Strategies to Minimize Embryo Degeneration in Intracytoplasmic Sperm Injection: From Foundational Mechanisms to Clinical Applications
This article provides a comprehensive analysis of the causes and innovative solutions for reducing embryo degeneration following intracytoplasmic sperm injection (ICSI), a significant challenge in assisted reproductive technology.
Strategies to Minimize Embryo Degeneration in Intracytoplasmic Sperm Injection: From Foundational Mechanisms to Clinical Applications
Abstract
This article provides a comprehensive analysis of the causes and innovative solutions for reducing embryo degeneration following intracytoplasmic sperm injection (ICSI), a significant challenge in assisted reproductive technology. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational knowledge on oocyte damage mechanisms with cutting-edge methodological advances such as PIEZO-ICSI and cumulus cell-based sperm selection. The scope extends to troubleshooting through non-invasive biomarkers and pharmacological interventions, alongside rigorous validation of emerging techniques against conventional ICSI. By integrating foundational, methodological, optimization, and comparative perspectives, this review aims to equip professionals with the multidisciplinary knowledge needed to develop safer, more effective ICSI protocols and improve clinical outcomes.
Understanding Embryo Degeneration: Core Mechanisms and Contributing Factors in ICSI
This technical support center provides researchers and scientists with targeted troubleshooting guides and FAQs, specifically framed within the thesis research on reducing embryo degeneration post-intracytoplasmic sperm injection (ICSI). The content focuses on the core biomechanical challenges of conventional ICSI—namely, the forced aspiration of ooplasm and the subsequent damage to the oolemma. The guides below synthesize current research and data to help diagnose issues, optimize protocols, and improve experimental outcomes.
Frequently Asked Questions (FAQs)
1. What are the primary biomechanical causes of oocyte degeneration during conventional ICSI? The main causes are the mechanical forces required to rupture the oolemma. Conventional ICSI uses a sharp, bevelled needle and requires the aspiration of ooplasm to ensure rupture. This process physically displaces intracellular components and can cause sudden breakage and cytoplasmic leakage, leading to immediate degeneration [1] [2]. The fragility of the oolemma and the cytoplasmic viscosity of the specific oocyte are also contributing factors [1].
2. How does the injection technique influence oocyte stress? The technique is a critical variable. In conventional ICSI, the practitioner must use mechanical force and ooplasmic aspiration, which introduces significant variability. The angle of injection, the speed of aspiration, and the force applied can differ between practitioners and even between injections, leading to inconsistent outcomes and potential damage [3] [4]. Furthermore, the positioning of the oocyte during injection, traditionally with the polar body at 6 or 12 o'clock, is based on an assumed location of the meiotic spindle, which is not always accurate, risking spindle damage and aneuploidy [3].
3. Does oocyte degeneration in a cohort predict the developmental potential of sibling oocytes? No, cycle-based evidence indicates that the degeneration of some oocytes after ICSI is not a reliable indicator of the cumulative live birth rate for the entire cohort in young women. The developmental potential of the surviving sibling oocytes remains uncompromised [1].
4. What are the key performance indicators (KPIs) to monitor for ICSI optimization? Embryologists should track several KPIs to monitor laboratory performance. Key indicators include [5] [4]:
- Normal fertilization rate (2PN rate)
- Oocyte degeneration rate post-ICSI
- Cleavage rate
- Blastulation rate
- Implantation rate A drop in these metrics, particularly the implantation rate, can signal a systemic problem in the ICSI process that requires root cause analysis [4].
Troubleshooting Guides
Guide 1: Addressing High Oocyte Degeneration Rates
Problem: A high rate of oocyte degeneration is observed immediately after conventional ICSI, characterized by oocyte lysis or dark, retracted ooplasm the following day [1].
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Over-aspiration of ooplasm | Review video recordings of ICSI procedure to assess aspiration volume and timing. | Standardize the aspiration volume to the minimal amount required for oolemma breakage. Train staff on this standardized protocol. |
| Suboptimal oolemma breakage | Document the frequency of "difficult" oolemma breakage and the need for multiple aspiration attempts. | Consider adopting PIEZO-ICSI, which uses a blunt pipette and piezoelectric pulses to cleanly penetrate the zona pellucida and oolemma without aspiration, significantly reducing degeneration [6] [2]. |
| Inherent oocyte factors | Correlate degeneration rates with patient factors (e.g., age, diagnosis) and stimulation protocols. | While inherent oocyte quality is a factor, optimizing the stimulation protocol and ensuring consistent lab conditions can maximize oocyte resilience [1]. |
Guide 2: Addressing Low Fertilization Rates Despite Successful Injection
Problem: Oocytes survive ICSI but fail to fertilize normally.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Damage to the meiotic spindle | Use a polarized light microscope (if available) to visualize the spindle and confirm its location relative to the injection site. | If using conventional ICSI, avoid the 3 and 9 o'clock positions for sperm deposition. Some studies suggest positioning the polar body at 7 or 11 o'clock may reduce spindle damage [3]. |
| Improper sperm immobilization | Verify that sperm are properly immobilized prior to injection to ensure oocyte activation. | Ensure a rigorous sperm immobilization technique is followed consistently by all practitioners [7]. |
| Suboptimal timing of ICSI | Review the time interval between oocyte retrieval, denudation, and ICSI. | Perform ICSI within a consistent and optimized window post-retrieval. Evidence suggests that the timing of ICSI post-retrieval can impact outcomes [3]. |
The following tables summarize key experimental data comparing conventional ICSI and PIEZO-ICSI, a technology designed to mitigate biomechanical stress.
| Outcome Measure | Conventional ICSI | PIEZO-ICSI | P-value |
|---|---|---|---|
| Normal Fertilization Rate | 65.6% - 72.6% | 71.6% - 78.0% | < 0.05 |
| Oocyte Degeneration Rate | 6.3% - 12.1% | 3.2% - 6.3% | < 0.01 |
| Outcome Measure | Conventional ICSI | PIEZO-ICSI | P-value |
|---|---|---|---|
| Top Quality Blastocysts (Day 5) | 27.5% - 43.9% | 33.3% - 50.3% | < 0.05 |
| Fertilized Oocytes with Developmental Arrest | 2.48% | 1.20% | Not Significant |
Experimental Protocols
Protocol 1: PIEZO-ICSI for Reducing Ooplasmic Aspiration
Principle: Replace the mechanical force of a sharp needle with piezoelectric pulses to minimize cytoplasmic displacement and oolemma damage [2].
Materials:
- PIEZO-driven micromanipulation system
- Blunt-ended injection pipette (inner diameter ~5-6 µm)
- Polyvinylpyrrolidone (PVP) solution for sperm handling
Methodology:
- Oocyte Preparation: Denude cumulus-oocyte complexes using hyaluronidase. Select metaphase II (MII) oocytes for injection.
- Sperm Preparation: Immobilize a single spermatozoon by crushing its tail with the injection pipette in a PVP droplet.
- PIEZO Settings: Apply a low-intensity piezoelectric pulse to the blunt pipette to advance it through the zona pellucida without distortion.
- Oolemma Penetration: Position the pipette tip against the oolemma. Apply a single, high-speed, but low-amplitude piezoelectric pulse to rupture the oolemma at the point of contact. Crucially, this step requires no ooplasmic aspiration.
- Sperm Deposition: Gently expel the sperm into the ooplasm and withdraw the pipette smoothly.
Protocol 2: Meiotic Spindle Visualization for Injection Site Selection
Principle: Use polarized light microscopy to directly visualize the meiotic spindle, thereby avoiding it during sperm injection and reducing the risk of aneuploidy [3].
Materials:
- Inverted microscope equipped with a polarized light optics system (e.g., PolScope)
- Environmentally controlled stage to maintain 37°C
Methodology:
- After denudation, transfer the MII oocyte to a culture droplet on the PolScope stage.
- Spindle Imaging: Rotate the oocyte using the holding pipette to locate the meiotic spindle, which appears as a birefringent structure under polarized light.
- Injection Planning: Position the oocyte so that the planned injection trajectory (e.g., at the 3 o'clock position) is diametrically opposite to the visualized spindle.
- Proceed with ICSI (conventional or PIEZO) in the planned safe zone.
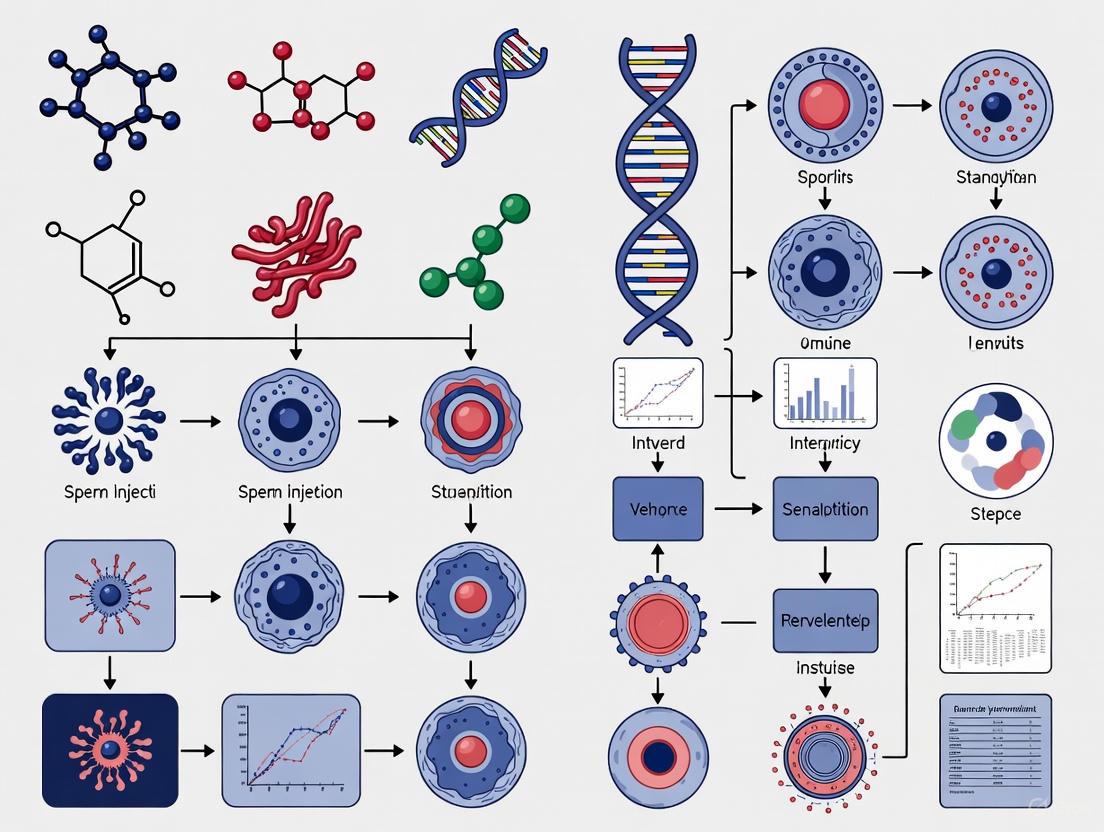
Visualization of Concepts and Workflows
Biomechanical Stress in Conventional vs. PIEZO-ICSI
Root Cause Analysis for ICSI Degeneration
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research | Application Note |
|---|---|---|
| PIEZO-ICSI System | Enables microinjection with minimal biomechanical stress by using ultrasonic pulses for penetration, eliminating the need for ooplasmic aspiration. | The core technology for mitigating ooplasmic aspiration and oolemma damage. Significantly reduces degeneration rates compared to conventional ICSI [6] [2]. |
| PolScope / SpindleView System | A non-invasive polarized light microscopy system for visualizing the meiotic spindle in live oocytes. | Allows for the precise positioning of the oocyte to avoid spindle damage during injection, potentially reducing aneuploidy [3]. |
| Hyase (Hyaluronidase) | Enzyme used to remove cumulus cells from the retrieved oocyte-cumulus complex (denudation). | The time of oocyte exposure to hyaluronidase should be minimized (e.g., < 20 seconds) to reduce chemical stress on the oocyte [1]. |
| Polyvinylpyrrolidone (PVP) | A viscous solution used to slow down sperm for easier selection and immobilization during ICSI. | A standard component of ICSI, though research into more physiological alternatives is ongoing [7]. |
| Stable Temperature Equipment | Heated stages and chambers to maintain a constant 37°C environment for oocytes outside the incubator. | Critical for oocyte viability. Temperature fluctuations are a known, silent threat to oocyte quality [5] [4]. |
| (-)-Epiafzelechin | (-)-Epiafzelechin|High-Purity Reference Standard | (-)-Epiafzelechin is a flavan-3-ol for research on bone health, inflammation, and metabolic diseases. This product is for Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Glucoraphanin | Glucoraphanin | High-purity Glucoraphanin, the precursor to Sulforaphane. Explore its research value in cell signaling and detoxification pathways. For Research Use Only. Not for human consumption. |
Frequently Asked Questions (FAQs) for Researchers
1. What is the typical baseline oocyte degeneration rate after ICSI, and what factors influence it? Reported degeneration rates after conventional ICSI typically range from 5% to 19% [1] [2]. Key non-modifiable patient factors influencing this rate include basal Day 3 FSH levels, the number of mature oocytes retrieved, and estradiol (E2) levels on the day of hCG trigger [8] [9]. Physician-adjustable ovarian stimulation variables are not significant independent predictors [8] [9].
2. Does the presence of a degenerated oocyte in a cohort indicate poorer quality of the sibling oocytes? The answer may depend on the insemination method. In conventional IVF cycles, the presence of oocyte degeneration is an indicator of poorer overall cohort quality, leading to significantly lower cumulative live birth rates [10]. However, in ICSI cycles for young women, the presence of oocyte degeneration does not appear to predict the developmental potential of sibling oocytes, with studies showing comparable cumulative live birth rates between cycles with and without degeneration [1].
3. What laboratory techniques can directly reduce the oocyte degeneration rate? Implementing PIEZO-ICSI is a proven method. This technique uses a piezoelectric pulse to perforate the oolemma instead of mechanical puncturing and cytoplasmic aspiration. Studies consistently show it significantly reduces degeneration rates compared to conventional ICSI [6] [2].
4. Beyond degeneration, what other embryo development metrics are improved with PIEZO-ICSI? Compared to conventional ICSI, PIEZO-ICSI is associated with a higher normal fertilization rate [6] [2] and can lead in an increased number of high-quality blastocysts [6]. Some studies also report a higher blastocyst formation rate on Day 5 [2].
Troubleshooting Guide: Managing and Reducing Oocyte Degeneration
Common Problems & Solutions
| Problem | Possible Cause | Recommended Solution | Key Experimental Evidence |
|---|---|---|---|
| High Degeneration Rate (>10%) with Conventional ICSI | Inherent oocyte quality/fragility; Technical invasiveness of procedure. | Implement PIEZO-ICSI to minimize physical damage to the oolemma. | A sibling oocyte split trial (N=108) showed degeneration decreased from 12.1% (Conventional ICSI) to 6.3% (PIEZO-ICSI) [6]. |
| Variable Degeneration Rates Between Operators | Technician-dependent mechanical skill in membrane puncture. | Standardize injection technique. Training should emphasize minimal cytoplasmic aspiration. | A multivariate analysis of 6,653 injected oocytes found the ICSI technician was not a significant predictor of degeneration rate, suggesting inherent oocyte quality is a stronger factor [8] [9]. |
| Poor Embryo Development Despite Acceptable Fertilization | Sublethal oocyte damage during injection affecting later development. | Adopt PIEZO-ICSI to preserve cytoplasmic integrity. | One study found that while fertilization was similar, PIEZO-ICSI resulted in a higher number of grade A and B quality blastocysts (33.3% vs. 27.5%) [6]. |
| Degenerated Oocytes at OPU in Conventional IVF | Needle gauge or aspiration pressure during oocyte retrieval; Oocyte cohort quality. | Review OPU technique. The presence of degenerated oocytes at this stage is a significant marker of poorer embryo development potential in conventional IVF [10]. | A study of 399 cycles found the use of a GnRH agonist protocol and specific needle gauge (17-20G) were predictors for degenerated oocytes at retrieval [11]. |
Detailed Experimental Protocol: Sibling Oocyte Split Trial Comparing ICSI Techniques
This protocol is designed to quantify the impact of different ICSI techniques on oocyte degeneration within the same patient, thereby controlling for patient-specific variables.
Objective: To compare the oocyte degeneration rate, fertilization rate, and subsequent embryo development between conventional ICSI and PIEZO-ICSI.
Materials List:
- PIEZO-ICSI Unit: Comprising a controller and a piezoelectric actuator mounted on the micromanipulator.
- Injection Pipettes (Blunt-ended): Specifically designed for use with the PIEZO system to avoid sharp punctures.
- Conventional ICSI Pipettes (Sharp): Standard sharp-tipped injection pipettes.
- Hyaluronidase Solution: For cumulus cell removal.
- Time-Lapse Incubator (Optional but recommended): For continuous, undisturbed culture and detailed morphokinetic analysis of embryos.
Methodology:
- Oocyte Collection and Denudation: Perform ovum pick-up (OPU) 35-36 hours post-hCG trigger. Treat cumulus-oocyte complexes with hyaluronidase and mechanically remove corona cells to identify maturity.
- Randomization and Grouping: Select only metaphase II (MII) oocytes for the trial. For a patient with an even number of oocytes, randomly split the cohort into two equal groups. If the number is uneven, assign the extra oocyte to the conventional ICSI group. The order of the injection technique used first should also be randomized to prevent bias [6].
- Micromanipulation:
- Conventional ICSI Group: Perform ICSI according to standard lab protocol. Position the polar body at 6 or 12 o'clock, puncture the zona pellucida and oolemma with a sharp pipette using a single, swift motion, and aspirate cytoplasm gently to confirm membrane rupture before sperm deposition.
- PIEZO-ICSI Group: Position the oocyte similarly. Use the PIEZO unit to apply a controlled pulse to advance a blunt-ended pipette through the zona pellucida without touching the oolemma. Position the pipette against the oolemma and apply a very short, low-intensity piezo pulse to rupture it. Minimize or avoid cytoplasmic aspiration before depositing the sperm [2].
- Post-Injection Culture and Assessment:
- Culture all injected oocytes and assess for degeneration and fertilization 16-18 hours post-injection.
- Degeneration Definition: Identify oocytes that show immediate lysis post-injection or display a retracted and/or darkened ooplasm at the fertilization check [10] [1].
- Culture fertilized oocytes (2PN) to the blastocyst stage using standard media and conditions.
- Assess blastocysts on Days 5 and 6 using the Gardner grading system or a similar standardized morphological assessment.
Outcome Measures and Data Analysis:
- Primary Outcome: Oocyte degeneration rate.
- Secondary Outcomes: Normal fertilization (2PN) rate, blastocyst formation rate, and utilization rate (number of blastocysts suitable for transfer or cryopreservation per injected oocyte).
- Statistical Analysis: Use paired t-tests or Chi-square tests to compare outcomes between the two groups within the same patient. A p-value of <0.05 is considered statistically significant.
