Spatial Multiomics: Mastering ISH and Immunohistochemistry Co-Localization for Precision Biomarker Discovery
This article provides a comprehensive guide to in situ hybridization (ISH) and immunohistochemistry (IHC) co-localization studies, a cornerstone of spatial biology.
Spatial Multiomics: Mastering ISH and Immunohistochemistry Co-Localization for Precision Biomarker Discovery
Abstract
This article provides a comprehensive guide to in situ hybridization (ISH) and immunohistochemistry (IHC) co-localization studies, a cornerstone of spatial biology. Tailored for researchers and drug development professionals, it covers foundational principles, advanced methodological workflows, critical optimization strategies, and rigorous validation frameworks. By synthesizing current techniques—from automated protease-free assays to super-resolution expansion microscopy—this resource empowers scientists to precisely visualize nucleic acids and proteins within their morphological context, thereby accelerating biomarker development, therapeutic efficacy assessments, and mechanistic action studies in oncology and beyond.
The Spatial Biology Landscape: Core Principles of ISH and IHC Co-Localization
The spatial relationship between RNA, DNA, and proteins within the cellular architecture provides critical insights into gene regulation, disease mechanisms, and therapeutic development. Co-localization studies aim to precisely determine where these biomolecules interact within their morphological context, revealing functional relationships that are obscured in bulk analyses. This field has gained significant momentum with advancements in spatial biology technologies and computational frameworks that enable researchers to move beyond simple pairwise interactions to complex multi-molecular relationships. The integration of in situ hybridization (ISH) with immunohistochemistry (IHC) has emerged as a powerful approach for visualizing multiple molecular species within intact tissues and cells, preserving the architectural context essential for understanding biological complexity. This guide compares the leading methodological approaches for studying these interactions, evaluating their technical capabilities, applications, and limitations to inform research and drug development efforts.
Methodological Approaches for Co-Localization Analysis
Researchers have developed several sophisticated methods to tackle the challenges of visualizing and quantifying RNA-DNA-protein interactions. The table below compares three advanced approaches for co-localization studies.
Table 1: Comparison of Co-Localization Methodological Approaches
| Method | Core Principle | Spatial Resolution | Key Applications | Throughput |
|---|---|---|---|---|
| Sequential IHC & Image Registration [1] | Sequential staining of adjacent tissue sections with image alignment | Cellular scale (a few cells) | Biomarker colocalization in FFPE tissue, protein-protein interaction studies | Medium |
| RNA Fluorescence Three-Hybrid (rF3H) [2] | Anchoring RNA to specific subcellular structures to detect recruited proteins | Subcellular | RNA-protein interaction dynamics in living cells, characterization of RBPs | High |
| Interaction Triad Analysis [3] | Computational filtering of pairwise interaction data (RNA-DNA, protein-DNA, RNA-protein) | Genomic locus level | Identification of functional RNA-protein-DNA complexes, chromatin regulation studies | Very High (computational) |
Detailed Experimental Protocols
Combined ISH and IHC on Archival Tissues
This protocol enables simultaneous detection of RNA and protein within the same tissue section, allowing precise compartmentalization of signals between tumor epithelia and stroma [4].
- Tissue Preparation: Cut 3 µm sections from formalin-fixed paraffin-embedded (FFPE) tissue blocks. Deparaffinize in xylene and rehydrate through a graded ethanol series.
- Antigen Retrieval & Permeabilization: Incubate sections with 15 μg/mL Proteinase K at 37°C for 10 minutes. Optimal concentration and time should be determined by titration.
- In Situ Hybridization:
- Pre-hybridize with ISH buffer for 30 minutes.
- Hybridize with DIG-labeled miR probes (e.g., miR-204-5p) at 53°C for 2 hours.
- Perform stringent washes with SSC buffer at the corresponding hybridization temperature.
- Immunohistochemistry:
- Block with 2% sheep serum and 1% BSA.
- Incubate with primary antibody against epithelial markers (e.g., pan-cytokeratin) followed by HRP-conjugated secondary antibody.
- Dual Detection:
- Detect miR signals using alkaline phosphatase (AP)-conjugated anti-DIG antibody with NBT/BCIP chromogen (purple/black precipitate).
- Detect protein signals using DAB chromogen (brown precipitate).
- Quantification: Use image analysis software (e.g., ImageJ or Aperio ImageScope) to quantify miR expression specifically within the stromal compartment defined by the absence of pan-cytokeratin staining.
RNA Fluorescence Three-Hybrid (rF3H) Method
This live-cell method detects RNA-protein interactions by visualizing protein recruitment to artificially anchored RNAs [2].
- Plasmid Design:
- Construct an RNA trap plasmid (e.g., pMCP-EGFP-LacI) encoding a fusion protein with an RNA-binding module (e.g., MS2 coat protein), a fluorescent protein (e.g., EGFP), and a localization signal (e.g., LacI for lacO genomic sites).
- Engineer the RNA of interest (ROI) to include recognition sequences (e.g., MS2 stem-loops).
- Tag the putative RNA-binding protein (RBP) with a fluorescent marker (e.g., mCherry).
- Cell Culture & Transfection:
- Culture appropriate cell lines (e.g., BHK cells with genomic lacO integration or HeLa cells).
- Co-transfect the three plasmids (RNA trap, ROI, RBP) in a mass ratio of 1:1:1 using lipid-based transfection reagents.
- Live-Cell Imaging & Analysis:
- Image cells 24-48 hours post-transfection using confocal microscopy.
- Detect co-localization by the enrichment of the RBP-mCherry signal at the specific subcellular structures where the RNA trap-EGFP is anchored.
- Quantify fluorescence intensity at these anchored structures compared to the nucleoplasm.
Interaction Triad Analysis
This computational approach integrates heterogeneous omics datasets to identify functional three-component interactions [3].
- Data Collection:
- RNA-DNA contacts (RD-contacts): From all-to-all methods like RADICL-seq or GRID-seq.
- Protein-DNA contacts (PD-contacts): From ChIP-seq experiments (e.g., from ENCODE, ReMap).
- RNA-protein contacts (PR-contacts): From RIP-seq, fRIP-seq, or eCLIP experiments.
- Data Processing:
- Process ChIP-seq data with MACS2 peak caller (q-value < 0.05).
- Map RNA-protein immunoprecipitation data to the genome using HISAT2 and call peaks using Piranha.
- Triad Construction:
- Intersect the three pairwise interaction datasets.
- Define a triad when an RNA (R), a protein (P), and a DNA locus (D) are connected by significant R-D, P-D, and R-P interactions.
- Statistical Validation:
- Assess significance by comparing against background models of random pairwise interactions.
- Filter triads further using functional annotations (e.g., ChromHMM chromatin states).
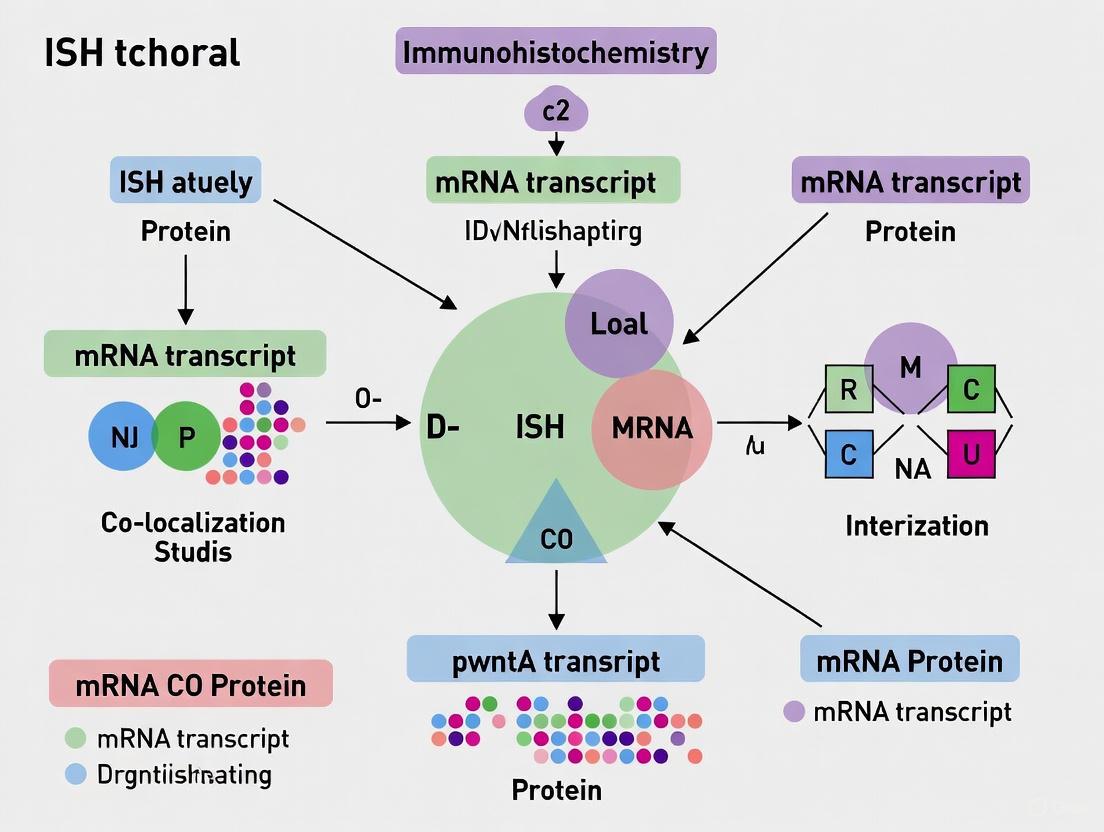
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful co-localization experiments require carefully selected reagents and tools. The following table details key solutions for implementing these methodologies.
Table 2: Essential Research Reagents and Materials for Co-Localization Studies
| Reagent/Material | Function | Example Application |
|---|---|---|
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissues | Preserves tissue morphology and biomolecule integrity for archival studies | Combined ISH-IHC on patient cohorts [4] |
| Locked Nucleic Acid (LNA) Probes | Enhanced sensitivity and specificity for RNA detection in ISH | Detection of microRNAs (e.g., miR-204) in tumor stroma [4] |
| Digoxigenin (DIG)-Labeled Probes | Non-radioactive label for nucleic acid detection | ISH with anti-DIG antibodies and colorimetric detection [5] [4] |
| Proteinase K | Enzyme for antigen retrieval and tissue permeabilization | Unmasking target epitopes and RNA in FFPE sections [5] [4] |
| Saline-Sodium Citrate (SSC) Buffer | Controls stringency of hybridization through ion concentration | Post-hybridization washes to remove non-specific probe binding [5] [4] |
| MS2 Stem-Loop System | RNA tagging and trapping in live cells | rF3H method for visualizing RNA-protein interactions [2] |
| NBT/BCIP Substrate | Chromogenic substrate for alkaline phosphatase | Colorimetric detection (purple/black) of RNA in ISH [4] |
| DAB Substrate | Chromogenic substrate for horseradish peroxidase | Colorimetric detection (brown) of proteins in IHC [4] |
| Image Analysis Software (ImageJ, Aperio) | Digital quantification of signal intensity and localization | Objective measurement of expression in specific tissue compartments [4] |
| victoria blue 4R(1+) | Victoria Blue 4R(1+) | Basic Blue 8 | For Research Use | Victoria Blue 4R(1+) is a cationic triphenylmethane dye for histology and research. It is applied in elastic fiber staining. For Research Use Only. Not for human use. |
| 2-(4-hydroxy-3-methoxyphenyl)acetaldehyde | 2-(4-Hydroxy-3-methoxyphenyl)acetaldehyde|Homovanillin | 2-(4-Hydroxy-3-methoxyphenyl)acetaldehyde (Homovanillin), a key dopamine metabolite. For Research Use Only. Not for human or veterinary use. |
Quantitative Comparison of Method Performance
Understanding the capabilities and limitations of each method is crucial for experimental design. The table below summarizes key performance metrics based on published data.
Table 3: Performance Metrics of Co-Localization Methods
| Performance Metric | Sequential IHC & Registration | Combined ISH-IHC | rF3H Method | Interaction Triads |
|---|---|---|---|---|
| Registration Accuracy | Cellular scale (a few cells) [1] | Cellular/subcellular [4] | Subcellular [2] | Locus level [3] |
| Multiplexing Capacity | Limited by serial sections | 2-3 targets simultaneously [4] | Multiple targets with different colors [2] | Genome-wide [3] |
| Throughput | Medium | Medium | Medium to High | Very High |
| Tissue Context Preservation | High (archival tissues) [1] | High (archival tissues) [4] | Limited (cell cultures) | Computational inference |
| Live-Cell Capability | No | No | Yes [2] | No |
| Noise Reduction Efficiency | Not applicable | Not applicable | Not applicable | Significant vs pairwise data [3] |
The methodological landscape for co-localization studies has expanded significantly, offering researchers multiple pathways to investigate RNA-DNA-protein interactions within morphological context. Combined ISH-IHC provides a robust, accessible approach for archival tissues with direct clinical relevance. The rF3H method enables dynamic studies of RNA-protein interactions in living cells with high specificity. Interaction triad analysis offers a powerful computational framework for extracting functional insights from noisy genome-wide datasets. The choice of method depends critically on the research question, required resolution, tissue availability, and technical capabilities. As these technologies continue to evolve, they will further illuminate the spatial organization of molecular interactions, advancing both basic research and drug development efforts.
Immunohistochemistry (IHC) stands as a cornerstone technique in life science research and clinical diagnostics, enabling the precise detection and localization of specific antigens within tissue samples. By leveraging highly specific antibody-epitope interactions, IHC allows researchers and pathologists to visualize the distribution and abundance of proteins in their proper histological context, providing invaluable insights into cellular function, disease mechanisms, and treatment responses [6] [7]. The technique has evolved significantly since its inception, with modern IHC offering both chromogenic and fluorescent detection capabilities to address diverse research needs [6] [8]. This guide explores the fundamental principles and procedural workflow of IHC, with particular emphasis on its application in co-localization studies alongside in situ hybridization (ISH) for comprehensive spatial biology analysis. Understanding the complete IHC workflow—from sample preparation through antibody selection to final detection—is essential for generating reliable, reproducible data that advances our understanding of complex biological systems in both health and disease.
Fundamental Principles of IHC
Historical Development and Core Principles
The conceptual foundation of IHC traces back to pioneering work in immunology and histology, with critical developments emerging throughout the 20th century. The technique fundamentally combines anatomical, immunological, and biochemical approaches to image discrete components in tissues using appropriately labeled antibodies that bind specifically to their target antigens in situ [9]. The earliest breakthroughs came with the identification of antibody-antigen interactions, for which Paul Ehrlich received the Nobel Prize in 1908 [6]. However, it was Albert H. Coons and colleagues in the 1940s who developed the first fluorescently conjugated antibody system closely resembling contemporary methods, using fluorescein-labeled anti-pneumococcal antibodies to detect bacteria within macrophages [6] [7]. Reflecting on his work, Coons noted the aesthetic appeal of fluorescent antibodies, describing how they "shine in the dark, a brilliant greenish-yellow glow" like "pebbles in the moonlight" that "weave a pattern in the forest which leads the weary children home" [6].
The core principle of IHC involves specific binding of antibodies tagged with labels to target antigens within tissues, enabling visualization of the localization and distribution of specific antigens [7]. This binding occurs between the paratope of an antibody and a specific epitope on the target antigen, creating a stable complex that can be visualized through various detection methods. The technique can be performed using either direct or indirect methods, with the indirect approach employing secondary antibodies that bind to the primary antibody to provide signal amplification [7] [10]. IHC is particularly valued for its ability to provide spatial context that other protein detection methods like western blot or ELISA cannot offer, as it preserves the architectural relationships between cells and tissues while enabling specific protein detection [6].
Comparison with Other Protein Detection Techniques
When selecting appropriate protein detection methodologies, researchers must consider the unique advantages and limitations of each technique. The table below provides a comparative analysis of IHC against other common protein detection methods:
Table 1: Comparison of IHC with Other Protein Detection Techniques
| Parameter | IHC/ICC | Western Blot | ELISA |
|---|---|---|---|
| Sample Preparation | Fixed cells on coverslip (ICC) or fixed tissue sections (IHC) | Lysed cells, denatured protein | Lysed cells or tissue, biological fluids |
| Protein State | In situ, but fixed | Denatured | Native, unfixed |
| Multiplex Capability | Easily up to 4 targets; more possible with advanced methods | Possible with fluorescent multiplexing or sequential blotting | Typically requires bead-based immunoassays |
| High Throughput | Yes | Rarely | Commonly |
| Sensitivity | Medium | High | High |
| Specificity | Medium | High | High, particularly sandwich ELISA |
| Subcellular Localization | Highly suitable | Limited to subcellular fractionation | Limited to subcellular fractionation |
| Expression in Mixed Cell Populations | Highly suitable | Limited to cell sorting | Limited to cell sorting |
This comparative analysis highlights IHC's unique strength in providing spatial context for protein localization, which is particularly valuable for understanding protein function in heterogeneous tissues and investigating co-localization patterns with other biomarkers [6].
The Complete IHC Workflow
Sample Preparation and Fixation
The initial steps of sample preparation and fixation are critical for preserving tissue architecture and antigen integrity, ultimately determining the success of any IHC experiment. Proper fixation stabilizes cells and tissues to prevent degradation during processing while maintaining morphological detail essential for accurate interpretation [7]. The choice of fixing solution depends on sample type, target antigen, and downstream applications, with no universal fixative suitable for all situations [6]. Formaldehyde-based fixatives are most commonly used due to their strong tissue penetration and low background, creating methylene cross-links between proteins or between proteins and nucleic acids [6]. However, overfixation with formaldehyde can mask target epitopes through excessive cross-linking, necessitating optimization of fixation conditions including duration, temperature, and pH [6].
Alternative fixatives include glutaraldehyde, which provides stronger cross-linking but penetrates tissue more slowly and can produce high autofluorescence, and precipitative fixatives like methanol and ethanol, which cause protein precipitation by changing dielectric points but preserve morphology less effectively than formaldehyde [6]. Researchers can employ either perfusion fixation, where fixative is injected through the vascular system of an intact organism, or immersion fixation, where dissected tissue is placed directly into fixative [6]. Following fixation, tissues are typically embedded in paraffin or optimal cutting temperature (OCT) compound and sectioned into thin slices (usually 4-5μm) using a microtome or cryostat, then mounted onto slides, preferably charged or APES-coated slides for IHC to ensure proper adhesion during subsequent processing steps [10].
Antigen Retrieval and Tissue Blocking
For formalin-fixed, paraffin-embedded tissues, antigen retrieval represents a crucial step to reverse the cross-links formed during fixation that can mask target epitopes and prevent antibody binding [7]. This process typically involves heat-induced epitope retrieval (HIER), where slides are heated in a buffer solution (commonly citrate or EDTA-based at varying pH levels) using a microwave, pressure cooker, or water bath [10]. The specific retrieval conditions must be optimized for each primary antibody and tissue type, as insufficient retrieval results in weak staining while excessive retrieval can damage tissue morphology or create non-specific background [10]. Following antigen retrieval, tissues are blocked to prevent non-specific antibody binding. This involves incubating sections with protein-based blocking solutions (such as normal serum, BSA, or commercial blocking reagents) to occupy hydrophobic and charged sites that might otherwise interact non-specifically with antibodies [6] [9]. Additionally, for peroxidase-based detection systems, endogenous peroxidase activity must be quenched using hydrogen peroxide solutions, while endogenous phosphatase activity should be blocked when using alkaline phosphatase-based detection [10].
Antibody Incubation and Detection Systems
The core of IHC involves sequential antibody applications to specifically label target antigens. The process begins with incubation of the primary antibody, which specifically recognizes the target antigen [10]. Researchers must carefully select primary antibodies validated for IHC applications and optimize their concentrations through titration to balance specific signal against background staining [9]. Both monoclonal and polyclonal antibodies can be effective for IHC, with monoclonal antibodies offering higher specificity to a single epitope but potentially greater risk of epitope burial, while polyclonal antibodies recognize multiple epitopes, providing increased sensitivity but potentially more cross-reactivity [9].
Following primary antibody incubation, detection typically employs indirect methods using enzyme-conjugated secondary antibodies that recognize the host species of the primary antibody [7] [10]. Modern detection systems often utilize polymer-based technologies where multiple enzyme molecules are conjugated to a polymer backbone that binds to the primary antibody, providing significant signal amplification compared to traditional avidin-biotin complex (ABC) or streptavidin-biotin methods [10]. The enzymes most commonly used are horseradish peroxidase (HRP) and alkaline phosphatase (AP), each with distinct substrate options that produce different colored precipitates at the antigen site [10] [11]. The visualization step then employs chromogenic or fluorescent substrates that produce insoluble precipitates or fluorescence at the antigen location, enabling visualization under light or fluorescence microscopy, respectively [6] [10].
Counterstaining, Mounting, and Visualization
The final steps in IHC processing involve counterstaining to provide morphological context, mounting for preservation, and visualization through microscopy. Counterstaining uses dyes such as hematoxylin (for chromogenic detection) or nuclear stains like DAPI (for fluorescent detection) to highlight tissue architecture and cellular components that are not specifically labeled by the primary antibody [6] [10]. For chromogenic IHC, hematoxylin provides a blue nuclear stain that contrasts with brown (DAB) or red (AP-based) chromogen signals, allowing pathologists to assess the relationship between antigen expression and tissue morphology [10]. Following counterstaining, sections are dehydrated through graded alcohols, cleared in xylene, and mounted under coverslips using permanent mounting media for chromogenic detection or aqueous media for fluorescent detection [9]. Visualization then occurs using brightfield microscopy for chromogenic detection or fluorescence microscopy with appropriate filter sets for fluorescent detection, with digital imaging often employed for documentation and analysis [6] [8].
Figure 1: Comprehensive IHC Workflow. This flowchart illustrates the sequential steps in the immunohistochemistry process, from initial sample preparation through final visualization.
Detection Methods: Chromogenic vs. Fluorescent
Chromogenic Detection
Chromogenic detection represents the most widely used IHC detection method, particularly in clinical settings, due to its convenience, reliability, and compatibility with standard brightfield microscopy [12] [8]. This method utilizes enzyme-conjugated antibodies (typically HRP or AP) that generate colored precipitates at the antigen site when incubated with appropriate substrates [6] [10]. The most common chromogen is 3,3'-diaminobenzidine (DAB), which produces a brown precipitate when reacted with HRP and is preferred for most applications due to its permanent nature and strong staining intensity [10]. For tissues with inherent brown pigmentation (such as melanin), or for multiplexing applications, alternative chromogens including red (Vector Red, Fast Red), blue (Vector Blue), or purple substrates are available [8] [11]. Chromogenic IHC offers several advantages, including permanent slides that do not fade over time, compatibility with routine histology infrastructure, and the ability to easily visualize tissue morphology alongside specific staining [12] [8]. However, limitations include potential diffusion of the reaction product away from the antigen site, difficulty in multiplexing beyond 2-3 targets due to color overlap, and quantification challenges [8].
Fluorescent Detection
Immunofluorescence (IF) detection utilizes fluorophore-conjugated antibodies that are directly visualized using fluorescence microscopy [6]. This method has grown in popularity due to advances in fluorescence microscopy and the increasing availability and flexibility of fluorophores [6] [8]. Fluorescent detection can be performed using either direct methods (with fluorophore-conjugated primary antibodies) or, more commonly, indirect methods (with fluorophore-conjugated secondary antibodies) [9]. The key advantage of fluorescent detection lies in its capability for multiplexing, as multiple targets can be visualized simultaneously using fluorophores with non-overlapping emission spectra [6] [8]. Modern imaging systems can distinguish between 4-7 targets on the same tissue section, enabling sophisticated co-localization studies [8]. Additionally, fluorescent detection generally offers better resolution for subcellular localization and is more amenable to quantification than chromogenic methods [8]. Limitations include potential photobleaching, tissue autofluorescence, requirement for specialized microscopy equipment, and the inability to visualize underlying tissue morphology without additional counterstains [8].
Table 2: Comparison of Chromogenic and Fluorescent Detection Methods
| Parameter | Chromogenic Detection | Fluorescent Detection |
|---|---|---|
| Microscopy Requirements | Standard brightfield microscope | Fluorescence microscope with specific filter sets |
| Permanence | Permanent, fade-resistant | Subject to photobleaching over time |
| Multiplexing Capacity | Limited (typically 2-3 targets) | High (4+ targets with spectral separation) |
| Spatial Resolution | Good | Excellent for subcellular localization |
| Tissue Morphology | Easily visualized with counterstain | Obscured without brightfield counterstain |
| Quantification | Semi-quantitative, challenging | More amenable to quantification |
| Primary Applications | Diagnostic pathology, single targets | Multiplexing, co-localization studies, research |
| Cost Considerations | Lower equipment costs | Higher equipment and reagent costs |
Substrate Selection Considerations
Choosing appropriate substrates represents a critical decision point in IHC experimental design, with several technical factors influencing optimal selection [11]. For HRP-based systems, DAB provides the highest sensitivity and produces a sharp, dense precipitate ideal for intracellular targets or highly delineated locations [11]. Alternative HRP substrates are available in various colors including purple, red, blue, and green for multiplexing applications [11]. For AP-based systems, Vector Red, Vector Blue, and BCIP/NBT are common choices, with AP substrates generally producing more diffuse and translucent precipitates that allow better visualization of underlying tissue structure [11]. Sensitivity requirements should guide substrate selection, with different formulations of the same substrate offering varying detection thresholds; for example, ImmPACT substrates provide maximum sensitivity compared to standard formulations [11]. Researchers should also consider compatibility with visualization methods (brightfield, darkfield, electron microscopy), heat resistance for protocols requiring heating steps, and color contrast with both the tissue specimen and any counterstains [11].
Figure 2: Detection Method Decision Framework. This diagram outlines key considerations when selecting between chromogenic and fluorescent detection methods for IHC applications.
IHC in Co-localization Studies with ISH
Complementary Techniques for Spatial Biology
The integration of IHC with in situ hybridization (ISH) represents a powerful approach for co-localization studies, enabling researchers to simultaneously investigate protein expression and nucleic acid distribution within the spatial context of tissues [12]. While IHC detects protein antigens using antibody-epitope interactions, ISH identifies specific DNA or RNA sequences through complementary nucleic acid probes [12]. This combination provides comprehensive molecular profiling within morphological context, particularly valuable for understanding gene expression patterns, viral infection detection, and characterizing genetic alterations alongside protein expression [12]. For cancer research specifically, IHC-ISH co-localization can identify tumor cells with specific genetic abnormalities while characterizing their protein expression profiles, enabling more precise tumor classification and insights into tumor heterogeneity [12] [13]. Studies have demonstrated high concordance between IHC and ISH for certain markers, with one investigation reporting 91.3% agreement (κ-coefficient: 0.848) between TTF-1 protein detection by IHC and TTF-1 mRNA detection by ISH in non-small cell lung carcinoma [13].
Experimental Design for IHC-ISH Co-localization
Designing effective IHC-ISH co-localization studies requires careful consideration of several experimental parameters. Researchers must determine whether to perform the techniques sequentially on the same section or on serial sections, with each approach offering distinct advantages [12]. Sequential staining on the same section preserves perfect spatial registration but requires optimization to prevent interference between detection systems, while serial sections maintain protocol integrity but introduce registration challenges during analysis [12]. The order of staining represents another critical consideration, with ISH typically performed before IHC when detecting RNA targets to prevent degradation, while DNA targets may be more stable to subsequent IHC processing [12]. Control experiments are essential to validate specificity and prevent false positives, including omission of primary antibody or probe, use of sense or scrambled probes for ISH, and validation with known positive and negative samples [12] [13]. For detection method selection, chromogenic IHC paired with chromogenic ISH allows simultaneous brightfield visualization but limits multiplexing capacity, while fluorescent detection of both enables higher multiplexing but may complicate morphological assessment [8]. Hybrid approaches using chromogenic for one method and fluorescent for the other can provide balanced solutions for specific research questions [8].
Advanced Applications and Recent Developments
Recent technological advances have significantly expanded the capabilities of IHC-ISH co-localization studies, particularly through multiplexing approaches and computational integration. Modern multiplex immunofluorescence (mIF) panels now enable simultaneous detection of 5-10 protein markers alongside RNA or DNA targets, providing unprecedented resolution of cellular phenotypes and functional states within tissue architecture [14]. These advanced applications have been facilitated by improvements in probe design, signal amplification systems, and imaging technologies including spectral imaging and confocal microscopy [8] [14]. Computational approaches for image analysis have similarly evolved, with co-registration algorithms enabling precise alignment of IHC and ISH images at the single-cell level, as demonstrated in recent studies where the average cell-cell distance between H&E and mIF images was 3.1 microns, below the average nucleus size of 7.6 microns [14]. The integration of artificial intelligence and machine learning further enhances these applications, with deep learning models now capable of classifying cell types on H&E images with 86%-89% overall accuracy when trained using mIF-defined cell types as ground truth [14]. These developments open new possibilities for spatial biomarker discovery and comprehensive tissue analysis in both research and clinical contexts.
Essential Reagents and Research Solutions
Successful IHC experiments require careful selection of reagents and research solutions optimized for specific applications. The table below outlines key components of the IHC toolkit with their respective functions and selection considerations:
Table 3: Essential Research Reagents for IHC Experiments
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Fixatives | Formalin, Paraformaldehyde (PFA), Ethanol, Methanol | Preserve tissue architecture and antigen integrity; formaldehyde-based fixatives most common for cross-linking |
| Antigen Retrieval Reagents | Citrate buffer (pH 6.0), EDTA/TRIS-EDTA (pH 8.0-9.0) | Reverse formaldehyde cross-linking; pH and buffer choice depend on target antigen |
| Blocking Reagents | Normal serum, BSA, Commercial protein blocks | Reduce non-specific antibody binding; should match host species of secondary antibody |
| Primary Antibodies | Monoclonal vs. polyclonal; concentrate vs. ready-to-use (RTU) | Recognize specific target antigens; require validation for IHC applications |
| Detection Systems | HRP-based, AP-based, polymer systems, avidin-biotin | Signal amplification and visualization; polymer systems offer enhanced sensitivity |
| Chromogenic Substrates | DAB (brown), Vector Red, Vector Blue, BCIP/NBT (blue) | Enzyme substrates producing insoluble colored precipitates |
| Fluorophores | Alexa Fluor series, FITC, TRITC, Cy dyes | Fluorescent labels for detection; selection based on microscope filter availability |
| Counterstains | Hematoxylin, DAPI, Methyl Green | Provide morphological context; nuclear staining for orientation |
| Mounting Media | Aqueous (fluorescence), Permanent (chromogenic) | Preserve staining and enable visualization |
When selecting antibodies for IHC, researchers must consider whether the antibody has been validated for IHC applications, its specificity for the target epitope, and the host species, particularly for multiplexing experiments where primary antibodies from different species are required to prevent cross-reactivity [9]. The format of antibodies—concentrated versus ready-to-use (RTU)—represents another consideration, with concentrates offering flexibility and lower initial costs but requiring validation of working dilutions, while RTU formats provide consistency and save preparation time [10]. For detection systems, polymer-based technologies generally offer enhanced sensitivity compared to traditional avidin-biotin systems, with multiple enzyme molecules conjugated to antibody-binding polymers providing significant signal amplification [10]. Recent advances in reagent development include increased sensitivity substrates allowing higher primary antibody dilutions, expanded color options for multiplexing, and improved fluorophores with brighter signals and enhanced photostability [11].
