are key variables when studying sucrose's protective synergy [12] [13]. |
| Ultra RapidWarm Blast (0.25 M Sucrose) | A commercial, low-sucrose single warming medium validated for human blastocysts; a key tool for studying the benefits of reduced osmotic stress [11]. |
| Hyaluonran-Enriched Transfer Medium | Used in post-warming culture to assess embryo viability and implantation potential. It may provide additional protection against cryodamage [11]. |
| Density Functional Theory (DFT) Models | Computational method to model hydrogen bonding between sucrose and water, predicting cryoprotective efficiency by analyzing electron density and solvation shell stability [10]. |
| Mouse Embryo Assay (MEA) | A quality control bioassay used to test the toxicity and efficacy of cryopreservation solutions, ensuring batch-to-batch consistency [11]. |
Experimental Protocol: Optimizing Sucrose Concentration for Embryo Warming
Objective: To systematically evaluate the effect of reduced sucrose concentration in warming media on the survival and developmental competence of vitrified blastocysts.
Background: Conventional warming protocols often use sucrose concentrations of 0.5 M to 1.0 M. Emerging evidence suggests that lower sucrose concentrations (e.g., 0.25 M) reduce osmotic shock, leading to faster re-expansion and improved outcomes [11].
Materials:
- Vitrified blastocysts (e.g., murine or human model)
- Experimental warming media: Test groups with sucrose concentrations (e.g., 0.25 M, 0.5 M, 1.0 M)
- Base culture medium
- Sterile 35-mm culture dishes
- Water bath or heated stage at 37°C
- Timer
- Inverted microscope with imaging capabilities
Methodology:
- Preparation: Pre-warm all experimental warming media and culture media to 37°C. Label dishes for each test group.
- Warming Process:
- For the test group (Ultra-Fast Protocol): Place 1 mL of the low-sucrose (e.g., 0.25 M) warming medium in a dish. Immediately upon removal from liquid nitrogen, plunge the storage device into the medium and leave for exactly 2 minutes [11].
- For the control group (Standard Protocol): Use a multi-step warming protocol with decreasing sucrose concentrations (e.g., 1.0 M → 0.5 M → 0.25 M), spending several minutes in each solution.
- Post-Warming Handling: After the warming step, wash the blastocysts from all groups several times in pre-warmed culture medium.
- Assessment and Incubation:
- Transfer the washed blastocysts to a culture medium droplet and incubate until further analysis.
- Monitor and record the time to initial and full re-expansion (e.g., at 1, 2, 3 hours post-warming).
- Assess survival rates based on morphological integrity (e.g., membrane integrity, cell cohesion).
- For longer-term studies, culture the blastocysts to assess developmental competence, including hatching rates and cell count.
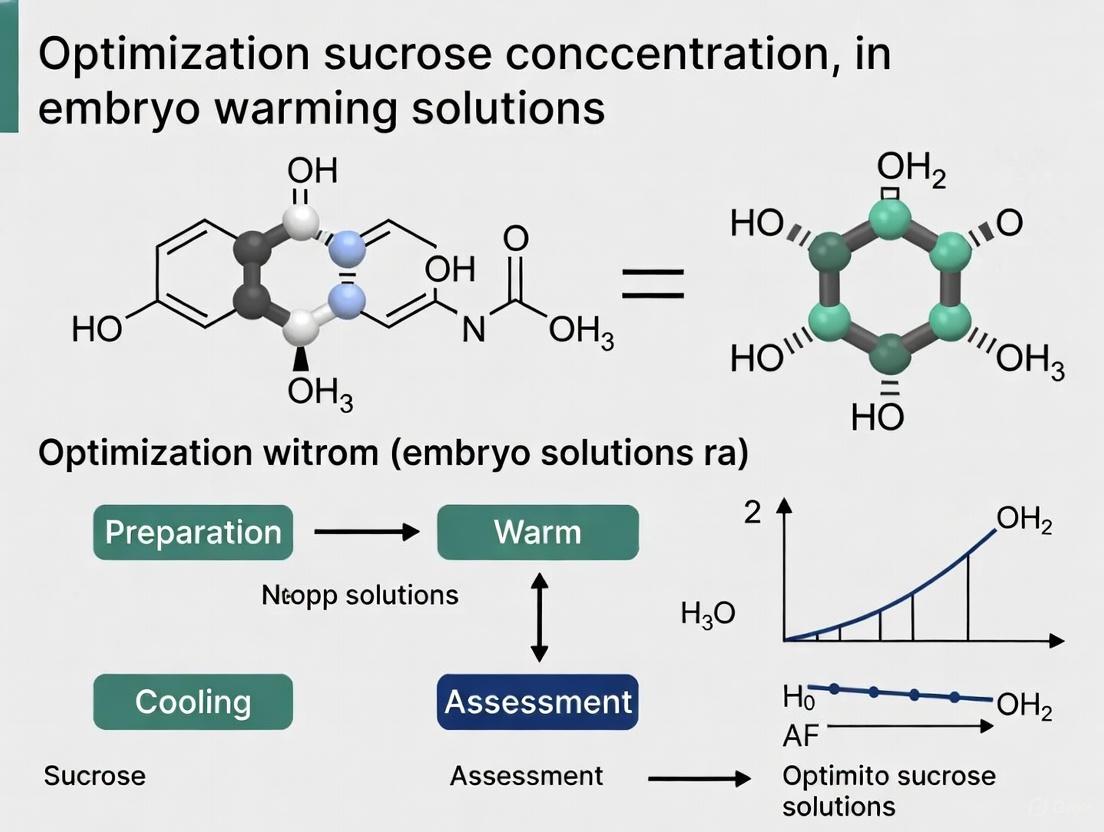
Diagram 1: Sucrose concentration optimization experimental workflow.
Visualizing Sucrose's Protective Mechanism
The following diagram illustrates the multi-faceted protective role of sucrose during the cryopreservation warming process, highlighting its synergistic action with permeating cryoprotectants.
Diagram 2: The multi-faceted protective mechanism of sucrose during warming.
Fundamental Principles of Vitrification and Warming in Assisted Reproduction
Core Principles and FAQs
What is the fundamental goal of vitrification?
The goal of vitrification is to achieve a glass-like (vitreous) state in cells by using an ultra-rapid cooling rate, which prevents the formation of damaging intracellular and extracellular ice crystals. This is distinct from slow freezing, where ice forms extracellularly. Vitrification depends on a combination of a high cooling rate, high concentration of cryoprotectants (CPAs), and a very small sample volume to solidify the cell's contents into a non-crystalline, amorphous solid [15] [16].
Why is the warming rate as critical as the cooling rate?
A rapid warming rate is crucial to avoid the lethal process of recrystallization. During slow warming, small ice crystals that may have formed have time to merge and grow, causing severe damage to the cellular structure. It has been demonstrated that the lethality of a slow warming rate is a direct consequence of this recrystallization [16].
How does sucrose function in warming solutions?
Sucrose, a non-permeating cryoprotectant, acts as an osmotic buffer during the warming and dilution process. It creates a hypertonic environment outside the cell, which draws water out in a controlled manner. This prevents a rapid influx of water into the cell as permeating CPAs (e.g., Ethylene Glycol, DMSO) diffuse out, thereby avoiding lethal cellular swelling and osmotic shock [17] [5].
What are the key variables to optimize in a vitrification protocol?
The success of vitrification hinges on a delicate balance of several variables [18] [16] [19]:
- Cryoprotectant Toxicity and Concentration: The type, concentration, and exposure time to CPAs must minimize chemical toxicity while achieving sufficient dehydration.
- Cooling and Warming Rates: Ultrafast rates (greater than -10,000°C/min for cooling) are essential.
- Sample Volume: Minimal volumes (1-3 µL) are used to maximize heat transfer.
- Temperature at Exposure: The temperature during CPA exposure can influence toxicity and osmotic stress.
Troubleshooting Common Vitrification and Warming Issues
Low survival rates post-warming
- Potential Cause: Suboptimal sucrose concentration in the warming solution.
- Solution: Empirically determine the ideal sucrose molarity for your specific cell type. Research on rat zygotes showed that a 0.1 M sucrose concentration in the warming solution significantly enhanced survival and developmental rates compared to other concentrations [5]. Refer to Table 1 for specific data.
- Potential Cause: Slow warming rate leading to recrystallization.
- Solution: Ensure your warming method achieves the most rapid warming rate possible (e.g., +24,000°C/min by swirling the device in a 37°C water bath) [17]. Verify that the water bath has a sufficient volume (≥500 mL) for efficient heat transfer.
Osmotic shock and damage during CPA removal
- Potential Cause: Incorrect sequence or timing of the multi-step warming and dilution process.
- Solution: Adhere strictly to validated protocols. A typical protocol involves moving the specimen sequentially from Thawing Solution (TS, containing sucrose) to a Dilution Solution (DS, lower sucrose), and then through one or more Washing Solutions (WS, sucrose-free) to rehydrate the cell gently [17].
Concerns regarding cryoprotectant toxicity
- Potential Cause: Overexposure to permeable CPAs like DMSO or Ethylene Glycol at room temperature.
- Solution: Shorten the exposure time to the final vitrification solution. Recent research focuses on shortening equilibration and dilution steps. Perform CPA addition and removal steps at precisely controlled temperatures to mitigate toxic effects [18] [19].
Optimizing Sucrose Concentration: Experimental Data and Protocols
Quantitative Data on Sucrose Concentration Impact
The following table summarizes key experimental data on the effect of sucrose concentration during warming on the survival and development of vitrified-warmed rat zygotes [5].
Table 1: Effect of Sucrose Concentration in Warming Solution on Vitrified-Warmed Rat Zygotes
| Sucrose Concentration (M) | Survival Rate (%) | Development to 2-Cell Stage (%) | Key Findings |
|---|---|---|---|
| 0.0 | ~60% | ~50% | Baseline for comparison; high osmotic stress. |
| 0.05 | Data not specified | Data not specified | -- |
| 0.1 | ~90% | ~85% | Optimal concentration for survival and development. |
| 0.2 | ~80% | ~75% | Viable but suboptimal. |
| 0.3 | ~70% | ~65% | Higher concentration may cause over-dehydration. |
Detailed Experimental Protocol: Warming with Optimized Sucrose
This protocol is adapted from established methods for warming oocytes/embryos and incorporates the principle of sucrose optimization [17] [5].
Title: Protocol for Warming Vitrified Embryos with Sucrose-Optimized Solutions
Principle: A one-step fast warming protocol using a Thawing Solution (TS) containing an optimized concentration of sucrose (e.g., 0.1 M) has been shown to yield clinical outcomes comparable to standard, longer protocols while significantly shortening the procedure time [20] [5].
Workflow Diagram:
Materials:
- Pre-equilibrated culture medium with protein supplement (e.g., 20% SSS)
- Waterbath at 37°C (minimum volume 500 mL)
- Warming dish
- Sterile scissors, syringe, connector (for devices like CryoTip)
- Solutions:
- Thawing Solution (TS): Contains an optimized molarity of sucrose (e.g., 0.1 M) [5].
- Dilution Solution (DS): Contains a lower concentration of sucrose.
- Washing Solution (WS): Sucrose-free medium.
Procedure:
- Preparation: Pre-equilibrate all solutions and the culture dish. Set up the warming dish with drops of TS and DS as required by the specific device protocol [17].
- Warm: Quickly transfer the vitrification device from liquid nitrogen and fully immerse it in the 37°C waterbath for approximately 3 seconds, swirling gently to ensure a rapid and uniform warming rate [17].
- Content Retrieval: Quickly open the device (following manufacturer's instructions) and dispense its contents directly into the pre-warmed TS drop. Allow the specimen to remain in the TS for 1 minute [17].
- Dilution: Transfer the specimen to the DS drop for 4 minutes. Gently pipette the specimen once to ensure complete rinsing [17].
- Washing: Transfer the specimen through two drops of WS, allowing 4 minutes in each drop [17].
- Recovery: Transfer the warmed specimen to the pre-equilibrated culture medium for the required recovery period (e.g., 2-3 hours for oocytes, 3 hours or immediate transfer for embryos) [17].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Vitrification and Warming Research
| Item | Function |
|---|---|
| Permeating CPAs | Small molecules that penetrate the cell membrane (e.g., Ethylene Glycol (EG), Dimethyl Sulfoxide (DMSO)). They depress the freezing point and enable vitrification [16] [19]. |
| Non-Permeating CPAs | Large molecules that do not enter the cell (e.g., Sucrose, Trehalose). They act as osmotic agents to dehydrate the cell before cooling and control rehydration during warming [17] [5]. |
| Open Cryo-Devices | Carriers like CryoTop or Open Pulled Straw (OPS) that expose the sample directly to liquid nitrogen. They maximize cooling/warming rates but pose a potential contamination risk [16]. |
| Closed Cryo-Devices | Sealed systems like the HSV Security Straw that protect the sample from direct contact with liquid nitrogen, reducing contamination risk, potentially at the cost of slightly lower cooling rates [17] [16]. |
| Base Medium | The isotonic culture medium (e.g., PB1, mHTF) used as the solvent for preparing all vitrification and warming solutions [5]. |
| Protein Supplement | (e.g., Human Serum Albumin - HSA). Added to warming and culture media to reduce stickiness and protect the cellular membrane during handling [17]. |
Core Concepts and Frequently Asked Questions
What is the fundamental challenge in using cryoprotectants?
The central challenge in cryopreservation is balancing two opposing factors: the cryoprotection offered by these agents against freezing damage, and their inherent cytotoxicity at the concentrations required for effective preservation. High levels of penetrating cryoprotectants (CPAs) can eliminate ice formation during cooling to cryogenic temperatures, but they become increasingly toxic as concentration increases. In fact, for complex biological systems like organs, CPA toxicity is considered the greatest obstacle to cryopreservation [13].
What are the common types of cryoprotectants and their toxicities?
Cryoprotectants are broadly categorized based on their ability to cross cell membranes, which influences their mechanism of action and toxicity profile [1].
- Penetrating (Permeating) Cryoprotectants: These are small, neutral molecules that can diffuse across cell membranes. They protect cells primarily through colligative effects—depressing the freezing point and reducing the amount of ice formed at a given temperature, which in turn moderates the harmful concentration of electrolytes. However, they can cause specific chemical toxicity [13] [1]. Common examples include:
- Dimethyl sulfoxide (DMSO)
- Ethylene glycol (EG)
- Propylene glycol (PG)
- Glycerol (GLY)
- Non-Penetrating Cryoprotectants & Sugars: These are larger molecules or polymers that cannot easily cross the cell membrane. They protect cells by increasing the viscosity of the solution and modulating ice crystal growth outside the cell. They generally have lower cytotoxicity and can help reduce the required concentration of penetrating CPAs [1]. This category includes:
- Sucrose
- Trehalose
- Raffinose
- Polymers like Hydroxyethyl starch (HES) and Ficoll
The following table summarizes the specific toxicities associated with common penetrating cryoprotectants [13]:
| Cryoprotectant | Documented Toxicities and Effects |
|---|---|
| Dimethyl Sulfoxide (DMSO) | Induces ultrastructural alterations in rat myocardium at high concentrations; reduces clonogenic potential of blood progenitor cells; causes cell membrane undulations and swelling [13]. |
| Ethylene Glycol (EG) | Metabolized to glycolic and oxalic acid, leading to metabolic acidosis and formation of calcium oxalate crystals in tissues like the kidney [13]. |
| Propylene Glycol (PG) | Can impair the developmental potential of mouse zygotes by decreasing intracellular pH at concentrations exceeding 2.5 M [13]. |
| Glycerol (GLY) | Can induce renal failure in rats via inflammation, oxidative stress, and apoptosis; depletes reduced glutathione, leading to oxidative stress; polymerizes the actin cytoskeleton in spermatozoa [13]. |
| Formamide (FMD) | A highly corrosive amide that can cause kidney and blood cell injury; can denature DNA, an effect believed to be due to displacement of hydrating water [13]. |
| Methanol (METH) | Metabolized to formaldehyde and formic acid, which can cause metabolic acidosis, cardiovascular instability, and destruction of the optic nerve [13]. |
How does cytotoxicity quantitatively compare between cryoprotectants?