Table 1: Comparative Outcomes of Conventional ICSI vs. PIEZO-ICSI from Clinical Studies
| Parameter | Conventional ICSI | PIEZO-ICSI | P-value | Study |
|---|---|---|---|---|
| Oocyte Degeneration Rate | 12.1% | 6.3% | <0.05 | [6] |
| Oocyte Degeneration Rate | 6.3% | 3.2% | 0.0055 | [2] |
| Normal Fertilization (2PN) Rate | 65.6% | 71.6% | <0.05 | [6] |
| Normal Fertilization (2PN) Rate | 72.6% | 78.0% | 0.0176 | [2] |
| High-Quality Blastocyst Rate | 27.5% | 33.3% | <0.05 | [6] |
| Day 5 Blastocyst Formation Rate | 43.9% | 50.3% | 0.0367 | [2] |
Table 2: Impact of Oocyte Degeneration on Cumulative Live Birth Rate (CLBR)
| Insemination Method | Group | Cumulative Live Birth Rate | Adjusted Odds Ratio (95% CI) for CLBR | Study |
|---|---|---|---|---|
| Conventional IVF | Degeneration Group | 70.2% | 0.82 (0.72–0.93) | [10] |
| Conventional IVF | Non-Degeneration Group | 74.0% | Reference | [10] |
| ICSI (Women <35) | Degeneration Group | 63.4% | Not Significant | [1] |
| ICSI (Women <35) | Non-Degeneration Group | 64.8% | Reference | [1] |
Research Reagent Solutions
Table 3: Essential Materials for PIEZO-ICSI and Oocyte Quality Research
| Item | Function/Application | Example/Note |
|---|---|---|
| PIEZO-ICSI Unit | Provides controlled vibrations for a less invasive oolemma puncture, reducing mechanical damage. | Consists of a controller and an actuator mounted on the micromanipulator. |
| Blunt-Ended Injection Pipettes | Used with the PIEZO unit to penetrate the zona pellucida and oolemma without a sharp cut. | Typically have an inner diameter of 5-6 µm [1]. |
| Polarized Light Microscopy | Non-invasively visualizes the meiotic spindle to aid in injection positioning and assess oocyte maturity. | Used in some studies to select mature oocytes with a visible spindle for injection [2]. |
| Time-Lapse Incubator System | Allows continuous culture and monitoring of embryo development without removing from stable conditions. | Enables detailed morphokinetic analysis (e.g., KID Score, ESHRE Score) to compare embryo quality between groups [11]. |
| Vitrification Kit | For the cryopreservation of blastocysts using the Cryotop method or similar, to assess utilization rates. | Essential for calculating cumulative outcomes like CLBR [1]. |
Experimental Workflow Visualization
Sperm DNA Fragmentation (SDF) refers to the presence of single or double-stranded breaks in the genetic material of spermatozoa. This condition is increasingly recognized as a critical biomarker of male infertility, independent of traditional semen analysis parameters like concentration, motility, and morphology. In assisted reproductive technology (ART), particularly intracytoplasmic sperm injection (ICSI), high levels of SDF have been associated with impaired embryo development, despite the technique's ability to bypass natural selection barriers [12] [13]. Understanding SDF mechanisms and their clinical implications is essential for reducing embryo degeneration post-ICSI and improving overall treatment outcomes.
Key Questions & Troubleshooting Guides
FAQ 1: How does sperm DNA fragmentation affect early embryo development?
Sperm DNA fragmentation negatively impacts several critical stages of early embryogenesis, even when using ICSI.
- Impact on Fertilization and Cleavage Stages: While some studies indicate that fertilization rates may not be significantly affected, the integrity of the paternal genome becomes crucial as the embryo starts dividing [12] [14]. The oocyte's repair mechanisms can correct a certain amount of DNA damage, but this capacity is limited.
- Impact on Blastulation: High SDF is strongly correlated with reduced blastocyst formation (blastulation). A 2017 study found a significant negative correlation (R = -0.5) between DNA fragmentation levels and blastulation rates. Embryos derived from sperm with high DNA damage are less likely to develop to the blastocyst stage [12].
- Activation of Apoptotic Pathways: Sperm with high DNA fragmentation can induce cellular stress in the developing embryo. Research shows that blastomeres from such embryos have a higher incidence of activating the apoptotic pathway (programmed cell death), leading to embryo arrest and degeneration [12]. Samples with high SDF (TUNEL ≥15%) resulted in 21.9% of blastomeres activating apoptosis, compared to only 16.4% in low SDF samples [12].
FAQ 2: Does high SDF lead to increased embryonic aneuploidy?
Yes, elevated SDF levels are associated with a higher risk of embryonic aneuploidy (an abnormal number of chromosomes).
- Evidence from PGT Cycles: A large retrospective study on couples undergoing ICSI with Preimplantation Genetic Testing (PGT) found that an SDF value greater than 30% was a significant predictor of embryonic aneuploidy [15].
- Threshold and Risk: The study established a cut-off value of 30.36% SDF using the Receiver Operating Characteristic (ROC) curve analysis. Patients with SDF above this threshold had a significantly higher risk of producing aneuploid embryos, which are a major cause of implantation failure and early pregnancy loss [15].
FAQ 3: What is the relationship between SDF and clinical pregnancy outcomes?
The influence of SDF on clinical pregnancy and miscarriage rates is complex and depends on several factors.
- Early Embryo Development vs. Pregnancy: A 2025 study of 870 ICSI cycles concluded that while SDF significantly impairs early embryological outcomes (fertilization and blastocyst development), it was not a strong independent predictor of clinical pregnancy rates after accounting for other variables [13] [16]. However, it showed a borderline significant relationship with increased miscarriage rates [13].
- Miscarriage Risk: A 2024 comprehensive analysis of 6,330 IVF/ICSI cycles provided clearer evidence, demonstrating a positive correlation between SDF and miscarriage rates. The risk of miscarriage increased progressively with higher SDF levels [14].
- Offspring Safety: The same large-scale study also found a statistically significant negative correlation between sperm DFI and infant birth weight, highlighting potential long-term impacts on offspring health [14].
FAQ 4: Can the oocyte repair sperm DNA damage?
The oocyte possesses a remarkable, albeit limited, capacity to repair DNA damage in the fertilizing sperm.
- Critical Repair Window: Following fertilization, the oocyte's repair machinery is activated and remains the primary mechanism for correcting sperm DNA damage until the embryonic genome is activated (around the 4- to 8-cell stage in humans) [17].
- Repair Capacity is Limited: The oocyte's repair capacity is finite. It has been postulated that oocytes can effectively repair damage only when the SDF level does not exceed approximately 8% [17]. When the damage surpasses the oocyte's reparability, it can lead to failed fertilization, embryo arrest, or trigger apoptosis [12] [17].
- Dependence on Oocyte Quality: The efficiency of this repair process is heavily influenced by the quality of the oocyte, which is often linked to maternal age. A decline in oocyte quality with advanced maternal age corresponds to a reduced capacity to repair sperm DNA damage, exacerbating the negative effects of SDF [17].
FAQ 5: Which laboratory techniques can help mitigate the effects of SDF?
Several advanced laboratory techniques can be employed to select better sperm or reduce oocyte damage during ICSI.
- PIEZO-ICSI: This technique uses a piezoelectric actuator to create high-speed vibrations for a blunt pipette to penetrate the zona pellucida, instead of a sharp pipette and mechanical pressure used in conventional ICSI.
- Benefits: Significantly reduces mechanical stress on the oocyte, leading to lower oocyte degeneration rates (6.3% vs. 12.1%) and higher fertilization rates (71.6% vs. 65.6%) compared to conventional ICSI [6] [18].
- Outcome: While it may not directly change the SDF level, by causing less trauma to the oocyte, it may help preserve its inherent repair capacity, resulting in more transferable embryos and higher blastocyst quality [6].
- Advanced Sperm Selection Techniques: Technologies like microfluidic sperm sorters can help select sperm with lower DNA fragmentation, better motility, and morphology. Physiological sperm selection methods, such as exposing sperm to the cumulus cell secretome, have also been shown to reduce DNA damage [13].
The following tables consolidate key quantitative findings from recent clinical studies on SDF.
Table 1: Impact of SDF on Embryological and Clinical Outcomes (Large-Scale Studies)
| Outcome Measure | Study 1 (2025): 870 ICSI cycles [13] [16] | Study 2 (2024): 6,330 IVF/ICSI cycles [14] |
|---|---|---|
| Fertilization Rate | Each 1% SDF increase reduced odds of FR>80% by 1.6% (OR=0.984) | No significant difference found |
| Blastocyst Quality | Each 1% SDF increase reduced odds of top-quality blastocysts by 2.5% (OR=0.975) | Not Specified |
| Clinical Pregnancy | No significant association found (OR=0.989) | No significant difference found |
| Miscarriage Rate | Borderline significant increase (OR=0.961, p=0.053) | Significant increase, positively correlated with DFI (OR=1.095) |
| Birth Weight | Not Reported | Significant decrease, negatively correlated with DFI (OR=0.913) |
Table 2: SDF Thresholds and Associated Risks
| SDF Threshold | Associated Risk and Clinical Impact | Supporting Evidence |
|---|---|---|
| SDF > 20% | Associated with reduced semen quality and poorer blastocyst development. | [13] |
| SDF ≥ 30% | Significantly associated with lower blastulation rates and a higher risk of embryonic aneuploidy. | [12] [15] |
| SDF ~8% | Postulated upper limit for efficient repair by the oocyte. Damage beyond this level exceeds repair capacity. | [17] |
Essential Experimental Protocols
Protocol 1: Assessing Apoptotic Markers in Arrested Embryos
This protocol is used to investigate the mechanism of embryo arrest in research settings.
- 1. Embryo Collection and Preparation: Collect arrested or surplus human embryos donated for research with informed consent. Fix embryos in 2% formaldehyde for 45 minutes. To prepare for immunostaining, the zona pellucida is dissolved by brief incubation in acidic Tyrode's solution [12].
- 2. Immunocytochemistry (ICC): Perform ICC to detect key apoptotic markers.
- Cleaved Caspase-3 (CC3): An executor of apoptosis. Use a rabbit monoclonal anti-CC3 antibody (e.g., Cell Signaling) at a 1:100 dilution.
- Survivin: An apoptosis inhibitor. Use a mouse monoclonal anti-Survivin antibody (e.g., Novus Biologicals) at a 1:100 dilution.
- Visualization: Use appropriate Alexa Fluor-conjugated secondary antibodies.
- 3. TUNEL Assay: Perform the TUNEL (Terminal deoxynucleotidyl transferase dUTP Nick End Labeling) assay to directly label DNA strand breaks, using a commercial kit (e.g., from Roche).
- 4. DNA Staining and Analysis: Counterstain the DNA with a fluorescent stain like Hoechst 33258. Analyze the embryos under a fluorescence microscope to quantify the co-localization of DNA fragmentation (TUNEL) and apoptotic markers (CC3) [12].
Protocol 2: Sperm Chromatin Dispersion (SCD) Test for SDF
A common method for quantifying sperm DNA fragmentation.
- 1. Semen Sample Preparation: Obtain a fresh semen sample and process it using density gradient centrifugation or a simple wash to isolate motile sperm.
- 2. Agarose Embedding: Mix a small aliquot of the processed sperm with low-melting-point agarose to create a microgel on a pre-coated slide.
- 3. Denaturation and Lysis: Place the slide in an acidic denaturing solution to disrupt DNA strands at the sites of breaks. This is followed by immersion in a lysing solution to remove membranes and proteins.
- 4. Staining and Scoring: Stain the DNA with a fluorescent dye (e.g., DAPI) or a specific DNA stain (e.g., Wright's stain). Sperm with non-fragmented DNA will display large halos of dispersed DNA loops, while sperm with fragmented DNA will show very small or no halos. A minimum of 500 sperm should be scored to calculate the DFI percentage [13] [16].
Visualizing Key Concepts
Diagram 1: Sperm DNA Fragmentation and Embryo Developmental Pathways
This diagram illustrates the two potential pathways an embryo can take based on the level of sperm DNA fragmentation and the oocyte's repair capacity.
Diagram 2: Oocyte-Mediated DNA Repair Mechanism
This diagram outlines the key steps and molecules involved in the oocyte's repair of sperm DNA damage after fertilization.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for SDF and Embryo Competence Research
| Reagent / Kit | Primary Function in Research | Example Application |
|---|---|---|
| TUNEL Assay Kit | Enzymatically labels DNA strand breaks for direct visualization and quantification of fragmentation. | Detecting SDF in sperm samples and DNA breaks in individual blastomeres of arrested embryos [12]. |
| Anti-Cleaved Caspase-3 Antibody | Detects the activated form of Caspase-3, a key enzyme in the execution phase of apoptosis. | Immunocytochemistry on embryos to confirm the activation of apoptotic pathways in relation to high SDF [12]. |
| Anti-Survivin Antibody | Detects Survivin, an inhibitor of apoptosis protein. Useful for studying the balance between cell death and survival. | Co-staining with apoptotic markers to understand the embryo's response to DNA damage stress [12]. |
| Sperm Chromatin Dispersion (SCD) Kit | Provides reagents for a simple and reliable method to assess sperm DNA fragmentation based on halo formation. | Routine screening and quantification of SDF in patient semen samples prior to ART cycles [13]. |
| Hyaluronidase | Enzyme used to remove cumulus cells from the oocyte, a necessary step before ICSI or morphological assessment. | Preparing denuded oocytes for ICSI or for research on oocyte quality [1] [19]. |
| PIEZO-ICSI Unit | Micromanipulation system that uses piezoelectric pulses for oocyte membrane penetration instead of mechanical force. | Research aimed at reducing oocyte degeneration and improving outcomes in cases of previous ICSI failure or high SDF [6] [18]. |
| Homoarbutin | Homoarbutin CAS 25712-94-1 - Supplier | High-purity Homoarbutin for research applications. CAS 25712-94-1, Molecular Formula C13H18O7. For Research Use Only. Not for human or veterinary use. |
| Eucalyptin | Eucalyptin, CAS:3122-88-1, MF:C19H18O5, MW:326.3 g/mol | Chemical Reagent |
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary cellular causes of embryo degeneration following Intracytoplasmic Sperm Injection (ICSI)? The primary cellular causes are mechanical damage to oocyte structures and oxidative stress. Conventional ICSI uses a sharp, bevelled needle that deforms the oocyte and increases internal pressure, which can lead to physical damage of the meiotic spindle and other organelles, resulting in oocyte degeneration [18]. Additionally, imbalances in reactive oxygen species (ROS) within the follicular fluid, the oocyte's developmental microenvironment, can cause oxidative stress, damaging DNA, cell membranes, and proteins, thereby reducing oocyte quality and developmental competence [20].
FAQ 2: How can we reduce mechanical damage to oocytes during the ICSI procedure? Adopting the PIEZO-ICSI technique significantly reduces mechanical damage. This method uses a piezoelectric actuator to create high-speed vibrations, allowing a blunt injection pipette to penetrate the zona pellucida smoothly without deforming the oocyte. This eliminates the need for forceful physical pressure and reduces the aspiration of ooplasm required to break the membrane with conventional ICSI [18]. Furthermore, using polarized light microscopy to visualize the meiotic spindle ensures the injection is aligned with the spindle, avoiding this critical structure and preserving its function [21].
FAQ 3: What role does oxidative stress play in oocyte quality, and how can it be monitored? Oxidative stress, caused by an imbalance between reactive oxygen species (ROS) and the antioxidant system in follicular fluid, is a key factor negatively impacting oocyte quality and ART outcomes [20]. High ROS levels can damage the oocyte's DNA and cell membranes. It can be monitored by measuring oxidative stress biomarkers in follicular fluid, such as malondialdehyde (MDA) for lipid peroxidation, 8-OHdG for DNA oxidation, and the total antioxidant capacity (TAC) [20]. Direct measurement of ROS levels in follicular fluid provides predictive insights into oocyte health.
FAQ 4: For which patient populations are advanced ICSI techniques like PIEZO-ICSI most beneficial? Evidence suggests that patients with a history of poor outcomes from conventional ICSI benefit the most. This includes those with previous cycles resulting in low fertilization rates (<50%), high oocyte degeneration rates (>15%), or poor embryo utilization [18]. Significant improvements are also seen in patients of advanced maternal age (≥38 years), whose oocytes may have more fragile membranes [18], and in POSEIDON group 4 patients (older with diminished ovarian reserve) when ICSI is combined with meiotic spindle alignment [21].
Troubleshooting Guides
Guide 1: Addressing High Oocyte Degeneration Rates Post-ICSI
| Problem | Potential Causes | Recommended Solutions | Key Performance Indicators to Monitor |
|---|---|---|---|
| High Oocyte Degeneration | Mechanical damage from conventional ICSI needle [18] | Implement PIEZO-ICSI to use a blunt needle and reduce oocyte deformation [18] [22]. | Degeneration Rate: Target <10% [22]. |
| Damage to the meiotic spindle during injection [21] | Use polarized light microscopy for spindle visualization and injection alignment [21]. | Fertilization Rate [18]. | |
| Suboptimal timing of oocyte denudation/injection [4] | Review and standardize timings from trigger to denudation to injection (e.g., ensure 37 hours post-trigger for ICSI) [4]. | Embryo Utilization Rate [18]. |
Guide 2: Mitigating Oxidative Stress in the IVF Laboratory
| Problem | Potential Causes | Recommended Solutions | Key Biomarkers & Outcomes |
|---|---|---|---|
| Elevated Oxidative Stress | Imbalance in follicular fluid ROS/antioxidants [20] | Analyze follicular fluid for biomarkers (e.g., MDA, 8-OHdG, TAC) to assess patient-specific OS status [20]. | MDA Levels: Increase significantly from age 37 [20]. |
| Environmental contaminants (e.g., VOCs) in lab air [4] [5] | Implement rigorous air quality control and use volatile organic compound (VOC) filters in laboratory and theatre [4] [5]. | Fertilization Rate [20]. | |
| Culture conditions (e.g., high Oâ‚‚ levels) [20] | Use low-oxygen culture incubators (e.g., 5% Oâ‚‚) to mimic physiological conditions and reduce ROS generation [20]. | Embryo Quality / Blastocyst Rate [20] [23]. |
Experimental Protocols & Data
Protocol 1: Implementing PIEZO-ICSI
Methodology:
- Oocyte Preparation: Denude cumulus cells from metaphase II (MII) oocytes using hyaluronidase [18].
- Equipment Setup: Use a piezo-driven micromanipulation unit. The injection pipette should be blunt-ended and filled with a biocompatible operating fluid like perfluoro-n-octane, not polyvinylpyrrolidone (PVP), to slow sperm [18].
- Sperm Immobilization: Apply a few piezo pulses to the sperm tail's mid-piece to immobilize it [18].
- Zona Pellucida Penetration: Use gentle piezo pulses to drill through the zona pellucida without deforming the oocyte.
- Oolemma Penetration: Advance the blunt pipette smoothly into the ooplasm. The membrane will invaginate and break with a single piezo pulse, avoiding cytoplasmic aspiration.
- Sperm Deposition: Deposit a single immobilized sperm into the cytoplasm and withdraw the pipette gently [18].
Protocol 2: Meiotic Spindle-Aligned ICSI
Methodology:
- Spindle Visualization: After oocyte denudation, place the MII oocyte under an inverted microscope equipped with a polarized light optics (PolScope) system.
- Orientation: Rotate the oocyte so that the meiotic spindle is positioned at the 12 o'clock or 6 o'clock position.
- Injection: Perform the ICSI procedure (conventional or PIEZO) with the injection pipette aligned along the spindle's axis to minimize the risk of physical disruption [21].
- Post-injection: Confirm spindle integrity post-injection using the PolScope.
Summarized Quantitative Data
Table 1: PIEZO-ICSI vs. Conventional ICSI Outcomes
| Outcome Measure | Conventional ICSI | PIEZO-ICSI | P-value | Study |
|---|---|---|---|---|
| Fertilization Rate | 65.6% | 71.6% | Significant | Sibling Oocyte Trial [22] |
| Oocyte Degeneration Rate | 12.1% | 6.3% | Significant | Sibling Oocyte Trial [22] |
| Fertilization Rate (Poor-Prognosis) | 45.3% | 61.9% | <0.0001 | Retrospective Cohort [18] |
| Degeneration Rate (Poor-Prognosis) | 18.2% | 7.7% | 0.0001 | Retrospective Cohort [18] |
| Top-Quality Day 3 Embryos | Reference | Odds Ratio: 4.22 | <0.001 | Spindle-Aligned Study [21] |
Table 2: Impact of Sperm Oxidative Stress on IVF/ICSI in Mammalian Models
| Fertilization Method | Effect on Fertilization Rate | Effect on Blastocyst Rate | Review Findings |
|---|---|---|---|
| IVF | Negative (80% of studies) | Negative (100% of studies) | Significant reduction in embryo development [23]. |
| ICSI | Positive (75% of studies) | Positive (83% of studies) | Sperm oxidative stress is associated with better outcomes vs. IVF in models [23]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Advanced ICSI Research
| Reagent / Material | Function | Technical Notes |
|---|---|---|
| PIEZO-ICSI Unit | Provides high-frequency vibrations for precise, blunt microdrilling of the zona pellucida, minimizing oocyte deformation [18]. | Use with blunt-ended injection pipettes. Requires a biocompatible operating fluid. |
| Perfluoro-n-octane | A biocompatible, safe operating liquid for the PIEZO-ICSI injection pipette, replacing historically used but unsafe mercury or fluorinert [18]. | Ensures clinical safety while transmitting piezo pulses effectively. |
| Polarized Light Microscope (PolScope) | Enables non-invasive, real-time visualization of the meiotic spindle in living MII oocytes [21]. | Critical for aligning the ICSI procedure to avoid spindle disruption. |
| Hyaluronidase | Enzyme used to remove cumulus cells from the retrieved oocyte-cumulus complexes, a process known as denudation [18]. | Essential for preparing oocytes for ICSI. Concentration and exposure time must be optimized. |
| Malondialdehyde (MDA) Assay Kit | A key biomarker for measuring lipid peroxidation, indicating the level of oxidative stress damage in biological samples like follicular fluid [20]. | Higher MDA levels in follicular fluid are linked to poorer oocyte quality. |
| Total Antioxidant Capacity (TAC) Assay | Measures the cumulative action of all antioxidants present in follicular fluid, representing the fluid's ability to counteract oxidative stress [20]. | Results can be controversial; may not directly predict fertilization but is higher in pregnant patients. |
| Integerrimine N-oxide | Integerrimine N-oxide, CAS:85955-28-8, MF:C18H25NO6, MW:351.4 g/mol | Chemical Reagent |
| (+)-Intermedine | (+)-Intermedine, CAS:10285-06-0, MF:C15H25NO5, MW:299.36 g/mol | Chemical Reagent |
Signaling Pathways and Workflows
Diagram 1: Logical workflow depicting the relationship between cellular triggers, research interventions, and outcomes in reducing embryo degeneration.
