Overcoming the Cellular Diversity Gap in Organoid Models: Strategies for Enhanced Physiological Relevance
Organoid technology has revolutionized biomedical research by providing three-dimensional, self-organizing models that mimic human organs.
Overcoming the Cellular Diversity Gap in Organoid Models: Strategies for Enhanced Physiological Relevance
Abstract
Organoid technology has revolutionized biomedical research by providing three-dimensional, self-organizing models that mimic human organs. However, a significant limitation hindering their full translational potential is their often limited cellular diversity, typically lacking key components like immune cells, vasculature, and nerves. This article addresses this critical challenge by exploring the foundational causes of this limitation, detailing advanced methodological solutions such as co-culture systems and organ-on-chip technologies, providing troubleshooting and optimization strategies for improved reproducibility, and validating these enhanced models against traditional systems. Aimed at researchers, scientists, and drug development professionals, this review synthesizes cutting-edge approaches to build more physiologically complete organoids, thereby advancing their application in disease modeling, drug discovery, and personalized medicine.
The Cellular Diversity Problem: Why Basic Organoids Fall Short
Frequently Asked Questions (FAQs)
Why is the absence of vasculature a critical limitation in organoid technology? Organs such as the kidney, brain, and heart are highly vascularized in the body. The lack of vasculature in organoids prevents adequate nutrient and oxygen diffusion, leading to the formation of a necrotic core in larger organoids and failing to recapitulate essential physiological interactions, such as waste filtration in kidney glomeruli [1].
What are the primary methods for vascularizing organoids? The main strategies include in vivo engraftment into immunodeficient host models, co-culturing organoids with endothelial cells (ECs) or mesodermal progenitor cells (MPCs), and using genetic engineering to direct cells within the organoid toward an endothelial fate [1] [2].
How can I incorporate immune cells into my organoid model? The most common technique is to establish a co-culture system where organoids are cultured with specific immune cells, which can be either immortalized cell lines or autologous immune cells derived from patients [1].
My patient-derived tissue sample cannot be processed immediately. What is the best way to preserve it for organoid generation? For short-term delays (≤6-10 hours), wash the tissue with an antibiotic solution and store it at 4°C in DMEM/F12 medium supplemented with antibiotics. For longer delays (>14 hours), cryopreservation is recommended. Wash the tissue and cryopreserve it in a freezing medium (e.g., 10% FBS, 10% DMSO in 50% L-WRN conditioned medium). Note that a 20-30% variability in live-cell viability can be expected between these two methods [3].
What are the advantages of using Mesodermal Progenitor Cells (MPCs) to create complex organoids? MPCs can differentiate into multiple cell lineages, including endothelial cells (forming vascular networks) and smooth muscle cells (providing vessel support). They can also give rise to Iba1+ immune cells, such as microglia-like cells in neural organoids, thereby providing vasculature and stromal components simultaneously [2].
Troubleshooting Guides
Problem: Poor Organoid Growth and Central Necrosis
- Potential Cause: Inadequate vascularization, leading to insufficient nutrient and oxygen delivery to the organoid's core.
- Solution:
- Incorporate Mesodermal Progenitor Cells (MPCs): Mix MPCs with your organoid-forming cells in a 1:1 ratio. Culture the aggregates under pro-angiogenic conditions (e.g., 2% O₂) to promote an evenly distributed vascular network [2].
- Co-culture with Endothelial Cells: Directly co-culture your organoids with human umbilical vein endothelial cells (HUVECs) or similar endothelial cells to initiate vessel formation [1].
- Consider In Vivo Engraftment: For ultimate maturation and vascularization, engraft organoids into an immunodeficient mouse model (e.g., NSG mice) at sites like the kidney capsule or cranial window, which allows host vasculature to invade the organoid [1].
Problem: Failure to Model Immune-Mediated Diseases or Drug Responses
- Potential Cause: The organoid model lacks resident or circulating immune cells, making it unsuitable for studying inflammation, infection, or immunotherapy.
- Solution:
- Establish an Immune Co-culture System: Isolate peripheral blood mononuclear cells (PBMCs) or specific immune cell subtypes (e.g., T cells) from the same patient. Introduce these cells into the organoid culture medium to create an epithelial-immune co-culture [1].
- Utilize MPC-Based Models: When generating organoids with MPCs, monitor for the development of Iba1+ macrophage/microglia-like cells that can infiltrate the tissue, providing a native immune component [2].
Problem: Low Viability or Organoid Formation Efficiency from Patient Tissue
- Potential Cause: Delays in processing or improper handling of the surgically resected patient tissue.
- Solution:
- Minimize Processing Time: Transfer samples to cold, antibiotic-supplemented medium immediately after collection and process as quickly as possible [3].
- Choose the Right Preservation Method: Adhere to the guidelines for short-term refrigerated storage versus cryopreservation based on your expected processing delay to maximize cell viability [3].
- Use a ROCK Inhibitor: When thawing or passaging cryopreserved organoids, include a ROCK inhibitor (e.g., Y-27632) in the culture medium for the first few days to reduce anoikis and improve cell survival [4].
Experimental Protocols
This protocol describes how to create vascularized tumor or neural organoids by incorporating mesodermal progenitor cells.
1. Materials
- Cell Sources: hiPSCs, human tumor cell line (e.g., MDA-MB-435s), or neural spheroids.
- Induction Medium: For MPC induction from hiPSCs: use a medium containing the GSK3β-inhibitor Chir99021 and BMP4.
- Culture Vessels: Suspension culture plates (e.g., low-adhesion 6-well plates).
- Extracellular Matrix (ECM): Matrigel or similar ECM hydrogel.
- Hypoxia Chamber: For culture at 2% O₂.
2. Step-by-Step Procedure
Part A: Differentiation of Mesodermal Progenitor Cells (MPCs) from hiPSCs
- Culture hiPSCs in a standard maintenance medium.
- To induce MPCs, switch to an induction medium supplemented with Chir99021 and BMP4.
- Culture for 3 days. Monitor for the loss of pluripotency markers and the appearance of Brachyury+ cells (approximately 80% by day 2).
Part B: Formation of Vascularized Organoids
- For Tumor Organoids: Mix induced MPCs with GFP-labelled tumor cells in a 1:1 ratio.
- For Neural Organoids: Generate Sox1+ neural spheres and Brachyury+ MPC spheres separately, then bring them into co-culture to allow fusion.
- Culture the resulting aggregates in suspension.
- To promote uniform vascular network distribution, transfer the cultures to a hypoxic environment (2% O₂) for several days.
- Maintain the organoids in suspension culture on a rocking plate for long-term studies (up to 280 days).
3. Validation and Analysis
- Immunofluorescence: Stain for CD31 (PECAM-1) to confirm endothelial network formation and α-Smooth Muscle Actin (αSMA) to identify pericytes/smooth muscle cells in the vessel wall.
- Electron Microscopy: Use TEM to confirm the ultrastructure of formed vessels, including lumen formation, endothelial cell-cell junctions, and basement membrane.
Table 1: Comparison of Strategies to Address Missing Cell Types in Organoids
| Strategy | Methodology | Key Advantages | Key Limitations |
|---|---|---|---|
| In Vivo Engraftment [1] | Transplantation of organoids into immunodeficient mice (e.g., kidney capsule, cranial window). | Provides a natural, functional host vasculature; leads to enhanced organoid maturation. | Technically challenging; introduces host variables; less suitable for high-throughput screening. |
| Co-culture with MPCs [2] | Incorporation of mesodermal progenitor cells into the organoid during formation. | Generates a complex, hierarchically organized human vascular network; can also yield microglia-like cells. | Requires additional differentiation step for MPCs; network organization may require hypoxia. |
| Co-culture with Specific Immune Cells [1] | Introduction of immortalized or patient-derived immune cells into the organoid culture. | Enables study of specific epithelial-immune interactions (e.g., in cancer or infection). | Lack of standardized protocol; may not fully recapitulate the native immune niche. |
| Genetic Engineering [1] | Gene editing (e.g., CRISPR) to manipulate cells within organoids to adopt an endothelial fate. | Endothelial cells are intrinsic and autologous to the organoid. | Can be inefficient; requires sophisticated technical expertise. |
Research Reagent Solutions
Table 2: Essential Materials for Complex Organoid Generation
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| Matrigel [4] | An undefined extracellular matrix (ECM) hydrogel that provides a 3D scaffold for organoid growth and self-organization. | Used as the core scaffold for embedding organoids in "dome" cultures. |
| Chir99021 [2] | A GSK3β inhibitor that activates Wnt signaling, crucial for inducing mesodermal progenitor cells (MPCs) from pluripotent stem cells. | Key component in MPC induction medium. |
| BMP4 [2] | Bone Morphogenetic Protein 4, a growth factor that favors lateral plate mesodermal fate, guiding MPCs toward vascular lineages. | Used in combination with Chir99021 for MPC induction. |
| ROCK Inhibitor (Y-27632) [4] | Improves cell survival after dissociation and thawing by inhibiting apoptosis (anoikis). | Added to culture medium for the first 2-3 days after thawing or passaging organoids. |
| Noggin [3] | A BMP signaling pathway antagonist, often used in intestinal and colon organoid media to promote epithelial growth. | Standard component of many complete organoid culture media. |
| R-spondin Conditioned Medium [3] | Contains R-spondin protein, a potent activator of Wnt signaling, essential for stem cell maintenance in many epithelial organoids. | Used in colon, esophageal, and pancreatic organoid media formulations. |
Signaling Pathways and Workflows
Vascularization via MPCs Workflow
Immune Cell Co-culture Workflow
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary limitations of the self-organizing nature of organoids? The self-organization of organoids, while powerful, leads to several key technical challenges for researchers:
- Heterogeneity and Variability: The stochastic nature of self-assembly results in significant batch-to-batch differences in organoid size, cellular composition, and structure, making it difficult to draw consistent conclusions [5] [6].
- Limited Maturity: Most organoids model a fetal or early developmental stage rather than a mature adult organ. They often lack key cell types, such as immune cells, vascular cells, and nerves, which limits their physiological relevance [5] [7] [6].
- Necrotic Core Formation: Without a functional vascular network, nutrients and oxygen cannot diffuse into the center of larger organoids. This leads to hypoxia and cell death in the core, limiting the organoid's lifespan and size [5] [7] [6].
FAQ 2: Why is Standard Matrigel a problem for advanced organoid research? Matrigel, the ubiquitous matrix derived from mouse sarcomas, presents major hurdles for reproducible and clinically relevant science:
- Batch-to-Batch Variability: Its complex and undefined composition varies from lot to lot, introducing an uncontrollable variable that compromises experimental reproducibility [8] [9].
- Animal-Derived Origin: Being derived from mouse tumors, it contains xenogenic components and growth factors that limit the translational potential of findings for human therapies and can trigger unwanted immune responses in co-culture models [8] [9].
- Limited Control: Its natural composition makes it difficult to engineer or tune specific biochemical and mechanical properties to guide organoid development in a precise manner [10].
FAQ 3: How can limited cellular diversity in organoid models be addressed? Strategies to enhance cellular diversity focus on engineering the microenvironment and incorporating missing components:
- Co-culture Systems: Introducing other cell types, such as endothelial cells to form vasculature or immune cells, can help recapitulate a more complex tissue environment [6].
- Engineered Matrices: Using defined, synthetic, or human-derived hydrogels allows for the precise incorporation of adhesion motifs and growth factors to guide the differentiation and organization of multiple cell types [8] [10].
- Assembloids: Fusing organoids of different regional identities (e.g., cortical and thalamic) can model complex cell-cell interactions and circuit formation that are absent in single organoids [5].
Troubleshooting Guides
Issue 1: High Heterogeneity and Poor Reproducibility in Organoid Cultures
| Observed Problem | Potential Root Cause | Solution and Recommended Actions |
|---|---|---|
| High variability in organoid size and shape between batches. | Stochastic self-assembly; manual cell seeding and handling. | Automate processes. Use robotic liquid handling systems for consistent cell seeding, media changes, and differentiation protocols [5]. |
| Inconsistent cellular composition and differentiation outcomes. | Uncontrolled initial conditions (cell number, matrix concentration). | Standardize protocols. Precisely control the initial stem cell number and ECM-to-cell ratio. Use validated, assay-ready organoid models where available [6]. |
| Batch-to-batch differences despite identical protocols. | Variability in critical reagents, especially Matrigel. | Implement quality control. Use single-cell RNA sequencing to validate cellular composition. Transition to defined, animal-free hydrogels to eliminate Matrigel variability [6] [8]. |
Issue 2: Limited Organoid Growth and Necrotic Core Formation
| Observed Problem | Potential Root Cause | Solution and Recommended Actions |
|---|---|---|
| Cell death in the organoid center after reaching a certain size. | Lack of vascularization; limited nutrient and oxygen diffusion. | Improve nutrient access. Culture organoids in bioreactors with agitation or use the slice culture method to increase surface area and permeability [5] [7]. |
| Organoids fail to grow beyond a small diameter. | Hypoxia and metabolic waste accumulation. | Promote vascularization. Co-culture with endothelial cells to encourage rudimentary vessel formation [6]. |
| Inability to deliver substances to the organoid interior. | Absence of a perfusable vascular network. | Integrate with Organ-Chips. Use microfluidic devices to fluidically link organoids, providing perfusion and mechanical cues that can enhance maturation and function [5] [6]. |
Issue 3: Incomplete Maturity and Functionality
| Observed Problem | Potential Root Cause | Solution and Recommended Actions |
|---|---|---|
| Organoids exhibit fetal, not adult, characteristics. | Missing physiological cues from the native microenvironment. | Provide external stimulation. Apply relevant mechanical forces (e.g., stretch, flow), electrical stimulation, or co-culture with supporting mesenchymal cells [5]. |
| Absence of key functional responses (e.g., electrical activity, secretion). | Lack of specific mature cell types or neuronal innervation. | Extend culture time and use patterning factors. Optimize protocols for long-term culture and incorporate small molecules to promote specific regional identities and advanced maturation [7]. |
Experimental Protocols for Enhanced Reproducibility
Protocol 1: Establishing a Defined, Animal-Free Culture System for Vascular Organoids
This protocol replaces murine Matrigel with a human-derived, defined matrix system, enhancing translational potential and reproducibility [8].
1. Materials (The Scientist's Toolkit)
| Item | Function / Rationale |
|---|---|
| Vitronectin XF | A recombinant human protein coating for 2D iPSC culture; supports feeder-free, xeno-free expansion and maintains pluripotency. |
| Fibrinogen | A human plasma protein; forms the structural basis of the 3D hydrogel when combined with thrombin. |
| Thrombin | An enzyme that catalyzes the polymerization of fibrinogen to form a fibrin hydrogel. |
| Advanced DMEM/F12 | Basal medium for organoid culture. |
| Essential Growth Factors | Including EGF, FGF, and BMP for directing vascular differentiation. |
2. Step-by-Step Workflow
- 2D hiPSC Culture and Maintenance:
- Culture human induced pluripotent stem cells (hiPSCs) on Vitronectin-coated plates in defined mTeSR or equivalent medium.
- Passage cells upon reaching 70–80% confluency using a gentle enzyme-free method.
- Quality Control: Verify pluripotency by immunostaining for markers like Nanog and OCT3/4 [8].
- Differentiation Initiation and 3D Embedding:
- Begin directed differentiation toward mesoderm by changing to a specific differentiation medium.
- On day 13, harvest the differentiating cell aggregates.
- Prepare Fibrin Gel: Mix cells with a solution of fibrinogen and thrombin to initiate polymerization. Plate the mixture in droplets and incubate to form a solid gel.
- Overlay the gel with vascular differentiation medium.
- Culture and Maturation:
- Culture the vascular organoids for 18-21 days, with medium changes every 2-3 days.
- Functional Validation: Analyze sprouting behavior under a brightfield microscope. Confirm endothelial (CD31) and mural cell (PDGFRβ) identity via flow cytometry and whole-mount immunostaining [8].
Protocol 2: Troubleshooting Guide for Patient-Derived Colorectal Organoids
A standardized guide for generating organoids from colorectal tissues, addressing common pitfalls from sample collection to culture [3].
1. Materials (The Scientist's Toolkit)
| Item | Function / Rationale |
|---|---|
| Advanced DMEM/F12 | Transport and wash medium; preserves tissue integrity. |
| Penicillin-Streptomycin | Antibiotic supplement to prevent microbial contamination. |
| L-WRN Conditioned Medium | Source of Wnt3a, R-spondin, and Noggin; critical for intestinal stem cell growth. |
| Matrigel (or Alternative) | Basement membrane extract for 3D support (transition to defined hydrogels is recommended). |
| DMSO | Cryoprotectant for freezing cells and tissues. |
2. Step-by-Step Workflow & Troubleshooting
- Tissue Procurement and Processing:
- Action: Collect human colorectal tissue samples (normal, polyp, or tumor) and immediately place them in cold Advanced DMEM/F12 with antibiotics.
- Critical Step/Troubleshooting: Process samples within 6-10 hours. If delayed, use one of two methods:
- Short-term storage (<14h): Wash tissue with antibiotics and store at 4°C in DMEM/F12 with antibiotics.
- Long-term storage (>14h): Cryopreserve tissue in a freezing medium (e.g., 10% FBS, 10% DMSO in L-WRN medium).
- Data: A 20–30% variability in live-cell viability is observed between these preservation methods. Cryopreservation is preferred for long delays [3].
- Crypt Isolation and Seeding:
- Action: Mechanically and enzymatically dissociate the tissue to isolate crypts. Mix the crypt suspension with Matrigel or an alternative hydrogel and plate as droplets.
- Troubleshooting: Low organoid formation efficiency is often due to poor initial cell viability. Adhere strictly to the recommended processing timelines and use high-growth factor concentration media for tumor samples.
- Long-Term Culture and Analysis:
- Action: Culture in IntestiCult or similar organoid growth medium. Passage organoids when they become large and dense.
- Troubleshooting: To avoid necrotic cores, do not let organoids grow too large before passaging [11]. For functional analysis like drug screening, consider generating "apical-out" organoids for direct access to the luminal surface [3].
Table 1: Comparison of Organoid Preservation Methods for Colorectal Tissues [3]
| Preservation Method | Processing Delay | Estimated Cell Viability Impact | Recommended Use Case |
|---|---|---|---|
| Refrigerated Storage (4°C) | ≤ 6-10 hours | Lower impact (baseline) | Same-day or next-morning processing in the same lab. |
| Cryopreservation | > 14 hours | 20-30% reduction in viability | Long-term storage or when transport to a remote lab is required. |
Table 2: Functional Characterization of Animal-Free Vascular Organoids vs. Matrigel Controls [8]
| Characterization Metric | Matrigel-Based Organoids | Vitronectin/Fibrin-Based Organoids | Significance |
|---|---|---|---|
| Pluripotency Marker (OCT4) Expression | Baseline (High in iPSCs, downregulated during differentiation) | No significant difference | Vitronectin supports normal exit from pluripotency. |
| Mesoderm Marker (TWIST) Expression | Baseline | No significant difference | Normal developmental progression. |
| Surface Area (by Brightfield) | Baseline | No significant difference | Similar growth and size characteristics. |
| Endothelial Cell Content (CD31+ by FACS) | Baseline | No significant difference | Successful differentiation of endothelial lineage. |
| Mural Cell Content (PDGFRβ+ by FACS) | Baseline | No significant difference | Successful differentiation of supportive mural cells. |
The Diversity Gap in Organoid Research: Quantifying the Problem
The limited genetic diversity in biomedical research, often called the "diversity gap," presents a significant challenge for accurately modeling human diseases and predicting drug responses. The table below summarizes the quantitative evidence of this disparity and its documented impact on research outcomes.
Table 1: Evidence and Impact of Limited Diversity in Biomedical Models
| Aspect of Diversity Gap | Quantitative Evidence | Impact on Research & Healthcare |
|---|---|---|
| Genetic Ancestry in Genomic Studies [12] | Most Genome-Wide Association Studies (GWAS) are predominantly based on European ancestry populations. | Impedes the development of accurate Polygenic Risk Scores (PRS) for underrepresented populations, exacerbating health disparities. |
| Sex-Based Differences [12] | Significant disparities exist in disease susceptibility, treatment efficacy, and drug toxicity between sexes. | Drug metabolism, immune response, and disease prevalence data become skewed without sex-stratified analyses. |
| Drug Trial Failure Rate [6] | The clinical trial failure rate exceeds 85%, partly due to safety and efficacy concerns not predicted by non-diverse models. | High costs and slow progress in drug development; released drugs may have unforeseen, population-specific adverse effects. |
Scientific Foundations: How Limited Diversity Skews Biological Data
Limited diversity in model systems introduces bias at multiple biological levels, compromising the translational value of research.
- Disease Modeling Fidelity: Organoids derived from a narrow genetic background fail to capture the full spectrum of disease manifestations. For instance, certain monogenic disorders like cystic fibrosis and Alagille syndrome have been modeled using patient-derived organoids, revealing how different mutations lead to variable clinical outcomes [13]. Restricting models to a single haplotype overlooks this critical variability.
- Drug Response Prediction: Genetic ancestry and biological sex are critical factors influencing drug metabolism, efficacy, and toxicity [12]. A drug screened on organoids from a limited genetic background may show efficacy but could be ineffective or harmful in a genetically distinct population. Integrating donor-specific organoids from diverse backgrounds into early drug discovery can help identify these population-specific drug responses [12] [6].
- Cellular Complexity and Maturity: The diversity challenge is not only inter-donor but also intra-organoid. Many organoid models, particularly those derived from Pluripotent Stem Cells (PSCs), often exhibit a fetal phenotype that is inappropriate for studying adult-onset diseases [6]. Furthermore, the common lack of key tissue-specific cell types, such as immune cells, vasculature, and nerves, creates an oversimplified system that does not fully recapitulate the tissue microenvironment [13] [6].
Researcher's Toolkit: Protocols for Enhancing Diversity in Organoid Models
A. Establishing a Diverse Organoid Biobank
Creating a biobank from healthy and diseased donors with varying genetic backgrounds is a fundamental step [12] [6]. The workflow for establishing such a biobank from colorectal tissues, which can be adapted for other organs, is detailed below.
Protocol: Generating Patient-Derived Colorectal Organoids [3]
Tissue Procurement and Initial Processing:
- Collect human colorectal tissue samples (cancerous, pre-cancerous polyps, or normal) from surgical resections or colonoscopies under IRB-approved protocols and informed consent.