Troubleshooting and Quality Control
Common IHC Challenges and Solutions
Even with optimized protocols, IHC experiments can present various challenges that require systematic troubleshooting. Common issues include non-specific background staining, weak or absent specific signal, high background fluorescence, and poor tissue morphology [7] [10]. Non-specific background staining often results from inadequate blocking, improper antibody concentrations, or incomplete washing, and can be addressed by optimizing blocking conditions, titrating antibodies, and ensuring thorough washing between steps [10]. Weak specific signal may indicate insufficient antigen retrieval, primary antibody concentration too low, or detection system limitations, potentially resolved by optimizing retrieval conditions, increasing primary antibody concentration, or switching to more sensitive detection systems [10]. For fluorescent detection, high background can stem from tissue autofluorescence, which can be reduced using autofluorescence quenching reagents, or from overamplification, addressed by reducing antibody concentrations or detection incubation times [8]. Proper controls are essential for effective troubleshooting, including positive control tissues known to express the target antigen, negative controls omitting the primary antibody, and internal positive controls within the test tissue when available [7] [10].
Quality Assurance in IHC
Implementing robust quality control measures is essential for generating reliable, reproducible IHC data, particularly in research settings and especially when integrating IHC with ISH for co-localization studies [7]. Quality assurance begins with proper tissue handling and fixation, using standardized fixation conditions (fixative type, pH, temperature, duration) to minimize variability [10]. Validation of each primary antibody for its intended application represents another critical component, following established guidelines for antibody validation including demonstration of specificity through appropriate controls [9]. Routine monitoring of equipment performance, including microscopes, stainers, and water baths, ensures consistent results [10]. For quantitative or semi-quantitative IHC, implementation of standardized scoring systems helps minimize inter-observer variability, with digital pathology approaches and artificial intelligence algorithms increasingly used to provide more objective assessment [7] [15] [14]. Documentation of all protocol details and quality control results enables traceability and facilitates troubleshooting when issues arise [10]. For IHC-ISH co-localization studies, additional quality measures include validation of co-registration accuracy and controls for potential interference between the two techniques [13] [14].
Future Perspectives in IHC Technology
The field of IHC continues to evolve with emerging technologies and methodologies enhancing its capabilities for research and clinical applications. Several key trends are shaping the future of IHC and its integration with spatial biology approaches. Digital pathology and artificial intelligence represent perhaps the most transformative development, with whole-slide imaging enabling automated analysis and AI algorithms providing objective, quantitative assessment of staining patterns [7] [15]. These technologies facilitate high-throughput analysis and discovery of novel morphological patterns beyond human perception, with studies demonstrating AI models capable of classifying cell types on H&E images with 86%-89% accuracy when trained using multiplex immunofluorescence as ground truth [14]. Multiplexing capabilities continue to expand, with new methodologies enabling simultaneous detection of numerous protein markers alongside DNA and RNA targets, providing comprehensive molecular profiling within tissue architecture [8] [14]. These advances include cyclic immunofluorescence approaches that overcome spectral limitations through sequential staining and imaging, potentially enabling dozens of targets to be visualized on the same section [14]. Integration with other omics technologies represents another frontier, with spatial transcriptomics and proteomics approaches complementing IHC data to provide comprehensive understanding of tissue organization and function [14]. Finally, standardization and automation continue to improve reproducibility, with automated stainers, standardized reagents, and quantitative analysis pipelines increasing consistency across experiments and laboratories [7] [10]. These developments collectively promise to enhance the precision, throughput, and informational yield of IHC and its applications in co-localization studies with ISH.
In situ hybridization (ISH) is a foundational technique in molecular biology that enables the precise localization of specific nucleic acid sequences within fixed tissues and cells, providing crucial temporal and spatial information about gene expression and genetic loci [16]. As life science research increasingly focuses on spatial context, ISH has become indispensable for visualizing the distribution of genes or transcripts directly in their native morphological environment [17]. This capability is particularly valuable in co-localization studies with immunohistochemistry (IHC), where researchers can correlate nucleic acid localization with protein expression patterns within the same sample [18]. The technique's power lies in its ability to bypass the need for nucleic acid extraction and purification, instead preserving the architectural context of the tissue while obtaining specific localization data [16]. As technology advances, ISH continues to evolve with improvements in precision, speed, and adaptability, making it an increasingly powerful tool for researchers and clinicians investigating gene expression patterns, disease mechanisms, and therapeutic development [17].
Core ISH Methodologies: A Technical Comparison
The fundamental principle of ISH involves using a labeled, target-specific nucleic acid probe that hybridizes with complementary sequences within a biological sample [16]. While this core concept remains consistent across methodologies, implementation varies significantly based on detection method and application requirements. Modern ISH platforms primarily utilize two detection approaches: fluorescence (FISH) and chromogenic (CISH), each with distinct advantages and ideal applications [16].
Table 1: Comparison of Core ISH Methodologies
| Technique | Instrument/Visualization Method | Primary Advantage | Primary Application |
|---|---|---|---|
| CISH | Bright-field microscopy | Ability to view signal and tissue morphology simultaneously | Molecular pathology diagnostics |
| DNA-FISH | Fluorescence microscopy | Multiplexible: visualize multiple targets in the same sample | Gene presence, copy number, and location; mutation analysis |
| RNA-FISH | Fluorescence microscopy, HCS, and flow cytometry | Multiplexible: visualize multiple targets in the same sample | Gene expression, RNA temporal and spatial localization |
Fluorescence in situ hybridization (FISH) enables researchers to assay multiple targets simultaneously and visualize co-localization within a single specimen [16]. Using spectrally distinct fluorophore labels for each hybridization probe, this approach provides the power to resolve several genetic elements or multiple gene expression patterns in a single specimen with multicolor visual display [16]. RNA-FISH using branched DNA signal amplification, such as in Invitrogen ViewRNA and PrimeFlow assays, represents a particularly advanced implementation that employs specialized signal amplification for detection, resulting in greater specificity, lower background, and higher signal-to-noise ratios [16].
Chromogenic ISH (CISH), in contrast, utilizes enzyme-based detection methods that produce a permanent, precipitating colorimetric signal visible under standard bright-field microscopy [16]. This characteristic makes CISH especially valuable for diagnostic pathology applications where simultaneous assessment of tissue morphology and genetic alterations is required, and where archival tissue samples may need to be stored long-term without signal degradation [16].
The Complete ISH Workflow: From Probe Design to Detection
Probe Design and Selection
Selecting the appropriate probe is a critical factor determining ISH experimental success [5]. RNA probes, particularly antisense RNA probes, have become a preferred approach due to their high sensitivity and specificity for target RNA sequences [5]. These probes are commonly generated by in vitro transcription from a DNA template and designed to hybridize specifically to target RNA sequences within tissue samples [5]. Optimal RNA probes should be 250–1,500 bases in length, with probes of approximately 800 bases long typically exhibiting the highest sensitivity and specificity [5]. For DNA probes, which provide high sensitivity but don't hybridize as strongly to target mRNA molecules compared to RNA probes, formaldehyde should be avoided in post-hybridization washes [5].
Probe specificity is paramount for successful ISH experiments [5]. If the exact nucleotide sequence of the target mRNA or DNA is known, a precise complementary probe can be designed. However, if more than 5% of base pairs are not complementary, the probe will only loosely hybridize to the target sequence, making it more likely to be washed away during processing and potentially not correctly detected [5]. Transcription templates should allow for transcription of both probe (antisense strand) and negative control (sense strand) RNAs, typically achieved by cloning into a vector with opposable promoters [5].
Figure 1: Core ISH Experimental Workflow. The process begins with sample preparation and probe design, proceeds through hybridization and washing steps, and culminates in signal detection and analysis.
Sample Preparation and Storage
Proper storage of tissue samples is critical for preserving nucleic acid integrity and ensuring reliable ISH results [5]. To prevent RNA degradation, tissue samples must be handled with care and stored under conditions that inhibit RNase activity [5]. Common approaches include flash-freeting samples in liquid nitrogen immediately after collection or fixing them in formalin followed by paraffin embedding (FFPE) [5]. FFPE tissues are particularly valuable for ISH as they can be stored for long periods without significant loss of RNA integrity [5]. For slide storage, best practices recommend against storing slides dry at room temperature; instead, storage in 100% ethanol at -20°C, or in a plastic box covered in saran wrap at -20°C or -80°C preserves slides for several years [5].
The preparation and sectioning of tissue samples are essential steps in the ISH protocol [5]. Proper fixation using agents such as paraformaldehyde or formalin preserves tissue structure and nucleic acid integrity, making targets accessible for probe hybridization [5]. After fixation, tissues are typically embedded in paraffin to facilitate thin sectioning with a microtome, producing tissue sections that can be mounted on slides for ISH analysis [5]. A critical consideration throughout sample preparation is preventing RNase contamination, as this enzyme quickly destroys RNA in cells or the RNA probe itself [5]. Users must employ sterile techniques, gloves, and RNase-free solutions to prevent contamination [5].
Hybridization and Stringency Washes
The hybridization process represents the core of the ISH technique, where the probe anneals to its complementary target sequence within the tissue [5]. For paraffin-embedded sections, slides must first be deparaffinized and rehydrated through a series of washes including xylene, ethanol gradients, and finally cold tap water [5]. From this point onward, slides cannot dry as this will cause non-specific antibody binding and high background staining [5].
Antigen retrieval is typically performed by digesting with proteinase K (e.g., 20 µg/mL in pre-warmed 50 mM Tris for 10–20 minutes at 37°C) [5]. Incubation time and proteinase K concentration require optimization for different tissue types, fixation lengths, and tissue sizes [5]. Insufficient digestion reduces hybridization signal, while over-digestion results in poor tissue morphology, making localization of hybridization signal difficult [5].
Hybridization itself involves applying a hybridization solution containing the probe to the tissue section and incubating in a humidified chamber at optimized temperatures (typically between 55–65°C) [5]. During this step, the probe hybridizes to its corresponding target mRNA or cellular DNA [5]. The optimal hybridization temperature depends on the probe sequence and tissue type, and should be optimized for each experimental system [5].
Table 2: Hybridization Solution Components
| Reagent | Final Concentration | Volume per mL of Solution |
|---|---|---|
| Formamide | 50% | 500 µL |
| Salts | 5x | 250 µL |
| Denhardt's solution | 5x | 50 µL |
| Dextran sulfate | 10% | 100 µL |
| Heparin | 20 U/mL | 10 µL |
| SDS | 0.1% | 1 µL |
Signal Detection and Imaging
Following hybridization, stringency washes remove non-specifically bound probes to enhance signal-to-noise ratio [5]. Solution parameters such as temperature, salt concentration, and detergent concentration can be manipulated to remove non-specific interactions while preserving specific hybridization [5]. Wash stringency should be optimized based on probe characteristics: for very short probes (0.5–3 kb) or complex probes, washing temperature should be lower (up to 45°C) with lower stringency (1–2x SSC), while for single-locus or large probes, temperature should be around 65°C with high stringency (below 0.5x SSC) [5].
For chromogenic detection systems using digoxigenin-labeled probes, slides are typically blocked with appropriate buffer (e.g., MABT + 2% BSA, milk, or serum) for 1–2 hours at room temperature before applying anti-digoxigenin antibody conjugated to alkaline phosphatase or horseradish peroxidase [5]. After antibody incubation and washing, colorimetric substrates are added to generate precipitating signals at the site of probe hybridization [5].
Fluorescence detection involves similar principles but uses fluorophore-conjugated antibodies or directly labeled probes, followed by visualization with fluorescence microscopy equipped with appropriate filter sets [16]. Multiplexed FISH experiments require careful selection of spectrally distinct fluorophores and specialized imaging systems capable of distinguishing between multiple fluorescence signals [16].
Advanced ISH Technologies and Performance Comparison
Recent technological advances have significantly enhanced ISH capabilities, particularly through automation, multiplexing, and improved detection efficiency [17]. By 2025, adoption of ISH is expected to accelerate, driven by technological innovations like multiplexing and automation that enable simultaneous detection of multiple targets, reducing analysis time and increasing data richness [17].
The Xenium In Situ platform, commercialized by 10x Genomics, represents a cutting-edge spatial transcriptomics technology capable of mapping hundreds of genes in situ at subcellular resolution [19]. Independent evaluations of this platform demonstrate its high detection efficiency, which matches that of established ISH-based technologies like MERSCOPE and Molecular Cartography [19]. For Xenium, detection efficiency was found to be between 1.2 and 1.5 times higher than that of scRNA-seq (Chromium v2), depending on the metric and region analyzed [19]. When compared to sequencing-based spatial methods like Visium, Xenium was significantly more sensitive at the tissue level, detecting a median of 12.8 times more reads for the same anatomical region [19].
Figure 2: Evolution of ISH Multiplexing Capabilities. ISH technologies have progressed from single-plex detection to highly multiplexed systems capable of simultaneously visualizing hundreds of targets.
Specificity is another crucial performance parameter for evaluating ISH technologies [19]. Negative co-expression purity (NCP) quantifies the percentage of non-co-expressed genes in reference single-cell datasets that do not appear to be co-expressed in SRT datasets [19]. Most modern SRT technologies present high specificity (NCP > 0.8), with Xenium showing slightly lower specificity than some other commercial platforms but consistently higher than CosMx, which presented the lowest values [19].
Advanced ISH platforms also provide three-dimensional and subcellular resolution [19]. Xenium's 3D coordinates enable detection of potential mixed-source signals from cells overlapping strongly in the z-dimension, found in approximately 1.8% of total cells [19]. Segmentation-free analysis approaches can identify subcellular mRNA clusters classified as nuclear, cytoplasmic, or extracellular, revealing subtle yet distinct expression variations between nuclear and cytoplasmic clusters linked to the same cell population [19].
Research Reagent Solutions for ISH Experiments
Table 3: Essential Research Reagents for ISH Workflows
| Reagent/Category | Function | Examples/Notes |
|---|---|---|
| Probe Synthesis | Generate labeled nucleic acid probes for target detection | RNA probes (250-1500 bases), DIG-labeled probes, fluorescent probes [5] |
| Tissue Preservation | Maintain nucleic acid integrity and tissue morphology | Formalin, paraformaldehyde, FFPE protocols, flash-freezing [5] |
| Hybridization Buffers | Create optimal conditions for specific probe-target annealing | Formamide, salts (SSC), Denhardt's solution, dextran sulfate [5] |
| Detection Systems | Visualize hybridized probes | Anti-DIG antibodies, fluorophore conjugates, enzyme substrates [5] |
| Stringency Wash Solutions | Remove non-specifically bound probes | SSC buffers with varying concentrations, temperature control [5] |
| Mounting Media | Preserve samples for microscopy | Aqueous mounting for fluorescence, permanent mounting for brightfield [16] |
Integration with IHC and Multiomic Approaches
The combination of ISH with immunohistochemistry (IHC) creates a powerful multiomic approach for correlating nucleic acid localization with protein expression within the same tissue section [18] [20]. This integration is particularly valuable for studying complex biological processes where spatial relationships between different molecular types provide critical insights [20]. For example, in Alzheimer's disease research, a multiomic approach integrating IHC with mass spectrometry imaging has been used to decipher three-dimensional biomolecular distribution, revealing co-localization patterns between pathological protein aggregates and region-specific lipid dysregulation [20].
In inflammation research, multiplex IHC (MP-IHC) enables quantification of immune cells to assess tissue inflammation [18]. Colocalization analysis in these experiments defines colocalized cells as those co-stained for nuclear markers (e.g., DAPI) and specific immune cell markers (e.g., CD4, CD8, CD20, CD68) [18]. Advanced computational methods like object-based colocalization analysis (OBCA) have been developed to improve accuracy and efficiency in quantifying these colocalized immune cells in tissue sections [18]. Both semi-automated and automated OBCA techniques demonstrate sufficient reliability across diverse cell morphologies and significantly reduce analysis time compared to manual counting, making them particularly valuable as sample sizes increase [18].
When designing integrated ISH-IHC experiments, careful consideration must be given to protocol optimization to preserve both nucleic acid integrity and antigenicity [18] [20]. Experimental conditions must be balanced to avoid compromising either detection method, often requiring validation of antibody compatibility with ISH hybridization conditions and potential adjustments to fixation, permeabilization, or retrieval steps [18].
In situ hybridization remains a cornerstone technique for spatial molecular analysis, with continuous technological advancements expanding its applications and capabilities [17]. The ongoing development of more sensitive, multiplexed, and automated ISH platforms will further establish its role in both basic research and clinical diagnostics [17] [19]. As these technologies evolve, they are likely to become more accessible and integrated into routine workflows, supporting advances in precision medicine and personalized therapies [17].
The current trajectory of ISH innovation focuses on several key areas: enhanced multiplexing capacity through improved probe design and detection chemistries, computational methods for data analysis and image processing, integration with complementary spatial omics technologies, and miniaturization/automation for higher throughput and reproducibility [17] [19]. These developments will continue to push the boundaries of what can be visualized and quantified within intact tissues and cells, providing researchers with increasingly powerful tools to understand spatial gene expression patterns in health and disease [17].
Why Integrate IHC and ISH? Advantages over Western Blot and ELISA for Spatial Multiomics
In the quest to understand complex biological systems, traditional analytical techniques like Western blot and ELISA have provided invaluable, but incomplete, molecular pictures. These conventional methods require tissue homogenization, which irrevocably destroys the spatial context of molecular events—information that is particularly critical in architecturally complex tissues like the brain or tumor microenvironments [21]. The integration of Immunohistochemistry (IHC) and In Situ Hybridization (ISH) represents a paradigm shift, enabling researchers to perform spatial multiomics by visualizing both protein and RNA targets within their native tissue architecture. This co-localization approach preserves the crucial "where" that is lost in bulk analysis techniques, offering unprecedented insights into cellular function, heterogeneity, and intercellular communication [21] [22]. This guide objectively compares this integrated spatial approach against established biochemical methods, providing the experimental data and protocols essential for researchers and drug development professionals to advance their investigative capabilities.
Fundamental Differences: Spatial Techniques vs. Bulk Assays
Core Principles and Outputs
IHC uses antibody-epitope interactions to detect and localize proteins directly in tissue sections, providing visual data on protein distribution, abundance, and subcellular localization in a semi-quantitative manner [6]. Similarly, ISH employs nucleic acid probes that hybridize to specific DNA or RNA sequences, allowing precise microscopic localization of genetic material within preserved cells and tissues [12]. Both techniques maintain the structural integrity of samples.
In contrast, Western blot separates denatured proteins by molecular weight via gel electrophoresis before detection with specific antibodies, providing information on protein size and relative abundance in a homogenized sample [23]. ELISA (Enzyme-Linked Immunosorbent Assay) detects and quantifies soluble antigens or antibodies in complex mixtures using antigen-antibody binding in microplate wells, offering high sensitivity for quantification but no spatial information [23].
The table below summarizes the key characteristics of these techniques:
| Feature | IHC | ISH | Western Blot | ELISA |
|---|---|---|---|---|
| Target | Proteins (antigens) | RNA/DNA (nucleic acids) | Proteins | Proteins, antibodies, hormones |
| Spatial Context | Preserved (cellular/subcellular) | Preserved (cellular/subcellular) | Lost | Lost |
| Sample Processing | Fixed tissue sections [6] | Fixed cells/tissue preparations [12] | Lysed and denatured cells [23] | Lysed cells or biological fluids [23] |
| Protein State | In situ, fixed [6] | N/A | Denatured [23] | Native, unfixed [23] |
| Multiplexing Capability | Moderate (typically up to 4 targets) [6] | Moderate (e.g., 4-plex with ViewRNA) [21] | Low (fluorescent multiplexing possible) | Low (typically single-plex) [6] |
| Throughput | Medium | Medium | Low | High [23] |
| Key Output | Protein localization & semi-quantification | Nucleic acid localization & expression | Protein size & relative abundance | Absolute protein quantification [23] |
Comparative Advantages of IHC-ISH Integration for Spatial Multiomics
Preservation of Spatial Architecture
The most significant advantage of integrating IHC and ISH is the ability to correlate gene expression data (via ISH) with protein localization data (via IHC) within the exact same tissue section. This reveals cell-to-cell heterogeneity and intricate molecular relationships within functional tissue units, such as neuronal circuits or tumor nests, which are completely obliterated in Western blot and ELISA workflows [21] [22]. For instance, a brain mapping study successfully preserved both GFAP (protein) and Gad2 (mRNA) signals in hippocampal regions, revealing intricate neuronal patterns that would be impossible to reconstruct from bulk analyses [21].
Comprehensive Molecular Profiling
Combining IHC and ISH moves beyond single-modality analysis to true spatial multiomics. While Western blot and ELISA provide data on proteins only, integrated IHC-ISH can answer simultaneous questions: Is the mRNA transcript present in a cell (ISH)? Is the corresponding protein also present and where is it localized (IHC)? Are there discrepancies that suggest post-transcriptional regulation? This is invaluable for understanding disease mechanisms and therapeutic responses [21] [24].
Enhanced Validation in Translational Research
IHC and ISH serve as complementary validation tools in spatial biology. In HER-2 breast cancer testing, a combination of IHC for protein overexpression and FISH (a form of ISH) for gene amplification is standard clinical practice. Studies show high concordance rates (84.72% overall, with 100% for IHC 0/1+ and 83.33% for IHC 3+ groups), validating the necessity of both techniques for accurate patient stratification [25]. This cross-validation is more direct and spatially informed than using ELISA to screen and Western blot to confirm, which lacks topological context.
Direct Visualization in Diagnostic Pathology
For diagnostic applications, IHC and ISH provide visually interpretable results within the histopathological context that pathologists are trained to evaluate. The stained slides can be directly correlated with tissue morphology, enabling precise diagnosis and prognosis [12]. Western blot and ELISA, while quantitative, generate data (bands or absorbance values) divorced from tissue structure, requiring inference about cellular origin.
The following diagram illustrates the conceptual relationship between these techniques in the context of spatial information and molecular profiling depth:
Performance and Concordance Data
Empirical studies consistently demonstrate correlations and discrepancies between these methods, underscoring the need for technique selection based on specific research questions.
| Comparison | Key Finding | Implication for Spatial Biology |
|---|---|---|
| Western Blot vs. IHC (p185neu in breast cancer) [26] | 83.1% concordance when considering intermediate and high expressors as positive; rose to 89.1% when only high expressors were considered positive. | IHC provides critical spatial distribution data that Western blot cannot, but semi-quantitative IHC scoring may not capture the full dynamic range of protein abundance. |
| ELISA vs. IHC (p185neu in breast cancer) [26] | 78.9% concordance for combined positive groups; rose to 93.3% when only high expressors were considered positive. | ELISA's quantitative strength is clear, but it fails to identify rare positive cells or heterogeneous expression patterns within a tissue sample. |
| IHC vs. FISH (HER-2 in breast cancer) [25] | 84.72% total concordance; 100% for IHC 0/1+, 18.18% for IHC 2+, and 83.33% for IHC 3+. | Highlights the clinical necessity of combining protein (IHC) and gene (FISH) analysis, especially for equivocal IHC 2+ cases, to guide targeted therapy. |
Technical Protocols for IHC and ISH Integration
Successfully integrating IHC and ISH in the same tissue section requires overcoming significant technical challenges, as optimal conditions for each technique often conflict [21].
Critical Protocol Modifications
The standard protocol conflict is a key hurdle: protease treatments essential for ISH can destroy antibody epitopes for IHC, and RNases introduced during IHC can degrade RNA targets [21]. The following workflow outlines the modified protocol to overcome these challenges:
1. Tissue Preparation: Both formalin-fixed paraffin-embedded (FFPE) and cryopreserved tissues can be used. FFPE samples offer lower RNase activity, while cryopreserved tissues typically provide higher RNA integrity [21].
2. RNase Inhibition: Before IHC labeling, tissues must be pretreated with robust RNase inhibitors (e.g., RNaseOUT) to protect RNA integrity during subsequent antibody incubations [21].
3. Antibody Crosslinking: Following IHC labeling but prior to ISH steps, antibodies must be crosslinked to the tissue using a suitable crosslinker. Standard formaldehyde fixation is insufficient to withstand the harsh protease treatments required for ISH protocols [21].
Detection and Imaging
- RNA Detection: Branched DNA (bDNA) ISH probes (e.g., ViewRNA) enable highly sensitive detection, often at the single-molecule level, preserving spatial context. Fluorescence kits allow simultaneous visualization of up to four RNA targets [21].
- Protein Detection: Directly labeled antibodies or antibodies labeled in-house with kits (e.g., ReadyLabel) provide spectral flexibility. Careful panel design is crucial to minimize spectral overlap and autofluorescence [21].
- Imaging Platforms: Versatile systems ranging from widefield microscopes to specialized spectral imaging instruments (e.g., EVOS S1000) capable of resolving up to nine fluorophores simultaneously are employed. Mounting media (e.g., ProLong RapidSet) prevent photobleaching and ensure signal stability [21].
Essential Research Reagent Solutions
The table below catalogs key reagents and instruments critical for successful implementation of integrated IHC-ISH spatial multiomics studies.
| Reagent/Instrument | Function | Specific Example |
|---|---|---|
| RNase Inhibitor | Protects RNA targets from degradation during IHC steps. | RNaseOUT recombinant ribonuclease inhibitor [21] |
| ISH Detection Kit | Enables sensitive, multiplexed RNA detection via bDNA signal amplification. | ViewRNA Tissue Assay Kits (fluorescence or colorimetric) [21] |
| Antibody Labeling Kit | Allows flexible conjugation of fluorophores to antibodies for multiplex IHC. | ReadyLabel Antibody Labeling Kits [21] |
| Spectral Imaging System | Simultaneously resolves multiple fluorescence signals for high-plex analysis. | EVOS S1000 Spatial Imaging System [21] |
| Automated IHC Stainer | Provides standardized, high-throughput processing for complex workflows. | ONCORE Pro X Automated IHC Stainer [27] |
| Mounting Medium | Preserves fluorescence and colorimetric signals for long-term archiving. | ProLong RapidSet Mountant [21] |
The integration of IHC and ISH establishes a powerful framework for spatial multiomics, offering a transformative advantage over traditional bulk analysis techniques like Western blot and ELISA. While Western blot and ELISA remain valuable for specific applications requiring high-throughput quantification or protein size characterization, their fundamental limitation is the loss of all spatial information. The IHC-ISH synergy directly addresses this by enabling the co-localization of multiple molecular types within an intact tissue architecture. This capability is proving indispensable for unraveling cellular heterogeneity, understanding the complex biology of the tumor microenvironment, mapping neural circuits, and advancing translational research and diagnostic precision. As the field of spatial biology continues to evolve, the combined use of IHC and ISH will undoubtedly remain a cornerstone technique for comprehensively understanding the spatial organization of biological systems.
Immunohistochemistry (IHC) and In Situ Hybridization (ISH) represent cornerstone techniques in modern investigative pathology, enabling the precise visualization of biomolecules within their native tissue context. IHC uses antibody-epitope interactions to selectively label and visualize proteins in tissue samples, providing data on protein distribution, subcellular localization, and abundance in a semi-quantitative manner [6]. ISH, conversely, detects specific nucleic acid sequences (DNA or RNA) within preserved tissue sections, allowing researchers to visualize gene expression, gene amplification, and chromosomal alterations [28] [29]. The power of these techniques is magnified when they are combined in co-localization studies, which enable researchers to correlate genomic alterations with their functional protein products within the same cellular or tissue compartment. This integrated approach is indispensable for biomarker validation, therapeutic development, and elucidating complex molecular mechanisms in disease pathogenesis, ultimately fueling the advancement of precision medicine [30].
Technical Comparison of Core Methodologies
Immunohistochemistry (IHC): Principles and Detection Systems
The fundamental IHC workflow involves preparing tissue sections (typically formalin-fixed paraffin-embedded, or FFPE), performing antigen retrieval to unmask epitopes, incubating with a primary antibody specific to the target protein, and then detecting the bound antibody using a visualization system [6] [31]. The choice of detection system significantly impacts the sensitivity, specificity, and multiplexing capability of an IHC assay.
Table 1: Comparison of Common IHC Detection Methods
| Detection Method | Principle | Key Advantage | Key Limitation |
|---|---|---|---|
| Direct Method [31] | Primary antibody directly conjugated to an enzyme (e.g., HRP) or fluorophore. | Simple, rapid protocol; minimal non-specific binding. | Low sensitivity; not practical to conjugate every primary antibody. |
| Indirect Method (Secondary Antibody) [31] | Unconjugated primary antibody is detected by an enzyme- or fluorophore-conjugated secondary antibody. | Enhanced sensitivity due to signal amplification; versatile as one secondary antibody can be used for many primaries from the same species. | Potential for non-specific binding from secondary antibody. |
| Avidin-Biotin Complex (ABC) [31] | Biotinylated secondary antibody binds a pre-formed complex of Avidin and Biotin-conjugated enzyme (HRP). | High sensitivity due to significant enzyme deposition. | Endogenous biotin in tissues can cause high background. |
| Labeled Streptavidin-Biotin (LSAB) [31] | Biotinylated secondary antibody is detected by enzyme-conjugated Streptavidin. | Reduced non-specific binding compared to ABC due to Streptavidin's neutral charge. | Still susceptible to issues from endogenous biotin. |
| Polymer-Based Method [31] | Secondary antibody and enzyme (HRP/AP) are co-conjugated to a dextran polymer backbone. | High sensitivity; no endogenous biotin interference; faster protocols. | Large polymer size can cause steric hindrance for some epitopes. |
Two enzymes are most commonly used in chromogenic IHC detection: Horseradish Peroxidase (HRP) and Alkaline Phosphatase (AP). HRP, in the presence of hydrogen peroxide, catalyzes the oxidation of substrates like 3,3'-Diaminobenzidine (DAB) to produce a brown, insoluble precipitate [29]. AP reacts with substrates like Fast Red or Fast Blue to yield red or blue colored products, respectively [31]. The choice of enzyme and substrate is critical for single-plex and multiplexing experiments.
In Situ Hybridization (ISH): Principles and Modalities
ISH involves the hybridization of a labeled complementary DNA or RNA probe to a specific nucleic acid sequence within a tissue section. The two primary modalities are:
- Fluorescence ISH (FISH): Uses fluorescently labeled probes for detection under a fluorescence microscope. It is highly quantitative and allows for multiplexing with multiple colored probes [28].
- Chromogenic ISH (CISH): Uses enzyme-conjugated probes (similar to IHC) that are visualized with a chromogenic substrate, producing a permanent stain viewable with a standard brightfield microscope [29].
While FISH is often considered the gold standard for its precision in gene amplification assessment (e.g., HER2 in breast cancer), it is more costly, requires a fluorescent microscope, and the signal can fade over time. CISH, while less quantitative, is more easily integrated into a standard pathology workflow and provides better morphological context [28].
Experimental Design and Protocols for Co-Localization Studies
Workflow for Sequential IHC and ISH Multiplexing
A robust protocol for performing IHC and ISH on a single slide to co-localize protein and nucleic acid targets is outlined below. This workflow is based on established methods from the literature and can be implemented on automated staining platforms like the Roche DISCOVERY ULTRA [29].