Advanced Techniques and Protocols to Safeguard Embryo Viability
PIEZO-ICSI represents a significant technological advancement in intracytoplasmic sperm injection (ICSI) procedures. Unlike conventional ICSI (C-ICSI), which uses a sharp needle and requires cytoplasmic aspiration to breach the oolemma, PIEZO-ICSI utilizes piezoelectric pulses to drive a blunt-ended pipette with minimal physical disruption [24] [25]. This technique is particularly valuable for research aimed at reducing embryo degeneration, as it significantly decreases mechanical stress on oocytes during the injection process [24] [2].
Performance Data: PIEZO-ICSI vs. Conventional ICSI
The tables below summarize key comparative outcomes between PIEZO-ICSI and Conventional ICSI, demonstrating the potential of PIEZO-ICSI to improve early embryological outcomes.
Table 1: Key Embryological Outcome Comparisons
| Outcome Measure | PIEZO-ICSI | Conventional ICSI | P-value | Source |
|---|---|---|---|---|
| Normal Fertilization Rate | 78.0% | 72.6% | 0.0176 | [24] [2] |
| Oocyte Degeneration Rate | 3.2% | 6.3% | 0.0055 | [24] [2] |
| Blastocyst Formation Rate (Day 5) | 50.3% | 43.9% | 0.0367 | [24] [2] |
| Developmental Arrest of Zygotes | 1.20% | 2.48% | 0.1250 | [24] [2] |
Table 2: Age-Specific Efficacy of PIEZO-ICSI
| Patient Cohort | Outcome Measure | PIEZO-ICSI vs. C-ICSI | P-value | Source |
|---|---|---|---|---|
| Women >35 years | Fertilization Rate | Significantly Higher | 0.008 | [26] |
| Women >35 years | Blastocyst Development Rate (D5/D6) | Significantly Higher | 0.016 | [26] |
| Women ≤35 years | Fertilization & Blastocyst Rates | No Significant Difference | N/S | [26] |
Troubleshooting Common PIEZO-ICSI Challenges
FAQ 1: We are observing inconsistent oolemma penetration with the piezoelectric pulse. What could be the cause?
This is often related to incorrect pulse settings or pipette issues.
- Solution A: Calibrate Piezo Settings: The recommended pulse settings for the oolemma are a speed setting of 2.0 and an intensity setting of 1.0 [26]. Ensure these are correctly configured on your PIEZO unit (e.g., Prime Tech Ltd. PIEZO PMM4G).
- Solution B: Inspect and Replace the Pipette: Use ultrathin, flat-tip injection needles (e.g., ~6 µm outer diameter) [26]. A damaged or clogged tip can dampen the pulse energy. Regularly inspect pipettes under high magnification and replace them if any defects are visible.
FAQ 2: Our fertilization rates with PIEZO-ICSI are not improving as expected. What factors should we investigate?
Beyond technique mastery, focus on patient and sperm factors.
- Solution A: Analyze Patient Age: The benefits of PIEZO-ICSI are most pronounced in oocytes from women over 35, whose oocytes may have more fragile plasma membranes [26]. Stratify your outcome analysis by female age.
- Solution B: Assess Sperm DNA Integrity: High sperm DNA fragmentation (SDF) independently impairs fertilization and blastocyst development [13]. Each 1% increase in SDF can reduce the odds of a >80% fertilization rate by 1.6% [13]. Consider measuring SDF and using techniques like microfluidic sperm selection to mitigate this issue [13].
FAQ 3: The procedure feels slower than conventional ICSI. How can we improve efficiency without compromising oocyte health?
Efficiency gains should not come at the cost of increased oocyte exposure.
- Solution: Implement a Sperm Pre-Catching Workflow: A proven method is the Pre-Catching Sperm (PCS) technique. This involves identifying, immobilizing, and loading all sperm into the pipette before the oocytes are removed from the incubator [27]. This reduces oocyte exposure time outside the incubator by approximately 5 minutes, which has been shown to significantly lower degeneration rates (1.4% vs. 3.5%) and improve fertilization rates [27].
Detailed Experimental Protocol: Sibling Oocyte Study Design
This protocol is ideal for conducting an intra-laboratory validation of PIEZO-ICSI against conventional ICSI, controlling for patient-specific variables [26] [28].
1. Patient Selection and Oocyte Preparation:
- Cohort: Recruit patients with an adequate number of mature oocytes (e.g., ≥6-8 Metaphase II oocytes) [24] [28].
- Stimulation: Use a standard superovulation protocol (e.g., GnRH antagonist or agonist) [26].
- Denudation: Remove cumulus cells using hyaluronidase. Only mature (MII) oocytes with a visible first polar body should be used for the study [24].
2. Sperm Preparation:
- Prepare sperm from the partner's semen using a two-layer Percoll density gradient (e.g., 90% and 45%) centrifugation at 300 g for 20 minutes [26].
- Resuspend the sperm pellet in a suitable culture medium (e.g., Universal IVF Medium) [26].
3. Randomization and Group Allocation:
- For each patient, randomly allocate sibling MII oocytes into two groups:
- Experimental Group: To be injected using PIEZO-ICSI.
- Control Group: To be injected using Conventional ICSI.
- If an odd number of oocytes is available, allocate the extra oocyte to the control group to minimize bias [28].
4. Micromanipulation Setup:
- Use an inverted microscope equipped with a micromanipulator system and a PIEZO unit (e.g., PIEZO PMM4G from Prime Tech Ltd.) [26].
- PIEZO-ICSI Pipette: Use a blunt-ended, flat-tip pipette (e.g., PINU06-20FT with a 6 µm outer diameter) [26].
- Holding Pipette: Use a standard holding pipette to secure the oocyte.
- Operating Liquid: Draw ~12 µL of mercury or a specialized commercial solution into the center of the injection pipette to transmit the pulse [26].
5. PIEZO-ICSI Injection Procedure:
- Sperm Immobilization: Immobilize a morphologically normal spermatozoon by tapping its tail with the injection pipette in a polyvinylpyrrolidone (PVP) droplet [26] [27].
- Sperm Loading: Aspirate the immobilized sperm from the tail-first into the pipette [26].
- Oocyte Positioning: Restrain the oocyte with the holding pipette. Unlike C-ICSI, the polar body position is less critical [26].
- Zona Pellucida Penetration: Apply several Piezo pulses (e.g., speed 2.0, intensity 2.0) to the zona pellucida at the 3 o'clock position to create an opening [26].
- Oolemma Penetration: Advance the pipette tip to the middle of the oocyte cytoplasm. Apply a single, sharp Piezo pulse (e.g., speed 2.0, intensity 1.0) to rupture the oolemma. Do not aspirate the cytoplasm [26].
- Sperm Injection: Expel the spermatozoon into the cytoplasm and withdraw the pipette smoothly [26].
6. Conventional ICSI Control Procedure:
- Perform C-ICSI on the control oocytes according to standard lab protocol. This typically involves using a sharp needle, positioning the polar body at 6 or 12 o'clock, inserting the needle at 3 o'clock, and rupturing the oolemma by aspirating cytoplasm before sperm injection [26].
7. Post-Injection Culture and Evaluation:
- Culture all injected oocytes from both groups under identical conditions (e.g., in SAGE 1 Step Medium at 37°C under 5.5% CO2, 5% O2) [26].
- Primary Outcomes (16-20 hours post-injection):
- Fertilization Rate: Calculate the percentage of oocytes with two pronuclei (2PN).
- Degeneration Rate: Calculate the percentage of oocytes that degenerated post-injection [24].
- Secondary Outcomes (Day 5/6):
- Blastocyst Development Rate: Calculate the percentage of fertilized oocytes that develop into blastocysts. Grade blastocysts using the Gardner classification system [26].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials for PIEZO-ICSI Implementation
| Item | Function/Description | Example Product/Specification |
|---|---|---|
| Piezo Unit | Generates high-frequency pulses for precise pipette movement. | Prime Tech Ltd. PIEZO PMM4G Unit [26] |
| Blunt-Ended Pipettes | Flat-tip pipette for sperm injection; transmits piezo pulse without cutting. | PINU06-20FT (6 µm OD, 5.1 µm ID) [26] |
| Operating Fluid | Fluid medium inside pipette to transmit piezoelectric pulse. | Mercury or specialized commercial solution [26] |
| Polyvinylpyrrolidone (PVP) | Viscous solution for slowing sperm for easy immobilization and pickup. | 7% PVP Solution [26] |
| Culture Medium | For post-injection embryo culture. | SAGE 1 Step Medium [26] |
| Time-Lapse Incubator | Allows undisturbed culture and morphokinetic analysis of development. | Various systems (e.g., Geri+) [29] |
| (+)-Isolariciresinol | (+)-Isolariciresinol, CAS:548-29-8, MF:C20H24O6, MW:360.4 g/mol | Chemical Reagent |
| Isomedicarpin | Isomedicarpin, CAS:74560-05-7, MF:C16H14O4, MW:270.28 g/mol | Chemical Reagent |
PIEZO-ICSI Experimental Workflow
The diagram below illustrates the key procedural differences and workflow for a sibling oocyte study comparing PIEZO-ICSI to Conventional ICSI.
Intracytoplasmic sperm injection (ICSI), while a breakthrough in treating male factor infertility, mechanically bypasses the physiological selection barriers sperm would naturally encounter in the female reproductive tract. This can increase the risk of selecting a genetically compromised spermatozoon, potentially leading to compromised embryo development and degeneration [30]. Functional sperm selection methods, such as the Cumulus Cell Column (CCC), have been developed to address this critical issue. The CCC technique is a biomimetic approach designed to isolate spermatozoa based on their functional competence, mirroring the natural selection process that occurs as sperm pass through the cumulus-oocyte complex [30]. By selecting sperm with enhanced chromatin integrity and functional capability, the CCC method aims to improve embryo quality and reduce post-ICSI embryo degeneration, a key focus in advanced assisted reproductive technology (ART) research [30].
Key Research Reagent Solutions
The following table details essential materials and reagents required for implementing the CCC sperm selection protocol in a research setting.
| Reagent/Material | Function in the CCC Protocol |
|---|---|
| Cumulus Cells (CCs) | Forms the biological filtration column; sourced from the patient's own denuded mature oocytes to ensure biological relevance [30]. |
| Micro-hematocrit Capillary Pipettes | Serves as the physical scaffold for constructing the three-layer column, including the cumulus cell barrier [30]. |
| Buffered Culture Medium | Base medium for collecting and housing cumulus cells prior to column loading [30]. |
| Sperm Medium with 10% HSA | Creates the bottom layer of the column; provides nutrients and a protein source for sperm that successfully migrate through the CC barrier [30]. |
| Density Gradient (e.g., Isolate) | Used for the initial sperm preparation step prior to the CCC selection process to isolate motile sperm [30]. |
| Hyaluronidase | Enzyme used to denude oocytes and separate cumulus cells from the oocyte-cumulus complex for column preparation [30]. |
Experimental Protocol: Sperm Selection via Cumulus Cell Column
This section provides a detailed, step-by-step methodology for the CCC technique as described in the literature [30].
Preliminary Steps
- Cumulus Cell Collection: Following oocyte retrieval, manually separate excess cumulus cells (CCs) from mature oocytes (Metaphase II) using insulin needles.
- Cell Handling: Collect the separated CCs into a buffered culture medium and maintain them at 37°C until column loading.
- Sperm Preparation: Obtain a fresh semen sample and process it using standard density gradient centrifugation (e.g., 40%/80% Isolate) to isolate motile spermatozoa according to WHO guidelines [30].
- Oocyte Denudation: Denude the remaining oocytes using hyaluronidase in preparation for the ICSI procedure.
Cumulus Cell Column Assembly
- Capillary Preparation: Take a 7 cm non-heparinized micro-hematocrit capillary pipette and rinse it with sterilized water.
- Column Layering: Connect the pipette to an insulin syringe and load it sequentially with three distinct layers:
- Bottom Layer: Approximately 2 cm of sperm medium enriched with 10% Human Serum Albumin (HSA).
- Middle Layer: Approximately 1 cm of the freshly collected cumulus cells to create the biological barrier.
- Top Layer: Approximately 4 cm of the prepared sperm sample, containing roughly 1 x 10^6 sperm cells.
- Incubation: Hold the loaded capillary pipette upright under a laminar flow hood for 45 minutes to allow for sperm migration.
Sperm Collection and ICSI
- Sperm Retrieval: After incubation, carefully extract the sperm that have successfully migrated through the cumulus cell barrier and entered the bottom medium layer. This is done using a pulled Pasteur pipette inserted into the top of the capillary.
- ICSI Dish Preparation: Transfer the collected, selected sperm directly to a polyvinylpyrrolidone (PVP) droplet on an ICSI dish.
- ICSI Procedure: Perform intracytoplasmic sperm injection by selecting individual sperm from this population based on standard morphological and motility criteria.
Diagram 1: Experimental workflow for sperm selection using the Cumulus Cell Column (CCC) technique.
Quantitative Outcomes of CCC Selection
The efficacy of the CCC technique is demonstrated by significant improvements in key sperm and embryo quality metrics, as summarized in the tables below.
Table 1: Impact of CCC Selection on Sperm DNA Fragmentation and Embryo Development
| Parameter | Control Group (Density Gradient Only) | Study Group (Density Gradient + CCC) | P-value |
|---|---|---|---|
| Sperm DNA Fragmentation (%) | 37.08% | 23.36% | 0.0001 [30] |
| Embryos with Accelerated Developmental Kinetics | Baseline | Significantly Increased | - |
| Embryos with Cleavage Abnormalities | Baseline | Significantly Reduced | - |
Table 2: Impact of CCC Selection on Clinical ICSI Outcomes
| Clinical Outcome | Control Group (Density Gradient Only) | Study Group (Density Gradient + CCC) | P-value |
|---|---|---|---|
| Implantation Rate | 28.4% | 58.0% | 0.001 [30] |
| Clinical Pregnancy Rate | 25.0% | 77.3% | 0.001 [30] |
| Live Birth Rate | 25.0% | 72.7% | 0.001 [30] |
Troubleshooting Guides & FAQs
Q1: A significant portion of sperm fails to pass through the cumulus cell column during the experiment. What could be the cause? A: This is a key indicator of the technique's selective function. A high failure rate typically suggests that the original sperm sample has a high proportion of functionally incompetent or immature spermatozoa. The CCC acts as a biological filter; only sperm with adequate motility, hyaluronic acid-binding capability, and intact acrosomes can penetrate the cumulus barrier. This outcome, while reducing yield, effectively enriches for a superior sperm population. Ensure the cumulus cell layer is not overly dense, which could physically block passage, and verify that the incubation time and temperature (37°C) are strictly maintained [30].
Q2: The collected cumulus cells appear clumped or non-homogeneous. How does this affect the column's efficiency? A: Clumped or non-homogeneous cumulus cells can create an irregular barrier with channels of varying density, compromising the consistency and selectivity of the filtration process. This can allow some suboptimal sperm to pass through while blocking others. To mitigate this, ensure gentle but thorough mechanical dispersal of the cumulus cells after hyaluronidase treatment before loading them into the capillary pipette. Using a consistent volume and gentle pipetting technique when creating the middle layer is crucial for forming a uniform barrier [30].
Q3: How does the CCC method differ from simply using Hyaluronic Acid (HA) binding assays for sperm selection? A: While both methods leverage the interaction between sperm and hyaluronic acid (a major component of the cumulus matrix), the mechanism is fundamentally different. HA-binding assays typically involve selecting sperm that bind to a glass surface or dish coated with HA. The CCC, however, uses a natural, complex matrix of whole cumulus cells, which more closely mimics the in vivo environment. This natural barrier is believed to test a broader range of sperm functions simultaneously, including progressive motility, hyperactivation, and the capacity for the acrosome reaction, potentially leading to a more robust selection of mature sperm with lower DNA fragmentation [30].
Q4: Our results show reduced DNA fragmentation with CCC, but the subsequent embryo quality is inconsistent. Where should we look next? A: While CCC selection significantly improves the sperm population, embryo development is multifactorial. Investigate these areas:
- Oocyte Quality: The developmental potential of the oocyte remains a critical factor. Consider correlating outcomes with oocyte morphology and patient age.
- Cumulus Cell Viability: The health and transcriptomic profile of the cumulus cells used in the column may impart important signals. Research indicates that cumulus cells are not just a passive filter but are biologically active, and their condition can reflect oocyte quality [31].
- Embryo Culture Conditions: Ensure that all other variables, including culture media, gas composition, and incubation systems (e.g., time-lapse), are optimized and consistent. The improved outcomes from CCC were documented in conjunction with time-lapse monitoring, which may be necessary to capture the subtle kinetic improvements [30].
Diagram 2: Functional mechanism of the Cumulus Cell Column (CCC) for isolating high-quality sperm.
The Cumulus Cell Column technique represents a significant advancement in functional sperm selection for ICSI. By emulating the body's natural biological filters, it effectively isolates a sperm subpopulation with superior DNA integrity and functional maturity. The implementation of this method, as detailed in the provided protocols and troubleshooting guides, offers a robust strategy for researchers and clinicians aiming to mitigate the risk of embryo degeneration and enhance overall ART success rates. The quantitative data clearly demonstrates its potential to improve key metrics, from sperm quality to live birth outcomes, making it a powerful tool in the pursuit of reducing post-ICSI embryo attrition.
Core Concepts & Techniques FAQ
What is sperm DNA fragmentation (SDF) and why is it critical for ICSI outcomes? Sperm DNA fragmentation (SDF) refers to breaks or damage in the genetic material carried by sperm. This integrity is crucial because, during ICSI, the sperm is injected directly into the oocyte. High SDF levels can lead to compromised embryonic development, reduced blastocyst quality, implantation failure, and early pregnancy loss [32]. The damage can be in the form of single-strand breaks (SSBs) or the more detrimental double-strand breaks (DSBs) [32].
What are the primary origins of SDF? SDF originates from two main mechanisms:
- Testicular Factors: Defective maturation during spermatogenesis, where DNA breaks created for chromatin packaging are not properly repaired, and abortive apoptosis, where faulty sperm that should be eliminated are not [32].
- Oxidative Stress (Post-testicular): An overproduction of reactive oxygen species (ROS) in the reproductive tract can directly damage sperm DNA. This can be caused by clinical conditions (e.g., varicocele, infection), lifestyle factors (e.g., smoking, obesity), or environmental exposures [32].
Which advanced sperm preparation techniques specifically target SDF reduction? Researchers have developed several techniques to selectively isolate sperm with higher DNA integrity:
- Migration-Gravity Sedimentation (MGS): A centrifuge-free technique where motile sperm swim out of raw semen and settle by gravity. It has been shown to significantly reduce SDF levels compared to both raw semen and Density Gradient Centrifugation (DGC) [33].
- Physiological ICSI (PICSI): This method selects mature sperm based on their ability to bind to hyaluronic acid, a component of the oocyte's vestments. Sperm that bind successfully are often more mature and have lower levels of DNA damage [34].
- PIEZO-ICSI: While not a sperm preparation method, this injection technique uses a piezoelectric shock to gently penetrate the oocyte membrane, minimizing physical trauma. This results in significantly lower oocyte degeneration rates post-injection, thereby increasing the number of viable oocytes available for fertilization and embryo development [2] [6].