- Critical Step: Transfer samples in cold Advanced DMEM/F12 medium supplemented with antibiotics to preserve tissue integrity. Process immediately or preserve using validated methods.
- For short-term delays (≤6-10 hours): Wash tissue with antibiotic solution and store at 4°C in DMEM/F12 medium with antibiotics.
- For longer delays (>14 hours): Cryopreserve tissue using a freezing medium (e.g., 10% FBS, 10% DMSO in 50% L-WRN conditioned medium).
Crypt Isolation and Culture Initiation:
- Mechanically and enzymatically digest the tissue to isolate crypts or single cells.
- Centrifuge to pellet the cells/crypts and resuspend in a cold, liquid extracellular matrix (ECM) like Matrigel.
- Plate the cell-ECM suspension as small domes in a pre-warmed culture plate. Incubate at 37°C for 10-15 minutes to allow the ECM to solidify.
- Overlay the gel domes with pre-warmed complete organoid culture medium.
Culture Maintenance:
- Passage organoids every 1-2 weeks by mechanically and enzymatically breaking down the structures. Re-embed the fragments in fresh ECM for continued expansion.
B. Key Research Reagent Solutions
Table 2: Essential Reagents for Diverse Organoid Culture
| Reagent Category | Example Components | Function in Culture |
|---|---|---|
| Base Medium | Advanced DMEM/F12 | Provides essential nutrients and salts for cell survival and growth. |
| Niche Factors | EGF (Epidermal Growth Factor), R-spondin 1, Noggin | Mimics the in vivo stem cell niche; critical for stem cell maintenance and proliferation. EGF promotes growth, R-spondin amplifies Wnt signaling, and Noggin (a BMP inhibitor) prevents differentiation. |
| Supplements | B-27, N-Acetylcysteine, Nicotinamide, A83-01 (TGF-β inhibitor) | Provides antioxidants, supports cell health, and inhibits differentiation pathways to enable long-term expansion. |
| Extracellular Matrix (ECM) | Matrigel, Cell Basement Membrane (e.g., ATCC ACS-3035) | Provides a 3D scaffold that mimics the native basement membrane, crucial for proper cell polarization and structure formation. |
| Conditioned Media | Wnt3A-conditioned medium, R-spondin1-conditioned medium | Supplies essential proteins that are difficult to purify or produce recombinantly, crucial for sustaining certain organoid types. |
Troubleshooting Guide & FAQs
Question: Our organoid yields from patient tissues are low and variable. How can we improve reliability?
- Answer: Low yield is often a processing issue. Adhere strictly to these critical steps:
- Minimize Processing Delay: The time from surgery to culture initiation drastically impacts viability. Process tissues immediately or use a reliable preservation method [3].
- Choose the Right Preservation: For delays under 10 hours, refrigerated storage in antibiotic-supplemented medium is suitable. For longer delays, cryopreservation is superior, though a 20-30% drop in viability should be expected [3].
- Optimize Digestion: Titrate enzyme concentration and digestion time to avoid under- or over-digestion, which can kill stem cells.
Question: How can we make our organoid models more physiologically relevant for studying drug delivery and immune interaction?
- Answer: Standard organoids often lack key physiological features. To enhance relevance:
- Induce Apical-Out Polarity: Modify protocols to generate "apical-out" organoids, which expose the luminal surface. This allows direct access for studying drug permeability, host-microbiome interactions, and immune cell co-cultures [3].
- Incorporate Fluidic Flow: Integrate organoids with Organ-Chips (microfluidic devices). This provides dynamic fluid flow and mechanical cues, enhancing cellular differentiation, creating well-polarized architectures, and enabling co-culture with immune cells or microbes [6].
- Attempt Vascularization: Co-culture organoids with endothelial cells to encourage blood vessel formation. This can alleviate nutrient diffusion problems, increase organoid size limits, and provide a more realistic model for studying drug delivery [6].
Question: Our organoids show high batch-to-batch variability, affecting experimental reproducibility. What solutions are available?
- Answer: Variability is a major challenge. Implement these strategies:
- Standardize and Automate: Use liquid handling robots for consistent media preparation and organoid passaging. This reduces human error and operational variability [6].
- Use Defined Reagents: Where possible, transition from undefined components (like conditioned media) to recombinant proteins to improve batch consistency.
- Leverage AI and Assay-Ready Models: New solutions combine automation with AI to standardize protocols and remove human bias from cell culture decisions. Alternatively, source validated, "assay-ready" organoid models from commercial suppliers to ensure a consistent starting point for experiments [6].
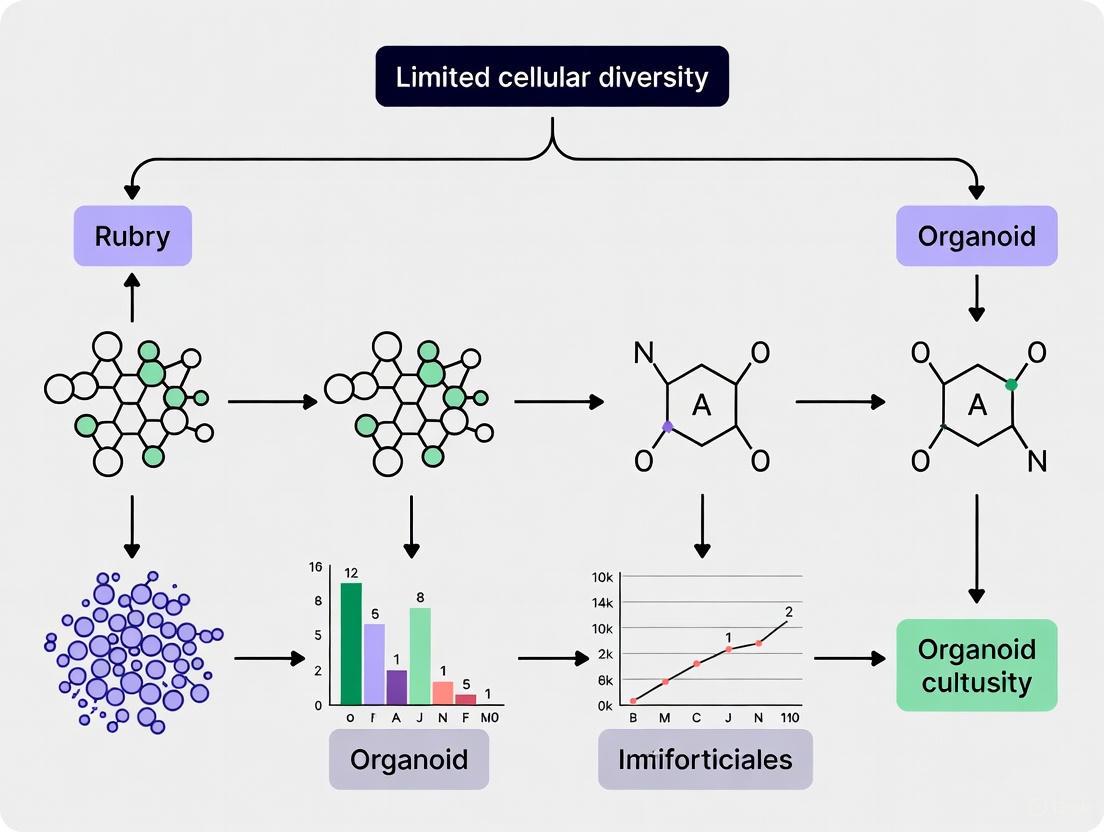
The following diagram summarizes the strategic approach to overcoming the diversity challenge in organoid research, from biobanking to advanced functional models.
A significant bottleneck in organoid research is the pervasive tendency for induced pluripotent stem cell (iPSC)-derived organoids to arrest at a fetal or early postnatal stage of development. Even after extended culture periods, these models often lack the cellular complexity, structural organization, and functional maturity characteristic of adult human organs. This "fetal phenotype" limitation severely constrains their utility in modeling adult-onset diseases, such as neurodegenerative disorders and many metabolic conditions, and reduces the predictive accuracy of drug screening campaigns [5] [14]. This technical support article delineates the core challenges and provides targeted troubleshooting guidance to help researchers advance organoid maturation.
The fundamental hurdle lies in the inadequacy of the standard in vitro environment to replicate the intricate cues of in vivo development. While organoids can initiate self-organization, the spontaneous and stochastic nature of this process often fails to progress fully without engineered intervention. Key missing elements include functional vascular networks for nutrient exchange, integrated immune cells, appropriate biomechanical forces, and sustained hormonal signaling [5]. Consequently, organoids frequently exhibit hypoxia-driven central necrosis, an underdeveloped extracellular matrix, and an immature transcriptomic profile that more closely resembles a fetal, rather than an adult, organ [14]. The following sections provide a structured framework to diagnose and address these specific issues.
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: My brain organoids develop a necrotic core after long-term culture. How can I improve their health and longevity?
- Problem: The formation of a necrotic core is a classic sign of insufficient nutrient and oxygen diffusion, a direct result of lacking a perfusable vascular network. This hypoxia not only causes cell death but also disrupts normal developmental gradients and limits organoid size [5] [14].
- Solutions:
- Co-culture with Endothelial Cells: Introduce human umbilical vein endothelial cells (HUVECs) or iPSC-derived endothelial cells during organoid formation. These cells can self-assemble into tube-like structures, enhancing nutrient delivery [14] [15].
- Induce Vascularization Genetically: Genetically engineer your iPSC line to overexpress pro-angiogenic factors like VEGF-A to encourage the formation of host-derived vasculature [16].
- Use Bioreactors: Culturing organoids in spinning bioreactors can improve medium circulation around the tissue, reducing diffusion barriers and promoting more uniform growth [16] [14].
- In Vivo Transplantation: Transplanting organoids into a mouse brain can facilitate vascularization by the host, leading to enhanced maturation and survival [15].
FAQ 2: How can I assess whether my organoids have reached a mature state?
- Problem: The field lacks universally standardized maturity metrics, leading to fragmented assessments and difficulties in cross-study comparisons [14].
- Solutions: Implement a multimodal assessment framework that goes beyond simple morphological inspection.
- Structural Analysis: Use immunofluorescence for deep-layer (TBR1, CTIP2) and upper-layer (SATB2) neuronal markers in brain organoids to confirm cortical layering. Electron microscopy can validate ultrastructural features like mature synapses with pre- (SYB2) and post-synaptic (PSD-95) densities [14].
- Functional Assays: Employ multi-electrode arrays (MEAs) to record synchronized neuronal network activity, such as gamma-band oscillations, which are a hallmark of mature circuits. Patch-clamp electrophysiology can detail the electrophysiological properties of individual neurons [14].
- Molecular Profiling: Conduct single-cell RNA sequencing (scRNA-seq) to compare the transcriptomic profile of your organoids against public databases of human fetal and adult brain tissue. This can quantitatively reveal the developmental stage of your model [14].
FAQ 3: How can I reduce the high heterogeneity and variability between organoid batches?
- Problem: The self-organizing nature of organoids introduces inherent variability in size, cellular composition, and structure, which can compromise experimental reproducibility [5].
- Solutions:
- Standardize Initial Conditions: Precisely control the initial cell number and aggregation method. Using microwell arrays or microfluidic devices can generate uniformly sized embryoid bodies, the starting point for organoids [5] [15].
- Incorporate Bioengineering Tools: Utilize organoids-on-chips platforms. These microfluidic devices provide precise control over the microenvironment, including the spatiotemporal delivery of morphogens, which guides more consistent patterning [5].
- Automate Culture Processes: Implement robotic liquid handling systems for tasks like media changes and passaging. This minimizes manual handling errors and increases protocol consistency [5].
FAQ 4: What strategies can I use to introduce missing cell types, like microglia or vascular cells?
- Problem: Many standard organoid protocols generate models that lack critical non-epithelial or non-neuronal cell populations, such as the immune and vascular systems, limiting their physiological relevance [5] [15].
- Solutions:
- Assembloid Approach: Differentiate iPSCs separately into different organoid types (e.g., cortical organoids and microglia organoids) and then fuse them together to create a more complex "assembloid." This is effective for modeling interactions between brain regions and between neurons and microglia [15].
- Co-culture from the Start: Add pre-differentiated microglia or endothelial cells at the beginning of the organoid formation process, allowing them to integrate during self-organization. For example, co-culturing brain organoids with induced vascular organoids can lead to the formation of a functional blood-brain barrier [15].
Key Maturity Assessment Metrics
To systematically evaluate the success of maturation protocols, researchers should quantify a combination of structural, functional, and molecular parameters. The table below summarizes key benchmarks for brain organoids, which can be adapted for other organ types.
Table 1: Multidimensional Assessment of Brain Organoid Maturity
| Assessment Dimension | Key Metrics & Markers | Technical Methods |
|---|---|---|
| Structural Architecture | Cortical layering (SATB2, TBR1); Synaptic density (PSD-95, SYB2); Myelination (MBP) | Immunofluorescence (IF), Immunohistochemistry (IHC), Confocal Microscopy, Electron Microscopy [14] |
| Cellular Diversity | Presence of astrocytes (GFAP, S100β); Oligodendrocytes (O4, MBP); Microglia (IBA1) | IF, IHC, Flow Cytometry, scRNA-seq [14] |
| Functional Maturation | Synchronized network bursts; Gamma-band oscillations; Postsynaptic currents | Multi-electrode Arrays (MEA), Patch-Clamp Electrophysiology, Calcium Imaging [14] |
| Molecular & Metabolic Profile | Transcriptomic similarity to adult human tissue; Metabolic activity | scRNA-seq, RNA Sequencing, Metabolic Flux Assays [14] |
Experimental Protocols to Enhance Maturation
Protocol 1: Generating a Vascularized Brain Organoid via Co-culture
This protocol outlines the steps for fusing a brain organoid with a vascular organoid to create a vascularized assembloid.
- Workflow Diagram:
- Step-by-Step Methodology:
- Generate Brain Organoids: Differentiate your iPSC line into region-specific (e.g., cortical) brain organoids using a established protocol, typically involving neural induction with dual SMAD inhibition [15].
- Generate Vascular Organoids: In parallel, differentiate a separate batch of iPSCs into vascular organoids using a medium supplemented with VEGF (50-100 ng/mL) and BMP4 (25-50 ng/mL) to promote endothelial and perivascular cell fates [15].
- Fusion (Assemblation): At a predetermined stage (e.g., day 30-40), manually transfer one brain organoid and one vascular organoid into a single well of a low-adhesion 96-well plate. Allow them to contact each other and fuse over 24-48 hours in a minimal medium.
- Maturation Culture: Transfer the fused assembloid to a spinning bioreactor or an orbital shaker for long-term culture (≥60 days) to enhance nutrient exchange and support further maturation. Supplement the medium with factors that support both neural and vascular cell types.
- Validation: Confirm vascular network integration and functionality via immunofluorescence staining for CD31 (endothelial cells) and PDGFRβ (pericytes), and assess barrier properties with dextran permeability assays [14] [15].
Protocol 2: Active Bioengineering Acceleration Using Electrical Stimulation
Applying extrinsic physical cues can mimic in vivo activity and drive functional maturation.
- Workflow Diagram:
- Step-by-Step Methodology:
- Preparation: Generate brain organoids using your standard protocol and pre-culture them to a baseline stage of neural competency (e.g., day 60).
- Setup: For stimulation, consider embedding organoids in a conductive hydrogel (e.g., containing graphene or polypyrrole) to enhance charge delivery. Place the organoid-hydrogel construct onto a multi-electrode array (MEA) plate.
- Stimulation Regimen: Apply a chronic, low-intensity electrical stimulation protocol. A sample regimen is a biphasic pulse at 100 Hz for 2 hours per day over a period of 2-4 weeks. The specific parameters (frequency, duration, amplitude) should be optimized for your system [14].
- Real-time Monitoring: Use the same MEA system to periodically record electrophysiological activity throughout the stimulation period. Look for progressive increases in spike rate, burst frequency, and network synchronization complexity.
- Endpoint Analysis: After the stimulation period, fix the organoids for immunohistochemical analysis of synaptic markers (e.g., PSD-95) and glial maturation (e.g., GFAP), or process them for transcriptomic analysis [14].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Organoid Maturation
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Extracellular Matrix (Matrigel) | Provides a 3D scaffold mimicking the basal membrane; contains laminins, collagen, and growth factors. | Standard embedding matrix for supporting organoid growth and structure [16] [4]. |
| ROCK Inhibitor (Y-27632) | Improves cell survival after passaging and thawing by inhibiting apoptosis. | Add to medium for 24-48 hours after thawing cryopreserved organoids or after enzymatic dissociation [4]. |
| Recombinant Growth Factors (VEGF, BDNF) | Directs cell fate and maturation. VEGF promotes vascularization; BDNF supports neuronal survival and synaptic plasticity. | VEGF is used in vascular organoid protocols. BDNF can be added in later stages of neural culture to enhance maturation [14] [15]. |
| Small Molecule Inhibitors (e.g., A83-01) | A TGF-β receptor inhibitor that supports the growth of epithelial stem cells by preventing differentiation. | Common component in many culture media for gastrointestinal, hepatic, and pancreatic organoids [4]. |
| Multi-Electrode Arrays (MEAs) | Non-invasive platforms for long-term, electrophysiological monitoring of functional neural network activity. | Used to record spontaneous and evoked electrical activity from brain organoids to quantify functional maturity [14]. |
Engineering Complexity: Advanced Techniques to Build Better Organoids
Frequently Asked Questions
1. How can we improve the success rate of co-culturing tumor organoids with immune cells? The success of co-culture models depends on carefully replicating the natural stem cell niche. This involves using an optimized extracellular matrix (ECM), such as Matrigel, and a serum-free medium supplemented with essential growth factors. The specific combination and concentration of these factors—including EGF, Noggin, R-spondin-1, and Wnt3a—vary depending on the tumor type being cultured [17] [3]. Furthermore, the cellular components must be prepared correctly. For immune cells, a common approach involves using peripheral blood lymphocytes or peripheral blood mononuclear cells (PBMCs) from patients [17]. For Cancer-Associated Fibroblasts (CAFs), they can be isolated from tissue like colorectal liver metastases and are sometimes immortalized using lentiviral constructs encoding hTERT and BMI1 to extend their lifespan and improve experimental reproducibility [18].
2. What are the common signs of contamination in co-culture systems, and how can they be addressed? Contamination can manifest as sudden turbidity in the culture medium, unexpected pH shifts, or altered cell growth patterns [19]. Bacterial contamination often leads to rapid cell death and visible turbidity, while fungal contamination appears as filaments or spores under the microscope [19]. Mycoplasma contamination is more insidious, as cultures may appear normal while cell metabolism and gene expression are disrupted [19]. To address this, dispose of compromised cultures immediately and decontaminate equipment and workspaces thoroughly [19]. Prevention strategies include maintaining a strict cleaning schedule for incubators and biosafety cabinets, using dedicated reagent aliquots, and conducting routine mycoplasma testing [19].
3. Why is there little passage of liquid factors through the filter in a horizontal co-culture system? Insufficient passage of liquid factors through a filter in a co-culture plate can often be traced to two main issues. First, if the culture volume is too low, the area of the filter contacting the culture solution is reduced, significantly diminishing the co-culture effect [20]. Second, air can remain trapped in the pores of the filter, blocking the passage of factors. To resolve this, ensure the filter is properly pre-processed by washing with pure water and PBS after a one-minute treatment with 100% ethanol, and that it is sufficiently degassed before use [20].
4. What critical roles do tumor organoid-immune cell co-culture models play in advancing cancer diagnosis and treatment? These co-culture models serve as a powerful platform for personalized drug screening and the study of immunotherapy. They can be used to enrich tumor-reactive T cells from a patient's blood and assess their cytotoxic efficacy against the patient's own tumor organoids [17]. This provides a method to evaluate tumor cell sensitivity to T cell attack on an individual level, offering a theoretical basis for developing more effective immunotherapies and personalizing treatment plans [17].
Troubleshooting Common Experimental Challenges
Problem 1: Poor or Uncontrolled Cellular Organization in Co-culture
- Potential Cause: Lack of a proper foundational matrix that supports spontaneous cellular reorganization.
- Solution: Use an optimized ECM. Co-cultures of colon cancer organoids and CAFs embedded in a defined ECM can spontaneously form superstructures where collagen IV from CAFs creates a basement membrane, supporting the cancer cells in forming glandular structures that mimic in vivo histology [18].
Problem 2: Low Cell Viability in Co-culture
- Potential Cause: Suboptimal culture medium that does not support all cell types present.
- Solution: Adapt established organoid media to also support the growth of other cells, such as CAFs. Testing medium conditions with a cell viability assay (e.g., CellTiter-Glo 3D) can help identify the most suitable formulation [18].
Problem 3: Loss of Key Microenvironment Features in Long-Term Culture
- Potential Cause: Rapid loss of non-epithelial cells (like CAFs and immune cells) from traditional organoid cultures, leading to a loss of the mesenchymal phenotype and associated immunosuppressive signals.
- Solution: Employ robust, long-term co-culture systems. One study demonstrated that co-culturing colon cancer organoids with immortalized CAFs maintained a gene expression signature associated with aggressive, immunosuppressive cancer subtypes (like CMS4) and produced high levels of immunosuppressive factors such as TGFβ1, VEGFA, and lactate [18].
Problem 4: Low Success Rate in Establishing Patient-Derived Organoids
- Potential Cause: Delays in tissue processing or improper handling after collection, which reduce cell viability.
- Solution: Process tissue samples promptly. If same-day processing is not possible, use interim cold storage (6-10 hours with antibiotics in media at 4°C) or cryopreservation in an appropriate freezing medium (e.g., containing 10% FBS, 10% DMSO, and 50% L-WRN conditioned medium). Note that a 20-30% variability in live-cell viability can be expected between these two preservation methods [3].
