Troubleshooting Low Birth Rates After Mouse Embryo Transfer: A Comprehensive Guide for Researchers
This article provides a systematic guide for researchers and scientists troubleshooting low live birth rates in mouse embryo transfer (ET).
Troubleshooting Low Birth Rates After Mouse Embryo Transfer: A Comprehensive Guide for Researchers
Abstract
This article provides a systematic guide for researchers and scientists troubleshooting low live birth rates in mouse embryo transfer (ET). It synthesizes foundational principles, methodological refinements, and optimization strategies, covering the impact of assisted reproductive technologies (ARTs) on embryo genetics, procedural choices like surgical versus non-surgical transfer, and critical factors including embryo culture conditions, recipient strain selection, and technical execution. By integrating validation data and comparative analyses, the content offers evidence-based recommendations to enhance efficiency and reproducibility in transgenic and biomedical research.
Understanding the Core Principles and Causes of Embryo Transfer Failure
The Impact of In Vitro Culture on Embryonic Development and Viability
Troubleshooting Guides
Troubleshooting Low Birth Rates After Mouse Embryo Transfer
Q: Despite high-quality embryos, my mouse embryo transfers are resulting in low birth rates. What are the primary technical factors I should investigate?
Low birth rates following embryo transfer (ET) can stem from issues related to the embryo itself, the transfer procedure, or the recipient female's uterine environment. Systematically investigate the following areas.
Table 1: Troubleshooting Low Birth Rates: Procedure and Environment
| Problem Area | Specific Issue to Check | Suggested Solution |
|---|---|---|
| Embryo Transfer Technique | Excessive medium volume transferred, causing embryo expulsion [1]. | Reduce transfer volume to ≤ 1 µL [1]. |
| Trauma or bleeding during the transfer procedure [1]. | Use a sharp, ground transfer pipette to avoid pre-puncturing the oviduct [1]. | |
| Clogged or contaminated transfer catheter [1]. | Ensure catheters are free of mucus, blood, or bacterial contamination [1]. | |
| Recipient Uterine Environment | Suboptimal receptivity due to hormonal imbalance [2]. | Use an ovariectomized recipient model with exogenous hormone replacement for precise control [2]. |
| Uterine contractions during transfer [3]. | Consider using a smooth muscle relaxant prior to the procedure [3]. | |
| Genetic strain of the recipient female [4]. | Avoid strains with known low fertility; use robust outbred (e.g., NMRI) or F1 hybrid strains as recipients [1] [4]. |
Table 2: Troubleshooting Low Birth Rates: Embryo and Culture Conditions
| Problem Area | Specific Issue to Check | Suggested Solution |
|---|---|---|
| In Vitro Culture Conditions | Suboptimal culture media composition [5] [6]. | Test different media formulations; consider reduced nutrient concentrations that may better mimic in vivo conditions [6]. |
| Cumulative stress from pH, temperature, or osmolality fluctuations [5] [7]. | Tightly control incubator environment and use pre-equilibrated media [5]. | |
| Toxicity from culture media, oil, or labware [7]. | Use quality-tested, embryo-safe reagents and perform Mouse Embryo Assays (MEA) on all materials [7]. | |
| Embryo Viability | Undetected low developmental potential despite good morphology [7]. | Go beyond morphology; use time-lapse imaging and cell counting to select the most viable embryos [8] [7]. |
| Genetic abnormalities in the embryo [8] [3]. | Consider preimplantation genetic testing if using genetically modified strains. |
Q: How can I optimize my embryo transfer technique to maximize birth rates?
A refined ET technique can significantly improve birth rates. A study demonstrated that a novel method achieved a 42.4% live birth rate compared to 21.7% with a conventional technique [1].
Optimized Protocol for Oviductal Embryo Transfer [1]:
- Pipette Preparation: Use a pulled and ground glass micropipette with an inner diameter of 150-200 µm and a sharp, 45-degree angled tip.
- Loading Embryos: Load embryos using a manual piston micro-pump (e.g., Cell Tram). Arrange embryos in a minimal volume of medium (≤ 1 µL) with air bubbles for visualization.
- Transfer: Gently insert the sharp pipette tip directly into the wall of the second coil of the oviduct. Use the micro-pump to expel the embryos with minimal fluid volume.
- Key Advantage: This method eliminates the need to pre-puncture the oviduct with a needle, reduces transfer volume to prevent expulsion, and minimizes tissue trauma and bleeding.
Troubleshooting Embryo Culture Viability
Q: My embryos develop to blastocysts in culture but have low viability and implantation potential. How can I improve the culture system?
This is a common issue where morphology does not equate to viability. The problem often lies in the cumulative stress of suboptimal culture conditions [7].
Table 3: Troubleshooting Embryo Viability in Culture
| Critical Factor | Potential Problem | Evidence-Based Solution |
|---|---|---|
| Culture Media | Static media does not mimic the dynamic in vivo environment [5]. | Consider using sequential or single-step media optimized for metabolic shifts [5]. |
| Standard nutrient concentrations may be supraphysiological [6]. | Test reduced nutrient concentrations (e.g., 50% dilution), which have been shown to improve blastocyst rates and metabolic health in bovine models [6]. | |
| Laboratory Environment | Fluctuations in temperature, pH, and osmolality [5] [3]. | Use pre-equilibrated incubators with strict temperature and gas control. Minimize embryo exposure to room air [3]. |
| Toxicity | Undetected toxicity from plasticware, media components, or oil [7]. | Implement a sensitive Mouse Embryo Assay (MEA) for quality control. Use only reagents tested for embryo safety [7]. |
Essential Protocol: Sensitive Mouse Embryo Assay (MEA) for Quality Control [7] [9]
To ensure your entire culture system is free of toxins, a properly designed MEA is critical.
- Mouse Strain: For routine testing, use F1 hybrid strains (e.g., B6CBA/F1J). For increased sensitivity to detect subtle toxins, use an outbred strain (e.g., Swiss) [7] [9].
- Embryo Stage: Collect and culture zygotes (1-cell) rather than 2-cell embryos, as they are more sensitive to suboptimal conditions [9].
- Sensitization: For maximum sensitivity, remove the zona pellucida before culture [9].
- Endpoint Analysis: Do not rely solely on blastocyst formation rate at 96 hours.
- Perform Cell Counting: Differentiate between high- and low-quality blastocysts by staining and counting total cell numbers. A morphologically normal blastocyst with a low cell count indicates suboptimal conditions [7].
- Assess Developmental Timing: Use time-lapse imaging to check for developmental delays, which can be an early sign of stress [7].
Frequently Asked Questions (FAQs)
Q: Does the genetic background of the mouse strain affect embryo transfer outcomes? A: Yes, significantly. Inbred strains like 129 mice are known for poor reproductive performance, including low fertilization rates and small litter sizes, primarily due to female factors [4]. For optimal results in ET, use robust outbred strains (e.g., NMRI) or F1 hybrids (e.g., C57BL/6J x DBA/2) as embryo donors or recipients [1] [4].
Q: What is a "behavioral sink" and could it be affecting my animal colony's reproduction? A: The "behavioral sink" is a term from ethology describing a collapse in social behavior, including reproduction, due to extreme population density [10]. While observed in confined rodent populations, its direct applicability to standard laboratory housing is debated [10]. However, maintaining animals at recommended densities and providing a low-stress environment is essential for reliable reproductive data.
Q: How can I isolate the effect of the uterine environment from other variables in my study? A: The Ovariectomized Mouse Embryo Transfer Model is designed for this purpose [2].
- Method: Recipient females are ovariectomized to eliminate endogenous ovarian hormone production. They are then given exogenous hormones (estradiol and progesterone) to precisely control the uterine cycle. Embryos from healthy, unexposed donors are transferred into these prepared recipients [2].
- Benefit: This model ensures that any changes in pregnancy outcome (e.g., implantation sites, fetal growth) are due to the uterine environment of the recipient and not the embryo's quality or the recipient's ovarian function.
The Scientist's Toolkit
Table 4: Key Research Reagent Solutions
| Reagent/Material | Function in Experiment | Key Considerations |
|---|---|---|
| Sequential or Single-Step Culture Media | Supports embryo development from fertilization to blastocyst by providing stage-specific nutrients [5]. | Single-step media reduce embryo handling stress. Sequential media aim to mimic the oviduct-to-uterus metabolic transition [5]. |
| Hormones for Superovulation (PMSG/eCG & hCG) | Stimulates female donors to produce a large number of oocytes for collection [1] [2]. | Dose and timing are strain-dependent. Over-stimulation can affect oocyte quality. |
| Exogenous Hormone Regimen (Estradiol & Progesterone) | Creates a precisely synchronized and controlled uterine state in ovariectomized recipient females [2]. | Allows for the study of uterine-specific contributions, independent of the recipient's ovarian cycle [2]. |
| Modified M2 Medium | A handling medium used outside the incubator for procedures like embryo flushing and transfer. It buffers against air-level CO2 [1] [4]. | Embryos should not be kept in M2 for prolonged periods. Use pre-warmed medium to avoid temperature shock. |
| KSOM or SOFaa Media | Common complex culture media used for long-term in vitro development of mouse embryos to the blastocyst stage [1] [6]. | Often supplemented with amino acids and growth factors. Must be equilibrated in a CO2 incubator before use. |
| Sensitive Mouse Embryo Assay (MEA) | A bioassay to test the toxicity and safety of all materials (media, plastic, oil) that contact gametes/embryos [7]. | For high sensitivity, use zygotes from outbred strains, remove the zona pellucida, and use cell counting as an endpoint [7] [9]. |
| Fuscaxanthone C | Fuscaxanthone C, CAS:15404-76-9, MF:C26H30O6, MW:438.5 g/mol | Chemical Reagent |
| Traumatic Acid | Traumatic Acid, CAS:6402-36-4, MF:C12H20O4, MW:228.28 g/mol | Chemical Reagent |
Experimental Workflows and Pathways
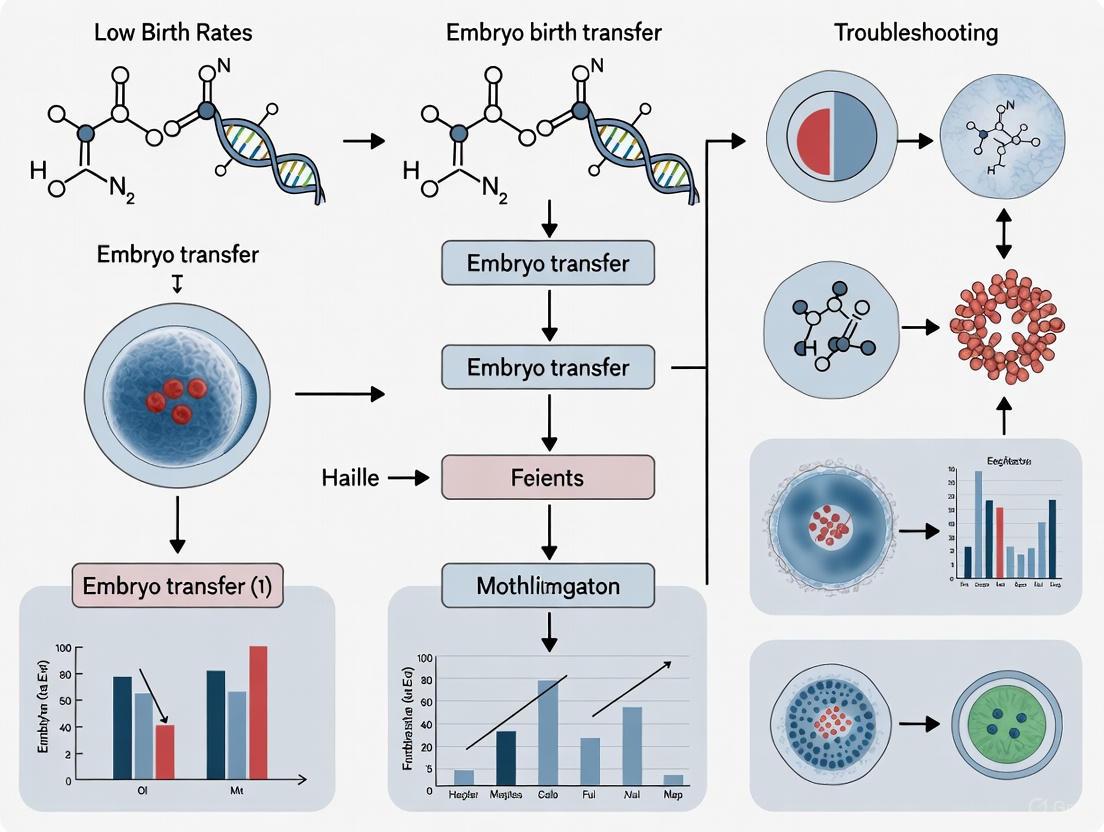
Diagram 1: Low Birth Rate Troubleshooting Workflow
How ART Procedures Can Introduce Genetic and Epigenetic Variations
For researchers troubleshooting low birth rates in mouse embryo transfer models, understanding the genetic and epigenetic variations introduced by Assisted Reproductive Technologies (ART) is paramount. ART procedures, while enabling conception, coincide with critical developmental windows and can act as environmental stressors, potentially disrupting delicate molecular programming. These variations are a plausible contributing factor to suboptimal experimental outcomes, including reduced live birth rates. This guide provides a targeted, technical resource to help you identify, understand, and mitigate these variations in your research.