Detailed Protocol Steps:
- Tissue Preparation: Cut 4-5 µm sections from FFPE tissue blocks and mount on charged slides. Dry slides thoroughly to prevent tissue detachment.
- Deparaffinization and Rehydration: Bake slides at 60°C for 30-60 minutes. Deparaffinize in xylene (or substitute) and rehydrate through a graded ethanol series to distilled water.
- Antigen Retrieval: Perform heat-induced epitope retrieval (HIER) using an appropriate buffer (e.g., citrate, EDTA, TRIS-EDTA at pH 6.0 or 9.0) in a pressure cooker or decloaking chamber. The specific buffer and conditions must be optimized for the primary antibody [6] [31].
- Protein Blocking: Block endogenous peroxidase activity with 3% Hâ‚‚Oâ‚‚. Block non-specific protein binding sites with an appropriate protein block (e.g., normal serum, casein, or commercial protein blocks) for 10-30 minutes at room temperature.
- Primary Antibody Incubation: Apply optimized dilution of the primary antibody in antibody diluent. Incubate according to validated conditions (typically 30-90 minutes at room temperature or overnight at 4°C).
- Polymer-Based Detection: Use a polymer-based HRP or AP detection system according to the manufacturer's instructions. Incubate with the polymer for 20-30 minutes at room temperature.
- Chromogen Development for IHC: Develop the signal using a chromogen such as DAB (brown) for HRP, or Fast Red (red) for AP. Do not apply a nuclear counterstain at this stage.
- ISH Target Retrieval and Denaturation: Depending on the ISH system, a second round of target retrieval and denaturation may be required. For DNA FISH/CISH, this step is critical to denature the DNA and make it accessible for the probe.
- Probe Hybridization: Apply the labeled nucleic acid probe to the tissue section. Coverslip and seal with rubber cement. Incubate in a pre-heated humidified hybridizer or thermal cycler according to the probe's specifications (often overnight at 37°C-45°C).
- Stringency Washes: The following day, remove the coverslip and perform stringency washes (e.g., in 2x SSC or a proprietary wash buffer at a specific temperature) to remove any unbound or loosely bound probe.
- ISH Signal Detection: If using a chromogenic ISH probe (CISH), detect the signal with an appropriate enzyme-conjugated antibody (e.g., anti-FITC-HRP) and a contrasting chromogen (e.g., Fast Blue or Vector Blue if DAB was used for IHC). For FISH, simply apply a DAPI counterstain and a non-fading mounting medium.
- Counterstain and Coverslip: Apply a light nuclear counterstain (e.g., Hematoxylin) if not already applied during the ISH step. Dehydrate through graded ethanols, clear in xylene, and mount with a permanent mounting medium.
Key Considerations for Experimental Design
- Order of Staining: The sequence of IHC and ISH can be reversed. Performing IHC first is often preferred as the harsh denaturation conditions for ISH (especially for DNA) can destroy many protein epitopes.
- Chromogen Selection: Choose chromogens with distinct, non-overlapping colors and that are stable throughout the entire procedure. Translucent chromogens are ideal for co-localization studies as they allow visualization of overlapping signals [29].
- Controls: Include critical controls for both IHC (positive tissue, negative/isotype control) and ISH (positive tissue, negative control probe, and for FISH, a probe for a centromere or another known non-amplified gene). A control slide with IHC or ISH alone is essential to confirm that the first stain does not interfere with or get altered by the second staining procedure.
Comparative Performance Data in Research and Diagnostics
The application of IHC and ISH, particularly in a co-localization context, provides critical data for biomarker validation and clinical diagnostics. The following table summarizes quantitative performance data from published studies, highlighting the strengths and limitations of each technique and their integrated use.
Table 2: Comparative Performance of IHC, ISH, and Integrated Methods in Biomarker Analysis
| Application / Biomarker | Technique | Key Performance Metric | Result / Finding | Implication for Development |
|---|---|---|---|---|
| HER2 Testing in Breast Cancer [28] | IHC (Manual Scoring) | Semi-quantitative scoring (0 to 3+) | Prone to interobserver variability [28] | Subjectivity can affect treatment decisions. |
| IHC (AI-Assisted Scoring) | Overall Accuracy vs. Pathologist | 91% ± 0.01 [28] | Reduces subjectivity; improves standardization. | |
| FISH | Quantitative (HER2 gene copy number) | Higher precision than IHC [28] | Gold standard for gene amplification; more resource-intensive. | |
| AI predicting FISH from IHC | Specificity | 0.96 ± 0.03 (Internal), 0.93 ± 0.01 (External) [28] | Potential to reduce need for reflex FISH testing. | |
| Predictive Biomarker Identification (e.g., EGFR in NSCLC) [30] | IHC / Molecular (DNA) | Predictive Power (Interaction Test) | P < 0.001 for treatment-biomarker interaction [30] | Requires data from a randomized clinical trial to establish predictive utility. |
| Prognostic Biomarker Identification (e.g., STK11 in NSCLC) [30] | IHC / Molecular | Prognostic Power (Main Effect Test) | Association with poorer overall survival [30] | Can be identified in properly conducted retrospective studies. |
| Multiplexed Co-localization [29] | IHC/ISH Combination | Information Gain | Enables protein co-localization and spatial relationship analysis in single sample [29] | Generates unique data not possible from serial sections. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of IHC and ISH co-localization studies relies on a suite of high-quality reagents and instruments.
Table 3: Essential Reagents and Tools for IHC-ISH Co-localization Studies
| Category | Item | Function / Application | Considerations |
|---|---|---|---|
| Tissue Preparation | Formalin, Paraffin | Standard fixation and embedding for morphology preservation. | Over-fixation can mask epitopes; requires antigen retrieval [6]. |
| Antigen Retrieval Buffers (Citrate, EDTA) | Unmask epitopes cross-linked by formalin fixation. | pH and buffer choice must be optimized for each antibody [31]. | |
| Detection Reagents | Primary Antibodies (Monoclonal, Polyclonal) | Bind specifically to the protein target of interest. | Monoclonals offer specificity; polyclonals can be more sensitive for some fixed targets [31]. |
| Polymer-Based Detection Kits (HRP/AP) | Signal amplification and visualization. | Offer high sensitivity and avoid endogenous biotin issues [31]. | |
| Chromogens (DAB, Fast Red, Fast Blue) | Enzyme substrates that produce colored precipitate at target site. | Choose for contrast, stability, and compatibility with automated stainers [29]. | |
| ISH-Specific Reagents | Labeled DNA/RNA Probes | Hybridize to specific DNA or RNA sequences in situ. | Must be validated for specificity and sensitivity on FFPE tissue. |
| Hybridization Buffer | Creates optimal ionic and pH conditions for probe binding. | Often contains formamide to lower melting temperature. | |
| Stringency Wash Buffer | Removes mismatched or unbound probe to ensure specificity. | Temperature and salt concentration are critical. | |
| Instrumentation | Automated Staining Platform (e.g., DISCOVERY ULTRA [29]) | Standardizes and automates complex staining protocols. | Essential for reproducibility and high-throughput in co-localization assays. |
| Disulfide, bis(3,4-difluorophenyl) | Disulfide, bis(3,4-difluorophenyl), CAS:60811-25-8, MF:C12H6F4S2, MW:290.3 g/mol | Chemical Reagent | Bench Chemicals |
| Ethyl 2-(2,6-dichlorophenyl)acetate | Ethyl 2-(2,6-dichlorophenyl)acetate, CAS:90793-64-9, MF:C10H10Cl2O2, MW:233.09 | Chemical Reagent | Bench Chemicals |
Signaling Pathways and Analytical Validation in Therapeutic Development
The ultimate goal of biomarker validation is to inform therapeutic development. Biomarkers are categorized based on their clinical application, and their validation follows a rigorous statistical and regulatory pathway [30] [32].
Key Analytical and Clinical Validation Steps:
- Analytical Validation: This ensures the test itself is reliable and reproducible. Key metrics include sensitivity (the proportion of true positives correctly identified), specificity (the proportion of true negatives correctly identified), and discrimination, often measured by the Receiver Operating Characteristic (ROC) Area Under the Curve (AUC) [30]. A perfect test has an AUC of 1.0, while 0.5 is no better than a coin flip.
- Clinical Validation: This establishes the clinical utility of the biomarker.
- Prognostic Biomarkers provide information on the overall disease outcome, independent of therapy. They are identified through a main effect test of association between the biomarker and the outcome (e.g., overall survival) in a statistical model [30]. An example is STK11 mutation in NSCLC, associated with poorer outcome [30].
- Predictive Biomarkers inform the likely response to a specific therapeutic agent. They must be identified in secondary analyses of data from a randomized clinical trial, through a statistical interaction test between the treatment and the biomarker [30]. The classic example is EGFR mutation status predicting response to gefitinib vs. carboplatin-paclitaxel in the IPASS study [30].
The successful integration of IHC and ISH in co-localization studies provides a powerful platform for discovering and validating such biomarkers, ultimately accelerating the development of safer and more effective targeted therapies.
Advanced Integrated Workflows: From Automated Platforms to Super-Resolution Techniques
Implementing the RNAscope Protease-Free ISH Assay on Automated Platforms
In the evolving field of spatial biology, the ability to simultaneously visualize RNA and protein biomarkers within their native tissue context has become invaluable for understanding complex molecular mechanisms. In situ hybridization (ISH) and immunohistochemistry (IHC) have long been complementary techniques, yet their integration posed significant technical challenges, primarily due to the protease-dependent steps required for traditional RNAscope assays which could damage sensitive protein epitopes [33]. The introduction of the RNAscope Protease-Free Workflow represents a methodological breakthrough, enabling robust same-section, multiomic co-detection on automated platforms like the Roche DISCOVERY ULTRA [34]. This guide objectively compares this innovative protease-free approach against traditional ISH and IHC methods, providing researchers with the experimental data and protocols needed to implement this advanced technology in their co-localization studies.
Technology Comparison: Protease-Free vs. Traditional Workflows
Key Advantages of the Protease-Free Workflow
The RNAscope protease-free assay fundamentally changes the multiomic detection paradigm by eliminating a key incompatibility between ISH and IHC protocols. Traditional ISH requires protease treatment to permeabilize tissues and allow probe access, but this enzymatic step often damages sensitive protein epitopes, compromising subsequent IHC detection [33]. The protease-free workflow overcomes this limitation through alternative permeabilization methods, preserving both RNA integrity and protein antigenicity.
Table 1: Quantitative Performance Comparison of Protease-Free vs. Standard Workflow
| Performance Metric | Standard Workflow with Protease | Protease-Free Workflow | Experimental Validation |
|---|---|---|---|
| Protease-Sensitive Antigen Detection (e.g., CD20) | Suboptimal or lost signal | Optimal signal comparable to IHC alone | Chromogenic detection on FFPE tissue [34] |
| Protease-Tolerant Antigen Detection (e.g., PD1) | Acceptable signal | Improved signal quality | Fluorescent co-detection with RNA markers [34] |
| Tissue Architecture Preservation | Variable depending on protease digestion | Better preservation of histology | H&E comparison on consecutive sections [34] |
| Workflow Compatibility | Limited for sequential RNA-protein detection | Ideal for simultaneous RNA-protein co-detection | Automated runs on Roche DISCOVERY ULTRA [34] |
Application Scope and Technical Specifications
The protease-free technology expands the range of detectable biomarkers, particularly enabling researchers to investigate previously incompatible target combinations. This has profound implications for immuno-oncology, infectious disease research, and cell and gene therapy development [34].
Table 2: Application-Specific Performance of RNAscope Protease-Free Assay
| Research Application | Target Combination Example | Traditional Workflow Performance | Protease-Free Performance |
|---|---|---|---|
| Immune Cell Profiling | CD4 protein + GZMB RNA | Compromised due to protease-sensitive CD4 | Successful co-detection with preserved epitopes [34] |
| Infectious Agent Interrogation | SARS-CoV-2 RNA + ACE-2 protein | Possible with protease-tolerant proteins only | Enhanced host-pathogen interaction studies [33] |
| Antibody Specificity Validation | CD8 mRNA + CD8 protein | Requires sequential slides or optimization | Same-section orthogonal validation [33] [35] |
| Cell Therapy Tracking | CAR-T RNA + cell marker proteins | Limited by protease sensitivity | Robust tracking of engineered cells in tissues [34] |
Experimental Protocols for Automated Platforms
Roche DISCOVERY ULTRA Workflow Implementation
The RNAscope protease-free assay has been specifically optimized for automated processing on the Roche DISCOVERY ULTRA platform, ensuring reproducibility and throughput for both research and clinical applications. The following protocol outlines the key steps:
Sample Preparation:
- Use freshly-cut tissue sections (less than 2 weeks since sectioning) mounted on histological slides [33].
- Formalin-fixed paraffin-embedded (FFPE) tissues are preferred, though fixed frozen tissues are also compatible [36].
- Establish a working IHC protocol independently before integrating it with ISH to determine optimal antibody concentrations [33].
Automated Protease-Free Protocol:
- Deparaffinization and Dehydration: Standard xylene and ethanol series.
- Protease-Free Pretreatment: Utilize the specialized pretreatment reagents included in the RNAscope LS Multiomic or HiPlex Pro kits [36].
- Target Probe Hybridization: Apply RNAscope target-specific probes (C1-C6 for multiomic assays; T1-T12 for HiPlex) [36].
- Signal Amplification: Employ the proprietary RNAscope amplification system without protease steps.
- Protein Immunodetection: Incubate with primary antibodies against protease-sensitive epitopes (e.g., CD20, CD4) [34].
- Simultaneous Detection: Visualize RNA and protein targets using chromogenic or fluorescent detection methods [37].
Experimental Design for Performance Validation
When implementing the protease-free workflow, proper experimental controls are essential to validate performance. The following methodological approach is recommended:
Positive Controls:
- Include tissues with known expression of both RNA and protein targets.
- For RNA detection: Use housekeeping genes (e.g., PPIB) with catalog-positive control probes [37].
- For protein detection: Utilize tissues with confirmed antigen expression using standard IHC.
Negative Controls:
- Implement negative control probes (e.g., bacterial DapB) to assess background signal [37].
- Include no-antibody controls for protein detection steps.
- Use tissues known to lack the target of interest.
Quantitative Assessment:
- Compare signal-to-noise ratios for both RNA and protein detection.
- Evaluate tissue architecture preservation through histological scoring.
- For multiplex assays, verify minimal channel bleed-through using single-stained controls.
Research Reagent Solutions for Multiomic Studies
Table 3: Essential Research Reagents for RNAscope Protease-Free Workflows
| Reagent Category | Specific Product Examples | Function in Workflow | Compatibility Notes |
|---|---|---|---|
| Protease-Free Kits | RNAscope LS Multiomic Assay [36] | Enables co-detection of up to 6 RNA/protein targets | Roche DISCOVERY ULTRA platform |
| Detection Kits | mRNA DAB Detection Kit (Roche #760-224) [37] | Chromogenic detection for RNA targets | HRP-based system for brown staining |
| mRNA RED Detection Kit (Roche #760-234) [37] | Chromogenic detection for RNA targets | AP-based system for red staining | |
| Probe Systems | RNAscope HiPlex Pro CS Probes [36] | 12-plex RNA detection on COMET platform | Formulated for protease-free workflow |
| RNAscope 2.5 VS Target Probes [37] | Target-specific detection on automated systems | Compatible with VS Universal HRP/AP kits | |
| Control Materials | Species-specific positive control probes [37] | Assay performance validation | Essential for experimental rigor |
| RNAscope Control Slides [37] | System performance monitoring | Optional but recommended |
Application Workflows in Research Contexts
The protease-free technology enables several advanced research applications that were previously challenging or impossible with standard workflows. The diagram below illustrates the decision pathway for implementing these applications in different research contexts:
Discussion and Future Directions
The implementation of RNAscope protease-free ISH assays on automated platforms represents a significant advancement for spatial biology research. By enabling robust detection of both RNA and protein targets on the same tissue section without compromising antigen integrity, this technology provides researchers with a powerful tool for understanding complex biological systems. The experimental data summarized in this guide demonstrates consistent performance improvements for challenging targets like CD20 and CD4, while expanding the possibilities for multiomic investigation.
Future developments in this field will likely focus on increasing multiplexing capabilities beyond the current 12-plex RNA detection, further streamlining automated workflows, and enhancing quantification algorithms for complex co-expression patterns. As the protease-free technology becomes more widely adopted, it will continue to drive discoveries in drug development, biomarker validation, and disease mechanism studies by providing comprehensive molecular profiling within morphological context.
Spatial biology represents a paradigm shift in our understanding of complex biological systems, preserving the crucial molecular context that traditional bulk analysis methods often sacrifice [38]. Rather than homogenizing tissue samples and losing all positional data, spatial biology techniques maintain structural integrity, allowing researchers to visualize and quantify proteins, RNA, and other biomolecules precisely where cells produce and utilize them [38]. This spatial context is particularly critical for neuroscientists studying brain architecture and oncologists investigating tumor microenvironments, as it provides the crucial difference between understanding isolated molecular events and grasping how those events coordinate across complex cellular networks [38] [39].
The integration of immunohistochemistry (IHC) and in situ hybridization (ISH) represents both a tremendous opportunity and a significant technical challenge in the spatial multiomics landscape [38]. While IHC reveals the final protein products of gene expression through antibody-based detection, ISH captures intermediate mRNA transcripts using nucleic acid probes that hybridize to target sequences [38]. Together, these techniques provide complementary insights into gene expression regulation, protein localization, and cellular function within native tissue architecture. This protocol guide systematically compares established and emerging methodologies for seamless IHC/ISH integration, providing researchers with validated experimental workflows, technical considerations, and performance metrics to enable robust spatial multiomics investigations across diverse research applications from basic science to drug development.
Technical Foundations: IHC and ISH Principles
Core Methodological Principles
Immunohistochemistry (IHC) employs antibodies that bind specifically to protein targets (antigens) within tissue sections. These antibodies can be labeled with fluorophores for direct visualization or with enzymes that generate colorimetric signals [38]. After decades of refinement by researchers, IHC offers reliable protein localization through well-validated antibodies and serves as a cornerstone technique for defining cell neighborhoods and tissue architecture in spatial analysis applications [38].
In Situ Hybridization (ISH) utilizes a fundamentally different approach, detecting RNA through complementary probes that hybridize to target sequences [38]. Advanced ISH methods like RNAscope employ pairs of probes that bind in close proximity along the RNA target, creating a structure that serves as the foundation for branched DNA amplification [40]. Successive layers of amplifiers and labeled probes build on this scaffold, producing a strong signal with minimal background and enabling highly sensitive detection often at the single-molecule level while preserving spatial context [38] [40].
Technical Comparison and Complementary Applications
Table 1: Fundamental Differences Between IHC and ISH Techniques
| Parameter | Immunohistochemistry (IHC) | In Situ Hybridization (ISH) |
|---|---|---|
| Primary Target | Proteins (antigens) | RNA transcripts (mRNA, miRNA) |
| Detection Mechanism | Antibody-antigen binding | Nucleic acid probe hybridization |
| Signal Amplification | Enzymatic (HRP/AP) or fluorescent | Branched DNA amplification systems |
| Key Applications | Defining cell neighborhoods, tissue architecture | Revealing active transcriptional states, cell heterogeneity |
| Typical Output | Protein localization and abundance | RNA expression patterns and distribution |
The complementary nature of these techniques enables powerful applications where ISH can identify cells producing a secreted protein or enzyme, while IHC informs where that protein ultimately localizes [40]. Similarly, IHC can identify cell types while ISH characterizes gene expression patterns to deconvolute complex tissue structures [40]. This synergy is particularly valuable for understanding regulation of gene expression in cell and developmental biology, allowing researchers to differentiate between effects mediated at the level of transcription versus protein stability or turnover [40].
Technical Challenges in IHC/ISH Integration
Fundamental Protocol Incompatibilities
Successful integration of IHC with ISH requires confronting a fundamental conflict: optimal conditions for each technique directly oppose each other [38]. IHC antibodies frequently degrade during the protease treatments that ISH requires for target accessibility, while the RNases present during standard IHC protocols destroy RNA targets needed for ISH detection [38]. These competing demands create significant technical hurdles that must be addressed through careful protocol optimization.
Additional challenges include spectral overlap when using fluorescent detection methods, tissue integrity preservation throughout demanding multi-step procedures, and the need for specialized equipment for signal visualization and analysis [38]. Each of these factors must be systematically addressed to achieve reliable, reproducible dual detection of protein and mRNA targets within the same tissue section.
Critical Workflow Modifications
Table 2: Essential Protocol Modifications for Successful IHC/ISH Integration
| Challenge | Solution | Implementation Example |
|---|---|---|
| RNase degradation during IHC | RNase inhibition | Add recombinant ribonuclease inhibitors during antibody incubation steps [38] |
| Antibody degradation during ISH | Antibody crosslinking | Crosslink antibodies to tissue after IHC labeling to protect epitopes [38] |
| Signal sensitivity limitations | Amplification systems | Employ branched DNA (RNAscope) or tyramide signal amplification [38] [40] |
| Spectral overlap in multiplexing | Careful panel design | Use spectrally distinct fluorophores; avoid green channel autofluorescence [38] |
| Preservation of tissue morphology | Optimization of permeabilization | Titrate protease concentration and duration; validate morphology preservation [4] |
Recent studies have identified that tissues need to be pretreated with RNase inhibitors before and during IHC labeling to protect RNA integrity [38]. Following IHC labeling, antibodies require crosslinking to the tissue—standard formaldehyde fixation alone cannot withstand the harsh protease treatments necessary for subsequent ISH protocols [38]. When executed properly, these modifications enable robust dual detection of both protein and mRNA targets in the same tissue section.
Established IHC/ISH Integration Protocols
Sequential Dual IHC/ISH Workflow
The sequential approach to dual IHC/ISH represents one of the most established methodologies, with two primary variations in workflow organization. The integrated co-detection workflow begins with permeabilization followed by primary antibody binding, then proceeds to ISH probe hybridization, signal amplification, secondary antibody application, and final visualization [40]. Alternatively, the sequential dual ISH-IHC method spreads the procedure over three days: beginning with permeabilization and ISH probe hybridization on day one, followed by ISH detection and primary antibody treatment on day two, and concluding with secondary antibody detection and visualization on day three [40].
Researchers highly recommend optimizing individual ISH and IHC protocols separately before combining them, as ISH procedures often lead to protein degradation due to requisite protease treatments [40]. Consequently, dual IHC/ISH typically works most reliably for highly expressed proteins, and requires thorough antibody validation to confirm performance under the modified conditions [40].
RNAscope-Based Multiomic Approaches
RNAscope technology represents a significant advancement in ISH methodology, employing a novel double-Z probe design that enables simultaneous noise suppression and signal amplification to detect even minimal amounts of RNA in individual cells [40] [39]. This approach has been successfully adapted for multiomic applications through several specialized platforms:
The RNAscope Multiomic LS Assay leverages proven RNAscope technology to enable simultaneous detection of up to six total proteins and RNA targets with single-cell resolution on automated platforms like the Leica Biosystems BOND RX system [39]. The RNAscope HiPlex Pro for COMET system combines RNAscope HiPlex Pro with sequential immunofluorescence (seqIF) on COMET with a protease-free, fully automated workflow, enabling same-section RNA and multiplex protein detection with the ability to select any 12 RNAscope targets and up to 24 immunofluorescence targets using standard, non-conjugated primary antibodies [39].
Additionally, protease-free sequential RNA-protein detection workflows leverage the robustness of RNAscope technology by combining in situ hybridization and IHC protocols on the same sample slide using sequential workflows compatible with both manual and automated platforms [39].
Performance Comparison and Validation Data
Concordance Between IHC and ISH Methodologies
Rigorous comparison of IHC and ISH methodologies for biomarker detection reveals generally high concordance between these techniques. A comprehensive study examining thyroid transcription factor-1 (TTF-1) expression in 196 cases of non-small cell lung carcinoma (NSCLC) demonstrated 91.3% overall agreement (179/196 cases) between IHC and mRNA ISH detection methods [13]. Statistical analysis showed near-perfect agreement with a κ-coefficient of 0.848, and McNemar-Bowker test analysis indicated no significant difference between the two methods (P=0.219) [13].
Table 3: Quantitative Comparison of IHC and ISH for TTF-1 Detection in NSCLC
| IHC Result | ISH Negative (-) | ISH Low (+) | ISH High (++) | Total |
|---|---|---|---|---|
| Negative (-) | 109 | 5 | 3 | 117 |
| Low (+) | 2 | 27 | 4 | 33 |
| High (++) | 0 | 3 | 43 | 46 |
| Total | 111 | 35 | 50 | 196 |
Notably, among the 46 cases detected with high TTF-1 protein expression via IHC, 43 showed high expression and 3 showed low expression by mRNA ISH, with no cases being negative when detected by mRNA ISH [13]. Conversely, of the 50 cases detected with high TTF-1 mRNA expression by ISH, 43 showed high expression, 4 showed low expression, and 3 were negative as detected by IHC [13]. These findings demonstrate that while generally concordant, each method provides unique information that may be complementary in specific research or diagnostic contexts.
Application-Specific Performance Metrics
In practical research applications, dual IHC/ISH methodologies have demonstrated significant utility across diverse fields. In cancer research, a study investigating stromal microRNA-204 in oral squamous cell carcinoma successfully combined chromogen-based ISH and IHC to exactly delineate stroma from tumor islands while simultaneously visualizing miR expression [4]. This approach revealed miR-204 stromal expression at the tumor front as an independent prognostic biomarker that predicted both recurrence-free survival (p=0.032) and overall survival (p=0.036) in multivariate Cox regression analysis [4].
In neuroscience applications, optimized protocols have enabled simultaneous visualization of multiple mRNA targets (e.g., Gad2, Ppib, Polr2a, Gapdh) alongside protein markers (e.g., GFAP, HuC/HuD) in mouse brain tissue, revealing intricate neuronal patterns in hippocampal regions with high sensitivity in both cryopreserved and FFPE tissue specimens [38]. The successful preservation of both RNA and protein signals in these multiplex assays demonstrates that ISH and IHC can indeed coexist in the same tissue section when appropriate protocol modifications are implemented [38].
Advanced Spatial Multiomics Integration
Integration with Spatial Transcriptomics Platforms
Recent advances enable even more sophisticated integration of IHC/ISH with cutting-edge spatial transcriptomics technologies. A 2025 protocol details methods for embedding irregular field-of-view annotations and immunohistochemistry data into Xenium spatial transcriptomics datasets at single-cell resolution using open-source tools [41]. This approach utilizes Warpy via FIJI and QuPath for image registration, followed by assignment of IHC fluorescence signals and binary masks of H&E annotations to individual cells based on Xenium cell segmentation boundaries [41].
The core innovation of this workflow is the combination of Warpy, a flexible image registration tool, with Scanpy, a Python framework for single-cell analysis [41]. By merging these platforms, researchers created a new pipeline that allows users to register IHC or H&E images, extract quantitative signals, and integrate this information directly with Xenium single-cell data, supporting context-aware spatial analysis that incorporates experimental insight from histological staining or manual annotations [41].
Automated Staining Platforms
The automation of IHC and ISH staining procedures represents another significant advancement, with the automated stainer market experiencing substantial expansion driven by increasing demand for precision diagnostics in pathology laboratories [42]. These automated systems offer improved throughput, accuracy, and reproducibility of staining processes while reducing manual errors and turnaround time [42].
Artificial intelligence is further transforming the automated IHC and ISH stainer landscape by enhancing accuracy, efficiency, and decision-making capabilities [42]. AI-powered image analysis tools enable more precise interpretation of stained tissue samples, reducing variability caused by human error, while integration of machine learning algorithms with stainer platforms helps optimize staining protocols and predict maintenance needs [42]. Key trends shaping this field include miniaturization and compact design of staining instruments, multiplexing capabilities allowing simultaneous detection of multiple biomarkers on a single slide, and a shift toward fully integrated systems combining staining, imaging, and analysis in one platform [42].
Essential Research Reagents and Tools
Core Reagent Solutions
Table 4: Essential Research Reagents for IHC/ISH Integration
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| RNase Inhibitors | RNaseOUT recombinant ribonuclease inhibitor [38] | Protects RNA integrity during antibody incubation steps |
| Antibody Crosslinkers | Formaldehyde-based crosslinking solutions [38] | Stabilizes antibody-antigen complexes against protease degradation |
| Signal Amplification Systems | ViewRNA ISH kits [38], RNAscope probes [40] | Enhances detection sensitivity through branched DNA amplification |
| Multiplex Detection | Alexa Fluor dyes [38], Opal reagent packs [41] | Enables simultaneous detection of multiple targets |
| Protease Reagents | Proteinase K [4], pepsin | Exposes target epitopes and nucleic acids while preserving morphology |
Instrumentation and Software Platforms
Successful IHC/ISH integration requires appropriate instrumentation for visualization, analysis, and data interpretation. Imaging platforms play a central role in multiplex workflows, as accurate signal detection depends on both sensitivity and spectral resolution [38]. Systems capable of spectral unmixing and multi-channel acquisition allow researchers to visualize numerous RNA and protein targets simultaneously, with flexibility for brightfield or fluorescence readouts depending on assay design [38]. Platforms range from versatile systems like the EVOS M5000 to specialized instruments such as the EVOS S1000 Spatial Imaging System, which can simultaneously resolve nine fluorophores during a single acquisition with integrated spectral unmixing [38].
For computational analysis and integration with spatial transcriptomics data, essential software tools include QuPath and FIJI for image analysis and registration [41], Python environments with Scanpy for single-cell analysis [41], and Warpy extensions for advanced image alignment and multi-modal data integration [41]. These computational tools are increasingly essential for extracting maximum biological insight from complex multiomic datasets.
The seamless integration of IHC and ISH methodologies represents a powerful approach for spatial multiomics investigations, enabling unprecedented insights into the relationship between gene expression and protein localization within native tissue contexts. While technical challenges remain, particularly regarding protocol compatibility and signal preservation, established workflows and emerging technologies are progressively overcoming these limitations.
As the field advances, several trends are likely to shape future developments: increased automation of staining and imaging processes, enhanced multiplexing capabilities through improved signal amplification and spectral separation technologies, more sophisticated computational tools for data integration and analysis, and broader accessibility of these techniques through commercialization and protocol standardization. The continued refinement of IHC/ISH integration methodologies will undoubtedly accelerate discoveries across diverse research domains including neuroscience, cancer biology, developmental biology, and therapeutic development, ultimately advancing our understanding of complex biological systems in health and disease.
DNA vs. RNA Probes, Direct vs. Indirect Detection
In the advancing fields of molecular pathology and genomics, the precision of in situ hybridization (ISH) and immunohistochemistry (IHC) is paramount for co-localization studies. These techniques allow researchers to visualize the spatial relationships between nucleic acids and proteins within the context of intact tissues, providing critical insights into gene expression and protein function. The foundational choices of probe type—DNA or RNA—and detection method—direct or indirect—profoundly impact the sensitivity, specificity, and ultimate validity of experimental data. This guide objectively compares these essential tools, providing researchers and drug development professionals with the data and protocols needed to make informed decisions for their experimental designs.