Toxicity is not just about the chemical itself, but also its concentration, exposure time, temperature, and the biological system. The table below compares the toxicity of different CPAs based on experimental data:
| Cryoprotectant | Biological System | Exposure Conditions | Toxicity Manifestation |
|---|---|---|---|
| Propylene Glycol (PG) | Mouse blastocysts | > 2.5 M | Reduced developmental potential [13] |
| Glycerol (GLY) | Stallion spermatozoa | > 1.5% (v/v) | Polymerization of actin cytoskeleton [13] |
| DMSO | Human dermal fibroblasts | 5-30% (v/v), 10-30 min, 4-37°C | Decreased viability with increased concentration, temperature, and time [13] |
| DMSO | Hamster fibroblasts | 10% (v/v), 1 hr, 37°C | Undulations in cell membrane; 20% caused swelling [13] |
| Linoleic Acid | Bovine oocytes | 100 µM (in maturation medium) | Induced significant apoptosis and disrupted membrane integrity [21] |
Troubleshooting Common Cryoprotectant Issues
Problem: Poor Post-Thaw Cell Viability and Recovery
Potential Causes and Solutions:
- Cause 1: Excessive Cytotoxicity from Penetrating CPAs.
- Solution: Reduce the concentration of the penetrating CPA (e.g., DMSO) by supplementing with non-penetrating agents. Sucrose is frequently used for this purpose. It acts as an osmotic buffer, helps dehydrate the cell before freezing, and reduces the amount of penetrating CPA needed, thereby lowering overall toxicity [1]. For example, in NK cell cryopreservation, combinations of osmolytes were found to mitigate the loss of cytotoxicity and membrane fluidity caused by CPAs [22].
- Cause 2: Osmotic Shock During Addition or Removal.
- Solution: Use a multi-step protocol for adding and removing CPAs. Gradually introduce and dilute the CPA in several steps rather than a single, abrupt change. This allows cells to adjust their volume progressively and minimizes membrane stress [23] [24]. The use of sucrose in warming solutions can similarly create a gentler osmotic gradient for rehydration [25].
- Cause 3: Suboptimal Cooling Rate.
- Solution: Optimize the cooling rate for your specific cell type. A controlled rate freezer, or a passive cooling device like an isopropanol chamber, can help achieve the standard slow cooling rate of approximately -1°C/minute, which is suitable for many mammalian cells. This slow rate prevents lethal intracellular ice formation while avoiding excessive dehydration [23] [24].
Problem: Compromised Cellular Function Post-Thaw
Even if viability is high, cells may not function correctly (e.g., impaired differentiation, reduced secretion, low fertilization rates).
Potential Causes and Solutions:
- Cause: Subtle CPA-Induced Damage.
- Solution: Extend functionality assessments beyond simple viability stains. For instance, research on NK cells showed that exposure to cryoprotectants reduced membrane fluidity and cell-induced cytotoxicity even before freezing, and that freezing disrupted cytolytic granules [22]. In bovine oocytes, vitrification was found to promote changes in the distribution of the transcription factor OCT4, a marker of developmental competence [21]. Monitoring such functional and molecular markers is crucial for protocol optimization.
Emerging Solutions and Experimental Protocols
Novel Materials: DNA Frameworks
Recent research introduces membrane-targeted, biodegradable DNA frameworks (DFs) as a next-generation strategy. These DFs, functionalized with cholesterol, are designed to specifically target and protect cell membranes during freezing. A key advantage is their autonomous biodegradation after thawing, eliminating long-term toxicity risks associated with conventional CPAs like DMSO. Studies on macrophage cell lines show they can recover cellular function and morphology effectively [26].
Optimizing Sucrose in Embryo/Oocyte Warming: A Sample Protocol
The concentration of non-penetrating cryoprotectants like sucrose in warming solutions is critical for managing osmotic stress. Recent clinical studies have explored modified warming protocols (MWP) to improve outcomes.
Background: A 2025 clinical study on donor oocytes compared a Conventional Warming Protocol (CWP) with a Modified Warming Protocol (MWP). The MWP simplified the process into an ultrafast, single-step by eliminating the dilution and wash solution steps, incubating oocytes only in a thawing solution for 1 minute [25].
Key Finding: While survival rates were similar (93.9% MWP vs. 93.7% CWP), the MWP group showed significantly higher rates of blastocyst formation (77.3% vs. 57.5%) and usable blastocysts (51.4% vs. 35.4%). Ongoing pregnancy/live birth rates were also higher in the MWP group (66.7% vs. 50.4%). This suggests that a faster, simplified warming protocol using optimized solutions can reduce cryoprotectant exposure time and improve clinical outcomes by better preserving developmental potential [25].
Methodology:
- Warming: Oocytes were rapidly warmed to 37°C in a thawing solution (TS) for 1 minute [25].
- Sucrose Dilution: In the CWP, a gradient dilution approach followed, involving incubation in a dilution solution (DS) containing sucrose for 3 minutes and a wash solution (WS) for 5-6 minutes at room temperature to remove CPAs and mitigate osmotic shock [25].
- Assessment: Oocytes were cultured for 2 hours before assessing survival, followed by fertilization (ICSI) and embryo culture to track development to blastocyst and pregnancy [25].
This highlights that optimizing the timing and concentration of sucrose during the warming phase is a critical area of research for reducing cryoprotectant-related damage.
The Scientist's Toolkit: Key Reagents
| Research Reagent | Function in Cryopreservation |
|---|---|
| Dimethyl Sulfoxide (DMSO) | A penetrating cryoprotectant that replaces intracellular water, reduces ice formation, and depresses the freezing point. The most common CPA for mammalian cells, but has known cytotoxicity [23] [1]. |
| Sucrose | A non-penetrating disaccharide. Used in freezing and warming solutions as an osmotic buffer to control cell dehydration/rehydration, and to reduce the required concentration of toxic penetrating CPAs [1]. |
| Trehalose | A non-penetrating disaccharide used by many organisms to survive freezing and drying. It stabilizes cell membranes and proteins during desiccation and freezing stress [1]. |
| Ethylene Glycol (EG) | A low-molecular weight, penetrating CPA often used in vitrification solutions for its rapid penetration into cells [13] [1]. |
| Hydroxyethyl Starch (HES) | A non-penetrating polymer that increases solution viscosity, modulates ice crystal growth, and can partially replace penetrating CPAs to reduce toxicity [1]. |
| CryoStor CS10 | A commercially available, ready-to-use, serum-free freezing medium containing 10% DMSO. Provides a defined and optimized environment for freezing various cell types [24]. |
Visualizing Cryoprotectant Mechanisms and Damage Pathways
The diagram below illustrates the central dilemma of cryoprotectant use, showing how the protective mechanisms of CPAs are intrinsically linked to their potential cytotoxic and osmotic damage pathways.
Diagram Title: The Cryoprotectant Dilemma: Protection vs. Damage
Key Takeaways for Your Research
- There is no universal solution. The optimal balance between cryoprotection and cytotoxicity depends heavily on the cell type.
- Sucrose is a key tool. Its role as a non-penetrating osmolyte is central to strategies aimed at reducing the concentration and exposure time of more toxic, penetrating CPAs.
- Protocol details matter. The rates of cooling, warming, and CPA addition/removal are as critical as the chemical composition of the solutions themselves.
- Assess function, not just viability. Moving beyond simple viability assays to measure specific cellular functions is essential for developing truly effective cryopreservation protocols.
Protocol Evolution: Implementing Simplified One-Step Warming with 1M Sucrose
Standard multi-step warming represents the foundational methodology for revitalizing vitrified embryos in assisted reproductive technologies (ART). This traditional protocol is engineered to mitigate osmotic shock by gradually removing cryoprotectants (CPAs) and reintroducing water to the cells through a series of solutions with carefully balanced solute concentrations. The integrity of this process is paramount to ensuring high rates of embryo survival, implantation, and subsequent development. As novel simplified protocols emerge, the multi-step method serves as the critical benchmark for evaluating new techniques, underscoring its enduring importance in reproductive science and clinical practice. This guide details the established multi-step protocols, provides quantitative performance data, and offers troubleshooting support to uphold the highest standards of laboratory efficacy.
Performance Data: Multi-Step vs. One-Step Warming
The following tables summarize key quantitative findings from recent comparative studies, providing a performance baseline for the standard multi-step warming protocol.
Table 1: Clinical Outcomes from Ebinger et al. (2025) Cohort Study [27] This large-scale retrospective analysis (1,402 transferred embryos) compared traditional multi-step warming with a one-step alternative.
| Outcome Measure | Multi-Step Warming | One-Step Warming | P-value |
|---|---|---|---|
| Survival Rate | Comparable | Comparable | N/S |
| Clinical Pregnancy Rate (CPR) | 42.6% | 44.3% | 0.78 |
| Ongoing Pregnancy Rate (OPR) | 33.2% | 37.5% | 0.21 |
| CPR (Top Quality Embryos - G1) | 52.3% | 54.6% | >0.05 |
| OPR (Top Quality Embryos - G1) | 46.0% | 48.1% | >0.05 |
| CPR (Day 5 Embryos) | 44.8% | 46.5% | >0.05 |
| CPR (Day 6 Embryos) | 28.0% | 31.2% | >0.05 |
Table 2: Laboratory and Preclinical Development Outcomes [28] This study compared the developmental potential of cleavage and blastocyst-stage embryos after warming.
| Outcome Measure | Multi-Step Warming | One-Step Warming | P-value |
|---|---|---|---|
| Survival Rate (Cleavage Stage) | 100% | 100% | N/S |
| Survival Rate (Blastocyst Stage) | 99% | 99% | N/S |
| Blastulation Rate (from Cleavage) | 73% | 78% | 0.4044 |
| Full-Blastocyst Formation Rate | 53% | 60% | 0.3196 |
| Frequency of Collapses (Time-Lapse) | 50% | 30% | 0.0410 |
| Full Re-expansion at 3h (Blastocyst) | 75% | 67% | 0.2417 |
| Full Re-expansion at 24h (Blastocyst) | 97% | 98% | 1.0000 |
Troubleshooting Guide & FAQs
FAQ 1: Post-warming survival is low. What are the primary factors to investigate?
Low survival rates often point to issues with osmotic stress or cryoprotectant toxicity.
- Solution A: Verify Sucrose Concentration Accuracy. Precise molarity is non-negotiable. In a rat model, a warming solution containing 0.1M sucrose significantly enhanced survival rates compared to other concentrations [5] [29]. Regularly calibrate equipment and use fresh, validated reagents.
- Solution B: Audit Timing in Each Warming Step. Prolonged exposure in one step or rushed transitions can cause osmotic damage. Adhere strictly to the protocol's designated timings (e.g., 1 min in 1M sucrose, 3 min in 0.5M sucrose, 10 min in washing solution) [27]. Use a dedicated timer and standardize embryologist movements.
- Solution C: Check for Temperature Fluctuations. Warming solutions must be pre-warmed and maintained at 37°C. Performing the procedure on a heated stage ensures a stable thermal environment, preventing chilling injury during this critical phase.
FAQ 2: Embryos appear morphologically intact after warming but exhibit poor implantation potential. Why?
This suggests sublethal cellular damage not visible under standard morphology assessment.
- Solution A: Assess Blastocoel Re-expansion Dynamics. A slowed re-expansion can indicate damage. Research shows that while multi-step warmed blastocysts might re-expand faster initially (2.14 ± 2.17 hours vs. 3.20 ± 3.03 hours for one-step), the final proportion of fully re-expanded blastocysts at 24 hours is equivalent (97-98%) [28]. Monitor re-expansion at 3h and 24h as a health indicator.
- Solution B: Review the Vitrification Protocol. The warming outcome is intrinsically linked to the quality of the initial vitrification. Suboptimal vitrification can cause irreparable damage to the cytoskeleton and organelles, compromising developmental competence even if the embryo survives the thaw.
- Solution C: Consider Time-Lapse Incubator Monitoring. Subtle abnormalities in morphokinetics, such as the frequency of blastocoel collapses, may be more prevalent in certain protocols and correlate with developmental potential [28].
FAQ 3: How does embryo quality influence the choice of warming protocol?
While standard multi-step warming is robust across embryo grades, its performance relative to simplified protocols can vary.
- Evidence: One study found that for top-quality (G1) blastocysts, ongoing pregnancy rates were 46.0% with multi-step versus 48.1% with one-step warming. For lower-quality (G2) blastocysts, the rates were 27.8% versus 33.0%, respectively [27]. The differences were not statistically significant, demonstrating that multi-step warming remains a effective method for embryos of varying quality.
Detailed Experimental Protocol
Below is a detailed methodology for the standard multi-step warming of vitrified blastocysts, as referenced in the clinical literature [27].
Objective: To safely and effectively warm vitrified blastocyst-stage embryos using a sequential dilution method to remove cryoprotectants and minimize osmotic stress.
Materials:
- Pre-warmed base medium (e.g., PB1, mHTF)
- Sucrose solutions: 1.0 M and 0.5 M in base medium
- Washing solution (base medium only)
- Pre-warmed culture dish (e.g., Falcon 1006)
- Sterile pipettes and tips
- Timer
- Heated stage (37°C)
Workflow:
Procedure:
- Preparation: Label a culture dish with patient details. Create droplets of the 1.0M sucrose, 0.5M sucrose, and washing solution. Pre-warm all solutions and the dish on a 37°C heated stage for at least 30 minutes before warming.
- Warming & Initial Dilution: Rapidly retrieve the vitrified straw or cryotube from liquid nitrogen and warm according to the manufacturer's instructions (e.g., air for 10 seconds, then water bath at 37°C for 20 seconds). Expel the contents into the pre-warmed 1.0M sucrose solution. Start the timer. Incubate for 1 minute. This high-osmolality solution initiates the slow removal of permeable CPAs.
- Secondary Dilution: Using a sterile pipette, gently transfer the embryos to the droplet of 0.5M sucrose solution. Incubate for 3 minutes. This step further reduces the CPA concentration in a controlled manner.
- Final Wash & Rehydration: Transfer the embryos through at least two droplets of the washing solution (sucrose-free base medium). The total time in this step should be approximately 10 minutes. This allows for complete rehydration of the cells.