Research Reagent Solutions
The table below summarizes key reagents and their functions in establishing co-culture systems.
| Reagent/Category | Specific Examples | Function in Co-culture System |
|---|---|---|
| Extracellular Matrix (ECM) | Matrigel, Collagen I, Collagen IV | Provides a 3D structural scaffold for cell growth and organization; Collagen IV is specifically produced by CAFs to form a basement membrane [17] [18]. |
| Essential Growth Factors | EGF, Noggin, R-spondin-1, Wnt3a, FGF | Creates a stem cell niche that supports the self-renewal and expansion of organoids and other cells; specific combinations are required for different tumor types [17] [3]. |
| Cell Culture Media | Advanced DMEM/F12, CAF Medium, Organoid Medium | Serves as the base nutrient medium; specialized formulations (e.g., serum-free CAF medium) are needed to support different cell populations in co-culture [3] [18]. |
| Cell Isolation Enzymes | Liberase TH | Digests tumor tissue for the isolation of primary cells, such as Cancer-Associated Fibroblasts (CAFs) [18]. |
| Cryopreservation Medium | FBS, DMSO, L-WRN Conditioned Medium | Preserves tissue samples or established cell lines for long-term storage and future use, maintaining cell viability [3]. |
Experimental Workflow for Establishing a Co-culture Model
The following diagram illustrates the key steps in creating a co-culture system that integrates tumor organoids, fibroblasts, and immune cells.
Key Protocols and Methodologies
1. Protocol for Establishing Patient-Derived Organoids from Colorectal Tissue [3]
- Tissue Procurement: Collect human colorectal tissue samples under sterile conditions immediately after colonoscopy or surgical resection. Transport in cold Advanced DMEM/F12 medium supplemented with antibiotics.
- Processing: Mechanically dissociate and enzymatically digest the tumor sample to obtain a cell suspension.
- 3D Culture: Seed the cell suspension onto a biomimetic scaffold like Matrigel. Use a growth factor-reduced medium supplemented with a specific cocktail of factors (e.g., EGF, Noggin, R-spondin-1) to minimize clone selection and support organoid growth.
- Cryopreservation: For long-term storage, cryopreserve tissue or organoids using a freezing medium such as 10% FBS, 10% DMSO in 50% L-WRN conditioned medium.
2. Protocol for Isolating and Immortalizing Cancer-Associated Fibroblasts (CAFs) [18]
- Isolation: Cut colorectal liver metastasis tissue into small pieces and digest using Liberase TH for 30 minutes at 37°C. Plate the cell suspension in a dish; after 30 minutes, wash away non-adherent cells. The adherent cells are CAFs, which are then cultured in a specialized CAF medium.
- Immortalization: To extend lifespan, immortalize low-passage primary CAFs (P1-P3) by transducing them with lentiviral constructs encoding hTERT and BMI1. Culture the transduced CAFs on a thin collagen coat.
3. Functional Assay: Assessing Immunosuppressive Capacity of Co-cultures [18]
- Conditioned Media Collection: Collect media from established co-cultures of tumor organoids and CAFs.
- T Cell Proliferation Assay: Use this conditioned media in a T cell proliferation assay. A potent inhibition of T cell proliferation indicates that the co-culture system is successfully recapitulating an immunosuppressive tumor microenvironment, a hallmark of aggressive cancer subtypes like CMS4 colon cancer.
Signaling Pathways in the Co-culture Microenvironment
The diagram below outlines the key signaling interactions between tumor cells, CAFs, and immune cells in a co-culture system.
Organoids, which are self-organizing three-dimensional (3D) cellular models derived from pluripotent stem cells, have become an invaluable tool for studying human development and disease. However, their utility is tempered by inherent limitations, including limited cellular diversity, lack of high-fidelity cell types, and limited maturation, which can restrict their reliability for modeling complex biological systems [7]. A key challenge is that traditional organoids form stochastic structures without external guidance and often fail to capture the dynamic interactions between different cell lineages and tissue regions that are crucial for physiological function [21] [22].
Assembloid technology has emerged as a transformative approach to bridge this gap. Assembloids are defined as self-organizing 3D systems formed by integrating multiple organoids or combining organoids with specialized cell types [22] [23]. This innovative platform enables researchers to model inter-tissue communication and inter-organ communication with greater physiological relevance, thereby addressing the critical limitation of cellular diversity in traditional organoid cultures. By recapitulating interactions between distinct tissue domains, assembloids provide deeper insights into tissue function and open new avenues for studying human development, disease mechanisms, and therapeutic development [24] [22].
Fundamental Concepts: Assembly Strategies and System Design
Categorization of Assembloid Approaches
The design of assembloid models can be systematically categorized into four primary assembly strategies, each engineered to replicate specific biological phenomena with high fidelity [23]:
- Multi-region assembloids: Combine organoids representing different brain regions or tissue compartments to study long-range interactions, such as thalamocortical pathways or forebrain interneuron migration [22] [25].
- Multi-lineage assembloids: Integrate cell types derived from different germ layers to model interactions between distinct lineages, such as neural crest cell migration or interactions between epithelial and mesenchymal components [22] [23].
- Multi-gradient assembloids: Incorporate spatial concentration gradients of signaling molecules to guide patterning and cell fate specification, mimicking developmental processes [23].
- Multi-layer assembloids: Stack or arrange different tissue layers to replicate the complex architecture of stratified organs or interfaces, such as the vascular-neural barrier [23].
The Scientist's Toolkit: Essential Reagents and Materials
Successful assembloid generation relies on a core set of research reagents and engineered materials. The table below details key components and their functions in assembloid protocols.
Table 1: Essential Research Reagent Solutions for Assembloid Generation
| Reagent/Material | Function/Application | Examples & Protocol Context |
|---|---|---|
| Human Induced Pluripotent Stem Cells (hiPSCs) | Foundational starting cell population for generating all organoid components; enables patient-specific disease modeling. | Used across all protocols; requires confirmation of chromosomal stability before organoid generation [21]. |
| Small Molecules & Growth Factors | Guide regional-specific differentiation by activating or inhibiting key developmental signaling pathways. | Wnt activators, Smad inhibitors, Retinoic Acid (RA), Sonic Hedgehog (SHH) agonists for patterning spinal motor neurons [21]. |
| Extracellular Matrix (ECM) Components | Provide 3D structural support and biochemical cues that promote cell survival, polarization, and self-organization. | Matrigel or other hydrogel systems; functionalized with Sulfo-SANPAH for covalent binding to device surfaces [21]. |
| Surface Modification Reagents | Create geometrically defined adhesion patterns to guide tissue morphogenesis and prevent nonspecific adhesion. | Pluronic-127 (hydrophilic barrier), Sulfo-SANPAH (heterobifunctional crosslinker) [21]. |
| Functional Assessment Tools | Enable real-time monitoring and quantification of functional integration and circuit activity. | Genetically encoded calcium indicators, microelectrode arrays, optogenetic actuators [21] [26]. |
Technical Guide: Protocols, Methodologies, and Troubleshooting
Detailed Protocol: Generating Human Motor Assembloids-on-a-Chip
This protocol leverages geometric engineering to create spatially patterned human motor assembloids, which model the neuromuscular junction [21].
Workflow Overview:
Step-by-Step Methodology:
Generation of Motor Neuron Spheroids (hMNS):
- Differentiate hiPSCs using a guided protocol with sequential addition of specific signaling molecules [21].
- Days 1-5: Treat with a Wnt activator and dual Smad inhibitors to induce neuroepithelial clusters. Confirm emergence of PAX6+, PAX7+, NESTIN+, and NEUROD1+ progenitor cells.
- Days 5-10: Add RA and SHH agonists while decreasing Wnt signaling to confer ventral identity. Verify generation of OLIG2+/NKX6.1+ motor neuron progenitors (MNPs) via immunofluorescence and qPCR. These MNPs can be passaged and cryopreserved at this stage.
- Days 16+: Enhance maturation with γ-secretase inhibitors and neurotrophic factors for at least 8 days. By day 24, confirm presence of mature motor neuron markers (ISL1, HB9, ChAT) and electrophysiological activity.
- Harvest MNP colonies and transfer to ultra-low attachment plates to form spheroids (target diameter: 250 ± 50 μm).
Device Fabrication and Surface Patterning:
- Fabricate a polydimethylsiloxane (PDMS) device featuring micro-patterns with semicircular endpoints to mimic natural muscle anchoring points [21].
- Critical Surface Modification:
- Treat the middle region of the device with Pluronic-127 to create a hydrophilic barrier that prevents nonspecific cell adhesion.
- Functionalize the semicircular anchoring points with the heterobifunctional crosslinker Sulfo-SANPAH. Upon UV photolysis, Sulfo-SANPAH covalently binds to the PDMS surface and subsequently links to ECM proteins in the culture, creating stable adhesion sites.
Generation of Anisotropic Skeletal Muscle Organoids (hSkM) and Assembly:
- Seed a cell-laden biomatrix (e.g., primary myoblasts or hiPSC-derived myogenic progenitors) into the pre-treated PDMS device.
- The middle tissue will progressively detach from the Pluronic-treated region and contract toward the functionalized anchoring points. Within 14 days, this process forms aligned myobundles along the anchoring axis.
- Place 3-4 pre-formed hMNS evenly distributed within the hSkM-containing device to promote integration.
Maturation and Functional Validation:
- Culture the assembloids for 3-5 weeks to allow for robust neuromuscular junction formation.
- Validate functional connectivity using a combination of optogenetics, microelectrode array mapping, and calcium imaging [21].
Detailed Protocol: Generating a Human Ascending Somatosensory Assembloid (hASA)
This advanced protocol integrates four distinct regional organoids to model the polysynaptic sensory pathway from the periphery to the brain [26].
Workflow Overview:
Step-by-Step Methodology:
Parallel Generation of Four Regional Organoids:
- Human Cortical Organoids (hCO) and Human Diencephalic Organoids (hDiO): Generate using established guided differentiation protocols with small molecules and growth factors [26].
- Human Dorsal Spinal Cord Organoids (hdSpO): Modify ventral spinal cord protocols by excluding ventralizing cues to promote dorsal identity. Confirm presence of HOXB4+ and PHOX2A+ projection neurons via immunostaining and scRNA-seq.
- Human Somatosensory Organoids (hSeO): Develop using a protocol that leverages neural crest differentiation cues. Validate by confirming a substantial population of POU4F1+/SIX1+ sensory neurons and SOX10+/FOXD3+ neural crest cells. Confirm expression of key sensory receptors (P2RX3, TRPV1) and functional responses to their specific agonists (α,β-methyleneATP, capsaicin) via calcium imaging.
Sequential Assembly:
- Fuse the generated organoids in a sequence that reflects the native biological pathway: hSeO → hdSpO → hDiO → hCO.
- This can be achieved by placing the organoids in close proximity in low-attachment wells or using supportive hydrogels to encourage natural migration and axonal projection between regions.
Circuit Validation and Functional Analysis:
- Connectivity Mapping: Use modified rabies virus tracing to demonstrate monosynaptic connectivity from sensory neurons to dorsal spinal cord neurons, and subsequently to thalamic neurons.
- Functional Response: Apply noxious chemical stimuli (e.g., capsaicin) to hSeO while performing multi-region calcium imaging to record coordinated neuronal activity across the entire assembloid.
- Synchrony Assessment: Use extracellular recordings and imaging to detect synchronized oscillatory activity across the four-component circuit. Pathogenic variants (e.g., in SCN9A/NaV1.7) can disrupt this synchrony, providing a readout for circuit-level dysfunction [26].
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ: Addressing Common Technical Questions
Q1: What are the primary advantages of using assembloids over co-culture systems or single organoids?
- Assembloids provide a modular yet integrated system that recapitulates the spatial organization and functional connectivity between distinct tissue regions or cell lineages. Unlike simple co-cultures, they support complex processes like cell migration, axon pathfinding, and synaptic integration within a 3D environment, offering a more physiologically relevant model for studying inter-cellular communication [22] [23].
Q2: How can I improve the reproducibility and reduce heterogeneity in my assembloid models?
- Incorporating bioengineering tools is key. Using geometrically engineered microdevices with defined surface chemistry, as in the motor assembloid-on-a-chip platform, standardizes tissue morphology and organization [21]. Furthermore, employing automated liquid handling systems for cell seeding, media changes, and differentiation factor addition can significantly minimize batch-to-batch variability [5].
Q3: My assembloids show poor cell viability in the core over time. What can I do?
- This is a common issue due to diffusive limitations. Strategies include:
- Reducing organoid size to ensure adequate oxygen and nutrient perfusion.
- Transitioning to slice culture, where assembloids are sectioned and maintained at an air-liquid interface, greatly improving viability in the internal regions [7] [5].
- Integrating vascularization strategies, either by incorporating endothelial cells during organoid formation or using microfluidic "organ-on-a-chip" platforms to enhance convective transport [5].
- This is a common issue due to diffusive limitations. Strategies include:
Troubleshooting Guide for Common Experimental Issues
Table 2: Troubleshooting Common Assembloid Generation and Culture Problems
| Problem | Potential Cause | Solution & Preventive Action |
|---|---|---|
| Incomplete or Failed Fusion | Organoids are not in sufficiently close contact; Mismatched developmental stages; Incorrect regional identity. | - Use low-attachment 96-well plates with V-shaped bottoms to force contact.\n- Carefully synchronize the differentiation timelines of individual organoids.\n- Validate regional identity (e.g., via qPCR/immunostaining for key markers) prior to fusion. |
| Lack of Functional Connectivity | Insufficient maturation time; Absence of necessary trophic support. | - Extend the maturation period post-fusion (can require 8+ weeks for neural circuits).\n- Ensure media contains essential neurotrophic factors (e.g., BDNF, GDNF, NT-3). |
| High Necrotic Core Formation | Limited diffusion of oxygen and nutrients into the 3D tissue mass. | - Culture assembloids in smaller sizes (<500 μm ideal).\n- Implement a slice culture methodology.\n- Use bioreactors or orbital shaking for improved medium perfusion. |
| Detachment from Microdevice | Inadequate or failed surface modification. | - Follow the surface pretreatment protocol strictly: ensure Pluronic-127 creates a non-adhesive middle region and Sulfo-SANPAH properly functionalizes the anchoring points [21]. A troubleshooting guide specific to the device is essential. |
| High Batch-to-Batch Variability | Stochastic self-organization; Manual protocol inconsistencies. | - Adopt engineered approaches (e.g., geometric confinement) to guide morphology.\n- Standardize cell seeding numbers and ECM composition.\n- Implement automated systems for reagent dispensing where possible [5]. |
Assembloid technology represents a significant leap forward in our ability to model the complex interactions that underlie human development, physiology, and disease. By providing a platform to integrate multiple cell types and tissue regions in a single, self-organizing system, assembloids directly address the critical challenge of limited cellular diversity in traditional organoid cultures. As demonstrated by their application in modeling intricate systems like the neuromuscular junction and the multi-synaptic sensory pathway, assembloids offer unprecedented insights into emergent properties that arise from inter-tissue communication [21] [26].
The future of assembloid research will likely focus on overcoming current limitations, such as enhancing vascularization to support larger and more mature tissues, improving cellular fidelity to better match in vivo counterparts, and incorporating immune cells and other stromal components to create even more holistic models [7] [5]. Furthermore, the integration of assembloids with advanced functional readouts, such as high-density electrophysiology and multi-omics profiling, will solidify their role as an indispensable platform for accelerating discovery in basic research and therapeutic development.
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: How can I introduce physiologically relevant mechanical forces, such as breathing motions, into my airway organoid culture?
Answer: Integrating mechanical stretch requires a chip design that incorporates flexible membranes and controlled actuation. A specialized airway-on-chip protocol uses a multi-layer microfluidic device with a porous flexible membrane made of PDMS [27]. Applying cyclic vacuum suction to side chambers adjacent to the cell culture chamber mimics breathing motions. This setup can be combined with dynamic fluid flow (0.02-0.1 µL/s) to simulate perfusion [27].
- Troubleshooting Guide:
- Problem: Inconsistent or non-uniform membrane stretching.
- Solution: Ensure the PDMS membrane and device layers are of uniform thickness. Verify the vacuum pressure is stable and evenly distributed across the side chambers. Using a computer-controlled pneumatic system improves reproducibility.
- Problem: Cell death or detachment under flow and stretch conditions.
- Solution: Start with lower flow rates and strain amplitudes (e.g., 5% linear stretch) and gradually increase to physiological levels (e.g., 10%) over several days to allow cells to acclimate [27].
FAQ 2: What is the best way to connect different tissue compartments to model organ interactions while maintaining tissue-specific microenvironments?
Answer: A successful connection requires a recirculating common media circuit that links discrete compartments. A user-friendly approach involves a 3D-printed multi-compartment chip coupled with a tubing-free impeller pump [28]. This design allows separate tissue samples (e.g., lymph node and an injection site) to be housed in individual, accessible compartments while being connected via a shared, recirculating flow.
- Troubleshooting Guide:
- Problem: Rapid degradation of soluble signals or insufficient concentration to elicit a response.
- Solution: Minimize the volume of the common media reservoir to increase the concentration of secreted factors. Use a pump that provides complete media recirculation to allow factors to accumulate [28].
- Problem: Cross-contamination of cells between compartments.
- Solution: Incorporate micro-engineered physical barriers or porous membranes (with pore sizes typically 0.4-8 µm) between compartments to allow molecular crosstalk while containing cells [29] [30].
FAQ 3: My organoid cultures in the chip lack maturity and key functional markers compared to in vivo tissue. What factors should I optimize?
Answer: Limited maturation often stems from an underdeveloped microenvironment. Beyond simple perfusion, you must incorporate organ-specific mechanical cues and complex 3D extracellular matrices (ECM).
- Troubleshooting Guide:
- Problem: Absence of polarization and mature mucociliary function in airway models.
- Solution: Apply a combination of perfusion, airflow, and cyclic stretch. Studies show this triple stimulation significantly accelerates mucociliary maturation, enhances polarization, and reduces baseline inflammatory secretion compared to static cultures [27].
- Problem: Poor structural organization and viability.
- Solution: Use natural hydrogels (e.g., Collagen, Matrigel) as ECM supports to provide essential biochemical cues [29] [31]. Optimize the channel geometry and flow rate using computational fluid dynamics models to ensure uniform nutrient and oxygen delivery [29].
FAQ 4: My microfluidic device is made from PDMS, but I'm concerned about small hydrophobic molecules being absorbed from the culture medium. What are my alternatives?
Answer: This is a known limitation of PDMS. Several strategies exist:
- Surface Coating: Treat PDMS surfaces with inert coatings like Parylene C to create a barrier that prevents absorption [28].
- Alternative Materials: Use thermoplastic polymers like PMMA (polymethyl methacrylate) or COP (cyclic olefin polymer), which are less absorptive and suitable for mass production [32].
- Advanced 3D Printing: Fabricate chips from PEGDA (poly(ethylene glycol) diacrylate) resins, which are biocompatible and do not suffer from the small molecule absorption issue [28].
Key Experimental Protocols
Protocol: Establishing a Biomimetic Airway-on-Chip with Perfusion and Mechanical Stretch
This protocol details the creation of an airway epithelium model that incorporates dynamic flow and breathing motions to accelerate maturation [27].
1. Chip Fabrication and Preparation:
- Materials: PDMS elastomer kit, vacuum-compatible membrane (e.g., flexible PDMS membrane), photo or soft lithography equipment for microfabrication [27].
- Procedure:
- Fabricate a multi-layer microfluidic device featuring a central cell culture channel, a porous flexible membrane, and two adjacent vacuum channels.
- Sterilize the assembled chip via autoclaving or UV irradiation.
- Coat the central membrane with a solution of human Collagen IV (e.g., 25 µg/mL) for 2 hours at 37°C to promote cell adhesion.
2. Cell Seeding and Culture:
- Materials: Primary human bronchial epithelial cells, differentiation media (e.g., PneumaCult-ALI medium).
- Procedure:
- Seed cells at a high density (e.g., 1-3 x 10^6 cells/cm²) onto the coated membrane.
- Allow cells to adhere under static conditions for 12-24 hours.
- Initiate perfusion of culture media at a low flow rate (0.02 µL/s) in the apical channel to create an air-liquid interface (ALI), removing the apical medium after 24-48 hours.
- Once confluent, apply cyclic mechanical stretch (10% linear strain, 0.15 Hz frequency) to simulate breathing using a computer-controlled vacuum system.
- Culture under these dynamic conditions for 3-4 weeks, with media changes every 2-3 days.
3. Functional Readouts for Maturation:
- Mucociliary Clearance: Track the movement of fluorescent beads placed on the epithelial surface.
- Cilia Beat Frequency: Measure using high-speed video microscopy.
- Transepithelial Electrical Resistance (TEER): Monitor regularly with microelectrodes to confirm barrier integrity.
- Immunofluorescence: Stain for tight junction proteins (e.g., ZO-1), ciliated cells (β-tubulin), and goblet cells (MUC5AC).
Workflow Diagram: Establishing a Biomimetic Airway-on-Chip
Protocol: Connecting Lymph Node and Injection Site in a Multi-Compartment Platform
This protocol enables the study of systemic immune responses, such as acute reactions to vaccination, by fluidically linking different tissue types [28].
1. Platform Assembly:
- Materials: 3D printer (DLP type), MiiCraft Clear resin or custom PEGDA resin, Parylene C coater, DC motor, magnets, PLA filament for pump housing.
- Procedure:
- 3D Print the Chip and Pump: Fabricate the multi-compartment device and removable mesh supports using a DLP 3D printer with a biocompatible resin (e.g., PEGDA or ITX-PEGDA).
- Apply Parylene C Coating: Deposit a ~1 µm film of Parylene C onto all printed parts via gas-phase deposition to enhance biocompatibility.
- Assemble Impeller Pump: Construct the tubing-free magnetic impeller pump. The pump sits in a reservoir on the chip and is driven by an external motor with a rotating magnet.
2. Tissue Preparation and Loading:
- Materials: Murine lymph nodes, mock tissue (e.g., collagen gel), complete cell culture media.
- Procedure:
- Prepare fresh lymph node slices (200-300 µm thick) using a vibratome.
- Load each tissue sample into its respective 3D-printed mesh support within the device compartment.
- Place the impeller bar into the common media reservoir and assemble the chip.
3. System Operation and Analysis:
- Procedure:
- Place the assembled chip onto the external pump platform and start the motor to initiate recirculating flow.
- "Vaccinate" by introducing antigen into the upstream injection site compartment.
- Run the experiment for the desired duration (e.g., 24 hours).
- For analysis, simply remove the mesh supports containing the tissues for imaging, flow cytometry, or RNA sequencing.