Fundamental Differences: DNA vs. RNA Probes
DNA and RNA probes, while both used for nucleic acid detection, possess distinct chemical and functional characteristics that dictate their application-specific performance.
Chemical Structure and Stability
The core difference lies in their sugar-phosphate backbones: DNA probes contain deoxyribose, while RNA probes contain ribose with a reactive 2'-hydroxyl group. This makes RNA probes more chemically unstable and susceptible to alkaline hydrolysis compared to their DNA counterparts [43]. Furthermore, DNA utilizes thymine, while RNA utilizes uracil in its base pairing.
Synthesis and Labeling
- DNA Probes: Synthesis is typically achieved through chemical synthesis, polymerase chain reaction (PCR), or nick translation [43] [44]. These methods allow for labeling with fluorescent dyes, radioactive isotopes, chemiluminescence, enzyme labels, and biotin.
- RNA Probes (Riboprobes): These are almost exclusively synthesized by in vitro transcription (IVT) from a DNA template, which allows for the efficient incorporation of labeled nucleotides to generate high-specific-activity probes [43] [44].
Table 1: Core Characteristics of DNA and RNA Probes
| Feature | DNA Probes | RNA Probes |
|---|---|---|
| Chemical Structure | Deoxyribose sugar, Thymine | Ribose sugar, Uracil, 2'-OH group |
| Inherent Stability | High; resistant to hydrolysis | Lower; susceptible to RNase degradation |
| Primary Synthesis Method | Chemical synthesis, PCR, Nick translation | In vitro transcription (IVT) |
| Typical Length | 20 bp to 10 Kb [43] | Variable, defined by transcription template |
| Hybridization Stringency | Good | Superior due to higher thermal stability |
Performance in Hybridization
A critical advantage of RNA probes is their capacity for higher hybridization stringency. RNA-RNA and RNA-DNA hybrids exhibit greater thermal stability than DNA-DNA hybrids, which allows researchers to use more stringent post-hybridization washes. This effectively reduces background noise and enhances the signal-to-noise ratio for superior specificity [43]. However, this requires meticulous handling to prevent RNase contamination.
Detection Methodologies: Direct vs. Indirect
The choice of detection strategy involves a trade-off between simplicity and signal amplification, significantly affecting assay sensitivity and multiplexing capability.
Direct Detection
Direct detection uses a single incubation step where the primary antibody or probe is directly conjugated to a detectable label, such as a fluorophore or enzyme [45] [46].
- Advantages: The workflow is fast and simple. It minimizes the risk of cross-reactivity, making it the preferred method for multiplexing experiments where primary antibodies from the same host species are used [46].
- Disadvantages: The main limitation is lower sensitivity due to the absence of signal amplification. This can be problematic for detecting low-abundance targets. Furthermore, conjugated primary antibodies are often more expensive and offer less flexibility [46].
Indirect Detection
Indirect detection is a two-step or more process. An unlabeled primary antibody or probe binds to the target, and its presence is then revealed by a labeled secondary reagent that recognizes the primary [45] [46]. This secondary reagent can be a secondary antibody or a streptavidin molecule binding to a biotinylated primary.
- Advantages: The key strength is powerful signal amplification. Multiple secondary antibodies, each carrying a label, can bind to a single primary antibody, dramatically enhancing the signal. This makes indirect detection ideal for detecting targets with low expression levels. It is also generally more cost-effective and offers a wider range of labeled reagents [45] [46].
- Disadvantages: The protocol is longer and introduces a greater risk of non-specific background signal due to secondary reagent cross-reactivity, which must be mitigated using cross-adsorbed secondary antibodies [46].
Table 2: Comparison of Direct and Indirect Detection Methods
| Aspect | Direct Detection | Indirect Detection |
|---|---|---|
| Protocol Steps | Single incubation step | Multiple incubation and wash steps |
| Sensitivity | Lower; no signal amplification | Higher; significant signal amplification |
| Multiplexing | Excellent for same-species primaries | More complex; requires host cross-adsorption |
| Cross-Reactivity Risk | Low | Higher; requires cross-adsorbed secondaries |
| Cost & Flexibility | Higher cost per primary; less flexible | Lower cost; highly flexible label options |
| Best For | High-abundance targets, multiplexing | Low-abundance targets, general purpose |
The following workflow outlines the key steps and decision points for selecting and implementing these detection methods in a co-localization study:
Supporting Experimental Data and Protocols
Empirical comparisons and standardized protocols are crucial for validating the choice of probes and detection methods.
Comparative Studies in Literature
A seminal 1999 study compared ISH, direct, and indirect in-situ PCR (IS-PCR) for detecting human papillomavirus (HPV) in cervical biopsies [47]. The study found that while IS-PCR was sensitive, it was technically cumbersome and prone to false positives in its direct form due to primer-independent incorporation of labeled nucleotides. The research concluded that ISH with tyramide signal amplification (TSA) could achieve nearly equivalent sensitivity to IS-PCR with superior reproducibility, highlighting the power of amplified indirect detection systems in formalin-fixed paraffin-embedded (FFPE) tissues [47].
An earlier 1993 study further underscored the challenges of direct IS-PCR, noting frequent false-positive results caused by DNA repair mechanisms or internal priming, particularly in tissue sections [48]. This reinforces that while direct methods can be powerful, their application requires rigorous controls to ensure specificity.
Detailed Protocol: RNA-ISH with Indirect Fluorescent Detection
This protocol is optimized for detecting mRNA in FFPE tissue sections for co-localization studies.
A. Sample Preparation and Pre-treatment
- Dewaxing and Rehydration: Cut 4-5 µm FFPE sections. Deparaffinize in xylene (2 x 10 min) and rehydrate through a graded ethanol series (100%, 95%, 70%) to nuclease-free water.
- Protease Digestion: Digest sections with Proteinase K (e.g., 10-15 µg/mL in TE buffer) for 15-30 minutes at 37°C. Optimization Note: Over-digestion damages morphology, while under-digestion reduces probe accessibility.
- Post-fixation: Briefly post-fix in 4% paraformaldehyde for 10 min to retain tissue architecture.
B. Hybridization
- Pre-hybridization: Apply a sufficient volume of pre-hybridization buffer to cover the section. Incubate in a humidified chamber for 1 hour at the assay temperature to block non-specific sites.
- Probe Application: Dilute the digoxigenin (DIG)-labeled RNA probe in hybridization buffer. Apply the mixture to the section, add a coverslip, and seal to prevent evaporation.
- Denaturation and Hybridization: Denature the probe and target simultaneously at 80-85°C for 5-10 min. Then, hybridize overnight (12-16 hours) in a humidified chamber at 55-60°C. Critical Parameter: RNA-RNA hybrids require specific temperature optimization.
C. Post-Hybridization Washes and Blocking
- Stringency Washes: Perform a series of stringent washes with Saline-Sodium Citrate (SSC) buffer, concluding with a high-stringency wash (e.g., 0.1x SSC) at the hybridization temperature to remove mismatched or unbound probe.
- Blocking: Incubate sections with a blocking solution (e.g., 2% normal sheep serum, 2% BSA in buffer) for 30-60 minutes to prevent non-specific antibody binding.
D. Indirect Immunofluorescence Detection
- Primary Antibody Incubation: Incubate with a mouse anti-DIG monoclonal antibody diluted in blocking buffer for 1-2 hours at room temperature.
- Washing: Wash thoroughly with buffer (e.g., PBS-T) 3 x 5 minutes to remove unbound antibody.
- Secondary Antibody Incubation: Incubate with a fluorophore-conjugated goat anti-mouse IgG (H+L) secondary antibody (cross-adsorbed against other species) for 1 hour at room temperature. Protect from light from this step onward.
- Counterstaining and Mounting: Wash again 3 x 5 minutes. Counterstain nuclei with DAPI or Hoechst stain [45]. Apply an aqueous anti-fade mounting medium and a coverslip.
Essential Research Reagent Solutions
Successful co-localization studies depend on a suite of reliable, high-quality reagents. The following table details key materials and their functions.
Table 3: Key Reagent Solutions for ISH and IHC Co-localization Studies
| Reagent / Kit | Function / Description | Key Considerations |
|---|---|---|
| RNAscope ISH Assays [49] | A proprietary RNA-ISH platform using a novel probe design and signal amplification system to enable single-molecule RNA detection in FFPE tissues. | Provides high sensitivity and specificity; available in chromogenic and fluorescent formats; suitable for automated platforms. |
| In Vitro Transcription Kits | For synthesizing high-specific-activity RNA probes (riboprobes) with labeled nucleotides (e.g., DIG-UTP, Fluorescein-UTP). | Essential for generating custom RNA probes; ensures high-fidelity transcription from DNA templates containing RNA polymerase promoters (SP6, T7, T3). |
| Poly-HRP Conjugated Secondaries [45] | Secondary antibodies conjugated to multiple horseradish peroxidase (HRP) enzyme molecules. | Offers superior signal amplification for chromogenic detection compared to traditional single-enzyme conjugates, enhancing sensitivity for low-abundance targets. |
| Cross-Adsorbed Secondary Antibodies [46] [50] | Secondary antibodies that have been purified to remove antibodies that cross-react with immunoglobulins from non-target species. | Critical for multiplex experiments to ensure species specificity and minimize background. |
| Tyramide Signal Amplification (TSA) Kits [47] | An enzyme-mediated detection method where HRP catalyzes the deposition of numerous fluorescent or chromogenic tyramide molecules at the target site. | Provides extreme signal amplification, capable of detecting low-copy-number targets; requires careful optimization to control background. |
| F(ab')â‚‚ Fragment Secondaries [46] [50] | Secondary antibodies lacking the Fc region, generated by enzymatic digestion of whole IgG. | Reduces non-specific binding to Fc receptors on immune cells (e.g., in spleen, lymph node samples), lowering background and improving specificity. |
| Multi-rAb Polymer HRP Secondaries [50] | Recombinant secondary antibodies formulated as a mixture of monoclonal antibodies recognizing multiple epitopes on the primary antibody. | Provides high sensitivity without biotin (eliminating background from endogenous biotin), excellent lot-to-lot consistency, and low background. |
| Antibody Labeling Kits (e.g., ReadiLink) [46] | Kits for in-house conjugation of fluorophores or other labels to primary antibodies. | Offers flexibility for direct detection and multiplexing; allows researchers to create custom-labeled primary antibodies. |
The selection between DNA and RNA probes and direct or indirect detection is not a matter of identifying a universally superior option, but rather of making a strategic choice aligned with the experimental hypothesis. For detecting DNA genomic targets, such as chromosomal translocations, DNA probes are the standard. For analyzing gene expression at the mRNA level, RNA probes offer superior specificity and signal-to-noise ratio. Similarly, direct detection provides simplicity and is ideal for multiplexing, while indirect detection is the method of choice for maximum sensitivity and flexibility, particularly for low-abundance targets. As the field progresses with innovations like automated ISH platforms [49] and novel probe chemistries like Locked Nucleic Acids (LNA) [43], this foundational understanding will empower researchers to effectively leverage these tools, driving discovery in drug development and diagnostic science.
In the study of cellular function, the spatial relationships between proteins and nucleic acids are often fundamental to understanding molecular mechanisms. Techniques like immunohistochemistry (IHC) and in situ hybridization (ISH) have long been used to visualize these biomolecules. However, accurately determining their co-localization has been persistently limited by the diffraction barrier of conventional light microscopy, which blurs structures smaller than about 200-250 nm. This is a critical limitation, as many molecular complexes and interactions occur on a much finer scale. The need to visualize these relationships with high fidelity is particularly acute in drug development, where understanding precise molecular interactions can inform therapeutic strategies. For example, in lung cancer diagnostics, the critical task of detecting EML4-ALK gene rearrangements has traditionally relied on fluorescence in situ hybridization (FISH), but studies have shown this method may miss a significant number of patients who could benefit from targeted therapy compared to more sensitive IHC screening [51].
Super-resolution microscopy techniques have overcome the diffraction limit, but often require expensive, specialized instrumentation. In this landscape, Expansion Microscopy (ExM) has emerged as a powerful alternative, enabling nanoscale imaging on conventional microscopes by physically expanding biological specimens embedded in a swellable hydrogel [52]. Until recently, a major challenge has been achieving efficient and simultaneous retention of both proteins and nucleic acids (like mRNA) within the same hydrogel matrix, which is essential for true co-localization studies. This guide compares a groundbreaking solution—Photoclick Dual Anchoring Expansion Microscopy (Phan-ExM)—against other leading-edge super-resolution alternatives, providing researchers with the experimental data and protocols needed for informed methodological selection.
Methodological Comparison: Phan-ExM Versus Other Super-Resolution Techniques
The field of super-resolution imaging offers multiple pathways to nanoscale resolution, each with distinct trade-offs in resolution, throughput, multiplexing capability, and accessibility. The following table provides a structured comparison of Phan-ExM with other advanced imaging platforms.
Table 1: Performance Comparison of Super-Resolution Imaging Techniques
| Imaging Technique | Principle of Operation | Effective Resolution | Throughput & Scalability | Key Advantage | Primary Limitation |
|---|---|---|---|---|---|
| Phan-ExM [53] | Physical expansion & hydrogel embedding | ~85 nm (co-imaging) | Conventional microscope; single specimen scale | Rapid (10 min), concurrent anchoring of proteins & mRNA; superior fluorescence intensity | Requires specific chemical anchoring reagent (MAP-mPyTC) |
| ExA-SPIM [54] | Physical expansion + light-sheet optics | 375 nm lateral, 750 nm axial (with 4x expansion) | Very High (946 megavoxels/s); centimeter-scale tissues | Aberration-free imaging over massive FOV (10.6x8.0 mm²) | Lower absolute resolution than Phan-ExM; more complex setup |
| SPI Microscopy [55] | Multifocal optical rescaling & panoramic integration | ~120 nm (after deconvolution) | Extremely High (5000-10,000 cells/s); high-content screening | Instant super-resolution images on-the-fly; minimal post-processing | Resolution enhancement is lower than expansion techniques |
| Computational SR (SRRF) [56] | Software analysis of fluorescence fluctuations | Varies (sub-diffraction) | High (works with standard datasets) | No specialized hardware; compatible with ImFCS for dynamics | Performance is algorithm-dependent and can vary |
Inside the Techniques: Core Technologies and Workflows
Photoclick Dual Anchoring Expansion Microscopy (Phan-ExM)
Phan-ExM introduces an innovative chemical approach to solve the co-localization problem. Its key innovation is the anchoring reagent N-(3-methacrylamidopropyl)-3-(2-methyl-1H-pyrrol-1-yl)-2H-tetrazole-2-carboxamide (MAP-mPyTC). This molecule enables the rapid and concurrent retention of both proteins and nucleic acids within the ExM gel matrix via photoclick chemistry [53]. The process is significantly faster than traditional ExM protocols, reducing anchoring time from hours (or overnight) to just 10 minutes. Furthermore, it enhances the fluorescence signal of labeled biomolecules, a critical factor for obtaining high-quality super-resolution images. The workflow enables high-resolution co-imaging of multiplex proteins and nucleic acids on a single specimen, allowing researchers to observe phenomena such as the aggregation of ACTB mRNA at sites of mitochondrial damage in cultured cells [53].
Diagram: Phan-ExM experimental workflow for protein and RNA co-imaging.
Expansion-Assisted Selective Plane Illumination Microscopy (ExA-SPIM)
ExA-SPIM combines physical expansion with a specialized light-sheet microscope designed for massive imaging volumes. It addresses the "volumetric imaging barrier" by employing optics with an exceptionally large field of view (10.6 × 8.0 mm²) and working distance (35 mm), while maintaining a numerical aperture (NA=0.305) sufficient for high resolution [54]. When coupled with tissue expansion, this system achieves isotropic resolution at impressive speeds (up to 946 megavoxels/s), making it possible to image an entire expanded mouse brain at subcellular resolution without physical sectioning. This is transformative for projects requiring complete 3D structural context, such as brain-wide reconstruction of neuronal arbors.
Super-resolution Panoramic Integration (SPI)
SPI is an on-the-fly optical super-resolution technique that does not rely on physical sample expansion. It leverages multifocal optical rescaling, high-content sample sweeping, and a synchronized line-scan (TDI) readout within a conventional epi-fluorescence framework [55]. SPI instantly generates sub-diffraction-limited images concurrently with acquisition, achieving a twofold resolution enhancement (~120 nm) without the need for complex post-processing. Its immense throughput (up to 1.84 mm²/s, imaging tens of thousands of cells per second) makes it uniquely suited for high-content screening applications where population-level heterogeneity is of interest.
Computational Super-Resolution Radial Fluctuations (SRRF)
For labs seeking to enhance resolution without capital investment in new hardware, computational methods like SRRF offer an accessible path. SRRF analyzes temporal fluctuations in fluorescence signals ("radial fluctuations") from standard diffraction-limited images to generate a super-resolution image [56]. This technique is particularly compatible with imaging Fluorescence Correlation Spectroscopy (ImFCS), allowing researchers to not only determine nanoscale structure, as in visualizing cortical actin fibers, but also to measure dynamics and diffusion coefficients within specific subcellular regions [56].
Diagram: A decision framework for selecting a super-resolution technique.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of these advanced imaging techniques, particularly Phan-ExM, relies on a specific set of reagents and materials.
Table 2: Key Research Reagents for Phan-ExM and Related Techniques
| Reagent / Material | Function / Role | Example Application / Note |
|---|---|---|
| MAP-mPyTC [53] | Dual-function anchoring reagent; enables rapid, concurrent retention of proteins and nucleic acids via photoclick chemistry. | The critical, novel component in Phan-ExM that differentiates it from other ExM methods. |
| Swellable Hydrogel Monomer [53] [54] | Forms the expandable polymer network that physically enlarges the specimen. | A common core component across all expansion microscopy protocols (e.g., sodium acrylate, acrylamide). |
| Validated IHC Antibodies [51] | High-specificity antibodies for targeting proteins of interest; validation is crucial for reliability. | The D5F3 anti-ALK antibody showed superior sensitivity in detecting EML4-ALK rearrangements vs. FISH [51]. |
| FISH / RNA Labeling Probes [53] [51] | Fluorescently labeled probes for detecting specific DNA sequences or mRNA transcripts. | Phan-ExM demonstrated enhanced fluorescence intensity for RNA spots compared to prior methods [53]. |
| Cell/Tissue Specific Reagents [55] | Labels for specific cellular structures (e.g., WGA for membranes, dyes for organelles). | Used in SPI for high-throughput blood smear analysis and differential white blood cell counting [55]. |
| 4-But-3-ynyl-2-methylthiomorpholine | 4-But-3-ynyl-2-methylthiomorpholine Research Chemical | |
| 4-Methyloxolane-2-carboxylic acid | 4-Methyloxolane-2-carboxylic Acid|CAS 2126177-86-2|RUO | 4-Methyloxolane-2-carboxylic acid (C6H10O3). A high-purity, chiral building block for pharmaceutical and organic synthesis. For Research Use Only. Not for human or veterinary use. |
Experimental Protocols: Key Methodologies for Reproduction
Phan-ExM Protocol for Protein and mRNA Co-Imaging
This protocol is adapted from the methodology that enabled the ~85 nm resolution co-imaging of proteins and nucleic acids [53].
- Sample Fixation and Permeabilization: Begin with standard chemical fixation (e.g., with paraformaldehyde) of cultured cells or thin tissue sections, followed by permeabilization (e.g., with Triton X-100) to allow entry of labels and reagents.
- Biomolecule Labeling: Fluorescently label target proteins using validated immunohistochemistry (IHC) protocols with primary and secondary antibodies. Simultaneously, or in sequence, label target mRNA molecules using validated fluorescence in situ hybridization (FISH) protocols with fluorescent probes.
- Dual Anchoring Reaction: Incubate the labeled sample with the key reagent, MAP-mPyTC. Following incubation, expose the sample to UV light to initiate the "photoclick" reaction. This step covalently links the fluorescently labeled biomolecules to the hydrogel precursor in approximately 10 minutes.
- Hydrogel Polymerization: Prepare the swellable polymer solution (typically containing sodium acrylate, acrylamide, and a crosslinker) with an initiator system (e.g., APS and TEMED). Embed the sample in this solution and allow it to polymerize into a solid hydrogel.
- Protein Digestion and Expansion: Digest the cellular proteins using a protease (e.g., proteinase K) to free the biomolecules from the physical structure, leaving them anchored to the hydrogel network. Finally, immerse the hydrogel in deionized water, triggering isotropic physical expansion by a factor of ~4-4.5.
- Image Acquisition and Analysis: Image the expanded, transparent hydrogel on a conventional fluorescence or confocal microscope. The physical expansion translates the original nanoscale structures into a microscale representation, effectively achieving ~85 nm resolution.
SPI Microscopy for High-Throughput Cell Screening
This protocol outlines the process for using SPI to achieve real-time super-resolution imaging of large cell populations, as demonstrated in peripheral blood smear analysis [55].
- Sample Preparation: Prepare cells on a slide or in a flow chamber. For blood smears, label with a general membrane stain like Wheat Germ Agglutinin (WGA).
- System Setup: Configure the SPI microscope, which integrates a TDI (Time-Delay Integration) sensor and multifocal optics into an epi-fluorescence framework. The TDI sensor's line-scan readout is synchronized with the mechanical stage for continuous sample sweeping.
- Data Acquisition: Continuously scan the sample. The SPI system performs optical photon reassignment and integration on-the-fly, generating a super-resolution image stream without the need for post-processing. The system can achieve a throughput of up to 1.84 mm²/s.
- Optional Deconvolution (Instant): Apply a non-iterative rapid Wiener-Butterworth (WB) deconvolution for an additional resolution enhancement. This processing is exceptionally fast (~10 ms), preserving the real-time nature of the output.
- Population Analysis: Use the generated high-resolution, large-field images for automated population-level analysis, such as differential white blood cell counting or morphological analysis of tens of thousands of cells.
The emergence of techniques like Phan-ExM, ExA-SPIM, and SPI represents a significant maturation of the super-resolution microscopy field, offering tailored solutions for distinct biological questions. Phan-ExM stands out for researchers whose primary need is the highest-resolution co-localization of proteins and nucleic acids within standard samples, leveraging its novel chemistry to maximize efficiency and signal. ExA-SPIM is the unequivocal choice for projects demanding the comprehensive imaging of very large, intact specimens at synaptic resolution. SPI Microscopy excels in applications where population-level statistics and high-throughput screening are the primary goals. Finally, computational SR methods provide a viable and accessible entry point for super-resolution, especially when paired with dynamics studies.
For the field of ISH and IHC co-localization research, these technologies move the goalpost from mere detection to precise, nanoscale mapping of molecular interactions. This precision, demonstrated by Phan-ExM's ability to reveal mRNA aggregation at specific organellar damage sites, provides a more powerful toolkit for drug development professionals to understand disease mechanisms and validate therapeutic targets.
The integration of artificial intelligence (AI) with digital pathology is fundamentally transforming the quantification of signals in whole slide imaging (WSI), particularly for immunohistochemistry (IHC) and in situ hybridization (ISH) co-localization studies. This technological synergy is moving pathology from a subjective, manual practice to a data-driven, quantitative discipline essential for precision medicine [57]. For researchers and drug development professionals, AI-enhanced tools provide reproducible, high-throughput analysis of biomarker expression, enabling more accurate patient stratification and therapeutic response assessment in clinical trials [58].
These advanced computational methods are particularly crucial for complex analytical tasks such as quantifying low-abundance biomarkers, standardizing scoring across multiple observers and sites, and identifying subtle morphological patterns that predict treatment response [59]. The emergence of "HER2-low" as a clinically relevant category in breast cancer, for instance, underscores the need for sensitive AI tools that can consistently identify and quantify low expression levels that may be challenging for human assessment alone [59].
Comparative Analysis of AI Digital Pathology Tools
The landscape of AI tools for digital pathology has expanded significantly, with numerous platforms now offering capabilities for automated signal quantification. The performance characteristics of these systems vary considerably based on their underlying algorithms, training datasets, and intended applications.
Table 1: Comparison of Leading AI Digital Pathology Platforms
| Platform/Developer | Primary Application | Quantification Capabilities | Regulatory Status | Key Strengths |
|---|---|---|---|---|
| Lunit | Breast cancer biomarkers | HER2, ER, PR scoring | FDA-cleared for some applications | High concordance at high expression levels |
| PathAI | Oncology biomarker quantification | IHC signal quantification | Research use and clinical trials | Robust algorithm training |
| Indica Labs | Pharma research & diagnostics | Multiplex IHC analysis | Research use platform | High-throughput processing |
| 4D Path | Cancer diagnostics & prognosis | Tumor microenvironment mapping | Research use | Predictive outcome modeling |
| Nucleai | Spatial biology & biomarkers | Tissue architecture analysis | Research use | Spatial relationship analysis |
Performance Metrics from Comparative Studies
Recent large-scale comparative studies have provided objective data on the performance characteristics of various AI platforms for biomarker quantification. The Digital PATH Project, sponsored by Friends of Cancer Research, represents one of the most comprehensive evaluations to date, comparing 10 different AI tools on a common set of approximately 1,100 breast cancer samples for HER2 status evaluation [59].
The study revealed several critical findings regarding AI performance. First, AI tools demonstrated high concordance with expert pathologists for samples with high HER2 expression, with minimal variability between different platforms. Second, the greatest performance variability occurred at low expression levels (0 and 1+), highlighting both a challenge and opportunity for AI enhancement. Third, the use of a common reference set of samples enabled standardized characterization of test performance across platforms, providing a model for future validation approaches [59].
Table 2: Performance Metrics from the Digital PATH Project (HER2 Assessment)
| Performance Metric | High HER2 Expression | Low HER2 Expression (0/1+) | Overall Concordance |
|---|---|---|---|
| Inter-platform Agreement | High (Minimal variability) | Moderate to High (Notable variability) | Not Reported |
| Pathologist Concordance | High | Moderate (Challenging for human assessment) | Not Reported |
| Key Challenge | Saturation effects | Sensitive detection and classification | Standardization across platforms |
| AI Advantage | Consistency and speed | Pattern recognition sensitivity | High-throughput analysis |
Experimental Protocols for AI Validation in IHC/ISH
Standardized Workflow for AI-Assisted Quantification
The validation of AI tools for signal quantification requires rigorous experimental protocols to ensure reliability and reproducibility. The following workflow outlines a standardized approach for evaluating AI performance in IHC and ISH co-localization studies:
Sample Preparation: Tissues are fixed in 10% neutral buffered formalin and processed for paraffin embedding following established histopathology protocols. Section thickness should be standardized (typically 4-5μm) to minimize pre-analytical variables [6].
Staining Protocol: For IHC, sections are stained using validated primary antibodies with appropriate positive and negative controls. For ISH, target-specific probes are applied using automated staining systems to ensure consistency. Multiplex staining protocols may be employed for co-localization studies [6].
Slide Digitization: Stained slides are scanned using high-throughput whole slide scanners (e.g., Leica Aperio GT450, Hamamatsu NanoZoomer S360) at ×40 equivalent magnification (0.25 μm/pixel) to generate high-resolution digital images [60].
Image Quality Control: Digital images undergo rigorous quality assessment for focus accuracy, tissue preservation, staining intensity, and absence of artifacts. Studies indicate that 8%-61% of digital slides may require rescanning due to quality issues, emphasizing the importance of this step [60].
AI Algorithm Processing: Digital slides are analyzed by AI algorithms trained for specific quantification tasks. For HER2 scoring, this includes membrane staining intensity, completeness of staining, and cellular localization [59].
Pathologist Review and Concordance Assessment: AI-generated results are compared against manual assessments by expert pathologists, with statistical analysis of concordance rates (e.g., Cohen's kappa) for categorical scores and intraclass correlation coefficients for continuous measurements [59].
Scanner Performance and Image Quality Considerations
The performance of AI quantification algorithms is heavily dependent on image quality, which varies significantly across different whole slide imaging systems. A comprehensive study evaluating 16 whole slide scanners from 7 different vendors revealed substantial variations in real-world performance [60].
Table 3: Scanner Performance Metrics in Clinical Settings
| Performance Metric | Range Across Scanners | Implications for AI Analysis |
|---|---|---|
| Instrument Scan Time | 7:30 - 43:02 (hours:minutes) | Affects throughput and workflow efficiency |
| Technician Operation Time | 1:30 - 9:24 (hours:minutes) | Impacts labor costs and operational scalability |
| Total Scan Run Time | 13:30 - 47:02 (hours:minutes) | Determines case completion timelines |
| Image Quality Errors | 8% - 61% of slides | Directly affects AI algorithm accuracy |
| Missing Tissue Errors | 0% - 21% of slides | Potential for incomplete analysis |
| Out-of-Focus Errors | 0% - 30.1% of slides | Compromises cellular detail quantification |
These findings highlight the critical importance of standardized scanning protocols and rigorous quality control measures in digital pathology workflows supporting AI analysis. Laboratories must implement comprehensive quality management systems specifically designed for digital pathology operations to ensure consistent image quality for AI applications [61].
Essential Research Reagent Solutions for AI-Enhanced Pathology
The successful implementation of AI-enhanced digital pathology requires not only computational tools but also high-quality reagents and materials throughout the workflow. The following table details essential research reagent solutions for automated signal quantification studies:
Table 4: Essential Research Reagents for AI-Enhanced IHC/ISH Studies
| Reagent/Material | Function | Considerations for AI Applications |
|---|---|---|
| Formalin-Based Fixatives | Tissue preservation and protein/epitope stabilization | Standardized fixation time critical for consistent staining [6] |
| Validated Primary Antibodies | Specific detection of target antigens | Lot-to-lot consistency vital for reproducible quantification [6] |
| ISH Probes | Detection of specific DNA/RNA sequences | Probe design affects signal intensity and specificity [6] |
| Chromogenic Substrates | Visual signal generation for IHC | Stable precipitation patterns improve AI segmentation [6] |
| Fluorescent Conjugates | Multiplex detection and quantification | Broader dynamic range for quantitative AI analysis [6] |
| Automated Staining Reagents | Standardized assay performance | Reduced variability compared to manual methods [61] |
| Quality Control Materials | Process monitoring and validation | Essential for AI model training and validation [61] |
Implementation Challenges and Future Directions
Technical and Regulatory Considerations
Despite the promising capabilities of AI-enhanced digital pathology, several significant challenges remain for widespread clinical and research implementation. Standardization of image acquisition and analysis represents a fundamental hurdle, as digital pathology images are generated using diverse scanners at multiple resolutions, leading to substantial variability in image quality [62]. This lack of standardization complicates cross-study comparisons and hinders the development of robust, generalizable computational pathology algorithms [58].
The regulatory landscape for AI-based pathology tools continues to evolve, with only three AI/ML Software as a Medical Device tools having received FDA clearance to date [58]. This limited regulatory adoption reflects challenges in validation rather than an absence of regulatory pathways. The development of independent reference sets of samples, as demonstrated in the Digital PATH Project, provides a promising approach for characterizing test performance and supporting regulatory validation [59].
Quality Management and Infrastructure Requirements
Successful implementation of AI-enhanced digital pathology requires comprehensive quality management systems (QMS) specifically tailored to digital pathology operations. Memorial Sloan Kettering Cancer Center has developed a structured Digital Pathology Quality Essentials (DPQE) framework that addresses the unique requirements of clinical digital pathology, including organization and leadership, facilities and safety management, personnel training, equipment management, and process management [61].
