Validating Mutant Alleles: Integrating Sanger Sequencing and NGS for Robust Discovery and Diagnostics
This article provides a comprehensive guide for researchers and drug development professionals on validating mutant alleles discovered through Next-Generation Sequencing (NGS).
Validating Mutant Alleles: Integrating Sanger Sequencing and NGS for Robust Discovery and Diagnostics
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on validating mutant alleles discovered through Next-Generation Sequencing (NGS). It covers the foundational principles of both Sanger and NGS technologies, detailing their respective strengths in discovery and confirmation. The content explores established and emerging methodological workflows for validation, addresses common troubleshooting and optimization challenges, and delivers a critical comparative analysis of accuracy, throughput, and cost-effectiveness. By synthesizing current best practices and future trends, this resource aims to equip scientists with the knowledge to design rigorous, reliable validation strategies that enhance data integrity in both research and clinical diagnostics.
The Pillars of Precision: Understanding Sanger and NGS Technologies for Mutant Allele Analysis
FAQ: What are the fundamental differences in chemistry between Sanger (Chain Termination) and Next-Generation Sequencing (Massively Parallel Sequencing)?
The core difference lies in the scale and approach. Sanger sequencing is based on the chain termination method using dideoxynucleotides (ddNTPs), performed on a single DNA fragment per reaction. In contrast, Massively Parallel Sequencing (MGS), or Next-Generation Sequencing (NGS), uses technologies like sequencing-by-synthesis (SBS) to simultaneously sequence millions to billions of DNA fragments immobilized on a flow cell [1] [2] [3].
Table 1: Fundamental Comparison of Sequencing Chemistries
| Feature | Sanger Sequencing (Chain Termination) | Massively Parallel Sequencing (NGS) |
|---|---|---|
| Core Chemistry Principle | Dideoxy chain termination with capillary electrophoresis [3] | Sequencing-by-synthesis, pyrosequencing, or ligation [1] [2] [3] |
| Throughput | Low (single reaction per capillary) [1] | Ultra-high (millions to billions of parallel reactions) [1] [2] |
| Read Length | Long (up to ~1000 bases) | Short to moderate (50-400 bases, with some technologies longer) [2] [3] |
| Typical Application | Targeted sequencing of single genes or few amplicons; gold standard for validation [4] [5] | Whole genomes, exomes, transcriptomes, targeted panels; discovery applications [1] |
| Data Output | Kilobases per run | Gigabases to Terabases per run [1] |
| Key Technical Step | In vitro chain termination and electrophoretic separation | In situ clonal amplification (e.g., bridge PCR, emulsion PCR) and parallelized sequencing [2] [3] |
Validation of Mutant Alleles: Sanger vs. NGS
FAQ: Is Sanger sequencing still necessary for validating mutant alleles identified by NGS?
For high-quality NGS variant calls, recent large-scale studies suggest that Sanger confirmation may be redundant. A 2021 study validating 1109 variants from 825 clinical exomes reported a 100% concordance for high-quality single-nucleotide variants (SNVs) and small insertions/deletions (indels) detected by NGS, concluding that Sanger sequencing is more useful as a general quality control than as a mandatory verification step for such variants [4]. This demonstrates the high analytical sensitivity and specificity of modern NGS workflows.
Table 2: Analytical Performance of NGS for Mutant Allele Detection
| Study Focus | Sample & Variant Size | Key Metric | Result |
|---|---|---|---|
| Clinical Exome Validation [4] | 1109 variants in 825 exomes | Concordance with Sanger | 100% for high-quality SNVs and indels |
| Detection of Simple & Complex Mutations [5] | 119 changes in 20 samples | Analytical Sensitivity & Specificity | 100% concordance with known Sanger data |
| Somatic Mutation Validation [6] | 27 selected variations in cervical cancer | Sanger Validation Rate | ~60% (highlighting need for careful NGS parameter setting) |
NGS Troubleshooting Guide
FAQ: My NGS run yielded low or no data. What are the common causes?
Failures in NGS often originate from the library preparation stage. Below is a guide to diagnosing common issues [7].
Problem Category 1: Low Library Yield
- Failure Signals: Low final concentration, faint or broad peaks on electropherogram, high adapter-dimer peaks.
- Root Causes:
- Poor Input Quality: Degraded DNA/RNA or contaminants (phenol, salts) inhibit enzymes [7].
- Fragmentation Issues: Over- or under-shearing produces fragments outside the optimal size range [7].
- Adapter Ligation Inefficiency: Caused by suboptimal adapter-to-insert molar ratio, inactive ligase, or poor reaction conditions [7].
- Corrective Actions:
- Re-purify input DNA/RNA and use fluorometric quantification (e.g., Qubit) instead of UV absorbance alone.
- Optimize fragmentation parameters (time, enzyme concentration).
- Titrate adapter:insert ratio and ensure fresh ligation reagents are used [7].
Problem Category 2: High Duplicate Read Rate & Low Complexity
- Failure Signals: Abnormally high proportion of PCR duplicates, flat coverage.
- Root Causes:
- Over-amplification: Too many PCR cycles during library amplification [7].
- Insufficient Input DNA: Starting with too little DNA reduces library complexity from the outset.
- Corrective Actions:
- Reduce the number of amplification cycles.
- Increase the amount of input DNA within the recommended range for your protocol.
Problem Category 3: Instrument-Specific Errors
- Failure Signals: Chip initialization failures, connectivity errors, low bead loading (for semiconductor sequencing).
- Root Causes & Actions:
- Chip Check Failures: Ensure the chip is properly seated and the clamp is closed. If the error persists, replace the chip [8].
- Low Bead Count: Confirm that control beads were added during template preparation. This can also indicate problems with library or template quality [8].
- Server Connectivity Issues: Restart the instrument and server. Check ethernet connections [8].
Detailed Experimental Protocol: Validating NGS-Indentified Mutant Alleles by Sanger Sequencing
This protocol is used to confirm putative variants from NGS analysis, a critical step in research and diagnostic settings [4] [6].
Step 1: Variant Review and Selection
- Visualize putative variants from NGS data using a genome browser (e.g., Integrative Genomics Viewer) [4].
- Prioritize variants based on quality metrics (e.g., read depth ≥20x, variant fraction ≥20%) and potential biological significance [4].
Step 2: PCR Primer Design
- Use tools like NCBI Primer-BLAST.
- Design primers to flank the variation, generating an amplicon of 250-400 bp.
- Check primers for specificity and to ensure they do not bind to common SNPs or repetitive regions [4] [6].
Step 3: PCR Amplification
- Set up 50 µL PCR reactions using 50 ng of genomic DNA, reaction buffer, dNTPs, primers, and a high-fidelity DNA polymerase.
- Use touch-down or standard PCR cycling conditions with an annealing temperature optimized for the primers [5] [6].
Step 4: Amplicon Purification
- Verify successful amplification via agarose gel electrophoresis.
- Purify PCR products using a commercial purification kit (e.g., QIAquick) to remove primers, dNTPs, and enzymes [6].
Step 5: Sanger Sequencing and Analysis
- Quantify the purified PCR product.
- Perform Sanger sequencing reactions using the same primers as for PCR.
- Analyze the resulting chromatograms using sequence analysis software to confirm or refute the presence of the NGS-identified variant [6].
The Scientist's Toolkit: Essential Reagents for NGS Validation Workflows
Table 3: Key Research Reagent Solutions
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| High-Fidelity DNA Polymerase | Accurate amplification of target regions for both NGS library prep and Sanger validation PCR. | Reduces PCR-introduced errors during amplicon generation for sequencing [5]. |
| NGS Library Prep Kit | Converts genomic DNA into a library of fragments with platform-specific adapters. | Preparing samples for whole-exome or targeted gene panel sequencing on platforms like Illumina [1]. |
| Magnetic Beads (SPRI) | Size selection and purification of DNA fragments; clean-up of PCR products. | Removing primer dimers after library amplification or purifying Sanger sequencing templates [7]. |
| Fluorometric Quantification Kit (Qubit) | Accurate quantification of DNA concentration using fluorescent dyes specific to DNA. | Measuring input DNA for NGS library prep and quantifying final library yield, more accurate than UV absorbance [7]. |
| Sanger Sequencing Kit | Provides the dideoxy chain-termination reagents for cycle sequencing. | Generating sequence traces for confirmatory analysis of NGS-identified variants [6]. |
Core Metrics for Sequencing Success
In the context of validating mutant alleles, understanding key performance metrics is fundamental to designing robust experiments and accurately interpreting results. The table below defines the core metrics that influence the capability and reliability of both Sanger and Next-Generation Sequencing (NGS) methods.
| Metric | Definition | Importance in Mutant Allele Validation |
|---|---|---|
| Read Length | The number of consecutive nucleotides (bases) produced from a single DNA fragment during a sequencing run. [9] [10] | Longer reads are beneficial for spanning repetitive genomic regions and for the de novo assembly of novel sequences or large structural variants. [10] |
| Sequencing Depth (Read Depth) | The average number of times a specific nucleotide in the genome is read during sequencing (e.g., 100x depth). [11] [12] | Higher depth increases confidence in base calls and is critical for detecting low-frequency variants (e.g., somatic mutations or heteroplasmic alleles); it directly impacts the limit of detection. [13] [12] [14] |
| Throughput | The total amount of sequence data generated by a sequencing instrument in a single run, often measured in gigabases (Gb) or terabases (Tb). [13] [10] | High-throughput platforms (NGS) enable the parallel sequencing of millions of fragments, making it feasible to screen hundreds of samples or genes cost-effectively. [13] |
Sanger Sequencing vs. NGS: A Quantitative Comparison for Validation
Choosing the appropriate sequencing technology depends on the scale and objective of your validation project. The following table provides a direct, data-driven comparison of Sanger sequencing and NGS.
| Feature | Sanger Sequencing | Next-Generation Sequencing (NGS) |
|---|---|---|
| Typical Read Length | Long; typically 800-1000 base pairs. [9] | Varies by platform; short-read (e.g., Illumina: 50-300 bp), long-read (e.g., PacBio: 15,000-20,000 bp). [10] |
| Typical Sequencing Depth | Not applicable in the same way as NGS; a single fragment is sequenced per reaction. [13] | Highly scalable; can range from tens to thousands of reads per base to detect low-frequency variants. [13] [12] |
| Throughput | Low; sequences one DNA fragment at a time. [13] | Massively parallel; sequences millions of fragments simultaneously per run. [13] |
| Key Strengths | - "Gold standard" accuracy (~99.99%). [9]- Simple data analysis. [10]- Cost-effective for interrogating a small number of targets (e.g., <20). [13] | - High sensitivity for low-frequency variants (detection limit down to ~1% vs. 15-20% for Sanger). [13] [10]- High discovery power to identify novel variants. [13]- Cost-effective for screening many targets or samples. [13] |
| Common Applications in Validation | - Validating DNA sequences, including those identified by NGS. [9] [15]- Sequencing a short region in a limited number of samples. [13] [10] | - Discovery screening for novel or rare variants across hundreds to thousands of genes. [13]- Detecting low-abundance mutations, such as in cancer or measurable residual disease (MRD). [12] |
Troubleshooting Guide: FAQs on Performance Metrics
How does sequencing depth affect the detection of low-frequency mutant alleles?
Sequencing depth is the most critical factor determining the lower limit of variant detection. The limit of detection for NGS is directly related to the depth of sequencing performed. [12] For example, to confidently identify a variant present in only 1% of cells (Variant Allele Frequency, VAF = 1%), a significantly higher sequencing depth is required compared to detecting a variant present in 50% of cells. [12] A higher depth provides more statistical power to distinguish a true low-frequency variant from background sequencing errors. [11] [14] In contrast, Sanger sequencing, which produces a composite chromatogram, has a much higher limit of detection, typically around 15-20%, making it unsuitable for finding low-frequency variants. [13] [10]
My Sanger sequencing chromatogram shows mixed/overlapping peaks after a clear start. What is the cause?
A chromatogram that starts with high-quality data but then becomes mixed, showing two or more peaks at each position, typically indicates the presence of multiple DNA templates in the reaction. [16] Common causes include:
- Colony contamination: Accidentally picking more than one bacterial colony when preparing plasmid DNA for sequencing. [16]
- Multiple priming sites: The sequencing primer is binding to more than one location on the template DNA. [16]
- Incomplete PCR purification: Residual primers or salt from the PCR amplification reaction can cause spurious priming events. [16] Solution: Ensure you are sequencing a single, pure DNA template. Re-streak bacterial colonies to isolate a single clone, check your primer for specificity, and thoroughly clean up PCR products before sequencing. [16]
My sequencing data terminates abruptly. How can I resolve this issue?
Early termination in sequencing reads can occur in both Sanger and NGS workflows for different reasons.
- In Sanger sequencing: Good quality data that comes to a hard stop is often a sign of secondary structure (e.g., hairpins) in the DNA template that the polymerase cannot pass through. [16] Long stretches of Gs or Cs can cause similar issues.
- Solution: Use an alternate sequencing chemistry designed for "difficult templates," or design a new primer that sits on or just after the problematic region to sequence through it. [16]
- In NGS: A sudden drop in coverage in a specific region can be due to high GC or AT content, repeat sequences, or other genomic complexities that make library preparation or sequencing inefficient. [15] [17] Solution: Consider using library preparation methods optimized for high-GC regions and ensure you have sufficient overall sequencing depth to compensate for regions with naturally lower coverage. [17]
Experimental Protocol: Validating NGS-Identified Mutants with Sanger Sequencing
This protocol details the steps to confirm variants discovered through NGS using the Sanger method, a common practice in research and diagnostics. [15]
Primer Design
- Design primers that flank the variant of interest using a tool like Primer3. [15]
- Amplicon size should be appropriate for Sanger sequencing (typically 500-1000 bp). [9]
- Critical Check: Use tools like Primer-BLAST to check for primer specificity across the genome. Always check that the primer sequences themselves do not contain known single-nucleotide polymorphisms (SNPs), as this can cause allelic dropout (ADO) and failure to amplify one allele. [15]
PCR Amplification and Purification
- Perform a standard PCR reaction using a high-fidelity DNA polymerase to minimize amplification errors. [15]
- Purify the PCR product to remove excess salts, dNTPs, and primers. This step is crucial for obtaining a high-quality Sanger sequence. [16] This can be done using enzymatic cleanup (e.g., Exonuclease I and Alkaline Phosphatase) or column-based purification kits. [15]
Sanger Sequencing Reaction and Analysis
- The purified PCR product is sequenced using a cycle sequencing reaction with fluorescently labeled dideoxynucleotides (ddNTPs). [9]
- The reaction products are capillary electrophoresis to generate the chromatogram. [9]
- Analyze the chromatogram trace file (.ab1) by visually inspecting the position of the variant. The base call at the specific position should clearly correspond to the mutant allele identified by NGS. [15] [18]
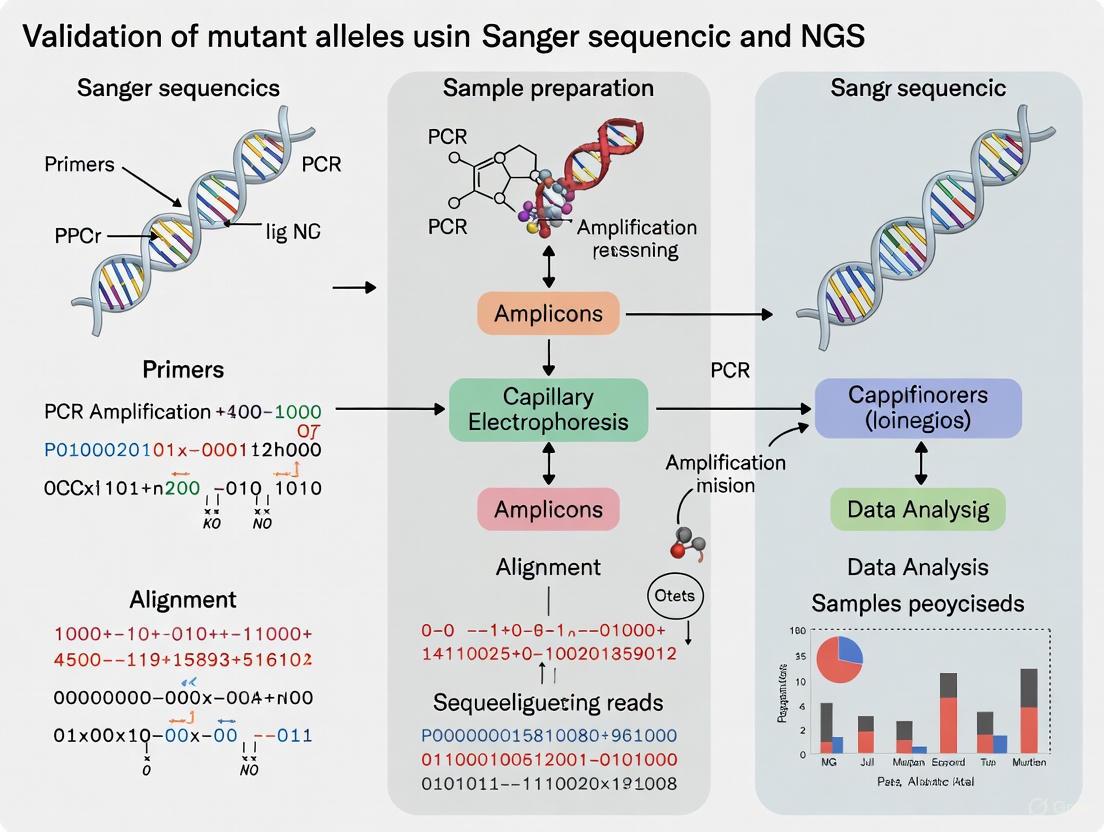
Workflow Diagram: From NGS Discovery to Sanger Validation
The following diagram illustrates the logical workflow for validating a mutant allele discovered via NGS, incorporating key decision points and troubleshooting steps.
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and materials used in sequencing workflows for mutant allele validation, along with their critical functions.
| Reagent / Material | Function in Validation Workflow |
|---|---|
| High-Fidelity DNA Polymerase | Used for PCR amplification prior to Sanger sequencing. Its high accuracy reduces the introduction of errors during amplification, ensuring the sequence represents the original template. [15] |
| Unique Molecular Identifiers (UMIs) | Short random nucleotide sequences ligated to each DNA fragment in an NGS library before amplification. UMIs allow bioinformatic correction of PCR duplicates and sequencing errors, improving the accuracy of variant calling, especially for low-frequency alleles. [12] |
| Sanger Sequencing Primers | Oligonucleotides designed to be complementary to the region flanking the variant of interest. They provide the starting point for the dideoxy chain-termination sequencing reaction. [9] [15] |
| Fluorescent ddNTPs | Dideoxynucleotide triphosphates (ddATP, ddGTP, ddCTP, ddTTP), each labeled with a distinct fluorescent dye. They are incorporated by DNA polymerase during Sanger sequencing, terminating strand elongation and generating fragments of different lengths that are detected by capillary electrophoresis. [9] |
| Targeted Gene Panels (NGS) | A pre-designed set of probes used to capture and sequence a specific subset of genes of interest from a complex genome. This focuses sequencing power on relevant regions, allowing for higher depth and more cost-effective screening compared to whole-genome sequencing. [15] |
NGS as a Discovery Powerhouse for Novel and Rare Variants
Next-generation sequencing (NGS) has revolutionized genetic research by enabling the simultaneous analysis of millions of DNA fragments, dramatically accelerating the discovery of novel and rare variants associated with disease [19]. Despite these technological advances, the question of how and when to validate NGS findings using Sanger sequencing remains central to rigorous scientific practice. This technical support center addresses this critical interface, providing researchers with troubleshooting guidance, validation protocols, and strategic frameworks to ensure the highest data quality while optimizing resource allocation in their discovery pipelines.
Foundational Concepts: NGS Accuracy and Validation Rationale
How accurate is NGS, and why is validation still discussed?
NGS demonstrates exceptionally high accuracy, with studies reporting validation rates of 99.965% against Sanger sequencing [20]. This performance exceeds many accepted medical tests that don't require orthogonal confirmation. Research examining over 5,800 NGS-derived variants found only 19 were not initially validated by Sanger data, and 17 of these were confirmed as true positives upon re-testing with optimized primers [20].
The persistence of validation discussions stems from several factors:
- Clinical reporting standards: Traditional guidelines often mandated orthogonal confirmation for clinical reporting [21]
- Variant-specific concerns: Certain variant types and genomic regions remain challenging
- Quality parameter thresholds: Establishing laboratory-specific quality thresholds determines which variants require confirmation [21]
What is the current consensus on Sanger validation of NGS variants?
The field is shifting toward a risk-based approach rather than universal validation. Recent research indicates that "high-quality" NGS variants defined by specific thresholds may not require routine Sanger confirmation [21] [20]. One large-scale study concluded that "validation of NGS-derived variants using Sanger sequencing has limited utility, and best practice standards should not include routine orthogonal Sanger validation of NGS variants" [20].
Troubleshooting Guide: Common NGS Challenges and Solutions
Library Preparation Issues
| Problem Category | Typical Failure Signals | Common Root Causes | Corrective Actions |
|---|---|---|---|
| Sample Input/Quality | Low starting yield; smear in electropherogram; low library complexity | Degraded DNA/RNA; sample contaminants; inaccurate quantification; shearing bias | Re-purify input sample; use fluorometric quantification (Qubit) instead of UV; assess sample quality via 260/230 and 260/280 ratios [7] |
| Fragmentation & Ligation | Unexpected fragment size; inefficient ligation; adapter-dimer peaks | Over-/under-shearing; improper buffer conditions; suboptimal adapter-to-insert ratio | Optimize fragmentation parameters; titrate adapter:insert molar ratios; ensure fresh ligase and buffer [7] |
| Amplification & PCR | Overamplification artifacts; bias; high duplicate rate | Too many PCR cycles; inefficient polymerase; primer exhaustion | Reduce PCR cycles; use high-fidelity polymerases; optimize primer design and annealing conditions [7] |
| Purification & Cleanup | Incomplete removal of small fragments; sample loss; carryover of salts | Wrong bead ratio; bead over-drying; inefficient washing; pipetting error | Optimize bead:sample ratios; avoid over-drying beads; implement pipette calibration [7] |
Data Quality and Variant Validation Challenges
How can I identify which NGS variants truly require Sanger validation?
Research indicates that implementing quality thresholds can drastically reduce validation workload. A study of 1,756 WGS variants established that caller-agnostic thresholds (DP ≥ 15, AF ≥ 0.25) reduced variants requiring validation to 4.8% of the initial set, while caller-dependent thresholds (QUAL ≥ 100) reduced this further to 1.2% [21].