Technique Selection & Comparative Data
How do MGS and traditional DGC compare in reducing SDF and affecting embryo quality? A prospective study comparing MGS and DGC using sibling oocytes provided the following quantitative data [33]:
Table 1: Comparison of MGS and DGC Techniques
| Parameter | Migration-Gravity Sedimentation (MGS) | Density Gradient Centrifugation (DGC) |
|---|---|---|
| SDF Reduction | Significant reduction vs. raw semen and DGC | Less effective than MGS |
| Fertilization Rate | Comparable to DGC | Comparable to MGS |
| Blastocyst Development | Comparable to DGC | Comparable to MGS |
| Clinical Pregnancy Rate | Comparable to DGC | Comparable to MGS |
| Key Advantages | Centrifuge-free, low-cost, simple protocol, superior SDF reduction | Standardized, widely adopted protocol |
Does PICSI improve embryo quality and cumulative pregnancy rates over conventional ICSI? A triple-blinded, prospective study revealed that while live birth rates per transfer were similar, PICSI showed benefits in other key areas [34]:
Table 2: Comparison of PICSI and Conventional ICSI Outcomes
| Parameter | PICSI | Conventional ICSI |
|---|---|---|
| Live Birth Rate | Comparable to ICSI | Comparable to PICSI |
| Cumulative Pregnancy Rate (after 4 transfers) | 88% | 72% |
| Proportion of Good-Quality D5 Blastocysts | 68.27% | 63.47% |
| Clinical Application | Beneficial for patients with recurrent pregnancy loss or in egg donation programs. | Standard selection based on morphology and motility. |
Does PIEZO-ICSI offer tangible benefits over conventional ICSI? Multiple studies confirm that PIEZO-ICSI improves key procedural outcomes, though clinical pregnancy and live birth rates per transfer remain comparable [2] [6]:
Table 3: Comparison of PIEZO-ICSI and Conventional ICSI
| Parameter | PIEZO-ICSI | Conventional ICSI |
|---|---|---|
| Normal Fertilization Rate | 78.0% [2] | 72.6% [2] |
| 71.6% [6] | 65.6% [6] | |
| Oocyte Degeneration Rate | 3.2% [2] | 6.3% [2] |
| 6.3% [6] | 12.1% [6] | |
| Blastocyst Quality (Day 5 AA/B) | 33.3% [6] | 27.5% [6] |
| Day 5 Blastocyst Formation Rate | 50.3% [2] | 43.9% [2] |
| Clinical Pregnancy Rate | Comparable to C-ICSI | Comparable to P-ICSI |
Troubleshooting Guide: Addressing Common Scenarios
Problem: Unexplained low fertilization or total fertilization failure (TFF) in ICSI cycles.
- Potential Cause: Oocyte Activation Deficiency (OAD), often linked to a deficiency or dysfunction of the sperm-specific factor phospholipase C zeta (PLCζ) [35].
- Investigation & Solution:
- Diagnostic Testing: Consider testing for PLCζ presence and localization in the patient's sperm using immunocytochemistry, if available [35].
- Rescue Technique: Implement Artificial Oocyte Activation (AOA). This protocol involves exposing injected oocytes to a calcium ionophore, which induces the necessary calcium oscillations to trigger embryonic development [35].
- AOA Protocol: After sperm injection, wash oocytes and place them in a culture medium containing a calcium ionophore (e.g., ionomycin) for a brief, specified duration (e.g., 10-15 minutes). Then, thoroughly wash the oocytes again before returning them to standard culture conditions [35].
Problem: Consistently high SDF rates in prepared sperm samples despite using DGC.
- Potential Cause: The centrifugal forces of DGC may exacerbate DNA damage in vulnerable sperm samples, or the sample may have high levels of oxidative stress [33] [32].
- Solution:
- Technique Switch: Adopt a gentler, centrifuge-free preparation method like Migration-Gravity Sedimentation (MGS). This allows the most motile and robust sperm to self-select without mechanical stress [33].
- Combine with Antioxidants: Review patient lifestyle and consider the use of antioxidant supplements (e.g., CoQ10) for the male partner to reduce intrinsic oxidative stress, though this is a clinical rather than lab-based intervention [32] [36].
Problem: High rates of oocyte degeneration immediately following ICSI.
- Potential Cause: Physical damage from the conventional ICSI needle during oolemma puncture, often due to the excessive aspiration required to rupture the membrane [2] [6].
- Solution: Implement PIEZO-ICSI. The piezoelectric technology uses a blunt needle and high-frequency vibrations to cleanly penetrate the zona pellucida and oolemma, eliminating the need for forceful aspiration and drastically reducing mechanical trauma to the oocyte [2] [6].
Experimental Protocols & Workflows
Detailed Protocol: Migration-Gravity Sedimentation (MGS)
- Principle: Leverages sperm's innate motility and natural sedimentation to isolate a population with lower DNA damage [33].
- Materials: Sterile conical tubes, pre-warmed culture media (e.g., HTF), incubator (37°C, 5-6% CO₂).
- Procedure:
- Gently layer 1.0-1.5 mL of liquefied raw semen underneath 2-3 mL of pre-equilibrated culture media in a sterile conical tube. Avoid mixing the layers.
- Incubate the tube at a 45-degree angle for 60 minutes at 37°C in a CO₂ incubator. Motile sperm will actively swim up into the culture media layer.
- After incubation, carefully collect the top media layer (approximately 1-1.5 mL), which now contains the motile sperm population.
- Assess the concentration and motility of the collected sperm.
- Use the prepared sample for ICSI. The SDF level of this sample is expected to be significantly lower than the raw semen and DGC-prepared counterparts [33].
Detailed Protocol: Calcium Ionophore AOA
- Principle: Pharmacologically induces the critical calcium oscillations required for oocyte activation, bypassing deficiencies in sperm-derived PLCζ [35].
- Materials: Calcium ionophore solution (e.g., ready-to-use commercial formulations), pre-warmed wash media, organ culture dishes, timer.
- Procedure:
- Perform ICSI as usual.
- Immediately after injection, transfer the oocytes into a dish containing a pre-equilibrated calcium ionophore solution (concentration and duration as per manufacturer or validated internal protocol, typically ~10 µM for 10 minutes).
- Strictly monitor the exposure time. After incubation, thoroughly wash the oocytes 3-5 times in fresh, pre-warmed culture media to completely remove the ionophore.
- Transfer the oocytes to a standard culture dish and place in the incubator for further development [35].
Signaling Pathways & Experimental Workflows
Diagram 1: Logical workflow for improving embryo quality post-ICSI.
Diagram 2: Oocyte activation signaling pathway and AOA rescue mechanism.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for SDF Research
| Reagent/Material | Function/Application | Example Use in Context |
|---|---|---|
| Hyaluronic Acid (HA) | Selection of mature sperm via surface binding for PICSI [34]. | Coating culture dishes or using commercial PICSI dishes to isolate sperm with lower DNA fragmentation and better nuclear maturity. |
| Calcium Ionophore | Artificial oocyte activation (AOA) to induce Ca²⺠oscillations [35]. | Rescuing fertilisation failure in cases of suspected PLCζ deficiency post-ICSI. |
| Polyvinylpyrrolidone (PVP) | Medium for slowing sperm motility during ICSI [7]. | Used in conventional ICSI to facilitate sperm handling and immobilization prior to injection. |
| Blunt-Ended Piezo Pipette | Core tool for PIEZO-ICSI, generates vibrations for precise penetration [2]. | Used to reduce oocyte degeneration by minimizing physical trauma during the injection process. |
| Protamine-Deficient Assay Kits | Assess sperm chromatin maturity and compaction. | Investigating the root cause of high SDF, as poor protamination is a key risk factor for DNA damage [32]. |
| Maculine | Maculine|High-Purity Reference Standard | Maculine: A high-purity biochemical for research use only (RUO). Explore its specific applications and value in scientific discovery. Not for human or veterinary use. |
| Malvidin Chloride | Malvidin Chloride, CAS:643-84-5, MF:C17H15ClO7, MW:366.7 g/mol | Chemical Reagent |
Integrating Time-Lapse Imaging for Non-Invasive Embryo Development Monitoring
Frequently Asked Questions (FAQs)
Q1: How does time-lapse imaging (TLI) improve embryo selection compared to traditional morphological assessment?
Time-lapse imaging provides continuous monitoring of embryo development without removing embryos from the incubator, thus avoiding disturbances to culture conditions. This allows embryologists to document and evaluate embryo morphology and the precise timing of developmental events through continuous live image tracking. TLI creates predictive models of in vitro fertilization outcomes by analyzing morphokinetic parameters that indicate the ability to reach blastocyst stage, implantation rates, pregnancy rates, live birth outcomes, and embryo ploidy [37].
Q2: What specific developmental parameters can time-lapse imaging track to predict embryo viability?
Time-lapse systems track key morphokinetic parameters including the time intervals between specific cell divisions: t2 (start of 2-cell stage), t3 (3-cell stage), t4 (4-cell stage), and t5 (5-cell stage). The system also monitors the dynamics of changes in embryo morphology, the start of the blastocyst stage, and the time intervals between adjacent cell stages (t2-t3, t3-t4). These parameters collectively indicate the implantation potential of an embryo [38].
Q3: Can time-lapse imaging be integrated with artificial intelligence for enhanced embryo assessment?
Yes, deep learning methods are being developed to forecast human embryo development in time-lapse videos. These AI systems can predict upcoming frames in time-lapse videos, capturing developmental changes over subsequent hours. This allows for earlier embryo transfer decisions, potentially diminishing epigenetic risks associated with prolonged incubation periods. The AI system utilizes current morphology dynamics to forecast future embryo development, helping identify key biomarkers important for evaluating embryo quality at an early developmental stage [38].
Q4: What technical specifications are typical for time-lapse incubator imaging systems?
The Embryoscope system by Vitrolife captures 8-bit images with a resolution of 500 × 500 pixels on different focal planes (usually between 3-5) at intervals of 7, 15, or 20 minutes. The system uses a camera with a LED light source (under 635 nm) passing through Hoffman's contrast modulation optics. Images are compiled into time-lapse videos depicting the entire embryonic development process for assessment by embryologists [38].
Troubleshooting Guides
Issue: Poor Quality Time-Lapse Images
Problem Description: Blurry, unfocused, or low-contrast images compromising embryo assessment accuracy.
Impact: Inaccurate morphokinetic annotation and embryo selection decisions.
Context: Typically occurs during system setup, maintenance periods, or with specific patient samples.
Diagnostic Steps:
- Verify the focal plane settings and adjust if necessary
- Check the LED light source intensity and alignment
- Inspect the Hoffman's contrast modulation optics for cleanliness
- Confirm the imaging interval settings (7, 15, or 20 minutes)
- Validate camera resolution settings (500 × 500 pixels, 8-bit)
Resolution:
- Quick Fix (5 minutes): Clean the external optics and recalibrate focal planes
- Standard Resolution (15 minutes): Perform full system calibration including light source intensity and camera settings
- Root Cause Fix (30+ minutes): Schedule manufacturer maintenance for optical component inspection and replacement if necessary
Prevention: Implement weekly calibration checks and maintain proper environmental controls to reduce particulate contamination.
Issue: Inconsistent Morphokinetic Annotations Between Operators
Problem Description: Significant inter-operator variability in identifying developmental timepoints (t2, t3, t4, t5).
Impact: Reduced reproducibility and reliability of embryo selection criteria.
Context: Common in multi-operator laboratories without standardized annotation protocols.
Diagnostic Steps:
- Review annotation guidelines for each developmental stage
- Conduct blinded re-annotation of sample videos by multiple operators
- Analyze variance in recorded timepoints for identical embryos
- Assess operator training and experience levels
Resolution:
- Quick Fix (5 minutes): Provide reference images for each developmental stage
- Standard Resolution (15 minutes): Conduct group training sessions with sample videos to establish consensus
- Root Cause Fix (30+ minutes): Implement AI-assisted annotation systems to reduce human variability [38]
Prevention: Establish regular proficiency testing and continuing education programs for all embryologists.
Issue: Integration Challenges Between Time-Lapse and AI Prediction Systems
Problem Description: Discrepancies between observed embryo development and AI-generated forecasts.
Impact: Reduced confidence in predictive embryo selection models.
Context: Typically occurs when implementing new AI algorithms or with atypical embryo development patterns.
Diagnostic Steps:
- Verify input data quality and preprocessing steps
- Validate AI model training parameters and dataset composition
- Compare forecasted versus actual development for multiple embryos
- Assess model performance across different patient populations
Resolution:
- Quick Fix (5 minutes): Retrain model with current laboratory-specific data
- Standard Resolution (15 minutes): Implement ensemble methods combining multiple prediction approaches
- Root Cause Fix (30+ minutes): Develop laboratory-specific AI models optimized for local patient demographics and protocols
Prevention: Establish ongoing validation protocols and model updating schedules based on cumulative laboratory data.
Table 1: Comparison of ICSI Techniques and Outcomes
| Parameter | Conventional ICSI | PIEZO-ICSI | Pre-Catching Sperm (PCS) ICSI |
|---|---|---|---|
| Fertilization Rate | 65.6% [6] | 71.6% [6] | 84.0% [39] |
| Oocyte Degeneration Rate | 12.1% [6] | 6.3% [6] | 1.4% [39] |
| Good Quality Blastocyst Formation | 27.5% [6] | 33.3% [6] | 54.9% [39] |
| Clinical Pregnancy Rate | No significant difference [6] | No significant difference [6] | Similar between groups [39] |
| Live Birth Rate | No significant difference [6] | No significant difference [6] | Similar between groups [39] |
Table 2: Time-Lapse Imaging Monitoring Parameters
| Morphokinetic Parameter | Developmental Stage | Predictive Value |
|---|---|---|
| t2 | 2-cell stage | Baseline developmental progression |
| t3 | 3-cell stage | Cleavage symmetry assessment |
| t4 | 4-cell stage | Implantation potential indicator |
| t5 | 5-cell stage | Blastocyst formation prediction |
| t2-t3 interval | Early cleavage | Embryo viability correlation |
| t3-t4 interval | Compaction phase | Developmental competence |
| Blastocyst start time | Blastulation | implantation potential [38] |
Experimental Protocols
Protocol 1: Time-Lapse Imaging Setup and Embryo Culture
Purpose: To continuously monitor embryo development without disturbing culture conditions.
Materials:
- Time-lapse incubator (e.g., Embryoscope by Vitrolife)
- Embryoslide culture plates
- Culture media (G-MOPS PLUS, Ovoil Heavy)
- Temperature and gas-controlled environment
Methodology:
- Prepare embryoslide with individual wells for embryo culture
- Load embryos into designated wells following ICSI procedure
- Place embryoslide into time-lapse incubator
- Set imaging parameters: 500 × 500 pixels resolution, 8-bit images, multiple focal planes (3-5)
- Configure imaging intervals: 7, 15, or 20 minutes depending on experimental requirements
- Maintain culture conditions at 37°C, 5% O₂, 6% CO₂
- Collect images continuously for 5-7 days of development
- Compile images into time-lapse videos for analysis [38]
Protocol 2: Morphokinetic Annotation and Analysis
Purpose: To quantitatively assess embryo development timing and predict viability.
Materials:
- Time-lapse video sequences
- Annotation software with timestamp capability
- Standardized grading criteria
Methodology:
- Review time-lapse videos for each embryo
- Record exact timings (hours post insemination) for each developmental stage:
- t2: initiation of 2-cell stage
- t3: initiation of 3-cell stage
- t4: initiation of 4-cell stage
- t5: initiation of 5-cell stage
- Calculate time intervals between stages (t2-t3, t3-t4)
- Note blastocyst formation time and morphology
- Apply Gardner grading system for blastocyst assessment (grade 3BB or higher considered good quality)
- Correlate morphokinetic parameters with clinical outcomes [37] [38]
Workflow Visualization
Time-Lapse Reproductive Intelligence Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Time-Lapse Imaging Embryo Research
| Reagent/Equipment | Function | Example Product |
|---|---|---|
| Time-Lapse Incubator | Continuous embryo monitoring with stable culture conditions | Embryoscope (Vitrolife) [38] |
| Embryoslide Culture Plates | Individual embryo wells for simultaneous imaging and culture | Embryoslide (Vitrolife) [38] |
| Culture Media | Support embryo development during extended culture | G-MOPS PLUS, Ovoil Heavy [39] |
| Polyvinylpyrrolidone (PVP) | Sperm viscosity control during ICSI procedure | 7% PVP (Irvine Scientific) [39] |
| Annotation Software | Morphokinetic parameter tracking and analysis | Custom or commercial TLI analysis platforms [37] |
| AI Forecasting Tools | Predictive modeling of embryo development | Deep learning frameworks [38] |
| (+)-Matairesinol | (+)-Matairesinol|High-Purity Lignan for Cancer Research | (+)-Matairesinol is a plant lignan with anticancer and immunomodulatory activity. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Geraldol | Geraldol, CAS:21511-25-1, MF:C16H12O6, MW:300.26 g/mol | Chemical Reagent |
Refining ICSI Protocols: Biomarkers, Pharmacological Aids, and Quality Control
In the field of assisted reproduction, particularly in research aimed at reducing embryo degeneration post-intracytoplasmic sperm injection (ICSI), the analysis of spent embryo culture media has emerged as a powerful, non-invasive diagnostic tool. Spent culture media—the fluid in which embryos have been cultured—contains a rich reservoir of biochemical information reflecting embryonic health and developmental potential. Unlike traditional invasive methods that require embryo biopsy, spent media analysis preserves embryo integrity while providing comprehensive data on embryo viability.
This approach leverages advanced "omics" technologies to analyze the genomic, transcriptomic, proteomic, and metabolomic signatures that embryos release into their culture environment. These biomarkers offer a window into embryonic function and can help researchers identify embryos with the highest likelihood of successful development, thereby addressing the critical challenge of embryo degeneration following ICSI procedures. The non-invasive nature of these techniques makes them particularly valuable for ICSI research, where minimizing additional stress on embryos is paramount to improving outcomes.
Table 1: Categories of Non-Invasive Biomarkers in Spent Culture Media
| Biomarker Category | Analytical Focus | Representative Analytical Techniques |
|---|---|---|
| Genomics | Embryo ploidy status (chromosomal abnormalities) | Next-generation sequencing (NGS), quantitative real-time PCR (qRT-PCR) |
| Metabolomics | Metabolic activity and substrate utilization | Raman spectroscopy, mass spectroscopy, near-infrared spectroscopy, nuclear magnetic resonance (NMR) |
| Proteomics/Secretomics | Protein secretion and expression patterns | Mass spectroscopy, high-performance liquid chromatography (HPLC), nanoparticle tracking analysis |
| Transcriptomics | Gene transcription and expression profiles | Next-generation sequencing, quantitative real-time PCR (qRT-PCR) |
Key Analytical Techniques and Methodologies
Core Omics Technologies
The analytical power of spent media analysis stems from a suite of high-throughput omics technologies that have largely replaced earlier, more subjective methods. These modern techniques enable objective, rapid, and non-invasive assessment of embryo quality, which is essential for contemporary ICSI research [40] [41].
Genomics: Focuses on assessing chromosomal ploidy status through analysis of embryonic DNA released into culture media. Aneuploidy (an abnormal number of chromosomes) is a major cause of implantation failure and miscarriage, and its detection is crucial for selecting viable embryos. Next-generation sequencing techniques applied to spent media can identify these chromosomal abnormalities without the need for trophectoderm biopsy [40].
Metabolomics: Examines the metabolites consumed and released by developing embryos, providing insights into their metabolic activity and energy utilization. Raman spectroscopy has proven particularly valuable here, as it can obtain biochemical information without being destructive or requiring dyes/stains. This technique requires only minimal sample volume (a few microliters) and preparation, making it ideal for analyzing spent culture media [42].
Proteomics and Secretomics: Investigates the proteins and secretory factors embryos release into their environment. These protein signatures reflect functional cellular processes and developmental competence. Mass spectroscopy and high-performance liquid chromatography are commonly employed to identify and quantify these protein biomarkers [40].
Transcriptomics: Analyzes RNA transcripts present in spent media, which provide information about gene expression patterns and embryonic gene activation. This approach can reveal critical aspects of embryonic development and function through analysis of the transcriptome [40].
Diagram 1: Experimental workflow for spent culture media analysis, showing the pathway from sample collection through various analytical techniques to biomarker identification.
Raman Spectroscopy Protocol for Metabolomic Profiling
Raman spectroscopy has emerged as a particularly valuable technique for metabolomic profiling of spent culture media in ICSI research. Below is a detailed methodology based on established protocols [42]:
Sample Preparation:
- Collect spent culture media from ICSI-derived embryos at specific developmental stages (2-cell, 4-cell, 8-cell, 16-cell, 32-cell, and blastocyst stages).