Infrastructure requirements represent another significant consideration, particularly for resource-limited settings. The substantial variation in scanner throughput and performance highlighted in comparative studies necessitates careful planning of institutional resources [60]. Additionally, the creation of large, annotated image datasets for training machine learning algorithms remains labor-intensive and often requires international collaboration, as demonstrated by projects in Sub-Saharan Africa funded by global health organizations [62].
AI-enhanced digital pathology represents a transformative approach to automated signal quantification in whole slide imaging, offering researchers and drug development professionals unprecedented capabilities for objective, reproducible biomarker analysis. The comparative assessment of AI tools reveals both substantial promise in standardized quantification and ongoing challenges in low-expression detection and cross-platform consistency.
The successful implementation of these technologies requires not only sophisticated algorithms but also rigorous standardization of pre-analytical conditions, comprehensive quality management systems, and appropriate infrastructure. As the field continues to evolve, collaborative efforts between pathologists, computer scientists, and regulatory bodies will be essential to fully realize the potential of AI-enhanced digital pathology for advancing precision medicine and therapeutic development.
For research applications, particularly in IHC and ISH co-localization studies, these tools offer the potential to uncover novel biomarker relationships and spatial patterns that were previously undetectable through manual analysis. The continued refinement and validation of AI quantification platforms will undoubtedly accelerate drug discovery and improve diagnostic accuracy in the coming years.
Solving Common Pitfalls: A Practical Guide to Optimizing Co-Localization Assays
In the advanced realms of in situ hybridization (ISH) and immunohistochemistry (IHC) co-localization studies, the integrity of the target biomolecule—be it protein or nucleic acid—is paramount. A critical, yet often under-optimized, step governing this integrity is antigen retrieval. For researchers and drug development professionals working with challenging tissues, choosing the correct retrieval method is not a mere procedural detail but a decisive factor for experimental success. This guide provides a objective comparison between Heat-Induced Epitope Retrieval (HIER) and enzyme-based Proteolytic-Induced Epitope Retrieval (PIER), with a focused examination of Proteinase K digestion. We present supporting experimental data to equip scientists with the evidence needed to select and optimize the right protocol for their specific research context, particularly in multiplexed staining and co-localization workflows.
Antigen Retrieval: HIER vs. PIER
Antigen retrieval is a foundational technique for reversing the protein crosslinks formed during formalin fixation, which mask epitopes and limit antibody binding [63]. The two primary methods are HIER and PIER, which operate through distinct mechanisms.
The following table summarizes the core characteristics of each method.
Table 1: Fundamental Comparison of HIER and PIER
| Feature | Heat-Induced Epitope Retrieval (HIER) | Proteolytic-Induced Epitope Retrieval (PIER) |
|---|---|---|
| Fundamental Principle | Uses heat to reverse protein crosslinks, causing crosslinked proteins to unfold [63]. | Uses enzymes (e.g., Proteinase K, trypsin) to degrade protein crosslinks [63]. |
| Key Mechanism | Disruption of methylene bridges via thermal energy [64]. | Proteolytic cleavage of peptide bonds within crosslinks [65]. |
| Typical Conditions | 90-120°C for 10-20 min in a specific buffer (e.g., citrate, Tris-EDTA) [65] [64]. | 37°C for 10-90 min in a buffer suited to the enzyme (e.g., Tris/HCl for Proteinase K) [65] [66]. |
| Advantages | Broad applicability; effective for many antigens; lower risk of morphology loss vs. early enzymatic methods [64]. | Gentler on tissue adhesion; often essential for densely packed matrices (e.g., cartilage, bone) [65] [66]. |
| Disadvantages | Can cause tissue section detachment; may destroy certain heat-labile epitopes [65]. | Risk of over-digestion and loss of antigenicity; requires precise optimization of concentration and time [66]. |
The decision to use HIER or PIER hinges on the nature of the target antigen, the tissue type, and the degree of fixation. The following workflow diagram outlines the key decision points for selecting and optimizing an antigen retrieval strategy.
Proteinase K in PIER: Protocol and Optimization
Proteinase K is a serine protease with broad specificity for cleaving peptide bonds, making it highly effective in PIER for digesting crosslinking proteins [67]. Its activity is optimal at a pH between 8.0 and 9.0 and a temperature of around 37°C, though it remains active over a wide range of conditions [67].
Standard Proteinase K PIER Protocol
A typical Proteinase K retrieval protocol, as used for detecting CILP-2 in osteoarthritic cartilage, involves the following steps [65]:
- Deparaffinization and Rehydration: Following standard IHC protocols, slides are deparaffinized in xylene and rehydrated through a graded series of ethanol to water.
- Enzymatic Retrieval: Incubate sections with 30 µg/mL Proteinase K solution in 50 mM Tris/HCl buffer (pH 6.0) for 90 minutes at 37°C [65].
- Optional Additional Treatment: For certain tissues like cartilage, a subsequent treatment with 0.4% bovine hyaluronidase in HEPES-buffered medium for 3 hours at 37°C can be applied to digest the dense extracellular matrix further [65].
- Inactivation and Washing: Gently rinse the slides in phosphate-buffered saline (PBS) to remove the enzyme and stop the reaction.
- Proceed with IHC/ISH: Continue with the standard protocol for immunohistochemistry or in situ hybridization.
Critical Optimization Parameters
The effectiveness of Proteinase K digestion is highly sensitive to specific conditions. Systematic optimization is required to balance epitope unmasking with tissue preservation.
Table 2: Proteinase K Digestion Optimization Guide
| Parameter | Typical Range | Optimization Tips and Evidence |
|---|---|---|
| Concentration | 10 - 100 µg/mL | In skeletal tissue ISH, 10 µg/mL improved signal and morphology vs. 100 µg/mL [66]. Titrate to find the lowest effective concentration. |
| Incubation Time | 30 min - Overnight | Time varies with sample type. Overnight digestion is common for FFPE tissues, but shorter times (e.g., 90 min) are often sufficient [65] [68]. |
| Temperature | 37°C - 65°C | 37°C is standard for IHC retrieval [65]. Higher temperatures (55-65°C) are used in DNA extraction for faster lysis [67] [68]. |
| pH | 6.0 - 9.0 | While optimal activity is at pH 8.0-9.0 [67], specific IHC protocols successfully use pH 6.0 [65]. The buffer should match the experimental requirement. |
| Inhibitors | SDS, EDTA, PMSF | Common reagents can inhibit Proteinase K. SDS denatures the enzyme, while EDTA chelates calcium ions essential for its stability [67]. |
Comparative Experimental Data in Research
Direct comparisons in recent scientific literature demonstrate that the choice between HIER and PIER is context-dependent, with Proteinase K-based PIER often proving superior for specific challenging targets.
Case Study: CILP-2 Detection in Articular Cartilage
A 2024 study directly compared four antigen retrieval protocols for IHC detection of CILP-2, a minor glycoprotein in dense osteoarthritic cartilage [65].
- Experimental Groups:
- PIER (Proteinase K and hyaluronidase)
- HIER (95°C for 10 min)
- Combined HIER/PIER
- No retrieval (control)
- Key Findings:
- Conclusion: For this low-abundance protein in a voluminous extracellular matrix, gentle enzymatic retrieval was more effective than heat-based methods.
Case Study: ISH in Skeletal Tissues
Research on skeletal tissues highlighted the need for optimized Proteinase K digestion in ISH to preserve tissue morphology while achieving adequate signal [66].
- Experimental Findings:
- A standard concentration of 100 µg/mL Proteinase K produced inconsistent results and often impaired tissue morphology.
- Reducing the concentration to 10 µg/mL optimized the detection of mRNAs for lubricin (Prg4) and type X collagen (Col10a1) in rat femoral FFPE sections, resulting in robust signals with well-preserved tissue structure [66].
- Conclusion: For ISH on skeletal tissues, lower, carefully titrated concentrations of Proteinase K are critical for success.
Performance in Expansion Microscopy
Proteinase K also plays a vital role in expansion microscopy (proExM), where it digests proteins to allow for physical tissue expansion. A 2021 study found that immunostaining before expansion (IHC-pre) followed by 8 hours of Proteinase K digestion consistently resulted in robust fluorescence retention for immunolabeled subcellular organelles like mitochondria and Golgi apparatus in mouse brain tissue [69]. This "organelle optimized" protocol enabled accurate quantification of mitochondria size and number, which was less effective with milder, protease-free digestion methods [69].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table lists essential reagents and their functions for implementing and optimizing the discussed protocols.
Table 3: Essential Reagents for Antigen Retrieval and Co-localization Studies
| Reagent / Kit | Primary Function | Application Note |
|---|---|---|
| Proteinase K | Serine protease for enzymatic antigen retrieval (PIER) by digesting protein crosslinks. | Critical for dense tissues and specific epitopes; requires optimization of concentration and time [65] [67]. |
| HIER Buffer Solutions | (e.g., Citrate, Tris-EDTA, Reveal Decloaker). Buffered solutions used in heat-induced retrieval to maintain specific pH. | Buffer pH is a critical factor for the success of HIER [65] [63]. |
| Hyaluronidase | Enzyme that digests hyaluronic acid, a major component of the cartilage matrix. | Used in combination with Proteinase K in dense tissues to improve antibody penetration [65]. |
| Dako REAL EnVision Detection System | Peroxidase/DAB+ detection system for chromogenic IHC. | Used for visualization in comparative studies after antigen retrieval [65]. |
| Multiplex IHC/IF Kits | (e.g., DISCOVERY Green HRP kit). Kits enabling simultaneous detection of multiple biomarkers. | Advances in multiplexing allow for complex co-localization studies post-retrieval [70]. |
Within the rigorous framework of ISH and IHC co-localization research, there is no universal "best" antigen retrieval method. The experimental evidence clearly shows that HIER is a powerful, broad-spectrum technique, but Proteinase K-based PIER is an indispensable tool for specific challenges. PIER proves superior for detecting vulnerable epitopes in delicate or densely packed tissues like cartilage and bone, where HIER can cause damage. Success hinges on systematic optimization of Proteinase K concentration, time, and temperature. Mastering both HIER and PIER, and understanding their respective strengths, provides researchers with the precision needed to unveil critical protein and gene expression patterns in complex biological systems.
Spatial multi-omics represents a significant advancement in biological research, enabling scientists to study complex tissues while preserving crucial molecular context. For researchers investigating the intricate relationships between gene expression and protein localization, combining in situ hybridization (ISH) and immunohistochemistry (IHC) provides a powerful approach to correlate transcriptional activity with translational output within the same tissue section [38]. However, this integration faces a fundamental technical conflict: optimal conditions for each technique directly oppose each other. IHC antibodies degrade during the protease treatments that ISH requires, while the RNases present during IHC protocols destroy RNA targets needed for ISH detection [38]. These methodological incompatibilities often manifest as two persistent problems that compromise data quality: weak target-specific staining and excessive non-specific background, which can obscure biological insights and reduce experimental reliability.
This guide systematically compares current methodologies and reagent systems for overcoming these signal challenges, providing objective performance data and detailed protocols to enable robust RNA-protein co-localization studies in tissue environments.
Technical Foundations: ISH and IHC Methodologies
Core Techniques and Detection Principles
Table 1: Fundamental Techniques in Spatial Multi-omics
| Technique | Target | Detection Mechanism | Primary Output | Spatial Application |
|---|---|---|---|---|
| Immunohistochemistry (IHC) | Proteins (antigens) | Antibodies tagged with fluorophores or enzymes bind to target proteins | Fluorescent or chromogenic protein localization | Defining cell neighborhoods and tissue architecture [38] |
| In Situ Hybridization (ISH) | RNA transcripts (mRNA, miRNA) | Nucleic acid probes hybridize to target RNA; amplified via branched DNA systems | Fluorescent or chromogenic transcript localization | Revealing active transcriptional states and cell heterogeneity [38] |
| Fluorescence In Situ Hybridization (FISH) | DNA/RNA sequences | Fluorescently labeled probes complementary to target sequences | Fluorescence signal detection | Gene mapping, chromosomal abnormalities, RNA expression [71] |
| Dual Bright-field ISH | DNA targets (e.g., HER2, CEP17) | Enzyme-based colorimetric detection with chromogens | Chromogenic signals visible by bright-field microscopy | Clinical diagnostics, gene amplification assessment [72] |
Signal Amplification Innovations in FISH
Recent technical innovations have significantly improved signal detection for low-abundance targets. Branched DNA (bDNA) systems employ successive layers of amplifiers and labeled probes that build on initial probe-target hybridization, producing substantially amplified complexes with minimal background noise [38]. For fluorescence detection, CRISPR-mediated fluorescence in situ hybridization amplifier (CRISPR FISHer) systems utilize phase separation techniques to precisely detect single-copy and multi-copy genes on chromosomes in living cells [71]. Additionally, SABER (Signal Amplification By Exchange Reaction) and HCR (Hybridization Chain Reaction) techniques enable exponential signal amplification through enzyme-free, hybridization-based approaches, dramatically improving detection sensitivity for rare transcripts while maintaining low background [71].
Systematic Troubleshooting: Weak Staining and High Background
Weak Staining: Causes and Evidence-Based Solutions
Weak or absent specific staining represents one of the most frequent challenges in IHC and ISH workflows, with multiple potential failure points requiring systematic investigation.
Primary antibody/probe issues represent a fundamental cause of weak staining. Researchers should confirm that primary antibodies are validated for the specific application (e.g., FFPE tissue) and storage conditions haven't compromised reactivity [73]. Performing antibody titration experiments is essential, starting with the manufacturer's recommended concentration and testing several dilutions (e.g., 1:50, 1:100, 1:200) to identify optimal signal-to-noise ratios [73].
Suboptimal antigen retrieval frequently undermines staining intensity, particularly in formalin-fixed tissues where methylene cross-links can mask epitopes. If using heat-induced epitope retrieval (HIER), researchers should empirically optimize buffer selection (e.g., Citrate pH 6.0 or Tris-EDTA pH 9.0), temperature, and incubation duration, as insufficient heating fails to unmask epitopes while excessive heating may destroy them [6] [73]. Over-fixation presents another common challenge, as prolonged formalin exposure can create epitope masking that requires more aggressive retrieval conditions [73].
For ISH, probe design and hybridization efficiency critically impact signal strength. Factors including probe length, GC content, number of probes, and dimer formation potential require careful optimization [71]. For low-abundance transcripts, traditional single-probe approaches often yield signals below detection thresholds, necessitating advanced amplification strategies like bDNA systems that can achieve single-molecule sensitivity while preserving spatial context [38].
Excessive background staining obscures specific signal interpretation and stems from distinct technical failures requiring different remediation approaches.
Primary antibody concentration that is too high represents the most common cause of high background in IHC, leading to non-specific binding [73]. Titration experiments that balance specific signal against background are essential, often revealing that lower antibody concentrations maintain specific staining while dramatically reducing background [74] [73].
Insufficient blocking enables non-specific antibody binding to tissue components. Researchers should implement comprehensive blocking protocols including peroxidase blocking (e.g., with 3% H2O2) for enzyme-based detection, avidin/biotin blocking when using biotin-based systems, and normal serum from the secondary antibody species to minimize non-specific interactions [74] [73]. For fluorescent detection, endogenous tissue autofluorescence presents additional challenges, particularly from lipofuscin in aged tissues or formaldehyde-induced fluorescence [73]. Applying quenching reagents such as Sudan Black B or using spectral unmixing techniques can effectively separate true signal from background [73].
Inadequate washing permits residual unbound antibodies to generate diffuse background signal [74]. Increasing washing duration and volume between steps, particularly after primary and secondary antibody incubations, significantly reduces this background source. Additionally, tissue section drying during processing causes irreversible non-specific antibody binding and edge artifacts, emphasizing the importance of maintaining humidified chambers throughout extended incubation steps [74] [73].
Table 2: Troubleshooting Guide for Signal Issues in IHC and ISH
| Problem | Primary Causes | Recommended Solutions | Supporting Evidence |
|---|---|---|---|
| Weak or No Staining | Primary antibody issues (invalidated, degraded) | Validate antibody for specific application; check storage conditions; run positive controls [73] | Systematic verification eliminates reagent failure [73] |
| Suboptimal antibody concentration | Perform titration experiments; test serial dilutions [73] | Identifies optimal signal-to-noise ratio [73] | |
| Inefficient antigen retrieval | Optimize HIER buffer, temperature, duration; increase retrieval intensity for over-fixed tissues [73] | Formalin fixation masks epitopes via cross-linking [6] | |
| Inactive detection system | Verify secondary antibody and detection components with control tissues [73] | Confirms detection system functionality [73] | |
| High Background | Excessive primary antibody | Reduce antibody concentration; optimize dilution [74] [73] | High antibody concentrations promote non-specific binding [73] |
| Inadequate blocking | Implement comprehensive blocking: peroxidase, avidin/biotin, serum blocking [74] [73] | Reduces non-specific antibody binding [73] | |
| Insufficient washing | Increase wash duration and volume; ensure complete coverage [74] | Removes unbound antibodies causing diffuse background [74] | |
| Tissue drying | Maintain humidified chambers throughout incubations [74] [73] | Prevents irreversible non-specific binding [73] | |
| Endogenous enzyme activity | Block with H2O2 (peroxidase) or Levamisol (alkaline phosphatase) [74] | Eliminates false-positive signals from tissue enzymes [74] |
Integrated ISH-IHC Protocols: Experimental Design and Performance Comparison
Optimized Co-Localization Workflow
Successfully integrating IHC with ISH requires specific protocol modifications that address their fundamentally incompatible requirements. Recent studies have established robust workflows that preserve both protein and RNA targets:
Critical modification 1: RNase inhibition - Implementing rigorous RNase containment using recombinant ribonuclease inhibitors (e.g., RNaseOUT) during antibody incubation and wash steps is essential to protect RNA integrity throughout IHC labeling [38].
Critical modification 2: Antibody crosslinking - After IHC labeling, antibodies must be crosslinked to tissue using standard formaldehyde fixation alone cannot withstand subsequent harsh ISH protease treatments [38].
Sequential detection approach - Performing IHC detection first, followed by crosslinking, then proceeding with ISH detection minimizes methodological interference while preserving both epitopes and RNA targets [38].
Scanner and Imaging Platform Comparison
Imaging platform selection significantly impacts signal detection quality, particularly for multiplexed co-localization studies. Recent comparative studies evaluating WSI scanners for AI-integrated ISH analysis revealed substantial performance differences:
Table 3: Scanner Performance in Automated ISH Analysis
| Scanner Protocol | Resolution | Numerical Aperture | Concordance with Manual FISH | Key Limitations |
|---|---|---|---|---|
| A1 | 0.12 µm/pixel | 0.95 NA | High concordance | Requires specialized equipment [72] |
| A2 | 0.12 µm/pixel | 1.2 NA | High concordance | Water immersion requirements [72] |
| B2 | 0.17 µm/pixel | Not specified | High concordance | Lower resolution than A1/A2 [72] |
| B3 | 0.17 µm/pixel with extended focus | Not specified | High concordance | Best performance with extended focus [72] |
| C1 | 0.26 µm/pixel | Not specified | Poor concordance (6/10 cases failed) | Nuclei detection failure due to resolution limits [72] |
This systematic comparison demonstrated that protocols with optimized resolutions of 0.12 µm/pixel and 0.17 µm/pixel with extended focus enabled accurate AI-based HER2 assessment, while lower-resolution scanning (0.26 µm/pixel) resulted in analysis failures in 60% of cases due to inadequate nuclei detection [72]. These findings highlight the critical importance of matching scanner capabilities to analytical requirements, particularly for automated quantification of multiplexed signals.
Research Reagent Solutions for Signal Optimization
Table 4: Essential Research Reagents for Signal Quality Control
| Reagent Category | Specific Examples | Primary Function | Role in Signal Optimization |
|---|---|---|---|
| RNase Inhibitors | Recombinant ribonuclease inhibitor (e.g., RNaseOUT) | Protects RNA integrity during IHC steps | Prevents RNA degradation in ISH-IHC co-detection [38] |
| Antibody Crosslinkers | Formaldehyde, DSG, DSP | Stabilizes antibody-antigen complexes after IHC | Preserves protein signals during subsequent ISH steps [38] |
| Signal Amplification Systems | Branched DNA (ViewRNA), Tyramide signal amplification | Enhances detection sensitivity for low-abundance targets | Enables visualization of rare transcripts without increased background [38] [71] |
| Blocking Reagents | Normal serum, BSA, commercial blocking mixtures | Reduces non-specific antibody binding | Minimizes background staining in IHC [74] [73] |
| Enzyme Blockers | H2O2 (peroxidase), Levamisol (alkaline phosphatase) | Inhibits endogenous enzyme activity | Prevents false-positive chromogenic development [74] |
| Autofluorescence Quenchers | Sudan Black B, commercial quenching kits | Reduces tissue autofluorescence | Improves signal-to-noise ratio in fluorescent detection [73] |
| Mounting Media | ProLong RapidSet, other anti-fade mountants | Preserves fluorescence and signal integrity | Prevents photobleaching and signal degradation during imaging [38] |
Overcoming signal challenges in ISH and IHC co-localization requires systematic optimization of both individual techniques and their integration. The fundamental methodological conflicts between these approaches necessitate specific protocol modifications, particularly RNase inhibition during IHC steps and antibody crosslinking before ISH procedures. Evidence-based troubleshooting of weak staining must address antibody validation, concentration optimization, and antigen retrieval efficiency, while reducing background requires meticulous attention to blocking conditions, antibody concentrations, and washing stringency. Scanner capabilities and imaging parameters further critically impact signal detection quality, particularly for automated analysis platforms. As spatial biology continues to evolve, these systematic approaches to signal optimization will enable more reliable, reproducible, and informative multi-omic investigations of tissue architecture and function.
In situ hybridization (ISH) and immunohistochemistry (IHC) represent cornerstone techniques in spatial biology, enabling researchers to localize nucleic acids and proteins within tissue architecture. The reliability of these techniques, particularly ISH, hinges critically on hybridization stringency—the set of conditions that determines the specificity of probe-target binding. In co-localization studies aimed at understanding complex biological relationships, such as the spatial correlation between complement C1q mRNA and specific cell types in mouse brain [75] or between EGFR RNA and phosphorylated EGFR protein in lung cancer [76], uncontrolled stringency can yield misleading results from non-specific binding or false negatives. Mastering stringency parameters—primarily temperature, salt concentration, and wash conditions—becomes paramount for generating reproducible, interpretable data that accurately reflects underlying biology.
This guide objectively compares the performance of different stringency approaches, providing experimental data and detailed methodologies to empower researchers in making informed decisions for their ISH and IHC co-localization studies.
The Science of Stringency: Principles and Parameters
Fundamental Principles of Hybridization Stringency
Stringency in molecular hybridization refers to the specificity with which a probe binds to its perfectly complementary target sequence versus mismatched sequences. The underlying principle revolves around the thermodynamic stability of nucleic acid duplexes, which is influenced by hydrogen bonding between base pairs and electrostatic repulsion between negatively charged phosphate backbones. Under low-stringency conditions, even imperfectly matched sequences (with one or more base mismatches) may remain hybridized, while high-stringency conditions ensure that only perfectly complementary sequences form stable hybrids, with mismatched sequences dissociating [77].
The stability of nucleic acid hybrids is governed by their melting temperature (Tm), defined as the temperature at which half of the DNA duplexes dissociate into single strands. The Tm depends on several factors including GC content, duplex length, and critically, the concentration of monovalent cations in the solution [78].
Key Parameters Controlling Stringency
Three primary parameters govern hybridization stringency, each with distinct mechanistic influences:
- Temperature: Higher temperatures disrupt hydrogen bonds between base pairs, particularly affecting mismatched hybrids which have fewer stabilizing interactions. Increasing temperature thereby increases stringency by selectively denaturing imperfect hybrids [77].
- Salt Concentration: Monovalent cations (such as Na⺠in SSC buffer) neutralize the negative charges on phosphate groups of nucleic acid backbones, reducing electrostatic repulsion between strands. Lower salt concentrations decrease this shielding effect, increasing repulsion and reducing hybrid stability, particularly for mismatched sequences [77] [79].
- Time: The duration of wash steps determines whether equilibrium conditions are reached. Sufficient time allows for the dissociation of weakly bound probes, but excessively long washes may risk dissociation of perfect matches.
These parameters interact in complex ways; for instance, formamide is often included in hybridization buffers to destabilize nucleic acid duplexes, allowing equivalent stringency to be achieved at lower temperatures that better preserve tissue morphology [78].
Comparative Analysis of Stringency Conditions
Systematic Comparison of Wash Buffer Conditions
Table 1: Comparison of Wash Buffer Conditions and Their Effects on Hybridization Stringency
| Condition | Salt Concentration | Temperature | Effect on Stringency | Best Applications |
|---|---|---|---|---|
| High Stringency | Low (0.1X-0.4X SSC) | High (72±1°C) | Allows detection of only perfectly matched hybrids | Detection of single-base mutations; highly homologous gene families |
| Moderate Stringency | Moderate (1X-2X SSC) | Intermediate (65-70°C) | Balances specificity and signal intensity | Routine detection of specific mRNA species |
| Low Stringency | High (2X-6X SSC) | Low (37-45°C) | Permits some mismatched hybrids | Cross-species hybridization; degenerate probes |
Experimental data from hematology FISH protocols indicates that specific wash conditions are optimized for different probe types: 0.4X SSC for 2 minutes at 72±1°C, followed by 2X SSC/0.05% Tween for 30 seconds at room temperature works optimally for most probes, while 0.25X SSC at the same temperature is recommended for enumeration probes [79]. The inclusion of TWEEN 20 detergent in wash buffers decreases background staining by reducing non-specific adhesion and enhances reagent spreading [79].
Performance Comparison of ISH Versus IHC Across Applications
Table 2: Technique Performance Comparison Across Biological Applications
| Application Context | Technique | Sensitivity | Specificity | Interobserver Agreement | Key Findings |
|---|---|---|---|---|---|
| SARS-CoV-2 Detection in Tissues [80] | RNA-ISH | 86.7% | 100% | Moderate to almost perfect | Superior specificity for viral RNA localization |
| SARS-CoV-2 Detection in Tissues [80] | IHC (Nucleocapsid) | 85.7% | 53.3% | Slight to moderate | Lower specificity due to potential cross-reactivity |
| CCND1 Rearrangement in Plasma Cell Myeloma [81] | FISH | Gold Standard | Gold Standard | Not specified | Requires high-quality samples and plasma cell purification |
| CCND1 Rearrangement in Plasma Cell Myeloma [81] | IHC (Cyclin D1) | 97% PPV* | 100% NPV | Not specified | Faster, more accessible alternative when validated |
| Complement C1q Localization [75] | Combined ISH/IH | Not specified | Not specified | Not specified | Identifies producing cells (ISH) and protein localization (IHC) |
PPV: Positive Predictive Value; *NPV: Negative Predictive Value*
The comparative study of SARS-CoV-2 detection demonstrated that while both RNA-ISH and IHC showed similar sensitivities (86.7% vs. 85.7%), RNA-ISH exhibited significantly higher specificity (100% vs. 53.3%) [80]. This performance advantage is critical for diagnostic applications and precise localization studies. Similarly, in plasma cell myeloma, cyclin D1 IHC showed excellent concordance with FISH for IGH::CCND1 fusion status, with positive and negative predictive values of 97% and 100% respectively in the testing cohort [81].
Experimental Protocols for Stringency Optimization
Standardized High-Stringency Wash Protocol for FISH
The following protocol, adapted from hematology FISH guidelines, provides a robust foundation for high-stringency applications [79]:
Post-Hybridization Washes:
- Prepare two Coplin jars with 0.4X SSC (pH 7.0-7.5) and pre-warm to 72±1°C in a water bath.
- Immediately following hybridization, immerse slides in the first 0.4X SSC bath for 2 minutes with gentle agitation.
- Transfer slides to the second 0.4X SSC bath for an additional 2 minutes at the same temperature.
- Remove slides and briefly tap to remove excess buffer.
Room Temperature Wash:
- Prepare a solution of 2X SSC with 0.05% TWEEN 20.
- Immerse slides for 30 seconds at room temperature with gentle agitation.
- Proceed to detection steps or counterstaining.
For enumeration probes, the protocol modification to 0.25X SSC at 72±1°C is recommended to enhance specificity [79]. The optimal pH should be maintained between 7.0-7.5, as deviations can affect the availability of positive ions and thus hybrid stability.
Combined ISH/IHC Co-Localization Protocol
For simultaneous detection of RNA and protein in the same tissue section, as employed in complement C1q and EGFR localization studies [75] [76]:
Tissue Preparation:
- Prepare free-floating vibratome sections (40-100μm) or formalin-fixed paraffin-embedded (FFPE) sections.
- For FFPE tissues, perform deparaffinization and rehydration through xylene and graded ethanol series.
Proteinase K Digestion Optimization (Critical for ISH):
- Titrate Proteinase K concentration (typically 1-5 μg/mL) in a time course experiment.
- Incubate sections for 10 minutes at room temperature.
- Determine optimal concentration that maximizes signal while preserving morphology [78].
In Situ Hybridization:
- Apply labeled probes (DNA, RNA, or oligonucleotide-based) in hybridization buffer.
- Hybridize at optimized temperature (37-65°C) for 2-16 hours depending on probe.
- Perform stringency washes as described in Section 4.1.
Immunohistochemistry:
Mounting and Visualization:
- Dehydrate through graded ethanols, clear in xylene, and mount with permanent mounting medium.
- For fluorescent detection, use anti-fade mounting medium.
Advanced Applications and Emerging Technologies
High-Throughput and Automated Approaches
Recent advances have enabled automation of ISH protocols, dramatically increasing throughput while maintaining specificity. The development of high-throughput hybridization chain reaction (HT-HCR) for sea urchin embryos demonstrates the scalability of ISH, processing 192 gene probe sets within 32 hours using 96-well plate formats and robotic liquid handlers [82]. This automated approach maintains the essential stringency controls while standardizing conditions across large sample sets, enabling spatial expression profiling at unprecedented scale.
For mRNA delivery and siRNA knockdown studies in primary hepatocytes, optimized high-throughput transfection protocols leverage the principles of nucleic acid hybridization under controlled stringency conditions, facilitating large-scale screening of gene modulation effects [83].
Integrated Co-Detection Workflows
The integration of ISH with IHC in Integrated Co-Detection Workflow (ICW) protocols represents a powerful approach for spatial biology. In lung cancer research, this has enabled simultaneous detection of EGFR RNA and phosphorylated EGFR protein at single-cell resolution [76]. Such co-detection reveals not only which cells express a particular gene, but also how protein activation states correlate with gene expression patterns—revealing complex regulatory relationships that would be obscured when techniques are applied separately.
Similarly, in neuroscience applications, combined ISH/IH has elucidated the relationship between complement-producing cells and their targets in mouse brain, revealing that C1q immunostaining alone does not necessarily identify sites of complement production, which can be precisely localized using C1q mRNA detection [75].