FAQs: Core Concepts for the Researcher
1. What is the fundamental distinction between genetic and epigenetic variations introduced by ART?
- Genetic Variations are changes to the DNA sequence itself. An example is the introduction of single-nucleotide variants (SNVs), which are alterations in a single DNA base pair. A 2025 mouse study found that ART-conceived pups had approximately 30% more new SNVs compared to naturally conceived counterparts [11].
- Epigenetic Variations are changes in gene expression that do not involve alterations to the underlying DNA sequence. These include changes in DNA methylation, which is the addition of a methyl group to a cytosine base, often silencing gene expression. ART procedures can disrupt the natural cycles of global DNA methylation erasure and re-establishment during gametogenesis and early embryogenesis [12] [13].
2. Which specific ART procedures are most associated with introducing these variations?
The risk is cumulative, but several key procedures have been identified as particularly impactful [12]:
- Ovarian Hyperstimulation: High-dose hormonal treatments can alter DNA methylation reprogramming and imprint acquisition in oocytes [12].
- In Vitro Fertilization (IVF) & Intracytoplasmic Sperm Injection (ICSI): The physical and chemical manipulation of gametes occurs during a highly sensitive period of epigenetic reprogramming. ICSI has been most consistently linked to multi-locus imprinting disturbances [12].
- Embryo Culture: Exposure to non-physiological conditions (e.g., oxygen concentration, pH, culture media composition) can alter methylation at critical imprinting control regions (ICRs) [12].
3. Are there sex-specific differences in how embryos respond to ART-induced epigenetic changes?
Yes, emerging evidence indicates significant sex-specific effects. A 2024 human cohort study found that ART-conceived newborn girls and boys exhibited distinct patterns of DNA methylation variation in cord blood [14]. The study identified:
- 37 differentially methylated CpGs in ART-conceived girls.
- 70 differentially methylated CpGs in ART-conceived boys.
- Only 10 CpGs were altered in both sexes, highlighting that the epigenetic impact of ART is nuanced and sex-specific [14]. This suggests that experimental outcomes, including birth rates, may vary significantly based on the sex of the embryos used.
4. What are Imprinting Disorders (IDs) and why are they relevant to my mouse model?
Imprinting Disorders (IDs) are diseases caused by the aberrant expression of imprinted genes—genes expressed in a parent-of-origin-specific manner [12]. ART procedures can disrupt the epigenetic marks that regulate these genes. In mouse models, this may not manifest as a full-blown disorder but as developmental abnormalities, growth irregularities, or prenatal lethality, all of which directly contribute to low birth rates. Key genes and regions to monitor include those associated with Beckwith-Wiedemann syndrome (BWS) and Silver-Russell syndrome (SRS) [12].
Troubleshooting Guide: Low Birth Rate After Mouse Embryo Transfer
Problem: Suspected ART-Induced Genetic and Epigenetic Variations
| Observed Symptom | Potential Underlying Variation | Recommended Experimental Analysis | Citations |
|---|---|---|---|
| High rates of pre-/post-implantation loss | Disruption of genomic imprinting; Imprinting Disorders (IDs) | Preimplantation Genetic Diagnosis (PGD): Analyze methylation status of Imprinting Control Regions (ICRs) like H19/IGF2 and SNRPN. | [12] |
| Reduced litter size; developmental delays | General epigenetic dysregulation from culture conditions | DNA Methylation Analysis: Perform whole-genome bisulfite sequencing (WGBS) or targeted analysis of differentially methylated regions (DMRs) in blastocysts. | [12] [14] |
| Offspring with growth abnormalities | Altered methylation at growth-related genes (e.g., IGF2) | Targeted Methylation Assay: Use pyrosequencing to validate methylation levels at specific growth-related DMRs. | [12] |
| Sex-biased reduction in birth rates | Sex-specific epigenetic alterations | Sex-Stratified Analysis: Separate male and female embryo data and conduct sex-specific epigenetic profiling (e.g., immunofluorescence for H3K27me3). | [14] |
| Increased minor physical anomalies | Accumulation of single-nucleotide variants (SNVs) | Whole-Genome Sequencing: Compare SNV load in ART-conceived vs. naturally conceived pups to confirm ~30% increase. | [11] |
Experimental Protocols for Detection and Validation
Protocol 1: Assessing DNA Methylation at Imprinted Loci
Method: Combined Bisulfite Restriction Analysis (COBRA) or Pyrosequencing. Application: Targeted, quantitative analysis of known imprinted genes. Steps:
- DNA Extraction: Isolate genomic DNA from mouse blastocysts or placental tissue.
- Bisulfite Conversion: Treat DNA with sodium bisulfite, which converts unmethylated cytosines to uracils (read as thymine in sequencing), while methylated cytosines remain unchanged.
- PCR Amplification: Amplify the Imprinting Control Region (ICR) of interest using primers designed for bisulfite-converted DNA.
- Quantification:
- COBRA: Digest the PCR product with a restriction enzyme that cuts at a site dependent on methylation status. Separate fragments by gel electrophoresis and quantify the ratio.
- Pyrosequencing: Sequence the PCR product to provide a quantitative percentage of methylation at each CpG site within the amplicon [12] [14].
Protocol 2: Genome-Wide Mutation Load Screening
Method: Whole-Genome Sequencing (WGS). Application: Identifying the full spectrum of genetic variants, including single-nucleotide variants (SNVs). Steps:
- Library Preparation: Fragment genomic DNA from ART-conceived and control pups and prepare sequencing libraries.
- High-Throughput Sequencing: Sequence to a high coverage depth (e.g., 30x).
- Variant Calling: Use a bioinformatics pipeline (e.g., BWA for alignment, GATK for variant calling) to identify new SNVs present in the ART pups but absent in the parental genomes.
- Validation: Confirm a subset of the identified SNVs using Sanger sequencing. The expected signal is an increase in the total number of de novo SNVs in the ART group [11].
Signaling Pathways and Workflow Diagrams
ART-Induced Variations Pathway
Troubleshooting Experimental Workflow
The Scientist's Toolkit: Key Research Reagents & Materials
| Item / Reagent | Critical Function | Application in ART Variation Research |
|---|---|---|
| Sodium Bisulfite | Chemically converts unmethylated cytosine to uracil for methylation detection. | Essential for COBRA, pyrosequencing, and whole-genome bisulfite sequencing to map DNA methylation patterns [14]. |
| DNMT/TET Inhibitors | Pharmacologically modulates the DNA (de)methylation machinery. | Used in controlled experiments to mimic ART-induced epigenetic disruption and test resilience of embryos [13]. |
| Defined Culture Media | Provides a controlled, physiological environment for embryo development. | Critical for testing the hypothesis that media composition (e.g., methyl donors) affects epigenetic marks; a key mitigation variable [12] [15]. |
| Anti-5-Methylcytosine Antibody | Enables immunodetection of global DNA methylation levels. | Used in immunofluorescence or immunoprecipitation (MeDIP) protocols to visually quantify and localize DNA methylation in embryos [13]. |
| Primers for Imprinted DMRs | Amplifies specific Imprinting Control Regions (ICRs) for analysis. | Required for targeted methylation analysis of key regions like H19/IGF2 and SNRPN via COBRA or pyrosequencing [12]. |
| Electronic Witnessing System | Uses barcodes or RFID to track gametes/embryos, preventing misidentification. | A critical quality control measure to eliminate sample mix-ups, a potential confounder in data analysis [15] [16]. |
| (-)-Epipodophyllotoxin | (-)-Epipodophyllotoxin, CAS:4375-07-9, MF:C22H22O8, MW:414.4 g/mol | Chemical Reagent |
| Gentianose | Gentianose, CAS:25954-44-3, MF:C18H32O16, MW:504.4 g/mol | Chemical Reagent |
For researchers troubleshooting low birth rates in mouse embryo transfer experiments, achieving consistent success hinges on mastering three interdependent factors: the intrinsic quality of the embryo, the receptivity of the recipient's uterus, and the precise synchrony between the embryo's developmental stage and the recipient's hormonal milieu. This guide provides targeted troubleshooting advice and FAQs to help diagnose and resolve the common challenges that compromise litter sizes in reproductive and developmental studies.
## Troubleshooting Guide: Diagnosing Low Birth Rates
This guide helps you systematically identify and address the most common causes of low birth rates in mouse embryo transfer experiments.
| Problem Area | Key Questions for Diagnosis | Potential Causes & Solutions |
|---|---|---|
| Embryo Quality | • What is the morphological grade of transferred embryos?• Were the embryos vitrified/warmed or used fresh?• What was the developmental stage (cleavage vs. blastocyst)? | • Cause: Poor morphological quality [17].• Solution: Prioritize transfer of high-quality blastocysts.• Cause: Suboptimal vitrification protocol [18].• Solution: Standardize cryopreservation reagents and protocols to minimize transcriptomic stress. |
| Recipient Receptivity | • What was the endometrial thickness prior to transfer?• Was the uterine morphology evaluated?• What was the recipient's age and hormonal status? | • Cause: Inadequate endometrial thickness [17] [19].• Solution: Ensure endometrial thickness meets minimum thresholds via ultrasound.• Cause: Advanced recipient age or poor ovarian reserve (low AMH) [19].• Solution: Use young, reproductively proven recipients with confirmed hormonal cyclicity. |
| Embryo-Uterine Synchrony | • How was the timing of progesterone administration calibrated?• Was the recipient's natural cycle used or an artificial protocol? | • Cause: Imperfect synchronization between embryo developmental age and uterine receptivity window.• Solution: Precisely time the transfer relative to the recipient's ovulation or progesterone administration [20]. |
## Frequently Asked Questions (FAQs)
Q1: What is the single most critical factor for a successful embryo transfer? While all factors are interlinked, high embryo quality is consistently identified as the strongest independent predictor of successful implantation and clinical pregnancy [17]. In multivariate analyses, embryo quality often outweighs other variables, making it a primary focus for optimization.
Q2: Does using frozen-thawed (vitrified) embryos compromise birth rates compared to fresh embryos? Not necessarily. When optimized, vitrification can yield high success. One transcriptomic study in mice even reported a significantly higher implantation rate for vitrified-warmed blastocysts (83.3%) compared to fresh ones (56.7%) [18]. The freeze-thaw process induces specific transcriptomic changes that may enhance implantation potential. Success depends heavily on a reliable vitrification protocol.
Q3: How does the developmental stage of the embryo (cleavage vs. blastocyst) impact success? Transferring blastocysts is generally associated with significantly higher clinical pregnancy rates compared to cleavage-stage embryos [19]. Blastocyst transfer allows for better selection of viable embryos and may be more physiologically synchronous with the uterine environment.
Q4: What endometrial thickness should I target in the recipient mouse? While specific metrics for mice are less defined, principles from clinical studies emphasize the importance of adequate endometrial thickness. In human studies, a thicker endometrium on the day of transfer is an independent factor associated with higher pregnancy rates [19]. Researchers should establish and monitor baseline thickness metrics for their mouse strain.
Q5: Beyond the embryo and uterus, what other patient factors should I consider in my model? Recipient factors such as younger age and robust ovarian reserve (reflected in higher AMH levels) are significantly associated with improved pregnancy outcomes [19]. These should be standard controlled variables in experimental design.
## Experimental Protocols for Key Analyses
Protocol 1: Transcriptomic Analysis of Vitrified-Warmed vs. Fresh Blastocysts
This protocol is based on a study that investigated the molecular mechanisms behind the improved implantation rates of vitrified mouse blastocysts [18].
1. Embryo Collection and Group Allocation:
- Collect blastocysts from superovulated mice.
- Randomly allocate embryos to either the vitrified-warmed group or the fresh control group.
2. Vitrification and Warming:
- Vitrify the embryos using a standardized clinical vitrification kit and protocol (e.g., Kitazato Cryotop method).
- After a defined storage period, warm the embryos according to the manufacturer's protocol.
3. Embryo Transfer and Implantation Rate Calculation:
- Surgically transfer an equal number of vitrified-warmed and fresh embryos into the left and right uterine horns, respectively, of the same recipient mouse. This controls for inter-individual variability.
- After a set period, euthanize the mouse and count the number of implantation sites in each uterine horn.
- Calculate the implantation success rate as: (Number of implantation sites / Number of embryos transferred) * 100.
4. RNA Sequencing (RNA-Seq):
- Pool blastocysts from each group (vitrified-warmed and fresh) and extract total RNA.
- Prepare cDNA libraries and perform high-throughput RNA sequencing.
5. Bioinformatic Analysis:
- Identify Differentially Expressed Genes (DEGs) using criteria such as fold-change >1.5 and p-value <0.05.
- Perform Gene Ontology (GO) enrichment analysis to identify affected biological processes, cellular components, and molecular functions.