Systematic validation decision workflow:
This workflow reflects evidence that variants meeting these quality thresholds demonstrated 100% concordance with Sanger sequencing in validation studies [21].
Experimental Protocols: Methodologies for Robust Variant Detection
Protocol 1: Establishing Laboratory-Specific Quality Thresholds
Purpose: To determine optimal quality score thresholds that distinguish high-quality variants requiring no orthogonal validation from lower-quality variants needing Sanger confirmation.
Materials:
- NGS data from 30-50 samples with mean coverage ≥30x
- Orthogonal validation capability (Sanger sequencing)
- Bioinformatics pipeline for variant calling
Methodology:
- Call variants using your standard bioinformatics pipeline
- Annotate each variant with key parameters: DP, AF, QUAL, FILTER status
- Perform Sanger sequencing on all variants regardless of quality
- Analyze concordance between NGS and Sanger results
- Generate receiver operating characteristic (ROC) curves for each quality metric
- Determine optimal thresholds that provide 100% sensitivity for true positives
- Validate thresholds on an independent sample set
Expected Outcomes: Laboratory-specific quality thresholds that minimize unnecessary Sanger validation while maintaining >99.9% concordance for high-quality variants [21].
Protocol 2: Troubleshooting Library Preparation Failures
Purpose: To systematically diagnose and resolve common NGS library preparation problems.
Materials:
- BioAnalyzer or TapeStation
- Fluorometric quantitation system (Qubit)
- PCR purification beads
- Fresh preparation of all buffers and enzymes
Troubleshooting Steps:
- Low Library Yield Diagnosis:
- Compare Qubit and BioAnalyzer quantification values
- Check 260/230 and 260/280 ratios on nanodrop
- Examine electropherogram for adapter dimer peaks (~70-90bp)
- Verify fragmentation size distribution
- Corrective Actions:
- Re-purify input DNA if contaminants detected
- Optimize adapter:insert molar ratios (typically 1:5 to 1:10)
- Adjust bead purification ratios (typically 0.8x-1.8x)
- Verify enzyme activity and buffer conditions [7]
Advanced Applications: Rare Variants and Structural Detection
How does NGS facilitate rare variant discovery?
NGS enables rare variant analysis through several strategic approaches:
- Gene-level association tests: Overcome power limitations by aggregating rare variants within functional units [22]
- Burden tests: Compare whether rare variants in a gene are associated with traits by analyzing the total number of rare variants [22]
- Sequence kernel association tests (SKAT): Detect associations without assuming all variants have the same effect direction [22]
What specialized approaches detect structural variants?
Long-read sequencing technologies address NGS limitations in detecting structural variants (SVs):
Performance Comparison of Long-Read Technologies:
| Feature | PacBio HiFi | Oxford Nanopore (ONT) |
|---|---|---|
| Read Length | 10–25 kb | Up to >1 Mb |
| Accuracy | >99.9% | ~98–99.5% |
| Strengths | Exceptional accuracy, clinical applications | Ultra-long reads, portability, real-time analysis |
| SV Detection F1 Score | >95% | 85–90% |
Long-read sequencing increases diagnostic yield by 10–15% in rare disease populations after extensive short-read sequencing fails to provide diagnoses [23]. These technologies particularly excel at resolving complex SVs in repetitive regions that are inaccessible to short-read technologies.
Frequently Asked Questions
Should I always validate NGS variants by Sanger before publication?
Not necessarily. The 2025 study on WGS variants recommends that high-quality variants meeting specific thresholds do not require validation [21]. For clinical reporting, each laboratory should establish a confirmatory testing policy based on their validated quality thresholds [21]. Research publications should clearly state validation practices and quality metrics.
What are the most critical parameters for defining "high-quality" variants?
Caller-agnostic parameters:
Caller-specific parameters:
How does NGS performance compare with standard techniques clinically?
In non-small cell lung cancer, NGS demonstrates high diagnostic accuracy compared to standard techniques:
Diagnostic Performance in Advanced NSCLC:
| Mutation Type | Tissue Sensitivity | Tissue Specificity | Liquid Biopsy Sensitivity |
|---|---|---|---|
| EGFR | 93% | 97% | 80% |
| ALK rearrangements | 99% | 98% | Limited |
| BRAF V600E | - | - | 80% |
| KRAS G12C | - | - | 80% |
Liquid biopsy NGS had significantly shorter turnaround time (8.18 vs. 19.75 days; p < 0.001) compared to standard tissue testing [24].
Research Reagent Solutions
| Essential Material | Function in NGS Workflow | Implementation Notes |
|---|---|---|
| SureSelect/SureSelect ICGC System | Solution-hybridization exome capture | Target enrichment for WES; ensure adequate input DNA [20] |
| TruSeq systems (V1/V2) | Library preparation | Compatible with Illumina platforms; follow manufacturer's cycling recommendations [20] |
| Qubit fluorometric system | Nucleic acid quantification | More accurate than UV spectrophotometry for library quantification [7] |
| AMPure XP beads | Library purification and size selection | Optimize bead:sample ratio for target fragment retention [7] |
| HaplotypeCaller (GATK) | Variant calling | Generate QUAL scores for variant filtering; version-dependent parameters [21] |
| DeepVariant | Variant calling | Alternative caller for verification; performs well on challenging variants [21] |
The powerful synergy between NGS discovery and strategic validation enables researchers to maximize both efficiency and accuracy in variant detection. By implementing evidence-based quality thresholds, establishing laboratory-specific validation protocols, and leveraging appropriate technologies for different variant types, research and clinical laboratories can harness the full potential of NGS as a discovery powerhouse for novel and rare variants while maintaining rigorous standards of verification.
Sanger Sequencing as the Gold Standard for Targeted Confirmation
Next-Generation Sequencing (NGS) has revolutionized genetic discovery, enabling the simultaneous analysis of hundreds to thousands of genes. However, in both clinical and research settings, the verification of critical genetic variants, such as suspected mutant alleles, remains paramount. Within this framework, Sanger sequencing continues to be employed as the trusted gold standard for orthogonal validation of NGS-derived variants prior to reporting. This guide provides targeted technical support, offering detailed troubleshooting and best practices to ensure that your Sanger confirmation data is of the highest quality, thereby solidifying the reliability of your genetic findings.
Technical Support Center: FAQs & Troubleshooting Guides
FAQ: Foundational Principles
1. Why is Sanger sequencing still considered the gold standard for validating NGS variants?
Sanger sequencing is regarded as a gold standard due to its high accuracy (over 99%) and the straightforward interpretability of its output data [25]. It provides long reads (500-1000 base pairs) from a single, specific amplicon, making it ideal for confirming individual variants identified by broader, more complex NGS tests [26]. This orthogonal method uses a completely different chemistry and workflow than NGS, providing an independent check that minimizes the risk of systematic errors.
2. Is it always necessary to validate NGS variants with Sanger sequencing?
Emerging evidence from large-scale studies suggests that for high-quality NGS variants, Sanger confirmation may be redundant. One systematic evaluation of over 5,800 NGS variants found a validation rate of 99.965%, concluding that routine Sanger validation has limited utility [20]. Another study of 1,109 variants from 825 clinical exomes showed 100% concordance for high-quality single-nucleotide variants and small insertions/deletions, suggesting labs can establish their own quality thresholds to discontinue universal Sanger confirmation [27].
3. What are the key limitations of Sanger sequencing compared to NGS?
The primary limitation is throughput. Sanger sequencing is designed to interrogate one DNA fragment per reaction, whereas NGS is massively parallel, sequencing millions of fragments simultaneously [13]. This makes Sanger cost-effective for a low number of targets (~20 or fewer) but impractical for sequencing large numbers of genes or samples. Sanger also has a higher limit of detection (~15-20%), making it less sensitive for identifying low-frequency variants in heterogeneous samples compared to deep sequencing with NGS [13] [25].
Troubleshooting Guide: Common Experimental Issues
The table below summarizes frequent problems, their causes, and solutions.
| Problem | Identifying Characteristics | Possible Causes & Solutions |
|---|---|---|
| Failed Reaction [16] | Sequence data contains mostly N's; messy trace with no discernable peaks. | - Cause: Low template concentration, poor quality DNA, or contaminants.- Solution: Precisely quantify DNA (e.g., with a NanoDrop); ensure A260/A280 ratio is ~1.8; clean up DNA to remove salts and primers. |
| High Background Noise [16] [28] | Discernable peaks with significant background noise along the baseline; low quality scores. | - Cause: Low signal intensity from poor amplification, often due to low template concentration or inefficient primer binding.- Solution: Optimize template concentration; check primer design and binding efficiency. |
| Sequence Degradation/ Early Termination [16] [28] | High-quality sequence starts strongly but stops prematurely or becomes messy. Signal intensity drops sharply. | - Cause: Secondary structures (e.g., hairpins) or long homopolymer stretches that the polymerase cannot pass through. Too much template DNA can also cause this.- Solution: Use an alternate sequencing chemistry designed for "difficult templates"; redesign primer to sequence from the opposite strand; optimize template concentration. |
| Mixed Sequence (Double Peaks) [16] [29] | The sequence trace becomes mixed, showing two or more peaks at the same position starting from a certain point or from the beginning. | - Cause: Multiple templates in the reaction (e.g., colony contamination, multiple priming sites, or insufficient PCR cleanup leaving residual primers).- Solution: Ensure a single colony is picked; verify primer specificity to a single site; perform thorough PCR cleanup. |
| Dye Blobs [16] [28] | Large, broad peaks (typically C, G, or T) that can obscure base calling, often seen around 70 base pairs. | - Cause: Incomplete removal of unincorporated dye terminators during cleanup, or contaminants in the DNA sample.- Solution: Ensure proper cleanup procedure (e.g., ensure sample is dispensed onto the center of spin columns, vortex thoroughly with BigDye XTerminator reagent). |
| Poor Data After a Mononucleotide Repeat [16] | Sequence trace becomes mixed and unreadable after a stretch of a single base (e.g., AAAAA). | - Cause: DNA polymerase slippage on the homopolymer stretch.- Solution: Design a new primer that binds just after the problematic region to sequence through it. |
Experimental Protocols for Robust Validation
Protocol 1: Sample Preparation and Submission for Sanger Sequencing
This protocol ensures the generation of high-quality template DNA for reliable sequencing results [29] [26].
- Amplicon Generation: Perform PCR using primers designed with online tools (e.g., NCBI Primer-BLAST, Primer3). The amplicon size should be appropriate for your sequencing instrument (typically up to 800-1000 bp).
- Verify Amplicon Purity: Analyze the PCR product by gel or capillary electrophoresis. A single, sharp band must be present. If multiple bands are seen, gel purification of the specific band of interest is required.
- Purify the Amplicon: Use a commercial bead-based or column-based PCR purification kit to remove excess salts, dNTPs, enzymes, and primers from the PCR reaction. This step is critical for a clean sequencing reaction.
- Quantify Accurately: Precisely measure the concentration of the purified DNA. Using a instrument like a NanoDrop is recommended for low-volume quantification. Ensure the A260 reading is between 0.1 and 0.8 for accuracy; dilute the sample if necessary [29].
- Submit with Correct Concentrations: Submit the DNA and primer at the recommended concentrations. General guidelines for template quantity per reaction are provided in the table below [28].
Table: Recommended Template Quantities for Sanger Sequencing
| DNA Template Type | Quantity per Reaction (non-BDX cleanup) | Quantity per Reaction (with BigDye XTerminator cleanup) |
|---|---|---|
| PCR Product: 100–500 bp | 3–10 ng | 1–10 ng |
| PCR Product: 500–1000 bp | 5–20 ng | 2–20 ng |
| Plasmid DNA | 150–300 ng | 50–300 ng |
| Bacterial Artificial Chromosome (BAC) | 0.5–1.0 μg | 0.2–1.0 μg |
Protocol 2: Validation of NGS-Derived Variants
This protocol outlines the steps for using Sanger sequencing to confirm a variant identified via NGS [27].
- Variant Review from NGS: Identify the variant (SNV or indel) and its genomic coordinates from your NGS analysis pipeline. Ensure it meets high-quality thresholds (e.g., PASS filter, depth ≥20x, variant fraction ≥20%).
- Primer Design: Design primers to amplify a 400-700 bp region surrounding the variant of interest.
- Follow best practices: primers should be 18-24 bases, have a Tm of 50-60°C, and GC content of 45-55% [30].
- Check for specificity using tools like UCSC In-Silico PCR.
- Check for common SNPs in the primer-binding site using a tool like SNPcheck to avoid allele-specific amplification failure.
- Wet-Lab Validation: Perform PCR and Sanger sequencing as outlined in Protocol 1, sequencing in both the forward and reverse directions for bidirectional confirmation.
- Data Analysis: Manually inspect the chromatogram in the region of the variant using a viewer like SnapGene or FinchTV. Confirm the presence of the expected base change in the sequencing trace. For heterozygous variants, look for two overlapping peaks at the variant position.
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Sanger Sequencing Validation
| Reagent | Function | Key Considerations |
|---|---|---|
| BigDye Terminator Kit [28] | The core chemistry for cycle sequencing. Contains fluorescently labeled ddNTPs, DNA polymerase, dNTPs, and buffer. | Store properly, protect from light, and check expiration dates. Includes control DNA (pGEM) for troubleshooting. |
| PCR Purification Kit [29] [26] | Removes unwanted components from PCR reactions (primers, enzymes, salts) to provide a clean template. | Bead-based or column-based. Critical for reducing background noise and failed reactions. |
| Hi-Di Formamide [28] | Used to resuspend the sequencing reaction product before capillary electrophoresis. Facilitates sample denaturation. | A standard component of the injection process. |
| BigDye XTerminator Kit [28] | Purification kit for removing unincorporated dye terminators and salts from sequencing reactions via a bead-based method. | Helps eliminate "dye blobs" and reduces salt artifacts. Vortexing is a critical step for success. |
| pGEM Control DNA & Primer [28] | Provided in the BigDye kit. Used as a positive control to determine if a failed reaction is due to template/primers or other issues. | Essential for systematic troubleshooting of failed runs. |
The Critical Role of Orthogonal Validation in Clinical and Research Settings
Orthogonal validation, the practice of confirming genetic variants using a method fundamentally different from the initial discovery technique, is a cornerstone of reliable clinical and research genomics. In the context of next-generation sequencing (NGS), this most often involves confirming variants with Sanger sequencing, the established gold standard for accuracy [31]. Despite the high throughput of NGS, the technique is not error-free; factors such as sequencing artifacts, alignment challenges in complex genomic regions, and bioinformatic filtering limitations can introduce false positives and false negatives [15] [31]. Orthogonal validation acts as a critical quality control step to ensure the accuracy of variants before they are reported, used in patient diagnosis, or inform therapeutic decisions, thereby upholding the highest standards of data integrity and patient safety [32].
The Necessity of Validation: Quantitative Evidence
The following table summarizes key findings from recent studies that have systematically evaluated the concordance between NGS and Sanger sequencing, providing a quantitative basis for validation practices.
| Study Focus / Panel Type | Cohort / Variant Size | Key Concordance Finding | Notes and Recommendations |
|---|---|---|---|
| Whole Genome Sequencing (WGS) [21] | 1,756 variants from 1,150 patients | 99.72% (5 discrepancies) | Sanger validation is crucial for variants with low-quality scores. |
| Exome Sequencing (ClinSeq Cohort) [20] | ~5,800 NGS-derived variants | >99.9% (19 initial discrepancies, 17 resolved for NGS) | A single Sanger round may incorrectly refute a true NGS variant. |
| Targeted Gene Panels (Illumina MiSeq/Haloplex) [15] | 945 variants from 218 patients | >99% (3 discrepancies, all resolved in favor of NGS) | Allelic dropout during Sanger sequencing can cause discrepancies. |
| Machine Learning for Sanger Bypass [33] | Model trained on GIAB benchmarks | 99.9% precision and 98% specificity achieved | ML models can reliably identify high-confidence SNVs, reducing confirmatory testing needs. |
These studies demonstrate that while the vast majority of high-quality NGS variants are confirmed, a small but critical number of discrepancies exist. Furthermore, evidence suggests that not all discrepancies are due to NGS errors, highlighting that Sanger sequencing, while a gold standard, is not itself infallible [15] [20].
Detailed Experimental Protocols
Protocol 1: Standard Sanger Validation of NGS-Detected Variants
This is a common workflow for confirming variants identified through targeted NGS panels or whole exome/genome sequencing [15] [31].
1. Variant Identification and Selection:
- Perform NGS using your established platform (e.g., Illumina MiSeq/NextSeq) and bioinformatic pipeline (e.g., BWA-MEM for alignment, GATK HaplotypeCaller for variant calling) [15].
- Filter variants based on quality metrics. Variants for validation are often selected according to criteria such as:
2. Primer Design:
- Design oligonucleotide primers that flank the target variant using tools like Primer3 [15].
- Critical Step: Check primer sequences against a single-nucleotide polymorphism (SNP) database to ensure no common variants interfere with primer binding, which can cause allelic dropout [15].
- Verify amplicon specificity using a tool like Primer-BLAST [15]. A typical amplicon size is 500-800 base pairs [20].
3. PCR Amplification and Purification:
- Set up a 25 µL PCR reaction using approximately 100 ng of genomic DNA, standard PCR buffers, dNTPs, and a robust DNA polymerase (e.g., FastStart Taq DNA Polymerase) [15].
- Purify the PCR products to remove excess primers and dNTPs using an enzymatic cleanup mixture (e.g., Exonuclease I and Alkaline Phosphatase) [15].
4. Sanger Sequencing and Capillary Electrophoresis:
- Perform the sequencing reaction using a chain-termination kit (e.g., BigDye Terminator v1.1 or v3.1) [20] [21].
- Purify the sequencing reactions to remove unincorporated dyes.
- Run the products on a capillary electrophoresis sequencer (e.g., ABI 3500Dx or 3730xl Genetic Analyzer) [15] [33].
5. Data Analysis:
- Analyze the resulting chromatograms using software such as GeneStudio Pro, Sequencher, or UGENE [33].
- Manually inspect the chromatogram for the variant position, assessing peak clarity, shape, and the absence of artifacts to confirm the NGS call [34] [20].
Protocol 2: Orthogonal NGS for High-Throughput Confirmation
For large-scale studies where Sanger validation of thousands of variants is impractical, an orthogonal NGS approach can be used [35].
1. Sample Preparation:
- Extract genomic DNA from patient samples (e.g., from whole blood).
2. Orthogonal Library Preparation and Sequencing:
- Prepare two independent NGS libraries for each sample using fundamentally different technologies:
- Sequence the libraries on different platforms with distinct chemistries (e.g., Illumina NextSeq with reversible terminators and Ion Proton with semiconductor sequencing) [35].
3. Data Integration and Analysis:
- Analyze data from each platform independently using their respective optimized bioinformatic pipelines.
- Use a custom algorithm or combinatorial tool to integrate variant calls from both platforms.
- Classify variants based on whether they are called by one or both platforms. Variants identified by both orthogonal methods have a significantly higher positive predictive value (PPV) and can be reported without Sanger confirmation, while those on only one platform are flagged for further review [35].
Orthogonal NGS Confirmation Workflow
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our lab is moving to whole genome sequencing (WGS). Are the standard quality thresholds for validating NGS variants still applicable?
A: WGS data, often with a lower mean coverage (~30-40x) than targeted panels, requires specific consideration. A 2025 study on WGS data suggests that while previously published thresholds (e.g., QUAL ≥ 100, DP ≥ 20, AF ≥ 0.2) work with 100% sensitivity (all false positives filtered out), their precision is low. For WGS, the study recommends:
- Caller-agnostic thresholds: DP ≥ 15 and AF ≥ 0.25 to achieve high precision while maintaining sensitivity [21].
- Caller-specific threshold: Using a QUAL ≥ 100 (for GATK HaplotypeCaller) alone can drastically reduce the need for Sanger validation, filtering out ~98% of variants into a "high-quality" bin [21]. Each laboratory should validate thresholds for their specific WGS pipeline.
Q2: I am getting a discrepancy between NGS and Sanger sequencing, where the NGS data shows a heterozygous variant but Sanger appears homozygous wild-type. What is the most likely cause?
A: This is a classic symptom of Allelic Dropout (ADO) during the Sanger sequencing process. This occurs when one allele fails to amplify in the initial PCR step, often due to:
- A private SNP in the primer-binding site: A genetic variant present in your sample (but not in the reference genome) prevents one of the primers from annealing correctly [15].
- Solution: Redesign your PCR primers, shifting them further away from the variant location, and re-run the Sanger validation. Always check primers against SNP databases during the design phase [15].
Q3: When looking at my Sanger chromatogram, what are the key indicators of a high-quality, reliable result?
A: A high-quality chromatogram will have:
- Low and flat baseline between peaks, indicating minimal background noise [34].
- Sharp, single, and symmetrical peaks for each base call [34].
- Even spacing between consecutive peaks, which reflects uniform DNA fragment migration [34]. Be wary of broad or overlapping peaks (compressions), double peaks (potential heterozygosity or polymerase stuttering), and "dye blobs" (large, misshapen peaks caused by unincorporated dye) [34].
Q4: Is orthogonal validation still necessary for all NGS variants, given the improving technology?
A: The field is evolving. Best practices are shifting from blanket Sanger validation for all variants to a more nuanced, risk-based approach.
- For high-quality variants: Recent guidelines suggest that "high-quality" NGS variants meeting strict, lab-validated thresholds for depth, allele frequency, and quality scores may not require Sanger confirmation [20] [21].
- For borderline or clinically critical variants: Orthogonal validation remains essential for variants with low-quality scores, those in difficult-to-sequence regions (e.g., high GC-content, homopolymers), and those with major clinical implications [15] [32].
- Emerging approaches: Machine learning models are now being trained to automatically classify single nucleotide variants (SNVs) as high or low-confidence, significantly reducing the burden of orthogonal confirmation while maintaining >99.9% precision [33].