- Culture: After the final wash, transfer the embryos into a pre-equilibrated culture medium. Assess survival and morphological integrity before scheduling for transfer or further culture.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Multi-Step Warming Protocols
| Reagent / Solution | Function in Protocol | Key Considerations |
|---|---|---|
| Permeating Cryoprotectants(e.g., Ethylene Glycol, DMSO) | Small molecules that enter the cell, preventing intracellular ice crystal formation during vitrification. Their removal during warming must be controlled. | Potential cytotoxicity with prolonged exposure dictates strict adherence to warming timings [27]. |
| Non-Permeating Cryoprotectants(e.g., Sucrose) | Remains outside the cell, creating an osmotic gradient that draws water out and facilitates controlled CPA efflux during warming [27]. | Concentration is critical (e.g., 1M vs. 0.5M). Accuracy directly impacts survival by preventing osmotic shock [5]. |
| Base Medium(e.g., PB1, mHTF, Human Tubal Fluid) | Buffered salt solution that serves as the foundation for preparing all warming solutions. Provides physiological pH and nutrient support. | Must be pre-warmed to 37°C to avoid thermal stress. Osmolality should be verified regularly [5]. |
| Protein Supplement(e.g., Human Serum Albumin - HSA) | Often added to warming and culture media. Helps stabilize the cell membrane and reduces embryo stickiness to labware. | Use a concentration appropriate for the specific embryo stage and media system. |
The one-step fast warming protocol is an innovative technique for devitrifying vitrified embryos and oocytes. It is designed to streamline the traditional, multi-step process, significantly reducing procedure time and laboratory workload while maintaining high survival and clinical pregnancy rates. This protocol is a focus of ongoing research, particularly in the context of optimizing sucrose concentrations and other cryoprotectant agents to ensure maximum cell viability post-warming [30] [31].
This technical support center provides a detailed guide for researchers and scientists implementing this protocol, addressing common questions and troubleshooting specific experimental issues.
Detailed Experimental Protocols
The following section outlines the specific methodologies for one-step warming as cited in key studies, providing a reproducible framework for your experiments.
Methodology from Karagianni et al. (2025)
This prospective cohort study provides a direct comparison between one-step and conventional multi-step warming.
- Study Design: The research was conducted at the Embryolab Fertility Clinic. The fast-warming group used the one-step protocol, while the control group used a conventional multi-step protocol. Both groups consisted of patients with good-quality expanded blastocysts, matched for maternal age, embryo quality, and other key factors [30] [20].
- One-Step Fast Warming Protocol:
- Standard Multi-Step Warming Protocol (Control):
- Blastocysts were warmed by exposure to 1M sucrose for 1 minute.
- Then transferred to 0.5M sucrose for 2 minutes.
- Then transferred to 0.25M sucrose for 2 minutes.
- Finally, rinsed in a washing solution for 3 minutes at room temperature before being placed into culture media for laser-assisted hatching [30] [20].
Methodology from Mass General Validation Study (2025)
An external validation study confirmed the efficacy of a single-step protocol.
- Single-Step Warming Protocol (SS):
- Exposure: Blastocysts were exposed to a thaw solution (1M sucrose, 20% dextran serum supplement [DSS], and gentamicin) at 37°C for 1 minute [32].
- Rinsing and Incubation: Embryos were then vigorously rinsed through five separate 25-µL drops of Continuous Single Culture-NX Complete culture media.
- They were subsequently incubated for 1–4 hours prior to embryo transfer [32].
- Key Finding: This protocol saved at least 15 minutes per cryothaw procedure compared to their standard protocol, enhancing laboratory efficiency without compromising outcomes [32].
Methodology for a Diluted One-Step Protocol (2025)
A variation of the one-step protocol using a different sucrose concentration has also been validated.
- Diluted One-Step Warming Protocol:
- Conclusion: This study concluded that eliminating the first step of the standard warming procedure (typically 1M sucrose) not only reduces execution time but also simplifies the learning curve while maintaining effectiveness [31].
The table below summarizes quantitative data from key studies, allowing for easy comparison of the one-step protocol's performance against traditional methods.
| Study & Protocol | Survival Rate | Clinical Pregnancy Rate | Ongoing Pregnancy Rate | Miscarriage Rate | Key Efficiency Note |
|---|---|---|---|---|---|
| Karagianni et al. (2025)One-Step (1M sucrose) vs. Standard | Comparable | 56.86% vs. 57.36% | 50.62% vs. 51.12% | 6.23% vs. 6.23% | Significant reduction in warming time [30] |
| Mass General (2025)Single-Step vs. Standard Warming | 100% vs. 100% | No significant difference | No significant difference | No significant difference | Saves ≥15 minutes per procedure [32] |
| Diluted One-Step (2025)One-Step (0.5M sucrose) vs. Standard | 94% vs. 98% | Not Reported | Not Reported | Not Reported | Reduces execution time and learning curve [31] |
| Ebinger et al. (2025)One-Step (1M sucrose) vs. Multi-Step | Comparable | 44.3% vs. 42.6% | 37.5% vs. 33.2% | Not Reported | Decreases procedure time by >90% [33] |
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Does the one-step warming protocol compromise embryo survival or pregnancy outcomes?
- Answer: No. Multiple studies have found no statistically significant differences in survival, implantation, clinical pregnancy, ongoing pregnancy, or live birth rates between the one-step and conventional multi-step protocols [30] [32] [33]. The primary advantage of the one-step protocol is increased efficiency without sacrificing efficacy.
FAQ 2: What is the optimal sucrose concentration for a one-step warming protocol?
- Answer: Research indicates that more than one concentration is viable. Studies have successfully used a 1M sucrose solution for 1 minute [30] [33]. Another study demonstrated that a 0.5M sucrose solution for 3 minutes is also effective, potentially offering a gentler osmotic transition [31]. Optimization in your specific lab environment is recommended.
FAQ 3: We have oocytes vitrified with Kitazato media. Can we warm them using a different brand's warming kit?
- Answer: Evidence suggests yes. A multicenter study demonstrated the feasibility of a "Universal Warming Protocol," where oocytes vitrified with Kitazato media were successfully warmed using kits from Irvine Scientific and Vitrolife with comparable fertilization and pregnancy outcomes [34]. This provides flexibility and can reduce costs.
Troubleshooting 1: We are observing lower-than-expected survival rates after switching to a one-step protocol. What could be the cause?
- Check the Temperature: Ensure the sucrose solution is pre-warmed and maintained precisely at 37°C during the exposure step. Temperature fluctuation is a critical variable.
- Verify Solution Concentrations: Accurately prepare and quality-check the sucrose solutions. A deviation in molarity can cause osmotic shock.
- Review the Timing: Strictly adhere to the exposure and rinse times. Over-exposure to the sucrose solution can be detrimental.
Troubleshooting 2: How can we validate the one-step protocol in our laboratory?
- Phased Approach: Follow a model like the Mass General validation study [32].
- Research Phase: Begin by thawing donated research-grade blastocysts, dividing them between the standard and one-step protocols. Compare survival and re-expansion rates at 2 and 4 hours.
- Clinical Implementation: Only after confirming safety and efficacy in the research phase should the protocol be uniformly adopted for clinical frozen embryo transfer cycles.
- Phased Approach: Follow a model like the Mass General validation study [32].
The Scientist's Toolkit: Essential Research Reagents
The following table details key materials and reagents used in the one-step warming protocols described in the research.
| Reagent / Material | Function in the Protocol | Examples from Literature |
|---|---|---|
| Sucrose Solution (1M or 0.5M) | Primary cryoprotectant; creates an osmotic gradient to remove water and prevent ice crystal formation during warming. | 1M sucrose [30] [33]; 0.5M sucrose [31] |
| Thaw / Dilution Solution | Contains sucrose and supplements to initiate the rehydration process in a controlled manner. | 1M sucrose with 20% DSS [32] |
| Culture Media | Provides nutrients and a stable environment for the embryo to recover and re-expand post-warming. | Continuous Single Culture-NX Complete [32] |
| Protein Supplement | Added to solutions to stabilize the cell membrane and reduce osmotic stress. | Dextran Serum Supplement (DSS) [32] |
| Washing Solution | Used to fully remove cryoprotectants after the initial sucrose exposure. | M-199 HEPES-buffered medium [32] |
Experimental Workflow Visualization
The diagram below illustrates the key decision points and steps in the one-step warming protocol workflow, from preparation to post-warming assessment.
In the field of assisted reproductive technologies (ART) and biomedical research, the cryopreservation of oocytes, zygotes, and embryos is a fundamental practice. Recent advancements have focused on optimizing warming protocols to enhance efficiency while maintaining—or even improving—developmental potential. Traditional warming procedures are often multi-step, time-consuming processes that can take 15 minutes or more. The emergence of one-step fast warming protocols represents a significant breakthrough, reducing procedure times by over 90% while achieving comparable or superior clinical outcomes. This technical support center provides comprehensive guidance on implementing these rapid protocols, with particular focus on the critical role of sucrose concentration optimization in warming solutions.
Key Research Reagent Solutions
The following table details essential reagents and materials referenced in optimized warming protocols, with explanations of their functions in the cryopreservation workflow.
Table 1: Key Research Reagent Solutions for Vitrification and Warming
| Reagent/Material | Function/Application | Research Context |
|---|---|---|
| Ultra RapidWarm Blast | Commercial warming medium containing 0.25 M sucrose for one-step human blastocyst warming [35]. | Human embryo vitrification/warming |
| DAP213 Vitrification Solution | Contains 2 M DMSO, 1 M acetamide, and 3 M propylene glycol; used for zygote vitrification [5] [29]. | Rat zygote vitrification |
| PB1 Medium with Sucrose | Base solution for preparing warming solutions with varying sucrose concentrations (0-0.3 M) [5] [29]. | Optimization of rat zygote warming |
| Linoleic Acid (LA) | Polyunsaturated fatty acid supplemented during in vitro maturation to modulate membrane fluidity and improve cryotolerance [21]. | Bovine oocyte cryopreservation |
| Cryotop Device | Surface vitrification device enabling ultra-small sample volumes (~0.1 μL) for high cooling rates [21]. | Oocyte/embryo vitrification |
| Open-Pulled Straw (OPS) | Tubular vitrification device with reduced diameter for improved cooling rates [21]. | Embryo vitrification in domestic species |
Protocol Comparison: Conventional vs. Rapid Warming
The following table provides a detailed comparison of conventional and rapid warming protocols across different biological materials, highlighting the dramatic reduction in procedure time.
Table 2: Workflow Comparison Between Conventional and Rapid Warming Protocols
| Parameter | Conventional Warming Protocol (CWP) | Rapid/One-Step Warming Protocol | Time Reduction |
|---|---|---|---|
| Human Blastocysts | Multi-step process with sequential solutions [25] | Single-step warming in 1 minute [20] [35] | ~90% (from ~10-15 min to ~1 min) |
| Human Oocytes (Donor) | Thawing solution (1 min) + Dilution solution (3 min) + Wash solution (5-6 min) [25] | Modified Warming Protocol (MWP) with simplified steps [25] | Significant time saving (exact % not specified) |
| Rat Zygotes | Not explicitly detailed in search results | Optimized warming in PB1 with 0.1 M sucrose for 60 seconds at 25°C [5] [29] | Protocol specifically developed for efficiency |
| Procedure Steps | Multiple equilibration steps in solutions with decreasing sucrose concentrations [25] | Single-step direct transfer to warming solution [20] [35] | Minimal handling steps |
| Laboratory Efficiency | Approximately 1 hour of embryologist time per day [35] | Saves up to 1 hour of work time per day [35] | Increases daily productivity |
Experimental Protocols & Methodologies
One-Step Fast Warming of Human Blastocysts
Reference: Karagianni et al. (2025) [20]
Objective: To compare the efficacy of a one-step fast warming protocol versus standard warming for vitrified human blastocysts.
Methodology:
- Study Design: Prospective cohort study at Embryolab Fertility Clinic (Greece) from January 2023 to June 2024.
- Patient Groups: 802 cycles divided into study group (one-step fast warming) and control group (standard warming), with matched maternal age, treatment type, and embryo quality.
- Fast Warming Protocol: Blastocysts were warmed using a single-step protocol with specific warming media.
- Outcome Measures: Survival rate, pregnancy rate, clinical pregnancy rate, implantation rate, ongoing pregnancy rate, biochemical pregnancy rate, miscarriage rate, and live birth rate.
Key Findings: The one-step fast warming protocol yielded comparable outcomes to standard warming across all measured parameters, while offering practical advantages including significantly shorter warming duration.
Optimization of Rat Zygote Warming
Reference: Nakagata et al. (2025) [5] [29]
Objective: To evaluate the effects of warming solutions containing different sucrose concentrations and oocyte donor age on the viability of vitrified-warmed rat zygotes.
Methodology:
- Vitrification Protocol: Zygotes were pretreated with PB1 containing 1 M DMSO at 25°C, transferred to cryotubes, placed at 0°C for 5 minutes, then vitrification solution (DAP213) was added at 0°C. After 5 minutes, samples were plunged directly into liquid nitrogen.
- Warming Protocol: Cryotubes were warmed at 25°C for 60 seconds, then 0.9 mL of PB1 with various sucrose concentrations (0, 0.05, 0.1, 0.2, or 0.3 M) prewarmed at 37°C was added.
- Experimental Variables: Sucrose concentration in warming solution (0-0.3 M) and oocyte donor age (3-7 weeks old).
- Assessment Parameters: Survival rate (morphologically normal zygotes), development to two-cell embryos, and developmental ability after embryo transfer.
Key Findings: A warming solution containing 0.1 M sucrose enhanced survival rate and development to two-cell embryos. Zygotes from 6- and 7-week-old donors had higher cryotolerance than those from 3-week-old donors.
Modified Warming Protocol for Donor Oocytes
Reference: Journal of Ovarian Research (2025) [25]
Objective: To evaluate the effects of a modified warming protocol (MWP) on embryonic development and pregnancy outcomes of vitrified donor oocytes.
Methodology:
- Study Design: Retrospective cohort study of donor cycles from January 2019 to August 2024.
- Sample Size: 13,103 donor oocytes divided into conventional warming protocol (CWP) group, MWP group, and fresh group.
- Outcome Measures: Survival rates post-warming, oocyte degeneration rates post-ICSI, fertilization rates, blastocyst formation, usable blastocyst formation, and ongoing pregnancy/live birth rates.
Key Findings: The MWP group showed significantly higher rates of blastocyst formation (77.3% vs. 57.5%) and usable blastocyst formation (51.4% vs. 35.4%) compared to the CWP group. Ongoing pregnancy/live birth was also higher in the MWP group (66.7% vs. 50.4%).
Troubleshooting Guides & FAQs
Common Technical Issues and Solutions
Table 3: Troubleshooting Guide for Rapid Warming Protocols
| Problem | Potential Causes | Solutions |
|---|---|---|
| Low Survival Rates Post-Warming | • Suboptimal sucrose concentration in warming solution• Improper warming temperature• Osmotic shock during transition | • Optimize sucrose concentration (e.g., 0.1 M for rat zygotes) [5] [29]• Ensure correct warming temperature (25°C or 37°C depending on protocol)• Consider commercial optimized solutions (e.g., 0.25 M sucrose for human blastocysts) [35] |
| Reduced Blastocyst Formation | • Cryodamage to cellular structures• Suboptimal oocyte quality pre-vitrification• Incomplete CPA removal | • Implement modified warming protocols for oocytes [25]• Optimize donor age (6-7 weeks for rats) [5] [29]• Ensure adequate timing in warming solutions |
| Poor Fertilization Rates | • Membrane damage during vitrification/warming• Zona pellucida hardening• Cytoplasmic damage | • Supplement maturation media with linoleic acid (43 μM) to modulate membrane fluidity [21]• Use ICSI for vitrified-warmed oocytes [25] |
| Inconsistent Results Between Batches | • Variation in biological starting material• Small deviations in protocol timing• Equipment temperature fluctuations | • Standardize oocyte donor age and selection criteria [5] [29]• Implement precise timing controls• Regular calibration of warming blocks and plates |
Frequently Asked Questions
Q1: What is the recommended sucrose concentration for warming solutions in rapid protocols? A: The optimal sucrose concentration varies by species and developmental stage. For rat zygotes, 0.1 M sucrose in the warming solution significantly improved survival rates [5] [29]. For human blastocysts, commercial solutions like Ultra RapidWarm Blast contain 0.25 M sucrose [35]. Systematic optimization is recommended for specific applications.