- Conduct KEGG pathway enrichment analysis to pinpoint significantly altered signaling pathways (e.g., Thermogenesis, MAPK signaling).
Protocol 2: Assessing Factors in a Frozen-Thawed Embryo Transfer (FET) Cycle
This protocol outlines the key parameters to measure when evaluating the success of frozen embryo transfers, as derived from large-scale clinical analyses [17] [19].
1. Preliminary Recipient Assessment:
- Record baseline characteristics: age, weight, and hormonal markers (e.g., AMH levels via ELISA).
- Prepare the endometrium using hormone replacement therapy (estrogen followed by progesterone).
2. Endometrial Receptivity Evaluation:
- On the day of progesterone initiation or embryo transfer, use ultrasound to measure:
- Endometrial Thickness: Measure in the midsagittal plane.
- Endometrial Morphology: Classify as Type A (triple-line) or Type B (homogeneous) [17].
- (Optional) Assess endometrial-subendometrial blood flow using Power Doppler.
3. Embryo Assessment and Transfer:
- Thaw cryopreserved embryos using a standardized warming protocol.
- Grade embryos according to consensus systems (e.g., Gardner and Schoolcraft for blastocysts).
- Select the highest-quality embryo(s) for transfer.
- Perform the embryo transfer procedure under ultrasound guidance.
4. Outcome Measurement:
- Confirm pregnancy by measuring serum ß-hCG levels at a defined time post-transfer (e.g., 12 days).
- Confirm clinical pregnancy by visualizing a gestational sac via ultrasound at 6 weeks.
5. Statistical Analysis:
- Compare characteristics between pregnant and non-pregnant groups using appropriate statistical tests (e.g., Chi-square, Mann-Whitney U-test).
- Use logistic regression analysis to identify independent variables (e.g., embryo quality, endometrial thickness, age) associated with successful pregnancy outcomes.
## Signaling Pathways in Embryo Implantation
Transcriptomic analysis of vitrified-warmed blastocysts reveals activation of specific signaling pathways that enhance implantation potential. The following diagram illustrates the interconnected pathways and cellular processes involved.
{{< svg >}} {{< /svg >}}
Cryo-Induced Signaling Pathways for Implantation Figure 1: Vitrification stress activates upstream pathways like thermogenesis and reactive oxygen species (ROS) generation, which promote oxidative phosphorylation to boost cellular energy (ATP). This enhanced energy activates the MAPK signaling pathway, driving cellular processes critical for successful embryo implantation [18].
## The Scientist's Toolkit: Key Research Reagents
The following table details essential materials and their functions for conducting robust embryo transfer research.
| Item Name | Function / Application |
|---|---|
| Recombinant FSH (r-FSH) | Used for controlled ovarian hyperstimulation in donor mice to retrieve multiple oocytes [17]. |
| GnRH Agonist/Antagonist | Regulates the natural menstrual/hormonal cycle to prevent premature ovulation and allow for timed procedures [17]. |
| Kitazato Vitrification Kit | A standardized set of solutions and devices (e.g., Cryotop) for the rapid cryopreservation of embryos via vitrification, minimizing ice crystal formation [17]. |
| Hormone Replacement Therapy (HRT) Drugs | Estrogen and progesterone are used to artificially prepare and control the recipient's uterine lining in a programmed cycle, ensuring receptivity [17] [21]. |
| G-TL Culture Media | A specific sequential culture medium used for in-vitro embryo development from fertilization up to the blastocyst stage [17]. |
| Power Doppler Ultrasound | Used to non-invasively assess endometrial receptivity by measuring endometrial thickness, morphology, and subendometrial blood flow [17]. |
| Preimplantation Genetic Testing (PGT) Reagents | Kits for trophectoderm biopsy and genetic analysis (e.g., for aneuploidy screening) to select the most viable, euploid embryos for transfer [21] [20]. |
| 5-O-Methylvisammioside | 5-O-Methylvisammioside, CAS:84272-85-5, MF:C22H28O10, MW:452.5 g/mol |
| Harmalol | Harmalol|Beta-Carboline Alkaloid|For Research |
Selecting and Implementing the Right Embryo Transfer Technique
This technical support center provides targeted troubleshooting guidance for researchers experiencing low birth rates in mouse embryo transfer experiments. Embryo transfer is a critical step in generating genetically engineered mouse models, and its success is vital for efficient research and drug development. This guide offers a comparative analysis of surgical and non-surgical embryo transfer (NSET) protocols, focusing on practical solutions for optimizing outcomes in a laboratory setting.
Troubleshooting Guides
FAQ: Addressing Low Birth Rates in Mouse Embryo Transfer
Q1: What are the primary procedural factors that could lead to low birth rates after mouse embryo transfer? Low birth rates can stem from several procedural factors. The choice of transfer method itself is significant. The NSET procedure uses a small, tapered catheter inserted through the cervix, while surgical transfer requires an incision to exteriorize the reproductive tract [22]. This fundamental difference impacts physiological stress; studies show the NSET procedure is associated with less fluctuation in cardiac rhythm and lower levels of the stress biomarker fecal corticosterone compared to surgery [22]. Additionally, embryo handling, the skill of the technician, and the use of anesthesia and analgesia in surgical protocols can all influence success [22].
Q2: Beyond the procedure, what embryo-related factors should I investigate? The quality and developmental stage of the embryos are paramount. You should examine:
- Morphological Quality: Assess embryos for appropriate cell number, degree of fragmentation, and blastomere symmetry. The presence of multinucleated blastomeres is associated with diminished developmental potential [23].
- Genetic Status: If working with genetically modified embryos, the modification process itself (e.g., DNA microinjection, embryonic stem cell-containing embryos) can affect viability [22]. Consider that some assisted reproductive technologies, like IVF, have been linked to a slight increase in de novo mutations in mice, though most are neutral [11].
- Developmental Stage: Ensure the embryo stage (e.g., morula, blastocyst) is synchronized with the recipient's pseudopregnant state [22].
Q3: How does the recipient mouse's condition affect the birth rate? The health and management of the pseudopregnant recipient are critical. Key factors include:
- Physiological Stress: As noted, surgical transfer induces a greater stress response, which can negatively impact implantation and pregnancy maintenance [22].
- Uterine Receptivity: The success of implantation depends on a synchronized "dialogue" between the embryo and the endometrium during a short period known as the window of implantation (WOI) [23]. While methods to precisely define the WOI in mice are less common than in human IVF, ensuring recipients are at the correct days post-coitum (dpc) is essential [22].
- Health Status: Underlying infections, poor nutrition, or environmental stressors can compromise the recipient's ability to carry a pregnancy to term.
Quantitative Data Comparison
The following tables summarize key comparative data between surgical and NSET embryo transfer protocols.
Table 1: Comparison of Procedural and Outcome Parameters
| Parameter | Surgical Embryo Transfer | Non-Surgical Embryo Transfer (NSET) |
|---|---|---|
| Method Description | Surgical incision; exteriorization of reproductive tract; embryo deposition [22] | Trans-cervical insertion of catheter; embryo deposition into uterine horn [22] |
| Anesthesia & Analgesia | Required [22] | Not required [22] |
| Physiological Stress (Cardiac Rhythm & Fecal Corticosterone) | Higher fluctuation and levels [22] | Lower fluctuation and levels [22] |
| Technical Expertise | Significant training required [22] | Less training required [22] |
| Post-operative Pain | Yes, requires post-operative analgesia [22] | No obvious discomfort reported [22] |
| Pup Production Efficacy | Effective for producing healthy pups [22] | Comparable to surgery in producing a similar number of healthy pups [22] |
Table 2: "The Scientist's Toolkit" - Essential Materials for Embryo Transfer
| Research Reagent / Material | Function in Protocol |
|---|---|
| NSET Device (catheter and specula) | Core device for trans-cervical embryo deposition in the NSET method [22]. |
| Isoflurane Inhalation Anesthesia | General anesthesia for surgical embryo transfer procedures [22]. |
| Meloxicam (or other NSAID) | Pre- and post-operative analgesic and anti-inflammatory for surgical protocols [22]. |
| Pseudopregnant Recipient Mice | Females at 2.5 days post-coitum (dpc) used as recipients for transferred embryos [22]. |
| Vasectomized Male Mice | Used to generate pseudopregnant female recipients [22]. |
| Embryo Culture Media | For handling and short-term maintenance of embryos during the transfer process. |
Experimental Protocols and Workflows
Detailed Protocol: NSET Procedure
Methodology:
- Recipient Preparation: Place a pseudopregnant mouse at 2.5 dpc on a wire-top cage lid, allowing it to grip the bars securely [22].
- Cervical Exposure: Sequentially place the small and large specula into the vagina to open and expose the cervix [22].
- Embryo Transfer: Load the NSET catheter with embryos. Carefully insert the catheter through the large speculum, past the cervical opening, and into the uterine horn [22].
- Deposition and Recovery: Gently expel the embryos. Withdraw the catheter and specula, and return the mouse to its home cage [22]. No recovery from anesthesia is needed.
Detailed Protocol: Surgical Embryo Transfer
Methodology:
- Anesthesia and Pre-operative Care: Anesthetize the pseudopregnant mouse (e.g., with 2.5% isoflurane). Administer a pre-operative analgesic such as meloxicam (5 mg/kg IP) [22].
- Surgical Site Preparation: Shave and disinfect the dorsal incision site [22].
- Surgical Access: Make an incision through the skin and muscle along the dorsal midline. Gently exteriorize the ovarian fat pad, ovary, oviduct, and upper uterine horn [22].
- Embryo Transfer: Create a small hole in the uterine horn using a 26-gauge needle. Deposit the embryos into the horn [22].
- Closure and Recovery: Reposition the reproductive organs into the body cavity. Close the incision with wound clips or sutures. Allow the mouse to recover in a clean cage on a warming pad until normal behavior resumes [22].
Experimental Workflow Diagram
Experimental Workflow and Stress Impact
Signaling Pathway: Stress Impact on Birth Rates
Stress Pathway Affecting Birth Rates
For researchers troubleshooting low live birth rates in mouse embryo transfer studies, the in vitro culture environment is a critical focal point. The period between fertilization and transfer is highly sensitive, and suboptimal laboratory conditions can significantly impair embryonic development and subsequent pregnancy outcomes. This guide synthesizes current evidence to help you diagnose and resolve issues related to three fundamental aspects of embryo handling: culture media composition, oxygen tension, and transfer techniques. The recommendations are framed within the context of improving the consistency and success of your preclinical mouse models.
â—£ Experimental Workflow for Culture Optimization
The following diagram outlines a systematic experimental approach to troubleshooting low birth rates by investigating and optimizing culture conditions.
Key Research Reagent Solutions
The table below details essential reagents and materials used in embryo culture and transfer experiments, along with their critical functions in supporting embryonic development.
| Reagent/Material | Primary Function in Experiment |
|---|---|
| Sequential Culture Media | Mimics changing metabolic needs from oviduct to uterine stages; supports embryonic genome activation [5]. |
| Single-Step Culture Media | Reduces embryo stress by eliminating medium changes; maintains consistent environment [5]. |
| Amino Acid Supplements | Serves as energy sources, antioxidants, and osmolytes; crucial for blastocyst formation [5]. |
| Macromolecules (e.g., BSA) | Provides a protein source and reduces shear stress; replaces patient serum in modern media [5]. |
| Hyaluronan-Enriched Transfer Media | May improve embryo viability and implantation potential during the transfer procedure [24]. |
| Fertilin Peptide | In mouse models, accelerates blastocyst formation and increases live birth rate [24]. |
Frequently Asked Questions (FAQs)
How significant is the impact of oxygen tension on embryo development?
Oxygen tension is one of the most critical factors. Culturing embryos at non-physiological, atmospheric oxygen levels (20%) is strongly associated with reduced developmental potential.
- Evidence from Bovine Model: A 2025 study using bovine embryos (a relevant model for human development) found a stark contrast in blastocyst formation rates: 36% under physiological hypoxia (6% Oâ‚‚) versus only 13% in normoxia (20% Oâ‚‚) [25].
- Metabolic Consequences: Transcriptomic analysis revealed that normoxic conditions fail to upregulate genes involved in glycolysis, forcing embryos to rely solely on oxidative phosphorylation. This alters the energy metabolism from what is typical for in vivo embryos [25].
- Recommendation: For optimal results, use physiological Oâ‚‚ tension (5-6%) throughout the culture period.
What is the difference between sequential and single-step culture media, and which is better?
The choice involves a trade-off between mimicking nature and minimizing procedural stress.
- Sequential Media: Designed to mirror the dynamic environment of the female reproductive tract, with different media used before and after embryonic genome activation to match changing metabolic needs (e.g., a shift from pyruvate/lactate to glucose) [5].
- Single-Step Media: A "simplex optimization" approach where embryos are cultured in one medium from fertilization to blastocyst. The key advantage is the reduction of stress from physical handling and environmental changes during media replacement [5].
- Recommendation: While the "best" medium may be lab-specific, the single-step system is a valid and often preferable approach due to its simplicity and reduced embryo stress.
Does the method of conception (IVF vs. natural mating) affect embryo viability?