Modern Variant Validation Decision Tree
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials required for the orthogonal validation workflows described.
| Reagent / Material | Function / Application | Example Products / Kits |
|---|---|---|
| DNA Polymerase (Robust) | PCR amplification of target regions from genomic DNA prior to Sanger sequencing. | FastStart Taq DNA Polymerase Kit [15] |
| Exonuclease I / Alkaline Phosphatase | Enzymatic cleanup of PCR products to degrade excess primers and dNTPs that would interfere with the Sanger sequencing reaction. | ExoStar Cleanup Mix [15] |
| Cycle Sequencing Kit | Contains fluorescently labeled dideoxynucleotides (ddNTPs) and DNA polymerase for the chain-termination sequencing reaction. | BigDye Terminator v3.1 Cycle Sequencing Kit [20] [21] |
| Capillary Electrophoresis Sequencer | Instrument for separating sequencing fragments by size and detecting fluorescent signals to generate the chromatogram. | Applied Biosystems 3500xL or 3730xl Genetic Analyzer [15] [33] |
| Hybridization-Based Capture Kit | For target enrichment in orthogonal NGS workflows; uses biotinylated probes to capture genomic regions of interest. | Agilent SureSelect Clinical Research Exome (CRE) [35] |
| Amplification-Based Capture Kit | For orthogonal target enrichment; uses a multiplex PCR approach to amplify target regions. | Ion AmpliSeq Exome Kit [35] |
| Primer Design Software | Critical for designing specific primers for Sanger validation that avoid known SNPs. | Primer3 [15], Primer3Plus [33] |
From Data to Validation: Implementing Robust Workflows for Mutant Allele Confirmation
Establishing a Best-Practice NGS-to-Sanger Validation Pipeline
Next-generation sequencing (NGS) has revolutionized genomic analysis in research and clinical diagnostics, enabling the simultaneous detection of millions of variants. However, the establishment of a robust validation pipeline remains crucial for ensuring data accuracy, particularly for variant confirmation. Sanger sequencing, often termed the "gold standard" for DNA sequencing, continues to play a vital role in orthogonal validation of NGS-derived variants, especially in contexts where definitive proof is required for clinical decision-making or publication [36] [37]. This technical resource center provides comprehensive guidance for establishing an efficient NGS-to-Sanger validation workflow, complete with troubleshooting guides and frequently asked questions to address common experimental challenges.
The necessity for Sanger validation stems from various potential sources of error in NGS workflows, including those introduced during library preparation, sequencing, or bioinformatic analysis [38]. Factors such as low read depth, sequencing errors in GC-rich regions, and alignment difficulties can generate false positive or false negative results [38]. While recent evidence suggests that high-quality NGS variants demonstrate exceptionally high validation rates (exceeding 99.9%), confirmation remains particularly important for variants with borderline quality metrics or those with significant clinical implications [20] [21].
Establishing Validation Guidelines: When is Sanger Confirmation Necessary?
Quality Thresholds for High-Confidence NGS Variants
Recent large-scale studies have established that variants meeting specific quality thresholds may not require routine Sanger validation, potentially saving significant time and resources. The following table summarizes evidence-based quality metrics for identifying high-confidence NGS variants:
Table 1: Evidence-Based Quality Thresholds for NGS Variant Validation
| Study | Sequencing Type | Sample Size | Concordance Rate | Recommended Quality Thresholds |
|---|---|---|---|---|
| ClinSeq Study [20] | Exome Sequencing | 5,800+ variants | 99.965% | MPG score ≥10 |
| WGS Validation [21] | Whole Genome Sequencing | 1,756 variants | 99.72% | FILTER=PASS, QUAL≥100, DP≥15, AF≥0.25 |
| Multi-Center Analysis [38] | Targeted Gene Panels | 945 variants | >99% | Depth≥30×, Phred Q≥30, Allele Balance>0.2 |
Based on this accumulated evidence, a practical validation pipeline can be established that prioritizes Sanger confirmation for variants failing to meet these quality thresholds, while potentially exempting high-quality variants from additional validation.
Decision Framework for Sanger Validation
The following workflow diagram provides a visual guide for determining when Sanger validation is necessary based on variant characteristics and quality metrics:
Essential Research Reagents and Materials
Successful Sanger validation requires careful selection of laboratory reagents and materials. The following table outlines key components for establishing a reliable validation workflow:
Table 2: Essential Research Reagents for NGS-to-Sanger Validation
| Reagent/Material | Function | Specifications & Quality Controls |
|---|---|---|
| PCR Primers [30] [38] | Amplification of target regions for Sanger sequencing | 18-24 bases; Tm 50-60°C; GC content 45-55%; Check for SNPs in binding sites |
| DNA Polymerase [38] | PCR amplification of target regions | High-fidelity enzymes; validated for genomic DNA |
| BigDye Terminators [20] [38] | Fluorescent dideoxy terminator sequencing | Kit version 1.1 or 3.1; proper storage conditions |
| Purification Systems [30] [7] | Cleanup of PCR products and sequencing reactions | Ethanol precipitation, column-based, or bead-based systems |
| Size Selection Beads [7] | Removal of primer dimers and nonspecific products | SPRl, AMPure, or similar; fresh ethanol washes |
| Capillary Electrophoresis Polymers [36] | Matrix for fragment separation in sequencers | Performance-optimized polymers for sequence resolution |
Troubleshooting Common Experimental Issues
Failed or Poor-Quality Sanger Sequencing
Problem: Sequencing reactions produce poor-quality chromatograms or fail entirely.
Solutions:
- Primer Design Issues: Verify primers are 18-24 bases with 45-55% GC content and melting temperature of 56-60°C [30] [39]. Avoid primers with secondary structures or self-complementarity.
- Template Contamination: Check for contaminants by assessing 260/230 ratios (<1.6 suggests organic contaminants) and ensure elution buffers do not contain EDTA [30].
- Template Quality: Assess DNA purity via spectrophotometry (260/280 ratio ~1.8) and quantify using fluorometric methods rather than UV absorbance alone [39] [7].
- Difficult Templates: For GC-rich regions or templates with secondary structures, use specialized protocols or additives (e.g., DMSO, betaine) to improve sequencing through problematic regions [30] [39].
Discrepancies Between NGS and Sanger Results
Problem: Variants identified by NGS are not confirmed by Sanger sequencing.
Solutions:
- Investigate Allelic Dropout (ADO): ADO during PCR amplification can cause false negatives in Sanger sequencing, particularly if polymorphisms occur in primer-binding sites [38]. Redesign primers to bind to alternative regions.
- Verify NGS Quality Metrics: Check that the NGS variant meets established quality thresholds (depth, quality scores, allele frequency) before pursuing validation [21].
- Review Sanger Experimental Conditions: Optimize PCR conditions and consider repeating Sanger sequencing with newly designed primers before concluding the NGS result is a false positive [20] [38].
Low NGS Library Yield
Problem: Inadequate library quantity for sequencing, potentially affecting variant calling.
Solutions:
- Input DNA Quality: Re-purify input DNA if contaminants are suspected (residual phenol, salts, EDTA) and verify purity ratios (260/230 > 1.8, 260/280 ~1.8) [7].
- Quantification Accuracy: Use fluorometric quantification (Qubit, PicoGreen) rather than UV spectrophotometry alone, as the latter may overestimate usable DNA [7].
- Adapter Ligation Efficiency: Titrate adapter-to-insert molar ratios and ensure fresh ligase and optimal reaction conditions (temperature, buffer) [7].
Frequently Asked Questions (FAQs)
Q1: Is Sanger validation still necessary for all NGS-derived variants in clinical diagnostics?
A: Not necessarily. Recent evidence demonstrates that NGS variants meeting established quality thresholds (e.g., depth ≥15×, allele frequency ≥0.25, quality score ≥100) show >99.9% concordance with Sanger sequencing [20] [21]. Many laboratories are implementing policies that exempt high-quality variants from mandatory Sanger confirmation, particularly for research applications. Clinical applications may maintain stricter requirements, especially for variants with significant medical implications.
Q2: What are the most critical factors in designing primers for Sanger validation?
A: Optimal primer characteristics include: length of 18-24 bases, melting temperature between 56-60°C, GC content of 45-55%, and a G or C base at the 3' end [30] [39]. Crucially, primers should be designed to avoid known polymorphisms in binding sites and should be tested for specificity using tools like Primer-BLAST [38].
Q3: How can I troubleshoot a specific variant that fails Sanger validation despite good NGS quality metrics?
A: First, repeat the Sanger sequencing with newly designed primers to exclude allelic dropout due to polymorphisms in primer binding sites [38]. Second, verify that the variant does not reside in a region with technical challenges (high GC content, repetitive elements). Third, if possible, confirm using an alternative method such as a different NGS approach or digital PCR [21].
Q4: What are the key differences between Sanger sequencing and NGS that justify using both methods?
A: Sanger sequencing provides long, contiguous reads (500-1000 bp) with very high per-base accuracy (Q50, or 99.999%) but limited throughput [36]. NGS generates millions of shorter reads (50-300 bp) with slightly lower per-read accuracy, but achieves high overall accuracy through deep coverage [36]. The combination leverages NGS's comprehensive screening capability with Sanger's precision for specific variant confirmation.
Q5: What specific quality metrics should I examine for NGS variants prior to Sanger validation?
A: Key metrics include: depth of coverage (DP ≥15), variant quality score (QUAL ≥100), allele frequency (AF ≥0.25 for heterozygous calls), and FILTER status (PASS) [21]. Additionally, visual inspection of aligned reads using a genome browser can identify alignment issues or strand bias that might indicate false positives.
As NGS technologies continue to mature, the requirements for orthogonal Sanger validation are evolving. The current evidence supports a balanced approach that utilizes quality thresholds to identify high-confidence variants that may not require confirmation, while maintaining Sanger sequencing for borderline cases or clinically impactful findings. By implementing the troubleshooting guides, reagent specifications, and quality thresholds outlined in this technical resource, researchers and clinicians can establish efficient, cost-effective validation pipelines that maintain rigorous standards for variant verification.
Primer Design Strategies for Amplifying and Sequencing Target Mutations
Core Design Parameters for Effective Primers
Adhering to established parameters for primer design is fundamental for successful amplification and sequencing of target mutations. The following table summarizes the key quantitative criteria to guide your primer design process.
| Parameter | Optimal Range | Importance & Rationale |
|---|---|---|
| Primer Length | 17–25 nucleotides [40], ideally 18–24 bases [41] [39] | Balances specificity (long enough) with binding efficiency (not too long). |
| GC Content | 40%–60% [42], ideally 45%–55% [39] or ~50% [41] [40] | Ensures stable primer-template binding; extremes can cause instability or non-specific binding. |
| Melting Temperature (Tm) | 50–70°C [40], ideally 55–65°C [40] or 56–60°C [39] | Critical for setting the correct annealing temperature; primers in a pair should be within 2°C of each other [42]. |
| GC Clamp | 1-2 G/C bases at the 3' end; avoid >3 G/C in the last 5 bases [42] | Stabilizes binding at the 3' end where polymerase initiation occurs, but too many can promote mispriming. |
| Avoid | Poly-base regions, dinucleotide repeats, self-complementary sequences [41] [42] | Prevents mispriming, slippage, and the formation of secondary structures like hairpins and primer-dimers. |
Workflow for Primer Design and Validation
A systematic approach to primer design, from target definition to in silico validation, ensures the highest chance of experimental success. The workflow below outlines this process.
Step-by-Step Protocol
- Define Your Target Region: Select the exact genomic or cDNA interval you wish to sequence. Obtain the reference sequence from a curated database like NCBI RefSeq or Ensembl using a FASTA format or accession number. Decide on primer flanking boundaries so that the primers bind outside the variant or region of interest [42].
- Use Primer Design Tools: Utilize online tools like NCBI Primer-BLAST, which integrates the design engine of Primer3 with specificity checking via BLAST [42]. In the interface, input your target sequence and set constraints such as:
- Product size range: For Sanger sequencing, ensure your PCR product is at least 200 bp, with 500 bp or more being ideal [39].
- Tm limits and maximum Tm difference (e.g., ≤2°C).
- Organism specificity to limit off-target priming [43] [42].
- Exon/intron constraints if designing for cDNA vs. genomic templates [43].
- Evaluate and Filter Candidate Primers: For each suggested primer pair from the tool, check that their GC% and Tm fall within the optimal design criteria. Screen for secondary structures and primer-dimer formation using thermodynamic tools (e.g., OligoAnalyzer). Prefer primer pairs that show minimal off-target matches in the Primer-BLAST specificity report [42].
- In Silico Validation and Final Selection: Simulate amplicons using in silico PCR tools (e.g., UCSC in silico PCR) to confirm the expected product size and the absence of spurious products. Record the final primer sequences, Tm, GC%, amplicon size, and expected specificity [42].
Troubleshooting Common Primer Design Issues
Why is my sequencing result poor or blank?
- Problem: Insufficient primer binding to the template.
- Solution: Verify that your primer is designed with a Tm of 56–60°C and a GC content of 45–55% [39]. Ensure the primer matches the template exactly, especially in the last 8 bases at the 3' end [40]. Avoid primers that can form hairpin loops or primer-dimers [42] [40].
How do I prevent non-specific amplification or multiple bands?
- Problem: Primer binds to off-target sites.
- Solution: Always use Primer-BLAST to check primer specificity against the target organism's genome [43] [42]. Increase the stringency of the annealing temperature (Ta) by 2–5°C [42]. Avoid placing primers in repetitive or homologous sequence regions [42].
What causes primer-dimer formation and how can I avoid it?
- Problem: Primers anneal to themselves or each other.
- Solution: Redesign primers to avoid complementarity, especially at the 3' ends. Use analysis tools to screen for dimer formation and eliminate primers with strong predicted binding (ΔG values that are too negative) [42]. For highly multiplexed PCR, advanced algorithms like SADDLE can be used to minimize dimer formation across large primer sets [44].
Why is the signal weak or the coverage uneven in my NGS data?
- Problem: Imbalanced primer efficiency or overamplification.
- Solution: For multiplex PCR panels, ensure all primers in the set have closely matched Tm values to ensure uniform amplification [42]. Avoid an excessive number of PCR cycles, which can introduce size bias and increase duplicate rates [7]. Verify the quantity and quality of the input library [8].
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Tool | Function in Experiment |
|---|---|
| NCBI Primer-BLAST | A free online tool that designs primer pairs and checks their specificity against a selected database to ensure they only amplify the intended target [43] [42]. |
| Betaine | An additive used in Sanger sequencing reactions to lower the Tm and anneal temperature of the primer, helping to sequence through templates with high GC content or secondary structures [40] [39]. |
| DMSO | A stabilizer added to PCR reactions to improve the amplification of GC-rich regions or complex templates by reducing secondary structure formation [42]. |
| Thermostable DNA Polymerase | Enzyme that catalyzes the template-dependent synthesis of DNA during PCR and sequencing; essential for cycle sequencing in Sanger methods [13]. |
| SADDLE Algorithm | A computational framework (Simulated Annealing Design using Dimer Likelihood Estimation) for designing highly multiplexed PCR primer sets that minimize primer-dimer formation [44]. |
Frequently Asked Questions (FAQs)
Q1: Why is orthogonal validation with Sanger sequencing still necessary for NGS-identified variants?
While NGS technologies can identify millions of variants simultaneously, validation remains crucial for confirming potentially causative mutations before reporting. Sanger sequencing provides an orthogonal method with exceptionally high accuracy at the single-base level, serving as the "gold standard" for verifying variants detected through NGS pipelines. This is particularly important for clinical reporting and research validation, as NGS platforms can produce false positives due to sequencing artifacts, alignment errors, or amplification biases. Current guidelines recommend that each laboratory establish a confirmatory testing policy for variants, with Sanger sequencing being the most widely accepted method for this purpose [21] [32].
Q2: What are the key quality thresholds for determining which NGS variants require Sanger validation?
Research indicates that establishing quality thresholds can significantly reduce the number of variants requiring validation. Based on recent studies of 1756 WGS variants, the following thresholds effectively separate high-quality variants from those needing confirmation [21]:
Table: Quality Thresholds for NGS Variant Validation
| Parameter Type | Parameter | Recommended Threshold | Precision Achieved |
|---|---|---|---|
| Caller-Agnostic | Depth (DP) | ≥15 | 6.0% |
| Caller-Agnostic | Allele Frequency (AF) | ≥0.25 | 6.0% |
| Caller-Dependent | Quality (QUAL) | ≥100 | 1.2% |
Implementing these thresholds can reduce Sanger validation to just 1.2-6.0% of the initial variant set, significantly saving time and resources while maintaining accuracy [21].
Q3: What are the optimal primer design parameters for Sanger sequencing validation?
Proper primer design is critical for successful Sanger sequencing. Follow these evidence-based guidelines [45]:
- Length: 18-30 bases
- Melting Temperature (Tm): 60-64°C (ideal 62°C)
- Tm Difference Between Primers: ≤2°C
- GC Content: 35-65% (ideal 50%)
- Amplicon Length: 70-150 bp for optimal amplification (up to 500 bp possible)
- Avoid: Regions of 4 or more consecutive G residues
- Specificity: Verify uniqueness to target sequence using BLAST analysis
Q4: How do I troubleshoot failed Sanger sequencing reactions?
Failed reactions can result from multiple factors. Consider these troubleshooting steps:
- Check Primer Quality: Ensure primers are properly purified, dissolved, and stored. Verify secondary structures using tools like OligoAnalyzer (ΔG > -9.0 kcal/mol) [45].
- Optimize Template Quality: Assess DNA purity (A260/280 ratio ~1.8-2.0) and quantity. Avoid degraded or inhibitor-contaminated samples.
- Validate Thermal Cycler Conditions: Confirm annealing temperature is set 5°C below primer Tm. Verify extension times are sufficient for amplicon length.
- Review Sequencing Chemistry: Ensure proper BigDye terminator ratios and cycling conditions. Verify capillary electrophoresis injection parameters.
- Inspect Electroherogram: Poor signal may indicate low template concentration, while multiple peaks may suggest primer dimer formation or contamination.
Q5: When should Sanger sequencing not be used for NGS validation?
Sanger sequencing has limitations in certain scenarios [46]:
- Low Variant Allele Frequency (VAF): Sanger detection sensitivity is limited to approximately 10-20% VAF, making it unsuitable for validating low-frequency somatic mutations in heterogeneous tumor samples.
- Large-Scale Validation: When dealing with hundreds of variants, Sanger sequencing becomes impractical due to throughput limitations and cost.
- Complex Structural Variants: Large insertions, deletions, or rearrangements may be challenging to validate with Sanger sequencing alone.
- Routine Clinical NGS: For well-validated NGS pipelines with established quality metrics, some laboratories are moving toward eliminating orthogonal validation for high-quality variants.
Technical Troubleshooting Guides
Issue: Poor Sequence Quality in Sanger Validation
Symptoms: Low signal-to-noise ratio, high background, unreadable sequences.
Solution Protocol:
Template Quality Control
- Quantify DNA using fluorometric methods (e.g., Qubit) for accuracy
- Verify DNA integrity via gel electrophoresis
- Perform PCR optimization with template dilution series (1-100 ng)
Primer Re-design and Validation
- Re-design primers following optimal parameters above
- Include positive control primers for known working amplicons
- Verify primer specificity using in silico PCR tools
Sequencing Reaction Optimization
- Prepare fresh BigDye terminator mixtures
- Optimize primer concentration (0.5-3.2 μM range)
- Test different thermal cycling conditions:
- 96°C for 1 minute (initial denaturation)
- 25-30 cycles of: 96°C for 10s, 50°C for 5s, 60°C for 4 minutes
- Hold at 4°C
Purification Improvement
- Implement ethanol/sodium acetate precipitation for cleaner results
- Consider alternative purification methods (column-based, magnetic beads)
- Ensure complete removal of unincorporated dyes
Issue: Discordant Results Between NGS and Sanger Sequencing
Symptoms: Variant detected by NGS but not confirmed by Sanger, or vice versa.
Solution Protocol:
Verify NGS Variant Quality Metrics
- Check variant allele frequency (VAF) in NGS data
- Review read alignment around variant position for artifacts
- Confirm strand bias metrics are within acceptable ranges
- Verify quality scores (Q≥20 for bases, QUAL≥100 for variants)
Investigate Technical Artifacts
- Check for homopolymer regions near variant that may cause alignment issues
- Verify amplicon design doesn't overlap problematic genomic regions
- Confirm primer binding sites don't contain polymorphisms
Experimental Verification
- Repeat Sanger sequencing with independent PCR amplification
- Design alternative primers targeting the same variant
- Consider bidirectional sequencing for confirmation
- Validate with alternative method (e.g., pyrosequencing, digital PCR) if available
Biological Explanation Assessment
- Evaluate potential sample mix-up or contamination
- Consider tumor heterogeneity affecting variant detection
- Assess clonal evolution between sample collection times
Issue: Primer Design Challenges for Difficult Genomic Regions
Symptoms: Repeated primer failure in GC-rich, repetitive, or complex genomic regions.
Solution Protocol:
Advanced Primer Design Strategies
- Incorporate locked nucleic acids (LNAs) for GC-rich regions
- Use touchdown PCR protocols with graduated annealing temperatures
- Design primers spanning exon-exon junctions to avoid genomic DNA amplification
- Consider long-range PCR with internal sequencing primers
Alternative Amplification Approaches
- Implement PCR additives:
- DMSO (1-10%)
- Betaine (0.5-2M)
- Formamide (1-5%)
- GC-rich specific buffers
- Optimize magnesium concentration (1.5-4.0 mM range)
- Test different polymerase enzymes with higher processivity
- Implement PCR additives:
Template Modification
- Use genome-wide amplification for limited template
- Implement nested PCR approaches for low-complexity regions
- Consider fragmentation and subcloning for extremely problematic regions
Research Reagent Solutions
Table: Essential Materials for Sanger Validation Workflow
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Polymerase Enzymes | High-fidelity DNA polymerase (e.g., Phusion, Q5) | PCR amplification with proofreading activity; reduces amplification errors |
| Sequencing Chemistry | BigDye Terminator v3.1 | Chain-termination sequencing with fluorescent ddNTPs; standard for capillary electrophoresis |
| Purification Methods | Ethanol precipitation, column purification, magnetic beads | Remove unincorporated dyes, salts, and primers before sequencing |
| Capillary Arrays | POP-7 polymer, 50cm arrays | Matrix for fragment separation by size in automated sequencers |
| Quality Control Tools | Bioanalyzer, TapeStation, Qubit fluorometer | Assess DNA quality, quantity, and fragment size distribution |
| Primer Design Software | Primer3, OligoAnalyzer, NCBI Primer-BLAST | In silico primer design, validation, and specificity checking |
| Sequence Analysis Tools | Sequencing Analysis Software, 4Peaks, Geneious | Base calling, sequence alignment, and variant identification |
Workflow Integration Diagrams
Advanced Integration Protocols
Protocol: High-Throughput Validation for Large Variant Sets
For studies involving numerous variants, implement this efficient workflow:
Multiplex Primer Design
- Design primers with similar Tm (60±2°C)
- Incorporate unique tags for sample multiplexing
- Verify no cross-homology between multiplexed assays
96-Well Plate Setup
- Standardize reaction volumes and concentrations
- Implement robotic liquid handling for reproducibility
- Include controls in each plate (positive, negative, no-template)
Capillary Electrophoresis Optimization
- Utilize 96-capillary instruments for high throughput
- Implement rapid run protocols (1-2 hours)
- Use polymer formulations allowing rapid separation
Automated Data Analysis
- Implement batch processing of sequence files
- Use quality score thresholds for automatic pass/fail
- Generate consolidated reports for all validated variants
Protocol: Low-Frequency Variant Validation
For variants with VAF below Sanger's detection limit:
Enrichment Strategies
- Implement peptide nucleic acid (PNA) clamping
- Use co-amplification at lower denaturation temperature PCR (COLD-PCR)
- Consider digital PCR for absolute quantification
Sensitivity Enhancement
- Increase input DNA amount (up to 100ng)
- Optimize PCR cycles (30-35 cycles maximum)
- Implement nested PCR approaches
Alternative Validation Methods
- Pyrosequencing for quantitative results
- MassARRAY for multiplexed validation
- ddPCR for precise allele frequency determination
The Sanger-NGS Validation Paradigm: Is Orthogonal Confirmation Always Necessary?