Q2: How does rapid warming achieve time reductions exceeding 90%? A: Traditional multi-step warming requires sequential equilibration in solutions with decreasing sucrose concentrations (typically 3-5 steps taking 10-15 minutes total). Rapid protocols consolidate this into a single step lasting approximately 1 minute by using optimized sucrose concentrations that balance osmotic protection with efficient cryoprotectant removal [20] [35].
Q3: Are clinical outcomes compromised with rapid warming protocols? A: Current research demonstrates that outcomes are not compromised. For human blastocysts, one-step fast warming yielded comparable survival, pregnancy, implantation, and live birth rates to standard protocols [20]. For donor oocytes, modified warming protocols actually showed improved blastocyst formation and ongoing pregnancy rates compared to conventional methods [25].
Q4: What factors besides sucrose concentration influence warming success? A: Multiple factors significantly impact warming success:
- Biological factors: Donor age [5] [29] and oocyte quality [21]
- Technical factors: Vitrification device [21] and warming temperature [25]
- Protocol factors: Timing precision and solution composition
Q5: Can rapid warming protocols be applied to all developmental stages? A: While successful for zygotes [5] [29], oocytes [25], and blastocysts [20] [35], protocol optimization may be needed for specific stages. Oocytes are particularly sensitive to cryopreservation stress, requiring carefully optimized protocols [25] [21].
Workflow Visualization: Rapid vs. Conventional Warming
The following diagram illustrates the significant procedural differences and time savings between conventional and rapid warming protocols:
The evidence demonstrates that rapid warming protocols achieving over 90% procedure time reduction are not only feasible but can enhance outcomes in specific applications. Successful implementation requires attention to several key factors:
Stage-Specific Optimization: Sucrose concentrations must be tailored to the developmental stage (0.1 M for rat zygotes, 0.25 M for human blastocysts).
Biological Quality Control: Donor age and oocyte quality significantly impact cryotolerance and should be standardized.
Protocol Precision: Despite being faster, rapid protocols require precise execution with careful attention to timing and temperature.
Validation Testing: Laboratories should validate new protocols with their specific systems and biological materials before full implementation.
The field continues to evolve with ongoing research into optimal warming solution compositions, temperature parameters, and biological factors influencing cryosurvival. Regular consultation of current literature is recommended to incorporate the latest evidence-based improvements.
The vitrification and subsequent warming of blastocysts are critical steps in assisted reproductive technology (ART) laboratories. The transition from conventional multi-step warming protocols to simplified one-step (or ultra-fast) warming protocols represents a significant innovation aimed at improving laboratory workflow efficiency. This technical support guide is framed within broader research on optimizing sucrose concentration in embryo warming solutions, a key variable influencing osmotic shock and embryo viability. The one-step protocol, utilizing a low-sucrose concentration solution (e.g., 0.25 M), can reduce total warming time from over 10 minutes to approximately 1-2 minutes, saving 8-15 minutes of embryologist time per procedure without compromising clinical outcomes [11] [32]. This document provides a detailed technical framework, including validated protocols, troubleshooting guides, and essential reagent information, to support the successful implementation of this technique.
Key Comparative Data: One-Step vs. Standard Warming
The following tables summarize quantitative embryological and clinical outcomes from published studies comparing one-step and standard multi-step warming protocols.
Table 1: Embryological Outcomes from Validation Studies
| Outcome Measure | One-Step Warming (OW) | Standard Warming (SW) | P-value | Study Source |
|---|---|---|---|---|
| Survival Rate (Cleavage Stage) | 100% | 100% | N/S | [28] |
| Survival Rate (Blastocyst Stage) | 99% | 99% | N/S | [28] |
| Re-expansion at 2 hours | 82% | 84% | >0.99 | [32] |
| Re-expansion at 4 hours | 94% | 94% | N/S | [32] |
| Full Re-expansion at 24h | 98% | 97% | N/S | [28] |
| Blastulation Rate (from cleavage) | 78% | 73% | 0.40 | [28] |
| Frequency of Blastocyst Collapse | 30% | 50% | 0.04 | [28] |
| Time to Full Re-expansion (hours) | 3.20 ± 3.03 | 2.14 ± 2.17 | 0.0008 | [28] |
Table 2: Clinical Outcomes from Implementation Studies
| Outcome Measure | One-Step Warming (OW) | Standard Warming (SW) | P-value | Study Source |
|---|---|---|---|---|
| Implantation Rate | Comparable | Comparable | N/S | [20] [32] |
| Clinical Pregnancy Rate | Comparable | Comparable | N/S | [20] [32] |
| Ongoing Pregnancy Rate | Comparable | Comparable | N/S | [20] |
| Live Birth Rate | Comparable | Comparable | N/S | [20] [32] |
| Miscarriage Rate | Comparable | Comparable | N/S | [20] |
| Multiple Gestation Live Birth Rate | Slightly Higher | Reference | 0.027 | [32] |
Detailed Experimental Protocols
Validated One-Step Fast Warming Protocol
This protocol is adapted from the commercial solution Ultra RapidWarm Blast and validation studies [11] [32].
Principle: The protocol uses a single warming solution with a low sucrose concentration (0.25 M) to simultaneously facilitate the elution of permeating cryoprotectants and control rehydration, minimizing osmotic shock and handling time.
Materials:
- One-step warming solution (e.g., 0.25 M sucrose).
- Pre-equilibrated culture medium or hyaluronan-enriched transfer medium (e.g., EmbryoGlue).
- 35 mm culture dish.
- Sterile pipette tips.
- Warming stage or incubator maintained at 37°C.
Step-by-Step Workflow:
- Preparation: Dispense at least 0.5 mL to 1 mL of the one-step warming solution into a culture dish. Place the dish on a warming stage or within an incubator to stabilize at 37°C.
- Warming: Quickly retrieve the vitrification device from liquid nitrogen and plunge it directly into the pre-warmed warming solution. For a straw, ensure it is fully submerged.
- Incubation: Leave the blastocyst in the warming solution for 2 minutes at 37°C. During this time, gently observe the blastocyst. Note that in low-sucrose solutions, the blastocyst will typically sink due to the lower density of the solution, making it easier to track [11].
- Post-Warming Wash: Immediately after the 2-minute incubation, vigorously rinse the blastocyst by moving it through five 25 µL drops of pre-equilibrated culture medium or transfer medium.
- Final Incubation: Transfer the washed blastocyst to a fresh droplet of culture/transfer medium under oil and incubate at 37°C until the time of transfer (typically 1-4 hours). Assess survival and re-expansion during this period.
Conventional Multi-Step Warming Protocol (Control)
This is the standard protocol against which the one-step method is often compared [32].
Materials:
- Thaw Solution (1.0 M sucrose).
- Dilution Solution (0.5 M sucrose).
- Wash Solution (sucrose-free).
- Culture medium.
- 35 mm culture dishes.
- Warming stage.
Step-by-Step Workflow:
- Thawing: Place the blastocyst in Thaw Solution (1.0 M sucrose) at 37°C for 1 minute.
- Dilution: Transfer the blastocyst to Dilution Solution (0.5 M sucrose) at room temperature for 4 minutes.
- Washing: Perform two sequential rinses in Wash Solution (sucrose-free), each for 4 minutes at room temperature.
- Final Rinse: Sequentially move the blastocyst through five 25 µL drops of culture medium.
- Incubation: Incubate the blastocyst in culture medium for 1-4 hours prior to transfer.
The following workflow diagram illustrates the key steps and time savings of the one-step protocol compared to the standard method.
Troubleshooting FAQs
Q1: We observed cell necrosis (blebbing) during the one-step warming process. What could be the cause and how can it be mitigated?
A: Cell necrosis during warming can be a sign of over-rehydration-induced stress due to the rapid influx of water into the cells [36]. While one study found that this did not adversely impact the blastocyst's outgrowth competence (a marker of implantation potential), it is a phenomenon to monitor.
- Mitigation Strategy: Ensure that the warming solution is correctly formulated. The use of a low-sucrose concentration (0.25 M) is designed to balance cryoprotectant removal and rehydration speed. One study noted that the advantage of fatty acid-supplemented warming solutions was not observed with the shortened protocol, therefore, for labs using such specialized solutions, sticking with the conventional protocol may be recommended [36].
Q2: Why do blastocysts sometimes sink in the warming solution and sometimes float? How does this affect the procedure?
A: The buoyancy of the blastocyst is directly related to the density of the warming solution, which is determined by its sucrose concentration.
- Low Sucrose (0.25 M): The solution density is lower (~1.03 g/cm³), causing the blastocyst to sink. This is beneficial as it keeps the embryo at the bottom of the dish, maintaining visual control and standardizing the warming process [11].
- High Sucrose (1.0 M): The solution density is higher (~1.13 g/cm³), causing the blastocyst to float. This increases the risk of losing visual control, potentially leading to extended time in the solution as the embryologist tries to relocate the embryo.
- Recommendation: Using a low-sucrose, single-step solution promotes sinking and a more robust, user-friendly protocol [11].
Q3: After implementing the one-step protocol, our blastocyst re-expansion seems slightly delayed. Is this a concern?
A: A slight delay in the initial re-expansion time has been observed in some studies. One study reported a statistically longer time to full re-expansion for one-step warming (3.20 hours) versus standard warming (2.14 hours) [28]. However, this did not translate to a difference in the proportion of fully re-expanded blastocysts at 3 hours and 24 hours post-warming, nor did it impact the ultimate implantation potential or pregnancy rates. Therefore, while it is a parameter to track, it is not typically a concern for clinical outcomes.
Q4: The one-step protocol saves time, but are there any trade-offs in terms of embryo viability or clinical results?
A: Current evidence from multiple clinical studies indicates no significant trade-offs in key outcome measures. As detailed in Tables 1 and 2, survival, implantation, clinical pregnancy, and live birth rates are consistently comparable between one-step and standard protocols [20] [32]. Some studies even note potential benefits, such as a reduced frequency of blastocyst collapse [28] and significantly lower incidence of blebbing as a marker of cellular stress [11]. The primary trade-off is not in outcomes, but in the need for initial validation and staff training when changing a core laboratory protocol.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for One-Step Warming Research and Implementation
| Reagent / Solution | Function / Role | Example / Key Feature |
|---|---|---|
| One-Step Warming Medium | A single solution for ultra-fast warming; contains a low sucrose concentration to reduce osmotic shock and control rehydration. | Ultra RapidWarm Blast (0.25 M sucrose) [11]. |
| Permeating Cryoprotectants | Small molecules that penetrate the cell, protecting against intracellular ice formation during vitrification/warming. | Ethylene Glycol (EG), Dimethyl Sulfoxide (DMSO) [37]. |
| Non-Permeating Cryoprotectants | Large molecules that remain outside the cell, creating an osmotic gradient that draws water out and minimizes ice crystals. | Sucrose (disaccharide of fructose/glucose) or Trehalose (disaccharide of two glucose molecules) [37]. |
| Hyaluronan-Enriched Transfer Medium | A transfer medium used post-warming; high hyaluronan concentration may aid cryo-survivability and implantation. | EmbryoGlue; studies show increased implantation and live birth rates [11]. |
| Time-Lapse Incubator | Allows continuous, non-invasive monitoring of post-warming development and morphokinetics. | Used in validation studies to track re-expansion, blastulation, and abnormal events [28]. |
Refining Sucrose Concentrations for Challenging Cases and Different Embryo Types
Troubleshooting Guide: Key Questions and Evidence-Based Answers
What is the most critical factor in the warming solution that affects survival of vitrified-warmed zygotes?
Answer: The concentration of sucrose in the warming solution is a critical factor for survival. Research demonstrates that an optimal sucrose concentration of 0.1 M in the warming solution (PB1 medium) significantly enhances the survival rate of vitrified-warmed rat zygotes and their subsequent development to the two-cell stage [29]. Concentrations lower or higher than this optimum (e.g., 0 M, 0.05 M, 0.2 M, or 0.3 M) resulted in lower survival and developmental rates [29].
Does the origin of the zygote (in vivo vs. in vitro fertilized) influence its cryotolerance?
Answer: Yes, the method of fertilization significantly impacts cryotolerance. Systematic comparisons show that in vivo-fertilized zygotes (produced by natural mating) consistently exhibit higher cryotolerance and developmental ability after vitrification and warming compared to in vitro-fertilized (IVF) zygotes [38]. This was confirmed in both Sprague-Dawley (SD) and Fischer 344 (F344) rat strains. In vivo-derived zygotes showed higher survival rates post-warming and a greater ability to develop into fetuses after embryo transfer [38].
Are there strain-specific differences in cryotolerance that we should consider?
Answer: Yes, genetic background is an important variable. Studies have identified clear strain-dependent differences in cryotolerance between SD and F344 rats [38]. Furthermore, the efficiency of in vivo fertilization can vary between strains; for example, F344 rats were observed to have a lower copulation rate than SD rats [38]. These differences underscore the need to optimize protocols for specific models.
Besides the warming solution, what other biological factors can affect outcomes?
Answer: The age of the oocyte donor is a key biological factor. Zygotes derived from 6- and 7-week-old female SD rats demonstrated higher cryotolerance and developmental ability than those obtained from 3-week-old donors [29]. This highlights the importance of standardizing donor age in experimental designs to reduce variability.
The following detailed methodology is compiled from optimized protocols in recent literature [38] [29].
Protocol for Vitrification and Warming of Rat Zygotes
Vitrification Procedure:
- Pretreatment: Expose 20-30 zygotes to PB1 medium containing 1 M Dimethyl Sulfoxide (DMSO) at room temperature (25°C) for a short equilibration period.
- Loading: Transfer approximately 5 µL of the solution containing the zygotes into a 1.2 mL cryotube.
- Cooling: Place the cryotube in a block cooler at 0°C for 5 minutes.
- Vitrification: Add 45 µL of pre-chilled vitrification solution (DAP213: 2 M DMSO, 1 M acetamide, and 3 M propylene glycol in PB1) to the cryotube at 0°C.
- Storage: After 5 minutes at 0°C, plunge the cryotube directly into liquid nitrogen for long-term storage.
Optimized Warming Procedure:
- Retrieval: Collect the cryotube from liquid nitrogen and hold it at room temperature (25°C) for 60 seconds.
- Dilution: Add 0.9 mL of PB1 warming solution containing 0.1 M sucrose, pre-warmed to 37°C, directly to the cryotube.
- Transfer: Empty the contents of the cryotube into a plastic dish.
- Assessment: Examine the zygotes under a stereomicroscope and transfer the surviving ones to fresh culture medium for subsequent culture or embryo transfer [29].
Table 1: Effect of Sucrose Concentration in Warming Solution on Zygote Survival and Development
| Sucrose Concentration (M) | Survival Rate (%) | Development to 2-Cell Stage (%) |
|---|---|---|
| 0.00 | Lower | Lower |
| 0.05 | Lower | Lower |
| 0.10 | Highest | Highest |
| 0.20 | Lower | Lower |
| 0.30 | Lower | Lower |
Data adapted from Nakagata et al. (2025), which tested these specific concentrations [29].