Yes, the method of conception is a significant variable that must be controlled for and reported.
- Mouse Model Data: A 2020 study directly compared the two methods and found that embryos generated by natural mating (FB) had a predicted live birth rate of 44.7%, which was 4.7 times higher than the 14.7% rate for IVF-generated embryos [26].
- Implication: This demonstrates a profound "method of conception" effect. Researchers should standardize their embryo source and not assume IVF-derived embryos are equivalent to in vivo-derived ones when measuring live birth outcomes.
Can a technically difficult embryo transfer reduce pregnancy success?
In experienced hands, the subjective "ease" of a single embryo transfer may not be a primary determinant of success.
- Clinical Study Insight: A 2025 prospective study of 365 transfers performed by a single experienced physician found no correlation between pregnancy rates and the physician's real-time ratings of transfer ease, visibility, or the presence of blood or mucus [27].
- Key Confounder: The strongest predictor of a positive outcome was the transfer of a euploid embryo (as determined by PGT-a) [27].
- Recommendation: While a smooth, atraumatic transfer is always the goal, these findings suggest that for a skilled operator, embryo intrinsic factors are more critical. Focus efforts on ensuring embryo quality and genetic normality in your model.
Troubleshooting Low Live Birth Rates
The table below outlines common problems, their potential causes, and evidence-based solutions to improve live birth rates in your mouse experiments.
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low Blastocyst Formation | Non-physiological oxygen tension (20% Oâ‚‚) altering metabolism [25]. | Culture embryos at 5-6% Oâ‚‚ to support proper glycolytic pathway activity and blastulation [25]. |
| Poor Embryo Quality | Suboptimal or static culture media failing to meet metabolic demands [5]. | Use either sequential media to match metabolic shifts or a validated single-step medium to reduce handling stress [5]. |
| High Resorption/Low Birth Rate | Method of conception effect or suboptimal culture conditions [26]. | Use naturally conceived embryos if possible. For IVF, optimize all steps. Consider adding Fertilin peptide (in mice) to reduce resorption [24]. |
| Variable Outcomes Between Operators | Inconsistent embryo transfer technique or volume [27]. | Standardize the transfer protocol across all researchers, including catheter type, volume, and placement technique. |
â—£ Decision Pathway for Birth Rate Failure
When faced with low live birth rates, follow this logical pathway to diagnose and address the most likely causes in your experimental setup.
Advanced Techniques: Spent Culture Media Analysis
For labs seeking to minimize embryo manipulation, analysis of the spent embryo culture medium (SECM) offers a non-invasive method to assess embryo viability.
- Principle: The embryo secretes molecules (the "secretome"), including microRNAs (miRNAs) and metabolites, into its culture environment. The profile of these molecules can reflect the embryo's health and implantation potential [28].
- Methodology:
- miRNA Analysis: Isolate miRNAs from SECM and use qRT-PCR to validate the expression of specific targets (e.g., hsa-miR-16-5p and hsa-miR-92a-3p, which show differential expression between implantation-successful and failed groups) [28].
- Metabolomic Profiling: Use 3D fluorescence analysis or other spectroscopic techniques to identify metabolic fingerprints associated with viable embryos [28].
- Benefit: This is a zero-impact assessment on the embryo itself, making it ideal for sensitive experiments where embryo viability must be preserved.
In mouse embryo transfer research, the choice of recipient, her physiological status, and overall health are pivotal for achieving high birth rates. This guide addresses common challenges in recipient management, providing evidence-based troubleshooting strategies to optimize the success of your experiments. The following sections are structured to help you systematically identify and resolve issues related to strain selection, pseudopregnancy induction, and animal health.
Frequently Asked Questions (FAQs)
1. Why is the strain of the foster mother so important for pup survival?
The genetic background of the foster mother significantly influences her maternal instincts, milk quality, and overall nursing capability. Some strains are inherently better mothers, directly impacting the weaning success of transferred embryos.
- Solution: Select a foster strain with proven high maternal care and reproductive fitness. Data from recent studies indicate clear performance differences.
- Evidence: A 2025 study systematically evaluating germ-free foster mothers found that BALB/c and NSG strains exhibited superior nursing and weaning success. In contrast, C57BL/6J foster mothers had the lowest weaning rate, a finding that contrasts with their performance under specific pathogen-free (SPF) conditions [29].
2. How can I reliably schedule the preparation of pseudopregnant recipients?
The conventional method of visually selecting females at the proestrus stage for mating with vasectomized males is inefficient and operator-dependent. Inconsistent timing leads to low mating rates and unsuccessful pseudopregnancy.
- Solution: Implement an estrous cycle synchronization protocol using progesterone (P4) pretreatment. This method bypasses the need for visual estrus staging and allows for the scheduled preparation of recipients [30].
- Protocol: Subcutaneously inject females with 2 mg of progesterone once daily for two days. This synchronizes most females (around 85%) to the metestrus stage. Three days after the first injection, pair the treated females with vasectomized males for several days. This method has achieved a 63% vaginal plug rate and produced pseudopregnant recipients that supported a 52% embryo development rate into offspring, comparable to conventional methods [30].
3. My recipient mice are healthy, but birth rates are low. Could the issue be related to the embryo donor?
Yes, the method used to produce the donor embryos can be a factor. While the recipient's health is crucial, the controlled production of donor embryos ensures healthy, time-matched pups for transfer.
- Solution: For highly efficient and scheduled production of donor mothers, use in vitro fertilization (IVF). This allows for precise control over the delivery date of donor pups, which enhances experimental reproducibility and simplifies the coordination with recipient pseudopregnancy [29].
- Application: Using IVF-derived embryos and coordinating the transfer with synchronized recipients creates a more streamlined and predictable workflow for embryo transfer experiments.
4. Does the surgical technique for deriving pups impact their survival before transfer?
Yes, the cesarean section technique used to obtain pups from donor mothers can significantly impact fetal survival rates.
- Solution: Optimize the surgical approach to preserve the female reproductive tract (FRT-CS). This technique, which involves selective clamping at the cervix base, has been shown to significantly improve fetal survival rates while maintaining sterility, compared to traditional C-section methods [29].
Troubleshooting Low Birth Rates
Use the following flowchart to diagnose and address the most common causes of low birth rates in embryo transfer experiments.
Data Tables for Experimental Planning
Table 1: Strain Performance as Germ-Free Foster Mothers
Data from a 2025 study evaluating the maternal care capabilities of different strains used as germ-free foster mothers. Success is measured by the weaning rate of pups [29].
| Strain | Type | Key Maternal Characteristics | Weaning Success |
|---|---|---|---|
| BALB/c | Inbred | Superior nursing care, milk contributes significantly to pup weight gain | High |
| NSG | Inbred | Superior nursing and weaning success | High |
| KM | Outbred | Moderate maternal capabilities | Moderate |
| C57BL/6J | Inbred | Lowest weaning rate in germ-free conditions; contrast with SPF findings | Low |
Table 2: Estrous Synchronization Protocol for Pseudopregnancy
Step-by-step methodology based on a proven protocol for synchronizing recipient mice using progesterone [30].
| Protocol Step | Details | Purpose & Notes |
|---|---|---|
| Day 1 & 2 | Subcutaneous injection of 2 mg Progesterone (P4) | Synchronizes the estrous cycle to metestrus. |
| Day 3 | - | Majority of females (∼85%) are in metestrus. |
| Days 4-8 | House with vasectomized male(s). | 4-day mating window. |
| Day 7 (Example) | Check for vaginal plug. | Indicates successful mating and induction of pseudopregnancy. |
The Scientist's Toolkit: Essential Reagents and Materials
Key materials and reagents required for implementing the recipient management and synchronization protocols discussed above.
| Item | Function in Experiment | Example Source / Specification |
|---|---|---|
| Progesterone (P4) | For estrous cycle synchronization in recipient females [30]. | Progehormon (Mochida Pharmaceutical) |
| Vasectomized Males | Sterile mating to induce pseudopregnancy in recipients [30]. | ICR, CD-1, or other robust strains |
| Acidified Water | Maintains a sterile environment for germ-free or SPF mice [31]. | Ultrapure water adjusted to pH 2.5–3.0 with HCl |
| Guard-type IVC | Provides a controlled, sterile housing environment [31]. | Individually Ventilated Cage (IVC) systems |
| Tribromoethanol | Anesthesia for surgical embryo transfer procedures [30]. | - |
| 4'-Hydroxyflavanone | 4'-Hydroxyflavanone|High Purity Reference Standard | |
| 6-Hydroxyflavone | 6-Hydroxyflavone - CAS 6665-83-4 - For Research Use Only |
Strategic Solutions for Common and Complex ET Challenges
Frequently Asked Questions (FAQs)
Q1: How does the choice of catheter impact embryo transfer success in mouse models? The choice of catheter is critical for an atraumatic transfer. Using a "soft" catheter is associated with optimal pregnancy and implantation rates, as it minimizes trauma to the endometrium. The procedure should avoid blood, mucus, and bacterial contamination to ensure success [32].
Q2: Can uterine contractions be measured in mice, and how is it done? Yes, uterine contractility can be quantitatively measured in vivo in mice. A method involves the transcervical insertion of a small intrauterine pressure catheter (IUPC), such as a Millar 1.4F or 3.5F catheter [33]. This technique allows for the sensitive assessment of contraction frequency, duration, amplitude, and area under the curve (AUC) without the need for operative approaches, similar to clinical methods used in high-risk human pregnancies [33].
Q3: What is the relationship between uterine contractions and embryo expulsion? Excessive uterine contractions are a key factor associated with reduced implantation rates and potential embryo expulsion after transcervical transfer [32]. Inadequate uterine contractility is also linked to issues like infertility and miscarriages, while hyper-contractility can disrupt implantation [33].
Q4: What procedural aspects are crucial for a successful embryo transfer? Several technical factors are vital [32]:
- Preparation: Performing a trial transfer and using ultrasonographic guidance for the actual procedure.
- Technique: Employing a "soft" catheter to minimize endometrial trauma.
- Asepsis: Ensuring the avoidance of blood, mucus, and bacterial contamination during the transfer process.
Troubleshooting Guides
Problem: Low Implantation Rate
| Potential Cause | Investigation Method | Corrective Action |
|---|---|---|
| Excessive uterine contractions | Measure in vivo IUP with a transcervical catheter on relevant gestation days (e.g., D16-D19) [33]. | Optimize transfer technique to be more atraumatic; review catheter type and hormone protocol. |
| Suboptimal catheter type | Perform a trial transfer with different "soft" catheters [32]. | Switch to a softer, more flexible catheter to reduce endometrial trauma and contractions [32]. |
| Physical handling of embryos | Review lab protocols for embryo culture and handling. | Minimize physical and chemical stress on embryos; ensure optimal culture conditions (pH, temperature, osmolality) [5]. |
Problem: Inconsistent Pregnancy Outcomes Across Experimental Batches
| Potential Cause | Investigation Method | Corrective Action |
|---|---|---|
| Unmonitored uterine contractility | Implement periodic IUP monitoring in a subset of animals to establish a baseline [33]. | Standardize the timing of embryo transfer relative to the estrous cycle and monitor uterine activity to perform transfers during periods of low contractility. |
| Variable transfer technique | Use ultrasound guidance during transfer to standardize embryo placement [32]. | Implement a standardized transfer protocol with a single, experienced operator if possible, and always use a trial transfer. |
| Embryo quality issues | Review embryo culture media and conditions [5]. | Standardize culture media and protocols. Consider using sequential or simplex optimization media to support development and reduce stress [5]. |
Experimental Protocols & Quantitative Data
Protocol: Measuring Intrauterine Pressure (IUP) in Mice
Objective: To quantitatively assess in vivo uterine contractile activity in pregnant mice.
Materials:
- Pregnant mice (e.g., CD-1 strain)
- Intrauterine pressure catheter (IUPC), Millar 1.4F or 3.5F [33]
- Anesthetic (e.g., 1-2% isoflurane [33])
- Heating pad
- Speculum tube
- Pressure recording hardware and software (e.g., PowerLab with LabChart Pro [33])
Methodology:
- Anesthetize: Place the mouse under general anesthesia using an approved anesthetic agent like isoflurane [33].
- Position and Visualize: Position the mouse on a heating pad. Gently insert a speculum tube into the vaginal canal to visualize the cervix [33].
- Insert Catheter: Carefully insert the sterilized pressure catheter transcervically to a depth of 3-6 cm, ensuring the tip passes the uterocervical junction [33].
- Record Data: Once rhythmic contractions with consistent amplitude and frequency are observed, record the baseline intrauterine contractile pressure for a set period (e.g., 10 minutes) [33].
- Analyze Data: Using analysis software, calculate key parameters over the recording period [33]:
- Amplitude (mmHg): The mean strength of contractions.
- Frequency: The number of contractions per time unit.
- Area Under the Curve (AUC): The integrated contractile activity.
- Montevideo Units (MVUs): The sum of amplitudes in a 10-minute period.