The Evolving Standard of Care
A significant shift is occurring in molecular diagnostics regarding the need to validate next-generation sequencing (NGS) findings with Sanger sequencing. While traditionally considered the "gold standard," Sanger sequencing adds considerable time and cost to clinical reporting [47]. Emerging evidence from large-scale studies suggests that for high-quality NGS variants, orthogonal Sanger confirmation may have limited utility [20].
Quantitative Evidence from Large-Scale Studies
Recent studies involving thousands of variants demonstrate exceptionally high concordance between NGS and Sanger sequencing:
Table 1: Concordance Rates Between NGS and Sanger Sequencing in Major Studies
| Study Scope | Sample Size | Number of Variants | Concordance Rate | Key Findings |
|---|---|---|---|---|
| Clinical Exomes [47] | 825 exomes | 1,109 variants | 100% | All high-quality SNVs and indels were confirmed; Sanger useful for quality control but not essential for verification |
| ClinSeq Cohort [20] | 684 exomes | ~5,800 variants | 99.965% | Single-round Sanger sequencing more likely to incorrectly refute true positive NGS variants than identify false positives |
| Whole Genome Sequencing [21] | 1,150 WGS | 1,756 variants | 99.72% | Caller-agnostic thresholds (DP≥15, AF≥0.25) effectively identified variants needing validation |
Decision Framework for Sanger Validation
Laboratories can establish quality thresholds to determine when Sanger validation is necessary:
NGS Validation Protocol: Establishing Laboratory Confidence
Sample Preparation and Sequencing
For reliable NGS validation, follow this detailed experimental workflow:
DNA Isolation and Sample Enrichment
- Extract genomic DNA from appropriate sources (peripheral blood, saliva, or tissue) using standard extraction systems [5]
- Amplify coding regions and at least 20 bp of flanking intronic sequence using custom-designed primers
- Use PCR conditions: initial denaturation at 95°C for 3 minutes, followed by 10 cycles of step-down annealing, then 25 cycles with annealing at 55°C [5]
- Visualize PCR products on 2% agarose gel and purify using appropriate purification systems
Library Preparation and Sequencing
- Pool enriched amplicons in equimolar amounts after quantitation in triplicate
- Perform end-repair and concatenation of pooled samples
- Shear concatenated sample to 150-180 bp fragments
- Ligate sequencing adaptors with unique barcodes for sample multiplexing
- Quantify final library and perform emulsion PCR for template amplification
- Sequence using appropriate NGS platform parameters (e.g., 50-bp barcoded fragment sequencing) [5]
Data Analysis and Variant Calling
Bioinformatics Processing
- Align raw sequencing data against reference sequences using appropriate alignment tools
- Perform variant calling using established algorithms for SNP detection and small/large indel calling
- Run multiple cycles of condensation to ensure comprehensive variant detection [5]
Quality Metrics Establishment
- Define high-quality variants as: FILTER=PASS, QUAL≥100, depth coverage≥20x, variant fraction≥20% [47]
- Manually visualize putative variants using genome browser tools
- Classify variants according to ACMG standards: pathogenic, likely pathogenic, uncertain significance, likely benign, benign [48]
Troubleshooting Guide: NGS and Sanger Sequencing Challenges
Common Sanger Sequencing Issues and Solutions
Table 2: Sanger Sequencing Troubleshooting Guide
| Problem | Identification | Possible Causes | Solutions |
|---|---|---|---|
| Failed Reactions | Messy trace with no discernable peaks; mostly N's in data | Low template concentration; poor quality DNA; too much DNA; bad primer | Ensure template concentration 100-200 ng/μL; verify DNA quality (260/280 ≥1.8); check primer quality and binding site [16] |
| Secondary Structure | Good quality data that suddenly terminates | Hairpin structures; long stretches of G/C residues | Use alternate dye chemistry for difficult templates; design primers sitting on or avoiding secondary structure regions [16] |
| Mixed Sequences | Double peaks from beginning of trace | Multiple templates; colony contamination; multiple priming sites | Ensure single colony pickup; verify single priming site per template; purify PCR reactions properly [16] |
| Primer Dimers | Sequence starts noisy then improves downstream | Primer self-hybridization due to complementary bases | Analyze primer with design tools; avoid complementary regions in primer [16] |
NGS-Specific Challenges in Clinical Settings
Addressing Incidental Findings NGS multi-gene panel testing can uncover unexpected, non-germline incidental findings indicative of mosaicism, clonal hematopoiesis, or hematologic malignancies [49]. These findings require specific interpretation frameworks:
- Low allele fractions (<30%) may indicate mosaicism or clonal hematopoiesis rather than germline variants
- Multiple pathogenic variants in the same patient warrant secondary tissue analysis
- Variants inconsistent with family history require additional investigation
Secondary Tissue Analysis Workflow
- Perform skin biopsy with direct and cultured fibroblast analysis
- Compare allele fractions across different tissues
- Review complete blood counts and medical history for hematologic disorders
- Classify findings as germline, mosaic, clonal hematopoiesis, or hematologic malignancy [49]
Research Reagent Solutions: Essential Materials for Validation Studies
Table 3: Key Research Reagents for Sanger and NGS Validation
| Reagent Category | Specific Products | Function/Application |
|---|---|---|
| DNA Extraction | Puregene DNA Extraction System (Qiagen); DNA Genotek saliva collection | High-quality DNA isolation from blood or saliva for reliable sequencing results [5] |
| PCR Amplification | FastStart Taq PCR System (Roche); Platinum Taq PCR System | Robust amplification of target regions with high fidelity and yield [5] |
| Library Preparation | SOLiD Fragment Library Oligo Kit; Millipore MultiScreen PCR UF plates | Efficient end-repair, adaptor ligation, and purification for NGS library construction [5] |
| Sequencing Kits | SOLiD ePCR Kit; BigDye Sequencing Kits | Template amplification and fluorescent dye termination for Sanger sequencing [5] [20] |
| Bioinformatics Tools | NextGENe (SoftGenetics); Burrows-Wheeler Alignment; GATK | Data analysis, alignment, variant calling, and visualization for NGS data interpretation [5] |
| Validation Primers | Custom-designed primers; PrimerTile automated design | Target-specific amplification for Sanger confirmation of NGS variants [20] |
Advanced Considerations in Validation Strategies
Specialized Applications in Oncology
In hereditary cancer testing, NGS multi-gene panels have demonstrated particular utility beyond traditional BRCA1/2 testing [48]. These panels identify additional individuals with hereditary cancer susceptibility who would have been missed by single-gene testing approaches. Key considerations include:
- Gene Selection: Panels should include established high-penetrance genes and emerging cancer susceptibility genes
- Variant Interpretation: Laboratory-specific expertise in variant classification is essential, particularly for genes with less established risk profiles
- Pre-test Counseling: Patients should be informed about the potential for variants of uncertain significance and incidental findings
Technological Comparison and Workflow Integration
Quality Assurance and Laboratory Standards
For clinical implementation, laboratories must establish rigorous quality metrics:
- Analytical Validation: Demonstrate >99% sensitivity, specificity, and accuracy through validation studies [48]
- Depth of Coverage: Establish minimum coverage between 20-50x for targeted inherited cancer panels [48]
- Proficiency Testing: Participate in external quality assurance programs
- Data Sharing: Contribute to public databases such as ClinVar to improve variant classification [48]
The evidence supports a nuanced approach to NGS validation. For high-quality variants meeting established thresholds, Sanger confirmation may be unnecessary. However, Sanger sequencing remains valuable for troubleshooting low-quality variants, resolving complex regions, and validating potentially false-positive calls. Each laboratory should establish and validate their own quality thresholds based on their specific NGS methodologies and clinical applications.
In the era of next-generation sequencing (NGS), the validation of mutant alleles remains a critical step in genetic research and diagnostic pipelines. While NGS provides unparalleled breadth for variant discovery, Sanger sequencing is often employed for its robustness and accuracy in confirming findings. The challenge, however, lies in detecting low-frequency somatic variants that fall near the traditional detection limit of conventional Sanger analysis. Minor Variant Finder (MVF) Software represents a significant advancement in the Sanger sequencing toolbox, enabling researchers to reliably detect minor alleles at frequencies as low as 5% [50]. This technical support center provides troubleshooting guides and FAQs to help researchers and drug development professionals effectively integrate this specialized software into their workflows for validating mutant alleles.
What is Minor Variant Finder Software?
Minor Variant Finder Software is an analytical tool developed for the detection and reporting of minor variants from Sanger sequencing data. Minor variants are single nucleotide polymorphisms (SNPs) present as a minor component with a contribution of less than 25% at a given allele. The software's innovative algorithm neutralizes background noise using a control sample, enabling calling of minor variants at a detection level as low as 5% [50]. This makes it particularly valuable in oncology, infectious disease, and inherited disease research, where detecting low-frequency somatic mutations is critical.
System Requirements and Compatibility
Before installation, ensure your computing environment meets these minimum requirements:
Table 1: Computer System Requirements for Minor Variant Finder Software
| Component | Requirements |
|---|---|
| Computer | Windows computer with 2 GB hard disk space and minimum 4 GB memory (8 GB recommended) |
| Operating System | Windows 7 SP1 (32-bit or 64-bit) or Windows 10 Pro/IoT (64-bit) |
| Browser | Google Chrome, Mozilla Firefox, Microsoft Internet Explorer v.11, or Microsoft Edge |
| Screen Resolution | 1024 x 768 or higher (optimized for 1280 x 1024) |
| Instrument Compatibility | Applied Biosystems SeqStudio, 3500, 3130, and 3730 genetic analyzers (3100 models supported with specific basecaller) |
| Basecaller | Requires .ab1 files basecalled with KB Basecaller v1.4 or later [50] |
The software runs in a web browser window but does not require an internet connection for operation, ensuring data security on your desktop computer [50].
Experimental Protocols and Workflows
Standard Operating Procedure for Minor Variant Detection
Principle: The MVF software detects low-frequency variants by comparing test samples to control samples to neutralize background noise, followed by analysis of clean electropherograms for visual confirmation [50].
Materials and Equipment:
- Control sample (wild-type)
- Test samples
- Same primers for control and test samples
- Identical sample clean-up methods
- Compatible genetic analyzer
- Minor Variant Finder Software
Procedure:
- Sample Preparation and Sequencing:
- Prepare and sequence control and test samples using identical materials and procedures (same primers, same sample clean-up method, same instrument) [50].
- Ensure template DNA concentration is between 100-200 ng/μL for optimal sequencing results [16].
- Verify DNA quality with 260/280 OD ratio of 1.8 or greater to avoid contaminants that hinder sequencing [16].
Software Setup:
- Create a new project in Minor Variant Finder Software.
- Input the control forward and reverse reactions, followed by the forward and reverse reactions of the test samples [50].
Data Analysis:
- Review the variants called by the software and examine the electropherograms before and after noise minimization.
- Pay attention to review indicators set up by the software that highlight potential minor variants [50].
- Confirm minor variants on both forward and reverse strands to validate findings [50].
Integrating MVF with NGS Validation Workflows
In high-throughput labs using NGS technology, MVF provides a cost-effective method to confirm NGS findings. The software facilitates visualization of confirmation data in alignment views and Venn diagrams for comprehensive reporting [50]. This is particularly important given that Sanger validation of NGS-detected variants remains mandatory in many clinical diagnostics due to factors producing false-positive/negative NGS data [15].
Table 2: Comparison of Variant Detection Platforms
| Parameter | NGS | Traditional Sanger | Sanger with MVF |
|---|---|---|---|
| Detection Limit | Varies (0.025%-1% with specialized callers) [51] | ~15-20% | 5% [50] |
| Cost-effectiveness | Lower for large target numbers | Higher for limited targets | Cost-effective for limited targets [50] |
| Turnaround Time | Days to weeks | Same day [50] | Same day [50] |
| Throughput | High | Moderate | Moderate |
| Confirmatory Capability | Primary discovery | Gold-standard validation | Enhanced validation for low-frequency variants |
Troubleshooting Guides
Common Data Quality Issues and Solutions
Problem 1: Failed Sequencing Reactions (Sequence data contains mostly N's)
- Identification: The trace is messy with no discernable peaks [16].
- Possible Causes and Solutions:
- Low template concentration: Ensure template concentrations are between 100-200 ng/μL. Use instruments like NanoDrop designed for accurate measurement of small quantities [16].
- Poor quality DNA: Verify 260/280 OD ratio is 1.8 or greater. Clean up DNA to remove excess salts, contaminants, and PCR primers [16].
- Too much DNA: Excessive template DNA can kill a sequencing reaction - dilute to recommended concentration [16].
- Bad primer or incorrect primer: Use high-quality primer with confirmed priming site location on the template strand [16].
Problem 2: Chromatograms show excessive noise along trace baseline
- Identification: Trace has discernable peaks but with high background noise interfering with base calling [16].
- Possible Causes and Solutions:
- Low signal intensity: Optimize template concentration to 100-200 ng/μL range [16].
- Poor primer binding efficiency: Verify primer quality, ensure it's not degraded, and check for large n-1 population [16].
- Incomplete background noise neutralization: Ensure control sample is properly prepared and sequenced using identical conditions as test samples [50].
Problem 3: Good quality data that suddenly terminates
- Identification: Sequence begins with high quality then suddenly stops or signal intensity drops dramatically [16].
- Possible Causes and Solutions:
MVF Software-Specific Issues
Problem: Inconsistent minor variant calls between forward and reverse strands
- Solution: Ensure both forward and reverse reactions for each sample are properly input into the software. The software is designed to detect variants on both strands to confirm findings [50]. If inconsistencies persist, check sequencing quality for both directions and resequence if necessary.
Problem: Failure to achieve 5% detection sensitivity
- Solution: Verify that control and test samples were prepared and sequenced using identical materials and procedures. Even minor deviations can affect the software's ability to properly neutralize background noise [50].
Frequently Asked Questions (FAQs)
Q1: What is the minimum variant frequency detectable by Minor Variant Finder Software? The software can detect minor variants at frequencies as low as 5% when optimal conditions are met, including proper control sample preparation and adequate sequencing quality [50].
Q2: How does the background noise neutralization algorithm work? The software uses a control sample sequenced under identical conditions as test samples to establish a background noise profile. This profile is then used to neutralize or subtract the background noise from test samples, enhancing the signal-to-noise ratio for minor variant detection [50].
Q3: Can MVF Software be used to confirm variants detected by NGS? Yes, the software is particularly valuable for confirming NGS findings. It supports visualization of confirmation data in alignment views and Venn diagrams, making it an ideal tool for validating low-frequency variants identified through NGS [50].
Q4: What are the advantages of using Sanger sequencing with MVF over NGS for low-frequency variant detection? Sanger sequencing with MVF offers several advantages: faster turnaround time (same-day results), lower cost for limited targets, and no change to existing Sanger workflows. It is particularly beneficial for oncology and pathology research labs where the number of relevant targets is often limited [50].
Q5: Why is it critical to use the same materials and procedures for control and test samples? Using identical materials and procedures ensures that the background noise profile in the control sample accurately represents the technical noise in test samples. This allows the software to effectively distinguish true biological variants from technical artifacts [50].
Q6: What should I do if the software identifies a potential minor variant but the electropherogram appears noisy? The software includes review indicators to flag potential minor variants that may require manual inspection. If the electropherogram remains noisy after processing, consider resequencing the sample, ensuring optimal template concentration and quality, and verifying that the control sample was properly prepared [50] [16].
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Minor Variant Analysis
| Reagent/Material | Function/Application | Considerations |
|---|---|---|
| High-Quality Control DNA | Wild-type reference for background noise neutralization | Must be prepared and sequenced identically to test samples |
| KB Basecaller (v1.4+) | Basecalling of .ab1 files | Required for compatibility with MVF Software [50] |
| Optimized Sequencing Primers | Amplification of target regions | Should have high binding efficiency; avoid self-complementarity to prevent dimer formation [16] |
| PCR Purification Kits | Removal of contaminants and excess primers | Critical for reducing background noise in sequencing reactions [16] |
| Template DNA (100-200 ng/μL) | Sequencing substrate | Concentration critical for optimal signal intensity [16] |
Advanced Applications and Integration
The Minor Variant Finder Software enables sensitive detection of low-frequency variants in scenarios where NGS may be impractical or cost-prohibitive. Its ability to confirm NGS findings provides a critical validation step, especially in clinical research settings where accuracy is paramount [50]. This is particularly relevant given that Sanger sequencing validation of NGS-detected variants remains mandatory in routine diagnostics due to the paucity of internationally accepted regulatory guidelines providing specified NGS quality metrics [15].
For comprehensive variant analysis, researchers can integrate MVF with other Sanger sequencing software tools such as:
- SeqScape Software: For resequencing applications, mutation detection, and analysis [52]
- Variant Reporter Software: For reference-based and non-reference-based analysis [52]
- Variant Analysis Module: For automated retrieval of reference sequences and variant reporting in VCF format [52]
The software represents a strategic tool in the expanding genetic analysis toolbox, bridging the gap between traditional Sanger sequencing and modern NGS approaches for reliable detection of low-frequency variants in research and drug development.
Navigating Challenges: Troubleshooting and Optimizing Your Validation Assays
Troubleshooting Guides
Sanger Sequencing Troubleshooting
This section addresses common issues encountered with Sanger sequencing, a key technology for validating Next-Generation Sequencing (NGS) findings.
Table 1: Common Sanger Sequencing Problems and Solutions
| Problem | How to Identify | Possible Cause | Solution |
|---|---|---|---|
| Failed Reaction [16] | Trace is messy with no discernable peaks; data contains mostly "N"s. | - Low template concentration/depth [16] [53]- Poor DNA quality/purity [16] [53]- Bad primer- Instrument failure | - Ensure template concentration is 100-200 ng/µL [16]- Check DNA purity (OD 260/280 ≥1.8) [16]- Use high-quality primer- Request core facility rerun |
| High Background Noise [16] | Discernable peaks with high background noise; low quality scores. | - Low signal intensity- Poor amplification- Low primer binding efficiency | - Optimize template concentration [16]- Check primer design and quality [16] |
| Sequence Termination [16] | Good quality data ends abruptly; signal intensity drops. | - Secondary structures (e.g., hairpins)- Long homopolymer stretches [16] | - Use "difficult template" chemistry [16]- Design primer after or facing the structure [16] |
| Double Sequence [16] | Single, high-quality trace becomes mixed (two or more peaks per location). | - Colony contamination (multiple clones) [16]- Toxic sequence in vector [16] | - Sequence single colony [16]- Use low-copy vector or grow cells at 30°C [16] |
| Mixed Sequence from Start [16] | Two or more peaks from the beginning; many "N"s in text. | - Multiple templates/primers [16]- Multiple priming sites [16]- Incomplete PCR cleanup [16] | - Use single template and primer per reaction [16]- Verify unique priming site [16]- Purify PCR product thoroughly [16] |
| Early Termination [16] | Sequence starts strong but dies out prematurely; high initial signal. | - Too much template DNA [16] | - Reduce template concentration to 100-200 ng/µL [16] |
| Poor Peak Resolution [16] | Peaks are broad and blobby, not sharp and distinct. | - Unknown contaminant in DNA [16] | - Try alternative DNA cleanup method [16] |
NGS Assay Failure Troubleshooting
While NGS is a powerful tool, assay failures can occur. Understanding the root causes is essential for robust validation workflows.
Table 2: NGS Failure Analysis and Prevention Strategies [53]
| Failure Category | Frequency | Key Associated Factors | Preventive Strategies |
|---|---|---|---|
| Insufficient Tissue (INST) | 65% of failures | - Site of biopsy (SOB)- Type of biopsy (TOB)- Clinical setting (initial vs. recurrence)- Age of specimen & tumor viability | - Ensure adequate tissue at acquisition (≥2mm)- Prefer excisional or core biopsies- Consider specimen age |
| Insufficient DNA (INS-DNA) | 28.9% of failures | - DNA yield <100 ng [53]- Site/Type of biopsy- Number of cores- DNA purity & degradation | - Obtain multiple cores during biopsy- Use fluorometry (Qubit) for accurate DNA quantification [53] |
| Failed Library (FL) | 6.1% of failures | - DNA purity & degradation [53]- Type of biopsy | - Assess DNA purity (Nanodrop) and degradation (gel) [53]- Use high-quality, intact DNA |
Frequently Asked Questions (FAQs)
1. Why is my Sanger sequencing data noisy or unreadable, especially at the beginning? This is often due to primer dimer formation, where the primer self-hybridizes. The trace becomes clean further downstream. To fix this, analyze your primer sequence using online tools to ensure it is unlikely to form dimers and redesign if necessary [16].
2. My NGS results are inconsistent between runs. How can I improve reproducibility? Inconsistency often stems from assay drift. To prevent this:
- Use proper truth set reference materials that are highly characterized and have lot-to-lot reproducibility, rather than relying on homebrew cell lines or remnant samples [54].
- Ensure your QC materials reflect the breadth of variant types (SNVs, InDels, CNVs) in your assay [54].
- Implement liquid handling automation to minimize variability in library preparation, a major source of inconsistency [55].
3. I am getting a "double sequence" in my Sanger chromatogram. What does this mean? A double sequence (two or more peaks at the same position) indicates a mixed template. This can be caused by accidentally picking more than one bacterial colony, sequencing a toxic DNA sequence that causes rearrangements in E. coli, or having more than one priming site on your template [16]. Ensure you are sequencing a pure, single clone.
4. What are the most common pre-analytical reasons for NGS failure? Pre-analytical issues, specifically insufficient tissue (INST) and insufficient DNA (INS-DNA), account for about 90% of all failed clinical NGS cases [53]. Factors like the clinical setting of the biopsy, the type and site of the biopsy, and the number of cores taken are major predictors of success [53].