Essential Reagents and Research Solutions
Table 3: Research Reagent Solutions for Hybridization Stringency Optimization
| Reagent/Category | Specific Examples | Function in Stringency Control | Technical Notes |
|---|---|---|---|
| Salt Solutions | SSC Buffer (20X, 2X, 0.4X, 0.25X) | Controls ionic strength; lower concentration increases stringency | pH critical (7.0-7.5); prepare fresh periodically |
| Detergents | TWEEN 20 | Reduces background; enhances buffer spreading | Use at 0.05% in final wash buffers [79] |
| Proteinase K | Molecular biology grade | Digests proteins obscuring target access; requires optimization | Titrate (1-5 μg/mL) to balance signal and morphology [78] |
| Formamide | Molecular biology grade | Denaturant allowing lower hybridization temperatures | Reduces melting temperature; preserves morphology |
| Probe Types | Double-stranded DNA, Riboprobes, LNA probes | RNA probes form more stable hybrids; LNA enhances affinity | RNA-RNA hybrids > RNA-DNA > DNA-DNA hybrids [78] |
| Detection Labels | Biotin, Digoxigenin, Fluorescent dyes | Direct vs indirect detection; digoxigenin reduces background | Endogenous biotin may require blocking [78] |
Mastering hybridization stringency through precise control of temperature, time, and wash conditions remains fundamental to generating reliable ISH and IHC co-localization data. The comparative data presented in this guide demonstrates that high-stringency conditions (elevated temperature with reduced salt concentration) consistently outperform alternatives for specific detection of perfectly matched hybrids [77] [79]. The integration of these principles into standardized protocols, whether for manual FISH or automated high-throughput HCR platforms, ensures reproducibility and accuracy in spatial localization studies.
For researchers embarking on co-localization studies, the strategic implementation of stringency controls should be prioritized from experimental design through data interpretation. As spatial biology continues to evolve with increasingly multiplexed approaches, the fundamental principles of hybridization stringency will remain essential for distinguishing true biological signals from technical artifacts, ultimately advancing our understanding of complex biological systems at the molecular level.
In the realm of histopathology and molecular tissue research, particularly for immunohistochemistry (IHC) and in situ hybridization (ISH) co-localization studies, fixation serves as the foundational step that determines the success of all subsequent analyses. Fixation permanently preserves tissue architecture and cellular morphology while stabilizing biomolecules for detection. Among fixatives, formalin-based solutions remain the most prevalent, yet confusion often arises between the specific applications of 10% Neutral Buffered Formalin (NBF) and 4% Paraformaldehyde (PFA). While both are formaldehyde-based fixatives, they are not identical and exhibit critical differences that impact morphological preservation and experimental outcomes. This guide provides an objective comparison of these fixatives, supported by experimental data, to inform researchers and drug development professionals in selecting the optimal fixation strategy for studies where preserving tissue context is paramount.
Chemical Foundations: Unraveling the Formalin and PFA Composition
Understanding the distinct chemical properties of these fixatives is crucial for predicting their performance in experimental protocols.
Paraformaldehyde (PFA): Paraformaldehyde is a polymerized solid form of formaldehyde [84]. To create a usable fixative, this white powder must be depolymerized in hot buffer (typically phosphate-buffered saline, PBS) to create a 4% formaldehyde solution. The resulting 4% PFA solution is methanol-free and highly pure, making it particularly suited for cell fixation and perfusion due to its rapid action and minimal introduction of artifactual precipitates [85] [84].
Formalin: Formalin is a saturated aqueous solution of formaldehyde gas, historically containing 10-15% methanol as a stabilizer to prevent polymerization [85] [84]. The most common variant in histopathology is 10% Neutral Buffered Formalin (NBF), which is prepared by diluting stock formalin (approximately 37-40% formaldehyde) 1:10 with buffer. This results in an actual formaldehyde concentration of approximately 4% [85] [86]. The buffering agent, often phosphate, is critical as it prevents the formation of formalin pigment (acid formaldehyde hematein) and maintains a stable pH for optimal fixation [86].
Core Fixation Mechanism: Both PFA and formalin function primarily as cross-linking fixatives. The formaldehyde molecules form reversible methylene bridges (-CH2-) between amino groups and other reactive sites on adjacent proteins and nucleic acids [85]. This cross-linking network stabilizes cellular structures and protects tissue integrity against subsequent processing and staining steps.
Direct Comparative Analysis: Morphology, RNA, and IHC Performance
The following data, synthesized from controlled studies, highlights how the nuanced differences between fixatives translate to tangible experimental outcomes.
Table 1: Comparative Performance of Common Fixatives in Key Applications
| Performance Metric | 10% NBF (4% Formaldehyde) | 4% PFA | 99% Ethanol |
|---|---|---|---|
| Tissue Morphology | Excellent nuclear and cytoplasmic detail [87] [88] | High quality, comparable to NBF [87] | Poor, causes significant cell contraction and shrinkage [87] [88] |
| RNA Preservation Quality | High-quality RNA suitable for qRT-PCR [87] | High-quality RNA suitable for qRT-PCR [87] | Degraded/Damaged RNA [87] |
| IHC Staining Intensity | Good, but may require antigen retrieval [88] | Good, but may require antigen retrieval | Variable; decreased Ki-67 & VEGF-A, improved cytokeratin [87] |
| Background Staining | Can be more prominent, requires optimization [88] | Similar to NBF | Generally lower background in some protocols [88] |
A study comparing xenograft tumor tissues demonstrated that while RNA from PFA- and NBF-fixed tissues was of high quality, ethanol-fixed tissues showed significant RNA degradation [87]. Furthermore, immunohistochemical results were highly dependent on the fixation method and the specific antibody used. For instance, 99% ethanol fixation led to decreased immunoreactivity for Ki-67 and VEGF-A but improved staining for cytokeratin [87]. This underscores the necessity of matching the fixative to the specific target antigen.
Table 2: Impact of Alcohol-Based vs. Formalin-Based Fixation on IHC [88]
| Parameter | 10% NBF | Alcohol-Based Fixative |
|---|---|---|
| Nuclear Detail (Score 0-3) | 2.7 ± 0.3 | 2.3 ± 0.4 |
| Tissue Shrinkage (Score 0-3) | 1.1 ± 0.3 | 2.0 ± 0.4 |
| Cytokeratin Staining (3+ Intensity) | 63.3% | 86.6% |
| CD3 Staining (3+ Intensity) | 66.6% | 83.3% |
| Prominent Background Staining | 36.7% | 13.3% |
Recent comparative evaluations confirm that while formalin fixation provides superior morphological preservation, alcohol-based fixatives can offer enhanced antigenicity and stronger IHC staining intensity for many markers, along with reduced background staining [88]. This presents a practical trade-off: form-aldehyde-based fixatives (NBF/PFA) for superior morphology, and alcohol-based fixatives for certain challenging IHC targets, albeit with potential tissue shrinkage.
Optimized Experimental Protocols for Reliable Fixation
Protocol 1: Preparation of 4% Paraformaldehyde (PFA) in PBS
For consistent and high-quality IHC/ISH results, especially in sensitive co-localization studies, fresh preparation of PFA is often recommended [84].
Procedure:
- In a ventilated fume hood, add 800 mL of 1X PBS to a glass beaker on a stir plate. Heat while stirring to approximately 60°C. Caution: Avoid boiling [84].
- Add 40 g of paraformaldehyde powder to the heated PBS. The powder will not dissolve immediately [84].
- Slowly raise the pH by adding 1 N NaOH dropwise from a pipette until the solution becomes clear [84].
- Once dissolved, cool the solution. Filter it if necessary.
- Adjust the final volume to 1 L with 1X PBS. Check the pH and adjust it to approximately 6.9 using dilute HCl [84].
- The solution can be aliquoted and stored at 2-8°C for up to one month [84].
Protocol 2: Standard Tissue Fixation and Processing for Morphology
A standardized fixation protocol is vital for comparative studies. The following workflow ensures consistency across samples.
Critical Steps and Parameters:
- Rapid Fixation: To prevent ischemic degradation and autolysis, place tissues into fixative immediately after dissection. For IHC targets like Ki-67 and phosphoproteins, rapid fixation is especially critical as they are highly vulnerable to ischemia [89].
- Fixation Duration and Ratio: Immersion fixation in 10% NBF or 4% PFA for 24 hours at room temperature is a standard recommendation [89] [86]. Maintain a tissue-to-fixative volume ratio between 1:10 and 1:20 to ensure adequate penetration [89].
- Sectioning: For optimal morphology and IHC/ISH, section paraffin-embedded tissues at a thickness of 3-5 µm [89].
The Scientist's Toolkit: Essential Reagents for Fixation and Analysis
Table 3: Key Research Reagents and Materials for Fixation and Staining
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Paraformaldehyde (PFA) Powder | Primary component for making pure, methanol-free formaldehyde fixative [84]. | Must be depolymerized in hot buffer for use [84]. |
| 10% Neutral Buffered Formalin (NBF) | Gold standard for routine histopathology and morphological preservation [86]. | Ready-to-use; contains stabilizers; actual formaldehyde concentration is ~4% [85]. |
| Citrate Buffer (pH 6.0) | Common buffer for heat-induced epitope retrieval (HIER) for IHC on FFPE tissue [89]. | Unmasks antigenic sites cross-linked by formalin fixation [89]. |
| Proteinase K | Enzyme used for digesting proteins during RNA extraction from FFPE tissues [87]. | Critical for recovering nucleic acids from cross-linked samples [87]. |
| DAB (3,3'-Diaminobenzidine) | Chromogen for chromogenic IHC detection; produces a brown, insoluble precipitate [89] [90]. | Yields a permanent stain; resistant to fading [90] [91]. |
| Hematoxylin | Standard nuclear counterstain for both H&E and IHC [89]. | Provides contrast by staining nuclei blue [89]. |
The choice between formalin and PFA is not a matter of one being universally superior, but rather which is optimal for a specific research context. 10% Neutral Buffered Formalin remains the undisputed gold standard for general histopathology where superior and consistent morphological detail is the primary objective, and its compatibility with automated processors and established IHC protocols makes it a workhorse for clinical and research laboratories.
4% PFA, prepared fresh from powder, is often the preferred choice for sensitive molecular studies, cell fixation, and perfusion due to its high purity and absence of stabilizers like methanol that can introduce artifacts. For advanced IHC and ISH co-localization studies, where the integrity of both protein epitopes and nucleic acids is paramount, PFA can provide a slight edge. However, this must be balanced against the practical convenience and standardization of commercial NBF.
Ultimately, researchers must weigh the trade-offs between perfect morphology, optimal antigenicity, and practical workflow. The most reliable approach is to empirically validate the fixation protocol for each specific antigen-antibody pair and tissue type, using the guidelines and data presented here as a foundational starting point.
Multiplex immunohistochemistry (mIHC) and immunofluorescence (mIF) have revolutionized the study of complex biological systems by enabling the simultaneous detection of multiple biomarkers on a single tissue section. These techniques provide unprecedented insights into cellular heterogeneity, cell-cell interactions, and the spatial organization of tissues, particularly in cancer and immunology research. However, as researchers push the boundaries of multiplexing to detect more targets simultaneously, they face significant technical challenges related to cross-reactivity and signal bleed-through. These artifacts can compromise data integrity, leading to false positives and inaccurate biological interpretations. This guide examines the core challenges in multiplex imaging and objectively compares the performance of various solutions, providing researchers with practical experimental frameworks to achieve reliable, high-plex spatial data.
Understanding the Core Challenges
The pursuit of higher-plex imaging inevitably introduces technical artifacts that can obscure true biological signals if not properly managed. Cross-reactivity occurs when antibodies non-specifically bind to off-target antigens or when secondary detection reagents recognize multiple primary antibodies. This challenge becomes increasingly complex as more antibodies are incorporated into a panel. Spectral overlap, or bleed-through, happens when the emission spectrum of one fluorophore is detected in the channel assigned to another fluorophore due to broad emission profiles of organic fluorophores. The accuracy of subsequent spatial analysis, including cell phenotyping and interaction studies, is fundamentally dependent on overcoming these challenges [92] [93].
The foundation of reliable multiplexing lies in understanding the signal-to-noise ratio for each antibody-epitope pair under specific experimental conditions. Factors including tissue fixation methods, antigen retrieval efficiency, antibody clone specificity, and fluorophore brightness collectively influence this ratio. Furthermore, the spatial context of the target antigens—whether they are expressed in the same cellular compartments or distinct cell types—affects the approach required for accurate unmixing and interpretation [7] [92].
Comparative Analysis of Multiplexing Platforms
Multiple technological platforms have been developed to address multiplexing challenges, each with distinct mechanisms for signal discrimination and varying capacities for target multiplexing. The table below provides a performance comparison of major platforms based on key parameters relevant to cross-reactivity and bleed-through management.
Table 1: Performance Comparison of Multiplex Imaging Platforms
| Technology | Multiplexing Capacity | Primary Challenge Addressed | Signal Discrimination Mechanism | Spatial Resolution | Required Instrumentation |
|---|---|---|---|---|---|
| Chromogenic mIHC | 3-5 targets | Color separation | Enzyme-mediated precipitation of chromogens with distinct colors | High | Standard brightfield microscope |
| Fluorescent mIF | 4-8 targets (per round) | Spectral overlap | Emission wavelength filtering and spectral unmixing | High | Fluorescence microscope with filter sets |
| Tyramide Signal Amplification (TSA) | 5-10+ targets (with cycling) | Signal sensitivity | Enzyme-mediated covalent deposition of fluorophores | Very High | Standard fluorescence microscope |
| Mass Cytometry (IMC/MIBI) | 40+ targets | Spectral overlap | Metal isotope tags detected by mass spectrometry | Medium-High | Specialized mass spectrometry imaging |
| DNA Barcoding (CODEX/etc.) | 50+ targets | Antibody cross-reactivity | Oligonucleotide-conjugated antibodies with sequential hybridization | High | Fluorescence microscope with hybridization system |
| PICASSO | 15+ targets (single round) | Spectral overlap without reference | Computational mutual information minimization | High | Standard fluorescence microscope |
Analysis of Platform Performance Characteristics
Fluorescence-based platforms face inherent spectral overlap challenges but offer excellent spatial resolution and relatively accessible instrumentation. The Tyramide Signal Amplification (TSA) system provides exceptional sensitivity through enzymatic amplification, enabling detection of low-abundance targets. However, TSA requires careful optimization of deposition time to prevent over-amplification that can obscure morphology or cause off-target deposition [92]. TSA achieves approximately 100-fold signal amplification compared to conventional immunofluorescence, making it particularly valuable for detecting low-abundance targets. The covalent nature of tyramide deposition allows for antibody stripping between cycles, enabling higher multiplexing without host species limitations [92].
Mass spectrometry-based platforms like Imaging Mass Cytometry (IMC) and Multiplexed Ion Beam Imaging (MIBI) fundamentally avoid spectral overlap by using metal-tagged antibodies detected by mass spectrometry rather than optical emission. This allows for highly multiplexed panels of 40+ markers with minimal signal interference. However, these technologies require specialized instrumentation and offer lower spatial resolution than optical methods, typically around 1μm [94].
DNA barcoding approaches such as CODEX and Digital Spatial Profiling transform the challenge of spectral separation into one of DNA sequence recognition. By conjugating antibodies with unique oligonucleotide barcodes and using sequential hybridization with fluorescent reporters, these systems can achieve extremely high multiplexing (50-60 markers) while using standard fluorophores. The primary challenges include managing hybridization efficiency and tissue integrity over multiple cycles [94].
Experimental Protocols for Artifact Reduction
Antibody Panel Validation Protocol
Robust multiplexing requires rigorous antibody validation through a systematic protocol:
Singleplex Validation: Test each antibody individually on control tissues to confirm specificity, optimal dilution, and subcellular localization. Include positive and negative control tissues to establish staining patterns [92].
Cross-reactivity Assessment: Use isotype controls and antibody "drop-out" experiments to identify non-specific binding. For secondary detection systems, verify species specificity by testing each secondary antibody against all primaries in the panel [7].
Titration Matrix Testing: Perform checkerboard titrations of antibody pairs that may exhibit cross-reactivity or target co-localization to determine optimal concentrations that minimize off-target binding while preserving signal [92].
Signal Specificity Confirmation: For highly multiplexed panels, validate with genetic knockout tissues or siRNA knockdown controls where possible to confirm target specificity [92].
This validation process typically requires 2-3 weeks for a 5-10 antibody panel but is essential for generating reliable data. Comprehensive validation can reduce false positives by up to 80% compared to unvalidated antibody panels [92].
Spectral Unmixing Workflow for Fluorescent Multiplexing
For fluorescent multiplexing, accurate spectral unmixing is essential to address bleed-through. The following protocol outlines a robust approach:
Reference Spectra Acquisition: Capture emission spectra from single-fluorophore-stained control tissues identical to experimental samples. For heterogeneous tissues, collect reference spectra from multiple regions to account for microenvironmental effects on fluorophore emission [93].
Linear Unmixing Implementation: Apply the linear mixing equation:
IMG = M × F, where IMG represents acquired mixed images, F represents unmixed images, and M is the mixing matrix derived from reference spectra. This mathematically separates overlapping signals based on their spectral signatures [93].Validation with Control Samples: Verify unmixing accuracy using test samples with known staining patterns, including samples with single fluorophores and defined mixtures.
Algorithm Selection: Choose unmixing algorithms based on experimental needs—traditional linear unmixing for well-characterized systems, or blind unmixing approaches like PICASSO for heterogeneous tissues where reference spectra are difficult to obtain [93].
Advanced computational approaches like PICASSO (Process of ultra-multiplexed Imaging of biomoleCules viA the unmixing of the Signals of Spectrally Overlapping fluorophores) enable robust unmixing without reference spectra by iteratively minimizing mutual information between channels. This approach has demonstrated >99% unmixing accuracy even for spatially overlapping proteins in complex tissues like the brain [93].
Spectral Unmixing Decision Workflow: A flowchart guiding researchers through the process of selecting and implementing appropriate spectral unmixing methods based on experimental conditions and available reference data.
The Scientist's Toolkit: Essential Reagents and Materials
Successful multiplexing requires careful selection of reagents and materials optimized for high-plex applications. The following table catalogs essential solutions for robust multiplex experiments.
Table 2: Essential Research Reagent Solutions for Multiplex Imaging
| Reagent Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Validated Primary Antibodies | Recombinant monoclonal antibodies | Target recognition with high specificity | Lot-to-lot consistency; recommend recombinant clones for reproducibility |
| Signal Amplification Systems | Tyramide Signal Amplification (TSA) kits | Signal enhancement for low-abundance targets | Requires optimization of deposition time to prevent over-amplification |
| Fluorophore Conjugates | Alexa Fluor series, Cy dyes | Signal generation | Brightness, photostability, and spectral overlap characteristics |
| Antibody Stripping Reagents | Acid-based eluents, high-temperature buffer | Antibody removal for cyclic staining | Must completely remove antibodies without damaging tissue antigenicity |
| Tissue Clearing Agents | Organic solvent-based, hydrogel-based | Reduce light scattering in thick samples | Compatibility with fluorophores and antigen preservation |
| Autofluorescence Quenchers | Sudan Black B, TrueBlack Lipofluor | Reduce tissue autofluorescence | Treatment time must be optimized for different tissue types |
| Mounting Media | Anti-fade mounting media | Preserve fluorescence during imaging | Curing time and refractive index matching for optimal resolution |
Advanced Framework for Spatial Validation
As multiplexing capacity increases, so does the need for robust spatial validation frameworks. The colocatome analysis framework provides a quantitative approach for validating spatial relationships across samples and conditions. This method combines pairwise cell-cell colocalization metrics with spatial permutation testing to establish significance thresholds for observed spatial patterns [95].
The core of this approach uses the colocation quotient (CLQ) spatial metric, which identifies cell subpopulation pairs in close proximity (positive colocalization) versus those that are distant (negative colocalization). By applying spatial randomization, researchers can assess whether observed colocalizations occur more frequently than chance, with p-values determined through permutation testing. This rigorous statistical framework is particularly valuable for comparing spatial features between model systems (e.g., organoids) and human tissue samples [95].
Implementation of this validation framework involves:
- Image Acquisition using multiplex platforms (PhenoCycler, CODEX, or IMC)
- Cell Segmentation and Phenotyping using tools like CELESTA
- Spatial Metric Calculation (CLQ for all cell-type pairs)
- Significance Assessment through spatial permutation
- Cross-Sample Comparison using normalized colocalization scores
This approach has demonstrated utility in validating that patient-derived assembloids recapitulate human tumor spatial organization, enabling more physiologically relevant drug perturbation studies [95].
Spatial Validation Framework: A structured approach for quantitatively validating spatial relationships in multiplex imaging data using colocatome analysis and statistical testing.
Multiplex immunohistochemistry and immunofluorescence represent powerful tools for spatial biology, but their effective implementation requires careful management of cross-reactivity and signal bleed-through. No single platform universally addresses all multiplexing challenges; rather, researchers must select technologies based on their specific experimental needs, instrumentation access, and required multiplexing capacity. Fluorescence-based methods with spectral unmixing offer accessibility and good resolution, while mass cytometry and DNA barcoding approaches provide higher plex capacity at the cost of more specialized equipment and complex workflows.
The key to success lies in rigorous experimental design, comprehensive antibody validation, appropriate application of spectral unmixing techniques, and implementation of quantitative spatial validation frameworks. As the field advances, integration of machine learning approaches and standardized validation pipelines will further enhance the reliability and reproducibility of multiplex imaging data, enabling more profound insights into complex biological systems in health and disease.
Ensuring Clinical and Analytical Rigor: Validation Frameworks and Method Comparison
Clinical Validation vs. Indirect Clinical Validation for Predictive Biomarkers
In the era of precision medicine, predictive biomarkers are indispensable tools that guide treatment decisions by identifying patients most likely to respond to specific therapies. For researchers and drug development professionals, particularly those utilizing in situ hybridization (ISH) and immunohistochemistry (IHC) co-localization studies, understanding the distinct pathways for validating these biomarkers is critical. Validation ensures that a biomarker assay is not only analytically sound but also clinically meaningful. The two cornerstone processes in this endeavor are clinical validation and indirect clinical validation. Clinical validation demonstrates a biomarker's ability to accurately predict clinical outcomes, such as response to therapy or survival, within the context of a clinical trial. In contrast, indirect clinical validation provides a necessary pathway for Laboratory Developed Tests (LDTs) to establish clinical utility when repeating clinical trials is unfeasible, by showing diagnostic equivalence to a clinically validated reference assay [96]. This guide objectively compares these two validation frameworks, providing the experimental data and protocols essential for robust biomarker implementation in research and clinical development.
Core Concepts and Definitions
What is Clinical Validation?
Clinical validation is the process of confirming, through the provision of objective evidence, that a predictive biomarker reliably stratifies patients based on their expected response to a specific therapeutic intervention within a defined clinical population. According to ISO 9000 definitions, validation hinges on three components: confirmation (level of certainty), objective evidence (test performance characteristics), and intended use (fit-for-purpose) [96]. In practice, clinical validation occurs within prospective clinical trials where the biomarker's performance is directly linked to patient outcomes, such as overall survival or progression-free survival. This process is mandatory for regulatory approval of companion diagnostics (CDx) and establishes the "gold standard" for that biomarker-therapy relationship.
What is Indirect Clinical Validation?
Indirect clinical validation (ICV) is a method used to establish the clinical relevance of a Laboratory Developed Test (LDT) when direct clinical validation in a new trial is not available or feasible. The purpose of ICV is not to re-establish the clinical utility of the biomarker itself—which is already proven—but to provide evidence that the new LDT assay is diagnostically equivalent to a previously clinically validated assay, usually a CDx [96]. This process is crucial for laboratories that modify a CDx assay or develop an LDT, as any modification automatically transforms a CDx into an LDT requiring ICV [96]. The need for ICV is increasingly emphasized by regulatory frameworks like the FDA regulations and the European In Vitro Diagnostic Regulation (IVDR).
The Relationship in the Biomarker Development Workflow
The following diagram illustrates how these validation processes fit into the overall timeline of biomarker and assay development, from research to clinical application:
Comparative Analysis: Clinical Validation vs. Indirect Clinical Validation
A direct comparison of these validation approaches is essential for selecting the appropriate pathway. The table below summarizes the key differentiating factors.
Table 1: Key Differences Between Clinical Validation and Indirect Clinical Validation
| Feature | Clinical Validation | Indirect Clinical Validation |
|---|---|---|
| Definition | Confirmation that a biomarker predicts clinical outcomes in a specific patient population [96]. | Demonstration that an LDT is diagnostically equivalent to a clinically validated reference assay [96]. |
| Primary Objective | Establish a new biomarker-clinical outcome link. | Verify performance equivalence of an alternative assay for a known biomarker. |
| Typical Context | Prospective clinical trials for drug and CDx co-development [96]. | Transfer of a validated biomarker to an LDT in a clinical laboratory [96]. |
| Data Source | Clinical outcomes from patients in a trial [96]. | Comparative assay results from patient samples [96]. |
| Regulatory Role | Mandatory for CDx and drug approval. | Required for LDTs, especially under FDA and IVDR [96]. |
| Cost & Complexity | High (requires running a clinical trial). | Lower (requires a well-designed comparative study). |
A Conceptual Framework for Indirect Clinical Validation
The strategy for indirect clinical validation is not one-size-fits-all; it depends fundamentally on the biological and clinical characteristics of the biomarker. Expert consensus guidance recommends categorizing predictive biomarkers into distinct Indirect Clinical Validation (ICV) Groups to determine the appropriate validation pathway [96].
ICV Group 1: Specific Biological Event Biomarkers
This group includes biomarkers that detect a specific, often binary, biological event that triggers oncogenesis, such as gene fusions (e.g., ALK, NTRK) or gene amplification (e.g., HER2) [96]. These events are typically characterized by minimal tumor heterogeneity.
- Goal of ICV: The purpose is to provide evidence that the LDT is highly accurate in detecting the specific biological event itself. The focus is on analytical accuracy against a reference method [96].
ICV Group 2: Biomarkers with Clinical Cut-offs
This group includes biomarkers where not just the presence, but the level of expression relative to a clinically validated cut-off determines a "positive" or "negative" result. Examples include PD-L1 (using Tumor Proportion Score or Combined Positive Score), tumor mutation burden, and c-MET protein overexpression [96]. These often exhibit tumor heterogeneity.
- Goal of ICV: The purpose is to demonstrate diagnostic equivalence to the gold-standard assay. The LDT must stratify patients into "positive" and "negative" categories in high concordance with the comparator CDx assay [96].
ICV Group 3: Technical Screening Assays
This group consists of assays developed to efficiently screen out patients with a very low probability of being positive, thereby reducing the cost and turnaround time of testing. An example is pan-TRK IHC used as a screen before definitive NTRK fusion testing [96].
- Goal of ICV: Similar to Group 2, this requires diagnostic validation. The accuracy of the screening assay must be compared to the definitive biomarker assay to ensure a high negative predictive value [96].
The following diagram visualizes this decision-making framework for indirect clinical validation:
Case Study: Validation of ALK Testing in NSCLC
The evolution of ALK rearrangement testing in non-small cell lung cancer (NSCLC) provides a powerful real-world example of these validation pathways in action, involving IHC and ISH methodologies.
Experimental Protocol and Comparative Data
A seminal 2015 study systematically compared Fluorescence In Situ Hybridization (FISH—the FDA-approved standard), IHC (with D5F3 antibody), and Next-Generation Sequencing (NGS) in 51 lung adenocarcinoma patients [51].
- IHC Protocol: Staining was performed on a Ventana BenchMark XT autostainer using the D5F3 antibody. Antigen retrieval used standard cell conditioning. The result was reported as an H-score (0-300), with a cutoff of ≥40 defined as positive to minimize background effects [51].
- FISH Protocol: The Vysis ALK Break Apart FISH Probe Kit was used on formalin-fixed paraffin-embedded (FFPE) specimens. A minimum of 50 non-overlapping nuclei were analyzed according to manufacturer's guidelines [51].
- NGS Protocol: Discordant cases were resolved using the FoundationOne NGS assay on the Illumina HiSeq 2000 platform, which served as an arbiter of truth [51].
The quantitative results from this comparative study are summarized below.
Table 2: Comparative Performance of FISH and IHC for ALK Rearrangement Detection (N=51) [51]
| Method | Positive Cases (n) | Sensitivity (vs. NGS) | Specificity (vs. NGS) | Key Finding |
|---|---|---|---|---|
| FISH (CDx) | 4 (7.8%) | 42.9% | 97.7% | Missed over half of the true positive cases. |
| IHC (LDT) | 8 (15.7%) | 100% | 97.7% | Identified all true positive cases, including FISH-negative ones. |
| NGS (Arbiter) | 7 (13.7%) | - | - | Confirmed IHC-positive/FISH-negative patients responded to Crizotinib. |
Interpretation and Impact
This study underscores a critical point: the method approved via clinical validation (FISH) was found to have low sensitivity, potentially denying effective therapy to a significant number of patients. The IHC LDT, through a rigorous indirect clinical validation process using NGS as a reference, demonstrated superior sensitivity while maintaining high specificity [51]. This evidence has been instrumental in leading to broader acceptance of IHC as a primary screening tool for ALK rearrangements, demonstrating how robust ICV can refine and improve clinical practice.
Essential Reagents and Research Tools
Success in both clinical and indirect clinical validation, especially in IHC and ISH co-localization studies, depends on carefully selected and validated reagents.
Table 3: Research Reagent Solutions for Biomarker Validation
| Reagent / Solution | Critical Function in Validation | Key Considerations |
|---|---|---|
| Primary Antibodies (e.g., D5F3 for ALK) [51] | Binds specifically to the target protein antigen for detection. | Clone specificity, species (monoclonal vs. polyclonal), vendor validation, and concentration are critical for reproducibility [97] [98]. |
| ISH Probes (e.g., Break-apart FISH probes) [51] | Labels specific DNA or RNA sequences for in situ detection. | Probe design, labeling efficiency, and specificity must be validated for each assay platform. |
| Antigen Retrieval Buffers | Unmasks epitopes cross-linked by formalin fixation, enabling antibody binding [97]. | The pH (acidic vs. basic) and method (Heat-Induced Epitope Retrieval) must be optimized for each antibody [97]. |
| Detection Kits (e.g., UltraView DAB) [51] | Amplifies the primary antibody signal for visualization. | Chromogenic (DAB) or fluorescent kits must be selected based on the platform and required sensitivity. |
| Control Cell Lines & Tissues | Serves as positive and negative controls for assay performance [97]. | Use of CAP-validated FFPE samples or cell lines with known expression (e.g., H2228 for ALK) is essential [51] [97]. |
| Tissue Microarrays (TMAs) | Enable high-throughput validation of antibody performance across multiple tissue types in a single experiment [97]. | Ideal for pre-clinical prevalence studies and initial assay optimization. |
Clinical validation and indirect clinical validation are complementary yet distinct processes in the ecosystem of predictive biomarker development. Clinical validation is the foundational process that establishes a biomarker's clinical utility through a direct link to patient outcomes in a trial. Indirect clinical validation, guided by a fit-for-purpose framework of ICV Groups, provides a rigorous and practical pathway for clinical laboratories to implement reliable LDTs, ensuring that patients receive the benefits of precision medicine regardless of the testing platform used. The case of ALK testing in NSCLC demonstrates that a well-executed ICV can not only verify equivalence but can also reveal limitations of the original clinically validated assay, ultimately driving progress in the field. For scientists engaged in IHC and ISH co-localization research, adhering to these validation principles and using highly characterized reagents is paramount for generating trustworthy data that can successfully transition from the research bench to clinical application.