Quantitative Data on Murine Uterine Contractions
The table below summarizes normative IUP data from late-stage pregnant CD-1 mice, which can serve as a benchmark for troubleshooting.
| Gestational Day | Contractile Activity (AUC, mmHg*s) | Key Labor Phase | Significance |
|---|---|---|---|
| Day 16 - 18 | Lowest [33] | Inactive Labor | Baseline, low contractility. |
| Day 19 (Morning) | Significantly increased (p<0.05) [33] | Pre-labor | Onset of labor progression. |
| Day 19 (Afternoon) & Intrapartum | Maximal levels [33] | Active Labor | AUC threshold of >2.77 mmHg discriminates active from inactive labor [33]. |
Signaling Pathways & Experimental Workflows
Diagram: IUP Measurement Workflow
Diagram: Causes of Low Birth Rates
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Description | Example Use Case |
|---|---|---|
| Soft Catheter | An atraumatic catheter designed to minimize endometrial damage and reduce uterine contractions during the transfer procedure [32]. | Essential for all mouse embryo transfers to maximize implantation rates. |
| Intrauterine Pressure Catheter (IUPC) | A small, sterile catheter (e.g., Millar 1.4F) used to measure real-time intrauterine pressure and contractile activity in vivo [33]. | Quantifying uterine contractions on different gestational days for research on low implantation rates. |
| Sequential Culture Media | A culture system that changes media composition to align with the embryo's metabolic shift during development (e.g., from pyruvate/lactate to glucose) [5]. | Supporting embryo development to the blastocyst stage for higher-quality transfers. |
| Simplex Optimization Medium | A single medium that supports embryo development from fertilization to blastocyst, reducing stress from media changes [5]. | Culturing embryos under consistent conditions to optimize viability and development. |
| Isoflurane Anesthesia | An inhaled anesthetic agent suitable for maintaining stable anesthesia during surgical and non-surgical procedures like IUP measurement [33]. | Providing safe and controlled anesthesia for in vivo uterine pressure monitoring. |
| 6-Hydroxygenistein | 6-Hydroxygenistein (6-OHG) - CAS: 107534-93-2 | 6-Hydroxygenistein is a potent bioactive isoflavone for neuroscience and cytoprotection research. This product is for Research Use Only (RUO). Not for human or veterinary diagnostic or therapeutic use. |
Refining Protocols for Genetically Sensitive Strains (e.g., C57BL/6)
Frequently Asked Questions (FAQs)
Q1: Why are birth rates particularly low when working with C57BL/6 embryos?
Several factors specific to C57BL/6 substrains can contribute to low birth rates in embryo transfer experiments:
- Genetic Substrain Divergence: The C57BL/6 strain is not a single entity. Significant genetic and phenotypic differences have accumulated between substrains such as C57BL/6J (B6/J) and C57BL/6N (B6/N). These substrains were separated in 1951 and now differ by dozens of single nucleotide polymorphisms (SNPs) and structural variants [34]. Using a background strain for recipient mice that is genetically different from the embryonic stem (ES) cell-derived strain (e.g., placing a KOMP mutation generated in B6/N-derived ES cells onto a B6/J background) can create a mixed genetic background that negatively impacts pregnancy outcomes [34].
- Inherent Strain Sensitivity: Embryos from inbred strains like C57BL/6 are known to be more sensitive to culture conditions and environmental stressors compared to hardier hybrid or outbred strains [35] [36]. This inherent sensitivity can make them less tolerant of suboptimal in vitro handling or subtle contaminants.
- Technical Expulsion of Embryos: The small reproductive tract of mice, combined with positive pressure in the oviduct, can lead to the discharge of freshly transferred embryos. This risk is exacerbated if the transfer volume is too large [1].
Q2: My transgenic line is on a C57BL/6 background. How do I choose the right recipient strain to maximize birth rates?
The most critical rule is to avoid genetic mismatch. The recipient strain should be the same C57BL/6 substrain as the embryos being transferred [34].
- Action Item: Meticulously document the substrain source of both your ES cells and your recipient mice. Treat different substrains (e.g., B6/J, B6/N, B6/NTac) as genetically distinct, not interchangeable [34].
- Example Problem: If your mutation was generated in a B6/N-derived ES cell line (common for KOMP projects), but you use B6/J mice as recipients and for backcrossing, the resulting phenotypic effects could be caused by genetic variants linked to the mutation rather than the mutation itself [34].
Q3: What is the most critical technical aspect of the embryo transfer procedure to prevent embryo expulsion?
Minimizing the volume of medium transferred into the oviduct is paramount. A novel technique demonstrated that reducing the transfer volume from the conventional 10-15 µL to ≤ 1 µL significantly improved birth rates by preventing embryos from being expelled from the oviduct due to positive pressure [1]. This method uses a modified micropipette and a manual piston micro-pump for precise control.
Q4: Are there more sensitive assays to test my culture media for toxicity when working with sensitive strains?
Yes. The standard Mouse Embryo Assay (MEA) using robust hybrid embryos may not detect subtle contaminants. To improve sensitivity:
- Use Sensitive Strains: Employ embryos from outbred strains (e.g., CF1, SW) or inbred strains, which are genetically diverse and more sensitive to toxins than hybrid embryos [35] [36].
- Assess Blastocyst Quality: Move beyond simple blastocyst formation rates. Evaluate blastocyst cell number and allocation to the inner cell mass (ICM) and trophectoderm (TE), as these parameters are more sensitive indicators of stress [35].
- Use One-Cell Embryos: Initiate culture from the one-cell stage, as these embryos are more sensitive to the culture environment than two-cell embryos [35].
Troubleshooting Guide: Low Birth Rates after Embryo Transfer
Problem: Low Birth Rates with Genetically Sensitive Strains
This guide addresses the common issue of poor pup yield following embryo transfer in demanding strains like C57BL/6.
Background and Strategic Planning
Key Concepts:
- Genetic Stability: While inbred strains are theoretically genetically identical, residual heterozygosity and spontaneous mutations lead to the formation of distinct substrains over time [34].
- Strain Selection: The choice of mouse strain significantly impacts embryo transfer outcomes. Some strains, like DBA/2J, have poor reproductive performance, while F1 hybrids and outbred strains like NMRI often show superior results [1].
Actionable Protocol:
- Subrain Verification: Before beginning, confirm the exact substrain of your donor embryos and recipient mice. Consult supplier documentation (e.g., [37]) and sequence critical regions if necessary [34].
- Recipient Choice: Select a robust pseudopregnant recipient strain with proven reproductive performance, such as outbred NMRI or ICR mice [1].
Optimized Embryo Transfer Protocol
The following refined surgical transfer protocol is designed to maximize embryo survival, based on a novel technique that significantly improved live birth rates compared to conventional methods [1].
Workflow Diagram: Optimized Oviductal Embryo Transfer
Detailed Methodology:
Materials Preparation:
- Modified Transfer Micropipette: Prepare borosilicate glass micropipettes (1 mm outer diameter) using a pipette puller and grinder to create a tip with a flat, diagonal opening at a 45° angle and a sharp point of 70-80 µm [1].
- Manual Piston Pump: Use a device like a Cell Tram oil for fine control during embryo loading and transfer [1].
- Anesthesia: Anesthetize the pseudopregnant recipient mouse with an intraperitoneal injection of ketamine (62.5 mg/kg) and xylazine (6.25 mg/kg) [1].
Procedure:
- Make a 1 cm dorsal skin incision to expose the oviduct.
- Load Embryos: Under a stereomicroscope, load the embryos into the modified pipette using the manual pump. Arrange them with minimal medium (≤ 1 µL total volume) and air bubbles for visualization [1].
- Insert Pipette: Using watchmaker's forceps, gently stabilize the oviduct. Insert the sharp tip of the modified pipette directly through the wall of the second coiled corner of the oviduct (counting from the ampullae). Note: This eliminates the need to pre-puncture the oviduct with a needle [1].
- Transfer Embryos: The first operator turns the adjusting screw on the pump to gently expel the embryos into the oviduct. The minimal volume (≤ 1 µL) is critical to prevent backflow and expulsion [1].
- Check for no leakage, return the oviduct to the abdominal cavity, and surgically close the incision.
Quantitative Data on Protocol Efficacy
The table below summarizes the superior performance of the optimized low-volume transfer technique compared to the conventional method.
Table 1: Comparison of Embryo Transfer Technique Outcomes
| Technique | Transfer Volume | Average Live Birth Rate | Key Advantage |
|---|---|---|---|
| Conventional [1] | 10-15 µL | 21.7% | Standard, widely-used method. |
| Optimized Low-Volume [1] | ≤ 1 µL | 42.4% | Prevents embryo expulsion, less trauma, higher success. |
Quality Control for Media and Reagents
Sensitive strains require more rigorous quality control. The table below compares mouse strains used in the Mouse Embryo Assay (MEA) for detecting toxicity.
Table 2: Mouse Strain Sensitivity in Quality Control Assays
| Mouse Strain Type | Example Strains | Sensitivity to Toxins | Recommended Use |
|---|---|---|---|
| F1 Hybrid | BDF1 (B6/CBA) | Lower | Standard, less sensitive MEA. |
| Inbred | C57BL/6, FVB | Intermediate | Modeling specific genetic backgrounds. |
| Outbred | CF1, Swiss Webster (SW) | Higher | More sensitive MEA for detecting subtle contaminants [35] [36]. |
Actionable Protocol:
- Perform QC testing of all culture media and reagents (e.g., mineral oil, water) using a sensitive MEA with outbred CF1 or SW one-cell embryos [36].
- Assess endpoints beyond blastocyst formation, including total cell count and ICM/TE cell allocation, as these are more sensitive indicators of stress [35].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Refined Embryo Transfer Protocols
| Item | Function/Description | Considerations for Sensitive Strains |
|---|---|---|
| Manual Piston Micro-pump (e.g., Cell Tram oil) | Provides fine, precise control for loading and transferring embryos with minimal fluid volume [1]. | Critical for achieving the sub-1µL transfer volume that prevents embryo expulsion. |
| Borosilicate Glass Capillaries | Used to create custom, sharp transfer pipettes with a controlled tip diameter (~70-80 µm) [1]. | A sharp, finely-ground tip allows for direct insertion into the oviduct without a needle puncture, reducing trauma. |
| Sensitive Strain Embryos (e.g., CF1, SW) | Genetically diverse outbred embryos used for quality control Mouse Embryo Assays (MEAs) [35] [36]. | More effectively detects low-level contaminants in culture media that might not affect hardier hybrid embryos. |
| Preimplantation Genetic Testing (PGT-A) | A technique to screen embryos for chromosomal abnormalities (aneuploidy) before transfer [38]. | Embryo aneuploidy is a major cause of implantation failure. Transferring genetically normal (euploid) embryos significantly increases the odds of successful implantation and live birth [38]. |
| Defined Culture Media | Sequential media systems designed to support embryo development from zygote to blastocyst stage. | For C57BL/6 and other sensitive strains, use media with proven performance in sensitive MEAs. Avoid batch-to-batch variability. |
Leveraging Sequential vs. Single-Step Culture Media for Improved Blastocyst Formation
Within the critical field of mouse embryo transfer research, a frequently encountered challenge is the phenomenon of low birth rates. A pivotal, and often variable, factor influencing this outcome is the selection and application of embryo culture media. The in vitro environment must faithfully support embryonic development from fertilization to the blastocyst stage, and the choice between sequential media and single-step media represents a fundamental technical decision. This technical support center is designed to help researchers troubleshoot low birth rates by providing detailed guidance on optimizing these culture systems. A thorough understanding of the advantages, limitations, and correct protocols for each media type is essential for generating viable blastocysts capable of achieving successful implantation and culminating in live births.
Embryo culture media is a complex aqueous solution formulated to mimic the natural environment of the female reproductive tract. It provides essential nutrients, energy sources, and maintains optimal pH and osmolality to sustain embryo viability from the zygote stage to a fully formed blastocyst [39]. The two dominant approaches in modern laboratories are sequential and single-step culture media.
Sequential Culture Media utilize different formulations tailored to the changing metabolic needs of the developing embryo. Typically, one medium supports early cleavage stages (Day 1 to Day 3), after which embryos are transferred to a second, distinct medium optimized for blastocyst formation (Day 3 to Day 5/6) [39]. This strategy aims to closely replicate the dynamic in vivo conditions of the oviduct and uterus [5].
Single-Step Culture Media, also known as continuous media, are designed to support the entire development from zygote to blastocyst in a single, unchanging medium. These formulations contain a balanced cocktail of all necessary nutrients and energy sources, allowing for uninterrupted culture [39].
The following workflow outlines the key decision points and experimental steps for utilizing these media systems in mouse embryo transfer research:
Table 1: Core Characteristics of Sequential and Single-Step Media
| Feature | Sequential Media | Single-Step Media |
|---|---|---|
| Philosophy | Stage-specific support mimicking the in vivo tract [39] | Unified support allowing embryo self-regulation [5] |
| Handling | Requires a medium change on day 3 [39] | Uninterrupted culture; minimal handling [39] |
| Key Advantage | Replenishes nutrients, removes waste at a critical juncture [39] | Minimizes handling stress and environmental fluctuations [39] |
| Primary Challenge | Increased labor and risk of handling stress [39] | Potential accumulation of metabolic by-products [39] |
| Compatibility | Traditional incubators | Ideal for time-lapse systems [39] |
Troubleshooting Low Birth Rates: FAQs and Guides
Low birth rates following embryo transfer can stem from multiple factors related to the in vitro culture environment. The following FAQs address common challenges and provide evidence-based troubleshooting strategies.