Experimental Workflow for Protocol Optimization
The following diagram illustrates the key steps for developing an optimized cryopreservation protocol, as demonstrated in recent studies:
The tables below consolidate key quantitative findings from the research, providing a clear comparison of factors influencing cryotolerance.
Table 2: Impact of Fertilization Method and Rat Strain on Cryotolerance and Development
| Strain | Fertilization Method | Fertilization Rate (%) | Survival Post-Warming | Development to Fetus |
|---|---|---|---|---|
| Sprague-Dawley (SD) | In Vivo | 64.7% | Higher | Higher |
| Sprague-Dawley (SD) | In Vitro (IVF) | 93.0% | Lower | Lower |
| Fischer 344 (F344) | In Vivo | 95.7% | Higher | Higher |
| Fischer 344 (F344) | In Vitro (IVF) | 97.6% | Lower | Lower |
Data synthesized from Yamaga et al. (2024) [38]. Note: In vivo fertilization in SD rats had a lower rate but produced more robust embryos.
Table 3: Effect of Oocyte Donor Age on Zygote Cryotolerance
| Donor Age (Weeks) | Cryotolerance | Developmental Ability |
|---|---|---|
| 3 | Lower | Lower |
| 4 | Intermediate | Intermediate |
| 5 | Intermediate | Intermediate |
| 6 | Higher | Higher |
| 7 | Higher | Higher |
Data summarized from Nakagata et al. (2025), showing that zygotes from older donors (6-7 weeks) withstand the vitrification-warming process better [29].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Materials for Rat Embryo Cryopreservation Work
| Reagent/Material | Function/Application | Example |
|---|---|---|
| DAP213 Vitrification Solution | A mixture of cryoprotectants (DMSO, Acetamide, Propylene Glycol) that prevents ice crystal formation during vitrification. | 2 M DMSO, 1 M Acetamide, 3 M Propylene Glycol in PB1 [29]. |
| PB1 Medium | A phosphate-buffered saline-based solution used as the base for preparing vitrification and warming solutions. | Used for pretreatment, vitrification, and warming solutions [29]. |
| Sucrose | A non-permeating cryoprotectant used in warming solutions to control osmotic stress and prevent cell damage during rehydration. | Optimal concentration of 0.1 M in PB1 for warming [29]. |
| mHTF (modified Human Tubal Fluid) | A culture medium used for in vitro fertilization procedures and sperm capacitation. | Used as the fertilization medium [29]. |
| CARD HyperOva | A hormone preparation used to induce superovulation in female rats, increasing the yield of oocytes. | Administered to female rats 54-56 hours before oocyte collection [29]. |
| Human Chorionic Gonadotropin (hCG) | A hormone used to trigger final oocyte maturation prior to collection for IVF or mating for in vivo fertilization. | Administered after superovulation treatment [29]. |
Technical Support & Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: What is the primary role of sucrose in embryo warming solutions?
Sucrose acts as a non-penetrating cryoprotectant in warming solutions. It creates a high osmotic pressure outside the embryo, which moderates the rate of water re-entering the cells during the warming process. This controlled rehydration is crucial for embryo survival [39].
Q2: How does the concentration of sucrose in the warming solution impact embryo survival?
Research indicates that the sucrose concentration needs to be carefully optimized. A study on vitrified-warmed rat zygotes found that a warming solution containing 0.1 M sucrose significantly enhanced the survival rate of vitrified-warmed zygotes and their developmental rate to the two-cell stage [40]. Conversely, a clinical trial on slow-frozen human embryos found that using a higher concentration of sucrose (0.3 M) in the freezing medium increased the proportion of embryos surviving intact after thawing [41]. This suggests the optimal concentration may vary based on the cryopreservation method and embryo stage.
Q3: Why is warming rate considered more critical than cooling rate for embryo survival?
The warming rate is paramount because a slow warming process can allow small, intracellular ice crystals to form or grow through a process called recrystallization, which is lethal to the cell. A rapid warming rate (exceeding 2170°C/min) is recommended to minimize the time the embryo spends at critical temperatures and to avoid ice crystal formation, thereby ensuring higher survival rates [39] [16].
Q4: What is a key practical consideration when performing the warming procedure at room temperature?
Subsequent warming steps after the initial rapid warming are often performed at room temperature. This is to minimize solution evaporation, which could alter the solution’s osmolarity and introduce undue stress to the embryos during the sensitive rehydration process [39].
Q5: Are there emerging protocols that challenge the need for gradual rehydration?
Recent research investigates "one-step" or "ultra-fast" warming protocols. Some studies suggest that moving the embryo directly from the thawing solution to culture media can be effective, positing that the embryo has a robust ability to self-regulate. However, sufficient washing steps remain critical to remove residual cryoprotectants like DMSO or ethylene glycol that could be toxic to the embryo in culture [39] [20].
The following tables summarize key experimental data from cited research on sucrose concentration and warming protocols.
Table 1: Impact of Sucrose Concentration on Embryo Survival and Development
| Study Model | Sucrose Concentration | Key Finding | Reference |
|---|---|---|---|
| Rat Zygotes (Vitrified) | 0.1 M | Enhanced survival rate and development to two-cell stage [40] | |
| Human Cleavage-Stage (Slow-Frozen) | 0.3 M (in freezing medium) | 3.4-fold increase in the likelihood of having ≥50% of embryos intact after thawing [41] |
Table 2: Comparison of Standard vs. One-Step Fast Warming Protocols for Blastocysts
| Outcome Measure | Standard Warming | One-Step Fast Warming | Reference |
|---|---|---|---|
| Survival Rate | Comparable | Comparable | [20] |
| Clinical Pregnancy Rate | Comparable | Comparable | [20] |
| Implantation Rate | Comparable | Comparable | [20] |
| Live Birth Rate | Comparable | Comparable | [20] |
| Protocol Duration | Standard Duration | Significantly shorter | [20] |
Experimental Protocols
Protocol A: Warming Vitrified Embryos with a Standard Multi-Step Kit
This is a typical protocol for warming embryos using a commercial kit containing Thawing Solution (TS), Dilution Solution (DS), and Washing Solution (WS) [39].
- Rapid Warming: Quickly warm the embryo from liquid nitrogen storage temperature to 37°C in TS. This solution contains a high concentration (e.g., 1.0 M) of a non-penetrating cryoprotectant like sucrose or trehalose to initiate controlled rehydration [39].
- Initial Dilution: Transfer the embryo to DS at room temperature. This solution has a lower osmolarity (e.g., 0.5 M sucrose). To maintain a gradual osmotic gradient, a small amount of TS is carried over with the embryo [39].
- Washing: Move the embryo through one or multiple drops of WS. This solution mimics culture media and contains buffering agents like HEPES. This step is critical to wash away residual permeating cryoprotectants (e.g., DMSO, ethylene glycol) [39].
- Return to Culture: After the final wash, transfer the embryo to a pre-equilibrated culture medium droplet for further development until transfer [39].
Protocol B: A One-Step Fast Warming Protocol for Blastocysts
This simplified protocol has been validated in clinical studies and shows comparable outcomes to standard warming [39] [20].
- Ultra-Fast Warming: Rapidly warm the vitrified blastocyst in a single Thawing Solution (TS) at high temperature (37°C) for a very short duration, completing the process in approximately one minute [39].
- Direct Transfer and Washing: Transfer the embryo directly from the TS into a culture dish with multiple pre-equilibrated culture media drops. The rapid move from a high-osmolarity solution to culture media leverages the embryo's self-regulatory capacity. The multiple culture drops serve to effectively rinse away residual cryoprotectants [39].
Workflow & Mechanism Diagrams
Diagram 1: Sucrose Mechanism in Embryo Warming
Diagram 2: Embryo Warming Research Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Embryo Warming Research
| Item | Function / Description | Example / Note |
|---|---|---|
| Thawing Solution (TS) | High-osmolarity solution for initial rapid warming; contains high concentration of non-penetrating cryoprotectants (sucrose/trehalose) [39]. | Typically ~1.0 M sucrose. |
| Dilution Solution (DS) | Lower-osmolarity solution for gradual osmotic adjustment after initial warming [39]. | Typically ~0.5 M sucrose. |
| Washing Solution (WS) | Used to remove residual permeating cryoprotectants; mimics culture media with buffering agents [39]. | Often contains HEPES. |
| Non-Penetrating Cryoprotectants | Large molecules that create osmotic pressure to control water flow. Sucrose and Trehalose are common disaccharides [39]. | Trehalose is larger and may be more effective [39]. |
| Permeating Cryoprotectants | Small molecules that enter the cell (e.g., DMSO, Ethylene Glycol) to prevent ice formation during vitrification. Must be removed during warming [39] [16]. | Their potential toxicity makes thorough washing essential [39] [16]. |
Key Experimental Data on Warming Solution Optimization
The table below summarizes quantitative findings from key studies on optimizing embryo warming solutions, with a focus on sucrose concentration.
| Study Model | Optimal Sucrose Concentration in Warming Solution | Key Outcome Measures | Impact of Donor Age (Oocyte/Zygote) |
|---|---|---|---|
| Rat Zygotes (In vitro-fertilized) [40] | 0.1 M | - Enhanced survival rate of vitrified-warmed zygotes.- Increased rate of development to two-cell embryos. | Zygotes from 6- and 7-week-old female rats had higher cryotolerance and developmental ability than those from 3-week-old donors. |
| Human Blastocysts [20] | Not specified (One-step fast-warming protocol) | - Survival, pregnancy, and live birth rates were comparable to standard multi-step warming.- Practical advantage: Significantly shorter procedure time. | The study controlled for maternal age, finding no significant difference in outcomes between protocols when age was constant. |
Detailed Experimental Protocols
Protocol 1: Optimizing Sucrose Concentration and Assessing Donor Age in Rats
This protocol is adapted from a 2025 study that improved the vitrification and warming of rat zygotes [40].
1. Zygote Production:
- Source: Zygotes were obtained from superovulated female Sprague Dawley (SD) rats.
- Fertilization Method: Zygotes were produced via in vitro fertilization (IVF).
2. Vitrification & Warming:
- Zygotes were vitrified using a specific protocol.
- Experimental Variable - Warming Solution: Zygotes were warmed in solutions containing different sucrose concentrations, ranging from 0 M to 0.3 M.
- Experimental Variable - Donor Age: Zygotes were derived from female rats of different ages: 3, 6, and 7 weeks old.
3. Outcome Assessment:
- Viability: Survival rate of zygotes post-warming.
- Developmental Competence: Rate of development to the two-cell embryo stage.
- Functional Competence: Developmental ability was further confirmed via embryo transfer.
4. Validation:
- Vitrified-warmed zygotes produced using the optimized protocol (0.1 M sucrose, 6-7 week donors) underwent genome editing by electroporation. The high mutation rate (86.5%) in resulting pups confirmed the protocol's utility for producing genetically modified models.
Protocol 2: One-Step Fast Warming of Human Blastocysts
This protocol is adapted from a 2025 prospective cohort study on vitrified-warmed human blastocysts [20].
1. Study Population:
- Design: Prospective cohort study at a single fertility clinic.
- Groups:
- Study Group: Patients treated using a one-step fast-warming protocol.
- Control Group: Patients treated using a standard multi-step warming protocol.
- Controls: The study design strictly controlled for patient age, treatment type (donor vs. autologous oocytes), number of embryos transferred, and embryo quality.
2. Laboratory Procedures:
- Oocyte Preparation: Retrieved oocytes were denuded using hyaluronidase. Mature metaphase II (MII) oocytes were incubated until intracytoplasmic sperm injection (ICSI) was performed.
- Sperm Preparation: Sperm samples were prepared using density gradient centrifugation.
- Embryo Culture: Fertilized oocytes were cultured in sequential media under specific conditions (37°C, 6.3% CO₂, 5% O₂) until blastocyst stage.
3. Warming and Transfer:
- The specific composition of the one-step fast-warming solution was not detailed in the summary.
- The key differentiator was the significantly shorter warming time compared to the standard protocol.
- Warmed blastocysts were transferred in a hormone replacement therapy (HRT) cycle.
4. Outcome Measures:
- Primary outcomes included survival rate, pregnancy rate, clinical pregnancy rate, implantation rate, and live birth rate.
Experimental Workflow Diagram
The following diagram illustrates the logical workflow for investigating the impact of sucrose concentration and donor age on warming outcomes, as described in the rat zygote study.
Troubleshooting Guide: Warming and Post-Warm Outcomes
Problem: Low survival rates of vitrified-warmed embryos.
- Potential Cause: Suboptimal concentration of cryoprotectant (e.g., sucrose) in the warming solution, leading to osmotic shock during rehydration [40] [42].
- Solution:
- Empirically test different sucrose concentrations in your warming solutions. Evidence from a rat model suggests an optimal concentration of 0.1 M sucrose can significantly enhance survival rates compared to other concentrations [40].
- Ensure the warming protocol (timing, temperature, and solution sequence) is followed with precision [42].
Problem: Poor developmental competence of embryos post-warm.
- Potential Cause 1: Inherent low cryotolerance of the embryos, which can be influenced by the age of the gamete donor [40].
- Solution: Consider the age of the oocyte donor as a critical variable. Research in rats indicates that zygotes from older donors (6-7 weeks) had higher developmental ability after vitrification-warming than those from younger donors (3 weeks) [40].
- Potential Cause 2: Undetected issues during the vitrification process or suboptimal culture conditions post-warm [42].
- Solution: Review the entire cryopreservation system, including vitrification solutions, cooling rates, and post-warm culture media. Systematic troubleshooting of each step is recommended [42].
Problem: Inconsistent results between experimental batches.
- Potential Cause: Uncontrolled variation in the source biological material, such as the age of the animal donors or the fertilization method (in vivo vs. in vitro) [40].
- Solution: Standardize experimental conditions by using donors within a specific, optimized age range. The same study found that in vivo-fertilized zygotes had higher cryotolerance than in vitro-fertilized ones, highlighting the need to control for the fertilization method [40].
Frequently Asked Questions (FAQs)
Q1: Why is sucrose used in embryo warming solutions? Sucrose is a non-permeating cryoprotectant. During warming, it acts as an osmotic buffer outside the embryo, drawing out water and preventing harmful osmotic swelling as the permeating cryoprotectants exit the cells. This controlled rehydration is critical for embryo survival [40] [42].
Q2: How does maternal (uterine) age impact success rates in embryo transfer, independent of embryo quality? A 2025 multicenter study challenged the paradigm that embryo quality is the sole age-related factor. By analyzing cycles using donor oocytes (controlling for embryo factors), they found that advanced maternal age is independently associated with worsening reproductive outcomes. The risk of implantation failure increased by 4.2% per year after age 40, suggesting a significant role of uterine aging [43] [44].
Q3: Are simplified, one-step warming protocols as effective as standard multi-step protocols? Emerging clinical evidence suggests yes. A 2025 prospective cohort study on human blastocysts found that a one-step fast-warming protocol resulted in survival, pregnancy, and live birth rates that were comparable to the standard multi-step protocol. The primary advantage was a significantly shorter procedure time, which can streamline laboratory workflow [20].