5. Why might a variant called by NGS not validate by Sanger sequencing? While NGS is highly accurate, discrepancies can occur. Sometimes, the error is not in the NGS call but in the Sanger validation process. Allelic dropout (ADO) during PCR or Sanger sequencing can occur, often due to a private single-nucleotide polymorphism (SNP) under the primer-binding site, preventing amplification of one allele. Always check your Sanger primer sequences for known SNPs [15].
Experimental Protocols
This protocol is used to confirm variants identified through NGS.
- Primer Design: Design flanking intronic primers using an algorithm like Primer3.
- Primer Check: Check primer sequences against an SNP database to avoid allelic dropout.
- PCR Amplification:
- Reaction Mix: Combine 2 µl genomic DNA (~50 ng/µl), 0.5 µl of each primer (10 pmol/µl), 1 µl dNTPs (2.5 mM), and FastStart Taq DNA Polymerase in a 25 µl total volume [15].
- Cycling Conditions: Use standard cycling conditions suitable for the primer pair and template.
- PCR Cleanup: Purify amplicons using a mixture of Exonuclease I and Thermosensitive Alkaline Phosphatase to remove residual primers and dNTPs [15].
- Sanger Sequencing: Sequence the purified PCR product using a BigDye Terminator kit and run on a sequencer (e.g., ABI 3500Dx) [15].
Implement this QC protocol to monitor for assay drift and ensure consistent performance.
- Select Reference Materials: Choose commercial, quantitative reference materials that are highly characterized and cover the variant types (SNVs, InDels, etc.) in your assay.
- Run in Parallel: Include these reference materials alongside patient samples in every sequencing run.
- Track Metrics: Monitor key performance metrics such as variant detection, allele frequency, and coverage.
- Use QC Software: Employ a QC management software (e.g., SeraCare iQ NGS QC Management Software) to track data across time, users, and reagent lots to identify drift [54].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Item | Function | Example/Note |
|---|---|---|
| High-Quality DNA Polymerase | Critical for accurate PCR amplification during library prep or Sanger validation. | Use kits from reputable manufacturers (e.g., Roche, Thermo Fisher). |
| QC Reference Materials | Multiplexed controls with known variants to monitor NGS assay performance and drift [54]. | SeraCare offers materials manufactured under ISO/cGMP [54]. |
| DNA Quantitation Tools | Accurately measure DNA concentration and quality before sequencing. | Use fluorometry (Qubit) for concentration and Nanodrop for purity (260/280 ratio) [16] [53]. |
| PCR Purification Kits | Remove salts, enzymes, and primers after amplification to prevent Sanger sequencing failures [16]. | Many commercial kits available (e.g., Qiagen, Thermo Fisher). |
| "Difficult Template" Chemistry | Specialized dye chemistry (e.g., from ABI) to help sequence through secondary structures [16]. | Often costs more than standard chemistry [16]. |
| Automated Liquid Handler | Automates pipetting in NGS library prep to improve consistency and reduce human error [55]. | DISPENDIX's I.DOT Liquid Handler is one example [55]. |
Strategies for Sequencing Difficult Genomic Regions (GC-rich, Repetitive)
FAQs: Understanding Sequencing Challenges in Mutation Validation
Q1: What makes a genomic region "difficult" to sequence, and why is this a critical issue in validating mutant alleles?
Genomic regions are considered "difficult to sequence" when their inherent biochemical properties cause premature termination, misincorporation, or ambiguous mapping of sequencing reads. This is particularly critical for validating mutant alleles because false positives or negatives can directly impact research conclusions and clinical diagnostics. The primary challenging contexts are:
- GC-Rich Regions: DNA with high GC-content (typically >60%) can form stable secondary structures that prevent the polymerase from processing through the template efficiently [56]. This often results in rapid signal deterioration or abrupt stops in the sequence data [56].
- Repetitive Regions: Sequences such as homopolymers (e.g., a run of 'A's), short tandem repeats, or longer interspersed elements (e.g., Alu repeats) are problematic [57]. For Sanger sequencing, the polymerase tends to dissociate from the template [56]. In NGS, these repeats create ambiguities in aligning short reads to a unique genomic location, complicating variant calling and assembly [57].
- Homopolymeric Regions: A specific class of repeats involving consecutive identical bases (e.g., poly-A tails). The polymerase can "stutter" during synthesis, leading to imprecise incorporation and a wave-like pattern in the chromatogram downstream of the region [56].
Q2: When validating NGS-derived variants, is orthogonal Sanger sequencing always necessary?
While Sanger sequencing has been the historical gold standard for orthogonal validation of NGS variants, recent large-scale studies suggest its routine use may have limited utility. One systematic evaluation of over 5,800 NGS-derived variants found a validation rate of 99.965% using Sanger sequencing [20]. The study concluded that a single round of Sanger sequencing is more likely to incorrectly refute a true positive NGS variant than to correctly identify a false positive. Best practices are evolving, and the necessity of Sanger confirmation may depend on the specific NGS assay's quality metrics, the genomic context of the variant, and the application (e.g., clinical vs. research) [20].
Q3: How do the challenges of sequencing GC-rich and repetitive regions differ between Sanger and NGS methods?
The fundamental challenges stem from the same biochemical properties, but they manifest differently due to the technologies' underlying principles.
Table: Challenge Comparison Between Sanger and NGS
| Sequencing Challenge | Manifestation in Sanger Sequencing | Manifestation in NGS |
|---|---|---|
| GC-Rich Regions | Rapid signal strength decline; abrupt stops in sequencing trace [56]. | Under-representation in sequencing libraries due to biased PCR amplification; uneven coverage [58]. |
| Repetitive Regions | Loss of signal as polymerase dissociates from template [56]. | Ambiguous alignment of short reads, causing misassembly and difficulties in variant discovery [57]. |
| Homopolymeric Regions "Stutter" effect seen as overlapping peaks downstream of the homopolymer [56]. | Incorrect determination of the number of bases, leading to insertion/deletion errors [59]. |
Troubleshooting Guides & Experimental Protocols
Guide 1: Troubleshooting Sanger Sequencing of Difficult Templates
Problem: Rapid signal loss or abrupt stops in the chromatogram, often associated with high GC-content.
- Potential Cause: Stable secondary structures (hairpins) in the template DNA that the sequencing polymerase cannot melt through [56].
- Solutions:
- Use Specialized Reagents: Employ proprietary protocols and reagent kits specifically designed for difficult templates [60]. These often contain additives or specialized polymerases that help denature secondary structures.
- Increase Denaturing Temperature: Optimize the cycle sequencing protocol by increasing the denaturation temperature.
- Utilize DMSO or Betaine: Add DMSO (dimethyl sulfoxide) or betaine to the sequencing reaction to lower the melting temperature of DNA and disrupt secondary structures [28].
Problem: "Stutter" or a wave-like pattern of mixed bases following a homopolymer region (e.g., a poly-A tract).
- Potential Cause: The dissociation and re-association of the DNA polymerase as it processes through the repetitive stretch [56].
- Solutions:
- Sequence from Both Directions: Design primers to sequence the same region from the opposite strand. The stutter effect is often strand-specific, and data from the other side may be clear.
- Use Anchored Primers: For templates with long homopolymer tracts like poly-A tails, use a mixture of oligo-dT primers that are "anchored" with one or two specific nucleotides (e.g., C, A, or G) at the 3' end to provide a defined binding site [28].
Problem: Low signal intensity or failure across the entire read.
- Potential Cause: The sequencing primer may be binding to multiple sites on the template, or the template itself may have a complex secondary structure.
- Solutions:
- Redesign Primers: Verify the primer sequence for specificity and avoid regions of self-complementarity. Design primers to bind in a unique, non-repetitive region.
- Check Template Quality: Ensure the DNA template is pure and of sufficient quality. Re-purify the template if necessary [28].
- Optimize Template-to-Primer Ratio: Follow recommended guidelines for template and primer amounts. For example, for a 500-1000 bp PCR product, 5-20 ng is typically used [28].
Guide 2: Addressing NGS Challenges in Difficult Regions
Problem: Low or uneven coverage in GC-rich regions, leading to gaps in variant calling.
- Potential Cause: GC bias during library amplification, where both very high-GC and very high-AT fragments are under-represented in the final sequenced library [58]. This is largely attributed to PCR amplification efficiency being influenced by GC content [58].
- Solutions:
- Optimize Library Preparation: Use PCR-free library preparation protocols to entirely avoid amplification bias [59].
- Employ Specialized Polymerases: Use polymerases and buffer systems specifically formulated to handle a wide range of GC content.
- Bioinformatic Correction: Apply bioinformatic tools to correct for GC bias in the data. One method involves modeling the relationship between fragment count and GC content and using this model to normalize coverage [58].
Problem: Ambiguous alignment and false variant calls in repetitive regions.
- Potential Cause: Short NGS reads (e.g., 50-150 bp) cannot be uniquely mapped to a single location in the genome if they originate from repetitive elements [57].
- Solutions:
- Use Longer Reads: Utilize long-read sequencing technologies like PacBio Single-Molecule Real-Time (SMRT) sequencing or Oxford Nanopore sequencing, which can generate reads spanning thousands of bases, enough to cover entire repetitive elements and anchor on unique flanking sequences [59].
- Adjust Bioinformatics Parameters: Use alignment software that is designed to handle repeats and can report multiple mapping locations. For variant calling, adjust parameters to be more stringent in repetitive regions, potentially requiring higher read depths [57].
- Paired-End Sequencing: Use paired-end sequencing strategies. The additional information from the two ends of a fragment provides a larger "footprint" that can often be uniquely mapped even if one read falls within a repeat [57].
Workflow: A Strategic Approach to Difficult Regions
The following diagram summarizes a recommended strategic workflow for tackling difficult genomic regions, integrating both laboratory and computational methods.
Strategic Workflow for Difficult Genomic Regions
Research Reagent Solutions
Table: Essential Reagents for Sequencing Difficult Regions
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Specialized Polymerase Kits | Engineered enzymes resistant to secondary structures; often include additives like DMSO. | Sanger sequencing through GC-rich hairpins [60]. |
| PCR-Free NGS Kits | Library prep protocols that eliminate PCR amplification, thereby removing GC bias. | Achieving even coverage across genomic regions with extreme GC content [59]. |
| Long-Read Sequencing Kits | Reagents for platforms like PacBio SMRT or Oxford Nanopore that generate multi-kilobase reads. | Resolving complex structural variants and spanning long repetitive elements [59]. |
| Anchored Homopolymer Primers | Oligo-dT primers with defined 3' anchors (e.g., VN). | Sequencing through long poly-A tails without stutter [28]. |
| GC Bias Correction Software | Bioinformatics tools that model and normalize coverage based on GC content. | Correcting for under-representation of GC-rich exons in DNA-seq data [58]. |
Frequently Asked Questions
What are the main sources of error that limit the detection of low-frequency variants? The primary sources of error are the high background error rate of standard NGS technologies (approximately 0.26%–1.78% per base, which is much higher than Sanger sequencing's 0.001%) and errors introduced during sample preparation, particularly during PCR amplification [17]. These errors can manifest as base misincorporations and allelic frequency skewing [17].
What is the typical detection limit of standard NGS, and what is needed for detecting rare variants? Standard Illumina NGS technologies can report variant allele frequencies (VAFs) as low as 0.5% per nucleotide [61]. However, detecting rarer precursor events, such as somatic mutations in normal tissues or minimal residual disease (MRD) in cancer, requires methods that can detect VAFs in the range of 10⁻⁶ to 10⁻⁴ (0.0001% to 0.01%) or even lower [61] [62].
How can I determine if a detected low-frequency variant is a true positive? Sequencing alone cannot directly distinguish between a single mutation that has clonally expanded and multiple independent mutation events at the same site [61]. It is essential to use methods that employ molecular barcodes (Unique Molecular Tags, UMTs) to track original DNA molecules and bioinformatic filters to eliminate artifacts [63]. Furthermore, independent validation using a different method (e.g., digital PCR) is often required for confirmation [32].
My NGS library yield is low. What could be the cause? Low library yield can result from several factors in the preparation process [7]:
- Poor input quality: Degraded DNA/RNA or contaminants (e.g., phenol, salts) can inhibit enzymes.
- Inaccurate quantification: Overestimation of input DNA using absorbance methods (e.g., NanoDrop) can lead to suboptimal reaction conditions.
- Fragmentation or ligation inefficiency: Over- or under-fragmentation and poor ligase performance can reduce adapter incorporation.
- Overly aggressive purification: Incorrect bead-to-sample ratios during cleanup can lead to significant sample loss [7].
Experimental Protocols for Enhanced Detection
The following optimized protocols are designed to overcome the limitations of standard NGS for detecting low-frequency variants.
Protocol 1: Molecular Barcoding and Bioinformatics Filtering (eVIDENCE Method)
This protocol outlines a method for identifying low-frequency variants in cell-free DNA (cfDNA) with high specificity [63].
- Library Preparation: Use a molecular barcoding kit (e.g., ThruPLEX Tag-seq). This step ligates unique molecular tags (UMTs) and stem sequences to both ends of each DNA molecule [63].
- Targeted Capture: Hybridize the library to a custom panel targeting your genes of interest [63].
- Sequencing and Primary Data Processing: Sequence the library and map reads to the reference genome. Use software (e.g., Connor) to generate consensus sequences from reads that share the same UMT (forming a "UMT family") [63].
- Bioinformatic Filtering with eVIDENCE: Apply a two-step filtering process [63]:
- Remove UMT and Stem Sequences: Reprocess the BAM files to soft-clip the UMT and stem sequences from the reads. This prevents artificial mismatches at the read ends from being interpreted as variants.
- UMT Family Consolidation: For each candidate variant, examine all reads within a UMT family. Discard the candidate if any UMT family contains two or more reads that do not support the variant call. This ensures that a variant is only called if it is present in the original DNA molecule before amplification.
Validation: This method was successfully validated on an artificial library with known variants at 0.25-1.5% VAF and on cfDNA from hepatocellular carcinoma patients, achieving reliable detection of variants with VAFs as low as 0.2% [63].
Protocol 2: Optimized Targeted Sequencing for MRD Detection
This protocol focuses on optimizing wet-lab conditions to push the detection limit for single nucleotide variants (SNVs) on an Ion Torrent PGM system [62].
- DNA Polymerase Selection: A key optimization is the use of high-fidelity, proofreading DNA polymerases during PCR. This significantly reduces G>A and C>T transition errors, which are a major source of noise [62].
- Library Preparation and Sequencing: Prepare libraries using optimized conditions and sequence on the chosen platform.
- Data Analysis and Site-Specific Cut-offs: Analyze the data with an understanding of the transition vs. transversion bias (a 3.57:1 ratio was observed). This bias means that the theoretical detection limit can vary for different mutation types. Therefore, site-specific cut-offs for variant calling should be established [62].
Performance: Using this optimized approach, researchers reliably detected a JAK2 gene mutation (c.1849G>T) with VAFs in the range of 0.01% to 0.0015% [62].
Data Presentation: Method Comparison and Performance
The table below summarizes the detection limits and key characteristics of different sequencing approaches for low-frequency variants.
| Method / Technology | Reported Detection Limit (VAF) | Key Principle | Best For |
|---|---|---|---|
| Standard Illumina NGS | ~ 0.5% [61] | Standard sequencing-by-synthesis | Routine variant detection in high-purity samples |
| Optimized Targeted NGS (Protocol 2) | 0.01% - 0.0015% [62] | Wet-lab optimization (e.g., proofreading enzymes) | Detecting known, specific low-frequency SNVs |
| eVIDENCE with Molecular Barcoding | ≥ 0.2% [63] | UMT-based error correction & bioinformatic filtering | Detecting unknown low-frequency variants in cfDNA |
| Ultrasensitive Methods (e.g., Duplex Seq, SaferSeq) | As low as 10⁻⁵ per nucleotide [61] | Parent-strand consensus sequencing from both DNA strands | Research applications requiring the highest sensitivity (e.g., mutation frequency in normal tissues) |
Quantitative Error Analysis: The following table breaks down the error rates of various NGS platforms, highlighting why standard methods are insufficient for ultra-rare variants.
| Sequencing Platform | Typical Base Substitution Error Rate | Common Error Types |
|---|---|---|
| Sanger Sequencing | 0.001% [17] | N/A |
| Illumina | 0.26% - 0.8% [17] | Substitutions in AT-rich/CG-rich regions [17] |
| SOLiD | ~ 0.06% [17] | Lower due to dual-base encoding |
| Ion Torrent | ~ 1.78% [17] | Homopolymer errors [17] |
| Roche/454 | ~ 1% [17] | Homopolymers >6-8 bp [17] |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in the Workflow |
|---|---|
| Molecular Barcoding Kits (e.g., ThruPLEX Tag-seq) | Tags each original DNA molecule with a unique identifier to track and eliminate PCR/sequencing errors [63]. |
| High-Fidelity/Proofreading DNA Polymerases | Reduces errors introduced during PCR amplification, specifically mitigating G>A and C>T transitions [62]. |
| Human Cot DNA | Used in hybridization capture to block repetitive genomic sequences, improving on-target efficiency [64]. |
| Streptavidin Beads | Binds to biotinylated capture probes during hybrid capture-based target enrichment [64]. |
| xGen Hybridization and Wash Kit | A commercial solution providing optimized reagents for the hybridization and post-capture washing steps [64]. |
Workflow Visualization
The following diagram illustrates the logical workflow for developing and validating an NGS assay for low-frequency variants, based on professional guidelines [32] and the methodologies described above.
Diagram 1: Assay development and validation workflow for low-frequency variants.
The diagram below details the molecular barcoding and consensus sequencing process, a cornerstone of ultrasensitive NGS methods [61] [63].
Diagram 2: Molecular barcoding and consensus sequencing workflow.
Managing Bioinformatics Bottlenecks and Data Storage Challenges
Troubleshooting Guides
FAQ: NGS and Sanger Validation
1. When is Sanger sequencing required to validate NGS variants, and when can it be skipped? Sanger sequencing is traditionally considered the gold standard for validating variants found by Next-Generation Sequencing (NGS). However, for "high-quality" NGS variants, orthogonal Sanger confirmation may not be necessary, saving significant time and cost. You can establish quality thresholds to identify these high-confidence variants [65] [66].
- When Sanger validation might be skipped: For Whole Genome Sequencing (WGS) data, variants with a sequencing depth (DP) ≥ 15, an allele frequency (AF) ≥ 0.25, and a caller-dependent quality score (QUAL) ≥ 100 showed 100% concordance with Sanger sequencing in one study. Applying these caller-agnostic thresholds (DP and AF) reduced the number of variants requiring validation to only 4.8% of the initial set [66].
- When Sanger validation is recommended: Variants falling below established quality thresholds for depth, allele frequency, or quality scores should be validated. Sanger is also typically used for confirming critical findings, such as key mutations in a clinical report [65].
2. Our NGS pipeline is producing unexpected variant calls. What are the first steps to diagnose the issue? Unexpected variants often stem from data quality issues or tool configuration problems [67].
- Check Data Quality: Start by running quality control tools like FastQC on your raw sequence data. Look for issues like adapter contamination, low Phred scores, or unusual GC content [67] [68].
- Verify Alignment Metrics: Use tools like SAMtools to check alignment rates. Low rates could indicate contamination, poor sequencing quality, or an incorrect reference genome [67] [68].
- Inspect Variant Quality Scores: Filter your variant call format (VCF) file based on quality scores. For example, a low QUAL score may indicate a false positive. Always consult the documentation for your specific variant caller (e.g., GATK) for best practices on filtering [67] [66].
- Confirm Tool Versions and Dependencies: Ensure you are using consistent and up-to-date versions of all software and that all dependencies are correctly installed. Containerization (e.g., Docker, Singularity) can prevent compatibility issues [67] [69].
3. We are struggling with the cost and scalability of storing large NGS datasets. What are our options? The massive volume of genomic data requires a strategic approach to storage [70] [69].
- Adopt a Tiered Storage Strategy: Not all data needs to be on expensive, high-performance storage. Implement a data lifecycle management policy:
- Active/High-Performance Storage: For data currently being analyzed.
- Cloud/Object Storage: For archived data that is infrequently accessed but must be kept (e.g., AWS S3, Google Cloud Storage).
- Cold Storage: For long-term backup of raw data, which is the cheapest option but has slower retrieval times [69].
- Use Data Compression: Convert large BAM files to the more efficient CRAM format. Use specialized genomic data compression tools to reduce footprint without losing information [69].
- Consider a Hybrid or Cloud Model: Cloud platforms (AWS, Google Cloud, Azure) offer scalable storage and can integrate with bioinformatics platforms that orchestrate computation, allowing you to bring the analysis to the data [70] [69].
4. How can we ensure our bioinformatics analyses are reproducible? Reproducibility is a cornerstone of scientific integrity and is achievable through automation and documentation [67] [69].
- Use Workflow Management Systems: Platforms like Nextflow, Snakemake, or Galaxy standardize your pipelines. They ensure that the same software versions and parameters are used every time a workflow is run, creating a portable and reproducible analysis environment [67] [69].
- Implement Version Control: Use Git to track changes to all your custom scripts and pipeline code. This creates an audit trail and allows you to revert to previous states [67].
- Containerize Software: Package your analysis tools and their dependencies into containers (e.g., Docker, Singularity). This eliminates the "it works on my machine" problem and guarantees a consistent software environment across different systems [69].
- Document Everything: Maintain detailed records of pipeline configurations, tool versions, parameters, and key decisions. Modern bioinformatics platforms can automatically capture this provenance data, creating an immutable audit trail for every analysis run [69] [68].
Experimental Protocol: Validating an NGS-Based Oncopanel
This protocol outlines the steps for developing and validating a targeted NGS gene panel for somatic mutation profiling in solid tumours, based on a recent study [71].
1. Panel Design and Sample Preparation
- Objective: Design a custom hybrid capture panel targeting 61 cancer-associated genes.
- Sample Types: Use a variety of samples for validation, including:
- Clinical Formalin-Fixed Paraffin-Embedded (FFPE) tissue specimens.
- External Quality Assessment (EQA) samples.
- Commercial reference controls (e.g., HD701).
- Input Material: Extract DNA from samples. The protocol validated ≥50 ng of DNA as the minimum input for reliable library preparation [71].
2. Library Preparation and Sequencing
- Library Prep: Use a hybridization-capture-based library preparation kit (e.g., from Sophia Genetics) compatible with an automated system (e.g., MGI SP-100RS) to minimize human error and ensure consistency.
- Sequencing: Perform sequencing on a platform such as the MGI DNBSEQ-G50RS using a sequencing-by-synthesis chemistry. Aim for a high molecular coverage, with >98% of target regions covered at ≥100x [71].