- Include appropriate control samples (fresh unused culture media) for baseline comparison.
- Use minimal sample volumes (typically 2-5 μL) to preserve media for potential additional analyses.
- Avoid freeze-thaw cycles that might degrade metabolites of interest.
Instrumentation and Data Acquisition:
- Utilize a Raman spectroscopy system with laser excitation (typically 785 nm wavelength to minimize fluorescence background).
- Employ laser tweezer Raman spectroscopy (LTRS) for analyzing small volumes without the need for substrate attachment.
- Set acquisition parameters: 10-20 second integration time per spectrum, with multiple accumulations to improve signal-to-noise ratio.
- Collect spectra across a relevant wavenumber range (e.g., 500-1800 cmâ»Â¹) to capture fingerprint region of metabolites.
- Perform all measurements under consistent temperature conditions (37°C if possible) to mimic physiological environment.
Spectral Analysis and Data Processing:
- Pre-process raw spectra: subtract background, correct for baseline drift, and normalize to internal reference peaks.
- Identify characteristic spectral bands corresponding to key biomolecules:
- Lipids: 1307 cmâ»Â¹ and 1451 cmâ»Â¹
- DNA: 796 cmâ»Â¹ (O-P-O backbone vibration)
- Carbohydrates: 842 cmâ»Â¹ and 936 cmâ»Â¹
- Proteins: Multiple bands including Amide I (1640-1680 cmâ»Â¹)
- Employ multivariate statistical analysis (e.g., Discriminant Function Analysis) to develop diagnostic algorithms for differentiating embryo quality.
- Generate metabolic fingerprints that reflect the metabolic status of embryos and their developmental potential.
Table 2: Key Research Reagent Solutions for Spent Media Analysis
| Reagent/Equipment | Application Purpose | Technical Specifications |
|---|---|---|
| Raman Spectroscopy System | Metabolomic profiling via spectral analysis | 785 nm laser, resolution: 2-4 cmâ»Â¹, detection range: 500-1800 cmâ»Â¹ |
| High-Performance Liquid Chromatography | Separation and quantification of media components | Reverse-phase columns, UV/fluorescence detection |
| Next-Generation Sequencer | Genomic analysis of embryo-derived DNA | High-throughput platform for cell-free DNA sequencing |
| Mass Spectrometer | Proteomic and metabolomic identification | High-resolution, LC-MS/MS compatibility |
| Culture Media | Embryo support and biomarker source | Defined composition without protein supplements |
Troubleshooting Guide: Common Technical Challenges and Solutions
Sample Quality and Contamination Issues
Problem: Low biomarker concentration in spent media.
- Potential Cause: Insufficient embryo secretion or dilution from excessive media volume.
- Solution: Optimize culture media volume to embryo ratio (typically 20-50 μL per embryo). Consider culture duration extension but maintain within physiological limits (not exceeding 24 hours for analysis). Concentrate samples using centrifugal filters with appropriate molecular weight cut-offs if necessary [40] [42].
Problem: High background interference in spectroscopic analysis.
- Potential Cause: Contamination from culture oil, laboratory plastics, or particulate matter.
- Solution: Use mass spectrometry-grade reagents and high-purity culture oils. Filter media through 0.22 μm filters before analysis. Include blank controls (media without embryo culture) in every experiment to identify and subtract background signals. For Raman spectroscopy, ensure proper cleaning of sampling chambers between measurements [42].
Problem: Inconsistent results between technical replicates.
- Potential Cause: Sample degradation or improper storage conditions.
- Solution: Process samples immediately after collection when possible. If storage is necessary, snap-freeze in liquid nitrogen and store at -80°C. Avoid repeated freeze-thaw cycles. Implement standardized protocols for sample handling across all experimental batches [43].
Instrumentation and Data Analysis Challenges
Problem: Poor signal-to-noise ratio in Raman spectra.
- Potential Cause: Insufficient laser power or suboptimal integration time.
- Solution: Optimize laser power to balance signal intensity with potential sample damage. Increase integration time (up to 30 seconds) while monitoring for sample degradation. Apply smoothing algorithms during data processing, but ensure they don't eliminate legitimate spectral features [42].
Problem: Inability to distinguish viable from non-viable embryos based on metabolic profiles.
- Potential Cause: Insufficient model training or inappropriate biomarker selection.
- Solution: Increase sample size for model training, ensuring balanced representation of known viable and non-viable embryos. Apply machine learning algorithms (e.g., random forest, support vector machines) with cross-validation. Combine multiple biomarker types (multi-omics approach) rather than relying on single parameters [40] [43].
Problem: Batch effects obscuring biological signals.
- Potential Cause: Technical variation between different experimental runs or reagent lots.
- Solution: Implement randomization of sample processing order. Include internal standards in each batch. Use statistical methods like ComBat or remove unwanted variation (RUV) algorithms to correct for batch effects during data analysis. Validate findings across multiple independent experimental batches [43].
Frequently Asked Questions (FAQs)
Q1: How does spent media analysis specifically benefit ICSI research compared to conventional IVF studies? Spent media analysis is particularly valuable in ICSI research because ICSI-derived embryos may exhibit different metabolic and developmental profiles compared to conventional IVF embryos. Research has shown that ICSI-derived cattle embryos demonstrate distinct Raman spectral signatures in their culture media, particularly in lipid and DNA-related bands, suggesting fundamental differences in metabolic activity [42]. These differences may reflect the unique biochemical demands and potential stresses experienced by embryos following the mechanical injection procedure. By identifying these specific metabolic fingerprints, researchers can develop targeted strategies to reduce embryo degeneration post-ICSI.
Q2: What is the optimal timing for spent media collection to assess embryo viability? The optimal collection time depends on the specific biomarkers of interest. For comprehensive assessment, multiple collection timepoints are recommended:
- Early cleavage stage (Day 1-2): For analysis of initial metabolic activation
- Embryonic genome activation stage (Day 2-3 in human embryos): For assessment of critical developmental transitions
- Blastocyst stage (Day 5-6): For evaluation of pre-implantation competence Metabolomic studies using Raman spectroscopy have successfully detected meaningful patterns at specific developmental stages including 2-cell, 4-cell, 8-cell, 16-cell, 32-cell, and blastocyst stages [42]. Consistent timing across experiments is crucial for reliable comparisons.
Q3: Can spent media analysis truly replace traditional morphological assessment of embryos? While spent media analysis provides valuable biochemical information that complements traditional morphological assessment, current evidence suggests it works best as a complementary approach rather than a complete replacement. Morphological evaluation provides information about temporal development patterns and structural normalcy, while omics analyses of spent media reveal functional metabolic and molecular characteristics [40]. The most powerful predictive models often integrate both morphological/kinetic data and biochemical biomarker data from spent media to provide a more comprehensive assessment of embryo viability, particularly in the context of ICSI where subtle functional deficiencies may not be morphologically apparent.
Q4: How can researchers validate the predictive value of biomarkers identified in spent media? Validation should follow a multi-step process:
- Technical validation: Confirm analytical reproducibility using appropriate controls and replicates.
- Biological validation: Correlate biomarker patterns with established viability indicators (blastocyst formation, genetic normalcy).
- Clinical validation: For human applications, correlate with implantation and live birth outcomes in sufficiently powered studies.
- Independent validation: Confirm findings in separate experimental batches and, if possible, across different laboratories. Rigorous quality control measures should be implemented throughout, including monitoring of read mapping rates, sequencing depth, signal-to-noise ratios, and ensuring sample consistency where replicates cluster appropriately in multivariate analysis [43].
Diagram 2: Troubleshooting workflow for common technical challenges in spent media analysis, showing the logical progression from problem identification through validation of solutions.
The analysis of spent culture media through omics technologies represents a paradigm shift in embryo assessment post-ICSI, offering a non-invasive window into embryonic function and developmental potential. As research in this field advances, the integration of multiple biomarker types—genomic, metabolomic, proteomic, and transcriptomic—into comprehensive predictive models holds particular promise for reducing embryo degeneration. Future directions include the development of standardized protocols across laboratories, the validation of specific biomarker panels for ICSI-derived embryos, and the integration of artificial intelligence approaches to improve predictive accuracy. By addressing the technical challenges outlined in this guide and implementing robust troubleshooting practices, researchers can accelerate progress toward the ultimate goal of improving embryo viability and treatment outcomes in ICSI.
Ubiquitin-specific protease 30 (USP30) is a deubiquitinating enzyme anchored in the outer mitochondrial membrane that plays a critical role in mitochondrial quality control by counteracting Parkin-mediated mitophagy [44] [45]. In cellular stress conditions, USP30 removes ubiquitin tags from mitochondrial proteins, thereby inhibiting the selective autophagy of damaged mitochondria [46] [47]. While current research has primarily explored USP30 inhibition in neurodegenerative diseases like Parkinson's [48] and conditions such as subarachnoid hemorrhage [47], its potential application in embryonic health represents an emerging frontier. Given that mitochondrial dysfunction and oxidative stress are significant contributors to embryo degeneration post-intracytoplasmic sperm injection (ICSI) [49], targeted inhibition of USP30 offers a promising strategy to enhance mitophagy, reduce apoptotic signaling, and potentially improve embryo quality and developmental outcomes.
Frequently Asked Questions (FAQs) on USP30 Inhibition
Q1: What is the primary biological function of USP30? USP30 is a deubiquitinating enzyme localized to the outer mitochondrial membrane that antagonizes Parkin-mediated mitophagy by removing ubiquitin chains from mitochondrial proteins such as TOM20 and MFN2. This activity regulates mitochondrial quality control by preventing the premature clearance of mitochondria [46] [44] [47].
Q2: Why would USP30 inhibition be relevant to embryonic development and ICSI outcomes? Embryonic development requires substantial energy, with mitochondria supplying ATP for critical differentiation processes. Oxidative stress is a known pathological factor in infertility that can disrupt redox balance in gametes [49]. By enhancing mitophagy, USP30 inhibition could help clear damaged mitochondria, reduce oxidative stress, and support healthier embryonic development, particularly in the context of ICSI where embryo degeneration can occur [49] [50].
Q3: What specific mitochondrial proteins are affected by USP30 inhibition? USP30 preferentially cleaves Lys6-linked ubiquitin chains from mitochondrial proteins including TOM20, TOM40, TIM23, and MFN2. Inhibition of USP30 leads to increased ubiquitination of these proteins, facilitating their recognition by autophagic machinery [46] [47].
Q4: Are there any safety concerns with inhibiting USP30 in developing systems? Current evidence from Usp30 knockout mice shows no overt pathologies, with animals born at expected Mendelian frequencies and displaying no detectable deleterious effects with aging. In fact, enhanced mitophagy has been associated with protective effects in various disease models [48]. However, comprehensive toxicological studies in embryonic models are still needed.
Q5: What is the relationship between PINK1/Parkin and USP30? PINK1 and Parkin form a key pathway that promotes mitophagy by ubiquitinating mitochondrial proteins. USP30 acts in opposition to this pathway by deubiquitinating these same substrates, thereby raising the threshold for mitophagy induction [46] [44]. PINK1 phosphorylation of both Parkin and ubiquitin enhances this signaling cascade.
Troubleshooting Guides for USP30 Inhibition Experiments
Problem: Inconsistent Mitophagy Induction in Cellular Models
Potential Causes and Solutions:
Cause 1: Variable expression levels of endogenous Parkin across cell lines.
- Solution: Use HeLa cells stably expressing YFP-Parkin (Hela-Parkin) for consistent results, as wild-type HeLa cells express little to no endogenous Parkin [46].
Cause 2: Inadequate mitochondrial stress induction.
- Solution: Optimize concentration and duration of mitochondrial stress inducers. A common approach is treatment with antimycin A (1-2 µM) and oligomycin (1-10 µM) for 2-18 hours [46].
Cause 3: Insufficient USP30 inhibitor concentration or exposure time.
- Solution: Perform dose-response experiments with USP30 inhibitors (e.g., ST-539, MF094) and include time-course assessments. For ST-539, effective concentrations typically range from 1-10 µg/ml [46].
Problem: Difficulty in Detecting Mitophagy Flux
Potential Causes and Solutions:
Cause 1: Limitations in current detection methodologies.
- Solution: Implement the mt-Keima assay, a pH-sensitive, dual-excitation ratiometric fluorescent probe targeted to mitochondria. When mitophagy occurs, mt-Keima shifts to longer-wavelength excitation in acidic autolysosomes, enabling quantification via FACS analysis [46].
Cause 2: Low basal mitophagy levels in your experimental system.
- Solution: Combine USP30 inhibition with mitochondrial stressors. Alternatively, use the mito-QC reporter system, which features a GFP-mCherry tandem fused to a mitochondrial localization signal, enabling visualization of mitophagy as red-only puncta when GFP is quenched in acidic lysosomes [48].
Problem: Off-Target Effects of USP30 Inhibitors
Potential Causes and Solutions:
Cause 1: Lack of inhibitor specificity.
- Solution: Validate findings with multiple inhibitory approaches. Use genetic knockdown/knockout of USP30 alongside pharmacological inhibition. Activity-based protein profiling can confirm target engagement and selectivity [51].
Cause 2: Compensatory mechanisms in prolonged inhibition.
- Solution: Conduct time-course experiments and assess alternative mitophagy pathways. Monitor expression of other mitochondrial DUBs (USP8, USP15, USP35) that might compensate for USP30 inhibition [44].
Experimental Protocols for Key Assays
Protocol 1: Assessing Mitophagy Using the mt-Keima Assay
Principle: The mt-Keima probe exhibits a pH-dependent excitation shift, with shorter wavelengths (440 nm) predominant in neutral mitochondrial pH and longer wavelengths (550 nm) in acidic autolysosomes [46].
Procedure:
- Transfect cells with mt-Keima construct using appropriate transfection reagent.
- Allow 24-48 hours for expression and mitochondrial localization.
- Treat cells with USP30 inhibitor (e.g., ST-539 at 10 µg/ml) with or without mitochondrial stress inducers (A/O: 1 µM antimycin A + 1 µM oligomycin).
- After 18 hours, analyze cells using fluorescence-activated cell sorting (FACS) with dual-excitation (440 nm and 550 nm) and 620 nm emission.
- Calculate mitophagy index as the ratio of 550 nm excitation/620 nm emission to 440 nm excitation/620 nm emission.
Interpretation: Increased ratio indicates enhanced mitophagy flux.
Protocol 2: Monitoring Mitochondrial Protein Ubiquitination
Principle: USP30 inhibition increases ubiquitination of outer mitochondrial membrane proteins, which can be detected via immunoblotting [46].
Procedure:
- Treat Hela-Parkin cells with USP30 inhibitor (e.g., MF094 at 5 µM) for 6 hours.
- Induce mitochondrial stress with A/O treatment for additional 2 hours.
- Harvest cells and isolate mitochondrial fraction using differential centrifugation.
- Perform Western blotting with antibodies against TOM20, TIM23, TOM40, and ubiquitin.
- Quantify band intensity using densitometry software.
Interpretation: USP30 inhibition should increase ubiquitin smearing and decrease TOM20, TOM40, and TIM23 protein levels, indicating enhanced mitophagy.
Protocol 3: Evaluating USP30 Inhibitor Efficacy in Primary Neurons
Principle: This protocol can be adapted for embryonic cell models to assess USP30 inhibition effects [47].
Procedure:
- Culture primary neurons from embryonic brain tissue.
- Treat with USP30 inhibitor MF094 (5 µM) for 24 hours.
- Induce mitochondrial damage if required for your experimental context.
- Fix cells and immunostain for TOM20 (mitochondrial marker), LAMP1 (lysosomal marker), and neuronal markers.
- Image using confocal microscopy and quantify colocalization of mitochondrial and lysosomal markers.
Interpretation: Increased colocalization indicates enhanced mitophagy.
Table 1: Efficacy of USP30 Inhibitors in Preclinical Models
| Inhibitor | Model System | Key Readouts | Results | Citation |
|---|---|---|---|---|
| ST-539 | Hela-Parkin cells | TOM20 ubiquitination | ~90% decrease in TOM20 protein levels | [46] |
| MTX115325 | A53T-αSyn mouse PD model | Dopaminergic neuron survival | 66.15% protection vs 47.35% in controls | [48] |
| MF094 | Mouse SAH model | Neurological score improvement | Significant improvement at 5 mg/kg dose | [47] |
| Genetic KO | USP30 KO mice | Basal mitophagy in DA neurons | 12.7 vs 8.8 mCherry puncta/neuron in WT | [48] |
Table 2: Research Reagent Solutions for USP30 Studies
| Reagent | Type | Function/Application | Example Sources |
|---|---|---|---|
| ST-539 | Small molecule inhibitor | Racemic phenylalanine derivative that inhibits USP30 enzyme function | Custom synthesis [46] |
| MF094 | Small molecule inhibitor | USP30-specific inhibitor used in SAH models | MedChemExpress (#HY-112438) [47] |
| MTX115325 | Small molecule inhibitor | Potent, selective, brain-penetrant USP30 inhibitor | Developed by Mission Therapeutics [48] |
| mt-Keima | Fluorescent probe | pH-dependent mitophagy reporter for FACS analysis | Available as plasmid constructs [46] |
| Mito-QC | Reporter mouse | GFP-mCherry tandem fusion for in vivo mitophagy tracking | Available through repositories [48] |
The Scientist's Toolkit: Essential Research Reagents
USP30 Inhibitors:
- ST-539: A racemic phenylalanine derivative that selectively inhibits USP30 enzyme function in vitro, promoting mitophagy in Parkin-expressing cells at concentrations of 1-10 µg/ml [46].
- MF094: A specific USP30 inhibitor used in subarachnoid hemorrhage models, effective at promoting mitophagy and reducing neuronal apoptosis at 5 mg/kg in vivo [47].
- MTX115325: A potent, selective, brain-penetrant USP30 inhibitor with drug-like properties developed by Mission Therapeutics, showing efficacy in protecting dopaminergic neurons in Parkinson's disease models [48].
Cell Lines and Models:
- Hela-Parkin cells: HeLa cells stably expressing YFP-Parkin provide a consistent system for studying USP30 inhibition and mitophagy, as they lack significant endogenous Parkin expression [46].
- USP30 KO mice: Constitutive knockout mice lacking USP30 show enhanced basal mitophagy without overt pathology, providing a valuable tool for validating pharmacological effects [48].
- Primary neuronal cultures: Isolated from embryonic brain tissue, these cells enable assessment of USP30 inhibition in post-mitotic cells relevant to neurological function [47].
Critical Assays:
- mt-Keima mitophagy assay: A robust FACS-based method for quantifying mitophagy flux using pH-dependent fluorescence properties [46].
- Mitochondrial protein ubiquitination: Western blot analysis of OMM proteins (TOM20, TOM40, MFN2) to monitor ubiquitination status following USP30 inhibition [46] [47].
- Immunofluorescence colocalization: Confocal microscopy to assess colocalization of mitochondrial and lysosomal markers as an indicator of mitophagy [48] [47].
Signaling Pathways and Experimental Workflows
Diagram 1: USP30 Inhibition Enhances Mitophagy. USP30 removes ubiquitin from mitochondrial proteins, counteracting Parkin-mediated mitophagy. Pharmacological inhibition of USP30 preserves ubiquitination, promoting clearance of damaged mitochondria.
Diagram 2: Experimental Workflow for USP30 Inhibition Studies. This workflow outlines key steps for evaluating USP30 inhibitors, from cell model selection through data analysis of mitophagy parameters.
Frequently Asked Questions
FAQ: What are the primary laboratory factors that contribute to embryo degeneration post-ICSI? Multiple laboratory factors can contribute to embryo degeneration. The ICSI procedure itself is a significant factor, with conventional ICSI carrying a 5-19% risk of oocyte degeneration due to the mechanical force required to rupture the oolemma [1]. The culture environment is also critical; suboptimal conditions including fluctuations in temperature, pH, and exposure to volatile organic compounds (VOCs) in the laboratory air can induce cumulative stress on embryos [4] [52] [53]. Furthermore, the timing of procedures such as oocyte collection, if performed too early (<36 hours post-trigger), can compromise oocyte viability and subsequent development [4].
FAQ: How can we verify if our culture media and consumables are safe for embryos? Implement a rigorous Mouse Embryo Assay (MEA) as a functional bioassay. To ensure sensitivity, this assay should not rely solely on blastocyst formation at 96 hours as an endpoint. Incorporate total cell count analysis of the resulting blastocysts, as morphologically normal blastocysts with low cell counts indicate sublethal toxicity and reduced developmental potential [53]. This method is more effective at detecting toxicity that can delay development or reduce embryo viability.