FAQ 1: Our blastocyst formation rates are good, but subsequent live birth rates are low. Could the culture media be a factor?
Yes, this is a recognized phenomenon. While blastocyst formation is a key indicator, it does not guarantee full developmental competence. The culture conditions can induce subtle cellular stresses that compromise the embryo's ability to implant and develop to term.
- Potential Cause: Altered gene expression and metabolic function. Suboptimal culture conditions can affect epigenetic reprogramming and the expression of genes critical for implantation and fetal development [5] [40]. For instance, single-step media has been associated with increased odds of large-for-gestational-age (LGA) offspring in some human studies, suggesting a long-term impact on fetal growth regulation [41].
- Troubleshooting Steps:
- Review Media Refreshment Protocol: If using single-step media, consider the timing of medium refreshment. A sibling oocyte study found that refreshing medium on Day 3 versus Day 5 did not significantly affect euploidy rates but may slightly enhance the yield of high-quality blastocysts [42]. Evaluate if a Day 3 refreshment could benefit your specific setup.
- Analyze Blastocyst Quality: Move beyond simple morphology. Where possible, analyze gene expression markers related to implantation competence. Research in mouse models has shown that blastocysts hatched from different sites (e.g., B-site vs. C-site) have distinct transcriptional profiles and significantly different birth rates (65.6% vs. 21.3%) [40]. This suggests that hatching success and molecular quality are critical.
- Validate with a Different Media System: Perform a controlled trial using a sibling oocyte split between sequential and single-step media. Compare outcomes not just at the blastocyst stage, but through to implantation and live birth rates to identify the optimal system for your laboratory conditions [39].
FAQ 2: We observe high rates of blastomere fragmentation and developmental arrest. How can media handling improve this?
Excessive fragmentation and arrest often point to stress during the culture process.
- Potential Cause: Suboptimal pH, osmolality, and temperature fluctuations. These physical parameters are crucial for normal cell division. Sequential media systems are particularly susceptible during the required medium change on Day 3, as additional handling increases exposure to room air and temperature variations [39] [5].
- Troubleshooting Steps:
- Optimize Handling Speed and Environment: Ensure all medium changes and embryo manipulations are performed rapidly within a warmed chamber or on a heated stage to maintain a constant 37°C.
- Switch to Single-Step Media: To eliminate the stress of a medium change, consider adopting a validated single-step medium. This provides a stable environment and minimizes handling-related risks, which is particularly beneficial for labs without a highly optimized workflow [39].
- Check Incubator and Gas Calibration: Regularly verify that COâ‚‚ and, if used, Oâ‚‚ concentrations are accurately maintained. Even brief exposures to atmospheric oxygen levels (20%) can be detrimental to sensitive embryos compared to more physiological levels (5%) [5].
FAQ 3: Is there a way to non-invasively assess embryo viability in culture to predict birth outcomes?
This is an area of active research, and metabolic profiling shows great promise.
- Solution: Spent Embryo Culture Media (SECM) Analysis. The metabolic activity of embryos leaves a fingerprint in the culture medium. Analyzing the turnover of nutrients like glucose, pyruvate, and amino acids, or performing broader metabolomic profiling of the SECM, can serve as a non-invasive biomarker for embryo viability [43].
- Implementation Protocol:
- Sample Collection: Carefully collect the microdroplet of culture medium from around an individual blastocyst after its selection for transfer or vitrification.
- Storage and Analysis: Flash-free the sample at -80°C. Subsequently, analyze it using targeted platforms (e.g., for glucose/amino acid uptake) or untargeted metabolomic platforms (e.g., mass spectrometry) to identify metabolic signatures associated with high implantation potential [43].
- Data Integration: While not yet a routine clinical tool, research labs can use this data to build predictive models. For example, a mouse study developed a model using expression of genes like Lyz2, Cd36, Cfb, and Cyp17a1 to predict implantation success, which could be correlated with metabolic findings [40].
Essential Experimental Protocols
Protocol: Sibling Oocyte Trial for Media Comparison
Objective: To impartially compare the efficacy of sequential versus single-step media systems on blastocyst development and quality within a single experiment, controlling for patient/oocyte genetic variability.
Materials:
- MII oocytes from superovulated female mice.
- Pre-equilibrated droplets of sequential media (e.g., G1/G2 or equivalent) and single-step media (e.g., Global or KSOM).
- Benchtop dry incubator or traditional CO₂ incubator, set at 37°C, 5-6% CO₂, and 5% O₂.
Method:
- Randomization: After fertilization (IVF or ICSI), randomly divide all zygotes from a single cohort into two groups.
- Culture:
- Sequential Group: Culture in cleavage-stage medium (e.g., G1) until Day 3, then perform a medium change to blastocyst-stage medium (e.g., G2).
- Single-Step Group: Culture continuously in a single-step medium (e.g., Global) from Day 1 to Day 5/6 without any medium change or with a refreshment on Day 5 [42].
- Assessment: On Day 5 and Day 6, assess blastocyst formation rates, morphology (e.g., Gardner score), and expansion grade for both groups.
- Downstream Analysis: Transfer blastocysts from each group to pseudopregnant females to compare implantation and live birth rates. Alternatively, for molecular analysis, a subset of blastocysts can be fixed for immunostaining or collected for transcriptomic analysis [40].
Protocol: Targeted Hatching Site Manipulation
Rationale: Research shows that the site of blastocyst hatching from the zona pellucida (ZP) is not random and is correlated with implantation potential. Blastocysts hatching near the inner cell mass (ICM; B-site) showed significantly higher birth rates (65.6%) than those hatching opposite the ICM (C-site; 21.3%) [40].
Objective: To improve implantation rates by artificially inducing hatching at the preferred B-site.
Materials:
- Expanded mouse blastocysts.
- Laser system for assisted hatching or a fine acidic Tyrode's solution pipette.
- Time-lapse imaging system (optional but recommended).
Method:
- Orientation: Identify the ICM under a high-magnification microscope.
- Zona Drilling: Using a laser or chemical digestion, create a small, localized opening in the ZP at the 3 o'clock position relative to the ICM (defined as the B-site) [40].
- Culture and Transfer: Return the embryos to culture and allow hatching to proceed through the artificial opening. Select fully hatched blastocysts for embryo transfer.
- Validation: Compare pregnancy and birth outcomes between blastocysts with assisted hatching at the B-site versus untreated controls or those hatched from other sites.
The Scientist's Toolkit: Key Reagents and Materials
Successful embryo culture relies on a suite of carefully selected reagents and equipment. The following table details essential items for setting up and performing these experiments.
Table 2: Essential Research Reagents and Materials for Mouse Embryo Culture
| Item | Function / Description | Example Brands / Types |
|---|---|---|
| Sequential Media | Two-part system (Cleavage + Blastocyst) for stage-specific support. | G-Series (Vitrolife), Quinn's Advantage (CooperSurgical) [41] |
| Single-Step Media | Unified medium for uninterrupted culture from zygote to blastocyst. | Global (CooperSurgical), CSC+ (FujiFilm) [41] |
| Mineral Oil | Overlays culture droplets to prevent evaporation and osmolarity shifts. | Light Mineral Oil (Irvine Scientific), OVOIL (Vitrolife) [41] |
| Protein Supplement | Added to media; commonly used for embryo culture. | Human Serum Albumin (HSA) or Serum Substitute Supplement (SSS) [41] |
| Hyaluronidase | Enzyme used to remove cumulus cells from zygotes after fertilization. | Available from multiple biotechnology suppliers [44] |
| PMSG & hCG | Hormones for superovulation in female mouse donors. | Available from pharmaceutical or specialized biotech suppliers [40] |
| Benchtop Incubator | Compact, dry incubator with stable gas and temperature control; ideal for single-step culture with time-lapse. | Geri (Genea Biomedx) [39] |
| Time-Lapse System | Integrated camera system for continuous, non-invasive embryo monitoring. | Often built into advanced benchtop incubators [39] |
Data Presentation: Quantitative Comparisons
The following tables consolidate key quantitative findings from recent studies to aid in experimental planning and data interpretation.
Table 3: Impact of Media Refreshment Timing in Single-Step Culture [42]
| Outcome Measure | Refresh on Day 3 (R-D3) | Refresh on Day 5 (R-D5) | Statistical Significance |
|---|---|---|---|
| Expanded Blastocyst Rate per MII | Slightly Higher | Slightly Lower | Modest improvement (p<0.05) |
| Usable Blastocyst Yield | Comparable | Comparable | Not Significant (NS) |
| Euploidy Rates | Comparable | Comparable | NS |
Table 4: Comparative Outcomes of Single-Step vs. Sequential Media in Clinical Births [41]
| Outcome Measure | Single-Step Media | Sequential Media | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|
| Large-for-Gestational-Age (LGA) | Increased Incidence | Baseline | 2.1 (1.04 - 4.22) |
| Small-for-Gestational-Age (SGA) | Comparable | Comparable | NS |
| Placental Abnormalities | Comparable | Comparable | NS |
Table 5: Blastocyst Hatching Site and Birth Outcomes in a Mouse Model [40]
| Hatching Site | Description | Live Birth Rate |
|---|---|---|
| B-Site | 3 o'clock position, beside the ICM | 65.6% |
| A-Site | 1-2 o'clock position, near the ICM | 55.6% |
| C-Site | 4-5 o'clock position, opposite the ICM | 21.3% |
| Failure to Hatch | Blastocyst does not escape the ZP | 5.1% |
The relationship between media choice, embryo quality, and final birth outcomes involves multiple interconnected factors, as summarized below:
Evaluating Efficacy Through Data and Comparative Outcomes
FAQs: Addressing Common Experimental Challenges
Q1: What is a typical live birth rate I should expect from a mouse embryo transfer experiment, and what factors influence it most?
The live birth rate from mouse embryo transfer can vary significantly based on the technique and embryo quality. In studies comparing transfer methods, a novel oviductal transfer technique achieved an average live birth rate of 42.4%, a significant improvement over the 21.7% rate from conventional methods [1]. Key influencing factors include:
- Technical skill and equipment: Using precise micropipettes with minimal medium volume reduces embryo expulsion [1].
- Embryo quality: Genetically abnormal embryos have lower developmental potential [1].
- Strain of mouse: Some strains, like DBA/2J, have poor reproductive performance, while hybrid strains like B6D2F1 often perform better [1].
- Uterine receptivity: Affected by the recipient's hormonal status and synchronization with embryo development [1].
Q2: Can the type of endometrial preparation for frozen embryo transfer impact birth outcomes?
Yes, the choice between natural cycles (NC-FET) and artificial/hormone therapy cycles (AC-FET/HT-FET) can influence outcomes, particularly with embryo quality. A large clinical study found that while overall rates were similar, for low-quality embryos, NC-FET yielded a significantly higher live birth rate (adjusted odds ratio 2.57) compared to HT-FET [45]. For high-quality embryos, HT-FET resulted in a higher implantation rate (45% vs. 34%) [45]. This suggests the optimal protocol may depend on the quality of the embryos being transferred.
Q3: What environmental contaminants or common medications should I be concerned about in my mouse embryo transfer studies?
Recent evidence suggests that some common substances can impair early embryo development:
- Acetaminophen (Tylenol, Paracetamol): A 2025 study found that at concentrations measurable in human reproductive tissues after a standard dose, acetaminophen can slow DNA synthesis, disrupt cell division, and impair blastocyst formation in mouse and human embryo models. In mice, exposure led to reduced implantation rates and increased pregnancy loss [46].
- Endocrine Disrupting Chemicals (EDCs): Chemicals like Bisphenol A (BPA) and Triclosan (TCS) have estrogenic properties. In mice, preimplantation exposure can lead to implantation failure, with gestational day 2-3 being a particularly sensitive window [47].
Q4: Does in vitro culture of embryos affect their long-term developmental potential and offspring health?
Yes, studies in mouse models indicate that assisted reproductive technologies (ART) can have lasting effects. Mouse pups conceived via IVF showed a ~30% increase in new single-nucleotide variants (DNA mutations) compared to naturally conceived pups, though the absolute risk of harmful mutations remains low [11]. Furthermore, persistent Wnt signaling in IVF embryos can disrupt the naïve-to-primed pluripotency transition, leading to implantation failure and subsequent metabolic abnormalities in offspring. Inhibiting this pathway in mice improved implantation and ameliorated metabolic disorders [48].