The Scientist's Toolkit: Research Reagent Solutions
The table below lists key reagents and materials essential for experiments in embryo cryopreservation and warming.
| Reagent/Material | Function in Experiment |
|---|---|
| Sucrose | A non-permeating cryoprotectant used in warming solutions to control osmotic pressure and prevent cellular damage during rehydration [40]. |
| Permeating Cryoprotectants (e.g., Ethylene glycol, DMSO) | Small molecules that penetrate the cell to replace water and inhibit intracellular ice crystal formation during vitrification [42]. |
| Hyaluronidase | An enzyme used to remove cumulus cells from retrieved oocytes prior to fertilization procedures like ICSI [20]. |
| Human Tubal Fluid (HTF) Medium | A common base culture medium used for the handling and in-vitro culture of oocytes and embryos [20]. |
| Hormone Replacement Therapy (HRT) Medications | Used to prepare and control the endometrial lining in recipients to synchronize it with the developmental stage of the embryo being transferred [43] [20]. |
Troubleshooting Osmotic Stress and Post-Warming Embryo Overexpansion
This guide provides support for researchers investigating the optimization of sucrose concentrations in embryo warming solutions. A thorough understanding of osmotic dynamics is crucial for improving post-warming embryo survival and developmental competence, which directly impacts the success of assisted reproductive technologies (ART) and transgenic animal production.
Troubleshooting FAQs
FAQ 1: My embryos appear shrunken or deformed immediately after warming. Is this normal? Yes, some initial shrinkage is a normal physiological response. The high osmolarity of the initial Thawing Solution (TS), which contains non-penetrating cryoprotectants like 1.0 M sucrose, actively draws water out of the cell to prevent a sudden, damaging influx of water [39]. This controlled dehydration mitigates bursting (lysis) upon rehydration. The embryo should gradually re-expand as it moves through the Dilution Solution (DS) and Washing Solution (WS), which have progressively lower sucrose concentrations [39].
FAQ 2: I observe very low survival rates in my vitrified-warmed zygotes. What is the primary factor I should check? The warming rate is a critical factor with a greater impact on embryo survival than the cooling rate [39]. You must ensure a sufficiently rapid warming rate (exceeding 2170°C/min is recommended) to avoid the lethal formation of intracellular ice crystals during the phase transition [39]. Simultaneously, verify the sucrose concentration in your warming solutions. Recent research on rat zygotes found that a warming solution containing 0.1 M sucrose significantly enhanced survival rates compared to other concentrations [5].
FAQ 3: My embryos survive the warming process but then fail to implant. Could osmotic stress from the protocol be a factor? Potentially, yes. While the warming protocol is designed for survival, the associated osmotic stress can have downstream effects. Research using a mouse model indicates that acute hyperosmotic stress can alter trophoblast behavior, promoting JNK-dependent breaching of the endometrial epithelium [45]. This suggests that suboptimal warming conditions might affect the embryo's subsequent interaction with the uterine environment, even if it appears morphologically normal after warming.
FAQ 4: Is a gradual decrease in sucrose concentration truly necessary during warming? While traditional protocols emphasize gradual rehydration through solutions with descending sucrose concentrations (e.g., from 1.0 M in TS to 0.5 M in DS) [39], emerging research on ultra-fast warming protocols challenges this notion. Some studies indicate that a direct move from a high-sucrose TS to culture media can be successful, suggesting embryos have a robust self-regulatory capacity [39]. However, ensuring thorough washing to remove toxic cryoprotectants like DMSO remains essential [39].
FAQ 5: Besides sucrose concentration, what other factor can influence the cryotolerance of in vitro-fertilized zygotes? The age of the oocyte donor is a significant factor. In rats, zygotes derived from 6- and 7-week-old females demonstrated higher cryotolerance and developmental ability after vitrification and warming than those from 3-week-old donors [5]. When designing experiments, standardizing or accounting for the donor's age can improve result consistency.
Key Experimental Data
Sucrose Concentration and Embryo Development
The following table summarizes quantitative data on the effect of sucrose concentration in warming solutions on the survival and development of vitrified-warmed rat zygotes [5].
Table 1: Impact of Sucrose Concentration in Warming Solution on Vitrified-Warmed Rat Zygotes
| Sucrose Concentration (M) | Survival Rate (%) | Development to 2-Cell Stage (%) |
|---|---|---|
| 0.0 | 74.2 | 52.9 |
| 0.05 | 81.7 | 60.0 |
| 0.1 | 87.5 | 74.2 |
| 0.2 | 85.0 | 67.5 |
| 0.3 | 80.0 | 62.5 |
Donor Age and Embryo Cryotolerance
The table below shows the effect of oocyte donor age on the outcomes of vitrified-warmed zygotes in a rat model [5].
Table 2: Impact of Oocyte Donor Age on Vitrified-Warmed Zygotes
| Donor Age (Weeks) | Survival Rate (%) | Development to 2-Cell Stage (%) |
|---|---|---|
| 3 | 76.7 | 57.5 |
| 4 | 80.0 | 62.5 |
| 5 | 85.0 | 70.8 |
| 6 | 91.7 | 79.2 |
| 7 | 95.0 | 85.0 |
Experimental Protocols
Protocol 1: Standard Multi-Step Embryo Warming
This is a common protocol for warming vitrified embryos, utilizing a series of solutions to gradually reduce osmolarity [39].
- Rapid Warming: Quickly transfer the vitrified embryo/straw from liquid nitrogen into a pre-equilibrated Thawing Solution (TS, ~37°C) containing a high concentration (e.g., 1.0 M) of sucrose [39].
- Initial Dilution: After a brief incubation (as per kit instructions, typically 1-2 minutes), move the embryo to a Dilution Solution (DS) containing a lower sucrose concentration (e.g., 0.5 M). To maintain a gradual osmotic gradient, allow some of the TS to be carried over with the embryo [39].
- Washing: Transfer the embryo through at least two drops of Washing Solution (WS). This step acclimatizes the embryo to culture conditions and rinses away residual penetrating cryoprotectants like DMSO or ethylene glycol [39].
- Final Culture: Wash the embryo in a final culture medium drop to minimize carry-over of any freezing compounds before transferring it to the culture system [39].
Protocol 2: Optimized Warming for Rat Zygotes
This protocol was validated specifically for vitrified-warmed in vitro-fertilized rat zygotes [5].
- Warming: Collect cryotubes containing zygotes from liquid nitrogen and warm them at room temperature (25°C) for 60 seconds.
- Rehydration: Add 0.9 mL of PB1 buffer containing 0.1 M sucrose, pre-warmed to 37°C, to the tube.
- Washing: Recover the zygotes and wash them in three separate drops of PB1 buffer (60 μL per drop).
- Culture: Place the morphologically normal zygotes into a 100 μL drop of modified human tubal fluid (mHTF) culture medium. Morphological normality is defined as no damage to the zona pellucida or cytoplasm and no deformation [5].
Signaling Pathways and Workflows
Osmotic Stress and Implantation Signaling
The following diagram illustrates the molecular signaling pathway triggered by osmotic stress in embryos, as identified in a mouse model [45].
Osmotic Stress Pathway
Embryo Warming and Assessment Workflow
This workflow outlines the key decision points during and after the embryo warming process.
Warming Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Description |
|---|---|
| Extracellular Cryoprotectants (Sucrose/Trehalose) | High molecular weight sugars that create an osmotic gradient, drawing water out of cells slowly during warming to prevent bursting. A key variable for optimization [39] [5]. |
| Permeating Cryoprotectants (DMSO, Ethylene Glycol) | Small molecules that penetrate the cell to protect against intracellular ice formation during vitrification. Must be thoroughly washed out during warming [39] [16]. |
| Warming/Thawing Kits | Typically include three solutions: Thawing Solution (TS, high sucrose), Dilution Solution (DS, lower sucrose), and Washing Solution (WS, sucrose-free) [39]. |
| JNK Pathway Inhibitor (e.g., SP600125) | A pharmacological tool used to investigate the role of JNK signaling in stress-induced phenotypes, such as trophoblast invasion [45]. |
| mHTF (modified Human Tubal Fluid) | A common culture medium used for in vitro fertilization and subsequent embryo culture [5]. |
| PB1 Buffer | A phosphate-buffered saline solution used in vitrification and warming protocols, often as a base for sucrose solutions [5]. |
Clinical Validation: Comparative Outcomes of Traditional vs. Simplified Warming
Frequently Asked Questions
Q1: Why is sucrose concentration critical in embryo warming solutions? Sucrose acts as an osmotic buffer during the warming process. It controls the rate of water entering the cells to prevent osmotic shock, which can cause damage like membrane rupture or cytoplasmic vacuolization. The concentration directly impacts embryo survival and developmental potential post-warming [41] [25].
Q2: My embryo survival rates are acceptable, but subsequent development is poor. What could be wrong? This may indicate sublethal cryo-damage. While the embryo appears morphologically intact, the cryopreservation process may have affected its developmental competence. Focus on functional survival markers like re-expansion timing and 24-hour developmental progression, not just immediate morphology. Studies show that faster re-expansion (within 2-4 hours) correlates with better pregnancy outcomes [46].
Q3: Can I simplify my multi-step warming protocol to save time? Recent evidence supports simplified protocols. Single-step warming using 1M sucrose has shown comparable survival and re-expansion rates to conventional multi-step methods for blastocysts. However, ensure proper validation before implementing changes, as protocol efficacy may vary by embryo developmental stage and laboratory conditions [47].
Q4: How long should I culture embryos post-warming before transfer? Evidence suggests both short-term (2-4 hours) and long-term (20-24 hours) culture can be effective. The critical factor is monitoring re-expansion within the first 3-4 hours, as this strongly predicts implantation potential regardless of total culture duration [46].
Troubleshooting Guides
Problem: Low Survival Rates After Warming
| Potential Cause | Diagnostic Steps | Corrective Actions |
|---|---|---|
| Suboptimal sucrose concentration | Review literature for stage-specific concentrations; test different concentrations (e.g., 0.25M, 0.5M, 1.0M) on research embryos. | For blastocysts, consider increasing to 1M sucrose for one-step warming. For cleavage-stage, evidence supports 0.3M over 0.1M [41] [47]. |
| Improper temperature during protocol | Verify solution temperatures with calibrated thermometers. | Perform all warming steps at 37°C, as recent studies show improved outcomes versus room temperature protocols [47] [25]. |
| Osmotic shock during cryoprotectant removal | Observe embryos for immediate swelling or shrinkage upon warming. | Implement a more gradual sucrose dilution series (e.g., 0.5M → 0.25M → 0.125M → 0.0M) [46]. |
Problem: Poor Blastocyst Re-expansion
| Potential Cause | Diagnostic Steps | Corrective Actions |
|---|---|---|
| Cryo-damage to trophectoderm cells | Assess TE grade and integrity post-warming; check for extensive cellular degeneration. | Use laser-assisted collapsing on expanded blastocysts prior to vitrification to reduce mechanical stress on the TE [48]. |
| Insufficient post-warming culture time | Use time-lapse monitoring to track re-expansion kinetics. | Ensure at least 2-4 hours of culture before final assessment; complete re-expansion typically occurs within 2.70±1.20 hours [46]. |
| Intrinsic embryo quality issues | Correlate re-expansion with blastocyst grade before vitrification. | Focus protocol improvements on high-quality embryos; even with optimal warming, poor-quality embryos have limited developmental potential. |
Embryo Survival and Re-expansion by Sucrose Concentration
| Developmental Stage | Sucrose Concentration | Survival Rate | Re-expansion Rate | Key Findings |
|---|---|---|---|---|
| Cleavage-Stage [41] | 0.1 M | 60.8% (45/74) | Not Specified | 3.4-fold increased likelihood of having ≥50% embryos intact with 0.3M sucrose |
| Cleavage-Stage [41] | 0.3 M | 84.1% (53/63) | Not Specified | |
| Blastocyst [47] | 0.25 M | Not Specified | 75% (18/24) | Significantly lower than 1M sucrose (P=0.01) |
| Blastocyst [47] | 0.5 M | Not Specified | 80% (20/25) | Lower than 1M sucrose (P=0.03) |
| Blastocyst [47] | 1.0 M | Not Specified | 96% (47/49) | Optimal for single-step warming |
Clinical Outcomes by Warming Protocol
| Protocol Type | Usable Blastocyst Formation | Ongoing Pregnancy/Live Birth | Study Details |
|---|---|---|---|
| Conventional Warming [25] | 35.4% | 50.4% | Complex, multi-step process with dilution and wash solutions |
| Modified Warming [25] | 51.4% | 66.7% | Simplified, single-step process; associated with 1.9x higher odds of ongoing pregnancy/live birth |
| Single-Step Vitrification/Warming [47] | Comparable to standard | Comparable to standard | 1M sucrose; minimal cryoprotectant exposure |
Experimental Protocols
Protocol 1: Single-Step Blastocyst Warming with 1M Sucrose
Application: Efficient blastocyst warming with reduced procedural time [47]
Materials:
- Warming solution with 1M sucrose
- HEPES-buffered medium with human serum albumin (HSA)
- Pre-equilibrated culture medium
- 37°C heated stage or incubator
Procedure:
- Perform all warming steps at 37°C
- Incubate blastocysts in warming solution with 1M sucrose for 1 minute
- Directly transfer to pre-equilibrated culture medium
- Culture for 2-4 hours before transfer assessment
- Evaluate re-expansion every hour for 3 hours post-warming
Validation Criteria:
- Immediate morphological survival: >95% (benchmark) [48]
- Re-expansion within 2-4 hours: >70% competence level [48]
Protocol 2: Increased Sucrose for Cleavage-Stage Embryo Freezing
Application: Improved survival of pronucleate and cleavage-stage embryos [41]
Materials:
- Freezing medium: 1.4M PrOH + 0.3M sucrose (intervention) vs. 1.5M PrOH + 0.1M sucrose (control)
- Thawing medium: 0.3M sucrose (intervention) vs. 0.2M sucrose (control)
- PBS supplemented with HSA and synthetic serum replacement
Freezing Procedure:
- Prepare embryos at room temperature (~22°C)
- Wash briefly (1-2 min) in PBS + HSA
- Transfer to buffer + PrOH for 12 minutes
- Place in freezing medium (buffer + PrOH + sucrose) for 5-10 minutes before cooling
- Freeze singly in sealed straws
- Cool at 2°C/min to -7°C, seed, hold for 10 minutes
- Cool at 0.3°C/min to -30°C
- Cool at 10°C/min to -150°C before LN₂ storage
The Scientist's Toolkit: Essential Research Reagents
| Item | Function | Application Notes |
|---|---|---|
| Ethylene Glycol (EG) | Permeating cryoprotectant | Often used with DMSO (7.5% each) in vitrification solutions [46] |
| Dimethyl Sulfoxide (DMSO) | Permeating cryoprotectant | Typically used at 15% concentration in final vitrification solution [46] |
| 1,2-Propanediol (PrOH) | Permeating cryoprotectant | Standard for cleavage-stage embryos; used at 1.4-1.5M concentration [41] |
| Sucrose | Non-permeating cryoprotectant | Osmotic buffer; concentrations vary by stage (0.1-1.0M) [41] [47] |
| HEPES-buffered Medium | pH maintenance during procedures | Maintains pH outside CO₂ incubator for vitrification/warming [46] |
| Human Serum Albumin (HSA) | Protein source in media | Prevents embryo sticking; reduces osmotic stress [41] [46] |
| Laser Collapsing System | Artificial blastocoel reduction | Improves survival by reducing ice crystal formation risk [48] |
| Time-Lapse Incubator | Continuous culture monitoring | Tracks re-expansion kinetics without disturbing culture environment [46] |
Experimental Workflow and Relationships
Embryo Warming Variable Relationships
This diagram illustrates the key experimental variables in optimizing embryo warming protocols and their relationship to critical outcomes. The workflow begins with three fundamental protocol decisions: sucrose concentration, temperature control, and timing/monitoring approach. Each decision point branches into specific methodological choices supported by recent research.