FAQ: Our ICSI implantation rates have dropped. What is a systematic approach to identify the cause? Employ Quality Improvement (QI) methodologies like Root Cause Analysis (RCA). One clinic used this approach to discover that a change in operating theatre schedules had led to some ICSI egg collections occurring at suboptimal times (<36 hours post-trigger) [4]. As part of the RCA, form a multidisciplinary team to review all processes and data. If internal review does not yield improvements, an external "fresh eyes" review can help identify overlooked issues [4]. Implementing a bundle of corrective actions, such as personalizing trigger times based on list order, can subsequently restore performance [4].
Troubleshooting Guide
The following table outlines common problems, their potential root causes, and evidence-based solutions.
| Problem Observed | Potential Root Causes | Recommended Corrective Actions & Rationale |
|---|---|---|
| High Oocyte Degeneration Rate | • Overly aggressive cytoplasmic aspiration during conventional ICSI [1].• Oolemma fragility or high cytoplasmic viscosity [1]. | Switch to PIEZO-ICSI: Uses a blunt pipette and piezoelectric pulse to penetrate the zona pellucida and oolemma, minimizing mechanical damage. This significantly reduces degeneration rates (e.g., from 12.1% to 6.3%) compared to conventional ICSI [6]. |
| Poor Fertilization & Embryo Development | • Suboptimal culture medium composition not supporting metabolic needs [54] [55].• Cumulative stress from toxic compounds in consumables (e.g., gloves, catheters) [53].• Uncontrolled culture environment (e.g., nutrient depletion, waste accumulation) [54]. | Optimize Culture Medium: Employ active learning and machine learning to efficiently fine-tune the concentrations of dozens of medium components (e.g., amino acids, vitamins) for improved outcomes [55].Quality Test All Consumables: Use a sensitive MEA to test all devices (40% of tested brands showed toxicity) [53].Rationalize Assay Conditions: Ensure cells are not cultured to over-confluence and that nutrients are not depleted during assays, which causes drastic metabolic shifts and confounds results [54]. |
| Low Implantation Rates / Poor Embryo Viability | • Suboptimal air quality in the lab (particulate matter, VOCs) [52].• Inconsistent temperature control during handling [4].• Embryo manipulation stress (e.g., from biopsy) [56]. | Implement Air Quality Control (Cleanrooms): Constructing laboratories to cleanroom standards for particles and VOCs has been shown to increase live birth rates and decrease miscarriage rates [52].Use Portable Safety Cabinets & Heated Stages: Improve control of the immediate microenvironment during oocyte retrieval and handling to ensure consistent temperature [4].Review All Accompanying Procedures: Ensure complex manipulations like vitrification and biopsy are performed to the highest standard, as improper execution can negatively impact reproductive potential [56]. |
Experimental Protocols for Optimization
Protocol 1: Active Learning for Culture Medium Optimization
This protocol uses machine learning to efficiently optimize complex culture media, moving beyond traditional one-factor-at-a-time approaches [55].
- Define Medium Components: Select the medium components to be optimized (e.g., the 29 components from Eagle's Minimum Essential Medium, excluding phenol red and antibiotics) [55].
- Acquire Initial Training Data: Perform cell cultures using a wide variety of medium combinations with component concentrations varied on a logarithmic scale. A large dataset (e.g., 232+ combinations) with biological replicates is ideal.
- Quantify Cellular Output: Use a high-throughput, quantitative assay to measure culture success. The cellular NAD(P)H abundance, measured by absorbance at 450 nm (A450) after a CCK-8 assay, can serve as a proxy for cell concentration and activity [55].
- Train the Model and Predict: Employ a white-box machine learning algorithm, such as the Gradient-Boosting Decision Tree (GBDT). Train the model with your initial dataset and allow it to predict new medium combinations that should yield higher A450.
- Validate and Iterate: Culture cells in the top predicted medium combinations. Add the experimental results back into the training dataset and repeat the cycle to refine the model and progressively improve the medium formulation.
Protocol 2: Enhanced Mouse Embryo Assay (MEA) for Toxicity Screening
This protocol details a sensitive MEA to test the safety of culture media and contact materials [53].
- Mouse Strain Selection: For increased sensitivity, use an outbred mouse strain in addition to the common F1 hybrid strain to detect more subtle toxicity [53].
- Embryo Collection & Culture: Collect 1-cell or 2-cell embryos from superovulated mice. Wash and place a defined number of embryos into microdrop cultures under oil, containing the test medium or exposed to the test material (e.g., a piece of plasticware).
- Culture and Assess: Culture the embryos for 96 hours. Assess and record the rate of development to the blastocyst stage based on morphology.
- Cell Counting (Critical Step): Fix and stain the resulting blastocysts with a nuclear dye (e.g., Hoechst). Use fluorescence microscopy to count the total number of nuclei in each blastocyst.
- Analysis: Compare both the blastocyst formation rate and the average total cell count per blastocyst between the test and control groups. A significant reduction in either parameter, especially cell count without affected morphology, indicates toxicity [53].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Research |
|---|---|
| PIEZO-ICSI Unit | A micromanipulation system that uses piezoelectric technology for a less invasive oocyte injection, significantly reducing mechanical damage and degeneration rates [24] [6]. |
| Gradient-Boosting Decision Tree (GBDT) Algorithm | A machine learning model with high interpretability; used in active learning cycles to model complex interactions between culture medium components and cell growth, predicting optimal formulations [55]. |
| CCK-8 Assay Kit | A colorimetric kit used to measure cellular NAD(P)H abundance (A450), serving as a high-throughput, quantitative metric for cell viability and proliferation in medium optimization experiments [55]. |
| Portable Biological Safety Cabinet (Unica) | Provides a controlled, clean air environment for procedures like oocyte retrieval outside the main lab, protecting gametes from airborne particulates and VOCs present in open theatres [4]. |
| Volatile Organic Compound (VOC) Filtration System | Integrated into laboratory HVAC to remove airborne chemical contaminants that can impair embryo development and reduce clinical outcomes [52]. |
| Electronically Controlled Heated Stages | Maintain a consistent temperature for gametes and embryos during all handling steps outside the incubator, preventing stress from thermal fluctuations [4]. |
Workflow and Relationship Diagrams
Experimental Optimization Workflow
The following diagram illustrates the logical workflow for troubleshooting and optimizing laboratory conditions, integrating key concepts from the FAQs and protocols.
Impact of Environmental Stress on Embryo Viability
This diagram visualizes the concept of cumulative stress, where multiple suboptimal factors combine to impact embryo development and viability.
FAQs: Core Concepts and Technology
Q1: What is the fundamental difference between a morphokinetic algorithm and an AI model for embryo selection?
A1: Morphokinetic algorithms and AI models represent different generations of embryo evaluation technology. Morphokinetic algorithms are typically rule-based systems developed by analyzing specific, manually annotated time points in embryo development. For example, the KIDScore algorithm uses six key annotations: time to 2 pronuclei (PN) fading, and the times from insemination to the 2-cell, 3-cell, 5-cell, and 8-cell stages to rank embryos according to their implantation potential [57]. In contrast, AI models like deep learning convolutional neural networks (CNNs) are "trained" on vast datasets of embryo images (over 150,000 in some cases) to automatically identify complex, sub-visual patterns correlated with developmental outcomes, without relying on manually pre-defined rules [58] [59].
Q2: How can these tools specifically help in reducing embryo degeneration post-ICSI?
A2: By improving the selection of embryos with the highest inherent potential, these tools indirectly address degeneration. Embryo arrest (degeneration) is often linked to underlying factors like aneuploidy or other cellular deficiencies. While no tool can prevent arrest in a compromised embryo, AI and morphokinetic scoring can identify embryos most likely to continue developing robustly. For instance, the MAGENTA oocyte score is correlated with the likelihood of an egg developing into a blastocyst, a key milestone that filters out embryos prone to early degeneration [58]. Selecting such embryos for transfer reduces the likelihood of transferring an embryo that will later arrest.
Q3: What are the typical performance metrics for these technologies, and how should I interpret them?
A3: Performance is measured using diagnostic metrics that assess prediction accuracy. The table below summarizes pooled metrics from a recent meta-analysis and specific model performances [60] [59].
Table 1: Performance Metrics of Embryo Selection AI Models
| Model / Analysis | Area Under Curve (AUC) | Sensitivity | Specificity | Accuracy |
|---|---|---|---|---|
| Pooled AI Analysis (Meta-analysis) | 0.70 | 0.69 | 0.62 | - |
| MAIA Platform (Prospective Test) | 0.65 | - | - | 66.5% |
| FiTTE System | 0.70 | - | - | 65.2% |
| Life Whisperer | - | - | - | 64.3% |
- Area Under Curve (AUC): Evaluates the model's overall ability to distinguish between embryos that will implant and those that will not. An AUC of 0.7 suggests a moderate to good predictive capability [60] [61].
- Sensitivity: The model's ability to correctly identify embryos that will lead to pregnancy.
- Specificity: The model's ability to correctly identify embryos that will not lead to pregnancy.
- Accuracy: The overall proportion of correct predictions. It is crucial to note that these metrics are often derived from evaluations on embryos already preselected for transfer by embryologists, which may inflate performance compared to a model tasked with evaluating all embryos from a cohort [61].
FAQs: Troubleshooting and Experimental Setup
Q4: Our AI model performs well on training data but generalizes poorly to new data from a different patient population. What could be the cause?
A4: This is a common challenge often stemming to a lack of demographic diversity in the training dataset. AI models are highly sensitive to the data on which they are trained. A model developed primarily with images from one ethnic or geographic population may not perform optimally on images from another due to variations in demographic and ethnic profiles [59]. Solution: Develop or fine-tune a laboratory-adapted model using your own in-house data. One study demonstrated that developing an in-house model based on specific laboratory morphokinetics complemented general models and improved live birth prediction [62]. Ensure your training set is large, diverse, and representative of your entire patient population.
Q5: We are getting inconsistent results after implementing a time-lapse selection algorithm. What environmental factors should we validate?
A5: Embryo morphokinetics are sensitive to culture conditions. Inconsistent results can arise from uncontrolled variables in the lab environment. Before concluding on algorithm performance, rigorously validate these factors [57] [63]:
- Temperature: Validate the heated stage to ensure microdroplet temperature is maintained at 37.0 °C with an accuracy of +/- 0.1 °C. Note that a single temperature setting may not be sufficient if you use different types of culture dishes (e.g., plastic vs. glass), as their material can affect heat transfer. Each dish type requires separate validation [63].
- Vibration: The micromanipulation station must be located in a quiet area with minimal vibration, away from doors, elevators, or other machinery. Use efficient anti-vibration platforms (e.g., air cushion tables) to isolate the microscope [63].
- Optics: Ensure microscope optics are clean and properly configured. For Hoffman modulation optics, verify that the condenser turret is correctly matched to the objective in use to achieve optimal 3D visualization for manipulation [63].
Q6: How do we objectively evaluate whether a new AI tool is superior to our embryologists' standard morphological assessment?
A6: A rigorous, prospective, and blinded comparison is essential. Crucially, you must be aware of selection bias, which is inevitable in retrospective comparisons. In a retrospective study, the AI is often tested on embryos that were previously selected for transfer by embryologists. This means the AI is only evaluated on a pre-screened "good" cohort, which can make its performance appear inflated or non-representative of its ability to assess all embryos [61].
Solution: Design a study where all embryos from a cohort are scored by both the AI and embryologists, and the outcomes are tracked. The key is to compare the performance in a head-to-head, prospective trial. A recent study comparing the MAIA AI platform to embryologist selection across three centers used linear regression analysis to correlate predictions with clinical pregnancy outcomes, finding that MAIA's predictions showed a stronger and more consistent correlation [59].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Advanced Embryo Selection Research
| Item | Function in Research | Example / Note |
|---|---|---|
| Time-Lapse Incubator | Enables continuous, non-invasive monitoring of embryo development, generating the morphokinetic data essential for algorithm development and validation. | EmbryoScopeⓇ, GeriⓇ [59] |
| Micromanipulation Station | Provides the stable, high-precision environment required for ICSI and biopsy procedures, which are foundational for research on pre-implantation genetic testing. | Must include an anti-vibration platform and modulated contrast optics (e.g., Hoffman) [63]. |
| AI Software Platforms | Serve as the analytical engine for evaluating embryo images, providing quantitative scores for embryo viability, and automating selection. | iDAScore, AI Chloe, MAIA Platform [59] |
| Polyvinylpyrrolidone (PVP) | A substance used to slow down sperm motility for immobilization prior to ICSI, a critical step in the procedure. | Consider exploring physiological alternatives [7]. |
| Preimplantation Genetic Testing (PGT) Reagents | Used to assess the chromosomal health (ploidy) of embryos. This provides a crucial outcome measure (euploidy) for validating new selection algorithms. | Kits for Comprehensive Chromosomal Screening (CCS) like CGH or microarrays [64]. |
Experimental Protocols for Validation
Protocol 1: Validating a Laboratory-Adapted Morphokinetic Model
This protocol is based on a study that successfully developed an in-house model to complement general algorithms [62].
- Data Collection: Retrospectively compile a dataset of time-lapse embryos with known implantation data (KID). The study used 3275 embryos transferred on Day 3 as a foundation [57].
- Morphokinetic Analysis: Annotate key time points for each embryo. The core parameters often include: tPNa (appearance of pronuclei), tPNf (fading of pronuclei), t2, t3, t4, t5, t8 (times to 2, 3, 4, 5, and 8 cells).
- Statistical Comparison: Compare the distribution of these timings between implantation-positive (KID+) and implantation-negative (KID-) embryos using appropriate statistical tests (e.g., Student's t-test) to identify parameters with significant differences in your lab environment.
- Model Building: Use the significantly different parameters to build a prediction model. This can be done using automated recursive partitioning or other statistical modeling techniques [57].
- Validation: Test the predictive power of your new model on a separate, blinded validation set of embryos. Express the results using Receiver Operating Characteristic (ROC) curves and calculate the Area Under the Curve (AUC). The goal is to see if the in-house model outperforms or adds value to a general model [62].
Protocol 2: Prospective Clinical Evaluation of an AI Selection Tool
This protocol outlines a method for testing an AI tool in a real-world clinical setting, as demonstrated by the MAIA platform study [59].
- Study Design: Conduct a prospective observational study. Define your primary endpoint (e.g., clinical pregnancy confirmed by gestational sac and fetal heartbeat).
- Patient Cohort: Recruit patients undergoing single embryo transfer (SET). The MAIA study prospectively tested 200 single embryo transfers [59].
- Intervention: For all embryos in the cohort, generate an AI score (e.g., on a scale of 0-10) prior to the embryologist's final selection. Define a cutoff score for a positive vs. negative prediction of pregnancy (e.g., MAIA used ≥6.0 as positive) [59].
- Blinding and Selection: The embryologist should make the final transfer decision, potentially with the AI score available as an aid, depending on the study design.
- Outcome Analysis: Correlate the AI scores with the clinical pregnancy outcomes. Calculate standard performance metrics like accuracy, AUC, and use linear regression to assess the correlation between the AI score and the clinical outcome [59].
- Comparison: Compare the success rates of embryos selected by the AI tool versus those selected by standard embryologist morphology.
Workflow and Conceptual Diagrams
Diagram 1: Integrated Workflow for Embryo Selection
Diagram 2: AI Model for Blastocyst Assessment
Evaluating Efficacy: Clinical Outcomes and Comparative Analysis of ICSI Techniques
The table below summarizes key quantitative findings from recent clinical studies comparing PIEZO-ICSI and Conventional ICSI.
Table 1: Comparison of Fertilization and Degeneration Rates between PIEZO-ICSI and Conventional ICSI
| Study Population & Citation | Normal Fertilization Rate (PIEZO-ICSI vs. Conventional ICSI) | Oocyte Degeneration Rate (PIEZO-ICSI vs. Conventional ICSI) | Key Embryo Development Outcomes |
|---|---|---|---|
| Patients with previous poor prognosis [18] [65] | 61.9% vs 45.3% (P<0.0001) | 7.7% vs 18.2% (P=0.0001) | Significantly higher number of embryos utilized (frozen or transferred) per cycle. |
| First IVF cycle patients [2] [24] | 78.0% vs 72.6% (P=0.0176) | 3.2% vs 6.3% (P=0.0055) | Higher blastocyst formation rate on Day 5 (50.3% vs 43.9%, P=0.0367); No significant difference in cumulative blastocyst rate or clinical pregnancy rate. |
| Prospective case-matched cohort [66] | 80.5% vs 65.8% (P<0.0001) | 4.4% vs 8.6% (P=0.019) | Increased number of good-quality embryos for cryopreservation/transfer (3.8 vs 3.1, P=0.038); No significant difference in fresh transfer pregnancy rates. |
| Women >35 years old [26] | Significantly higher with PIEZO-ICSI (P=0.008) | Not significantly different | Significantly higher blastocyst development rate with PIEZO-ICSI (P=0.016). |
Experimental Protocols for Technique Comparison
Protocol: Conventional ICSI (c-ICSI)
- Oocyte Positioning: The mature oocyte (MII) is held by a holding pipette with the first polar body positioned at the 12 or 6 o'clock position [26].
- Sperm Immobilization: A single, morphologically normal spermatozoon is immobilized in a polyvinylpyrrolidone (PVP) solution using a sharp, beveled injection needle [26].
- Injection Procedure: The injection needle is inserted at the 3 o'clock position, penetrating the zona pellucida and oolemma through physical pressure [18] [26].
- Oolemma Rupture: The oolemma is ruptured by aspirating a small amount of ooplasm into the injection needle [26].
- Sperm Deposition: The sperm is deposited into the ooplasm, along with the aspirated cytoplasm, and the needle is withdrawn [18].
Protocol: PIEZO-ICSI (P-ICSI)
- Equipment Setup: The system is equipped with a piezoelectric actuator (e.g., PIEZO PMM4G) and blunt-ended, ultrathin injection pipettes [26]. The pipette is pre-loaded with a biocompatible operating fluid, such as perfluoro-n-octane [18] [66].
- Sperm Handling: A spermatozoon is immobilized by applying a few Piezo pulses to its tail and is then aspirated, head-first, into the injection pipette [26].
- Zona Pellucida Penetration: The oocyte is restrained. Using Piezo pulses (e.g., speed: 2.0, intensity: 2.0), the zona pellucida is penetrated without considering the polar body's position [26].
- Oolemma Rupture: The blunt pipette tip is advanced to the middle of the ooplasm. The oolemma is punctured using a single, low-intensity Piezo pulse (e.g., speed: 2.0, intensity: 1.0) [26].
- Sperm Deposition: The sperm is injected into the cytoplasm without aspirating the ooplasm. The pipette is gently withdrawn after confirming deposition [18] [26].
Troubleshooting Guide: Addressing High Degeneration Rates
Problem: High rate of oocyte degeneration after ICSI.
Table 2: Troubleshooting High Oocyte Degeneration
| Possible Cause | Diagnostic Questions | Recommended Solution |
|---|---|---|
| Inherent Oocyte Quality | Are high degeneration rates correlated with higher patient age, elevated basal FSH, or higher E2 levels on hCG day? [1] [9] | Consider switching to PIEZO-ICSI, particularly for patients with a history of high degeneration or of advanced maternal age (>35-38 years) [18] [26]. |
| Technical Procedure (c-ICSI) | Is the oolemma difficult to rupture, requiring excessive aspiration? Is cytoplasmic leakage observed upon needle withdrawal? [1] | Ensure proper needle sharpness and minimize ooplasmic aspiration. Implement extensive technician training. Validate the procedure using control oocytes. |
| Technical Procedure (P-ICSI) | Are Piezo pulse settings (speed/intensity) too high for oolemma puncture? [26] | Optimize and calibrate Piezo settings. Use lower intensity pulses (e.g., intensity 1.0) specifically for oolemma puncture. |
| Oocyte Handling | Are oocytes exposed to temperature fluctuations, pH shifts, or mechanical stress during denudation or manipulation? | Review and standardize all handling procedures from retrieval to injection. Ensure consistent use of pre-equilibrated media and controlled environmental conditions. |
Frequently Asked Questions (FAQs)
Q1: What is the core mechanical difference between Conventional ICSI and PIEZO-ICSI that affects degeneration? A1: Conventional ICSI uses a sharp needle and physical pressure to cut through the membranes, followed by ooplasmic aspiration to rupture the oolemma. This aspiration step is highly invasive and is a primary cause of degeneration [2]. PIEZO-ICSI uses a blunt needle and high-frequency vibrations to cleanly puncture the membranes, eliminating the need for cytoplasmic aspiration and significantly reducing physical trauma [18] [26].