Quantitative Data Tables
Table 1: Comparison of Mouse Embryo Transfer Techniques and Outcomes
| Technique | Transfer Medium Volume | Average Live Birth Rate | Key Advantages |
|---|---|---|---|
| Novel Oviductal ET [1] | ≤ 1 µl | 42.4% | Prevents embryo expulsion; time-saving; less trauma. |
| Conventional Oviductal ET [1] | 10-15 µl | 21.7% | Widely used and established protocol. |
Table 2: Impact of Endometrial Preparation and Embryo Quality on FET Outcomes
| Embryo Quality | Endometrial Preparation Protocol | Implantation Rate | Live Birth Rate (Adjusted Odds Ratio) |
|---|---|---|---|
| High-Quality [45] | Hormone Therapy (HT-FET) | 45% | Not Significant |
| High-Quality [45] | Natural Cycle (NC-FET) | 34% | Not Significant |
| Low-Quality [45] | Hormone Therapy (HT-FET) | Not Specified | Reference (1.00) |
| Low-Quality [45] | Natural Cycle (NC-FET) | Not Specified | 2.57 |
Table 3: Effects of Substance Exposure on Preimplantation Embryo Development
| Substance | Experimental Model | Observed Effect on Embryos | Impact on Pregnancy |
|---|---|---|---|
| Acetaminophen (100-200 µM) [46] | Mouse & Human Embryos | Delayed division; prevented blastocyst formation; reduced ICM cell count. | In mice: Reduced implantation; increased pregnancy loss. |
| BPA / TCS [47] | Mouse Model | Disruption during preimplantation stage. | Implantation failure, especially with exposure on gestational day 2-3. |
Experimental Protocols
This protocol describes a technique that significantly improves live birth rates compared to conventional methods.
Key Materials:
- Micropipettes: Kwik-fil borosilicate glass capillaries (1 mm outer diameter).
- Puller and Grinder: Flaming/Brown micropipette puller and grinder to create a sharp tip with 70-80 µm diameter.
- Manual Piston Pump: Cell Tram oil pump for precise embryo handling.
- Embryo Transfer Media: M2 medium for handling, KSOM medium for culture.
Detailed Methodology:
- Preparation of Transfer Pipette: Pull and grind the glass micropipette to a fine, sharp point (70-80 µm) at a 45-degree angle using a microforge.
- Embryo Collection: Superovulate donor mice (e.g., NMRI) with HMG/hCG, mate with fertile males, and collect two-cell embryos from the oviducts using M2 medium.
- Embryo Culture: Wash and culture collected embryos in KSOM medium drops under mineral oil until transfer.
- Recipient Preparation: Mate recipient females with vasectomized males and select those with a vaginal plug. Anesthetize with ketamine/xylazine and expose the oviduct through a dorsal incision.
- Novel Transfer Technique:
- Load 2-cell stage embryos into the modified transfer pipette using the manual piston pump. The total medium volume must be ≤ 1 µl.
- Directly insert the sharp pipette tip into the wall of the second coiled corner of the oviduct (counting from the ampullae), without pre-puncturing with a needle.
- Use the pump's adjusting screw to gently expel the embryos into the oviduct.
- Post-Transfer: Return the oviduct to the abdominal cavity and close the incision. Monitor recipients for pregnancy and live births.
This protocol outlines an approach for testing the effects of compounds like acetaminophen on early embryogenesis.
Key Materials:
- Test Substance: e.g., Acetaminophen, prepared at relevant concentrations (e.g., 25 µM, 100 µM, 200 µM).
- Embryo Models: Yeast, human cell lines, donated human embryos, or mouse embryos.
- Analysis Tools: Assays for DNA synthesis (e.g., ribonucleotide reductase activity), cell counting, and apoptosis detection.
Detailed Methodology:
- Dose Determination: First, measure the concentration of the substance that reaches reproductive tissues (e.g., follicular fluid, endometrium) in vivo after a standard dose to inform in vitro exposure levels.
- In Vitro Exposure:
- Expose cleavage-stage mouse or human embryos to a range of concentrations of the test substance.
- Culture embryos according to standard protocols and monitor for rates of development, blastocyst formation, and cell death.
- Functional Assessment:
- For blastocysts, perform cell counts on the Inner Cell Mass (ICM) and Trophectoderm (TE) to assess quality.
- Use biochemical assays to investigate the mechanism, such as measuring DNA synthesis rates within the ICM.
- In Vivo Validation (Mouse Model):
- Expose embryos to the substance in vitro.
- Transfer the pre-exposed embryos into synchronized recipient females.
- Track and compare implantation rates, pregnancy maintenance, and live birth rates against a control group.
Signaling Pathways and Workflows
Embryo Transfer Success Workflow
Wnt Signaling in IVF Embryo Implantation
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Embryo Transfer and Developmental Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| KSOM Medium [1] | A common culture medium for preimplantation mouse embryos. | Used for in vitro culture of two-cell mouse embryos until the time of transfer [1]. |
| M2 Medium [1] | A handling medium with buffering capacity for use outside a COâ‚‚ incubator. | Used for flushing embryos from the oviduct and during the embryo transfer procedure [1]. |
| HMG/hCG [1] | Hormones for superovulation in donor mice. | Administered to donor female mice to stimulate the production of a large number of eggs [1]. |
| Wnt Inhibitor (IWP2) [48] | A small molecule inhibitor of Wnt signaling. | Treatment of IVF embryos to correct persistent Wnt signaling, improving implantation rates and normalizing offspring metabolic health in mouse models [48]. |
| Modified Glass Micropipettes [1] | Precisely manufactured capillaries for embryo handling and transfer. | Used with a manual piston pump for the novel oviductal transfer technique, allowing minimal medium volume transfer [1]. |
| Cell Tram Oil Manual Pump [1] | A precision piston pump for micro-injection and embryo handling. | Provides fine control for loading and expelling embryos during the novel transfer technique, minimizing volume and trauma [1]. |
Frequently Asked Questions
Q1: Which mouse strain should I select as a recipient for embryo transfer to maximize birth rates? The choice of recipient strain is crucial for reproductive success. While the genetic background of the embryos themselves significantly impacts outcomes, using robust, outbred strains like CD1 as recipient dams is a standard and effective practice. These recipients are often selected for their good mothering ability and large litter size, which can help in successfully carrying pregnancies to term, regardless of the embryo's genetic background [49].
Q2: How do birth rates and litter sizes compare between B6J and B6N embryos? Quantitative data from a large-scale study reveals clear performance differences between these common substrains. The table below summarizes key reproductive metrics after embryo transfer into CD1 recipients [49].
Table 1: Reproductive Performance of B6J vs. B6N Embryos after Transfer
| Metric | C57BL/6J (B6J) | C57BL/6N (B6N) | Significance |
|---|---|---|---|
| Birth Rate (Unilateral ET) | 30.8% | 24.5% | Significantly higher for B6J |
| Birth Rate (Bilateral ET) | 33.0% | 26.9% | Significantly higher for B6J |
| Pups per Embryo (Unilateral) | 0.31 | 0.24 | - |
| Pups per Embryo (Bilateral) | 0.33 | 0.27 | - |
| Embryos Needed per Pup | ~3.03 | ~3.70 - 4.09 | - |
Q3: Does unilateral or bilateral embryo transfer yield better results? The decision between unilateral and bilateral transfer involves a trade-off between efficiency and animal welfare. Bilateral transfer, where embryos are split between both uterine horns, generally produces a larger litter size for both B6J and B6N lines [49]. However, unilateral transfer, which involves surgery on only one side, reduces surgical trauma and contributes to refinement in animal research. The pregnancy rate was significantly higher for bilateral transfer only for B6J embryos, but not for B6N or other lines [49]. Your choice should balance the need for higher pup yield with the principles of the 3Rs (Replacement, Reduction, and Refinement).
Q4: Beyond strain, what other factors can cause low birth rates after embryo transfer? Successful embryo transfer depends on a complex interplay of many factors. If you are troubleshooting low birth rates, investigate these key areas [49]:
- Embryo Quality: The stage of the embryo, synchrony with the recipient's reproductive cycle, and overall morphological health are critical.
- Recipient Condition: The age, weight, and hormonal status (pseudopregnancy) of the recipient dam can significantly impact implantation and pregnancy maintenance.
- Technical Skill: The experience level of the person performing the microsurgery is a well-known variable.
- Husbandry: Post-operative care and housing conditions, including noise levels, can affect pregnancy outcomes.
Troubleshooting Low Birth Rates
Problem: Consistently low birth rates despite successful embryo transfer surgery.
Investigation and Solution Pathway:
- Audit Embryo Source and Quality: First, confirm the quality and genetic background of your embryos. As the data shows, B6N embryos intrinsically have a lower birth rate than B6J embryos. Ensure you are using morphologically intact embryos and have adjusted your expected outcomes and colony sizing calculations accordingly [49].
- Evaluate Transfer Method: If your primary goal is to maximize the number of pups per recipient, consider switching from unilateral to bilateral embryo transfer. This can increase litter size, though it also increases potential pain and discomfort for the recipient [49].
- Review Recipient Management: Standardize the selection of recipient dams. Use nulliparous, pseudopregnant females within an optimal age and weight range (e.g., 8-15 weeks). Ensure proper synchrony between the developmental stage of the embryos and the recipient's reproductive state [49].
- Assess Surgical and Post-Operative Protocols: Provide appropriate analgesic support (e.g., carprofen) post-surgery. Ensure a clean and stress-free recovery environment with warming support until the recipient regains consciousness. Consistent, skilled surgical technique is paramount [49].
Experimental Protocols for Key Cited Studies
Protocol 1: Embryo Transfer for Reproductive Performance Comparison This methodology was used to generate the comparative data in Table 1 [49].
- Embryo Production: Fresh 2-cell embryos were produced via in vitro fertilization. Donor backgrounds included C57BL/6J (B6J), C57BL/6N (B6N), and backcrossed lines.
- Recipients: Nulliparous, pseudopregnant Crl:CD1(ICR) (CD1) outbred mice (age 8-15 weeks) were used as recipients.
- Transfer Procedure: Recipients were anesthetized. Either 15-18 embryos were transferred unilaterally into the left oviduct, or the same total number was split bilaterally between both oviducts.
- Post-Operative Care: Analgesia (carprofen, 10 mg/kg) was administered. Animals recovered on a warming plate and were housed singly until birth.
- Data Collection: The numbers of litters and pups born were recorded to calculate pregnancy rates, birth rates, and litter sizes.
Protocol 2: Gut Microbiota Transfer via Embryo Transfer This protocol highlights another application of ET, where the technique is used to study the influence of gut microbiota by transferring embryos into surrogate dams with a defined microbiome [50].
- Donors and Embryos: B6J or B6N mice were bred, and embryos were collected at the two-cell stage.
- Surrogate Dams: Pseudopregnant CD-1 surrogate dams, which harbored a specific gut microbiome (e.g., high-richness or low-richness), were used.
- Surgical Transfer: Embryos were surgically transplanted into the surrogate dams.
- Outcome: The resulting pups acquired their initial gut microbiota from the surrogate dam during birth and the postpartum period, allowing for the study of microbiome effects on various phenotypes.
Signaling Pathways and Workflows
The following diagrams illustrate key logical relationships and experimental workflows relevant to troubleshooting embryo transfer.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Mouse Embryo Transfer Experiments
| Item | Function / Application |
|---|---|
| C57BL/6J (B6J) & C57BL/6N (B6N) Mice | Defined genetic backgrounds for use as embryo donors to study strain-specific effects on development and reproductive performance [49] [50]. |
| Crl:CD1(ICR) Outbred Mice | Frequently used as robust pseudopregnant recipient dams due to good mothering ability and large litter size [49]. |
| Ketamine/Xylazine Anesthesia | Intraperitoneal injectable anesthetic cocktail for surgical anesthesia of recipient mice during the embryo transfer procedure [49]. |
| Carprofen | Non-steroidal anti-inflammatory drug (NSAID) administered subcutaneously for post-operative analgesic support and pain management [49]. |
| Pregnant Mare Serum Gonadotropin (PMSG) | Hormone used for superovulation in donor females to induce the production of a larger number of oocytes [49]. |
| Human Chorionic Gonadotropin (hCG) | Hormone used to trigger ovulation in superovulated donor females, allowing for timed mating and embryo collection [49]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary factors contributing to low birth rates after mouse embryo transfer? Low birth rates can stem from multiple factors related to the embryo, the laboratory environment, and the transfer technique. Key factors include:
- Embryo Origin and Culture: Mouse embryos generated via In Vitro Fertilization (IVF) have a significantly lower predicted live birth rate (14.7%) compared to those derived from in vivo fertilization and culture (FB) (44.7%). Suboptimal culture conditions can further reduce these rates [26].
- Genetic Integrity: A 2025 mouse study found that pups conceived via IVF had about 30% more new single-nucleotide variants (small DNA changes) compared to those conceived naturally. While most are likely neutral, this indicates that the ART process can increase genetic errors [11].
- Exposure to Toxins: Exposure of mouse and human embryos to acetaminophen (at concentrations found in reproductive tissues after a standard dose) can disrupt DNA synthesis, cause embryo arrest, and reduce implantation rates [46].
- Embryo Quality: The developmental stage and quality of the embryo are the strongest predictors of success. Blastocysts have a higher implantation potential than cleavage-stage embryos [51] [17].