In the evolving landscape of personalized medicine, Companion Diagnostics (CDx) and Laboratory Developed Tests (LDTs) serve distinct yet complementary roles. A Companion Diagnostic is a medical device, often an in vitro diagnostic (IVD), that provides information essential for the safe and effective use of a corresponding drug or biological product [99]. These tests identify patients most likely to benefit from a particular therapeutic, identify those at increased risk for serious side effects, or monitor response to treatment. In contrast, a Laboratory Developed Test (LDT) is a type of diagnostic test designed, manufactured, and used within a single laboratory [100] [101]. LDTs are developed by individual laboratories to meet specific clinical needs, expand services, or support specialized clinical applications not addressed by commercially available tests.
The regulatory frameworks governing these tests differ significantly. CDxes undergo comprehensive FDA premarket review as medical devices, requiring demonstration of safety and effectiveness for their intended use with specific therapeutic products [99] [102]. Conversely, LDTs have historically been regulated under the Clinical Laboratory Improvement Amendments (CLIA) through the Centers for Medicare & Medicaid Services, with a primary focus on laboratory quality standards rather than pre-market test approval [100] [103]. This article compares these test types within the specific context of ISH and immunohistochemistry co-localization studies, providing researchers with guidance for navigating their respective applications in drug development and clinical research.
Comparative Analysis: CDx vs. LDTs
Key Characteristics and Regulatory Pathways
Table 1: Fundamental Characteristics of CDx and LDTs
| Characteristic | Companion Diagnostic (CDx) | Laboratory Developed Test (LDT) |
|---|---|---|
| Definition | IVD that provides information essential for safe/effective use of corresponding therapeutic product [99] | Test designed, manufactured, and used within a single laboratory [100] [101] |
| Primary Regulator | U.S. Food and Drug Administration (FDA) [99] | Centers for Medicare & Medicaid Services (under CLIA) [100] [103] |
| Premarket Review | Required (Premarket Approval [PMA], 510(k), or De Novo classification) [99] [102] | Not required under current enforcement discretion; laboratories self-validate [103] |
| Intended Use | Specifically linked to therapeutic product use [99] | Determined by developing laboratory; often for specialized needs [100] |
| Geographic Availability | Can be distributed to multiple laboratories [100] | Limited to developing laboratory [101] |
| Labeling | Must reference corresponding therapeutic; typically describes specific group of oncology therapeutics rather than single brand name [99] [102] | No therapeutic product claims; must include disclosure that test not cleared/approved by FDA when using ASRs [103] |
Performance Comparison in Molecular Oncology
A comprehensive study analyzing 6,897 proficiency testing (PT) responses for three oncology biomarkers (BRAF, EGFR, and KRAS) provides insightful performance data between LDTs and FDA-approved companion diagnostics [104].
Table 2: Analytical Performance Comparison from Proficiency Testing (n=6,897 responses)
| Gene | Test Type | Overall Acceptability Rate | Variant-Specific Performance Differences |
|---|---|---|---|
| BRAF | FDA-CD | 93.0% | p.V600K: 66.1% acceptable |
| LDT | 96.6% | p.V600K: 88.0% acceptable | |
| EGFR | FDA-CD | 99.1% | p.L861Q: 100% acceptable |
| LDT | 97.6% | p.L861Q: 90.7% acceptable | |
| KRAS | FDA-CD | 98.8% | No significant variant-specific differences |
| LDT | 97.4% | No significant variant-specific differences | |
| All Genes Combined | Both | >97% accuracy | Rare variant-specific differences not consistently favoring either test type [104] |
This study revealed that more than 60% of laboratories using FDA-CDs reported adapting their assays from the approved procedure to accommodate broader sample types, lower tumor content, or different instrumentation, effectively rendering them LDTs [104]. This modification practice highlights the dynamic relationship between these test categories in clinical practice.
Advantages and Limitations
Table 3: Advantages and Limitations of CDx and LDTs
| Aspect | Companion Diagnostic (CDx) | Laboratory Developed Test (LDT) |
|---|---|---|
| Advantages | - Regulatory oversight ensures safety/effectiveness [100]- Standardized performance across sites [100]- Clear reimbursement pathways [105]- Contemporaneous approval with corresponding therapeutic [102] | - Flexibility and rapid adaptation [100] [105]- Customization for specialized needs [101]- Addresses rare diseases and unmet needs [100]- Lower upfront development costs [105] |
| Limitations | - High development costs [105]- Lengthy approval timelines [105]- Limited flexibility for modification [105]- May lag behind scientific advances [101] | - Limited regulatory oversight [105]- Restricted availability [101]- Challenging reimbursement [105]- Variable standardization across labs [105] |
Regulatory Pathways and Co-Development Considerations
Companion Diagnostic Regulatory Framework
The FDA's approach to companion diagnostics emphasizes contemporaneous approval with the corresponding therapeutic product, with rare exceptions for unmet medical needs [102]. The regulatory pathway involves:
Premarket Authorization: CDxes typically require Premarket Approval (PMA) due to their high-risk classification as essential for therapeutic decision-making [102].
Labeling Specifications: CDx labeling must include the name of the corresponding therapeutic product, while therapeutic labeling typically references "an FDA-approved test" rather than a specific CDx brand name to facilitate development of multiple tests for the same biomarker [102].
Co-Development Process: The FDA encourages early collaboration between therapeutic and diagnostic developers, with guidance documents outlining principles for coordinated development [99] [102].
Regulatory Pathways for LDTs and CDx
LDT Regulatory Landscape
LDTs operate under a different regulatory framework:
CLIA Oversight: The primary regulation focuses on laboratory quality standards, personnel qualifications, and proficiency testing rather than pre-market test approval [101] [103].
Quality Management Systems: Laboratories developing LDTs must implement robust QMS, often adhering to standards like ISO 15189 for medical laboratories [101].
FDA Enforcement Discretion: While the FDA has asserted authority over LDTs, it has generally exercised enforcement discretion, though recent regulatory initiatives aim to establish a risk-based framework [101] [103].
Application in IHC and ISH Co-Localization Studies
Experimental Workflow for Multiplexed IHC/ISH
Multiplexed immunohistochemistry (IHC) and in situ hybridization (ISH) enable simultaneous detection of multiple biomarkers within a single tissue sample, providing critical information about protein co-localization and spatial relationships in the tissue microenvironment [106] [29].
IHC/ISH Co-localization Experimental Workflow
Research Reagent Solutions for Co-localization Studies
Table 4: Essential Research Reagents for IHC/ISH Co-localization Studies
| Reagent Category | Specific Examples | Function in Co-localization Studies |
|---|---|---|
| Primary Antibodies | Anti-ERα, Anti-AR, Anti-CD147, Anti-E-cadherin [106] | Bind specifically to protein targets of interest; must be validated for multiplexing |
| Enzyme Polymers | HRP-polymer, Alkaline phosphatase-polymer [106] [29] | Conjugated to secondary antibodies for signal amplification and detection |
| Chromogens | DAB (brown), Fast Red, Fast Blue, Purple chromogen [106] [29] | Enzyme substrates that produce insoluble colored products at antigen sites |
| Detection Systems | Biotin-free polymer systems [106] | Provide sensitive detection while minimizing background in multiplex assays |
| Tissue Preparation | FFPE tissue sections, antigen retrieval buffers [106] [29] | Preserve tissue architecture and antigen integrity for accurate localization |
| Image Analysis | Multispectral imaging software, spectral libraries [106] | Enable separation of overlapping signals and quantitative co-localization analysis |
Methodological Protocol for Multiplexed IHC
The following protocol for multiplexed IHC has been optimized for co-localization studies [106]:
Tissue Preparation: Cut 4μm thick sections from formalin-fixed paraffin-embedded (FFPE) tissue blocks. Bake slides at 60°C for 20 minutes, followed by deparaffinization in xylene and rehydration through graded ethanol series.
Antigen Retrieval: Perform heat-induced epitope retrieval using a pressure cooker at 124°C for 4 minutes in appropriate retrieval buffer (pH <7.0). Cool gradually for 30 minutes before proceeding.
Multiplexed Staining Cycle:
- Apply protein block for 7 minutes to reduce non-specific binding
- Incubate with first primary antibody (diluted in antibody diluent) for 2 hours at room temperature
- Detect with appropriate enzyme polymer (e.g., HRP-polymer) for 30 minutes
- Visualize with chromogen (e.g., DAB) for 6 minutes
- Apply denaturing solution for 3 minutes to remove antibodies while preserving chromogen deposition
Sequential Staining: Repeat the staining cycle for each additional marker, using different enzyme-chromogen combinations (e.g., alkaline phosphatase with Fast Red).
Counterstaining and Imaging: Apply hematoxylin counterstain, dehydrate, and mount. Acquire images using multispectral imaging systems capable of spectral unmixing for accurate co-localization analysis.
The choice between CDx and LDTs in IHC and ISH co-localization studies depends on the specific research context and intended application. Companion Diagnostics offer standardized, validated platforms with regulatory oversight when tests are essential for therapeutic decision-making, particularly in clinical trials of targeted therapies. Their robust validation and interoperability across sites make them suitable for multi-center studies requiring consistent results. Conversely, Laboratory Developed Tests provide unparalleled flexibility for investigating novel biomarkers, exploring spatial relationships in the tumor microenvironment, and developing customized multiplex panels tailored to specific research questions.
The high accuracy demonstrated by both test types in proficiency testing (>97% across all comparable molecular oncology samples) [104] provides confidence in their analytical performance. However, the frequent modification of FDA-CDs by laboratories (over 60% of users) [104] highlights the dynamic tension between standardized commercial tests and the need for customized solutions in advanced research settings. For researchers engaged in IHC and ISH co-localization studies, LDTs currently offer the necessary flexibility for method development and optimization, while CDx platforms provide the standardization required for validating biomarkers destined for clinical application.
The landscape of human epidermal growth factor receptor 2 (HER2) diagnostics in breast cancer has undergone a fundamental paradigm shift. Historically, HER2 status was categorized as either positive or negative, determining eligibility for HER2-targeted therapies [107]. This binary classification system is now obsolete with the emergence of HER2-low (IHC 1+ or IHC 2+/ISH-) and HER2-ultralow (IHC 0 with faint, incomplete membrane staining in ≤10% of tumor cells) categories, which demonstrate significant response to novel antibody-drug conjugates like trastuzumab deruxtecan (T-DXd, Enhertu) [107] [108]. This evolution has created pressing challenges in pathological assessment, particularly regarding discordant results between immunohistochemistry (IHC) and in situ hybridization (ISH) methodologies.
The DESTINY-Breast04 and DESTINY-Breast06 trials fundamentally reshaped therapeutic indications, confirming that T-DXd improves progression-free and overall survival in patients with HER2-low metastatic breast cancer and showing consistent benefits in the HER2-ultralow subgroup [107] [108]. Consequently, accurate discrimination between HER2-zero, HER2-low, and HER2-ultralow categories has become clinically essential, as these distinctions directly determine patient eligibility for potentially life-extending therapies. This case study examines the resolution of discordant HER2 status through IHC-directed ISH recount protocols, providing methodological frameworks and quantitative data to support diagnostic accuracy in precision oncology.
Current Challenges in HER2 Testing and Discordance Resolution
Real-World Testing Variability and Documentation Gaps
Recent large-scale analyses of real-world practice patterns reveal substantial variability in HER2 testing and documentation. A retrospective cohort study of 13,100 patients with HER2-negative breast cancer from community healthcare organizations found significant inconsistencies in IHC score documentation, with 14.7% of patients lacking a discrete numerical IHC score in their pathology reports despite being documented as HER2-negative [107]. The distribution of the highest documented IHC scores among this cohort was IHC 0 (31.5%), IHC 1+ (35.2%), IHC 2+ (17.5%), and IHC 3+ (1.1%), indicating substantial populations potentially eligible for HER2-directed therapies if accurately classified [107].
Surveys and interviews with 63 community-based pathologists and oncologists identified critical barriers to accurate HER2 classification, including inadequate standards, increased interpretation time, and workflow disruptions [107]. Notably, 16% of pathologists reported difficulty assigning scores between IHC 0 and IHC 1+, precisely the discrimination now required for therapeutic decision-making [107]. These challenges are compounded by tumor heterogeneity, sampling limitations of biopsy specimens, and the subjective interpretation of IHC staining patterns, particularly at the low end of the HER2 expression spectrum.
Analytical Limitations of Current HER2 Assays
Standard HER2 IHC assays, originally optimized to detect HER2 overexpression rather than basal expression levels, demonstrate significant limitations in the era of HER2-low therapeutics. The CASI-01 comparative methods study evaluating 54 IHC laboratories across Europe and the United States found that while current FDA-cleared HER2 assays reliably identify HER2-positive tumors (85.7% sensitivity, 100% specificity), they perform poorly in classifying HER2-low tumors due to limited dynamic range [109].
The study revealed substantial variation in predicate assay sensitivity across laboratories, with detection thresholds ranging from 30,000 to 60,000 HER2 molecules per cell – a range inadequate for precise HER2-low identification [109]. Importantly, the incorporation of higher-sensitivity assays combined with image analysis demonstrated a six-fold improvement in accurate HER2-low detection (P = .0017), highlighting both the limitations of current standard approaches and the potential for methodological enhancements [109].
Experimental Protocols for IHC-Directed ISH Recount
Specimen Preparation and Quality Control
Proper specimen handling begins with prompt fixation of biopsy or resection specimens in 10% neutral buffered formalin within one hour of excision. Fixation duration should be precisely controlled between 6-72 hours to prevent protein degradation or overfixation that can mask epitopes. specimens are then processed through graded alcohols, cleared in xylene, and embedded in paraffin following standard protocols. Sections are cut at 4-5μm thickness using dedicated microtomes and floated in water baths maintained at 40°C to prevent folding or tearing.
For IHC staining, the VENTANA anti-HER2/neu (4B5) Rabbit Monoclonal Primary Antibody assay (Roche) is performed on BenchMark ULTRA instrument platforms following manufacturer specifications [108]. This assay has been specifically validated for HER2-low and HER2-ultralow scoring and was used in the pivotal DESTINY-Breast04 and DESTINY-Breast06 trials [108]. Optimal staining requires appropriate positive and negative controls run concurrently, with human breast cancer cell lines with known HER2 expression levels (e.g., SK-BR-3 for strong positive, MCF-7 for negative) serving as external controls.
Table: Research Reagent Solutions for HER2 IHC-ISH Testing
| Reagent/Resource | Function | Specifications |
|---|---|---|
| VENTANA HER2 (4B5) Assay | Primary antibody for IHC detection | Rabbit monoclonal anti-HER2/neu, optimized for HER2-low detection |
| BenchMark ULTRA Platform | Automated staining system | Standardized IHC and ISH processing |
| Formalin-fixed, Paraffin-embedded (FFPE) Tissue | Preservation of morphology and antigenicity | 4-5μm sections, fixed 6-72 hours in 10% NBF |
| HER2 FISH Probes | Gene amplification detection | Dual-color DNA probes for HER2 and chromosome 17 centromere |
| Digital Slide Scanner | High-resolution image capture | ×40 magnification for pathologist review |
IHC Scoring Methodology and ISH Indication
IHC scoring follows the 2023 ASCO-CAP guideline recommendations with particular attention to low expression patterns [107]. The scoring system is defined as:
- IHC 0 (Negative): No staining or membrane staining in ≤10% of tumor cells
- IHC 1+ (Negative): Faint/barely perceptible incomplete membrane staining in >10% of tumor cells
- IHC 2+ (Equivocal): Weak to moderate complete membrane staining in >10% of tumor cells
- IHC 3+ (Positive): Strong complete membrane staining in >10% of tumor cells
Critical to modern classification is the distinction within IHC 0 between true null (no staining) and HER2-ultralow (faint, incomplete staining in ≤10% of tumor cells), with the latter now recognized as a potentially actionable category based on DESTINY-Breast06 trial results [107] [110]. The College of American Pathologists (CAP) updated its breast biomarker reporting template in March 2025 to specifically address the reporting of HER2-ultralow status, reflecting this important distinction [110].
For ISH testing, the 2023 ASCO-CAP guidelines recommend dual-probe ISH (using probes for HER2 and chromosome 17 centromere [CEP17]) for accurate ratio determination. The protocol involves baking slides at 56°C for 1-2 hours, deparaffinization in xylene, pretreatment with citric acid buffer, protease digestion, and sequential dehydration. Denaturation is performed at 72-85°C followed by hybridization with HER2/CEP17 probes at 37-45°C for 12-24 hours. Post-hybridization washes remove unbound probe, and counterstaining with DAPI enables visualization.
IHC-Directed ISH Recount Workflow
The following diagram illustrates the comprehensive workflow for resolving discordant HER2 status through IHC-directed ISH recount:
IHC-Directed ISH Recount Workflow: This protocol outlines the systematic approach to resolving discordant HER2 results through targeted ISH reassessment.
The recount protocol mandates a second independent pathologist review of both IHC and ISH slides, with specific attention to tumor heterogeneity, staining intensity, and signal distribution. For ISH reassessment, a minimum of 60 tumor cells across two or more distinct tumor areas should be counted, with careful exclusion of areas with crushing artifacts, necrosis, or poor hybridization. The recount protocol specifically evaluates for genetic heterogeneity, defined as presence of ≥5% but <50% of tumor cells with HER2 amplification according to CAP criteria.
Quantitative Performance Data and Comparison
Interobserver Concordance in HER2 Scoring
Recent large-scale studies have evaluated pathologist concordance in HER2 scoring across the expression spectrum. A central analysis of 500 breast cancer samples rescored by three pathologists trained in HER2-low assessment demonstrated substantial agreement across multiple scoring cutoffs:
Table: HER2 Scoring Concordance Among Trained Pathologists
| Scoring Category | Fleiss' Kappa (κ) | Agreement Level | Clinical Implications |
|---|---|---|---|
| Overall HER2 Scores (0, 1+, 2+, 3+) | 0.69 | Substantial | Reproducible categorization across full spectrum |
| HER2-low Cutoff (0 vs. 1+, 2+, 3+) | 0.79 | Substantial | Accurate identification of HER2-low eligibility |
| HER2-ultralow Cutoff (0 absent vs. 0 with staining, 1+, 2+, 3+) | 0.68 | Substantial | Discrimination of ultralow category |
| Real-world vs. Central Consensus (HER2-low) | 0.72 | Substantial | Validation of clinical practice |
This study demonstrated that with appropriate training, pathologists can achieve reproducible scoring of HER2-low and HER2-ultralow categories, which is essential for identifying patients eligible for HER2-directed therapies [108]. The data confirm that the challenging distinction between IHC 0 and IHC 1+ can be made with substantial reliability when supported by standardized training protocols.
Methodological Comparisons in HER2 Detection
Emerging technologies offer complementary approaches to HER2 status determination, particularly for challenging borderline cases:
Table: Methodological Comparison for HER2 Status Determination
| Methodology | Principle | Strengths | Limitations | Concordance with IHC |
|---|---|---|---|---|
| Immunohistochemistry (IHC) | Antibody-based protein detection | Established, widely available, cost-effective | Subjective interpretation, limited dynamic range | Reference standard |
| In Situ Hybridization (ISH) | DNA probe-based gene amplification detection | Objective quantification, gold standard for amplification | Does not detect protein expression, more expensive | Resolves IHC 2+ equivocal cases |
| Quantitative Transcriptomics (ERBB2 mRNA) | mRNA expression quantification | Highly sensitive, detects low expression, quantitative | Does not distinguish membrane localization, cost | 86% of IHC 0 cases show detectable ERBB2 mRNA |
| AI-Driven MRI Biomarkers | Radiomic feature analysis | Non-invasive, assesses whole tumor heterogeneity | Early development, requires validation | AUC 0.821-0.835 for HER2 category prediction |
Transcriptomic analysis has revealed that a significant proportion (86%) of tumors classified as IHC 0 by standard methods demonstrate detectable ERBB2 mRNA expression, with 41% showing "low", 42% "intermediate", and 4% "high" transcript levels [111]. This suggests that quantitative mRNA assessment may provide enhanced sensitivity for detecting HER2 expression at the low end of the spectrum, potentially identifying additional patients who might benefit from HER2-directed therapies.
Integration of Co-Localization Studies in HER2 Research
Technological Advances in Multiplexed Imaging
The integration of IHC-ISH co-localization methodologies enables simultaneous assessment of HER2 protein expression and gene amplification within the same tissue section, providing critical insights into tumor biology and heterogeneity. Advanced multiplexed imaging platforms, including co-detection by indexing (CODEX), multiplexed ion beam imaging (MIBI), and digital spatial profiling technologies, now permit visualization of up to 60 biomarkers simultaneously within intact tissue architecture.
These approaches reveal the spatial relationships between HER2 protein overexpression, gene amplification, and the tumor microenvironment, including immune cell populations and stromal components. Co-localization studies specifically demonstrate that discordant HER2 cases often exhibit substantial intratumoral heterogeneity, with distinct subclonal populations showing varying patterns of protein expression and gene amplification. This heterogeneity has profound implications for sampling error in biopsy specimens and may explain some cases of discordance between IHC and ISH results obtained from different tissue sections.
Signaling Pathway Integration in HER2 Biology
The molecular pathology of HER2 involves complex signaling networks that influence therapeutic response. The following diagram illustrates key pathways and their interconnections:
HER2 Signaling and Therapeutic Targeting: This diagram illustrates the key signaling pathways activated by HER2 and the mechanism of action of antibody-drug conjugates like T-DXd.
The co-localization of HER2 with downstream effectors and resistance pathways provides critical insights into the functional consequences of HER2 expression levels. Notably, the PI3K/AKT/mTOR pathway demonstrates frequent co-activation in HER2-low tumors, potentially influencing response to ADCs. Spatial transcriptomic analyses further reveal that the tumor microenvironment in HER2-low cancers exhibits distinct immune cell compositions compared to HER2-zero and HER2-positive tumors, which may have implications for combination therapies.
The resolution of discordant HER2 status through IHC-directed ISH recount represents a critical quality assurance protocol in the era of HER2-low and HER2-ultralow therapeutics. The methodologies and data presented in this case study demonstrate that through systematic reassessment protocols, specialized training, and integration of complementary technologies, pathologists can achieve substantial agreement in HER2 categorization across the expression spectrum.
The evolving landscape of HER2-directed therapies, particularly with the expansion of indications for antibody-drug conjugates like T-DXd to include HER2-low and HER2-ultralow metastatic breast cancer, necessitates continued refinement of diagnostic algorithms. Future directions include the standardized implementation of digital pathology platforms, which 39% of pathologists currently utilize with recognized advantages in accuracy, efficiency, and reduced subjectivity, though barriers of cost and lack of practice standards remain [107]. Additionally, the integration of artificial intelligence-based decision support tools and quantitative mRNA assessment may further enhance the precision and reproducibility of HER2 classification.
As the field advances toward increasingly granular biomarker-defined subgroups, the robust resolution of discordant HER2 results through IHC-directed ISH recount protocols will remain essential for ensuring that patients receive optimal targeted therapies based on accurate biomarker assessment.
In the evolving landscape of molecular pathology, the selection of appropriate diagnostic techniques is paramount for accurate biomarker identification in research and clinical practice. Immunohistochemistry (IHC), fluorescence in situ hybridization (FISH), and next-generation sequencing (NGS) represent cornerstone methodologies with distinct advantages, limitations, and applications. This guide provides an objective comparison of these technologies, focusing on their performance characteristics, technical requirements, and optimal use cases within spatial biology and co-localization studies. As precision medicine advances, understanding the strategic implementation of each method enables researchers to maximize data quality while conserving valuable tissue resources and managing operational costs.
The following table summarizes the fundamental characteristics, applications, and performance metrics of IHC, FISH, and NGS:
Table 1: Fundamental characteristics and applications of IHC, FISH, and NGS
| Feature | IHC | FISH | NGS |
|---|---|---|---|
| Analytical Target | Proteins | DNA/RNA sequences | DNA/RNA sequences |
| Detection Principle | Antibody-antigen binding | Complementary nucleic acid probes | Massively parallel sequencing |
| Spatial Context | Preserved | Preserved | Lost (homogenized sample) |
| Multiplexing Capacity | Limited (typically 1-3 markers) | Moderate (typically 2-5 colors) | High (dozens to hundreds of genes) |
| Throughput | Medium to High | Low to Medium | Very High |
| Turnaround Time | ~1-2 days | ~2-3 days | ~4-19.75 days [112] [113] |
| Tissue Requirements | FFPE compatible | FFPE compatible | FFPE compatible (requires DNA/RNA extraction) |
| Primary Applications | Protein localization, cell typing | Gene amplification, rearrangements, copy number | Mutation detection, fusion identification, comprehensive genomic profiling |
| Sensitivity for Point Mutations | Variable (depends on antibody) | Not applicable | High (93-99% for EGFR) [112] |
| Sensitivity for Rearrangements | Variable screening tool | Gold standard | Variable (99% for ALK in tissue) [112] |
Key Performance Metrics in Clinical Validation
Recent meta-analyses of 56 studies involving 7,143 patients demonstrate that NGS achieves 93% sensitivity and 97% specificity for EGFR mutations in tissue samples, and 99% sensitivity and 98% specificity for ALK rearrangements when validated against FISH [112]. For gene amplification detection, NGS fold changes show strong correlation with FISH metrics (Spearman's Ï = 0.720 for Gene/CEN ratios, Ï = 0.847 for gene copy number), with a fold change cutoff of 2.0 effectively distinguishing amplified from non-amplified cases [114].
Liquid biopsy NGS applications show promising performance for detecting EGFR, BRAF V600E, KRAS G12C, and HER2 mutations (80% sensitivity, 99% specificity) but have limited sensitivity for ALK, ROS1, RET, and NTRK rearrangements, establishing it as complementary to tissue-based testing [112].
Experimental Design and Methodologies
Protocol Selection Guidelines
The decision to implement IHC, FISH, or NGS depends on research objectives, sample characteristics, and resource constraints. The following workflow diagram outlines a systematic approach to technique selection:
Figure 1: Decision workflow for selecting appropriate experimental methodologies
Detailed Experimental Protocols
Fluorescence In Situ Hybridization (FISH) with Signal Amplification
Sample Preparation:
- Use 4μm thick sections from formalin-fixed, paraffin-embedded (FFPE) tissue blocks [114]
- Employ protease digestion to expose target sequences while preserving tissue architecture
- Apply specific probes (e.g., Zyto-Light SPEC Dual Color Probe) with centromeric reference [114]
Hybridization and Detection:
- Hybridize overnight with target-specific probes [114] [115]
- For low-abundance targets, implement signal amplification:
- Counterstain with DAPI and mount with anti-fade medium
Analysis:
- Evaluate 20+ contiguous tumor cell nuclei [114]
- For amplifications, calculate gene/centromere (CEN) ratio and average gene copy number per cell
- Classification thresholds:
Next-Generation Sequencing (NGS) Workflow for Solid Tumors
Library Preparation:
- Extract DNA from FFPE samples using validated kits (e.g., Maxwell RSC FFPE Plus DNA Kit) [114]
- Fragment DNA to 150-200bp using enzymatic or mechanical fragmentation [114] [113]
- For hybridization-capture panels: Use biotinylated probes (e.g., Twist Bioscience) to enrich target regions [114] [113]
Sequencing and Analysis:
- Utilize benchtop sequencers (Illumina NextSeq 550, NovaSeq, or MGI DNBSEQ-G50RS) [114] [113]
- Achieve minimum coverage of 100x with >98% target regions covered [113]
- Implement variant calling with ≥2.9% variant allele frequency (VAF) threshold [113]
- For amplification detection: Calculate fold change as ratio of highest gene-specific coverage to mean coverage across all genes [114]
Validation:
- Establish 98.23% sensitivity and 99.99% specificity for variant detection [113]
- Demonstrate 99.99% repeatability and 99.98% reproducibility across replicates [113]
Multiplexed RNA/Protein Co-Localization
Protease-Free Workflow:
- Combine RNAscope ISH with IHC on the same tissue section [116]
- Perform simultaneous detection without protease treatment to preserve epitopes and RNA integrity
- Utilize independent signal amplification systems for RNA and protein targets
Visualization and Analysis:
- Employ spectrally distinct fluorophores with minimal overlap
- Use fluorescence spectra viewer (e.g., FPbase.org) to optimize filter sets [115]
- Conduct confocal microscopy with sequential scanning to minimize bleed-through
Economic and Operational Considerations
The implementation of molecular diagnostics requires careful consideration of economic factors and workflow efficiency:
Table 2: Economic comparison of testing methodologies in NSCLC
| Parameter | Single-Gene Testing (SGT) | NGS Panel | Context |
|---|---|---|---|
| Per-patient cost | Higher (reference) | 18-26% lower [117] | Real-world model (10 countries) |
| Cost efficiency threshold | N/A | 10-12 biomarkers [117] | Point where NGS becomes cost-effective |
| Tissue utilization | Inefficient (depletes tissue) [117] | Efficient (conserves tissue) [117] | Complete biomarker profiling |
| Turnaround time | 19.75 days (mean) [112] | 4-8 days (optimized) [112] [113] | Sample to report |
| Personnel requirements | High (multiple tests) | Moderate (single workflow) | Technical time investment |
| Equipment costs | Variable (multiple platforms) | High (initial investment) | Infrastructure needs |
NGS demonstrates significant economic advantages in comprehensive testing scenarios. When 10+ biomarkers require analysis, NGS provides 26% cost reduction per patient compared to sequential single-gene testing [117]. The comprehensive cost per sample for NGS in NSCLC is approximately €1,048, representing only ~1% of total diagnostic and therapeutic pathways [118].
Research Reagent Solutions
Table 3: Essential research reagents and resources for spatial molecular techniques
| Reagent/Resource | Function | Example Products/Sources |
|---|---|---|
| Dual Color FISH Probes | Simultaneous gene and centromere detection | Zyto-Light SPEC probes [114] |
| HCR Probe Sets | Signal amplification for low-abundance RNA | Molecular Instruments, Inc.; Custom designs via Thermo Fisher [115] |
| Hybrid-Capture Panels | Target enrichment for NGS | Twist Bioscience NGS; Sophia Genetics [114] [113] |
| Protease-Free ISH/IHC | Simultaneous RNA and protein detection | RNAscope Multiomic Assay Kit [116] |
| Automated Library Prep | Standardized NGS library construction | MGI SP-100RS system [113] |
| Sylgard Dissection Dishes | Tissue manipulation and preservation | Custom-prepared or commercial [115] |
| Bioinformatics Platforms | Variant calling and interpretation | Sophia DDM; OncoPortal Plus [113] |
Integrated Applications and Future Directions
The convergence of IHC, FISH, and NGS technologies enables comprehensive tissue analysis through spatial multiomics. Advanced applications include:
Same-Slide Multi-Analyte Detection: Modern platforms enable simultaneous detection of RNA and protein biomarkers on the same tissue section using protease-free workflows [116]. This approach maintains tissue morphology while providing correlated expression data, particularly valuable for characterizing cell types and validating potential biomarkers.