Workflow Diagram: Multi-Compartment Lymph Node Chip Assembly
Data Presentation Tables
Table 1: Comparison of Biomaterials for Organ-on-Chip Fabrication
| Biomaterial | Key Advantages | Key Limitations / Challenges | Ideal Application Examples |
|---|---|---|---|
| PDMS [33] [31] | Transparent, gas-permeable, easy to fabricate, low cytotoxicity. | Absorbs small hydrophobic molecules, can be difficult to sterilize for reuse. | General-purpose OoC, barrier models (e.g., gut, lung), models requiring optical clarity. |
| PEGDA [28] | Biocompatible, tunable mechanical properties, does not absorb small molecules. | Requires 3D printing expertise, may require surface coating for optimal cell adhesion. | Customizable, complex 3D architectures, multi-compartment chips. |
| Collagen [31] | Superior biocompatibility, enzymatic biodegradability, native cell-adhesion sites. | Lacks mechanical strength when hydrated, batch-to-batch variation. | Hydrogel matrices for 3D cell culture, Gut-on-a-Chip, Bone-on-a-Chip. |
| PMMA/COP [32] | High optical clarity, rigid, low absorption of small molecules, suitable for mass production. | Not gas-permeable, less flexible than PDMS, requires hot embossing/injection molding. | High-throughput screening chips, commercial-scale production. |
Table 2: Parameters for Simulating Physiological Mechanical Forces in OoCs
| Organ System | Mechanical Force | Typical In Vivo Value | Engineered OoC Parameters | Biological Impact |
|---|---|---|---|---|
| Lung/ Airway [27] | Cyclic Stretch (Breathing) | 10-15% linear strain | 5-10% linear strain, 0.15-0.3 Hz | Accelerated mucociliary maturation, reduced inflammatory signaling, proper polarization. |
| Vasculature [29] [32] | Fluid Shear Stress (Blood Flow) | 1-30 dyn/cm² | 0.5-20 dyn/cm² (controlled via channel geometry & flow rate) | Enhanced endothelial cell alignment, barrier function, and differentiation. |
| Intestine [29] | Peristalsis-like Motion & Flow | Rhythmic contractions | Cyclic deformation (e.g., 10-15%, 0.1-0.2 Hz) combined with flow | Improved villi formation, enhanced barrier integrity, and cell differentiation. |
| General (via Compression) [29] | Mechanical Compression | Varies by tissue (e.g., bone, cartilage) | Applied static or cyclic pressure via actuation | Mimics tissues that respond to compression loads. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for OoC Integration
| Item | Function / Purpose | Example in Context |
|---|---|---|
| PDMS (Polydimethylsiloxane) | The most common elastomer for soft lithography of microfluidic chips; transparent, gas-permeable, and flexible [33] [31]. | Used to fabricate the flexible membranes and main body of the breathing lung chip [27]. |
| PEGDA Resin (Poly(Ethylene Glycol) Diacrylate) | A photopolymer resin for 3D printing custom, complex chip architectures with high biocompatibility [28]. | Used to create the multi-compartment chip and impeller for the lymph node-on-chip platform [28]. |
| Parylene C | A chemically inert, biocompatible polymer deposited as a thin, conformal coating via vapor phase. Prevents small molecule absorption and improves biocompatibility of 3D-printed parts [28]. | Used to coat 3D-printed PEGDA chips to ensure cell viability and prevent compound absorption during immune response studies [28]. |
| Natural Hydrogels (Collagen, Matrigel) | Provide a 3D extracellular matrix (ECM) environment that supports cell embedding, organoid growth, and complex tissue morphogenesis [29] [31]. | Collagen IV used to coat the airway chip membrane for cell adhesion. Collagen I used as a scaffold for 3D tissue models [27]. |
| Microfluidic Impeller Pump | Provides recirculating fluid flow without complex external tubing, enabling easy-to-use multi-tissue connectivity [28]. | The magnetic impeller pump drives common media circulation between the lymph node and injection site compartments [28]. |
| Porous Membranes | Create tissue-tissue interfaces (e.g., between epithelium and endothelium) to study barrier function, absorption, and trans-cellular transport [29]. | A porous PDMS membrane in the lung chip separates alveolar epithelial cells from microvascular endothelial cells [29]. |
FAQs: Addressing Common Challenges in Vascularized Organoid Generation
FAQ 1: Why is vascularization critical for advanced organoid models?
Vascularization is essential to overcome the diffusion limit of oxygen and nutrients, which is approximately 150-400 µm [34] [35]. Without a functional vascular network, organoids developing beyond this size experience central cell necrosis and form an apoptotic core, which restricts further growth and maturation [34] [35]. Incorporating vasculature enables the development of more physiologically relevant, larger, and functionally mature organoids that better mimic in vivo conditions, such as the acquisition of improved blood-brain barrier characteristics in brain organoids [34].
FAQ 2: What are the primary strategies for introducing vasculature into organoids?
The three predominant strategies are:
- Co-culture with Endothelial Cells: Directly mixing organoid-forming cells with endothelial cells (e.g., HUVECs) to promote self-organization into vascular networks [34] [36].
- Incorporation of Mesodermal Progenitor Cells (MPCs): Co-culturing with bipotent MPCs, which can differentiate into both endothelial cells and pericytes/smooth muscle cells, leading to the formation of more structured, stable vessels [2].
- Genetic Induction: Engineering stem cells to overexpress pro-vascular transcription factors (e.g., ETV2) to drive the formation of vascular networks within the organoid [34] [36].
FAQ 3: Our co-cultured endothelial networks are unstable and regress over time. What can be done?
Network instability often stems from a lack of pericyte coverage and insufficient pro-angiogenic signaling. To address this:
- Incorporate supporting stromal cells, such as mesenchymal stem cells (MSCs) or fibroblasts, which can stabilize the nascent vessels [34] [35].
- Utilize Mesodermal Progenitor Cells (MPCs). MPCs can differentiate into both endothelial cells and pericytes, which are integral to forming a mature vessel wall with a basement membrane, thereby enhancing stability [2].
- Ensure optimal cytokine delivery. Supplementing culture media with Vascular Endothelial Growth Factor (VEGF) and other angiogenic factors is crucial for endothelial cell survival and network maintenance [35].
FAQ 4: How can I validate the functionality of the vascular networks in my organoids?
Functionality can be assessed through a combination of markers and functional assays:
- Molecular Markers: Confirm the presence of endothelial cells using immunohistochemistry for CD31 (PECAM-1) and von Willebrand Factor (vWF) [35] [2].
- Structural Analysis: Evaluate vessel architecture, including lumen formation (e.g., via electron microscopy), presence of endothelial cell-cell junctions, and association with α-smooth muscle actin (αSMA)+ pericytes [35] [2].
- Perfusion Assays: The gold standard for functionality. This can be demonstrated in vitro using microfluidic devices that show perfusion [36], or in vivo by transplanting the organoid and observing the connection between host and organoid vessels and the presence of host blood cells within the human vessels [2].
Troubleshooting Guides
Poor Vascular Network Formation
| Symptom | Possible Cause | Solution |
|---|---|---|
| Sparse or no endothelial network | Lack of pro-angiogenic signals | Supplement with VEGF and FGF in the culture medium [34] [35]. |
| Incorrect cell ratio in co-culture | Optimize the ratio of organoid cells to endothelial/MPCs; a starting point is a 1:1 ratio [2]. | |
| Suboptimal mechanical/ECM environment | Use a natural hydrogel (e.g., Matrigel, fibrin/collagen) that supports endothelial morphogenesis [35] [36]. |
Necrotic Core in Vascularized Organoids
| Symptom | Possible Cause | Solution |
|---|---|---|
| Central necrosis despite vascularization | Vasculature is not perfusable | Implement microfluidic (organ-on-a-chip) platforms to provide fluid flow and shear stress, which promotes the formation of perfusable lumen [37] [38] [36]. |
| Vascular network is underdeveloped | Apply hypoxic conditioning (2% O₂) to upregulate HIF-1α and enhance VEGF expression, boosting angiogenesis [2]. |
Key Experimental Protocols
Protocol: Vascularization via Mesodermal Progenitor Cell (MPC) Incorporation
This protocol is adapted from the work of et al., which details the generation of complex vascularized human organoids [2].
Workflow Overview:
Detailed Reagents and Steps:
Induction of Mesodermal Progenitor Cells (MPCs):
- Starting Cells: Human induced pluripotent stem cells (hiPSCs).
- Key Reagents: CHIR99021 (GSK3β inhibitor) to activate Wnt signaling, and BMP4 to promote lateral plate mesodermal fate.
- Procedure: Culture hiPSCs with these factors for 3 days. Success is indicated by the appearance of ~80% Brachyury+ cells, marking successful MPC induction [2].
Generation of Organoid and MPC Spheres:
- Generate organoid spheres (e.g., neural, tumor) according to standard protocols for your target tissue.
- Simultaneously, form spheres from the induced MPC population.
Co-culture and Fusion:
- Method: Combine the organoid spheres and MPC spheres in a 1:1 ratio in a low-attachment plate to allow for aggregation and fusion.
- Environmental Cue: For tumor organoids, subsequent culture under hypoxic conditions (2% O₂) can help distribute the vascular network throughout the organoid [2].
Long-term 3D Culture:
- Transfer the fused aggregates to a suspension culture on a rocking platform to enhance nutrient exchange.
- Culture can be maintained long-term (e.g., over 60 days for neural organoids) to allow for advanced maturation of both the tissue and its vascular network [2].
Validation and Analysis:
- Immunohistochemistry: Stain for CD31 (endothelial cells) and αSMA (pericytes/smooth muscle cells) to confirm structured vessel formation.
- Electron Microscopy: Use to identify ultrastructural features like lumens, basement membranes, and endothelial junctions.
- Functional Testing: Treat with anti-angiogenic drugs (e.g., Sorafenib) to confirm network responsiveness, or perform transplantation assays to demonstrate connection to a host circulatory system [2].
Protocol: Vascularization via Genetic Induction (ETV2 Overexpression)
This protocol is based on the strategy used by Cakir et al. to generate vascularized human cortical organoids [34] [36].
Key Steps:
- Genetic Engineering: Engineer human pluripotent stem cells (hPSCs) to inducibly or constitutively express the transcription factor ETV2.
- Organoid Differentiation: Initiate standard cortical organoid differentiation protocols from the engineered hPSCs.
- Induction of Vascular Fate: Activate ETV2 expression at the appropriate developmental timepoint. This reprograms a subset of cells within the organoid towards an endothelial cell fate.
- Maturation: Continue culture to allow for the self-organization of these endogenously generated endothelial cells into vascular networks, which has been shown to enhance organoid maturity and model features like the blood-brain barrier [34] [36].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Vascularized Organoid Generation
| Reagent | Function | Example Usage |
|---|---|---|
| Endothelial Cells | Form the inner lining of blood vessels. | Human Umbilical Vein Endothelial Cells (HUVECs) used in co-culture strategies [34]. |
| Mesodermal Progenitor Cells (MPCs) | Bipotent precursor that gives rise to both endothelial cells and pericytes. | Co-cultured with neural or tumor spheroids to generate structured, stable vasculature [2]. |
| VEGF (Vascular Endothelial Growth Factor) | Critical cytokine for endothelial cell survival, proliferation, and angiogenesis. | Added to culture medium to promote vascular network formation and maintenance [35]. |
| Matrigel / Fibrin/Collagen Hydrogels | Natural extracellular matrix (ECM) mimics that support 3D cell growth and vascular morphogenesis. | Used as the 3D scaffold for embedding cells in organoid and organ-on-a-chip cultures [35] [36] [2]. |
| CHIR99021 (GSK3β inhibitor) | Activates Wnt/β-catenin signaling pathway. | Used to direct differentiation of hiPSCs towards mesodermal progenitor fates [34] [2]. |
| CD31/PECAM-1 Antibody | Biomarker for identifying endothelial cells via immunostaining. | Used to visualize and quantify the formed vascular networks [35] [2]. |
| Microfluidic Device (Organ-on-a-Chip) | Provides perfusable culture environment with fluid flow and shear stress. | Enables the formation of perfusable vascular lumens and enhances nutrient delivery to organoids [37] [38] [36]. |
A technical guide for enhancing organoid diversity through defined microenvironments.
This technical support center addresses the critical challenge of limited cellular diversity in organoid cultures by providing practical solutions for transitioning from poorly-defined matrices, like Matrigel, to synthetic designer hydrogels. This shift is fundamental for establishing controlled, reproducible microenvironments that can guide complex cell signaling and support the co-differentiation of multiple cell lineages.
Troubleshooting Guide: Common Challenges with Synthetic Hydrogels
Problem 1: Poor Organoid Formation or Viability
Potential Causes and Solutions:
Cause: Lack of Essential Cell Adhesion Motifs.
- Solution: Incorporate integrin-binding peptides into the hydrogel backbone. The RGD peptide is the most common, but other motifs like IKVAV (from laminin) or GFOGER (from collagen) can provide more specific interactions [39].
- Protocol: Conjugate peptides to polymers (e.g., PEG) using standard chemical coupling (e.g., carbodiimide chemistry) or Michael addition reactions before crosslinking. A final concentration of 0.5-2.0 mM of RGD in the hydrogel is a typical starting point [39].
Cause: Incorrect Matrix Stiffness (Elastic Modulus).
- Solution: Tune the hydrogel's elastic modulus to match the target tissue. This is primarily achieved by varying the crosslinking density or polymer concentration [39] [40].
- Protocol:
- For a PEG-DA hydrogel, the modulus can be adjusted by changing the polymer weight percentage (e.g., 5-15%) or the concentration of the crosslinker.
- Validate stiffness using rheometry or atomic force microscopy (AFM). The table below provides target stiffness ranges for different organoid types.
Table 1: Target Hydrogel Stiffness for Organoid Cultures
| Organoid Type | Target Stiffness (Elastic Modulus) | Supporting References |
|---|---|---|
| Brain / Neural | 0.1 - 0.5 kPa | [39] [41] |
| Intestinal | 1 - 5 kPa | [41] |
| Hepatic (Liver) | ~5 kPa | [41] |
| Pancreatic | 2.5 - 7 kPa | [42] |
| Renal (Kidney) | 2 - 6 kPa | [42] |
| Bone | 10 - 50 kPa | [39] |
Problem 2: Limited Organoid Maturation and Complexity
Potential Causes and Solutions:
Cause: Static Mechanical Environment.
Cause: Absence of Critical Morphogen Signaling.
- Solution: Engineer hydrogels for the sustained and localized release of growth factors.
- Protocol: Covalently tether growth factors (e.g., EGF, Wnt, BMP) to the hydrogel network via protease-cleavable linkers. Alternatively, use hydrogel systems that can sequester heparin-binding proteins [39]. For example, intestinal organoids require precise Wnt signaling activation, which can be achieved by incorporating Wnt agonists into the matrix [39].
Problem 3: Batch-to-Batch Variability and Low Reproducibility
Potential Cause and Solution:
- Cause: Inconsistent Polymer Functionalization or Crosslinking.
- Solution: Adopt rigorous quality control (QC) measures for all hydrogel precursors.
- Protocol:
- Characterize Polymer Modification: Use nuclear magnetic resonance (NMR) or Fourier-transform infrared spectroscopy (FTIR) to confirm the degree of functionalization (e.g., acrylation, methacrylation, or peptide conjugation) for each synthesized batch.
- Standardize Crosslinking: Precisely control initiator concentrations (e.g., Irgacure 2959 for UV crosslinking) and light exposure time and intensity. Use rheometry to confirm the final storage modulus (G') of every hydrogel batch before cell culture experiments [40].
Frequently Asked Questions (FAQs)
Q1: Why should I switch from Matrigel to a defined synthetic hydrogel? Matrigel suffers from significant drawbacks, including poorly defined chemical composition, batch-to-batch variation, and limited tunability [39] [42]. These factors hinder reproducibility and make it difficult to elucidate specific ECM cues that drive organoid development. Defined synthetic hydrogels offer precise control over biochemical (adhesion ligands, growth factors) and biophysical (stiffness, viscoelasticity) properties, enabling more controlled and reproducible experiments [39] [43].
Q2: How can I make my hydrogel viscoelastic to better mimic living tissues? Viscoelasticity can be engineered through crosslinking chemistry. Use:
- Physical (reversible) crosslinks: based on ionic interactions, hydrogen bonds, or hydrophobic interactions [39] [40].
- Dynamic covalent chemistry: such as hydrazone bonds or boronate esters.
- Supramolecular polymers: like those using cucurbituril-based host-guest interactions [40]. These bonds can break and re-form, allowing the network to dissipate energy and flow, which is crucial for organoid expansion and maturation [41].
Q3: My organoids are not forming the correct 3D structure. What matrix parameters should I check? First, verify the stiffness against known tissue values (see Table 1). Second, ensure the hydrogel allows for cell-mediated remodeling. This requires incorporating motifs degradable by cell-secreted enzymes (e.g., MMPs) [39]. A non-degradable, static matrix will physically constrain organoid growth and self-organization.
Q4: Can synthetic hydrogels support the co-culture of multiple cell types to improve diversity? Yes, this is a key advantage. By presenting specific adhesion motifs and mechanical cues, synthetic matrices can be designed to support niche cells alongside stem cells. Furthermore, spatial patterning of biochemical cues using light-based techniques (e.g., two-photon patterning) can guide the organization of different cell types within the 3D structure [44], directly addressing the challenge of limited cellular diversity.
Experimental Protocols
Protocol 1: Formulating a Tunable PEG-Based Hydrogel for Intestinal Organoids
This protocol outlines the synthesis of a defined, MMP-degradable hydrogel to support intestinal organoid growth and crypt-villus structure formation.
1. Materials (The Scientist's Toolkit)
Table 2: Key Research Reagent Solutions
| Item | Function / Explanation |
|---|---|
| 8-arm PEG-Norbornene (PEG-NB) | Synthetic polymer backbone; provides a highly defined and tunable network. |
| MMP-sensitive Peptide Crosslinker (e.g., KCGPQG↓IWGQCK) | Forms degradable crosslinks; allows cells to remodel the matrix via secreted metalloproteinases (MMPs). |
| CRGDS Peptide | Cell adhesion ligand; promotes integrin-mediated cell attachment and survival. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Photoinitiator; generates radicals under UV/violet light to initiate crosslinking. |
| Recombinant Wnt-3A or R-spondin | Key growth factors for intestinal stem cell maintenance; can be tethered to the network. |
2. Hydrogel Preparation and Cell Encapsulation
- Step 1: Polymer Solution Preparation. Dissolve PEG-NB, MMP-sensitive peptide, and CRGDS peptide in a cell-compatible buffer (e.g., PBS). Sterilize the solution by passing it through a 0.22 µm filter.
- Step 2: Initiator Addition. Add the photoinitiator LAP to the polymer solution at a final concentration of 0.05% (w/v). Protect from light.
- Step 3: Cell Mixing. Centrifuge your intestinal stem cell suspension and resuspend the cell pellet in the polymer solution to achieve the desired cell density (e.g., 1-10 million cells/mL).
- Step 4: Crosslinking. Pipette the cell-polymer mixture into the desired culture vessel (e.g., a mold or multi-well plate). Expose to 365-405 nm light (5-10 mW/cm²) for 1-5 minutes to form the gel.
- Step 5: Culture. Overlay with complete intestinal organoid medium containing growth factors. Change the medium every 2-3 days.
Protocol 2: Modulating Hydrogel Stiffness via Crosslinking Density
This general protocol describes how to systematically vary hydrogel stiffness, a critical parameter for directing stem cell differentiation and organoid maturation.
1. Materials
- Base polymer (e.g., 4-arm PEG-Acrylate, Gelatin-Methacryloyl).
- Crosslinker (e.g., Dithiothreitol (DTT) for PEG-Acrylate, or the photoinitiator LAP for Ge-MA).
- Photoinitiator (if using light-activated crosslinking).
2. Method
- Prepare separate batches of your polymer solution at different weight-to-volume percentages (e.g., 5%, 7.5%, 10%). Higher polymer concentrations generally yield stiffer gels.
- For a constant polymer concentration, the crosslinker ratio can be adjusted. For a PEG-Acrylate system crosslinked with DTT, vary the molar ratio of thiol groups (on DTT) to acrylate groups (on PEG) from 0.5 to 1.0. A higher ratio increases crosslinking density and stiffness.
- Characterization: After gelation, measure the elastic modulus (G' or Young's Modulus) of each formulation using a rheometer. This creates a standard curve that correlates your formulation parameters with the resulting mechanical property.
Signaling Pathways and Experimental Workflows
Diagram 1: Mechanosensing in Organoid Development
This diagram illustrates the key signaling pathway (YAP/Notch) through which hydrogel mechanics influences cell fate and organoid development, a core concept in using synthetic matrices to control diversity.
Diagram 2: Workflow for Designing a Defined Hydrogel Experiment
This flowchart outlines the logical process for designing an experiment using synthetic hydrogels to address a specific biological question in organoid research.
Solving for Scalability and Reproducibility in Complex Organoid Cultures
Core Challenge: Understanding and Tackling Heterogeneity in Organoid Cultures
Organoids are three-dimensional, multicellular structures that mimic the architecture and function of real human organs, making them invaluable tools for disease modeling, drug screening, and personalized medicine [45] [46]. A significant hurdle in organoid research is limited cellular diversity, where the organoids fail to fully recapitulate the complete spectrum of cell types and complex cellular interactions found in native human tissues [23] [45]. This heterogeneity, or unwanted variability, between individual organoids can stem from several factors:
- Variable and Complex Construction Protocols: The process of building organoids involves screening numerous matrix materials, growth factors, and culture conditions, which often relies on manual techniques and literature speculation, leading to low success rates and high batch-to-batch variability [45].
- Limitations of Manual Culture: Manual methods are labor-intensive, require intervention during weekends and holidays over cultures that can last more than 100 days, and introduce variability through inconsistent handling, increasing the risk of contamination and unreliable downstream assays [47].
- Lack of Vascularization and Systemic Cues: Many organoid systems lack a functional vasculature, which limits nutrient delivery and organoid size, and they often miss key cellular interactions, such as those with immune cells, constraining their physiological relevance [23] [46].
Troubleshooting Guide: Addressing Common Experimental Challenges
This guide helps diagnose and resolve specific issues related to organoid heterogeneity and culture reproducibility.