Q2: For which patient populations is PIEZO-ICSI most beneficial? A2: Evidence strongly supports the use of PIEZO-ICSI in:
- Patients with a previous poor prognosis from Conventional ICSI, specifically those with low fertilization (<50%) or high degeneration (>15%) [18] [65].
- Women of advanced maternal age (≥35 years), as their oocytes may have more fragile membranes and benefit most from the gentler Piezo technique [26] [66].
Q3: Does the improvement in fertilization and degeneration rates with PIEZO-ICSI translate to higher pregnancy rates? A3: Current studies show a nuanced picture. While multiple studies report no significant difference in clinical pregnancy rates per fresh embryo transfer [2] [66], PIEZO-ICSI consistently increases the number of usable embryos (utilization rate) available for transfer or cryopreservation per cycle [18] [66]. This suggests that the cumulative pregnancy rate from a single retrieval cycle may be improved, though larger studies are needed for confirmation.
Q4: What are the main practical drawbacks of implementing PIEZO-ICSI in a lab? A4: The technique requires a higher initial investment for the Piezo equipment, and the procedure is often considered more time-consuming and technically demanding to master than Conventional ICSI [2]. It also requires the use of specialized blunt pipettes and a biocompatible operating fluid [26].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PIEZO-ICSI Implementation
| Item | Function | Consideration |
|---|---|---|
| Piezo Actuator Unit | Generates high-frequency pulses for precise drilling and membrane penetration. | Must be compatible with existing micromanipulators. Units like the Prime Tech PIEZO PMM4G are commonly used [26]. |
| Blunt-Ended Injection Pipettes | Used to inject sperm without cutting; requires Piezo pulses to penetrate membranes. | Ultrathin, flat-tip pipettes (e.g., ~6µm outer diameter) are recommended to minimize oocyte deformation [26]. |
| Biocompatible Operating Fluid | Transmits the Piezo pulse from the actuator to the pipette tip. | Historically, mercury was used, but modern, safe fluids like Perfluoro-n-octane are now available and recommended for clinical use [18] [66]. |
| Hyaluronidase | Enzyme used to remove cumulus cells from the retrieved oocyte-cumulus complexes (denudation). | Standard reagent for ICSI; exposure time should be minimized (e.g., <20-30 seconds) to reduce potential stress on oocytes [1]. |
| Polyvinylpyrrolidone (PVP) Solution | A viscous medium used to slow down sperm for selection and immobilization. | A standard reagent for both Conventional and PIEZO-ICSI [26]. |
Troubleshooting Guide: Common Challenges in Blastocyst Assessment
FAQ 1: Why are my blastocyst formation rates lower than expected, and how can I improve them?
Lower-than-expected blastocyst formation can result from multiple factors. Advanced maternal age is significantly correlated with increased developmental arrest rates, rising from a median of 33.0% in patients under 35 to 44.0% in patients over 42 [67]. The choice of ICSI technique also impacts survival; PIEZO-ICSI reduces oocyte degeneration rates to 3.2% compared to 6.3% with conventional ICSI [2] [24]. Day 3 embryo quality is another critical predictor – the mean cell number and proportion of 8-cell embryos are among the top features identified by machine learning models for predicting blastocyst yield [68].
Troubleshooting Steps:
- Patient Selection: For patients over 38, expect higher developmental arrest rates and adjust embryo cohort expectations accordingly.
- Technique Optimization: Implement PIEZO-ICSI, especially for cases with previous poor fertilization or high degeneration rates.
- Quality Monitoring: Closely track Day 3 embryo parameters including cell number, symmetry, and fragmentation levels.
FAQ 2: How should I handle blastocysts that fail to re-expand within 2-4 hours post-warming?
Blastocysts that remain completely shrunken (CSBs) 2-4 hours post-warming still retain implantation potential, though at significantly reduced rates compared to re-expanded blastocysts (REBs). Clinical pregnancy rates for CSBs are 28.8% versus 61.5% for REBs, while live birth rates are 20.2% versus 50.0% [69]. However, day 5 CSB blastocysts have 3.062 times higher odds of achieving clinical pregnancy compared to day 6 CSBs [69].
Action Protocol:
- Transfer Decision: Consider transferring CSBs when no other embryos are available, particularly if they are day 5 blastocysts.
- Quality Assessment: Favor CSBs derived from good-quality day 3 embryos, as these have higher implantation potential.
- Patient Counseling: Set appropriate expectations regarding reduced success rates when transferring non-re-expanded blastocysts.
FAQ 3: Does extended vitrification storage duration affect embryo viability?
Yes, prolonged cryostorage impacts success rates. Vitrification of embryos for more than 6 months is associated with reduced live birth rates, although no significant influence on neonatal health has been observed [70]. This suggests potential cryoprotectant toxicity or cumulative damage during extended storage.
Storage Recommendations:
- Prioritize Transfers: Schedule frozen embryo transfers within 6 months of vitrification when possible.
- Documentation: Maintain detailed records of cryostorage duration for outcome analysis.
- Protocol Review: Evaluate vitrification solutions and procedures if planning long-term storage.
Quantitative Data Tables for Blastocyst Assessment
Table 1: Machine Learning Models for Predicting Blastocyst Yield Performance Comparison
| Model | R² Score | Mean Absolute Error | Number of Features | Key Advantages |
|---|---|---|---|---|
| LightGBM (Optimal) | 0.673-0.676 | 0.793-0.809 | 8 | Fewer features, superior interpretability |
| XGBoost | 0.673-0.676 | 0.793-0.809 | 10-11 | High accuracy |
| SVM | 0.673-0.676 | 0.793-0.809 | 10-11 | Captures complex patterns |
| Linear Regression | 0.587 | 0.943 | N/A | Baseline comparison |
Data derived from analysis of 9,649 IVF/ICSI cycles [68]
Table 2: Developmental Arrest Rates by Maternal Age Group
| Age Group | Median Developmental Arrest Rate | Interquartile Range |
|---|---|---|
| <35 years | 33.0% | 22.0-50.0% |
| 35-37 years | 38.0% | 25.0-50.0% |
| 38-40 years | 40.0% | 29.0-54.0% |
| 41-42 years | 44.0% | 38.8-56.5% |
| >42 years | 44.0% | 40.0-58.0% |
Data from 25,974 embryos showing statistically significant increase with age (p < 0.0001) [67]
Table 3: PIEZO-ICSI vs. Conventional ICSI Outcomes
| Parameter | Conventional ICSI | PIEZO-ICSI | P-value |
|---|---|---|---|
| Normal Fertilization Rate | 72.6% | 78.0% | 0.0176 |
| Oocyte Degeneration Rate | 6.3% | 3.2% | 0.0055 |
| Developmental Arrest of Zygotes | 2.48% | 1.20% | 0.1250 |
| Blastocyst Formation Rate (Day 5) | 43.9% | 50.3% | 0.0367 |
| Clinical Pregnancy Rate | 64.3% | 66.7% | Not Significant |
Data from 100 patients (1,527 oocytes) undergoing first IVF cycle [2] [24]
Table 4: Post-Warming Blastocyst Re-expansion Impact on Clinical Outcomes
| Outcome Measure | Completely Shrunken Blastocysts (CSBs) | Re-expanded Blastocysts (REBs) | P-value |
|---|---|---|---|
| Clinical Pregnancy Rate | 28.8% | 61.5% | <0.001 |
| Ongoing Pregnancy Rate | 22.1% | 52.9% | <0.001 |
| Live Birth Rate | 20.2% | 50.0% | <0.001 |
Data from 104 CSBT and 2172 REBT single embryo transfer cycles [69]
Experimental Protocols for Key Assessments
Protocol 1: Blastocyst Yield Prediction Using Machine Learning
Purpose: To quantitatively predict blastocyst yields in IVF cycles using machine learning algorithms.
Methodology:
- Dataset Preparation: Collect data from 9,649 IVF/ICSI cycles with features including female age, number of 2PN embryos, number of extended culture embryos, Day 2 and Day 3 embryo morphology parameters [68].
- Feature Selection: Apply recursive feature elimination (RFE) to identify optimal feature subset (8-11 features).
- Model Training: Train multiple machine learning models (LightGBM, XGBoost, SVM) alongside traditional linear regression as baseline.
- Model Validation: Perform internal validation on testing set with metrics including R² and Mean Absolute Error (MAE).
- Interpretation Analysis: Use feature importance analysis and individual conditional expectation plots to identify key predictors.
Key Predictors Identified:
- Number of extended culture embryos (61.5% importance)
- Mean cell number on Day 3 (10.1% importance)
- Proportion of 8-cell embryos on Day 3 (10.0% importance)
- Proportion of 4-cell embryos on Day 2 (7.1% importance)
- Female age (2.4% importance) [68]
Protocol 2: Vitrification and Warming Procedure for Blastocysts
Purpose: To successfully vitrify and warm human blastocysts with maximum survival rates.
Vitrification Steps:
- Artificial Shrinking: Perform laser-assisted artificial shrinkage of blastocoel cavity prior to vitrification to minimize ice crystal formation [69].
- Equilibration: Transfer blastocysts to equilibration solution containing 7.5% ethylene glycol and 7.5% dimethyl sulfoxide for 8-10 minutes [69].
- Vitrification: Move blastocysts to vitrification solution (15% EG, 15% DMSO, 0.5M sucrose) for 1 minute [69].
- Loading and Cooling: Load blastocysts onto cryotop with minimal solution and plunge directly into liquid nitrogen [71].
Warming Steps:
- Rapid Warming: Plunge cryotop directly into 1.0M sucrose solution at 37°C for 1 minute [72] [71].
- Gradual Rehydration: Transfer blastocysts to 0.5M sucrose solution for 3 minutes [71].
- Washing: Wash blastocysts twice in culture medium for 5 minutes each [71].
- Assessment: Evaluate re-expansion status 2-4 hours post-warming [69].
Critical Parameters:
- Warming rate should exceed 2170°C/min to avoid ice crystal formation [72].
- Use extracellular cryoprotectants (sucrose or trehalose) to create high osmolarity for controlled rehydration [72].
- Perform all steps at specified temperatures (37°C for initial warming, room temperature for subsequent steps) [72].
Workflow Visualization
Diagram 1: Complete workflow from ICSI to blastocyst transfer showing key decision points and success rates.
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key Research Reagents for Blastocyst Studies
| Reagent Category | Specific Products | Function in Research | Key Considerations |
|---|---|---|---|
| Culture Media | G1-Plus, G2-Plus, Blast Assist Medium | Sequential media supporting embryo development from cleavage to blastocyst stage | Monitor for temperature excursions during transport; degradation accelerates at higher temperatures [73] |
| Cryoprotectants | Ethylene Glycol, DMSO, Sucrose | Permeating and non-permeating agents for vitrification | Concentrations critical: ES (7.5% EG + 7.5% DMSO), VS (15% EG + 15% DMSO + 0.5M sucrose) [69] |
| Vitrification Systems | Cryotop, Cryoloop | Carrier systems for ultrarapid cooling | Minimize volume (<1μL) when loading embryos [71] |
| Assessment Tools | Gardner Blastocyst Scoring System, Istanbul Consensus Criteria | Standardized morphology evaluation | Combine multiple grading systems for comprehensive assessment [69] |
| Laser Systems | Octax Laser, ZILOS-tk | For artificial shrinkage of blastocoel prior to vitrification | Optimize laser settings to minimize cellular damage [69] |
Advanced Troubleshooting: Environmental and Temporal Factors
FAQ 4: How do seasonal variations and environmental factors impact blastocyst development?
Seasonal variations significantly impact IVF outcomes, with clinical pregnancy likelihood 1.74-fold higher in spring and 1.53-fold higher in summer compared to winter [74]. Temperature shows a nonlinear relationship with clinical pregnancy outcomes, with optimal ranges observed between 26.13°C to 29.68°C [74]. These effects are more pronounced in long protocol cycles compared to antagonist protocols.
Mitigation Strategies:
- Protocol Selection: Consider antagonist protocols in environments with significant temperature fluctuations.
- Laboratory Control: Maintain strict temperature and environmental controls year-round.
- Seasonal Planning: When possible, schedule critical procedures during optimal seasonal periods.
FAQ 5: What is the relationship between developmental arrest and aneuploidy rates?
Developmental arrest and aneuploidy represent independent factors in determining embryo viability. While both are associated with female age, analysis of 25,974 embryos showed only a very weak correlation between arrest rates and aneuploidy rates (r: 0.07, R²: 0.00) [67]. After adjusting for age, no statistically significant relationship between aneuploidy and developmental arrest was observed.
Research Implications:
- Independent Pathways: Developmental arrest and aneuploidy likely involve different biological mechanisms.
- Assessment Strategy: Evaluate blastocyst formation and ploidy status as separate parameters in research protocols.
- Therapeutic Targets: Investigate maternal effect genes and mitochondrial function for addressing developmental arrest specifically.
FAQs: Troubleshooting Embryo Development Post-ICSI
FAQ 1: Does oocyte degeneration after ICSI predict poor long-term outcomes for the sibling oocytes in the same cycle?
Answer: No, the occurrence of oocyte degeneration in an ICSI cycle is not a reliable indicator of poor developmental potential for the remaining sibling oocytes. Evidence from a 2021 study shows that for young women (under 35), cycles with oocyte degeneration had comparable cumulative live birth rates to cycles with no degeneration [1].
- Key Supporting Data: The study found no significant differences in implantation rate (38.5% vs. 35.1%), clinical pregnancy rate (54.9% vs. 50.3%), or live birth rate per oocyte pickup cycle (47.0% vs. 42.9%) between the oocyte degeneration and non-degeneration groups. The cumulative live birth rate was also similar (63.4% vs. 64.8%) [1].
- Troubleshooting Implication: Isolated oocyte degeneration is likely a function of inherent oocyte quality or mechanical factors affecting individual oocytes, rather than a reflection of the entire cohort's viability. Researchers should proceed with embryo culture and transfer of sibling oocytes with confidence.
FAQ 2: For non-severe male factor infertility, does ICSI provide a higher live birth rate than conventional IVF?
Answer: A large 2024 randomized controlled trial (RCT) demonstrated that for couples with non-severe male factor infertility, ICSI does not improve the live birth rate after the first embryo transfer compared to conventional IVF [75].
- Key Supporting Data: The live birth rate after the first transfer was 33.8% for ICSI versus 36.6% for conventional IVF, with the difference being statistically non-significant. The study also found that while fertilization failure rates were similar, the ICSI group had fewer embryos available on day 3 [75].
- Troubleshooting Implication: The routine use of ICSI in the absence of severe male factor infertility or a history of fertilization failure is not justified. Researchers designing studies or clinics formulating policies should reserve ICSI for clear medical indications to avoid unnecessary costs and potential reduction in available embryos.
FAQ 3: Does using frozen-thawed embryos from Re-ICSI cycles affect implantation success?
Answer: Yes, the implantation success of Re-ICSI embryos is significantly influenced by the transfer strategy. Research indicates that using frozen-thawed embryos from Re-ICSI cycles can overcome the impaired outcomes often seen with fresh transfers [76].
- Key Supporting Data: A 2023 study found that in fresh embryo transfer cycles, Re-ICSI embryos had lower clinical pregnancy, implantation, and live birth rates compared to direct ICSI embryos. However, in subsequent frozen embryo transfer (FET) cycles, these differences were eliminated, and outcomes became comparable [76].
- Troubleshooting Implication: If a cycle involves Re-ICSI, a "freeze-all" strategy followed by frozen-thawed embryo transfer may yield better implantation and pregnancy results. This suggests that the uterine environment in a fresh cycle after ovarian stimulation may not be optimal for Re-ICSI-derived embryos.
FAQ 4: How does the source of sperm (fresh vs. frozen-thawed testicular) affect embryo implantation?
Answer: The use of frozen-thawed testicular sperm can lead to lower embryo implantation rates compared to fresh testicular sperm [77].
- Key Supporting Data: A study reported a significantly lower implantation rate per transferred embryo when using frozen-thawed testicular sperm (9.1%) compared to fresh testicular sperm (24.6%). The live birth rate per transferred embryo was also higher in the fresh sperm group (18.8% vs. 7.9%) [77].
- Troubleshooting Implication: When possible, using fresh testicular sperm is preferable for optimal outcomes. If frozen sperm must be used, researchers should account for a potentially lower efficiency in study designs and patient counseling.
The following tables summarize key quantitative findings from recent research on long-term ICSI outcomes.
Table 1: Impact of Oocyte Degeneration on Cycle Outcomes in Young Women (<35 years) [1]
| Outcome Metric | OD Group | Non-OD Group | P-value |
|---|---|---|---|
| Implantation Rate | 38.5% | 35.1% | 0.302 |
| Clinical Pregnancy Rate | 54.9% | 50.3% | 0.340 |
| Live Birth Rate (per OPU) | 47.0% | 42.9% | 0.395 |
| Cumulative Live Birth Rate | 63.4% | 64.8% | 0.760 |
Abbreviation: OPU, Oocyte Pick-up.
Table 2: Success Rates by Patient Prognosis (POSEIDON Criteria vs. Normal Response) [78]
| Patient Group | Definition | CLBR after ~4 Cycles |
|---|---|---|
| Non-POSEIDON | Age <35, adequate ovarian reserve, optimal response to stimulation | 79.6% |
| POSEIDON Group 1 | Age <35, adequate ovarian reserve, unexpected poor response | 67.9% |
| POSEIDON Group 3 | Age <35, diminished ovarian reserve | 51.9% |
Abbreviation: CLBR, Cumulative Live Birth Rate.
Table 3: Outcomes of Re-ICSI vs. ICSI in Fresh and Frozen Transfer Cycles [76]
| Outcome Metric | Fresh ET: Re-ICSI | Fresh ET: ICSI | FET: Re-ICSI | FET: ICSI |
|---|---|---|---|---|
| Clinical Pregnancy Rate | Lower | Higher | No significant difference | No significant difference |
| Implantation Rate | Lower | Higher | No significant difference | No significant difference |
| Live Birth Rate | Lower | Higher | No significant difference | No significant difference |
Abbreviation: ET, Embryo Transfer; FET, Frozen Embryo Transfer.
Experimental Protocols for Key Studies
Protocol 1: Assessing the Impact of Oocyte Degeneration on Cumulative Live Birth Rates [1]
- Study Design: Retrospective observational cohort study.
- Participants: 488 oocyte pickup (OPU) cycles from young women (<35 years) undergoing ICSI with fresh cleavage-stage embryo transfer.
- Group Stratification:
- OD Group: Cycles with at least one degenerated oocyte post-ICSI (n=236). Further subdivided by degeneration rate: <10%, 10-20%, >20%.
- Non-OD Group: Cycles with no oocyte degeneration (n=252).
- Intervention: Controlled ovarian stimulation followed by oocyte retrieval, ICSI procedure, and fresh embryo transfer on day 3. Surplus embryos were vitrified for subsequent frozen-thawed embryo transfer (FET) cycles.
- Primary Outcome Measures: Implantation rate, clinical pregnancy rate, live birth rate per OPU, and cumulative live birth rate (including all fresh and subsequent FET cycles from one OPU).
- Statistical Analysis: Comparisons using t-tests, Chi-square tests, and logistic regression to identify independent risk factors and calculate adjusted odds ratios.
Protocol 2: Randomized Controlled Trial Comparing ICSI vs. Conventional IVF for Non-Severe Male Infertility [75]
- Study Design: Multicenter, open-label, randomized controlled trial.
- Participants: 2,329 couples with non-severe male factor infertility from 10 reproductive centers.
- Randomization:
- ICSI Group: 1,154 couples.
- Conventional IVF Group: 1,175 couples.
- Intervention: Ovarian stimulation, oocyte retrieval, and fertilization via either ICSI or conventional IVF based on randomization. Fresh or frozen single embryo transfer was performed.
- Primary Outcome: Live birth after the first embryo transfer.
- Statistical Analysis: Primary analysis by intention-to-treat using log-binomial regression models to calculate risk ratios, adjusted for the participating center.