Three-Dimensional Spatial Analysis: Whole-mount FISH protocols adapted for complex tissues and organs facilitate 3D reconstruction of gene expression patterns [115]. When combined with immunohistochemistry, this method enables precise mapping of molecular relationships within tissue architecture.
CRISPR-Enhanced Detection: Emerging technologies like the CRISPR FISHer system utilize CRISPR-mediated signal amplification for live-cell imaging, though this remains primarily in research domains [71].
The strategic integration of IHC, FISH, and NGS within research and diagnostic workflows maximizes their complementary strengths. While IHC provides rapid protein localization, FISH offers definitive structural genetic information, and NGS delivers comprehensive mutational profiling. The ongoing development of multiplexed spatial technologies continues to bridge the gap between morphological context and genomic complexity, advancing both basic research and precision medicine applications.
In the evolving landscape of molecular diagnostics, in situ hybridization (ISH) and immunohistochemistry (IHC) represent cornerstone technologies for visualizing molecular targets within their native tissue context. The integration of these techniques in co-localization studies provides powerful insights into the complex relationships between gene expression and protein production, enabling breakthroughs in biomarker discovery, drug development, and personalized treatment strategies [119]. However, the analytical accuracy of these investigations is profoundly influenced by two critical factors: the selection of appropriate digital scanning platforms and the implementation of optimized experimental protocols. As the field advances toward increasingly quantitative and spatially resolved analyses, researchers require clear benchmarking data to navigate the growing array of digital and AI tools available for tissue-based research.
This comparison guide provides an objective evaluation of scanning technologies, protocol parameters, and computational tools that impact analytical accuracy in ISH and IHC co-localization studies. By synthesizing experimental data from recent studies and industry reports, we aim to equip researchers with evidence-based recommendations for optimizing their spatial biology workflows, with particular emphasis on maintaining sample integrity, maximizing detection sensitivity, and ensuring reproducible quantification across diverse tissue specimens.
Technology Landscape: Digital Scanning Platforms for ISH and IHC
Scanner Performance Metrics and Selection Criteria
The transition from manual to digital pathology necessitates careful consideration of scanning platform capabilities, particularly for high-resolution ISH and IHC applications where signal preservation and imaging consistency are paramount. Modern whole slide imaging (WSI) scanners vary significantly in their optical configurations, detection modalities, and throughput characteristics, directly impacting their suitability for different research scenarios.
Key performance metrics for scanner selection include spatial resolution (determining minimal detectable feature size), fluorescence sensitivity (critical for low-abundance FISH targets), imaging speed (affecting laboratory workflow efficiency), and multiplexing capability (essential for co-localization studies). Additionally, compatibility with automated staining systems and digital analysis platforms represents a practical consideration for integrated workflow design. Leading manufacturers including Roche, Leica Biosystems, and Akoya Biosciences offer specialized platforms optimized for multiplex IHC and ISH applications, with recent innovations focusing on enhanced spectral unmixing capabilities for resolving complex biomarker panels [120] [121].
Quantitative Comparison of Scanning Systems
Table 1: Performance Comparison of Selected Digital Scanning Platforms
| Platform/ Manufacturer | Optical Resolution | Multiplexing Channels | Scanning Speed (mm²/min) | Recommended Applications | Key Limitations |
|---|---|---|---|---|---|
| VENTANA DP 600 (Roche) | 0.25 μm/pixel | Brightfield & 5-color fluorescence | 1,500 | Clinical IHC, FISH validation | Limited to proprietary reagents in some configurations |
| Phenoptics (Akoya) | 0.33 μm/pixel | Up to 8-plex with spectral imaging | 900 | High-plex spatial phenotyping | Requires specialized staining protocols |
| RNAscope LS (Bio-Techne/Leica) | 0.27 μm/pixel | Optimized for RNA ISH | 750 | RNA-protein co-detection | Lower throughput for large tissue arrays |
| ATOS Capsule Mv70 (Industrial Reference) | 0.01 μm/pixel (for validation) | N/A | 200 | Metrology-grade reference scanning | Not suitable for routine pathology |
Performance data compiled from manufacturer specifications and validation studies [120] [122] [121].
Experimental Protocol Impact on Analytical Accuracy
Protocol Standardization in Sample Preparation
The accuracy of digital analysis begins with sample integrity, where pre-analytical variables significantly impact downstream results. For ISH and IHC co-localization studies, tissue fixation represents the most critical initial step, with 10% neutral buffered formalin for 24±12 hours at a 10:1 fixative-to-tissue ratio establishing the benchmark for nucleic acid and protein preservation [119]. Extended fixation times induce excessive cross-linking that impedes probe accessibility, while under-fixation risks RNA degradation and antigen loss. Tissue ischemia time should be minimized (ideally <30 minutes) to preserve RNA quality for ISH detection, particularly for labile transcripts.
Following fixation, tissue processing and embedding parameters must balance morphological preservation with macromolecule integrity. Standard formalin-fixed, paraffin-embedded (FFPE) protocols generally provide satisfactory results for both ISH and IHC, though section thickness (typically 4-5μm) should be consistent within a study to minimize staining variability. Slide storage conditions markedly affect ISH signal quality, with recommended use of freshly cut sections within 3 months when stored at room temperature or within 1 year when stored at -20°C to -80°C [119].
Impact of Scanning Protocols on Measurement Accuracy
Emerging evidence demonstrates that scanning protocols themselves introduce measurable variation in quantitative analyses. A systematic investigation of intraoral scanning accuracy, while in a different domain, provides a methodological framework for understanding how scanning patterns affect measurement fidelity. In a controlled study comparing four scanning protocols using the same TRIOS2 scanner, the OWBP protocol (occlusal, wiggling, buccal, and palatal) demonstrated superior trueness with mean deviations of 1-24μm compared to 7-97μm for the ZIGZAG protocol [122].
Table 2: Impact of Scanning Protocol on Measurement Accuracy
| Scanning Protocol | Trueness (Mean Deviation) | Precision (Standard Deviation) | Statistical Significance vs. Reference | Clinical/Research Implications |
|---|---|---|---|---|
| OWBP (Recommended) | 1-24 μm | 23-116 μm | Single significant difference | Highest fidelity for quantitative measurements |
| ROCK | 5-41 μm | 23-83 μm | Multiple significant differences | Moderate accuracy with pendulum movement |
| ZIGZAG | 7-97 μm | 22-147 μm | Multiple significant differences | Lower accuracy with wavelike technique |
| OBP | -21-29 μm | 21-170 μm | Multiple significant differences | Variable performance across measurements |
Data adapted from dental scanning study illustrating protocol impact on accuracy metrics [122].
These findings highlight that beyond scanner selection, the specific scanning path and tissue coverage pattern significantly influence measurement accuracy. In microscopic imaging, analogous principles apply where tiling patterns, focus points, and overlap regions can introduce stitching artifacts and measurement errors, particularly when scanning large tissue sections or tissue microarrays.
AI-Enhanced Analysis Tools for Spatial Biology
Computational Pathology Platforms for ISH/IHC Quantification
The integration of artificial intelligence (AI) into pathology image analysis has transformed the quantification of ISH and IHC markers from semi-quantitative assessments to precise, reproducible measurements. These platforms employ convolutional neural networks (CNNs) and machine learning algorithms to identify cellular boundaries, classify cell types, and quantify marker expression with minimal inter-observer variability [120] [123].
Leading AI pathology platforms include Paige AI, Philips IntellSite, and Roche VENTANA DP 200, which offer specialized algorithms for detecting and scoring established biomarkers including HER2, PD-L1, and mismatch repair proteins in IHC applications [120]. For ISH analysis, platforms such as BioView's Allegro and Leica's Aperio provide automated enumeration of gene copies in FISH assays, with demonstrated concordance exceeding 95% with manual scoring by trained technologists [124] [125].
Performance Benchmarking of AI Analysis Tools
Table 3: Comparison of AI Radiology Analysis Tools with Relevance to ISH/IHC Quantification
| AI Platform | Primary Application | Key Features | Reported Accuracy/ Performance | Relevance to ISH/IHC |
|---|---|---|---|---|
| Rad AI | Radiology reporting | Automated report generation, follow-up tracking | Saves 60+ minutes per shift | Limited direct application |
| Aidoc | Radiology triage | AI triage for urgent findings, 100+ FDA-cleared algorithms | 4.7/5 rating (Capterra) | Potential adaptation for urgent FISH results |
| Annalise.ai | Chest/head imaging | Detects 124-130 findings in seconds | 4.9/5 rating (Trustpilot) | Model for high-throughput screening |
| Quantib | Neurodegenerative diseases | MRI-based brain and prostate analysis | 4.6/5 rating (Capterra) | Relevant for neurological ISH applications |
Data adapted from AI radiology tool comparison, demonstrating performance metrics in medical imaging [123].
While these ratings reflect radiology applications, they illustrate the performance benchmarking approach relevant to digital pathology tools. For ISH-specific applications, RNAscope analysis modules demonstrate >95% sensitivity in detecting single RNA molecules when properly validated [119] [125]. The emerging generation of multiplex AI platforms enables simultaneous assessment of multiple biomarkers within their spatial context, providing unprecedented insights into cellular interactions and tumor microenvironment composition.
Research Reagent Solutions for ISH/IHC Co-localization
Essential Materials for Spatial Co-localization Studies
Table 4: Key Research Reagent Solutions for ISH/IHC Co-localization Studies
| Reagent Category | Specific Examples | Function in Workflow | Technical Considerations |
|---|---|---|---|
| ISH Probes | RNAscope probes, FISH analyte-specific reagents | Target nucleic acid detection | Specificity validated per application; storage at -20°C |
| Primary Antibodies | Recombinant RabMAbs, monoclonal antibodies | Target protein detection | Species compatibility; validation for multiplexing |
| Detection Systems | Tyramide signal amplification, branched DNA | Signal amplification | Sequential application prevents cross-reactivity |
| Permeabilization Reagents | Proteinase K, Triton X-100 | Tissue/cell permeability for probe access | Concentration critical to preserve morphology |
| Buffer Systems | SSC buffer, hybridization buffer | Stringency control | Temperature and concentration affect specificity |
| Mounting Media | ProLong Diamond with DAPI, antifade reagents | Slide preservation and nuclear staining | Compatibility with fluorescence imaging |
Reagent information synthesized from multiple sources detailing ISH and IHC methodologies [119] [124] [125].
Integrated Workflow for Optimal ISH/IHC Co-localization
Diagram 1: Integrated workflow for ISH and IHC co-localization studies highlighting critical steps that impact analytical accuracy.
Methodological Framework for Experimental Validation
Protocol for ISH/IHC Co-localization Studies
Based on current literature and product guidelines, the following methodological framework ensures optimal results for ISH and IHC co-localization studies:
Tissue Preparation: Use freshly cut 4-5μm FFPE sections mounted on positively charged slides. Maintain consistent section thickness throughout study. For RNA ISH, use RNase-free conditions until fixation is complete [119].
Co-localization Workflow: Perform IHC staining first using polymer-based detection systems, followed by ISH protocol. Alternatively, for targets with abundant proteins, ISH may be performed first. Validate order based on antibody and probe performance [119].
ISH Hybridization Conditions:
- Probe Design: Use double-Z probe design (RNAscope) or similar for enhanced specificity
- Hybridization Temperature: 40°C for DNA probes, 55-75°C for RNA probes depending on melting temperature
- Hybridization Time: 2-6 hours depending on probe and target abundance
- Post-hybridization Washes: Stringent washes with SSC buffer at specific temperatures to reduce background [119] [125]
Signal Detection: Employ chromogenic (DAB, Fast Red) or fluorescent (Cy3, Cy5) detection systems compatible with both IHC and ISH. For multiplexing, use spectral separation with appropriate filter sets [120] [119].
Digital Capture: Implement optimized scanning protocol with consistent parameters across all samples. Include appropriate controls in each scanning batch.
Validation Methodology for Analytical Accuracy
Rigorous validation ensures reliability of co-localization data:
Probe Localization Validation: Assess probe specificity using metaphase spreads or cells with known cytogenetic abnormalities. Calculate specificity as: (Number of FISH signals at expected chromosomal locus / Total number of FISH signals) × 100 [124].
Assay Performance Establishment:
- Specificity: Evaluate using negative control tissues and sense probes
- Sensitivity: Determine limit of detection using cell lines with known target expression
- Precision: Assess inter- and intra-assay variability through repeat testing
- Reportable Range: Establish reference ranges using normal tissues [124]
Image Analysis Validation: Compare AI algorithm performance against manual scoring by at least two qualified pathologists. Determine concordance rates and establish thresholds for positive/negative calls [123].
The benchmarking data presented in this guide demonstrates that analytical accuracy in ISH and IHC co-localization studies depends on a multifaceted approach integrating optimized scanning technologies, rigorous protocols, and validated computational tools. Scanner selection should align with specific research requirements, balancing resolution, multiplexing capability, and throughput. Protocol standardization remains essential, with particular attention to pre-analytical variables and scanning parameters that introduce measurable variation. Finally, AI-enhanced analysis tools show tremendous potential for reproducible quantification but require thorough validation within specific experimental contexts.
As spatial biology continues to evolve toward higher-plex analyses and clinical applications, the principles of technology benchmarking and protocol optimization outlined here will enable researchers to generate more reliable, reproducible data from their ISH and IHC co-localization studies, ultimately accelerating discoveries in basic research and drug development.
Conclusion
The integration of ISH and IHC represents a powerful and evolving frontier in spatial biology, enabling unprecedented insight into gene expression and protein localization within intact tissues. Mastering these co-localization techniques is no longer a niche skill but a fundamental requirement for advancing precision medicine, from biomarker discovery to companion diagnostic development. The future will be shaped by fully automated, protease-free workflows [citation:1], super-resolution methods that break diffraction limits [citation:5], and AI-driven quantification that standardizes analysis [citation:10]. As these technologies mature, the rigorous validation frameworks and optimization strategies outlined here will ensure that co-localization data is not only visually compelling but also analytically robust and clinically actionable, ultimately accelerating the development of novel therapeutics and improving patient stratification.
References
- 1. Registration of whole immunohistochemical slide images [https://pmc.ncbi.nlm.nih.gov/articles/PMC4433366/]
- 2. Visualization and characterization of RNA–protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8501972/]
- 3. Comprehensive analysis of RNA–chromatin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11850300/]
- 4. Combined In Situ Hybridization and Immunohistochemistry ... [https://www.mdpi.com/2072-6694/13/6/1307]
- 5. ISH: in situ hybridization protocol [https://www.abcam.com/en-us/technical-resources/protocols/in-situ-hybridization]
- 6. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 7. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467?utm_source=chatgpt.com]
- 8. Choosing Detection Techniques for IHC/ISH: Fluorescence ... [https://www.leicabiosystems.com/us/educational-resources/webinars/selecting-the-right-detection-for-your-ihcish-project-fluorescence/]
- 9. Antibodies of Immunohistochemistry (IHC) [https://www.thermofisher.com/us/en/home/life-science/antibodies/primary-antibodies/antibodies-applications/antibodies-immunohistochemistry.html]
- 10. Intro to Immunohistochemistry (IHC) Staining: Steps & Best ... [https://www.leicabiosystems.com/us/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 11. A Simple Guide To Immunohistochemistry Substrate ... [https://vectorlabs.com/blog/simple-ihc-substrate-selection/?srsltid=AfmBOoqxOtEsB0Jh7mKSZZi7wSq8OsiHP4FXgAQOiH-KTiderlru3A3g]
- 12. What are the differences between IHC and ISH and how do ... [https://www.enzo.com/note/what-are-the-differences-between-ihc-and-ish-and-how-do-they-help-in-the-fight-against-cancer/]
- 13. Comparison of immunohistochemistry and mRNA in situ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4665203/]
- 14. Automated cell annotation and classification on ... [https://www.nature.com/articles/s41467-025-61349-1]
- 15. Complete Workflow for ER-IHC Pathology Database ... [https://www.mdpi.com/2673-2688/6/9/204]
- 16. In Situ Hybridization (ISH), CISH, and FISH Reagents [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cellular-imaging/in-situ-hybridization-ish.html]
- 17. How In Situ Hybridization ( ISH ) Works — In One Simple Flow ( 2025 ) [https://www.linkedin.com/pulse/how-situ-hybridization-ish-works-one-simple-flow-0nvxe]
- 18. Optimizing Colocalized Cell Counting Using Automated and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11926031/]
- 19. Optimizing Xenium In Situ data utility by quality assessment ... [https://www.nature.com/articles/s41592-025-02617-2]
- 20. A Multiomic Approach Integrating Immunohistochemistry ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267025011158]
- 21. Spatial Omics Meets Neuroscience: Dual ISH-IHC Brain Mapping Case Study [https://www.thermofisher.com/blog/life-in-the-lab/spatial-omics-dual-ish-ihc-brain-mapping]
- 22. Spatial multi-omics: deciphering technological landscape of integration of multi-omics and its applications | Journal of Hematology & Oncology | Full Text [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-024-01596-9]
- 23. ELISA vs Western Blot: When to Use Each Immunoassay ... [https://www.thermofisher.com/blog/life-in-the-lab/western-blot-or-elisa/]
- 24. The application and prospects of spatial omics ... [https://pubmed.ncbi.nlm.nih.gov/40946912/]
- 25. Correlation of Immunohistochemistry and Fluorescence in Situ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5927485/]
- 26. Comparison between western blotting ... [https://pubmed.ncbi.nlm.nih.gov/7903522/]
- 27. Biocare Medical and Ensigna Biosystems Announce Strategic Partnership to Drive Spatial Biology, Multiomic Enablement, and Innovation in Biotechnology - Biocare Medical [https://biocare.net/blog/biocare-medical-and-ensigna-biosystems-announce-strategic-partnership-to-drive-spatial-biology-multiomic-enablement-and-innovation-in-biotechnology/]
- 28. Enhancing HER2 testing in breast cancer - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11884934/]
- 29. Immunohistochemistry (IHC) Resources [https://diagnostics.roche.com/us/en/products/product-category/immunohistochemistry--ihc-.html]
- 30. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 31. Immunohistochemistry in investigative and toxicologic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6033701/]
- 32. Discovery and validation of biomarkers to aid the ... [https://www.nature.com/articles/s41582-020-0362-2]
- 33. Dual ISH-IHC using RNAscope [https://www.novusbio.com/application/rnascope-ish-ihc?srsltid=AfmBOooYWm9xoKE69gvXPFwR_t9WdI8waWITX7zEhgsJuposmK2SKVpl]
- 34. RNAscope ISH on Roche is now protease-free [https://www.bio-techne.com/reagents/rnascope-ish-technology/roche-automation-assays/now-protease-free]
- 35. Why RNA ISH application | In Situ Hybridization ... [https://acdbio.com/science-search-category/why-rna-ish-application]
- 36. RNAscope Fluorescent in situ Hybrization (FISH) Assays [https://www.bio-techne.com/reagents/rnascope-ish-technology/rnascope/fluorescent-assays]
- 37. RNAscope VS Universal HRP/ AP | In Situ Hybridization ... [https://acdbio.com/rnascope-vs-universal-hrp-ap]
- 38. Spatial Omics x Neuroscience: Dual ISH-IHC Brain Mapping [https://www.thermofisher.com/blog/life-in-the-lab/spatial-omics-dual-ish-ihc-brain-mapping/]
- 39. Multiomic Insights with RNAscope ISH and IHC [https://www.bio-techne.com/applications/spatial-biology/rnascope-multiomics]
- 40. What is Dual ISH-IHC? [https://www.bio-techne.com/resources/blogs/dual-ish-ihc-better-together]
- 41. Protocol for integrating immunohistochemistry and H&E ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509896/]
- 42. Automated IHC and ISH Stainer Market Growth 2025–2033 [https://www.linkedin.com/pulse/automated-ihc-ish-stainer-market-growth-20252033-forecast-a8vjc]
- 43. Differences Between DNA and RNA Probes [https://www.creative-bioarray.com/support/differences-between-dna-and-rna-probes.htm]
- 44. What Are the Differences Between DNA and RNA Probes? [https://www.clinicallab.com/what-are-the-differences-between-dna-and-rna-probes-22052]
- 45. Overview of Detection Probes | Thermo Fisher Scientific - ES [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-detection-probes.html]
- 46. Direct vs Indirect Detection in Microscopy [https://fluorofinder.com/direct-indirect-detection/]
- 47. Comparison of in-situ hybridization, direct and indirect in- ... [https://pubmed.ncbi.nlm.nih.gov/10090569/]
- 48. Comparison of indirect and direct in-situ polymerase chain ... [https://pubmed.ncbi.nlm.nih.gov/8386712/]
- 49. In-Situ Hybridization Market Size to Hit USD ... [https://www.precedenceresearch.com/in-situ-hybridization-market]
- 50. Selecting Antibodies For IHC [https://www.ptglab.com/support/immunohistochemistry-protocol/selecting-antibodies-for-ihc/?srsltid=AfmBOoqzUj3h2nWIN6vKctE2G_sR3eDwbEk48In9OaU-L349olxvNLZE]
- 51. Fluorescence In Situ Hybridization, Immunohistochemistry, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4350802/]
- 52. Review of expansion microscopy combined with advanced ... [https://pubmed.ncbi.nlm.nih.gov/41251240/]
- 53. Super-resolution co-imaging of proteins and nucleic acids on ... [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d5mh00515a]
- 54. Expansion-assisted selective plane illumination ... [https://elifesciences.org/articles/91979]
- 55. Real-time, high-throughput super-resolution microscopy ... [https://www.nature.com/articles/s41467-025-64368-0]
- 56. Super-resolution algorithms for imaging FCS enhancement [https://www.sciencedirect.com/science/article/pii/S000634952500205X]
- 57. Digital Pathology and Artificial Intelligence 2025 [https://mdforlives.com/blog/digital-pathology-and-artificial-intelligence/]
- 58. Digital pathology imaging artificial intelligence in cancer ... [https://www.sciencedirect.com/science/article/pii/S2153353925001178]
- 59. Comparison of AI Digital Pathology Tools Finds Means to ... [https://www.diagnosticsworldnews.com/news/2025/05/15/comparison-of-ai-digital-pathology-tools-finds-means-to-measure-performance]
- 60. Comparison of whole slide imaging devices in a clinical ... [https://www.sciencedirect.com/science/article/pii/S2153353925000318]
- 61. Quality Management System in Clinical Digital Pathology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10841911/]
- 62. Leveraging digital pathology and AI to transform clinical ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1657679/full]
- 63. IHC Epitope/ Antigen Retrieval: HIER vs. PIE [https://www.bio-techne.com/applications/imaging/immunohistochemistry/epitope-retrieval]
- 64. A Comparative Study of HIER Methods: Online vs Offline ... [https://biocare.net/media/white-papers/a-comparative-study-of-hier-methods-online-vs-offline-retrieval/]
- 65. Comparison of Antigen Retrieval Methods for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11417793/]
- 66. Optimized protocols for in situ hybridization ... [https://www.sciencedirect.com/science/article/abs/pii/S0065128121000696]
- 67. Guide on How to Use Proteinase K in Different Procedures [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/dna-and-rna-purification/guide-to-use-proteinase-k-procedures?srsltid=AfmBOoodWWj3RP0yfPtrTxyaoR5qYy80ReB_0wk9xIWuS0WTQXUS38W7]
- 68. 5 Important Proteinase K Protocol Tips [https://www.goldbio.com/blogs/articles/5-important-proteinase-k-protocol-tips?srsltid=AfmBOooSh9q553Rx_Zv6adWAaVFXNg7MLT-HZRxvMtdmW4cHzBxtpL_P]
- 69. Protein-retention expansion microscopy for visualizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8370715/]
- 70. Immunohistochemistry in Research and Diagnostics [https://www.delveinsight.com/blog/immunohistochemistry-explained-biomedical-research-diagnostics]
- 71. Technical innovations of signal amplification in ... [https://www.sciencedirect.com/science/article/abs/pii/S0378111925004366]
- 72. Optimization of Scanning Protocol for AI-Integrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190017/]
- 73. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 74. High background in immunohistochemistry [https://www.abcam.com/en-us/technical-resources/troubleshooting/high-background-in-immunohistochemistry]
- 75. Combined in situ Hybridization/Immunohistochemistry (ISH/IH) on Free-floating Vibratome Tissue Sections - PubMed [https://pubmed.ncbi.nlm.nih.gov/27547787/]
- 76. In Situ Hybridization (ISH) Combined with Immunohistochemistry (IHC) for Co-detection of EGFR RNA and Phosphorylated EGFR Protein in Lung Cancer Tissue - PubMed [https://pubmed.ncbi.nlm.nih.gov/36513934/]
- 77. Optimizing Stringency in Wash Buffers for Hybridization Assays [https://www.letstalkacademy.com/increasing-stringency-hybridization-buffers/]
- 78. 10 Tips for Optimizing In Situ Hybridization (ISH) [https://www.enzo.com/note/10-tips-for-optimizing-in-situ-hybridization-ish/]
- 79. Hematology FISH protocol - Post-hybridization washes [https://www.ogt.com/us/resources/fish-resources-and-support/fish-support/hematology-fish-protocol-post-hybridization-washes/]
- 80. Comparison of RNA In Situ Hybridization and Immunohistochemistry Techniques for the Detection and Localization of SARS-CoV-2 in Human Tissues - PubMed [https://pubmed.ncbi.nlm.nih.gov/32826529/]
- 81. Comparison of Immunohistochemistry With Fluorescence ... [https://pubmed.ncbi.nlm.nih.gov/40407378/]
- 82. Automated, high-throughput in situ hybridization of sea urchin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12516323/]
- 83. ISSX 2025 - Optimization of High-Throughput Transfection ... [https://dls.com/resources/issx-2025-optimization-of-high-throughput-transfection-protocols-for-mrna-delivery-and-sirna-knockdown-in-mouse-and-human-hepatocytes/]
- 84. Protocol for Making a 4% Formaldehyde Solution in PBS [https://www.rndsystems.com/resources/protocols/protocol-making-4-formaldehyde-solution-pbs]
- 85. Fixation Strategies and Formulations Used in IHC Staining [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/fixation-strategies-formulations.html]
- 86. Popular Types of Fixatives used in Histopathology [https://www.leicabiosystems.com/us/knowledge-pathway/fixation-and-fixatives-4-popular-fixative-solutions/]
- 87. Comparison of Fixation Methods for Preservation of ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3201123/]
- 88. Comparative Evaluation of Formalin and Alcohol-Based ... [https://icr-heart.com/article/comparative-evaluation-of-formalin-and-alcohol-based-fixatives-on-tissue-morphology-and-immunostaining-in-routine-histopathology-2432/]
- 89. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 90. IHC detection systems: Advantages and Disadvantages [https://www.bio-techne.com/applications/imaging/immunohistochemistry/ihc-detection]
- 91. IHC or IF: Which is Best for My Study? [https://www.stagebio.com/blog/ihc-or-if-which-is-best-for-my-study]
- 92. Multiplex immunohistochemistry (mIHC): A technical deep ... [https://www.abcam.com/en-us/knowledge-center/immunohistochemistry/multiplex-immunohistochemistry-mihc]
- 93. PICASSO allows ultra-multiplexed fluorescence imaging of ... [https://www.nature.com/articles/s41467-022-30168-z]
- 94. Multiplex imaging analysis of the tumor immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1617906/full]
- 95. A quantitative spatial cell-cell colocalizations framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11802768/]
- 96. Indirect clinical validation for predictive biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488805/]
- 97. From Biomarker to Clinical Trial Assay [https://www.precisionformedicine.com/blog/immunohistochemistry-precision-medicine-biomarker-clinical-trial-assay]
- 98. A critical evaluation of strategies used for validation ... [https://www.sciencedirect.com/science/article/pii/S1574789114000568]
- 99. Companion Diagnostics [https://www.fda.gov/medical-devices/in-vitro-diagnostics/companion-diagnostics]
- 100. An introduction to diagnostic testing in laboratories [https://www.thermofisher.com/us/en/home/clinical/clinical-genomics/molecular-diagnostics/diagnostic-testing-laboratories-intro.html]
- 101. What is an LDT?: Laboratory developed test definition [https://www.ideagen.com/thought-leadership/blog/laboratory-developed-test-definition]
- 102. Regulatory Perspectives - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK195940/]
- 103. Types of in Vitro Diagnostics: Clearing up the Confusion [https://versiticlinicaltrials.org/resources/insights/types-of-in-vitro-diagnostics-clearing-up-the-confusion]
- 104. Comparison of Laboratory-Developed Tests and FDA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6145687/]
- 105. Laboratory-Developed Tests (LDTs) [https://worldwide.promega.com/products/molecular-diagnostics/ldt-education/]
- 106. Quantitation of Protein Expression and Co-localization Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4913774/]
- 107. HER2 testing results, practices, and preferences among ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638377/]
- 108. HER2 IHC scoring concordance in breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969812/]
- 109. New Findings Show Standard HER2 Assays Miss Key ... [https://www.pharmacytimes.com/view/new-findings-show-standard-her2-assays-miss-key-her2-low-cases]
- 110. CAP Breast Biomarker Reporting Template Update [https://www.her2know.com/newsletter/cap-breast-biomarker-report-mar-2025-update.html]
- 111. Enhancing HER2-low breast cancer detection with ... [https://www.nature.com/articles/s41523-025-00817-9]
- 112. Diagnostic accuracy of next-generation sequencing (NGS) ... [https://link.springer.com/article/10.1007/s12094-025-04040-7]
- 113. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 114. NGS coverage accurately predicts MET and HER2 (ERBB2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12340238/]
- 115. Protocol for multiplex whole-mount RNA fluorescence in situ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509983/]
- 116. Spatial Multiomics Simplified: Same-Tissue Co-Detection ... [https://acdbio.com/2024-nov-14-spatial-multiomics-simplified-same-tissue-co-detection-rna-and-protein-confidence-using]
- 117. Costs of biomarker testing in advanced nonâ€small cell lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11886603/]
- 118. Economic assessment of NGS testing workflow for NSCLC ... [https://www.sciencedirect.com/science/article/pii/S2405844024053039]
- 119. Review of In Situ Hybridization Techniques for Drug Research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10467011/]
- 120. Immunohistochemistry Market Share & Opportunities 2025- ... [https://www.coherentmarketinsights.com/market-insight/immunohistochemistry-market-4795]
- 121. Immunohistochemistry Market Size & Growth Forecast to ... [https://www.marketsandmarkets.com/Market-Reports/immunohistochemistry-market-121632939.html]
- 122. The effect of different scanning protocols on precision ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11559108/]
- 123. Top 10 AI Radiology Analysis Tools in 2025 [https://www.devopsschool.com/blog/top-10-ai-radiology-analysis-tools-in-2025-features-pros-cons-comparison/]
- 124. Validation of Fluorescence in Situ hybridization (FISH) ... [https://www.lidsen.com/journals/genetics/genetics-07-01-177]
- 125. $2.35 Billion by 2030: Why In Situ Hybridization Is ... [https://www.prnewswire.com/news-releases/2-35-billion-by-2030-why-in-situ-hybridization-is-revolutionizing-molecular-diagnostics--marketsandmarkets-302499850.html]