Table 1: Troubleshooting Organoid Culture Variability
| Problem | Potential Cause | Solution |
|---|---|---|
| High variability in organoid size and morphology | Inconsistent manual feeding schedules; Static culture conditions leading to necrotic cores. | Implement automated feeding on a fixed schedule using a liquid handler; Use a rocking incubator for constant motion to ensure even nutrient distribution [47]. |
| Low reproducibility between experimental batches | Animal-derived matrix materials (e.g., Matrigel) with inherent variability; Subjectivity in morphological assessment. | Adopt automated platforms for standardized handling; Use AI-driven image analysis for objective, quantitative assessment of organoid structure [45]. |
| Limited cellular diversity within organoids | Culture conditions that favor specific progenitor cells; Lack of multiple cell lineages. | Employ multi-lineage assembly strategies to integrate different cell types; Use AI to screen and optimize growth factor combinations for diverse differentiation [23] [45]. |
| Insufficient organoid maturation or functionality | Absence of key physiological cues and gradients; Short-term culture protocols. | Implement multi-gradient assembly strategies to create microenvironmental niches; Extend culture times with automated systems to maintain long-term viability [23]. |
Frequently Asked Questions (FAQs)
Q1: How can automation specifically reduce heterogeneity in my brain organoid cultures? Automation directly addresses key sources of variability. Automated systems ensure consistent feeding and media exchange on a strict schedule, including weekends and holidays, which is crucial for cultures lasting over 100 days [47]. They integrate rocking incubators that provide constant motion, preventing the formation of necrotic cores and ensuring even nutrient distribution—a critical factor for healthy brain organoid development [47]. One study demonstrated that automation can reduce manual workload by up to 90% while significantly improving reproducibility [47].
Q2: Can AI really help if I'm already using standardized protocols? Yes, AI enhances standardized protocols by adding a layer of intelligent optimization and analysis. While standard protocols provide a baseline, AI can:
- Rapidly Screen Construction Strategies: Machine learning algorithms can analyze vast combinations of matrix materials, growth factors, and culture conditions to identify the optimal recipe for generating more complex and representative organoids faster than traditional trial-and-error [45].
- Provide Cost-Effective, High-Content Analysis: AI, particularly convolutional neural networks (CNNs), can be trained to analyze simple bright-field images of organoids and non-invasively predict their differentiation status, identify morphological features, and detect functional outcomes, reducing reliance on expensive and destructive staining methods [45].
Q3: What are assembloids, and how do they address the problem of limited cellular diversity? Assembloids are the next evolution of organoid technology. They are self-organizing 3D systems formed by integrating multiple organoids or different cell types [23]. They are specifically designed to combat limited cellular diversity by modeling inter-tissue and inter-organ communication. Assembly strategies are categorized as follows:
- Multi-region: Connects organoids modeling different brain areas (e.g., cortical and striatal) to study circuit integration [23].
- Multi-lineage: Combines organoids of different lineages (e.g., neural and skeletal muscle) to model complex interactions [23].
- Multi-gradient: Introduces spatial concentration gradients of morphogens to guide patterned tissue development [23].
- Multi-layer: Creates layered structures, such as a vascular network within an organoid, to enhance nutrient delivery and maturity [23].
Q4: Are organoids reliable enough to replace animal models in drug development? Organoids are not yet a complete replacement but are becoming indispensable complementary tools. Their key advantages include human specificity, which avoids the pitfalls of interspecies variation, and the ability to model patient-specific diseases for personalized medicine [46]. Regulatory changes, like the U.S. FDA Modernization Act 2.0, now allow the use of validated non-animal models, including organoids, in preclinical drug development [46]. However, challenges remain, such as the lack of full immune system integration and complex organ-organ interactions found in whole organisms. The future lies in integrating data from organoids, animal studies, and computational models [46].
Experimental Protocols for Enhanced Reproducibility
Protocol 1: Automated Brain Organoid Culture and Monitoring
This protocol utilizes the CellXpress.ai Automated Cell Culture System to minimize manual variability [47].
- Seeding and Initial Culture: Begin with induced pluripotent stem cells (iPSCs). The automated system handles seeding into matrix-coated plates.
- Differentiation and Dynamic Culture: Initiate differentiation protocols with timed delivery of growth factors. The system transfers plates to the rocking incubator, which provides continuous motion for optimal nutrient availability and organoid maturation.
- Automated Feeding: The liquid handler performs media exchanges on a pre-programmed, fixed schedule (e.g., daily), ensuring consistency without weekend or holiday gaps.
- Automated Imaging and Analysis: At defined intervals, the integrated imager captures full-well images of the organoids. AI-driven software analyzes these images for key morphological milestones (e.g., bud formation around day 10) and provides quantitative data on size, number, and structure.
Protocol 2: AI-Assisted Optimization of Organoid Construction
This protocol uses machine learning to refine the factors that influence organoid composition [45].
- Data Collection: Compile a historical dataset from previous organoid experiments, including details on matrix elasticity, porosity, concentrations of growth factors (WNTs, BMPs, etc.), and the resulting cellular outcomes (e.g., cell type ratios from single-cell RNA sequencing).
- Model Training: Train a machine learning model (e.g., a random forest or neural network) on this dataset. The model learns the complex, non-linear relationships between the input culture parameters and the desired organoid characteristics.
- Prediction and Validation: Use the trained model to predict the most promising combination of culture parameters for achieving a specific cellular diversity goal. Test these AI-suggested conditions in vitro.
- Iterative Refinement: Feed the results from the validation experiments back into the dataset to continuously improve the model's accuracy and predictive power.
Key Signaling Pathways and Workflows
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Reagent Solutions for Advanced Organoid Research
| Item | Function in Research | Application Context |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | The foundational starting material for generating patient-specific organoids. | Sourced from patients to create personalized disease models for drug testing and study of genetic disorders [47] [46]. |
| Synthetic Hydrogels | Defined, reproducible extracellular matrix (ECM) mimic to support 3D growth. | Replaces variable, animal-derived Matrigel to reduce batch-to-batch variability and improve reproducibility of organoid formation [45]. |
| Rocking Incubator | Provides constant, dynamic motion to organoid cultures. | Integrated into automated systems to ensure even nutrient/oxygen distribution, prevent necrotic cores, and enhance organoid maturation [47]. |
| Growth Factor Cocktails (e.g., WNTs, BMPs) | Signaling molecules that direct stem cell differentiation into specific lineages. | Used in multi-gradient assembloid strategies to create patterned tissues; concentrations are optimized using AI screening [23] [45]. |
| AI-Enabled Image Analysis Software | Automated, quantitative assessment of organoid morphology and differentiation from microscopy images. | Non-destructively monitors organoid quality; a CNN model (e.g., DenseNet121) can predict kidney organoid differentiation from bright-field images [45]. |
Technical Support Center
Troubleshooting Guides
Guide 1: Addressing Central Necrosis in Mature Organoids
Problem: My organoids develop a necrotic core after prolonged culture (often beyond 30 days), characterized by central cell death, which compromises cellular diversity and experimental reproducibility.
Primary Cause: The core issue is diffusion limitation. As organoids grow beyond 400-500 μm in diameter, oxygen and nutrients cannot efficiently reach the center, and waste products cannot be removed, leading to hypoxia and necrosis [48] [14].
Solution Pathway:
Recommended Actions:
- Implement Regular Cutting: For organoids already in culture, use a sterile, 3D-printed cutting jig to slice them into smaller fragments every 3 weeks. This instantly reduces diffusion distances and has been shown to improve cell proliferation and extend culture viability up to five months [49] [50].
- Transition to Dynamic Culture: Move organoids from static culture to a system with constant motion. Integrate a rocking incubator or orbital shaker to ensure even nutrient distribution and prevent settling, which reduces necrotic core formation [47] [48].
- Evaluate Architectural Design: For future experiments, consider engineering self-assembling organoids with non-spherical morphologies. The cup-shaped Organoid-Tissue Module (Organoid-TM) has demonstrated enhanced surface-area-to-volume ratio, improving oxygen and nutrient diffusion in millimeter-scale structures [51].
Guide 2: Managing Variability and Immaturity in Long-Term Cultures
Problem: After implementing strategies to reduce necrosis, my organoids show high batch-to-batch variability and fail to reach desired mature, adult-like stages, limiting their use in disease modeling.
Primary Cause: Inconsistent culture conditions and the lack of a physiologically complex microenvironment (e.g., missing vascularization, biomechanical cues, and multi-cellular interactions) hinder synchronized maturation and functional development [52] [14].
Solution Pathway:
Recommended Actions:
- Adopt Organoid-on-Chip Technology: Culture organoids in a microfluidic chip. The perfusable network mimics vascular flow, enabling precise control over the microenvironment, delivering nutrients, and removing waste actively, which promotes maturation and reduces heterogeneity [52].
- Incorporate Vascularization Cues: Introduce endothelial cells or use protocols that encourage the formation of vascular-like structures within the organoids. This is critical for achieving organoids larger than 800 μm without necrosis and for modeling blood-brain barrier function in neural organoids [48] [14].
- Automate the Culture Process: Implement an automated cell culture system. Automation ensures consistent feeding and handling (even on weekends), standardizes imaging, and drastically reduces manual errors and contamination, leading to higher reproducibility and data quality [47].
Detailed Experimental Protocols
Protocol 1: Organoid Cutting Using a 3D-Printed Jig
This protocol enables the sterile sectioning of organoids to maintain viability during long-term culture [49].
Workflow:
Key Materials:
- Cutting Jig & Blade Guide: 3D-printed using BioMed Clear resin. A flat-bottom design proved most effective [49].
- Blade: Sterile double-edge safety razor blade.
- Environment: Biosafety cabinet for sterility.
Procedure:
- Perform all steps in a biosafety cabinet using pre-sterilized tools.
- Collect organoids from the bioreactor into a tube with DMEM/F12 + HEPES.
- Aspirate about 30 organoids using a cut 1000 µL pipette tip and deposit them into the channel of the jig base.
- Carefully remove excess medium from the channel to prevent organoids from floating.
- Use fine-point tweezers to gently align organoids at the bottom of the channel without contacting each other.
- Position the blade guide onto the jig base. Push the blade down through the guide slots until it contacts the base, cleanly slicing all organoids in the channel.
- Remove the blade and guide. Flush the cut organoids with culture medium into a clean dish.
- Check the underside of the blade guide for any stuck organoid halves and collect them with tweezers.
- Transfer all sliced organoids to a new tube and return them to the culture system (e.g., a mini-spin bioreactor).
- Repeat for all organoids. Begin cutting on day 34-35 of culture and repeat every 3 weeks (± 3 days). Allow 6 days of recovery post-cutting before analysis [49].
Protocol 2: Generating Cup-Shaped Organoid-Tissue Modules (Organoid-TMs)
This scaffold-free method generates large, millimeter-scale organoids with an architecture that inherently reduces diffusion limitations [51].
Key Materials:
- Cell Source: Human adipose-derived mesenchymal stem cells (ADMSCs).
- Core Reagent: Microblocks (MiBs) of controlled sizes, derived from ADMSCs.
Procedure:
- Isolate and Verify ADMSCs: Isolate ADMSCs from human adipose tissue and verify their multipotent differentiation potential [51].
- Generate Microblocks (MiBs): Create cellular aggregates of defined sizes. The critical parameter is controlling the mixing ratio of large and small MiBs.
- Promote Self-Assembly: Allow the MiBs to undergo fusion and condensation in a scaffold-free environment. The density of MiBs and their size distribution drives the self-organization process.
- Form Cup-Shaped Organoid-TMs: Under optimized conditions, the MiBs will self-assemble into a unique, millimeter-scale, cup-shaped structure. This morphology provides a larger surface area for nutrient exchange compared to a solid sphere of equivalent volume.
- Apply Differentiation Cues: During or after fabrication, expose the Organoid-TMs to specific cues (e.g., chondrogenic factors) to direct differentiation for regenerative applications [51].
Frequently Asked Questions (FAQs)
Q1: What is the maximum size my organoids can reach before necrosis becomes inevitable? A: Computational models indicate that under static culture conditions, necrosis is likely to occur when organoid diameter exceeds ~400-500 μm. Even with advanced methods like orbital shaking or basic microfluidic flow, preventing necrosis in organoids larger than ~800 μm is challenging. Achieving larger, viable organoids requires more sophisticated solutions, such as internal vascularization or 3D spatial perfusion within the tissue itself [48].
Q2: How does regular cutting actually improve cellular diversity in long-term cultures? A: Necrotic cores not only cause cell death but also create a toxic microenvironment and disrupt normal cell signaling gradients. By eliminating the necrotic core, cutting reduces stress and restores a healthier microenvironment throughout the organoid. This allows for the continued proliferation and differentiation of progenitor cells, supporting the development and maintenance of a broader range of cell types over extended periods, which is crucial for modeling complex tissues [49] [14].
Q3: We are studying electrical activity in brain organoids. Will cutting damage the neural networks? A: Cutting does disrupt existing macroscopic neural connections. However, the resulting fragments remain viable and re-establish functional neural activity post-cutting. The primary benefit is the prevention of large-scale central necrosis, which would permanently destroy all cellular networks in the core. For studies requiring intact, large-scale neural circuits over very long periods, integrating vascularization strategies on a microfluidic chip may be a more suitable alternative to cutting [49] [52].
Q4: Can automation truly improve the reproducibility of my organoid cultures? A: Yes, significantly. Manual organoid culture over weeks or months is prone to variability in feeding schedules, handling techniques, and contamination risk. Automated systems standardize every step: feeding, imaging, and environmental control on a fixed schedule, 24/7. One study showed automation can reduce hands-on time by up to 90% while producing morphologically and functionally consistent organoids, which is vital for robust, high-throughput drug screening [47].
Strategy Comparison and Data
Table 1: Quantitative Comparison of Strategies to Overcome Necrotic Cores
| Strategy | Reported Reduction in Necrosis | Typical Organoid Size | Key Technical Requirements | Impact on Cellular Diversity |
|---|---|---|---|---|
| Physical Cutting [49] | Prevents necrosis, enables 5+ month culture | Maintains size post-cut; allows regrowth | 3D printer, sterile jig, manual skill | High (enables long-term culture for diverse cell type development) |
| Organoids-on-Chip [52] | Significant reduction via active perfusion | Can support larger sizes | Microfluidic chip, perfusion pumps | High (improved maturity & allows co-culture) |
| Architectural Engineering (Organoid-TM) [51] | Enhanced diffusion in millimeter-scale structures | Millimeter-scale, cup-shaped | Controlled self-assembly of microblocks | Promising (maintains stemness in large structures) |
| Computational Prediction [48] | Informs design; prevents necrosis proactively | Modeled for various sizes | Finite element modeling software | Indirect (guides culture conditions to avoid diversity loss) |
Table 2: Research Reagent Solutions Toolkit
| Reagent / Material | Function in Overcoming Necrosis | Example Application |
|---|---|---|
| BioMed Clear Resin [49] | Fabrication of sterile, customizable cutting jigs and blade guides for uniform organoid sectioning. | Creating flat-bottom cutting jigs for high-efficiency organoid cutting. |
| Microblocks (MiBs) [51] | Self-assembling building blocks for creating large, scaffold-free organoids with optimized architectures (e.g., cup-shaped). | Generating AdMSC-based Organoid-Tissue Modules for chondrogenic regeneration. |
| GelMA / Geltrex [49] | Hydrogels for embedding and creating organized organoid arrays for consistent high-throughput analysis post-cutting. | Making densely packed organoid arrays for spatial transcriptomics. |
| Rocking Incubator [47] | Provides constant, gentle motion in an automated system to ensure even nutrient and oxygen distribution in culture media. | Integrated into the CellXpress.ai system for automated brain organoid culture. |
| Microfluidic Chip [52] | Creates a perfusable network that mimics vasculature, enabling dynamic control of the organoid microenvironment. | Culturing various organoid types (e.g., brain, kidney, liver) with enhanced functionality. |
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Reagent / Material | Function in Overcoming Necrosis | Example Application |
|---|---|---|
| BioMed Clear Resin [49] | Fabrication of sterile, customizable cutting jigs and blade guides for uniform organoid sectioning. | Creating flat-bottom cutting jigs for high-efficiency organoid cutting. |
| Microblocks (MiBs) [51] | Self-assembling building blocks for creating large, scaffold-free organoids with optimized architectures (e.g., cup-shaped). | Generating AdMSC-based Organoid-Tissue Modules for chondrogenic regeneration. |
| GelMA / Geltrex [49] | Hydrogels for embedding and creating organized organoid arrays for consistent high-throughput analysis post-cutting. | Making densely packed organoid arrays for spatial transcriptomics. |
| Rocking Incubator [47] | Provides constant, gentle motion in an automated system to ensure even nutrient and oxygen distribution in culture media. | Integrated into the CellXpress.ai system for automated brain organoid culture. |
| Microfluidic Chip [52] | Creates a perfusable network that mimics vasculature, enabling dynamic control of the organoid microenvironment. | Culturing various organoid types (e.g., brain, kidney, liver) with enhanced functionality. |
Frequently Asked Questions (FAQs)
Q1: What are the primary sources of batch-to-batch variability in organoid cultures? Batch-to-batch variability in organoids primarily stems from three key sources:
- Biological Raw Materials: The inherent biological variability of the starting cells, whether they are patient-derived immune cells for co-cultures or pluripotent stem cells, is a major factor [53]. Donor-specific differences in treatment history, age, and genetic background significantly impact the consistency of the resulting organoids [53].
- Research Reagents: Critical reagents like the extracellular matrix (e.g., Matrigel) exhibit significant batch-to-batch variations in their mechanical and biochemical properties [54]. Similarly, growth factors, cytokines, and small molecules used in differentiation media are biologics subject to natural variation [54].
- Protocol Execution: Manual, labor-intensive culturing processes are prone to deviations. Differences in cell seeding density, media change schedules, and passaging techniques introduce operator-dependent variability [5]. The stochastic nature of stem cell self-organization during in vitro development also contributes to heterogeneity [55] [5].
Q2: How does batch variability specifically impact research on cellular diversity in organoids? Inconsistent starting materials and culture conditions can lead to significant fluctuations in the cellular composition of the final organoid. For instance, one batch might yield organoids with a desired balance of neural progenitors, neurons, and astrocytes, while another might skew this ratio, fail to generate specific rare cell types, or even produce off-target cells from an unintended germ layer [55] [56]. This variability directly confounds experiments aimed at understanding neurodevelopment or modeling diseases that affect specific neuronal subtypes, as observed in cerebral organoid research [55].
Q3: What are the best practices for tracking and managing data to control for variability? Implementing a robust data management system is crucial. It is recommended to:
- Start Early: Establish data collection protocols and repositories at the beginning of a research program [53].
- Compile a Historical Dataset: Systematically record data on donor attributes, reagent lot numbers, key process parameters (e.g., cell counts, growth curves), and final organoid characteristics [53].
- Use Data for Process Adjustment: Analyze this historical dataset to identify trends and correlations. For example, understanding growth curves allows for dynamic adjustment of feed schedules to better control culture development [53].
Q4: Can automation truly improve organoid consistency, and at which steps is it most beneficial? Yes, automation is a powerful tool for reducing variability. Incorporating automated processes at key manufacturing stages minimizes manual handling deviations [53]. Early integration of automation is vital for standardizing critical steps such as initial cell seeding, media addition/exchange, and organoid passaging. Automation also facilitates high-throughput, consistent imaging and analysis, which are essential for objective quality assessment [5] [53].
Troubleshooting Guides
Guide: Addressing High Variability in Organoid Size and Morphology
Problem: Your organoid batches show unacceptable levels of variation in physical characteristics like size, shape, and overall morphology.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Inconsistent cell seeding | Review protocol for manual steps; quantify cell count accuracy and distribution. | Implement automated cell counters and dispensers; standardize initial cell aggregation using U-bottom plates or bioreactors. |
| Variability in Extracellular Matrix (ECM) | Record and compare results by ECM lot number; test rheological properties of new lots if possible. | Pre-quality new lots of ECM (e.g., Matrigel) against a reference standard; transition to defined, synthetic hydrogels [54]. |
| Fluctuations in media components | Audit supplier Certificates of Analysis for growth factor concentrations; test new media lots alongside current ones. | Establish a quality control check for new reagent lots; source growth factors from a single, reliable supplier; use pre-formulated, commercial media where available. |
Guide: Managing Batch Effects in Downstream Single-Cell RNA Sequencing (scRNA-seq)
Problem: Technical differences between organoid batches create strong "batch effects" in scRNA-seq data, obscuring true biological signals and complicating the analysis of cellular diversity.
Background: Batch effects arise when technical variations from different processing dates, reagent lots, or sequencing runs are confounded with your biological conditions of interest. When integrating datasets, especially from different biological systems (e.g., organoids vs. primary tissue), standard integration methods can fail, either leaving too much batch variation or, conversely, removing biological variation [57].
Protocol: A Robust scRNA-seq Data Integration Workflow
- Assess Batch Effect Strength: Before integration, use metrics to quantify the distance between cells from the same batch versus different batches. A significant difference confirms that strong batch effects are present [57].
- Select an Advanced Integration Method: For substantial batch effects, avoid relying solely on methods that use high Kullback–Leibler (KL) divergence regularization, as they non-specifically remove both technical and biological variation [57]. Similarly, adversarial learning methods can over-correct and mix unrelated cell types [57].
- Implement an Improved Model: Utilize a next-generation integration tool like sysVI, which combines a VampPrior with cycle-consistency constraints. This approach has been shown to better integrate datasets across challenging conditions (e.g., different species, organoids vs. tissue, scRNA-seq vs. snRNA-seq) while preserving delicate biological signals [57].
- Validate Integration: Post-integration, evaluate the results using metrics like graph integration local inverse Simpson’s Index (iLISI) for batch mixing and normalized mutual information (NMI) for biological preservation. Inspate UMAP plots to ensure cell types cluster by biology, not by batch [57].