Signaling Pathways and Workflows
ICSI Outcome Optimization Pathway
Research Reagent Solutions
Table 4: Essential Materials for ICSI and Embryo Culture Research
| Item | Function in Experiment |
|---|---|
| Recombinant FSH (e.g., Gonal-F) | For controlled ovarian stimulation to induce multifollicular development [1]. |
| Recombinant hCG (e.g., Ovidrel) | To trigger final oocyte maturation prior to retrieval [1] [78]. |
| Hyaluronidase Solution | Enzyme used to disperse cumulus and corona cells from the retrieved oocyte-cumulus complexes [1] [76]. |
| G-MOPS / G-IVF Medium | Handling and washing medium for oocytes post-retrieval and prior to ICSI [1]. |
| Sequential Culture Media (G1/G2) | Used for the in vitro culture of embryos, supporting development from fertilization to the blastocyst stage [1]. |
| Cryoprotectants & Vitrification Kits (e.g., Cryotop) | Essential for the vitrification (fast-freezing) and subsequent warming of embryos for frozen-thawed cycles [1] [76]. |
| Progesterone (e.g., Utrogestan) | Used for luteal phase support in fresh cycles and for endometrial preparation in programmed frozen embryo transfer cycles [1] [76]. |
Intracytoplasmic sperm injection (ICSI) is a cornerstone of assisted reproductive technology (ART), accounting for 70-80% of treatment cycles worldwide [79]. While it enables fertilization for couples facing severe infertility, the technique bypasses natural biological selection barriers for gametes. This raises important questions about the safety profiles and neonatal outcomes of children conceived via ICSI, particularly regarding birthweights and obstetric complications. A comprehensive analysis of these outcomes is essential for refining laboratory protocols, improving embryo viability, and reducing post-procedural complications such as embryo degeneration. This guide provides a structured, evidence-based overview of the associated risks and the laboratory techniques developed to mitigate them.
FAQs: ICSI Safety and Neonatal Outcomes
1. How does ICSI compare to conventional IVF in terms of congenital malformation risks?
Large-scale epidemiological studies and meta-analyses consistently report a statistically significant increase in the relative risk of major congenital malformations in children conceived via ART, including ICSI, compared to naturally conceived children. A sizeable study from Israel reported an adjusted odds ratio of 1.45 for congenital malformations in the IVF/ICSI population compared to naturally conceived infants [79]. Another meta-analysis of 56 studies estimated the relative risk at 1.37 [79]. The absolute increase in risk, however, remains low. The spectrum of defects often includes genitourinary, cardiovascular, musculoskeletal, and gastrointestinal anomalies [80].
2. What is the association between ICSI and imprinting disorders?
Imprinting disorders, caused by epigenetic errors at imprinting control regions, have been associated with ART. The most consistently linked syndromes are Beckwith-Wiedemann (BWS) and Angelman syndrome (AS) [79]. Crucially, 90-100% of ART-conceived children with BWS had imprinting defects as the cause, compared to only 40-50% in naturally conceived children with BWS. Similarly, imprinting defects accounted for 71% of AS cases in ART children versus only 5% in spontaneously conceived children [79]. This suggests ART procedures may interfere with the establishment or maintenance of epigenetic marks.
3. Are neonatal outcomes and birthweights different for ICSI-conceived infants?
ICSI-conceived pregnancies are at a higher risk of adverse obstetric and neonatal outcomes. A significant concern is the risk of low birth weight (LBW) and preterm delivery, even in singleton pregnancies [80]. These risks are partly confounded by the high rate of multiple gestations in ART. However, studies show that even singleton ICSI pregnancies have a higher risk of preterm delivery [80]. Maternal age is also an independent risk factor; neonates born to women aged 25.0-29.9 years have the lowest risk of LBW and perinatal mortality, while advanced maternal age (≥35 years) is associated with higher rates of hypertensive disorders and other pregnancy complications [81].
4. What laboratory techniques can improve fertilization and reduce oocyte degeneration?
Recent technical refinements focus on minimizing oocyte stress and physical damage during the injection process. The PIEZO-ICSI technique, which uses a piezoelectric pulse instead of a sharp needle to penetrate the oolemma, has shown superior outcomes compared to conventional ICSI (C-ICSI). A 2025 randomized controlled trial demonstrated that PIEZO-ICSI significantly improved the normal fertilization rate (78.0% vs. 72.6%) and significantly reduced the oocyte degeneration rate (3.2% vs. 6.3%) [82]. Furthermore, the Pre-Catching Sperm (PCS-ICSI) technique, where sperm are identified and immobilized before oocytes are loaded onto the dish, reduces oocyte exposure time outside the incubator. A 2025 retrospective study found PCS-ICSI increased fertilization rates (84.0% vs. 79.3%) and good-quality blastocyst formation (54.9% vs. 48.0%), while reducing degeneration (1.4% vs. 3.5%) [27].
Troubleshooting Guide: Addressing Common ICSI Challenges
Table: Troubleshooting Common ICSI Laboratory Challenges
| Problem | Potential Cause | Solution | Supporting Evidence |
|---|---|---|---|
| High Oocyte Degeneration Rate | Mechanical damage from conventional injection needle. | Implement PIEZO-ICSI technology. | Significantly lower degeneration rate (3.2% vs. 6.3%) [82]. |
| Suboptimal Fertilization Rates | Prolonged oocyte exposure to suboptimal conditions (temp, light) during sperm selection. | Adopt the Pre-Catching Sperm (PCS) technique. | Higher fertilization rate (84.0% vs. 79.3%) [27]. |
| Poor Blastocyst Development | Suboptimal sperm immobilization or oocyte damage. | Use PIEZO-ICSI and ensure proper sperm immobilization. | Higher blastocyst formation rate on Day 5 (50.3% vs. 43.9%) with PIEZO-ICSI [82]. |
| Recurrent Fertilization Failure | Underlying genetic defects in oocytes or sperm. | Perform exome sequencing for genetic diagnosis. | A 2025 study identified a genetic diagnostic yield of 13.2% in patients with oocyte/embryo defects [83]. |
Table: Quantitative Data on Maternal and Neonatal Risks from Key Studies
| Study Focus | Population | Key Finding | Metric |
|---|---|---|---|
| Maternal Age & Outcomes [81] | 203,517 singleton gestations. | Lowest risk of LBW and NICU admission for neonates born to women aged 25.0-29.9 yrs. | LBW: 7.2%; NICU admission: 11.5%. |
| Birthweight Extremes & Morbidity [84] | 1,855 neonates. | Morbidity is concentrated in low birthweight infants. | NICU admission: 81.5% for VLBW, 47.7% for LBW, 21.6% for macrosomic. |
| PIEZO-ICSI Efficacy [82] | 100 patients, 1,527 oocytes. | PIEZO-ICSI improves fertilization and reduces degeneration. | Normal fertilization: 78.0% (P-ICSI) vs. 72.6% (C-ICSI).Degeneration: 3.2% (P-ICSI) vs. 6.3% (C-ICSI). |
| PCS-ICSI Efficacy [27] | 617 ICSI cases. | PCS-ICSI improves lab outcomes. | Fertilization: 84.0% (PCS) vs. 79.3% (Conventional).Good Blastocyst: 54.9% (PCS) vs. 48.0% (Conventional). |
Experimental Protocols for Key Techniques
Protocol 1: PIEZO-ICSI Procedure
Objective: To fertilize oocytes while minimizing cytoplasmic damage and degeneration. Reagents:
- HEPES-buffered medium.
- Polyvinylpyrrolidone (PVP).
- Piezo-driven micropipette system.
Methodology:
- Oocyte Preparation: Denude oocytes 3-5 hours post-retrieval. Select metaphase-II oocytes for injection.
- Sperm Preparation: Immobilize a morphologically normal sperm in a PVP droplet using the piezo pulse. Avoid aggressive physical touching.
- Injection: Use a flat-tipped, hollow injection pipette. Apply a piezo pulse to penetrate the zona pellucida without pushing the pipette. Position the oolemma adjacent to the pipette tip and use a minimal piezo pulse to penetrate it.
- Post-injection Care: Gently expel the sperm with a minimal volume of medium into the ooplasm. Withdraw the pipette carefully. Wash and culture the injected oocytes in sequential culture media [82].
Protocol 2: Pre-Catching Sperm (PCS) Technique
Objective: To reduce oocyte exposure time to external environmental stress. Reagents:
- ICSI dish with 7% PVP droplets and G-MOPS PLUS medium.
- Heavy Ovoil for overlay.
Methodology:
- Sperm Pre-selection: Load the sperm sample into the 7% PVP droplet on the ICSI dish. Under the microscope, identify, wash, and immobilize multiple (e.g., 4-8) morphologically normal spermatozoa. Keep the oocytes in the incubator during this process.
- Oocyte Loading: After sperm are pre-caught and loaded into the injection pipette, transfer the mature oocytes from the incubator to the ICSI dish.
- Rapid Injection: Immediately proceed with injecting the pre-caught sperm into each oocyte. The goal is to complete the injection of all oocytes within the shortest possible time frame [27].
Visual Workflow: Optimizing ICSI to Improve Outcomes
The following diagram illustrates how integrating advanced ICSI techniques can address common failure points and lead to improved neonatal outcomes.
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagent Solutions for ICSI Optimization
| Reagent / Material | Function in ICSI Protocol | Application Note |
|---|---|---|
| Polyvinylpyrrolidone (PVP) | Slows down sperm for easier handling and immobilization. | A physiological replacement for PVP is sometimes used to avoid potential toxicity [7]. |
| HEPES-buffered Medium | Maintains stable pH outside the COâ‚‚ incubator. | Critical during dish preparation and the injection process itself. |
| Piezo-ICSI Unit | Provides high-frequency vibration for precise oolemma penetration. | Reduces mechanical damage compared to conventional sharp needles [82]. |
| Heavy Ovoil | Overlays microdroplets to prevent evaporation and osmolarity shifts. | Essential for maintaining a stable microenvironment for gametes during the lengthy procedure [27]. |
| Sequential Culture Media | Supports embryo development from zygote to blastocyst stage. | Formulated to meet changing metabolic demands of the developing embryo. |
| Hyaluronan | Used in sperm selection techniques to mimic natural selection. | Aids in choosing sperm with better DNA integrity and maturity [7]. |
Conclusion
Reducing embryo degeneration post-ICSI requires a multifaceted approach that integrates less invasive techniques like PIEZO-ICSI, advanced functional sperm selection, and rigorous laboratory optimization. Evidence confirms that PIEZO-ICSI significantly lowers oocyte degeneration and improves normal fertilization rates, while methods such as the cumulus cell column effectively reduce sperm DNA fragmentation, leading to superior embryo quality and clinical outcomes. Future research should focus on standardizing these protocols, validating non-invasive biomarkers for clinical use, and exploring novel pharmacological adjuvants. For biomedical and clinical research, the priority lies in large-scale randomized trials to confirm long-term safety and efficacy, alongside developing automated, AI-integrated systems to enhance reproducibility and accessibility of these advanced techniques, ultimately improving success rates for infertile couples.
References
- 1. Oocyte Degeneration After ICSI Is Not an Indicator of Live ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8415476/]
- 2. Comparison of the clinical outcomes between conventional ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330951]
- 3. Making ICSI Safer and More Effective: A Review of the ... [https://iv.iiarjournals.org/content/30/4/387]
- 4. Improving ICSI success rates following root cause analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9664290/]
- 5. Troubleshooting and Malfunction in the IVF Laboratory [https://www.artcompass.io/the-hidden-burden-troubleshooting-and-malfunction-in-the-ivf-laboratory/]
- 6. Improved fertilization, degeneration, and embryo quality ... [https://www.sciencedirect.com/science/article/pii/S0015028224000311]
- 7. Troubleshooting ICSI procedures (Chapter 11) [https://www.cambridge.org/core/books/troubleshooting-and-problemsolving-in-the-ivf-laboratory/troubleshooting-icsi-procedures/36609A723695FECD12336938442B6C6A]
- 8. Oocyte degeneration after intracytoplasmic sperm injection [https://pubmed.ncbi.nlm.nih.gov/16678177/]
- 9. Oocyte degeneration after intracytoplasmic sperm injection [https://www.sciencedirect.com/science/article/pii/S0015028206003700]
- 10. Oocyte degeneration in a cohort adversely affects clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10235780/]
- 11. Degenerated oocyte in the cohort adversely affects IVF outcome [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-020-00708-6]
- 12. Effect of sperm DNA fragmentation on embryo development [https://pmc.ncbi.nlm.nih.gov/articles/PMC5714603/]
- 13. Sperm DNA Fragmentation Impairs Early Embryo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12386859/]
- 14. Sperm DNA fragmentation index affect pregnancy ... [https://www.nature.com/articles/s41598-023-45091-6]
- 15. High sperm DNA fragmentation increased embryo ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648323004510]
- 16. Sperm DNA Fragmentation Impairs Early Embryo ... [https://www.mdpi.com/1422-0067/26/16/7923]
- 17. Oocyte-mediated repair of sperm DNA fragmentation [https://www.sciencedirect.com/science/article/abs/pii/S1472648325003724]
- 18. PIEZO-ICSI increases fertilization rates compared with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9935778/]
- 19. Biomarkers of human oocyte developmental competence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3059525/]
- 20. The Impact of Follicular Fluid Oxidative Stress Levels on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10740420/]
- 21. Enhancing embryo quality through meiotic spindle-aligned ... [https://www.sciencedirect.com/science/article/pii/S0929664625003869]
- 22. Improved fertilization, degeneration , and embryo quality rates with... [https://pubmed.ncbi.nlm.nih.gov/38272382/]
- 23. The Relationship between Sperm Oxidative Stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7408105/]
- 24. Comparison of the clinical outcomes between conventional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12396638/]
- 25. Reproductive Medicine gets Help from Piezo Technology [https://www.pi-usa.us/en/tech-blog/piezo-icsi-in-reproductive-medicine]
- 26. Piezoâ€assisted ICSI improves fertilization and blastocyst ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6780025/]
- 27. The Pre-Catching Sperm Technique Increases ... [https://www.mdpi.com/2077-0383/14/14/4872]
- 28. Journal Club Global LIVE at MRSi 2025: Sibling Oocyte ... [https://www.asrm.org/journals/fertility-and-sterility/journal-club-global/journal-club-global-live-at-mrsi-2025-sibling-oocyte-studies-in-art/]
- 29. Time-lapse imaging systems for embryo incubation and ... [https://pubmed.ncbi.nlm.nih.gov/40730404/]
- 30. Sperm Selection Using Cumulus Cell Column Improves ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631016/]
- 31. Transcriptomics of cumulus cells – a window into oocyte ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-020-00696-7]
- 32. Sperm DNA Fragmentation: A New Guideline for Clinicians [https://pmc.ncbi.nlm.nih.gov/articles/PMC7502318/]
- 33. An Effective Approach for Reducing Sperm DNA ... [https://pubmed.ncbi.nlm.nih.gov/41103587/]
- 34. Effects on Embryo Quality, Cumulative Pregnancy Rate, ... [https://pubmed.ncbi.nlm.nih.gov/40426931/]
- 35. Rescuing Fertilization Failure in ICSI: A Narrative Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383768/]
- 36. ICSI Pregnancy Success Rates by Age: What to Expect ... [https://geneticsandfertility.com/icsi-pregnancy-success-rates-by-age/]
- 37. Morphokinetic analysis of in vitro fertilization outcomes [https://pubmed.ncbi.nlm.nih.gov/37364673/]
- 38. Deep learning methods to forecasting human embryo ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330924]
- 39. The Pre-Catching Sperm Technique Increases ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295494/]
- 40. Noninvasive Biomarkers of Human Embryo Developmental ... [https://www.mdpi.com/1422-0067/26/10/4928]
- 41. Noninvasive Biomarkers of Human Embryo Developmental ... [https://pubmed.ncbi.nlm.nih.gov/40430065/]
- 42. Non-invasive metabolomic profiling of culture media of ICSI [https://www.sciencedirect.com/science/article/abs/pii/S0378432018303841]
- 43. Designing and Analysing Omics Experiments [https://insigene.com/omics-experiement-design/]
- 44. USP30: Structure, Emerging Physiological Role, and Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8927814/]
- 45. Spotlight on USP30: structure, function, disease and target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411550/]
- 46. Pharmacological Inhibition of USP30 activates Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8266733/]
- 47. Inhibition of USP30 Promotes Mitophagy by Regulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11976779/]
- 48. Knockout or inhibition of USP30 protects dopaminergic ... [https://www.nature.com/articles/s41467-023-42876-1]
- 49. The future of embryo engineering and fertility research in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12426076/]
- 50. Should ICSI be implemented on patients with poor-quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10362230/]
- 51. Structural Premise of Selective Deubiquitinase USP30 ... [https://www.sciencedirect.com/science/article/pii/S1535947623001202]
- 52. Implementation of air quality control in reproductive ... [https://pubmed.ncbi.nlm.nih.gov/23177417/]
- 53. How to ensure embryo viability in your culture system [https://blog.vitrolife.com/togetheralltheway/how-to-ensure-embryo-viability-in-your-culture-system]
- 54. Rational cell culture optimization enhances experimental ... [https://www.nature.com/articles/s41598-018-21050-4]
- 55. Employing active learning in the optimization of culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10229643/]
- 56. Optimizing the culture environment and embryo ... [https://www.sciencedirect.com/science/article/pii/S0015028216000765]
- 57. Development of a generally applicable morphokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5027927/]
- 58. FAQs from IVF-ICSI Patients About MAGENTAâ„¢ [https://futurefertility.com/en/resources/faqs-from-ivf-icsi-patients-about-magenta/]
- 59. MAIA platform for routine clinical testing: an artificial ... [https://www.nature.com/articles/s41598-025-17755-y]
- 60. Predicting pregnancy outcomes in IVF cycles: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476623/]
- 61. Embryo selection with artificial intelligence: how to evaluate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8324599/]
- 62. Improving embryo selection by the development of a ... [https://www.sciencedirect.com/science/article/abs/pii/S2666335X21000288]
- 63. Troubleshooting ICSI procedures [https://obgynkey.com/troubleshooting-icsi-procedures/]
- 64. Use of comprehensive chromosomal screening for embryo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2639447/]
- 65. PIEZO-ICSI increases fertilization rates compared with conventional ICSI in patients with poor prognosis - PubMed [https://pubmed.ncbi.nlm.nih.gov/36586007/]
- 66. PIEZO-ICSI increases fertilization rates compared with standard ICSI: a prospective cohort study - PubMed [https://pubmed.ncbi.nlm.nih.gov/34326006/]
- 67. Developmental arrest rate of an embryo cohort correlates ... [https://www.aging-us.com/article/206328/text]
- 68. Development and validation of machine learning models ... [https://www.nature.com/articles/s41598-025-06998-4]
- 69. The impact of completely shrunken blastocysts on clinical ... [https://www.nature.com/articles/s41598-025-17526-9]
- 70. Long-term embryo vitrification is associated with reduced ... [https://www.sciencedirect.com/science/article/abs/pii/S0301211524001167]
- 71. Elective cryopreservation of all day 5 blastocysts is more ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5891804/]
- 72. Understanding the Warming Procedure for Vitrified Embryos [https://www.aab.org/NewsBot.asp?MODE=VIEW&ID=1070]
- 73. What happens when culture media gets warm or cold ... [https://blog.vitrolife.com/togetheralltheway/what-happens-when-culture-media-gets-warm-or-cold-during-transport]
- 74. The impact of season, temperature, and direct normal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12287234/]
- 75. RCT Results: Does ICSI Improve Live Birth Rates ... [https://www.obgproject.com/2024/02/29/rct-results-does-icsi-improve-live-birth-rates-compared-to-conventional-ivf-for-non-severe-male-factor-infertility/]
- 76. Comparing the pregnancy outcomes of Re‑ICSI and ... [https://www.spandidos-publications.com/10.3892/br.2023.1648]
- 77. Fertilization, pregnancy and embryo implantation rates ... [https://pubmed.ncbi.nlm.nih.gov/9740444/]
- 78. Cumulative live birth rates and birth outcomes after IVF ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10098357/]
- 79. Potential Health Risks Associated to ICSI [https://pmc.ncbi.nlm.nih.gov/articles/PMC4235077/]
- 80. Intracytoplasmic Sperm Injection (ICSI) – What are the risks? [https://pmc.ncbi.nlm.nih.gov/articles/PMC2424218/]
- 81. Obstetric Complications, Neonatal Morbidity, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4189107/]
- 82. Comparison of the clinical outcomes between conventional ... [https://pubmed.ncbi.nlm.nih.gov/40880358/]
- 83. Genetic landscape of human oocyte/embryo defects [https://www.sciencedirect.com/science/article/pii/S2666979X2500268X]
- 84. Neonatal Birthweight Spectrum: Maternal Risk Factors and ... [https://www.mdpi.com/1648-9144/60/2/193]