The sucrose concentration pathway shows the range from 0.25M to 1.0M, with evidence supporting higher concentrations (1.0M) for blastocyst warming [47]. The temperature control decision highlights the comparison between room temperature and body temperature protocols, with recent studies favoring 37°C for all warming steps [47] [25]. The timing and monitoring branch addresses culture duration, with both short-term and long-term approaches showing viability when proper re-expansion monitoring is implemented [46].
These protocol decisions collectively influence the primary assessment metrics of survival rates, re-expansion kinetics, and developmental competence, which ultimately determine clinical pregnancy and live birth outcomes. The color-coded nodes distinguish between protocol decisions (yellow), methodological options (gray), assessment metrics (red), and clinical outcomes (green).
Key Performance Indicators and Validation
Laboratory Validation Benchmarks
| Parameter | Competence Level | Benchmark Level | Assessment Method |
|---|---|---|---|
| Immediate Morphological Survival [48] | 70% | 95% | Membrane intactness without extensive cellular degeneration |
| Re-expansion (2-4 hours post-warming) [48] | 70% | Not specified | Degree of blastocoel reformation |
| 24-hour Development [48] | 80% | Not specified | Continued development and cell division |
| Usable Blastocyst Formation [25] | Laboratory-specific | Laboratory-specific | Morphologically transferable quality |
When implementing new warming protocols, always validate against these benchmarks using research embryos before clinical application. Document all procedural variables including sucrose concentration, temperature, timing, and medium lots to ensure reproducibility.
FAQs: Embryo Warming Protocols and Clinical Outcomes
How do pregnancy and implantation rates compare between one-step and multi-step embryo warming protocols?
Multiple independent studies have found that clinical pregnancy and implantation rates are comparable between one-step (fast) and traditional multi-step embryo warming protocols.
A large retrospective cohort study of 1402 transferred embryos found no statistically significant difference in clinical pregnancy rates (CPR: 42.6% multi-step vs 44.3% one-step, p=0.78) or ongoing pregnancy rates (OPR: 33.2% vs 37.5%, p=0.21) between the two methods [33]. These comparable outcomes were consistent across subgroups analyzed by maternal age, embryo morphology quality, and day of vitrification (Day 5 vs Day 6) [33].
A prospective cohort study further confirmed these findings, reporting similar implantation rates between the standard warming protocol and the one-step fast-warming protocol (30.2% vs 29.8%, p>0.05) [20]. The study concluded that the fast-warming protocol offers a safe and effective alternative to conventional warming while significantly reducing procedure time [20].
Does the one-step warming protocol affect live birth and miscarriage rates?
Evidence indicates that the one-step warming protocol does not negatively impact live birth rates and may be associated with reduced miscarriage rates.
One multicenter study reported a statistically significant reduction in miscarriage rate with the fast warming protocol compared to the classic protocol (18.0% vs 32.3%, P=0.009) and a significant increase in ongoing pregnancy rate at 26 gestational weeks or over (66.9% vs 80.3%, P=0.016) [49].
Research on vitrified donor oocytes using a modified warming protocol (MWP) showed significantly higher ongoing pregnancy/live birth rates compared to the conventional warming protocol (CWP) (66.7% vs 50.4%, P<0.05) [50]. Multivariate analysis confirmed a positive association between the modified warming protocol and ongoing pregnancy/live birth outcomes (adjusted odds ratio=1.899, 95% CI=1.002 to 3.6, P<0.05) [50].
Are there differences in embryo survival rates between warming protocols?
Studies consistently show that embryo survival rates after warming are equivalent between one-step and multi-step protocols across different development stages.
The same high survival rates were observed in studies comparing the two approaches, with one analysis reporting "survival rates were comparable across all comparisons" in their evaluation of 1402 transferred embryos [33]. Another study specifically noted that "the same embryo survival rate was observed in the two groups" in their analysis of blastocyst and cleavage stage frozen embryo transfers [49].
For vitrified oocytes, research also demonstrated similar survival rates between conventional and modified warming protocols (93.7% vs 93.9%, P>0.05) [50], indicating the one-step method is equally gentle on delicate reproductive cells.
What are the practical advantages of one-step warming protocols beyond clinical outcomes?
Beyond equivalent clinical outcomes, one-step warming protocols offer significant practical advantages for IVF laboratory workflow and efficiency.
The primary benefit is the substantial reduction in procedure time. One study reported that one-step embryo warming decreases the procedure time by more than 90% compared to classical multi-step warming [33]. Another analysis confirmed "a difference in time required for warming procedures was found in favour of group 2" (the fast warming protocol) and noted that it "allows a reduction in the time needed to carry out the procedure and the workload of embryologists in an IVF laboratory" [49].
This time efficiency reduces potential fatigue among embryologists and optimizes clinical workflow without compromising embryo viability or developmental potential [50].
Experimental Protocols & Methodologies
Standard Multi-Step Warming Protocol
The conventional warming protocol typically involves three sequential solutions at specific temperatures and timing [39]:
Thawing Solution (TS): Embryos are rapidly warmed in TS containing 1.0M sucrose or trehalose at 37°C for 1 minute [33] [39]. The high extracellular disaccharide concentration creates an osmotic gradient that prevents water from rushing into cells too quickly and causing membrane rupture [39].
Dilution Solution (DS): Embryos are transferred to DS containing 0.5M sucrose at room temperature for 3 minutes [33] [39]. Media carry-over from TS is intentionally maintained to create a gradual gradient for osmotic adjustment [39].
Washing Solution (WS): Embryos undergo two washes in WS - first for 5 minutes, then for 1 minute at room temperature [33] [39]. This step removes lingering cryoprotectants like DMSO or ethylene glycol and acclimatizes embryos to culture conditions [39].
One-Step Fast Warming Protocol
The simplified one-step protocol significantly reduces process complexity:
Single Solution Exposure: Embryos are warmed using only TS containing 1M sucrose solution for 1 minute at 37°C [33].
Direct Transfer to Culture: After the 1-minute incubation, embryos are directly transferred to culture media without additional dilution or washing steps [33] [50].
The protocol leverages the embryo's robust ability to self-regulate osmotic pressure when moved directly from high-osmolarity TS to culture media, with research indicating that "sufficient washing through multiple culture drops to remove compounds associated with vitrification remains important" for optimal outcomes [39].
Comparative Clinical Outcomes Data
Table 1: Pregnancy and Implantation Outcomes by Warming Protocol
| Outcome Measure | Multi-Step Protocol | One-Step Protocol | P-value | Study Reference |
|---|---|---|---|---|
| Clinical Pregnancy Rate (CPR) | 42.6% | 44.3% | 0.78 | [33] |
| Ongoing Pregnancy Rate (OPR) | 33.2% | 37.5% | 0.21 | [33] |
| Implantation Rate | 30.2% | 29.8% | >0.05 | [20] |
| Miscarriage Rate | 32.3% | 18.0% | 0.009 | [49] |
| Ongoing Pregnancy (≥26 weeks) | 66.9% | 80.3% | 0.016 | [49] |
Table 2: Embryo Survival and Development Outcomes
| Outcome Measure | Multi-Step Protocol | One-Step Protocol | P-value | Study Reference |
|---|---|---|---|---|
| Embryo Survival Rate | Comparable | Comparable | >0.05 | [33] [49] |
| Oocyte Survival Rate (Vitrified) | 93.7% | 93.9% | >0.05 | [50] |
| Blastocyst Formation (Donor Oocytes) | 57.5% | 77.3% | <0.05 | [50] |
| Usable Blastocyst Formation | 35.4% | 51.4% | <0.05 | [50] |
| Ongoing Pregnancy/Live Birth (Donor Oocytes) | 50.4% | 66.7% | <0.05 | [50] |
Table 3: Subgroup Analysis by Embryo Quality and Development Day
| Subgroup | Outcome Measure | Multi-Step Protocol | One-Step Protocol | Study Reference |
|---|---|---|---|---|
| Top Quality Embryos (G1) | Clinical Pregnancy Rate | 52.3% | 54.6% | [33] |
| Good Quality Embryos (G2) | Clinical Pregnancy Rate | 38.6% | 40.0% | [33] |
| Day 5 Embryos | Clinical Pregnancy Rate | 44.8% | 46.5% | [33] |
| Day 6 Embryos | Clinical Pregnancy Rate | 28.0% | 31.2% | [33] |
| IVF Fertilization | Clinical Pregnancy Rate | 45.0% | 48.0% | [33] |
| ICSI Fertilization | Clinical Pregnancy Rate | 40.9% | 38.3% | [33] |
Experimental Workflow Visualization
Research Reagent Solutions
Table 4: Essential Materials for Embryo Warming Protocols
| Reagent Solution | Composition | Function in Protocol | Protocol Application |
|---|---|---|---|
| Thawing Solution (TS) | 1.0M sucrose or trehalose in HEPES-buffered medium [39] | Creates high osmolarity gradient for controlled rehydration; prevents ice crystal formation during rapid warming [39] | Used in both protocols as initial warming solution |
| Dilution Solution (DS) | 0.5M sucrose in HEPES-buffered medium [39] | Provides intermediate osmolarity for gradual removal of cryoprotectants; minimizes osmotic shock [39] | Multi-step protocol only (second step) |
| Washing Solution (WS) | HEPES-buffered medium mimicking culture conditions [39] | Removes residual cryoprotectants (DMSO, ethylene glycol); acclimatizes embryos to culture conditions [39] | Multi-step protocol only (final step) |
| Culture Media | Sequential medium (e.g., continuous single culture) [51] | Supports embryo development post-warming; maintains viability until transfer [51] | Used in both protocols after warming completion |
| Vitrification Solutions | Ethylene glycol, DMSO, sucrose in specific concentrations [51] | Cryoprotectants that enable glass-like state during freezing; prevent ice crystal formation [51] | Pre-warming storage condition |
Key Research Insights
The collective evidence demonstrates that one-step fast warming protocols achieve equivalent clinical outcomes to traditional multi-step methods while offering significant practical advantages. The comparable survival, pregnancy, implantation, and live birth rates across multiple study designs and patient populations support the clinical validity of simplified warming approaches [33] [20] [49].
The reduction in miscarriage rates and improvement in ongoing pregnancy rates observed with fast warming protocols in some studies [49] [50] suggest potential benefits beyond efficiency. The significant time savings (over 90% reduction in procedure time) [33] and decreased laboratory workload [49] represent substantial operational advantages for IVF laboratories implementing high-throughput cryopreservation programs.
These findings indicate that one-step warming protocols represent a viable optimization of sucrose concentration and exposure timing in embryo warming solutions, maintaining clinical efficacy while dramatically improving laboratory efficiency.
Experimental Protocols
Ultra-Fast Blastocyst Warming and Validation Protocol
This detailed methodology is adapted from a prospective study comparing standard and ultra-fast warming protocols for vitrified blastocysts [52].
1. Embryo Culture and Vitrification
- Culture Conditions: Culture embryos in a time-lapse device (e.g., Embryoscope+) in a single-step culture media (e.g., G-TL) under low oxygen atmosphere (6% CO₂, 5% O₂) from insemination/injection onwards [52].
- Blastocyst Selection: Evaluate blastocysts on day 5 (115 ± 1 h) or day 6 (139 ± 1 h) using Gardner and Schoolcraft’s classification. Vitrify day 5 blastocysts graded B3 to B6, excluding those with grade C trophectoderm. For day 6 blastocysts, vitrify those graded ≥ B4BB [52].
- Vitrification: Use a commercial vitrification kit (e.g., Rapid Vit Blast) according to manufacturer's instructions. Store embryos in liquid nitrogen [52].
2. Ultra-Fast Warming Procedure
- Materials: Use a commercial warming kit (e.g., Rapid Warm Blast). The entire procedure is performed at 37°C [52].
- Protocol:
- Step 1: Transfer the vitrified blastocyst directly into the pre-equilibrated "Warm 1 Blast" solution for 2 minutes [52].
- Step 2: After 2 minutes, move the blastocyst directly into conventional culture medium (e.g., G-TL). Note: The standard protocol includes two additional steps: 3 minutes in "Warm 2 Blast" and 10 minutes in "Warm 3 Blast." [52].
- Post-Warming Culture: Culture the warmed blastocysts for 4–5 hours at 37°C (6% CO₂, 5% O₂) before transfer or analysis. Assess blastocyst survival and re-expansion approximately 2 hours after warming [52].
3. Molecular Validation of Lineage Specification
- Immunofluorescence Staining: Fix blastocysts warmed using the ultra-fast protocol for immunofluorescence analysis [52].
- Primary Antibodies: Use antibodies against key lineage specification markers:
- Imaging and Analysis: Record the number and spatial distribution of positive cells for each marker to evaluate the conservation of lineage specification and overall blastocyst architecture [52].
Quantitative Outcomes of Ultra-Fast Warming
Table 1: Comparison of Embryology and Clinical Outcomes between Standard and Ultra-Fast Warming Protocols [52]
| Parameter | Standard Protocol (15 min) | Ultra-Fast Protocol (2 min) | Statistical Significance |
|---|---|---|---|
| Pilot Study (Cycles) | n=47 | n=39 | |
| Survival Rate | 100% | 100% | Comparable |
| Re-expansion Rate | 80% | 76% | Comparable |
| Live Birth Rate (LBR) | 29.8% | 30.7% | Comparable |
| Larger Cohort (Cycles) | n=547 (6 months) | n=321 (3 months) | |
| Survival Rate | 97.8% | 97.6% | p > 0.05 |
| Live Birth Rate (LBR) | 28.3% | 29.6% | p > 0.05 |
| Research Blastocysts | Not Applicable | n=27 | |
| Survival Rate | Not Applicable | 100% | |
| Re-expansion Rate | Not Applicable | 82% |
Table 2: Research Reagent Solutions for Blastocyst Warming and Validation [52]
| Reagent / Kit | Function |
|---|---|
| Rapid Vit Blast / Rapid Warm Blast Kit | Commercial kit for vitrifying and warming blastocysts. Contains solutions with defined sucrose and cryoprotectant concentrations. |
| G-TL Medium | Single-step culture medium for extended embryo culture pre- and post-warming. |
| Antibody: GATA4 | Marker for primitive endoderm lineage specification in the inner cell mass. |
| Antibody: NANOG | Marker for epiblast lineage specification in the inner cell mass. |
| Antibody: NR2F2 | Marker for trophectoderm lineage specification. |
Troubleshooting Guide
Table 3: Troubleshooting Guide for Ultra-Fast Warming and Lineage Validation
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low Blastocyst Survival Post-Warming | Improper storage or vitrification quality. | Verify integrity of liquid nitrogen storage and strict adherence to vitrification protocol. |
| Poor Blastocyst Re-expansion | Suboptimal sucrose concentration in warming solution or osmotic shock. | Ensure warming solutions are at correct temperature (37°C) and prepared accurately. |
| Weak or Absent Immunofluorescence Signal | Inefficient cell permeabilization or antibody issues. | Optimize permeabilization time/temperature; validate antibody concentrations and specificity on control samples. |
| Altered Spatial Organization of Lineage Markers | Severe warming-induced stress impacting cell fate. | Confirm warming procedure timing and temperature; ensure post-warming culture conditions are optimal. |
Frequently Asked Questions (FAQs)
Q1: What is the main advantage of the ultra-fast warming protocol over the standard method? The primary advantage is a significant improvement in laboratory workflow and time-efficiency. The ultra-fast protocol reduces the warming procedure from 15 minutes to just 2 minutes while maintaining equivalent embryology and clinical outcomes, including survival, re-expansion, and live birth rates [52].