The following workflow summarizes the key steps for quality control and data integration:
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials used in organoid research and their associated variability challenges.
| Item | Function in Organoid Culture | Variability Challenge & Mitigation Strategy |
|---|---|---|
| Extracellular Matrix (e.g., Matrigel) | Provides a 3D scaffold that supports cell polarization, proliferation, and self-organization. | High batch-to-batch variability in protein composition and mechanical stiffness [54]. Mitigation: Pre-test and qualify each new lot against a functional standard (e.g., organoid formation efficiency); transition to defined synthetic hydrogels (e.g., GelMA) for superior consistency [54]. |
| Growth Factors & Cytokines (e.g., Wnt3A, EGF, Noggin) | Activate specific signaling pathways to direct stem cell fate, maintenance, and differentiation. | Concentration and activity can vary between lots and suppliers [54]. Mitigation: Source from reputable suppliers with extensive COA; use recombinant human proteins where possible; establish in-house bioassays to verify activity. |
| Pluripotent Stem Cells (PSCs) | The foundational building blocks for generating most organoid types. | Inherent genetic and epigenetic variability between cell lines and donors affects differentiation potential [58] [53]. Mitigation: Use comprehensive cell banking (Master/Working banks); deeply characterize multiple cell lines; employ genome editing to create isogenic controls. |
| Chemically Defined Media | Provides nutrients and signaling molecules to sustain culture and guide differentiation. | Lot-to-lot differences in components like albumin and lipids can alter outcomes. Mitigation: Use single-sourced, pre-formulated media; for critical studies, produce a large, single lot of custom media to use throughout the project. |
| Starting Tissue (Apheresis/Tumor Biopsy) | Source of primary cells for immune co-cultures or patient-derived organoids. | High biological variability due to patient treatment history, disease stage, and tissue collection/handling [53] [54]. Mitigation: Harmonize collection procedures across clinics; perform pre-characterization of incoming material (e.g., cell composition); cryopreserve cells to create a standardized starting inventory [53]. |
Detailed Experimental Protocols
Protocol: Implementing a Quality Control Scoring System for Cerebral Organoids
Application: This protocol provides a standardized method for non-invasively and invasively assessing the quality of 60-day cortical organoids, crucial for ensuring batch-to-batch consistency in neurodevelopmental studies [55].
Principle: A hierarchical scoring system evaluates organoids against five critical criteria, beginning with simple, non-invasive checks and proceeding to deeper analytical assays. This allows for efficient screening and robust qualification of batches before use in resource-intensive experiments [55].
Procedure:
Initial QC (Pre-Study, Non-Invasive):
- Criterion A: Morphology. Visually inspect organoids under a bright-field microscope. Score from 0 (low quality) to 5 (high quality) based on the presence of well-defined borders, overall compactness/density, and the absence of large, protruding cystic structures or excessive cellular debris [55].
- Criterion B: Size and Growth Profile. Measure the diameter of organoids over time. Score based on consistency with expected growth trajectories for the protocol and absence of extreme size outliers within a batch [55].
- Decision Point: Organoids that fail to meet minimum thresholds for Criteria A and B are excluded from the study.
Final QC (Post-Study, In-Depth Analysis):
- Criterion C: Cellular Composition. Fix, section, and stain organoids with cell-type-specific antibodies (e.g., SOX2 for neural progenitors, TUJ1 for neurons, GFAP for astrocytes). Quantify the proportions of each cell type using fluorescence imaging and analysis software. Score based on the fidelity to the expected cellular diversity [55].
- Criterion D: Cytoarchitectural Organization. Assess the presence and organization of key structures like ventricular zones or neural rosettes in stained sections. A high score indicates clear, well-formed organizational patterns indicative of healthy development [55].
- Criterion E: Cytotoxicity. Perform a live/dead assay (e.g., using Calcein-AM and Ethidium homodimer-1) to quantify the proportion of dead cells within the organoid. A low level of cell death is required for a high score [55].
Validation: To validate this QC system, researchers can expose organoids to graded doses of a cytotoxic agent like hydrogen peroxide (H₂O₂) to intentionally create a range of quality outcomes, demonstrating the scoring system's ability to discriminate between high- and low-quality organoids [55].
Protocol: Low-Pressure Compression Test for Powder Packing Behavior
Application: While developed for active pharmaceutical ingredients (APIs), this quick and powerful method is highly applicable to characterizing protein powders, synthetic hydrogel precursors, or other powdered reagents used in organoid media, helping to identify variations between supplier lots [59].
Principle: The packing density of a powder under low pressure is sensitive to particle size and shape. Variations in these physical properties, which can arise from different manufacturing batches, affect the powder's behavior in solution and its performance in culture [59].
Procedure:
- Equipment Setup: Fit a die and a flat-faced punch to a texture analyzer or similar mechanical tester [59].
- Sample Loading: Precisely weigh a defined mass of the powder and load it into the die.
- Compression: Compress the powder at a constant speed to a target low pressure (e.g., 0.2 MPa). Record the force and displacement during compression to generate a compression profile [59].
- Data Analysis: Calculate the specific compressed density (e.g., d0.2) from the final volume of the powder plug at the target pressure.
- Multivariate Analysis: Combine the compressed density data with particle size distribution data (e.g., D90 from laser diffraction) in a multivariate model (e.g., Principal Component Analysis). This combination has proven highly effective in separating batches based on their processability and physical characteristics [59].
Interpretation: Batches of the same material that cluster together in the multivariate model are considered consistent. Batches that are outliers may have different physical properties and should be investigated further before use in critical experiments [59].
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions
Q1: Our neural organoid experiments are plagued by high, chronic cellular stress. What could be causing this and how can we mitigate it?
Chronic cellular stress in organoids, marked by the aberrant expression of metabolic and endoplasmic reticulum stress genes, is a common limitation of current 3D culture systems [7]. This can be caused by non-physiological culture conditions, including hyper- or hypo-oxygenation, lack of vasculature, and insufficient nutrient perfusion to the organoid's core [7].
- Solution: Implement a sliced organoid culture approach. Growing organoids as slice cultures instead of dense spheres significantly improves oxygen and nutrient permeability, rescuing cell death in the organoid interior [7].
Q2: We are using a high-density MEA, but the data output is overwhelming. Are there technologies that can help focus on biologically relevant signals?
Traditional MEAs that sample at high, fixed rates generate massive amounts of data, much of which may be noise or irrelevant [60].
- Solution: Consider an event-based biosensor. Systems like the GAIA MEA incorporate neuromorphic, event-driven circuits that digitize signals at the pixel level [60]. They output asynchronous digital "address-events" only when the bio-signal (e.g., an action potential) exceeds a set threshold, drastically reducing off-chip data traffic and power consumption while capturing meaningful activity [60].
Q3: Our organoid models lack the complex cellular diversity found in native human tissue. How can biosensor integration help address this?
Limited cellular diversity and impaired cell type specification are key challenges in organoid research, affecting the reliability of disease modeling and drug screening [7]. Biosensors provide a functional readout that can quantify this limitation.
- Solution: Employ organoid-immune co-culture models combined with functional monitoring. By co-culturing tumour organoids with autologous immune cells and using MEAs to monitor the resulting electrophysiological changes, you can assess whether key cellular interactions and functions are being restored [54]. This provides a quantitative metric beyond genetic analysis to validate improvements in organoid fidelity.
Q4: What type of electrode tip should I select for penetrating tougher tissues like the dura mater?
The standard electrode tip may be damaged or deflected when penetrating tough membranes.
- Solution: Use a heat-treated electrode. This specialized profile features a more gradual taper and toughened polymer insulation near the tip, allowing it to be pushed through tough membranes with less risk of damage [61].
Q5: We observe significant variability in organoid differentiation outcomes. How can we improve reproducibility?
Variability often stems from batch-to-batch differences in extracellular matrix (ECM) materials like Matrigel and inconsistencies in differentiation protocols [54].
- Solution:
- Standardize your ECM: Transition to synthetic hydrogels (e.g., GelMA) which offer consistent chemical and physical properties compared to animal-derived Matrigel [54].
- Implement rigorous data governance: For your experimental data, establish a common data language and assign data stewards to ensure consistent interpretation and usage across your team. This principle of data governance is critical for reconciling data from multiple sources and experiments [62].
Troubleshooting Common Experimental Issues
Issue: Low Signal-to-Noise Ratio in MEA Recordings
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Electrode Impedance | Measure electrode impedance upon receipt and before experiments. | Ensure impedance is within the manufacturer's specified range. Consider laser-exposed electrodes for more precise impedance control [61]. |
| Electrical Interference | Check for 50/60 Hz line noise and correlated noise across multiple channels. | Ground all equipment properly. Use a Faraday cage. Ensure recording solutions are well-aerated but not bubbling [63]. |
| Poor Cell-Electrode Coupling | Inspect cell viability and attachment over electrodes. | Optimize surface coating (e.g., poly-D-lysine, laminin) to promote cell adhesion. For tough membranes, use heat-treated electrodes for better penetration [61]. |
| Biofouling | Visually inspect electrodes for debris. | Clean electrodes according to manufacturer protocols. Use approved cleaning solutions without damaging delicate insulation [61]. |
Issue: Inconsistent Organoid Functional Responses to Drug Stimuli
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Necrotic Core | Perform live/dead staining on fixed organoids to assess viability in the interior. | Switch to sliced organoid cultures to improve perfusion [7]. Reduce organoid size to limit diffusion issues. |
| Off-Target Cell Types | Conduct single-cell RNA sequencing to validate cell type composition and specification. | Review differentiation protocol; optimize concentration and timing of key patterning factors (e.g., Wnt, BMP inhibitors) [7]. |
| Uncontrolled Maturation | Analyze marker expression over time to track developmental trajectory. | Establish a strict, standardized maturation timeline for all experiments. Use defined media to minimize variability [54]. |
Experimental Protocols & Methodologies
Detailed Protocol: Functional Assessment of Neural Organoids using a Multi-Electrode Array
This protocol outlines the use of an MEA biosensor to monitor spontaneous and evoked electrical activity in neural organoids, providing a functional readout to complement cellular diversity studies.
1. Principal Investigational Rationale To quantitatively assess the functional maturation and network formation within neural organoids in a non-invasive, label-free, and longitudinal manner. This protocol helps validate whether improved differentiation protocols lead to more physiologically relevant electrophysiological outputs [7].
2. Research Reagent Solutions
| Essential Material | Function/Explanation in the Protocol |
|---|---|
| Neural Organoids | 3D self-organizing structures derived from human pluripotent stem cells that model features of early brain development and are the subject of functional analysis [7]. |
| Multi-Electrode Array (MEA) | A biosensor device containing multiple embedded electrodes to simultaneously record extracellular field potentials and action potentials from multiple sites in the organoid [63] [60]. |
| Neurobasal or BrainPhys Medium | A cell culture medium formulated to support the survival and function of mature neurons during recording sessions. |
| Poly-D-Lysine/Laminin | Coating solutions used to treat the MEA surface to promote adhesion of organoid slices and improve the electrical seal. |
| Synaptic Receptor Agonists/Antagonists | Pharmacological agents (e.g., NMDA, CNQX, Bicuculline) used to probe the presence and function of specific synaptic components within the organoid network. |
| Action Potential Blocker | Tetrodotoxin (TTX), a sodium channel blocker, used to confirm that recorded signals are indeed neural action potentials. |
3. Step-by-Step Procedural Walkthrough
Preparation:
- Organoid Transfer: Gently transfer a mature neural organoid (e.g., >60 days) to the recording chamber of the MEA.
- Stabilization: Secure the organoid using a sterile harp or weighted net to ensure stable contact with the electrode surface.
- Acclimatization: Allow the organoid to equilibrate in the recording medium for at least 30 minutes at 37°C and 5% CO₂.
Data Acquisition:
- Setup: Set the amplifier to a gain of 1000x and apply a band-pass filter of 1 Hz - 5 kHz.
- Baseline Recording: Record spontaneous activity for a minimum of 10 minutes to establish a baseline. Note the presence of single-unit spikes and network-level bursts.
- Stimulus Application (Optional): If the MEA has stimulating capabilities, apply a biphasic current pulse (e.g., 100 µA, 200 µs per phase) through a subset of electrodes to evoke network responses.
Pharmacological Interrogation:
- Baseline Confirmation: Record a 5-minute baseline in the presence of the drug vehicle.
- Drug Application: Gently perfuse the recording chamber with a known synaptic blocker (e.g., 20 µM CNQX to block AMPA receptors).
- Response Recording: Record activity for 15-20 minutes post-application to observe the drug's effect on network dynamics.
- Washout (Optional): Perfuse with standard recording medium to see if the activity recovers.
Data Analysis:
- Spike Sorting: Use software to sort detected spikes into putative single units based on waveform shape and principal component analysis.
- Burst Detection: Apply algorithms to identify periods of high-frequency, synchronous firing (bursts) across the network.
- Metric Calculation: Calculate key parameters like mean firing rate, inter-spike interval, burst frequency, and network synchrony index.
Workflow: Organoid MEA Recording
Conceptual Diagram: Event-Based MEA Data Reduction
This diagram illustrates the core principle of an event-based MEA, which reduces data output by transmitting information only when a significant voltage change is detected [60].
Table: Key Specifications of Traditional vs. Event-Based MEAs
| Parameter | Traditional MEA (e.g., 60-electrode) | Advanced Event-Based MEA (e.g., GAIA) |
|---|---|---|
| Number of Channels | 60 electrodes [63] | 4096 electrodes [60] |
| Data Output Mode | Continuous, clocked stream at fixed sampling rate [60] | Sparse, asynchronous digital events only upon signal change [60] |
| Data Throughput | ~200 kbps per channel (scales linearly with channels) [60] | Peak throughput of 20 Mega events per second (total system) [60] |
| Power Consumption | High (due to constant sampling and clocking) [60] | Low (clock-less, event-driven operation) [60] |
| Typical Gain | Varies with system | Programmable up to 57 dB [60] |
| Key Advantage | Well-established, continuous raw data | Drastically reduced data traffic, inherent feature extraction [60] |
Table: Troubleshooting Electrode Selection for Organoid Penetration
| Electrode Tip Type | Best Use Case | Key Functional Advantage |
|---|---|---|
| Standard | Most neural recording applications; versatile performance [61]. | Provides an effective balance between tissue penetration and electrode durability [61]. |
| Blunted | Higher-intensity stimulation protocols; cell surface recording [61]. | Acts more as a point source for improved stimulation isolation; may reduce cell puncture [61]. |
| Extra Fine | Recording from small, tightly-packed cell populations (e.g., cortical layers) [61]. | Sharper taper and thinner insulation for minimal tissue displacement in shallow preparations [61]. |
| Heat Treated | Penetrating tough membranes (e.g., dura mater) [61]. | Gradual taper and toughened insulation for easier penetration with less risk of damage [61]. |
Benchmarking Success: How Enhanced Organoids Compare to Traditional Models
Troubleshooting Guide: Addressing Common PDO Experiment Challenges
This guide addresses frequent issues researchers encounter when establishing Patient-Derived Organoid (PDO) models and correlating their drug responses to clinical outcomes.
1. Problem: Low Organoid Establishment Success Rate
- Potential Causes: Delays in tissue processing, improper preservation techniques, or suboptimal culture conditions.
- Solutions:
- Process tissues immediately post-collection when possible. For unavoidable delays, use validated short-term storage (4°C with antibiotics for ≤6-10 hours) or cryopreservation methods. Cryopreservation is recommended for delays exceeding 14 hours [3].
- Optimize culture media with essential soluble factors like Wnt3A, R-spondin, and Noggin to promote tumor cell growth over non-tumour cells [54].
- Note that establishment success can be influenced by sample type; success rates for metastatic colorectal cancer biopsies increased from 22% to 75% with protocol optimization and experience [64].
2. Problem: High Variability in Drug Sensitivity Assays
- Potential Causes: Inconsistent organoid size, Matrigel batch effects, or uneven seeding density.
- Solutions:
- Reduce variation by seeding equivalent cell numbers using single-cell passaging with TrypLE Express and adding ROCK inhibitor (Y-27632) to maintain viability [65].
- Manually select organoids of similar size and morphology to reduce assay variability [65].
- Use lot-qualified Growth Factor Reduced (GFR) Matrigel or consider synthetic hydrogels to minimize batch-to-batch variability [54].
3. Problem: Poor Correlation Between PDO and Clinical Response
- Potential Causes: Lack of tumor microenvironment (TME) components, such as immune cells, or insufficient model validation.
- Solutions:
- Implement immune co-culture systems. "Innate immune microenvironment" models use tumor tissue retaining native TME, while "reconstituted" models add autologous immune cells back to tumor organoids [54].
- For clinical correlation, ensure PDO drug sensitivity is measured using multiple metrics (AUC, IC50, GR50) and correlate with patient radiological response [64].
- Fine-tune models with advanced computational approaches. The PharmaFormer model demonstrates that pre-training on large cell line datasets before fine-tuning on limited organoid data significantly improves clinical prediction accuracy [66].
4. Problem: Limited Cellular Diversity in Organoid Cultures
- Potential Causes: Overgrowth of dominant cell clones or culture conditions that fail to support all relevant cell types.
- Solutions:
- Systematically adjust growth factor combinations (e.g., EGF, FGF, HGF) to support diverse cell populations from different tissue regions [3] [54].
- Characterize organoid composition regularly through marker expression and karyotype analysis every 5-10 passages [65].
- Integrate microfluidic systems to better mimic in vivo gradients and mechanical forces, supporting a broader range of cell types [3].
Frequently Asked Questions (FAQs)
Q1: What is the typical success rate for establishing PDOs from patient biopsies, and what factors influence it? Success rates vary by tissue type and cancer. In a recent metastatic colorectal cancer study, an overall 52% success rate was achieved, influenced by factors like male sex, elevated lactate dehydrogenase levels, biopsy location, and laboratory experience with optimized culture conditions. Success rates can improve significantly with protocol refinement [64].
Q2: Which drug sensitivity metrics most accurately predict actual patient clinical outcomes? In validation studies, multiple metrics are used. For mCRC PDOs treated with 5-FU & oxaliplatin, drug sensitivity measured by the Area Under the Curve (AUC) and GR AUC (GRAUC) showed significant correlation with patient response in biopsied lesions (R=0.41-0.49) and all target lesions (R=0.54-0.60). These metrics demonstrated high predictive accuracy with an AUROC of 0.78-0.88 [64].
Q3: How can I enhance my PDO models to better mimic the tumor immune microenvironment? Two primary approaches exist:
- Innate Immune Microenvironment Models: Culture tumor tissue fragments at liquid-gas interfaces to preserve native tumor-infiltrating lymphocytes (TILs). These models have successfully replicated PD-1/PD-L1 checkpoint function [54].
- Immune Reconstitution Models: Co-culture tumor organoids with autologous immune cells, such as peripheral blood lymphocytes, to study specific immune interactions and therapy responses [54].
Q4: What are the best practices for ensuring my PDO models maintain genetic and phenotypic stability over long-term culture?
- Perform regular marker expression and karyotype analysis every 5-10 passages to ensure genetic stability and identity [65].
- Use defined, reproducible media formulations and lot-qualified extracellular matrices to minimize drift [65] [54].
- Cryopreserve early-passage organoids to create a master cell bank, avoiding continuous long-term culture and potential genetic drift [65].
Quantitative Data: Correlating PDO Response with Clinical Outcomes
Table 1: Predictive Performance of Colorectal Cancer PDOs for Chemotherapy Response
| Treatment | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Area Under ROC Curve (AUROC) | Correlation with Lesion Response (R) |
|---|---|---|---|---|
| 5-FU & Oxaliplatin | 0.78 | 0.80 | 0.78-0.88 | 0.41-0.60 [64] |
Table 2: Hazard Ratio Improvement with AI-Enhanced Prediction Models
| Cancer Type | Treatment | Pre-trained Model HR | Organoid Fine-tuned Model HR | Improvement |
|---|---|---|---|---|
| Colon Cancer | 5-Fluorouracil | 2.50 (95% CI: 1.12-5.60) | 3.91 (95% CI: 1.54-9.39) | 56% [66] |
| Colon Cancer | Oxaliplatin | 1.95 (95% CI: 0.82-4.63) | 4.49 (95% CI: 1.76-11.48) | 130% [66] |
| Bladder Cancer | Gemcitabine | 1.72 (95% CI: 0.85-3.49) | 4.91 (95% CI: 1.18-20.49) | 185% [66] |
Experimental Protocols
Protocol 1: Establishing PDOs from Colorectal Tissue
Materials:
- Cold Advanced DMEM/F12 with antibiotics
- Growth Factor Reduced Matrigel
- Organoid culture medium (Wnt3A, R-spondin, Noggin, EGF, B27, N-acetylcysteine)
- ROCK inhibitor (Y-27632)
Method:
- Tissue Procurement: Collect human colorectal tissue samples under sterile conditions immediately after colonoscopy or surgical resection. Transfer in cold antibiotic-supplemented medium [3].
- Processing: Minimize processing time. For delays <6-10 hours, use refrigerated storage with antibiotics. For longer delays, cryopreserve tissue using freezing medium (10% FBS, 10% DMSO in 50% L-WRN conditioned medium) [3].
- Crypt Isolation and Culture: Isolate crypts through mechanical dissociation and enzymatic digestion. Embed in Matrigel domes and culture with specialized medium containing Wnt agonist, R-spondin, Noggin, and other tissue-specific factors [3] [65].
- Maintenance: Replenish media every other day and passage every 7-12 days before organoids become too large or necrotic, using mechanical or enzymatic dissociation [65].
Protocol 2: Drug Sensitivity Testing in PDOs
Materials:
- 3D cell culture-approved white wall plates
- CellTiter-Glo 3D Cell Viability Assay
- Test compounds in concentration series
- Dimethyl sulfoxide (DMSO) as vehicle control
Method:
- PDO Preparation: Thaw/recover PDOs for 48 hours before assay. Dissociate to uniform fragments or single cells and seed in Matrigel at consistent density [65] [64].
- Drug Treatment: Incubate PDOs with a panel of drugs, including the patient's treatment regimen. Include multiple concentrations (typically 8-point dilution series) alongside DMSO controls [64].
- Incubation: Treat organoids for 5-7 days, refreshing drugs/media as needed [65].
- Viability Assessment: Measure cell viability using CellTiter-Glo 3D. This ATP-based luminescent assay is optimized for 3D cultures [65].
- Data Analysis: Calculate multiple sensitivity metrics: Area Under the dose-response Curve (AUC), half-maximal inhibitory concentration (IC50), and growth rate-based metrics (GR AUC, GR50) [64].