3. Data Analysis and Quality Control
- Primary Analysis: Use the instrument software for base calling and demultiplexing.
- Secondary Analysis:
- Alignment: Map reads to a reference genome (e.g., GRCh38).
- Variant Calling: Use a specialized somatic variant caller. The referenced study used Sophia DDM software, which incorporates machine learning for variant analysis.
- Quality Metrics: Ensure the run meets the following thresholds before proceeding [71]:
- >99% of bases with quality ≥ Q20.
- Coverage uniformity of >99%.
- Mean coverage depth of >1000x is achievable.
Table 1: Key Analytical Performance Metrics for a Validated NGS Oncopanel [71]
| Performance Measure | Result | Definition |
|---|---|---|
| Sensitivity | 98.23% | Ability to detect true positive variants |
| Specificity | 99.99% | Ability to exclude true negative variants |
| Precision | 97.14% | Proportion of called variants that are real |
| Accuracy | 99.99% | Overall correctness of the results |
| Limit of Detection | ~3.0% VAF | Lowest variant allele frequency reliably detected |
4. Orthogonal Validation and Reporting
- Validation: Confirm all variants detected by the NGS panel using an orthogonal method, such as Sanger sequencing or a different NGS platform. This step is crucial for verifying the panel's accuracy during its initial validation phase [71].
- Reporting: Integrate with a clinical decision support system (e.g., OncoPortal Plus) to classify somatic variants based on clinical significance and generate final reports. The goal should be to minimize turnaround time, potentially achieving results in as little as 4 days [71].
Workflow Visualization
The following diagram illustrates the logical workflow for managing NGS data, from sequencing to validation, and highlights key decision points to prevent bottlenecks.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for NGS and Validation Experiments
| Item | Function / Explanation |
|---|---|
| Nucleic Acid Stabilizer (e.g., GM tube) | Preserves DNA/RNA in cytology or tissue samples by inhibiting nuclease activity, allowing for non-frozen storage and transport without degradation [72]. |
| Hybridization-Capture Based Library Kit | Used to prepare sequencing libraries by selectively enriching for target genomic regions, making it ideal for focused gene panels [71]. |
| Reference Control DNA (e.g., HD701) | A well-characterized control sample containing known mutations. It is essential for validating assay performance, determining sensitivity, and monitoring reproducibility across sequencing runs [71]. |
| High-Fidelity DNA Polymerase | An enzyme with proofreading activity used in Sanger sequencing and PCR amplification. It reduces base incorporation errors, which is critical for achieving high accuracy [73]. |
| Automated Library Prep System (e.g., MGI SP-100RS) | A robotic system that automates library preparation steps, reducing manual errors, contamination risk, and improving consistency across samples [71]. |
Quality Management Systems (QMS) and Adherence to Regulatory Standards (CLIA)
FAQs: NGS and Sanger Sequencing Validation
1. Is orthogonal Sanger sequencing still necessary for validating every NGS-derived variant?
For clinical reporting, orthogonal confirmation of NGS variants has been the traditional standard. However, evidence from large-scale studies suggests this may not be necessary for all variants. A systematic evaluation of over 5,800 NGS-derived variants found that Sanger sequencing failed to initially validate only 19 variants. Upon re-testing with optimized primers, 17 of these 19 variants were confirmed, indicating the initial Sanger failure was often due to technical issues rather than NGS inaccuracy. The study concluded that a single round of Sanger sequencing is more likely to incorrectly refute a true positive variant than to correctly identify a false positive, with an overall validation rate of 99.965% for NGS variants [20].
2. What are the key performance characteristics to establish during NGS assay validation under CLIA?
CLIA guidelines require laboratories to verify or establish several key performance specifications for their test systems. The Technical Consultant or Laboratory Director is responsible for ensuring the validation procedure is adequate. Essential performance characteristics include [74]:
- Accuracy: The closeness of agreement between a test result and an accepted reference value.
- Precision: The reproducibility of test results, including within-run and between-run precision.
- Reportable Range: The range of values a method can reliably measure.
- Reference Intervals: Normal values for the laboratory's patient population.
- Limit of Detection (LOD): The lowest value at which an analyte can be reliably detected. For example, one validated NGS panel established a minimum detection threshold of 2.9% for both SNVs and INDELs [71].
3. How can our lab reduce the turnaround time for NGS results while maintaining CLIA compliance?
Reducing turnaround time (TAT) is a common challenge. While CLIA does not specify TAT requirements, robust processes are key to efficiency. One study demonstrated that optimizing an in-house NGS workflow could reduce the average TAT from approximately 3 weeks (for outsourced testing) to just 4 days [71]. This was achieved through:
- Process Automation: Using automated library preparation systems to reduce human error and increase consistency [71].
- Streamlined Bioinformatics: Implementing software with machine learning for rapid variant analysis [71].
- Sample Quality: Ensuring high-quality starting material, as cytology specimens preserved in nucleic acid stabilizers can yield high-quality DNA/RNA, with one study reporting a 98.4% success rate in gene panel analysis [75].
4. What are the foundational documentation requirements for CLIA compliance?
CLIA compliance is heavily dependent on comprehensive documentation. Foundational policies and procedures must cover the entire testing process [74]:
- Pre-analytic Systems: SOPs for specimen collection, accessioning, and checking specimen integrity.
- Analytic Systems: SOPs for the testing procedure itself, including instrument calibration, preventative maintenance, and reagent qualification.
- Post-analytic Systems: Procedures for result reporting and storage.
- Personnel Qualifications: Documentation of all staff credentials, training records, and competency assessments.
- Quality Control: Policies for daily, weekly, and monthly equipment maintenance and calibration.
Troubleshooting Guides
Issue: Low or Inconsistent Coverage in NGS Panel
| Possible Cause | Investigation Steps | Potential Solution |
|---|---|---|
| Insufficient DNA Input Quantity/Quality | - Quantify DNA using fluorometry [71].- Check DNA integrity (e.g., DIN, DV200%) [75]. | - Ensure input DNA is ≥ 50 ng [71].- Use specimens with a high ratio of double-stranded DNA [75]. |
| Suboptimal Library Preparation | - Review target enrichment metrics (e.g., percentage of reads on target) [71]. | - Titrate PCR cycles during library amplification.- Use automated library preparation systems for consistency [71]. |
| Sequencing Run Quality | - Check the percentage of bases with quality scores ≥ Q30 [76].- Review cluster density (for Illumina platforms). | - Rebalance library concentrations before loading.- Repeat the sequencing run if quality metrics are out of spec. |
Issue: Discrepant Results Between NGS and Sanger Sequencing
| Scenario | Investigation Steps | Resolution |
|---|---|---|
| Variant called by NGS but not by Sanger | - Verify NGS variant call quality (read depth, base quality, strand bias) [20].- Check if Sanger sequencing primer binds over a polymorphism [20].- Manually inspect Sanger chromatogram for low signal or background noise. | - Re-design Sanger sequencing primers [20].- If NGS quality metrics are high, trust the NGS result. Large-scale studies show NGS is highly accurate [20]. |
| Variant called by Sanger but missed by NGS | - Check NGS alignment in the variant region for gaps or poor mapping. | - Manually review the BAM file in a genome browser.- This is a rare event; ensure the NGS panel covers the specific genomic region. |
Experimental Protocols for Key Validation Experiments
Protocol 1: Determining Limit of Detection (LOD) for an NGS Panel
Purpose: To establish the lowest variant allele frequency (VAF) that can be reliably detected by your NGS assay [71].
Materials:
- Reference standard with known mutations (e.g., HD701 from Horizon Discovery) [71].
- Wild-type genomic DNA.
- Your NGS library prep kit and sequencing platform.
Method:
- Create Dilution Series: Serially dilute the reference standard into wild-type genomic DNA to create a series of samples with expected VAFs (e.g., 10%, 5%, 2.5%, 1%) [71].
- Sequencing: Process each dilution through your entire NGS workflow, including library preparation and sequencing, in multiple replicates.
- Data Analysis: For each known variant in the reference standard, calculate the observed VAF in each dilution.
- Establish LOD: The LOD is the lowest VAF at which the variant is detected with 100% sensitivity (i.e., in all replicates) and with high confidence (high-quality calls) [71]. The study by TTSH established a minimum detected VAF of 2.9% for their panel [71].
Protocol 2: Assessing Assay Precision (Repeatability and Reproducibility)
Purpose: To verify that your NGS assay produces consistent results within a run and between runs [71].
Materials:
- Several unique patient samples or reference standards.
- Your standard NGS reagents.
Method:
- Repeatability (Intra-run Precision):
- Reproducibility (Inter-run Precision):
Data Presentation
Table 1: Key Performance Metrics from a Validated NGS Oncopanel
Performance data from the validation of a 61-gene pan-cancer NGS panel (TTSH-oncopanel) [71].
| Performance Characteristic | Metric | Result |
|---|---|---|
| Sensitivity | Ability to detect true variants | 98.23% |
| Specificity | Ability to identify true negatives | 99.99% |
| Precision/Accuracy | Closeness to true value | 99.99% |
| Repeatability (Intra-run precision) | Consistency within a single run | 99.99% |
| Reproducibility (Inter-run precision) | Consistency between different runs | 99.98% |
| Limit of Detection (LOD) | Lowest reliable VAF for SNVs/INDELs | 2.9% |
Table 2: NGS Validation Reagent Solutions
Essential materials and their functions for establishing a robust NGS validation workflow, as cited in the literature.
| Reagent / Solution | Function / Purpose | Example from Literature |
|---|---|---|
| Reference Control Standards | Provides known mutations for determining LOD, accuracy, and precision [71]. | HD701 (Horizon Discovery) with 13 known mutations [71]. |
| Nucleic Acid Stabilizer | Preserves DNA/RNA in cytology or tissue samples by inhibiting nuclease activity, critical for sample quality [75]. | Ammonium sulfate-based stabilizer (GM tube) used for cytology specimens [75]. |
| Hybridization-Capture Based Library Kit | Enriches for target genomic regions prior to sequencing [71]. | Library kits from Sophia Genetics, used with an automated system (MGI SP-100RS) [71]. |
| Automated Library Preparation System | Reduces human error, contamination risk, and improves consistency in library construction [71]. | MGI SP-100RS system [71]. |
| Bioinformatics Software with Machine Learning | Automates variant calling, filtering, and provides visualization and clinical interpretation [71]. | Sophia DDM software with OncoPortal Plus for tiered classification [71]. |
Workflow and Relationship Visualizations
NGS Validation and CLIA Compliance Workflow
Sanger vs. NGS Validation Decision Pathway
Sanger vs. NGS: A Strategic Comparative Analysis for Validation Efficacy
This technical support center provides focused guidance for researchers validating mutant alleles, a critical step in genomics research and drug development. The choice between Sanger sequencing and Next-Generation Sequencing (NGS) involves careful consideration of accuracy, cost, and turnaround time, each with distinct implications for experimental design and validation protocols. The following guides and FAQs are designed to help you troubleshoot specific issues and select the most appropriate methodology for your research context.
Frequently Asked Questions (FAQs)
1. For validating a single known point mutation in a few samples, which method is more appropriate and why?
Sanger sequencing is the more appropriate and cost-effective method for this task [13]. It provides high-quality data for sequencing single DNA fragments, with typical read lengths up to 1000 bases, and is highly reliable for confirming a specific, known variant [60]. Using NGS for this purpose would be inefficient, as NGS's strength lies in its massively parallel capability, which is not utilized when targeting a single mutation in a low number of samples [13].
2. What are the primary factors that contribute to the longer turnaround time for NGS compared to Sanger sequencing?
The extended turnaround time for NGS is due to its more complex workflow. While the actual sequencing run is parallelized and fast, the required steps for NGS are more involved and time-consuming [77]:
- Library Preparation: NGS requires fragmenting DNA and attaching adapter sequences for millions of fragments, whereas Sanger sequencing prepares a single PCR product per reaction [19].
- Data Analysis: NGS generates terabytes of data requiring sophisticated bioinformatics pipelines for alignment and variant calling, a process that can take days. Sanger sequencing produces straightforward chromatogram data that is analyzed comparatively quickly [77] [19].
- Sequencing Volume: A single Sanger run processes one fragment, while an NGS run sequences millions, requiring more initial setup but ultimately providing more data per run [13].
3. How does the sensitivity of NGS for detecting low-frequency variants impact cancer research?
NGS's higher sensitivity is transformative for cancer research because tumors are often heterogeneous, meaning they contain sub-populations of cells with different mutations [77]. NGS can detect variants with a low variant allele frequency (VAF), with limits of detection reported as low as 1-3% in validated assays, compared to 15-20% for Sanger sequencing [71] [13] [77]. This capability allows researchers and clinicians to:
- Identify rare, resistant subclones within a tumor that may lead to disease recurrence [78].
- Monitor treatment response and emerging resistance mutations through liquid biopsies [77] [19].
- Uncover a more complete mutational landscape of cancer genomes, leading to better understanding of tumorigenesis.
4. What are the key troubleshooting steps for a failed Sanger sequencing reaction from a PCR template?
GENEWIZ Sanger sequencing experts recommend three basic troubleshooting steps to start with [60]:
- Check PCR Product Purity: Ensure your PCR product is a single, specific band on a gel. Contamination with nonspecific products or primer-dimers can cause poor sequencing results.
- Perform PCR Clean-up: Effectively purify the PCR product to remove excess primers, dNTPs, and enzyme, which can interfere with the sequencing reaction.
- Verify Concentration: Use a reliable method (e.g., fluorometry) to accurately quantify the DNA template before submission. Too much or too little template DNA is a common cause of failure.
5. When should I consider using a targeted NGS panel instead of a whole genome approach for validating mutant alleles in solid tumors?
Targeted NGS panels are specifically designed for efficient mutation profiling in cancer [71]. You should consider a targeted panel when:
- Your research focuses on a defined set of genes with known clinical or biological relevance in a specific solid tumor type.
- You have limited DNA input, often the case with Formalin-Fixed Paraffin-Embedded (FFPE) tissue samples, as panels require less input than whole genome sequencing (WGS).
- You need a faster, more cost-effective solution with deeper sequencing coverage (higher read depth) over your genes of interest, which increases sensitivity for detecting low-frequency variants [71] [77]. WGS spreads sequencing coverage thinly across the entire genome, resulting in lower depth at any specific locus.
Quantitative Comparison Tables
The following tables summarize the core performance metrics of Sanger sequencing and NGS to aid in experimental planning.
Table 1: Accuracy and Technical Specifications
| Aspect | Sanger Sequencing | Next-Generation Sequencing (NGS) |
|---|---|---|
| Typical Read Length | Long (500-1000 base pairs) [60] [19] | Short (50-600 bp) to Ultra-long (100,000+ bp) [77] [19] |
| Sensitivity (Limit of Detection) | ~15-20% variant allele frequency [13] [77] | High (down to ~1-3% for low-frequency variants) [71] [13] [77] |
| Variant Detection Capability | Ideal for single nucleotide variants (SNVs), small indels | Single-base resolution; detects SNPs, indels, CNVs, and large structural variants [77] |
| Data Output | Single DNA fragment per run [13] | Massively parallel; millions of fragments per run [13] [77] |
Table 2: Cost and Turnaround Time
| Aspect | Sanger Sequencing | Next-Generation Sequencing (NGS) |
|---|---|---|
| Cost-Effectiveness | Cost-effective for sequencing 1-20 targets [13] | Cost-effective for high sample volumes and many targets [13] |
| Typical In-house Turnaround Time | Same-day or overnight services available [60] | ~4 days for targeted panels to over a week for whole genomes [71] [77] |
| Send-out Turnaround Time | N/A (Typically an in-house service) | 14 to 28 days for external services [79] |
| Example Instrument Cost | Varies by platform (e.g., Illumina, MGI, Ultima) [80] [81] |
Experimental Protocols
Protocol 1: Sanger Sequencing for Mutant Validation from Purified Plasmid DNA
This protocol is adapted from standard GENEWIZ guidelines for purified templates [60].
Principle: Cycle sequencing using dye-terminator chemistry, followed by capillary electrophoresis to separate and detect the terminated fragments.
Materials:
- Purified plasmid DNA containing the mutant allele.
- Sequence-specific primer designed to bind ~50-100 bp upstream of the mutation.
- PCR tubes, thermal cycler, and standard molecular biology reagents.
Method:
- Template Preparation: Dilute purified plasmid DNA to a concentration of 25-50 ng/µL in nuclease-free water or TE buffer. Verify concentration via spectrophotometry (e.g., Nanodrop).
- Reaction Setup: In a PCR tube, combine:
- 1-5 µL of template DNA (50-100 ng total for plasmid)
- 1 µL of sequencing primer (5-10 µM stock)
- 4 µL of ready-to-use sequencing mix (BigDye Terminator)
- Add nuclease-free water to a final volume of 10-20 µL.
- Cycle Sequencing:
- Initial Denaturation: 96°C for 1 minute.
- 25-35 Cycles of:
- Denaturation: 96°C for 10 seconds.
- Annealing: 50°C for 5 seconds.
- Extension: 60°C for 4 minutes.
- Purification: Remove unincorporated dye-terminators using a column-based purification kit or ethanol precipitation.
- Capillary Electrophoresis: Submit the purified product for analysis on a sequencer. Data is output as a chromatogram (.ab1 file) for analysis.
Protocol 2: Targeted NGS for Profiling Mutations in Solid Tumors
This protocol is based on a hybridization-capture method as described for a custom 61-gene oncopanel [71].
Principle: DNA is fragmented, and libraries are prepared with adapters. Target regions are enriched using biotinylated probes, followed by massively parallel sequencing.
Materials:
- FFPE-derived or fresh frozen tumor tissue DNA.
- Targeted gene panel (e.g., Sophia Genetics panel).
- Library preparation kit (e.g., MGI SP-100RS system).
- Bioanalyzer/TapeStation for quality control.
Method:
- DNA Extraction & QC: Extract high-molecular-weight DNA. Quantify using a fluorometric method (e.g., Qubit). Input requirement is typically ≥ 50 ng [71].
- Library Preparation:
- Fragmentation & End-Repair: Mechanically or enzymatically shear DNA to a desired size (e.g., 200-300 bp). Repair ends to be blunt.
- Adapter Ligation: Ligate platform-specific adapter sequences to the fragment ends. These allow binding to the flow cell and contain sample index barcodes for multiplexing.
- Target Enrichment (Hybridization-Capture):
- Hybridization: Incubate the library with biotinylated oligonucleotide probes that are complementary to your target genes.
- Capture & Wash: Bind the probe-library hybrids to streptavidin-coated magnetic beads. Wash away non-specific, non-hybridized DNA.
- Amplification: Perform a PCR to amplify the captured library.
- Sequencing:
- Pool (multiplex) multiple barcoded libraries.
- Load onto the sequencer (e.g., MGI DNBSEQ-G50RS, Illumina MiSeq).
- Perform sequencing-by-synthesis.
- Bioinformatic Analysis:
- Demultiplexing: Assign reads to individual samples based on barcodes.
- Alignment: Map sequencing reads to a reference genome (e.g., hg38).
- Variant Calling: Use specialized software (e.g., Sophia DDM) to identify SNPs and indels against the reference. A typical report includes variant allele frequency (VAF) and coverage depth.
Workflow and Decision Diagrams
Sanger Sequencing Workflow
NGS Library Prep Workflow
Method Selection Guide
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Sequencing Experiments
| Item | Function | Application Notes |
|---|---|---|
| Dye-Terminator Kits | Contains fluorescently labeled dideoxynucleotides (ddNTPs) that terminate DNA synthesis during the sequencing reaction. | Core chemistry for Sanger sequencing. Kits are available from various suppliers (e.g., Thermo Fisher). |
| Sequence-Specific Primers | Short oligonucleotides that bind to a specific region of the DNA template to initiate the sequencing reaction. | For Sanger, design primers with a Tm of ~50-60°C, located 50-100 bp upstream of the region of interest. |
| Library Prep Kit | A collection of enzymes and buffers for converting a sample of DNA into a sequencing-ready library. | NGS essential. Kits are often platform-specific (e.g., Illumina, MGI). Includes enzymes for end-repair, A-tailing, and ligation. |
| Targeted Gene Panels | A predefined set of probes (e.g., biotinylated oligos) designed to capture and enrich specific genomic regions of interest. | For targeted NGS. Allows focused sequencing on genes relevant to cancer, inherited disease, etc. [71]. |
| Sample Indexes (Barcodes) | Short, unique DNA sequences ligated to each library, allowing multiple samples to be pooled and sequenced in a single run. | Critical for NGS multiplexing, drastically reducing cost per sample. |
| Bioinformatics Pipelines | Software for processing raw sequencing data, including demultiplexing, alignment, variant calling, and annotation. | Essential for NGS data analysis. Examples include BWA, GATK, and commercial software like Sophia DDM [71]. |
The choice between Next-Generation Sequencing (NGS) and Sanger sequencing is fundamentally determined by the required sensitivity for detecting genetic variants. Sanger sequencing operates with a limit of detection (LoD) of approximately 15-20% variant allele frequency (VAF), meaning a mutant allele must be present in at least 15-20% of the sequenced DNA molecules to be reliably detected [13] [82]. In contrast, NGS can confidently identify variants at frequencies as low as 1-5% VAF, and with specialized methods like Unique Molecular Identifiers (UMIs) or Blocker Displacement Amplification, this sensitivity can extend to 0.1% VAF [13] [83]. This order-of-magnitude difference in sensitivity dictates their applications: Sanger is ideal for confirming known, high-frequency variants, while NGS is essential for discovering novel or low-frequency mutations, as in tumor heterogeneity studies or early detection of drug-resistant viral populations.
Sensitivity Data Comparison Table
The quantitative differences in performance between Sanger and NGS sequencing are summarized in the table below.
Table 1: Key Performance Metrics for Sanger and NGS
| Parameter | Sanger Sequencing | Standard NGS (e.g., Whole Exome) | Ultra-Deep NGS (with UMIs) |
|---|---|---|---|
| Typical Limit of Detection (VAF) | 15-20% [13] [82] | 1-5% [13] [83] | 0.1-0.5% [83] |
| Typical Sequencing Depth | N/A (Single fragment) | 100x - 1,000x [83] | 35,000x or higher [83] |
| Throughput | Low (One fragment per reaction) [13] | High (Millions of fragments simultaneously) [13] | High (Millions of fragments simultaneously) |
| Best Use Case | Validating known variants in a small number of samples [13] [37] | Discovering novel variants and screening many genes/samples [13] | Detecting ultra-rare variants in liquid biopsies or for resistance mutation profiling [83] |
Experimental Protocol: Orthogonal Confirmation of Low-Frequency NGS Variants
Routine Sanger sequencing cannot directly confirm variants below its 15-20% LoD. This protocol describes an orthogonal method using Blocker Displacement Amplification (BDA) prior to Sanger sequencing to validate putative variants identified by NGS at VAFs ≤5% [83].