Q2: How does the ultra-fast protocol ensure that lineage specification is not compromised? A study validated this using immunofluorescence on research-donated blastocysts. Staining for key cell fate markers (GATA4 for primitive endoderm, NANOG for epiblast, and NR2F2 for trophectoderm) showed that their expression and spatial organization were conserved after ultra-fast warming, indicating normal lineage specification [52].
Q3: Can this ultra-fast warming protocol be applied to other cryopreserved tissues? The concept of simplifying and accelerating warming protocols is being explored in other areas. For example, research is ongoing to develop a universal rapid warming protocol for cryopreserved human ovarian tissue, which also aims to improve outcomes and standardize practices [53]. Always validate the protocol for each specific cell or tissue type.
Q4: My lab uses a different commercial vitrification/warming kit. Can we still implement this? The study used a specific kit (Rapid Vit Blast / Rapid Warm Blast), but the principle of reducing warming steps may be applicable to other systems. However, any protocol modification must be rigorously validated in your own laboratory with internal controls and, if possible, molecular assessment of embryo health before clinical implementation.
Frequently Asked Questions: Optimizing Sucrose Concentration in Embryo Warming
Q1: What is the primary role of sucrose in embryo warming solutions? Sucrose is a non-penetrating cryoprotectant that creates a high osmotic pressure in the warming solution. This establishes a controlled gradient that draws water out of the embryo gradually during initial rehydration, preventing a sudden influx of water that could cause the cells to burst ( [39]).
Q2: Does increasing the sucrose concentration in freezing/warming media improve clinical live birth rates? Research shows that increasing sucrose concentration improves embryo survival, but this does not necessarily translate to higher cumulative live birth rates. One randomized controlled trial found that freezing with 0.3M sucrose versus 0.1M sucrose significantly increased the likelihood of having ≥50% of embryos intact after thawing. However, the cumulative live birth rate from both fresh and frozen cycles showed no significant difference between the two groups ( [41]).
Q3: What is a key technique to improve blastocyst survival rates before vitrification? Artificially collapsing the blastocoel (the fluid-filled cavity) of blastocysts before vitrification is a well-established technique to improve survival rates. This can be induced using a laser pulse, an ICSI pipette, or a PZD pipette. Standardizing this step helps ensure more consistent dehydration times across all blastocysts in a cohort ( [54]).
Q4: How does the speed of the warming protocol affect embryo survival? A rapid warming rate is critical for survival as it minimizes the time the embryo spends at critical temperatures where damaging ice crystals can form. Recent research also indicates that ultra-fast or one-step warming protocols can achieve clinical outcomes, including survival and implantation rates, comparable to standard multi-step protocols while offering significant time savings in the laboratory workflow ( [39] [20]).
Comparative Data: Sucrose Concentration and Embryo Outcomes
Table 1: Embryo Survival and Live Birth Outcomes with Different Sucrose Concentrations (based on a prospective pragmatic RCT)
| Parameter | Control Group (0.1 M Sucrose) | Intervention Group (0.3 M Sucrose) | P-value / Significance |
|---|---|---|---|
| Couples with ≥50% embryos intact after thawing | 45 out of 74 couples | 53 out of 63 couples | P = 0.005 (Significant) |
| Likelihood of having ≥50% embryos intact | Reference | 3.4-fold increase [95% CI: 1.45, 7.82] | Significant |
| Live birth rate after frozen embryo transfer | 19 out of 63 couples | 9 out of 59 couples | P = 0.08 (Not significant) |
| Cumulative live birth rate (fresh + frozen cycles) | 53% | 42% | P = 0.17 (Not significant) |
Source: Adapted from PMC (2011). "A pragmatic RCT of conventional versus increased..." [41].
Table 2: Clinical Outcomes of Standard vs. One-Step Fast Warming Protocols
| Outcome Measure | Standard Warming Protocol | One-Step Fast Warming Protocol |
|---|---|---|
| Survival Rate | Comparable | Comparable |
| Clinical Pregnancy Rate | Comparable | Comparable |
| Implantation Rate | Comparable | Comparable |
| Ongoing Pregnancy/Live Birth Rate | Comparable | Comparable |
| Primary Workflow Advantage | Conventional protocol | Significantly shorter procedure time |
Source: Adapted from Fertility and Sterility (2025). "Effect of a one-step fast warming protocol..." [20].
Experimental Protocols for Key Investigations
Protocol 1: Investigating Sucrose Concentration in Embryo Freezing
This protocol is adapted from a prospective, randomized controlled trial comparing conventional and elevated sucrose concentrations ( [41]).
- Objective: To determine if an elevated sucrose concentration in the freezing medium increases the proportion of embryos surviving intact after thawing and improves clinical pregnancy outcomes.
- Materials:
- Control Freezing Medium: 1.5 M 1,2-Propanediol (PrOH) + 0.1 M sucrose.
- Intervention Freezing Medium: 1.4 M PrOH + 0.3 M sucrose.
- Thawing Solutions: Matched to the sucrose concentration of the freezing medium (0.2 M for control, 0.3 M for intervention).
- Basic Buffer: Dulbecco's phosphate-buffered saline (PBS) supplemented with human serum albumin (HSA).
- Methodology:
- Randomization: Supernumerary pronucleate or cleavage-stage embryos from IVF/ICSI cycles are prospectively randomized to be frozen in either control or intervention medium.
- Freezing Procedure:
- Equilibrate embryos at room temperature (~22°C).
- Wash embryos briefly (1-2 min) in PBS+HSA buffer.
- Transfer embryos to buffer + PrOH for 12 minutes.
- Finally, place embryos into the respective freezing medium (buffer + PrOH + sucrose) for 5-10 minutes before cooling.
- Freeze embryos singly in sealed straws using a controlled-rate freezer.
- Thawing Procedure: Utilize thawing solutions with sucrose concentrations matching the freezing group to ensure a step-wise dilution of cryoprotectants.
- Primary Outcome Assessment: The proportion of couples with at least 50% of their thawed embryos having all blastomeres intact.
- Secondary Outcome Assessment: Clinical pregnancy and cumulative live birth rates.
Protocol 2: Ultra-Fast One-Step Warming Validation
This protocol summarizes a modern approach to warming that challenges the necessity of gradual rehydration ( [39] [20]).
- Objective: To validate the efficacy of a one-step warming protocol against a standard multi-step protocol for vitrified-warmed blastocysts.
- Materials:
- One-Step Thawing Solution (TS): A solution containing a high concentration (e.g., 1.0 M) of sucrose or trehalose ( [39]).
- Culture Media.
- Methodology:
- Study Design: Prospective cohort study comparing a new fast-warming protocol to the standard protocol.
- Fast-Warming Procedure:
- Rapidly warm the vitrified straw in a 37°C water bath or heating block for the time specified by the device manufacturer.
- Immediately place the embryo directly into the One-Step Thawing Solution at 37°C for one minute. This single step replaces the traditional series of dilutions.
- Move the embryo through several drops of pre-equilibrated culture medium to wash away cryoprotectants.
- Transfer the embryo to a culture dish for ongoing development or transfer.
- Assessment: Compare survival rates, implantation rates, clinical pregnancy rates, and ongoing pregnancy/live birth rates between the standard and fast-warming groups.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Embryo Cryopreservation Research
| Reagent | Function in Protocol |
|---|---|
| Sucrose | A non-penetrating cryoprotectant that acts as an osmotic buffer. It draws water out of the cell during freezing/initial warming to minimize intracellular ice crystal formation and prevents osmotic shock during rehydration ( [41] [39]). |
| 1,2-Propanediol (PrOH) | A penetrating cryoprotectant that enters the cell. It replaces intracellular water, thereby reducing the amount of water that can form ice and lowering the freezing point of the cellular solution ( [41]). |
| Trehalose | An alternative non-penetrating disaccharide cryoprotectant. It is larger than sucrose and may be more effective at stabilizing cell membranes during cryopreservation ( [39]). |
| Dulbecco's PBS (DPBS) | A balanced salt solution used as a base for creating freezing and warming media. It provides a physiologically compatible ionic environment for the embryos during handling. |
| Human Serum Albumin (HSA) | Added to base buffers as a macromolecule. It helps stabilize the cell membrane and can sequester potential toxins. |
Experimental Workflow Diagrams
Conclusion
The optimization of sucrose concentration in embryo warming solutions represents a significant advancement in ART laboratory practice. The collective evidence confirms that simplified one-step warming protocols utilizing 1M sucrose yield embryology and clinical outcomes—including survival, pregnancy, and live birth rates—that are comparable to traditional multi-step methods. The primary advantage of these optimized protocols is a dramatic reduction in technical procedure time by over 90%, thereby enhancing laboratory workflow and reducing potential for operational error. Future research directions should focus on further refining sucrose concentrations for specific patient subgroups and embryo developmental stages, as well as exploring the molecular underpinnings of the observed clinical success. The widespread adoption of these evidence-based, optimized protocols holds strong potential to standardize and improve the efficiency of cryopreservation cycles in clinical and research settings globally.
References
- 1. Cryoprotectant - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/cryoprotectant]
- 2. Cryopreservation: An Overview of Principles and Cell- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7995302/]
- 3. Advances in the cryopreservation of mammalian oocytes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5904592/]
- 4. In vitro and in vivo viability of human blastocysts collapsed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3114962/]
- 5. Improved protocol for the vitrification and warming of rat ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416641/]
- 6. Chemical approaches to cryopreservation [https://www.nature.com/articles/s41570-022-00407-4]
- 7. 5 Key Differences Between Cryoprotectant Types [https://allanchem.com/key-differences-cryoprotectant-types/]
- 8. Cryoprotectants [https://www.coopersurgical.com/whitepaper/cryoprotectants/]
- 9. Cryoprotectant - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/cryoprotectant]
- 10. DFT-based evaluation of cryoprotectants and their role in ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224025000884]
- 11. Ultra RapidWarm™ Blast [https://www.vitrolife.com/products/cryopreservation/ultra-rapidwarm-blast/]
- 12. Optimization of cryoprotectant treatment for the vitrification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4685224]
- 13. Cryoprotectant Toxicity: Facts, Issues, and Questions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4620521/]
- 14. Sucrose increases the quality and fertilizing ability of ... [https://www.sciencedirect.com/science/article/pii/S0032579119307096]
- 15. Advantages of vitrification preservation in assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9632035/]
- 16. A review of best practices of rapid-cooling vitrification for ... [https://www.asrm.org/practice-guidance/practice-committee-documents/a-review-of-best-practices-of-rapid-cooling-vitrication-for-oocytes-and-embryos-a-committee-opinion-2021/]
- 17. Simplified Embryo and Oocyte Warming Protocols [https://fujifilmbiosciences.fujifilm.com/us/simplified-embryo-and-oocyte-warming-protocols]
- 18. Reproductive Technology Preservation Research [https://www.21cm.com/reproductive.html]
- 19. Shorter protocols for vitrification and post-warming dilution ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648325000641]
- 20. Effect of a one-step fast warming protocol on reproductive ... [https://www.sciencedirect.com/science/article/pii/S0015028225005783]
- 21. Optimization of bovine oocyte cryopreservation: membrane ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1628947/full]
- 22. Probing mechanisms of cryopreservation damage to ... [https://pubmed.ncbi.nlm.nih.gov/39918490/]
- 23. FAQ Series: The Science Behind Cryopreservation [https://allcells.com/faq-series-the-science-behind-cryopreservation/]
- 24. Protocols and Best Practices for Freezing Cells [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 25. Improved clinical outcomes with a modified warming protocol ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01776-2]
- 26. Membrane-targeted DNA frameworks with biodegradability ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925003130]
- 27. Efficacy and safety of a one-step warming protocol ... [https://www.medrxiv.org/content/10.1101/2025.10.02.25337068v1.full-text]
- 28. One-step warming of vitrified human cleavage and ... [https://pubmed.ncbi.nlm.nih.gov/39715345/]
- 29. Improved protocol for the vitrification and warming of rat ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328718]
- 30. Effect of a one-step fast warming protocol on reproductive ... [https://pubmed.ncbi.nlm.nih.gov/40651524/]
- 31. A diluted one-step warming protocol: survival of vitrified ... [https://pubmed.ncbi.nlm.nih.gov/40042768/]
- 32. Single-Step Blastocyst Warming Validated, Saves Time [https://advances.massgeneral.org/obgyn/journal.aspx?id=2626]
- 33. Efficacy and safety of a one-step warming protocol ... [https://www.medrxiv.org/content/10.1101/2025.10.02.25337068v1]
- 34. Application of a single “Universal warming protocol” for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12055733/]
- 35. Vitrolife Group at ESHRE - Igenomix [https://www.igenomix.eu/eshre2025/]
- 36. Influence of the shortened warming protocol on human ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648324006436]
- 37. Comparison of a commercial trehalose-based and laboratory ... [https://mefj.springeropen.com/articles/10.1186/s43043-025-00224-x]
- 38. In vivo fertilization improved the cryotolerance and ... [https://www.nature.com/articles/s41598-024-76073-x]
- 39. Understanding the Warming Procedure for Vitrified Embryos [https://www.aab.org/NewsBot.asp?MODE=VIEW&ID=1070]
- 40. Improved protocol for the vitrification and warming of rat ... [https://pubmed.ncbi.nlm.nih.gov/40920796/]
- 41. A pragmatic RCT of conventional versus increased ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3137387/]
- 42. Troubleshooting a cryopreservation system (Chapter 10) [https://www.cambridge.org/core/books/troubleshooting-and-problemsolving-in-the-ivf-laboratory/troubleshooting-a-cryopreservation-system/3F9698CD3F819CBC05767BB294706EEC]
- 43. Advanced maternal age was associated with an annual ... [https://pubmed.ncbi.nlm.nih.gov/40403911/]
- 44. What's New from the Fertility and Sterility Family of Journals [https://www.asrm.org/news-and-events/asrm-news/latest-news/October-2025-whats-new-from-fertility-and-sterility2/]
- 45. Osmotic stress induces JNK-dependent embryo invasion in ... [https://pubmed.ncbi.nlm.nih.gov/30131400/]
- 46. The impact of post-warming culture duration on clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7711098/]
- 47. Maximizing the efficacy of commercial vitrification and ... [https://www.sciencedirect.com/science/article/pii/S1472648324002062]
- 48. Comparative Assessment of Survival and Clinical Outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10643310/]
- 49. frozen embryo transfer outcomes with one-step warming ... [https://pubmed.ncbi.nlm.nih.gov/40782787/]
- 50. Improved clinical outcomes with a modified warming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357474/]
- 51. Comparison of Cumulative Live Birth Rates Between Fresh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087671/]
- 52. Ultra-Fast Warming Procedure of Vitrified Blastocysts ... [https://link.springer.com/article/10.1007/s43032-024-01762-x]
- 53. Towards a universal rapid warming protocol for ... [https://www.sciencedirect.com/science/article/pii/S147264832500358X]
- 54. Our best tips & tricks for successful vitrification [https://blog.vitrolife.com/togetheralltheway/our-best-tips-tricks-for-successful-vitrification]