Signaling Pathways and Experimental Workflows
Diagram 1: PDO Drug Response Testing Workflow
Diagram 2: Key Signaling Pathways in PDO Culture
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for PDO Culture and Drug Testing
| Reagent/Category | Function | Examples/Specific Factors |
|---|---|---|
| Extracellular Matrix | Provides 3D structural support for organoid growth | Growth Factor Reduced Matrigel, Synthetic hydrogels (GelMA) [65] [54] |
| Essential Growth Factors | Maintain stemness and support proliferation | Wnt3A, R-spondin-1, Noggin, EGF, FGF, HGF (liver models) [54] |
| Media Supplements | Enhance cell survival and function | B27, N2, N-acetylcysteine, Gastrin, Nicotinamide [65] |
| Small Molecule Inhibitors | Improve viability and control differentiation | ROCK inhibitor (Y-27632), A83-01, SB202190, CHIR99021 [65] |
| Assessment Assays | Measure drug response and viability | CellTiter-Glo 3D, Live/Dead staining (Calcein-AM/PI) [65] |
| Dissociation Reagents | Passage and single-cell preparation | TrypLE Express, Enzyme-free passaging reagents [65] |
Traditional two-dimensional (2D) cell cultures have long been a staple in biological research, but they lack the complexity of living tissues. Organoids—three-dimensional (3D), stem cell-derived structures that self-organize to mimic the architecture and functionality of human organs—represent a paradigm shift. These models preserve patient-specific genetic and phenotypic features, offering improved physiological relevance for disease modeling, drug screening, and personalized medicine [58]. This guide addresses common challenges in organoid research, with a special focus on strategies to enhance and characterize cellular diversity, moving your research beyond the limitations of monolayer cultures.
Frequently Asked Questions (FAQs) & Troubleshooting
1. Why do my organoids lack the cellular diversity found in native human tissue?
The cellular heterogeneity of your organoids is highly dependent on your culture conditions and protocol.
- Cause: The use of overly restrictive medium formulations that maintain a stem-cell-like state can inhibit necessary differentiation pathways. A lack of appropriate morphogenetic cues or an incorrect extracellular matrix can also lead to simplified structures.
- Solution: To drive the formation of multiple, distinct cell lineages, you must carefully modulate the differentiation signals in your culture medium. This often involves the timed withdrawal of stem cell-promoting factors (e.g., Wnt-3a) and the addition of differentiation-inducing agents [67]. Refer to the Experimental Protocols section below for a detailed methodology.
2. How can I reliably assess the cellular complexity and spatial organization of my organoids?
Confirming the presence of diverse cell types and their correct spatial arrangement is key to validating your model.
- Challenge: Traditional 2D analysis methods are insufficient for complex 3D structures. It can be difficult to quantitatively describe the cellular diversity and tissue architecture within an organoid.
- Solution: Employ advanced spatial profiling technologies and analytical frameworks. Tools like MESA (multiomics and ecological spatial analysis) adapt ecological concepts to quantify spatial diversity, identify cellular "hot spots," and integrate multiomics data to provide a deep, molecular understanding of cellular neighborhoods within your tissue models [68].
3. My organoid viability assays are inconsistent. How can I improve their reliability for 3D cultures?
Standard viability assays designed for 2D cultures often fail in 3D systems due to issues with normalization and reagent stability.
- Cause: Assays like Lactate Dehydrogenase (LDH) release face challenges in 3D cultures because precise cell density quantification is difficult without disrupting the culture integrity. Furthermore, LDH activity is not stable over time, complicating longitudinal studies.
- Solution: Implement an optimized LDH assay protocol tailored for 3D cultures. This includes normalizing LDH activity to the total protein concentration in the conditioned medium and using a dedicated preservation buffer to stabilize LDH activity for up to one month at -20°C, enabling accurate and reproducible longitudinal monitoring [69].
4. My organoids are not forming proper structural compartments. What could be wrong?
Recapitulating in vivo tissue architecture, such as the crypt-villus structures in the intestine, is a hallmark of a successful organoid culture.
- Cause: This often stems from suboptimal extracellular matrix (ECM) conditions or an imbalance in niche-inspired growth factors that guide self-organization and patterning.
- Solution: Ensure you are using a high-quality ECM hydrogel (e.g., Matrigel with a protein content ≥ 8.5 mg/mL) and a culture medium that provides the correct combination of niche signals, including Wnt agonists, R-spondins, and Noggin, which are critical for maintaining stem cells and inducing spatial organization [70] [67].
Experimental Protocols: Key Methodologies
Protocol 1: Generating Electrophysiologically Tight Intestinal Monolayers from 3D Organoids
This protocol harmonizes the process for creating 2D organoid-derived monolayers (ODMs) from human, mouse, chicken, and pig intestinal spheroids, providing an accessible model while preserving physiological properties [67].
Workflow Diagram: Creating Organoid-Derived Monolayers
Materials and Reagents:
- Transwell Inserts: (0.6 cm², 0.4 μm pores; e.g., Millicell PIHPCell-Free Systems, and Bioprinters) for creating complex 3D structures.
- Advanced DMEM/F-12: Base medium for organoid culture.
- Growth Factors & Inhibitors: Recombinant EGF, N-2 Supplement, B-27 Supplement, A83-01 (TGF-β receptor inhibitor), SB202190 (p38 inhibitor), Y-27632 (ROCK inhibitor).
- Dissociation Reagent: TrypLE Express Enzyme.
- Extracellular Matrix (ECM): Cultrex Reduced Growth Factor BME Type 2 or Corning Matrigel (protein content ≥ 8.5 mg/mL).
Procedure:
- Starting Material: Use intestinal spheroids, which are stem cell-enriched, non-budding 3D structures.
- Dissociation: Gently dissociate the spheroids using TrypLE Express to create a single-cell suspension.
- Seeding: Plate the dissociated cells onto Transwell inserts pre-coated with an appropriate ECM.
- Differentiation Medium: Culture the cells with a differentiation-induction medium. The key is to use a common base medium and withdraw stem cell-promoting factors like Wnt-3a, A83-01, and SB202190, while maintaining the presence of nicotinamide.
- Monitoring: Monolayers typically become confluent and form an electrophysiologically tight epithelium within 6 days, which can be verified by measuring Transepithelial Electrical Resistance (TEER).
Protocol 2: Quantitative Spatial Analysis of Cellular Diversity Using MESA
The MESA framework provides a systematic method to quantify the cellular diversity and spatial patterns in your organoids or tissue samples using spatial-omics data [68].
Workflow Diagram: MESA Spatial Analysis Framework
Procedure:
- Data Integration: Integrate your spatial-omics data (e.g., from CODEX or CosMx platforms) with corresponding single-cell RNA sequencing (scRNA-seq) data from the same tissue type using an algorithm like MaxFuse. This creates an in silico multiomics profile for each cell in the spatial dataset.
- Neighborhood Characterization: For each cell, aggregate multiomics information (e.g., average protein and mRNA expression levels) from its spatially determined neighbors (e.g., the 20 closest cells). This defines the local cellular environment without relying solely on pre-designated cell types.
- Identify Neighborhood Patterns: Use k-means clustering on these neighborhood profiles to identify conserved, distinct cellular neighborhoods (e.g., subniches within a germinal center).
- Quantify Spatial Diversity: Apply ecological metrics:
- Multiscale Diversity Index (MDI): Assesses how cellular diversity changes across different spatial scales.
- Global and Local Diversity Indices (GDI/LDI): Identify clusters of patches with high diversity ("hot spots") or low diversity ("cold spots").
- Diversity Proximity Index (DPI): Evaluates the spatial relationships between these spots.
- Functional Analysis: Perform differential expression and gene set enrichment analysis within the identified neighborhoods to uncover functional pathways.
Data Presentation: Quantitative Comparisons
Table 1: Viability Assay Comparison: 2D vs. Optimized 3D Protocol This table compares the standard LDH assay used in 2D cultures with the optimized protocol for 3D organoids, highlighting key challenges and solutions [69].
| Parameter | Traditional 2D LDH Assay | Standard 3D LDH Assay Challenge | Optimized 3D LDH Assay Solution |
|---|---|---|---|
| Normalization | Normalized to seeded cell number | Precise cell count is difficult; disrupts culture integrity | Normalize to total protein concentration in conditioned medium |
| LDH Stability | Assayed on fresh medium | LDH activity declines rapidly; not suitable for longitudinal studies | Use of preservation buffer stabilizes LDH activity at -20°C for one month |
| Linearity & Signal | Proportional to cell death | Signal can be saturated or non-linear without adaptation | Requires adapted dilutions (e.g., 1/2.5 to 1/4 with distilled water) for accurate measurement |
Table 2: Organoid Models and Their Applications in Preclinical Research This table summarizes various human organoid models and their demonstrated utility in mimicking human physiology and disease for drug development [70] [58].
| Organoid Type | Key Pathophysiological Features Recapitulated | Applications in Drug Discovery & Disease Modeling |
|---|---|---|
| Intestinal | Crypt-villus architecture; contains enterocytes, goblet cells, Paneth cells, enteroendocrine cells [70] | Host-pathogen interactions, nutrient uptake and transport studies, inflammatory bowel disease [67] [71] |
| Cerebral | Models human brain development; exhibits discrete brain region organization [70] | Neurodevelopmental disorders (e.g., microcephaly), neurotoxicity testing, neurodegenerative diseases [58] |
| Hepatic (Liver) | Functional hepatocytes; forms bile canaliculi [70] | Drug metabolism studies, hepatotoxicity assessment (a major cause of drug attrition) [58] |
| Patient-Derived Tumor (PDTO) | Retains histological/genomic features of original tumor; models intratumoral heterogeneity [58] | Personalized therapy selection; predicting individual responses to chemotherapy and targeted agents [58] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Intestinal Organoid Culture A selection of essential reagents for establishing and maintaining intestinal organoid cultures, based on harmonized protocols [67].
| Reagent | Function in Culture | Example |
|---|---|---|
| Wnt-3a | Critical stem cell niche factor; promotes proliferation and stemness [67] | Recombinant protein |
| R-spondin-1 | Potentiates Wnt signaling; essential for long-term growth of intestinal stem cells [70] | Conditioned medium or recombinant protein |
| Noggin | BMP pathway inhibitor; prevents differentiation and supports epithelial growth [70] | Conditioned medium or recombinant protein |
| A83-01 | TGF-β receptor inhibitor; prevents differentiation into undesirable lineages [67] | Small molecule inhibitor |
| B-27 & N-2 Supplements | Provide defined set of hormones, growth factors, and proteins for cell survival and growth | Serum-free supplements |
| Extracellular Matrix (ECM) | Provides a 3D scaffold that mimics the basal lamina; essential for organoid formation and growth | Cultrex BME Type 2 or Corning Matrigel |
The field of biomedical research is undergoing a significant transformation, driven by the ethical imperative of the 3Rs Principles (Replacement, Reduction, and Refinement of animal use) and enabled by groundbreaking regulatory and scientific advancements. The FDA Modernization Act 2.0, passed in December 2022, eliminates the long-standing requirement for animal testing prior to human clinical trials, opening the door for human-relevant testing methods such as cell-based assays, organoids, and computer models [72]. This technical support center is framed within the broader research thesis of addressing limited cellular diversity in organoid cultures, a key challenge in realizing their full potential as human-relevant test systems that align with the 3Rs. The following guides and FAQs provide targeted support for researchers navigating this evolving landscape.
Regulatory and Scientific Background
The 3Rs Framework
The 3Rs principles, first described by William Russell and Rex Burch in 1959, provide an ethical framework for animal research [73] [74]:
- Replacement: Substituting conscious living animals with insentient material. This can be absolute (e.g., human organoids, computer models) or relative (e.g., using animal-derived cells or tissues that don't involve full animal suffering) [74].
- Reduction: Obtaining comparable information from fewer animals or more information from the same number of animals through appropriate experimental design and statistical analysis [73] [74].
- Refinement: Modifying procedures to minimize pain, suffering, and distress, and to improve animal welfare [73] [74].
FDA Modernization Act 2.0
This landmark legislation, passed in December 2022, represents a paradigm shift in drug development [72]:
- It specifically replaces references to animal tests with the term "nonclinical tests" and explicitly includes cell-based assays, organoids, and computer models as acceptable alternatives [72].
- The U.S. Food and Drug Administration (FDA) has subsequently announced plans to phase out animal testing requirements for monoclonal antibodies and other drugs, encouraging the use of New Approach Methodologies (NAMs) including AI-based computational models and organoid toxicity testing [75] [72].
Troubleshooting Guides & FAQs for Organoid Research
This section addresses specific experimental challenges in organoid research, with particular focus on overcoming limitations in cellular diversity and maturation—key factors in developing robust animal alternatives.
FAQ: Addressing Limited Cellular Diversity in Organoid Models
Q: My neural organoids lack key specific cell types, such as microglia or vascular cells, limiting their physiological relevance. How can I enhance cellular diversity?
A: Limited cellular diversity is a common challenge in organoid research. Several engineering strategies can help recapitulate the complexity of native organs [5]:
- Co-culture systems: Introduce mesenchymal, immune, or endothelial cells during organoid differentiation to better mimic the in vivo cellular microenvironment [5].
- Engineering maturation: Improve protocols to generate organoids that more fully replicate complete organ function. For example, incorporate corresponding flora microorganisms, lymphatic vessels, or innervation [5].
- Modulate external factors: Apply relevant mechanical force stimulation, light stimulation, or electrical stimulation, which have been shown to improve maturation [5].
Q: How can I reduce heterogeneity and improve reproducibility in my organoid cultures for more reliable drug screening results?
A: Heterogeneity arises from the stochastic nature of in vitro self-assembly [5]. To address this:
- Implement automation: Use robotic liquid handling systems for initial stem cell allocation, media addition/replacement, and drug testing to minimize manual variation [5].
- Precisely control niche components: Standardize extracellular matrix composition and soluble factor concentrations through engineering tools [5].
- Monitor consistently: Employ high-content imaging and multi-electrode arrays to better characterize and quality-control organoid batches [5].
Q: My organoids show limited maturity and fail to replicate adult tissue phenotypes. What approaches can enhance maturation?
A: Many organoid models simulate fetal rather than adult stages [5] [7]. To promote maturation:
- Extend culture duration: Develop protocols that support long-term maintenance, though this requires addressing nutrient diffusion issues [5].
- Enhance vascularization: Implement strategies to improve nutrient and oxygen supply, which is critical for long-term growth and functional maintenance [5] [7].
- Apply physiological cues: Incorporate appropriate mechanical stimulation, flow dynamics, and electrical activity patterns that mirror native tissue development [5].
Troubleshooting Guide: Overcoming Functional Limitations
Problem: Organoids exhibit central necrosis and limited survival time, restricting long-term studies.
| Possible Cause | Diagnostic Approach | Solution Strategies |
|---|---|---|
| Inadequate vascularization | Histological staining for necrotic cores; oxygen sensor assays | Implement organoid slicing to increase oxygen permeability [7]; develop vascularized organoids through co-culture with endothelial cells [5] |
| Limited nutrient diffusion | Measure glucose/lactate levels in culture medium over time | Use oscillating cultures to improve nutrient exchange [5]; reduce organoid size or use spinoid cultures to enhance medium perfusion [5] |
| Metabolic waste accumulation | Analyze culture medium for accumulated metabolites | Increase medium exchange frequency; implement perfusion systems such as organoids-on-chips for continuous waste removal [5] |
Problem: Organoids show poor electrophysiological function and synaptic connectivity, particularly in neural models.
| Possible Cause | Diagnostic Approach | Solution Strategies |
|---|---|---|
| Insufficient maturation time | Track electrophysiological activity over extended periods (≥6 months) | Extend culture duration with enhanced maintenance protocols; consider transplantation into host models to promote maturation [7] |
| Lack of appropriate cell types | Single-cell RNA sequencing to characterize cellular composition | Incorporate interneurons or glial cells through co-culture; use patterning factors to direct regional specification [7] |
| Metabolic stress | Measure expression of stress marker genes (e.g., UPR genes) | Optimize culture medium composition; ensure proper oxygen levels without creating hypoxic cores [7] |
Experimental Protocols for Enhanced Organoid Research
Protocol: Establishing Co-culture for Enhanced Cellular Diversity
Objective: To introduce vascular endothelial cells into neural organoids to improve nutrient delivery and mimic neurovascular interactions.
Materials:
- Cultrex Basement Membrane Extract or similar ECM matrix [76]
- Neural organoids at early differentiation stage (day 20-30)
- Human umbilical vein endothelial cells (HUVECs) or iPSC-derived endothelial cells
- Endothelial cell growth medium supplements (VEGF, FGF-2)
Methodology:
- Allow neural organoids to form for 20-30 days using established protocols [77].
- Gently harvest organoids and resuspend in a solution of endothelial cells (1:5 ratio) in diluted ECM matrix [5].
- Plate the organoid-endothelial cell mixture in low-attachment plates and culture for 24 hours to allow aggregation.
- Transfer aggregates to ECM-coated plates for embedded culture or maintain in suspension based on experimental needs.
- Supplement culture medium with VEGF (50ng/mL) and FGF-2 (25ng/mL) to support endothelial network formation [5].
- Monitor endothelial integration daily via microscopy; validate through immunostaining for CD31 (endothelial marker) and neural markers (e.g., TUJ1, MAP2).
Quality Control:
- Include organoid-only controls without endothelial cells
- Assess viability weekly using live/dead staining
- Confirm functional integration through perfusion assays if using organoid-chip systems
Protocol: Reducing Organoid Heterogeneity Through Automated Culture
Objective: To minimize batch-to-batch variability in intestinal organoid cultures using automated systems.
Materials:
- Robotic liquid handling system with temperature control
- Commercially available intestinal organoid culture kit
- Lgr5+ stem cells or intestinal crypt isolates [77]
- 96-well ultra-low attachment plates
Methodology:
- Program liquid handler to prepare master mix of basement membrane matrix and cell suspension [5] [76].
- Dispense consistent 30μL droplets of the cell-matrix mixture into the center of each well of a 96-well plate.
- Polymerize matrix droplets at 37°C for 20 minutes.
- Automatically add precisely measured organoid culture medium (100μL/well) containing Wnt agonists and R-spondin [77].
- Program scheduled medium changes (every 3-4 days) with integrated waste removal and fresh medium addition.
- For passaging, use automated enzymatic digestion and re-plating at fixed ratios (recommended 1:3-1:5 split ratio).
Quality Control:
- Image 10+ random organoids per batch for size quantification
- Analyze marker expression (e.g., Lgr5 for stem cells, Muc2 for goblet cells) via qPCR to verify consistent cellular composition
- Compare size distribution and growth curves across batches to quantify reproducibility
Essential Research Reagent Solutions
Table: Key Reagents for Advanced Organoid Culture
| Reagent Category | Specific Examples | Function in Organoid Culture |
|---|---|---|
| Extracellular Matrices | Cultrex Basement Membrane Extract, Matrigel [76] | Provides 3D scaffold mimicking native stem cell niche; supports self-organization and polarization [5] [77] |
| Stem Cell Niche Factors | R-spondin-1, Noggin, Wnt-3a [77] | Maintains stemness and promotes self-renewal of adult stem cell-derived organoids; critical for long-term expansion [77] |
| Patterning Molecules | BMP inhibitors, FGF, Retinoic Acid [7] | Directs regional specification in pluripotent stem cell-derived organoids; enhances cellular diversity and arealization [7] |
| Maturation Factors | Thyroid hormone, Dexamethasone, BDNF [5] | Promotes functional maturation of organoids; particularly important for achieving adult-like phenotypes in neural models [5] |
| Cell Type-Specific Media | Intestinal, Cerebral, Hepatic Organoid Media [76] | Tailored formulations supporting specific organoid lineages; enhances reproducibility and protocol standardization [76] |
Visualizing Experimental Workflows
Organoid Quality Control and Troubleshooting Workflow
3Rs Implementation Strategy for Organoid Research
The convergence of the 3Rs principles with technological advancements in organoid research represents a pivotal moment in biomedical science. By addressing key challenges such as limited cellular diversity, functional immaturity, and batch-to-batch variability, researchers can develop increasingly sophisticated human-relevant models that reduce reliance on animal testing while potentially improving predictive accuracy for human outcomes. The protocols, troubleshooting guides, and resources provided here offer practical pathways for scientists to contribute to this evolving paradigm, aligning research practices with both ethical imperatives and regulatory evolution as embodied in the FDA Modernization Act 2.0.
Personalized medicine represents a paradigm shift in healthcare, moving away from a "one-size-fits-all" approach to therapies tailored to an individual's unique genetic makeup. This approach has demonstrated remarkable success in two distinct areas: oncology and cystic fibrosis (CF). In oncology, precision therapies target specific genetic mutations driving cancer growth [78] [79]. In cystic fibrosis, modulator drugs correct the underlying protein defects caused by genetic mutations [80] [81]. Organoid technology now serves as a crucial bridge in this pipeline, providing patient-derived in vitro models that replicate in vivo physiology for more effective drug screening and personalized treatment planning [82] [83]. However, a significant challenge remains in ensuring these organoid models fully capture the cellular diversity found in native tissues, which is essential for accurate disease modeling and treatment prediction.
Success Stories in Personalized Oncology
Bryce Olson: Genomic Sequencing and Targeted Therapy
Bryce Olson, a patient with advanced metastatic prostate cancer, exemplifies the power of genomic sequencing in personalized oncology. After standard treatments failed, he demanded comprehensive genomic sequencing of his tumor, which revealed a mutation in the PI3K signaling pathway and a tumor suppressor gene called PTEN [79]. Armed with this molecular information, he enrolled in a Phase I clinical trial at Cedar Sinai targeting this specific pathway. The targeted therapy suppressed his cancer for two years, more than tripling his median survival expectations [79]. Olson's experience inspired his "Sequence Me" movement, encouraging patients to seek genomic profiling to access targeted treatments and clinical trials beyond standard care options [79].
Precision Oncology Successes
Various patients have experienced remarkable recoveries through precision oncology approaches. Some patients who were told to prepare for palliative care achieved complete recovery by accessing targeted therapies based on their cancer's genetic profile [78]. These successes are made possible by precision oncology experts who utilize peer-reviewed scientific evidence to identify the most effective treatments for each unique form of cancer, dramatically increasing treatment success rates [78].
Table 1: Key Molecular Targets in Personalized Oncology
| Molecular Target | Associated Cancer | Therapeutic Approach | Outcome |
|---|---|---|---|
| PI3K Signaling Pathway | Advanced Prostate Cancer | Phase I Clinical Trial Inhibitor | Cancer suppression for 2+ years [79] |
| PTEN Tumor Suppressor | Advanced Prostate Cancer | Targeted Pathway Blockade | Tripled median survival [79] |
| Unspecified Mutations | Various Cancers | Precision Targeted Therapy | Complete recovery from palliative diagnosis [78] |
Organoids in Personalized Cancer Treatment
Patient-derived organoids (PDOs) have emerged as powerful tools in personalized oncology. These three-dimensional cultures are derived from patient tumor tissues and retain the histological and genetic composition of their tissue of origin [3]. They enable personalized drug screening and precision treatment strategies by replicating tumor heterogeneity in vitro [3]. The establishment of "living biobanks" from consecutive colorectal carcinoma patients has created resources that closely recapitulate original tumor properties, genetic changes, and molecular subtypes, facilitating drug development and personalized treatment approaches [3].