The following diagram illustrates the multi-step process for confirming low-frequency variants.
Step-by-Step Methodology
Candidate Variant Selection & BDA Assay Design
- From your NGS data (e.g., whole exome sequencing), select putative variants with VAFs between 0.5% and 5% that require confirmation [83].
- Use a specialized software platform (e.g., NGSure from NuProbe) to algorithmically design the BDA oligonucleotides. The assay requires:
- Forward and Reverse Primers: Flank the variant of interest.
- Blocker Oligo: A wildtype-specific oligonucleotide that binds to the sequence overlapping the variant site. It is modified at the 3'-end to prevent polymerase extension, thereby selectively inhibiting the amplification of wildtype sequences [83].
BDA qPCR Enrichment
- Set up two qPCR reactions for each sample and variant:
- Reaction with Blocker (BDA): Contains primers and the wildtype-specific blocker.
- Reaction without Blocker (Control): Contains only primers for total input DNA quantification.
- Use a SYBR Green master mix with 400 nM primers, 4 µM blocker, and 10 ng of sample DNA per well.
- Run qPCR with the following cycling conditions [83]:
- Initial Denaturation: 95°C for 3 minutes.
- 45 Cycles of:
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 60°C for 1 minute.
- Analytical Validation: Before testing samples, validate each BDA assay using a synthetic positive control (100% VAF) and a wildtype genomic DNA negative control (0% VAF). A valid assay will show a Cq difference of >10 cycles between the positive and negative controls [83].
- Set up two qPCR reactions for each sample and variant:
Sanger Sequencing and Analysis
- Purify the BDA qPCR product.
- Perform standard Sanger sequencing using the same forward or reverse primer from the BDA assay.
- Analyze the chromatogram. Successful enrichment will show a clear, distinct peak at the variant position, allowing for definitive confirmation or disconfirmation of the original NGS call [83].
Research Reagent Solutions
The following table lists key reagents and their critical functions for the BDA confirmation protocol and general sequencing workflows.
Table 2: Essential Reagents for Low-Frequency Variant Confirmation
| Reagent / Tool | Function / Application |
|---|---|
| BDA Oligos (Primers & Blocker) | Selectively enriches low-frequency variant alleles by suppressing wildtype amplification during PCR [83]. |
| Sanger Sequencing Reagents | Provides the "gold standard" for orthogonal confirmation of variants after enrichment [37]. |
| NGS Library Prep Kits | Prepares DNA samples for massively parallel sequencing on platforms like Illumina MiSeq or HiSeq [7] [84]. |
| DNA Repair Mix (e.g., NEBNext) | Crucial for working with suboptimal samples like FFPE tissue, which often contains damaged DNA [83]. |
| High-Fidelity DNA Polymerase | Essential for both NGS library prep and BDA qPCR to minimize introduction of errors during amplification [7]. |
| Bioanalyzer / TapeStation | Provides quality control (QC) for assessing DNA integrity and final library fragment size distribution [7] [83]. |
| Fluorometric Quantifier (e.g., Qubit) | Accurately quantifies DNA and library concentration, which is critical for achieving optimal sequencing performance [7]. |
Frequently Asked Questions (FAQs)
1. Is Sanger validation still necessary for all NGS-called variants? Growing evidence suggests that routine Sanger validation for every NGS variant has limited utility, especially when NGS data is of high quality with high-depth coverage. Large-scale studies have shown NGS validation rates can exceed 99.9%, and a single round of Sanger is more likely to incorrectly refute a true positive than to correctly identify a false positive [20]. Best practices are shifting towards using Sanger selectively, such as for confirming clinically actionable variants or those with low quality scores.
2. My NGS library yield is low. What are the most common causes? Low library yield is a frequent issue in NGS workflows. The primary causes and fixes are [7]:
- Poor Input DNA Quality: Degraded DNA or contaminants (phenol, salts) inhibit enzymes. Fix: Re-purify input sample, check purity ratios (260/230 >1.8).
- Inaccurate Quantification: UV absorbance (NanoDrop) overestimates concentration. Fix: Use fluorometric methods (Qubit).
- Inefficient Fragmentation/Ligation: Over- or under-shearing DNA, suboptimal adapter ratios. Fix: Optimize fragmentation parameters, titrate adapter concentration.
- Overly Aggressive Purification: Sample loss during clean-up steps. Fix: Optimize bead-to-sample ratios, avoid over-drying beads.
3. My Sanger chromatogram is noisy or has overlapping peaks. How can I fix this?
- Double Peaks (Overlapping Sequences): Indicates clone contamination or a heterozygous template. Fix: Re-plate bacterial clones or redesign PCR primers [85].
- High Background Noise: Can be caused by contaminated template or improper PCR purification. Fix: Check purification protocol, ensure thorough removal of salts and primers [85].
- Sequence Deterioration/Early Stop: Often due to secondary structures (e.g., high GC content) or salt impurities. Fix: Use a desalting kit to purify the template and consider sequencing from the opposite strand [85].
4. For HIV-1 drug resistance testing, what threshold should I use for NGS to match Sanger's results? A multi-laboratory comparison found that using a 20% threshold for reporting low-abundance variants (LAVs) in NGS generated consensus sequences that were most similar (>99.6% identity) to those from Sanger sequencing. Lower thresholds (5%, 10%, 15%) introduced significant differences and reduced inter-laboratory consistency [84]. For backward compatibility with existing Sanger-based data, a 20% threshold is currently recommended.
In the era of next-generation sequencing (NGS), researchers and drug development professionals face a critical methodological decision: whether to validate NGS-detected variants using the traditional gold standard of Sanger sequencing. This decision has significant implications for project timelines, costs, and resource allocation. The core thesis is that project scale serves as the primary deciding factor in this cost-benefit analysis. While Sanger validation provides orthogonal confirmation, emerging evidence suggests it has limited utility for high-quality NGS variants, with large-scale studies demonstrating validation rates exceeding 99.9% [20]. This technical support center provides evidence-based guidance and troubleshooting to optimize your validation strategy based on project-specific parameters.
FAQs: Addressing Core Technical Questions
Q1: What does current evidence say about the necessity of Sanger validation for all NGS variants?
Large-scale systematic evaluations demonstrate that Sanger validation has limited utility for high-quality NGS variants. A landmark study comparing over 5,800 NGS-derived variants against Sanger sequencing data found only 19 were not initially validated by Sanger. Upon re-testing with newly designed primers, 17 of these were confirmed as true positives, while the remaining two had low-quality scores from exome sequencing [20]. This resulted in an overall validation rate of 99.965%, higher than many established medical tests that don't require orthogonal validation [20]. The study concluded that a single round of Sanger sequencing is more likely to incorrectly refute a true positive NGS variant than to correctly identify a false positive [20].
Q2: In which specific scenarios does Sanger validation remain essential?
Sanger validation remains methodologically essential in these specific scenarios:
- Clinical diagnostics where single-gene variant confirmation has direct patient implications [37]
- Low-quality NGS calls with poor sequencing depth or quality scores [20]
- Regulatory requirements for diagnostic test validation [32]
- Borderline variant quality parameters where NGS data is ambiguous [38]
- Orthogonal confirmation for novel, high-impact discoveries
Understanding error profiles helps target validation efforts effectively [86]:
- Sample handling artifacts: C>A/G>T errors often derive from oxidative damage during sample processing
- PCR enrichment errors: Target-enrichment PCR causes approximately 6-fold increase in overall error rate
- Sequence context errors: C>T/G>A errors show strong sequence context dependency
- Base calling errors: Vary by substitution type, ranging from 10⁻⁵ for A>C/T>G changes to 10⁻⁴ for A>G/T>C changes [86]
- Mapping artifacts in complex genomic regions
Q4: What methodological considerations support moving away from universal Sanger validation?
The paradigm shift is supported by several methodological considerations:
- Resource allocation: Sanger validation consumes significant time and resources that could be allocated to additional NGS experiments [20]
- Error comparison: Modern NGS demonstrates accuracy comparable to or exceeding Sanger sequencing in controlled studies [38]
- Quality metrics: Established quality thresholds (e.g., Phred score ≥30, coverage depth ≥30×) reliably identify high-confidence variants [38]
- Complementary technologies: Emerging computational error suppression techniques can reduce substitution error rates to 10⁻⁵ to 10⁻⁴ [86]
Quantitative Analysis: Comparing Validation Approaches
Table 1: Methodological Comparison of Sequencing Validation Approaches
| Parameter | Universal Sanger Validation | Targeted Sanger Validation | No Sanger Validation |
|---|---|---|---|
| Validation Rate | >99.9% [20] | Focused on at-risk variants | Dependent on NGS quality controls |
| Cost Implications | High (reagent, labor, time) | Moderate | Low |
| Time Requirements | Significant (additional workflow) | Reduced | Minimal |
| Best Application | Regulatory clinical diagnostics; low-throughput studies | Research studies with specific quality concerns; medium-scale projects | Large-scale research studies; high-quality NGS data |
| Risk Profile | Lowest false positive rate | Moderate risk | Requires robust NGS QC |
Table 2: NGS Error Profiles by Substitution Type [86]
| Substitution Type | Error Rate | Primary Source |
|---|---|---|
| A>C / T>G | 10⁻⁵ | Polymerase errors |
| C>A / G>T | 10⁻⁵ | Sample-specific effects (oxidative damage) |
| C>G / G>C | 10⁻⁵ | Polymerase errors |
| A>G / T>C | 10⁻⁴ | PCR enrichment |
| C>T / G>A | 10⁻⁴ (context-dependent) | Spontaneous deamination |
Decision Framework: Project Scale Considerations
The following workflow provides a systematic approach to determining the appropriate validation strategy based on project-specific parameters:
Troubleshooting Guides
NGS-Sanger Discrepancy Resolution
When NGS and Sanger results conflict, follow this systematic troubleshooting protocol:
Step 1: Investigate NGS Data Quality
- Examine base quality scores (Phred ≥30 recommended) [38]
- Verify adequate coverage depth (>30× minimum) [38]
- Check for mapping artifacts or complex genomic regions
- Confirm allele balance (>0.2 recommended) [38]
Step 2: Evaluate Sanger Sequencing Issues
- Primer binding problems: Design new primers avoiding known SNPs in binding regions [38]
- Allelic dropout: Check for variants in primer-binding sites that cause preferential amplification [38]
- Template issues: Verify DNA quality and concentration (100-200 ng/μL recommended) [16]
- Chromatogram interpretation: Manually inspect fluorescence peaks for ambiguous bases [20]
Step 3: Methodological Reconciliation
- Repeat Sanger sequencing with newly designed primers [20]
- Consider alternative polymerases or sequencing chemistries for difficult templates [16]
- Implement computational error suppression methods [86]
- For persistent discrepancies, consider that NGS may be correct and Sanger may be error-prone in specific contexts [38]
Sanger Sequencing Failure Scenarios
Table 3: Common Sanger Sequencing Problems and Solutions [16] [30]
| Problem | Possible Causes | Solutions |
|---|---|---|
| Failed reaction (mostly N's) | Low template concentration; contaminants; bad primer | Verify concentration (100-200 ng/μL); check 260/230 ratio (>1.8); redesign primer |
| Poor data after mononucleotides | Polymerase slippage on homopolymer stretches | Design primer after the region or sequence from reverse direction |
| Good data that stops abruptly | Secondary structures; GC-rich regions | Use difficult template protocols; redesign primers; lower template concentration |
| Double peaks from beginning | Multiple templates; colony contamination; multiple priming sites | Ensure single template; verify primer specificity; improve PCR cleanup |
| Gradual signal deterioration | Excessive template DNA | Dilute template to recommended concentration (100-200 ng/μL) |
| Poor sequence start | Primer dimer formation | Redesign primer to avoid self-complementarity |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Sequencing Validation
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| High-fidelity DNA polymerases (Q5, Kapa) | PCR amplification with minimal errors | Different polymerases show varying error profiles [86] |
| Hybrid capture probes | Target enrichment for NGS | Longer probes tolerate mismatches better than PCR primers [32] |
| Primer design tools (Primer3, Primer-BLAST) | Design optimal sequencing primers | Check for SNPs in primer binding sites [38] |
| Computational error suppression tools | In silico error correction | Can reduce substitution error rates to 10⁻⁵-10⁻⁴ [86] |
| Reference materials (cell lines) | Assay performance evaluation | COLO829/COLO829BL useful for dilution experiments [86] |
Experimental Protocols
Protocol 1: Targeted Sanger Validation for Borderline NGS Variants
Purpose: Orthogonal confirmation of NGS variants with borderline quality metrics or high clinical significance.
Methodology:
- Primer Design
PCR Amplification
- Reaction volume: 25 μL
- Template DNA: 50-100 ng
- Primers: 10 pmol/μL each [38]
- Polymerase: High-fidelity enzyme (e.g., FastStart Taq)
- Cycling conditions: Standard protocol with optimization based on primer Tm
PCR Product Purification
- Use Exonuclease I/Thermosensitive Alkaline Phosphatase mixture [38]
- Alternative: Column-based purification systems
Sequencing Reaction
- Use BigDye Terminator kits [38]
- Follow manufacturer's recommended cycling conditions
- Ethanol precipitation for reaction cleanup
Capillary Electrophoresis
- Run on ABI sequencers (3130xl or similar) [38]
- Standard injection parameters
Data Analysis
- Align sequences to reference genome (e.g., hg19)
- Manual review of chromatograms for variant confirmation [20]
- Compare with NGS variant calls
Protocol 2: Computational Error Suppression for NGS Data
Purpose: Enhance NGS accuracy without Sanger validation for large-scale projects.
Methodology:
- Data Preprocessing
Error Profile Analysis
- Calculate position-specific error rates using flanking sequences known to be devoid of genetic variations [86]
- Evaluate error rates by substitution type
- Identify sample-specific error patterns
Error Suppression
- Implement context-aware error correction algorithms
- Apply sample-specific error adjustments
- Use unique molecular identifiers (UMIs) when available
Validation
- Compare with known variant databases
- Use dilution experiments with cell lines (e.g., COLO829/COLO829BL) to establish detection limits [86]
- Verify with orthogonal methods for subset of variants
Workflow Comparison: Traditional vs. Scale-Optimized Approaches
The following diagram illustrates the key differences in laboratory workflow between traditional and scale-optimized validation approaches:
The decision to implement Sanger validation should be driven by project-specific factors rather than universal mandates. The evidence-based recommendations are:
- Large-scale research studies: Implement rigorous NGS quality controls and computational error suppression without routine Sanger validation [20] [86]
- Medium-scale projects: Use targeted Sanger validation for borderline quality variants only [38]
- Small-scale clinical studies: Maintain traditional Sanger validation for regulatory compliance [32] [37]
- All projects: Establish clear quality metrics (Phred score ≥30, coverage ≥30×, allele balance >0.2) to guide validation decisions [38]
This strategic approach optimizes resource allocation while maintaining scientific rigor, ensuring that validation efforts are proportional to project scale and specific quality requirements.
Frequently Asked Questions (FAQs)
Q1: Why is Sanger sequencing often used to validate variants found by Next-Generation Sequencing (NGS)? Sanger sequencing is considered the "gold standard" for DNA sequencing due to its long read length and high accuracy [31]. It is used to confirm the existence of specific genetic variants, such as single nucleotide variants (SNVs) or small insertions and deletions (indels), initially detected by NGS platforms. This validation step ensures the accuracy and reliability of NGS data, which is critical for clinical decision-making and research [31] [32].
Q2: What are the main limitations of using short reads from NGS? Short reads, typically a few hundred base pairs in length, can struggle with complex genomic regions [31]. These include areas with mononucleotide repeats (e.g., long stretches of a single base), high GC content, or secondary structures that can cause the sequencing polymerase to slip or stall, leading to poor data quality or misassembly [16].
Q3: Is orthogonal Sanger validation always necessary for NGS variants? Not necessarily. Recent large-scale studies have demonstrated that NGS is highly accurate. One study evaluating over 5,800 NGS-derived variants found a validation rate of 99.965% with Sanger sequencing [20]. The study concluded that a single round of Sanger sequencing is more likely to incorrectly refute a true positive NGS variant than to correctly identify a false positive, suggesting that routine validation has limited utility for high-quality NGS data [20].
Q4: What are common issues in Sanger sequencing that can affect validation? Common issues include:
- Failed reactions or noisy data: Often caused by low template DNA concentration, poor DNA quality, or contaminants [16].
- Sequence stops abruptly: Can be caused by secondary structures (e.g., hairpins) in the DNA template that the polymerase cannot pass through [16].
- Mixed sequence (double peaks): Can result from colony contamination (sequencing more than one clone) or the presence of multiple priming sites on the template [16].
Troubleshooting Guides
Guide 1: Troubleshooting Sanger Sequencing for NGS Validation
Use this guide to diagnose and resolve common problems when using Sanger sequencing to confirm NGS results.
| Problem | How to Identify | Possible Cause & Solution |
|---|---|---|
| Failed Reaction | Sequence data contains mostly N's; trace is messy with no discernible peaks [16]. | Cause: Low template DNA concentration or poor quality DNA [16].Solution: Precisely quantify DNA using an instrument like a NanoDrop. Ensure DNA has a 260/280 OD ratio ≥1.8 and is free of contaminants [16]. |
| High Background Noise | Trace has discernible peaks but also significant background noise along the bottom, leading to low-quality scores [16]. | Cause: Low signal intensity, often from poor amplification due to low template concentration or inefficient primer binding [16].Solution: Check and adjust template concentration. Ensure the primer is of high quality, not degraded, and designed for high binding efficiency [16]. |
| Sequence Termination | Good quality data ends abruptly or signal intensity drops dramatically [16]. | Cause: Secondary structures (e.g., hairpins) or long homopolymer stretches (e.g., poly G/C) that block the polymerase [16].Solution: Use an alternate sequencing chemistry designed for "difficult templates" or design a new primer that sits on or just beyond the problematic region [16]. |
| Double Sequence | The trace begins clearly but then shows two or more peaks at each position downstream [16]. | Cause: Colony contamination (sequencing multiple clones) or a toxic DNA sequence causing rearrangements in the host [16].Solution: Ensure only a single colony is picked. For toxic sequences, use a low-copy vector or grow cells at a lower temperature [16]. |
Guide 2: Addressing NGS Short-Read Limitations
This guide helps mitigate challenges inherent to short-read NGS technologies.
| Challenge | Impact on Data | Mitigation Strategy |
|---|---|---|
| Low Coverage Depth | Reduced sensitivity to detect variants, especially heterozygous ones; lower confidence in base calling [20] [32]. | Sequence to a higher average coverage depth. For clinical panels, ensure coverage is sufficient to meet validated sensitivity thresholds for each variant type (e.g., SNVs, indels) [32]. |
| Mapping Ambiguity | Short reads may map to multiple locations in the genome, leading to misalignment and false positive/negative variant calls [31]. | Use sophisticated bioinformatics tools and alignment algorithms. For complex regions, consider long-read sequencing technologies or Sanger sequencing to resolve ambiguity [31]. |
| Difficulty with Indels & Structural Variants | Short reads may not fully span longer insertions, deletions, or breakpoints of structural variants, making them hard to detect accurately [32]. | Utilize specialized bioinformatics pipelines designed for indel and structural variant calling. For gene fusions, consider RNA-based NGS approaches or long-read sequencing [32]. |
Data Presentation
Table 1: Key Performance Metrics from a Large-Scale NGS-Sanger Validation Study
This table summarizes data from a systematic evaluation of Sanger-based validation of NGS variants, illustrating the high accuracy of NGS [20].
| Metric | Value | Context |
|---|---|---|
| NGS Variants Evaluated | >5,800 | From five genes across 684 participant exomes [20]. |
| Initial Validation Rate | 99.67% | 19 of 5,800+ variants were not initially confirmed by Sanger [20]. |
| Final Validation Rate | 99.965% | After re-testing 17 of the 19 discrepancies with newly designed primers, they were confirmed by Sanger. The remaining two had low NGS quality scores [20]. |
| Study Conclusion | Sanger validation has "limited utility" for routine confirmation of NGS variants, as NGS demonstrates higher accuracy than many established medical tests [20]. |
Table 2: Research Reagent Solutions for Sequencing Workflows
Essential materials and reagents used in NGS and Sanger sequencing validation workflows.
| Reagent / Material | Function in the Experiment |
|---|---|
| SureSelect / TruSeq Exome Capture Kits | Solution-hybridization based methods to enrich for exonic regions of the genome prior to NGS library sequencing [20]. |
| BigDye Terminator v3.1 Kit | Fluorescent dye-terminator chemistry used in Sanger sequencing reactions to generate chain-terminated fragments [20]. |
| PCR Purification Kits | For cleaning up PCR products to remove excess salts, enzymes, and primers before Sanger sequencing, which is critical for obtaining high-quality results [16]. |
| NanoDrop Spectrophotometer | Instrument designed to accurately measure the concentration and purity of small-volume nucleic acid samples, crucial for optimizing sequencing reactions [16]. |
Experimental Protocols
Protocol: Sanger Sequencing Validation of NGS-Detected Variants
This is a detailed methodology for confirming NGS variants using Sanger sequencing [20] [31].
Variant Identification by NGS:
Selection of Variants for Confirmation:
- Not all NGS variants require validation. Prioritize variants based on:
- Low quality scores: Variants with coverage depth or genotype quality scores below a predetermined threshold.
- Clinical or research significance: Variants that are critical for downstream analysis or reporting [31].
- Not all NGS variants require validation. Prioritize variants based on:
Primer Design:
- Design PCR and sequencing primers that flank the target variant.
- Use primer design software (e.g., Primer3) to ensure high specificity and efficiency [20].
- Verify that primer binding sites do not contain known polymorphisms that could lead to allele dropout.
PCR Amplification:
- Amplify the genomic region containing the variant using standard PCR protocols with the designed primers.
- Use high-fidelity DNA polymerase to minimize PCR errors.
PCR Product Cleanup:
- Purify the PCR product to remove residual primers, nucleotides, and enzymes. This step is critical for obtaining a clean Sanger sequence [16].
Sanger Sequencing Reaction:
- Set up the sequencing reaction using the purified PCR product as template.
- Use the BigDye Terminator v3.1 sequencing kit according to the manufacturer's instructions [20].
- Perform cycle sequencing.
Sequence Purification and Electrophoresis:
- Purify the sequencing reaction product to remove unincorporated dye terminators.