Q2: How does a sequential embryo transfer strategy improve outcomes, and when is it indicated? Sequential Embryo Transfer (ET) involves transferring embryos at different developmental stages (e.g., a cleavage-stage embryo and a blastocyst) in the same cycle to widen the window of implantation. Evidence from frozen ET cycles shows it can significantly improve clinical pregnancy and implantation rates compared to conventional single-stage transfer [52]. This strategy is particularly beneficial for models simulating Recurrent Implantation Failure (RIF), where it helps overcome inaccuracies in synchronizing the embryo with the receptive endometrium [52].
Q3: What key reagents and novel factors are critical for optimizing early embryonic development? Recent screenings using inhibitor libraries have identified several novel and known factors essential for mouse embryonic development. The table below lists key reagents and their functions in research.
Table: Key Research Reagent Solutions for Embryo Development Studies
| Reagent / Factor | Type | Primary Function in Research |
|---|---|---|
| PRIMA-1 [53] | p53 Activator | Used in research to study p53 pathway involvement in embryonic arrest. |
| Cathepsin D Inhibitors [53] | Protease Inhibitor | Research tool to investigate the role of the lysosomal protease Cathepsin D; gene knockout verifies its role in development. |
| CXCR2 Antagonists [53] | Chemokine Receptor Blocker | Used to study the function of the CXCR2 receptor in embryonic development; gene knockout arrests development. |
| Apamin (SK2/SK3 Blocker) [53] | Potassium Channel Inhibitor | Research chemical used to probe the role of calcium-activated potassium channels (SK2 and SK3) in early embryogenesis. |
| Acetaminophen (APAP) [46] | Pharmaceutical Agent | Used in experimental models to induce embryo arrest and study mechanisms of cell cycle disruption via ribonucleotide reductase inhibition. |
| ATPase Inhibitors [53] | Enzyme Inhibitor | Research tools to understand the essential role of ATPases in development; inhibition of different types arrests embryos at distinct stages. |
Q4: What procedural and laboratory factors are most critical for a successful transfer? Success depends on a combination of embryo, endometrial, and technical factors, many of which are summarized in the clinical data below.
Table: Factors Influencing Embryo Transfer Success Rates
| Factor | Impact on Success Rate | Key Findings |
|---|---|---|
| Maternal Age | Negative Correlation | Women >40 years had significantly lower clinical pregnancy rates (aOR: 0.260) compared to those <35 [51]. |
| Embryo Stage | Positive with Blastocyst | Blastocyst transfer significantly increased clinical pregnancy vs. day-3 embryos (aOR: 0.294 for day-3) [51]. |
| Number of Embryos | Positive Correlation | Double Embryo Transfer (DET) was 1.78 times more likely to result in pregnancy than Single Embryo Transfer (SET) [51]. |
| Endometrial Thickness | Positive Correlation | Endometrial thickness <8 mm was associated with decreased clinical pregnancy (aOR: 0.443) compared to ≥8 mm [51]. |
| Embryo Quality | Strong Positive Correlation | Embryo quality was the strongest independent predictor of successful outcomes in frozen embryo transfer cycles [17]. |
| Method of Conception | Critical in Models | In mice, IVF-derived embryos had a 3.3x lower predicted live birth rate than in vivo-derived (FB) embryos [26]. |
Experimental Protocols & Workflows
Protocol 1: Screening for Novel Embryonic Regulatory Factors Using Inhibitor Libraries
This protocol is adapted from a 2025 study that identified novel factors like Cathepsin D and CXCR2 in mouse early embryonic development [53].
1. Embryo Preparation:
- Animals: Use C57BL/6N mice. Induce ultra-superovulation in 4-week-old female mice using HyperOva and hCG.
- In Vitro Fertilization (IVF): Collect oocytes and fertilize them with sperm in HTF medium.
- Cryopreservation: Four hours post-fertilization, cryopreserve one-cell stage embryos using a freezing solution containing 1M DMSO and DAP213. Store in liquid nitrogen.
2. Inhibitor Library Screening:
- Library: Use standardized inhibitor kits (e.g., SCADS Inhibitor Kit).
- Preparation: Create 100 µM stock solutions of each inhibitor. Dilute to a final working concentration (e.g., 1 µM) in KSOM embryo culture medium.
- Screening Setup: Thaw cryopreserved one-cell embryos. Culture 20 embryos per treatment group in KSOM medium containing each inhibitor. Include a control group with no inhibitor.
- Replication: Perform each treatment and control in triplicate (e.g., 288 total culture experiments for 95 inhibitors).
- Outcome Measurement: Culture embryos and calculate the developmental rate:
Developmental Rate (%) = (Number of Developed Embryos / Total Number of Embryos) * 100 - Validation: Confirm the role of identified factors using CRISPR-Cas9 mediated gene knockout in subsequent experiments.
Screening for Novel Embryonic Regulatory Factors
Protocol 2: Evaluating Technique Efficacy via Sequential vs. Conventional Embryo Transfer
This protocol is based on clinical studies that can be adapted to a mouse model of recurrent implantation failure (RIF) [52].
1. Study Population and Endometrial Preparation:
- Grouping: Define a model for RIF (e.g., failure to implant after multiple high-quality embryo transfers). Divide subjects into two groups: Conventional ET and Sequential ET.
- Endometrial Prep: Prepare the endometrium using hormone replacement therapy (HRT). Administer estrogen until endometrial thickness reaches a predefined threshold (e.g., ≥8mm).
2. Embryo Transfer Protocol:
- Conventional ET Group: Transfer embryos at a single developmental stage. For mice, this could be either cleavage-stage embryos (on day 4 of progesterone administration) or blastocysts (on day 6 of progesterone administration).
- Sequential ET Group:
- First Transfer: Perform the first transfer with cleavage-stage embryos on day 4 of progesterone administration.
- Second Transfer: Perform the second transfer with blastocysts (Day 5 or Day 6) on day 6 of progesterone administration.
3. Outcome Measurement and Analysis:
- Primary Outcomes: Calculate and compare between groups:
- Clinical Pregnancy Rate:
(Number of clinical pregnancies / Number of ET cycles) * 100 - Implantation Rate:
(Number of gestational sacs / Total number of embryos transferred) * 100
- Clinical Pregnancy Rate:
- Statistical Analysis: Use appropriate tests (e.g., Chi-square) to compare rates between groups. Perform stratified analysis based on the number of previous failure cycles and embryo quality.
Sequential vs. Conventional Embryo Transfer Workflow
Conclusion
Optimizing mouse embryo transfer is a multifactorial endeavor requiring attention to genetic background, technical execution, and embryo culture environment. Foundational research confirms that ART procedures can influence embryonic genetics, but methodological refinements in transfer technique and culture conditions can significantly mitigate risks. Troubleshooting efforts must be data-driven, leveraging comparative outcomes to validate improvements. The consistent application of optimized, evidence-based protocols is paramount for enhancing live birth rates, ensuring animal welfare, and improving the reliability and efficiency of mouse models in preclinical and biomedical research. Future directions should focus on standardizing protocols across facilities and further elucidating the long-term health implications of ART-conceived offspring.
References
- 1. A Technique for Facile and Precise Transfer of Mouse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3572708/]
- 2. Development of an embryo transfer model to study uterine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8861889/]
- 3. Causes of IVF Failure - Why Does IVF Fail [https://txfertility.com/in-vitro-fertilization-ivf/causes-ivf-failure/]
- 4. Low fertility in vivo resulting from female factors causes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5904756/]
- 5. Association Between Human Embryo Culture Conditions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298697/]
- 6. Reduced nutrient concentration during in vitro culture ... [https://www.sciencedirect.com/science/article/pii/S0093691X21002351]
- 7. How to ensure embryo viability in your culture system [https://blog.vitrolife.com/togetheralltheway/how-to-ensure-embryo-viability-in-your-culture-system]
- 8. Why Does IVF Fail? 6 Reasons For IVF Failure [https://www.fertility-academy.co.uk/blog/why-does-ivf-fail/]
- 9. improving the sensitivity for use as a quality control assay ... [https://www.sciencedirect.com/science/article/pii/S0015028216556386]
- 10. Behavioral sink [https://en.wikipedia.org/wiki/Behavioral_sink]
- 11. In mice, fertility treatments linked to higher mutations than ... [https://www.jax.org/news-and-insights/2025/november/in-mice-fertility-treatments-linked-to-higher-mutations-than-natural-conceptions]
- 12. Imprinting Disorders and Epigenetic Alterations in Children ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562381/]
- 13. Epigenetic reprogramming in mouse and human primordial ... [https://www.nature.com/articles/s12276-024-01359-z]
- 14. Sex differences in DNA methylation variations according to ... [https://www.nature.com/articles/s41598-024-73845-3]
- 15. Errors in IVF laboratories: risks assessments and mitigations [https://mefj.springeropen.com/articles/10.1186/s43043-023-00130-0]
- 16. Errors in IVF | PPTX [https://www.slideshare.net/slideshow/errors-in-ivf/250641234]
- 17. Factors affecting frozen embryo transfer success rates [https://mefj.springeropen.com/articles/10.1186/s43043-025-00263-4]
- 18. Transcriptomic Analysis of Vitrified–Warmed vs. Fresh ... [https://www.mdpi.com/1422-0067/25/16/8658]
- 19. Analysis of factors influencing clinical pregnancy rates in ... [https://pubmed.ncbi.nlm.nih.gov/40636712/]
- 20. A review of factors influencing the implantation of euploid ... [https://www.sciencedirect.com/science/article/pii/S2666571922000032]
- 21. IVF Embryo Transfers: The Complete Guide 2025 [https://www.pfcla.com/blog/embryo-transfers]
- 22. Nonsurgical Embryo Transfer Device Compared with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3548196/]
- 23. When the Embryo Meets the Endometrium: Identifying ... [https://www.mdpi.com/1422-0067/25/5/2834]
- 24. What's New from the Fertility and Sterility Family of Journals [https://www.asrm.org/news-and-events/asrm-news/latest-news/October-2025-whats-new-from-fertility-and-sterility2/]
- 25. Oxygen level alters energy metabolism in bovine ... [https://www.nature.com/articles/s41598-025-95990-z]
- 26. Effect of culture conditions and method of conception on ... [https://www.sciencedirect.com/science/article/abs/pii/S2666335X20300367]
- 27. “How did it go?â€â€”investigation of physician's experience ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559518/]
- 28. New approaches in the analysis of spent embryo culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334517/]
- 29. Optimized cesarean techniques, IVF use, and foster strain ... [https://www.nature.com/articles/s41598-025-05411-4]
- 30. Efficient and scheduled production of pseudopregnant female ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5735264/]
- 31. Fertility test of mice (Mus musculus) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336854/]
- 32. Embryo transfer: techniques and variables affecting success [https://www.sciencedirect.com/science/article/pii/S0015028201027315]
- 33. Monitoring uterine contractility in mice using a transcervical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5903945/]
- 34. The blessings and curses of C57BL/6 substrains in mouse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4944652/]
- 35. effects of mouse strain and in vitro maturation on sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4759009/]
- 36. improved sensitivity of the mouse embryo assay with ... [https://www.sciencedirect.com/science/article/pii/S0015028212023904]
- 37. C57BL/6 Mice [https://www.criver.com/products-services/find-model/c57bl6-mouse]
- 38. Causes of embryo implantation failure: A systematic review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11867936/]
- 39. Embryo Culture Media for IVF: Sequential vs. One-Step ... [https://www.geneabiomedx.com/geneabiomedx/embryo-culture-media-for-ivf-sequential-vs-one-step-media/]
- 40. Gene expression changes in blastocyst hatching affect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11839805/]
- 41. The impact of single step and sequential embryo culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9206725/]
- 42. Day 3 versus Day 5 refreshment of single-step medium for ... [https://www.sciencedirect.com/science/article/abs/pii/S147264832500495X]
- 43. nutrients turn over and metabolomic analysis of human ... [https://pubmed.ncbi.nlm.nih.gov/40690766/]
- 44. Manipulating the Mouse Embryo: A Laboratory Manual ... [https://www.cshlpress.com/default.tpl?action=full&--eqskudatarq=1130]
- 45. Optimizing frozen embryo transfer for low-quality ... [https://www.sciencedirect.com/science/article/pii/S1028455925001731]
- 46. Acetaminophen (Tylenol) leads to embryo arrest in ... [https://www.remembryo.com/acetaminophen-tylenol-impairs-embryo-development-in-mouse-human-models/]
- 47. Preimplantation Exposure to Bisphenol A and Triclosan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4556842/]
- 48. Persistent Wnt signaling affects IVF embryo implantation ... [https://www.sciencedirect.com/science/article/pii/S2095927325004724]
- 49. Reproductive Performance after Unilateral or Bilateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5868376/]
- 50. Transfer efficiency and impact on disease phenotype of ... [https://www.nature.com/articles/s41598-022-24014-x]
- 51. Determining Factors Influencing The Successful Embryo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11589970/]
- 52. Stratified analysis of clinical pregnancy outcomes of ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-023-06111-5]
- 53. Screening for novel factors involved in mouse early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575340/]