Success Stories in Cystic Fibrosis Drug Screening
Caleb: CFTR Modulator Therapy
Ten-year-old Caleb exemplifies the transformative potential of CFTR modulator drugs. With a common CF mutation causing a gating abnormality in the CFTR protein, Caleb initially required 30+ daily enzymes, multivitamins, and several hours in a vibrating vest to loosen lung mucus [80]. His introduction to Orkambi (Kalydeco) represented "a complete 180" according to his mother [80]. This drug combination targets the genetic defect of CF by correcting the protein abnormality [80]. For Caleb, the results were dramatic: improved nutrient absorption and lung function, reduced vest therapy from three hours to just one daily, perfect school attendance, and the ability to play competitive basketball—an unthinkable achievement before treatment [80].
Evelyn: Early Diagnosis and Comprehensive Care
Evelyn's story highlights the importance of early diagnosis through newborn screening and comprehensive care. Diagnosed at just two weeks old through Florida's Newborn Screening program, Evelyn immediately received specialized care at Johns Hopkins All Children's Hospital [84]. This early intervention allowed her care team to avoid "failure to thrive" outcomes through meticulous weight management and nutritional support [84]. The hospital's accredited Cystic Fibrosis Center provided access to breakthrough therapies including recent modulator drugs that improve lung function, weight, and survival [84]. The center's designation as a CF Foundation Therapeutic Development Center provides patients access to research studies leading to breakthrough therapies [84].
Enid: Gene Therapy Clinical Trial
Enid Katz represents hope for CF patients with mutations not eligible for CFTR modulator treatments. Despite a rigorous daily care regimen starting at 4 a.m. that includes five different breathing treatments, an oscillating vest, and numerous medications, Enid developed antibiotic-resistant infections [81]. Since she lacks mutations eligible for CFTR modulator treatment, Enid became the first patient in an experimental gene therapy trial at Columbia University [81]. The therapy delivers a functional copy of the CFTR gene encased in a deactivated adeno-associated virus to airway cells via nebulizer, triggering production of normal CFTR protein without altering the genome itself [81]. Enid participates in the 53-week trial to determine safety and duration of effect, paving the way for new treatments for CF patients with rare mutations [81].
Table 2: Cystic Fibrosis Treatment Approaches and Outcomes
| Treatment Approach | Mechanism of Action | Patient Population | Documented Outcomes |
|---|---|---|---|
| CFTR Modulators (Orkambi/Kalydeco) | Correct protein gating abnormality | Specific CF mutations (~8% of CF population) | Improved lung function, reduced treatment time, normal activities [80] |
| Comprehensive Care Management | Multidisciplinary care, nutritional support, airway clearance | All CF patients | Avoided failure to thrive, improved nutritional scores [84] |
| Experimental Gene Therapy | Delivers functional CFTR gene via viral vector | Patients ineligible for modulators | Potential to benefit those with rare mutations [81] |
Technical Support: Organoid Culture for Drug Screening
FAQs for Organoid Research
Q: What are the key differences between PSC-derived and tissue stem cell-derived organoids? A: Pluripotent stem cell (PSC)-derived organoids are generated from embryonic or induced pluripotent stem cells through multi-step differentiation protocols mimicking embryonic development. They contain complex cellular components including mesenchymal, epithelial, and sometimes endothelial cells, making them ideal for developmental studies. Tissue stem cell-derived organoids come directly from adult tissues with simpler procedures, contain primarily epithelial cell types, and better represent adult tissue physiology. The choice depends on your research goals: developmental biology (PSC) versus adult tissue modeling and disease (tissue-derived) [82] [83].
Q: How can I improve cellular diversity in my organoid cultures? A: Enhancing cellular diversity requires mimicking the native tissue microenvironment. Consider these approaches: (1) Incorporate multiple cell types through co-culture systems; (2) Utilize specialized medium formulations containing appropriate growth factors and morphogens; (3) Implement "apical-out" organoid protocols for better access to luminal surfaces; (4) Optimize extracellular matrix composition to better represent native stem cell niches; (5) Integrate microfluidics devices to control flow, gradient formation, and shear stress [3] [83].
Q: What are common challenges in establishing patient-derived organoid lines? A: Key challenges include: (1) Maintaining tissue viability during processing—process within 6-10 hours or cryopreserve; (2) Microbial contamination—use antibiotic washes during tissue collection; (3) Batch-to-batch variation in matrices and media components; (4) Reproducibility across different patient samples; (5) Long-term maintenance of genetic stability [3] [4]. We recommend detailed record-keeping of all reagents and standardized protocols to improve reproducibility.
Q: How can I validate that my organoids adequately represent the original tissue? A: Validation should include: (1) Histological comparison to original tissue using immunofluorescence staining; (2) Genetic analysis to confirm maintenance of mutational profiles; (3) Functional assays appropriate to the tissue (e.g., barrier function, secretion, electrophysiology); (4) Single-cell RNA sequencing to characterize cellular heterogeneity; (5) Drug response profiling compared to known clinical responses [3] [83].
Troubleshooting Guide for Organoid Cultures
Table 3: Common Organoid Culture Issues and Solutions
| Problem | Potential Causes | Solutions | Prevention |
|---|---|---|---|
| Poor organoid formation | Low cell viability, suboptimal matrix, incorrect medium | Test matrix batches, verify growth factor activity, optimize seeding density | Process tissues promptly, use quality-controlled reagents [3] [4] |
| Limited cellular diversity | Missing niche factors, inadequate differentiation | Add relevant morphogens, implement co-culture, adjust differentiation timeline | Reference in vivo development for timing cues [82] [83] |
| Contamination | Non-sterile technique, contaminated reagents | Antibiotic/antimycotic treatment, test reagent sterility | Use antibiotics during initial processing, quarantine new shipments [3] |
| High batch-to-batch variability | Inconsistent tissue processing, reagent lot variations | Standardize protocols, bulk-purchase critical reagents | Maintain detailed records, use standardized SOPs [83] [4] |
| Poor drug penetration | Dense organoid structure, matrix barrier | Generate apical-out organoids, use smaller organoids, adjust matrix density | Optimize organoid size for specific assays [3] |
Research Reagent Solutions for Organoid Culture
Table 4: Essential Reagents for Organoid Research
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Extracellular Matrices | Engelbreth-Holm-Swarm (EHS) murine sarcoma matrix (e.g., Matrigel) | Provides 3D scaffold mimicking basement membrane | Use at 10-18 mg/ml concentration; batch variation requires testing [3] [4] |
| Essential Growth Factors | EGF, Noggin, R-spondin, Wnt3A | Maintain stemness and support proliferation | Critical for intestinal organoids; concentration varies by tissue type [3] [4] |
| Medium Supplements | N-Acetyl cysteine, Nicotinamide, B-27 | Antioxidant support, cell survival | Enhances viability across multiple organoid types [3] [4] |
| Signaling Inhibitors | A83-01, SB202190, Y-27632 | Inhibit differentiation, reduce apoptosis | Y-27632 (ROCK inhibitor) improves survival after passaging [4] |
| Tissue-Specific Factors | FGF-10, FGF-7, Gastrin, Heregulin-beta | Promote specific tissue identity | Varies by organoid type (e.g., FGF-10 for lung and pancreatic) [4] |
Experimental Protocols for Organoid-Based Drug Screening
Protocol: Establishing Patient-Derived Organoid Lines
Materials:
- Human colorectal tissue samples (normal, polyp, or tumor)
- Cold Advanced DMEM/F12 medium with antibiotics
- Engelbreth-Holm-Swarm (EHS) extracellular matrix
- Organoid culture medium with appropriate growth factors
- ROCK inhibitor Y-27632 (for improved viability)
- 6-well tissue culture plates
- Dissociation reagents (collagenase, dispase)
Procedure:
- Tissue Procurement: Collect human tissue samples under sterile conditions immediately after colonoscopy or surgical resection. Transfer in cold Advanced DMEM/F12 medium supplemented with antibiotics [3].
- Tissue Processing:
- For immediate processing (≤6-10 hour delay): Wash tissues with antibiotic solution and store at 4°C in DMEM/F12 medium with antibiotics.
- For delayed processing (>10 hours): Cryopreserve tissues using freezing medium (10% FBS, 10% DMSO in 50% L-WRN conditioned medium) [3].
- Crypt Isolation: Mechanically and enzymatically dissociate tissue to isolate crypt structures or single cells.
- Embedding in Matrix: Resuspend crypts/cells in liquid EHS matrix at 4°C. Dispense as droplets (~50μL) onto pre-warmed tissue culture plates. Incubate at 37°C for 20-30 minutes to solidify [4].
- Culture Initiation: Overlay solidified matrix domes with appropriate complete organoid medium. Include ROCK inhibitor for the first 2-3 days after initial plating to enhance survival [4].
- Medium Refreshment: Change medium every 2-3 days, observing organoid development under microscopy.
- Passaging: Once organoids reach appropriate size (typically 7-14 days), mechanically and enzymatically dissociate and replate at appropriate density.
Critical Steps:
- Maintain consistent temperature during matrix handling
- Process tissues promptly to maintain viability
- Adjust growth factor combinations based on tissue type
- Document organoid morphology and growth characteristics [3] [4]
Protocol: Drug Screening Using Patient-Derived Organoids
Materials:
- Established patient-derived organoids
- Test compounds in appropriate solvents
- Dimethyl sulfoxide (DMSO) for vehicle controls
- Cell viability assay reagents (e.g., ATP-based assays)
- Immunofluorescence staining reagents
- Matrigel or equivalent basement membrane matrix
Procedure:
- Organoid Preparation: Harvest and dissociate organoids to single cells or small fragments using enzymatic and mechanical dissociation.
- Seeding for Screening: Plate organoid fragments in matrix domes in 96-well plates suitable for high-throughput screening. Ensure uniform distribution and size.
- Drug Treatment: After organoids re-form (typically 3-5 days), add test compounds across a concentration range. Include vehicle controls and reference standards.
- Incubation and Assessment: Incubate for predetermined time (typically 5-7 days), refreshing drugs and medium as needed based on compound stability.
- Endpoint Analysis:
- Viability Assessment: Measure cell viability using ATP-based or similar assays.
- Morphological Analysis: Image organoids to assess size, structure, and viability markers.
- Molecular Analysis: For selected hits, process organoids for RNA/DNA extraction or immunohistochemistry.
- Data Analysis: Calculate IC50 values, compare to clinical response data when available, and prioritize hits based on efficacy and therapeutic index.
Validation:
- Compare organoid drug response to patient clinical response when available
- Include reference compounds with known activity
- Assess batch-to-batch variability using control organoids
- Confirm findings using orthogonal assay methods [3] [83]
Workflow and Signaling Pathway Diagrams
Diagram Title: Patient-Derived Organoid Workflow for Drug Screening
Diagram Title: Cystic Fibrosis Pathology and Treatment Strategies
Conclusion
Addressing the limited cellular diversity in organoid cultures is no longer an insurmountable challenge but an active frontier of innovation. The convergence of co-culture techniques, assembloid design, organ-on-chip engineering, and biofabrication is steadily closing the gap between in vitro models and in vivo physiology. While hurdles in standardization, vascularization, and long-term maturation remain, the integration of automation and AI promises to enhance reproducibility and scalability. The successful application of these complex organoids in predicting patient-specific drug responses and modeling intricate diseases underscores their transformative potential. Future efforts must focus on clinical translation, fostering interdisciplinary collaboration to fully realize the promise of organoids in ushering in a new era of human-relevant, ethical, and precise biomedical research and therapeutic development.
References
- 1. Give Them Vasculature and Immune Cells: How to Fill the Gap ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10711768/]
- 2. Generation of complex human organoid models including ... [https://www.nature.com/articles/s41598-019-52204-7]
- 3. A Practical Guide to Developing and Troubleshooting Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566426/]
- 4. Organoid Culture Guide [https://www.atcc.org/resources/culture-guides/organoid-culture-guide]
- 5. Strategies to overcome the limitations of current organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12033597/]
- 6. 2025 Trends: Organoids [https://www.genengnews.com/topics/genome-editing/2025-trends-organoids/]
- 7. Challenges of Organoid Research - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10559943/]
- 8. Animal-free alternatives for Matrigel in human iPSC- ... [https://www.nature.com/articles/s41598-025-20091-w]
- 9. Rethinking Matrigel: The Complex Journey to Matrix ... [https://pubmed.ncbi.nlm.nih.gov/41204762/]
- 10. The biological macromolecules constructed Matrigel for ... [https://www.sciencedirect.com/science/article/pii/S0927776524006945]
- 11. How to avoid common mistakes in organoid culture [https://www.linkedin.com/posts/proteintech-group_culturing-organoids-is-delicate-work-here-activity-7374836481858695168-lfuX]
- 12. Diversity in a dish: Leveraging organoids to reflect genetic ... [https://www.sciencedirect.com/science/article/pii/S2468451125000170]
- 13. Organoids are not organs: Sources of variation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10277837/]
- 14. Navigating Brain Organoid Maturation: From Benchmarking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383812/]
- 15. Brain organoids: a new paradigm for studying human ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1699814/full]
- 16. Trends and challenges in organoid modeling and expansion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11608026/]
- 17. Tumor organoid-immune co-culture models - Nature [https://www.nature.com/articles/s41420-025-02407-x]
- 18. Co-cultures of colon cancer cells and cancer-associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10228738/]
- 19. Troubleshooting Common Cell Culture Contamination Issues [https://cellculturecompany.com/troubleshooting-common-cell-culture-contamination-issues/]
- 20. Troubleshooting | Horizontal co-culture plate [https://i-coculture.com/troubleshooting/]
- 21. Geometrically-engineered human motor assembloids-on-a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484972/]
- 22. Assembloid models of cell-cell interaction to study tissue and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12143640/]
- 23. Evolving from organoid to assembloid with enhanced ... [https://www.sciopen.com/article/10.26599/CO.2025.9410010]
- 24. Assembloids | Nature Methods [https://www.nature.com/articles/s41592-020-01026-x]
- 25. Protocol for generating human assembloids to investigate ... [https://www.sciencedirect.com/science/article/pii/S266616672500036X]
- 26. Human assembloid model of the ascending neural sensory ... [https://www.nature.com/articles/s41586-025-08808-3]
- 27. Breathing on chip: Dynamic flow and stretch accelerate ... [https://www.sciencedirect.com/science/article/pii/S2590006423001734]
- 28. A 3D-printed multi-compartment organ-on-chip platform with a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11633827/]
- 29. The Role of Microfluidics for Organ on Chip Simulations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5590458/]
- 30. Human organoids-on-chips for biomedical research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10758054/]
- 31. Microfluidic Organ-on-A-chip: A Guide to Biomaterial Choice and Fabrication - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9966054/]
- 32. Organ-on-a-Chip Applications in Microfluidic Platforms [https://www.mdpi.com/2072-666X/16/2/201]
- 33. Organ-On-A-Chip: A Survey of Technical Results and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8866728/]
- 34. 类器官血管化的研究进展 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10477383/]
- 35. Vascularised organoids: Recent advances and applications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11882480/]
- 36. 图3 类器官培养流程和新技术 [https://www.china-oncology.com/CN/figure/showFigure.do?fid=3171]
- 37. 【日本科技動態】慶應大學確立運用飛秒雷射的極細人工血管 ... [https://www.facebook.com/tnstorg/posts/%E6%97%A5%E6%9C%AC%E7%A7%91%E6%8A%80%E5%8B%95%E6%85%8B%E6%85%B6%E6%87%89%E5%A4%A7%E5%AD%B8%E7%A2%BA%E7%AB%8B%E9%81%8B%E7%94%A8%E9%A3%9B%E7%A7%92%E9%9B%B7%E5%B0%84%E7%9A%84%E6%A5%B5%E7%B4%B0%E4%BA%BA%E5%B7%A5%E8%A1%80%E7%AE%A1%E5%9F%B9%E9%A4%8A%E6%8A%80%E8%A1%93%E8%BF%91%E5%B9%B4%E4%BE%86%E9%9A%A8%E8%91%97%E9%A1%9E%E5%99%A8%E5%AE%98%E5%9F%B9%E9%A4%8Aorganoid-culture%E5%92%8C%E4%BB%BF%E7%94%9F%E7%B3%BB%E7%B5%B1biomimetic-system%E7%AD%89%E7%B4%B0%E8%83%9E/1179938084241753/]
- 38. “未来健康”追踪系列:“人体替身”的技术革命——类器官和 ... [http://www.biecc.com.cn/Industrial/vehicles/2025/0916/1820.html]
- 39. Recent advances in defined hydrogels in organoid research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10273284/]
- 40. Effects of hydrogel stiffness and viscoelasticity on organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11877758/]
- 41. Dynamic hydrogel mechanics in organoid engineering [https://www.sciencedirect.com/science/article/pii/S2452199X2500427X]
- 42. Towards organoid culture without Matrigel [https://www.nature.com/articles/s42003-021-02910-8]
- 43. Recent advances in defined hydrogels in organoid research [https://www.sciencedirect.com/science/article/pii/S2452199X23001779]
- 44. Frontiers | Organoid scaffold materials: research and application [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1637456/full]
- 45. AI-enabled organoids: Construction, analysis, and application [https://pmc.ncbi.nlm.nih.gov/articles/PMC10511344/]
- 46. Could Organoids Make Animal Models Obsolete in Research? [https://www.news-medical.net/health/Can-Organoids-Replace-Animal-Models-in-Human-Disease-Research.aspx]
- 47. Automating Brain Organoid Culture Process [https://www.moleculardevices.com/lab-notes/3d-biology/automating-brain-organoid-culture]
- 48. Computational modeling of necrosis in neural organoids [https://pubmed.ncbi.nlm.nih.gov/40654625/]
- 49. An Efficient Organoid Cutting Method for Long-Term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209159/]
- 50. Geneva Researcher Develops Breakthrough Method to ... [https://genevausa.org/news/story/geneva-researcher-develops-breakthrough-method-to-improve-long-term-organoid-culture/]
- 51. Self-assembled organoid-tissue modules for scalable ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706125002016]
- 52. Organoids-on-a-chip: microfluidic technology enables ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1515340/full]
- 53. How To Promote Batch-To-Batch Consistency In CAR-T ... [https://www.cellandgene.com/doc/how-to-promote-batch-to-batch-consistency-in-car-t-therapies-0001]
- 54. Breakthroughs and challenges of organoid models for ... [https://www.nature.com/articles/s41420-025-02505-w]
- 55. Towards a quality control framework for cerebral cortical ... [https://www.nature.com/articles/s41598-025-14425-x]
- 56. An integrated transcriptomic cell atlas of human endoderm- ... [https://www.nature.com/articles/s41588-025-02182-6]
- 57. Integrating single-cell RNA-seq datasets with substantial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577435/]
- 58. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 59. Identifying sources of batch to batch variation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0032591007003683]
- 60. A 4096 channel event-based multielectrode array with ... [https://www.nature.com/articles/s41467-024-50783-2]
- 61. Technical Support (FAQ) [https://microprobes.com/support-and-download/technical-support]
- 62. 11+ Most Common Data Integration Challenges & Solutions [https://estuary.dev/blog/data-integration-challenges/]
- 63. A biosensor for detecting changes in cognitive processing ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566301001634]
- 64. Patient-derived organoids predict treatment response in ... [https://pubmed.ncbi.nlm.nih.gov/40982295/]
- 65. Organoid Culture Frequently Asked Questions [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/3d-cell-culture/organoid-culture-faqs?srsltid=AfmBOooeuwbyRDtTRnigklxoFGaqpIEjhnhSdlcyf2NsMwD5x-TN88NB]
- 66. PharmaFormer predicts clinical drug responses through ... [https://www.nature.com/articles/s41698-025-01082-6]
- 67. From 3D to 2D: Harmonization of Protocols for Two- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8799680/]
- 68. Quantitative characterization of tissue states using ... [https://www.nature.com/articles/s41588-025-02119-z]
- 69. Advancing Cellular Research Beyond 2D Cultures [https://pharmafeatures.com/the-3d-revolution-advancing-cellular-research-beyond-2d-cultures/]
- 70. Human organoids: model systems for human biology and ... [https://www.nature.com/articles/s41580-020-0259-3]
- 71. The Use of Organoid Cultures in Advancing Nutrition ... [https://www.sciencedirect.com/science/article/pii/S2161831325001255]
- 72. Regulatory Applications of 3Rs - National Toxicology Program [https://ntp.niehs.nih.gov/whatwestudy/niceatm/accept-methods/apps]
- 73. The 3Rs and Humane Experimental Technique [https://pmc.ncbi.nlm.nih.gov/articles/PMC6826930/]
- 74. Animal Use Alternatives (3Rs) | National Agricultural Library [https://www.nal.usda.gov/animal-health-and-welfare/animal-use-alternatives]
- 75. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 76. Protocols & Troubleshooting Guides [https://www.rndsystems.com/resources/protocols-troubleshooting-guides]
- 77. Organoids | Nature Reviews Methods Primers [https://www.nature.com/articles/s43586-022-00174-y]
- 78. Precision Oncology Success Stories | Personalized Cancer ... [https://www.ctoam.com/success-stories]
- 79. Personalized Medicine for Advanced Stage Cancer Patients [https://www.synthego.com/blog/bryce-olson-personalized-medicine-crispr/]
- 80. Caleb: Cystic Fibrosis Drug Helps him Live his Basketball ... [https://www.childrenscolorado.org/doctors-and-departments/departments/breathing-institute/patient-stories/caleb-cystic-fibrosis-drug-helps-him-live-his-dreams/]
- 81. Enid's Story: Cystic Fibrosis Clinical Trial Offers Hope [https://www.columbiadoctors.org/news/enids-story-cystic-fibrosis-clinical-trial-offers-hope]
- 82. Human organoids in basic research and clinical applications [https://www.nature.com/articles/s41392-022-01024-9]
- 83. Human organoids: a new dimension in cell biology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6724519/]
- 84. Cystic Fibrosis: Evelyn's Story [https://www.hopkinsmedicine.org/health/conditions-and-diseases/cystic-fibrosis/patient-story-evelyn]