- Load the product onto a capillary sequencer (e.g., ABI 3130xl) for electrophoresis [20].
Data Analysis and Interpretation:
- Analyze the resulting chromatogram (.ab1 file) using sequence analysis software (e.g., Sequencher).
- Manually inspect the trace file at the variant position to confirm the presence or absence of the NGS-called variant [20].
- Compare the Sanger sequence with the original NGS data to ensure concordance.
Workflow Diagrams
NGS Validation with Sanger Sequencing
In genomic research, particularly in the critical validation of mutant alleles, the debate is no longer about choosing between Next-Generation Sequencing (NGS) and Sanger sequencing. Instead, a powerful hybrid approach that leverages the unique strengths of both technologies has emerged as the gold standard for accuracy and efficiency. NGS provides unparalleled throughput for discovering variants across many genes, while Sanger sequencing offers definitive, base-by-base confirmation of those variants [73] [87]. This technical support guide outlines how to implement this hybrid model effectively, providing troubleshooting and best practices for researchers and drug development professionals focused on validating somatic mutations, such as those in oncology or rare disease research.
FAQs: Implementing a Hybrid Sequencing Workflow
Why is a hybrid model necessary if NGS is already highly accurate?
While modern NGS platforms demonstrate high concordance with Sanger sequencing for high-quality variants, the hybrid model is essential for several specific scenarios [27]:
- Validating Low-Frequency Variants: NGS variant calling at low variant allele frequencies (VAF ≤ 5%) is highly susceptible to false positives from sequencing errors or DNA damage [83]. Sanger sequencing, especially when coupled with pre-enrichment techniques, provides orthogonal confirmation.
- Resolving Ambiguous or Low-Quality NGS Calls: Variants with low depth of coverage, or those located in regions with high sequence complexity (e.g., homopolymers), require verification with a different methodology [27].
- Clinical Reporting Standards: For definitive diagnosis or clinical trial enrollment, many laboratories and regulatory bodies still require confirmation of key mutations by the proven Sanger method, considered the "gold standard" [87] [83].
What is the lowest variant allele frequency (VAF) that Sanger sequencing can confirm?
The standard limit of detection for conventional Sanger sequencing is between 5% and 20% VAF [83]. However, this sensitivity can be dramatically improved to 0.1% VAF or lower by integrating an initial enrichment step using techniques like Blocker Displacement Amplification (BDA) prior to Sanger sequencing [83]. This hybrid enrichment-Sanger approach is particularly valuable for confirming subclonal mutations in tumor samples or mosaic mutations in germline conditions.
Our NGS and Sanger results are discordant. What are the most likely causes?
Discordant results typically arise from pre-analytical or technical issues rather than a failure of either technology. A systematic troubleshooting approach is recommended:
| Potential Cause | Description | Recommended Action |
|---|---|---|
| Primer/PCR Failure | Sanger primer binding site may contain a SNP or variant, leading to preferential amplification or failure. | Redesign Sanger sequencing primers and repeat the assay [27]. |
| Low VAF Variant | The true VAF of the mutation is below Sanger's native detection limit. | Employ an allele enrichment method like BDA before Sanger sequencing [83]. |
| Sample Contamination | Cross-contamination with wildtype DNA can dilute the mutant signal. | Repeat the assay with a freshly prepared sample and include negative controls. |
| Variant in Complex Region | The variant may be located in a homopolymer-rich or highly repetitive region. | Manually inspect the NGS data (BAM files) in a genome browser to assess mapping quality. |
| Tumor Purity | The tumor sample may have a high proportion of normal cells, diluting the mutant allele. | Review histopathology estimates of tumor content and adjust expectations for VAF accordingly. |
When can we discontinue Sanger confirmation of NGS variants?
Sanger confirmation can be safely discontinued for high-quality NGS variants once a laboratory has validated its own NGS wet-lab and bioinformatics workflows. High-quality variants are typically defined as those meeting all the following criteria [27]:
- FILTER = PASS from the variant caller.
- QUAL score ≥ 100.
- Depth of coverage ≥ 20X.
- Variant fraction ≥ 20%.
One large-scale study of 1109 variants from 825 clinical exomes found a 100% concordance between NGS and Sanger for variants meeting similar high-quality standards [27]. It is critical for each lab to perform its own validation before implementing this policy.
Troubleshooting Guides
Issue: Failure to Confirm a Putative NGS Variant with Sanger Sequencing
Problem: A variant called by NGS at a low VAF (e.g., 1-5%) is not visible in the Sanger chromatogram.
Solution:
- Verify NGS Call: Manually inspect the NGS data in a genomic viewer (e.g., IGV). Check for mapping errors, strand bias, or low base quality that might indicate a false positive.
- Employ Allelic Enrichment: Use a method like Blocker Displacement Amplification (BDA) to preferentially amplify the mutant allele before Sanger sequencing [83].
- Principle: BDA uses a wildtype-specific blocker oligonucleotide that inhibits the amplification of the wildtype sequence, thereby enriching the relative fraction of the mutant allele during PCR.
- Procedure:
- Design a BDA assay with a primer set and a wildtype-specific blocker.
- Perform qPCR with and without the blocker to calculate the enrichment factor (ΔCq).
- Proceed with Sanger sequencing on the blocker-treated amplicon.
- Alternative Confirmation: Use an orthogonal quantitative method, such as droplet digital PCR (ddPCR), which is highly sensitive and specific for low-frequency variants [83].
Issue: High False Positive Rate in Low-Frequency NGS Variant Calling
Problem: Many putative variants at VAF < 5% are disconfirmed by orthogonal methods, wasting time and resources.
Solution:
- Implement Computational Error Suppression: Utilize bioinformatics tools that model and subtract context-specific sequencing errors. Studies show this can computationally suppress substitution error rates to 10⁻⁵ to 10⁻⁴ [86].
- Optimize Wet-Lab Protocols: Identify error sources in the workflow.
- Apply a Rigorous Wet-Lab Hybrid Protocol: For complex regions, use long-read sequencing (e.g., PacBio, Oxford Nanopore) for structural context and Sanger sequencing to polish specific regions of interest [73] [88].
- Workflow:
- Step 1: Generate long reads to span repetitive elements and obtain a complete genomic scaffold.
- Step 2: Use high-accuracy short reads (Illumina) for general error correction and variant calling.
- Step 3: For any remaining ambiguous or critical regions (e.g., suspected mutation sites), perform targeted PCR followed by Sanger sequencing for definitive base-by-base resolution [73] [89].
- Workflow:
Experimental Protocols
Protocol 1: Orthogonal Confirmation of Low-Frequency Variants using BDA-Enabled Sanger Sequencing
This protocol is adapted from methods used to confirm variants at ≤5% allele frequency [83].
1. Research Reagent Solutions
| Item | Function |
|---|---|
| High-Fidelity DNA Polymerase | For specific and efficient amplification of the target locus. |
| BDA Oligos (Primers & Blocker) | Wildtype-specific blocker to inhibit wildtype amplification; primers to amplify the target. |
| SYBR Green Master Mix | For qPCR to quantify amplification and enrichment. |
| Sanger Sequencing Reagents | Standard BigDye Terminator kits and capillary electrophoresis reagents. |
2. Methodology
- Step 1: BDA Assay Design. Use specialized software (e.g., NGSure) to design primers and a wildtype-specific blocker oligonucleotide that binds to the variant site and is tailed with a neutral, non-hybridizing sequence to slow its amplification.
- Step 2: Assay Validation. Validate each BDA assay using wildtype genomic DNA (negative control) and a synthetic DNA fragment with the target mutation (positive control). A valid assay should show a ΔCq (Cqno blocker - Cqwith blocker) of >10 in the positive control.
- Step 3: Sample Testing.
- Prepare two qPCR reactions for each sample: one with the full BDA system (primers + blocker) and one with primers only.
- Use 10-50 ng of sample DNA per reaction.
- Run qPCR: 95°C for 180s; 45 cycles of 95°C for 15s, 60°C for 60s.
- Step 4: Sanger Sequencing.
- Purify the PCR product from the BDA reaction (with blocker).
- Perform Sanger sequencing using standard protocols [87].
- Analyze the chromatogram for the presence of the mutant allele. Successful enrichment will make the mutant peak clearly visible.
Protocol 2: Hybrid Sequencing for Complex Region Assembly and Variant Validation
This protocol is useful for resolving mutations in difficult-to-sequence genomic regions, such as those with high GC-content or repeats [73] [88] [89].
1. Research Reagent Solutions
| Item | Function |
|---|---|
| High-Molecular-Weight DNA Kit | To extract intact DNA suitable for long-read sequencing. |
| Long-Range PCR Kit | Optional, for amplifying large target regions. |
| PacBio or ONT Library Prep Kit | For preparing libraries for long-read sequencing. |
| Illumina Library Prep Kit | For preparing high-accuracy short-read libraries. |
2. Methodology
- Step 1: Library Preparation and Sequencing.
- Prepare sequencing libraries for both a long-read platform (PacBio or Oxford Nanopore) and a short-read platform (Illumina) from the same DNA sample.
- Step 2: Hybrid Genome Assembly.
- Use a hybrid assembler (e.g., Unicycler) that integrates the long reads (for scaffold structure) and short reads (for base-pair accuracy) to generate a complete and accurate consensus genome [88].
- Step 3: Variant Calling and Identification.
- Call variants from the hybrid assembly or map short reads to the hybrid assembly to identify putative mutations.
- Step 4: Targeted Sanger Validation.
- For critical variant calls, especially in regions that were initially problematic, design primers flanking the variant based on the hybrid assembly.
- Perform PCR and Sanger sequencing to provide final, unambiguous validation of the mutation [73].
Table 1: Comparative Analysis of Sequencing Technologies in a Hybrid Model
| Feature | Sanger Sequencing | Next-Generation Sequencing (NGS) | Hybrid Sequencing |
|---|---|---|---|
| Read Length | 500 - 1000 bp [73] | 50 - 300 bp (Short-Read) [89] | Combines both |
| Theoretical Single-Base Accuracy | >99.99% (Gold Standard) [73] [87] | ~99.9% (per base) [89] | Leverages highest accuracy of both |
| Effective Limit of Detection (VAF) | Native: 15-20% [83]. With BDA: 0.1% [83] | WES: ~5% [83]. Deep Amplicon: Can be <0.1% [86] | Enables reliable <0.1% VAF confirmation |
| Best Application in Validation | Orthogonal confirmation of specific variants; clinical reporting. | High-throughput discovery of variants across many genes. | Comprehensive and definitive analysis, especially for complex regions/low VAF. |
Table 2: Error Handling Strategies for Ambiguous NGS Data
When NGS data contains ambiguities (e.g., 'N' calls) or low-quality variant calls, the choice of handling strategy impacts the reliability of the final data, particularly for clinical decision-making [90].
| Strategy | Description | Performance & Best Use Case |
|---|---|---|
| Neglection | Discards all sequencing reads that contain ambiguities. | Best performance when errors are random and not systematic. Can lead to data loss if errors are common [90]. |
| Worst-Case Assumption | Assumes the ambiguity represents the nucleotide that would lead to the worst clinical outcome (e.g., drug resistance). | Lowest performance. Leads to overly conservative predictions and should be avoided where possible [90]. |
| Deconvolution (Majority Vote) | Computationally generates all possible sequences from the ambiguity and uses the most common prediction outcome. | Moderate performance. Computationally expensive but reasonable when a large fraction of reads contain ambiguities and neglection is not feasible [90]. |
Conclusion
The validation of mutant alleles remains a critical step for ensuring data integrity in genomic research and clinical diagnostics. A strategic, hybrid approach that leverages the massive discovery power of NGS with the gold-standard accuracy of Sanger sequencing for confirmation provides the most robust framework. Current best practices firmly establish Sanger sequencing as the orthogonal method for validating key NGS findings, a standard underscored by clinical guidelines. Future directions point toward increased automation, the integration of AI and multiomics data, and the development of novel platforms that further blur the lines between discovery and validation. As sequencing technologies continue to evolve at a rapid pace, the fundamental principle of rigorous validation will only grow in importance, ensuring that genomic insights translate into reliable scientific and clinical outcomes.
References
- 1. Next-Generation Sequencing (NGS) | Explore the technology [https://www.illumina.com/science/technology/next-generation-sequencing.html]
- 2. Massive parallel sequencing [https://en.wikipedia.org/wiki/Massive_parallel_sequencing]
- 3. Review of massively parallel DNA sequencing technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC3238019/]
- 4. is no longer always necessary based on... Sanger sequencing [https://www.nature.com/articles/s41598-021-85182-w?error=cookies_not_supported&code=39c2d5b5-50ac-4cc1-96e6-8590e2e89acb]
- 5. Assessment of clinical analytical sensitivity and specificity of... [https://bmcgenomdata.biomedcentral.com/articles/10.1186/1471-2156-14-6]
- 6. of Validation by ngs | ppt sequencing sanger sequencing [https://www.slideshare.net/slideshow/validation-of-ngs-sequencing-by-sanger-sequencing/35512612]
- 7. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 8. NGS Sequencing Support-Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-support/ngs-support-troubleshooting.html]
- 9. Sanger Sequencing: Introduction, Principle, and Protocol [https://www.cd-genomics.com/blog/sanger-sequencing-introduction-principle-and-protocol/]
- 10. Sanger sequencing vs NGS - Integra Biosciences [https://www.integra-biosciences.com/united-states/en/blog/article/sanger-sequencing-vs-ngs]
- 11. Sequencing Depth vs. Coverage: Key Metrics in NGS ... [https://3billion.io/blog/sequencing-depth-vs-coverage]
- 12. Sequencing depth vs. sequencing batching [https://www.ogt.com/resources/ngs-resources-and-support/ngs-resources/sequencing-depth-vs-sequencing-batching/]
- 13. NGS vs Sanger Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-sanger.html]
- 14. Depth of Sequencing Plays a Determining Role in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10049078/]
- 15. Sanger Validation of High-Throughput Sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7738558/]
- 16. Sanger DNA Sequencing: Troubleshooting [https://dnacore.mgh.harvard.edu/new-cgi-bin/site/pages/sequencing_pages/seq_troubleshooting.jsp]
- 17. Methods to improve the accuracy of next-generation sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC9895957/]
- 18. the high-throughput Sanger sequencing analysis pipeline [https://pmc.ncbi.nlm.nih.gov/articles/PMC9710597/]
- 19. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 20. Systematic Evaluation of Sanger Validation of NextGen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4878677/]
- 21. Sanger validation of WGS variants | Scientific Reports [https://www.nature.com/articles/s41598-025-87814-x]
- 22. Methods for the analysis and interpretation for rare variants ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6455968/]
- 23. Long-Read Sequencing and Structural Variant Detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293859/]
- 24. Diagnostic accuracy of next-generation sequencing (NGS) ... [https://link.springer.com/article/10.1007/s12094-025-04040-7]
- 25. Sanger Sequencing vs. Next-Generation Sequencing (NGS) [https://www.genscript.com/gene-news/sanger-sequencing-vs-next-generation-sequencing.html]
- 26. Guidelines for Sanger sequencing and molecular assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7649556/]
- 27. Sanger sequencing is no longer always necessary based ... [https://www.nature.com/articles/s41598-021-85182-w]
- 28. Sanger Sequencing Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/capillary-electrophoresis-applications-support-center/sanger-sequencing-support/sanger-sequencing-support-troubleshooting.html]
- 29. Sanger Sequencing Best Practices - A guide to sample ... [https://genome.center.uconn.edu/cgi-services/sequencing-best-practices-a-guide-to-sample-preparation-and-troubleshooting/]
- 30. Troubleshooting DNA Templates with Sanger Sequencing [https://blog.genewiz.com/troubleshooting-dna-templates-with-sanger-sequencing]
- 31. Sanger Sequencing for Validation of Next-Generation ... [https://www.cd-genomics.com/resource-sanger-sequencing-for-next-generation-sequencing-validation.html]
- 32. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 33. Determination of high-confidence germline genetic variants in ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11889-z]
- 34. Understanding Chromatogram Sanger Sequencing Analysis [https://chromtech.com/blog/understanding-chromatogram-sanger-sequencing-analysis/]
- 35. Orthogonal NGS for High Throughput Clinical Diagnostics [https://www.nature.com/articles/srep24650]
- 36. Next-Generation Sequencers vs. Sanger ... [https://www.labx.com/resources/next-generation-sequencers-vs-sanger-sequencers-key-differences/5597]
- 37. Next-Generation Sequencing Validation [https://www.thermofisher.com/us/en/home/life-science/sequencing/sanger-sequencing/applications/next-generation-sequencing-validation.html]
- 38. Sanger Validation of High-Throughput Sequencing in ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.592588/full]
- 39. Sanger sequencing FAQs [https://www.genewiz.com/public/resources/faqs/faqs-dna-sequencing]
- 40. Sanger Sequencing: primer design [https://www.biotech.cornell.edu/core-facilities-brc/facilities/genomics-facility/qc-troubleshooting/sanger-sequencing-primer-design]
- 41. Designing PCR and Sanger Sequencing Primers [https://www.thermofisher.com/blog/behindthebench/designing-pcr-and-sanger-sequencing-primers-seq-it-out-5/]
- 42. How to Design Primers for DNA Sequencing | Practical Lab ... [https://www.cd-genomics.com/resource-how-to-design-primers-for-dna-sequencing.html]
- 43. Primer designing tool - NCBI - NIH [https://www.ncbi.nlm.nih.gov/tools/primer-blast/]
- 44. Designing highly multiplex PCR primer sets with Simulated ... [https://www.nature.com/articles/s41467-022-29500-4]
- 45. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 46. Current practices and guidelines for clinical next- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4850126/]
- 47. is no longer always necessary based on... Sanger sequencing [https://www.nature.com/articles/s41598-021-85182-w?error=cookies_not_supported]
- 48. Inherited Cancer in the Age of Next-Generation Sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC6030806/]
- 49. Incidental findings from cancer next generation sequencing ... [https://www.nature.com/articles/s41525-021-00224-6]
- 50. Minor Variant Finder Software [https://www.thermofisher.com/us/en/home/life-science/sequencing/sanger-sequencing/sanger-dna-sequencing/sanger-sequencing-data-analysis/minor-variant-finder-software.html]
- 51. Evaluating the performance of low-frequency variant ... [https://www.nature.com/articles/s41598-023-47135-3]
- 52. Sanger Sequencing and Fragment Analysis Software [https://www.thermofisher.com/us/en/home/life-science/sequencing/sanger-sequencing/sanger-dna-sequencing/sanger-sequencing-data-analysis.html]
- 53. Identification of major factors associated with failed clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528718/]
- 54. Prevent Assay Drift In Your Clinical NGS Assay by Avoiding ... [https://blog.seracare.com/ngs/prevent-assay-drift-in-your-clinical-ngs-assay-by-avoiding-2-common-mistakes]
- 55. From Bench to Breakthrough: Streamlining NGS Assay ... [https://dispendix.com/blog/ngs-assay-development-challenges]
- 56. Sanger Sequencing Services | Troubleshooting Guide [https://mugenomicscore.missouri.edu/difficulttemplates.html]
- 57. and next-generation sequencing: computational... Repetitive DNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC3324860/]
- 58. Summarizing and correcting the GC content bias in high- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3378858/]
- 59. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 60. Sanger Sequencing | GENEWIZ from Azenta [https://www.genewiz.com/public/services/sanger-sequencing]
- 61. Next-Generation Sequencing Methodologies To Detect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10843083/]
- 62. An optimized targeted Next-Generation Sequencing ... [https://www.sciencedirect.com/science/article/pii/S2214753517302115]
- 63. eVIDENCE: a practical variant filtering for low-frequency ... [https://www.nature.com/articles/s41598-019-51459-4]
- 64. Protocol tips to boost your NGS target capture success [https://eu.idtdna.com/page/support-and-education/decoded-plus/protocol-tips-to-boost-your-ngs-target-capture-success/]
- 65. of WGS variants Sanger validation [https://pubmed.ncbi.nlm.nih.gov/39881150/]
- 66. of WGS variants | Scientific Reports Sanger validation [https://www.nature.com/articles/s41598-025-87814-x?error=cookies_not_supported&code=0363c999-33a9-4517-8050-5c70d5bf1c5f]
- 67. Bioinformatics Pipeline Troubleshooting [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-troubleshooting]
- 68. Garbage In, Garbage Out: Dealing with Data Errors ... [https://blog.omni-inc.com/blog/garbage-in-garbage-out-dealing-with-data-errors-bioinformatics]
- 69. Bioinformatics Platform: Unlock Insights 2025 [https://lifebit.ai/blog/bioinformatics-platform-best-practices-2025/]
- 70. Bioinformatics Services Market Size to Hit USD 13.66 ... [https://www.precedenceresearch.com/bioinformatics-services-market]
- 71. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 72. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512683/]
- 73. The Future of Sanger Sequencing: Technical Development ... [https://www.cd-genomics.com/blog/sanger-sequencing-technology-innovation/]
- 74. Standard Operating Procedures for CLIA Compliance [https://www.ovation.io/sop-for-clia-compliance/]
- 75. Prospective multicenter validation of a next-generation ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14770-0]
- 76. Integrating next-generation sequencing and artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12127813/]
- 77. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 78. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 79. Evaluation of turnaround times and performance of in- ... [https://pubmed.ncbi.nlm.nih.gov/40328657/]
- 80. Cost of NGS | Comparisons and budget guidance [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/ngs-cost.html]
- 81. The $100 Genome: Where's the Limit? [https://frontlinegenomics.com/the-100-genome-wheres-the-limit/]
- 82. Sanger Sequencing vs. Next-Generation Sequencing (NGS) [https://www.cd-genomics.com/resource-sanger-sequencing-vs-next-generation-sequencing.html]
- 83. Confirming putative variants at ≤ 5% allele frequency ... [https://www.nature.com/articles/s41598-021-91142-1]
- 84. Multi-Laboratory Comparison of Next-Generation to Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7411816/]
- 85. | Coconote Sanger Sequencing Troubleshooting Guide [https://coconote.app/notes/ab3bf942-b03c-4269-8fca-2e226acf11d2]
- 86. Analysis of error profiles in deep next-generation sequencing ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1659-6]
- 87. Sanger Sequencing - Embryo Project Encyclopedia [https://embryo.asu.edu/pages/sanger-sequencing]
- 88. Comparison of long-read sequencing technologies in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6807382/]
- 89. Hybrid Sequencing: The Future of Accurate and Complete ... [https://strandls.com/articles/hybrid-sequencing-the-future-of-accurate-and-complete-genome-assembly/]
- 90. Comparative analyses of error handling strategies for next- ... [https://www.nature.com/articles/s41598-020-62675-8]